Imaging in Stroke A Rational Approach to acute


- Slides: 48
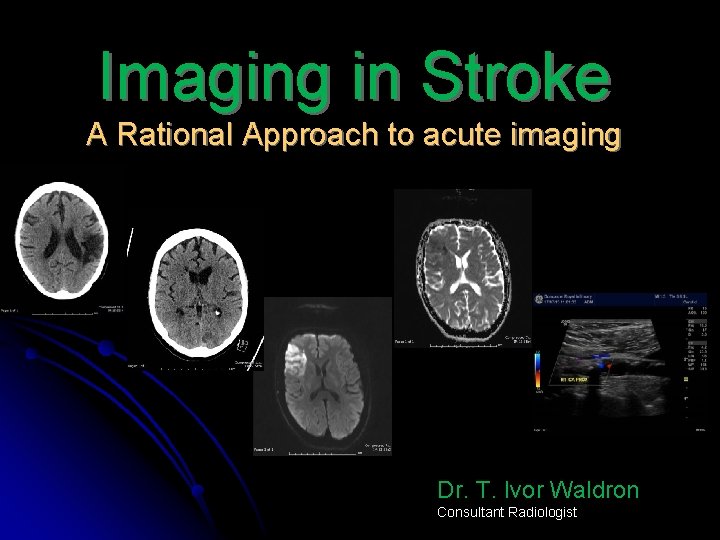
Imaging in Stroke A Rational Approach to acute imaging Dr. T. Ivor Waldron Consultant Radiologist
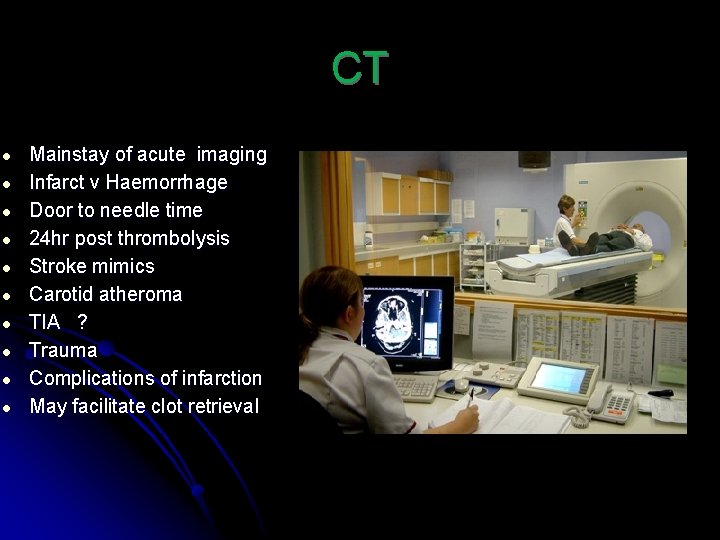
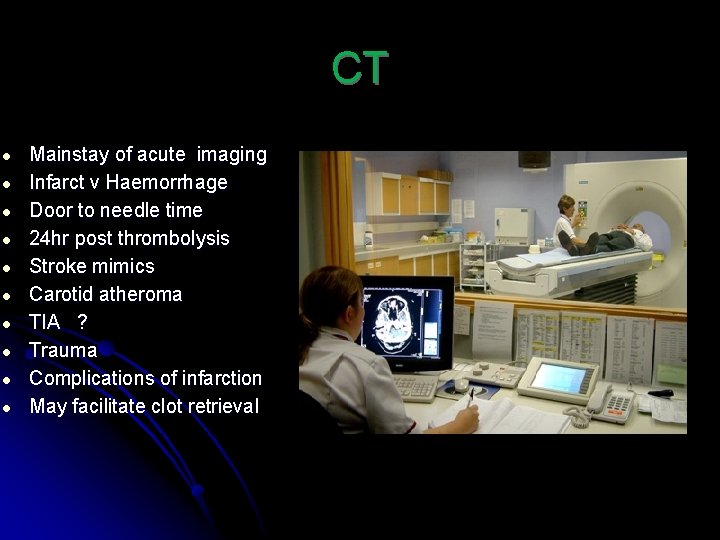
CT ● ● ● ● ● Mainstay of acute imaging Infarct v Haemorrhage Door to needle time 24 hr post thrombolysis Stroke mimics Carotid atheroma TIA ? Trauma Complications of infarction May facilitate clot retrieval
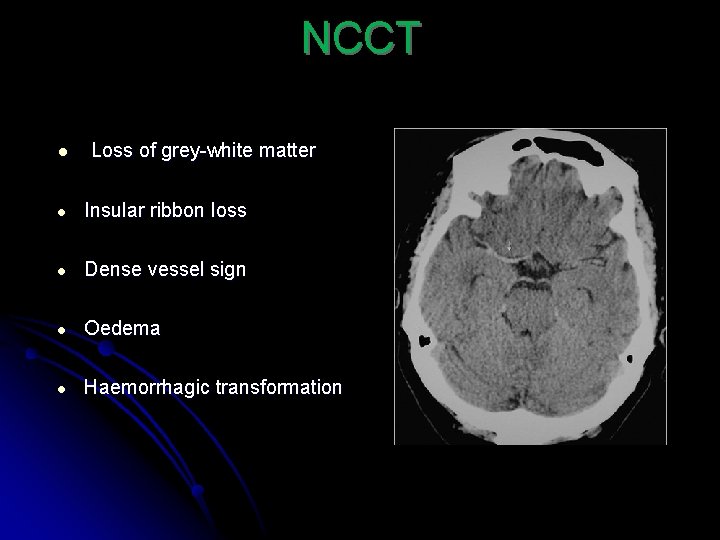
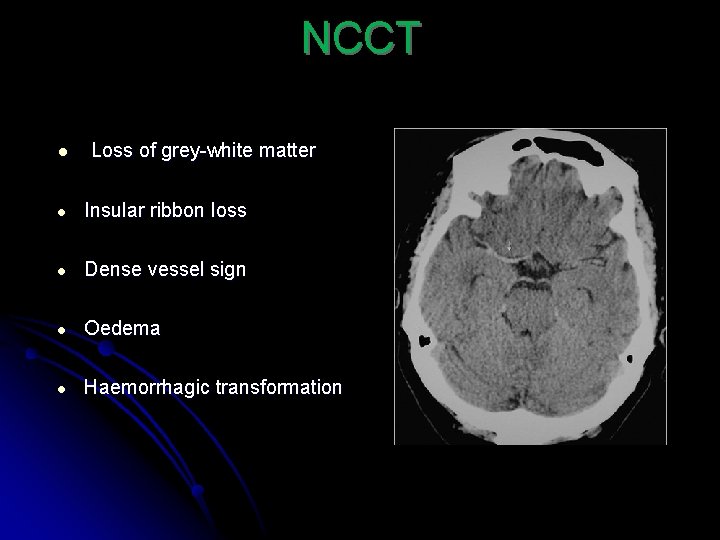
NCCT ● Loss of grey-white matter ● Insular ribbon loss ● Dense vessel sign ● Oedema ● Haemorrhagic transformation
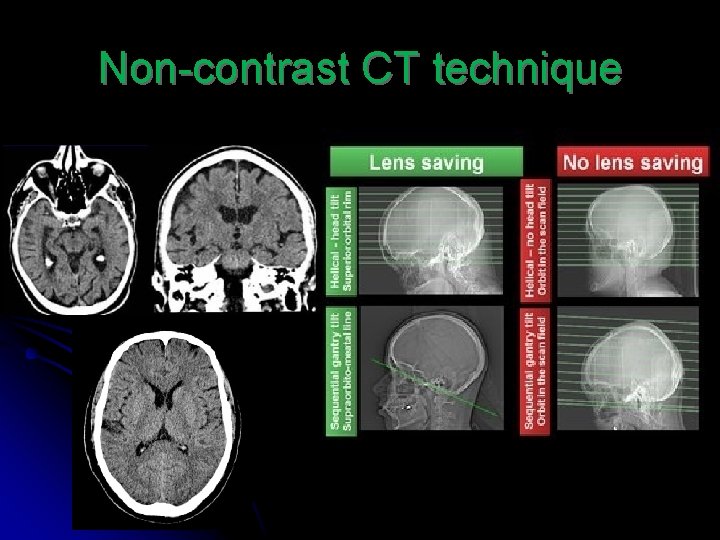
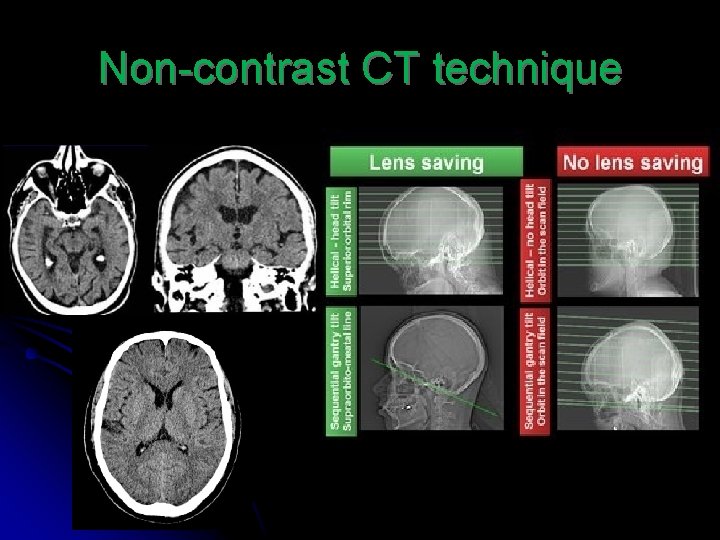
Non-contrast CT technique
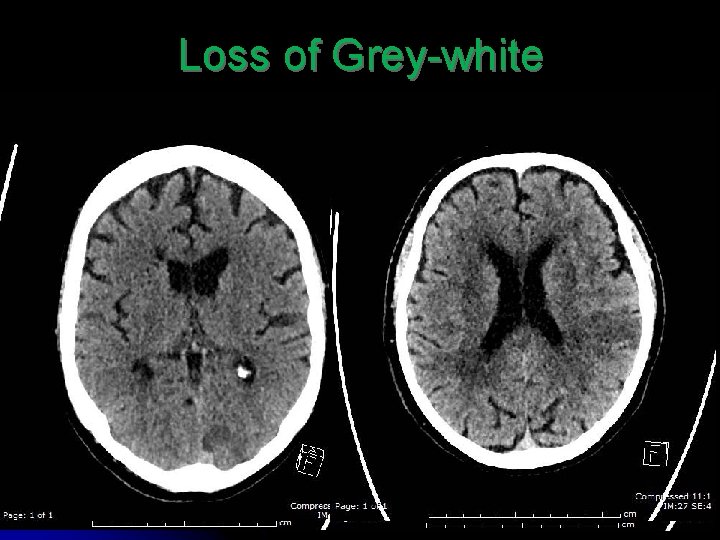
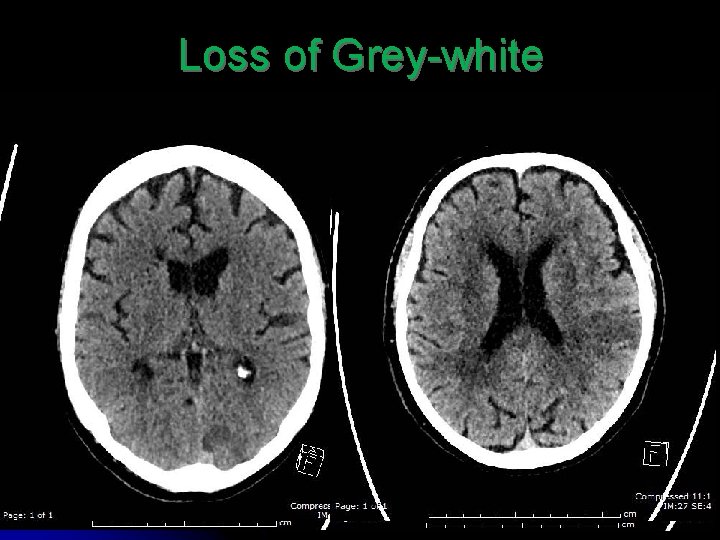
Loss of Grey-white

Loss of Grey-white Insular ribbon sign
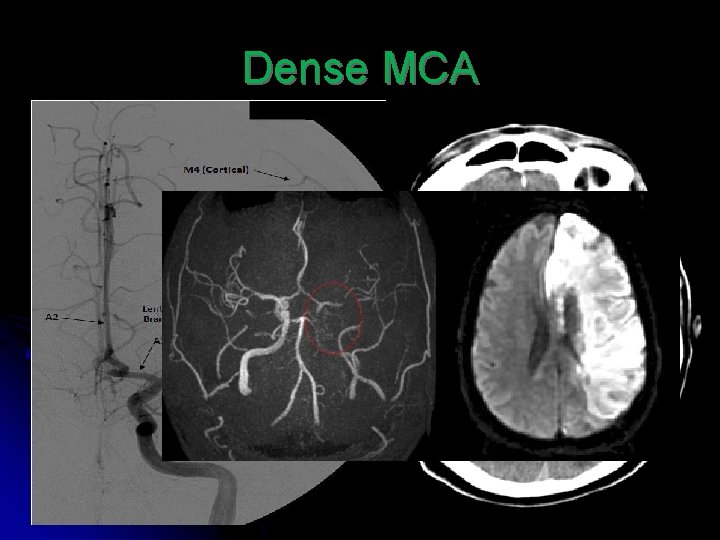
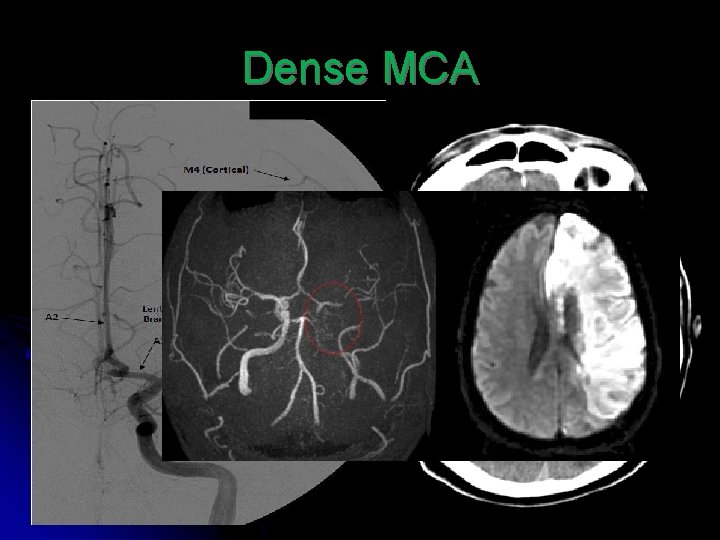
Dense MCA
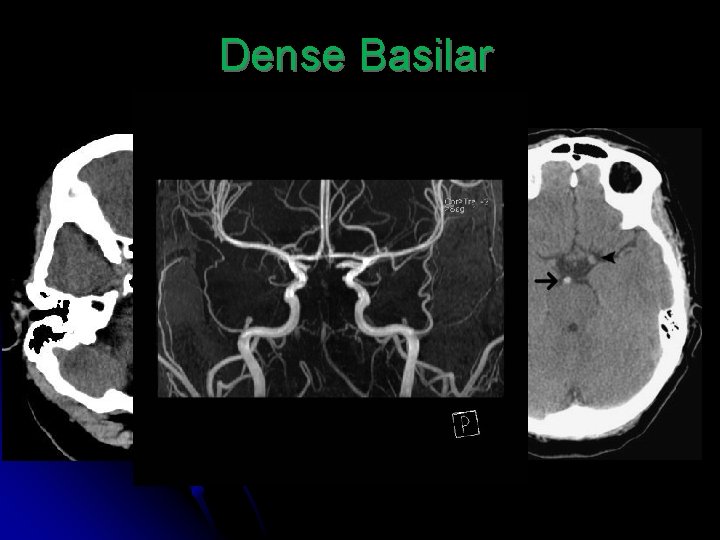
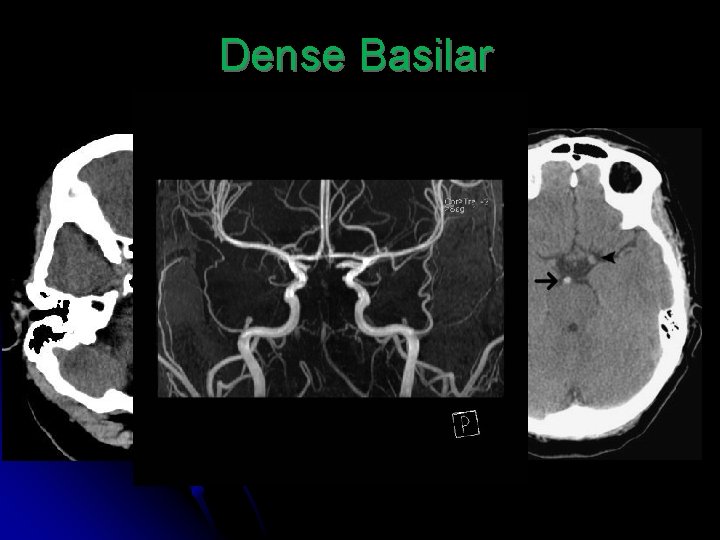
Dense Basilar
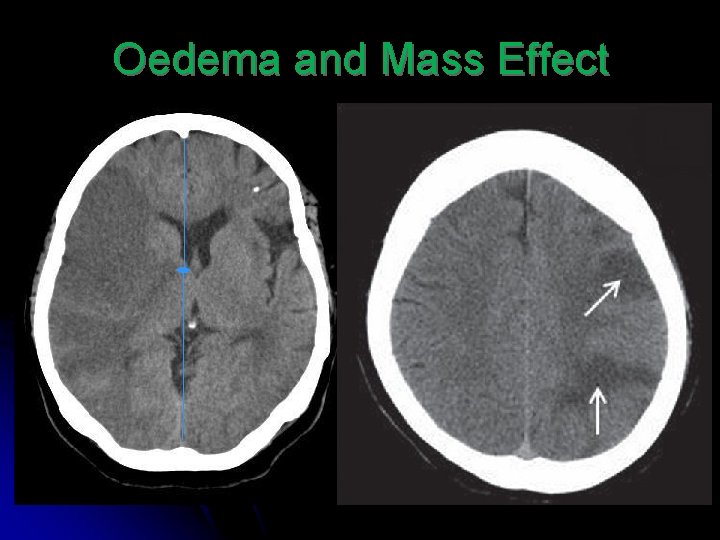
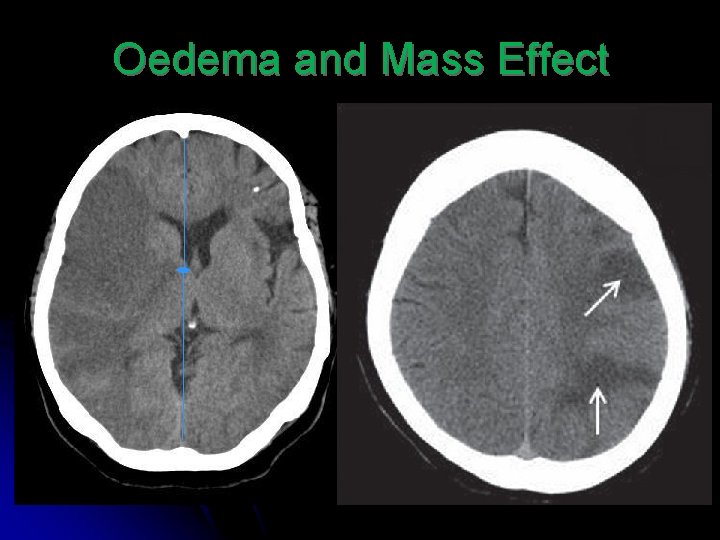
Oedema and Mass Effect
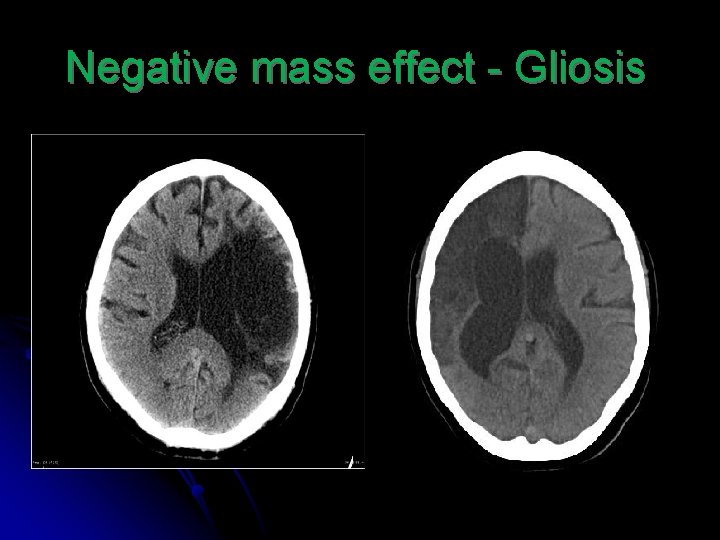
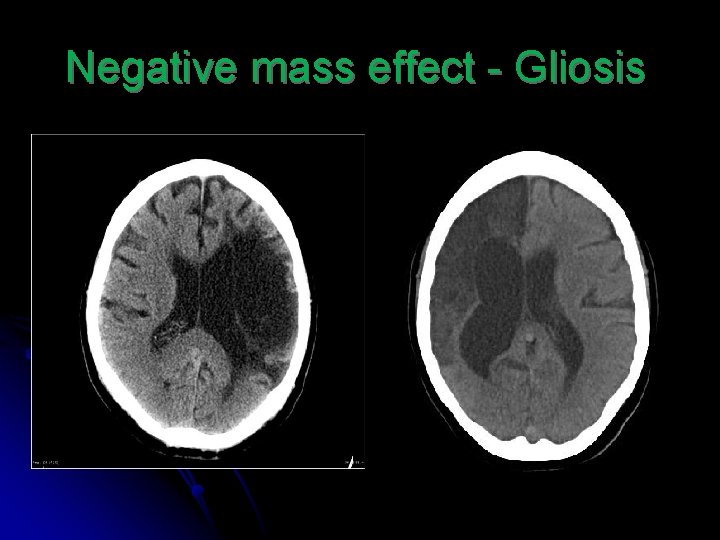
Negative mass effect - Gliosis
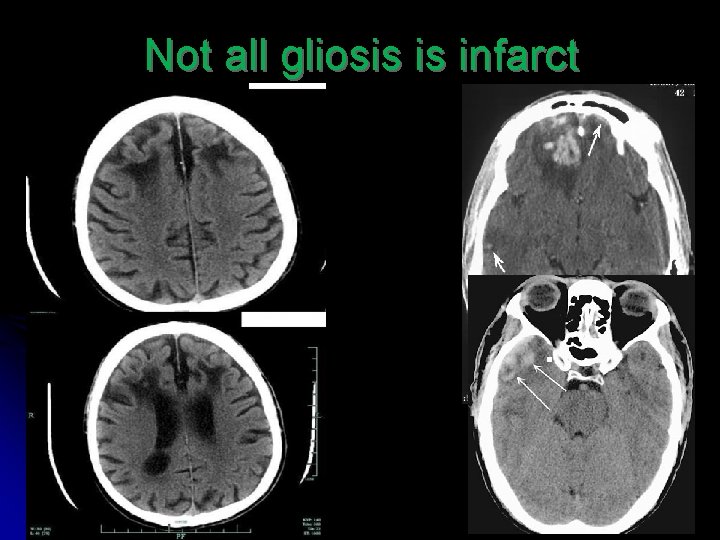
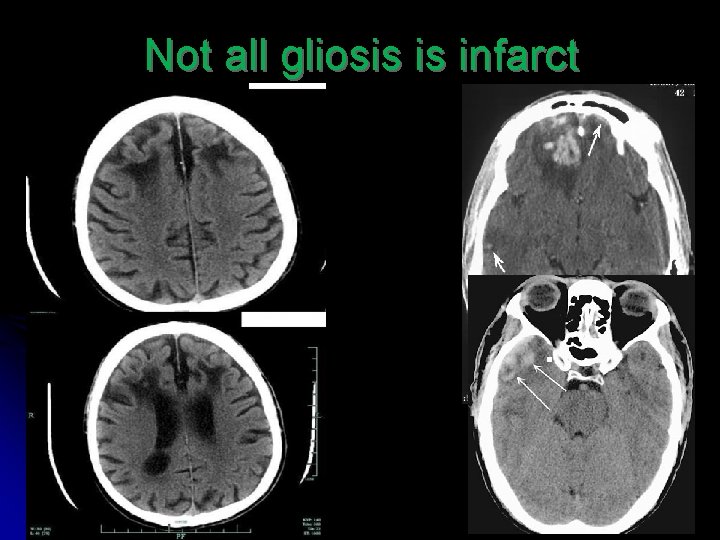
Not all gliosis is infarct
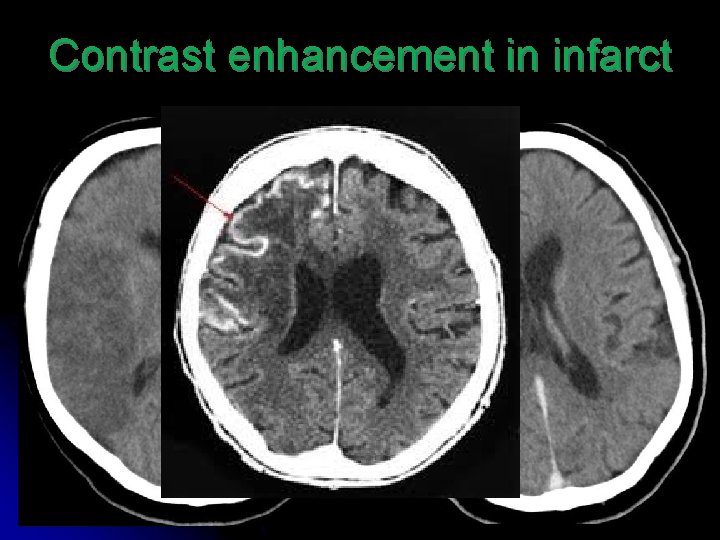
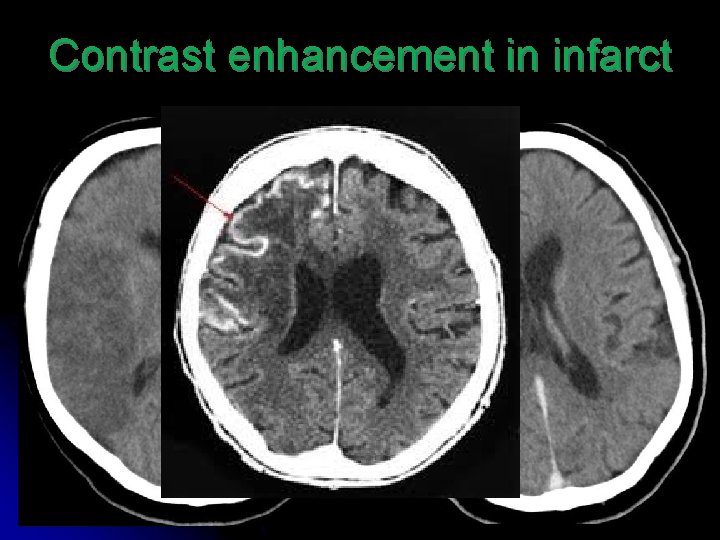
Contrast enhancement in infarct
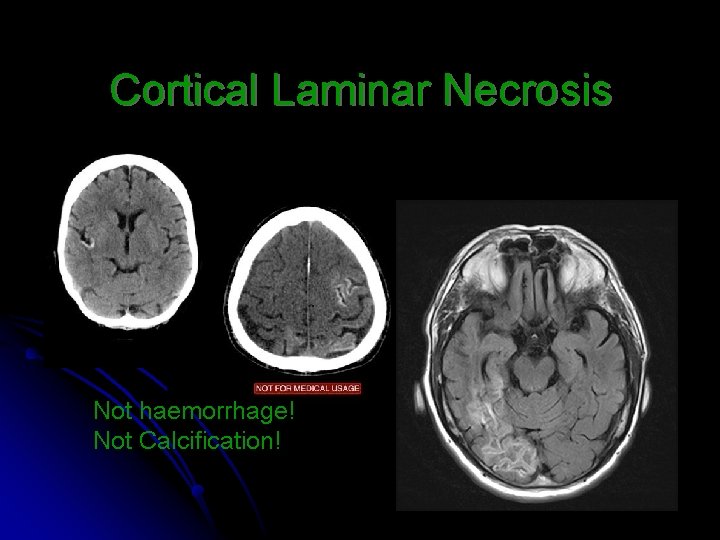
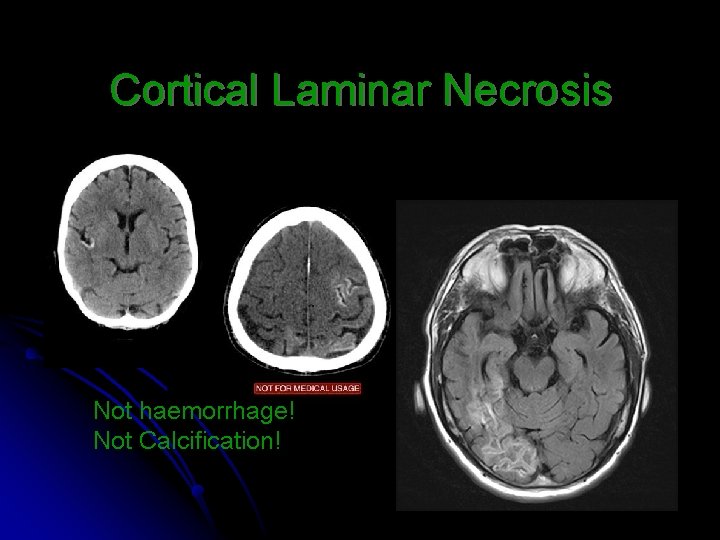
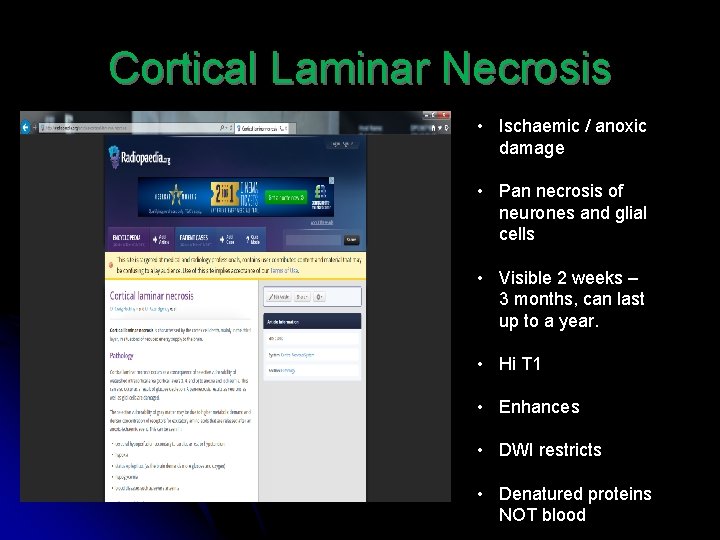
Cortical Laminar Necrosis Not haemorrhage! Not Calcification!
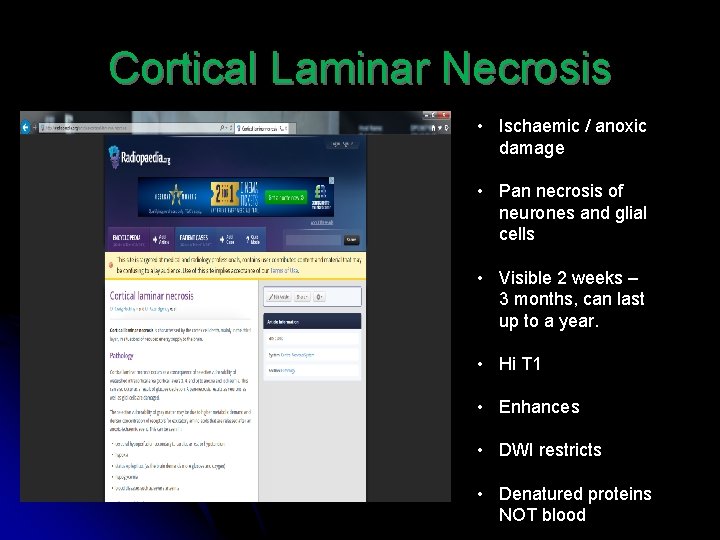
Cortical Laminar Necrosis • Ischaemic / anoxic damage • Pan necrosis of neurones and glial cells • Visible 2 weeks – 3 months, can last up to a year. • Hi T 1 • Enhances • DWI restricts • Denatured proteins NOT blood
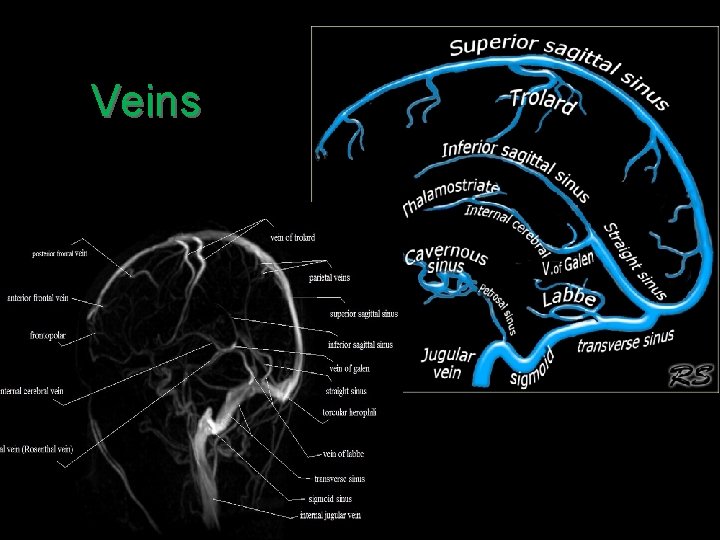
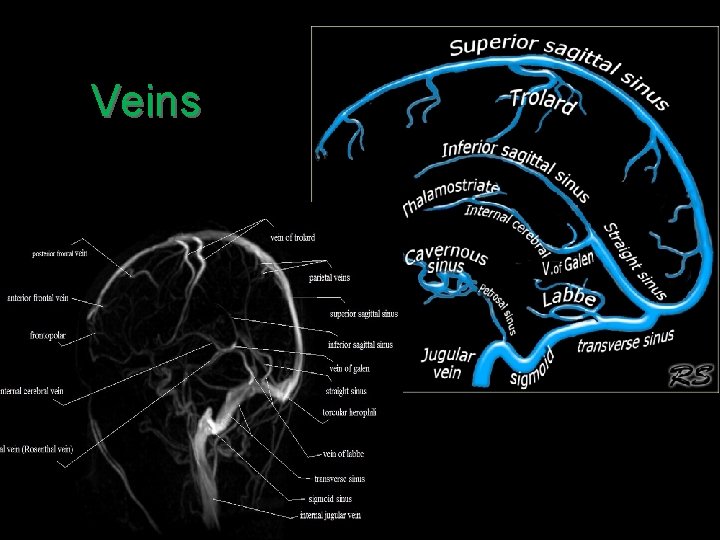
Veins
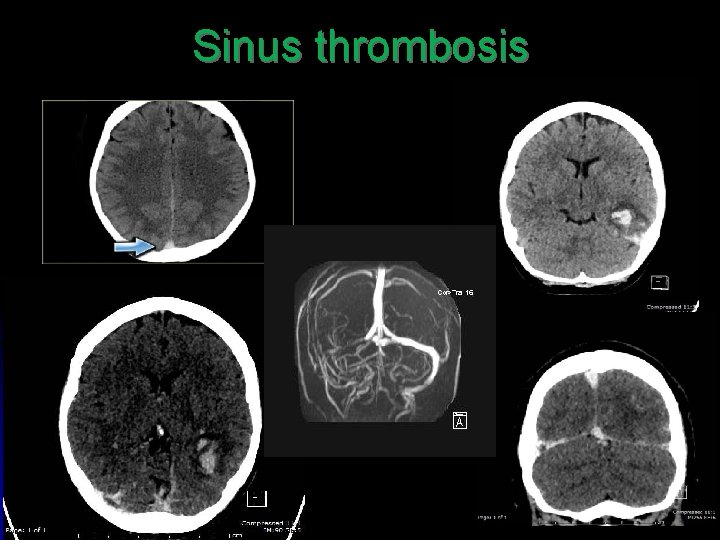
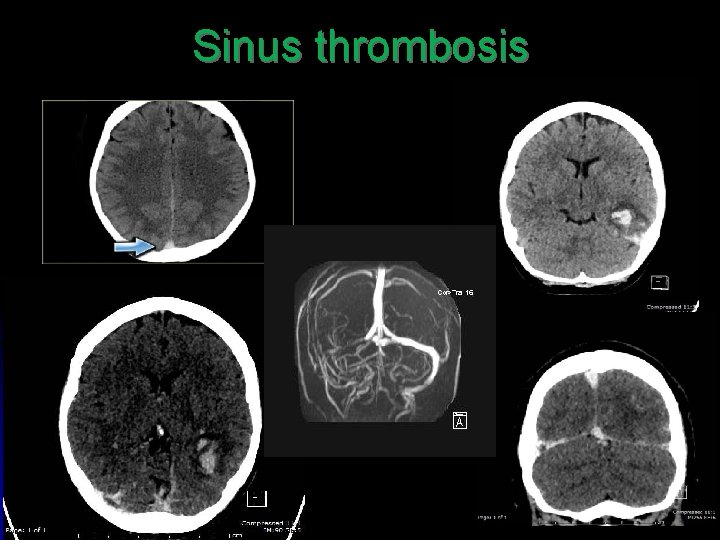
Sinus thrombosis
Wilhelm Roentgen 08 / 10 / 1895
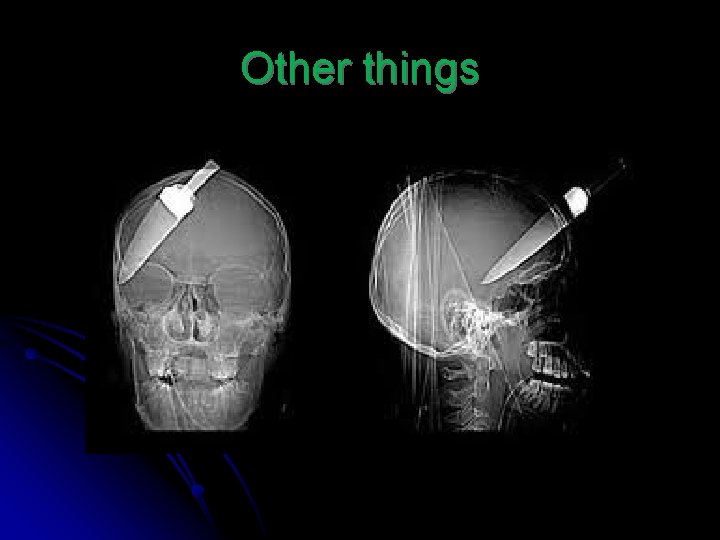
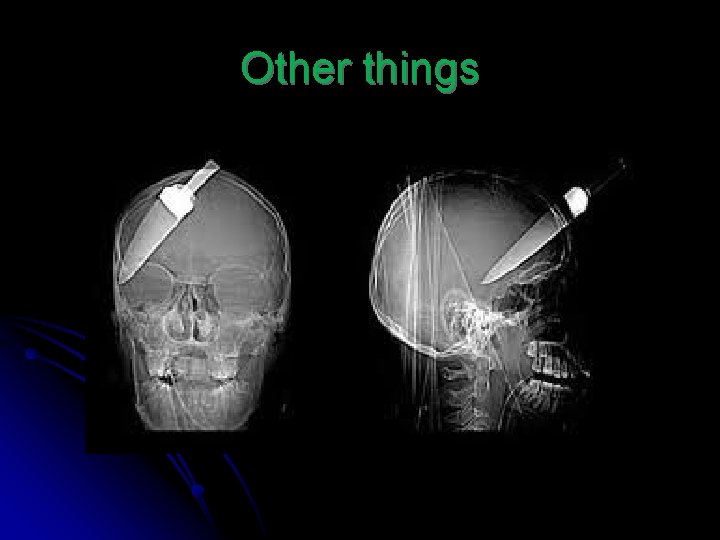
Other things
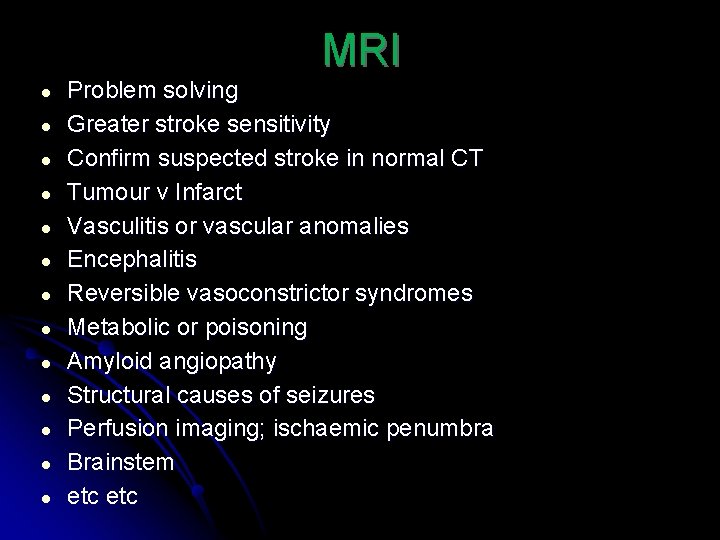
MRI ● ● ● ● Problem solving Greater stroke sensitivity Confirm suspected stroke in normal CT Tumour v Infarct Vasculitis or vascular anomalies Encephalitis Reversible vasoconstrictor syndromes Metabolic or poisoning Amyloid angiopathy Structural causes of seizures Perfusion imaging; ischaemic penumbra Brainstem etc
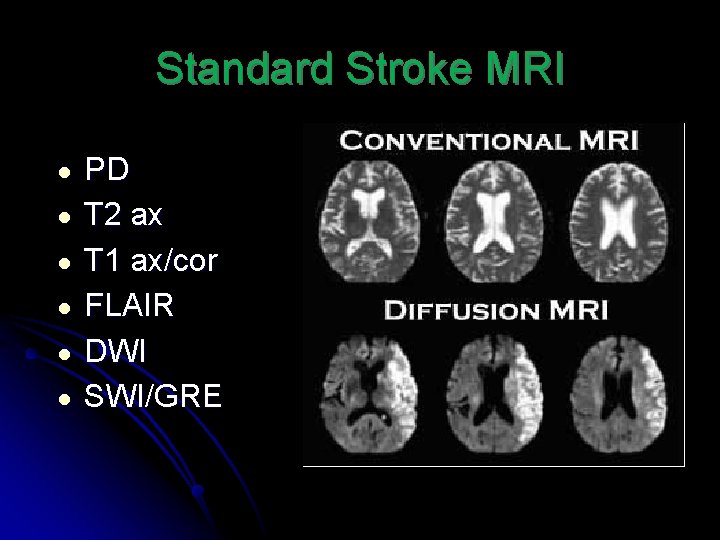
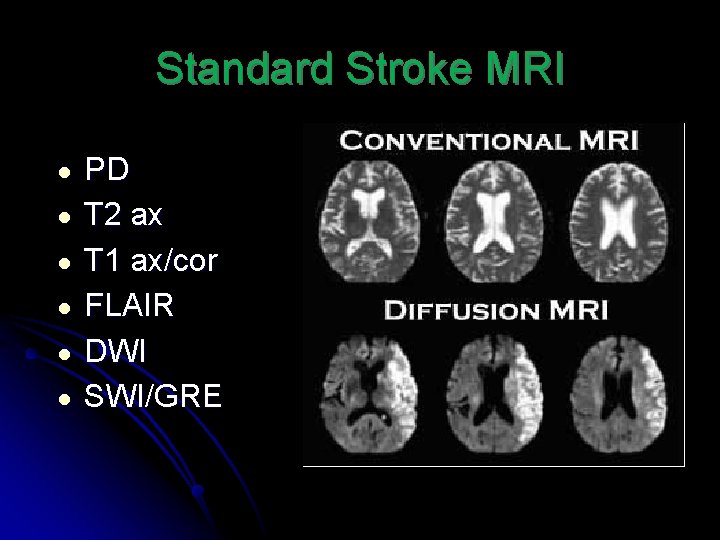
Standard Stroke MRI ● ● ● PD T 2 ax T 1 ax/cor FLAIR DWI SWI/GRE
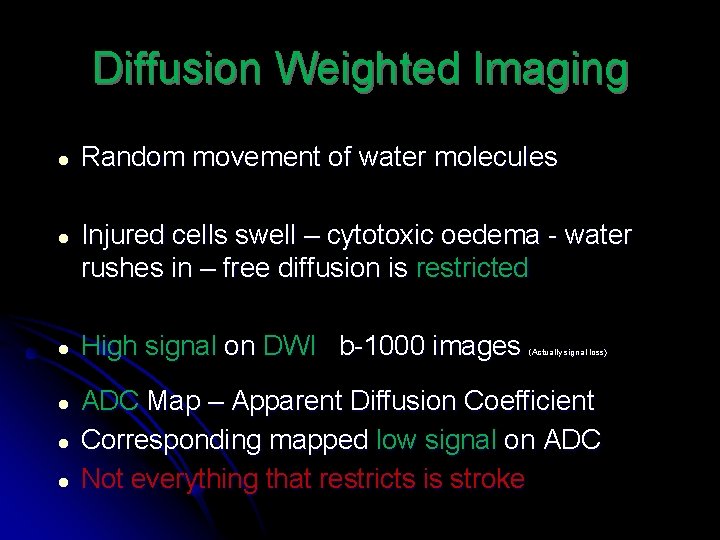
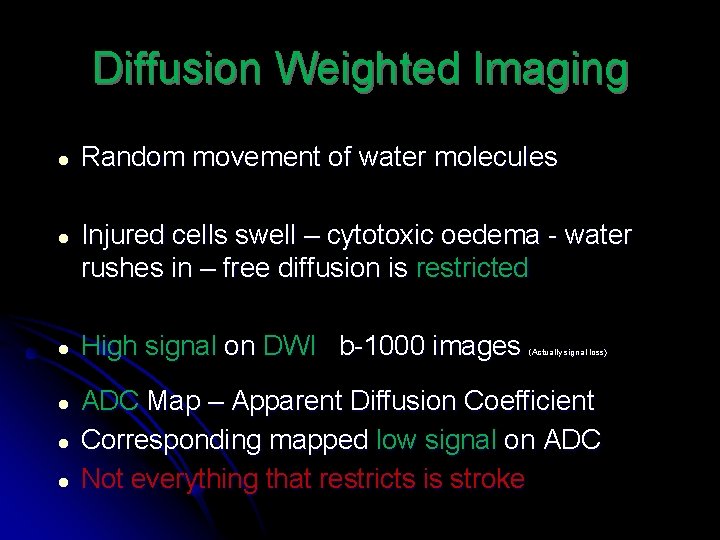
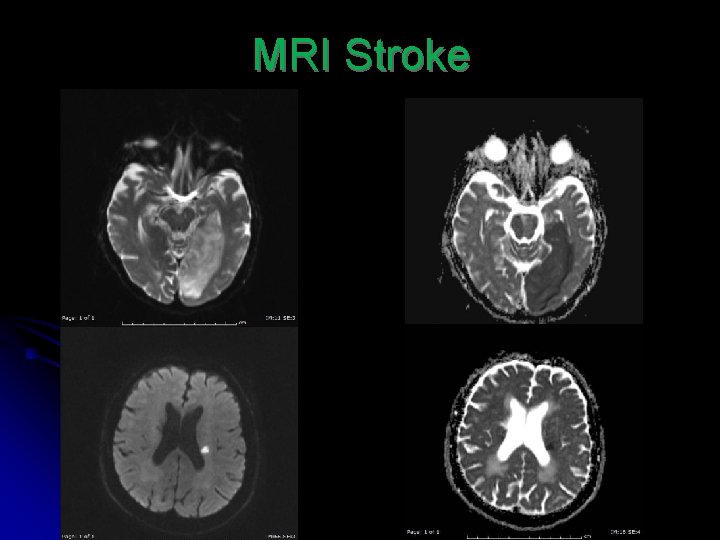
Diffusion Weighted Imaging ● Random movement of water molecules ● Injured cells swell – cytotoxic oedema - water rushes in – free diffusion is restricted ● High signal on DWI b-1000 images ● ADC Map – Apparent Diffusion Coefficient Corresponding mapped low signal on ADC Not everything that restricts is stroke ● ● (Actually signal loss)
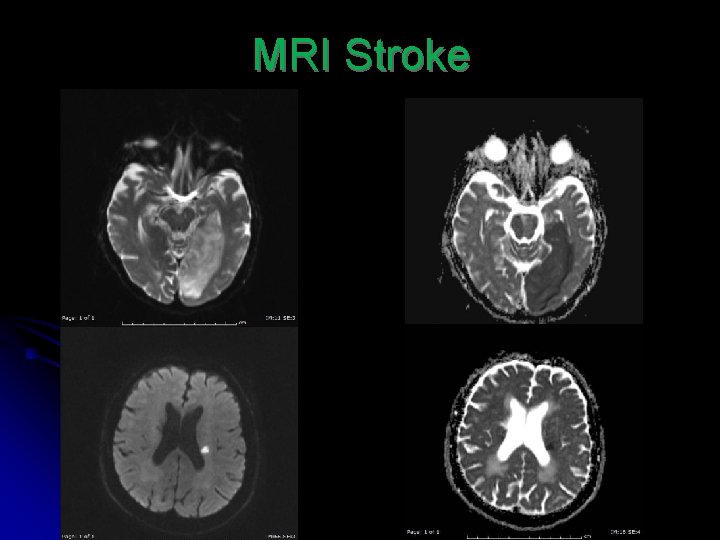
MRI Stroke
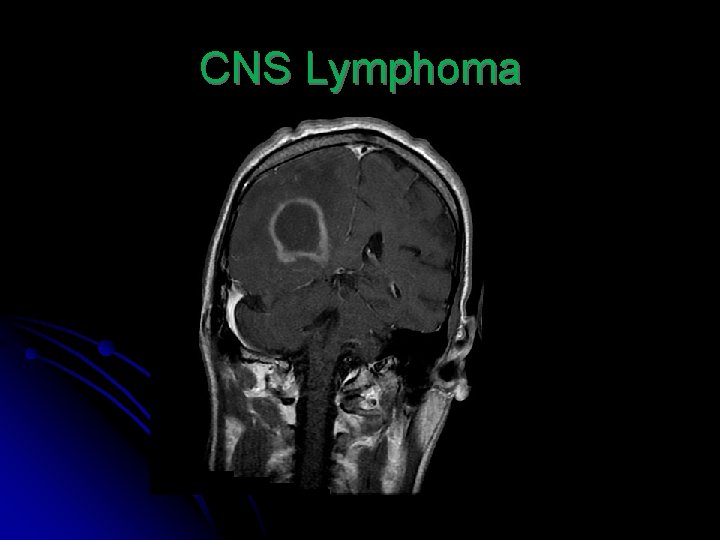
Not everything that restricts is stroke ● ● ● ● Seizures Encephalitis Low grade gliomas Metabolic (Hypoglycaemia) Abscess CJD Lymphoma Certain mets (mucinous adenoca)
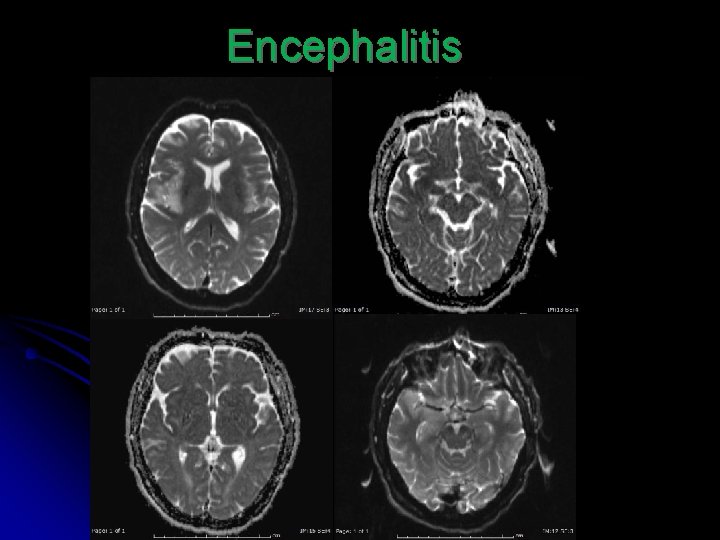
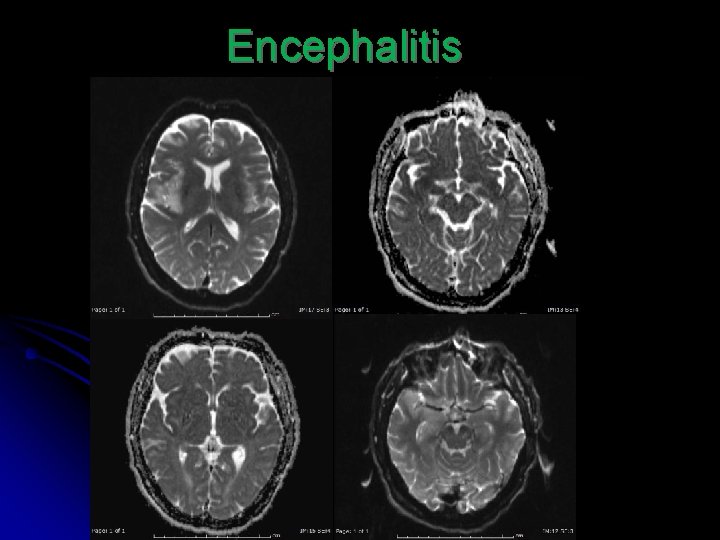
Encephalitis
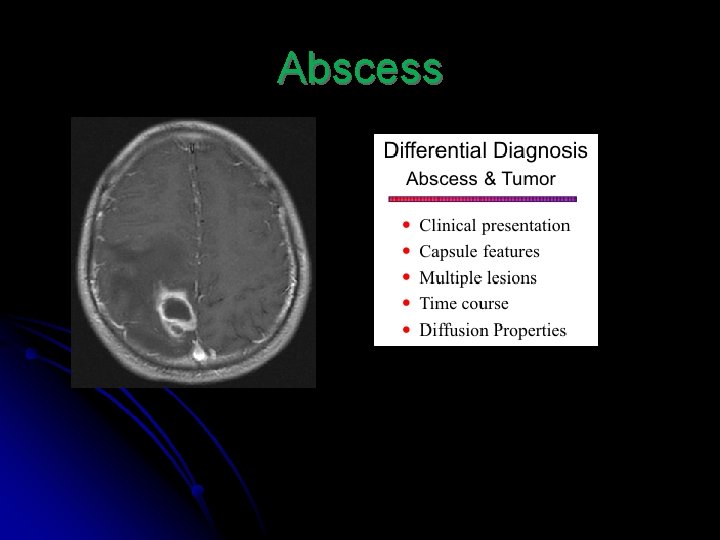
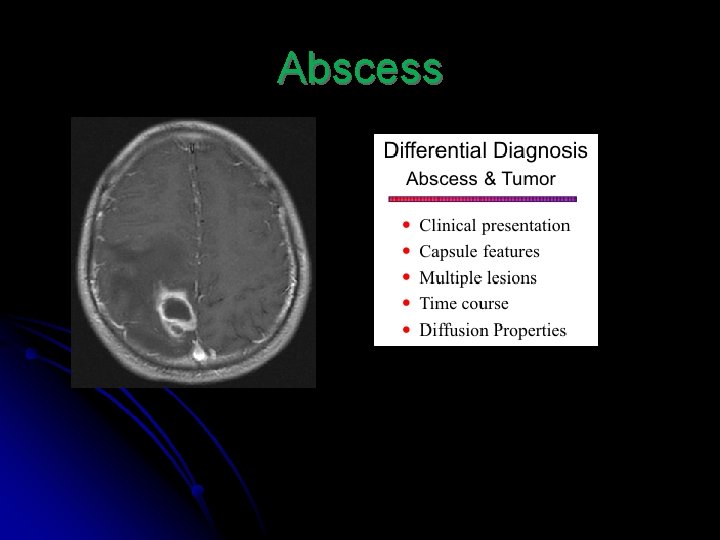
Abscess
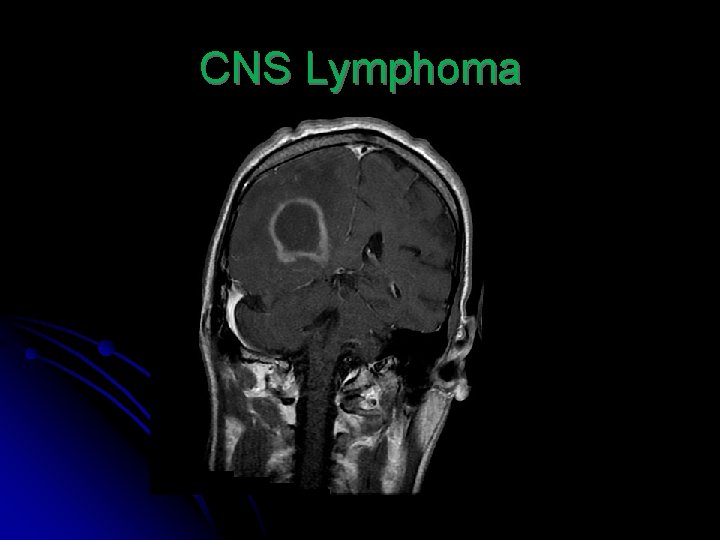
CNS Lymphoma
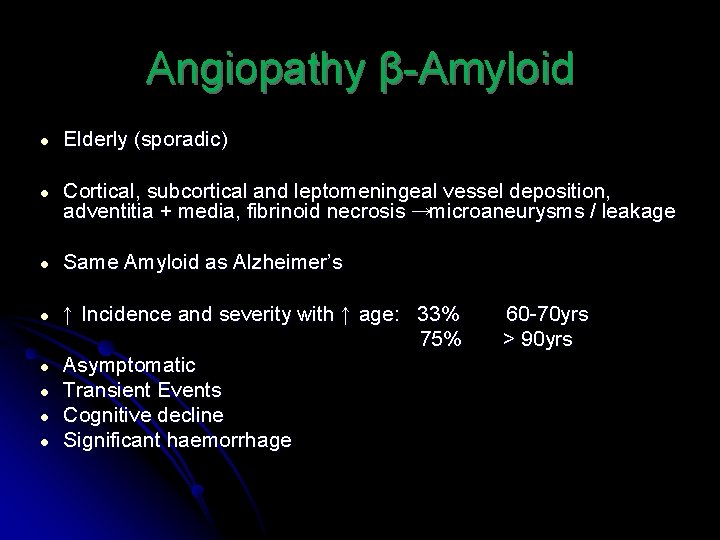
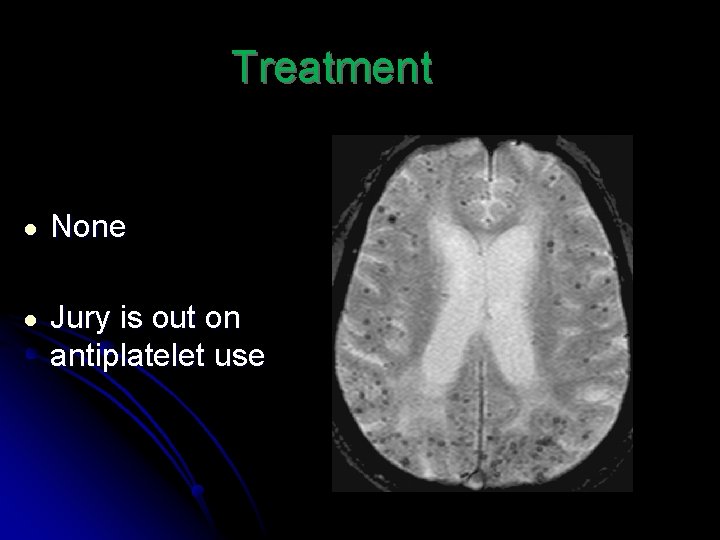
Angiopathy β-Amyloid ● Elderly (sporadic) ● Cortical, subcortical and leptomeningeal vessel deposition, adventitia + media, fibrinoid necrosis →microaneurysms / leakage ● Same Amyloid as Alzheimer’s ● ↑ Incidence and severity with ↑ age: 33% 75% Asymptomatic Transient Events Cognitive decline Significant haemorrhage ● ● 60 -70 yrs > 90 yrs
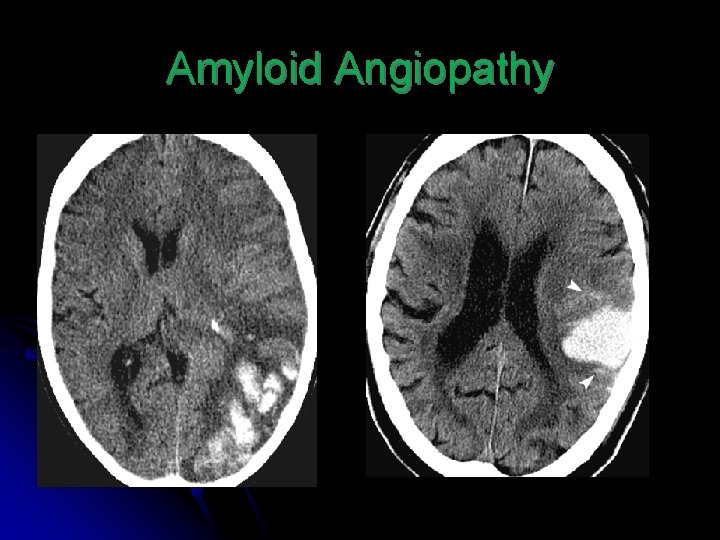
Radiological Hallmarks ● Cortical or subcortical micro haemorrhages ● Susceptibility artefact on MR ( Dark Blobs) ● Usually spares cerebellum ● Bigger bleeds usually peripheral supratentorial (frontal and parietal most commonly) ● Evidence of microbleeds in conjunction with macrobleed
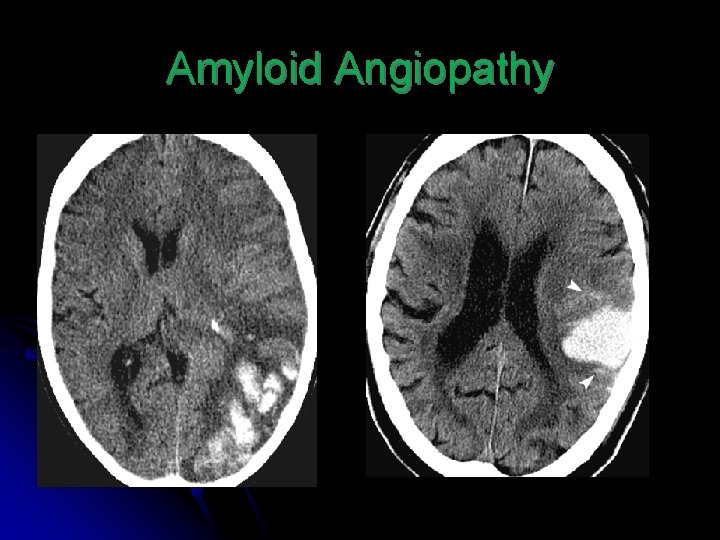
Amyloid Angiopathy
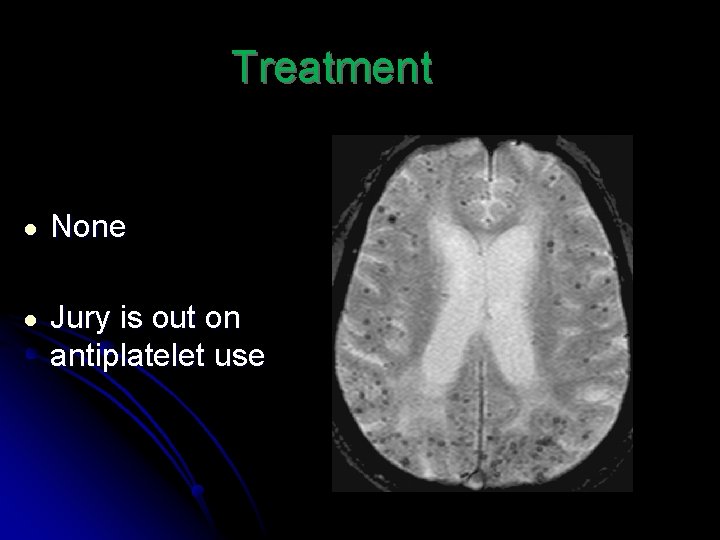
Treatment ● None ● Jury is out on antiplatelet use
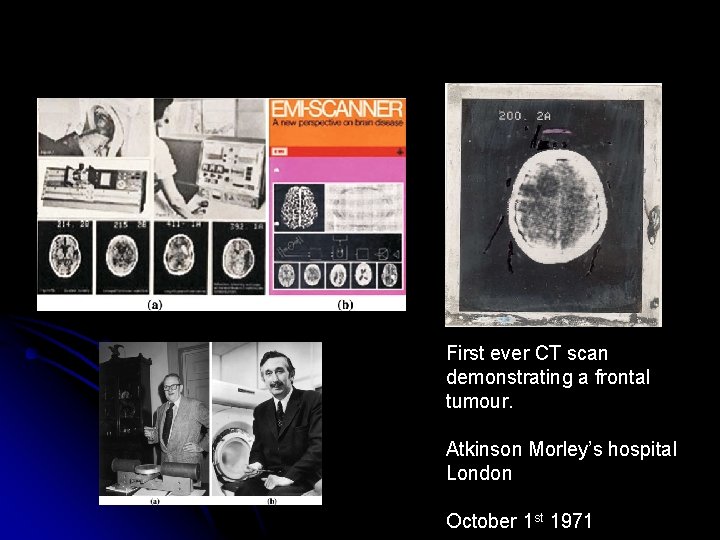
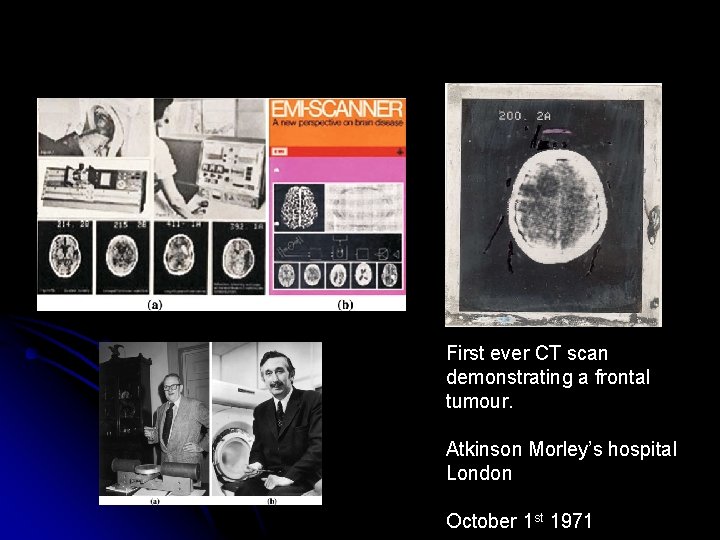
First ever CT scan demonstrating a frontal tumour. Atkinson Morley’s hospital London October 1 st 1971
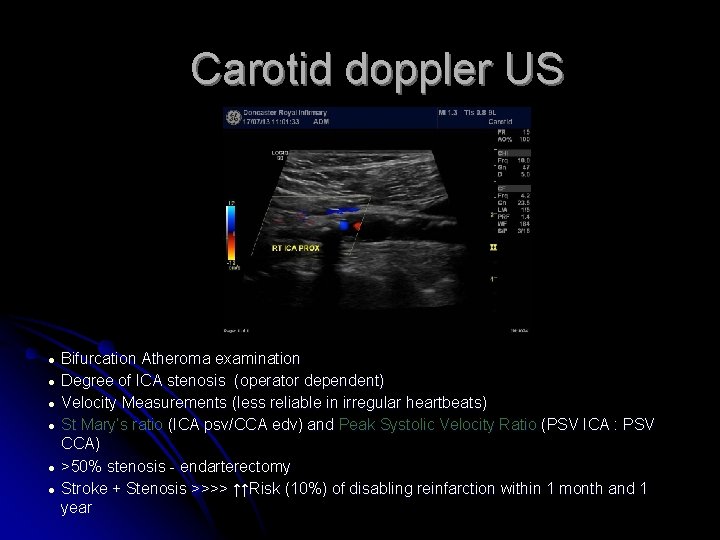
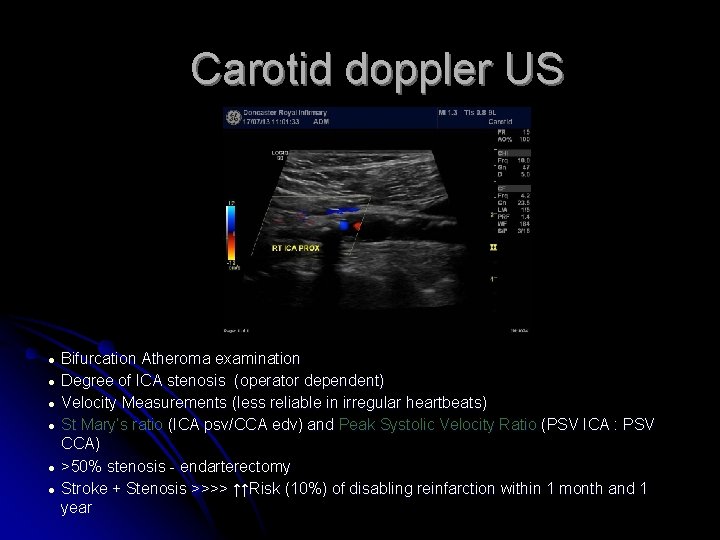
Carotid doppler US ● ● ● Bifurcation Atheroma examination Degree of ICA stenosis (operator dependent) Velocity Measurements (less reliable in irregular heartbeats) St Mary’s ratio (ICA psv/CCA edv) and Peak Systolic Velocity Ratio (PSV ICA : PSV CCA) >50% stenosis - endarterectomy Stroke + Stenosis >>>> ↑↑Risk (10%) of disabling reinfarction within 1 month and 1 year
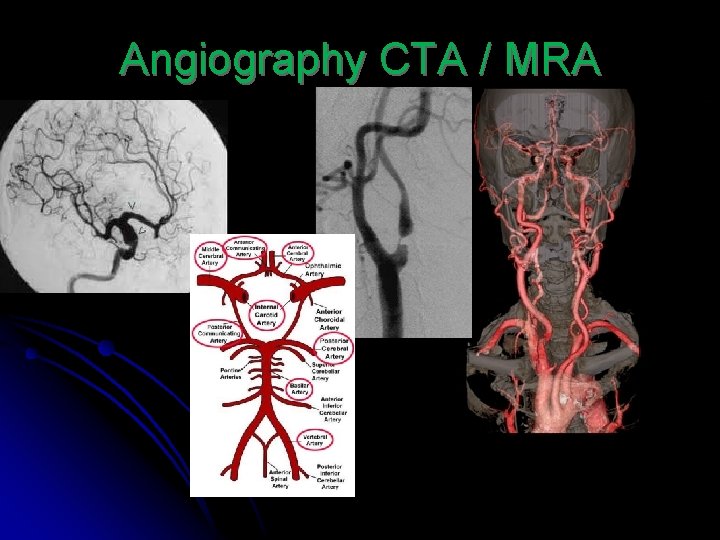
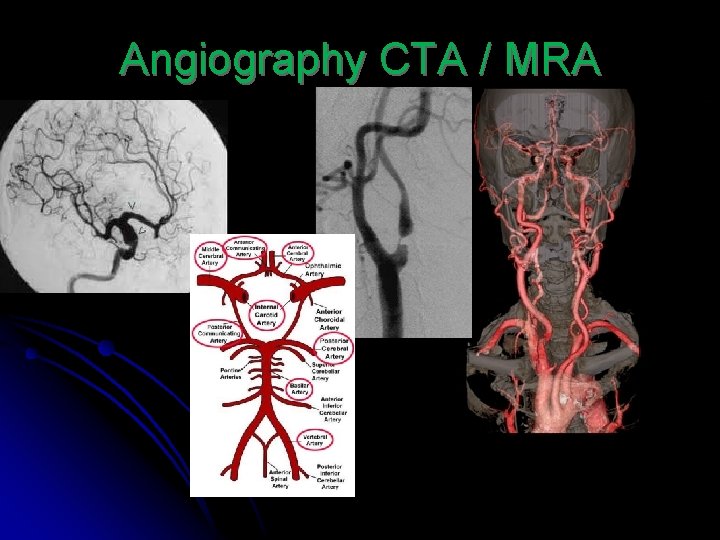
Angiography CTA / MRA
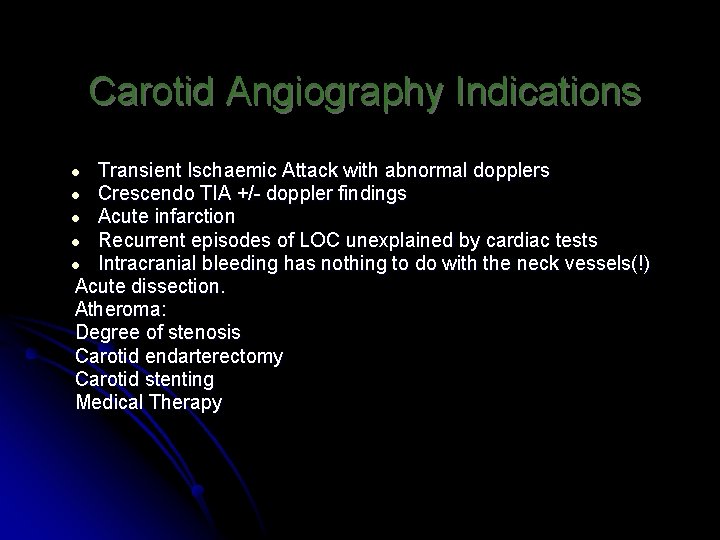
Carotid Angiography Indications Transient Ischaemic Attack with abnormal dopplers Crescendo TIA +/- doppler findings Acute infarction Recurrent episodes of LOC unexplained by cardiac tests Intracranial bleeding has nothing to do with the neck vessels(!) Acute dissection. Atheroma: Degree of stenosis Carotid endarterectomy Carotid stenting Medical Therapy ● ● ●
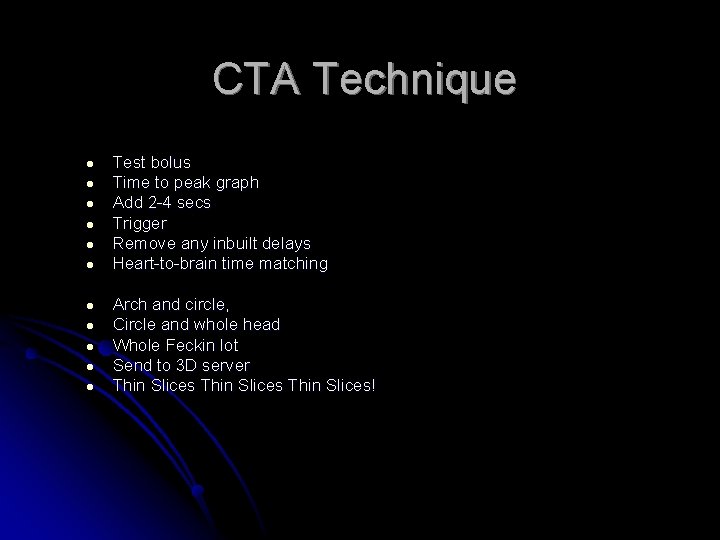
CTA Technique ● ● ● Test bolus Time to peak graph Add 2 -4 secs Trigger Remove any inbuilt delays Heart-to-brain time matching Arch and circle, Circle and whole head Whole Feckin lot Send to 3 D server Thin Slices!
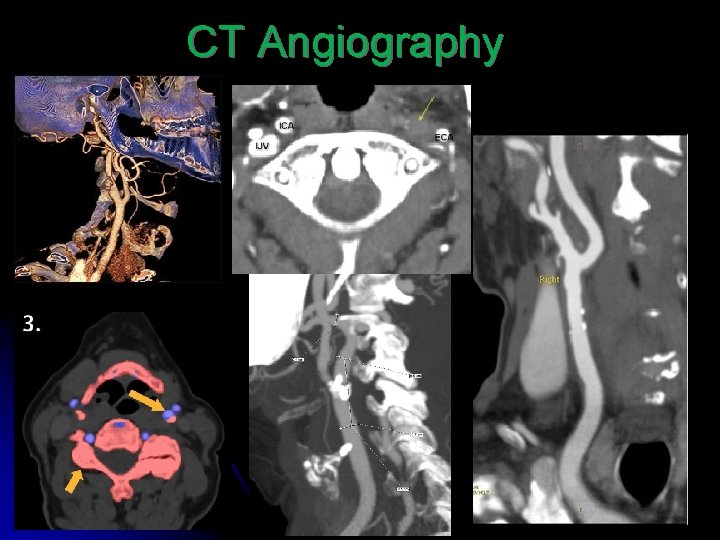
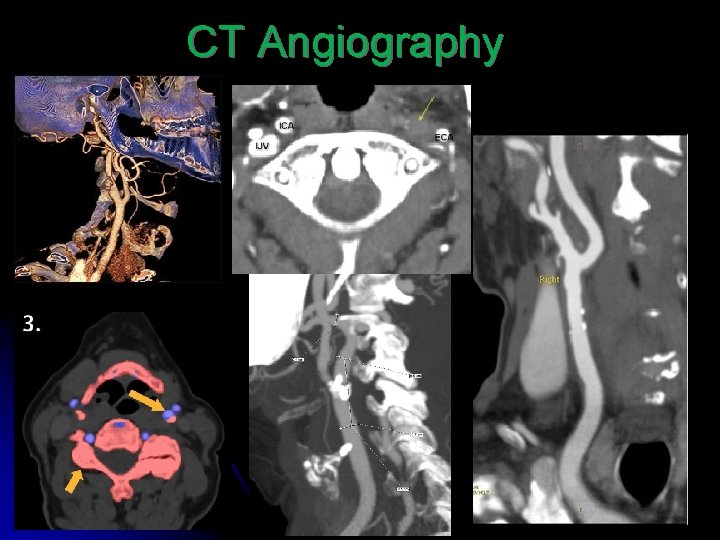
CT Angiography
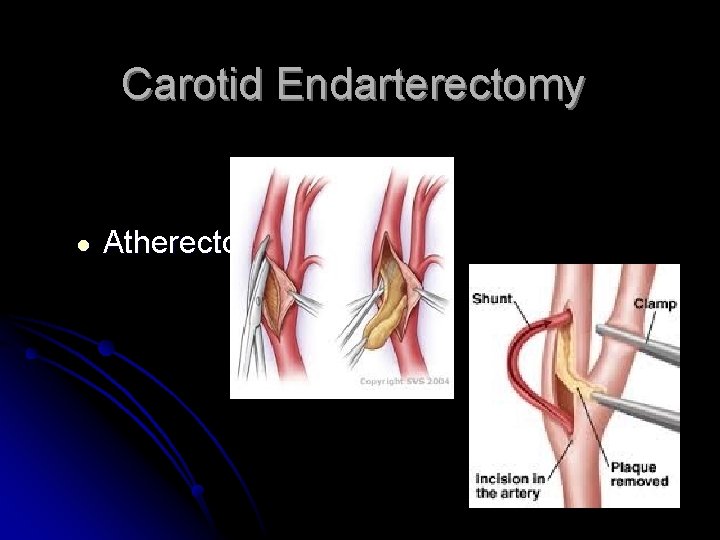
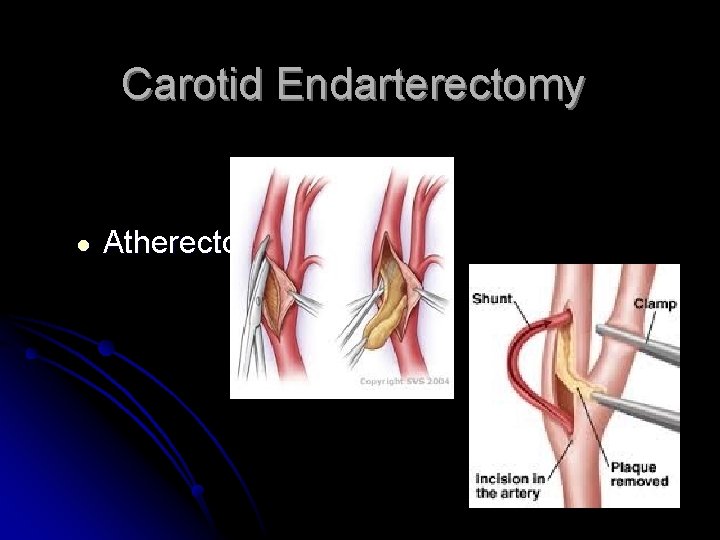
Carotid Endarterectomy ● Atherectomy
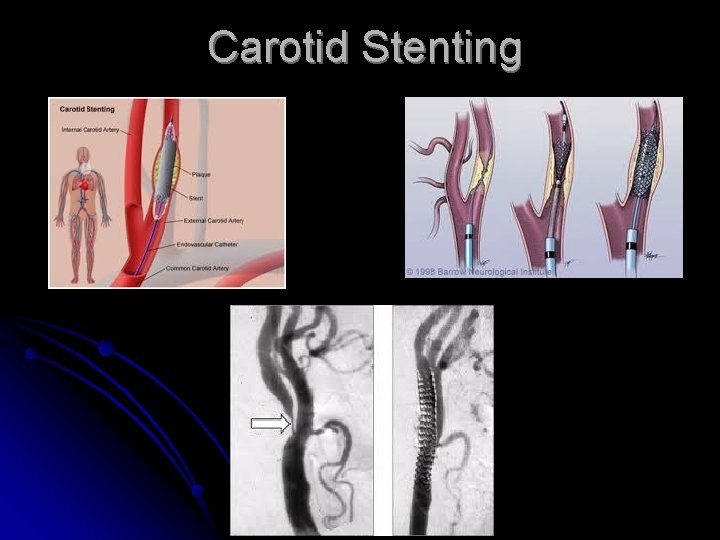
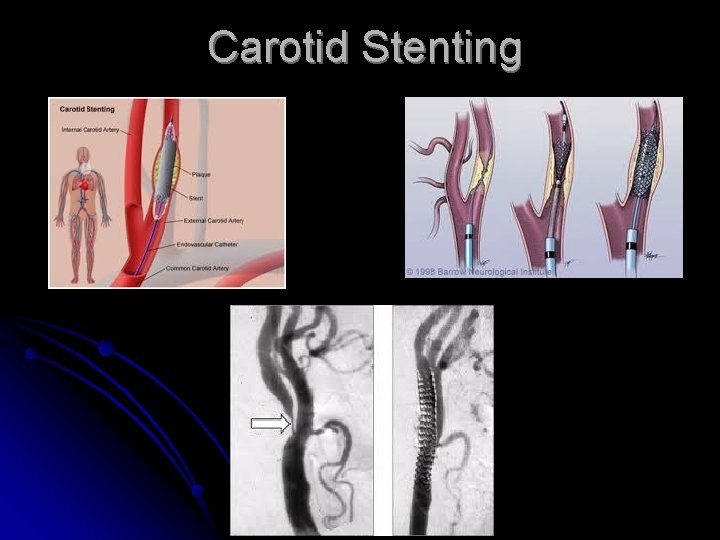
Carotid Stenting
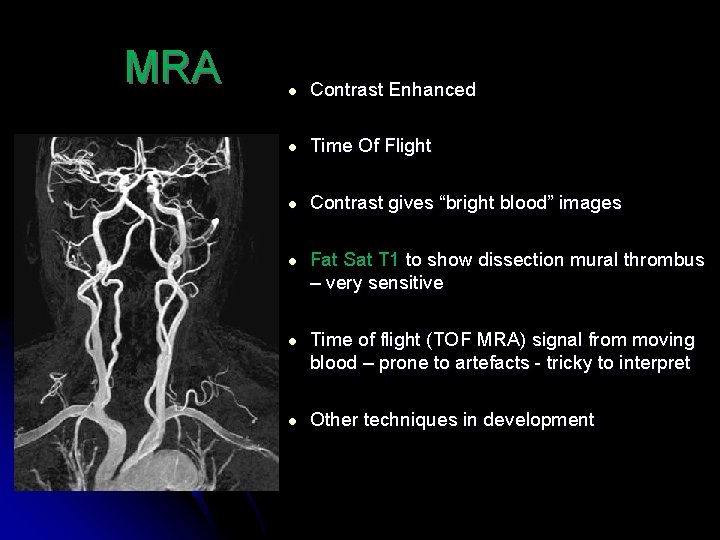
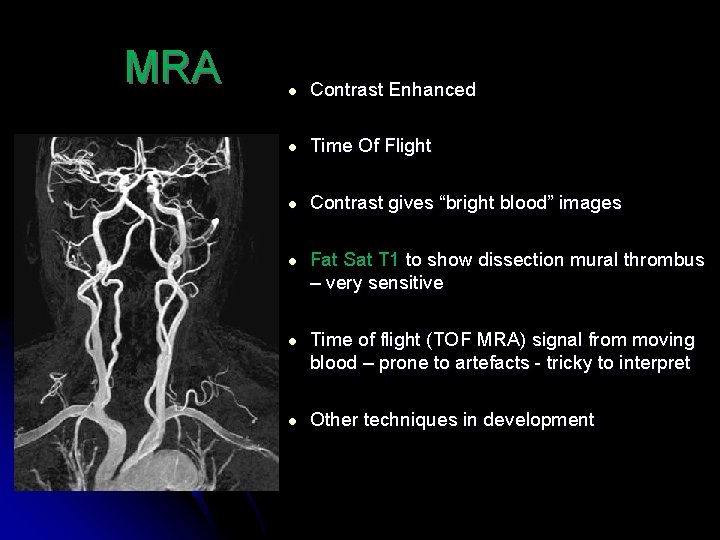
MRA ● Contrast Enhanced ● Time Of Flight ● Contrast gives “bright blood” images ● Fat Sat T 1 to show dissection mural thrombus – very sensitive ● Time of flight (TOF MRA) signal from moving blood – prone to artefacts - tricky to interpret ● Other techniques in development
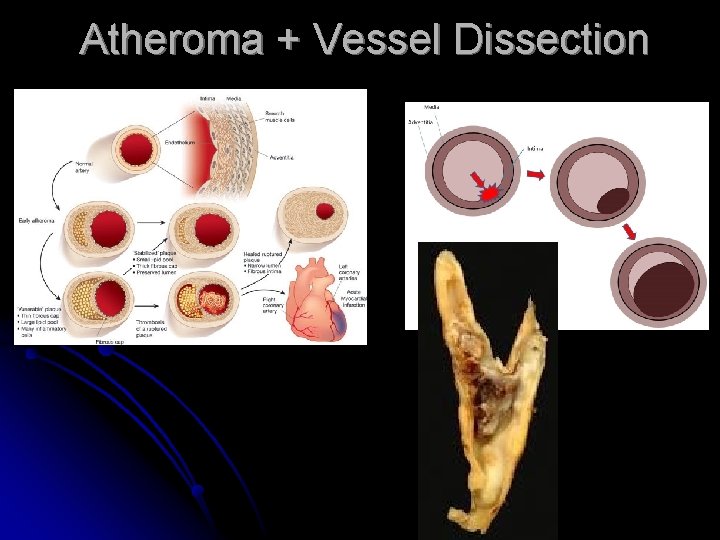
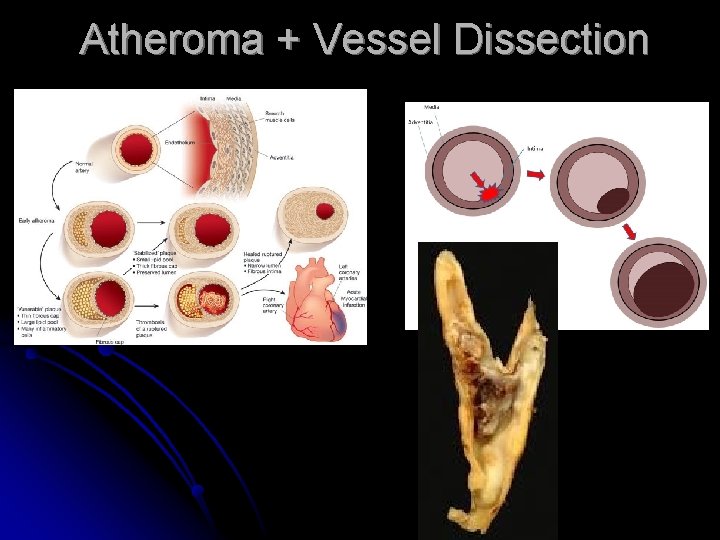
Atheroma + Vessel Dissection
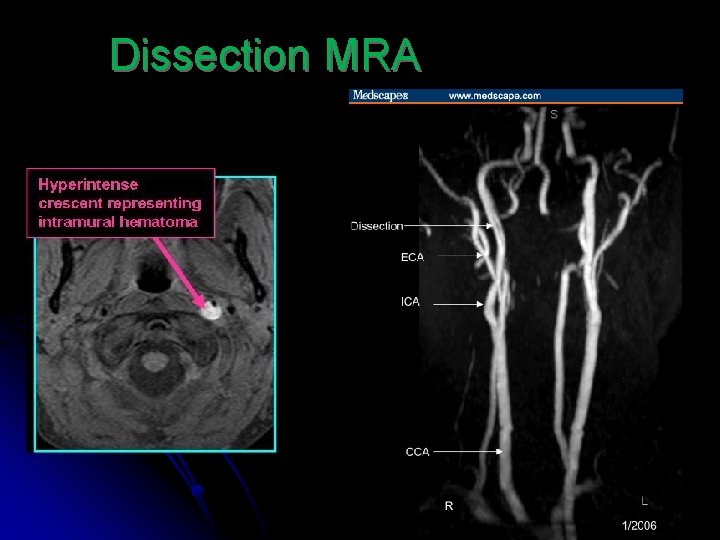
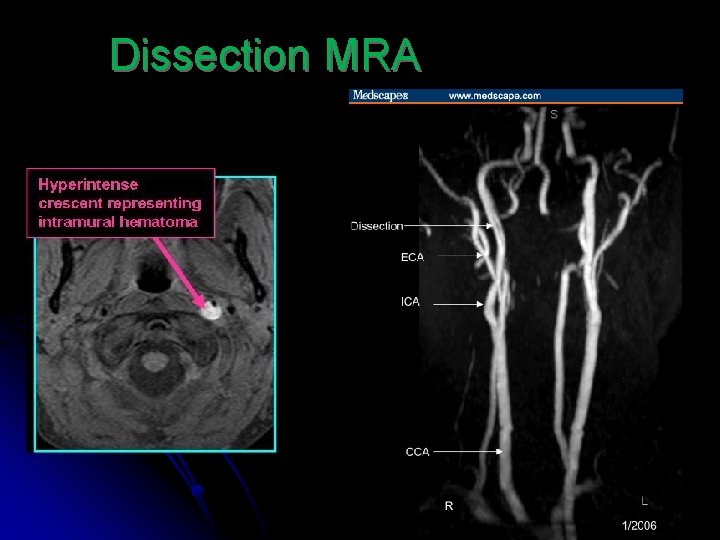
Dissection MRA
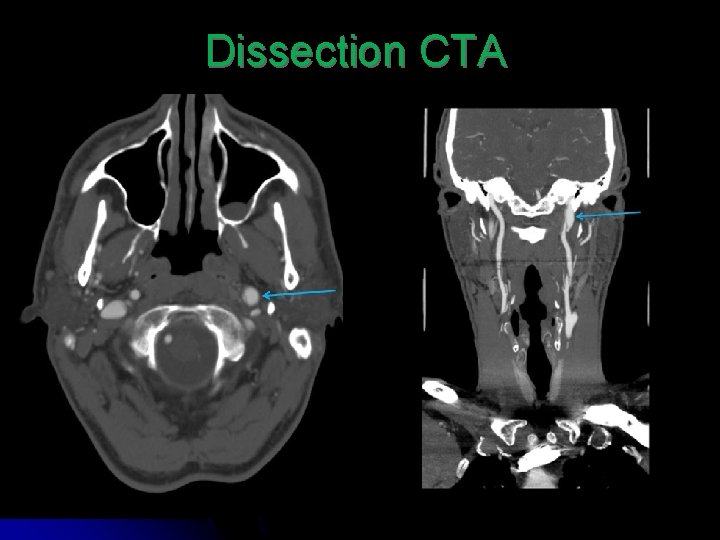
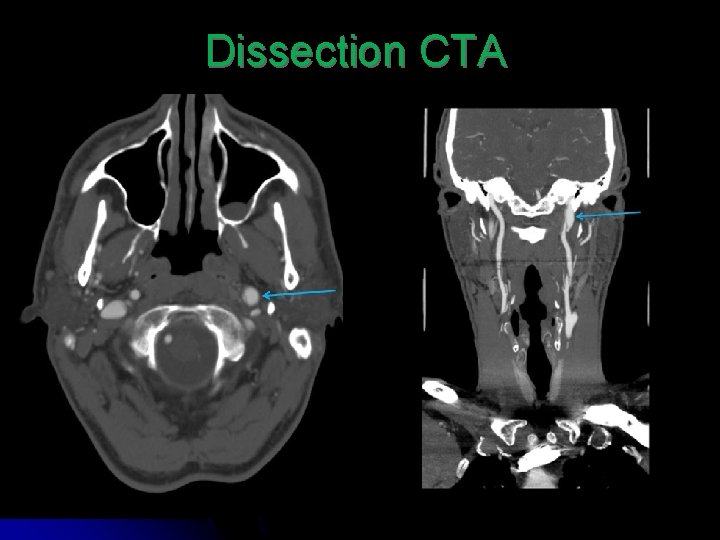
Dissection CTA
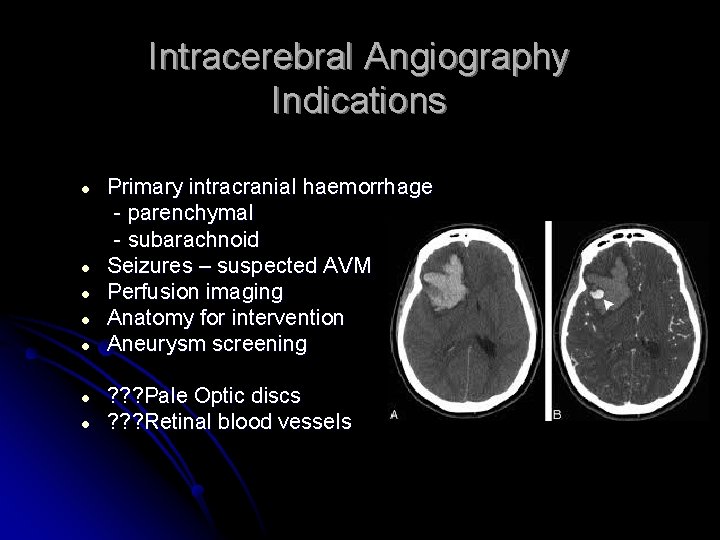
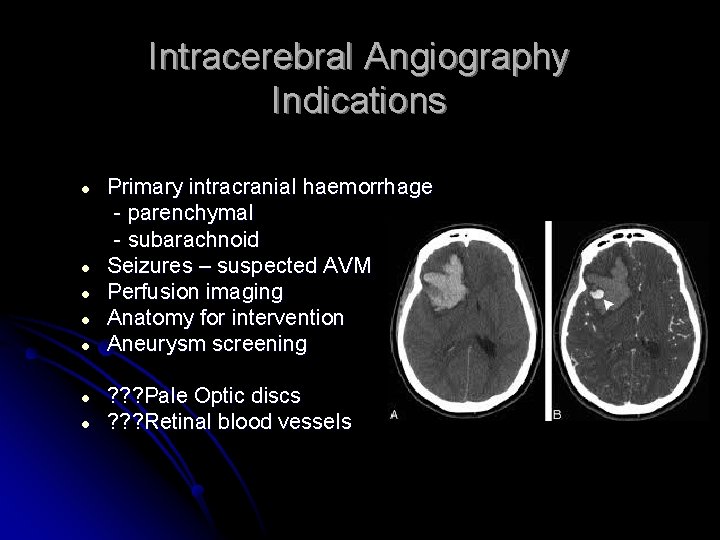
Intracerebral Angiography Indications ● ● Primary intracranial haemorrhage - parenchymal - subarachnoid Seizures – suspected AVM Perfusion imaging Anatomy for intervention Aneurysm screening ● ● ? ? ? Pale Optic discs ? ? ? Retinal blood vessels ● ● ●
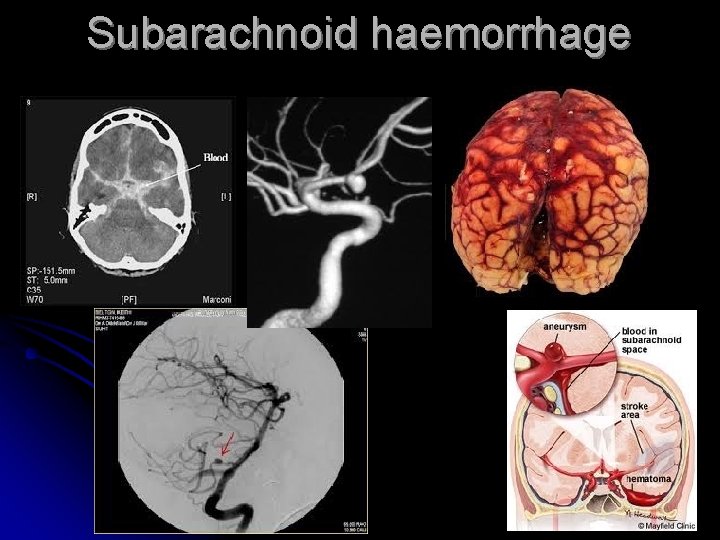
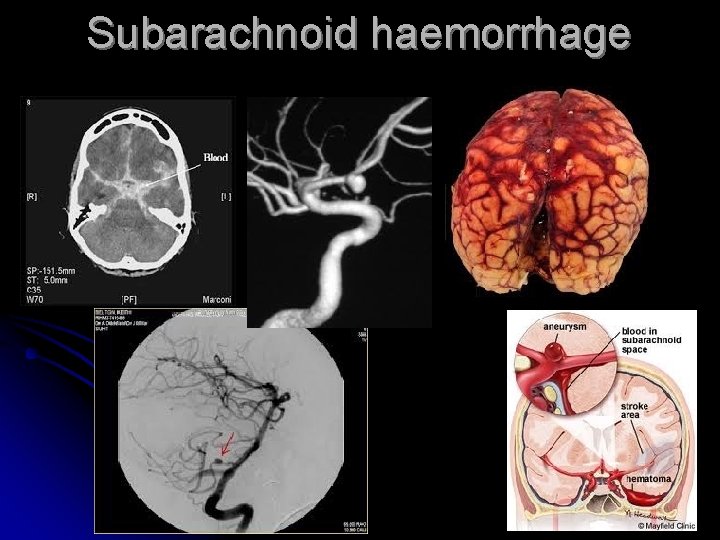
Subarachnoid haemorrhage
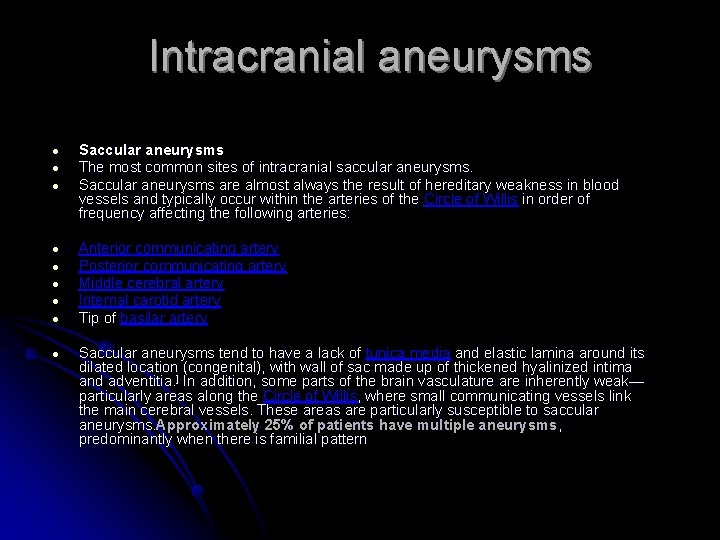
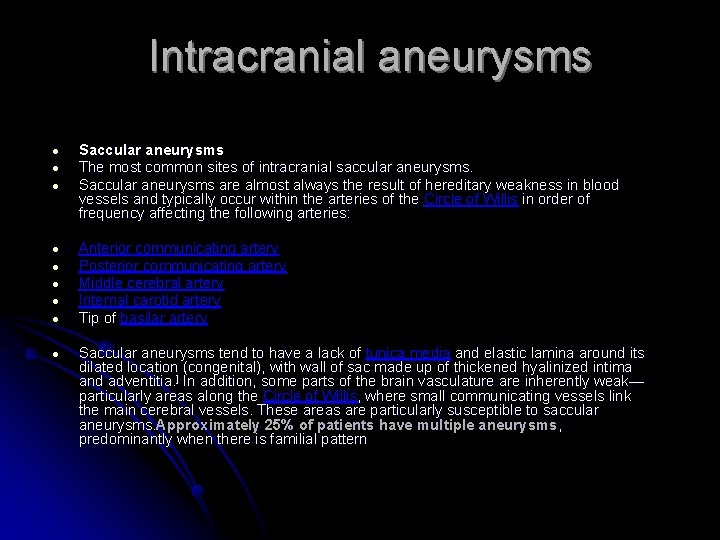
Intracranial aneurysms ● ● ● Saccular aneurysms The most common sites of intracranial saccular aneurysms. Saccular aneurysms are almost always the result of hereditary weakness in blood vessels and typically occur within the arteries of the Circle of Willis in order of frequency affecting the following arteries: ● ● ● Anterior communicating artery Posterior communicating artery Middle cerebral artery Internal carotid artery Tip of basilar artery ● Saccular aneurysms tend to have a lack of tunica media and elastic lamina around its dilated location (congenital), with wall of sac made up of thickened hyalinized intima and adventitia. ] In addition, some parts of the brain vasculature are inherently weak— particularly areas along the Circle of Willis, where small communicating vessels link the main cerebral vessels. These areas are particularly susceptible to saccular aneurysms. Approximately 25% of patients have multiple aneurysms, predominantly when there is familial pattern
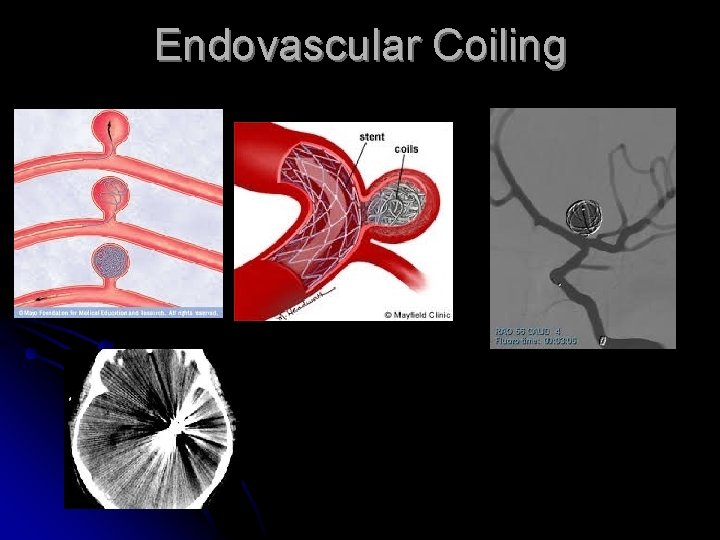
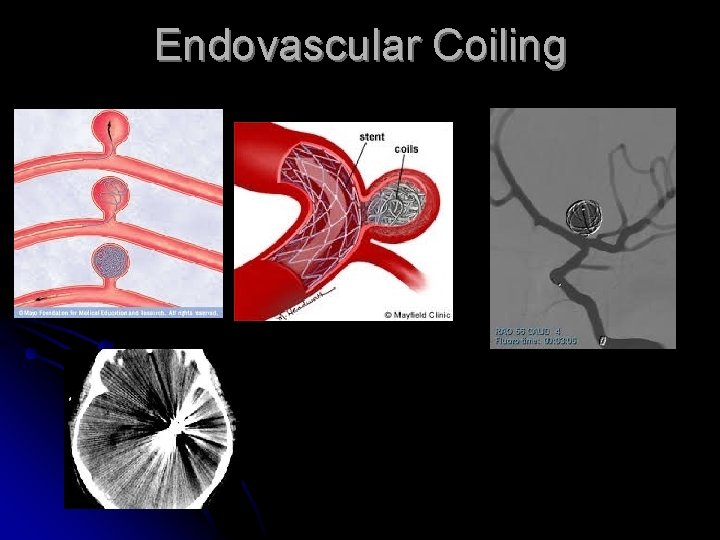
Endovascular Coiling
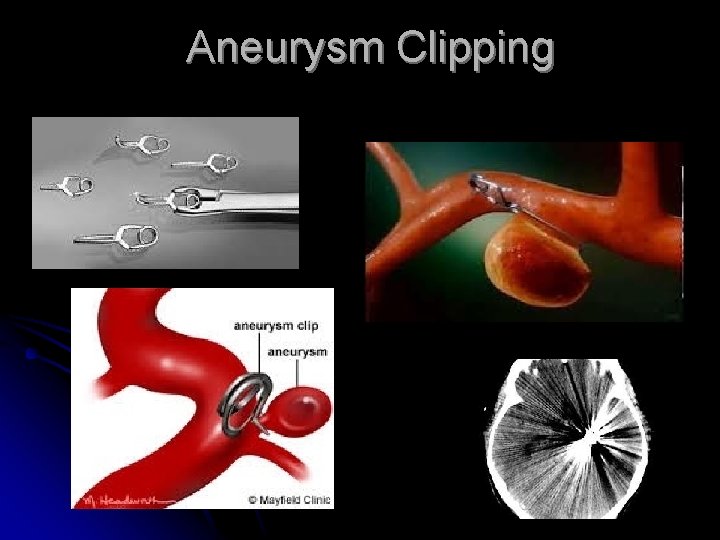
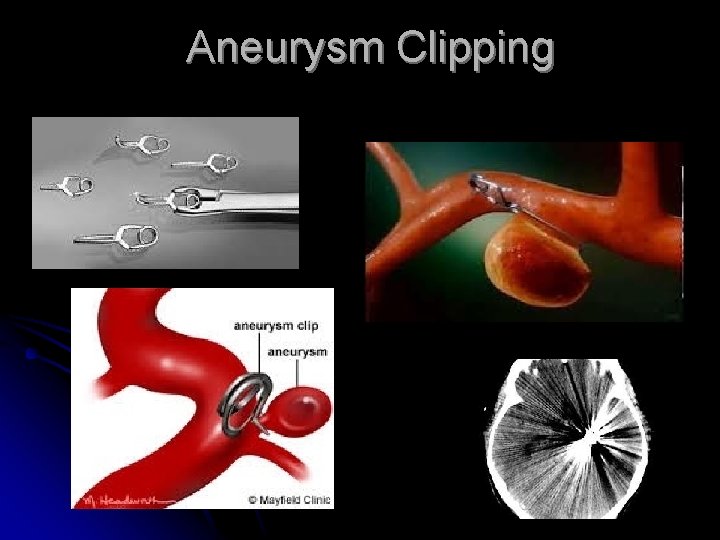
Aneurysm Clipping
