Hypoglycemia Prevention Treatment Gary Scheiner MS CDE Owner


- Slides: 45

Hypoglycemia Prevention & Treatment Gary Scheiner MS, CDE Owner, Integrated Diabetes Services 333 E. Lancaster Ave. , Suite 204 Wynnewood, PA 19096 877 -SELF-MGT (735 -3648) (610) 642 -6055 www. integrateddiabetes. com Gary@integrateddiabetes. com
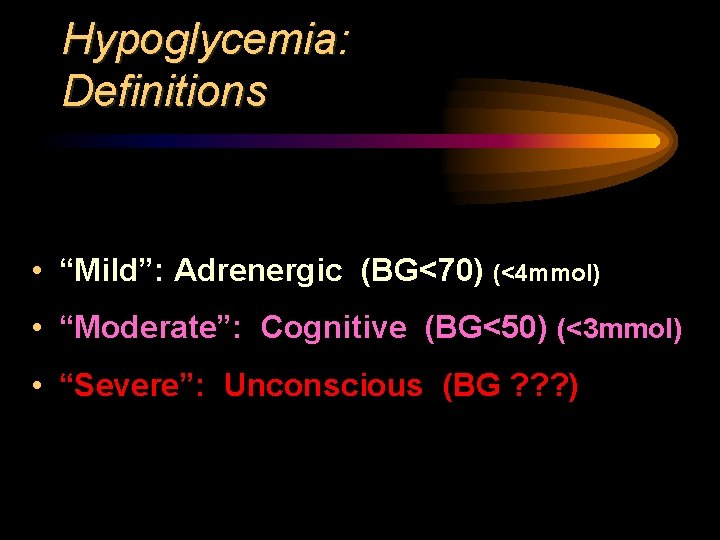
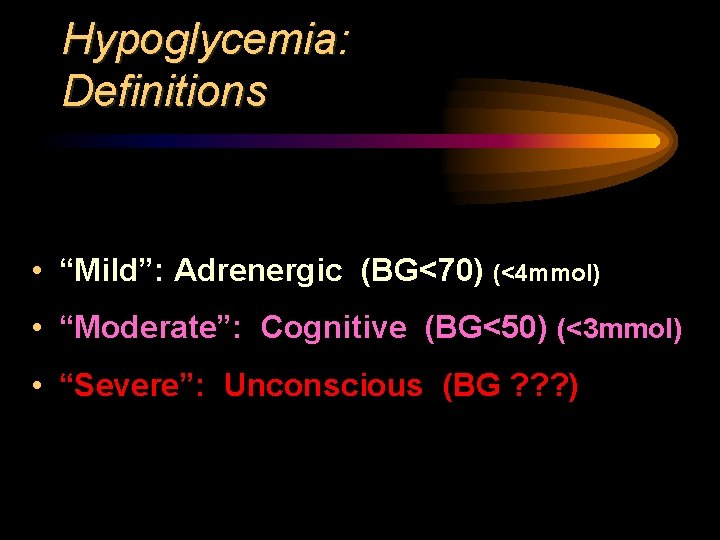
Hypoglycemia: Definitions • “Mild”: Adrenergic (BG<70) (<4 mmol) • “Moderate”: Cognitive (BG<50) (<3 mmol) • “Severe”: Unconscious (BG ? ? ? )
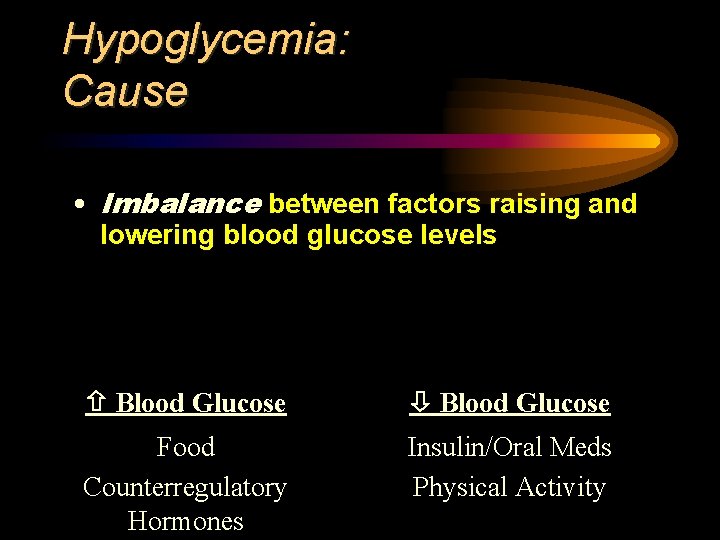
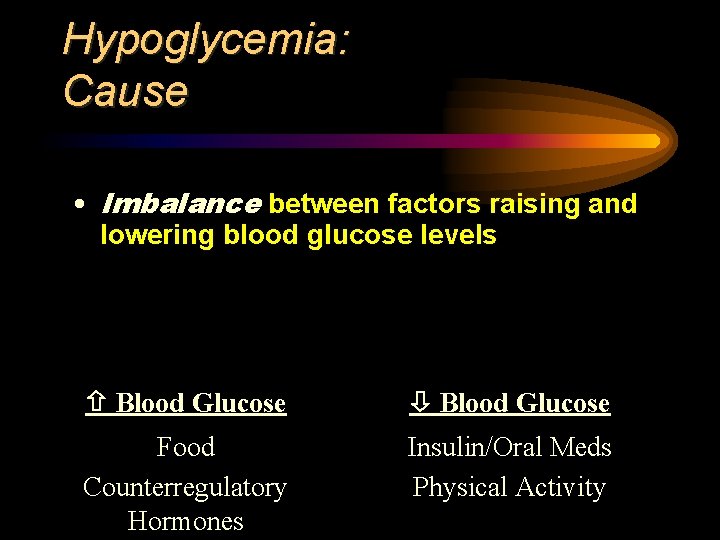
Hypoglycemia: Cause • Imbalance between factors raising and lowering blood glucose levels Blood Glucose Food Counterregulatory Hormones Insulin/Oral Meds Physical Activity
Hypoglycemia “The Greatest Limiting Factor In Diabetes Management”
The Great Limiting Factor • Performance Impairment
The Great Limiting Factor • Accident Risk
The Great Limiting Factor • Anxiety / Embarrassment
The Great Limiting Factor • Lasting Damage? • Spatial memory / performance (if before age 5)
The Great Limiting Factor • Diminished Symptoms (Hypoglycemic Unawareness)
The Great Limiting Factor • Rebound
The Great Limiting Factor • Weight Gain
Hypoglycemia: Targets/Goals • Unable to recognize & verbalize lows: >80 (4. 5 mmol) • Able to recognize & verbalize lows: >70 (4 mmol) • Pregnancy: >60 (3. 3 mmol) • <10% of readings below target at each time of day • No severe lows
Hypoglycemia Prevention Strategies 1. Insulin Program Setup (background/basal)
Hypoglycemia Prevention Strategies 1. Insulin Program Setup (background/basal)
Hypoglycemia Prevention Strategies 1. Insulin Program Setup (background/basal)
Hypoglycemia Prevention Strategies 1. Insulin Program Setup (background/basal)
Hypoglycemia Prevention Strategies 1. Insulin Program Setup (background/basal) Basal insulin should hold BG STEADY in the absence of food, exercise and bolus insulin!
Hypoglycemia Prevention Strategies 1 b. Insulin Program Setup (Meal/Bolus) Only rapid analogs work when needed – right after eating!
Hypoglycemia Prevention Strategies 2. Meal/Snack Timing ü Major issue w/a. m. NPH/Lente ü Minor issue w/Lantus or Levemir ü Not usually an issue with pump use
Hypoglycemia Prevention Strategies 3 a. Proper Correction Doses • 1500 -Rule (aggressive) (83 rule) • 1800 -Rule (conservative) (100 rule) (Total Daily Ins. )/1500 or 1800 • May vary day vs. night (nighttime often 50% more than day)
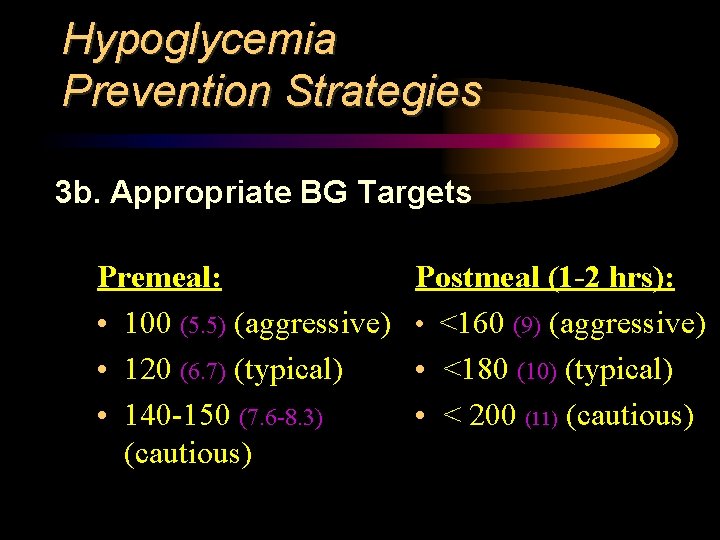
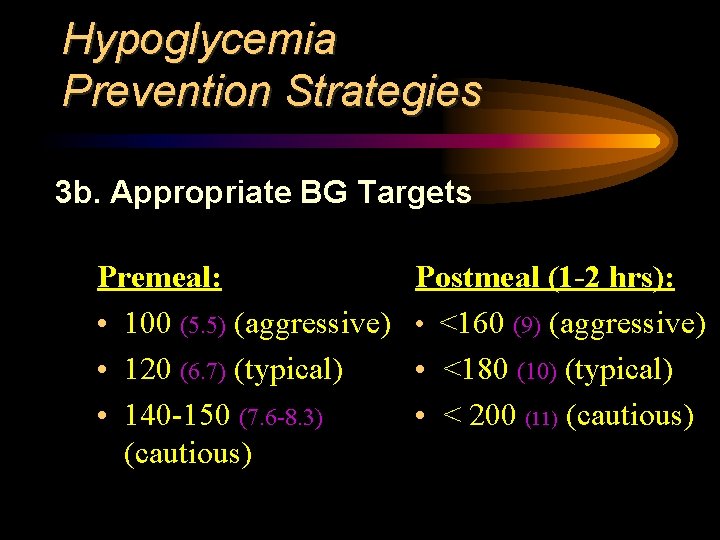
Hypoglycemia Prevention Strategies 3 b. Appropriate BG Targets Premeal: • 100 (5. 5) (aggressive) • 120 (6. 7) (typical) • 140 -150 (7. 6 -8. 3) (cautious) Postmeal (1 -2 hrs): • <160 (9) (aggressive) • <180 (10) (typical) • < 200 (11) (cautious)
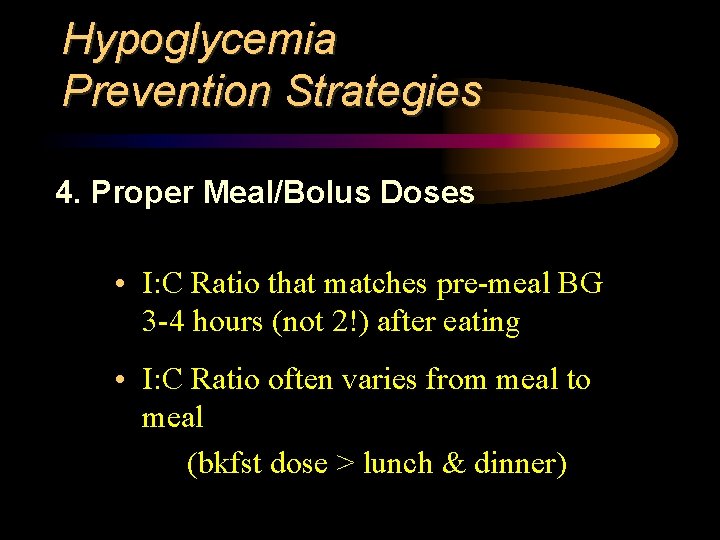
Hypoglycemia Prevention Strategies 4. Proper Meal/Bolus Doses • I: C Ratio that matches pre-meal BG 3 -4 hours (not 2!) after eating • I: C Ratio often varies from meal to meal (bkfst dose > lunch & dinner)
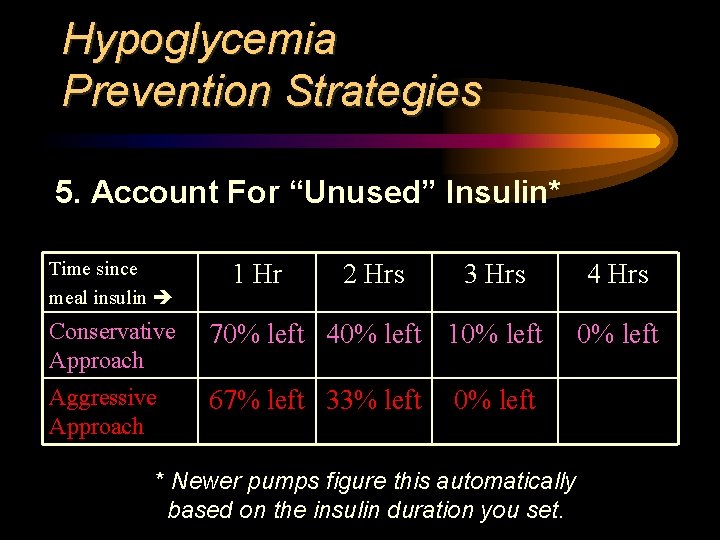
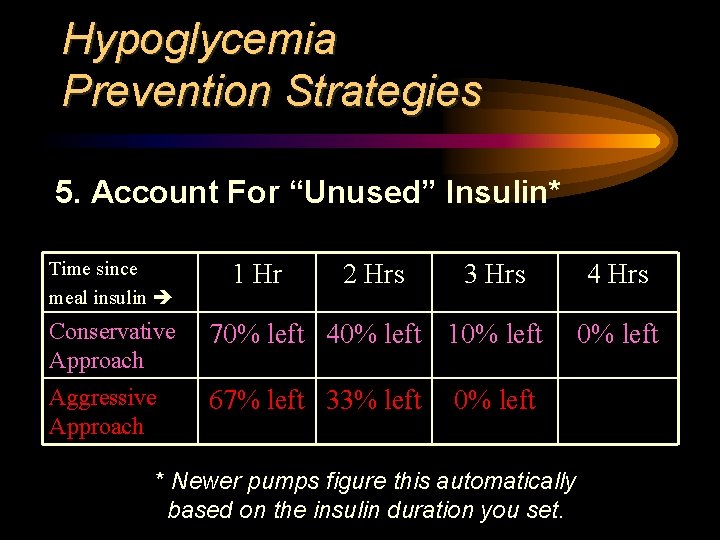
Hypoglycemia Prevention Strategies 5. Account For “Unused” Insulin* Time since meal insulin 1 Hr 2 Hrs 3 Hrs Conservative Approach 70% left 40% left 10% left Aggressive Approach 67% left 33% left 0% left * Newer pumps figure this automatically based on the insulin duration you set. 4 Hrs 0% left
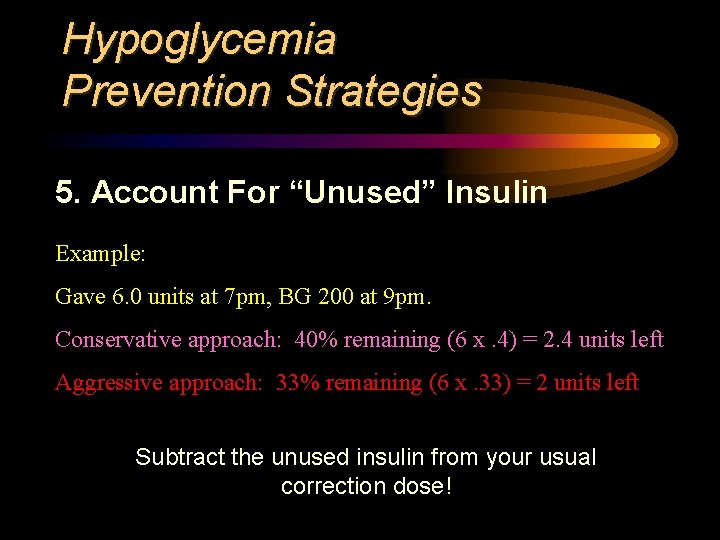
Hypoglycemia Prevention Strategies 5. Account For “Unused” Insulin Example: Gave 6. 0 units at 7 pm, BG 200 at 9 pm. Conservative approach: 40% remaining (6 x. 4) = 2. 4 units left Aggressive approach: 33% remaining (6 x. 33) = 2 units left Subtract the unused insulin from your usual correction dose!
Hypoglycemia Prevention Strategies 6. Carb Counting Accuracy • Proper Portion Measurement • Look Up Unknown / Restaurant Foods • Use Carb Factors • Subtract 100% of Fiber • Subtract 50% of Sugar Alcohols
Hypoglycemia Prevention Strategies 7. Extend Meal Insulin When Necessary Use When: • Portions are very large • Meal is prolonged • Food is low-glycemic index (pasta, legumes, dairy…) Apply Via: • Square/Dual/Extended/Combo bolus on pump • Delayed or Split bolus on injections
Hypoglycemia Prevention Strategies 8. Adjustment for Physical Activity ü Exercise, recreation, chores: all count! ü Reduce meal insulin (25%, 33%, 50%) after-meal activity for ü Snack prior to before/between meal activity ü Lower long-acting/basal insulin during and after prolonged activity
Hypoglycemia Prevention Strategies 8. Watch Out for D’OH! (Delayed Onset Hypoglycemia) ü Following High-Intensity Exercise ü Following Extended Duration Activity ü May Occur Up to 24 Hours After ü Adjustments to food/insulin after activity: o lower basal insulin for 8 -12 hours o low-G. I. Snacks o lower mealtime boluses
Hypoglycemia Prevention Strategies 9. Adjustment for Alcohol ü Alcohol reduces the liver’s output of glucose and masks hypoglycemic symptoms ü Delayed BG drops can occur ü Decrease basal insulin (or overnight long-acting insulin) after drinking
Hypoglycemia Prevention Strategies 10. Consistent Monitoring ü Before All Meals & Snacks ü Pre/Post Exercise ü Bedtime ü 3 a. m. (occasionally)
Hypoglycemia Prevention Strategies 11. Recording & Analysis ü Record all pertinent data § BGs § Carb § Activity § Insulin ü Use an organized form (multiple days on single page, if possible)
Hypoglycemia Prevention Strategies 11. Recording & Analysis ü Review every 7 -10 days ü Look for patterns § > 10% below target range @ given time § Lows during/post-activity § Lows on School/Work vs. off-day § Lows Post-Menstrual
Hypoglycemia Prevention Strategies 12. Continuous Glucose Monitoring ü Alarms to alert user/family of pending lows
Hypoglycemia Prevention Strategies 12. Continuous Glucose Monitoring
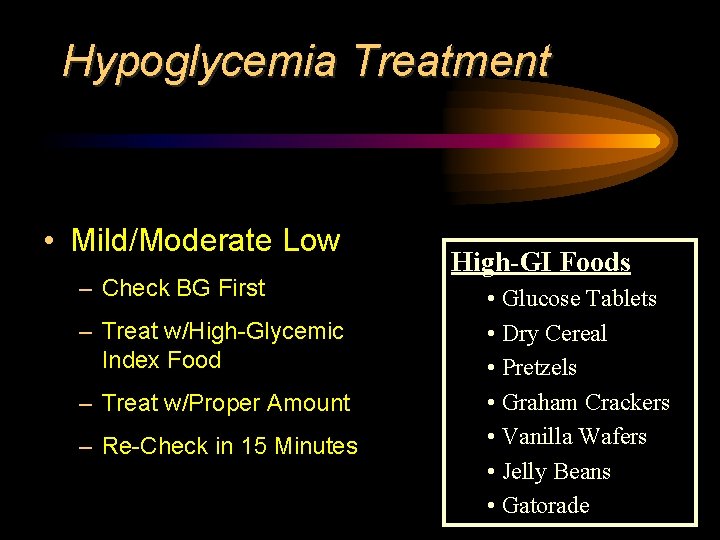
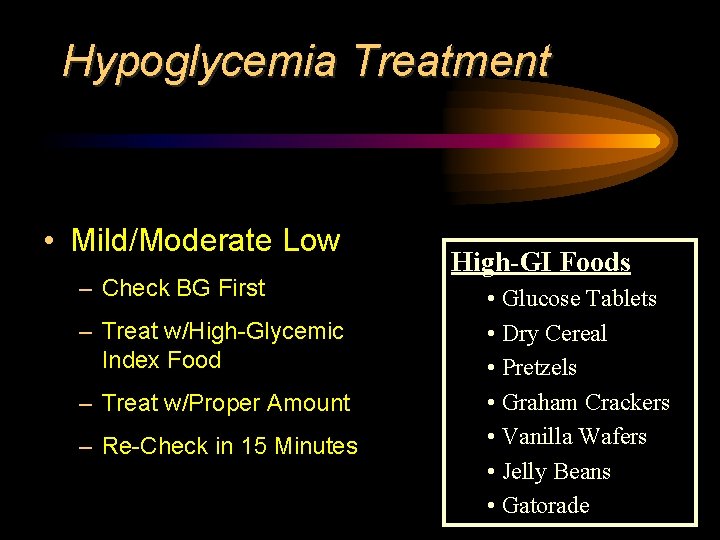
Hypoglycemia Treatment • Mild/Moderate Low – Check BG First – Treat w/High-Glycemic Index Food – Treat w/Proper Amount – Re-Check in 15 Minutes High-GI Foods • Glucose Tablets • Dry Cereal • Pretzels • Graham Crackers • Vanilla Wafers • Jelly Beans • Gatorade
Hypoglycemia Treatment Use of Glycemic Index – Lower GI foods digest & convert to glucose more slowly – High-fiber slower than low – Hi-fat slower than low – Solids slower than liquids – Cold foods slower than hot – Type of sugar/starch affects GI
Hypoglycemia Treatment Use of Glycemic Index (contd)
Hypoglycemia Treatment • Always Carry Rapid-Acting Carbs!
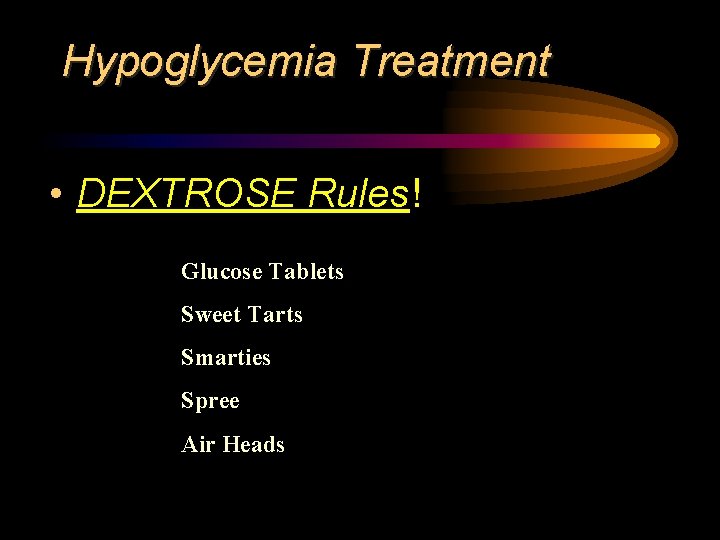
Hypoglycemia Treatment • DEXTROSE Rules! Glucose Tablets Sweet Tarts Smarties Spree Air Heads
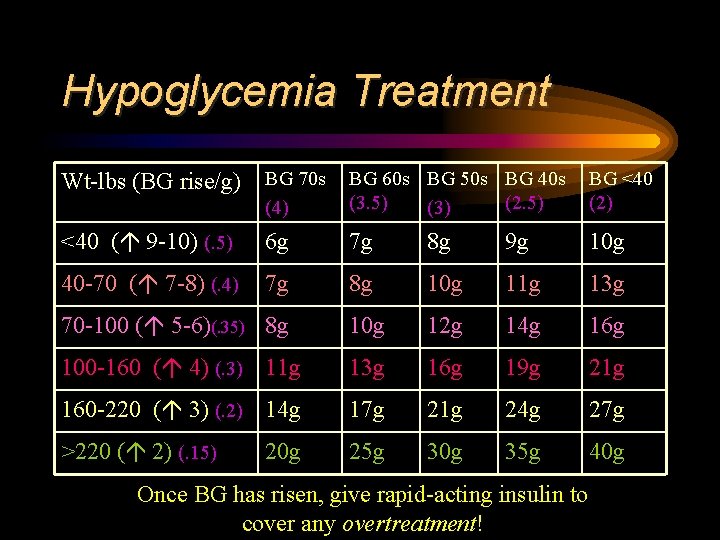
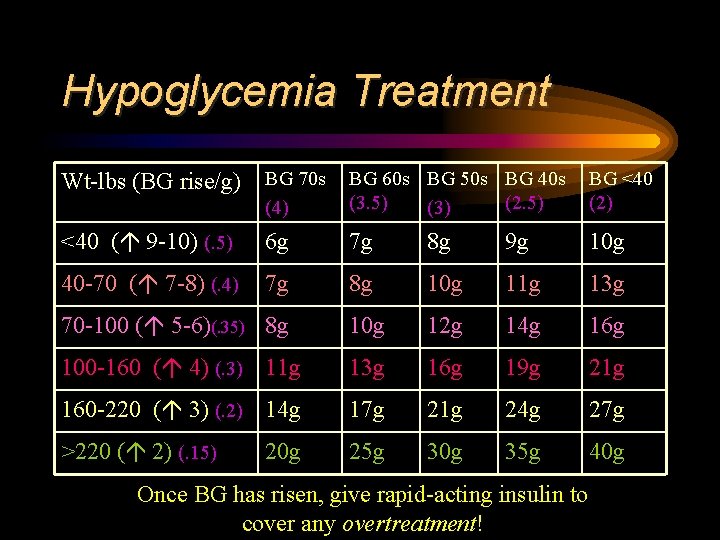
Hypoglycemia Treatment Wt-lbs (BG rise/g) BG 70 s (4) BG 60 s BG 50 s BG 40 s (3. 5) (2. 5) (3) BG <40 (2) <40 ( 9 -10) (. 5) 6 g 7 g 8 g 9 g 10 g 40 -70 ( 7 -8) (. 4) 7 g 8 g 10 g 11 g 13 g 70 -100 ( 5 -6)(. 35) 8 g 10 g 12 g 14 g 16 g 100 -160 ( 4) (. 3) 11 g 13 g 16 g 19 g 21 g 160 -220 ( 3) (. 2) 14 g 17 g 21 g 24 g 27 g >220 ( 2) (. 15) 25 g 30 g 35 g 40 g 20 g Once BG has risen, give rapid-acting insulin to cover any overtreatment!
Hypoglycemia Treatment “Idiosyncracies” Treatment amt. for insulin on board Treatment amt. for recent exercise âTreatment amt. for previous low-G. I. foods
Hypoglycemia Treatment • Severe Low – Unconscious / Unresponsive – Seizure – Uncooperative
Take-Home Messages • Quantify Your Lows • Strategize to Minimize • Plan for Proper Treatment

The Source of My Highs and Lows
 Gary scheiner ms cde
Gary scheiner ms cde Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Sukkot wiki
Sukkot wiki Aberrometry definition
Aberrometry definition Zach scheiner
Zach scheiner Insulin action
Insulin action Hypoglycemia factitia
Hypoglycemia factitia Hypoglycemia without diabetes
Hypoglycemia without diabetes Drugs causing hypoglycemia mnemonic
Drugs causing hypoglycemia mnemonic Starvation diabetes mellitus
Starvation diabetes mellitus Hypoglycemia mnemonic
Hypoglycemia mnemonic Hypoglycemia
Hypoglycemia Niphs symptoms
Niphs symptoms Nursing care plan for diabetes mellitus slideshare
Nursing care plan for diabetes mellitus slideshare Hypoglycemia cpg
Hypoglycemia cpg Cheese identification
Cheese identification Okstate cde
Okstate cde Cde ascent
Cde ascent Gmu cde
Gmu cde Calliphoridae
Calliphoridae Cde ced rima
Cde ced rima Cteig allowable expenses
Cteig allowable expenses Cde elat
Cde elat Cde uip
Cde uip Aroma cde
Aroma cde Tree identification nc
Tree identification nc Ornamental horticulture demonstrations ideas
Ornamental horticulture demonstrations ideas Cde eeos
Cde eeos Cde data pipeline
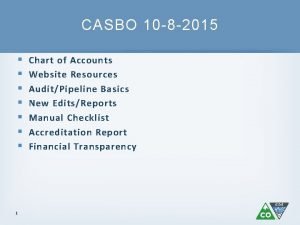
Cde data pipeline Cde chart of accounts
Cde chart of accounts Cde ffa definition
Cde ffa definition Ffa food science cde
Ffa food science cde Lesson 5-2 bisectors in triangles answer key
Lesson 5-2 bisectors in triangles answer key Expression tree
Expression tree Ffa cheese identification
Ffa cheese identification Google scholar
Google scholar Owner occupied housing gdp
Owner occupied housing gdp Hadie perkas
Hadie perkas Mauricio the owner of pizza aroma
Mauricio the owner of pizza aroma Product owner
Product owner Dilbert scrum
Dilbert scrum Mauricio the owner of pizza aroma
Mauricio the owner of pizza aroma Process owner
Process owner Building owner chapter 18
Building owner chapter 18 Creditcont
Creditcont Florent lothon
Florent lothon