Dawn Mc Carter MS RN CDE manager CDE







- Slides: 37

Dawn Mc. Carter MS, RN, CDE manager CDE program Jana Beckering RN quality project coordinator
Disclosure to Participants Dawn Mc Carter and Jana Beckering have had no personal financial relationship within the last 12 months with a manufacturer of the products or services discussed in his presentation.
Learning Objectives: At the completion of this presentation, the participant will be able to: – Describe how the triple aim fits into a multiple clinic DSME program. – Identify the tactics used from the triple aim model to improve outcomes in a DSME program. – Describe how a dashboard provides data needed for improving outcomes in a DSME program.
Allina Health is a notfor-profit health system consisting of clinics, hospitals, and other health services, providing care throughout Minnesota and western Wisconsin.

Incorporating the Tripe Aim into your DSME Program ES OU OM C T AG ST CO G EN NT E EM

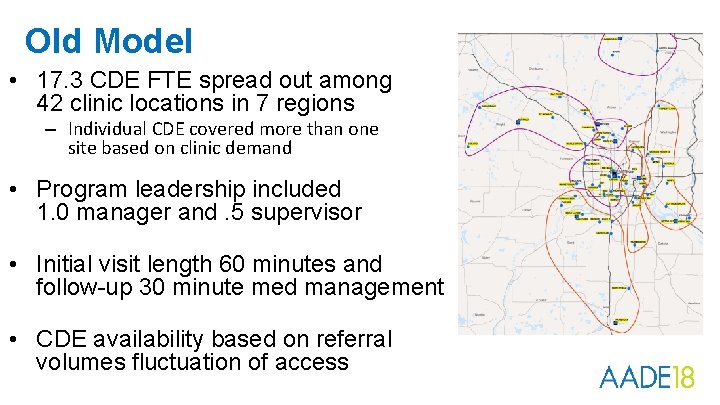
Old Model • 17. 3 CDE FTE spread out among 42 clinic locations in 7 regions – Individual CDE covered more than one site based on clinic demand • Program leadership included 1. 0 manager and. 5 supervisor • Initial visit length 60 minutes and follow-up 30 minute med management • CDE availability based on referral volumes fluctuation of access
Revenue Iceberg CDE travel time 5 Current no-show rate up to 16% Up to 5 week scheduling backlog 4 1 2 3 Slow response time to messages High rate of nonproductive time

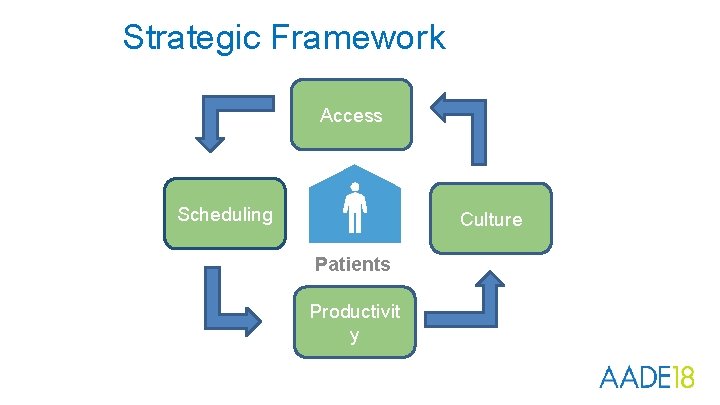
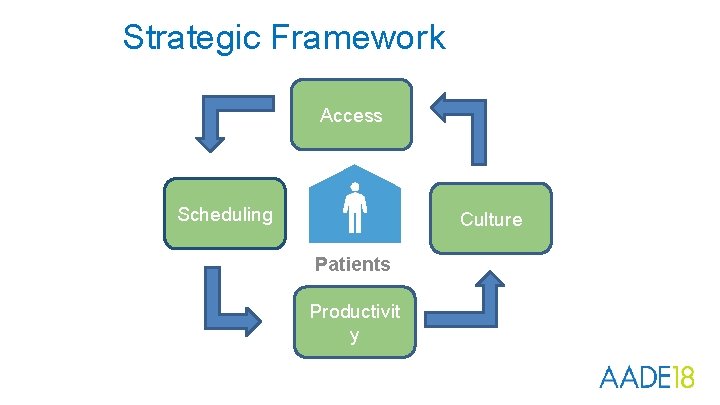
Strategic Framework Access Scheduling Culture Patients Productivit y
Begin with “No Surprises” Communication 1. Develop the why and how of the model 2. Communicate the model with leadership ü Listen to and address their concerns ü Gain their support ü Provide the “What we need from you” 3. Meet with CDEs 4. Meet with clinic staff that will be affected
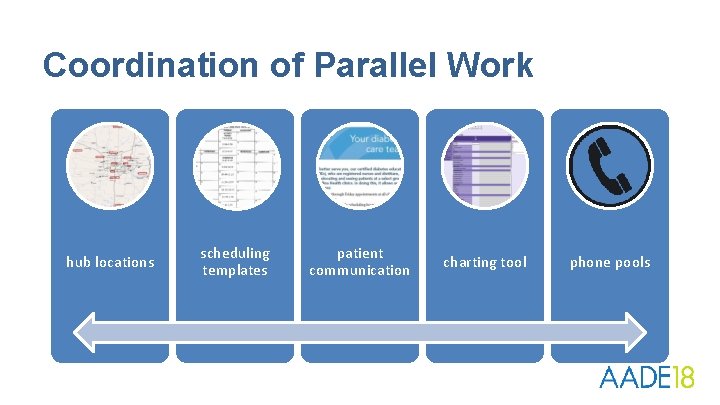
Coordination of Parallel Work hub locations scheduling templates patient communication charting tool phone pools

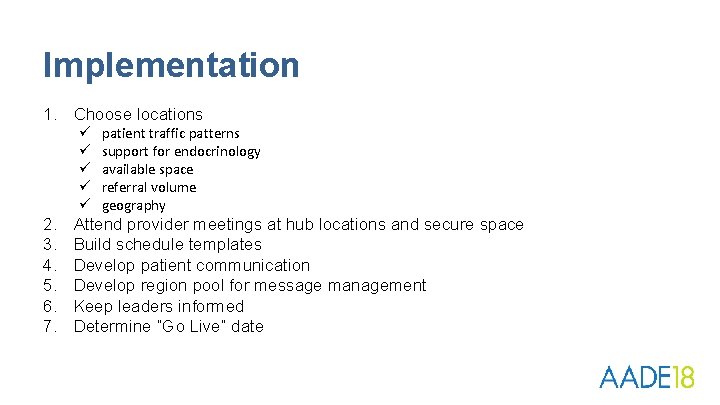
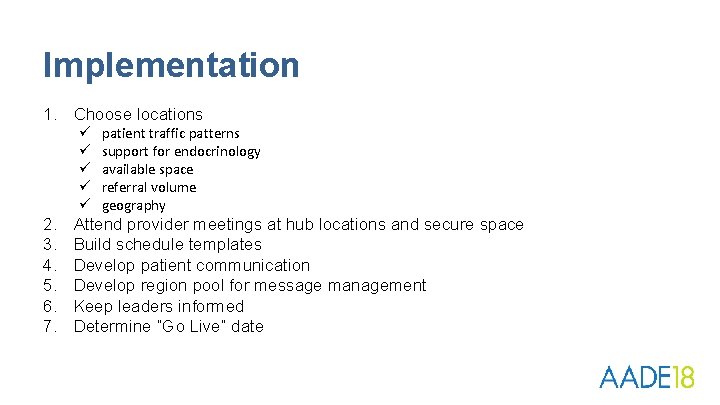
Implementation 1. Choose locations ü ü ü 2. 3. 4. 5. 6. 7. patient traffic patterns support for endocrinology available space referral volume geography Attend provider meetings at hub locations and secure space Build schedule templates Develop patient communication Develop region pool for message management Keep leaders informed Determine “Go Live” date
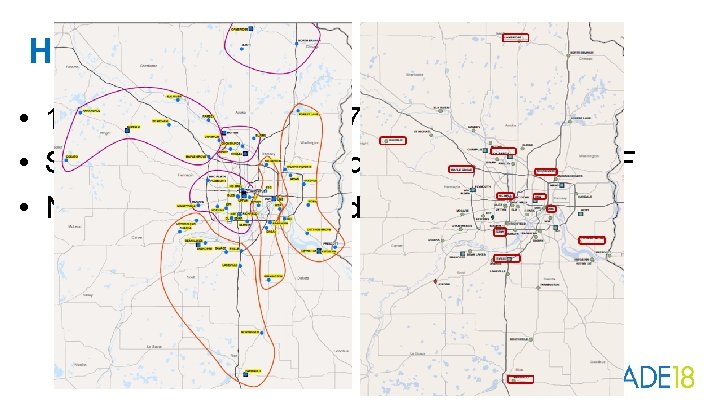
Hub Locations • 12 locations covering 7 regions • Services offered at each hub location M - F • Near elimination of mid-day travel by CDE
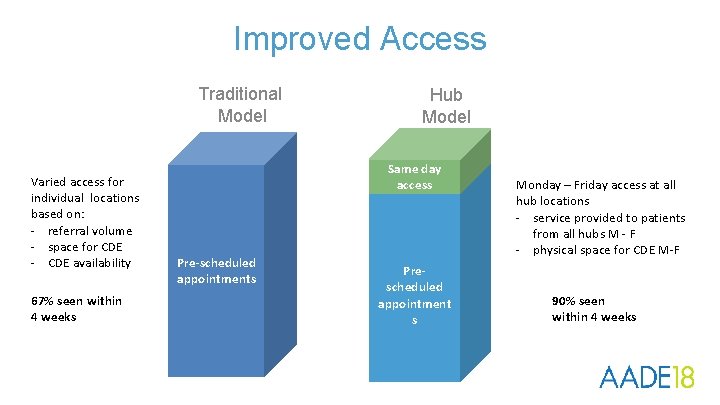
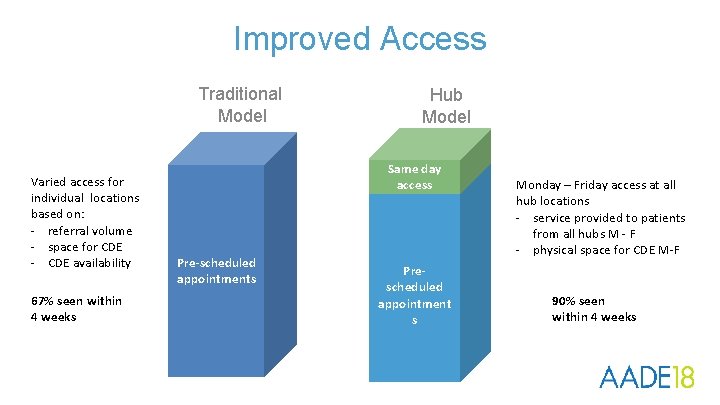
Improved Access Traditional Model Varied access for individual locations based on: - referral volume - space for CDE - CDE availability 67% seen within 4 weeks Hub Model Same day access Pre-scheduled appointments Prescheduled appointment s Monday – Friday access at all hub locations - service provided to patients from all hubs M - F - physical space for CDE M-F 90% seen within 4 weeks
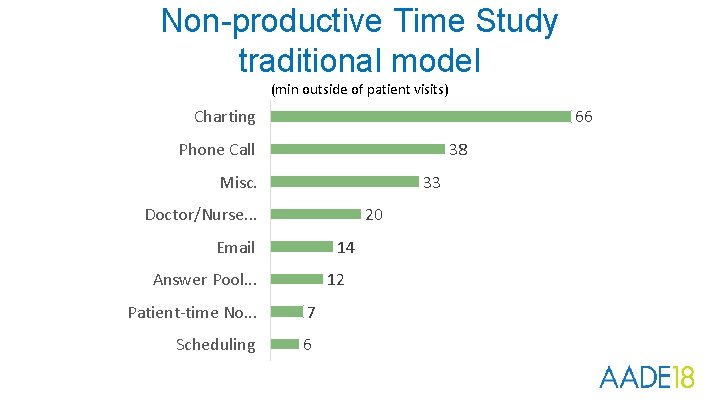
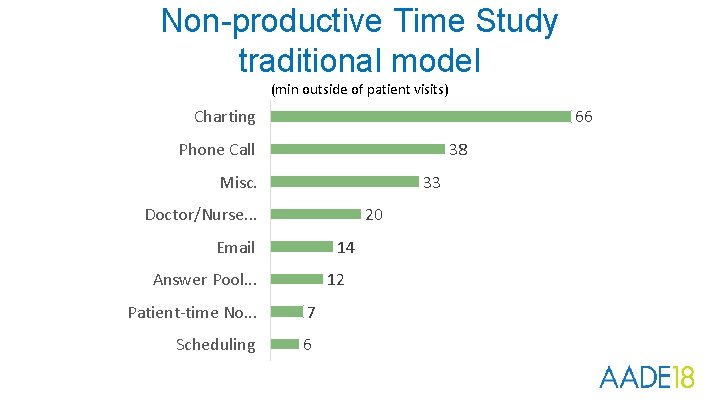
Non-productive Time Study traditional model (min outside of patient visits) 66 Charting Phone Call 38 33 Misc. 20 Doctor/Nurse. . . Email 14 Answer Pool. . . 12 Patient-time No. . . 7 Scheduling 6
Greatest Opportunities Better utilize Patient-CDE time by relieving non-productive tasks and time. charting phone calls
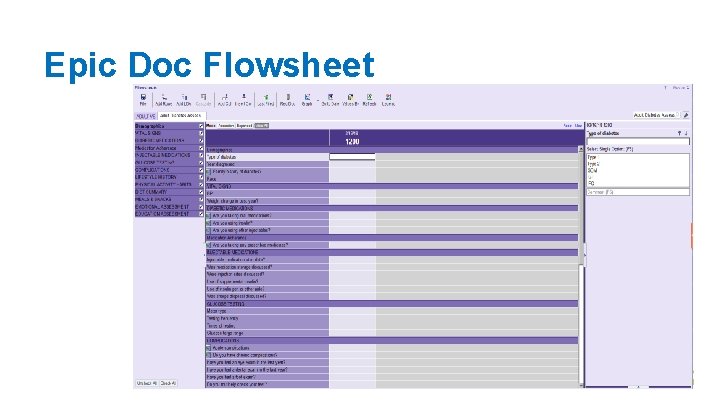
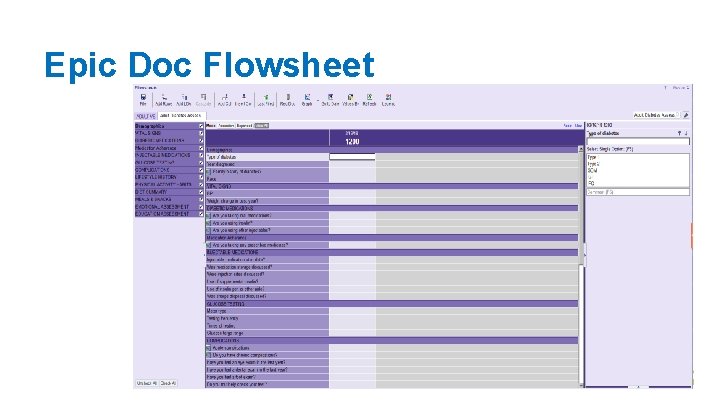
Epic Doc Flowsheet
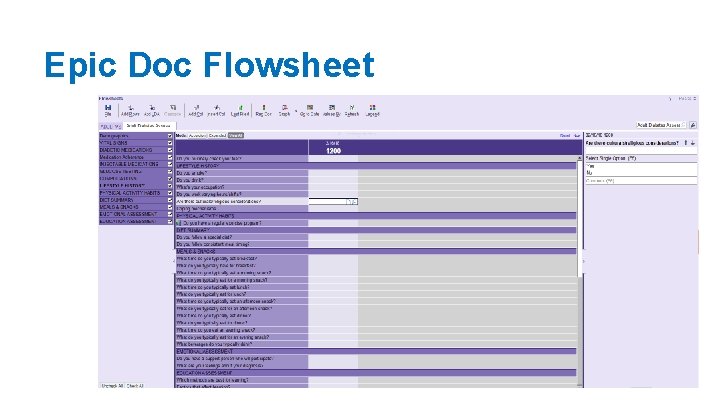
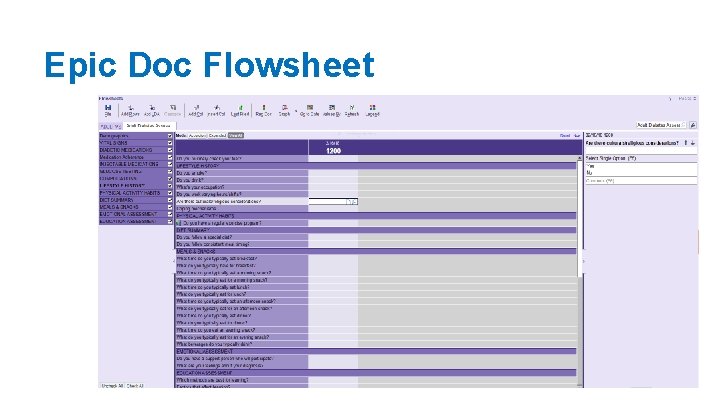
Epic Doc Flowsheet
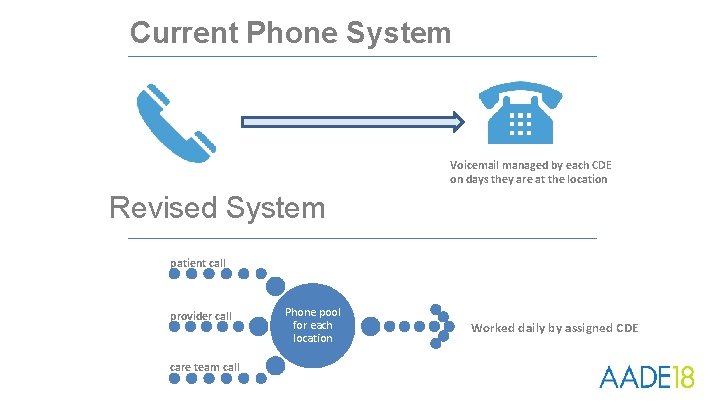
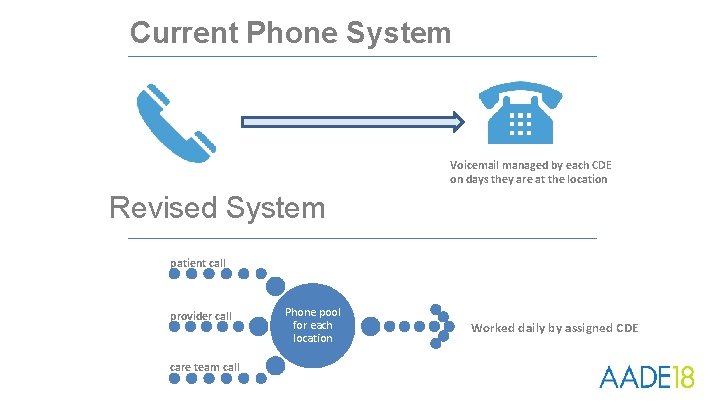
Current Phone System Voicemail managed by each CDE on days they are at the location Revised System patient call provider call care team call Phone pool for each location Worked daily by assigned CDE
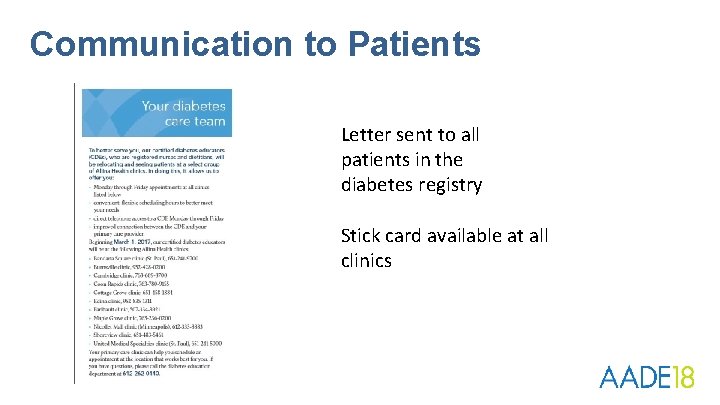
Communication to Patients Letter sent to all patients in the diabetes registry Stick card available at all clinics
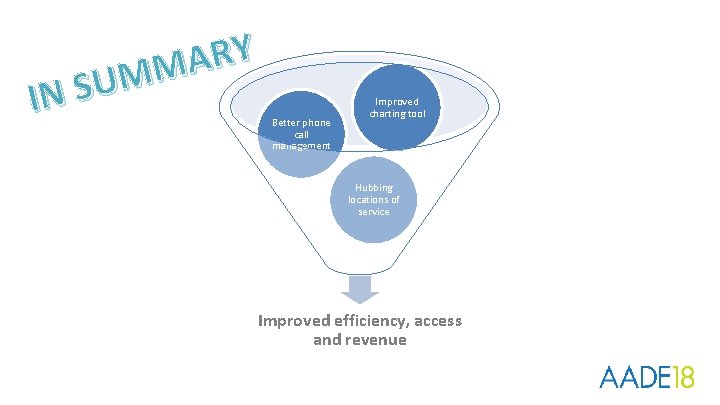
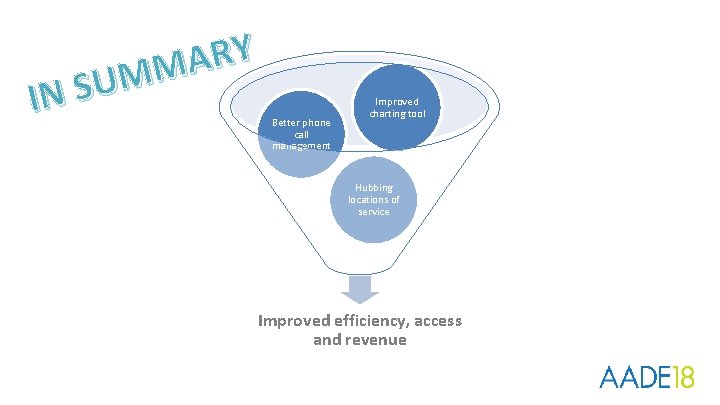
Y R A M M IN SU Better phone call management Improved charting tool Hubbing locations of service Improved efficiency, access and revenue
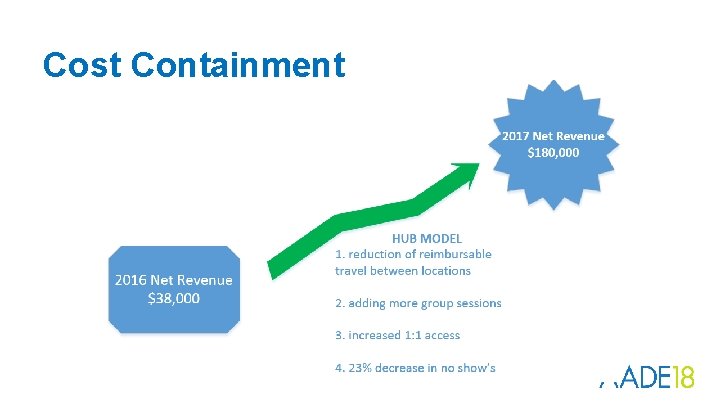
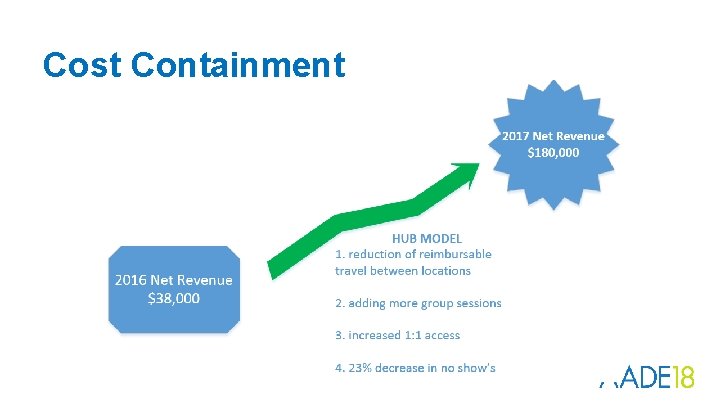
Cost Containment
How did we achieve financial stability/gain • Efficiency in staffing with hub model • Physician referrals – Provider education programs to build relationships/trust – Insulin quick start program • Class volumes vs. location • Significant decrease in travel reimbursement • Offering multiple services – CGMS – MNT – GDM classes
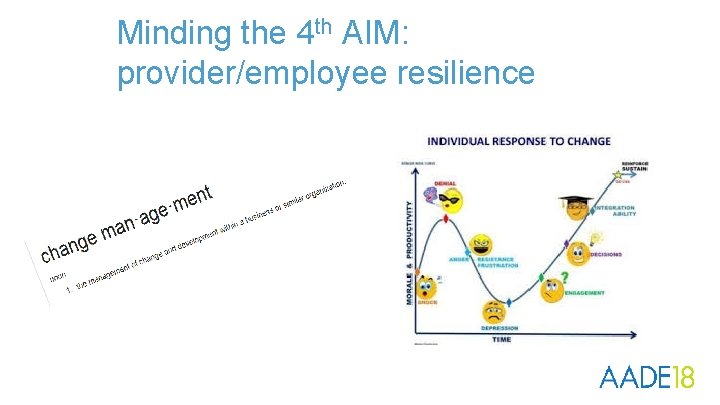
Minding the 4 th AIM: provider/employee resilience
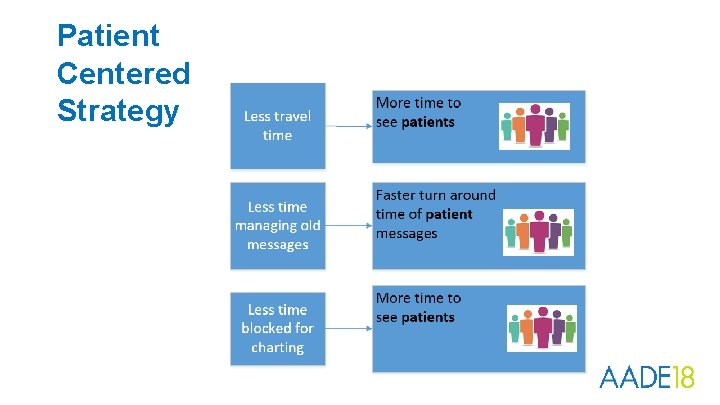
Patient Centered Strategy
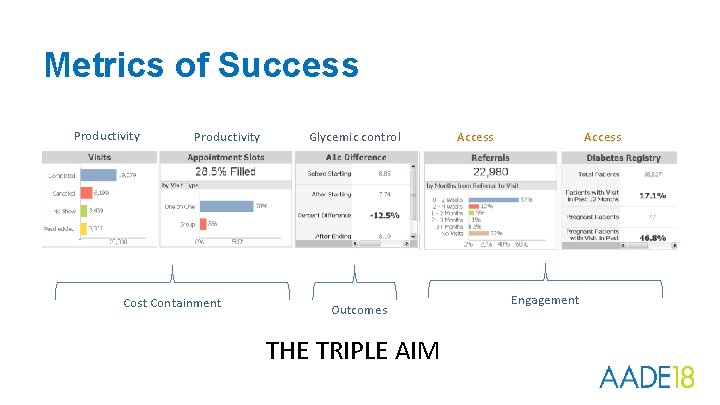
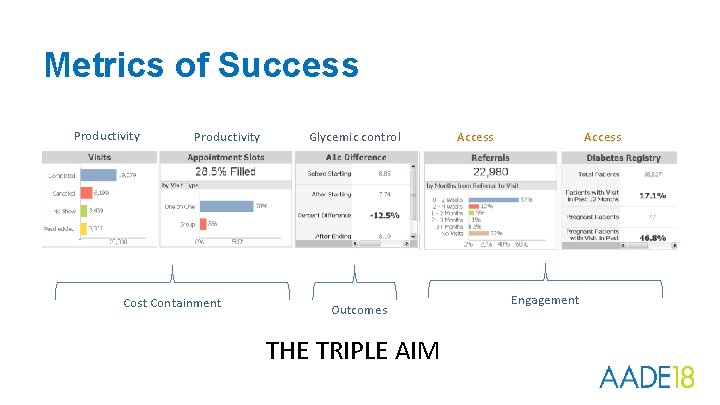
Metrics of Success Productivity Cost Containment Glycemic control Outcomes THE TRIPLE AIM Access Engagement
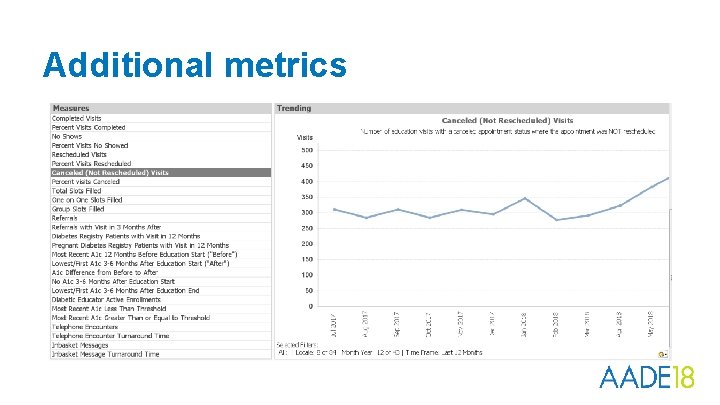
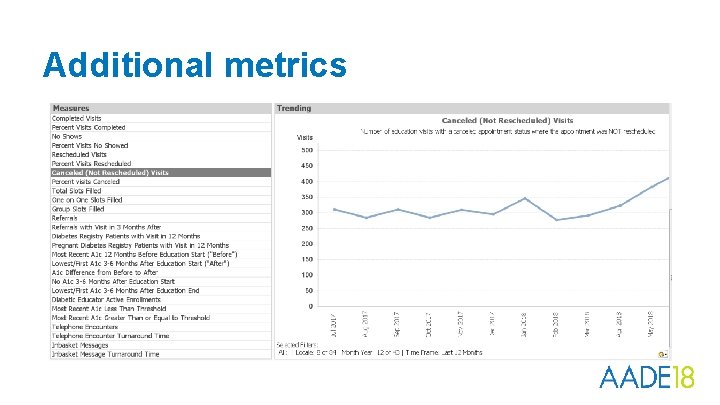
Additional metrics

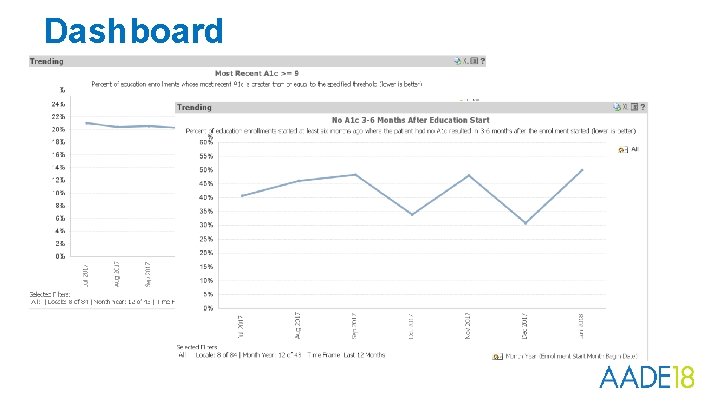
Monitor trends
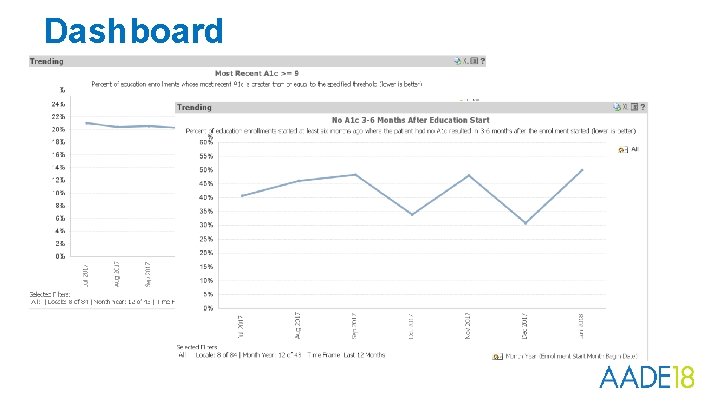
Dashboard
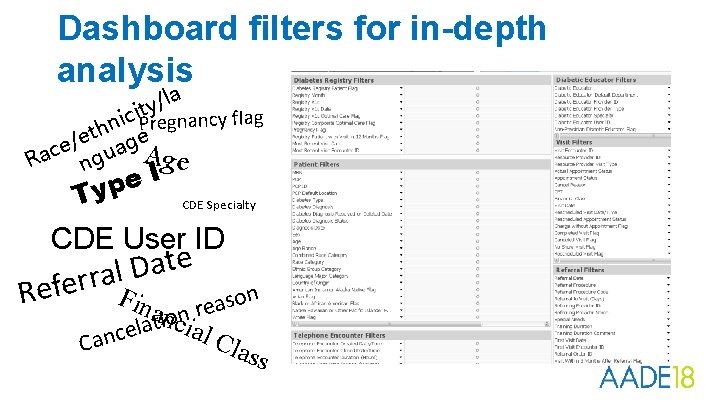
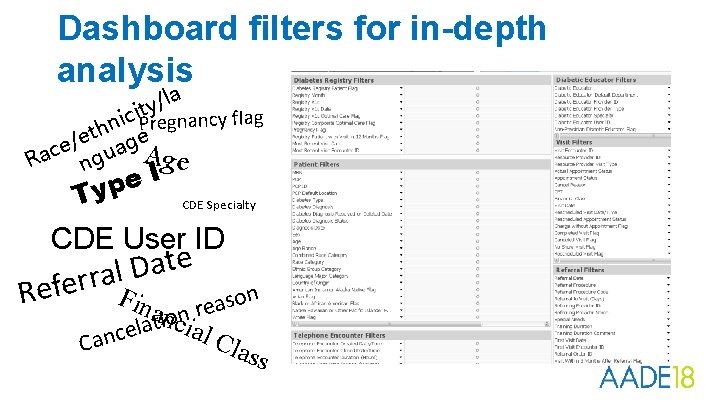
Dashboard filters for in-depth analysis la / y ici. Pt regnancy flag n th e e / e ag A c u a R ng Ige e p y T CDE Specialty CDE User ID e t a D l a r r e f Fina reason Re n ocnia i t a l e c l Cla n a C ss
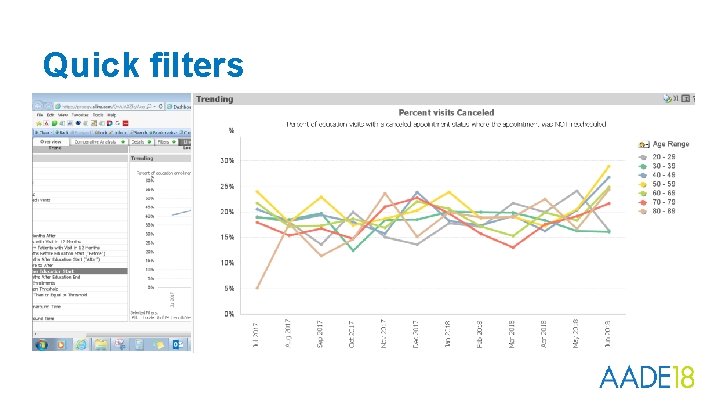
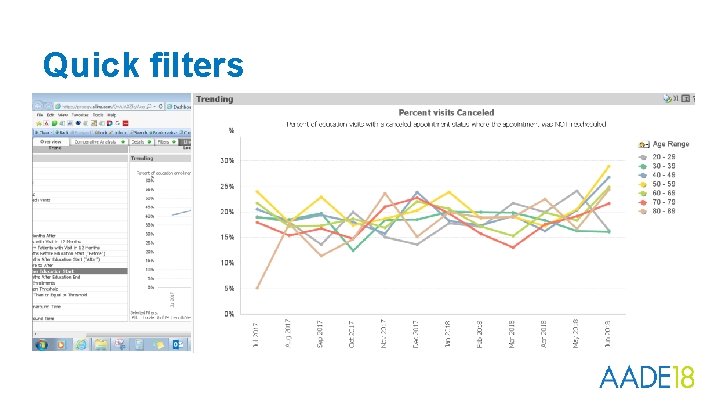
Quick filters
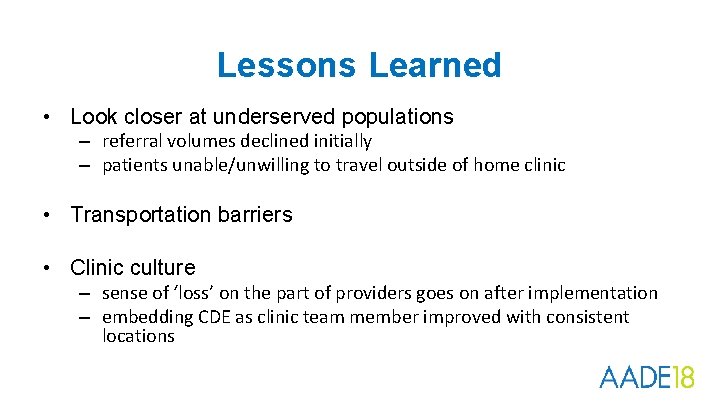
Lessons Learned • Look closer at underserved populations – referral volumes declined initially – patients unable/unwilling to travel outside of home clinic • Transportation barriers • Clinic culture – sense of ‘loss’ on the part of providers goes on after implementation – embedding CDE as clinic team member improved with consistent locations
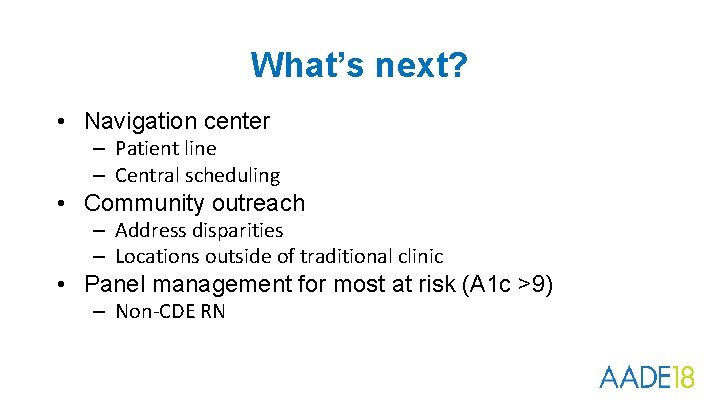
What’s next? • Navigation center – Patient line – Central scheduling • Community outreach – Address disparities – Locations outside of traditional clinic • Panel management for most at risk (A 1 c >9) – Non-CDE RN

Thank You…. . QUESTIONS? dawn. mccarter@allina. com jana. beckering@allina. com