Health Assessment Head Eyes Ears Nose Mouth Neck






- Slides: 59

Health Assessment Head, Eyes, Ears, Nose, Mouth, & Neck
ROS: Head n Recent head trauma? n Loss of consciousness? n Headaches? – Sinus, migraine, neurological n Use of helmet when appropriate? – Occupation, contact sports or cycling, rollerblading, and skateboarding
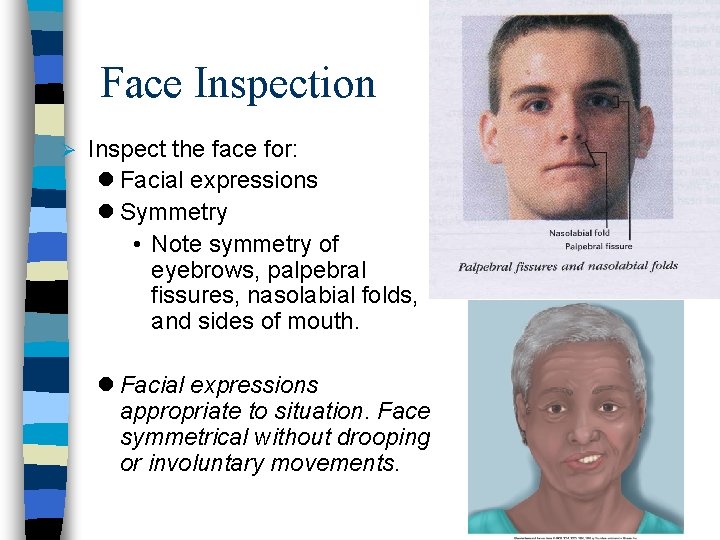
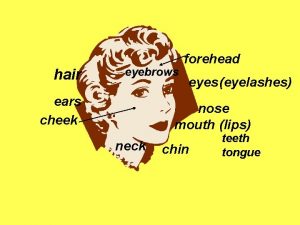
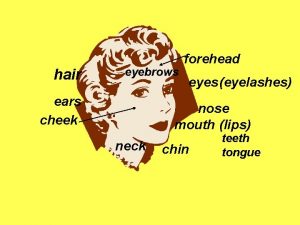
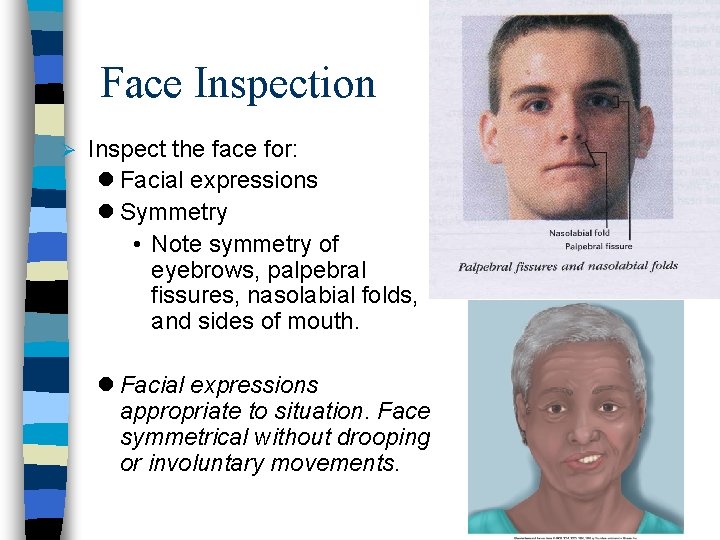
Face Inspection Ø Inspect the face for: l Facial expressions l Symmetry • Note symmetry of eyebrows, palpebral fissures, nasolabial folds, and sides of mouth. l Facial expressions appropriate to situation. Face symmetrical without drooping or involuntary movements.
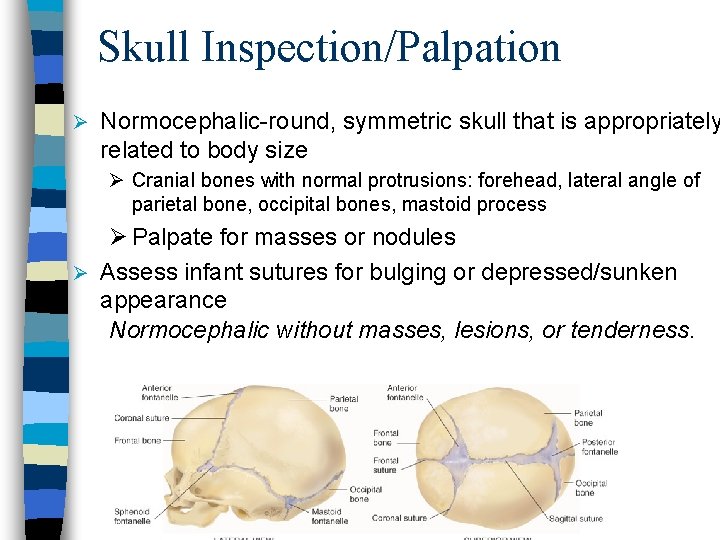
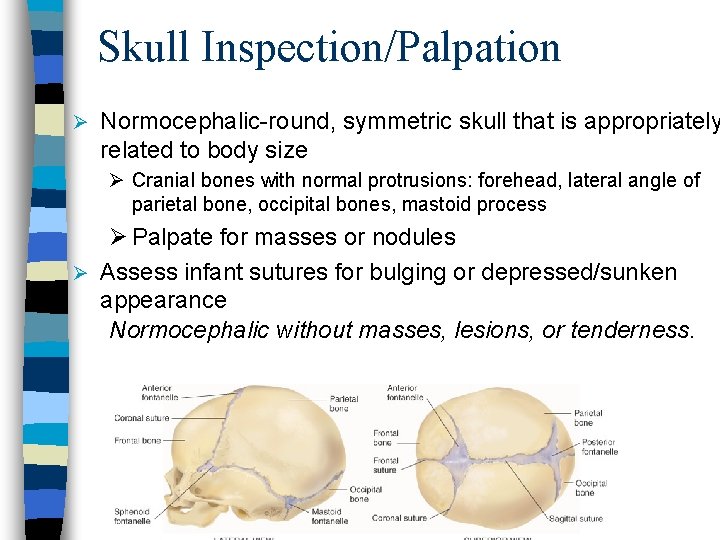
Skull Inspection/Palpation Ø Normocephalic-round, symmetric skull that is appropriately related to body size Ø Cranial bones with normal protrusions: forehead, lateral angle of parietal bone, occipital bones, mastoid process Ø Palpate for masses or nodules Ø Assess infant sutures for bulging or depressed/sunken appearance Normocephalic without masses, lesions, or tenderness.
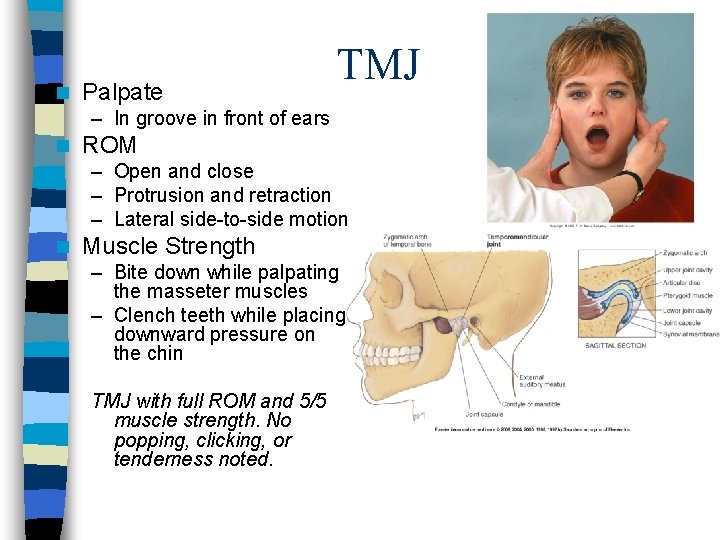
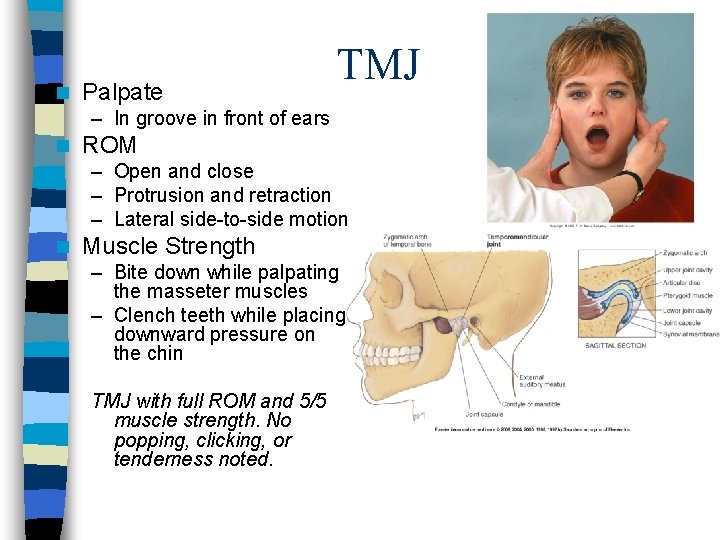
n Palpate TMJ – In groove in front of ears n ROM – Open and close – Protrusion and retraction – Lateral side-to-side motion n Muscle Strength – Bite down while palpating the masseter muscles – Clench teeth while placing downward pressure on the chin TMJ with full ROM and 5/5 muscle strength. No popping, clicking, or tenderness noted.
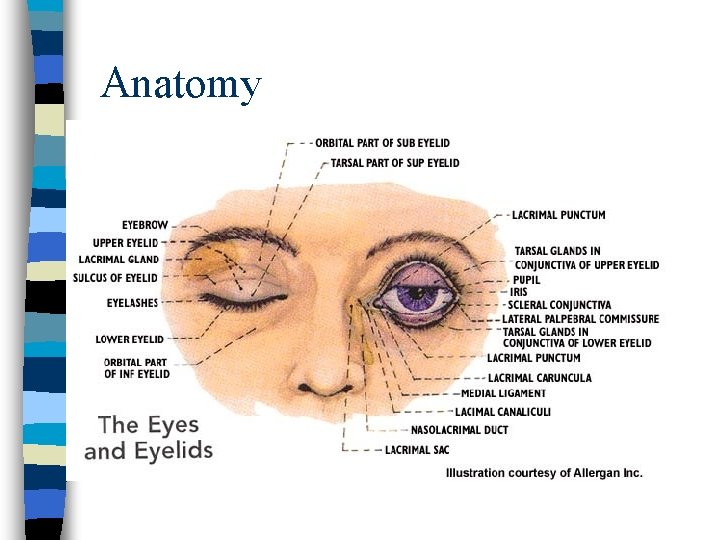
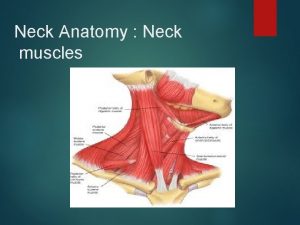
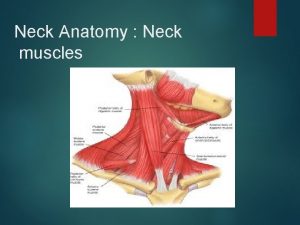
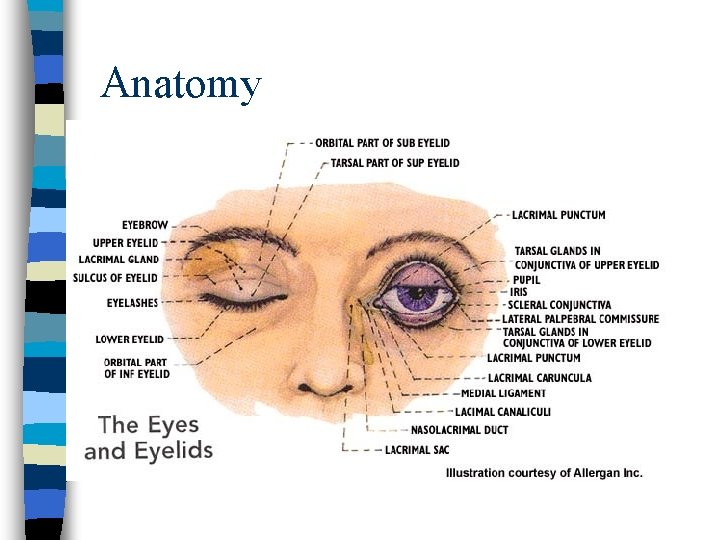
Anatomy

Basics of Vision n Light reflected from image n Light passess through pupil and cornea bends incoming light rays so they will be focus on the inner retina n Retina with sensory neurons n Nerve impulses sent through optic disc
ROS: Eyes Any visual or eye complaints? – Pain, photophobia, burning, itching, excess tearing or crusting, diplopia, blurred vision, “curtain over eye, ” floaters, flashing lights, or halos n Any personal or family history of eye disease? – Glaucoma, retinopathy, cataracts, macular degeneration (Box 33 -13) n • Closed angle (acute) is ocular emergency – sudden ocular pain, halos, red eye, very high pressure in eye, n/v, decreased vision, fixed mid-dilated pupil n Any history of eye trauma, diabetes, hypertension, or eye surgery?
ROS: Eyes n Wear glasses or contacts? n When was last exam by ophthalmologist or optometrist? – <40 y/o every 3 -5 years – >40 y/o every 2 years – >65 y/o, presence of eye disorder, or at risk for eye disease annually or more often if indicated n Use of eye protection when appropriate – Use of chemicals, welding, sawing, fencing, motorcycling
RN Chart Symptoms n n n Burning Discharge Discomfort Dryness Ecchymosis Edema n n n n Itching Pressure Redness Sclera hemorrhage Stye Tearing Visual field loss
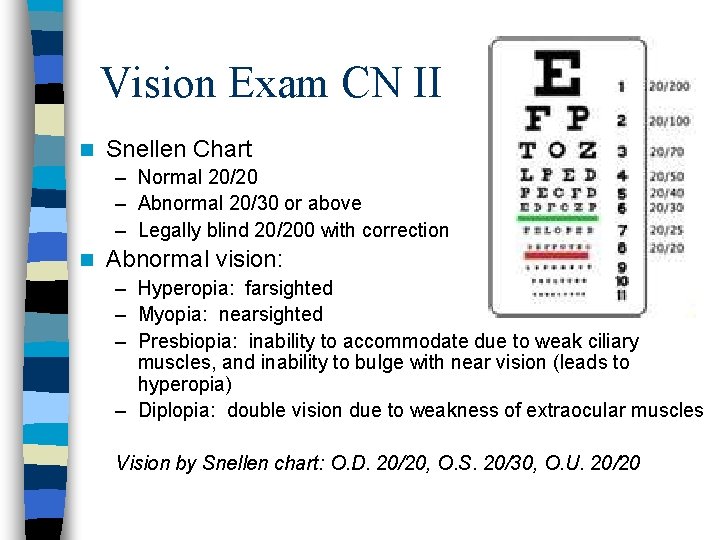
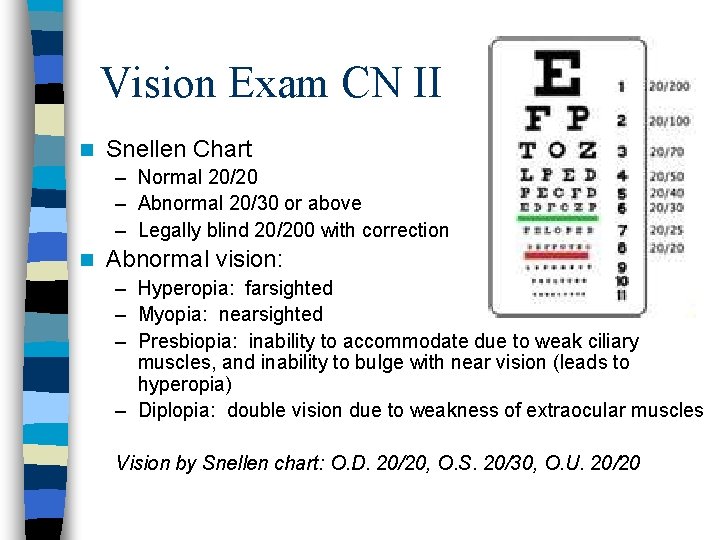
Vision Exam CN II n ………. Snellen Chart – Normal 20/20 – Abnormal 20/30 or above – Legally blind 20/200 with correction n Abnormal vision: – Hyperopia: farsighted – Myopia: nearsighted – Presbiopia: inability to accommodate due to weak ciliary muscles, and inability to bulge with near vision (leads to hyperopia) – Diplopia: double vision due to weakness of extraocular muscles Vision by Snellen chart: O. D. 20/20, O. S. 20/30, O. U. 20/20
Confrontation tests/Peripheral Visual Fields n Gross measure of a patient’s peripheral vision compared to that of your own n Have your patient look at you in the eyes 2 ft away n Move your fingers into the vision field and have the patient state “now” when they can see your fingers. n Normal=when you can see your own fingers at the same time that the patient does n If you find a defect, test each eye separate and establish the boundaries. n Enlarged blind spots occur in glaucoma, optic neuritis and papilledema Peripheral visual fields intact by confrontation test.
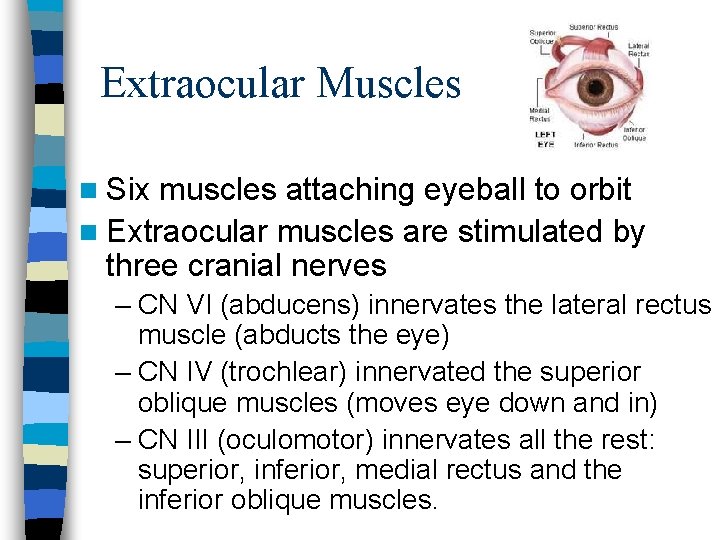
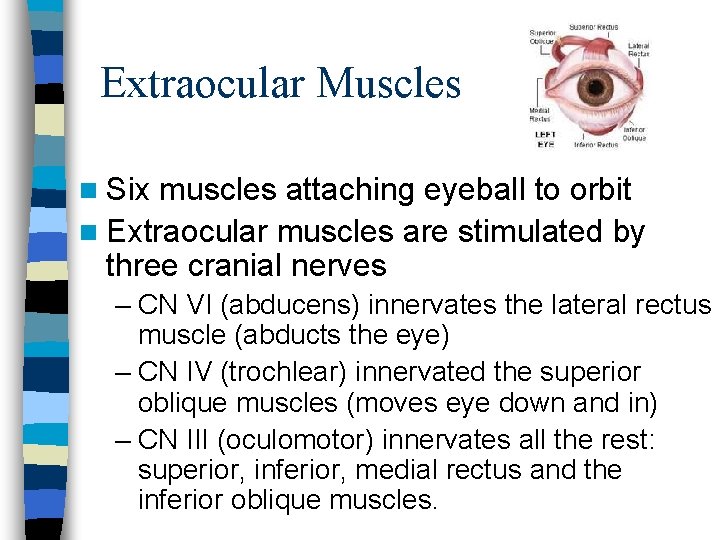
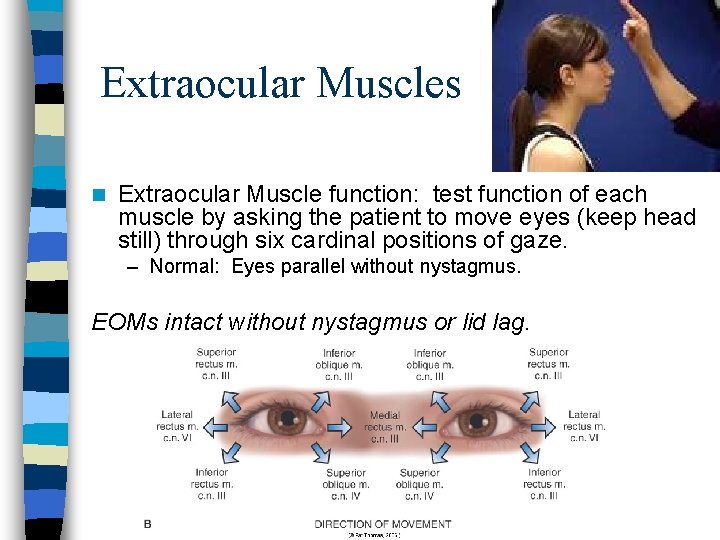
Extraocular Muscles n Six muscles attaching eyeball to orbit n Extraocular muscles are stimulated by three cranial nerves – CN VI (abducens) innervates the lateral rectus muscle (abducts the eye) – CN IV (trochlear) innervated the superior oblique muscles (moves eye down and in) – CN III (oculomotor) innervates all the rest: superior, inferior, medial rectus and the inferior oblique muscles.
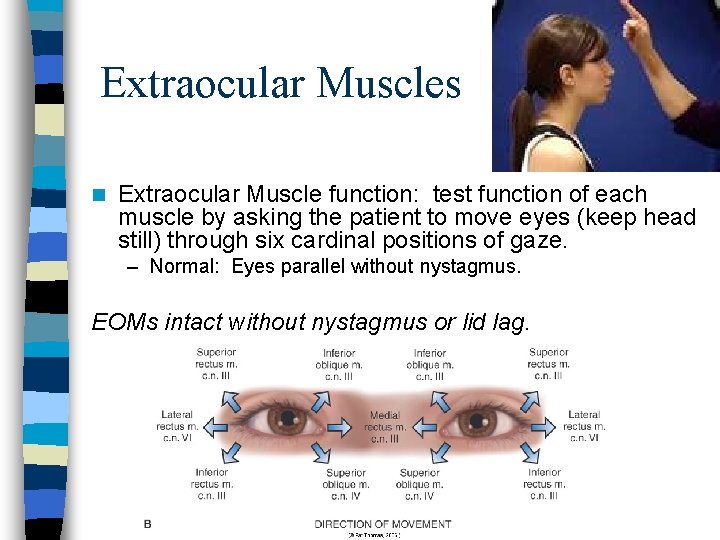
Extraocular Muscles n Extraocular Muscle function: test function of each muscle by asking the patient to move eyes (keep head still) through six cardinal positions of gaze. – Normal: Eyes parallel without nystagmus. EOMs intact without nystagmus or lid lag.
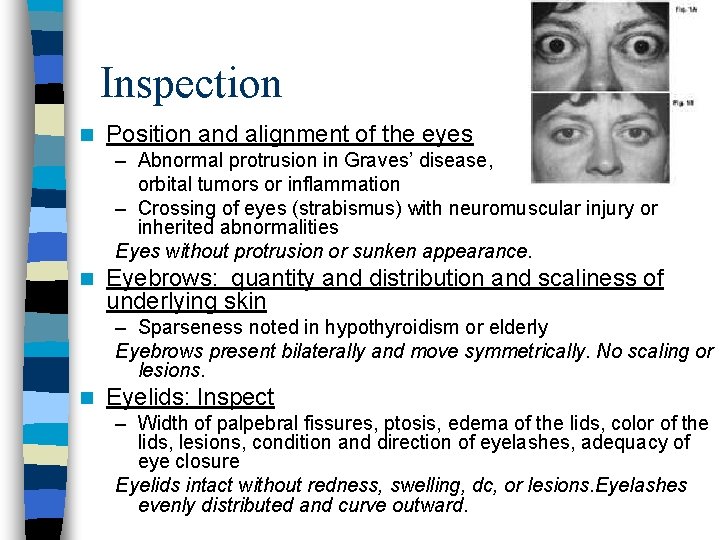
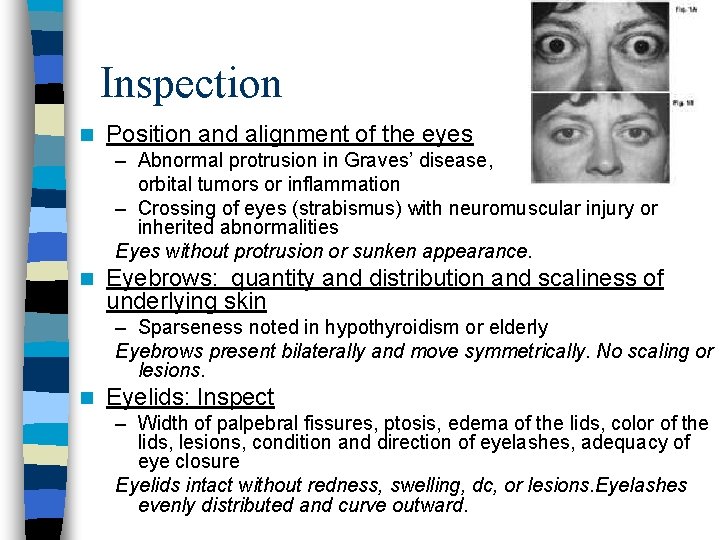
Inspection n Position and alignment of the eyes – Abnormal protrusion in Graves’ disease, orbital tumors or inflammation – Crossing of eyes (strabismus) with neuromuscular injury or inherited abnormalities Eyes without protrusion or sunken appearance. n Eyebrows: quantity and distribution and scaliness of underlying skin – Sparseness noted in hypothyroidism or elderly Eyebrows present bilaterally and move symmetrically. No scaling or lesions. n Eyelids: Inspect – Width of palpebral fissures, ptosis, edema of the lids, color of the lids, lesions, condition and direction of eyelashes, adequacy of eye closure Eyelids intact without redness, swelling, dc, or lesions. Eyelashes evenly distributed and curve outward.
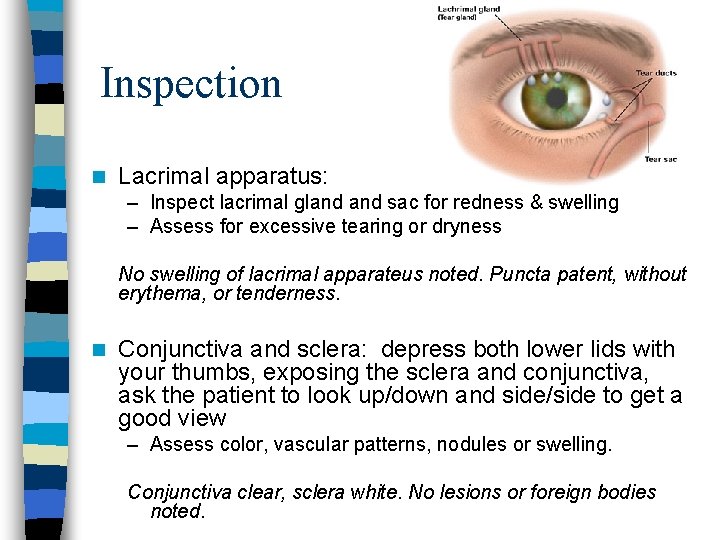
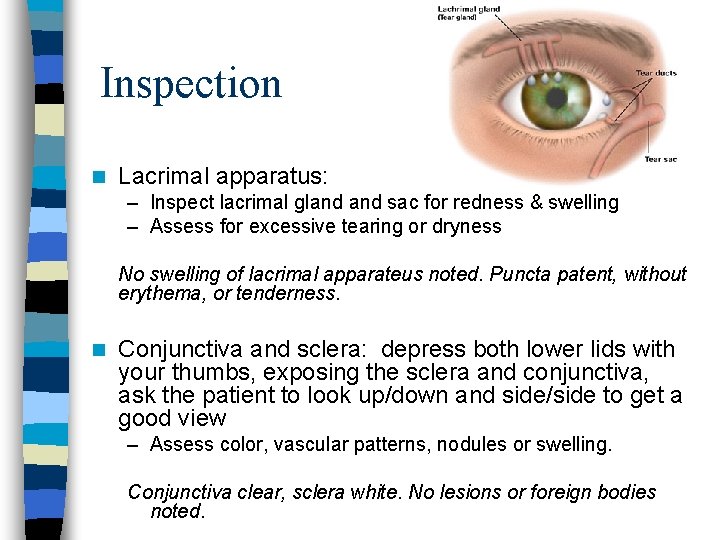
Inspection n Lacrimal apparatus: – Inspect lacrimal gland sac for redness & swelling – Assess for excessive tearing or dryness No swelling of lacrimal apparateus noted. Puncta patent, without erythema, or tenderness. n Conjunctiva and sclera: depress both lower lids with your thumbs, exposing the sclera and conjunctiva, ask the patient to look up/down and side/side to get a good view – Assess color, vascular patterns, nodules or swelling. Conjunctiva clear, sclera white. No lesions or foreign bodies noted.


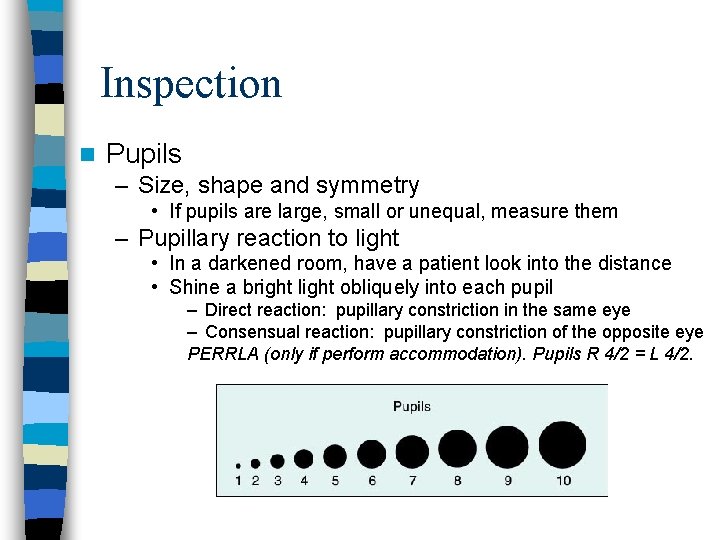
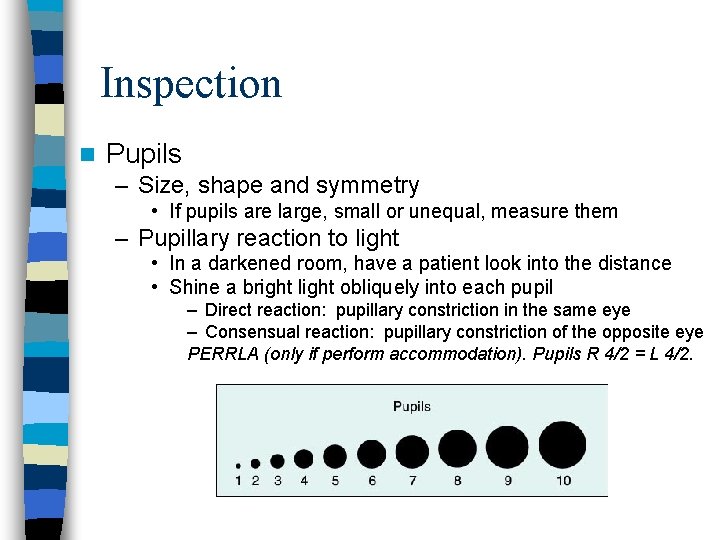
Inspection n Pupils – Size, shape and symmetry • If pupils are large, small or unequal, measure them – Pupillary reaction to light • In a darkened room, have a patient look into the distance • Shine a bright light obliquely into each pupil – Direct reaction: pupillary constriction in the same eye – Consensual reaction: pupillary constriction of the opposite eye PERRLA (only if perform accommodation). Pupils R 4/2 = L 4/2.
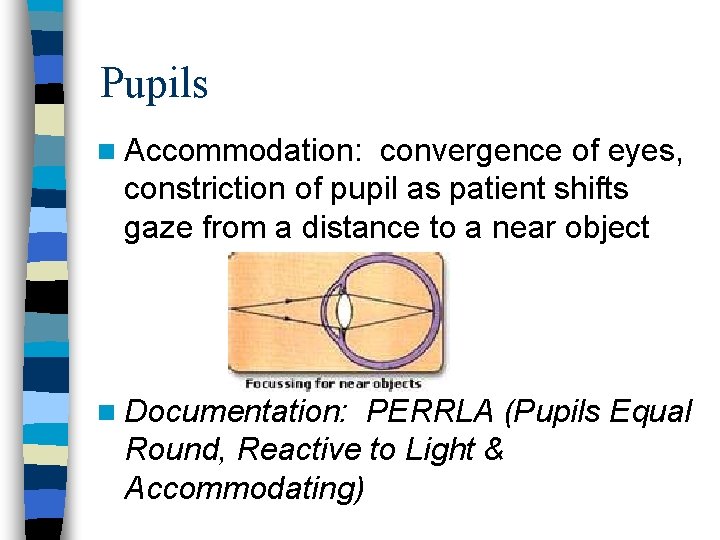
Pupils n Accommodation: convergence of eyes, constriction of pupil as patient shifts gaze from a distance to a near object n Documentation: PERRLA (Pupils Equal Round, Reactive to Light & Accommodating)
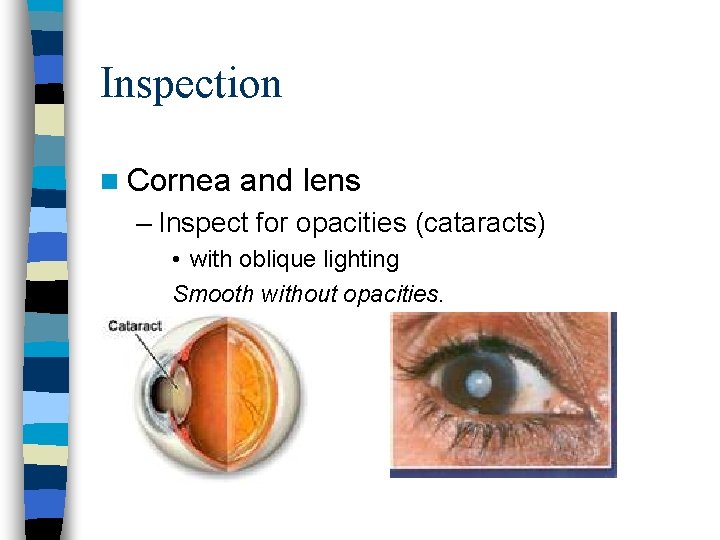
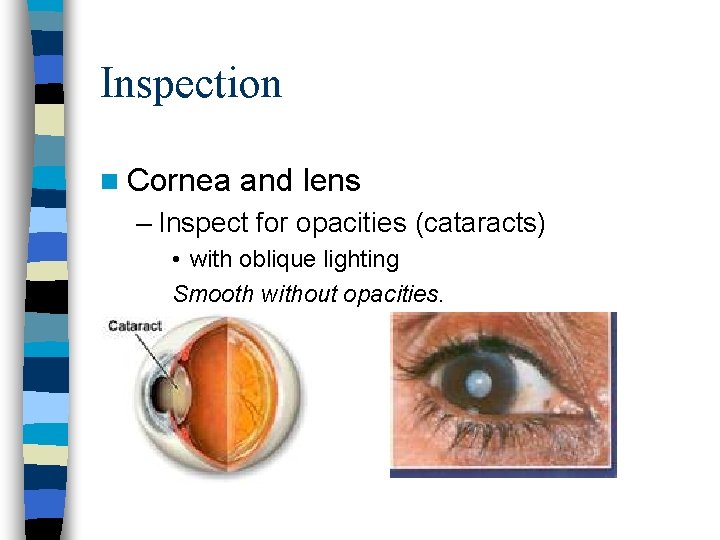
Inspection n Cornea and lens – Inspect for opacities (cataracts) • with oblique lighting Smooth without opacities.
Ophthalmoscopic Exam n Getting Started – Start at the “ 0” diopters – Use large, round beam of light – Use your right hand right eye for patient’s right eye, and your left eye for patient’s left eye – Get close – Darken room – Have patient gaze at a distant object
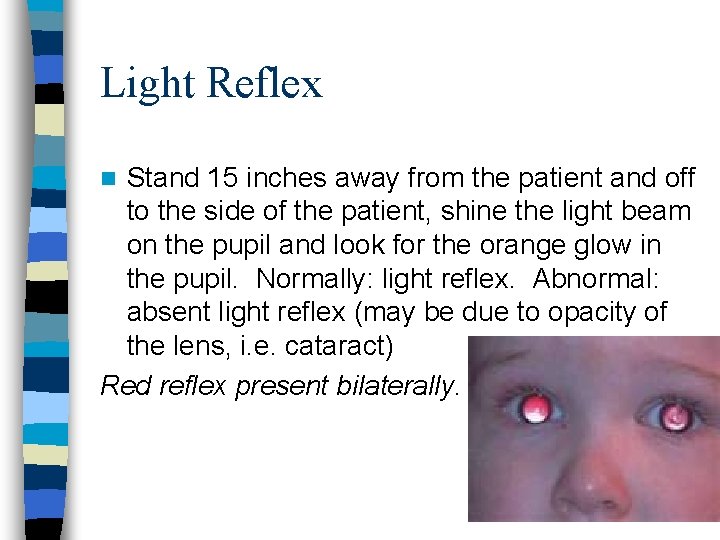
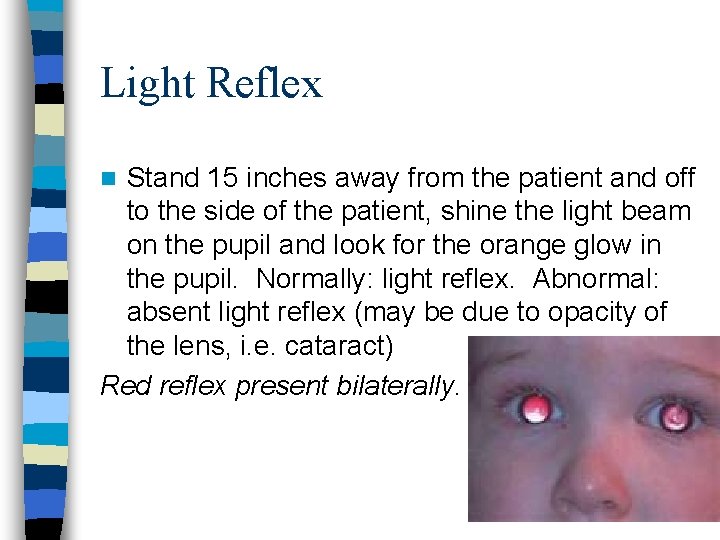
Light Reflex Stand 15 inches away from the patient and off to the side of the patient, shine the light beam on the pupil and look for the orange glow in the pupil. Normally: light reflex. Abnormal: absent light reflex (may be due to opacity of the lens, i. e. cataract) Red reflex present bilaterally. n
Examining the Optic Disc and Retina n First, locate the optic disc (you can follow a blood vessel centrally to find it) n Focus by adjusting the lens of your ophthalmoscope – If the patient is nearsighted (myopic), rotate the lens disc counterclockwise to the minus diopters – If the patient is farsighted (hyperopic), move the disc clockwise to the plus diopters – You can correct your own refractive error in the same way
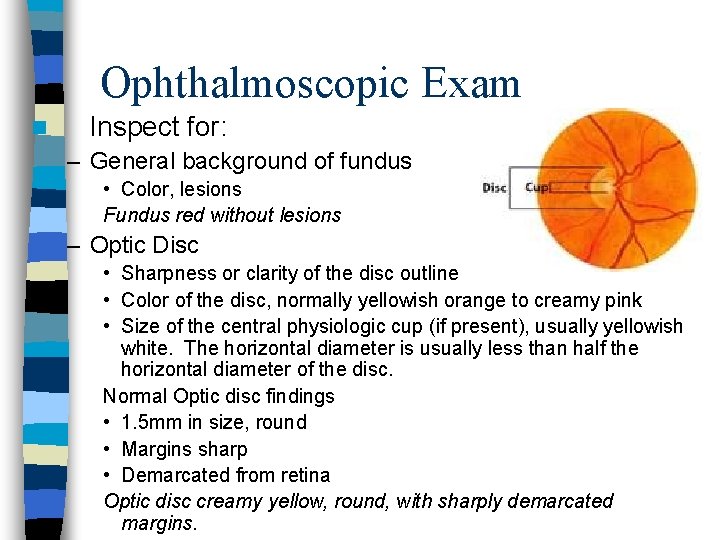
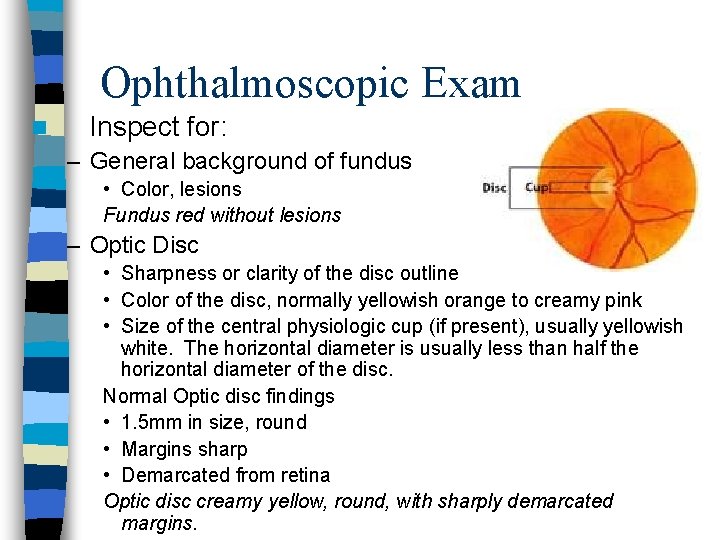
Ophthalmoscopic Exam n Inspect for: – General background of fundus • Color, lesions Fundus red without lesions – Optic Disc • Sharpness or clarity of the disc outline • Color of the disc, normally yellowish orange to creamy pink • Size of the central physiologic cup (if present), usually yellowish white. The horizontal diameter is usually less than half the horizontal diameter of the disc. Normal Optic disc findings • 1. 5 mm in size, round • Margins sharp • Demarcated from retina Optic disc creamy yellow, round, with sharply demarcated margins.
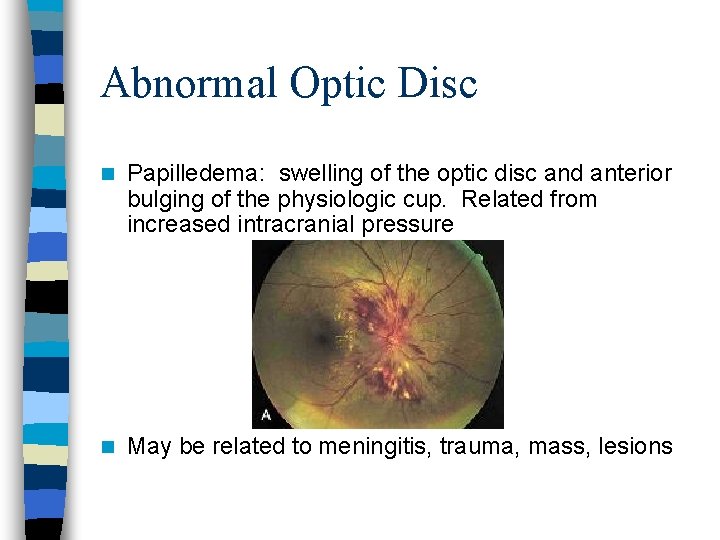
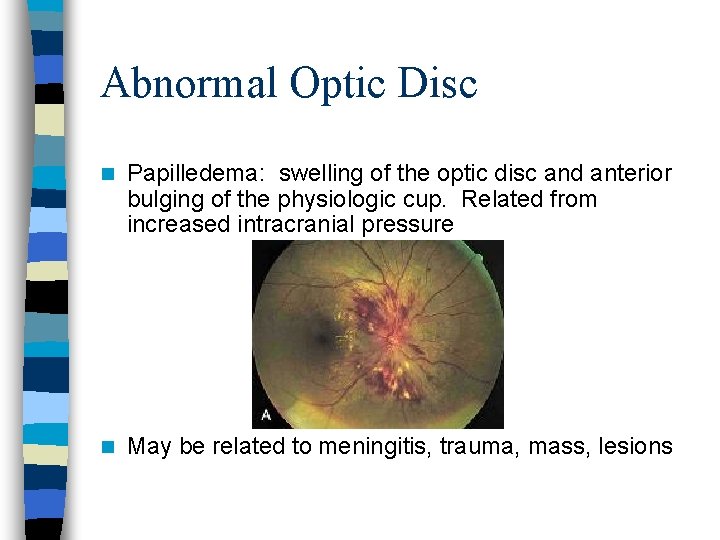
Abnormal Optic Disc n Papilledema: swelling of the optic disc and anterior bulging of the physiologic cup. Related from increased intracranial pressure n May be related to meningitis, trauma, mass, lesions
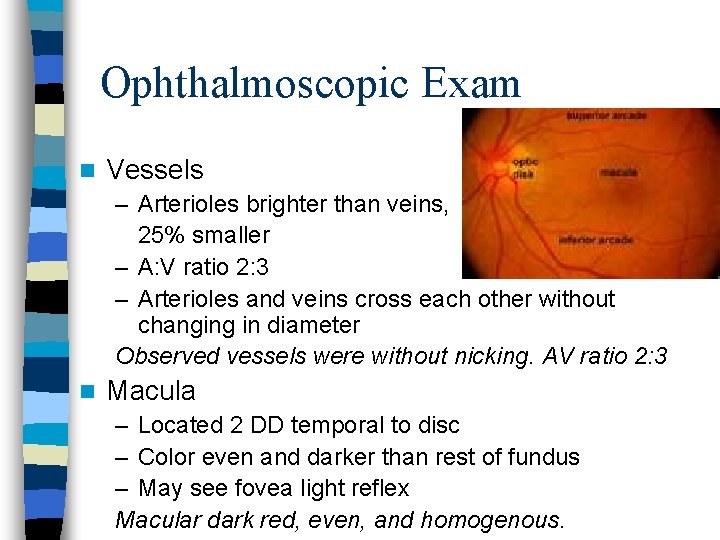
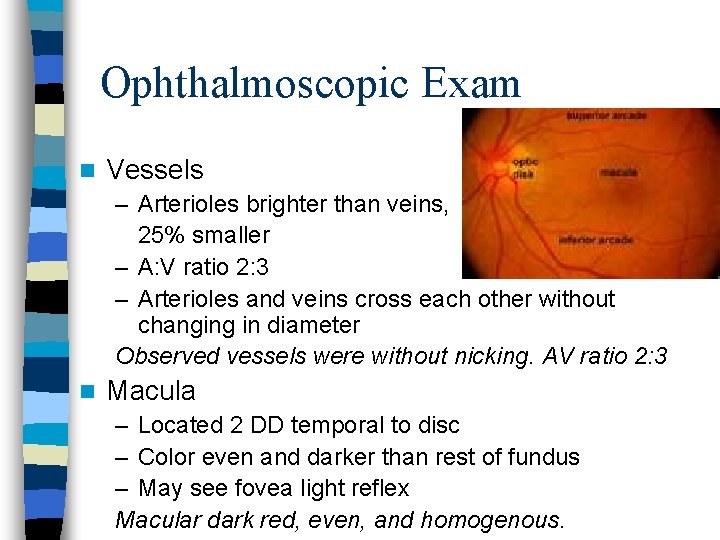
Ophthalmoscopic Exam n Vessels – Arterioles brighter than veins, 25% smaller – A: V ratio 2: 3 – Arterioles and veins cross each other without changing in diameter Observed vessels were without nicking. AV ratio 2: 3 n Macula – Located 2 DD temporal to disc – Color even and darker than rest of fundus – May see fovea light reflex Macular dark red, even, and homogenous.
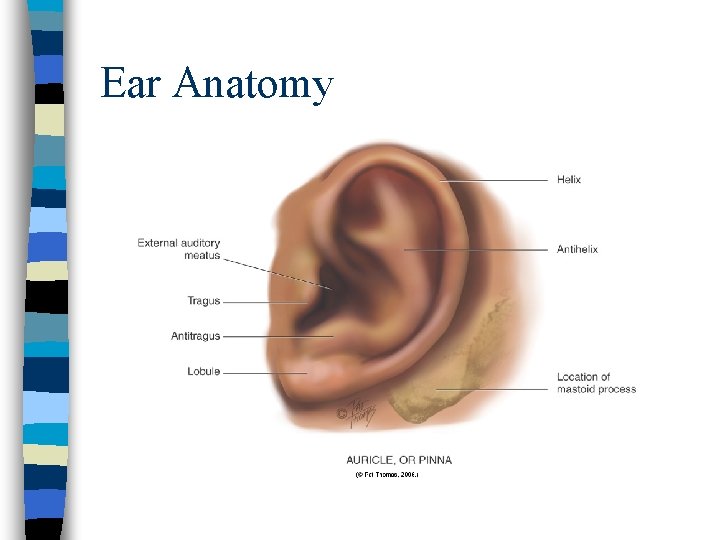
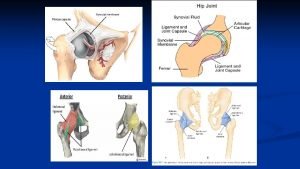
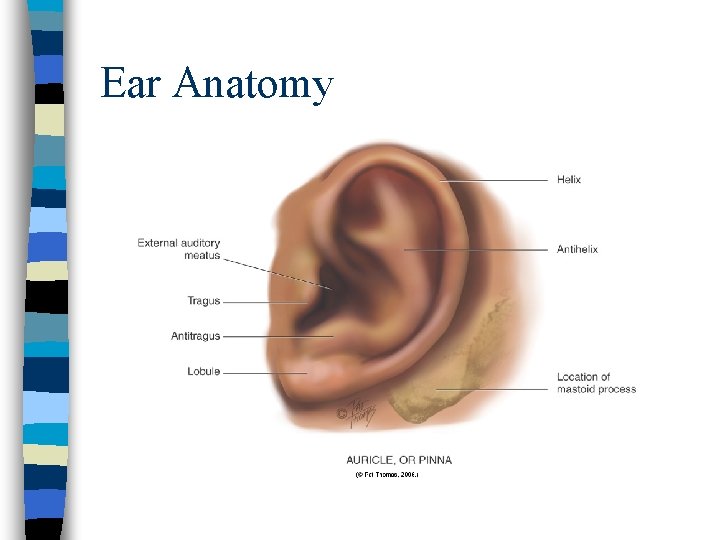
Ear Anatomy
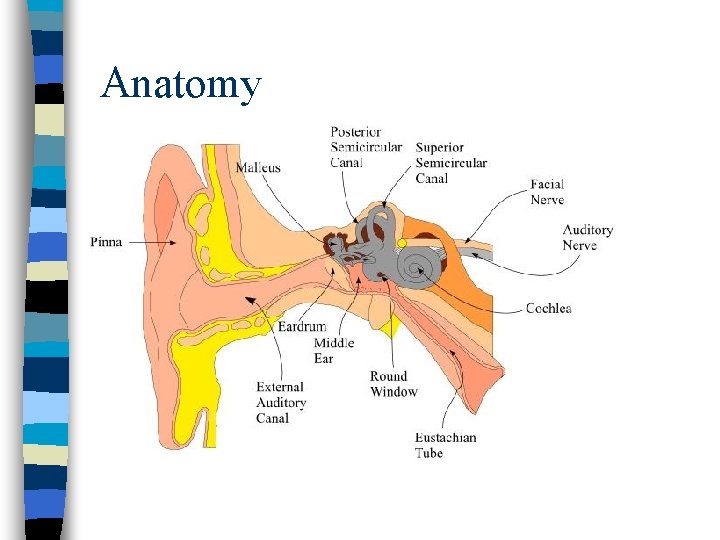
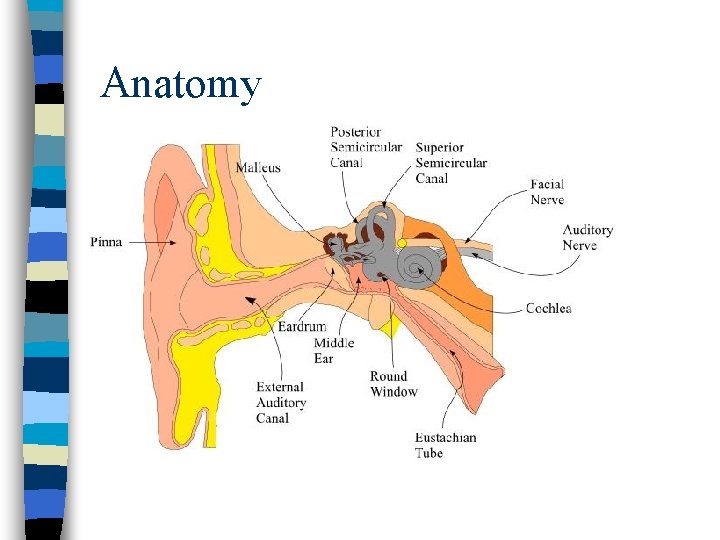
Anatomy
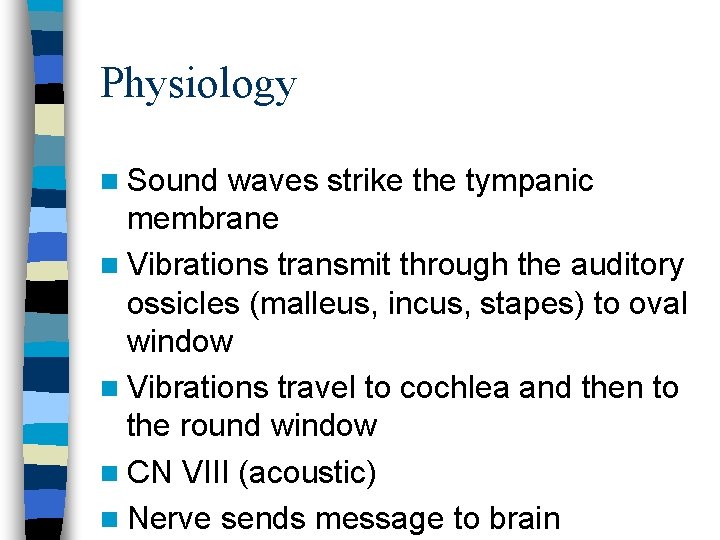
Physiology n Sound waves strike the tympanic membrane n Vibrations transmit through the auditory ossicles (malleus, incus, stapes) to oval window n Vibrations travel to cochlea and then to the round window n CN VIII (acoustic) n Nerve sends message to brain
The Aging Adult n Decreased hearing because: – Presbycusis • Gradual sensorineural hearing loss caused by nerve degeneration in inner ear or auditory nerve – Onset around 50 years old • First notices a high-frequency tone loss – Harder to hear consonants than vowels – Words sound garbled » Accentuated by background noise » Music, dishes clattering, large party noise
The Aging Adult – Cilia lining the ear canal becomes coarse and stiff • Decreased hearing as impedes sound waves • Causes cerumen to accumulate and oxidize – Cerumen drier due to atrophy of apocrine gland n Auditory reaction time increases after age 70. – Takes longer for the older adult to process sensory input and respond to it.
ROS: Ear n How is your hearing? – Use of hearing aid? – Taking ototoxic drugs? n Have you had any trouble with your ears or balance? – Are you having any vertigo? (feeling as if the room is spinning, different from dizzy) – Are you having any tinnitus? (musical ringing in the ear) n Does anyone smoke in your household? – Increased risk of otitis media in children
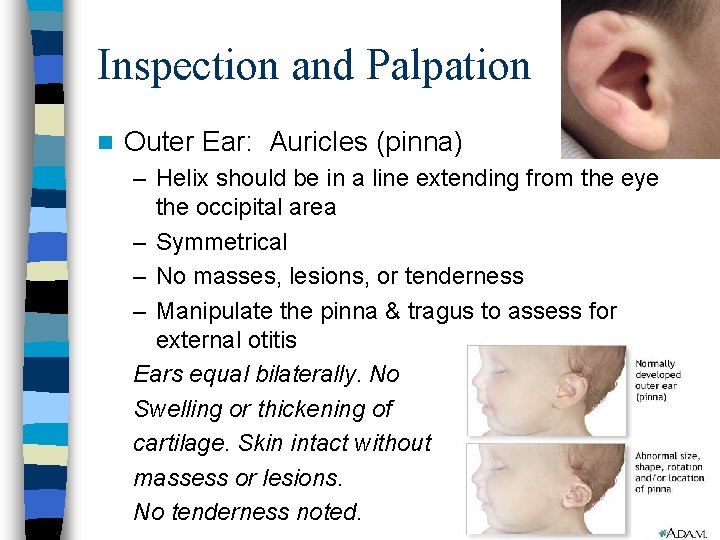
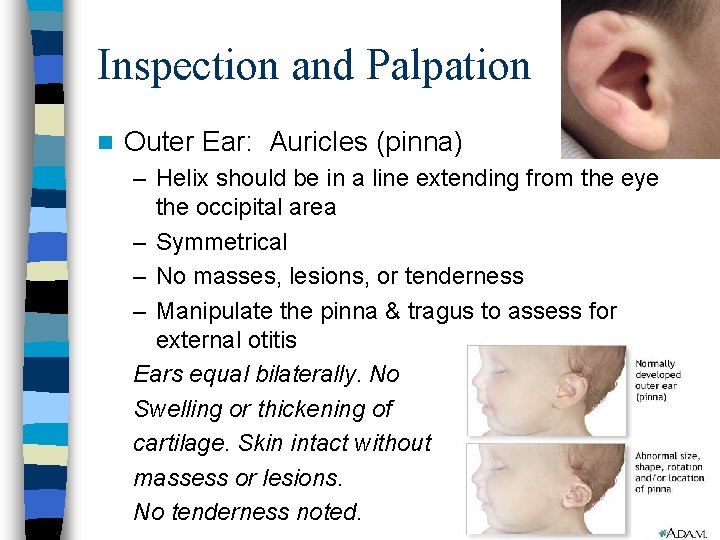
Inspection and Palpation n Outer Ear: Auricles (pinna) – Helix should be in a line extending from the eye the occipital area – Symmetrical – No masses, lesions, or tenderness – Manipulate the pinna & tragus to assess for external otitis Ears equal bilaterally. No Swelling or thickening of cartilage. Skin intact without massess or lesions. No tenderness noted.
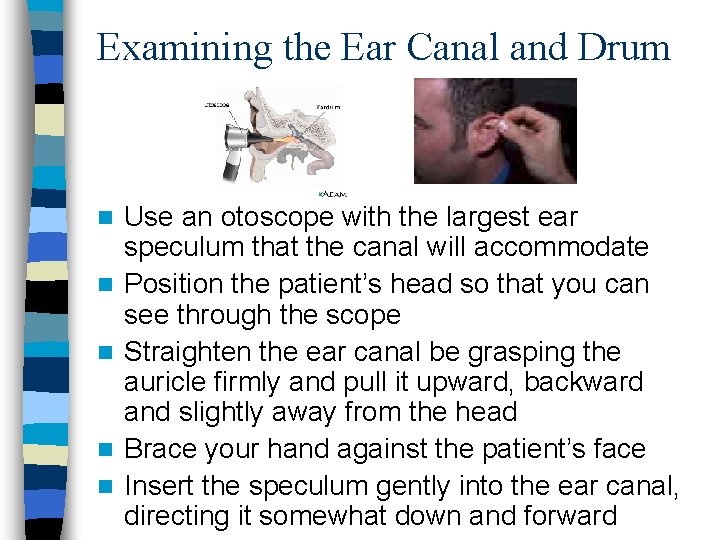
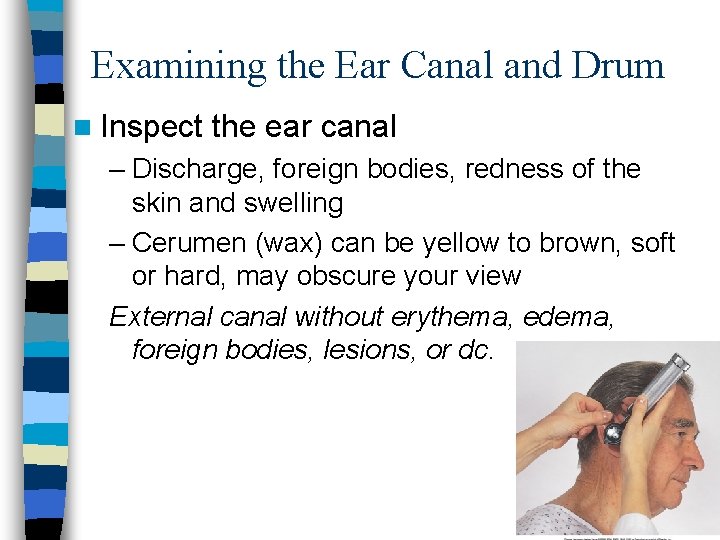
Examining the Ear Canal and Drum n n n Use an otoscope with the largest ear speculum that the canal will accommodate Position the patient’s head so that you can see through the scope Straighten the ear canal be grasping the auricle firmly and pull it upward, backward and slightly away from the head Brace your hand against the patient’s face Insert the speculum gently into the ear canal, directing it somewhat down and forward
Examining the Ear Canal and Drum n Inspect the ear canal – Discharge, foreign bodies, redness of the skin and swelling – Cerumen (wax) can be yellow to brown, soft or hard, may obscure your view External canal without erythema, edema, foreign bodies, lesions, or dc.

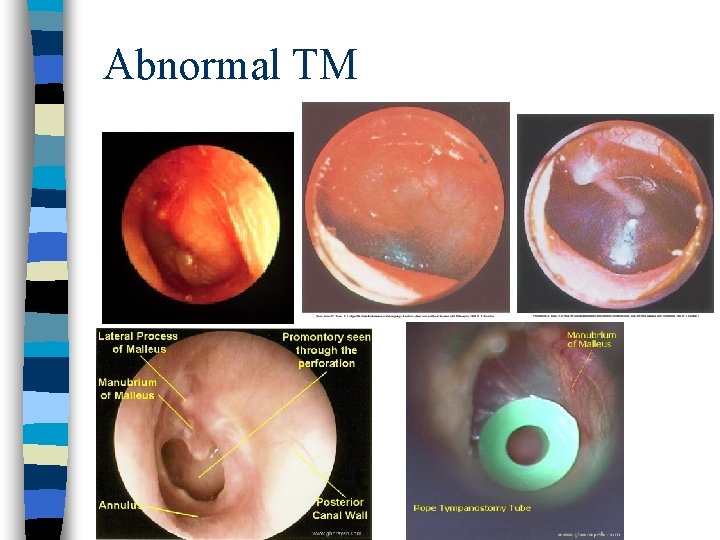
Inspect the Eardrum n Identify the handle of the malleus n Identify the short process of the malleus n Inspect the pars flaccida and Pars tensa n Normal – Shiny, transparent, pearly gray, slight concave, non-bulging, no perforation TM gray and intact bilaterally without erythema, bulging, or retraction.
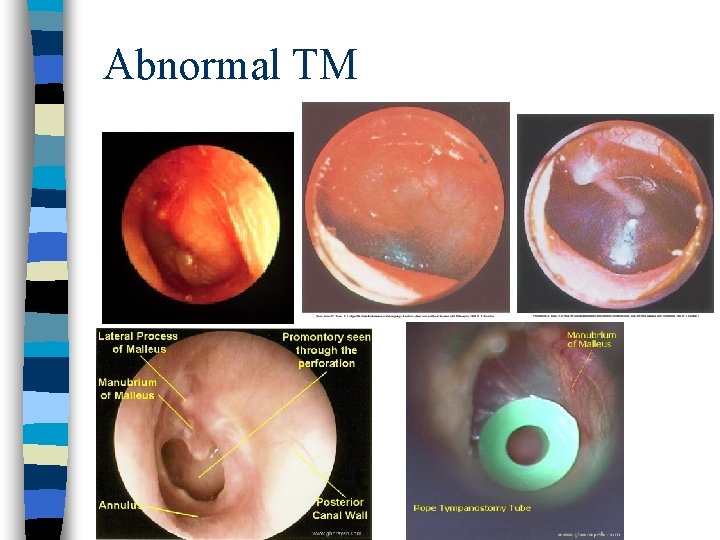
Abnormal TM n
Auditory Acuity n Estimating Hearing – Occlude one ear of your patient – Stand 1 -2 feet behind patient – Whisper a word (i. e. 88) – Repeat with other ear Gross hearing intact by whisper test.
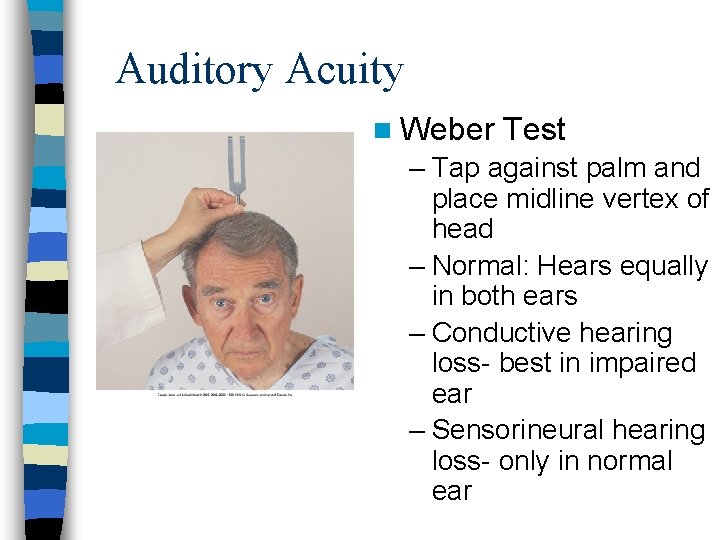
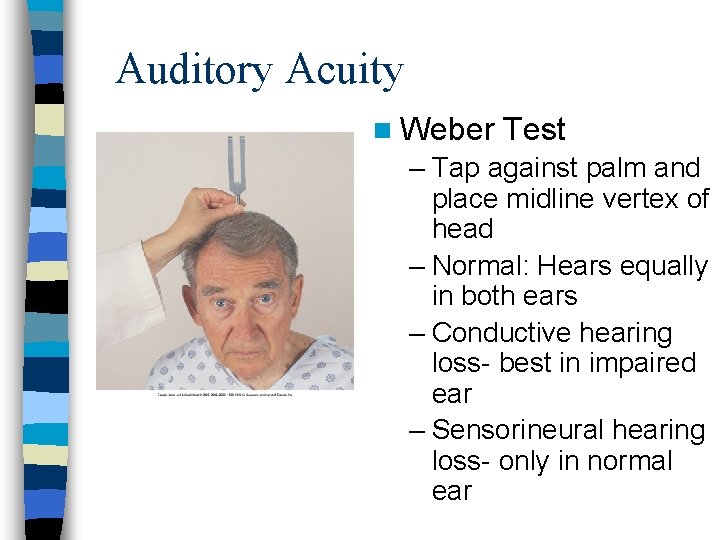
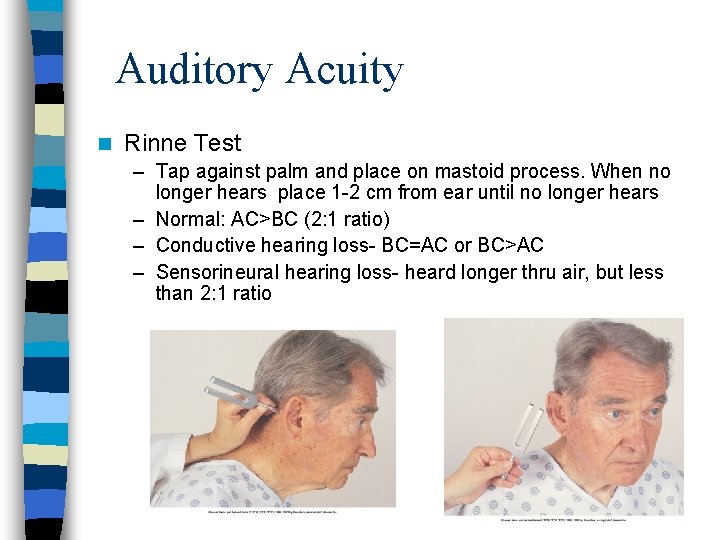
Auditory Acuity n Weber Test – Tap against palm and place midline vertex of head – Normal: Hears equally in both ears – Conductive hearing loss- best in impaired ear – Sensorineural hearing loss- only in normal ear
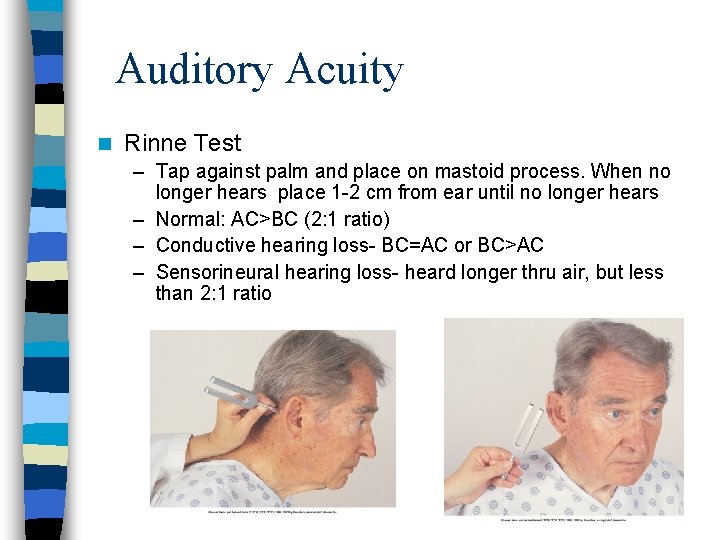
Auditory Acuity n Rinne Test – Tap against palm and place on mastoid process. When no longer hears place 1 -2 cm from ear until no longer hears – Normal: AC>BC (2: 1 ratio) – Conductive hearing loss- BC=AC or BC>AC – Sensorineural hearing loss- heard longer thru air, but less than 2: 1 ratio
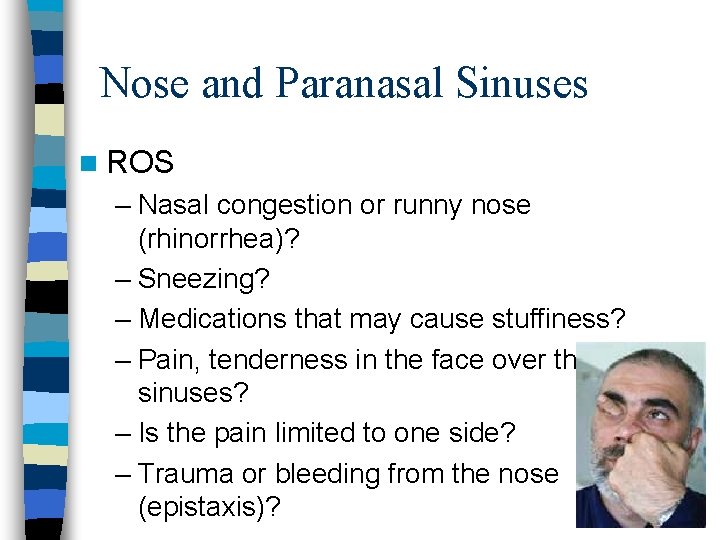
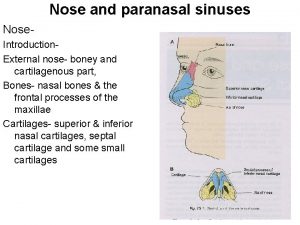
Nose and Paranasal Sinuses n ROS – Nasal congestion or runny nose (rhinorrhea)? – Sneezing? – Medications that may cause stuffiness? – Pain, tenderness in the face over the sinuses? – Is the pain limited to one side? – Trauma or bleeding from the nose (epistaxis)?
Nose and Paranasal Sinuses n Allergic Rhinitis – Itching – Swelling – Rhinorrhea – Sneezing – Tearing eyes – Later- stuffy nose, coughing, decreased smell, sore throat, dark circles under eyes
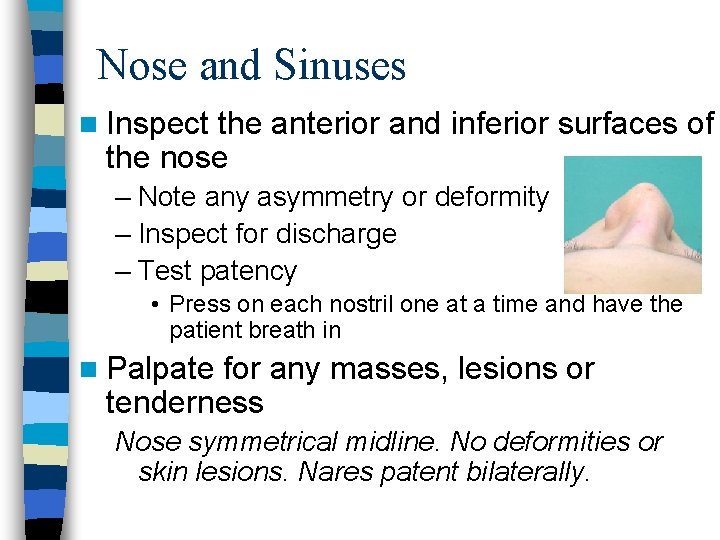
Nose and Sinuses n Inspect the anterior and inferior surfaces of the nose – Note any asymmetry or deformity – Inspect for discharge – Test patency • Press on each nostril one at a time and have the patient breath in n Palpate for any masses, lesions or tenderness Nose symmetrical midline. No deformities or skin lesions. Nares patent bilaterally.
Nose and Sinuses ……… n Inspect the inside of the nose – Inspect vestibule, septum and turbinates • Color of nasal mucosa • Foreign body • Discharge (note color: clear, yellow, green, bloody) • Masses, lesions, polyps • Septum: deviation, perforation, bleeding • Turbinates: color, swelling, exudate, polyps Normally no swelling, mucoid drainage; redder than oral mucosa Septum without deviation, perforation, or bleeding. Turbinates pink, without dc, edema, exudate, or polyp.
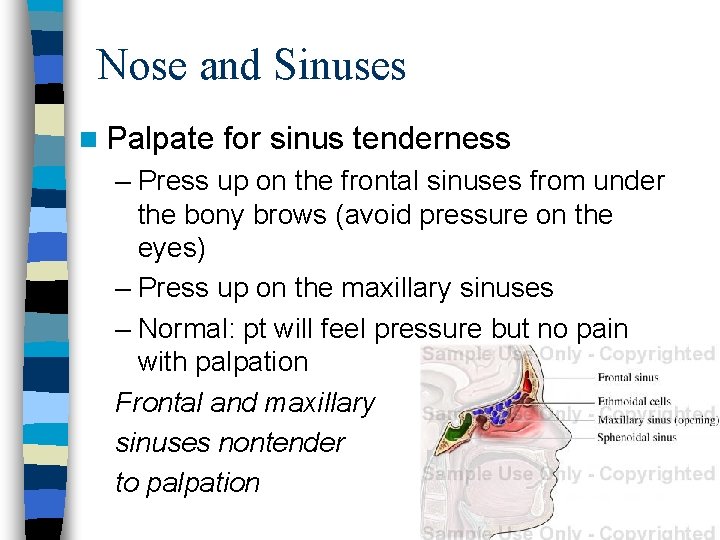
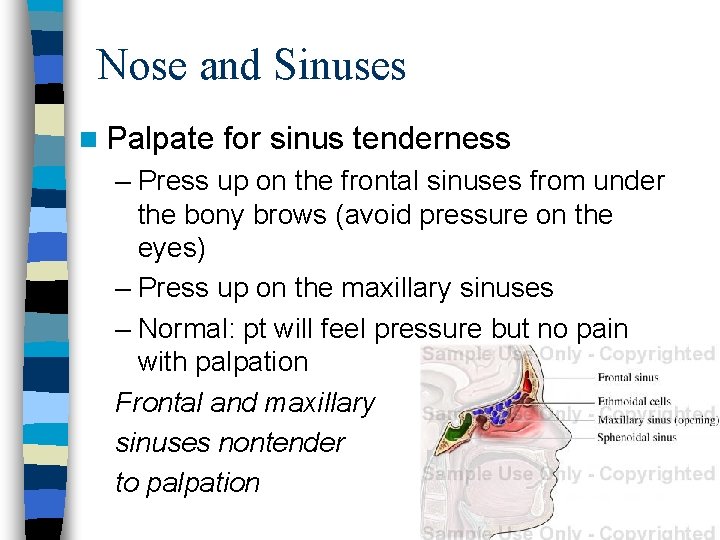
Nose and Sinuses n Palpate for sinus tenderness – Press up on the frontal sinuses from under the bony brows (avoid pressure on the eyes) – Press up on the maxillary sinuses – Normal: pt will feel pressure but no pain with palpation Frontal and maxillary sinuses nontender to palpation
Mouth and Pharynx n ROS – Sore throat – Sore tongue – Bleeding from the gums – Tooth pain – Hoarseness
Mouth and Pharynx n Inspect lips – – – – n Color Moisture Lumps Ulcers Cracking Symmetry Swelling (edema) Inspect oral mucosa (inside of mouth) – With good light and a tongue blade, inspect for color, ulcers, white patches, and nodules. Lips pink and moist without cracking or lesions. Buccal mucosa pink without nodules or lesions.
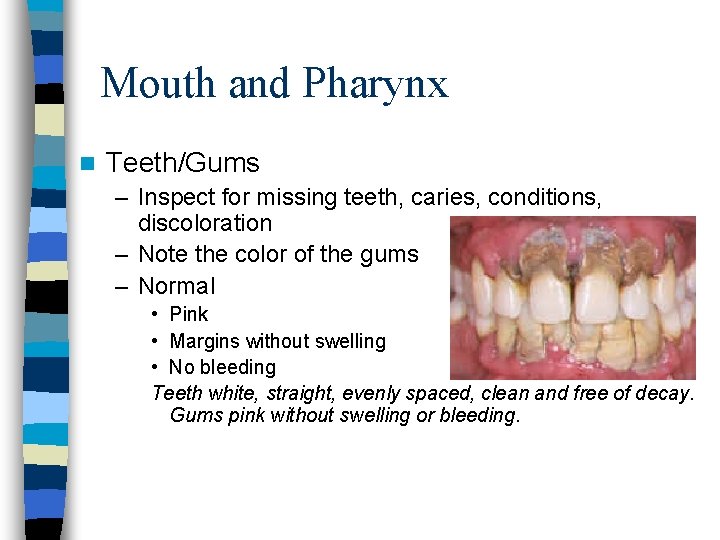
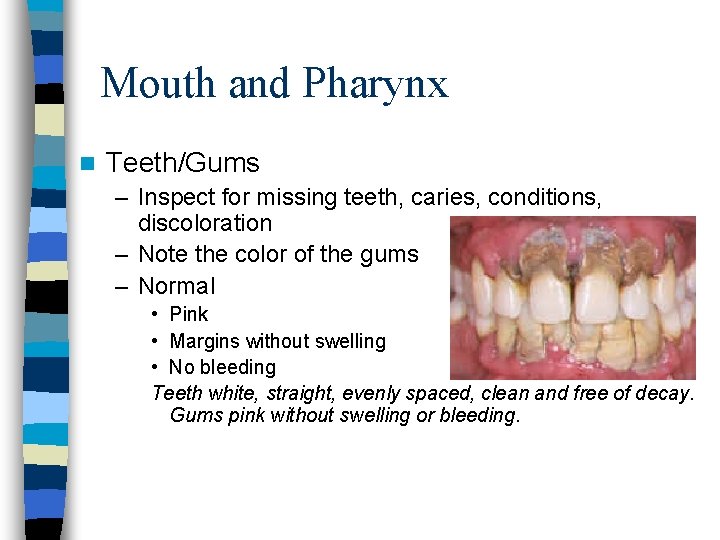
Mouth and Pharynx n Teeth/Gums – Inspect for missing teeth, caries, conditions, discoloration – Note the color of the gums – Normal • Pink • Margins without swelling • No bleeding Teeth white, straight, evenly spaced, clean and free of decay. Gums pink without swelling or bleeding.
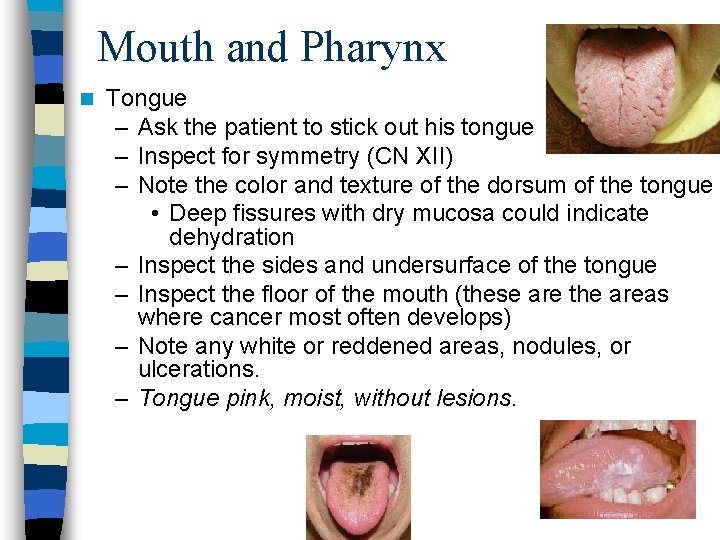
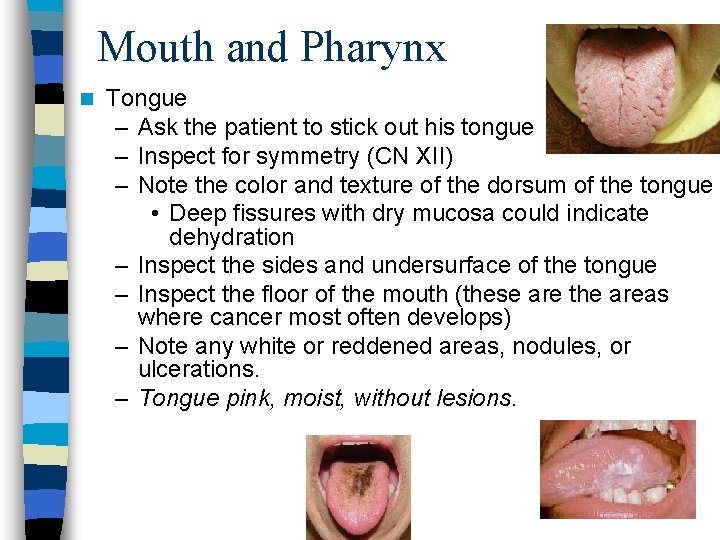
Mouth and Pharynx n Tongue – Ask the patient to stick out his tongue – Inspect for symmetry (CN XII) – Note the color and texture of the dorsum of the tongue • Deep fissures with dry mucosa could indicate dehydration – Inspect the sides and undersurface of the tongue – Inspect the floor of the mouth (these are the areas where cancer most often develops) – Note any white or reddened areas, nodules, or ulcerations. – Tongue pink, moist, without lesions.
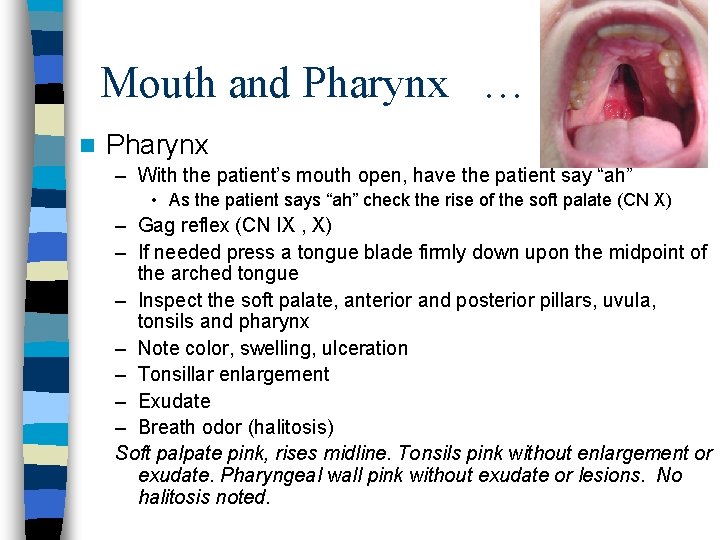
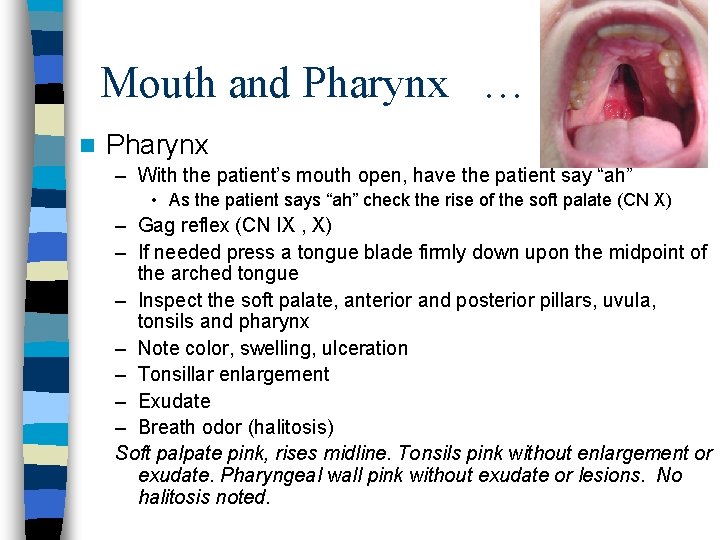
Mouth and Pharynx … n Pharynx – With the patient’s mouth open, have the patient say “ah” • As the patient says “ah” check the rise of the soft palate (CN X) – Gag reflex (CN IX , X) – If needed press a tongue blade firmly down upon the midpoint of the arched tongue – Inspect the soft palate, anterior and posterior pillars, uvula, tonsils and pharynx – Note color, swelling, ulceration – Tonsillar enlargement – Exudate – Breath odor (halitosis) Soft palpate pink, rises midline. Tonsils pink without enlargement or exudate. Pharyngeal wall pink without exudate or lesions. No halitosis noted.

Neck n ROS – Neck pain? – Lumps or swelling? – History of neck surgery? – History of neck trauma?
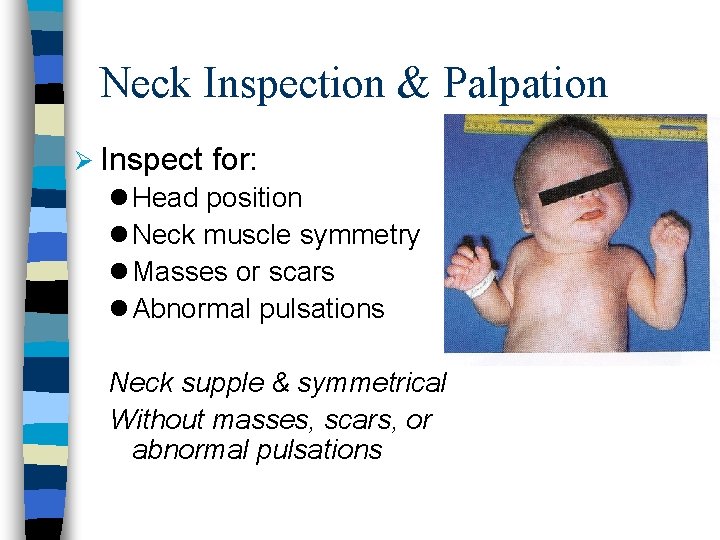
Neck Inspection & Palpation Ø Inspect for: l Head position l Neck muscle symmetry l Masses or scars l Abnormal pulsations Neck supple & symmetrical Without masses, scars, or abnormal pulsations
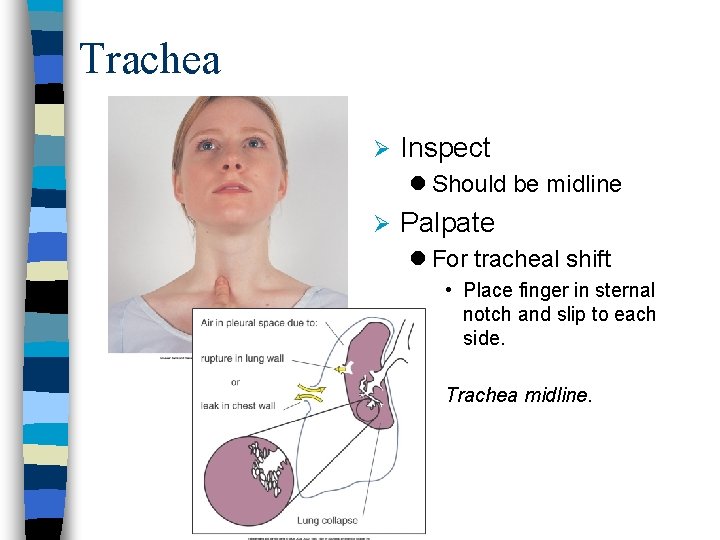
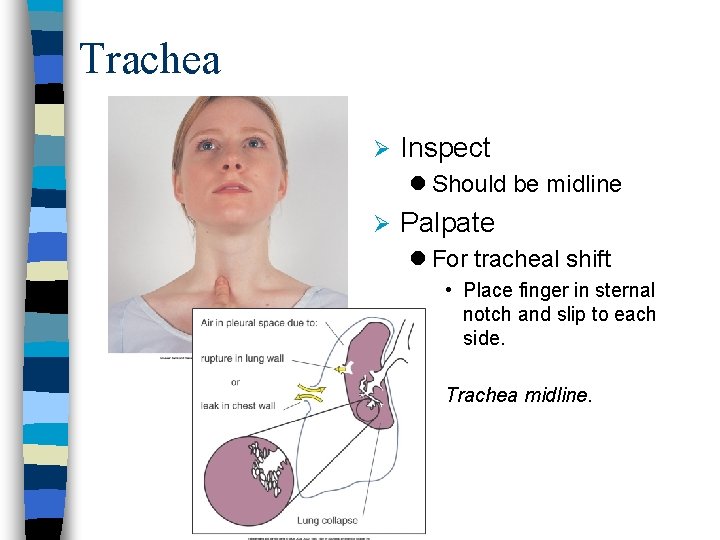
Trachea Ø Inspect l Should be midline Ø Palpate l For tracheal shift • Place finger in sternal notch and slip to each side. Trachea midline.
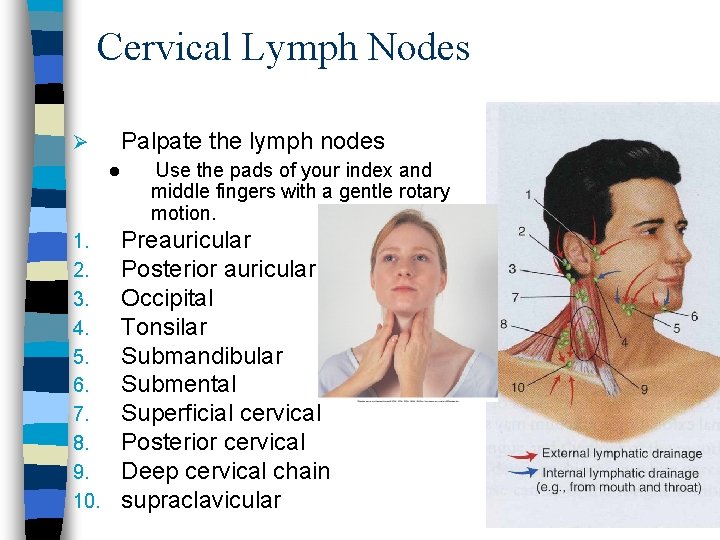
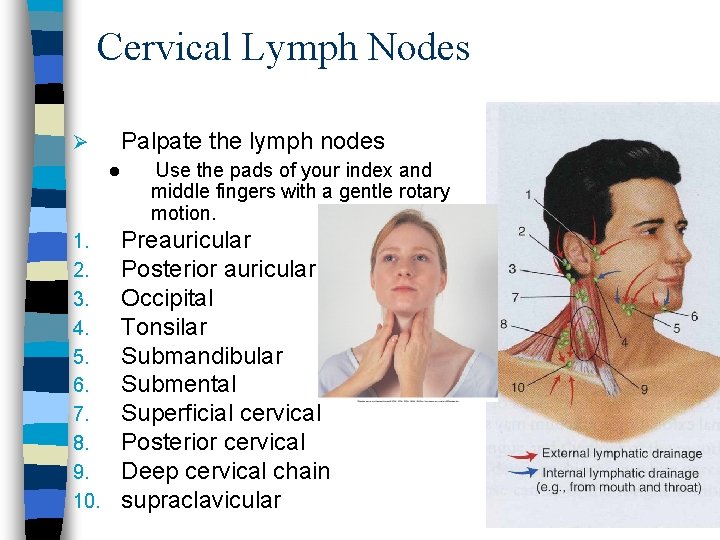
Cervical Lymph Nodes Ø Palpate the lymph nodes l 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Use the pads of your index and middle fingers with a gentle rotary motion. Preauricular Posterior auricular Occipital Tonsilar Submandibular Submental Superficial cervical Posterior cervical Deep cervical chain supraclavicular
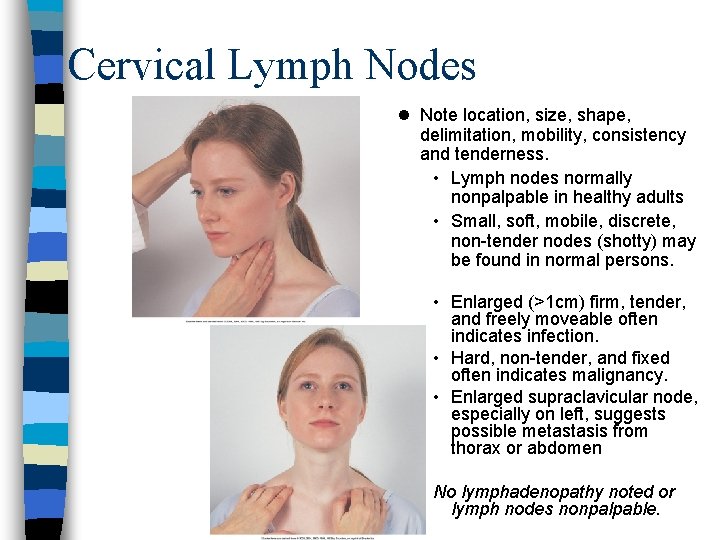
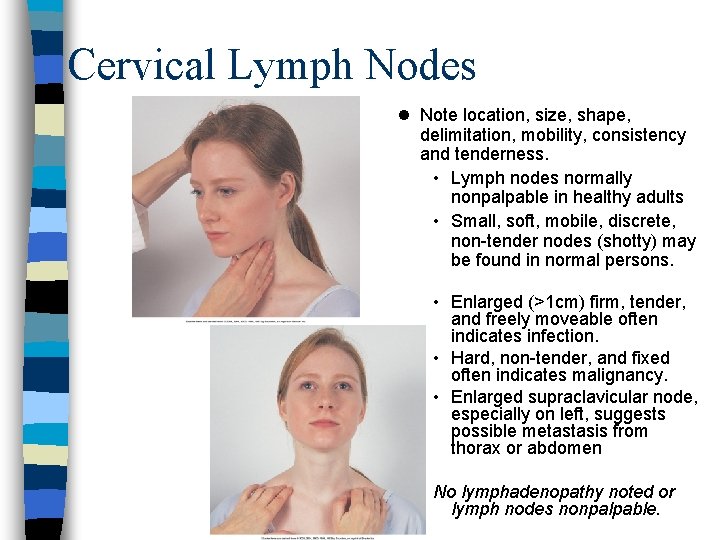
Cervical Lymph Nodes l Note location, size, shape, delimitation, mobility, consistency and tenderness. • Lymph nodes normally nonpalpable in healthy adults • Small, soft, mobile, discrete, non-tender nodes (shotty) may be found in normal persons. • Enlarged (>1 cm) firm, tender, and freely moveable often indicates infection. • Hard, non-tender, and fixed often indicates malignancy. • Enlarged supraclavicular node, especially on left, suggests possible metastasis from thorax or abdomen No lymphadenopathy noted or lymph nodes nonpalpable.
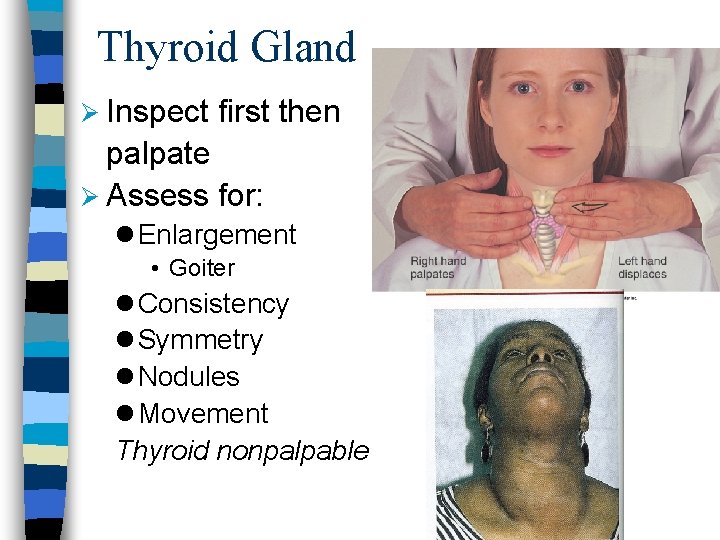
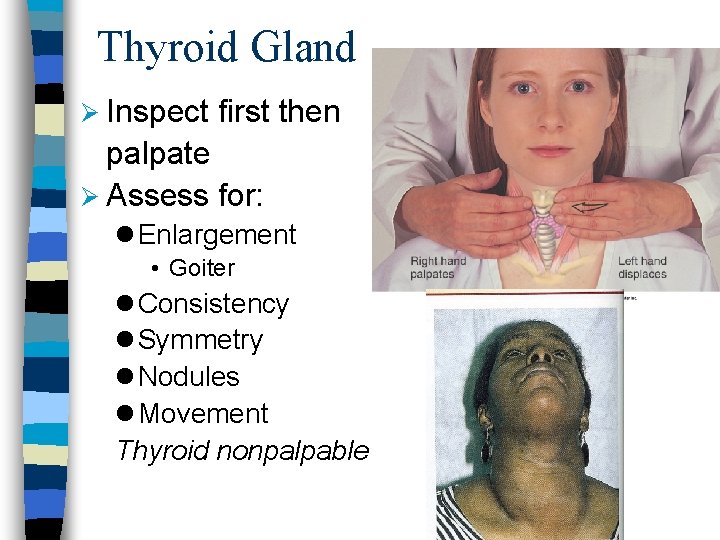
Thyroid Gland Ø Inspect first then palpate Ø Assess for: l Enlargement • Goiter l Consistency l Symmetry l Nodules l Movement Thyroid nonpalpable
 Low-set ears vs normal
Low-set ears vs normal The nose genre
The nose genre Flat nasal bridge
Flat nasal bridge We were given two ears but only one mouth
We were given two ears but only one mouth Box breathing through nose or mouth
Box breathing through nose or mouth Copyright
Copyright Eyes are to spectacles as ears are to
Eyes are to spectacles as ears are to Chapter 11 special senses the eyes and ears
Chapter 11 special senses the eyes and ears Open the blind eyes unlock the deaf ears
Open the blind eyes unlock the deaf ears Eyes that see and ears that hear
Eyes that see and ears that hear Mark 4:23-24
Mark 4:23-24 Impaired eyes and ears
Impaired eyes and ears Special senses the eyes and ears
Special senses the eyes and ears 5 animals whose ears cannot be seen
5 animals whose ears cannot be seen Head neck ratio
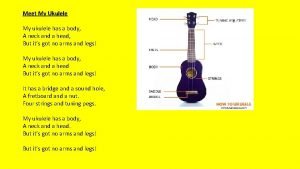
Head neck ratio Thumb brush strum
Thumb brush strum Tnm 8 head and neck
Tnm 8 head and neck Risk factors of head and neck cancer
Risk factors of head and neck cancer There once was a man from tennessee ukulele
There once was a man from tennessee ukulele Muscular system head and neck
Muscular system head and neck Zygomaticus major and minor muscle
Zygomaticus major and minor muscle Regional write up head face and neck
Regional write up head face and neck What has a neck but no head
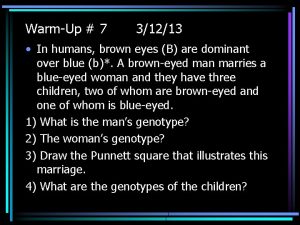
What has a neck but no head What is the genotype of the man? ii i a i i b i i a i a
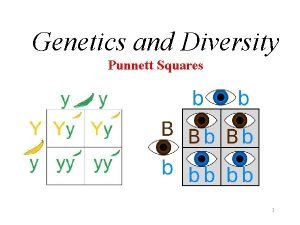
What is the genotype of the man? ii i a i i b i i a i a Eye color punnett square
Eye color punnett square Normal eye vs anemic eye
Normal eye vs anemic eye Two parents with green eyes
Two parents with green eyes Color wheel for brown eyes
Color wheel for brown eyes Nose assessment normal findings
Nose assessment normal findings Indexing head formula
Indexing head formula The attacking firm goes head-to-head with its competitor.
The attacking firm goes head-to-head with its competitor. Html tagi
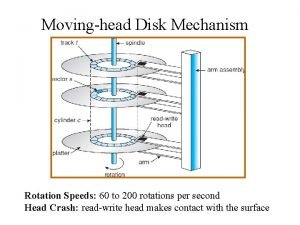
Html tagi The head of moving head disk
The head of moving head disk Head body head body gif
Head body head body gif What is a tonic syllable
What is a tonic syllable Suction lift
Suction lift Biceps femoris short head
Biceps femoris short head 7 tones
7 tones Moving head disk mechanism
Moving head disk mechanism 4 eyes in 4 hours
4 eyes in 4 hours Head injury assessment
Head injury assessment 4-h head heart, hands health who is served
4-h head heart, hands health who is served 4-h head heart hands health
4-h head heart hands health Why architects need to use their ears
Why architects need to use their ears Rhyme scheme highlighter
Rhyme scheme highlighter Whose misadventured piteous overthrows in modern english
Whose misadventured piteous overthrows in modern english Evs ppt for class 4
Evs ppt for class 4 Pig ears
Pig ears Hypertrichosis chromosome
Hypertrichosis chromosome Desire ability reason need
Desire ability reason need How to draw ears on a self portrait
How to draw ears on a self portrait Fas
Fas Two long ears four strong legs
Two long ears four strong legs Elephant with no ears
Elephant with no ears Classify each set of data as discrete or continuous
Classify each set of data as discrete or continuous A chapter on ears
A chapter on ears Whispering in the ears of princes
Whispering in the ears of princes What is supersition
What is supersition Coliflower ears
Coliflower ears Why mosquitoes buzz in people's ears summary
Why mosquitoes buzz in people's ears summary