Gas Exchangetopic 6 4 and H 6 Ventilation












- Slides: 45
Gas Exchange-topic 6. 4 and -H 6
Ventilation • Ventilation: The flow of air in and out of the alveoli is called ventilation • two stages: • inspiration (or inhalation) and expiration (or exhalation).
Why do we need it ? • to maintain concentration gradients in the alveoli. • Diffusing O 2 and CO 2
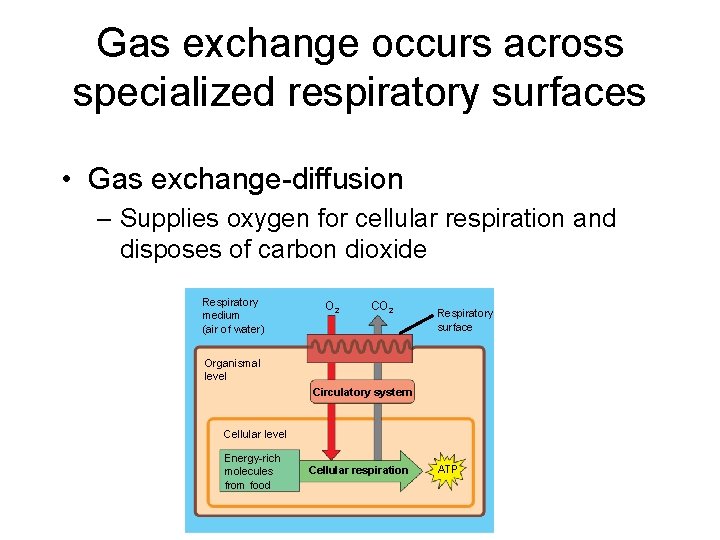
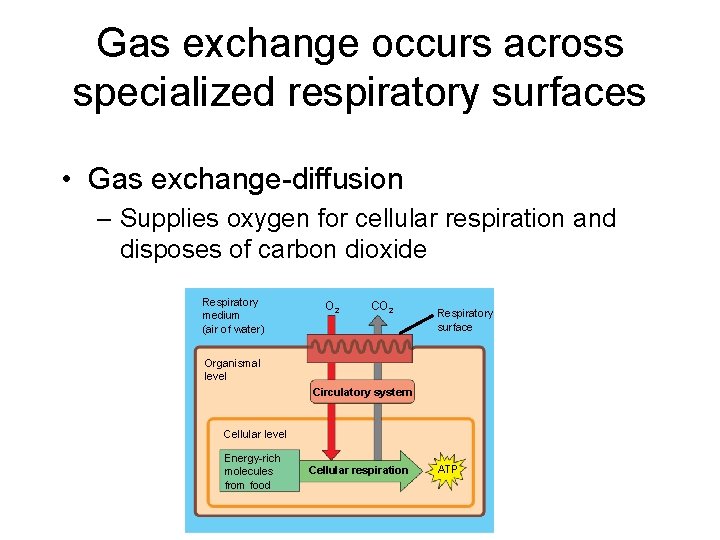
Gas exchange occurs across specialized respiratory surfaces • Gas exchange-diffusion – Supplies oxygen for cellular respiration and disposes of carbon dioxide Respiratory medium (air of water) O 2 CO 2 Respiratory surface Organismal level Circulatory system Cellular level Energy-rich molecules from food Cellular respiration ATP
• Animals require large, moist respiratory surfaces for the adequate diffusion of respiratory gases – Between their cells and the respiratory medium, either air or water
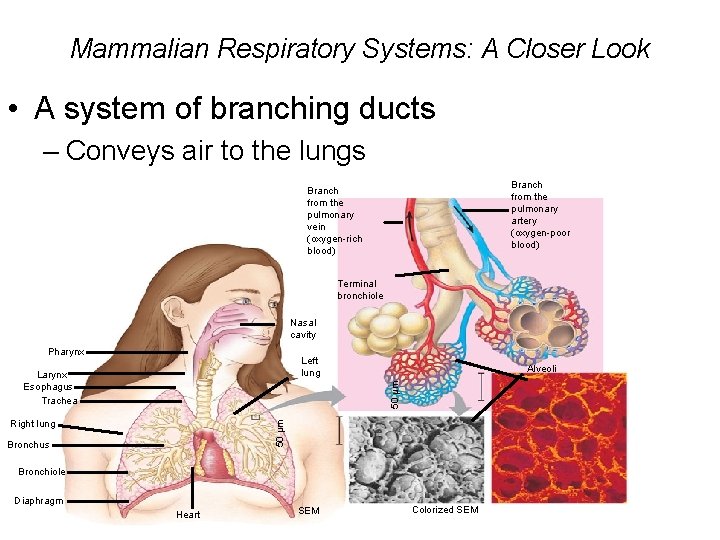
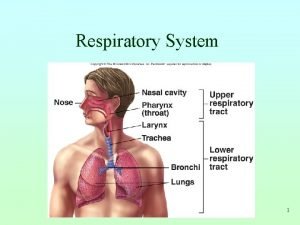
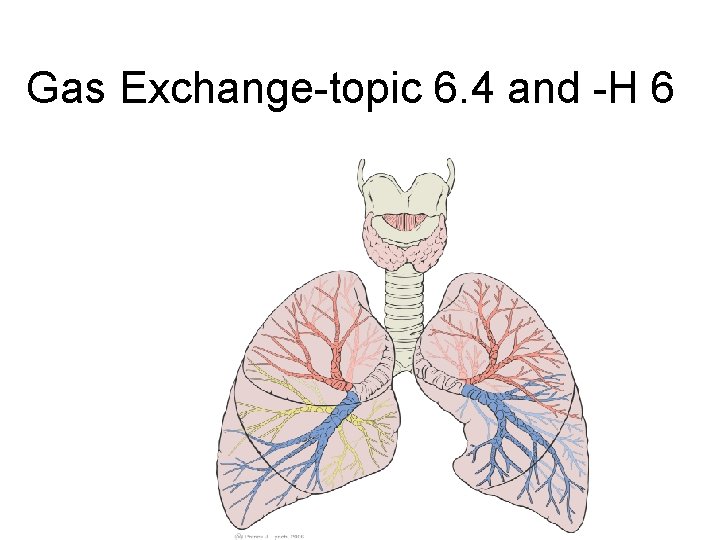
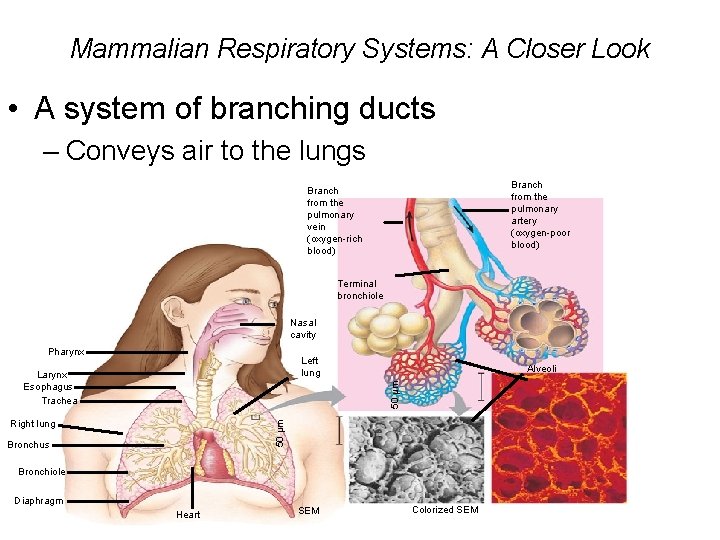
Mammalian Respiratory Systems: A Closer Look • A system of branching ducts – Conveys air to the lungs Branch from the pulmonary artery (oxygen-poor blood) Branch from the pulmonary vein (oxygen-rich blood) Terminal bronchiole Nasal cavity Pharynx Left lung Alveoli 50 µm Larynx Esophagus Trachea 50 µm Right lung Bronchus Bronchiole Diaphragm Heart SEM Colorized SEM
• In mammals, air inhaled through the nostrils – Passes through the pharynx into the trachea, bronchioles, and deadend alveoli, where gas exchange occurs
• Draw and label a diagram of the ventilation system, including trachea, lungs, bronchioles and alveoli, diaphragm
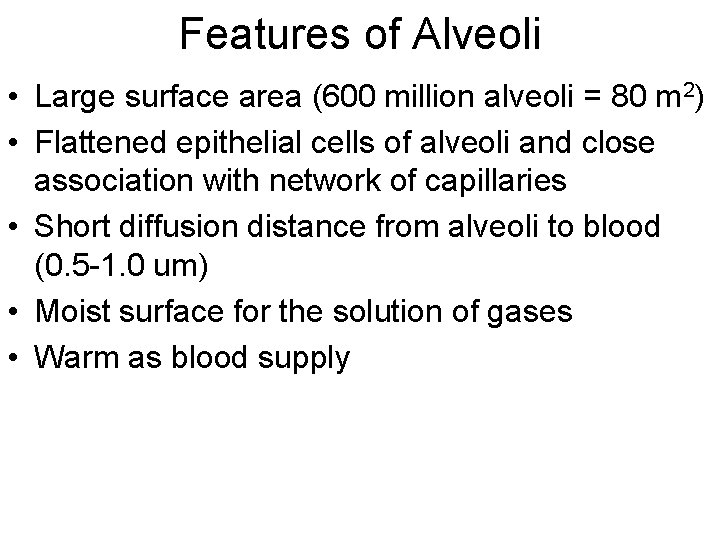
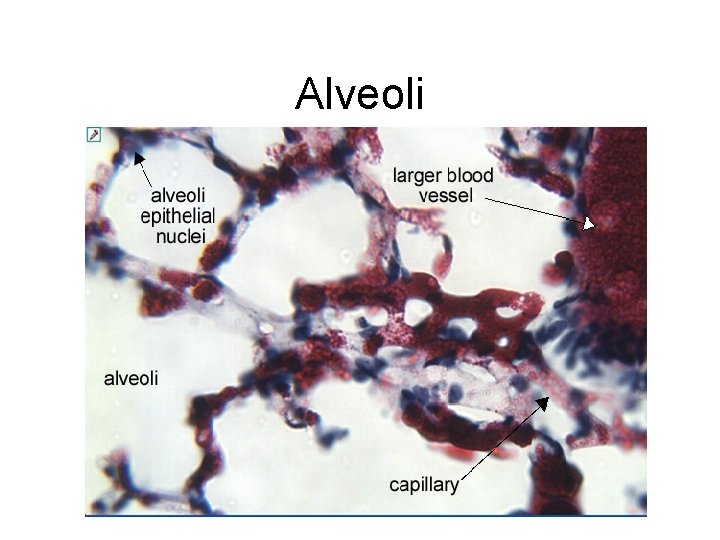
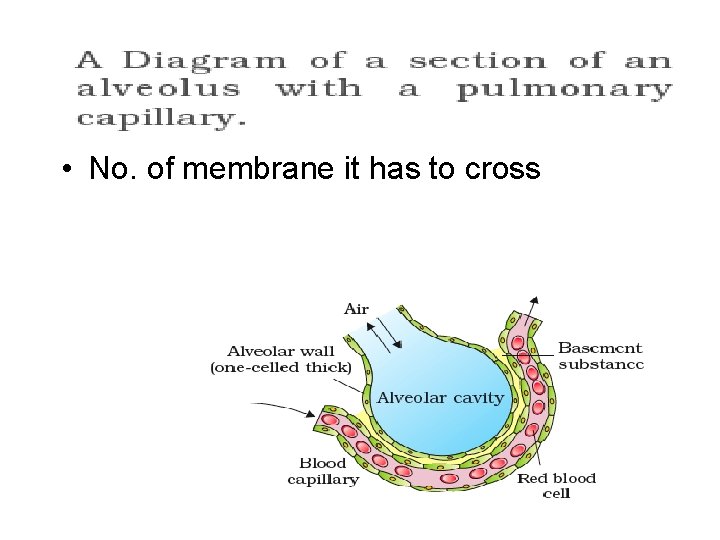
Features of Alveoli • Large surface area (600 million alveoli = 80 m 2) • Flattened epithelial cells of alveoli and close association with network of capillaries • Short diffusion distance from alveoli to blood (0. 5 -1. 0 um) • Moist surface for the solution of gases • Warm as blood supply

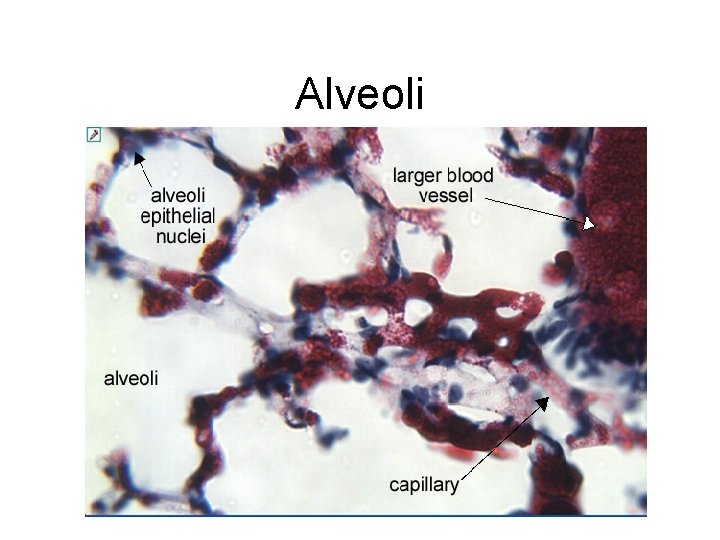
Alveoli

• Breathing ventilates the lungs • The process that ventilates the lungs is breathing – The alternate inhalation and exhalation of air – Is needed to maintain high concentration gradient in the alveoli.
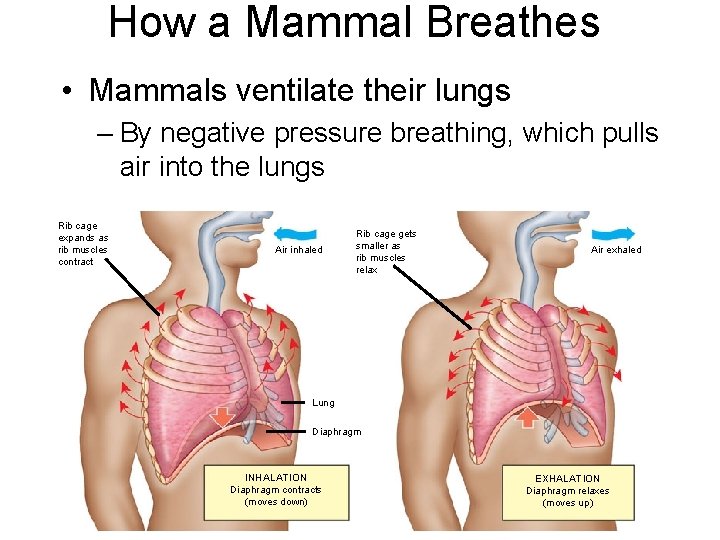
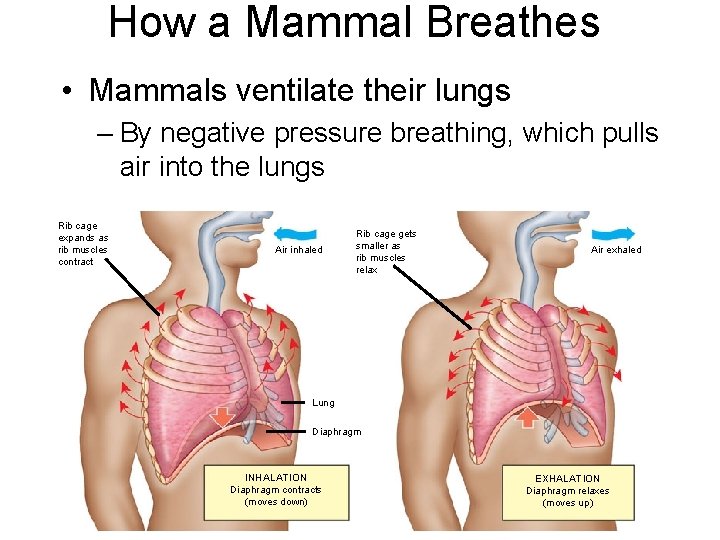
How a Mammal Breathes • Mammals ventilate their lungs – By negative pressure breathing, which pulls air into the lungs Rib cage expands as rib muscles contract Air inhaled Rib cage gets smaller as rib muscles relax Air exhaled Lung Diaphragm INHALATION Diaphragm contracts (moves down) EXHALATION Diaphragm relaxes (moves up)
Inhalation • • Diaphragm contracts- flattens-downwards External intercostal muscles contract. Ribs move up and out Volume in chest/thoracic cavity/lung increases • Pressure decrease • Air rushes in
Exhalation • • • Diaphragm relaxes-moves up-curved up External muscle relaxes Decrease in lung volume Increase in pressure Air is rushed out
During exercise • Abdominal muscles, • Intercoastal muscles contracts • Faster exhalation

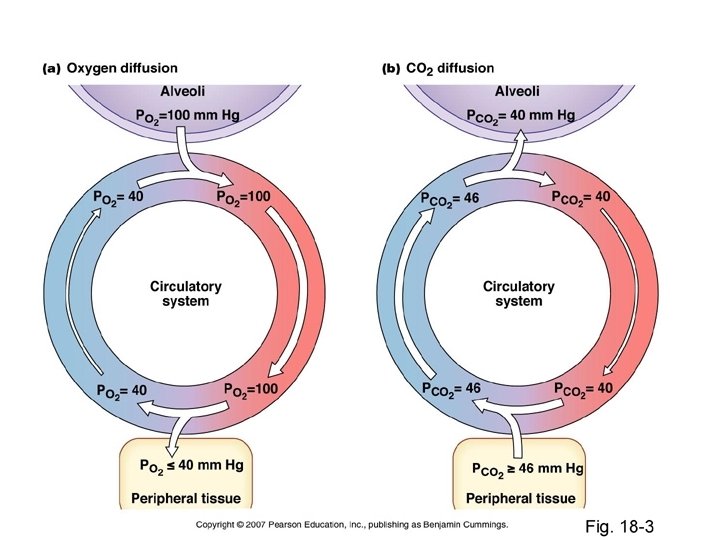
• Partial pressure-each gas has a partial pressure which is the pressure which the gas would have if it alone occupied the volume. • Units –k Pa-(kilo Pascal), mm Hg

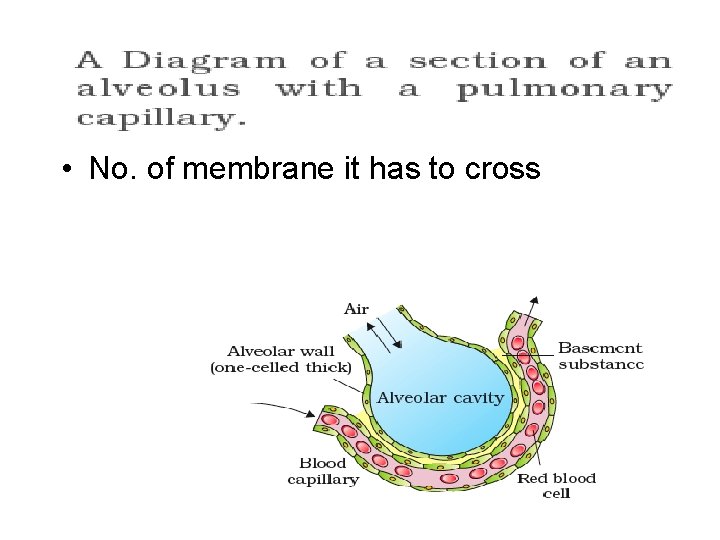
• No. of membrane it has to cross
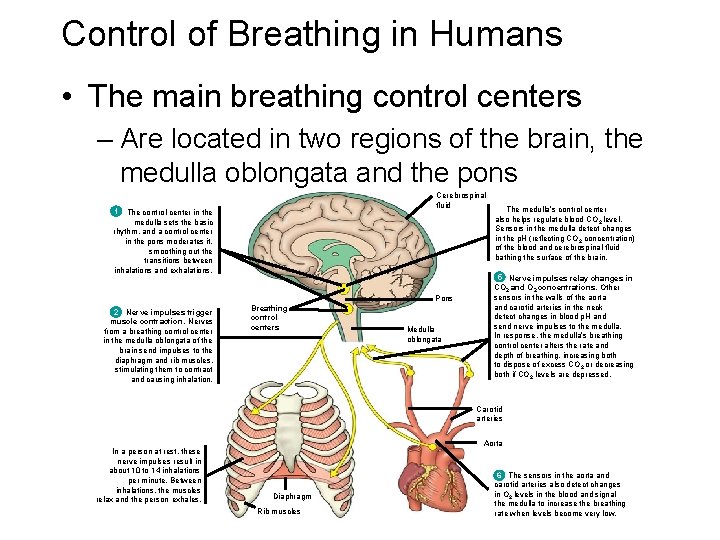
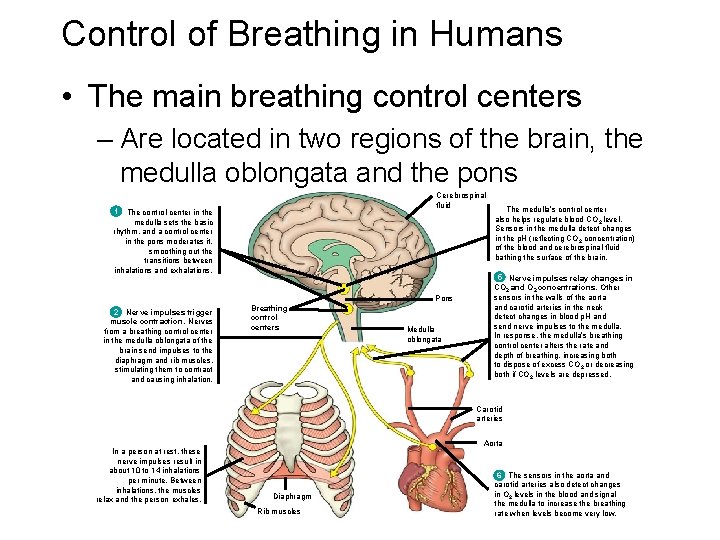
Control of Breathing in Humans • The main breathing control centers – Are located in two regions of the brain, the medulla oblongata and the pons Cerebrospinal fluid 1 The control center in the medulla sets the basic rhythm, and a control center in the pons moderates it, smoothing out the transitions between inhalations and exhalations. Pons 2 Nerve impulses trigger muscle contraction. Nerves from a breathing control center in the medulla oblongata of the brain send impulses to the diaphragm and rib muscles, stimulating them to contract and causing inhalation. Breathing control centers Medulla oblongata The medulla’s control center also helps regulate blood CO 2 level. Sensors in the medulla detect changes in the p. H (reflecting CO 2 concentration) of the blood and cerebrospinal fluid bathing the surface of the brain. 5 Nerve impulses relay changes in CO 2 and O 2 concentrations. Other sensors in the walls of the aorta and carotid arteries in the neck detect changes in blood p. H and send nerve impulses to the medulla. In response, the medulla’s breathing control center alters the rate and depth of breathing, increasing both to dispose of excess CO 2 or decreasing both if CO 2 levels are depressed. Carotid arteries In a person at rest, these nerve impulses result in about 10 to 14 inhalations per minute. Between inhalations, the muscles relax and the person exhales. Aorta Diaphragm Rib muscles The sensors in the aorta and 6 carotid arteries also detect changes in O 2 levels in the blood and signal the medulla to increase the breathing rate when levels become very low.
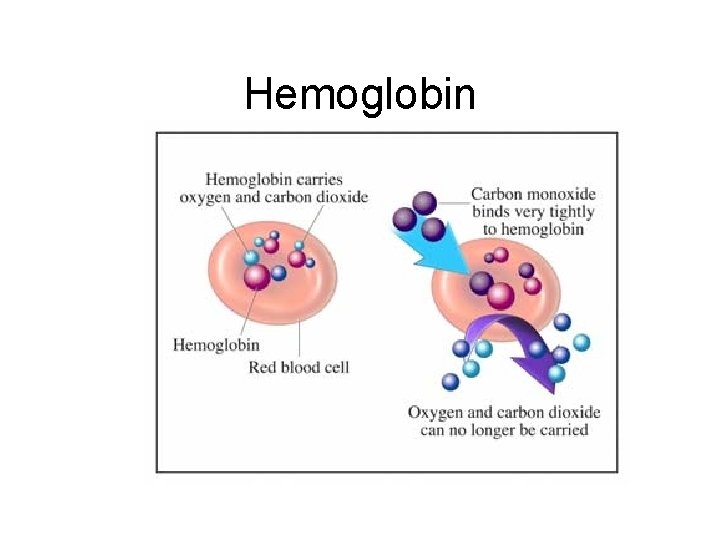
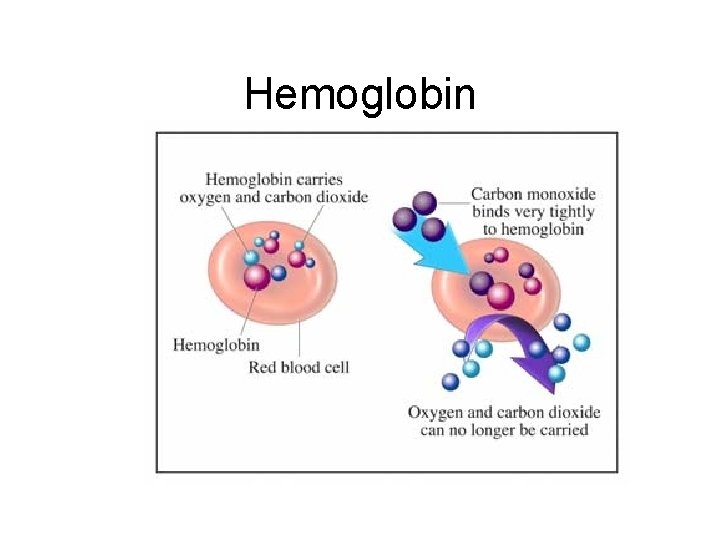
Hemoglobin

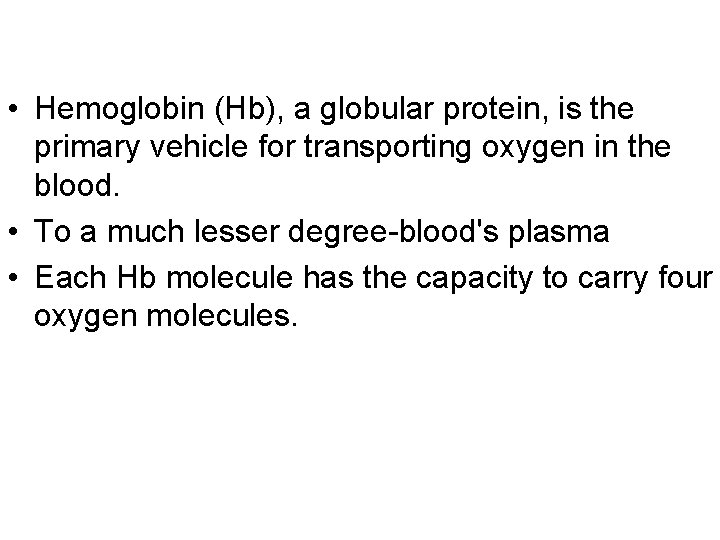
• Hemoglobin (Hb), a globular protein, is the primary vehicle for transporting oxygen in the blood. • To a much lesser degree-blood's plasma • Each Hb molecule has the capacity to carry four oxygen molecules.
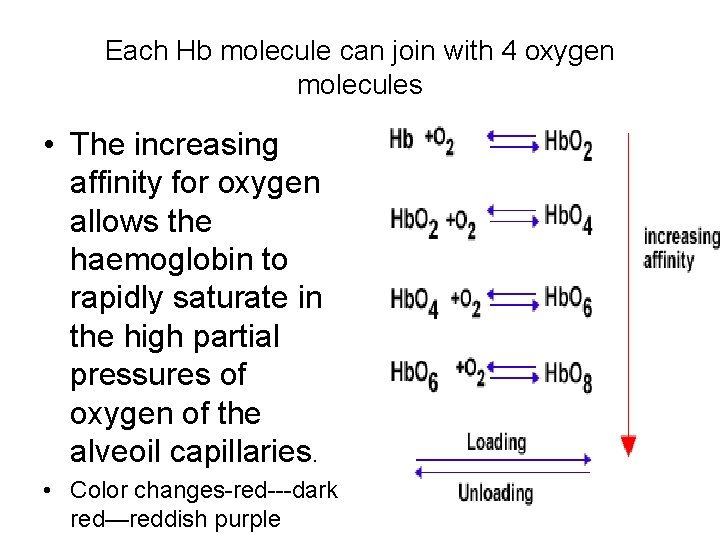
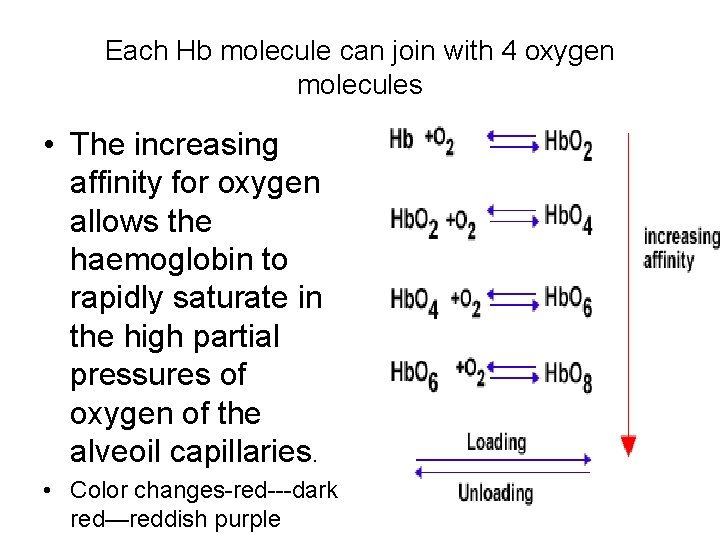
Each Hb molecule can join with 4 oxygen molecules • The increasing affinity for oxygen allows the haemoglobin to rapidly saturate in the high partial pressures of oxygen of the alveoil capillaries. • Color changes-red---dark red—reddish purple
The normal range of values for hemoglobin content • Female: 11. 5 -15. 5 g /dl • Male: 13. 5 -17. 5 g/dl
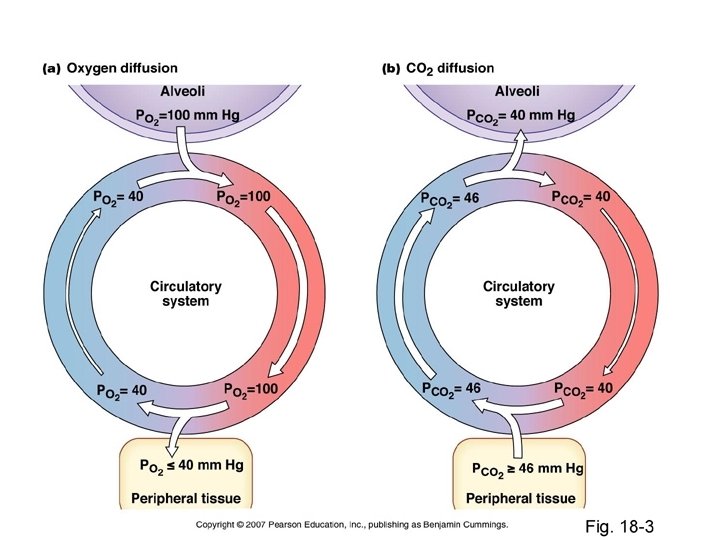
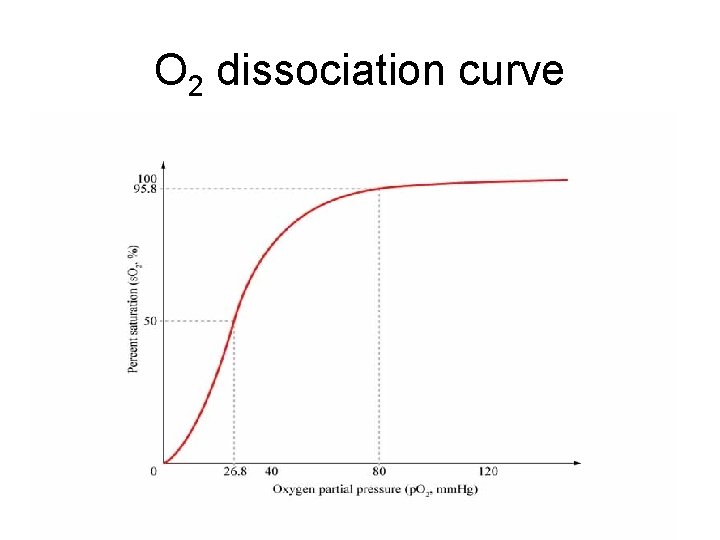
• The amount of oxygen bound to the Hb at any time is related, • to the partial pressure of oxygen to which the Hb is exposed. • In the lungs, at the alveolar–capillary interface, the partial pressure of O 2 is typically high, and therefore the oxygen binds readily to Hb that is present.
oxygen saturation. • How much of that capacity is filled by oxygen at any time is called the oxygen saturation. • Expressed as a percentage
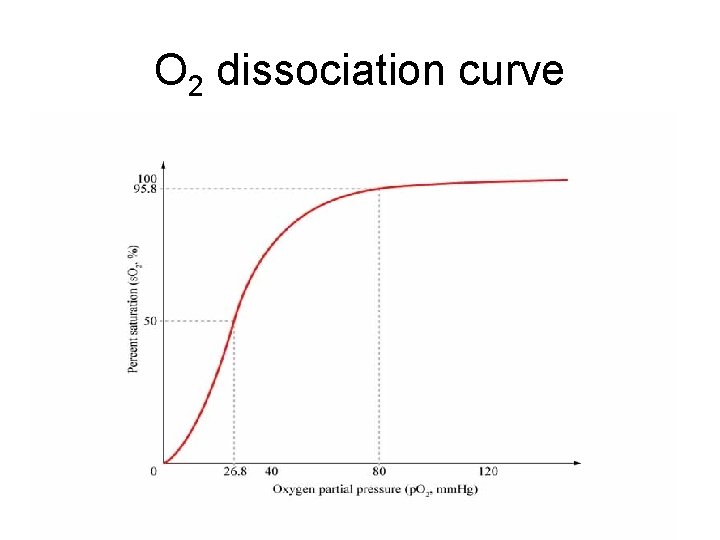
Oxygen dissociation curves. • Important tool for understanding how our blood carries and releases oxygen. • relates oxygen saturation and partial pressure of oxygen in the blood (p. O 2), and is determined by what is called “Hb's affinity for oxygen”; • how readily Hb acquires and releases oxygen molecules into the fluid that surrounds it.
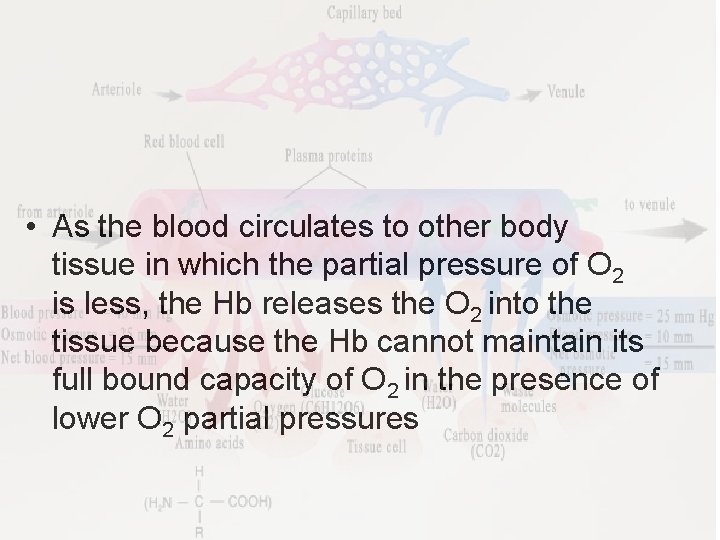
• As the blood circulates to other body tissue in which the partial pressure of O 2 is less, the Hb releases the O 2 into the tissue because the Hb cannot maintain its full bound capacity of O 2 in the presence of lower O 2 partial pressures
O 2 dissociation curve

The effect of carbon dioxide in the blood Hb can also bind carbon dioxide, but to a lesser extent. Carbaminohaemoglobin forms. Some carbon dioxide is carried in this form to the lungs from respiring tissues.
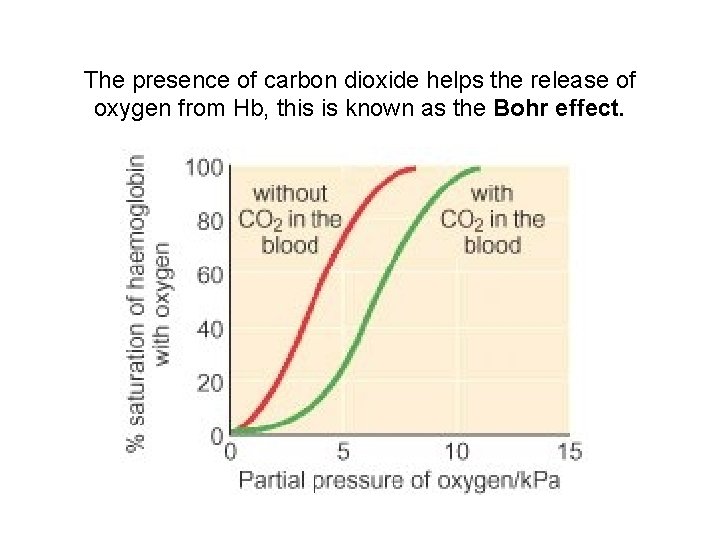
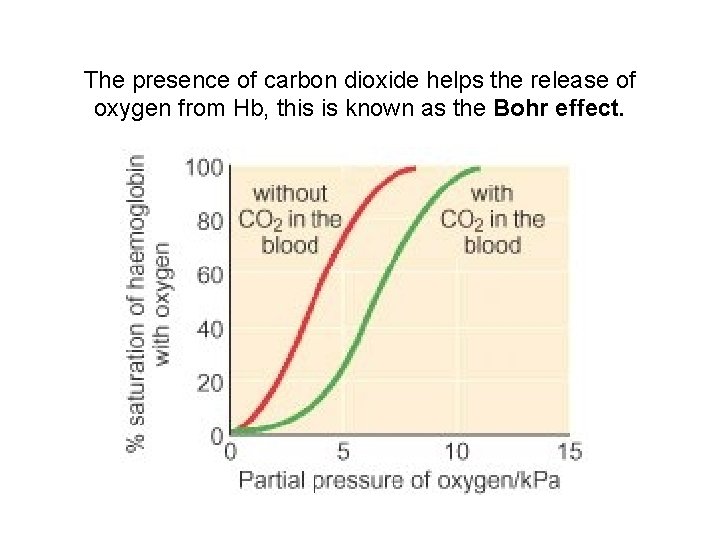
The presence of carbon dioxide helps the release of oxygen from Hb, this is known as the Bohr effect.



There are 3 ways in which carbon dioxide is transported in the blood: • 1. DISSOLVED CO 2 • more soluble in blood than oxygen • About 5 % of carbon dioxide is transported unchanged, simply dissolved in the plasma
2. BOUND TO HAEMOGLOBIN AND PLASMA PROTEINS • Carbon dioxide combines reversibly with Hb to form carbaminohaemoglobin. • Carbon dioxide does not bind to iron, as oxygen does, but to amino groups on the polypeptide chains of Hb. • 10 % of carbon dioxide is transported bound to Hb and plasma proteins
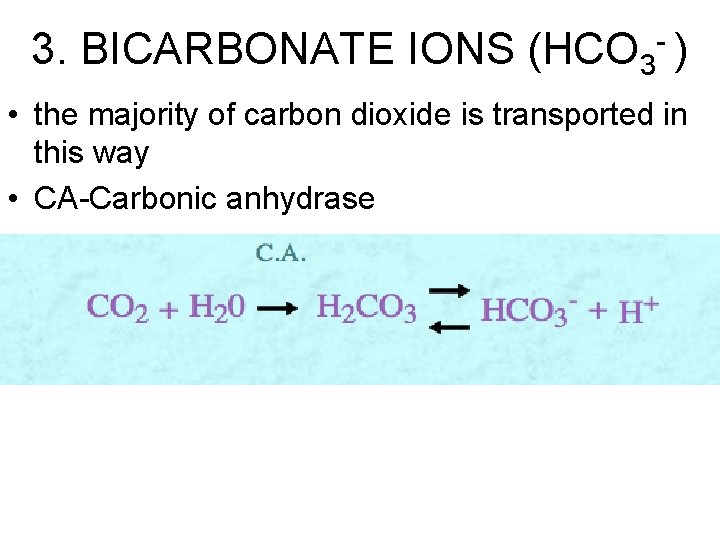
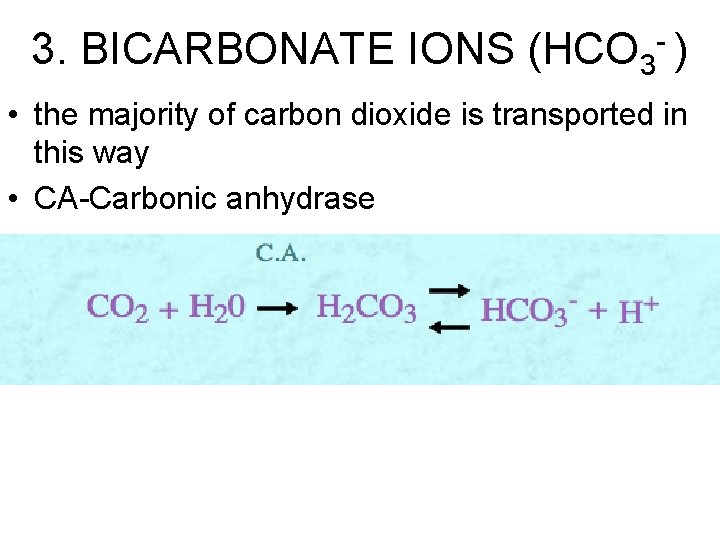
3. BICARBONATE IONS (HCO 3 - ) • the majority of carbon dioxide is transported in this way • CA-Carbonic anhydrase



 Mechanical ventilator modes
Mechanical ventilator modes Iso 21789
Iso 21789 Gas law
Gas law Difference between ideal gas and real gas
Difference between ideal gas and real gas Pseudo reduced specific volume
Pseudo reduced specific volume An ideal gas is an imaginary gas
An ideal gas is an imaginary gas Computational fluid dynamics
Computational fluid dynamics Conclusion
Conclusion Gas leaked in bhopal gas tragedy
Gas leaked in bhopal gas tragedy Gas reale e gas ideale
Gas reale e gas ideale Flue gas desulfurisation gas filter
Flue gas desulfurisation gas filter Poisonous gas leaked in bhopal gas tragedy
Poisonous gas leaked in bhopal gas tragedy Reaksi pembentukan gas no2f dari gas no2 dan f2
Reaksi pembentukan gas no2f dari gas no2 dan f2 Gas exchange key events in gas exchange
Gas exchange key events in gas exchange What are the factors affecting oxygenation
What are the factors affecting oxygenation Hvac presentation ppt
Hvac presentation ppt Pulmonary ventilation consists of two cyclic phases, , and
Pulmonary ventilation consists of two cyclic phases, , and Florence nightingale environment theory
Florence nightingale environment theory Basic terms and concepts of mechanical ventilation
Basic terms and concepts of mechanical ventilation East coast fire and ventilation
East coast fire and ventilation Local exhaust ventilation definition
Local exhaust ventilation definition Ventilasi di tempat kerja
Ventilasi di tempat kerja Indoor shooting range ventilation
Indoor shooting range ventilation Ventilator modes
Ventilator modes Ventilation sdb
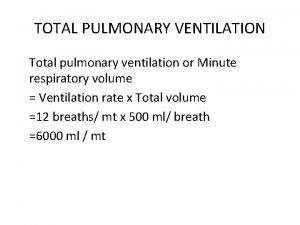
Ventilation sdb Normal minute ventilation
Normal minute ventilation Respiration vs ventilation
Respiration vs ventilation Desired co2 formula
Desired co2 formula 5 cut center rafter louver
5 cut center rafter louver Ashrae standard 15 refrigerant monitor
Ashrae standard 15 refrigerant monitor 405 field hospital
405 field hospital Bls algorithm
Bls algorithm Windpipe cells
Windpipe cells Bag mask ventilation
Bag mask ventilation Ventilation formula
Ventilation formula Natural ventilation
Natural ventilation 5 myths about attic ventilation
5 myths about attic ventilation T piece ventilation
T piece ventilation Mode of ventilation
Mode of ventilation Ventilators 101
Ventilators 101 Dyspnea index formula
Dyspnea index formula Normal minute ventilation
Normal minute ventilation Greenhouse ventilation calculator
Greenhouse ventilation calculator General shop safety rules
General shop safety rules Dilution ventilation
Dilution ventilation Ss-en 12097
Ss-en 12097