Fluids and electrolytes Terry Irwin MD FRCS Consultant











- Slides: 62
Fluids and electrolytes Terry Irwin MD FRCS Consultant Colorectal Surgeon
What we will cover § Assessing fluid needs § How to prescribe fluids and electrolytes § Common electrolyte problems
Who has agreed this protocol Surgery Anaesthesia Nephrology Medicine

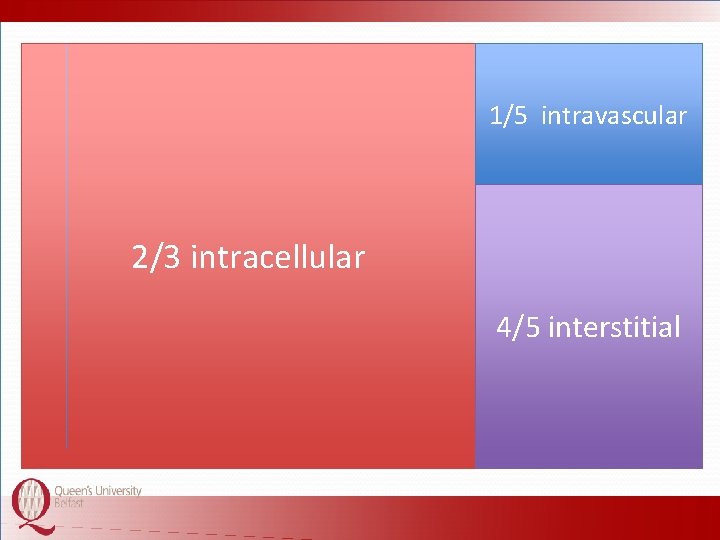
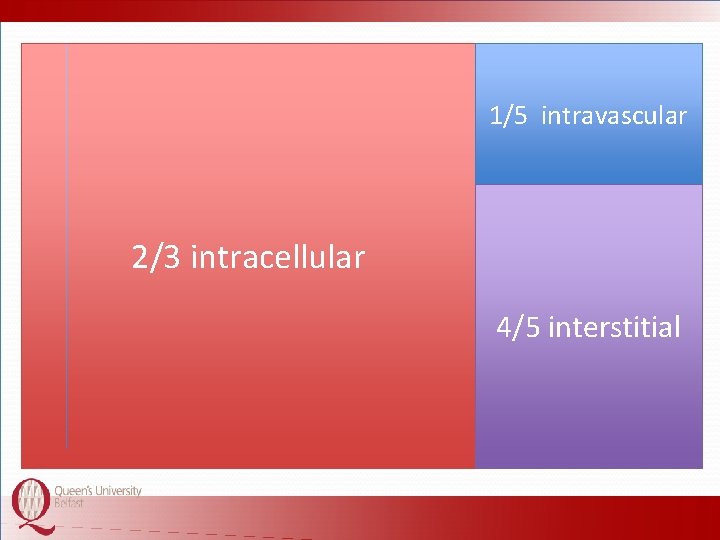
1/5 intravascular 1/3 Litres extracellular 602/3 tointracellular 70% water = 42 4/5 interstitial
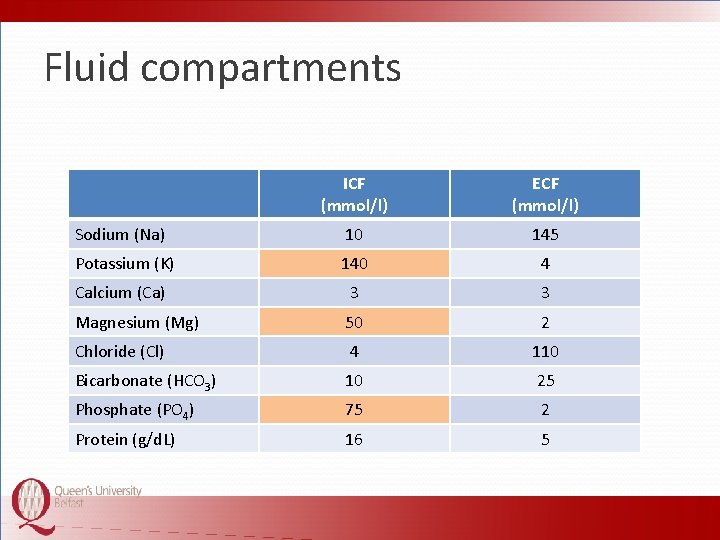
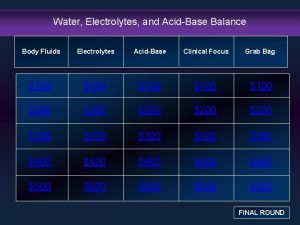
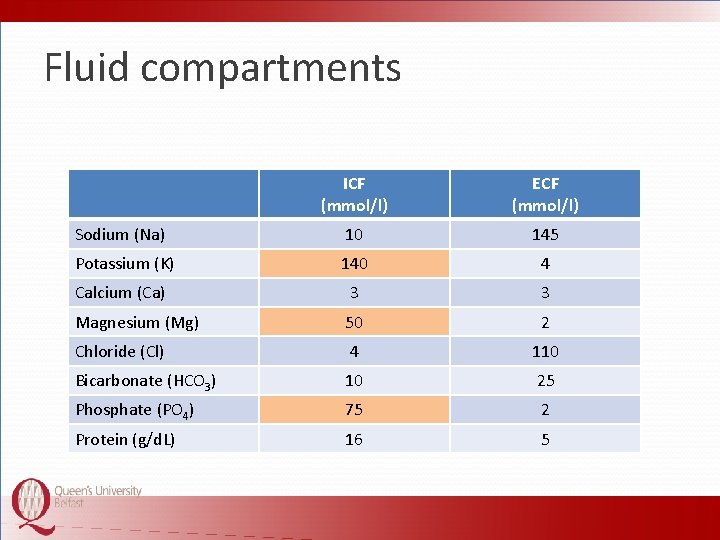
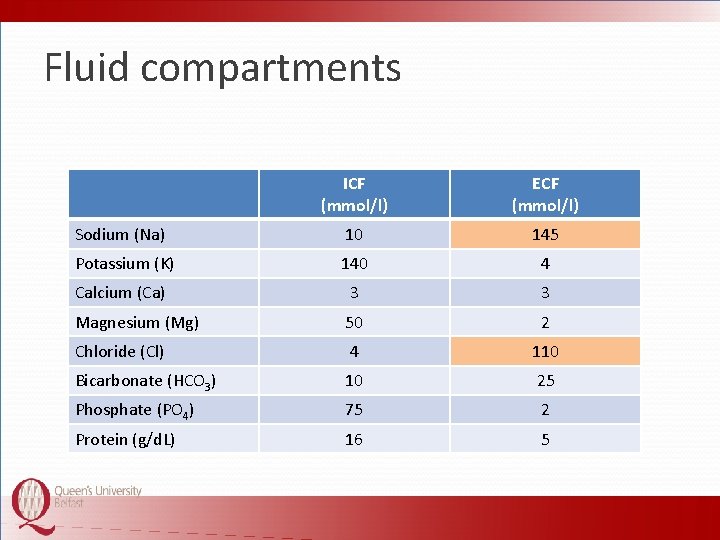
Fluid compartments ICF (mmol/l) ECF (mmol/l) Sodium (Na) 10 145 Potassium (K) 140 4 Calcium (Ca) 3 3 Magnesium (Mg) 50 2 Chloride (Cl) 4 110 Bicarbonate (HCO 3) 10 25 Phosphate (PO 4) 75 2 Protein (g/d. L) 16 5
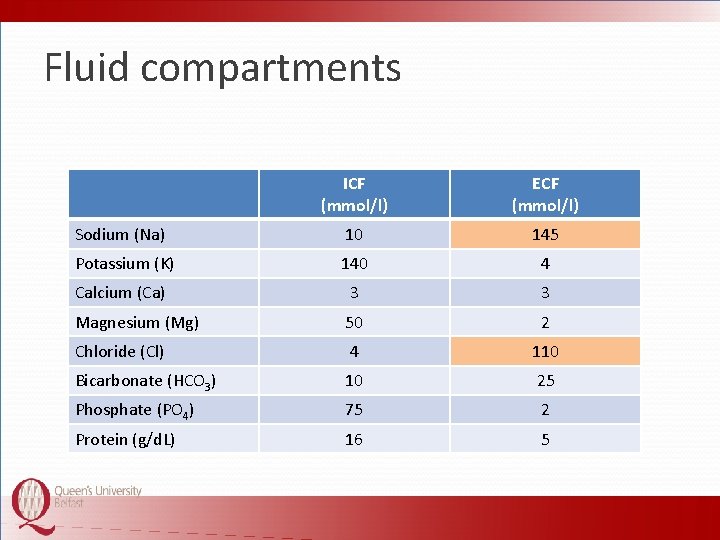
Fluid compartments ICF (mmol/l) ECF (mmol/l) Sodium (Na) 10 145 Potassium (K) 140 4 Calcium (Ca) 3 3 Magnesium (Mg) 50 2 Chloride (Cl) 4 110 Bicarbonate (HCO 3) 10 25 Phosphate (PO 4) 75 2 Protein (g/d. L) 16 5
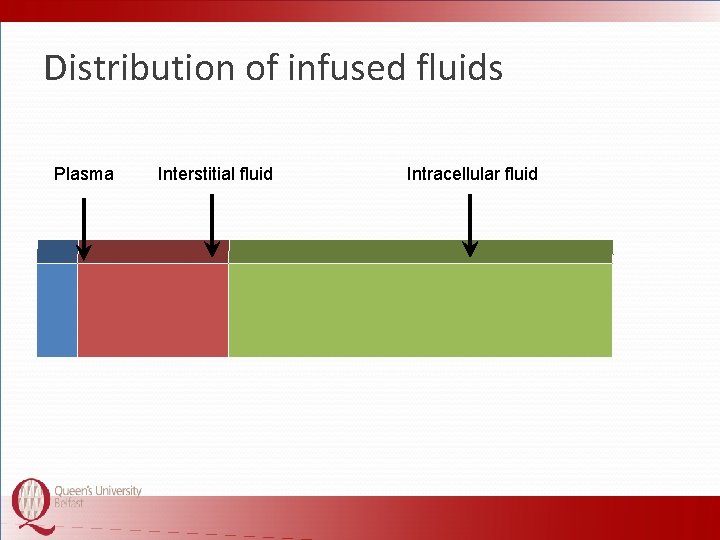
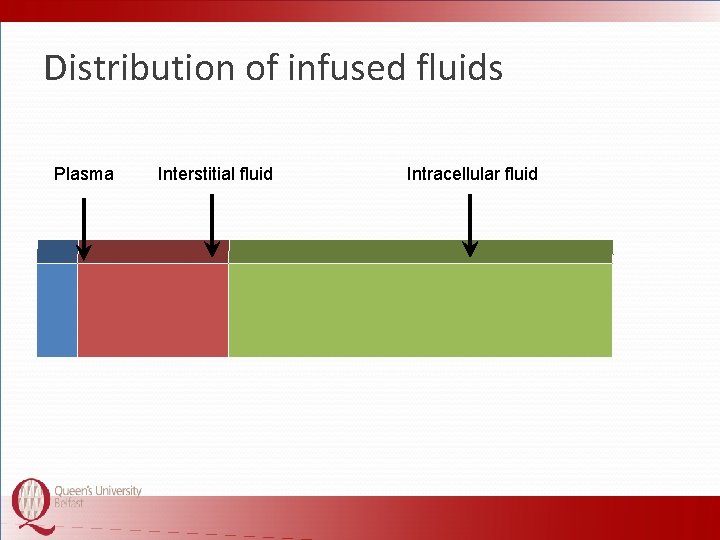
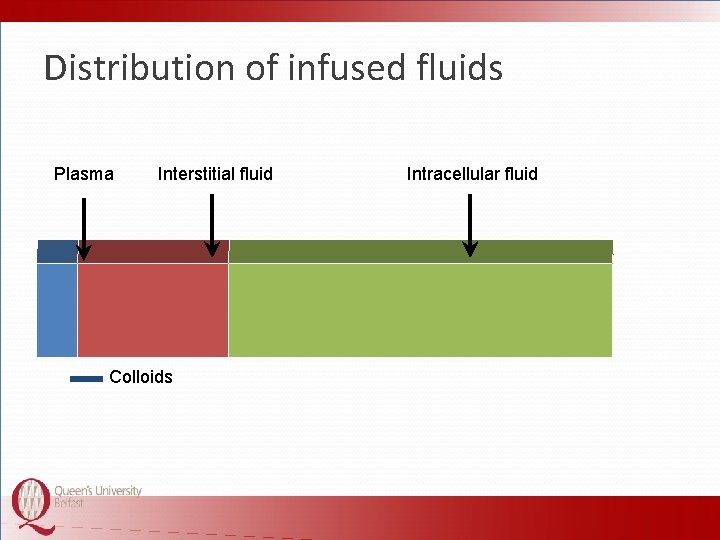
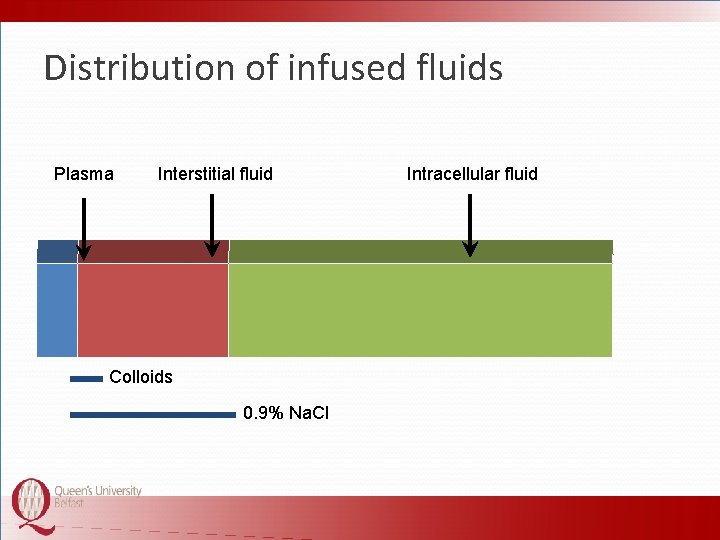
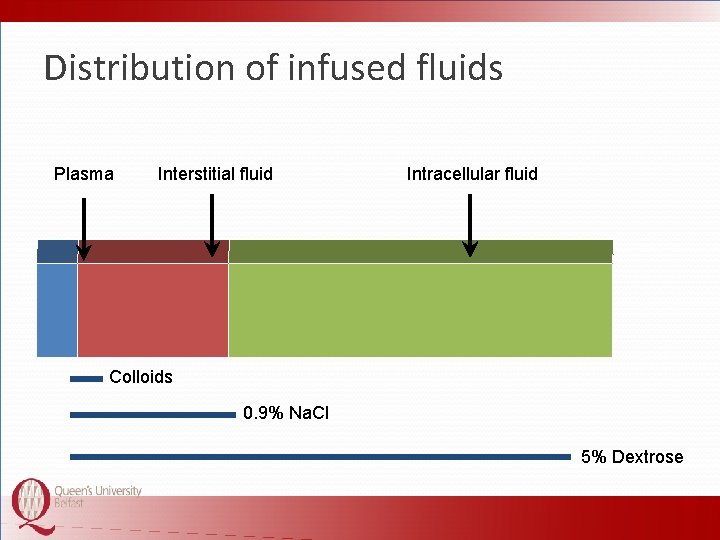
Distribution of infused fluids Plasma Interstitial fluid Intracellular fluid
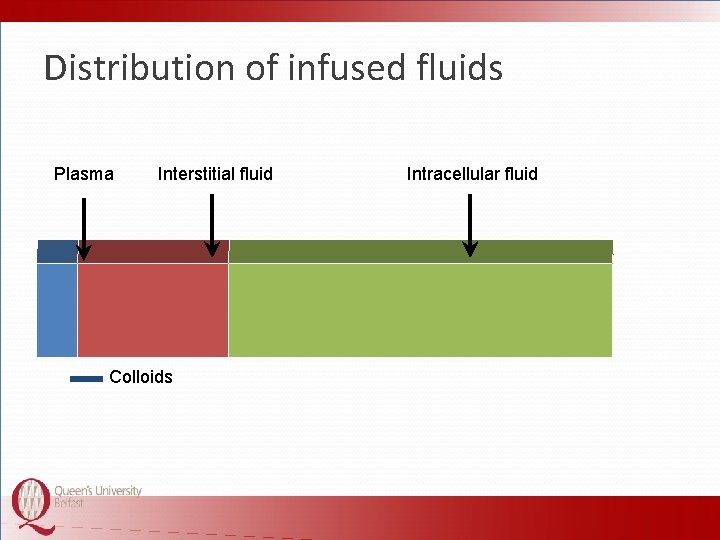
Distribution of infused fluids Plasma Interstitial fluid Colloids Intracellular fluid
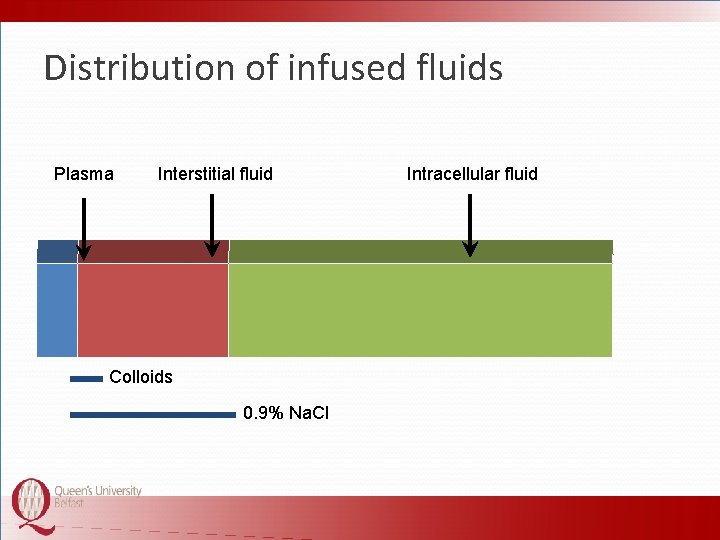
Distribution of infused fluids Plasma Interstitial fluid Colloids 0. 9% Na. Cl Intracellular fluid
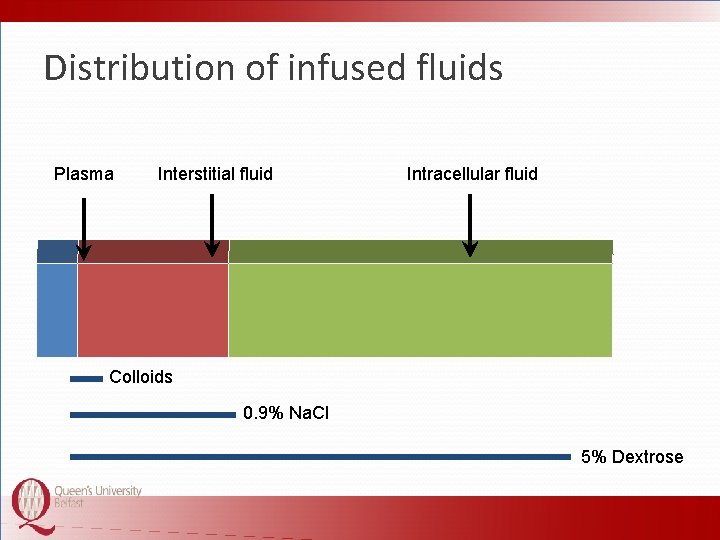
Distribution of infused fluids Plasma Interstitial fluid Intracellular fluid Colloids 0. 9% Na. Cl 5% Dextrose
Why do we give fluids § Replace lost volume § Maintenance of daily requirements § Replace haemoglobin § Replace blood component § Diluent for drugs § Physical effect
Why do we give fluids § Replace lost volume § Maintenance of daily requirements § Replace haemoglobin § Replace blood component § Diluent for drugs § Physical effect
Daily prescriptions § Water § Sodium § Potassium
How do you decide how much fluid to prescribe?
Fluid volume prescription § Shock § Replacement of any existing deficit § Daily maintenance fluids § Allowance for predicted excess losses






Shock § Fluid bolus (usually 200 ml) § Rapid infusion, not increased rate § Repeat as necessary § Monitor immediate response
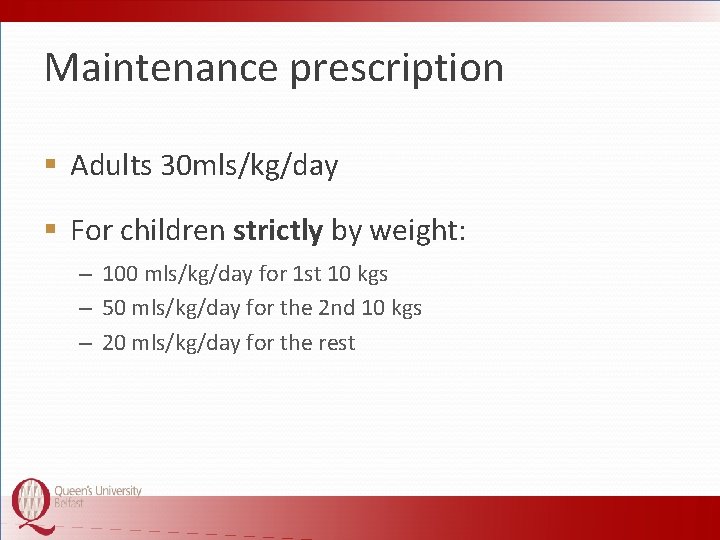
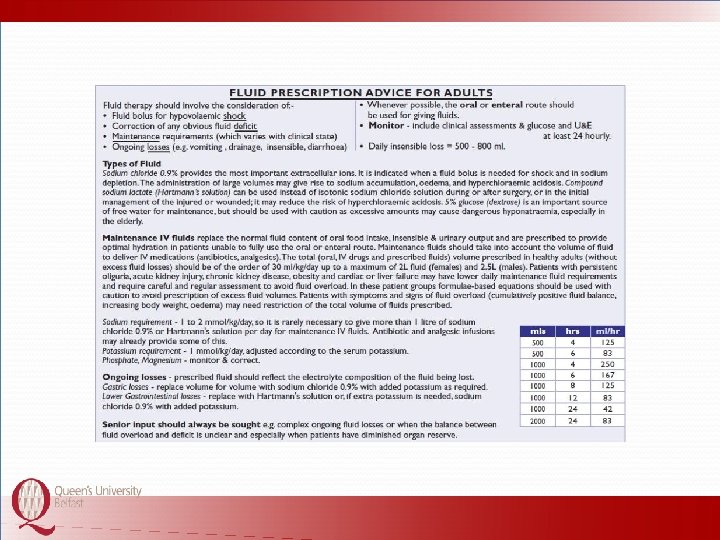
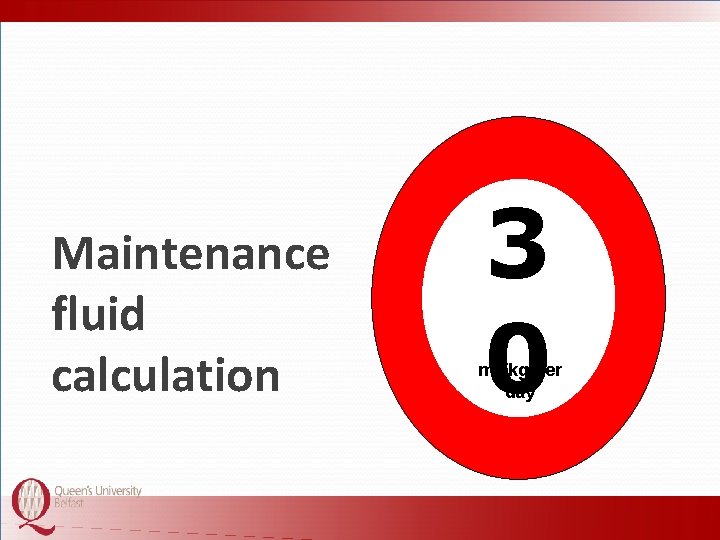
Maintenance prescription § Adults 30 mls/kg/day § For children strictly by weight: – 100 mls/kg/day for 1 st 10 kgs – 50 mls/kg/day for the 2 nd 10 kgs – 20 mls/kg/day for the rest

Maximum 2. 5 litres

Maximu m 2 litres
Sodium and Potassium
Sodium § 2 mmols/kg/day § Up to a maximum of 150 mmol/day
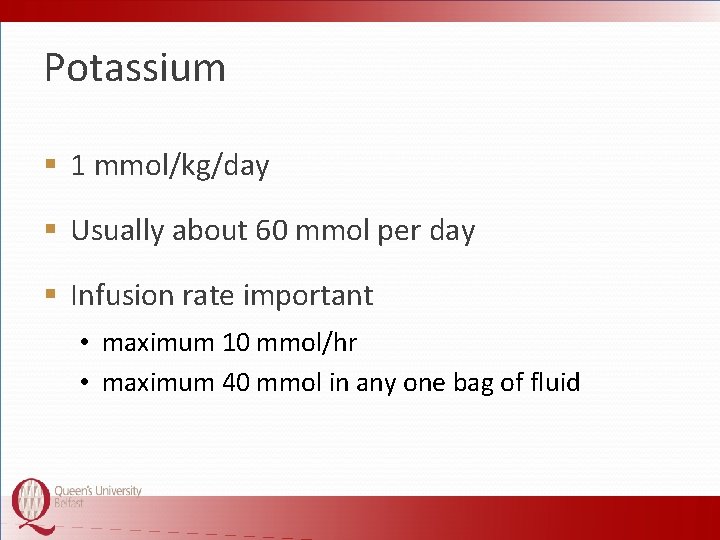
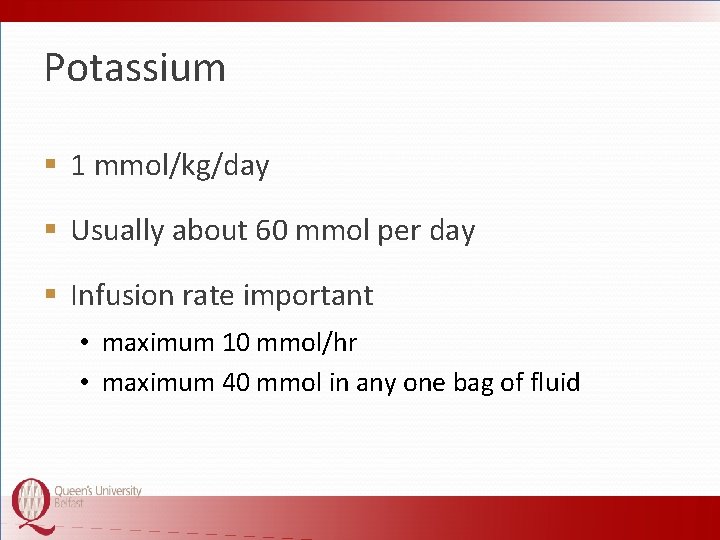
Potassium § 1 mmol/kg/day § Usually about 60 mmol per day § Infusion rate important • maximum 10 mmol/hr • maximum 40 mmol in any one bag of fluid
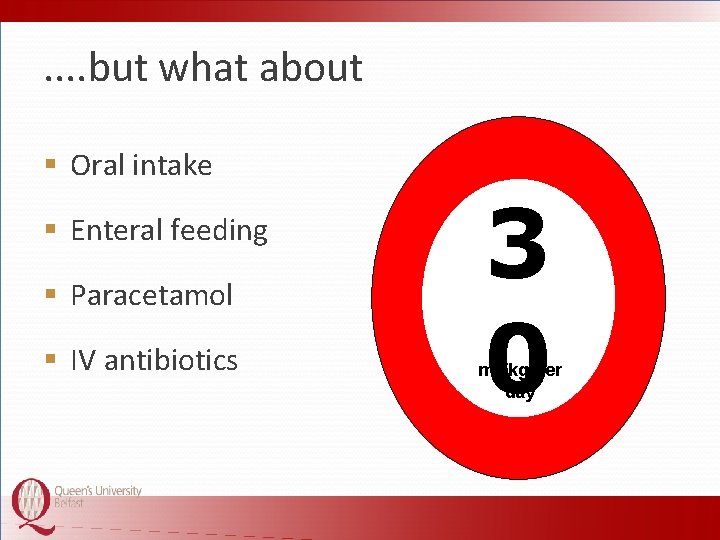
Maintenance fluid calculation 3 0 ml /kg per day

Can your patient drink?
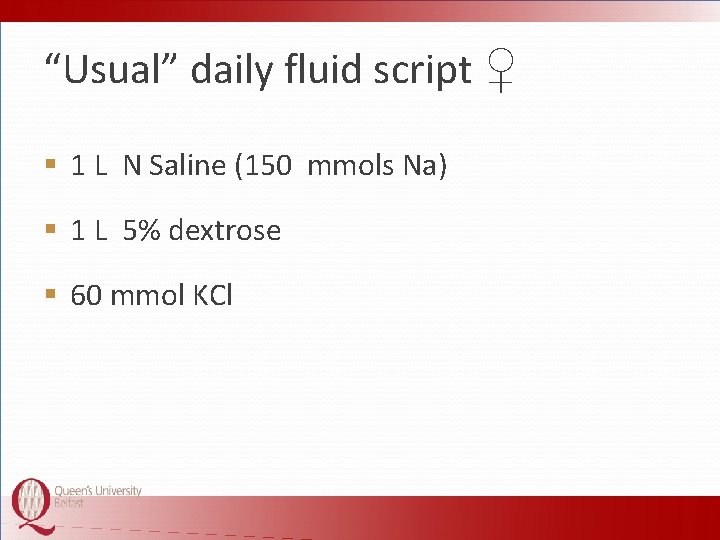
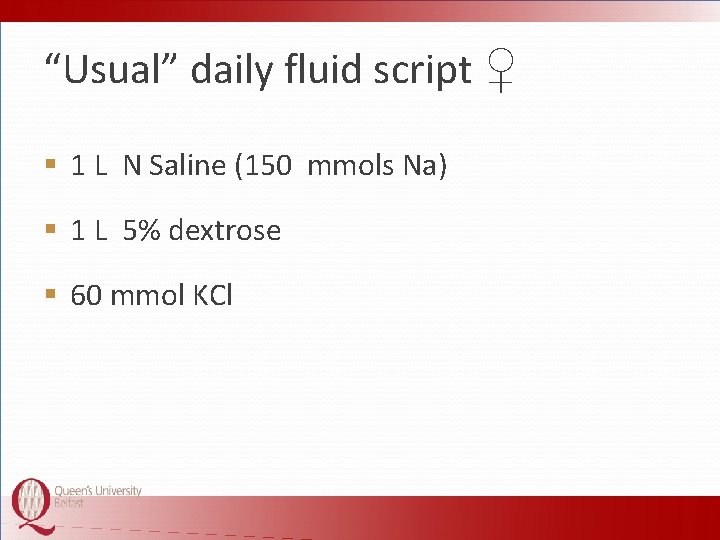
“Usual” daily fluid script ♀ § 1 L N Saline (150 mmols Na) § 1 L 5% dextrose § 60 mmol KCl
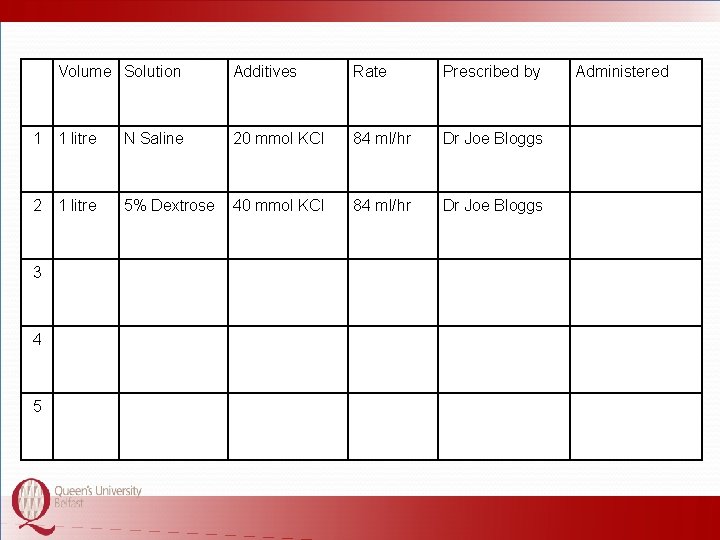
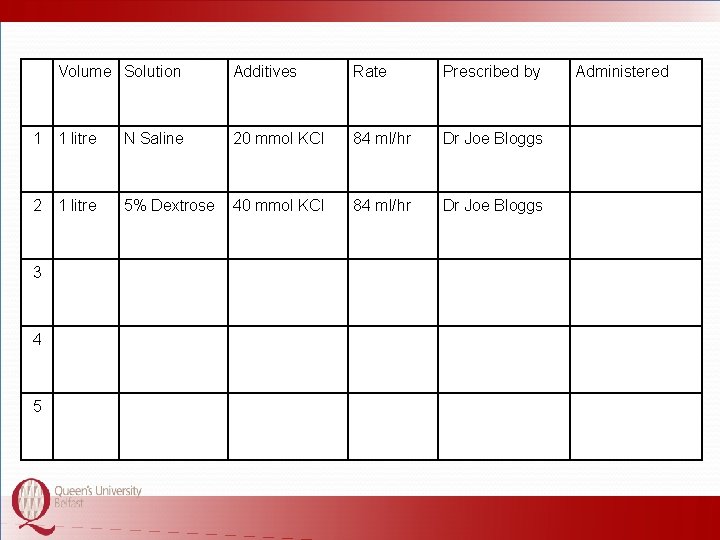
Volume Solution Additives Rate Prescribed by 1 1 litre N Saline 20 mmol KCl 84 ml/hr Dr Joe Bloggs 2 1 litre 5% Dextrose 40 mmol KCl 84 ml/hr Dr Joe Bloggs 3 4 5 Administered
. . but what about § Oral intake § Enteral feeding § Paracetamol § IV antibiotics 3 0 ml /kg per day
If she is receiving § 600 mls oral fluids per day § 100 ml paracetamol IV 6 hourly
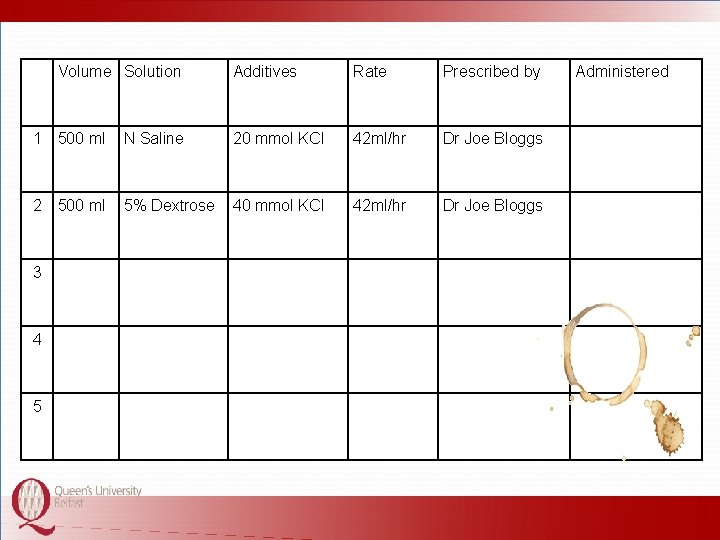
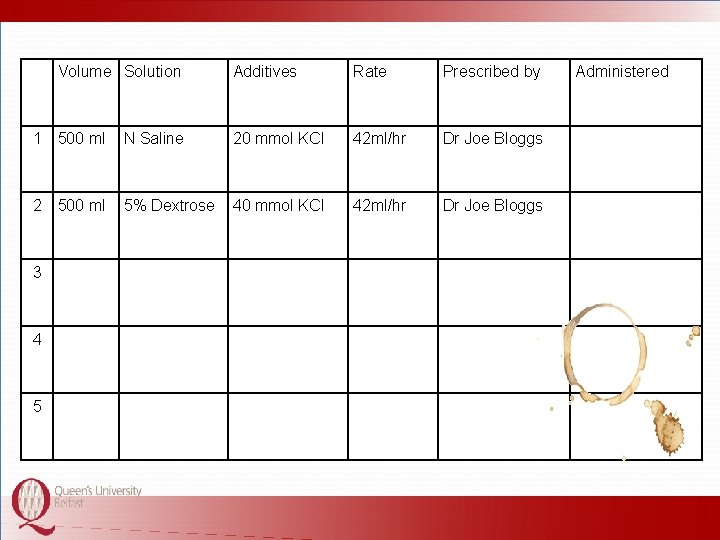
Volume Solution Additives Rate Prescribed by 1 500 ml N Saline 20 mmol KCl 42 ml/hr Dr Joe Bloggs 2 500 ml 5% Dextrose 40 mmol KCl 42 ml/hr Dr Joe Bloggs 3 4 5 Administered
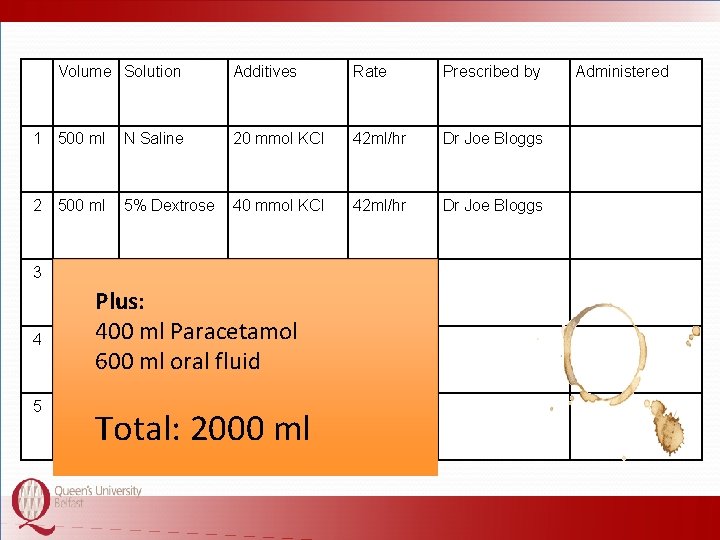
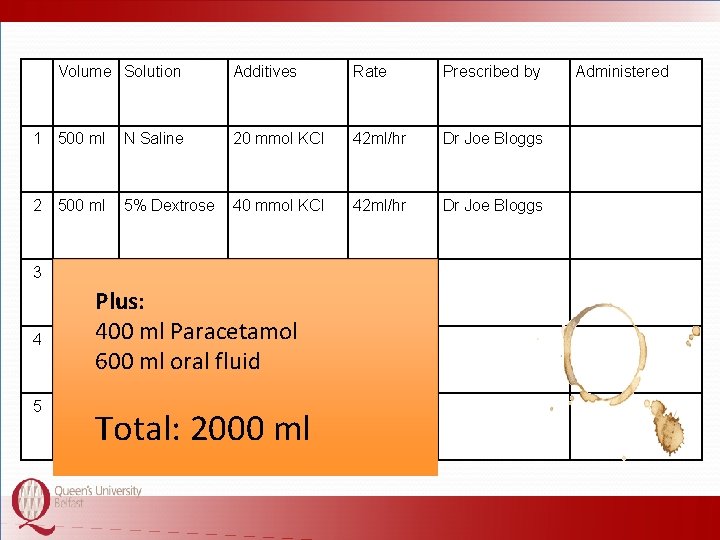
Volume Solution Additives Rate Prescribed by 1 500 ml N Saline 20 mmol KCl 42 ml/hr Dr Joe Bloggs 2 500 ml 5% Dextrose 40 mmol KCl 42 ml/hr Dr Joe Bloggs 3 4 5 Plus: 400 ml Paracetamol 600 ml oral fluid Total: 2000 ml Administered

Replacing the deficit
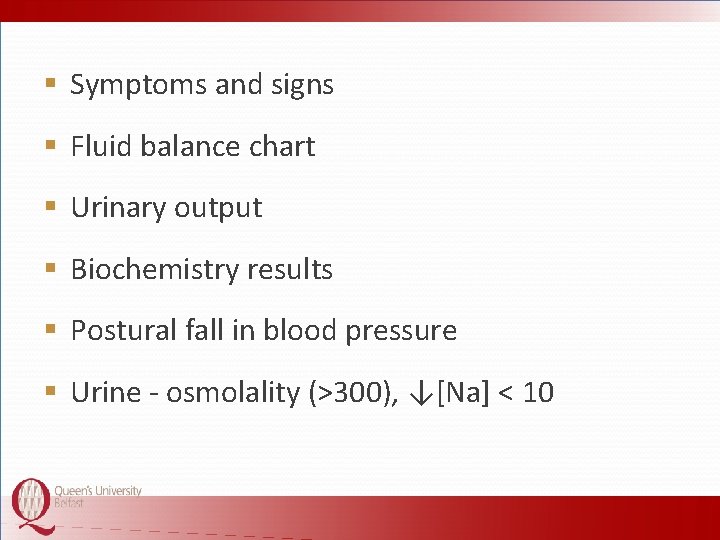
§ Symptoms and signs § Fluid balance chart § Urinary output § Biochemistry results § Postural fall in blood pressure § Urine - osmolality (>300), ↓[Na] < 10
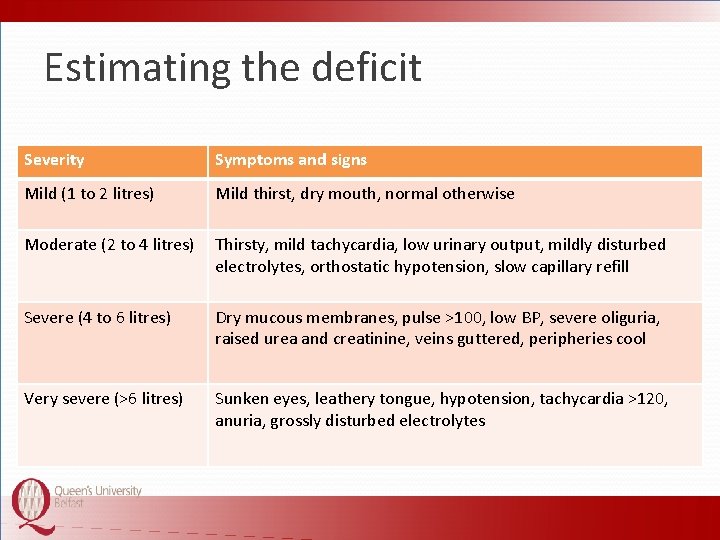
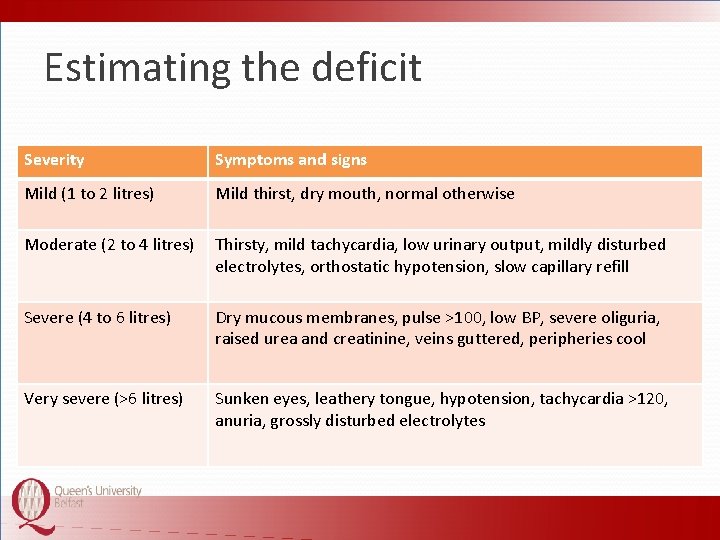
Estimating the deficit Severity Symptoms and signs Mild (1 to 2 litres) Mild thirst, dry mouth, normal otherwise Moderate (2 to 4 litres) Thirsty, mild tachycardia, low urinary output, mildly disturbed electrolytes, orthostatic hypotension, slow capillary refill Severe (4 to 6 litres) Dry mucous membranes, pulse >100, low BP, severe oliguria, raised urea and creatinine, veins guttered, peripheries cool Very severe (>6 litres) Sunken eyes, leathery tongue, hypotension, tachycardia >120, anuria, grossly disturbed electrolytes
Replacing the deficit § Estimate the deficit § Choose the most appropriate fluid § Replace over 24 to 36 hours § Monitor response
Excess losses Ongoing losses
Excess losses § Gastric – Vomiting – NG aspiration § Bowel – Diarrhoea – Stoma output § Fistulae
Excess losses § Calculate estimated volume § Replace with same volume of appropriate fluid § Always within the next 24 hour period
What fluid should be used?
Replace with N Saline with potassium as required
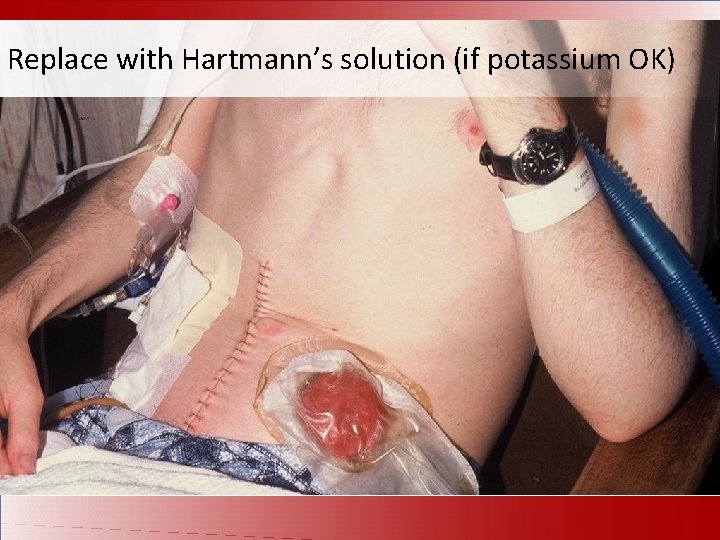
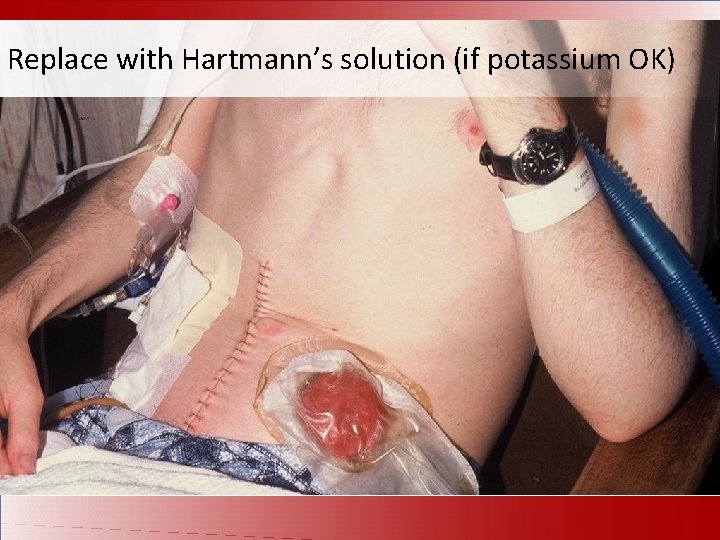
Replace with Hartmann’s solution (if potassium OK)
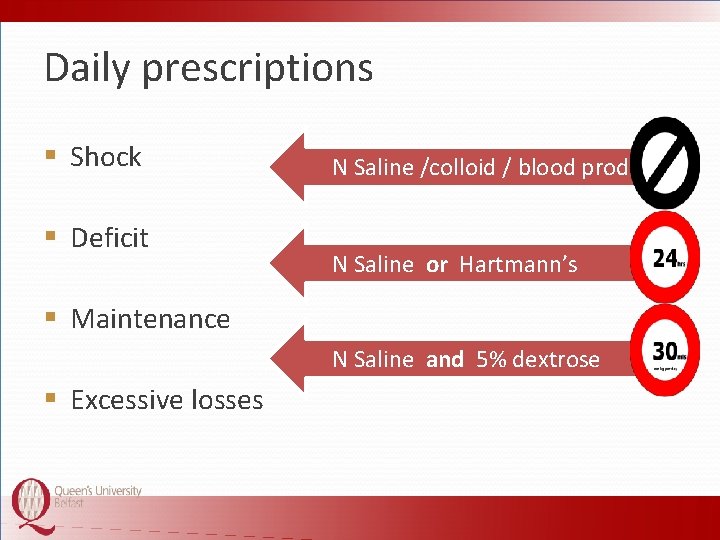
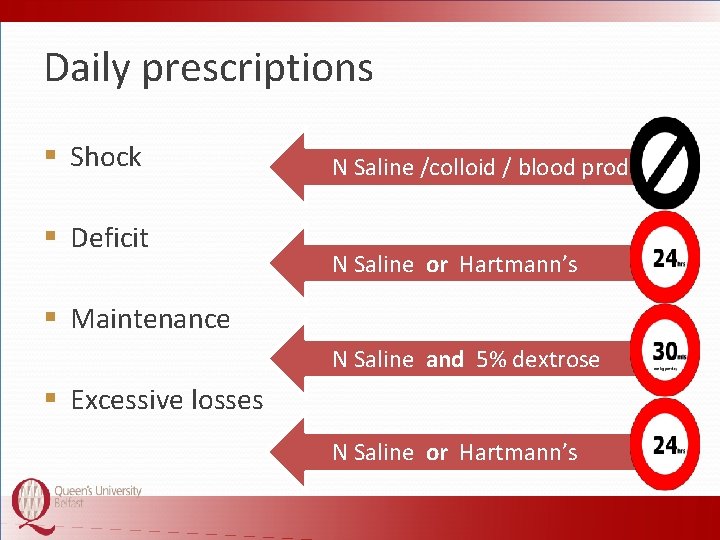
Daily prescriptions § Shock § Deficit § Maintenance § Excessive losses
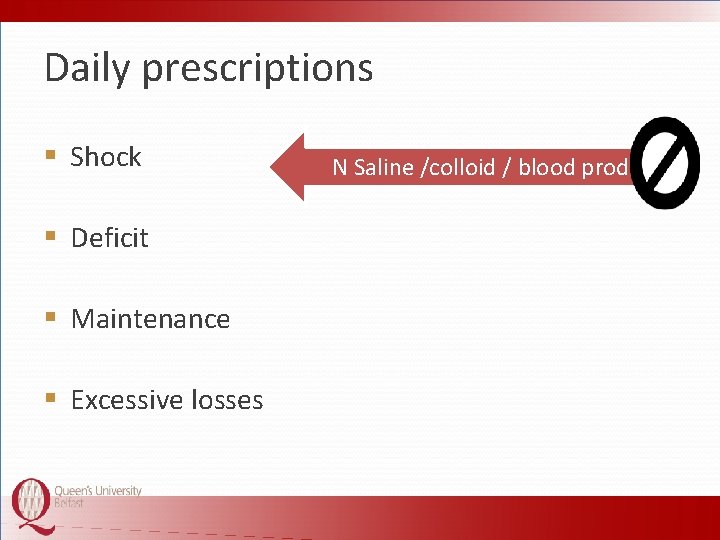
Daily prescriptions § Shock § Deficit § Maintenance § Excessive losses N Saline /colloid / blood products
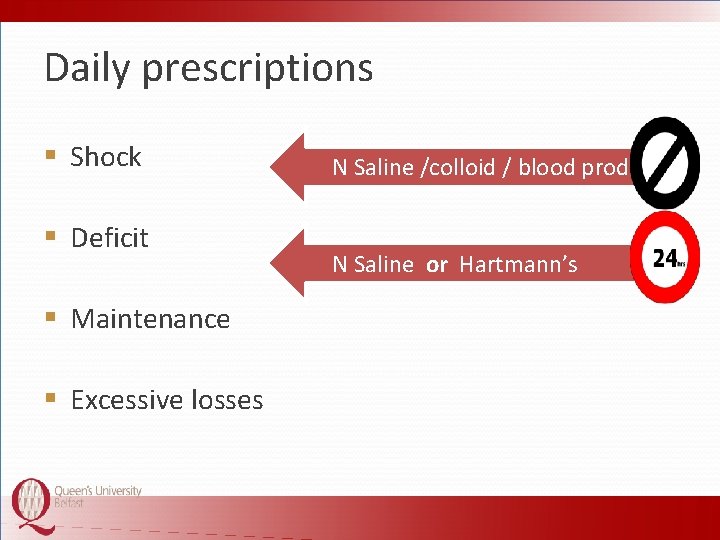
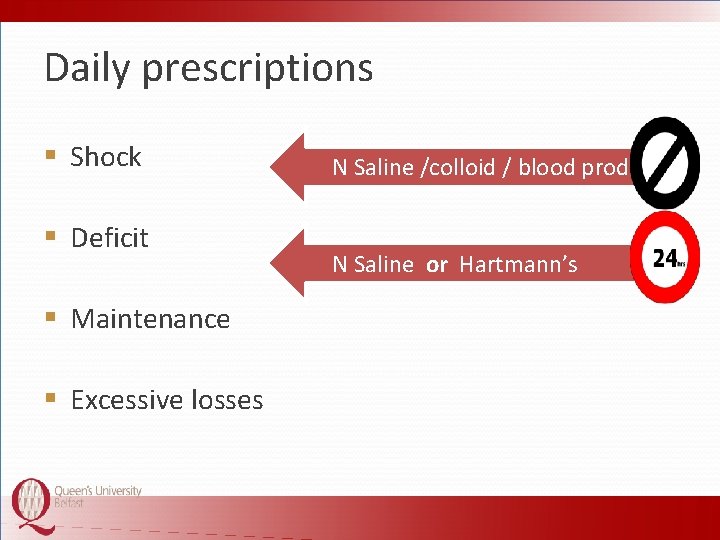
Daily prescriptions § Shock § Deficit § Maintenance § Excessive losses N Saline /colloid / blood products N Saline or Hartmann’s
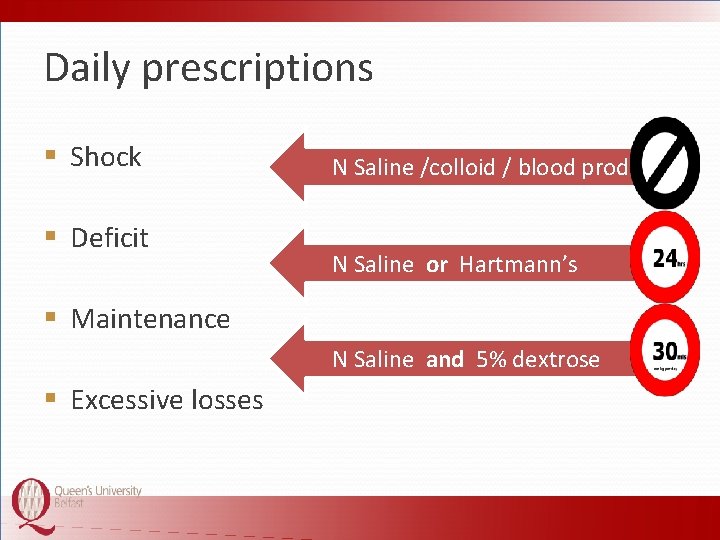
Daily prescriptions § Shock § Deficit N Saline /colloid / blood products N Saline or Hartmann’s § Maintenance N Saline and 5% dextrose § Excessive losses
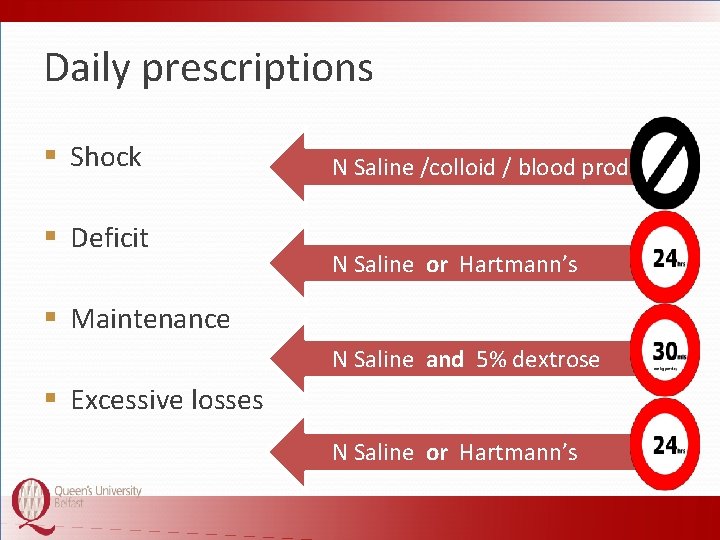
Daily prescriptions § Shock § Deficit N Saline /colloid / blood products N Saline or Hartmann’s § Maintenance N Saline and 5% dextrose § Excessive losses N Saline or Hartmann’s
Common problems
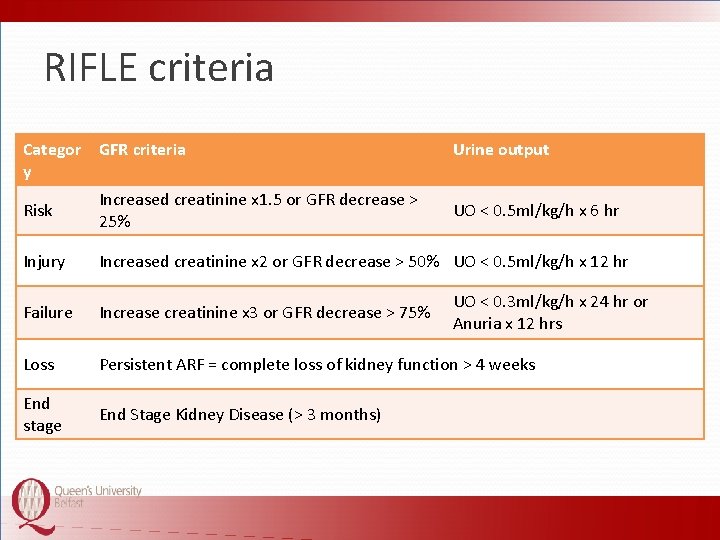
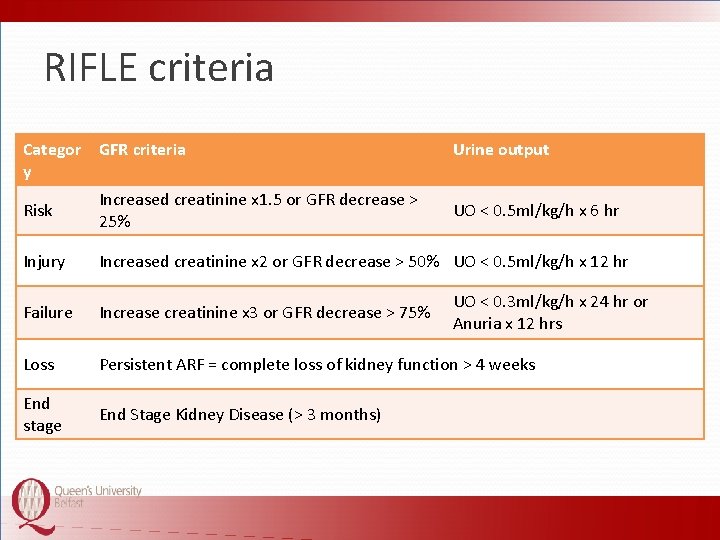
RIFLE criteria Categor GFR criteria y Urine output Risk Increased creatinine x 1. 5 or GFR decrease > 25% Injury Increased creatinine x 2 or GFR decrease > 50% UO < 0. 5 ml/kg/h x 12 hr Failure Increase creatinine x 3 or GFR decrease > 75% Loss Persistent ARF = complete loss of kidney function > 4 weeks End stage End Stage Kidney Disease (> 3 months) UO < 0. 5 ml/kg/h x 6 hr UO < 0. 3 ml/kg/h x 24 hr or Anuria x 12 hrs
Hyponatraemia
Hyponatraemia Too much water, not too few buildings!
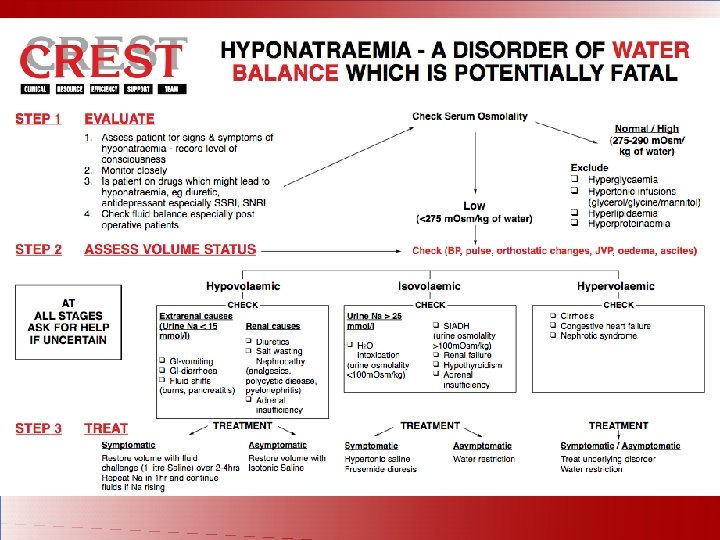
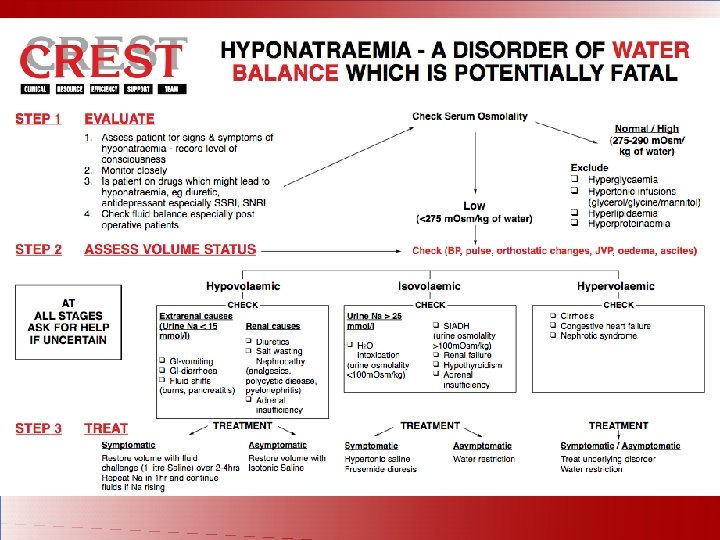
§ Usually caused by XS prescription of water § GAIN guidelines available www. gain-ni. org
Hypokalaemia § Often under-prescription of potassium § May be due to excessive losses
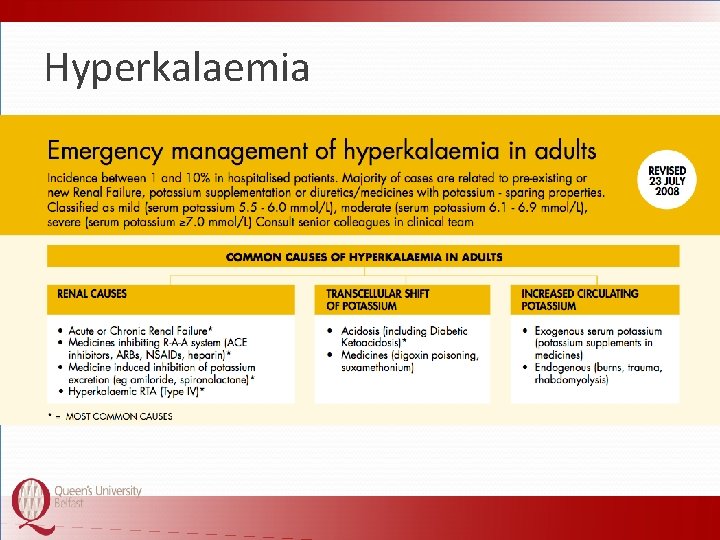
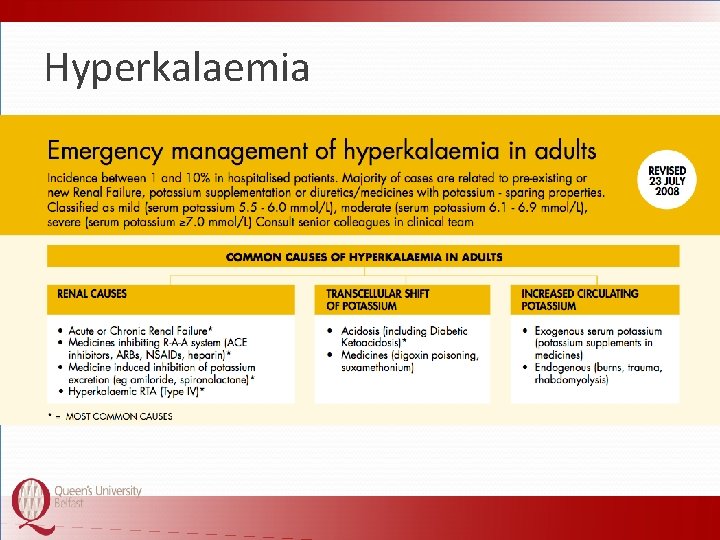
Hyperkalaemia
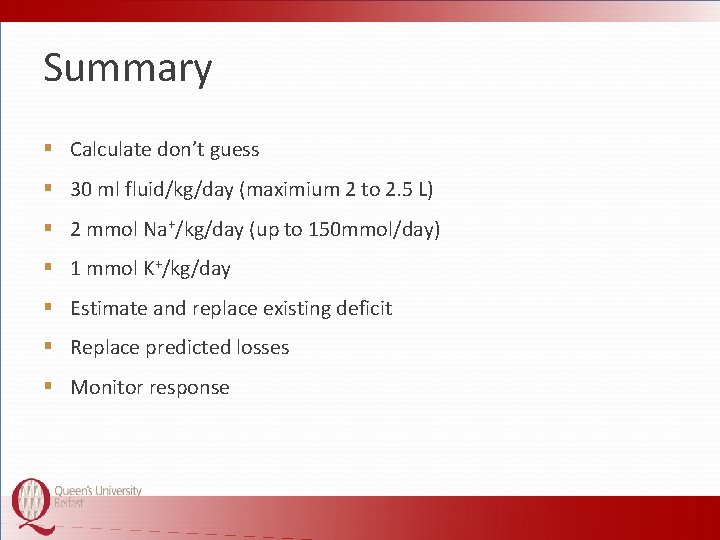
Summary § Calculate don’t guess § 30 ml fluid/kg/day (maximium 2 to 2. 5 L) § 2 mmol Na+/kg/day (up to 150 mmol/day) § 1 mmol K+/kg/day § Estimate and replace existing deficit § Replace predicted losses § Monitor response
 Chapter 18 fluids and electrolytes
Chapter 18 fluids and electrolytes Alpine course frcs
Alpine course frcs Frcs ed meaning
Frcs ed meaning Titul frcs(t)
Titul frcs(t) Dka and electrolytes
Dka and electrolytes Vacid definition
Vacid definition Negative deviation from raoult's law
Negative deviation from raoult's law Major intra and extracellular electrolytes
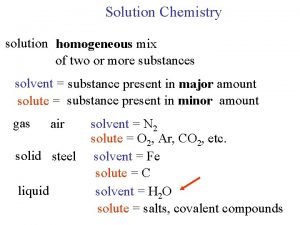
Major intra and extracellular electrolytes Electrolytes and nonelectrolytes
Electrolytes and nonelectrolytes Solubility curve
Solubility curve Pabrinex 1 and 2
Pabrinex 1 and 2 Medicare enteral qualification checklist
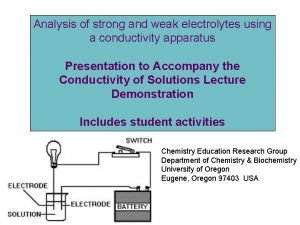
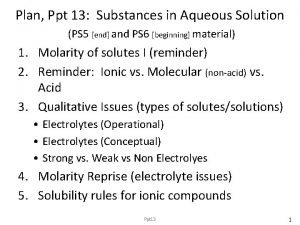
Medicare enteral qualification checklist Strong vs weak electrolytes
Strong vs weak electrolytes Dr dawn lim
Dr dawn lim Electrolytes normal range
Electrolytes normal range Normal values of potassium
Normal values of potassium Strong vs weak electrolytes
Strong vs weak electrolytes Strong vs weak electrolytes
Strong vs weak electrolytes How does electrolytes affects the chemical equilibria
How does electrolytes affects the chemical equilibria Weak electrolytes
Weak electrolytes Electrolytes ppt
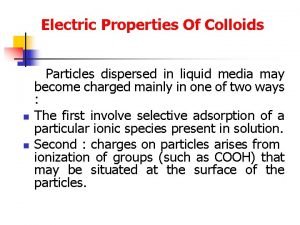
Electrolytes ppt Protective colloids
Protective colloids Definition of colloid
Definition of colloid Herbalife electrolytes
Herbalife electrolytes Irwin altman and dalmas taylor
Irwin altman and dalmas taylor Irwin altman and dalmas taylor
Irwin altman and dalmas taylor Dalmas taylor
Dalmas taylor Solids liquids and gases section 2 properties of fluids
Solids liquids and gases section 2 properties of fluids Compressible and incompressible fluids
Compressible and incompressible fluids Australian standards for texture modified foods and fluids
Australian standards for texture modified foods and fluids Compressible and incompressible fluids
Compressible and incompressible fluids Why are liquids incompressible
Why are liquids incompressible Fluids physics problems and solutions
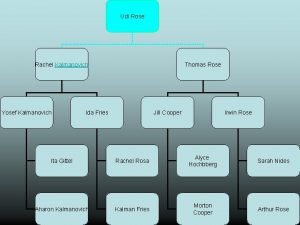
Fluids physics problems and solutions Ward temple and family history leader
Ward temple and family history leader Letter to viceroy lord irwin analyzing the text answers
Letter to viceroy lord irwin analyzing the text answers Gandhi letter to lord irwin rhetorical analysis
Gandhi letter to lord irwin rhetorical analysis Irwin fridovich
Irwin fridovich Intermediate math problems for students by m. colwell
Intermediate math problems for students by m. colwell Shannon paz
Shannon paz Jimmy irwin
Jimmy irwin Howard irwin titanic
Howard irwin titanic Irwin sanders
Irwin sanders Irwin rosenstock
Irwin rosenstock Irwin lasher
Irwin lasher Mr irwin lasher
Mr irwin lasher De jong
De jong Irwin rose indianapolis
Irwin rose indianapolis Irwin seating dealers
Irwin seating dealers Coming home mary irwin
Coming home mary irwin Chronic pain management irwin
Chronic pain management irwin Mary jane irwin
Mary jane irwin Eye drops off shelf
Eye drops off shelf Colloids fluids examples
Colloids fluids examples Learn composition of various synthetic bases
Learn composition of various synthetic bases Science 8- fluids under pressure worksheet answer key
Science 8- fluids under pressure worksheet answer key Plasmlyte
Plasmlyte 4 2 1 fluid rule
4 2 1 fluid rule Fluid order chart
Fluid order chart Hypertonic solution iv fluid
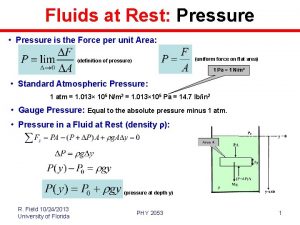
Hypertonic solution iv fluid Fluid at rest
Fluid at rest Colloid fluids
Colloid fluids Colloids iv fluids examples
Colloids iv fluids examples Crystalloid solutions
Crystalloid solutions