Dysmenorrhea Preeti Matkins MD CMC Dept of Pediatrics























- Slides: 54
Dysmenorrhea Preeti Matkins, MD CMC Dept of Pediatrics Teen Health Connection July 2006
Suzie chief complaint of “painful periods” n n n 14 ½ year old female periods about every month soaks through pads about every 3 hours

Menstrual Disorders n n n Amenorrhea Dysfunctional Uterine Bleeding n Longer menses or shortened cycle n Heavy menstrual flow n Longer and heavier flow n Painful menses Menorrhagia Metorrhagia Menometorrhagia Dysmenorrhea
Dysmenorrhea painful menses n Primary Begin in adolescence n Not due to pelvic disease n n Secondary Uncommon in adolescence n Due to pelvic pathology n
Dysmenorrhea n Most common gynecologic condition of adolescence n n Prevalence 20 -90% Most teens do not seek medical care Use OTC n Not sure who will treat n Fear pelvic exam n
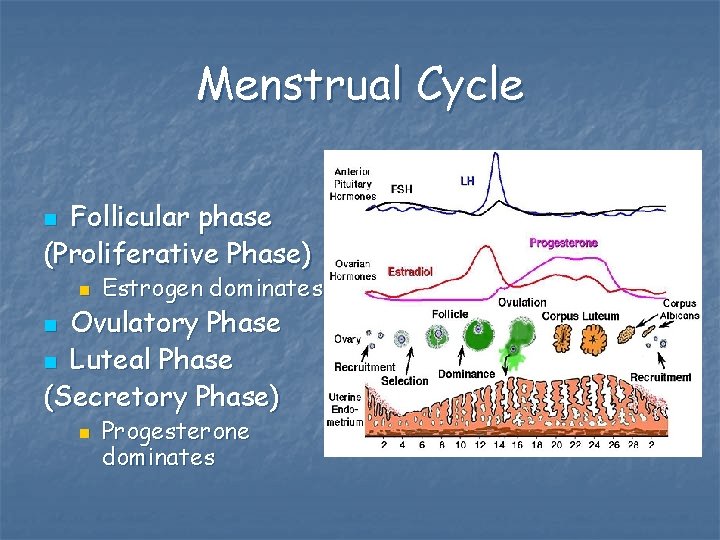
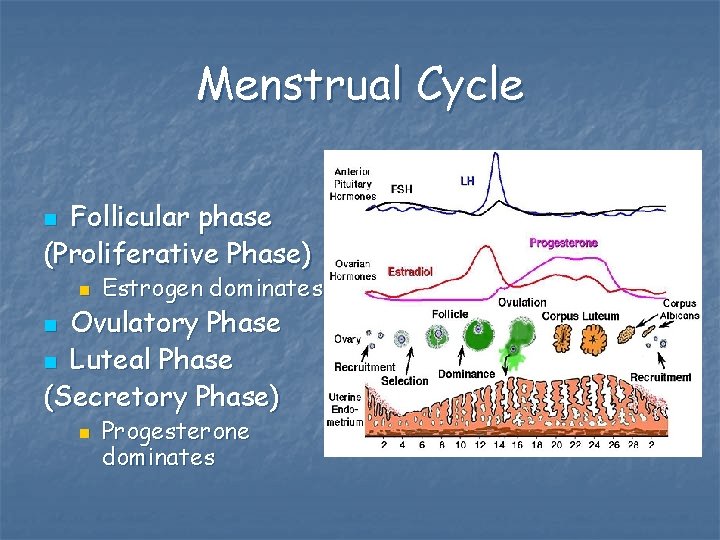
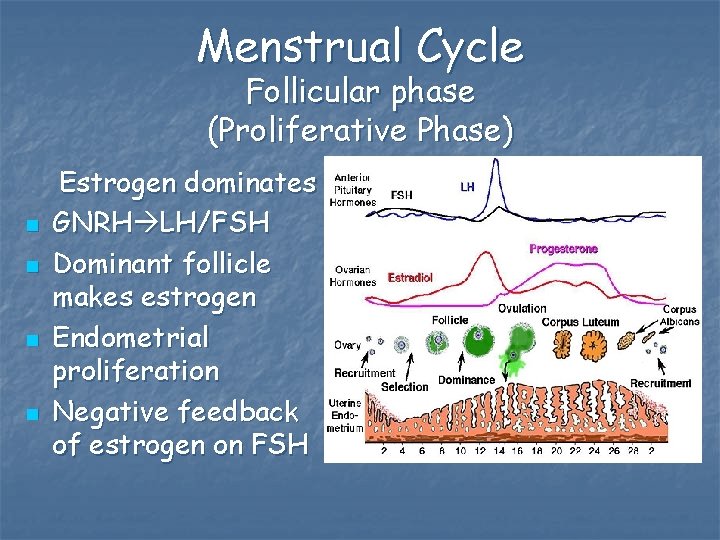
Menstrual Cycle Follicular phase (Proliferative Phase) n n Estrogen dominates Ovulatory Phase n Luteal Phase (Secretory Phase) n n Progesterone dominates
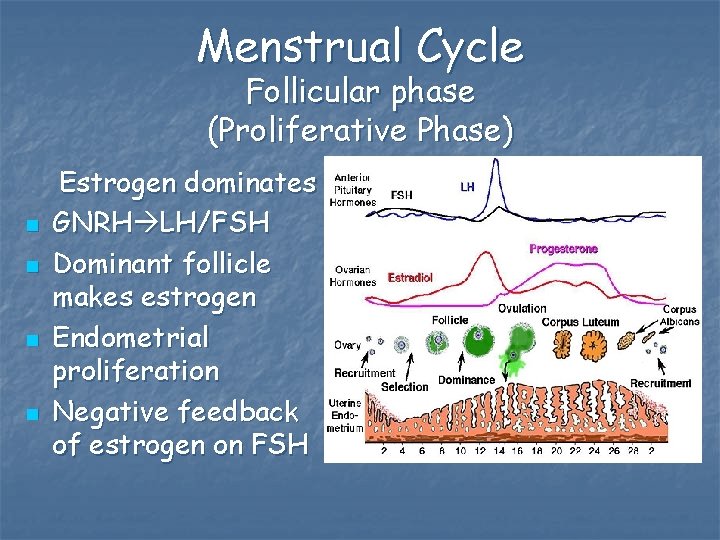
Menstrual Cycle Follicular phase (Proliferative Phase) n n Estrogen dominates GNRH LH/FSH Dominant follicle makes estrogen Endometrial proliferation Negative feedback of estrogen on FSH

Menstrual Cycle Ovulatory Phase n Estrogen LH surge ovulation
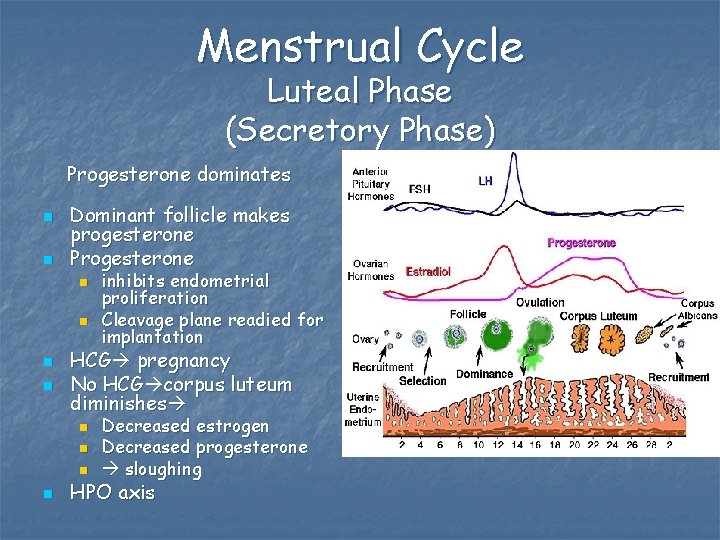
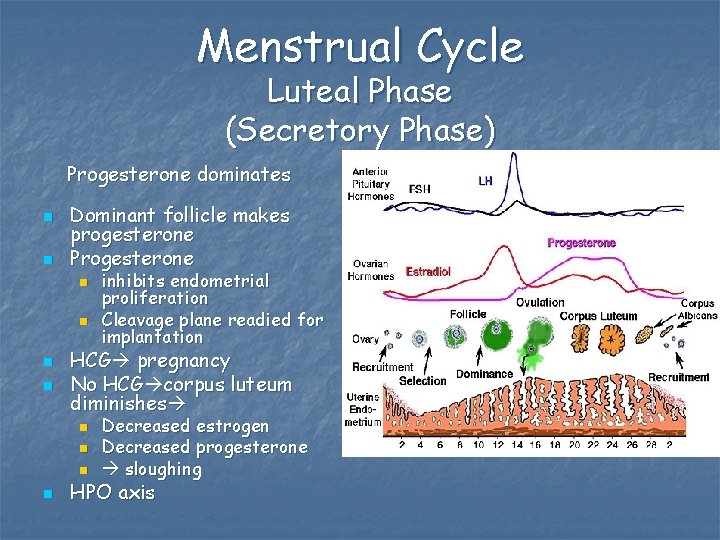
Menstrual Cycle Luteal Phase (Secretory Phase) Progesterone dominates n n Dominant follicle makes progesterone Progesterone n n HCG pregnancy No HCG corpus luteum diminishes n n inhibits endometrial proliferation Cleavage plane readied for implantation Decreased estrogen Decreased progesterone sloughing HPO axis
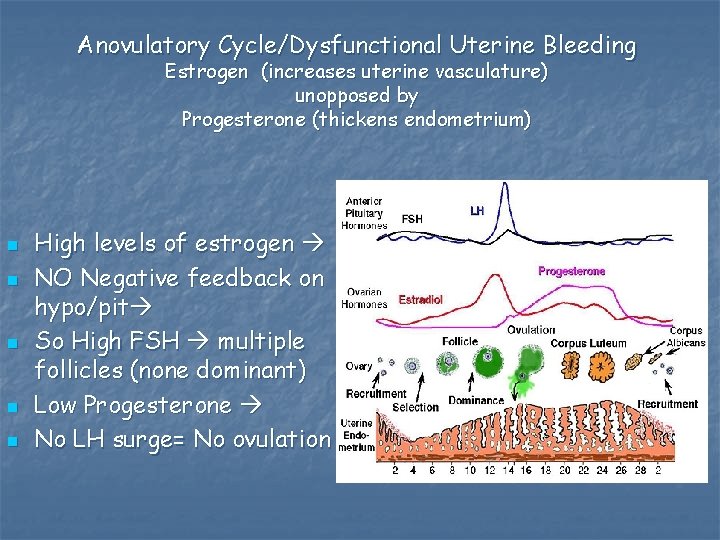
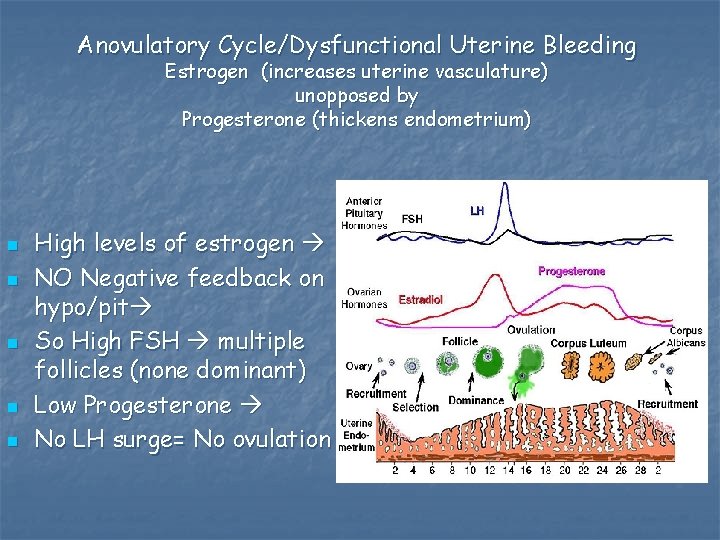
Anovulatory Cycle/Dysfunctional Uterine Bleeding Estrogen (increases uterine vasculature) unopposed by Progesterone (thickens endometrium) n n n High levels of estrogen NO Negative feedback on hypo/pit So High FSH multiple follicles (none dominant) Low Progesterone No LH surge= No ovulation
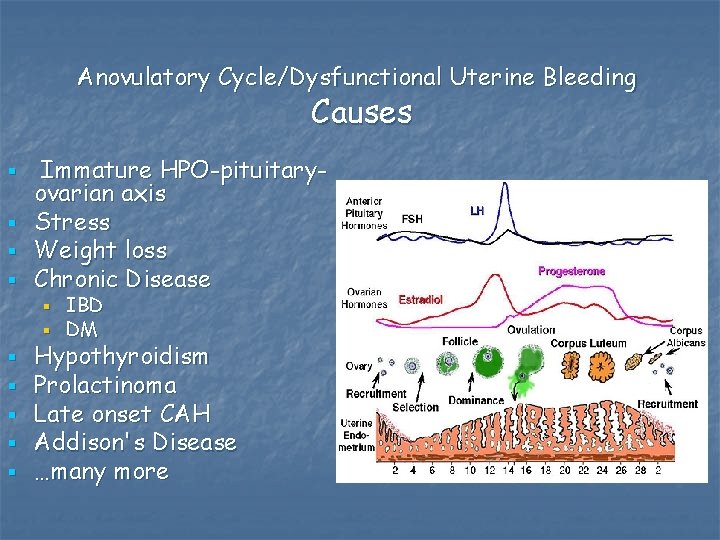
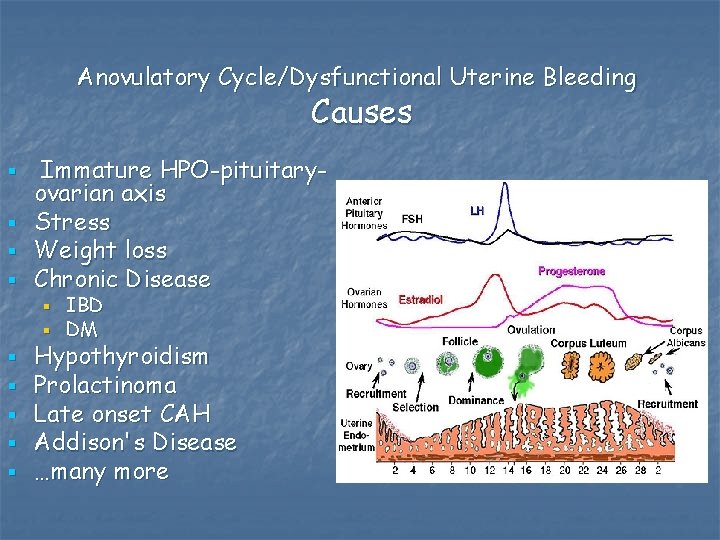
Anovulatory Cycle/Dysfunctional Uterine Bleeding Causes § § Immature HPO-pituitaryovarian axis Stress Weight loss Chronic Disease § § § § IBD DM Hypothyroidism Prolactinoma Late onset CAH Addison's Disease …many more
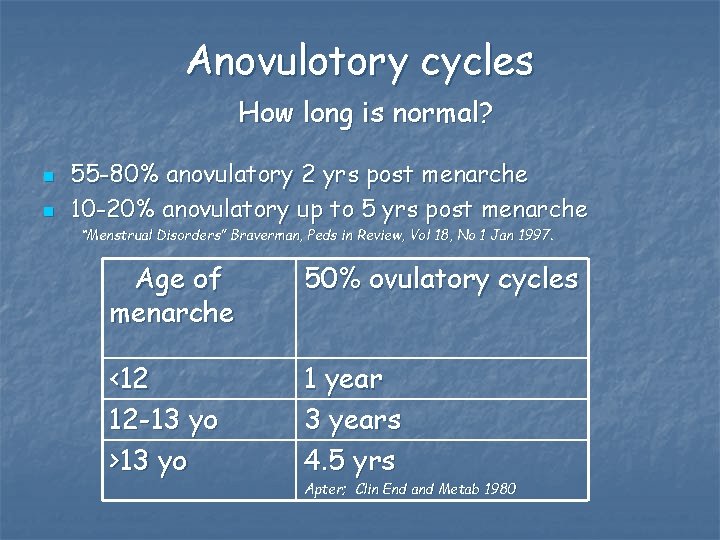
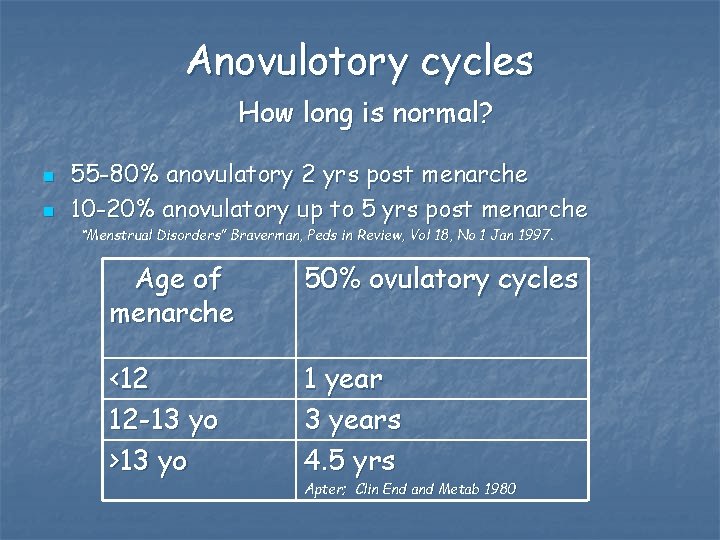
Anovulotory cycles How long is normal? n n 55 -80% anovulatory 2 yrs post menarche 10 -20% anovulatory up to 5 yrs post menarche “Menstrual Disorders” Braverman, Peds in Review, Vol 18, No 1 Jan 1997. Age of menarche 50% ovulatory cycles <12 12 -13 yo >13 yo 1 year 3 years 4. 5 yrs Apter; Clin End and Metab 1980
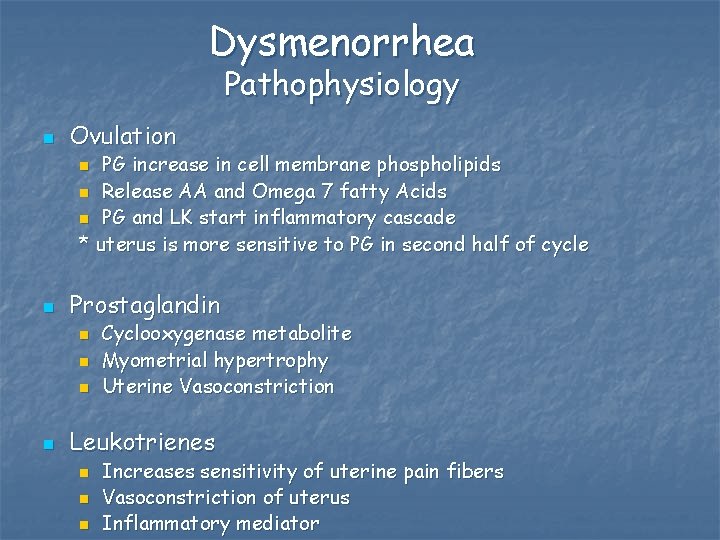
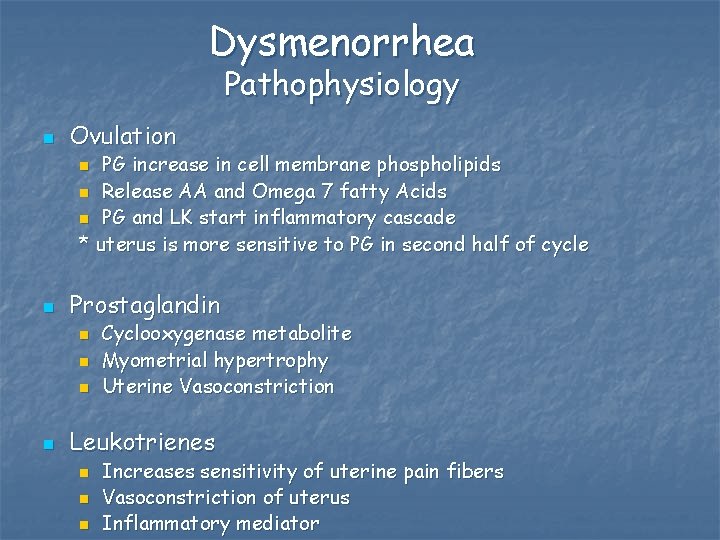
Dysmenorrhea Pathophysiology n Ovulation PG increase in cell membrane phospholipids n Release AA and Omega 7 fatty Acids n PG and LK start inflammatory cascade * uterus is more sensitive to PG in second half of cycle n n Prostaglandin n n Cyclooxygenase metabolite Myometrial hypertrophy Uterine Vasoconstriction Leukotrienes n n n Increases sensitivity of uterine pain fibers Vasoconstriction of uterus Inflammatory mediator

Dysmenorrhea § § § End of Luteal Phase Decreased progesterone Phospholipids A 2 Converts Phospholipids to Arachadonic Acid Via Cyclic peroxidase/PG synthetase PGE 2 and PGF 2 a
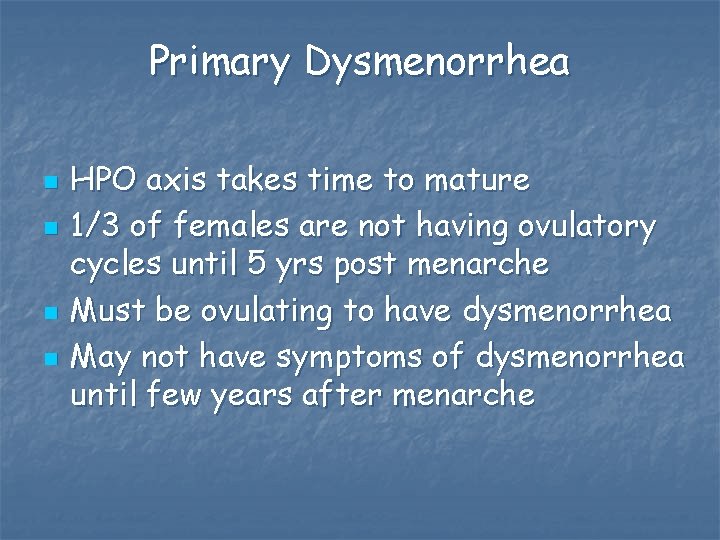
Primary Dysmenorrhea n n HPO axis takes time to mature 1/3 of females are not having ovulatory cycles until 5 yrs post menarche Must be ovulating to have dysmenorrhea May not have symptoms of dysmenorrhea until few years after menarche

2 o dysmenorrhea n n n Fibroid Endometriosis Adenomyosis

Risk factors n n n Early menarche Heavy flow Nulliparity n n Age <20 yo Family history Depression/anxiety +/- tobacco

Dysmenorrhea n Not risk factors n n n Ht Wt BMI History of abortion, uterine instrumentation, or surgery Protective? n Tobacco may decrease estrogen levels and result in anovulatory cycles (inconsistent)
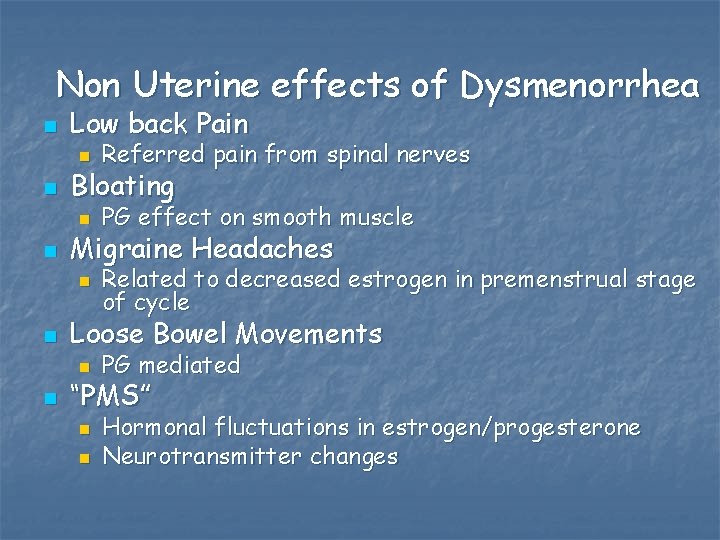
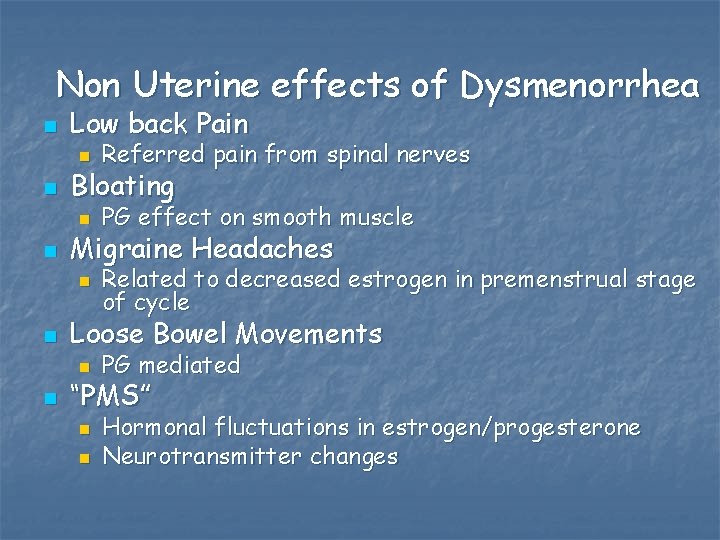
Non Uterine effects of Dysmenorrhea n n Low back Pain n Referred pain from spinal nerves n PG effect on smooth muscle n Related to decreased estrogen in premenstrual stage of cycle Bloating Migraine Headaches Loose Bowel Movements n n PG mediated “PMS” n n Hormonal fluctuations in estrogen/progesterone Neurotransmitter changes

PMDD premenstrual dysmorphic disorder n DSM-IV Depressive Disorder NOS 311. 0 Symptoms last week of luteal phase n Significantly impair life/work n Absence of symptoms at least 1 wk post menses n n Incidence 3 -5% menstruating women Serafem (flouxetine) Eli Lilly 10 -20 mg/d days 14 -28
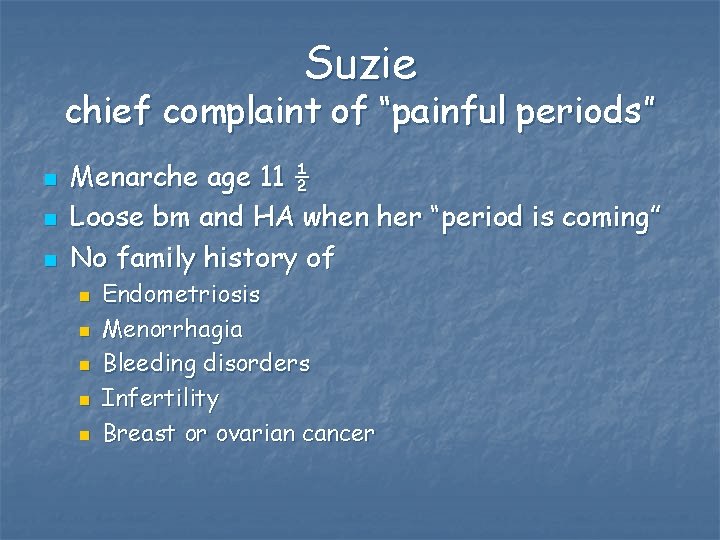
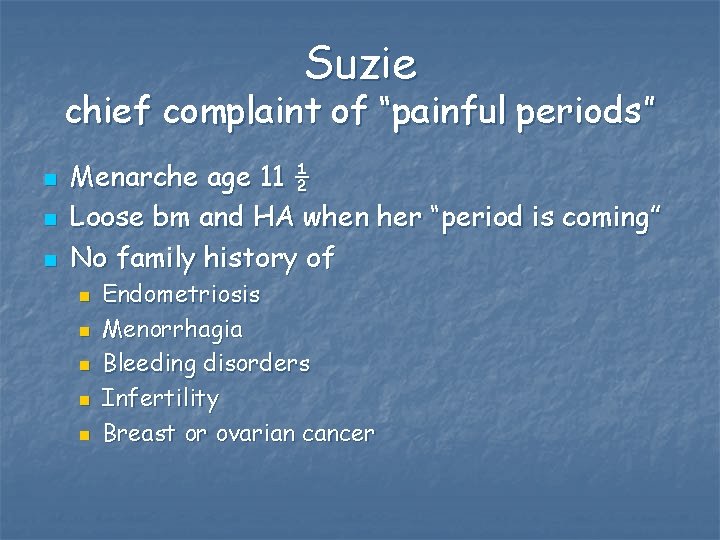
Suzie chief complaint of “painful periods” n n n Menarche age 11 ½ Loose bm and HA when her “period is coming” No family history of n n n Endometriosis Menorrhagia Bleeding disorders Infertility Breast or ovarian cancer

Differential Diagnosis n n n PID Pelvic adhesions Ovarian cysts IBD IBS Interstitial cystitis
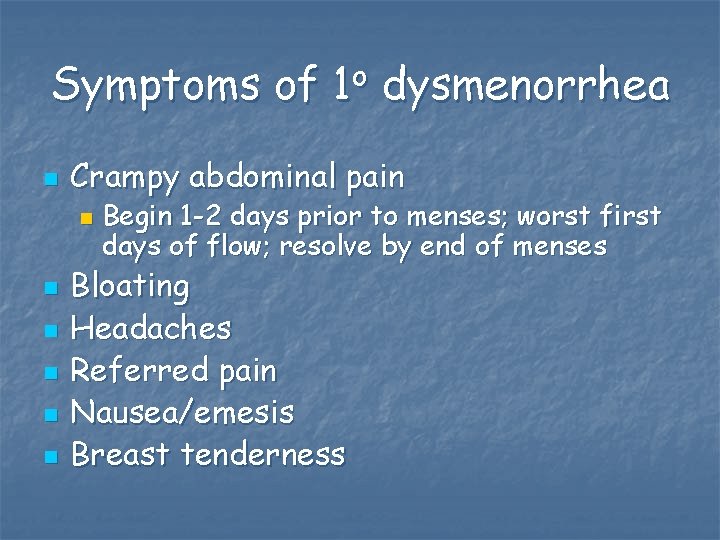
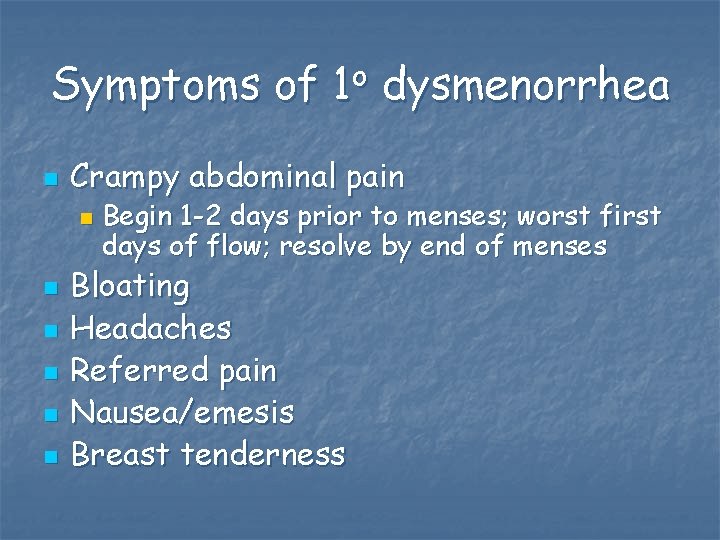
Symptoms of 1 o dysmenorrhea n Crampy abdominal pain n n n Begin 1 -2 days prior to menses; worst first days of flow; resolve by end of menses Bloating Headaches Referred pain Nausea/emesis Breast tenderness
Symptoms of 2 o dysmenorrhea n Begin several days to 2 w before flow n Persist throughout flow

Exam n n Mild mid abdominal pain No rebound No CMT or AT Mass n Consider uterine outlet obstruction n n severe pain early after menarche Other tumors
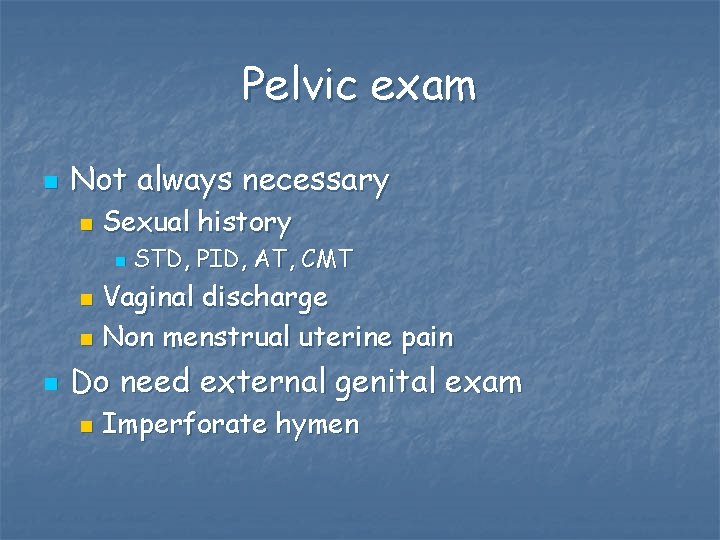
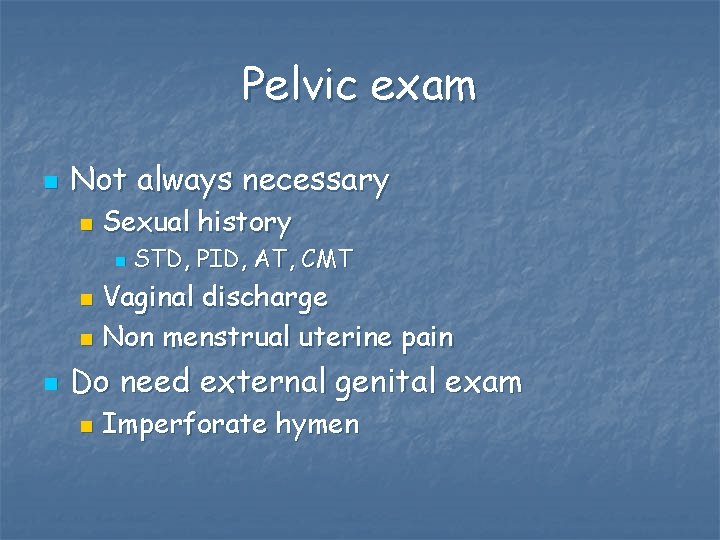
Pelvic exam n Not always necessary n Sexual history n STD, PID, AT, CMT Vaginal discharge n Non menstrual uterine pain n n Do need external genital exam n Imperforate hymen
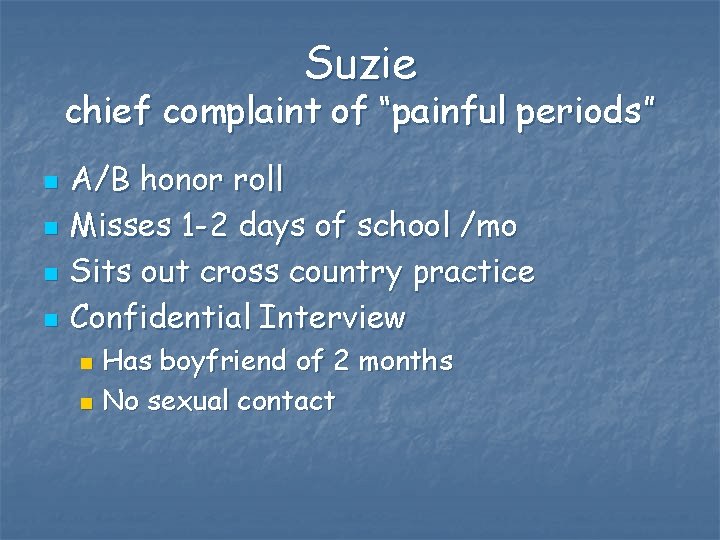
Suzie chief complaint of “painful periods” n n A/B honor roll Misses 1 -2 days of school /mo Sits out cross country practice Confidential Interview Has boyfriend of 2 months n No sexual contact n
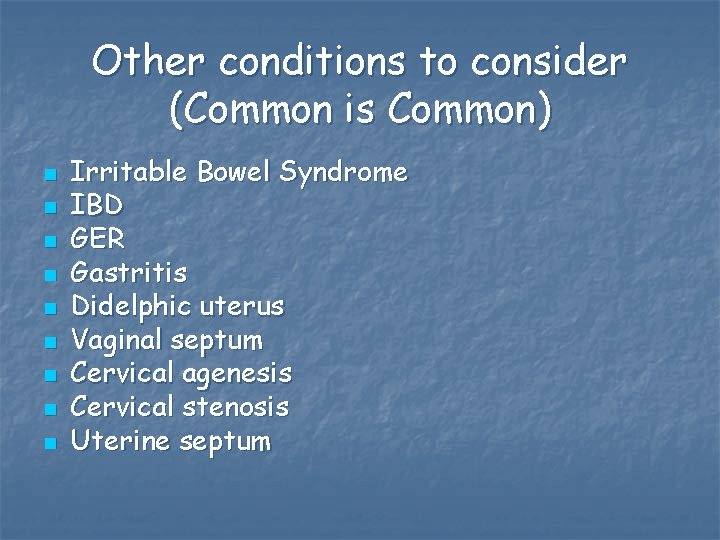
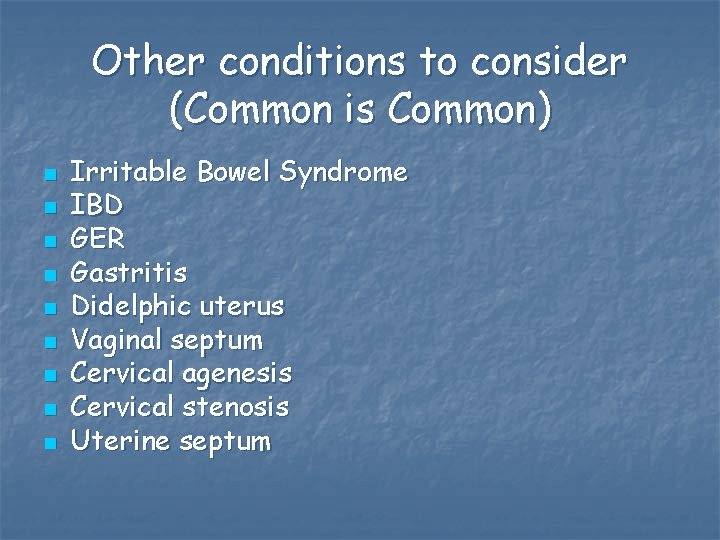
Other conditions to consider (Common is Common) n n n n n Irritable Bowel Syndrome IBD GER Gastritis Didelphic uterus Vaginal septum Cervical agenesis Cervical stenosis Uterine septum

Evaluation n Get a history first! n n Symptom Calendar Hemoglobin n Menorrhagia n n Bleeding disorder- von Willebrands Disease IBD Consider Hemoccult Consider bimanual exam or ultrasound if initial tx does not alleviate symptoms

Suzie chief complaint of “painful periods” n n Hemoglobin 11. 5 Medications Tylenol n Midol n n n periods about every month soaks through pads about every 3 hours

Treatment n n NSAIDS Other OTC n n OCP n n Used by 30 -70% of adolescents Extended cycling Other hormonal therapies Non medical treatments CAM
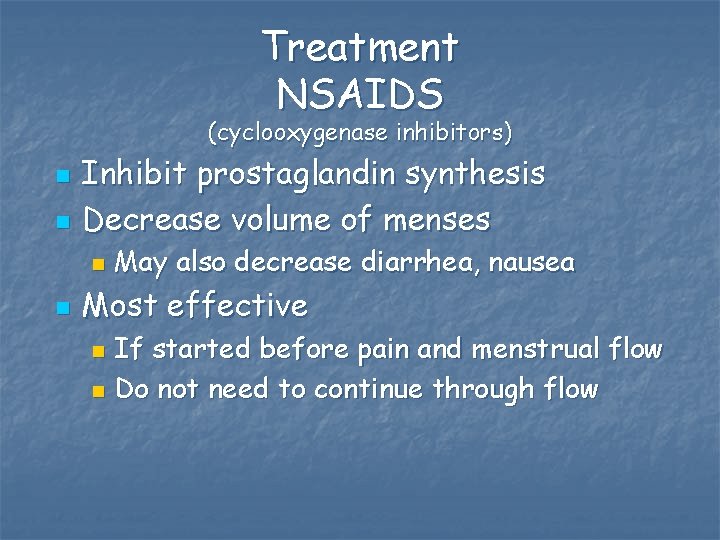
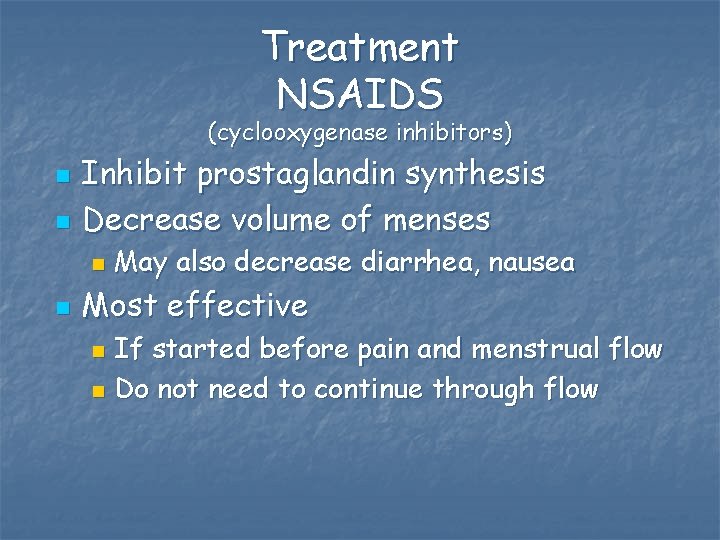
Treatment NSAIDS (cyclooxygenase inhibitors) n n Inhibit prostaglandin synthesis Decrease volume of menses n n May also decrease diarrhea, nausea Most effective If started before pain and menstrual flow n Do not need to continue through flow n
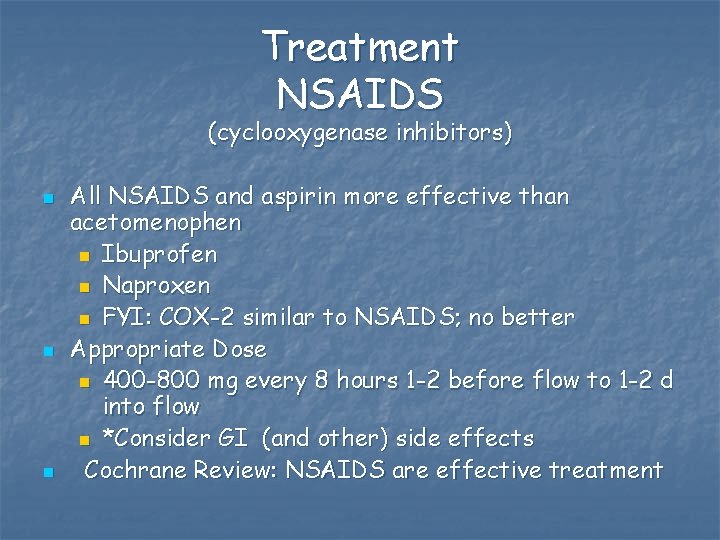
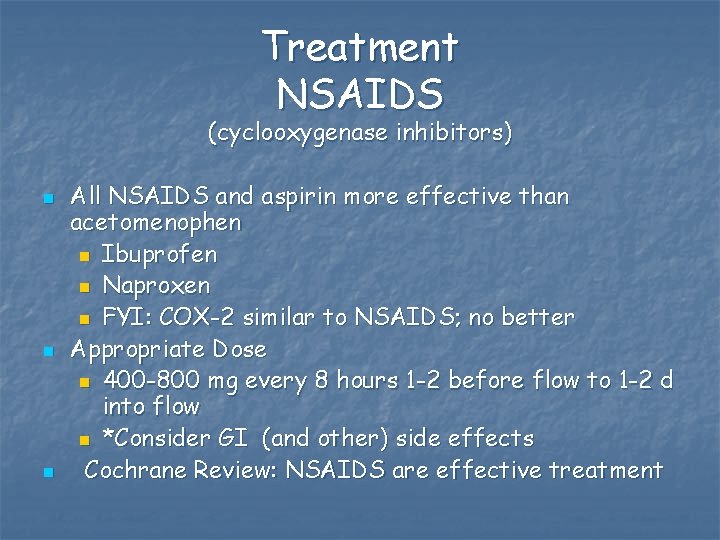
Treatment NSAIDS (cyclooxygenase inhibitors) n n n All NSAIDS and aspirin more effective than acetomenophen n Ibuprofen n Naproxen n FYI: COX-2 similar to NSAIDS; no better Appropriate Dose n 400 -800 mg every 8 hours 1 -2 before flow to 1 -2 d into flow n *Consider GI (and other) side effects Cochrane Review: NSAIDS are effective treatment
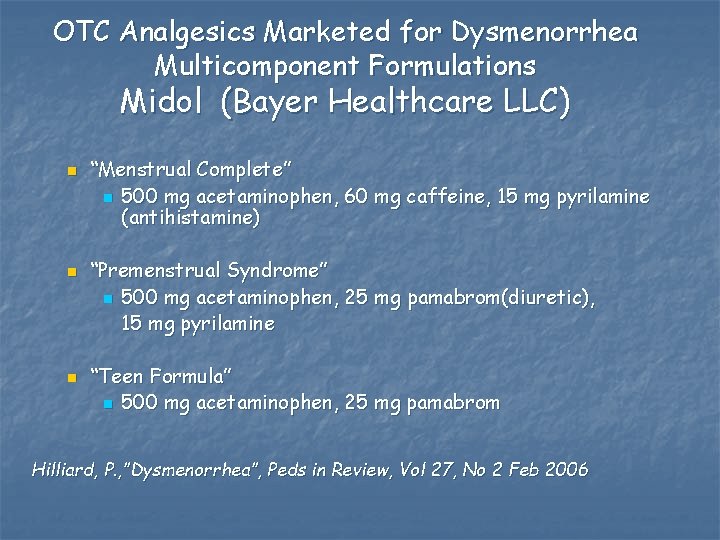
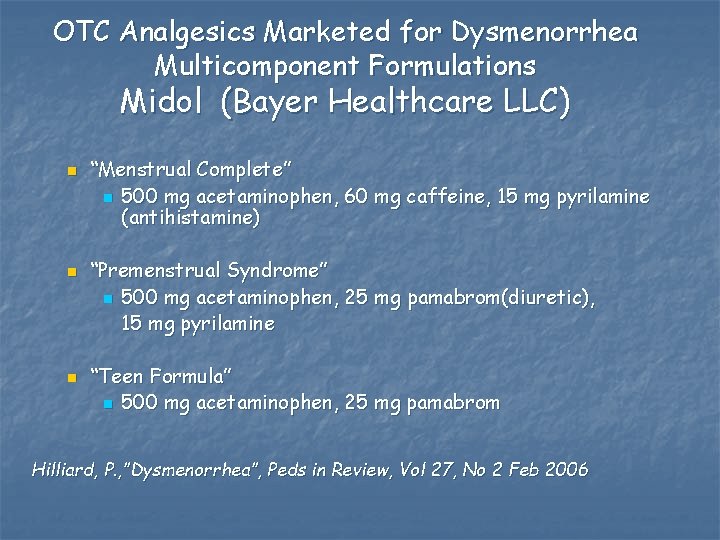
OTC Analgesics Marketed for Dysmenorrhea Multicomponent Formulations Midol (Bayer Healthcare LLC) n n n “Menstrual Complete” n 500 mg acetaminophen, 60 mg caffeine, 15 mg pyrilamine (antihistamine) “Premenstrual Syndrome” n 500 mg acetaminophen, 25 mg pamabrom(diuretic), 15 mg pyrilamine “Teen Formula” n 500 mg acetaminophen, 25 mg pamabrom Hilliard, P. , ”Dysmenorrhea”, Peds in Review, Vol 27, No 2 Feb 2006

OTC Analgesics Marketed for Dysmenorrhea Multicomponent Formulations Midol (Bayer Healthcare LLC) n n “Cramps and body aches” n ibuprofen 200 mg “Maximum strength extended relief” n naproxen sodium 200 mg (approved by FDA) Hilliard, P. , ”Dysmenorrhea”, Peds in Review, Vol 27, No 2 Feb 2006
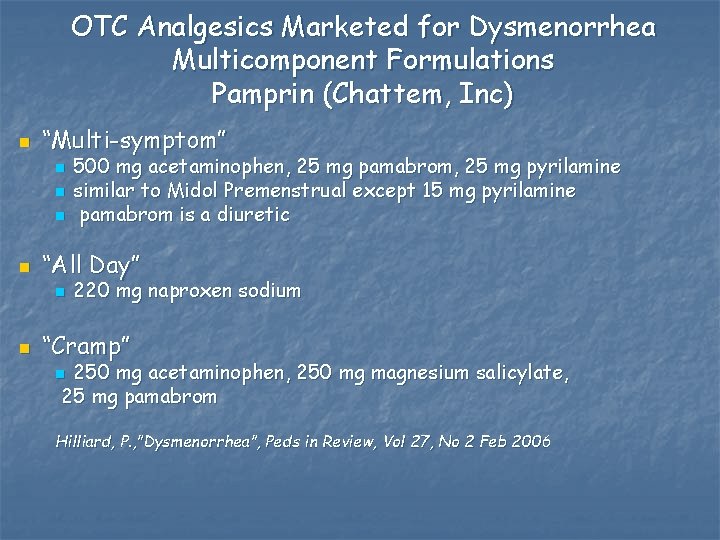
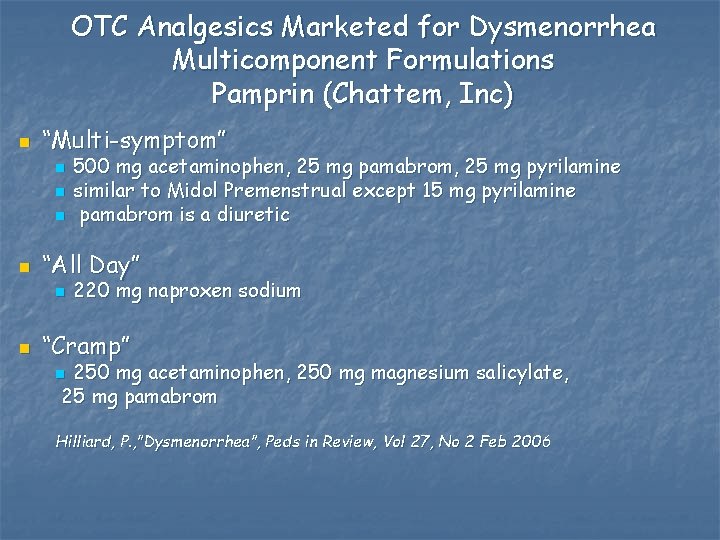
OTC Analgesics Marketed for Dysmenorrhea Multicomponent Formulations Pamprin (Chattem, Inc) n “Multi-symptom” n n “All Day” n n 500 mg acetaminophen, 25 mg pamabrom, 25 mg pyrilamine similar to Midol Premenstrual except 15 mg pyrilamine pamabrom is a diuretic 220 mg naproxen sodium “Cramp” 250 mg acetaminophen, 250 mg magnesium salicylate, 25 mg pamabrom n Hilliard, P. , ”Dysmenorrhea”, Peds in Review, Vol 27, No 2 Feb 2006

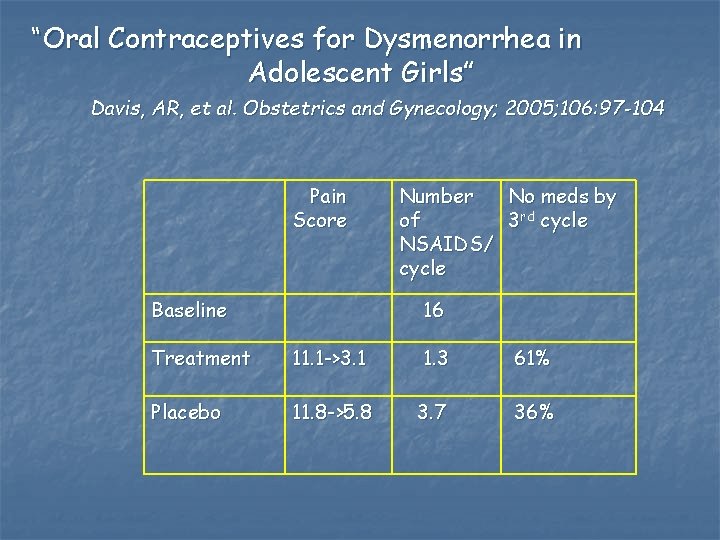
“Oral Contraceptives for Dysmenorrhea in Adolescent Girls” Davis, AR, et al. Obstetrics and Gynecology; 2005; 106: 97 -104 n n n n= 76; <19 yo Screen for depression, stress Randomized to low dose (20 mcg estrogen) OCP or placebo Could take other OTC meds Moos Menstrual Distress Scale Phone f/u monthly x 2; then exit interview month 3 Baseline : severe pain 58%; 55% nausea, 39% missed activites

Moos Menstrual Distress Scale n n n Designed 1968 6 point Likert Scale Cycle n n menstrual, premenstrual, intermenstrual Symptoms n n n Pain Concentration Behavior changes Autonomic reactions Water retention Control
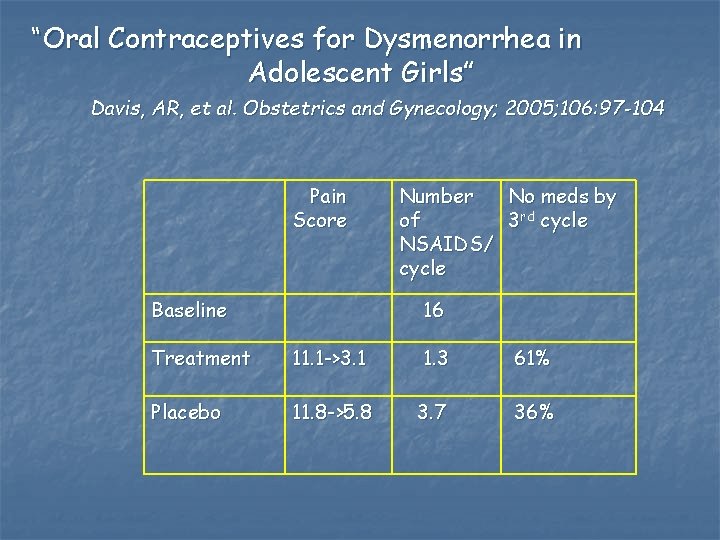
“Oral Contraceptives for Dysmenorrhea in Adolescent Girls” Davis, AR, et al. Obstetrics and Gynecology; 2005; 106: 97 -104 Pain Score Baseline Number No meds by of 3 rd cycle NSAIDS/ cycle 16 Treatment 11. 1 ->3. 1 1. 3 61% Placebo 11. 8 ->5. 8 3. 7 36%

Treatment Oral Contraceptive Pills n Inhibit ovulation Decreased progesterone less PG n Less menstrual flow n n Cochrane rates as effective n n No evidence low dose vs 30 or 35 mcg estrogen pills Pelvic exam not always required

Treatment Oral Contraceptive Pills n n Use Monophasic estrogen containing pills Lower estrogens n n spotting less efficacious as contraception if n n n >155 pounds Miss pills 30 mcg 35 mcg Some studies used 50+ mcg estrogen/pill n Nausea!
Treatment n n n Depo-Provera Extended cycling OCP Mirena

Treatment n Extended Cycling Oral Contraceptives n n n Reduced flow Less frequent flow Seasonale Can use any monophasic OCP Other benefits
Treatment Other Hormonal n Contraceptive Patch: Ortho Evra n n Less effective than oral OCP for dysmenorrhea Intravaginal OCP
Treatment Leukotriene Recepetor Antagonists Will Singulair decrease PG and relieve symptoms? * n n= 22 adolescents completed n n n mean age 16 4 + 1 year post menarche RDB crossover n n n 13 got 10 mg Singulair days 21 to end of cycle x 2 cycles; then 2 month placebo other group had reverse order 3 drop-outs: noncompliance, other disease dx “The Use of the Leukotriene Antagonist Montelukast (Singulair)in the Management of Dysmenorrhea in Adolescents” Harel, et al. J of Pediatric and Adolescent Gynecology, 2004; 17: 183 -186. * Funded by Merck
Treatment Leukotriene Receptor Antagonists Will Singulair decrease PG and relieve symptoms? * Cox Menstrual Scale n No difference in pain scores with use of Singulair for dysmenorrhea n “The Use of the Leukotriene Antagonist Montelukast (Singulair)in the Management of Dysmenorrhea in Adolescents” Harel, et al. J of Pediatric and Adolescent Gynecology, 2004; 17: 183 -186. * Funded by Merck
Treatment Depo-Provera n n n Most patients amenorrheic by 9 months May have irregular bleeding 3 -6 months Bone effects n May recover

Treatment Suppression of Menses n n n Danazol (Danocrine) Leuprolide acetate (Lupron) Expensive Significant Side effect Generally not for Primary dysmenorrhea
Treatment Other Modalities n Supplements RCT showed pain reduction compared to placebo Thiamine 100 mg daily n Fish Oil n Vitamin E n n Herbal remedies Insufficient data

Treatment Levonorgestrel Intrauterine System: Mirena n n n Duration: 5 years Vaginal Bleeding n 60% amenorrhea n 12% rare n 28% scant, regular Not appropriate if risk of STD (This is a schematic and is not anatomically proportional. ) schematic from www. contraceptiononline. org

Treatment Other Modalities n n Exercise Heat Relaxation/Yoga Acupuncture and Acupressure n n TENS (Transcutaneous electric nerve stimulation) n n Some randomized controlled studies show reduction in pain Insufficient evidence Spinal manipulation n No evidence to support

Suzie Primary Dysmenorrhea n NSAIDS n n Menstrual Symptom Diary n n 400 -600 mg ibuprofen 1 d prior to menses If continues symptoms, consider OCP Multivitamin with iron

Dysmenorrhea When to Refer to Gynecologist n Persists on appropriate dose medications n n n NSAIDS OCP STD ? (remember Urine PCR) n Severe symptoms with 1 o relative with endometriosis n Exam concerning for endometriosis n n n Posterior uterus pain Cul de sac pain Significant disability
Selected Bibliography n n n Braverman, PK, “Menstrual Disorders” Pediatrics in Review, Vol 18, No 1, Jan 1997, 17 -26. Rimsza, M. “Dysfunctional Uterine Bleeding” Pediatrics in Review, Vol 23, No 7, July 2002, 227 -233. French, L. “Dysmenorrhea” American Family Physician 2005; V 71: No 2 285 -291 Hilliard, P. , ”Dysmenorrhea”, Pediatrics in Review, Vol 27, No 2 Feb 2006 Davis, AR “Primary Dysmenorrhea in Adolescent Girls and treatment with Oral Contraceptives” J Pediatrics and Adolescent Gynecology, 2001 Vol 14 3 -8. n n n Apter “Anovulatroy Cycles” Clinical Endo and Metabolism 1980 “Oral Contraceptives for Dysmenorrhea in Adolescent Girls” Davis, AR, et al. Obstetrics and Gynecology; 2005; 106: 97 -104 “The Use of the Leukotriene Antagonist Montelukast (Singulair) in the Management of Dysmenorrhea in Adolescents” Harel, et al. J of Pediatric and Adolescent Gynecology, 2004; 17: 183 -186. Moos, R. The Development of a Menstrual Distress Questionnaire Psychosomatic Medicine 30: 853 -867 (1968) DSM IV –R American Psychiatric Association Pediatric and Adolescent Gynecology, Emans, Laufer, Goldstein, ed. Lippincot-Raven, 2004
 Preeti matkins
Preeti matkins Hysterorrhexis adalah
Hysterorrhexis adalah Dysmenorrhea
Dysmenorrhea Dysmenorrhea
Dysmenorrhea Introducing neeta anil said
Introducing neeta anil said Preeti ramaraj
Preeti ramaraj Preeti sandwich franchise
Preeti sandwich franchise Cmc otc
Cmc otc Sakai cmc
Sakai cmc Reduced social cues
Reduced social cues Rossman chance guess the correlation
Rossman chance guess the correlation Cmc computer
Cmc computer Cmc in physical pharmacy
Cmc in physical pharmacy Cmc hartmann
Cmc hartmann Oxs cmc
Oxs cmc Cmc vs mcm
Cmc vs mcm Comment rédiger un cahier de laboratoire
Comment rédiger un cahier de laboratoire Cmc vellore handbook of emergency medicine
Cmc vellore handbook of emergency medicine Cmc psychiatric hospital
Cmc psychiatric hospital Rubic cmc
Rubic cmc Maksud konjuktivitis
Maksud konjuktivitis Castidade cmc
Castidade cmc Cmc uncertainty
Cmc uncertainty 2010 cmc california mechanical code
2010 cmc california mechanical code What is cst method in physical pharmaceutics
What is cst method in physical pharmaceutics Kellogg cmc job board
Kellogg cmc job board Cmc instrumentation and controls
Cmc instrumentation and controls Pyterygium
Pyterygium Channel sharing and borrowing in cmc
Channel sharing and borrowing in cmc Firefighter interview tips
Firefighter interview tips Horizontal
Horizontal Liz welch mississippi
Liz welch mississippi Nys dept of homeland security
Nys dept of homeland security Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Vaginal dept
Vaginal dept City of worcester inspectional services
City of worcester inspectional services Dept nmr spectroscopy
Dept nmr spectroscopy Albany county dss
Albany county dss Dept of education
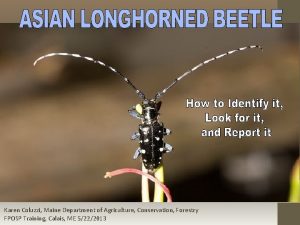
Dept of education Maine dept of agriculture
Maine dept of agriculture Gome dept
Gome dept Dept. name of organization
Dept. name of organization Nebraska dept of agriculture
Nebraska dept of agriculture La dept of revenue
La dept of revenue Dept a
Dept a Gome dept
Gome dept Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) Bromocicloesano
Bromocicloesano Dept of education
Dept of education Hoe dept
Hoe dept Employment first ohio
Employment first ohio Florida department of agriculture and consumer services
Florida department of agriculture and consumer services Iit
Iit La revenue dept
La revenue dept Central islip fire dept
Central islip fire dept