DR KAREN PONT EK CME EVENT FERNIE 5






- Slides: 51
DR KAREN PONT EK CME EVENT FERNIE 5 OCTOBER 2019 UPDATE ON PSORIATIC ARTHRITIS Footer for Disclaimer Text
I HAVE NO DISCLOSURES Footer for Disclaimer Text
LEARNING OBJECTIVES 1. Diverse clinical spectrum of psoriatic arthritis (Ps. A) 2. Implications of Ps. A 3. New treatment approaches to Ps. A
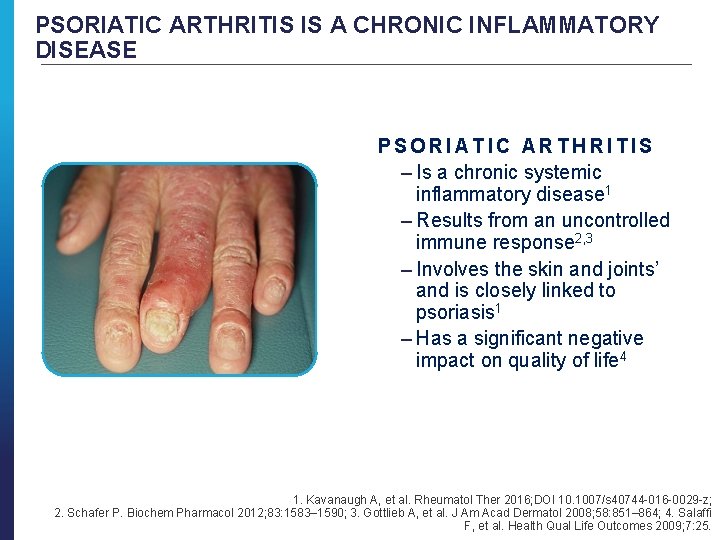
PSORIATIC ARTHRITIS IS A CHRONIC INFLAMMATORY DISEASE PSORIATIC ARTHRITIS – Is a chronic systemic inflammatory disease 1 – Results from an uncontrolled immune response 2, 3 – Involves the skin and joints’ and is closely linked to psoriasis 1 – Has a significant negative impact on quality of life 4 1. Kavanaugh A, et al. Rheumatol Ther 2016; DOI 10. 1007/s 40744 -016 -0029 -z; 2. Schafer P. Biochem Pharmacol 2012; 83: 1583– 1590; 3. Gottlieb A, et al. J Am Acad Dermatol 2008; 58: 851– 864; 4. Salaffi F, et al. Health Qual Life Outcomes 2009; 7: 25.
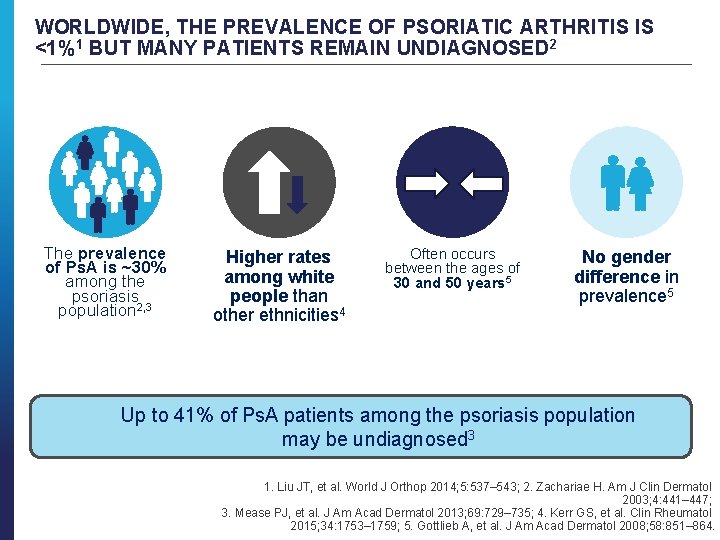
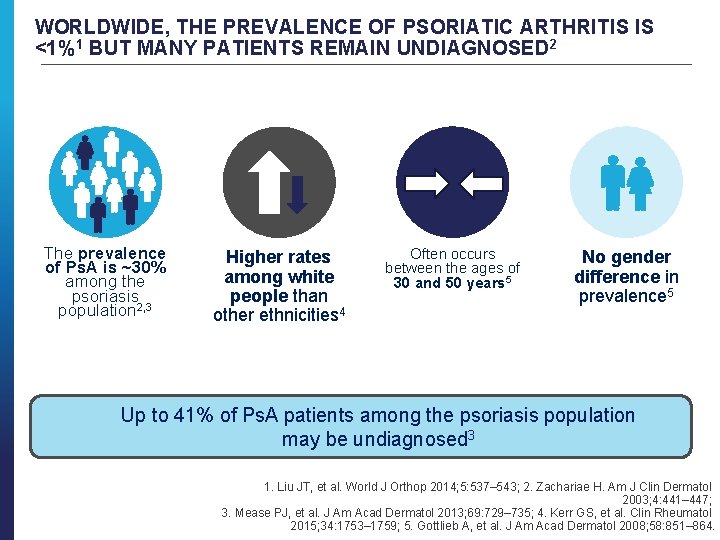
WORLDWIDE, THE PREVALENCE OF PSORIATIC ARTHRITIS IS <1%1 BUT MANY PATIENTS REMAIN UNDIAGNOSED 2 The prevalence of Ps. A is ~30% among the psoriasis population 2, 3 Higher rates among white people than other ethnicities 4 Often occurs between the ages of 30 and 50 years 5 No gender difference in prevalence 5 Up to 41% of Ps. A patients among the psoriasis population may be undiagnosed 3 1. Liu JT, et al. World J Orthop 2014; 5: 537– 543; 2. Zachariae H. Am J Clin Dermatol 2003; 4: 441– 447; 3. Mease PJ, et al. J Am Acad Dermatol 2013; 69: 729– 735; 4. Kerr GS, et al. Clin Rheumatol 2015; 34: 1753– 1759; 5. Gottlieb A, et al. J Am Acad Dermatol 2008; 58: 851– 864.
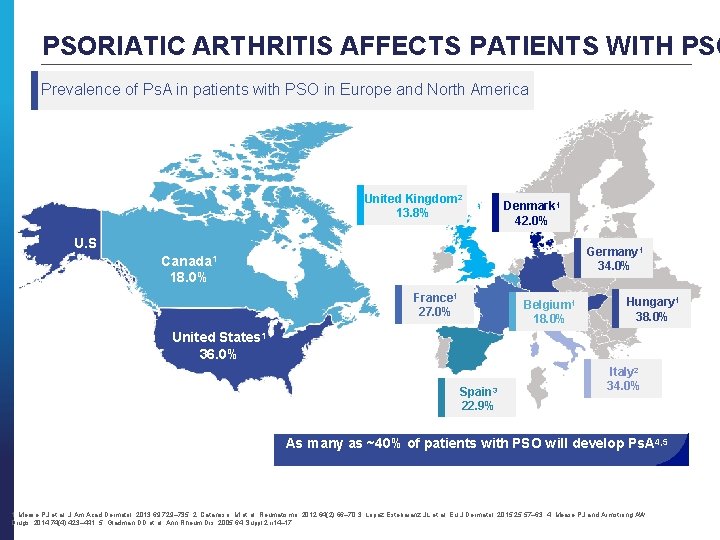
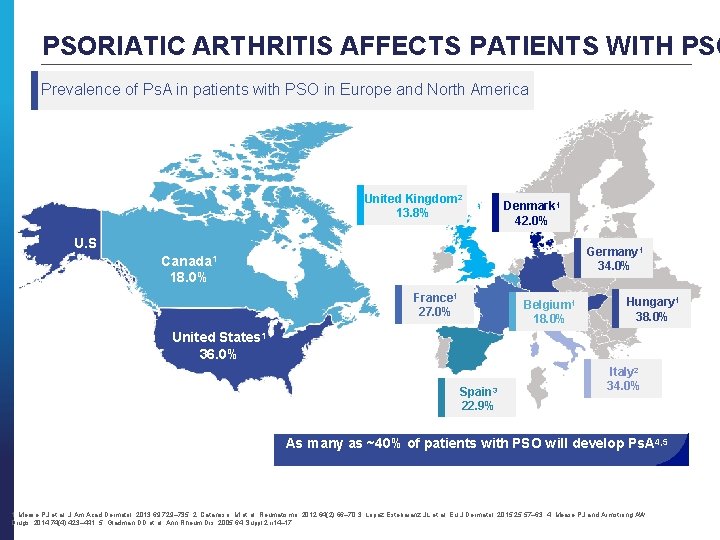
PSORIATIC ARTHRITIS AFFECTS PATIENTS WITH PSO Prevalence of Ps. A in patients with PSO in Europe and North America United Kingdom 2 13. 8% Denmark 1 42. 0% U. S Germany 1 34. 0% Canada 1 18. 0% France 1 27. 0% Belgium 1 18. 0% Hungary 1 38. 0% United States 1 36. 0% Spain 3 22. 9% Italy 2 34. 0% As many as ~40% of patients with PSO will develop Ps. A 4, 5 1. Mease PJ et al. J Am Acad Dermatol. 2013; 69: 729– 735. 2. Catanoso M et al. Reumatismo. 2012; 64(2): 66– 70. 3. Lopez Estebaranz JL et al. Eu J Dermatol. 2015; 25: 57– 63. 4. Mease PJ and Armstrong AW. Drugs. 2014; 74(4): 423– 441. 5. Gladman DD et al. Ann Rheum Dis. 2005; 64 Suppl 2: ii 14– 17.
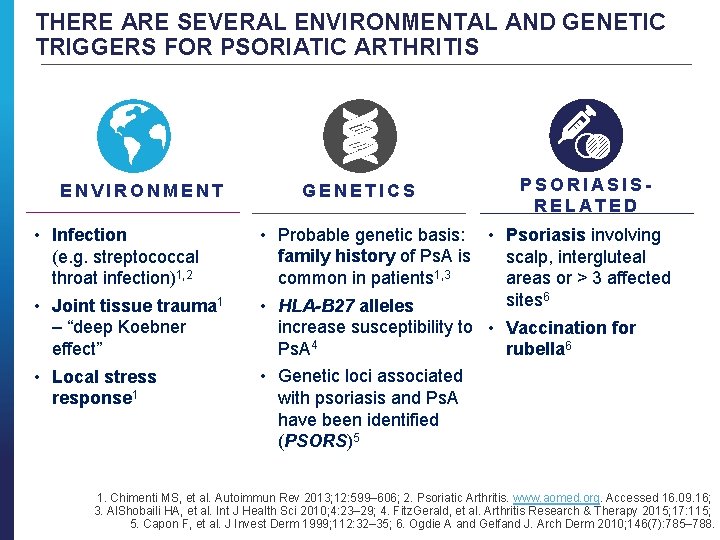
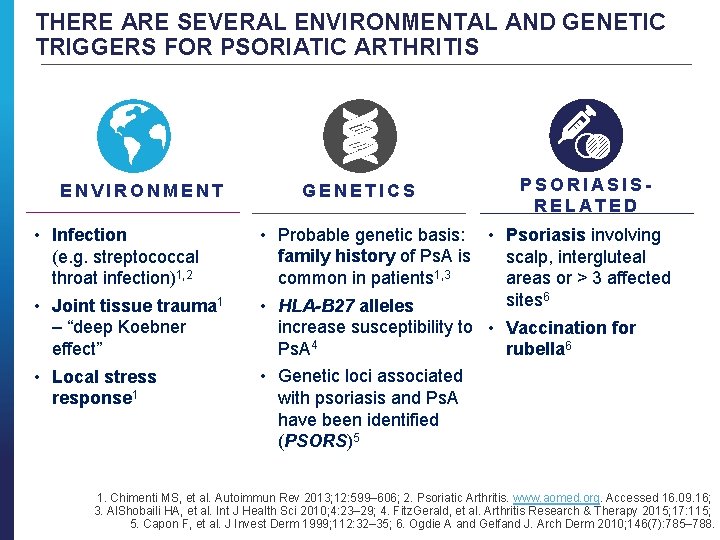
THERE ARE SEVERAL ENVIRONMENTAL AND GENETIC TRIGGERS FOR PSORIATIC ARTHRITIS ENVIRONMENT • Infection (e. g. streptococcal throat infection)1, 2 • Joint tissue trauma 1 – “deep Koebner effect” • Local stress response 1 GENETICS PSORIASISRELATED • Probable genetic basis: • Psoriasis involving family history of Ps. A is scalp, intergluteal common in patients 1, 3 areas or > 3 affected sites 6 • HLA-B 27 alleles increase susceptibility to • Vaccination for Ps. A 4 rubella 6 • Genetic loci associated with psoriasis and Ps. A have been identified (PSORS)5 1. Chimenti MS, et al. Autoimmun Rev 2013; 12: 599– 606; 2. Psoriatic Arthritis. www. aomed. org. Accessed 16. 09. 16; 3. Al. Shobaili HA, et al. Int J Health Sci 2010; 4: 23– 29; 4. Fitz. Gerald, et al. Arthritis Research & Therapy 2015; 17: 115; 5. Capon F, et al. J Invest Derm 1999; 112: 32– 35; 6. Ogdie A and Gelfand J. Arch Derm 2010; 146(7): 785– 788.
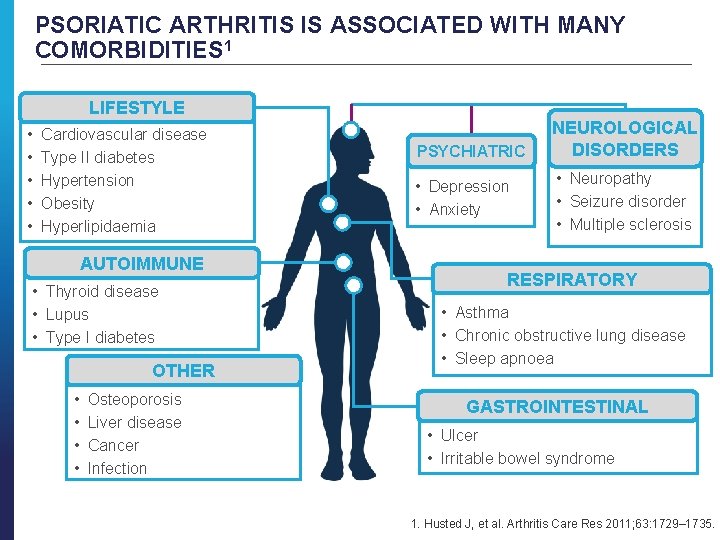
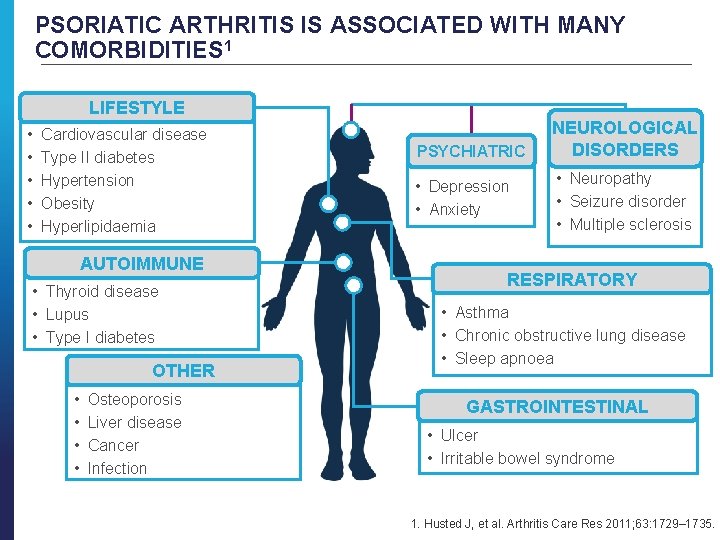
PSORIATIC ARTHRITIS IS ASSOCIATED WITH MANY COMORBIDITIES 1 LIFESTYLE • • • Cardiovascular disease Type II diabetes Hypertension Obesity Hyperlipidaemia AUTOIMMUNE • Thyroid disease • Lupus • Type I diabetes OTHER • • Osteoporosis Liver disease Cancer Infection PSYCHIATRIC • Depression • Anxiety NEUROLOGICAL DISORDERS • Neuropathy • Seizure disorder • Multiple sclerosis RESPIRATORY • Asthma • Chronic obstructive lung disease • Sleep apnoea GASTROINTESTINAL • Ulcer • Irritable bowel syndrome 1. Husted J, et al. Arthritis Care Res 2011; 63: 1729– 1735.
CLASSIFICATION, SYMPTOMS AND CLINICAL PRESENTATION
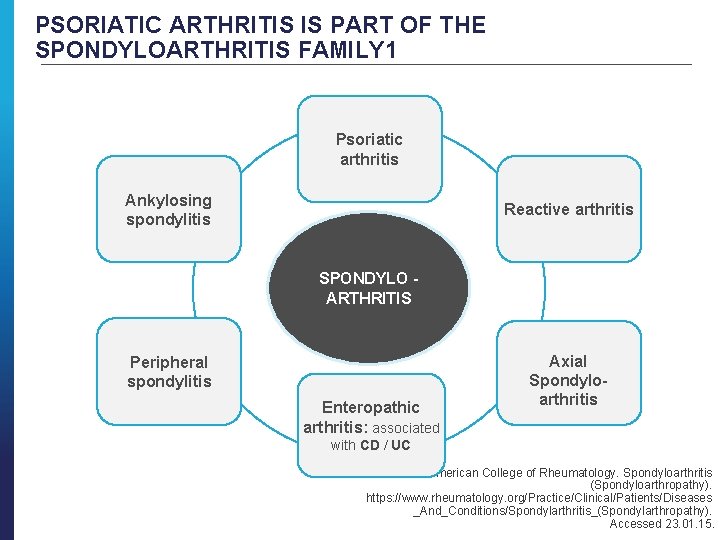
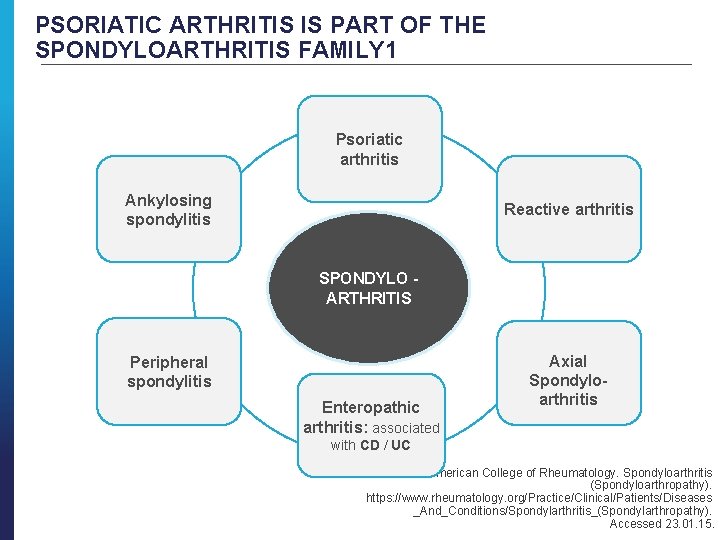
PSORIATIC ARTHRITIS IS PART OF THE SPONDYLOARTHRITIS FAMILY 1 Psoriatic arthritis Ankylosing spondylitis Reactive arthritis SPONDYLO ARTHRITIS Peripheral spondylitis Enteropathic arthritis: associated Axial Spondyloarthritis with CD / UC 1. American College of Rheumatology. Spondyloarthritis (Spondyloarthropathy). https: //www. rheumatology. org/Practice/Clinical/Patients/Diseases _And_Conditions/Spondylarthritis_(Spondylarthropathy). Accessed 23. 01. 15.
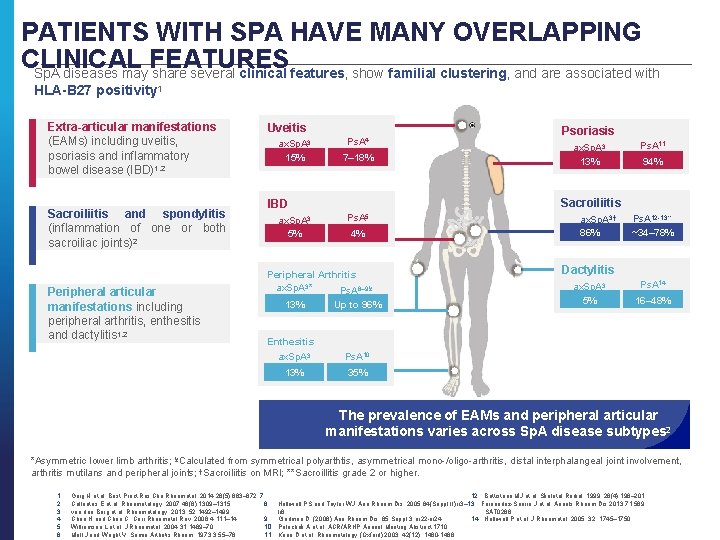
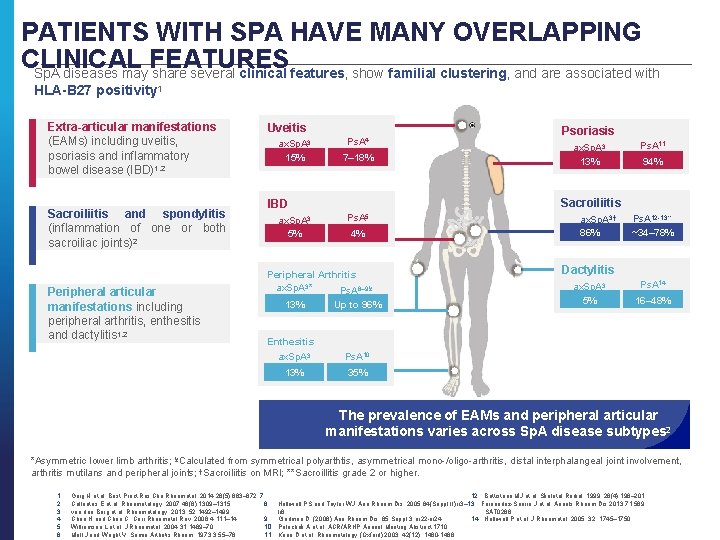
PATIENTS WITH SPA HAVE MANY OVERLAPPING CLINICAL FEATURES Sp. A diseases may share several clinical features, show familial clustering, and are associated with HLA-B 27 positivity 1 Extra-articular manifestations (EAMs) including uveitis, psoriasis and inflammatory bowel disease (IBD)1, 2 Sacroiliitis and spondylitis (inflammation of one or both sacroiliac joints)2 Peripheral articular manifestations including peripheral arthritis, enthesitis and dactylitis 1, 2 Uveitis ax. Sp. A 3 15% Ps. A 4 7– 18% Ps. A 5 4% Peripheral Arthritis ax. Sp. A 3* Ps. A 6– 9¥ 13% ax. Sp. A 3 13% Ps. A 11 94% Sacroiliitis IBD ax. Sp. A 3 5% Psoriasis Up to 96% ax. Sp. A 3† 86% Ps. A 12 -13** ~34– 78% Dactylitis ax. Sp. A 3 5% Ps. A 14 16– 48% Enthesitis ax. Sp. A 3 Ps. A 10 13% 35% The prevalence of EAMs and peripheral articular manifestations varies across Sp. A disease subtypes 2 *Asymmetric lower limb arthritis; ¥Calculated from symmetrical polyarthtis, asymmetrical mono-/oligo-arthritis, distal interphalangeal joint involvement, arthritis mutilans and peripheral joints; †Sacroiliitis on MRI; **Sacroillitis grade 2 or higher. 1. Garg N et al. Best Pract Res Clin Rheumatol. 2014; 28(5): 663– 672. 7. 12. Battistone MJ et al. Skeletal Radiol. 1999; 28(4): 196– 201. 2. Collantes E et al. Rheumatology. 2007; 46(8): 1309– 1315. 8. Helliwell PS and Taylor WJ. Ann Rheum Dis. 2005; 64(Suppl II): ii 3– 13. Fernandez-Sueiro J et al. Annals Rheum Dis 2013; 71: 569. 3. van den Berg et al. Rheumatology. 2013; 52: 1492– 1499. Ii 8. SAT 0288. 4. Chen H and Chou C. Curr Rheumatol Rev. 2008; 4: 111– 14. 9. Gladman D. (2006) Ann Rheum Dis. 65 Suppl 3, iii 22 -iii 24 14. Helliwell P et al. J Rheumatol. 2005; 32: 1745– 1750. 10. Polachek A et al. ACR/ARHP Annual Meeting Abstract 1710. 5. Williamson L et al. J Rheumatol. 2004; 31: 1469– 70. 11. Kane D et al. Rheumatology (Oxford) 2003; 42(12): 1460 -1468. 6. Moll J and Wright V. Semin Arthritis Rheum. 1973; 3: 55– 78.
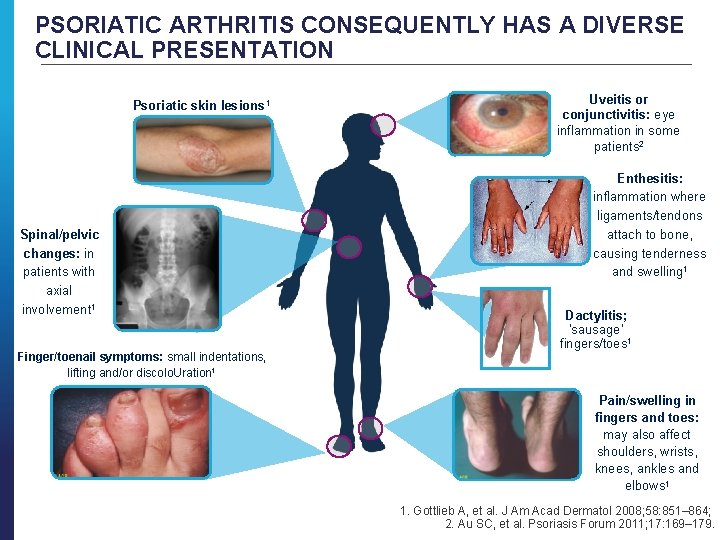
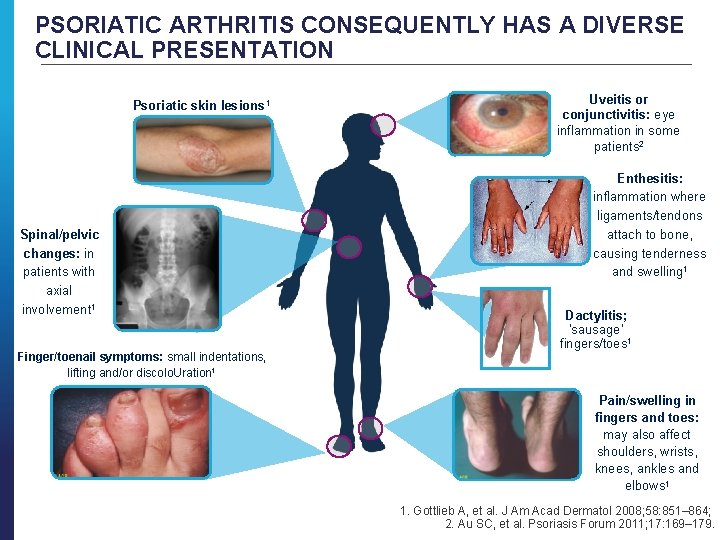
PSORIATIC ARTHRITIS CONSEQUENTLY HAS A DIVERSE CLINICAL PRESENTATION Psoriatic skin lesions 1 Spinal/pelvic changes: in patients with axial involvement 1 Finger/toenail symptoms: small indentations, lifting and/or discolo. Uration 1 Uveitis or conjunctivitis: eye inflammation in some patients 2 Enthesitis: inflammation where ligaments/tendons attach to bone, causing tenderness and swelling 1 Dactylitis; ‘sausage’ fingers/toes 1 Pain/swelling in fingers and toes: may also affect shoulders, wrists, knees, ankles and elbows 1 1. Gottlieb A, et al. J Am Acad Dermatol 2008; 58: 851– 864; 2. Au SC, et al. Psoriasis Forum 2011; 17: 169– 179.
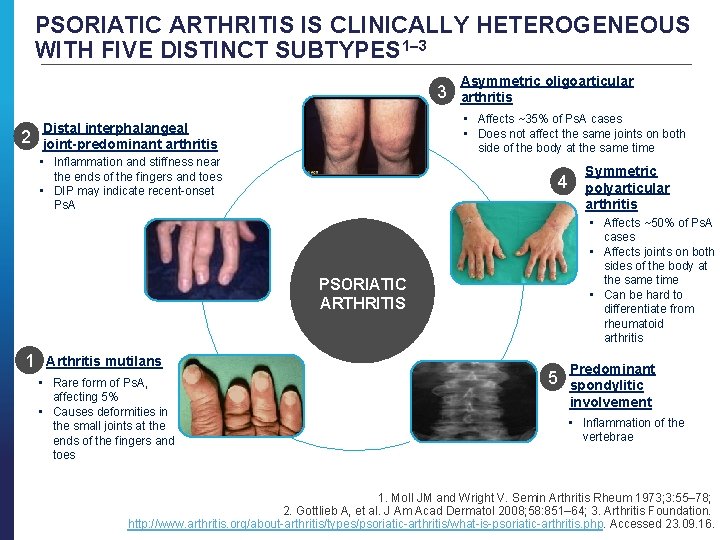
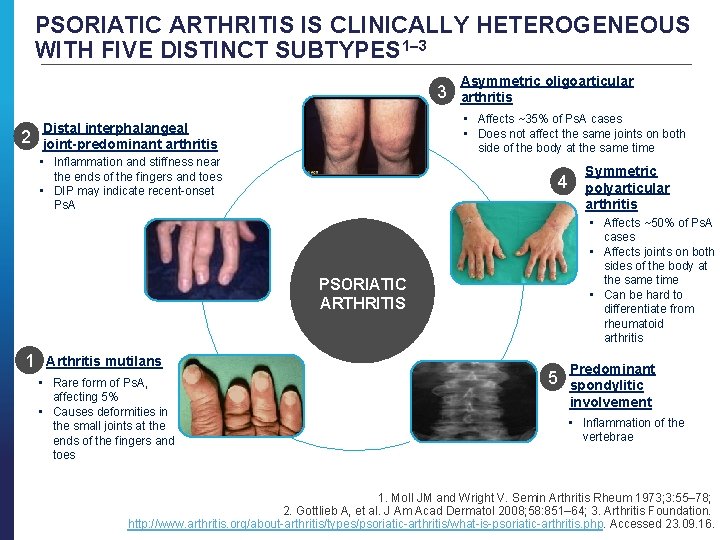
PSORIATIC ARTHRITIS IS CLINICALLY HETEROGENEOUS WITH FIVE DISTINCT SUBTYPES 1– 3 3 2 Distal interphalangeal joint-predominant arthritis • Inflammation and stiffness near the ends of the fingers and toes • DIP may indicate recent-onset Ps. A • Affects ~35% of Ps. A cases • Does not affect the same joints on both side of the body at the same time 4 PSORIATIC ARTHRITIS Arthritis mutilans • Rare form of Ps. A, affecting 5% • Causes deformities in the small joints at the ends of the fingers and toes Symmetric polyarticular arthritis • Affects ~50% of Ps. A cases • Affects joints on both sides of the body at the same time • Can be hard to differentiate from rheumatoid arthritis 1 Asymmetric oligoarticular arthritis 5 Predominant spondylitic involvement • Inflammation of the vertebrae 1. Moll JM and Wright V. Semin Arthritis Rheum 1973; 3: 55– 78; 2. Gottlieb A, et al. J Am Acad Dermatol 2008; 58: 851– 64; 3. Arthritis Foundation. http: //www. arthritis. org/about-arthritis/types/psoriatic-arthritis/what-is-psoriatic-arthritis. php. Accessed 23. 09. 16.
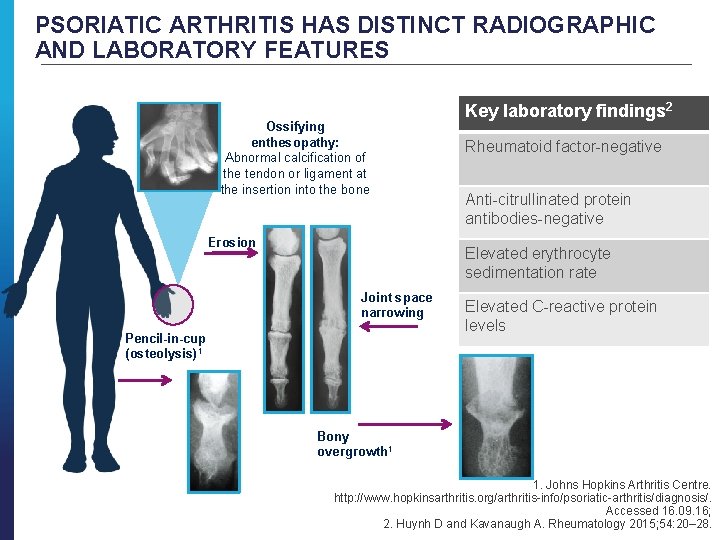
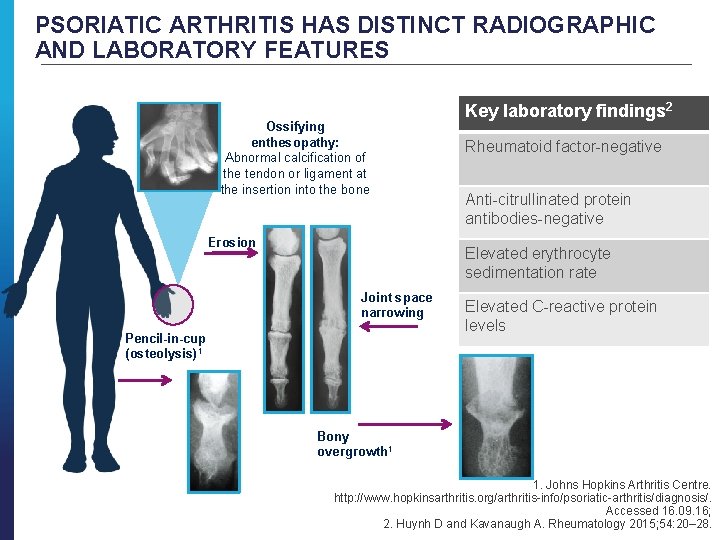
PSORIATIC ARTHRITIS HAS DISTINCT RADIOGRAPHIC AND LABORATORY FEATURES Ossifying enthesopathy: Abnormal calcification of the tendon or ligament at the insertion into the bone Erosion Key laboratory findings 2 Rheumatoid factor-negative Anti-citrullinated protein antibodies-negative Elevated erythrocyte sedimentation rate Joint space narrowing Pencil-in-cup (osteolysis) 1 Elevated C-reactive protein levels Bony overgrowth 1 1. Johns Hopkins Arthritis Centre. http: //www. hopkinsarthritis. org/arthritis-info/psoriatic-arthritis/diagnosis/. Accessed 16. 09. 16; 2. Huynh D and Kavanaugh A. Rheumatology 2015; 54: 20– 28.
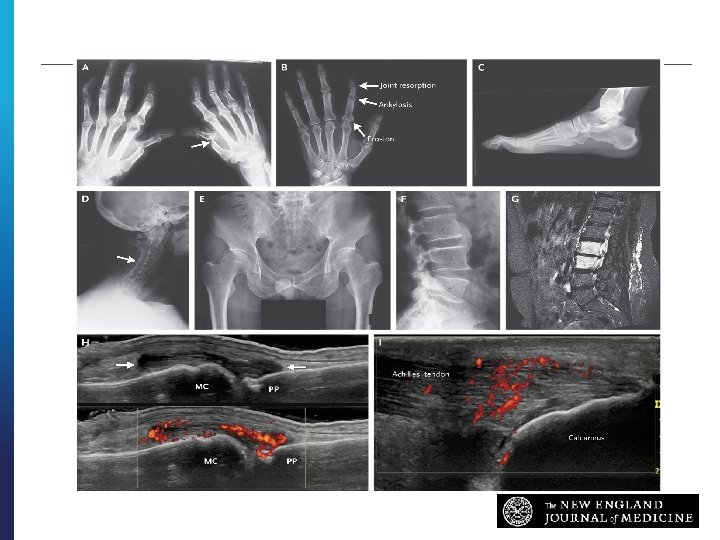
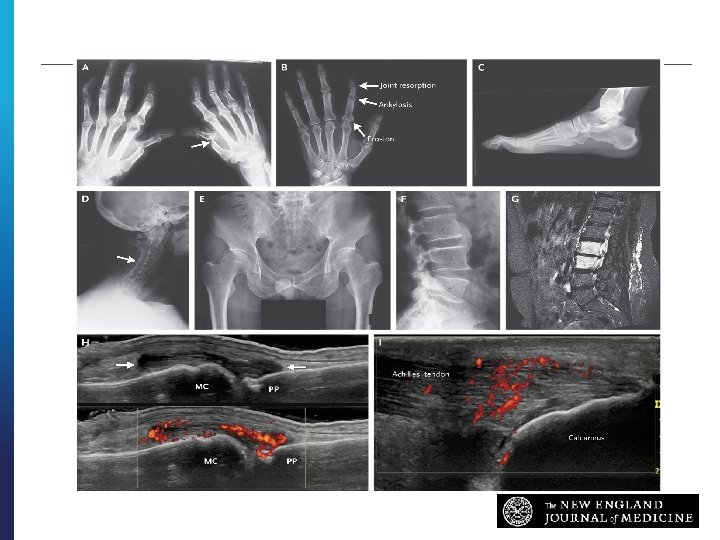
IMAGING Ritchlin CT et al. N Engl J Med ; 376: 957 -970

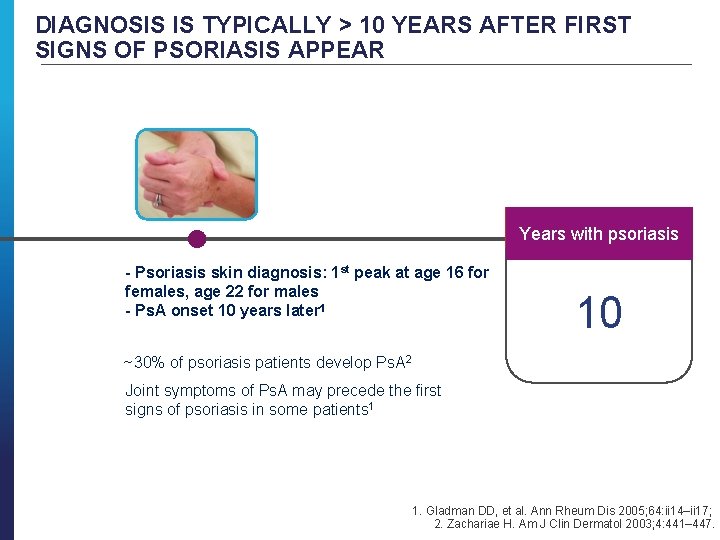
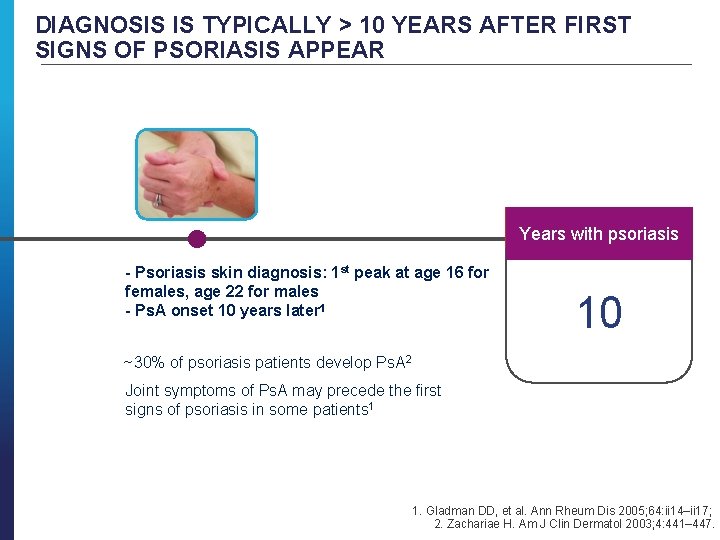
DIAGNOSIS IS TYPICALLY > 10 YEARS AFTER FIRST SIGNS OF PSORIASIS APPEAR Years with psoriasis Years with Ps. A - Psoriasis skin diagnosis: 1 st peak at age 16 for females, age 22 for males - Ps. A onset 10 years later 1 10 ~30% of psoriasis patients develop Ps. A 2 Joint symptoms of Ps. A may precede the first signs of psoriasis in some patients 1 1. Gladman DD, et al. Ann Rheum Dis 2005; 64: ii 14–ii 17; 2. Zachariae H. Am J Clin Dermatol 2003; 4: 441– 447.
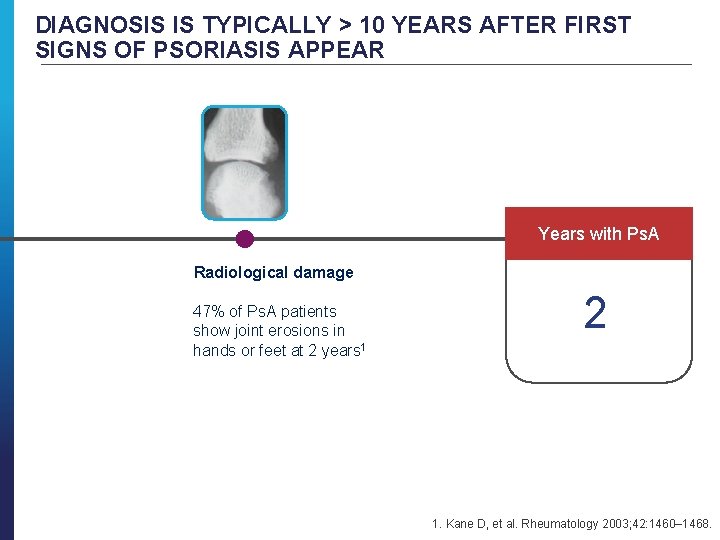
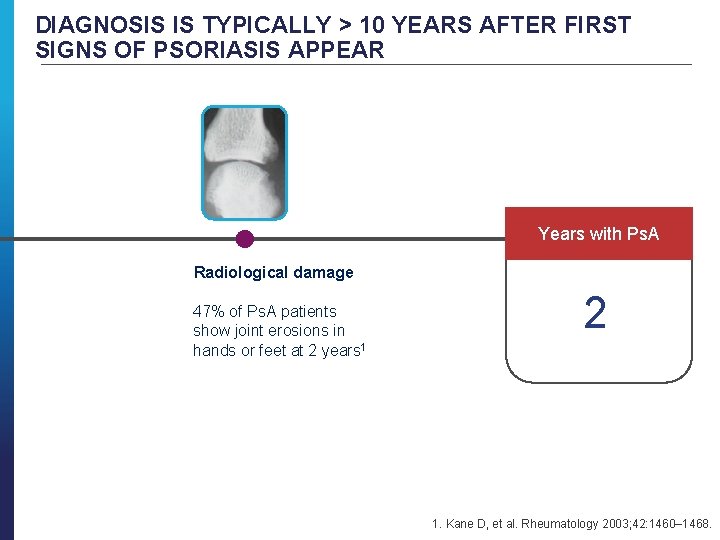
DIAGNOSIS IS TYPICALLY > 10 YEARS AFTER FIRST SIGNS OF PSORIASIS APPEAR Years with Ps. A Radiological damage 47% of Ps. A patients show joint erosions in hands or feet at 2 years 1 2 1. Kane D, et al. Rheumatology 2003; 42: 1460– 1468.
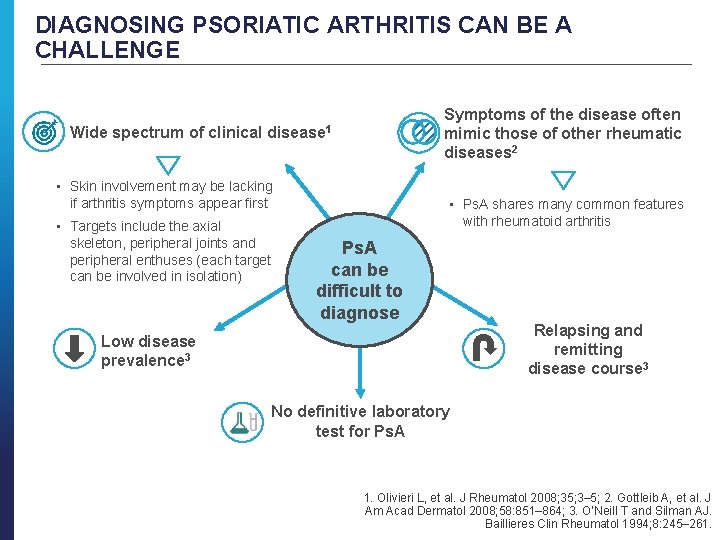
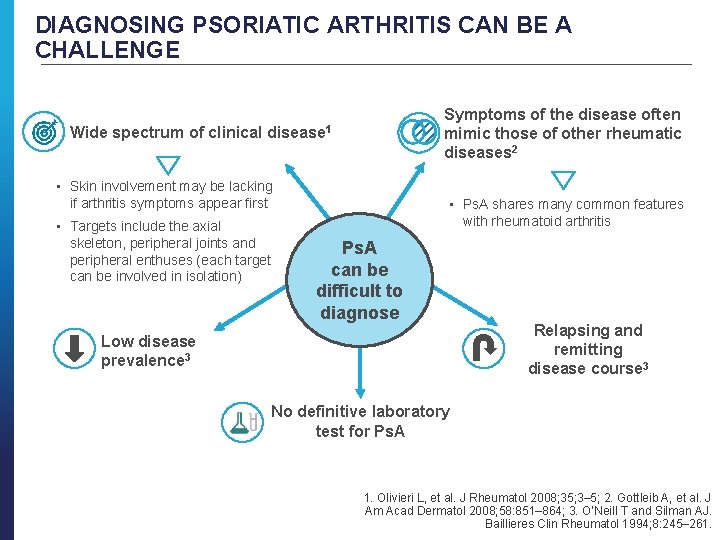
DIAGNOSING PSORIATIC ARTHRITIS CAN BE A CHALLENGE Symptoms of the disease often mimic those of other rheumatic diseases 2 Wide spectrum of clinical disease 1 • Skin involvement may be lacking if arthritis symptoms appear first • Targets include the axial skeleton, peripheral joints and peripheral enthuses (each target can be involved in isolation) • Ps. A shares many common features with rheumatoid arthritis Ps. A can be difficult to diagnose Low disease prevalence 3 Relapsing and remitting disease course 3 No definitive laboratory test for Ps. A 1. Olivieri L, et al. J Rheumatol 2008; 35; 3– 5; 2. Gottleib A, et al. J Am Acad Dermatol 2008; 58: 851– 864; 3. O’Neill T and Silman AJ. Baillieres Clin Rheumatol 1994; 8: 245– 261.
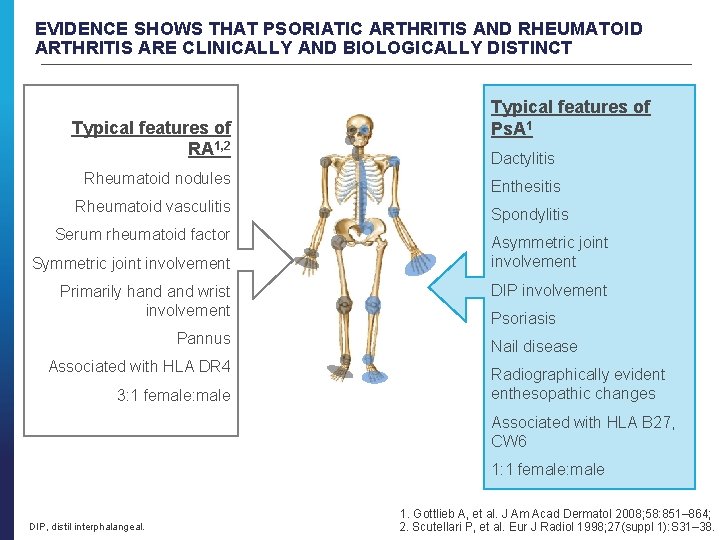
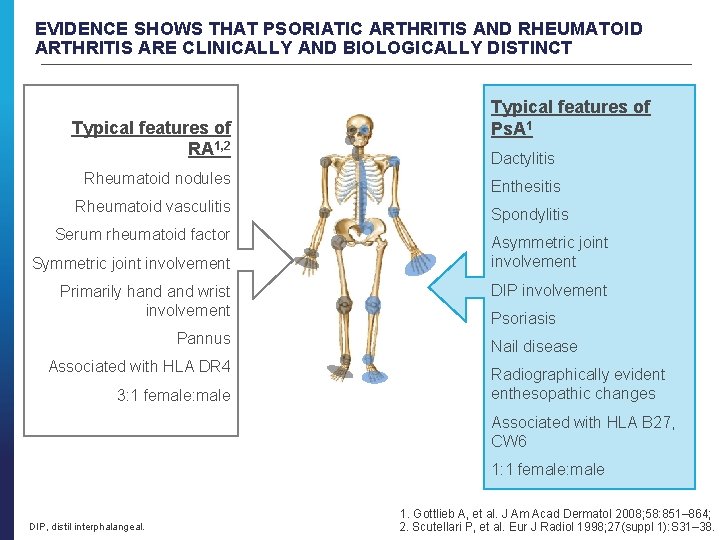
EVIDENCE SHOWS THAT PSORIATIC ARTHRITIS AND RHEUMATOID ARTHRITIS ARE CLINICALLY AND BIOLOGICALLY DISTINCT Typical features of RA 1, 2 Typical features of Ps. A 1 Dactylitis Rheumatoid nodules Enthesitis Rheumatoid vasculitis Spondylitis Serum rheumatoid factor Symmetric joint involvement Primarily hand wrist involvement Pannus Associated with HLA DR 4 3: 1 female: male Asymmetric joint involvement DIP involvement Psoriasis Nail disease Radiographically evident enthesopathic changes Associated with HLA B 27, CW 6 1: 1 female: male DIP, distil interphalangeal. 1. Gottlieb A, et al. J Am Acad Dermatol 2008; 58: 851– 864; 2. Scutellari P, et al. Eur J Radiol 1998; 27(suppl 1): S 31– 38.
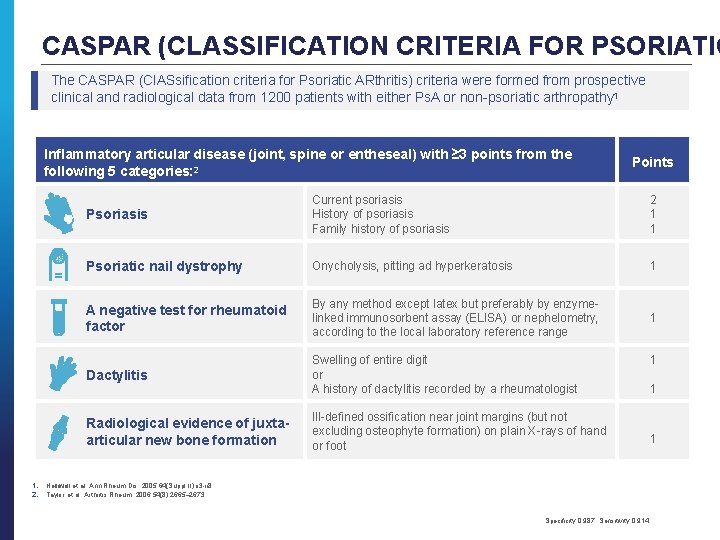
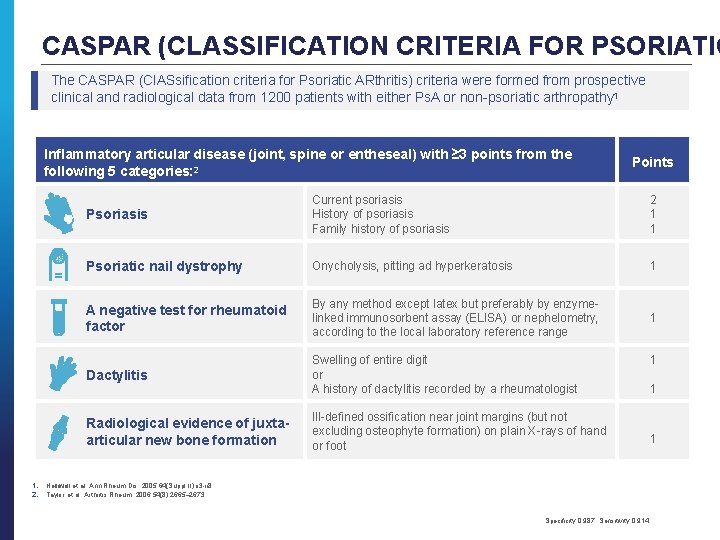
CASPAR (CLASSIFICATION CRITERIA FOR PSORIATIC The CASPAR (Cl. ASsification criteria for Psoriatic ARthritis) criteria were formed from prospective clinical and radiological data from 1200 patients with either Ps. A or non-psoriatic arthropathy 1 Inflammatory articular disease (joint, spine or entheseal) with ≥ 3 points from the following 5 categories: 2 1. 2. Points Psoriasis Current psoriasis History of psoriasis Family history of psoriasis 2 1 1 Psoriatic nail dystrophy Onycholysis, pitting ad hyperkeratosis 1 A negative test for rheumatoid factor By any method except latex but preferably by enzyme- linked immunosorbent assay (ELISA) or nephelometry, according to the local laboratory reference range 1 Dactylitis Swelling of entire digit or A history of dactylitis recorded by a rheumatologist Radiological evidence of juxta- articular new bone formation Ill-defined ossification near joint margins (but not excluding osteophyte formation) on plain X-rays of hand or foot 1 1 1 Helliwell et al. Ann Rheum Dis. 2005; 64(Suppl II): ii 3 -ii 8. Taylor et al. Arthritis Rheum. 2006; 54(8): 2665– 2673. Specificity 0. 987, Sensitivity 0. 914.
PSORIATIC ARTHRITIS AETIOLOGY AND PATHOPHYSIOLOGY
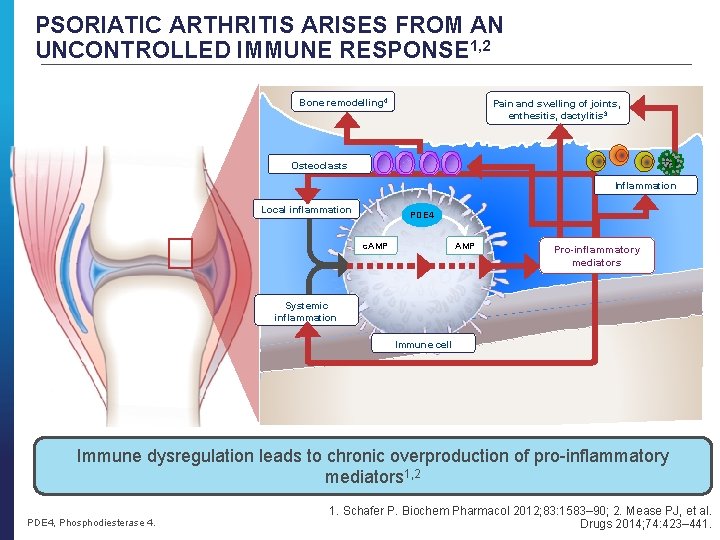
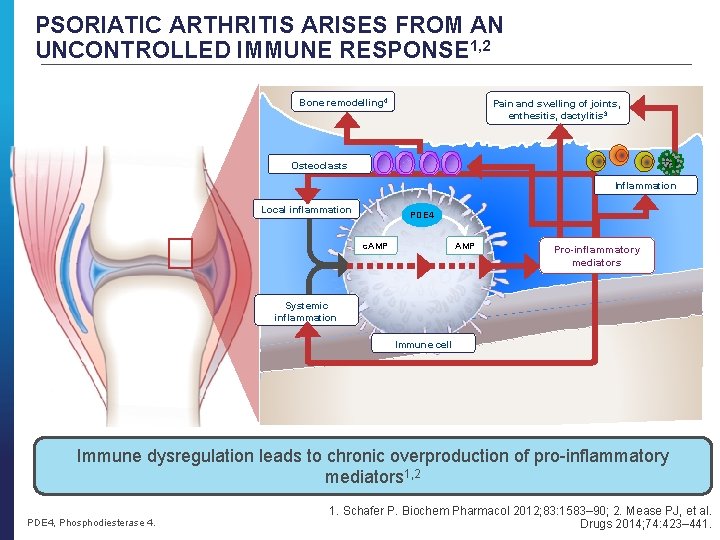
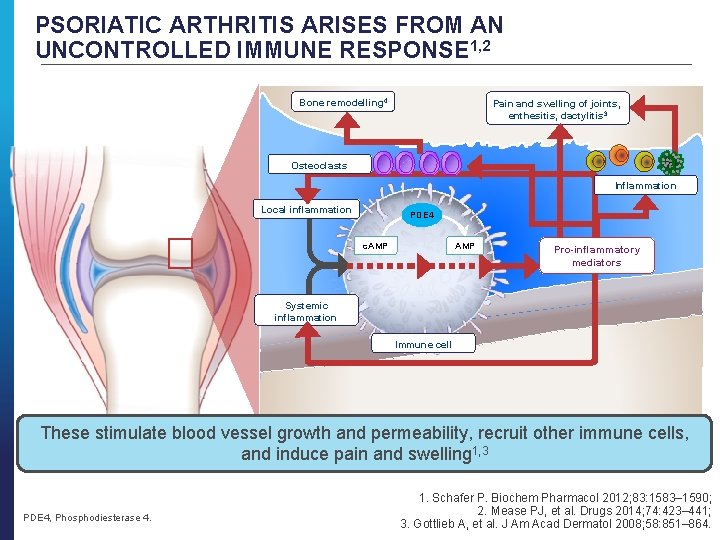
PSORIATIC ARTHRITIS ARISES FROM AN UNCONTROLLED IMMUNE RESPONSE 1, 2 Bone remodelling 4 Pain and swelling of joints, enthesitis, dactylitis 3 Osteoclasts Inflammation Local inflammation PDE 4 c. AMP Pro-inflammatory mediators Systemic inflammation Immune cell Immune dysregulation leads to chronic overproduction of pro-inflammatory mediators 1, 2 PDE 4, Phosphodiesterase 4. 1. Schafer P. Biochem Pharmacol 2012; 83: 1583– 90; 2. Mease PJ, et al. Drugs 2014; 74: 423– 441.
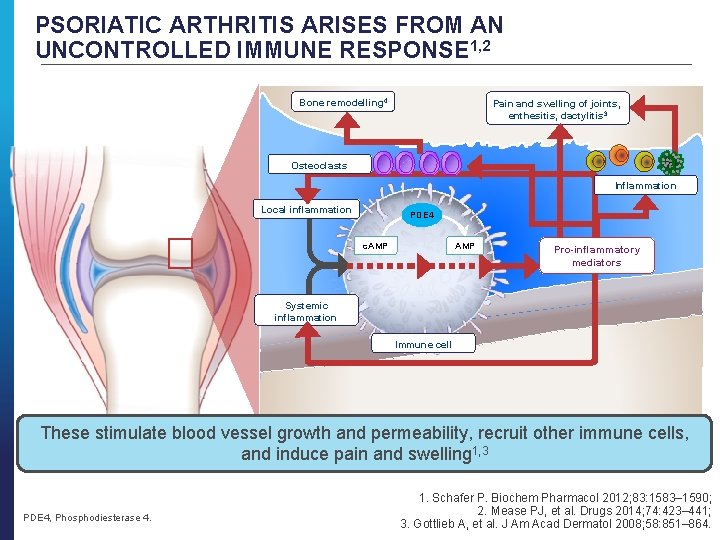
PSORIATIC ARTHRITIS ARISES FROM AN UNCONTROLLED IMMUNE RESPONSE 1, 2 Bone remodelling 4 Pain and swelling of joints, enthesitis, dactylitis 3 Osteoclasts Inflammation Local inflammation PDE 4 c. AMP Pro-inflammatory mediators Systemic inflammation Immune cell These stimulate blood vessel growth and permeability, recruit other immune cells, Immune dysregulation leads to chronic overproduction of pro-inflammatory mediators and induce pain and swelling 1, 3 PDE 4, Phosphodiesterase 4. 1. Schafer P. Biochem Pharmacol 2012; 83: 1583– 1590; 2. Mease PJ, et al. Drugs 2014; 74: 423– 441; 3. Gottlieb A, et al. J Am Acad Dermatol 2008; 58: 851– 864.
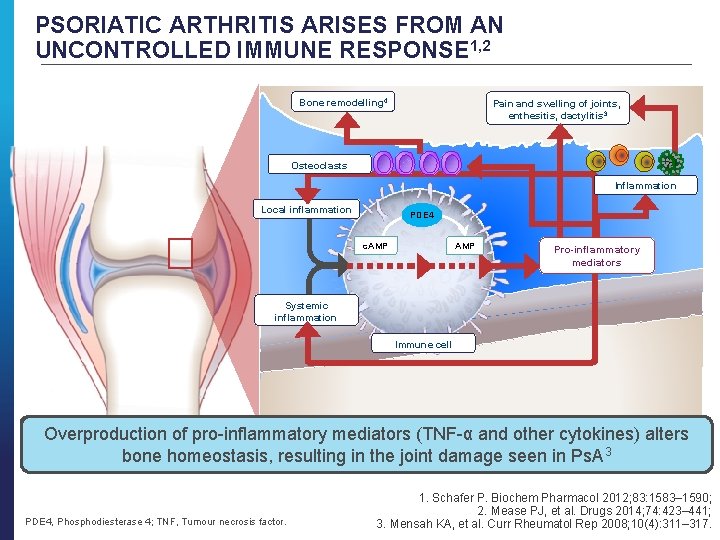
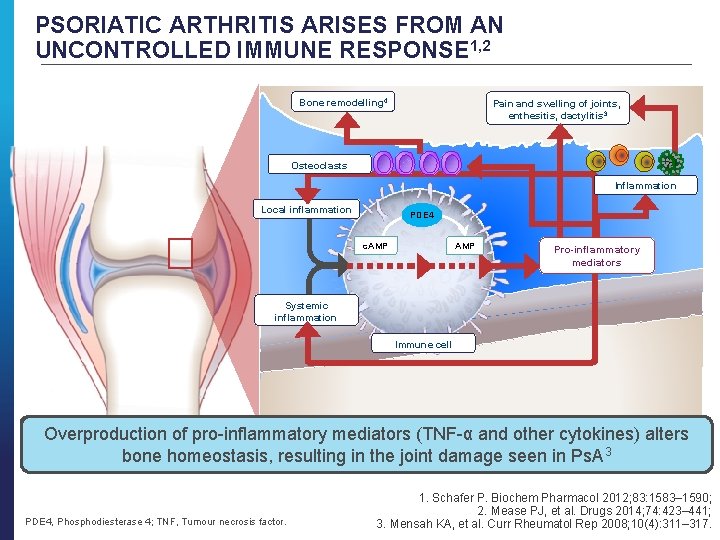
PSORIATIC ARTHRITIS ARISES FROM AN UNCONTROLLED IMMUNE RESPONSE 1, 2 Bone remodelling 4 Pain and swelling of joints, enthesitis, dactylitis 3 Osteoclasts Inflammation Local inflammation PDE 4 c. AMP Pro-inflammatory mediators Systemic inflammation Immune cell Immune dysregulation leads to chronic overproduction of pro-inflammatory mediators These stimulate blood vessel growth and permeability, recruits other immune cells Overproduction of pro-inflammatory mediators (TNF-α and other cytokines) alters 3 and induces pain and swelling 1, 3 bone homeostasis, resulting in the joint damage seen in Ps. A PDE 4, Phosphodiesterase 4; TNF, Tumour necrosis factor. 1. Schafer P. Biochem Pharmacol 2012; 83: 1583– 1590; 2. Mease PJ, et al. Drugs 2014; 74: 423– 441; 3. Mensah KA, et al. Curr Rheumatol Rep 2008; 10(4): 311– 317.
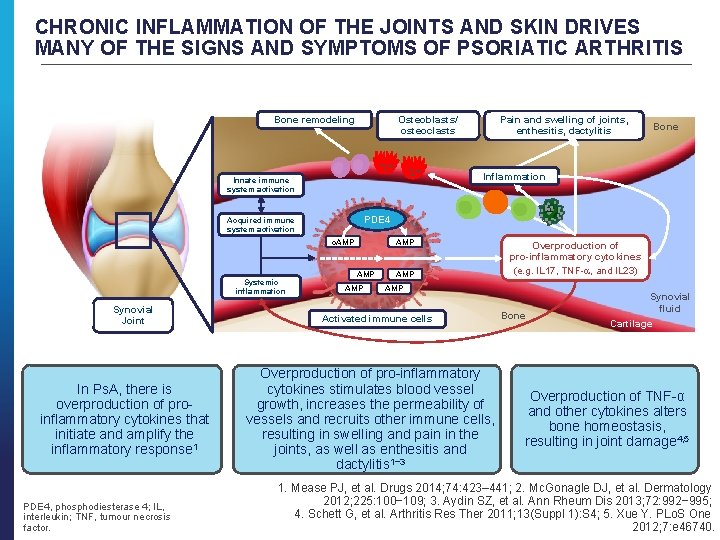
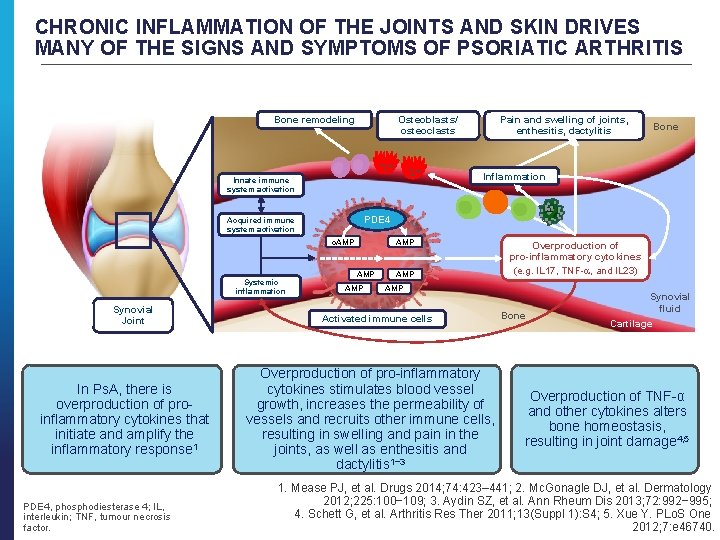
CHRONIC INFLAMMATION OF THE JOINTS AND SKIN DRIVES MANY OF THE SIGNS AND SYMPTOMS OF PSORIATIC ARTHRITIS Bone remodeling Osteoblasts/ osteoclasts PDE 4 Acquired immune system activation c. AMP Synovial Joint In Ps. A, there is overproduction of proinflammatory cytokines that initiate and amplify the inflammatory response 1 PDE 4, phosphodiesterase 4; IL, interleukin; TNF, tumour necrosis factor. Bone Inflammation Innate immune system activation Systemic inflammation Pain and swelling of joints, enthesitis, dactylitis AMP AMP Overproduction of pro-inflammatory cytokines (e. g. IL 17, TNF- , and IL 23) AMP Activated immune cells Overproduction of pro-inflammatory cytokines stimulates blood vessel growth, increases the permeability of vessels and recruits other immune cells, resulting in swelling and pain in the joints, as well as enthesitis and dactylitis 1− 3 Bone Synovial fluid Cartilage Overproduction of TNF-α and other cytokines alters bone homeostasis, resulting in joint damage 4, 5 1. Mease PJ, et al. Drugs 2014; 74: 423– 441; 2. Mc. Gonagle DJ, et al. Dermatology 2012; 225: 100− 109; 3. Aydin SZ, et al. Ann Rheum Dis 2013; 72: 992− 995; 4. Schett G, et al. Arthritis Res Ther 2011; 13(Suppl 1): S 4; 5. Xue Y. PLo. S One 2012; 7: e 46740.
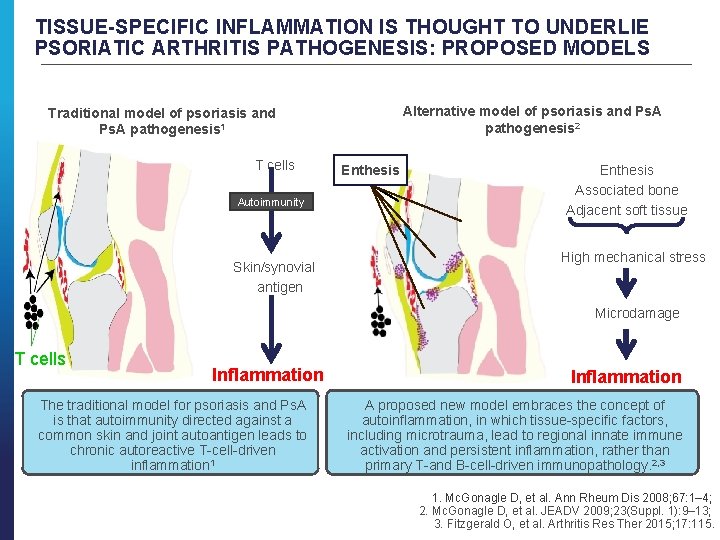
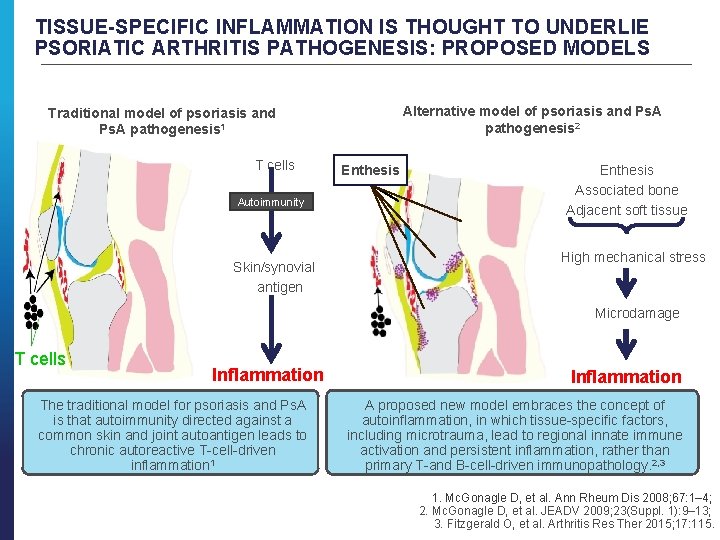
TISSUE-SPECIFIC INFLAMMATION IS THOUGHT TO UNDERLIE PSORIATIC ARTHRITIS PATHOGENESIS: PROPOSED MODELS Alternative model of psoriasis and Ps. A pathogenesis 2 Traditional model of psoriasis and Ps. A pathogenesis 1 T cells Autoimmunity Skin/synovial antigen Enthesis Associated bone Adjacent soft tissue High mechanical stress Microdamage T cells Inflammation The traditional model for psoriasis and Ps. A is that autoimmunity directed against a common skin and joint autoantigen leads to chronic autoreactive T-cell-driven inflammation 1 Inflammation A proposed new model embraces the concept of autoinflammation, in which tissue-specific factors, including microtrauma, lead to regional innate immune activation and persistent inflammation, rather than primary T-and B-cell-driven immunopathology. 2, 3 1. Mc. Gonagle D, et al. Ann Rheum Dis 2008; 67: 1– 4; 2. Mc. Gonagle D, et al. JEADV 2009; 23(Suppl. 1): 9– 13; 3. Fitzgerald O, et al. Arthritis Res Ther 2015; 17: 115.
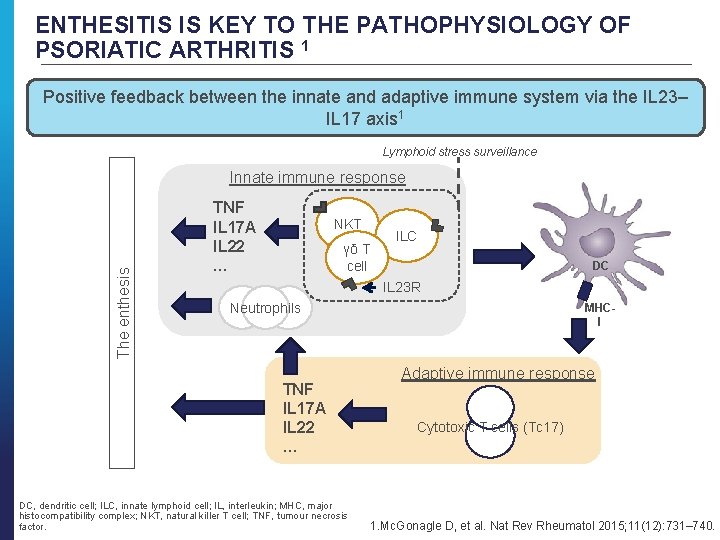
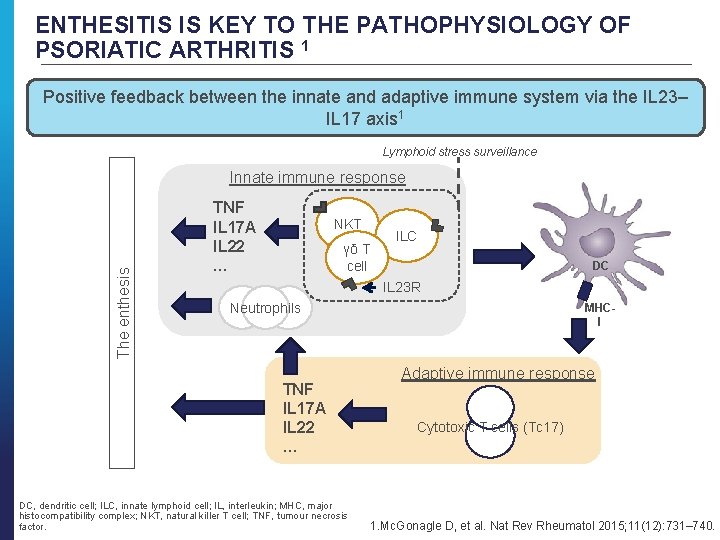
ENTHESITIS IS KEY TO THE PATHOPHYSIOLOGY OF PSORIATIC ARTHRITIS 1 Positive feedback between the innate and adaptive immune system via the IL 23– IL 17 axis 1 Lymphoid stress surveillance The enthesis Innate immune response TNF IL 17 A IL 22 … NKT γδ T cell ILC DC IL 23 R Neutrophils TNF IL 17 A IL 22 … DC, dendritic cell; ILC, innate lymphoid cell; IL, interleukin; MHC, major histocompatibility complex; NKT, natural killer T cell; TNF, tumour necrosis factor. MHCI Adaptive immune response Cytotoxic T cells (Tc 17) 1. Mc. Gonagle D, et al. Nat Rev Rheumatol 2015; 11(12): 731– 740.
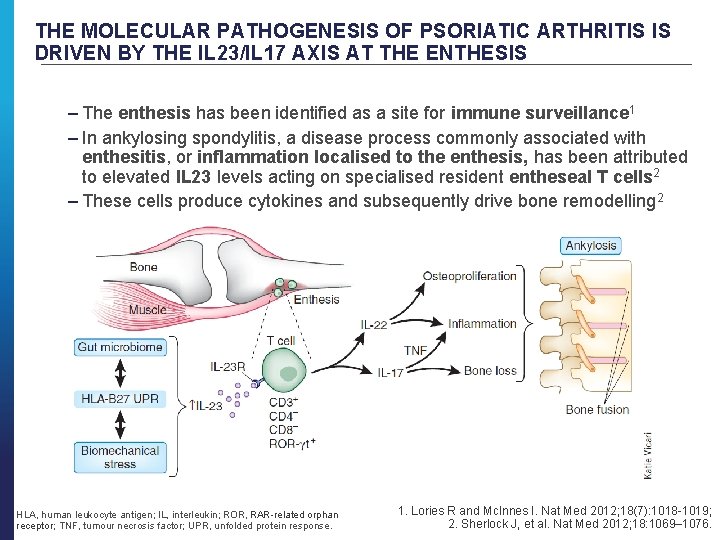
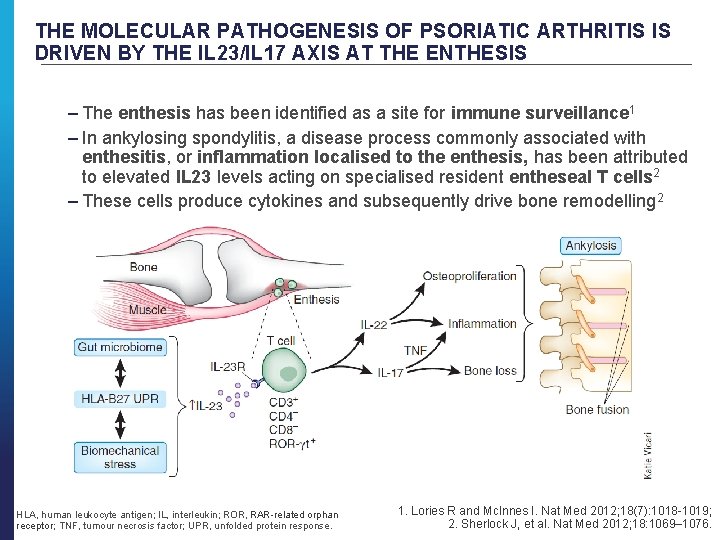
THE MOLECULAR PATHOGENESIS OF PSORIATIC ARTHRITIS IS DRIVEN BY THE IL 23/IL 17 AXIS AT THE ENTHESIS – The enthesis has been identified as a site for immune surveillance 1 – In ankylosing spondylitis, a disease process commonly associated with enthesitis, or inflammation localised to the enthesis, has been attributed to elevated IL 23 levels acting on specialised resident entheseal T cells 2 – These cells produce cytokines and subsequently drive bone remodelling 2 HLA, human leukocyte antigen; IL, interleukin; ROR, RAR-related orphan receptor; TNF, tumour necrosis factor; UPR, unfolded protein response. 1. Lories R and Mc. Innes I. Nat Med 2012; 18(7): 1018 -1019; 2. Sherlock J, et al. Nat Med 2012; 18: 1069– 1076.
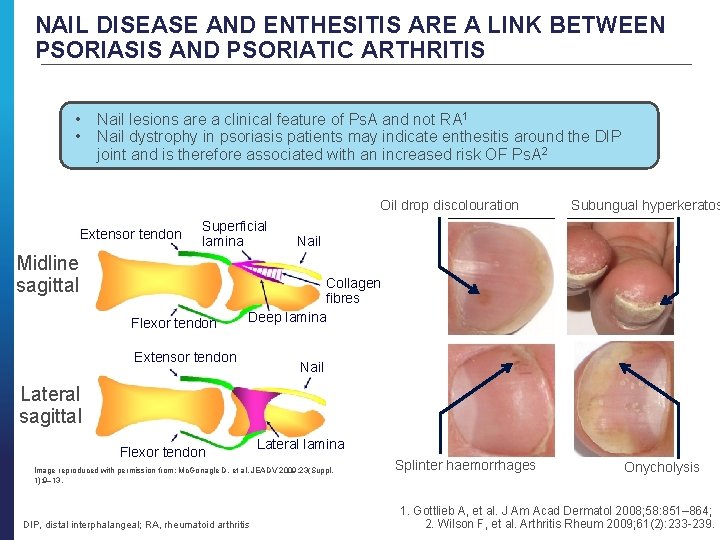
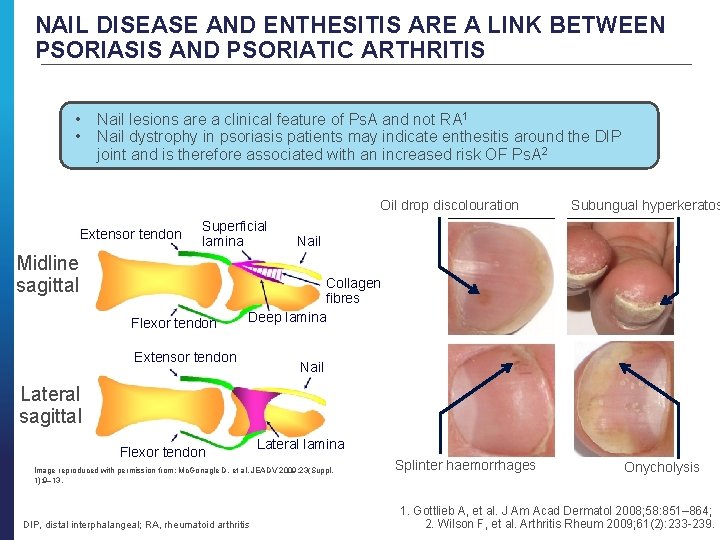
NAIL DISEASE AND ENTHESITIS ARE A LINK BETWEEN PSORIASIS AND PSORIATIC ARTHRITIS • • Nail lesions are a clinical feature of Ps. A and not RA 1 Nail dystrophy in psoriasis patients may indicate enthesitis around the DIP joint and is therefore associated with an increased risk OF Ps. A 2 Oil drop discolouration Extensor tendon Superficial lamina Midline sagittal Flexor tendon Subungual hyperkeratos Nail Collagen fibres Deep lamina Extensor tendon Nail Lateral sagittal Flexor tendon Lateral lamina Image reproduced with permission from: Mc. Gonagle D, et al. JEADV 2009; 23(Suppl. 1): 9– 13. DIP, distal interphalangeal; RA, rheumatoid arthritis Splinter haemorrhages Onycholysis 1. Gottlieb A, et al. J Am Acad Dermatol 2008; 58: 851– 864; 2. Wilson F, et al. Arthritis Rheum 2009; 61(2): 233 -239.

TREATMENT APPROACHES: PSORIATIC ARTHRITIS

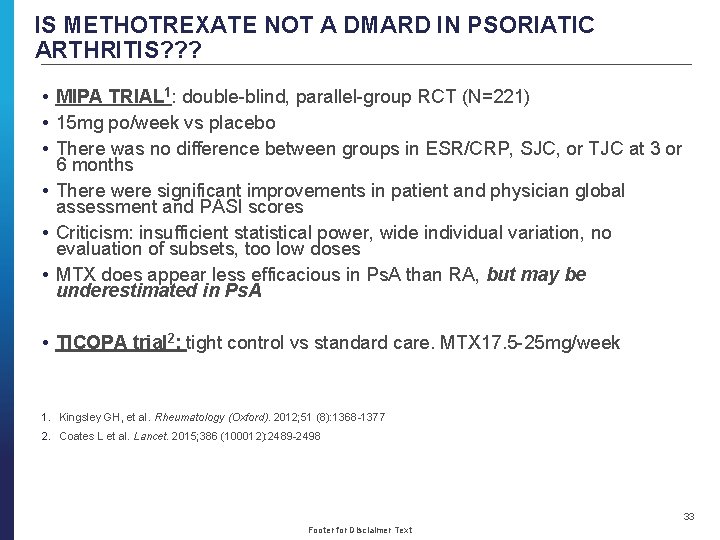
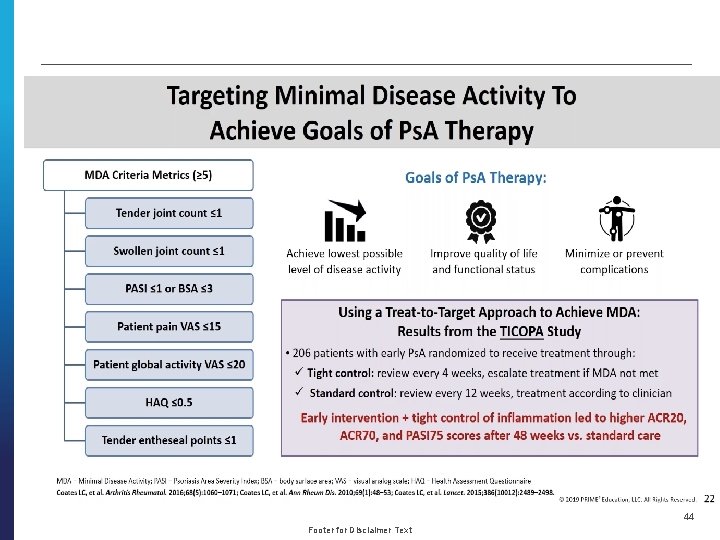
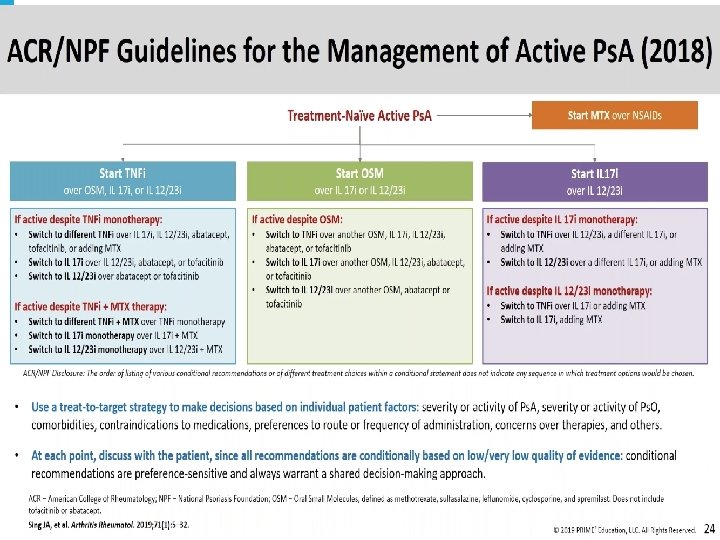
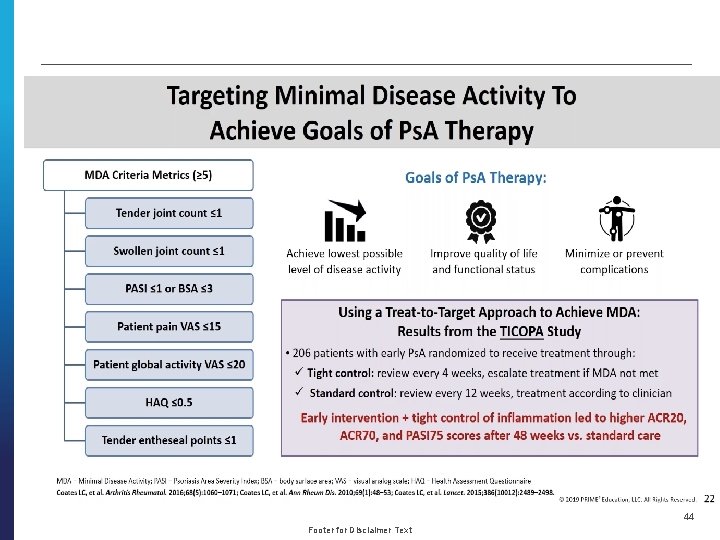
IS METHOTREXATE NOT A DMARD IN PSORIATIC ARTHRITIS? ? ? • MIPA TRIAL 1: double-blind, parallel-group RCT (N=221) • 15 mg po/week vs placebo • There was no difference between groups in ESR/CRP, SJC, or TJC at 3 or 6 months • There were significant improvements in patient and physician global assessment and PASI scores • Criticism: insufficient statistical power, wide individual variation, no evaluation of subsets, too low doses • MTX does appear less efficacious in Ps. A than RA, but may be underestimated in Ps. A • TICOPA trial 2: tight control vs standard care. MTX 17. 5 -25 mg/week 1. Kingsley GH, et al. Rheumatology (Oxford). 2012; 51 (8): 1368 -1377 2. Coates L et al. Lancet. 2015; 386 (100012): 2489 -2498 33 Footer for Disclaimer Text
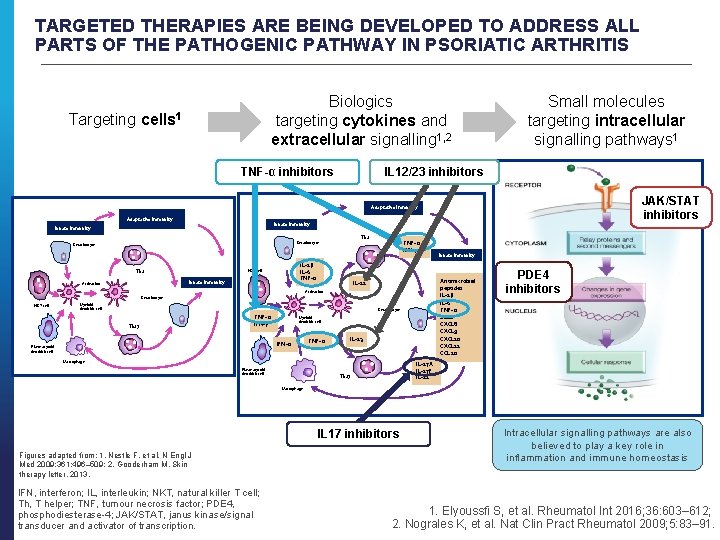
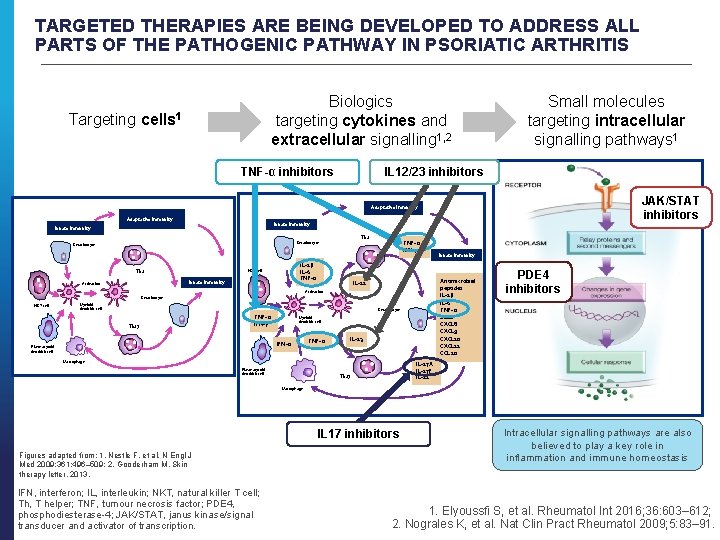
TARGETED THERAPIES ARE BEING DEVELOPED TO ADDRESS ALL PARTS OF THE PATHOGENIC PATHWAY IN PSORIATIC ARTHRITIS Biologics targeting cytokines and extracellular signalling 1, 2 Targeting cells 1 TNF-α inhibitors Small molecules targeting intracellular signalling pathways 1 IL 12/23 inhibitors JAK/STAT inhibitors Adaptative immunity Innate immunity Th 1 Keratinocyte IL-1β IL-6 TNF-α NKT cell Th 1 Innate immunity Activation TNF- α IFN-γ Antimicrobial peptides IL-1β IL-6 TNF- α S 100 CXCL 8 CXCL 9 CXCL 10 CXCL 11 CCL 20 IL-12 Activation Keratinocyte NKT cell Myeloid dendritic cell Keratinocyte Th 17 TNF- α IFN-γ Myeloid dendritic cell IFN-α Plasmacytoid dendritic cell TNF- α IL-23 Macrophage Plasmacytoid dendritic cell Innate immunity PDE 4 inhibitors IL-17 A IL-17 F IL-22 Th 17 Macrophage IL 17 inhibitors Figures adapted from: 1. Nestle F, et al. N Engl J Med 2009; 361: 496– 509; 2. Gooderham M. Skin therapy letter. 2013. IFN, interferon; IL, interleukin; NKT, natural killer T cell; Th, T helper; TNF, tumour necrosis factor; PDE 4, phosphodiesterase-4; JAK/STAT, janus kinase/signal transducer and activator of transcription. Intracellular signalling pathways are also believed to play a key role in inflammation and immune homeostasis 1. Elyoussfi S, et al. Rheumatol Int 2016; 36: 603– 612; 2. Nograles K, et al. Nat Clin Pract Rheumatol 2009; 5: 83– 91.
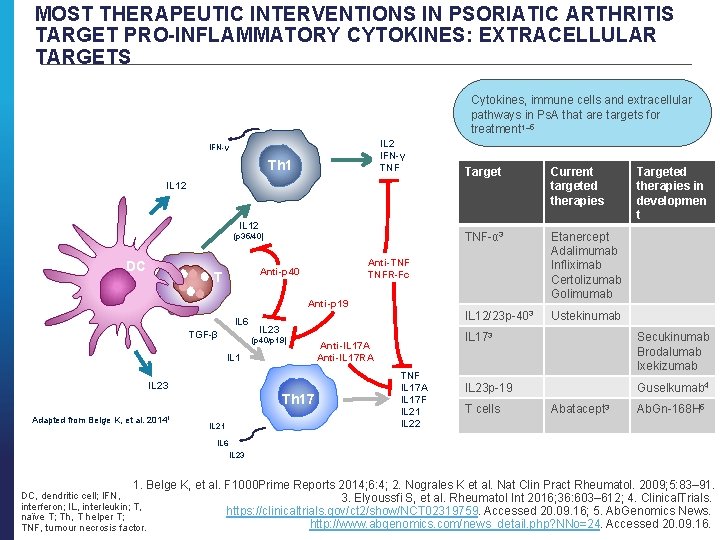
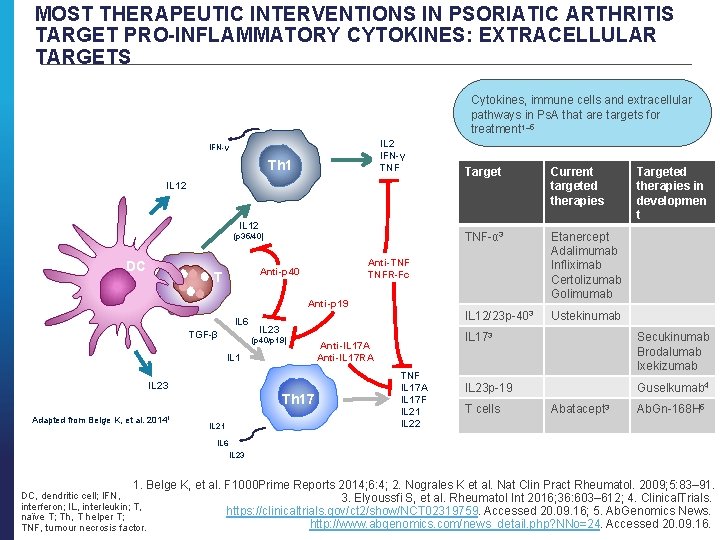
MOST THERAPEUTIC INTERVENTIONS IN PSORIATIC ARTHRITIS TARGET PRO-INFLAMMATORY CYTOKINES: EXTRACELLULAR TARGETS Cytokines, immune cells and extracellular pathways in Ps. A that are targets for treatment 1– 5 IL 2 IFN-γ TNF IFN-γ Th 1 Target Current targeted therapies TNF-α 3 Etanercept Adalimumab Infliximab Certolizumab Golimumab IL 12/23 p-403 Ustekinumab IL 12 (p 35/40) DC Anti-TNF TNFR-Fc Anti-p 40 T Anti-p 19 IL 6 TGF-β IL 23 (p 40/p 19) IL 1 IL 23 Adapted from Belge K, et al. 20141 Th 17 IL 21 Anti-IL 17 A Anti-IL 17 RA TNF IL 17 A IL 17 F IL 21 IL 22 Targeted therapies in developmen t IL 173 Secukinumab Brodalumab Ixekizumab IL 23 p-19 Guselkumab 4 T cells Abatacept 3 Ab. Gn-168 H 5 IL 6 IL 23 1. Belge K, et al. F 1000 Prime Reports 2014; 6: 4; 2. Nograles K et al. Nat Clin Pract Rheumatol. 2009; 5: 83– 91. DC, dendritic cell; IFN, 3. Elyoussfi S, et al. Rheumatol Int 2016; 36: 603– 612; 4. Clinical. Trials. interferon; IL, interleukin; T, https: //clinicaltrials. gov/ct 2/show/NCT 02319759. Accessed 20. 09. 16; 5. Ab. Genomics News. naïve T; Th, T helper T; http: //www. abgenomics. com/news_detail. php? NNo=24. Accessed 20. 09. 16. TNF, tumour necrosis factor.
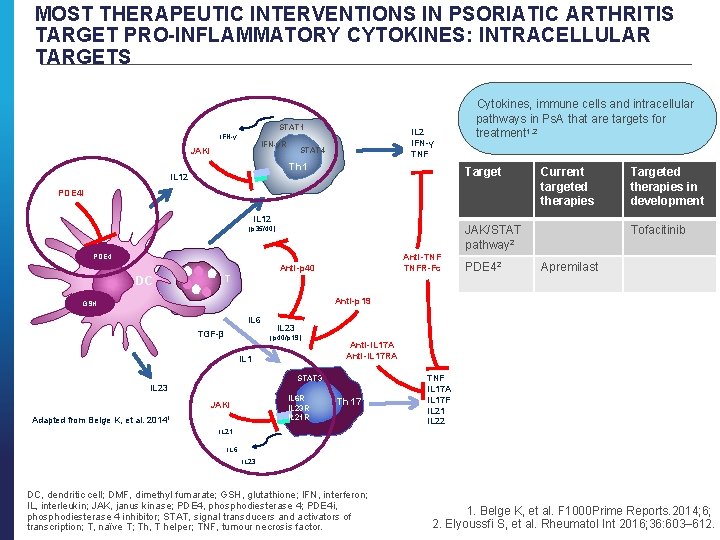
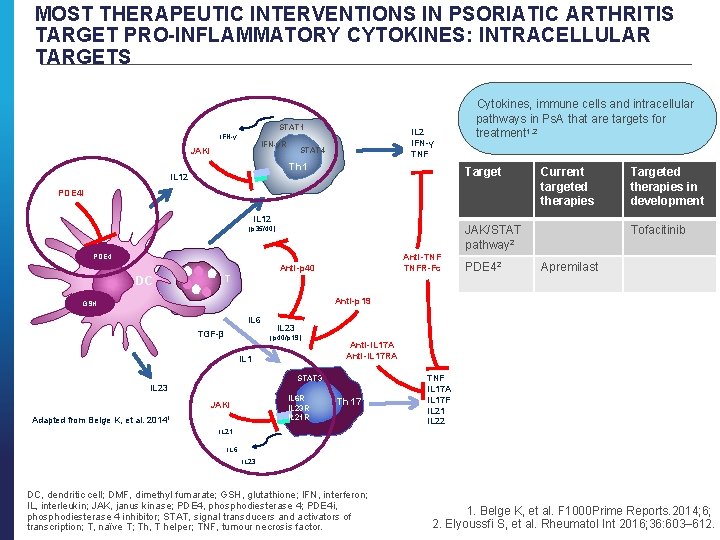
MOST THERAPEUTIC INTERVENTIONS IN PSORIATIC ARTHRITIS TARGET PRO-INFLAMMATORY CYTOKINES: INTRACELLULAR TARGETS STAT 1 IFN-γR JAKi IL 2 IFN-γ TNF STAT 4 Th 1 IL 12 Cytokines, immune cells and intracellular pathways in Ps. A that are targets for treatment 1, 2 Target PDE 4 i IL 12 JAK/STAT pathway 2 (p 35/40) Anti-TNF TNFR-Fc PDE 4 Anti-p 40 T DC Current targeted therapies PDE 42 Targeted therapies in development Tofacitinib Apremilast Anti-p 19 GSH IL 6 TGF-β IL 23 (p 40/p 19) IL 1 Anti-IL 17 A Anti-IL 17 RA STAT 3 IL 23 IL 6 R IL 23 R IL 21 R JAKi Adapted from Belge K, et al. 20141 Th 17 TNF IL 17 A IL 17 F IL 21 IL 22 IL 21 IL 6 IL 23 DC, dendritic cell; DMF, dimethyl fumarate; GSH, glutathione; IFN, interferon; IL, interleukin; JAK, janus kinase; PDE 4, phosphodiesterase 4; PDE 4 i, phosphodiesterase 4 inhibitor; STAT, signal transducers and activators of transcription; T, naïve T; Th, T helper; TNF, tumour necrosis factor. 1. Belge K, et al. F 1000 Prime Reports. 2014; 6; 2. Elyoussfi S, et al. Rheumatol Int 2016; 36: 603– 612.

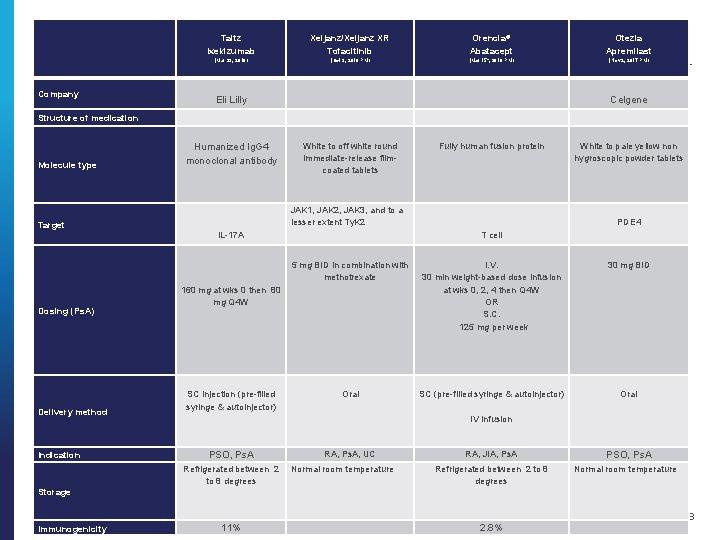
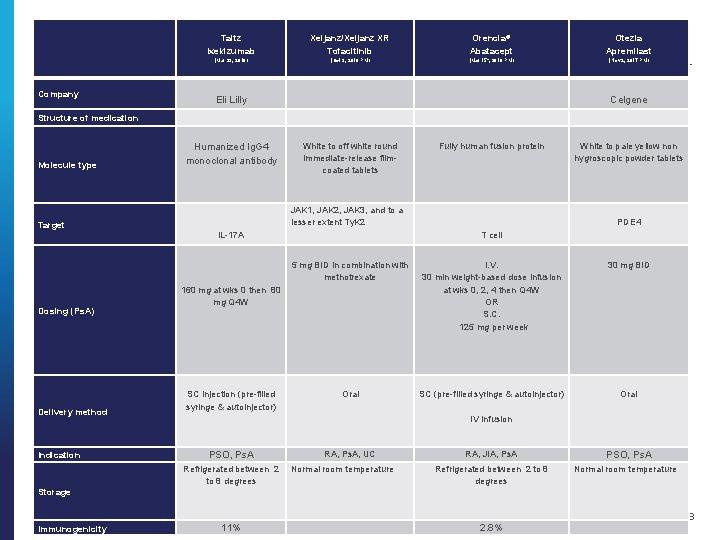
Company Structure of medication Taltz Ixekizumab Xeljanz/Xeljanz XR Tofacitinib Orencia® Abatacept Otezla Apremilast (Mar 29, 2018) (Oct 3, 2018 PM) (Mar 15 h, 2018 PM) (Nov 2, 2017 PM) Eli Lilly Celgene Molecule type IL-17 A Target Dosing (Ps. A) Fully human fusion protein White to pale yellow non hygroscopic powder tablets T cell PDE 4 I. V. 30 min weight-based dose infusion at wks 0, 2, 4 then Q 4 W OR S. C. 125 mg per week 30 mg BID SC (pre-filled syringe & autoinjector) IV infusion Oral JAK 1, JAK 2, JAK 3, and to a lesser extent Ty. K 2 5 mg BID in combination with methotrexate 160 mg at wks 0 then 80 mg Q 4 W SC injection (pre-filled syringe & autoinjector) Delivery method Oral RA, Ps. A, UC PSO, Ps. A Indication Refrigerated between 2 to 8 degrees Storage White to off white round immediate-release filmcoated tablets Humanized Ig. G 4 monoclonal antibody RA, JIA, Ps. A Normal room temperature Refrigerated between 2 to 8 degrees PSO, Ps. A Normal room temperature 38 Immunogenicity 11% Footer for Disclaimer Text 2. 8%

39 Footer for Disclaimer Text
40 Footer for Disclaimer Text
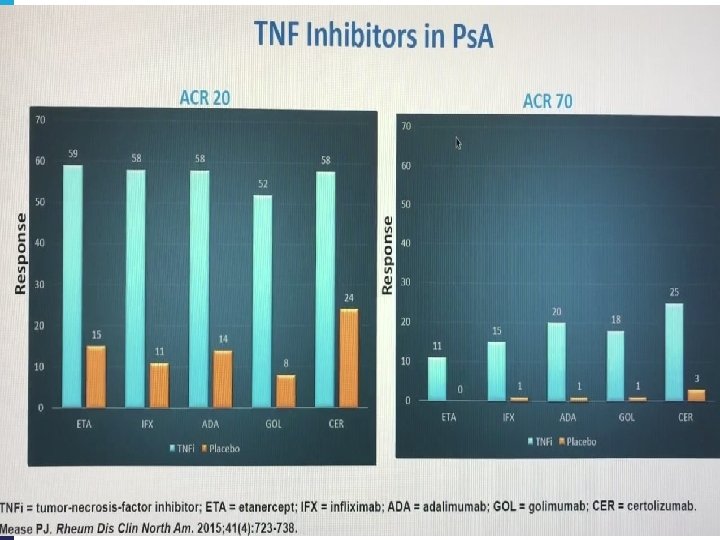
Footer for Disclaimer Text 41
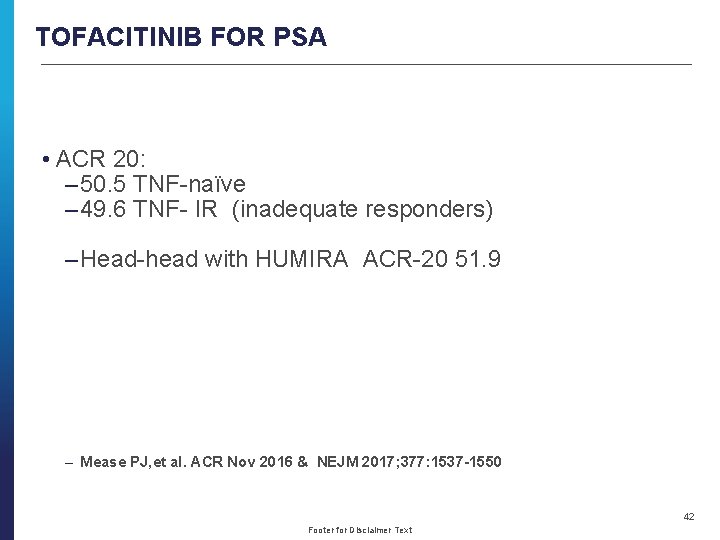
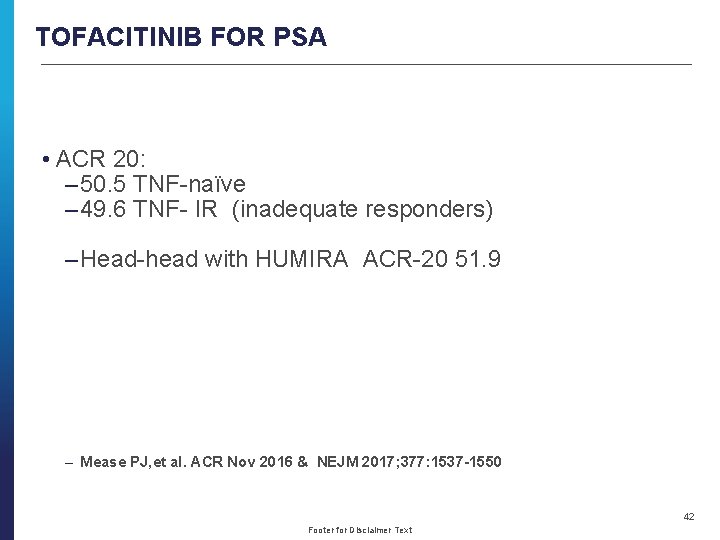
TOFACITINIB FOR PSA • ACR 20: – 50. 5 TNF-naïve – 49. 6 TNF- IR (inadequate responders) – Head-head with HUMIRA ACR-20 51. 9 – Mease PJ, et al. ACR Nov 2016 & NEJM 2017; 377: 1537 -1550 42 Footer for Disclaimer Text
43 Footer for Disclaimer Text
44 Footer for Disclaimer Text
THE BROADER IMPACT OF CHRONIC INFLAMMATION AND CLINICAL IMPLICATIONS
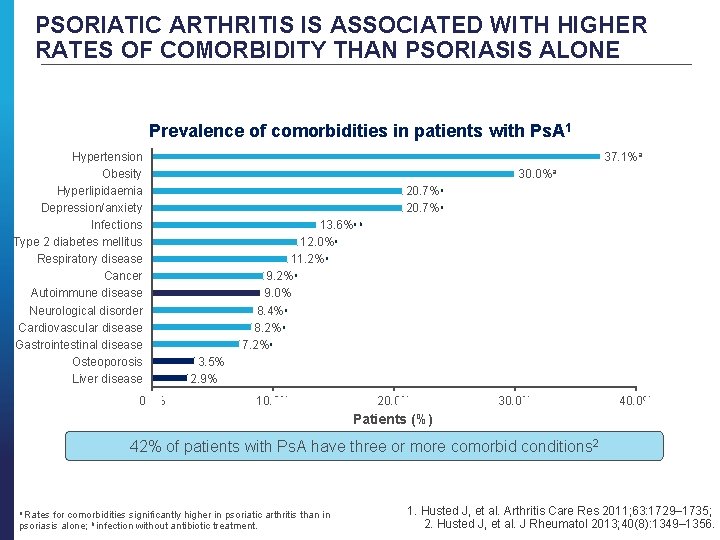
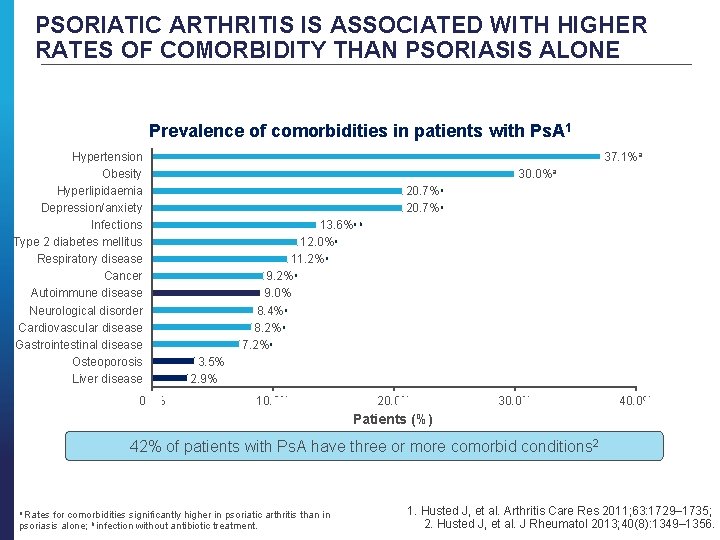
PSORIATIC ARTHRITIS IS ASSOCIATED WITH HIGHER RATES OF COMORBIDITY THAN PSORIASIS ALONE Prevalence of comorbidities in patients with Ps. A 1 Hypertension Obesity Hyperlipidaemia Depression/anxiety Infections Type 2 diabetes mellitus Respiratory disease Cancer Autoimmune disease Neurological disorder Cardiovascular disease Gastrointestinal disease Osteoporosis Liver disease 0. 0% 37. 1%a 30. 0%a 20. 7%a 13. 6%a, b 12. 0%a 11. 2%a 9. 0% 8. 4%a 8. 2%a 7. 2%a 3. 5% 2. 9% 10. 0% 20. 0% 30. 0% 40. 0% Patients (%) 42% of patients with Ps. A have three or more comorbid conditions 2 a Rates for comorbidities significantly higher in psoriatic arthritis than in psoriasis alone; b infection without antibiotic treatment. 1. Husted J, et al. Arthritis Care Res 2011; 63: 1729– 1735; 2. Husted J, et al. J Rheumatol 2013; 40(8): 1349– 1356.
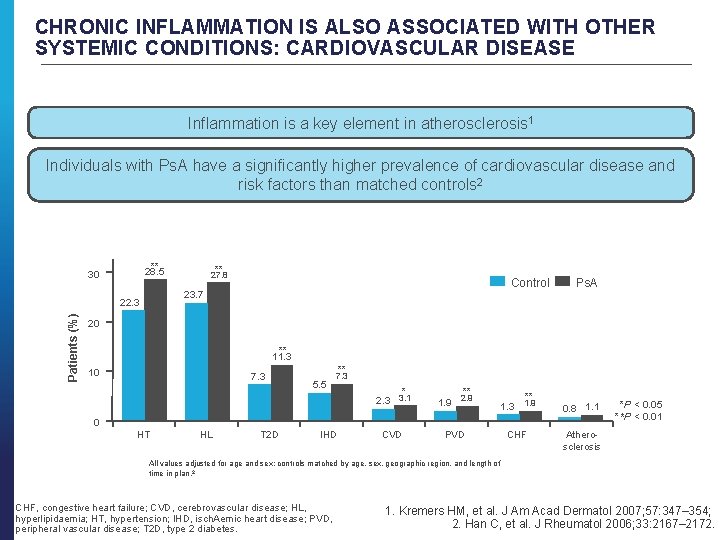
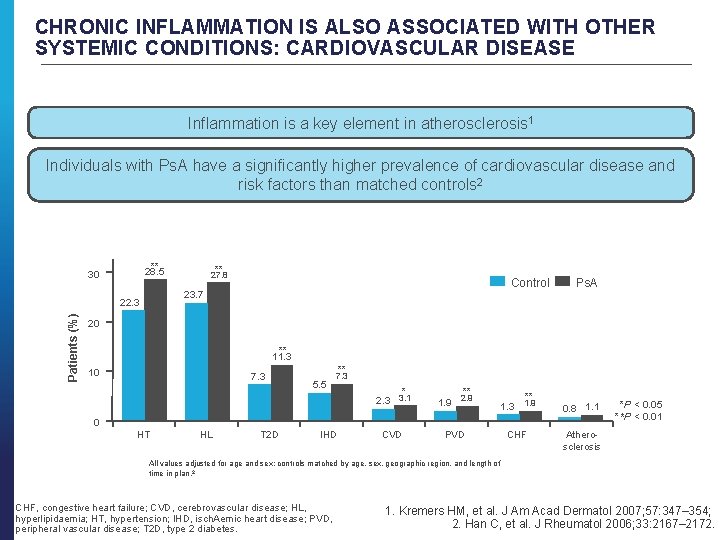
CHRONIC INFLAMMATION IS ALSO ASSOCIATED WITH OTHER SYSTEMIC CONDITIONS: CARDIOVASCULAR DISEASE Inflammation is a key element in atherosclerosis 1 Individuals with Ps. A have a significantly higher prevalence of cardiovascular disease and risk factors than matched controls 2 ** 28. 5 30 Control 23. 7 22. 3 Patients (%) ** 27. 8 Ps. A 20 ** 11. 3 10 7. 3 ** 5. 5 7. 3 * 2. 3 3. 1 ** 1. 9 2. 9 ** 1. 3 1. 9 CVD PVD CHF 0. 8 1. 1 0 HT HL T 2 D IHD *P < 0. 05 **P < 0. 01 Atherosclerosis All values adjusted for age and sex; controls matched by age, sex, geographic region, and length of time in plan. 2 CHF, congestive heart failure; CVD, cerebrovascular disease; HL, hyperlipidaemia; HT, hypertension; IHD, isch. Aemic heart disease; PVD, peripheral vascular disease; T 2 D, type 2 diabetes. 1. Kremers HM, et al. J Am Acad Dermatol 2007; 57: 347– 354; 2. Han C, et al. J Rheumatol 2006; 33: 2167– 2172.
PSA AND QUALITY OF LIFE • Patients with Ps. A have worse Qo. L than those with psoriasis alone 1 -HAQ -36 -item Short Form Health Survey -Euro. QOL-5 D • PATIENTS WITH Ps. A HAVE LOW LEVEL OF HRQo. L THAT IMPROVES WITH TREATMENT • HRQo. L=health related quality of life • 1. Rosen CF, et al. Rheumatology (Oxford). 2012; 51: 571 -576.

SUMMARY
SUMMARY • Ps. A is a chronic systemic inflammatory disease involving the skin and joints, and is closely related to psoriasis 1 • It is a clinically heterogeneous disease with five distinct subtypes 2, 3 • Diagnosing Ps. A is a major challenge; CASPAR classification helps to differentiate Ps. A from other arthropathies 4, 5 • In Ps. A overproduction of pro-inflammatory cytokines drives the chronic inflammatory response and results in the clinical hallmarks of the disease, including swelling/pain in the joints, enthesitis and dactylitis 6 – Several therapies are in development to target different components of the pathogenic pathways implicated in Ps. A 7 • Because dysregulated inflammation has systemic effects, Ps. A is associated with a number of serious co-morbidities including cardiovascular disease and metabolic syndrome 8, 9 1. Kavanaugh A, et al. Rheumatol Ther 2016; DOI 10. 1007/s 40744 -016 -0029 -z; 2. Moll JM and Wright V. Semin Arthritis Rheum 1973; 3: 55– 78; 3. Gottlieb A, et al. J Am Acad Dermatol 2008; 58: 851– 864; 4. Gottleib A, et al. J Am Acad Dermatol 2008; 58: 851– 864; 5. Taylor W, et al. Arthritis Rheum 2006; 54: 2665– 2673; 6. Mease PJ, et al. Drugs 2014; 74: 423– 441; 7. Elyoussfi S, et al. Rheumatol Int 2016; 36: 603– 612; 8. Han C, et al. J Rheumatol 2006; 33: 2167– 2172; 9. Raychaudhuri SK, et al. Metab Syndr Relat Disord 2010; 8: 331– 334.
THANK YOU FOR YOUR ATTENTION Questions are welcome
 Mike fernie wiki
Mike fernie wiki Dr karen pont
Dr karen pont Independent or dependent
Independent or dependent Newsworthy event (s); background event (s); sources
Newsworthy event (s); background event (s); sources Independent and dependent probability
Independent and dependent probability Near misses events
Near misses events 5 ws of event management
5 ws of event management Simple and compound events examples
Simple and compound events examples Peta konsep news item
Peta konsep news item Dr jeffrey sklar
Dr jeffrey sklar Cme task
Cme task Cme weather derivatives
Cme weather derivatives Cme invitation
Cme invitation Penicillin allergy cme
Penicillin allergy cme Cme fec
Cme fec Phosrenal
Phosrenal Cme semi centralizada
Cme semi centralizada Emory cme
Emory cme Dot price
Dot price Aapa self assessment
Aapa self assessment Pedialink cme
Pedialink cme Cme tracking tool
Cme tracking tool Market profile day types
Market profile day types Lente intensificadora de imagem para cme
Lente intensificadora de imagem para cme Continuing medical education
Continuing medical education Www nyp org nursing news cme
Www nyp org nursing news cme Cme 2012
Cme 2012 Dorsalisan
Dorsalisan Pont hydrogene
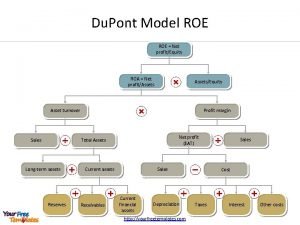
Pont hydrogene Du pont modellen
Du pont modellen Nir.bgazrt.hu
Nir.bgazrt.hu Du pont analiza
Du pont analiza Faaliyet oranları nelerdir
Faaliyet oranları nelerdir Du pontov rozklad
Du pontov rozklad Eper belépési pontok
Eper belépési pontok Osteotomie tibia
Osteotomie tibia Lactose formule haworth
Lactose formule haworth Sur le pont d'avignon filastrocca
Sur le pont d'avignon filastrocca Clemens xii pont max
Clemens xii pont max Pont du gare
Pont du gare Frecska ede
Frecska ede Transversus abdominis
Transversus abdominis Poutre prad
Poutre prad Pont fleur de lotus
Pont fleur de lotus De papy
De papy Eper belépési pont
Eper belépési pont Structurae pont a haubans
Structurae pont a haubans Du pont model
Du pont model Pont cassé collioure
Pont cassé collioure Pont
Pont Pont de wien
Pont de wien Disk shaped slices
Disk shaped slices