Why this CME on CKD CKD is a
- Slides: 30
Why this CME on CKD ? • CKD is a major global pandemic like DM • DM and HT make CKD burden very high • CKD predicts CVD – the major threat • Testing and therapy are inadequately used • Knowledge on CKD is at best sketchy • Testing and early therapy are economical • Most of the progression is preventable www. drsarma. in 1
Do we care about CKD ? 1. Doctors do not realize that CKD is hidden in their patients of DM, HT and in elderly people 2. Most doctors screen less than 10% of their clinic patients for CKD in its early stages 3. Patients are referred very late to nephrologists especially after the CKD is irreversible 4. Only < 1/4 of people with identified CKD get an ACE Inhibitor – all are true - all over the globe www. drsarma. in 2
What is the role of GPs ? 1. Recognize who is at risk of CKD 2. Consider all DM and HT as potential CKD pt. 3. Evaluate all at risk cases; Rx. hypertension 4. Understand e. GFR, Albuminuria, MAU 5. Stage the CKD and manage appropriately 6. Must start patients on ACEi or ARB early www. drsarma. in 3
Some useful Definitions 1. Azotemia - Elevated blood urea nitrogen - Biochemical (BUN >28 mg/dl) and creatinine (Cr >1. 5 mg/dl)2. Uremia is Azotemia + symptoms or signs of renal failure 3. End Stage Renal Disease (ESRD) - Uremia requiring transplantation or dialysis (Renal replacement therapy) 4. Chronic Renal Failure (CRF) - Irreversible kidney dysfunction with azotemia >3 months – now not used 5. Creatinine Clearance (CCr) - The rate of filtration of creatinine by the kidney (a marker of GFR) 6. Glomerular Filtration Rate (GFR) - The total rate of filtration of fluid from blood by the kidney www. drsarma. in 4
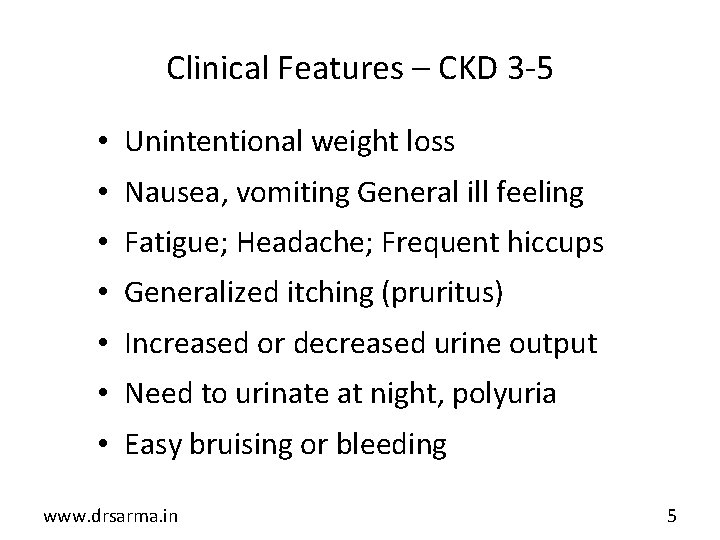
Clinical Features – CKD 3 -5 • Unintentional weight loss • Nausea, vomiting General ill feeling • Fatigue; Headache; Frequent hiccups • Generalized itching (pruritus) • Increased or decreased urine output • Need to urinate at night, polyuria • Easy bruising or bleeding www. drsarma. in 5
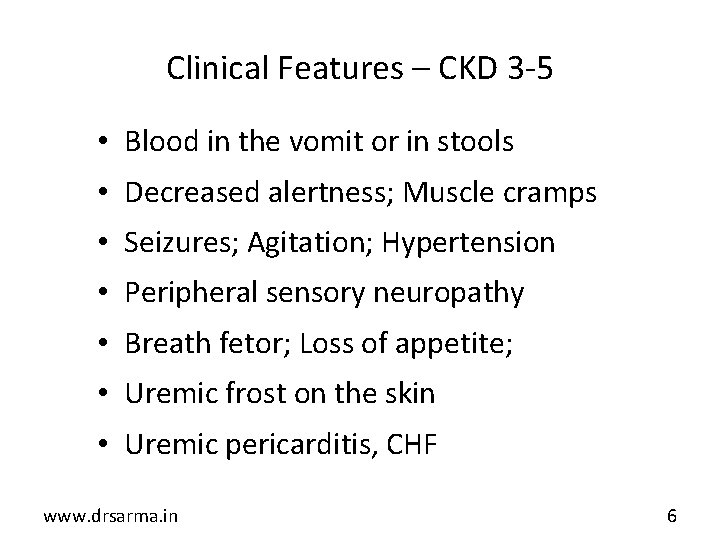
Clinical Features – CKD 3 -5 • Blood in the vomit or in stools • Decreased alertness; Muscle cramps • Seizures; Agitation; Hypertension • Peripheral sensory neuropathy • Breath fetor; Loss of appetite; • Uremic frost on the skin • Uremic pericarditis, CHF www. drsarma. in 6
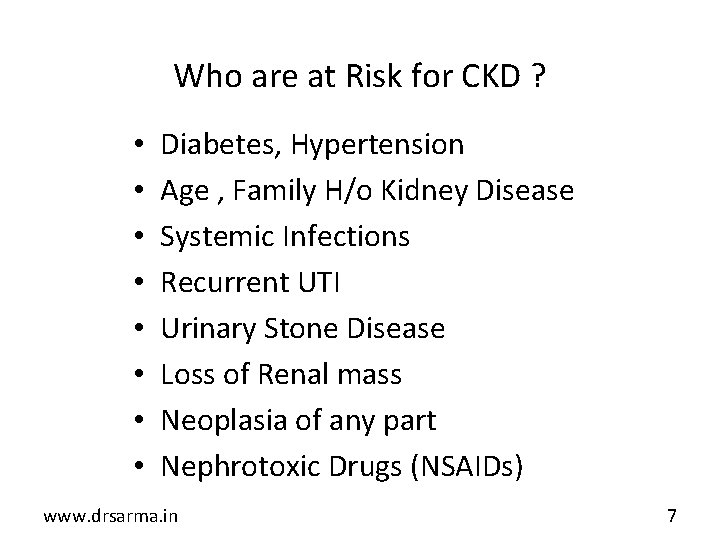
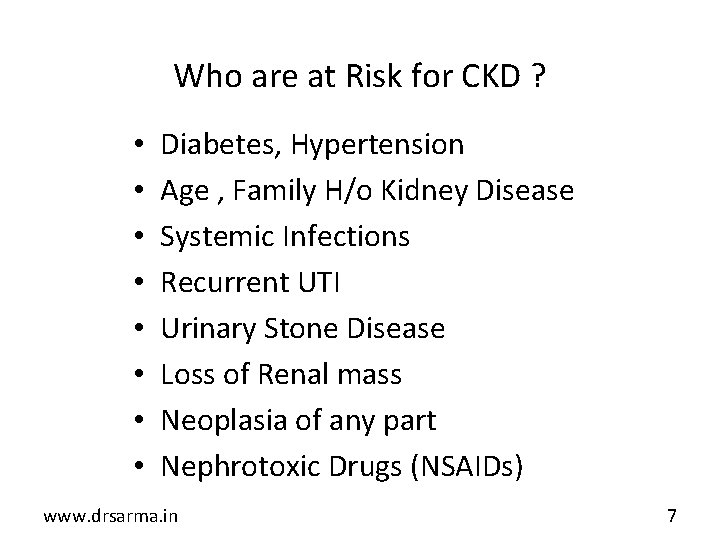
Who are at Risk for CKD ? • • Diabetes, Hypertension Age , Family H/o Kidney Disease Systemic Infections Recurrent UTI Urinary Stone Disease Loss of Renal mass Neoplasia of any part Nephrotoxic Drugs (NSAIDs) www. drsarma. in 7
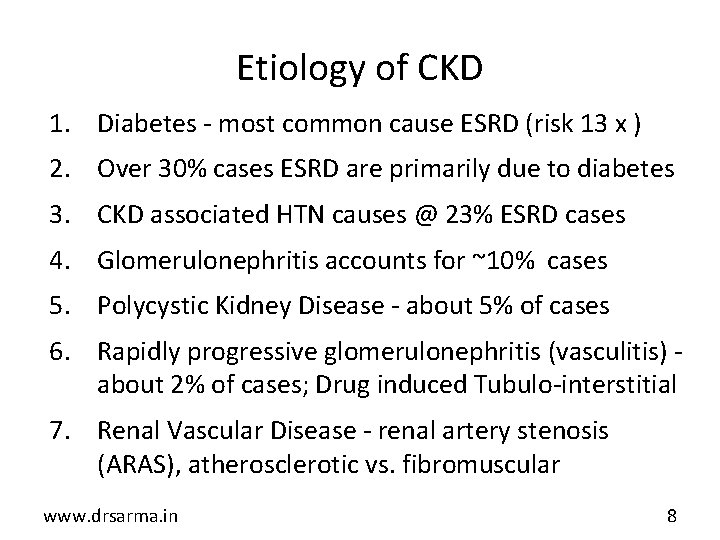
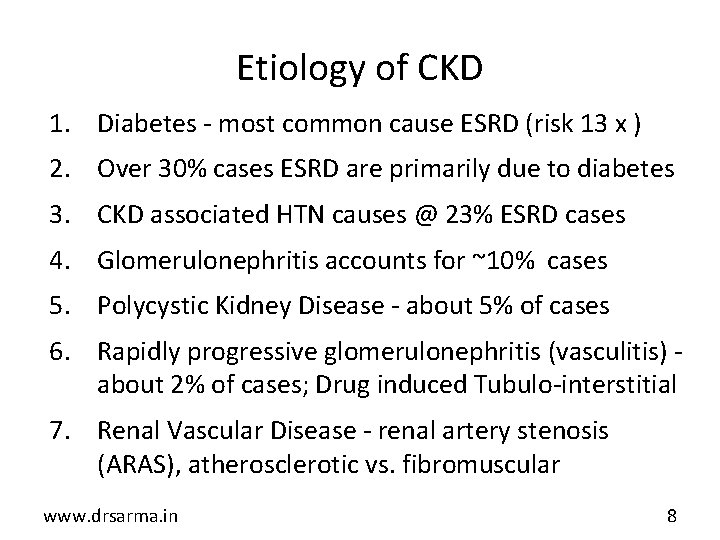
Etiology of CKD 1. Diabetes - most common cause ESRD (risk 13 x ) 2. Over 30% cases ESRD are primarily due to diabetes 3. CKD associated HTN causes @ 23% ESRD cases 4. Glomerulonephritis accounts for ~10% cases 5. Polycystic Kidney Disease - about 5% of cases 6. Rapidly progressive glomerulonephritis (vasculitis) about 2% of cases; Drug induced Tubulo-interstitial 7. Renal Vascular Disease - renal artery stenosis (ARAS), atherosclerotic vs. fibromuscular www. drsarma. in 8
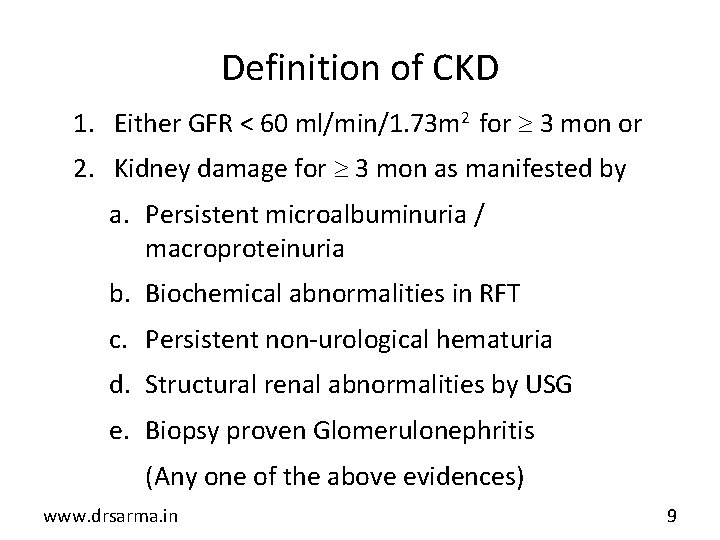
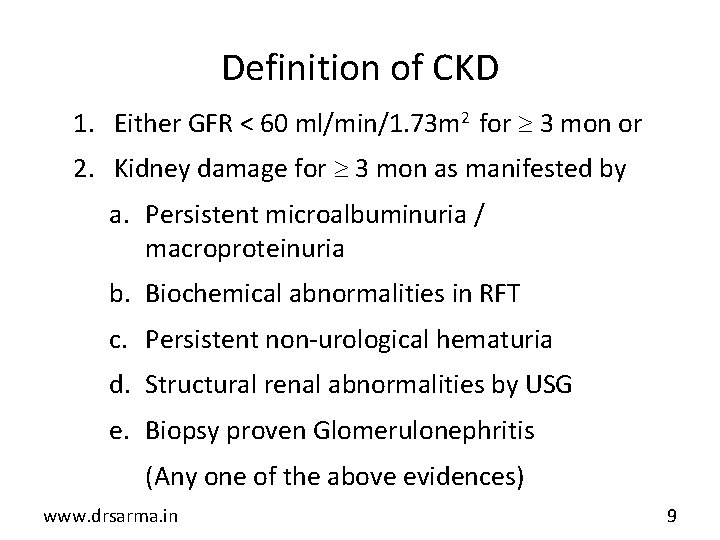
Definition of CKD 1. Either GFR < 60 ml/min/1. 73 m 2 for 3 mon or 2. Kidney damage for 3 mon as manifested by a. Persistent microalbuminuria / macroproteinuria b. Biochemical abnormalities in RFT c. Persistent non-urological hematuria d. Structural renal abnormalities by USG e. Biopsy proven Glomerulonephritis (Any one of the above evidences) www. drsarma. in 9
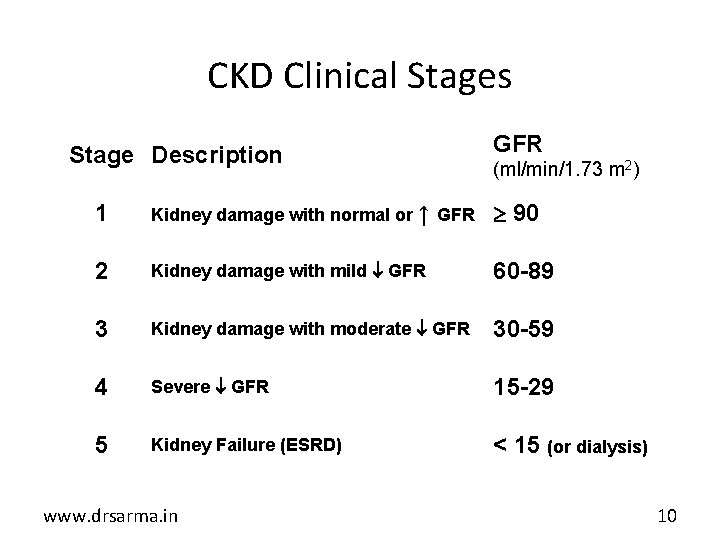
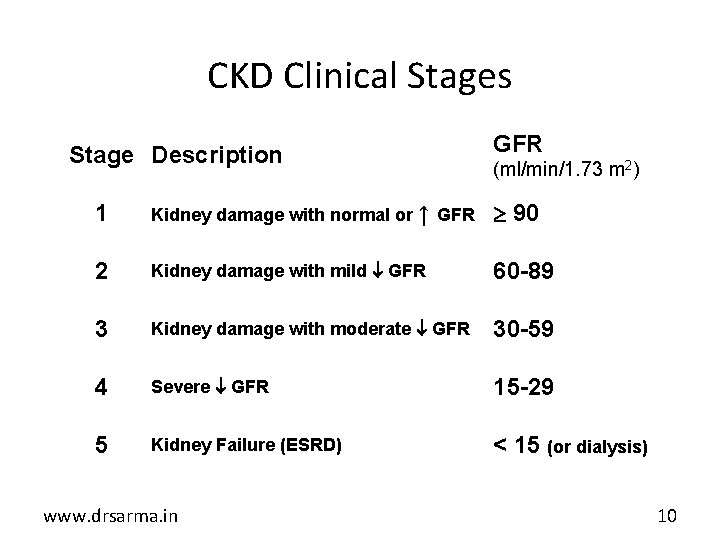
CKD Clinical Stages Stage Description GFR (ml/min/1. 73 m 2) 1 Kidney damage with normal or ↑ GFR 90 2 Kidney damage with mild GFR 60 -89 3 Kidney damage with moderate GFR 30 -59 4 Severe GFR 15 -29 5 Kidney Failure (ESRD) < 15 (or dialysis) www. drsarma. in 10
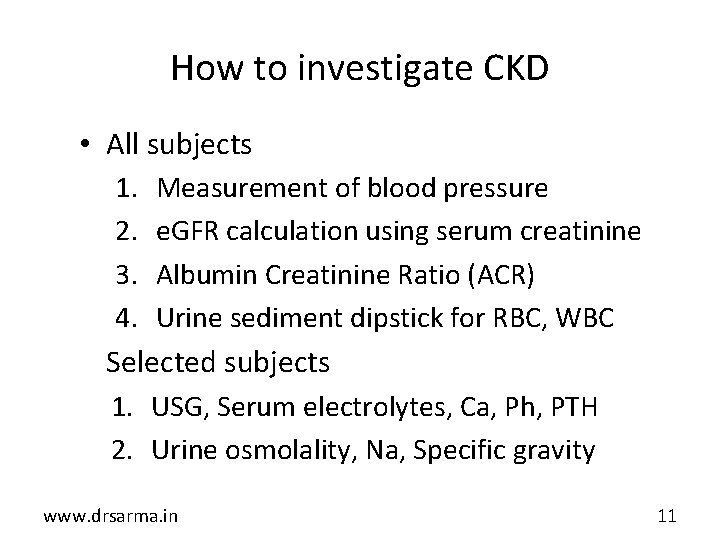
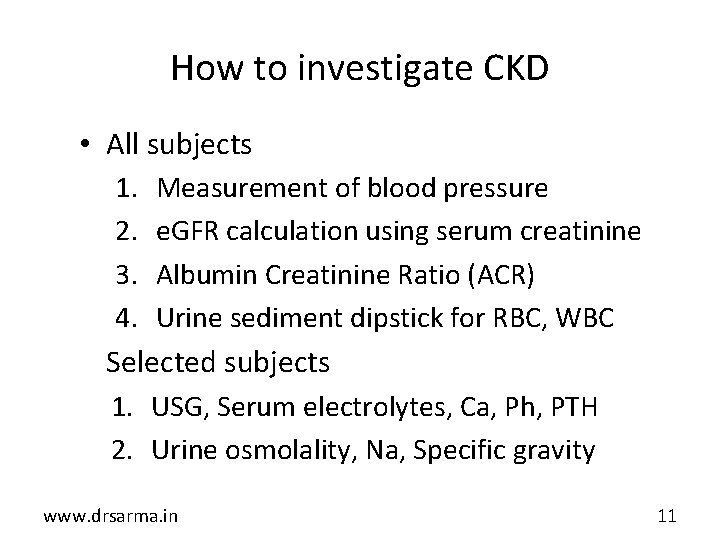
How to investigate CKD • All subjects 1. Measurement of blood pressure 2. e. GFR calculation using serum creatinine 3. Albumin Creatinine Ratio (ACR) 4. Urine sediment dipstick for RBC, WBC • Selected subjects 1. USG, Serum electrolytes, Ca, Ph, PTH 2. Urine osmolality, Na, Specific gravity www. drsarma. in 11
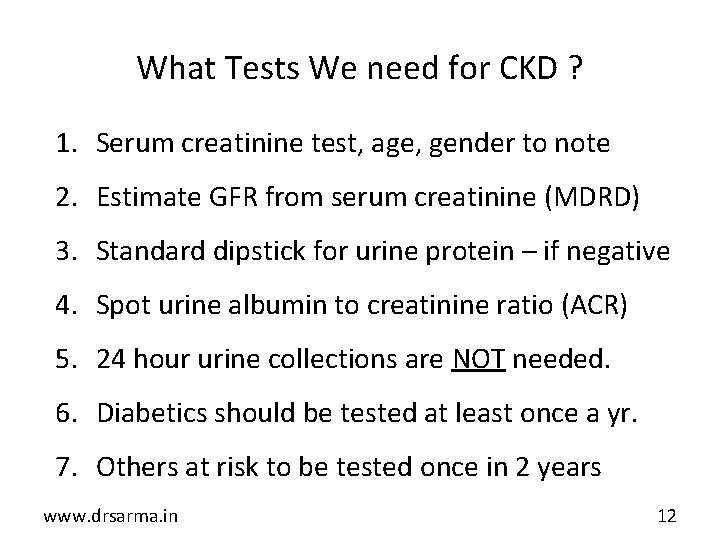
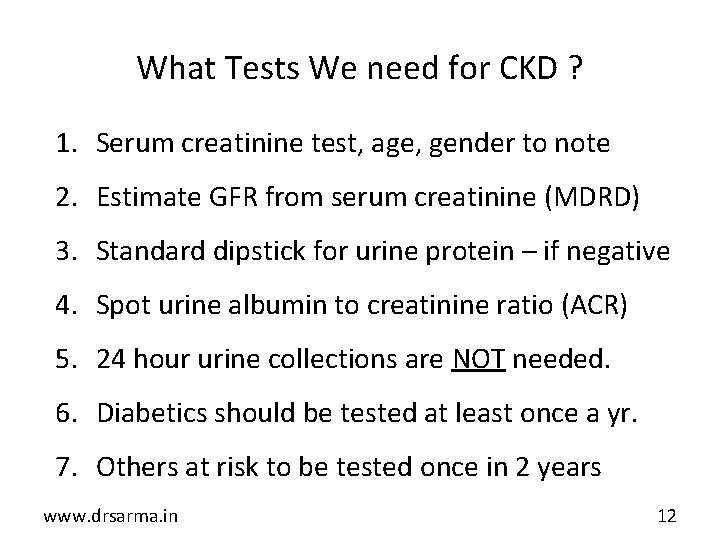
What Tests We need for CKD ? 1. Serum creatinine test, age, gender to note 2. Estimate GFR from serum creatinine (MDRD) 3. Standard dipstick for urine protein – if negative 4. Spot urine albumin to creatinine ratio (ACR) 5. 24 hour urine collections are NOT needed. 6. Diabetics should be tested at least once a yr. 7. Others at risk to be tested once in 2 years www. drsarma. in 12
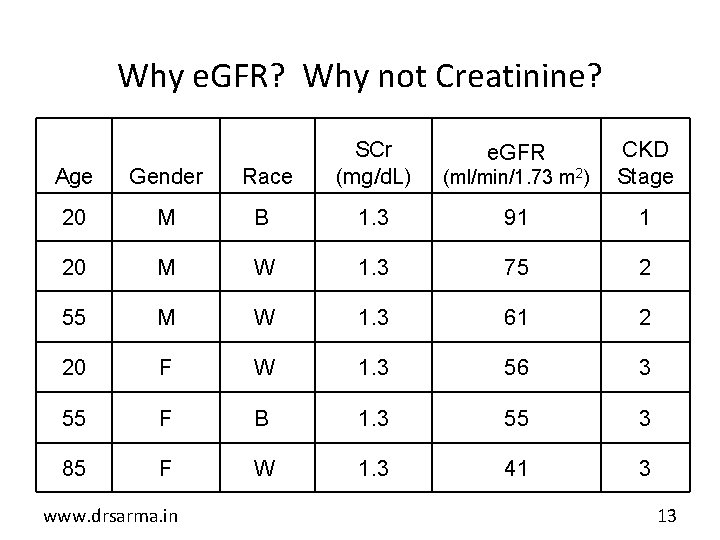
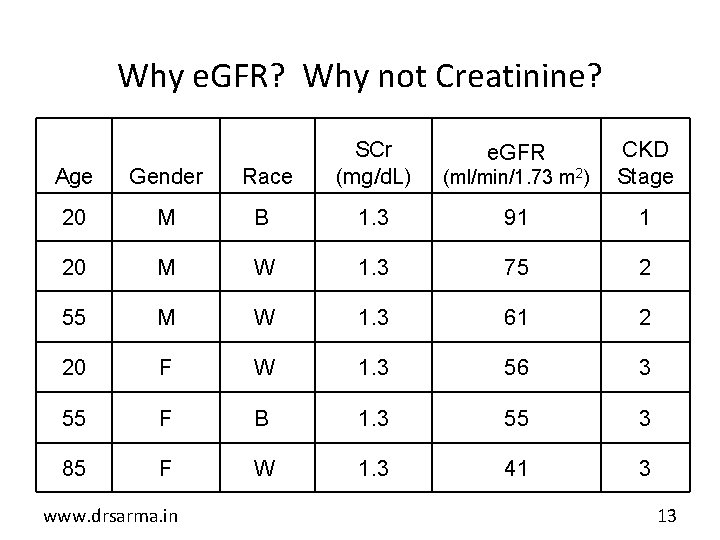
Why e. GFR? Why not Creatinine? Age Gender Race SCr (mg/d. L) 20 M B 1. 3 91 1 20 M W 1. 3 75 2 55 M W 1. 3 61 2 20 F W 1. 3 56 3 55 F B 1. 3 55 3 85 F W 1. 3 41 3 www. drsarma. in (ml/min/1. 73 m 2) CKD Stage e. GFR 13
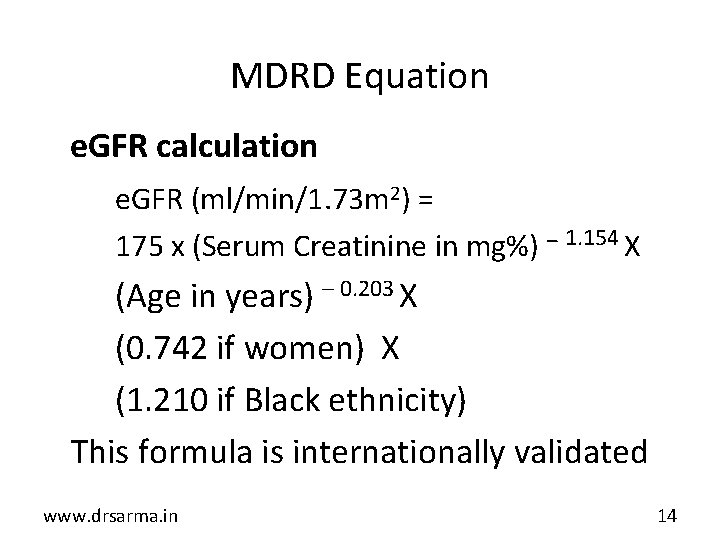
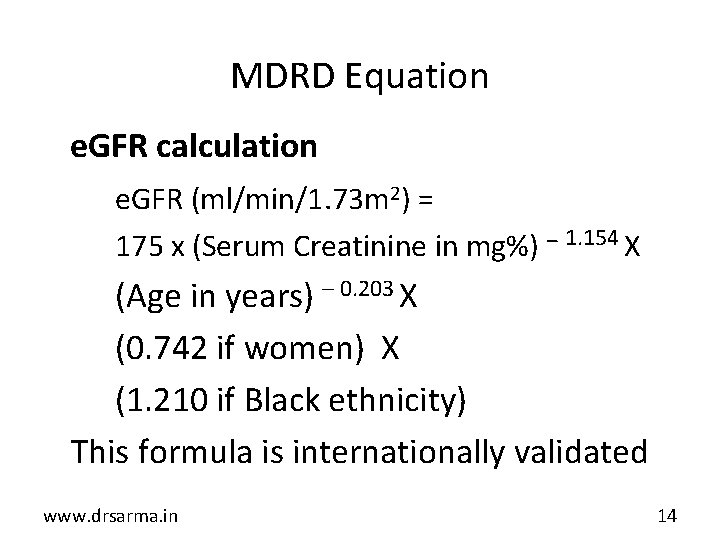
MDRD Equation e. GFR calculation e. GFR (ml/min/1. 73 m 2) = 175 x (Serum Creatinine in mg%) – 1. 154 X (Age in years) – 0. 203 X (0. 742 if women) X (1. 210 if Black ethnicity) This formula is internationally validated www. drsarma. in 14
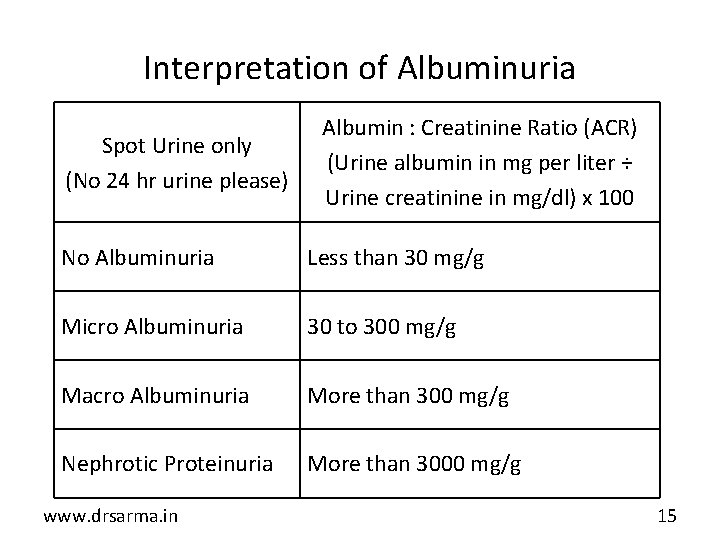
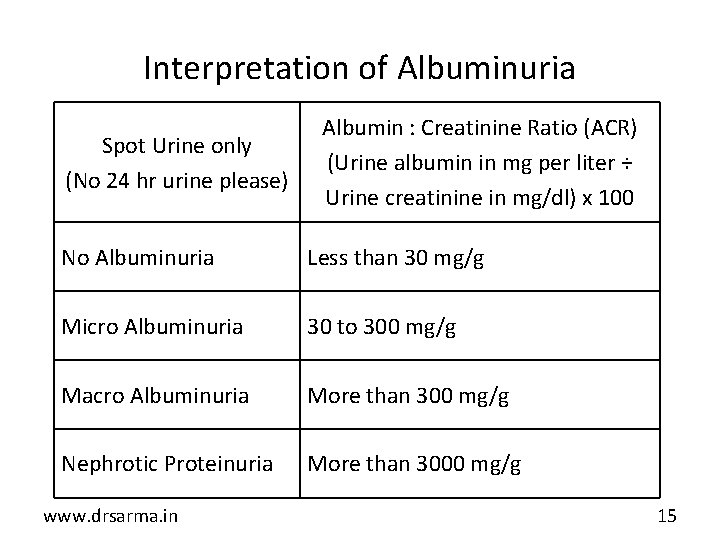
Interpretation of Albuminuria Spot Urine only (No 24 hr urine please) Albumin : Creatinine Ratio (ACR) (Urine albumin in mg per liter ÷ Urine creatinine in mg/dl) x 100 No Albuminuria Less than 30 mg/g Micro Albuminuria 30 to 300 mg/g Macro Albuminuria More than 300 mg/g Nephrotic Proteinuria More than 3000 mg/g www. drsarma. in 15
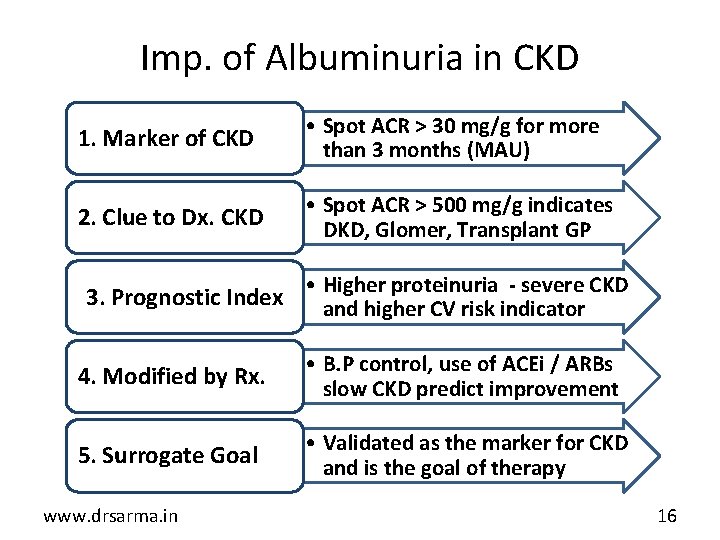
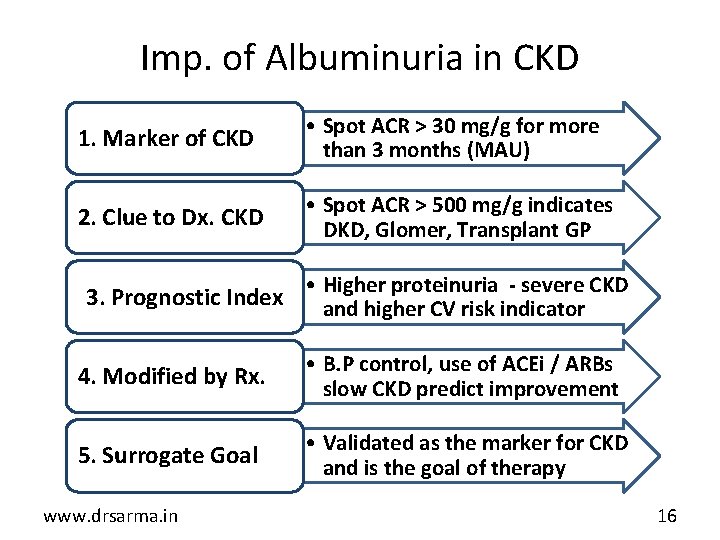
Imp. of Albuminuria in CKD 1. Marker of CKD • Spot ACR > 30 mg/g for more than 3 months (MAU) 2. Clue to Dx. CKD • Spot ACR > 500 mg/g indicates DKD, Glomer, Transplant GP • Higher proteinuria - severe CKD 3. Prognostic Index and higher CV risk indicator 4. Modified by Rx. • B. P control, use of ACEi / ARBs slow CKD predict improvement 5. Surrogate Goal • Validated as the marker for CKD and is the goal of therapy www. drsarma. in 16
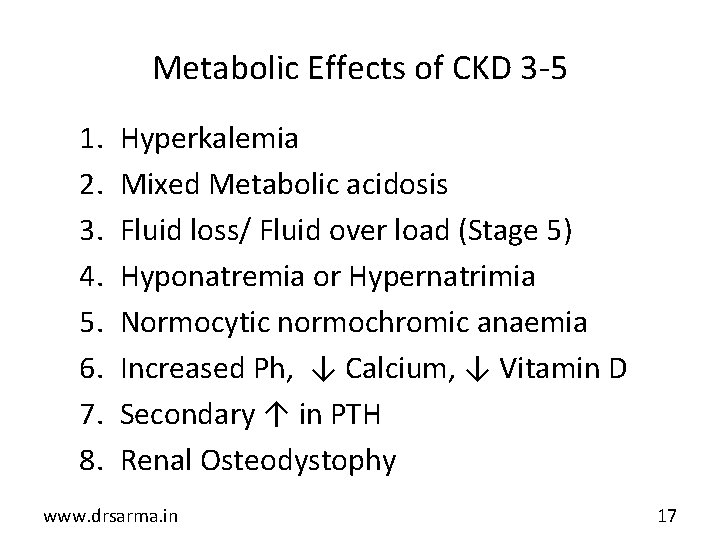
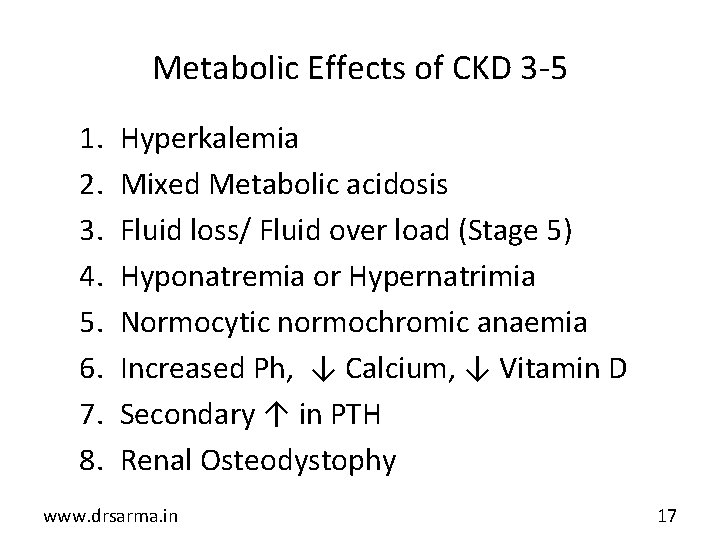
Metabolic Effects of CKD 3 -5 1. 2. 3. 4. 5. 6. 7. 8. Hyperkalemia Mixed Metabolic acidosis Fluid loss/ Fluid over load (Stage 5) Hyponatremia or Hypernatrimia Normocytic normochromic anaemia Increased Ph, ↓ Calcium, ↓ Vitamin D Secondary ↑ in PTH Renal Osteodystophy www. drsarma. in 17
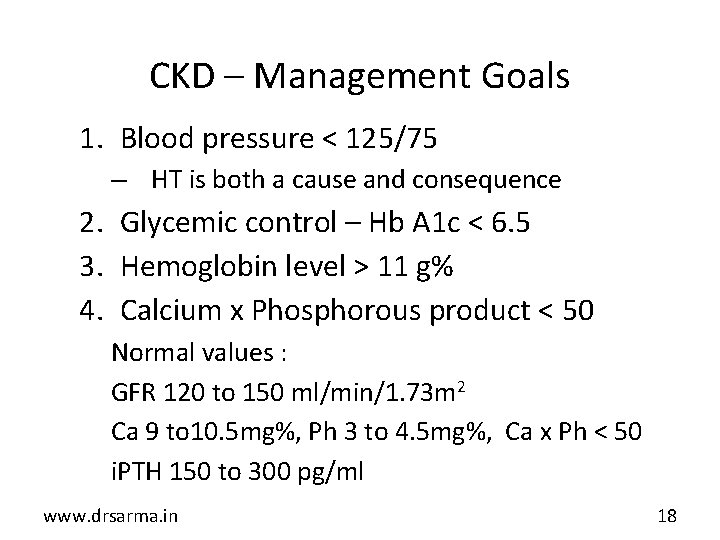
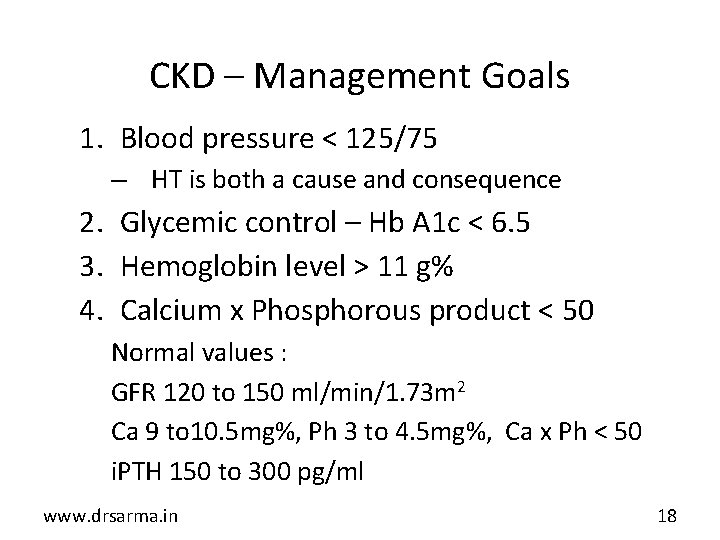
CKD – Management Goals 1. Blood pressure < 125/75 – HT is both a cause and consequence 2. Glycemic control – Hb A 1 c < 6. 5 3. Hemoglobin level > 11 g% 4. Calcium x Phosphorous product < 50 Normal values : GFR 120 to 150 ml/min/1. 73 m 2 Ca 9 to 10. 5 mg%, Ph 3 to 4. 5 mg%, Ca x Ph < 50 i. PTH 150 to 300 pg/ml www. drsarma. in 18
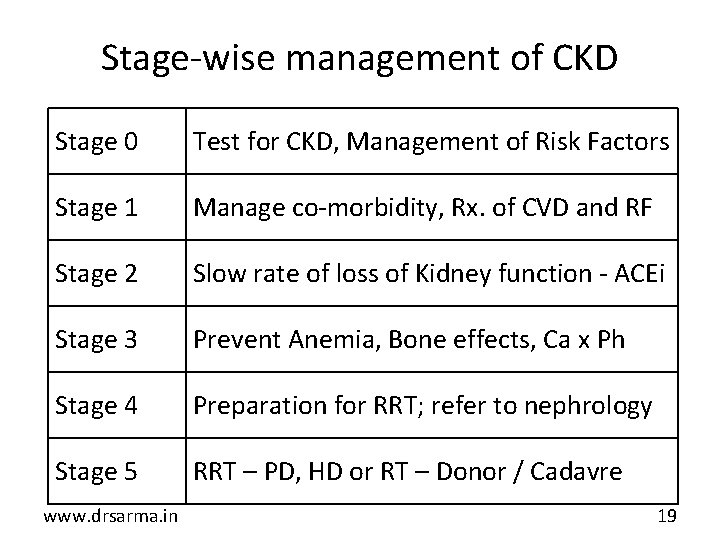
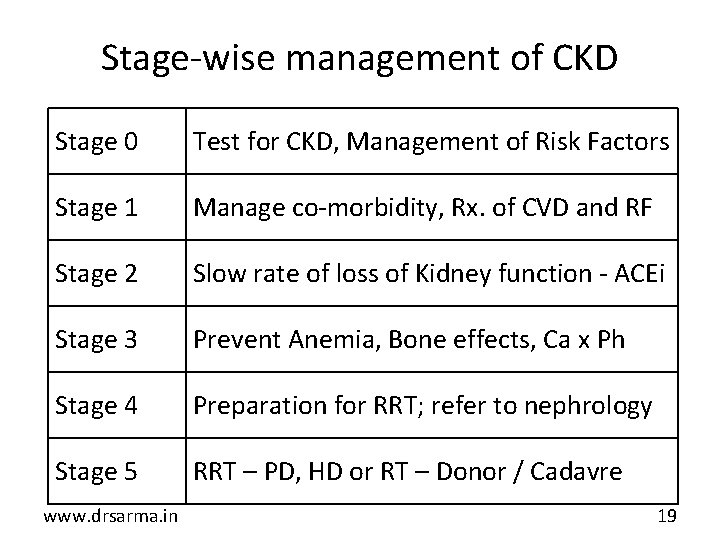
Stage-wise management of CKD Stage 0 Test for CKD, Management of Risk Factors Stage 1 Manage co-morbidity, Rx. of CVD and RF Stage 2 Slow rate of loss of Kidney function - ACEi Stage 3 Prevent Anemia, Bone effects, Ca x Ph Stage 4 Preparation for RRT; refer to nephrology Stage 5 RRT – PD, HD or RT – Donor / Cadavre www. drsarma. in 19
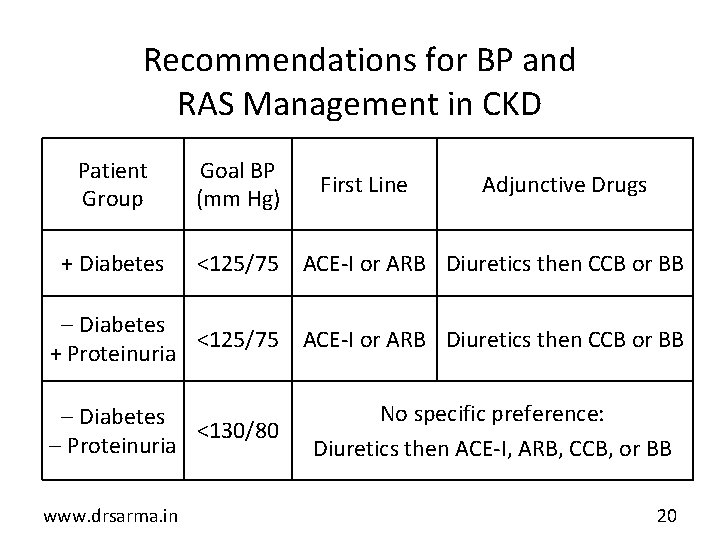
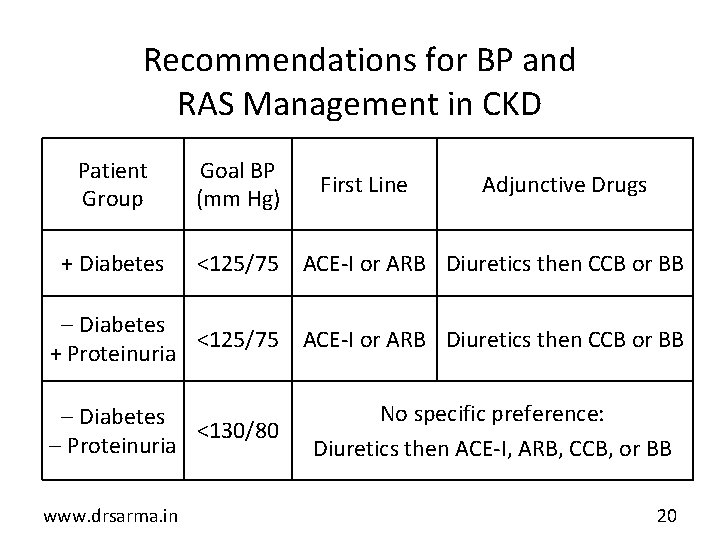
Recommendations for BP and RAS Management in CKD Patient Group + Diabetes Goal BP (mm Hg) First Line Adjunctive Drugs <125/75 ACE-I or ARB Diuretics then CCB or BB Diabetes <125/75 ACE-I or ARB Diuretics then CCB or BB + Proteinuria Diabetes <130/80 Proteinuria www. drsarma. in No specific preference: Diuretics then ACE-I, ARB, CCB, or BB © 2005 The Johns Hopkins University School of Medicine. 20
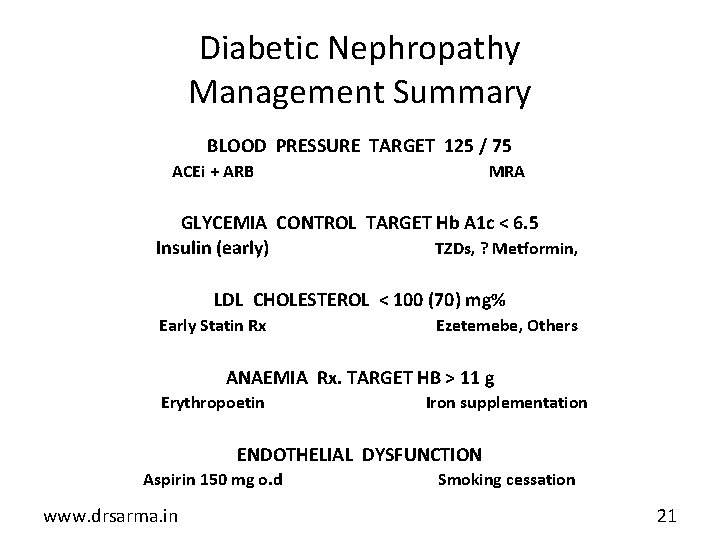
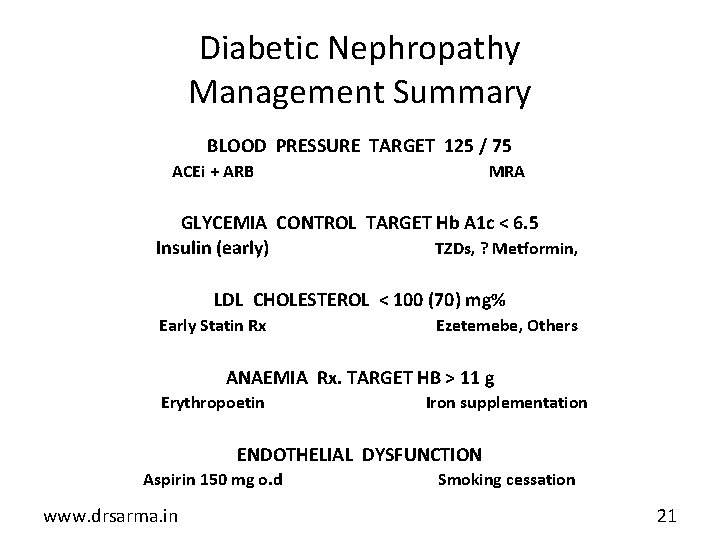
Diabetic Nephropathy Management Summary BLOOD PRESSURE TARGET 125 / 75 ACEi + ARB MRA GLYCEMIA CONTROL TARGET Hb A 1 c < 6. 5 TZDs, ? Metformin, Insulin (early) LDL CHOLESTEROL < 100 (70) mg% Early Statin Rx Ezetemebe, Others ANAEMIA Rx. TARGET HB > 11 g Erythropoetin Iron supplementation ENDOTHELIAL DYSFUNCTION Aspirin 150 mg o. d www. drsarma. in Smoking cessation 21
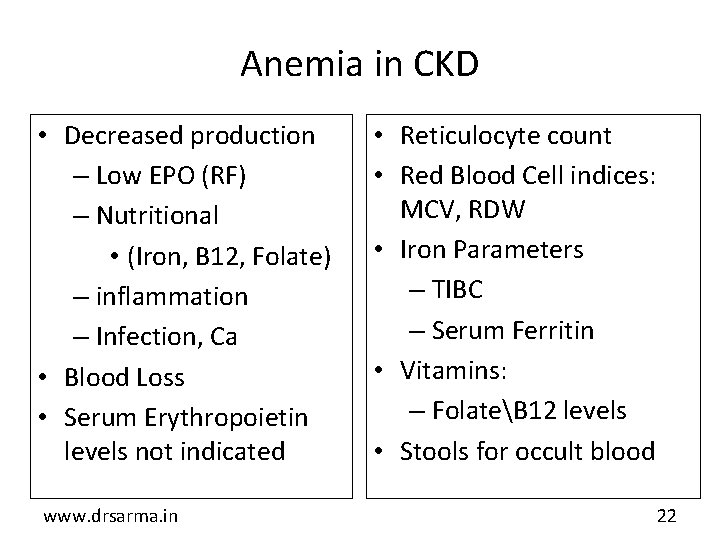
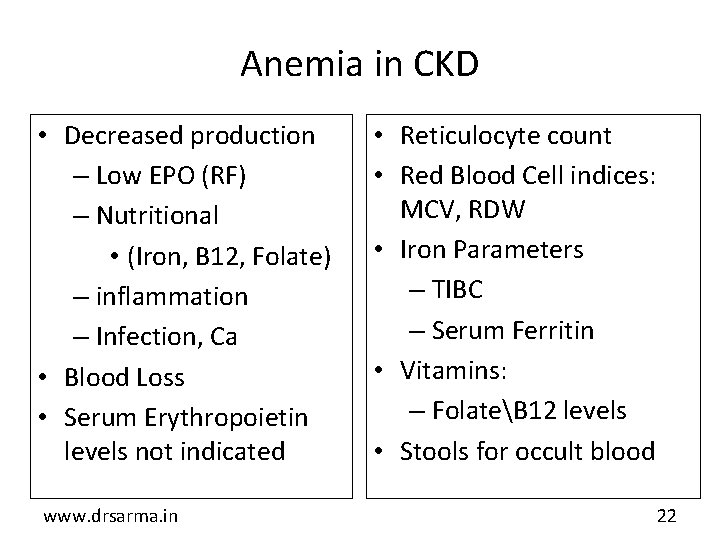
Anemia in CKD • Decreased production – Low EPO (RF) – Nutritional • (Iron, B 12, Folate) – inflammation – Infection, Ca • Blood Loss • Serum Erythropoietin levels not indicated www. drsarma. in • Reticulocyte count • Red Blood Cell indices: MCV, RDW • Iron Parameters – TIBC – Serum Ferritin • Vitamins: – FolateB 12 levels • Stools for occult blood 22
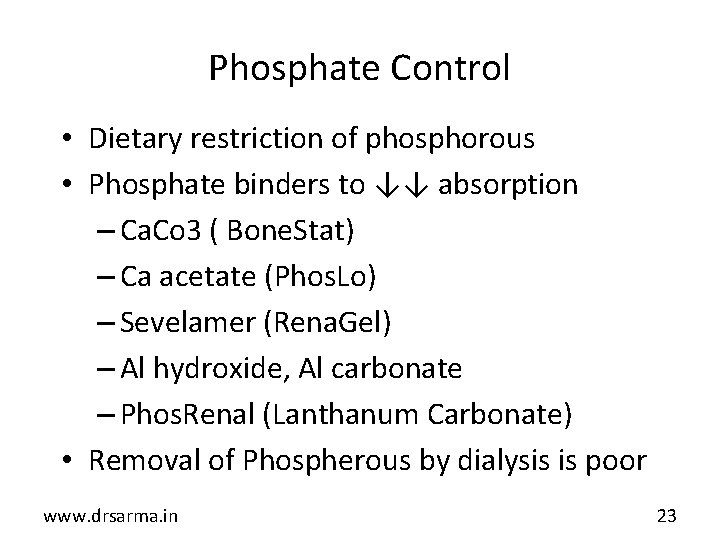
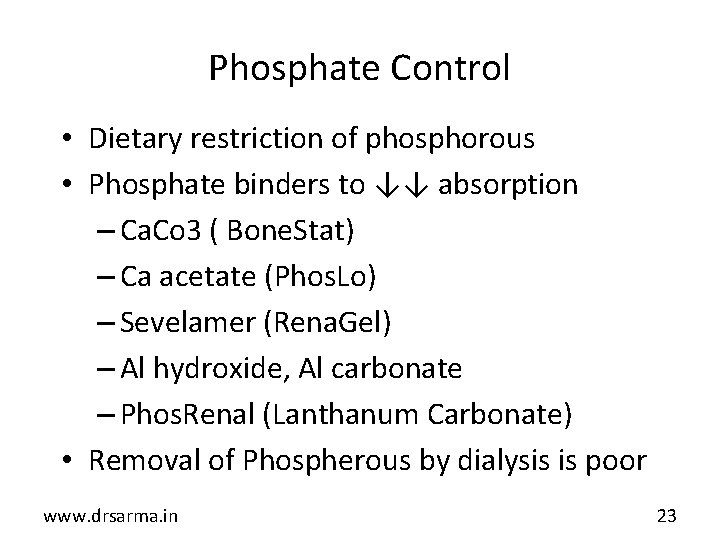
Phosphate Control • Dietary restriction of phosphorous • Phosphate binders to ↓↓ absorption – Ca. Co 3 ( Bone. Stat) – Ca acetate (Phos. Lo) – Sevelamer (Rena. Gel) – Al hydroxide, Al carbonate – Phos. Renal (Lanthanum Carbonate) • Removal of Phospherous by dialysis is poor www. drsarma. in 23
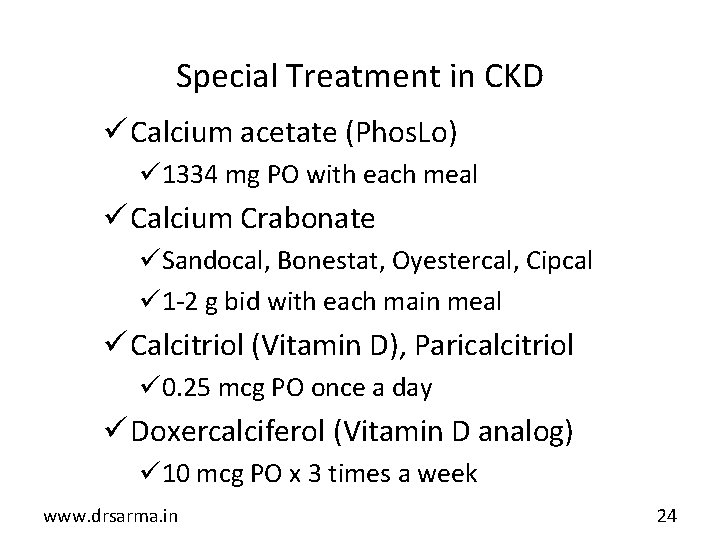
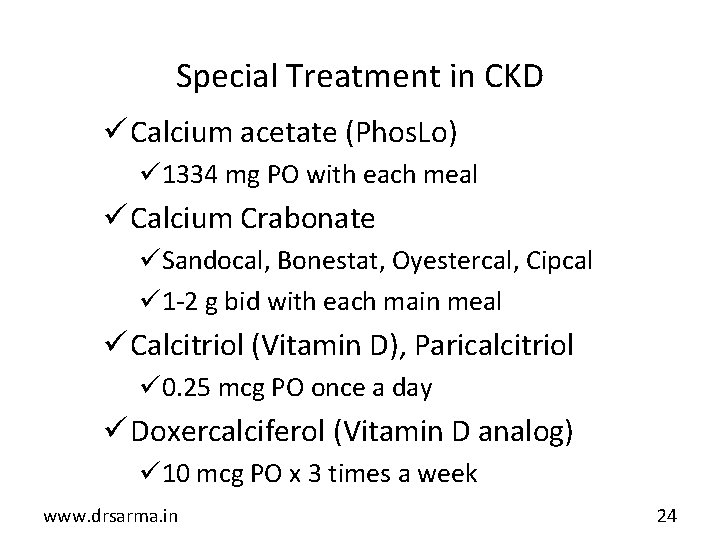
Special Treatment in CKD ü Calcium acetate (Phos. Lo) ü 1334 mg PO with each meal ü Calcium Crabonate üSandocal, Bonestat, Oyestercal, Cipcal ü 1 -2 g bid with each main meal ü Calcitriol (Vitamin D), Paricalcitriol ü 0. 25 mcg PO once a day ü Doxercalciferol (Vitamin D analog) ü 10 mcg PO x 3 times a week www. drsarma. in 24
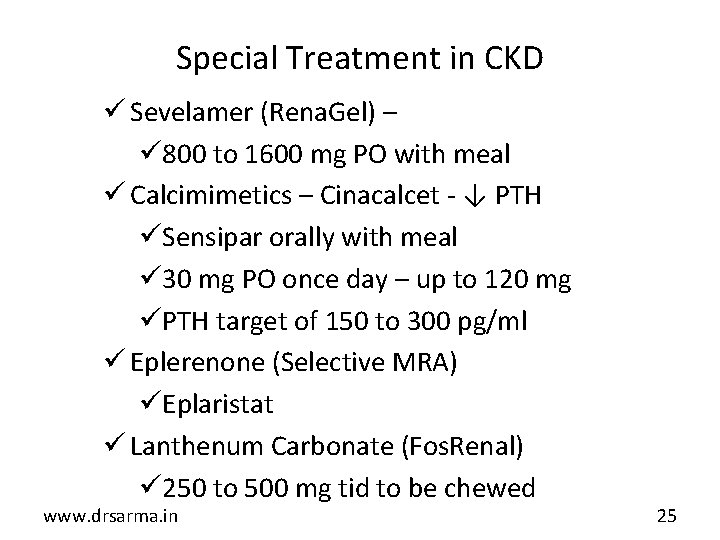
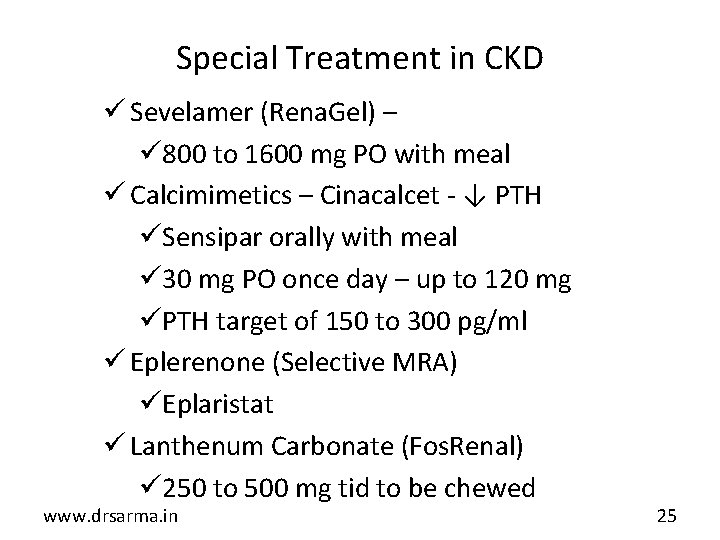
Special Treatment in CKD ü Sevelamer (Rena. Gel) – ü 800 to 1600 mg PO with meal ü Calcimimetics – Cinacalcet - ↓ PTH üSensipar orally with meal ü 30 mg PO once day – up to 120 mg üPTH target of 150 to 300 pg/ml ü Eplerenone (Selective MRA) üEplaristat ü Lanthenum Carbonate (Fos. Renal) ü 250 to 500 mg tid to be chewed www. drsarma. in 25
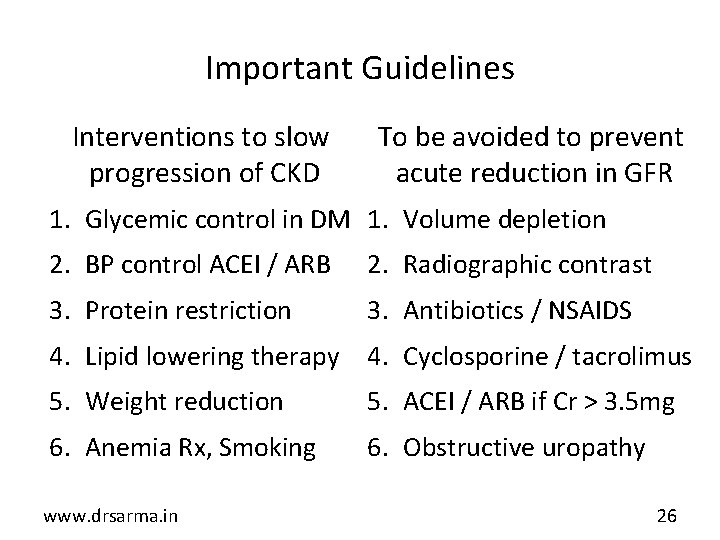
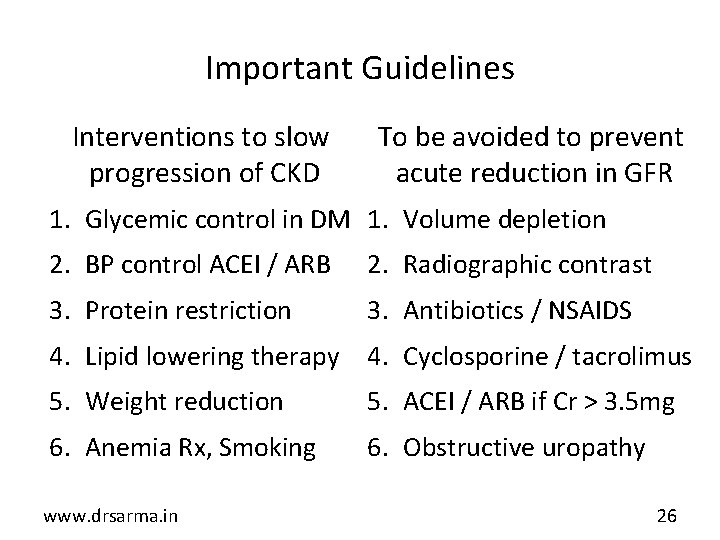
Important Guidelines Interventions to slow progression of CKD To be avoided to prevent acute reduction in GFR 1. Glycemic control in DM 1. Volume depletion 2. BP control ACEI / ARB 2. Radiographic contrast 3. Protein restriction 3. Antibiotics / NSAIDS 4. Lipid lowering therapy 4. Cyclosporine / tacrolimus 5. Weight reduction 5. ACEI / ARB if Cr > 3. 5 mg 6. Anemia Rx, Smoking 6. Obstructive uropathy www. drsarma. in 26
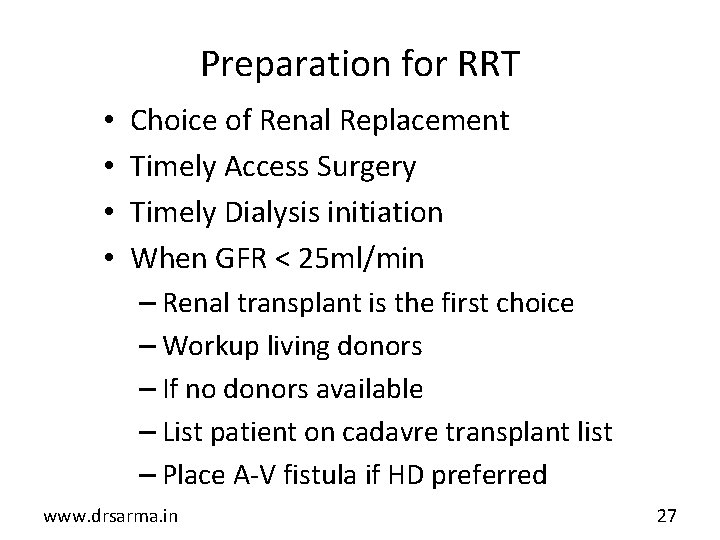
Preparation for RRT • • Choice of Renal Replacement Timely Access Surgery Timely Dialysis initiation When GFR < 25 ml/min – Renal transplant is the first choice – Workup living donors – If no donors available – List patient on cadavre transplant list – Place A-V fistula if HD preferred www. drsarma. in 27
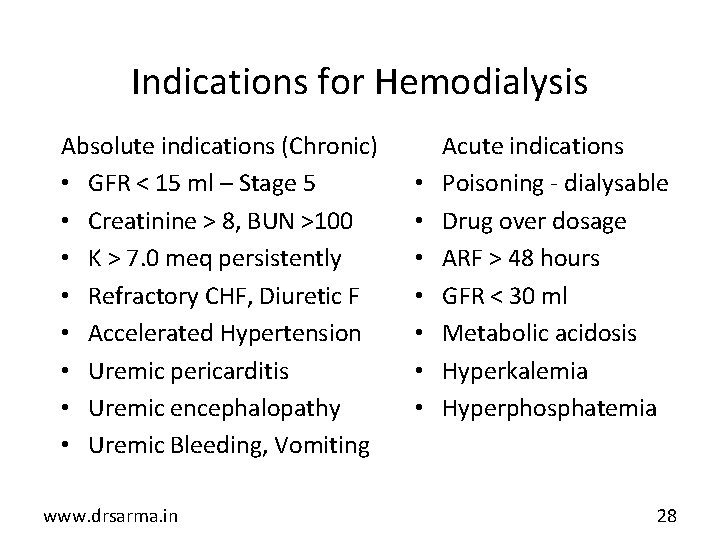
Indications for Hemodialysis Absolute indications (Chronic) • GFR < 15 ml – Stage 5 • Creatinine > 8, BUN >100 • K > 7. 0 meq persistently • Refractory CHF, Diuretic F • Accelerated Hypertension • Uremic pericarditis • Uremic encephalopathy • Uremic Bleeding, Vomiting www. drsarma. in • • Acute indications Poisoning - dialysable Drug over dosage ARF > 48 hours GFR < 30 ml Metabolic acidosis Hyperkalemia Hyperphosphatemia 28
Nephrotoxic Drugs • Which drug is (not) nephrotoxic? – Antibiotics • Aminiglycosides, Indinavir, Amphotericin • Penicillin / -lactums, Tetracyclines • Fluoroquinolones, Sulphas, Ketoconozole – NSAIDS/ COX 2 inhibitors, Indomethacin – Cancer: MTX, Cisplatin, Acyclovir, Pentamidine – Heavy metals: Hg, Pb, Ar, Bi, Lithium – IV Contrast dyes; ACE inhibitors / ARBS www. drsarma. in 29
Take Home Messages • CKD is a silent killer – we need to uncover it • CKD progression is preventable – Stage it and Rx. • DM most common cause of ESRD all over globe • CKD - more likely CV death than progress to ESRD • Multi-risk factor intervention is critical, Hb A 1 c goal • Lowering blood pressure with RAAS blockade • Combinations of ACEi + ARB ± MRA • Prevent cardiovascular morbidity and mortality www. drsarma. in 30