New YorkPresbyterianQueens PPS Town Hall Delivery System Reform
New. York-Presbyterian/Queens PPS Town Hall Delivery System Reform Incentive Payment (DSRIP) Program November 18, 2016
DSRIP Program Overview q Delivery System Reform Incentive Payment (DSRIP) Program • Health Transformation program being led by the NYS DOH q Goals of DSRIP: • Reduce avoidable hospitalizations & ED visits by 25% in 5 years • Improve access and utilization of primary care & preventative care services • Collaborate with community providers to improve care for patients
PPS Updates q PPS received AV (Achievement Value) Scorecard for DY 2, Q 1 from the IA in September 2016 q NYP/Q PPS has received all the AVs to date; only 32% of all the 25 PPSs in NYS accomplished this q Clinical Integration Strategy for the network developed q Population Health Roadmap completed for the entire network 3 NYPQ PPS PAC Meeting
PPS Updates q NYP/Queens PPS completed the NYSDOH Midpoint Assessment q The Mid-Point Assessment is a required component of the DSRIP Program for all PPSs q The Mid-Point Assessment focuses on the progress made by the PPSs through the end of the first quarter of DY 2 towards establishing the necessary organizational foundation and towards the implementation of the project requirements consistent with the approved DSRIP Project Plan. q Midpoint Assessment included: • Submission of project narratives • Primary Care Plan submission • 360 Partner Survey • Independent Assessor On Site Visit 4 NYPQ PPS PAC Meeting
PPS Updates Finance q All PPSs had to complete the Lead Financial Stability Test. q NYP/Queens PPS successfully completed the Financial Stability Test August, 2016. q NYP/Queens PPS is financially viable. q We have been distributing funds to partners bi-annually q To date, $458, 954. 13 have been distributed to the partners, which includes Community Based Organizations (CBOs). 5 NYPQ PPS PAC Meeting
PPS Updates Statewide Health Care Facility Transformation Program q A total of up to $195 million is available under this Request for Applications (RFA) to health care providers • A minimum of $30 million of this total amount is available for community-based health care providers • Priority given to projects that were not funded in whole or part, in response to the RFAs for the Capital Restructuring Financing Program (CRFP) q NYPQ grant submission: HIT Infrastructure project plan 6 NYP/Q PPS PAC Meeting
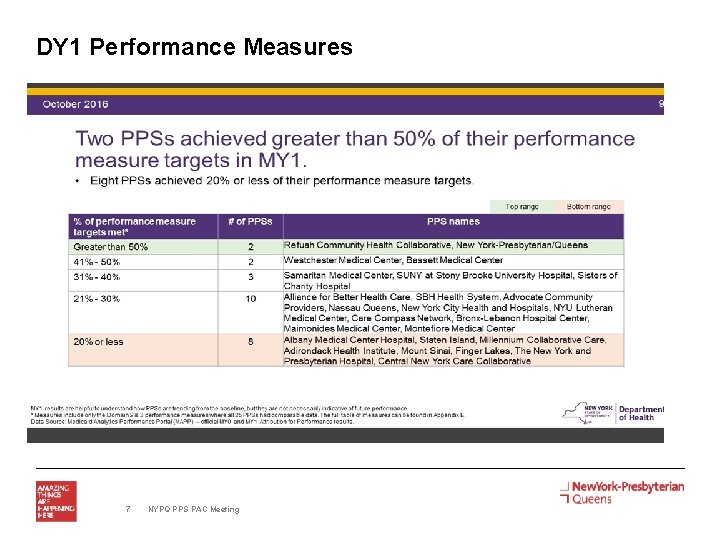
DY 1 Performance Measures 7 NYPQ PPS PAC Meeting
Value Based Payment (VBP) NYPQ PPS PAC Meeting 8
What is Value Based Payment (VBP)? q National healthcare strategy used by healthcare systems to promote quality and value of health care services, instead of fee for service payment methodologies focused to quality based outcomes. Goals include: § Shift from pure volume-based payment (Fee-for-Service) to those that are outcome related § Implement pay for performance programs that reward improvements in quality metrics & aligns risks of all parties § Establish methodologies that align with the complexity of the patient base as well as the offerings of the system with the strategies of the managed care organization § Engage multiple facets of the healthcare system to encourage quality based outcomes by assigning levels of risk § Establish data reporting & warehousing mechanisms for tracking and ongoing performance reporting 9 2016 V. B. P. Survey
Governing Process q The VBP baseline assessment was completed by the Project Management Office with reviews and approvals for publishing by the Finance Committee as well as the Executive Committee. q Approvals of this assessment completed in October 2016. 10 Presentation Title
Survey Categories q Organization Type q Current Value/Equity Payment Arrangements q VBP. Model Preferences q Current VBP. Aligned Medicaid Managed Care Organization (M. C. O. ) Strategies q Readiness to convert 90% of Medicaid revenue sources to a V. B. P. methodology q Training Topic Interest Areas 11 2016 V. B. P. Survey
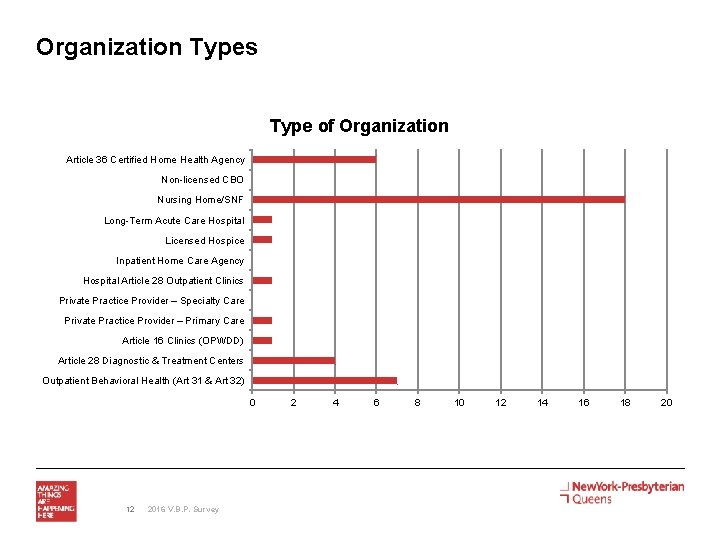
Organization Types Type of Organization Article 36 Certified Home Health Agency Non-licensed CBO Nursing Home/SNF Long-Term Acute Care Hospital Licensed Hospice Inpatient Home Care Agency Hospital Article 28 Outpatient Clinics Private Practice Provider – Specialty Care Private Practice Provider – Primary Care Article 16 Clinics (OPWDD) Article 28 Diagnostic & Treatment Centers Outpatient Behavioral Health (Art 31 & Art 32) 0 12 2016 V. B. P. Survey 2 4 6 8 10 12 14 16 18 20
Results q All network partners were surveyed q (35) unique partners provided responses q (40) organization types reported q Nursing Homes/Skilled Nursing Facilities represented 45% of the total responses q 34% of the partners reporting population indicated, YES, to current value/equity payment arrangements q 85% of the partners indicated NO preference to any specific VBP. model q 37% Unsure, 34% Slightly confident, 25% Confident for readiness to convert 90% of Medicaid revenue sources to a VBP methodology 13 2016 V. B. P. Survey
Next Steps/Opportunities q Education of unique types of VBP arrangements in the local market q Alignment of education with the findings from the Rapid Cycle Evaluation Unit q Engagement with MCO’s for discussions of concepts that align with population strategies q Incorporation of multiple provider / payer strategies by network partners q Lessons learned among network partners for VBP arrangements q Provide basic education models for partner network q Partner with Medicaid MCO’s to roll-out any existing educational programs for VBP q Utilize Rapid Cycle Evaluation Unit quality analysis to provide partners baseline quality assessments 14 NYPQ PPS PAC Meeting
Palliative Care Integration Into Nursing Homes: A DSRIP Model Cynthia X Pan, MD, FACP, AGSF NYP/Q PPS Palliative Care Project Chair Associate Professor of Clinical Medicine, Weill Cornell Medical College November 2016
What is Palliative Care? 緩和醫療 § Palliative care is specialized medical care for people with serious illnesses. § Patient and Family focused § Palliative care is provided by a team of doctors, nurses, and other specialists who work with a patient's other doctors to provide an extra layer of support. § Palliative care is appropriate at any age and at any stage in a serious illness, and can be provided together with curative treatment. 16
It takes Courage and Kindness to discuss palliative care and EOL care
DSRIP Project Review: PIP Requirement Development Integrate Palliative Care into practice model of participating Nursing Homes. Develop partnerships with community and provider resources, including Hospice, to bring the palliative care supports and services into the nursing home. Develop and adopt clinical guidelines agreed to by all partners including services and eligibility. Engage staff in trainings to increase role- appropriate competence in palliative care skills and protocols developed by the PPS. Engage with Medicaid Managed Care to address coverage of services. Use EHRs or other IT platforms to track all patients engaged in this project. 18
What challenges are we facing in the field of palliative care? § Misconceptions about palliative care § Misconceptions about morphine and pain management § Limited availability of palliative care in the outpatient and LTC setting § Limited access and penetration in minority groups § Understanding what aspects of palliative care effective § Not enough trained palliative physicians or clinicians § Levels of palliative care - Primary palliative care vs Secondary vs Tertiary 19
Trigger Case: Mrs. R § Mrs. R is a 72 yr old woman residing in the NH. She has ALS, Sjogren’s syndrome, sarcoid, respiratory failure, vent/trach, PEG. She is a retired HHA. § She has husband daughter who are involved. Dtr is her proxy. § Mrs. R transferred to ED recently for bleeding around PEG site § Pt able to communicate with Speech therapy and I-Link chart § Pt suffering from anxiety § A palliative care consult was called. § Daughter asked: “What is palliative care? ” 20
Question: What is the most appropriate definition of Palliative Care? § A) Care for patients at the end of life § B) Comfort care § C) Care for patients with serious illness § D) Care for patients who need hospice services 21
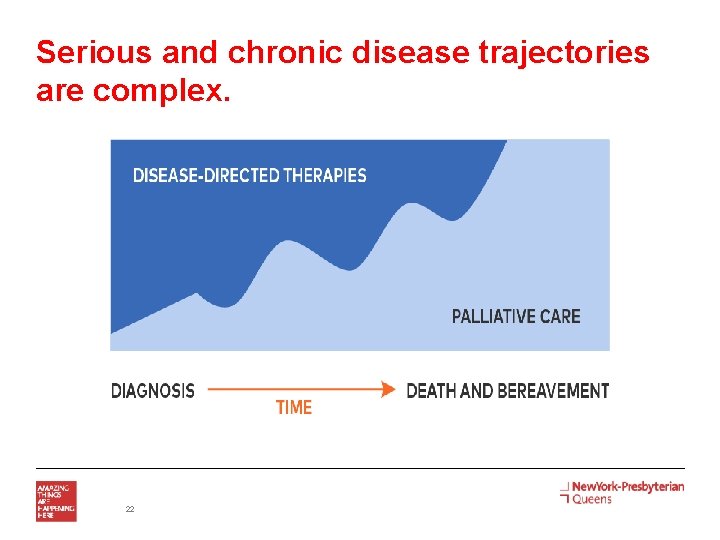
Serious and chronic disease trajectories are complex. 22
What Do Palliative Care Teams Do? § Relieve - Symptoms - Distress- emotional, spiritual, practical; patients AND families - Uncertainty § Communicate/Support/GOC - What to expect - Treatments that match person+family goals § Coordinate - Medical and practical needs across settings Ref: Weissman, DE: Consultation in Palliative Medicine. Archives in Internal Medicine 1997 23
Palliative care leads to positive outcomes Improves quality of life scores Reduces symptom burden Improves satisfaction with care Reduces overall healthcare costs Increases survival Refs: Bakitas et al, JAMA 2009; Rabow et al, Arch Int Med 2004; Rabow et al, JPSM 2003 24
Integrate Palliative Care into practice model of participating Nursing Homes § Palliative Care Champions § Interdisciplinary Team work § EPEC (Education on Palliative and End-of-Life Care) - Every 2 months - Rotating partner sites to host - Started in Feb 2016 25
EPEC (Education on Palliative and End-of-Life Care) § Gaps in End-of-life Care § PAS and Dignity in Dying § Legal Issues § Depression, Anxiety, Delirium § Elements & Models of End-of-life care § Goals of Care § Advanced Care Planning § Communicating Bad News § Whole Patient Assessment § Pain Management 26 § Sudden Illness § Medical Futility § Common Physical Symptoms § Last Hours of Living § Training of Trainers
EPEC Training Feedback § 66 participants completed the survey, of which - 100% reported that the program accomplished the stated objectives. - 98% reported that the program provided with new information that is pertinent to their practice and patient care. § Some Responses to the question “What did you like most about the program? ” - Practical example help solidify the information - Dr. Pan’s sharing of real experience 27 NYPQ PPS PAC Meeting
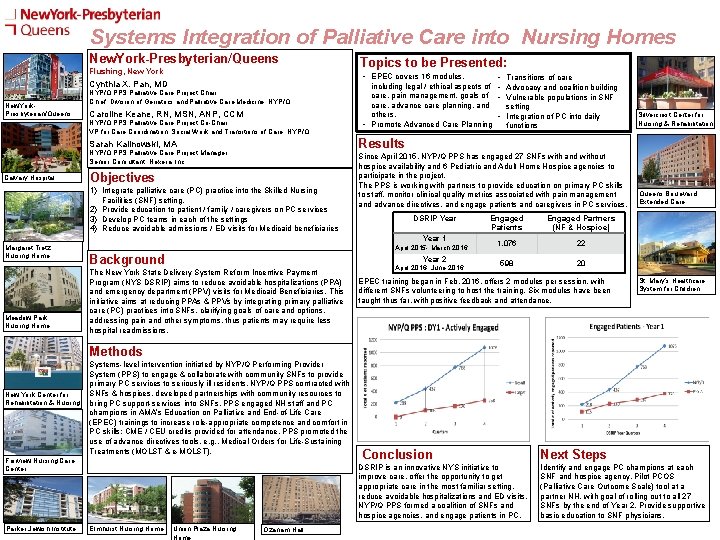
Systems Integration of Palliative Care into Nursing Homes New. York-Presbyterian/Queens Flushing, New York • EPEC covers 16 modules, Cynthia X. Pan, MD New. York. Presbyterian/Queens NYP/Q PPS Palliative Care Project Chair Chief, Division of Geriatrics and Palliative Care Medicine, NYP/Q Caroline Keane, RN, MSN, ANP, CCM NYP/Q PPS Palliative Care Project Co-Chair VP for Care Coordination, Social Work and Transitions of Care, NYP/Q PPS Palliative Care Project Manager Senior Consultant, Nexera, Inc. Objectives 1) Integrate palliative care (PC) practice into the Skilled Nursing Facilities (SNF) setting. 2) Provide education to patient / family / caregivers on PC services 3) Develop PC teams in each of the settings 4) Reduce avoidable admissions / ED visits for Medicaid beneficiaries Margaret Tietz Nursing Home Meadow Park Nursing Home • Transitions of care including legal / ethical aspects of • Advocacy and coalition building care, pain management, goals of • Vulnerable populations in SNF care, advance care planning, and setting others. • Integration of PC into daily • Promote Advanced Care Planning functions Silvercrest Center for Nursing & Rehabilitation Results Sarah Kalinowski, MA Calvary Hospital Topics to be Presented: Since April 2015, NYP/Q PPS has engaged 27 SNFs with and without hospice availability and 6 Pediatric and Adult Home Hospice agencies to participate in the project. The PPS is working with partners to provide education on primary PC skills to staff, monitor clinical quality metrics associated with pain management and advance directives, and engage patients and caregivers in PC services. DSRIP Year Engaged Partners Patients (NF & Hospice) Year 1 1, 076 22 Queens Boulevard Extended Care April 2015 - March 2016 Background Year 2 The New York State Delivery System Reform Incentive Payment Program (NYS DSRIP) aims to reduce avoidable hospitalizations (PPA) and emergency department (PPV) visits for Medicaid Beneficiaries. This initiative aims at reducing PPAs & PPVs by integrating primary palliative care (PC) practices into SNFs, clarifying goals of care and options, addressing pain and other symptoms, thus patients may require less hospital readmissions. April 2016 - June 2016 598 20 EPEC training began in Feb. 2016, offers 2 modules per session, with different SNFs volunteering to host the training. Six modules have been taught thus far, with positive feedback and attendance. St. Mary’s Healthcare System for Children Methods New York Center for Rehabilitation & Nursing Systems-level intervention initiated by NYP/Q Performing Provider System (PPS) to engage & collaborate with community SNFs to provide primary PC services to seriously ill residents. NYP/Q PPS contracted with SNFs & hospices, developed partnerships with community resources to bring PC support-services into SNFs. PPS engaged NH staff and PC champions in AMA’s Education on Palliative and End-of-Life Care (EPEC) trainings to increase role-appropriate competence and comfort in PC skills; CME / CEU credits provided for attendance. PPS promoted the use of advance directives tools, e. g. , Medical Orders for Life-Sustaining Treatments (MOLST & e-MOLST). Fairview Nursing Care Center Parker Jewish Institute Elmhurst Nursing Home Union Plaza Nursing Home Ozanam Hall Conclusion Next Steps DSRIP is an innovative NYS initiative to improve care, offer the opportunity to get appropriate care in the most familiar setting, reduce avoidable hospitalizations and ED visits. NYP/Q PPS formed a coalition of SNFs and hospice agencies, and engage patients in PC. Identify and engage PC champions at each SNF and hospice agency. Pilot PCOS (Palliative Care Outcome Scale) tool at a partner NH, with goal of rolling out to all 27 SNFs by the end of Year 2. Provide supportive basic education to SNF physicians.
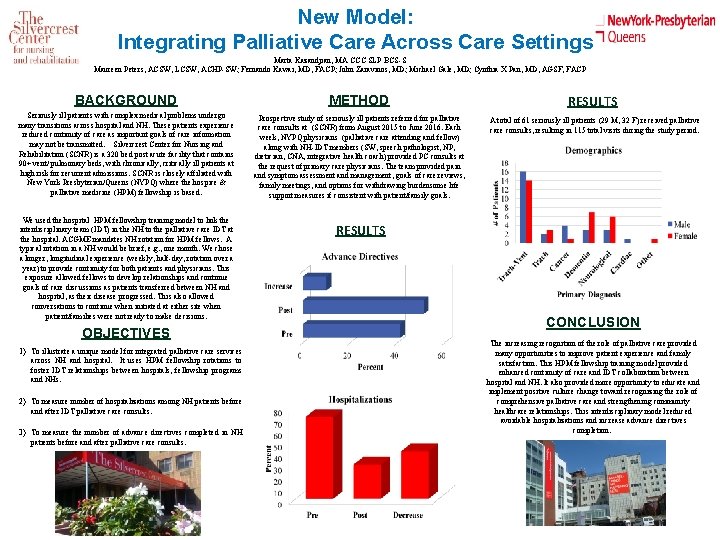
New Model: Integrating Palliative Care Across Care Settings Marta Kazandjian, MA CCC SLP BCS-S Maureen Peters, ACSW, LCSW, ACHP-SW; Fernando Kawai, MD, FACP; John Zaravinos, MD; Michael Gale, MD; Cynthia X Pan, MD, AGSF, FACP BACKGROUND METHOD Seriously ill patients with complex medical problems undergo many transitions across hospital and NH. These patients experience reduced continuity of care as important goals of care information may not be transmitted. Silvercrest Center for Nursing and Rehabilitation (SCNR) is a 320 bed post acute facility that contains 90+ vent/ pulmonary beds, with chronically, critically ill patients at high risk for recurrent admissions. SCNR is closely affiliated with New York Presbyterian/Queens (NYPQ) where the hospice & palliative medicine (HPM) fellowship is based. Prospective study of seriously ill patients referred for palliative care consults at (SCNR) from August 2015 to June 2016. Each week, NYPQ physicians (palliative care attending and fellow) along with NH-IDT members (SW, speech pathologist, NP, dietician, CNA, integrative health coach) provided PC consults at the request of primary care physicians. The team provided pain and symptom assessment and management, goals of care reviews, family meetings, and options for withdrawing burdensome life support measures if consistent with patient/family goals. We used the hospital HPM fellowship training model to link the interdisciplinary team (IDT) in the NH to the palliative care IDT at the hospital. ACGME mandates NH rotation for HPM fellows. A typical rotation in a NH would be brief, e. g. , one month. We chose a longer, longitudinal experience (weekly, half-day, rotation over a year) to provide continuity for both patients and physicians. This exposure allowed fellows to develop relationships and continue goals of care discussions as patients transferred between NH and hospital, as their disease progressed. This also allowed conversations to continue when initiated at either site when patient/families were not ready to make decisions. OBJECTIVES 1) To illustrate a unique model for integrated palliative care services across NH and hospital. It uses HPM fellowship rotations to foster IDT relationships between hospitals, fellowship programs and NHs. 2) To measure number of hospitalizations among NH patients before and after IDT palliative care consults. 3) To measure the number of advance directives completed in NH patients before and after palliative care consults. RESULTS A total of 61 seriously ill patients (29 M, 32 F) received palliative care consults, resulting in 115 total visits during the study period. RESULTS CONCLUSION The increasing recognition of the role of palliative care provided many opportunities to improve patient experience and family satisfaction. This HPM fellowship training model provided enhanced continuity of care and IDT collaboration between hospital and NH. It also provided more opportunity to educate and implement positive culture change toward recognizing the role of comprehensive palliative care and strengthening community healthcare relationships. This interdisciplinary model reduced avoidable hospitalizations and increase advance directives completion.
Criteria for a Palliative Care Assessment at the Time of Hospital Admission… § A potentially life-limiting or life-threatening condition and. . . § Primary Criteria - The ‘‘surprise question’’: You would not be surprised if the patient died within 12 months - Frequent admissions (e. g. , more than one admission for same condition within several months) - Admission prompted by difficult-to-control physical or psychological symptoms (e. g. , moderate-to-severe symptom intensity for more than 24– 48 hours) - Complex care requirements (e. g. , functional dependency; complex home support for ventilator/antibiotics/feedings) - Decline in function, feeding intolerance, or unintended decline in weight (e. g. , failure to thrive) Weissman, DE: Consultation in Palliative Medicine. Archives in 30 Internal Medicine 1997
…Criteria for a Palliative Care Assessment at the Time of Admission § Secondary Criteria - Admission from long-term care facility or medical foster home - Elderly patient, cognitively impaired, with acute hip fracture - Metastatic or locally advanced incurable cancer - Chronic home oxygen use - Out-of-hospital cardiac arrest - Current or past hospice program enrollee - Limited social support (e. g. , family stress, chronic mental illness) - No history of completing an advance care planning discussion/document 31
What’s Next? . . . § Ongoing education to gain competencies - CAPC membership for DSRIP members § Online modules for all disciplines, with CME and CEUs - Ongoing education with community partners, such as hospice and home care agencies § Active participation and feedback in DSRIP measurement tools § E. g. PCOS – to fit NH patients’ needs § Needs Assessment - Check in – how are we doing at end of Year 1? 32
…What’s Next? § Set standards for national NH /LTC care model for palliative care - E. g. Dr Unroe (Indiana Univ. )- describe palliative care services in LTC - Advocate for value based payment models in LTC § Data Measurement § What should be screening criteria for palliative care in LTC? - Can we use MDS data? § What are important outcomes? - # of days spent at Home (NH) in last year of life § Advocate for system change - DOH NYS; CMS – Dr Patrick Conway - Quadruple Aim 33
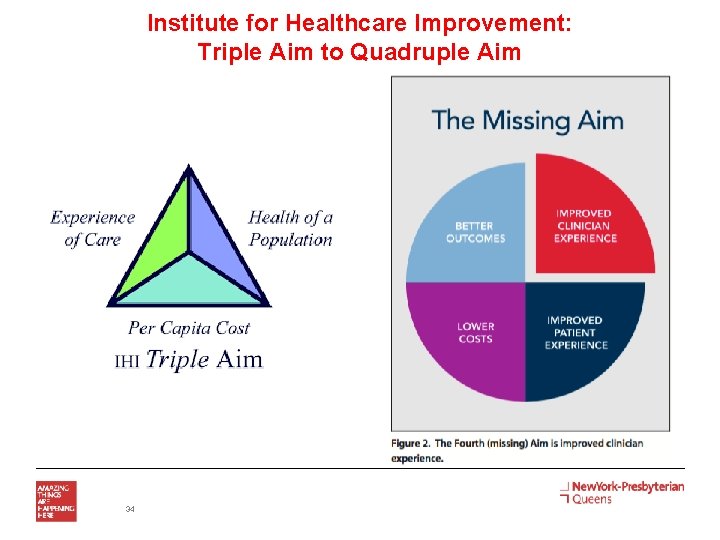
Institute for Healthcare Improvement: Triple Aim to Quadruple Aim 34
35
Useful Resources/Sites § www. capc. org Center to Advance Palliative Care - Technical assistance, tool kits, education modules § www. getpalliativecare. org - Info for pts/families, clinicians, policy makers § www. compassionandsupport. org - Info for caregivers/families, and professionals § www. vitaltalk. org - Communication training § http: //www. mypcnow. org/fast-facts - Fast Facts for learning on the go 36
Questions? Cynthia X Pan, MD cxp 9001@nyp. org Thank You 37
Rapid Cycle Process Improvement Small Interventions, Large Benefit November 2016
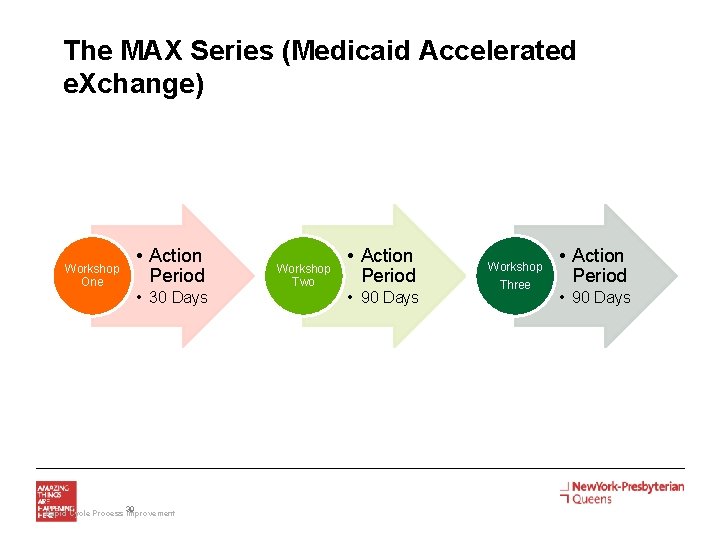
The MAX Series (Medicaid Accelerated e. Xchange) Workshop One • Action Period • 30 Days 39 Rapid Cycle Process Improvement Workshop Two • Action Period • 90 Days Workshop Three • Action Period • 90 Days
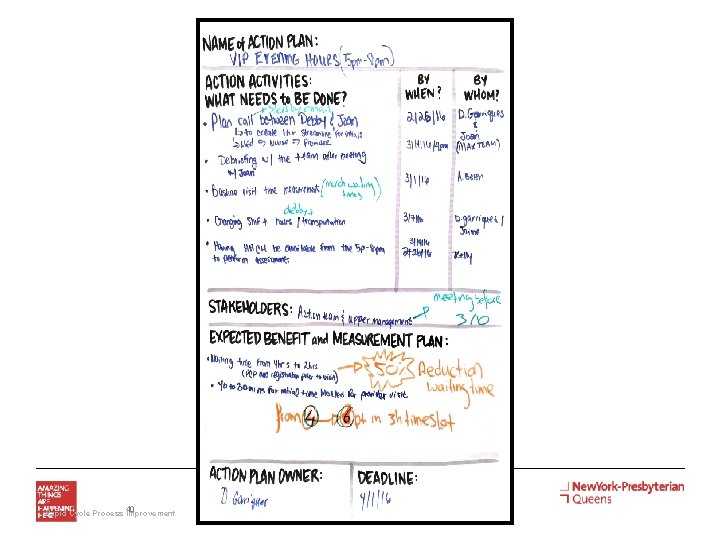
40 Rapid Cycle Process Improvement
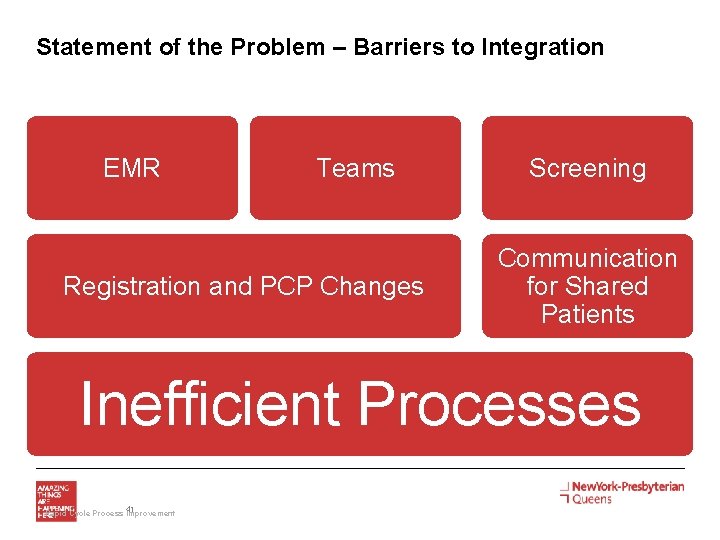
Statement of the Problem – Barriers to Integration EMR Teams Registration and PCP Changes Screening Communication for Shared Patients Inefficient Processes 41 Rapid Cycle Process Improvement
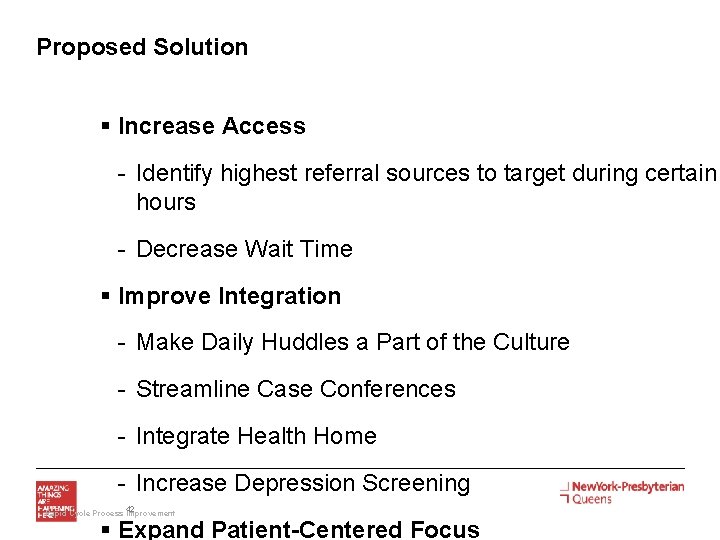
Proposed Solution § Increase Access - Identify highest referral sources to target during certain hours - Decrease Wait Time § Improve Integration - Make Daily Huddles a Part of the Culture - Streamline Case Conferences - Integrate Health Home - Increase Depression Screening 42 Rapid Cycle Process Improvement § Expand Patient-Centered Focus
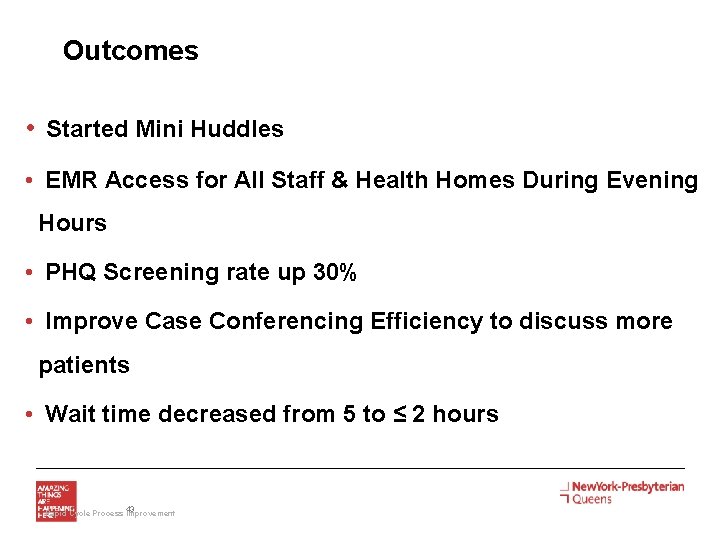
Outcomes • Started Mini Huddles • EMR Access for All Staff & Health Homes During Evening Hours • PHQ Screening rate up 30% • Improve Case Conferencing Efficiency to discuss more patients • Wait time decreased from 5 to ≤ 2 hours 43 Rapid Cycle Process Improvement
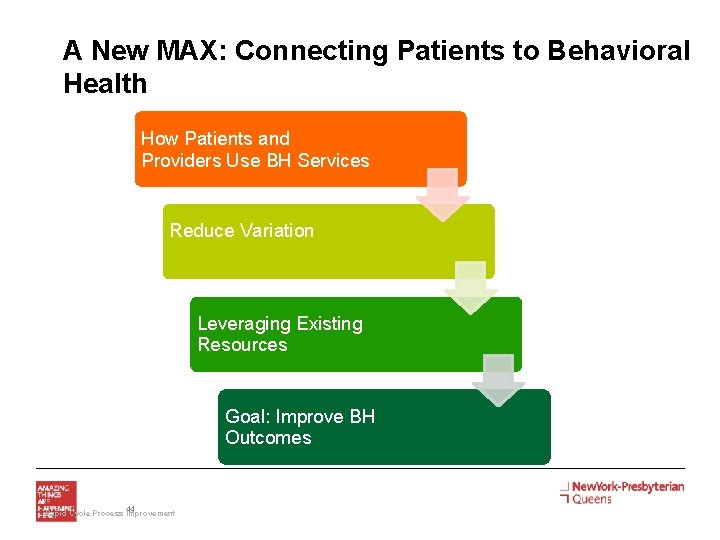
A New MAX: Connecting Patients to Behavioral Health How Patients and Providers Use BH Services Reduce Variation Leveraging Existing Resources Goal: Improve BH Outcomes 44 Rapid Cycle Process Improvement
Questions? 45 Rapid Cycle Process Improvement
46
Contact Us! PPS Website: http: //www. nyp. org/queens/dsrippps PMO Office: 718 -670 -1968 Executive Leadership: PMO Staff: • Maureen Buglino, RN, MPH • Sadia Choudhury Executive lead, DSRIP Director Vice President, Community Medicine sac 9139@nyp. org Co-Executive Lead, DSRIP Program cod 934@nyp. org • Kimberly Fung mabuglin@nyp. org • Maria D’Urso, RN, MSN • Coleen Dunkley • Sarah Kalinowski Project Manager, Operations Data Analyst kif 9020@nyp. org Administrative Director, Community sak 9034@nyp. org Medicine • Daniel Notarnicola mda 9005@nyp. org • Amanda Simmons Financial Analyst Project Manager, Finance dan 9032@nyp. org ams 9135@nyp. org 47
- Slides: 47