Diseases of Pericardium Seoul National University Hospital Department
- Slides: 30
Diseases of Pericardium Seoul National University Hospital Department of Thoracic & Cardiovascular Surgery
Pericardium ØAnatomy • The pericardial sac is composed of the fibrous and the serous pericardium • Fibrous pericardium is the tough external fibroelastic outermost layer of the pericardium & the inner layer, serous pericardium, is the smooth mesothelial layer • The inner layer pericardium consists of outer parietal and inner visceral layer • Outer parietal layer sits on the inner aspects of fibrous pericardium and the inner visceral layer of serous pericardium is the mesothelial component of epicardium • Epicardium consists of an inner fibroelastic connective tissue layer & outer superficial mesothelial membrane
Pericardium ØDevelopmental anatomy • During embryologic development, heart invaginates into the serous pericardium and is coated by the inner visceral layer of serous pericardium • At the roots of great vessels, the investing inner visceral layer of serous pericardium is continuous with the outer parietal layer of serous pericardium • The potential space between the outer parietal layer of serous pericardium and the inner visceral layer of serous pericardium is pericardial space and normally contains only a small amount of serous fluid and the pressure is subatmospheric under normal condition
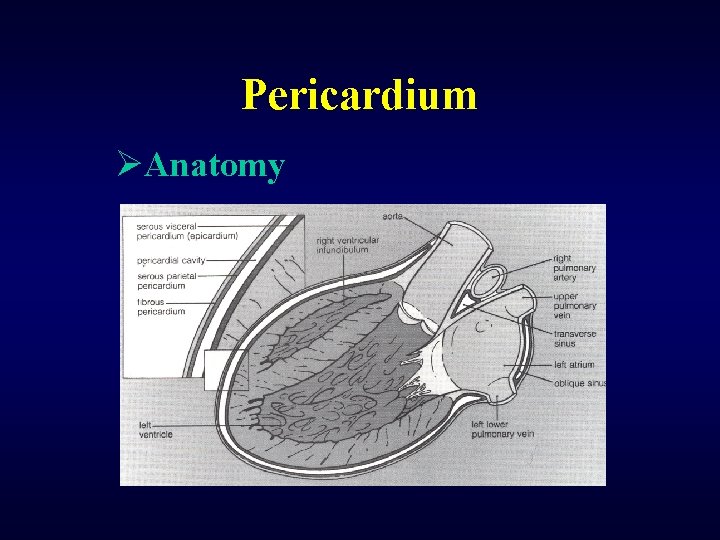
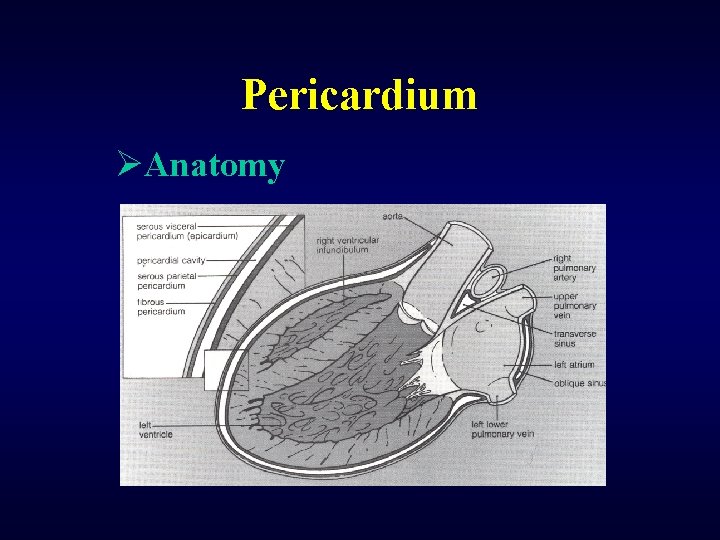
Pericardium ØAnatomy
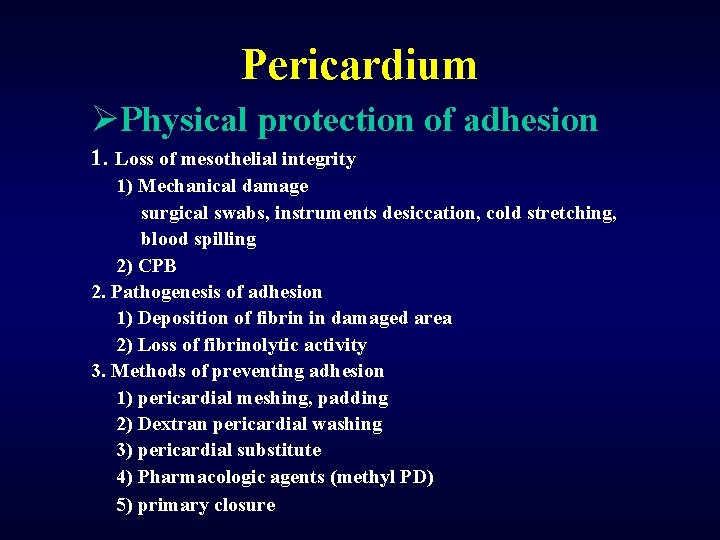
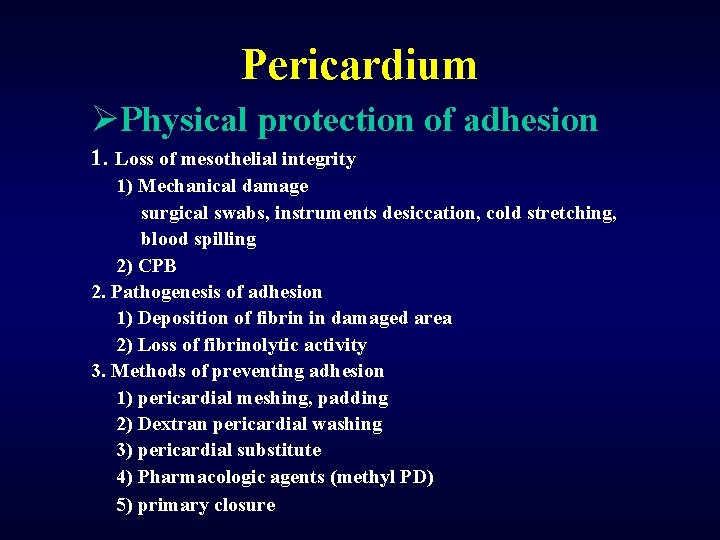
Pericardium ØPhysical protection of adhesion 1. Loss of mesothelial integrity 1) Mechanical damage surgical swabs, instruments desiccation, cold stretching, blood spilling 2) CPB 2. Pathogenesis of adhesion 1) Deposition of fibrin in damaged area 2) Loss of fibrinolytic activity 3. Methods of preventing adhesion 1) pericardial meshing, padding 2) Dextran pericardial washing 3) pericardial substitute 4) Pharmacologic agents (methyl PD) 5) primary closure
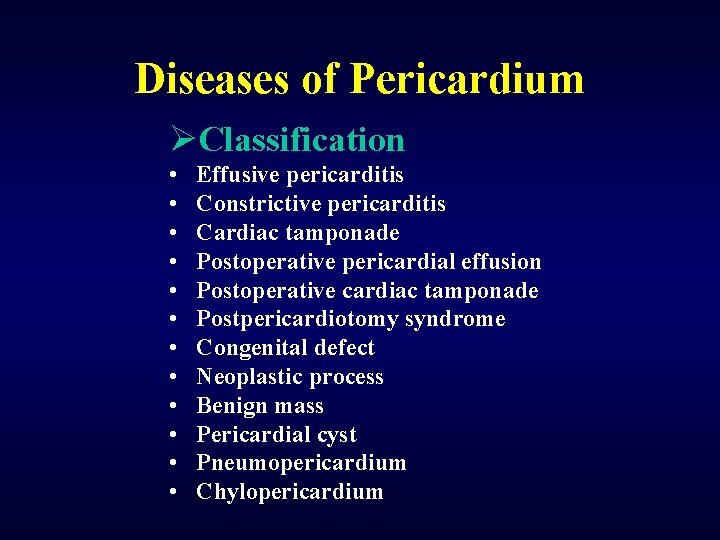
Diseases of Pericardium ØClassification • • • Effusive pericarditis Constrictive pericarditis Cardiac tamponade Postoperative pericardial effusion Postoperative cardiac tamponade Postpericardiotomy syndrome Congenital defect Neoplastic process Benign mass Pericardial cyst Pneumopericardium Chylopericardium
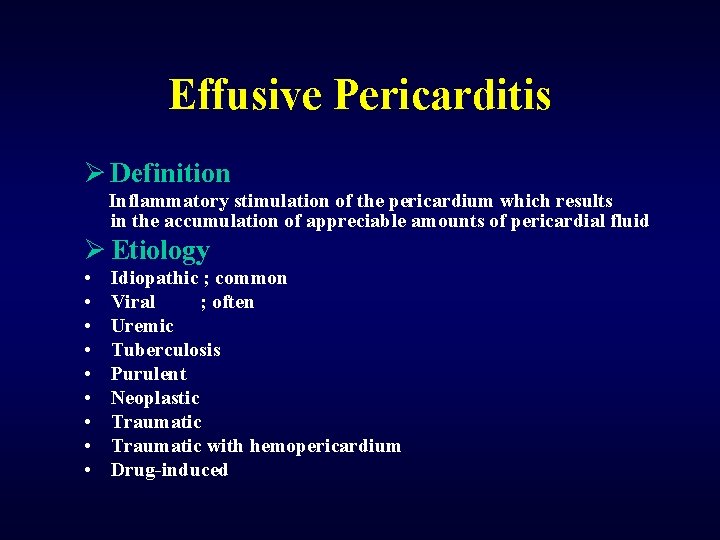
Effusive Pericarditis Ø Definition Inflammatory stimulation of the pericardium which results in the accumulation of appreciable amounts of pericardial fluid Ø Etiology • • • Idiopathic ; common Viral ; often Uremic Tuberculosis Purulent Neoplastic Traumatic with hemopericardium Drug-induced
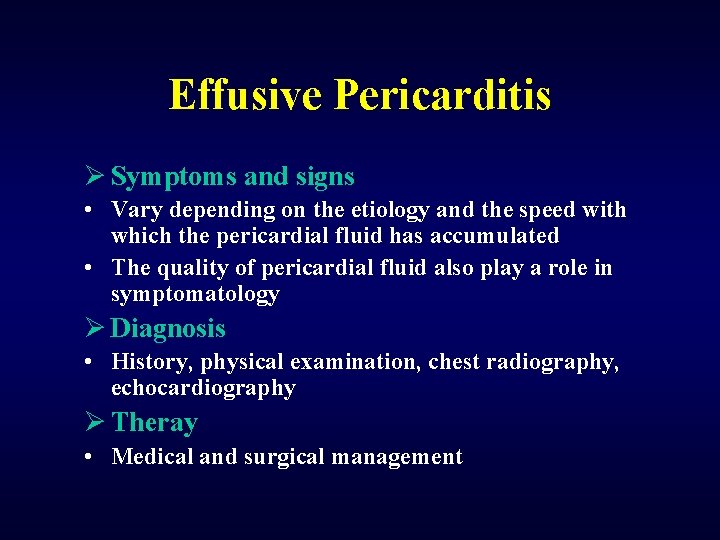
Effusive Pericarditis Ø Symptoms and signs • Vary depending on the etiology and the speed with which the pericardial fluid has accumulated • The quality of pericardial fluid also play a role in symptomatology Ø Diagnosis • History, physical examination, chest radiography, echocardiography Ø Theray • Medical and surgical management
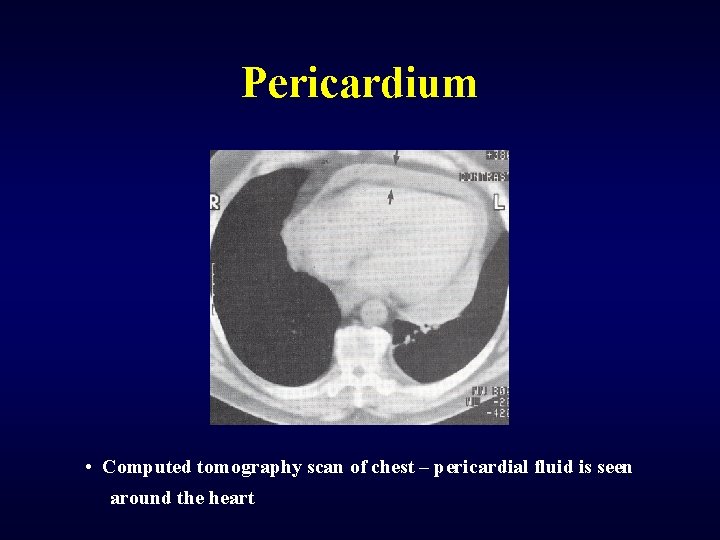
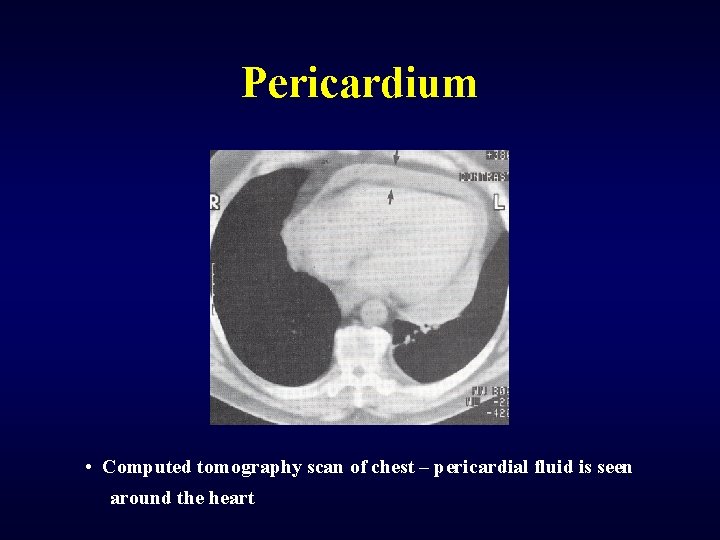
Pericardium • Computed tomography scan of chest – pericardial fluid is seen around the heart
Constrictive Pericarditis 1. Definition Chronic inflammatory process of fibrous and serous layers of the pericardium that leads to pericardial thickening and compression of the cardiac chambers, ultimately with an associated significant reduction in cardiac function 1. Etiology 2. 3. 4. 5. 6. 7. Idiopathic Viral Tuberculosis Effusive Postcardiotomy Radiation induced
Constrictive Pericarditis ØHistory • • • Galen ; Cicatrical thickening in animal in A. D 160 Lower ; Acute & chronic pericarditis in 1669 Lancisi ; Autopsy description in 1728 Pick ; A clinical report in 1896 Rehn & Sauerbruck ; Successful partial pericardiectomy in 1913 in German • Church, Beck ; Successful series in 1929, 1931 in States
Constrictive Pericarditis Ø Pathophysiology • Clinical features derives from basic abnormalities of diastolic function • Ventricular filling is impaired and ventricular stroke volume reduced as a result of reduced compliance of fused cardiac and pericardial mass. • For a brief period in early diastole, ventricular filling is rapid. However, the limit of ventricular distensibility is reached rapidly, and right ventricular pressure pulse displays an early diastolic dip and then a high diastolic plateau ( square root sign )
Constrictive Pericarditis Ø Symptoms and signs • Rare in childhood • Easy fatigability, DOE and even syncope on exertion • Jugular venous distention, distant heart sound, hepatomegaly, ascites in advanced cases Ø Diagnosis • Lack of cardiac enlargement and calcification on chest radiography , pericardial thickening but not always on echocardiography and CT • Equalization of mean RA, PA wedge, RVED and LVED pressure help differentiate constrictive pericarditis to LV failure on cardiac catheterization Ø Therapy • Medical and surgical early pericardiectomy
Constrictive Pericarditis ØNatural history • Knowledge of surgically untreated patients is incomplete • The interval between the etiologic event and onset of clinical evidence of constriction varies between the few months and many years, and the factors that determine rate of progression are unknown • Atrial fibrillation commonly occurs at some stage and results in sudden deterioration in circulatory status • Once signs and symptoms develop, only a semi-invalid life can be led over an interval of 5 to 15 more years • When the clinical syndrome includes ascites, progression is more rapid, particularly in children
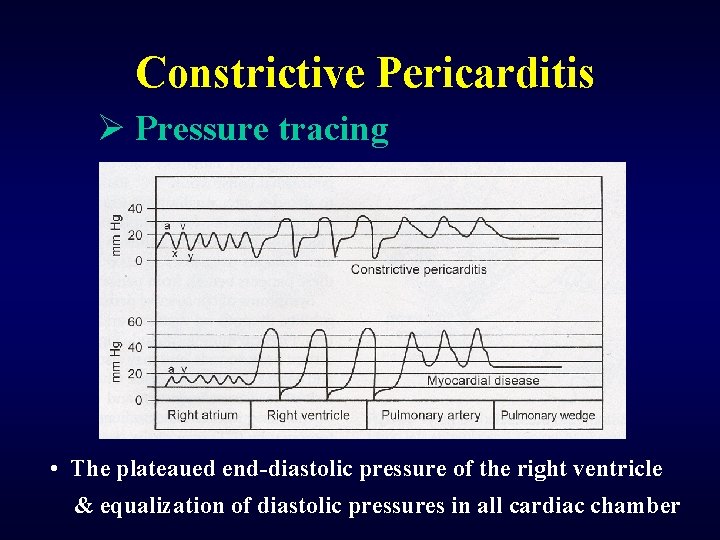
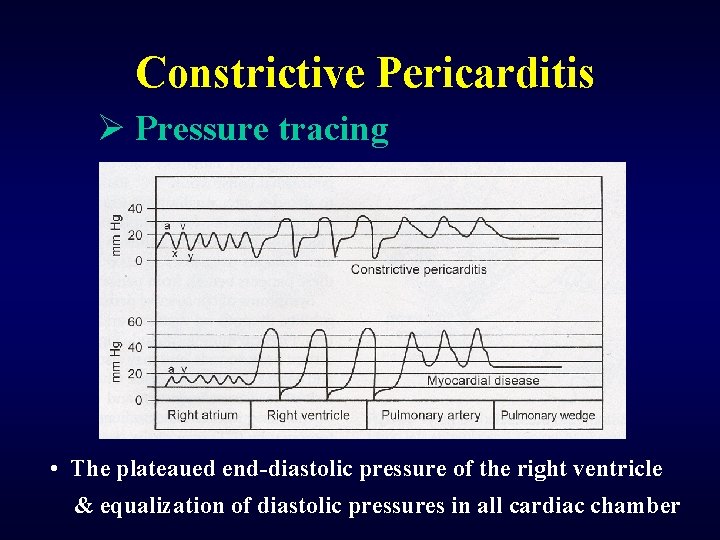
Constrictive Pericarditis Ø Pressure tracing • The plateaued end-diastolic pressure of the right ventricle & equalization of diastolic pressures in all cardiac chamber
Constrictive Pericarditis ØClinical spectrum • The advent of antitubercular chemotherapy brought down the mortality for tuberculous pericarditis from 90% to about 40% • In tuberculous pericarditis, institute the antitubercular therapy for a minimum period of 12 months • The role of corticosteroids in the management of tuberculous pericarditis is controversial • The diagnosis of constrictive pericarditis remains a challenge and is achieved by echocardiography, computed tomography, magnetic resonance imaging, and cardiac catheterization
Constrictive Pericarditis Ø Distinction to restrictive cardiomyopathy • Differentiation of constrictive pericarditis to from restrictive cardiomyopathy with diastolic ventricular dysfunction can be quite challenging • Clinical assessment, MRI, cardiac catheterization, echocardiography, radionuclide ventriculography & endomyocardial biopsy neeeded • For patients with constrictive pericarditis, early complete surgical pericardiectomy remains the only definitive treatment
Pericardiectomy ØDefinitions • Total pericardiectomy was defined as wide excision of the pericardium with the phrenic nerves defining the posterior extent, the great vessels including the intrapericardial portion of and superior vena cava–right atrium junction defining the superior extent, and the diaphragmatic surface, including the inferior vena cava–right atrium junction defining the inferior extent of the pericardial resection. • Constricting layers of the epicardium were removed whenever possible • Any excision less than total was considered partial.
Pericardiectomy ØSurgical techniques • The objective is to remove all pericardium from the cardiac structures including the right & left ventricle, right & left atrium, aorta, pulmonary artery, SVC, IVC, pulmonary veins • In epicardial peel is adherent, a cross-hatching waffle procedure, or multiple incision of peel ( turtle cage operation ) allow myocardial expansion. • On the ventricular surface, dissection may proceed outside the epicardium in the area of coronary arteries, but the dissection over the great arteries and atria should remove the overlying epicardium • Management is curative surgical pericardiectomy and should be instituted rapidly once diagnosis is made
Pericardiectomy ØSurgical approach • Left anterolateral thoracotomy was the preferred option in the setting of purulent pericarditis to avoid sternal infection • Median sternotomy approach was preferred in the following cases: (1) annular constrictive pericarditis, (2) calcific pericardial patch compressing the right atrium & right ventricular outflow tract, (3) extracardiac intrapericardial mass, (4) presence of a gradient between the superior & inferior venae cavae & right atrium 2 mm Hg or greater, (5) constriction after previous open heart surgery, and (6) recurrent constrictive pericarditis after partial pericardiectomy
Pericardiectomy ØSurgical results • Regardless of the operative approach or the extent of pericardial resection, a subset of patients with constrictive pericarditis will develop low-output syndrome after pericardiectomy • Poor results, with persistent elevation of ventricular filling pressures, have been variously attributed to inadequate decortication, fibrous invasion of the myocardium, atrophy of myocardial fibers, "remodeling" of the ventricles, worsening tricuspid regurgitation, and postoperative mitral regurgitation secondary to papillary muscle elongation
Constrictive Pericarditis ØResults of surgical treatment • Survival Early death Time-related survival • Modes of death • Incremental risk factors Preoperative functional class High RV end-diastolic pressure Previous radiation therapy over chest • Hemodynamic results • Functional status • Reoperation
Cardiac Tamponade ØCharacteristics • Accumulation of fluid within the pericardial space can cause a rise in pericardial pressure that leads to impairment of ventricular diastolic filling as defined cardiac compression • All intracardiac pressures will equalize during diastole • The end result of this physiologic state is a lack of left heart filling, leading to a lack of cardiac output and shock • Initial compensatory mechanisms such as tachycardia will precede & herald the eventual state of circulatory collapse
Cardiac Tamponade ØDiagnosis • Beck’s triad Elevated CVP Decreased arterial pressure Muffled heart tones • Pulsus paradoxicus • Kussmaul’s sign
Postpericardiotomy Syndrome ØDefinition • Pericardial inflammation secondary to either cardiac muscle damage or surgical cardiotomy associated with pain, friction rub, and occasionally ECG changes suggestive of ischemia. • Unclear etiology & thought to be an autoimmune disorder • Symptoms typically appear 3 – 6 weeks after pericardiotomy including fever, arthralgia, progressive pericardial effusion, and sometimes pleural effusion • Usually lymphocytosis, elevated ESR; eosinophilia and elevated C reactive protein may be present
Postpericardiotomy Syndrome 1. Etiology • Unclear and is thought to be an autoimmune disorder; concurrent fresh or reactivated viral illness is also felt to play a role in triggering the immunologic response & seasonal variation with a higher incidence in winter 1. Therapy • Initial bed rest & nonsteroidal antiinflammatory agents Indomethacin or salicylates ( 60 -80 mmg/Kg/day ) • Prednisolone for refractory cases or recurred case • Surgical intervention for difficult case
Pericardial Defect ØCongenital defects • A rare group of lesions which range from isolated defects to complete absence of pericardium • Three types are complete absence, left-sided defect (most common), and right-sided defect. • Patients may be completely asymptomatic or have exertional or nonexertional chest pain, cardiac arrhythmias, syncope, sudden death, or incarceration of myocardium • Surgery is indicated for arrhythmia, cardiac torsion, cardiac herniation, or debilitating chest pain • Surgical repair involves pericardial reconstruction ( pericardioplasty) using xenograft or Gore-tex
Chylopericardium Ø Definition • A chylous effusive process of the pericardium and cause either acute or chronic cardiac tamponade Ø Etiology • • • Idiopathic Posttraumatic After thoracic surgery Postpericardiotomy Neoplastic in origin
Chylopericardium Ø After cardiac surgery • Incidence 0. 2%, frequent after Fontan operation • Etiology Thoracic duct injury ; most common Damage of lymphatics of pericardium Elevation of systemic venous pressure Congenital lymphatic dysplasia (Down syndrome) • Treatment Diuresis & dietary modification ( low-fat mediumchain trigliceride ), parenteral nutrition, repeated centesis. Exploration to ligate after 2 weeks medical failure with pleuropericardial window or pericardiostomy
Pericardial Reentry ØSurgical adhesion • Lead to more difficult sternal reentry and cardiac dissection, to blunted visibility of distinct cardiac structures, to potential injury of cardiac structures (including the atria, ventricles, and coronary arteries), as well as to an increased risk of surgical bleeding, all associated with an increase in morbidity and mortality. • Reoperations due to adhesions are more timeconsuming, and because of the increased difficulty they are associated with a greater level of stress for the individual surgeon.
 Secondary action
Secondary action Seoul national university computer science
Seoul national university computer science Seoul national university medical school
Seoul national university medical school Seoul national university events
Seoul national university events Seoul university acceptance rate
Seoul university acceptance rate Seoul metal vietnam
Seoul metal vietnam The seoul accord agreement accredits
The seoul accord agreement accredits Seoul metro map
Seoul metro map Seoul semiconductor vina
Seoul semiconductor vina Neis korea
Neis korea Seoul semiconductor vina
Seoul semiconductor vina Seoul
Seoul Yoon hyun-min seoul chodang elementary school
Yoon hyun-min seoul chodang elementary school Seoul idrc
Seoul idrc Membrane covers the heart
Membrane covers the heart Functions of pericardium
Functions of pericardium Blood supply of mediastinum
Blood supply of mediastinum Anatomical body regions
Anatomical body regions Pericardium pleura and peritoneum
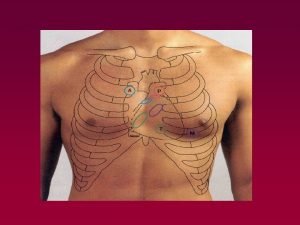
Pericardium pleura and peritoneum What intercostal space is the pulmonic valve
What intercostal space is the pulmonic valve Anatomie des brustkorbs
Anatomie des brustkorbs Valvey veins
Valvey veins Pericardium
Pericardium Kalbin facies diaphragmatica
Kalbin facies diaphragmatica Trigonum thymicum
Trigonum thymicum Venous drainage of the heart
Venous drainage of the heart Visceral pericardium
Visceral pericardium Reticulocyte characteristics
Reticulocyte characteristics Crista terminalis
Crista terminalis Granulation tissue
Granulation tissue Mediastinum
Mediastinum