Discussion group 2 External fixation in nonunion infection




- Slides: 60
Discussion group 2 External fixation in nonunion, infection, and treatment of bone defects AO Trauma Online Masters Course—External Fixation
Case 1: Nonunion of tibia 2
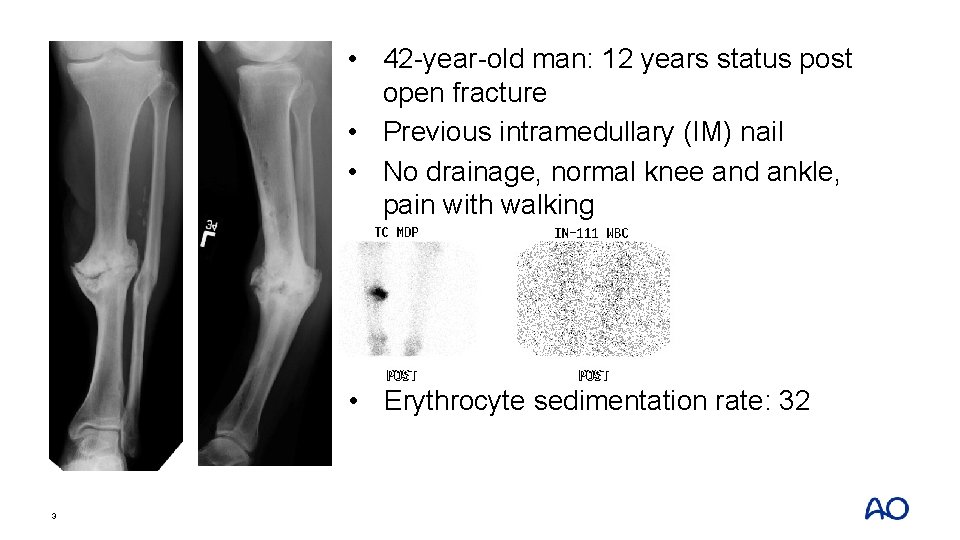
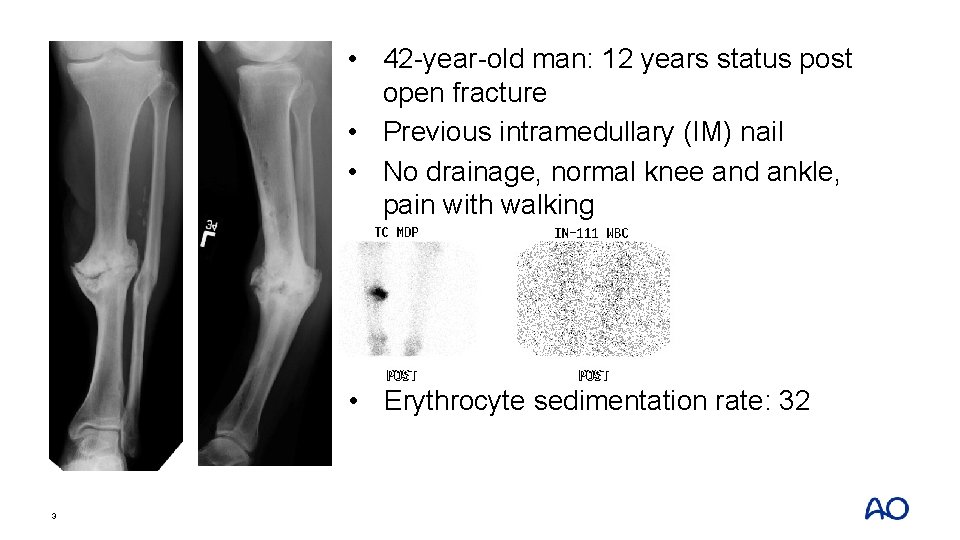
• 42 -year-old man: 12 years status post open fracture • Previous intramedullary (IM) nail • No drainage, normal knee and ankle, pain with walking • Erythrocyte sedimentation rate: 32 3
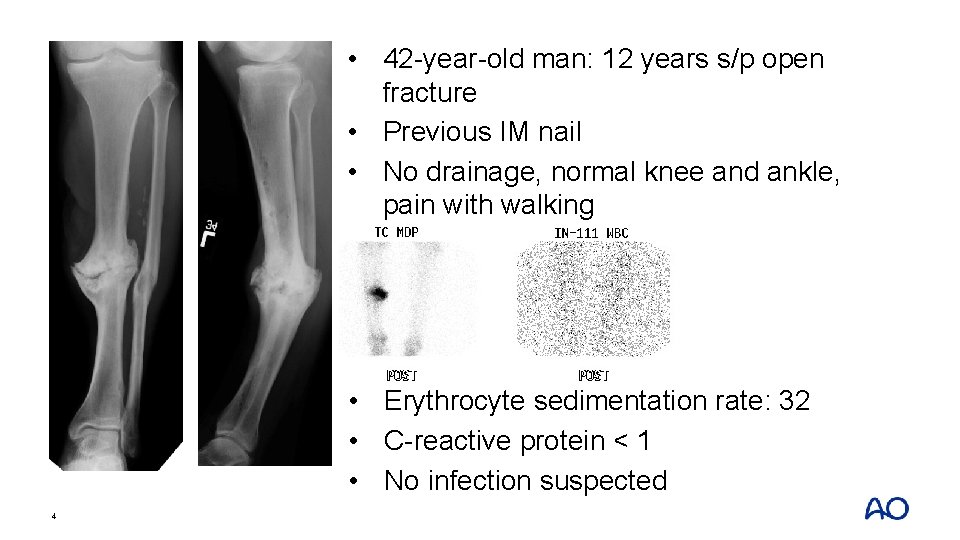
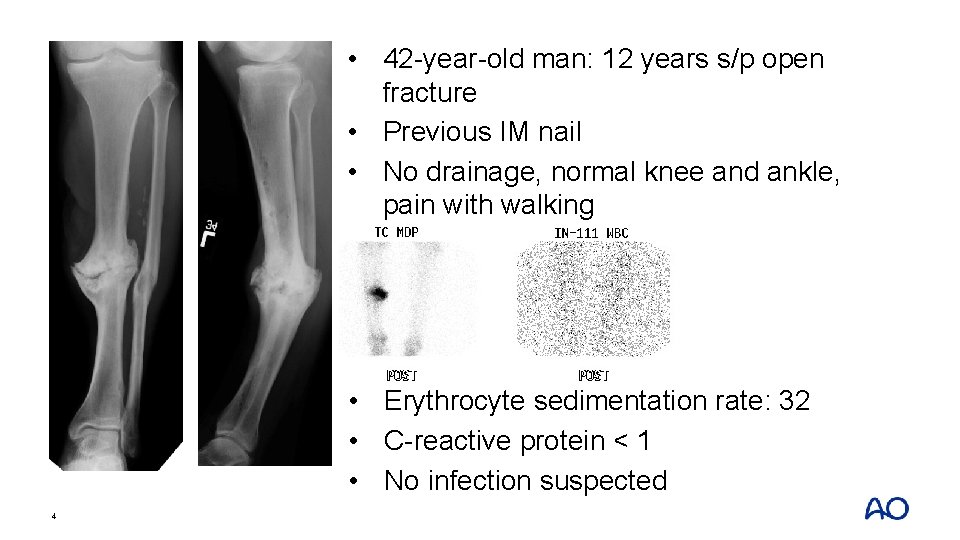
• 42 -year-old man: 12 years s/p open fracture • Previous IM nail • No drainage, normal knee and ankle, pain with walking • Erythrocyte sedimentation rate: 32 • C-reactive protein < 1 • No infection suspected 4
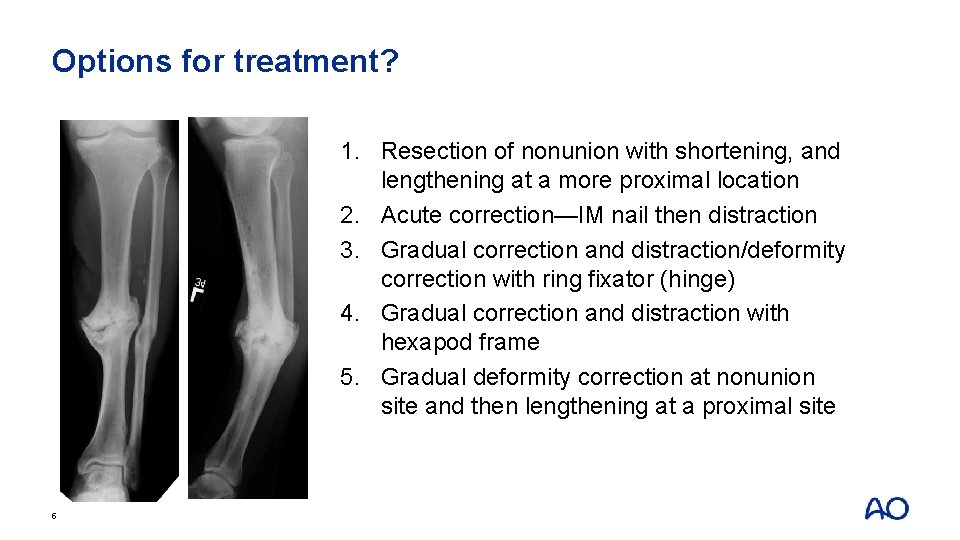
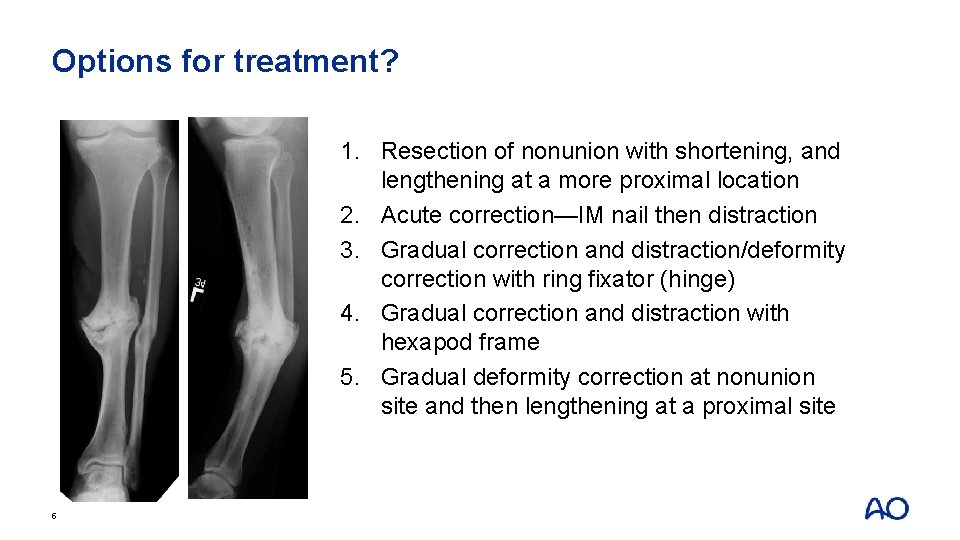
Options for treatment? 1. Resection of nonunion with shortening, and lengthening at a more proximal location 2. Acute correction—IM nail then distraction 3. Gradual correction and distraction/deformity correction with ring fixator (hinge) 4. Gradual correction and distraction with hexapod frame 5. Gradual deformity correction at nonunion site and then lengthening at a proximal site 5
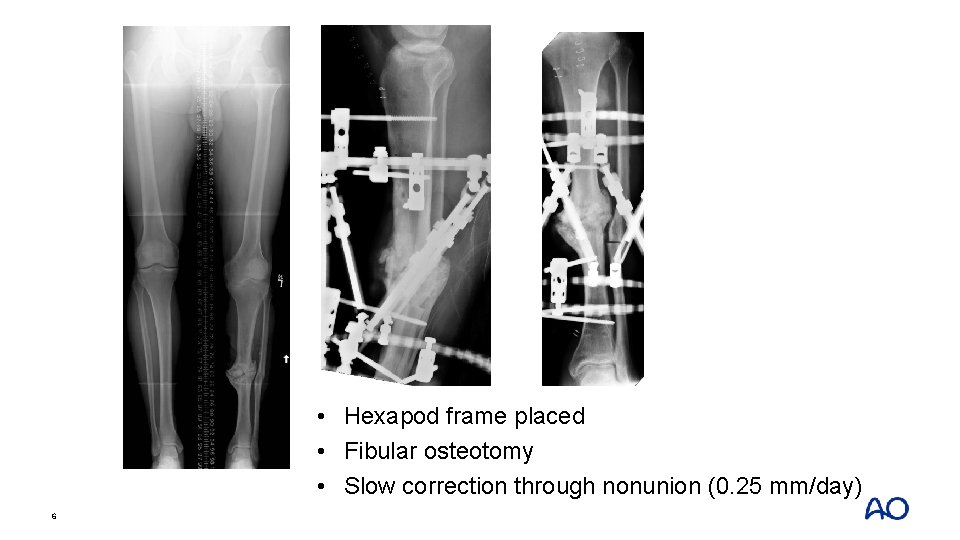
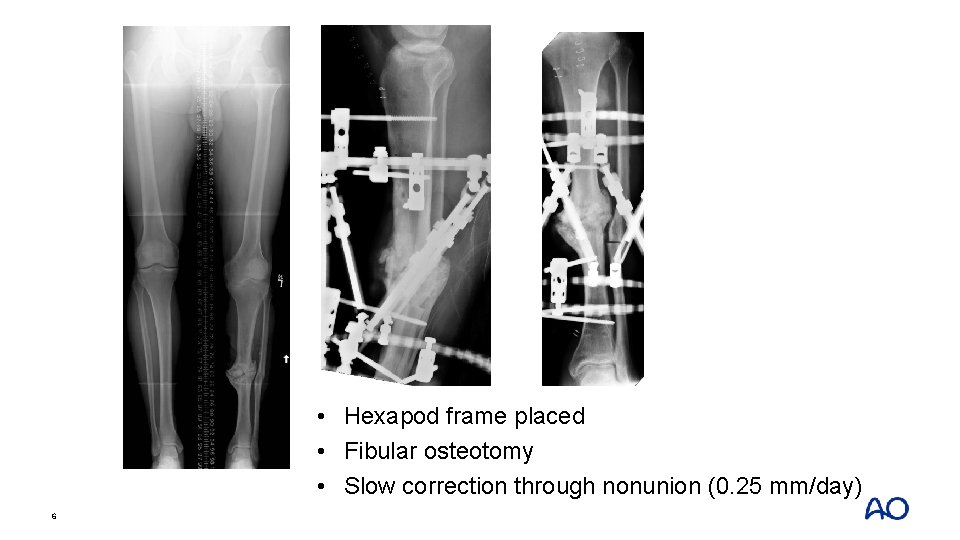
• Hexapod frame placed • Fibular osteotomy • Slow correction through nonunion (0. 25 mm/day) 6
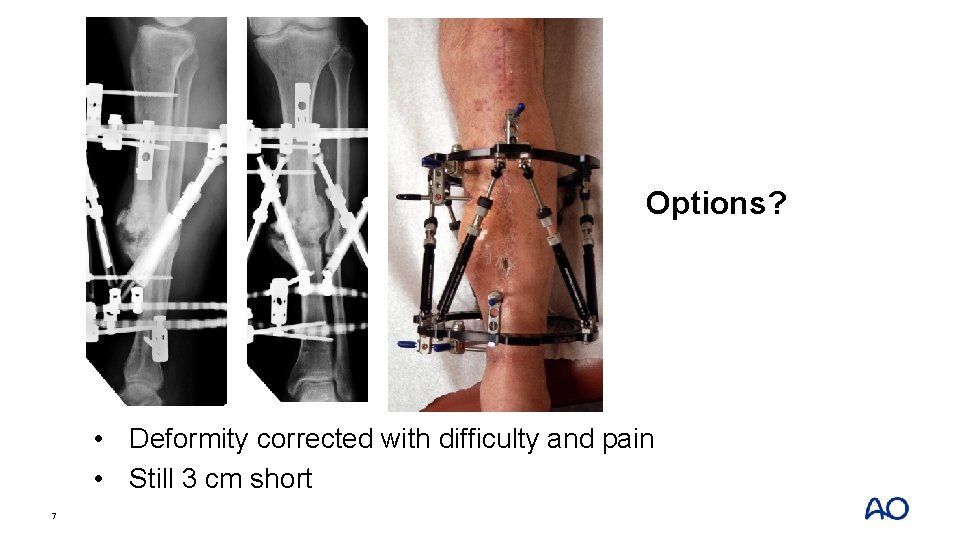
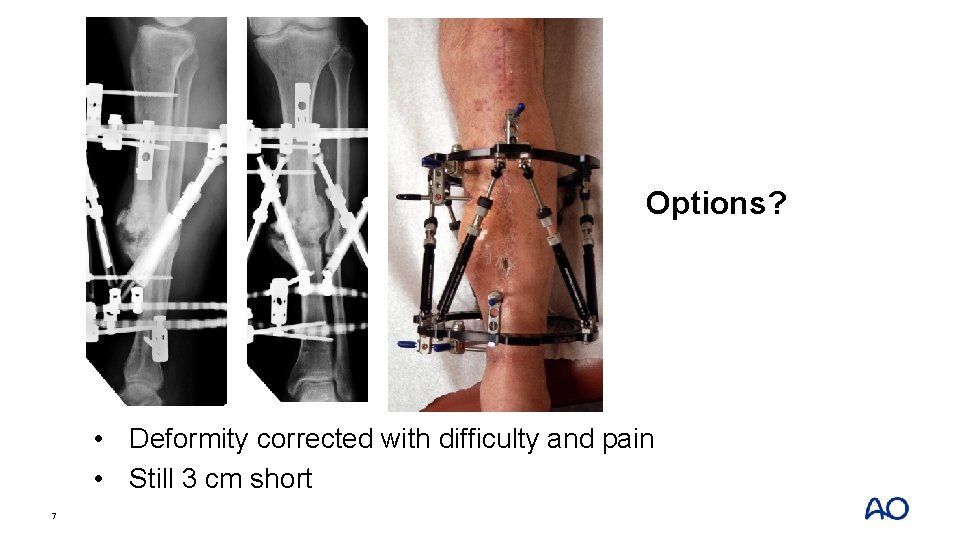
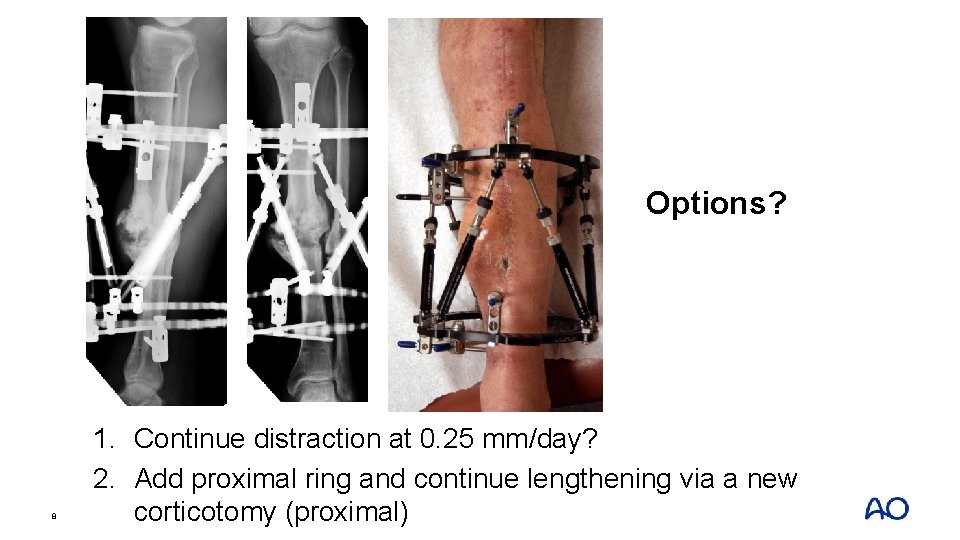
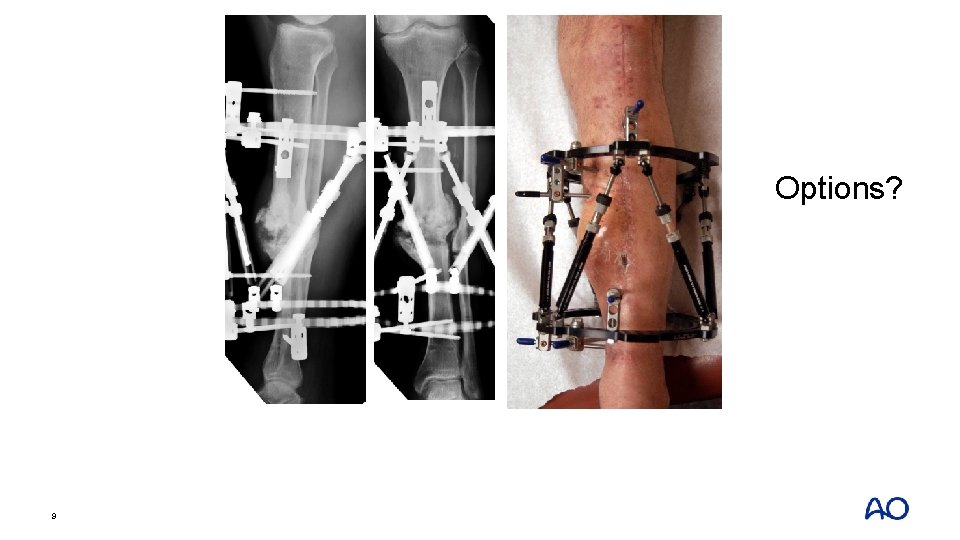
Options? • Deformity corrected with difficulty and pain • Still 3 cm short 7
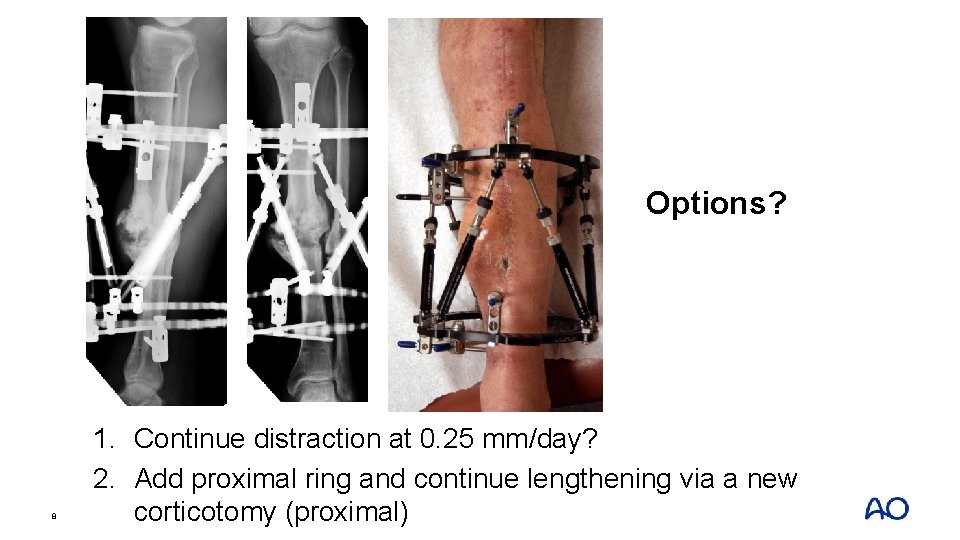
Options? 8 1. Continue distraction at 0. 25 mm/day? 2. Add proximal ring and continue lengthening via a new corticotomy (proximal)
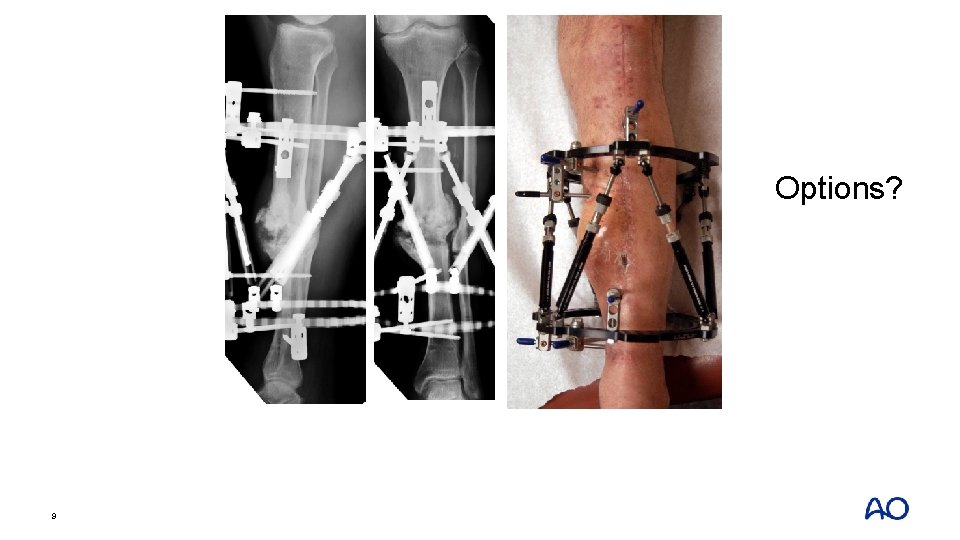
Options? 9
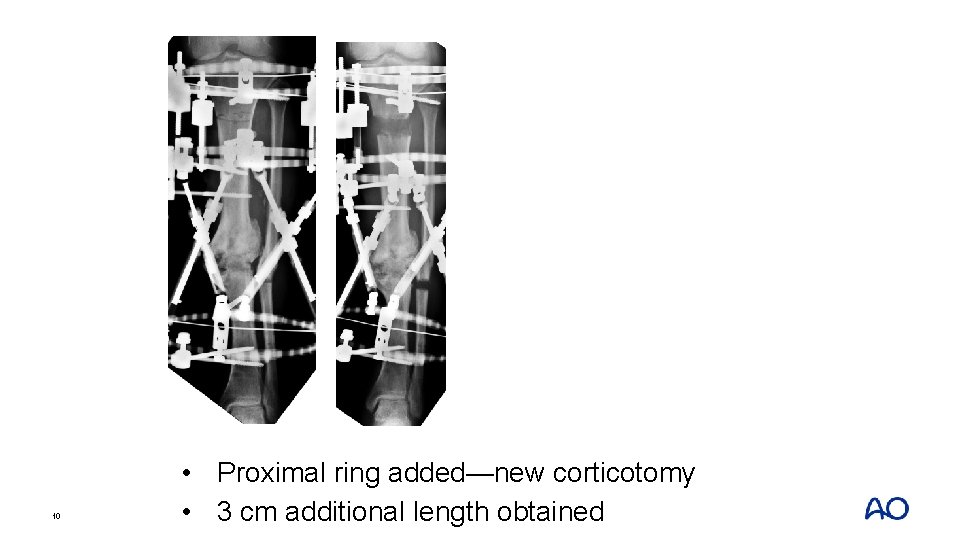
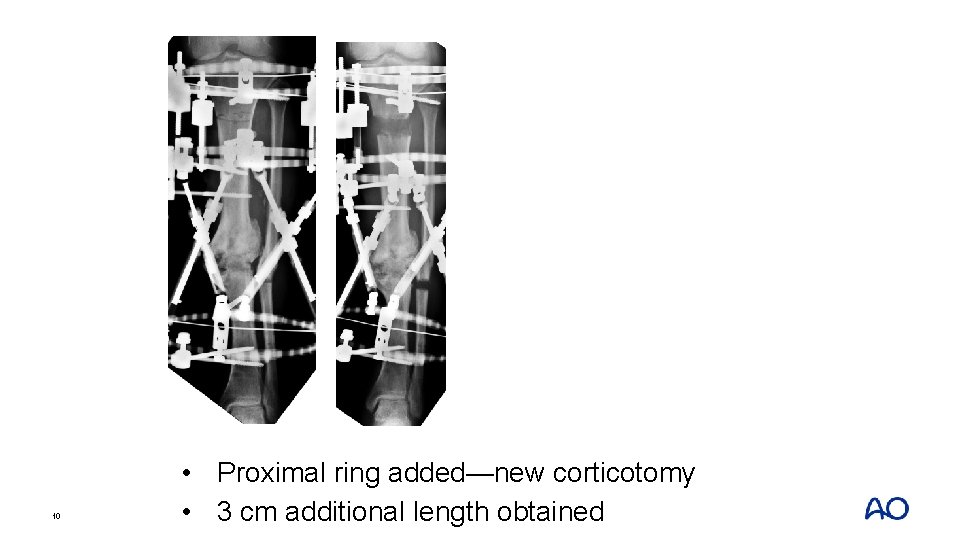
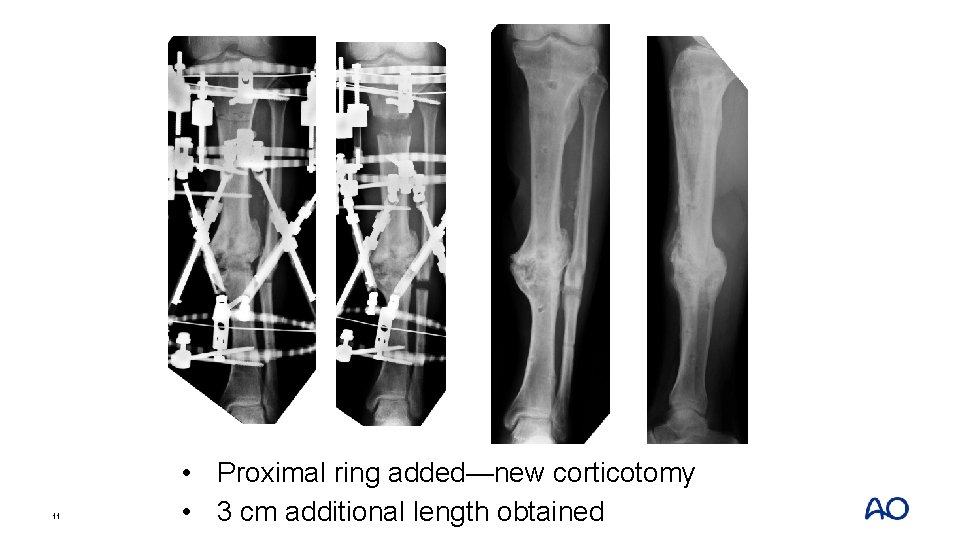
10 • Proximal ring added—new corticotomy • 3 cm additional length obtained
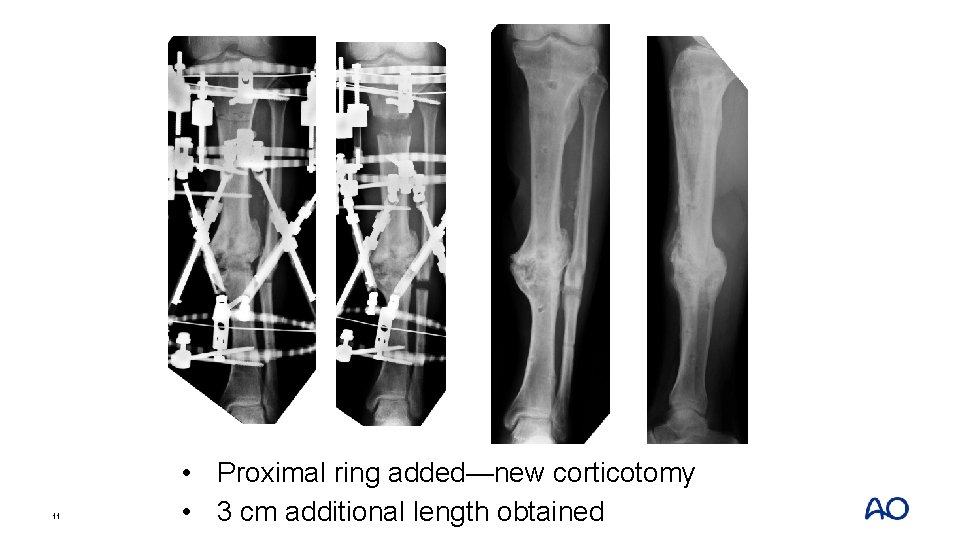
11 • Proximal ring added—new corticotomy • 3 cm additional length obtained
Take-home messages • Hypertrophic nonunion can be distracted to correct deformity and create new bone • Consider separate location for lengthening if amount of bone is significant or difficulties arise 12
Case 2: Tibial defect 13
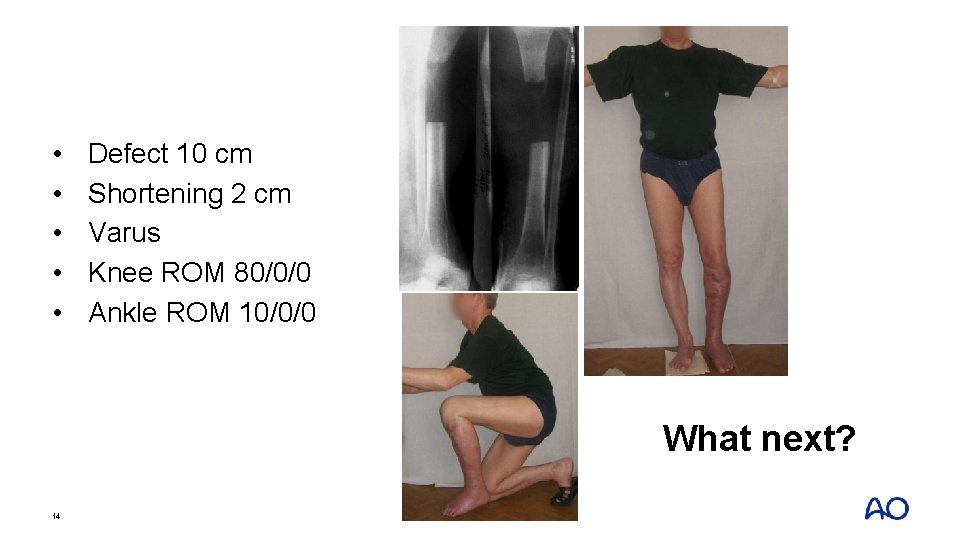
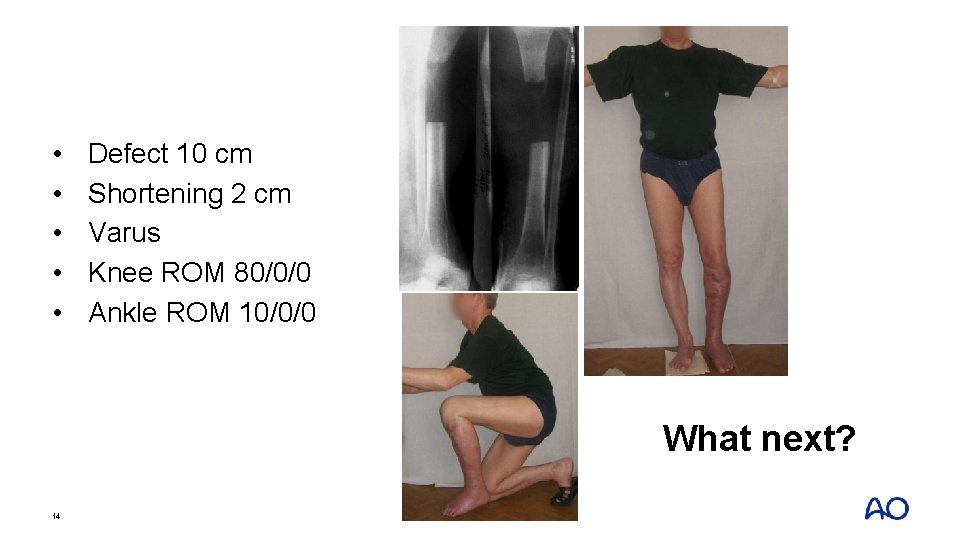
• • • Defect 10 cm Shortening 2 cm Varus Knee ROM 80/0/0 Ankle ROM 10/0/0 What next? 14

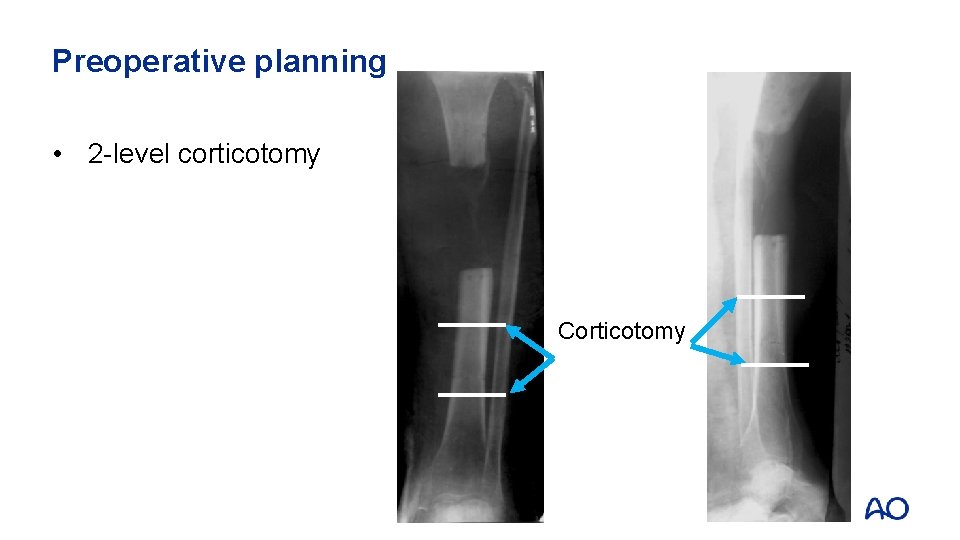
Preoperative planning 15
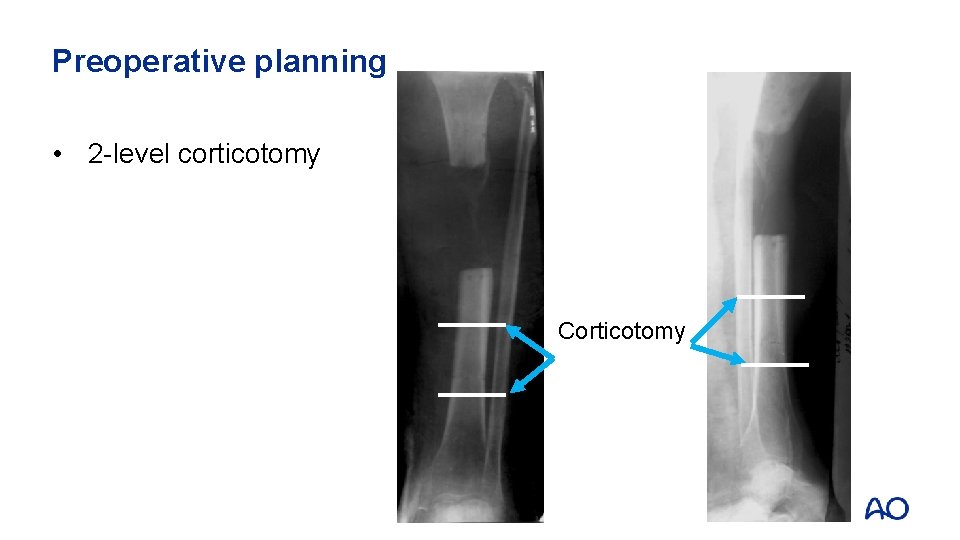
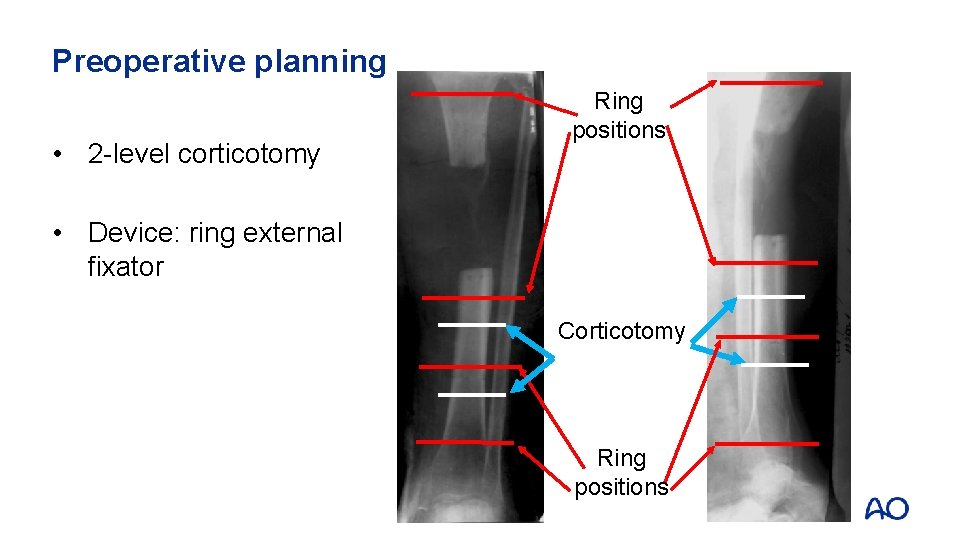
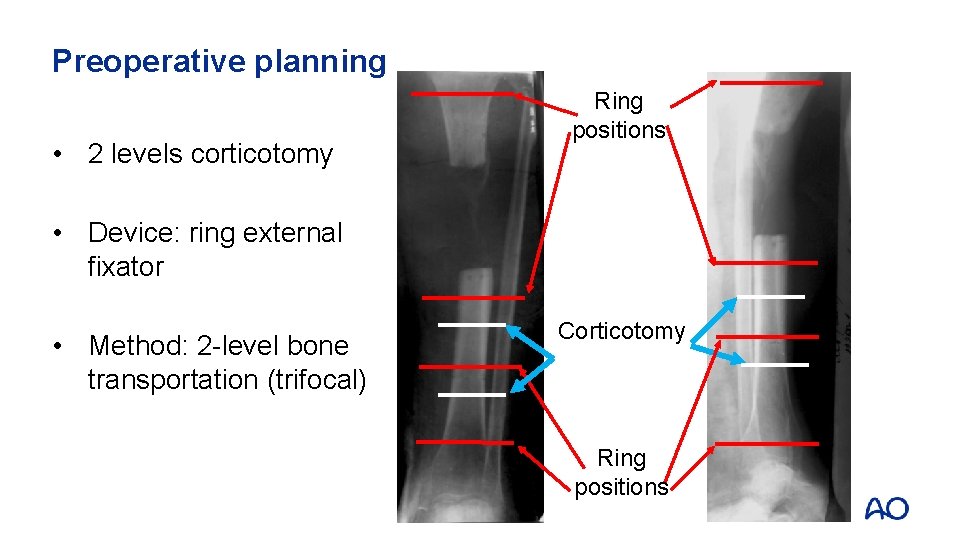
Preoperative planning • 2 -level corticotomy Corticotomy
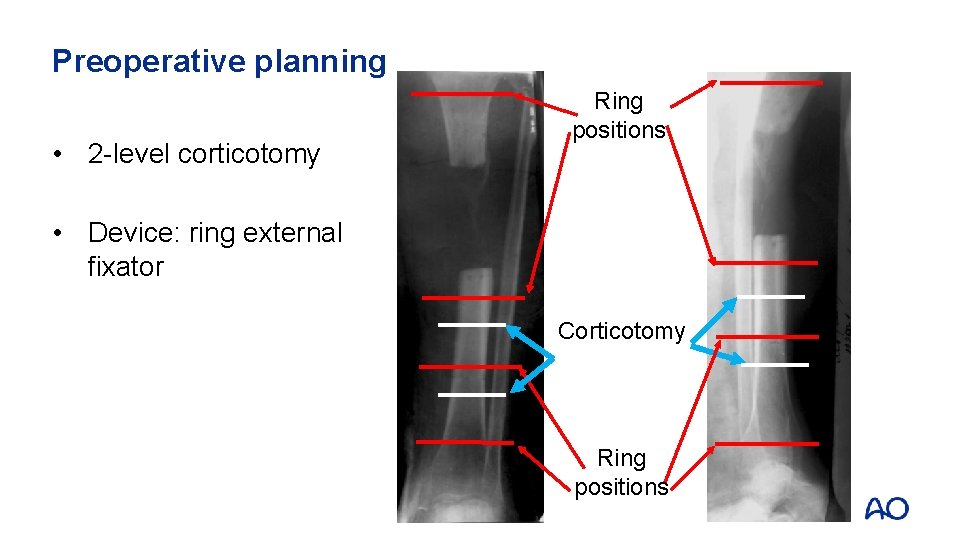
Preoperative planning • 2 -level corticotomy Ring positions • Device: ring external fixator Corticotomy Ring positions
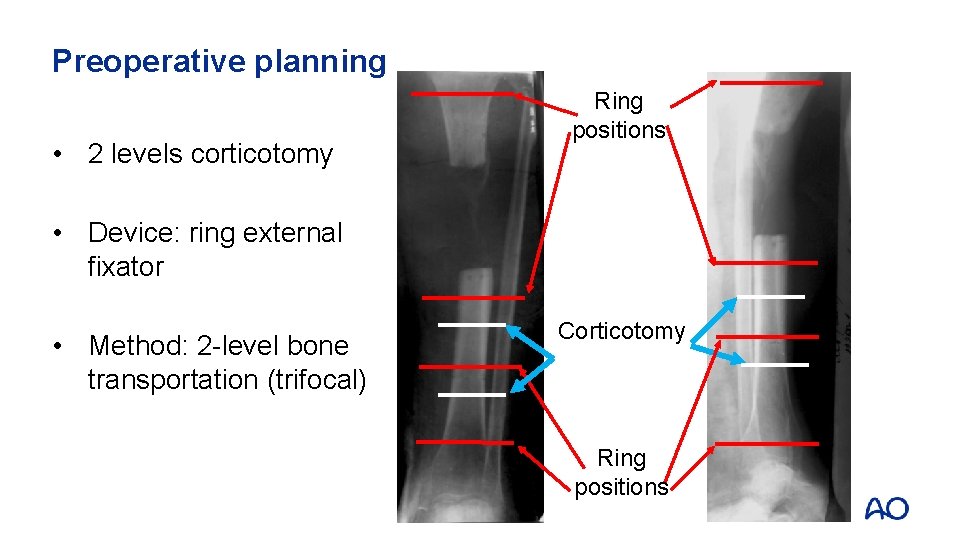
Preoperative planning • 2 levels corticotomy Ring positions • Device: ring external fixator • Method: 2 -level bone transportation (trifocal) Corticotomy Ring positions
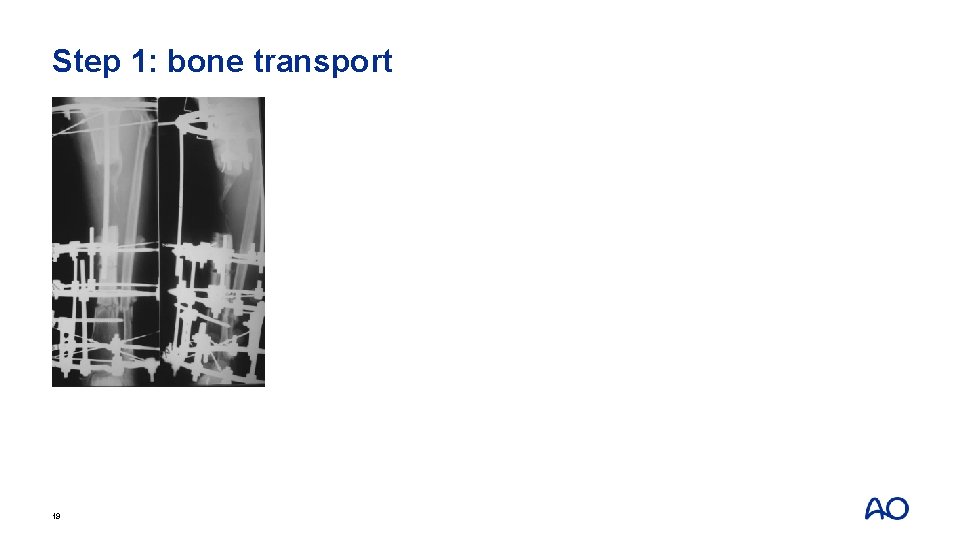
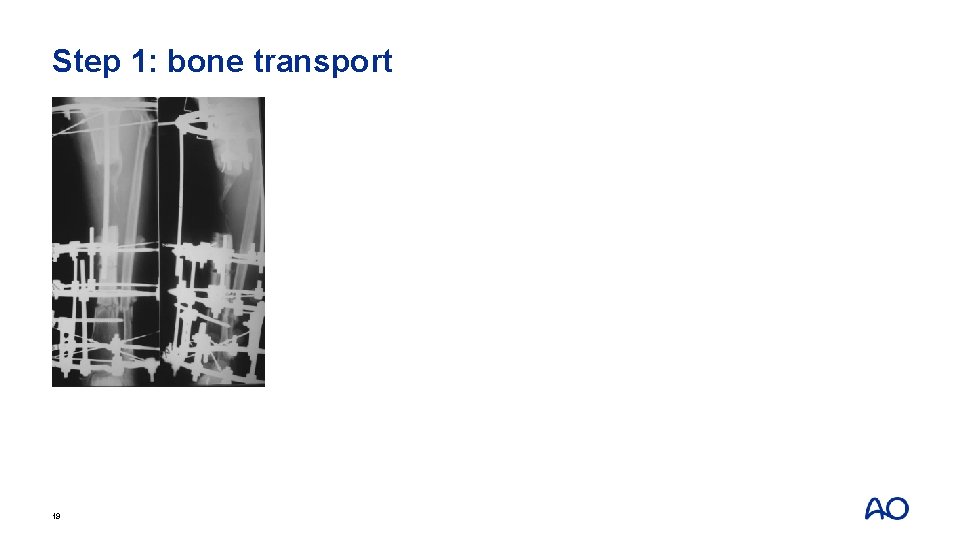
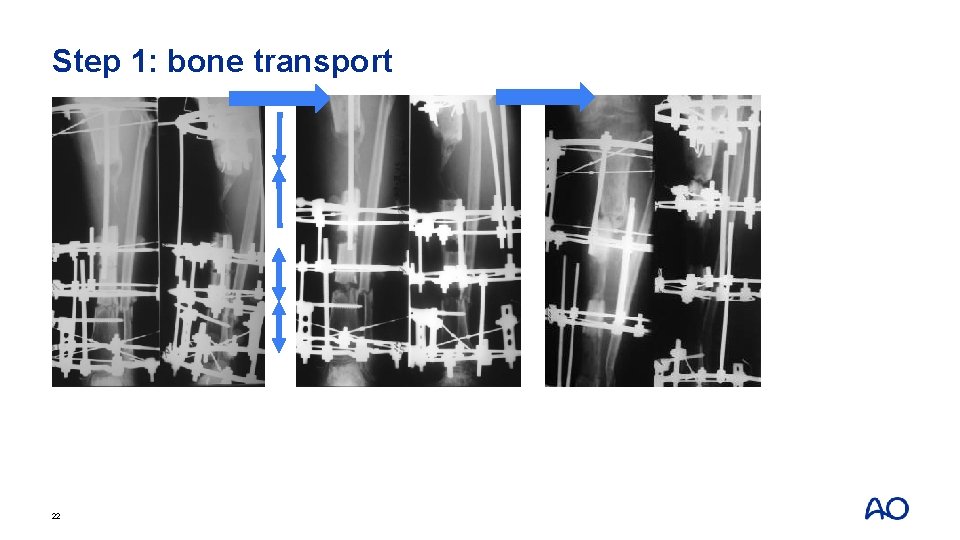
Step 1: bone transport 19
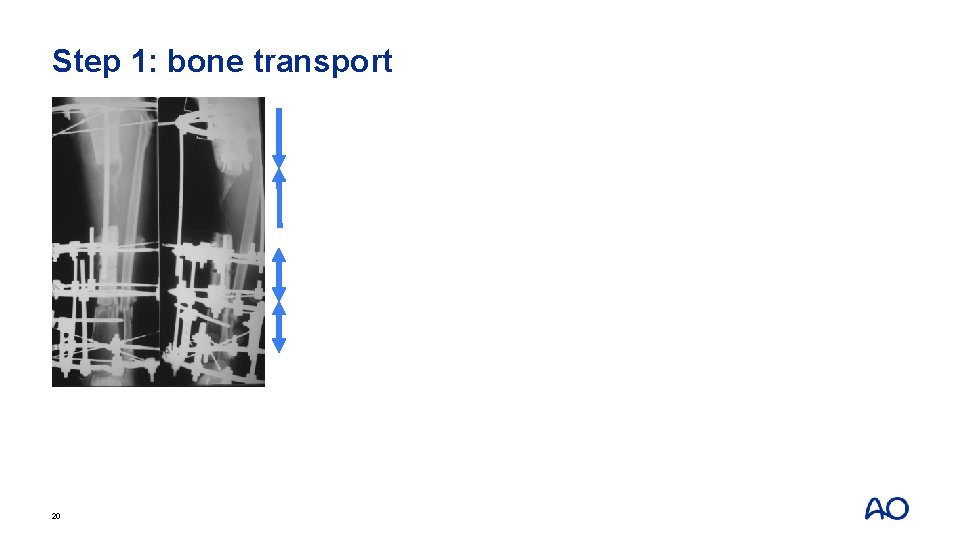
Step 1: bone transport 20
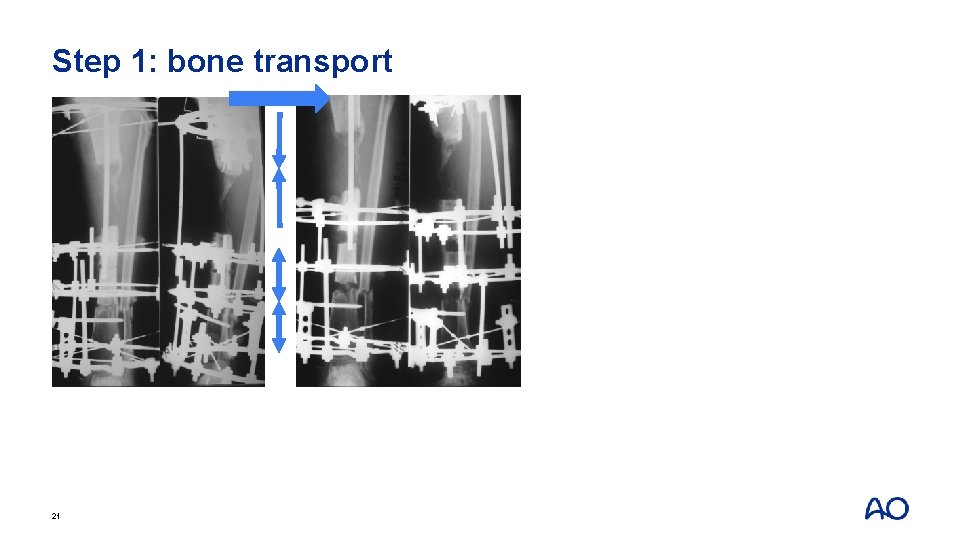
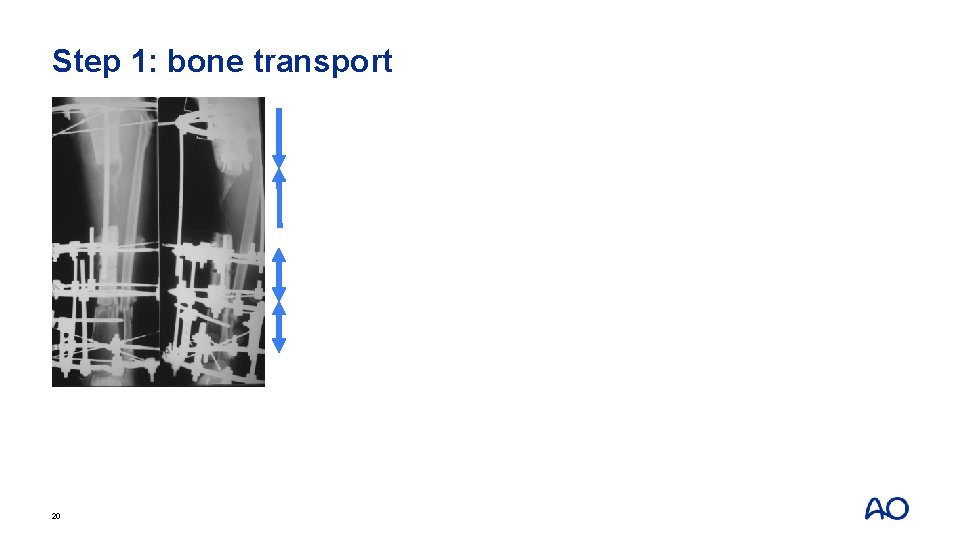
Step 1: bone transport 21
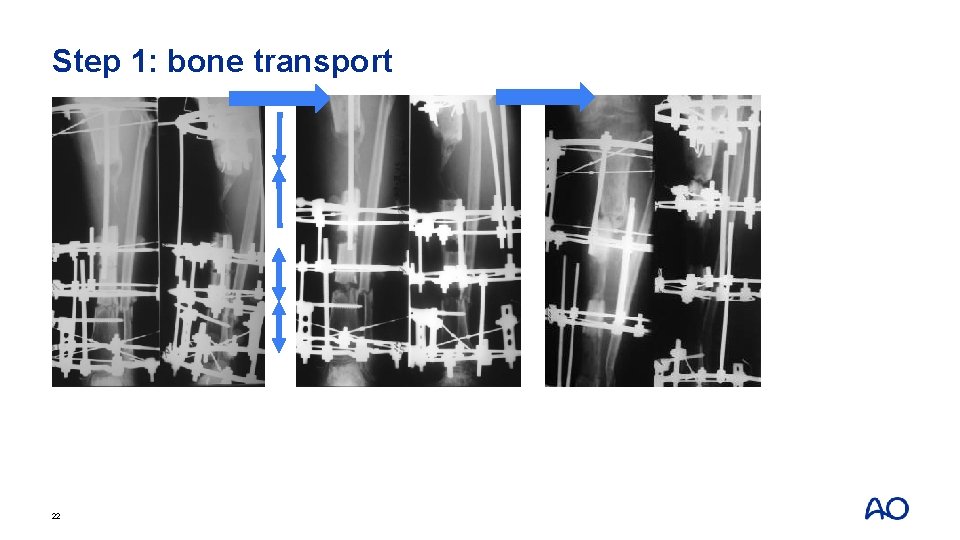
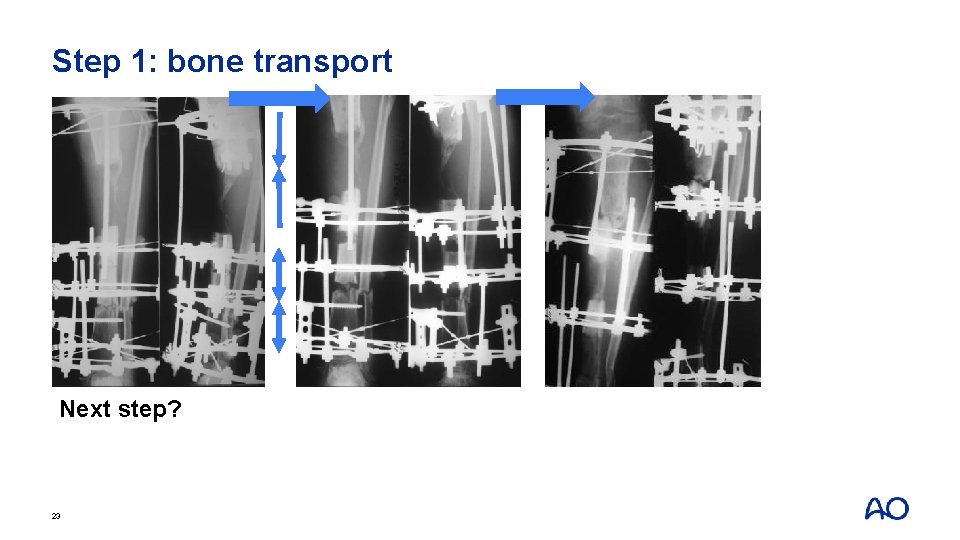
Step 1: bone transport 22
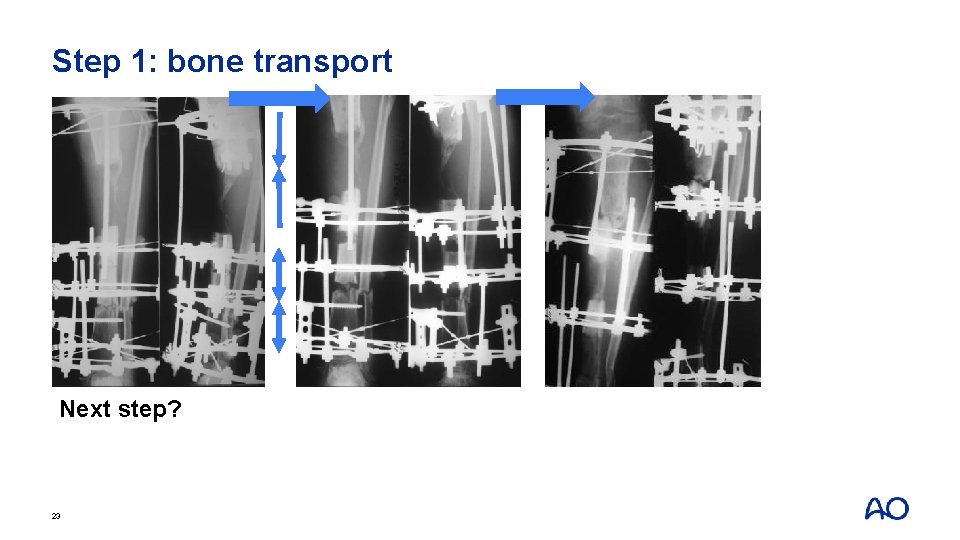
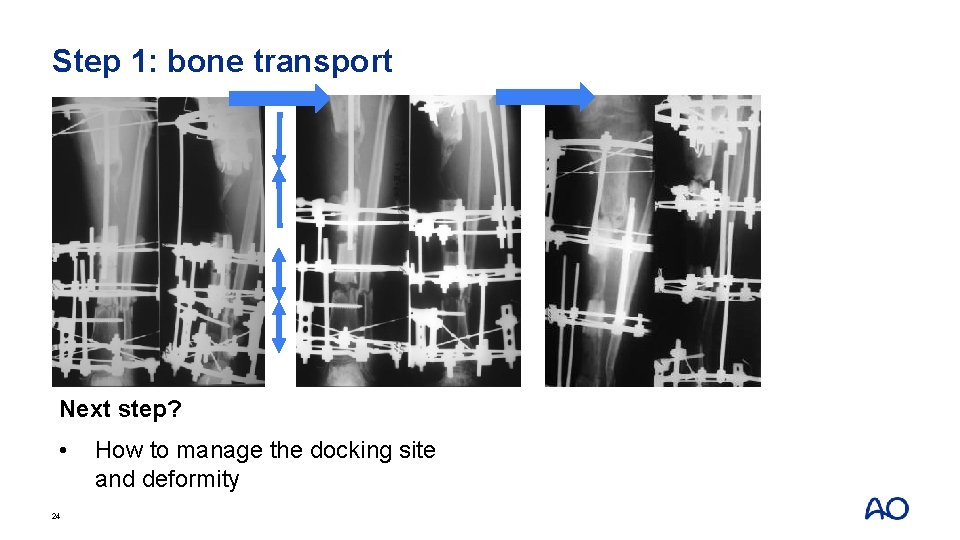
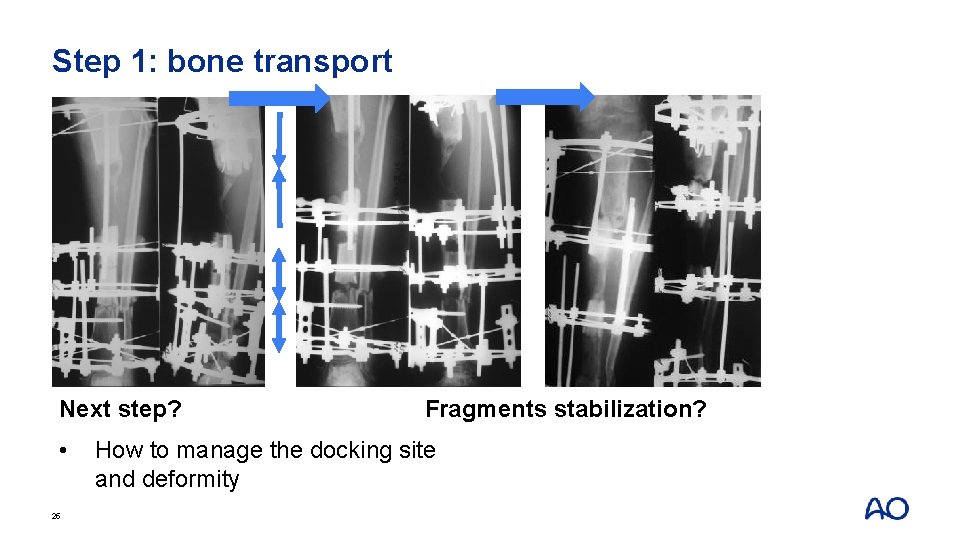
Step 1: bone transport Next step? 23
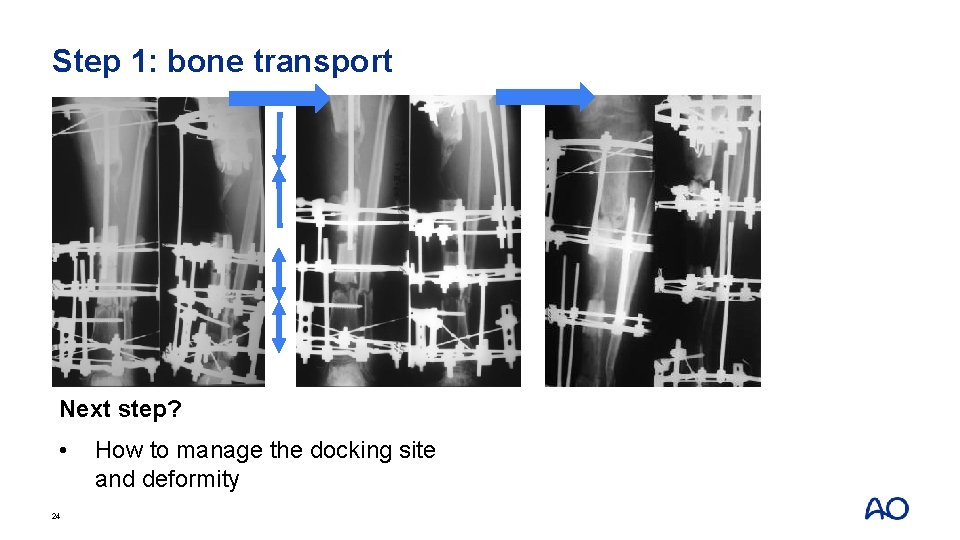
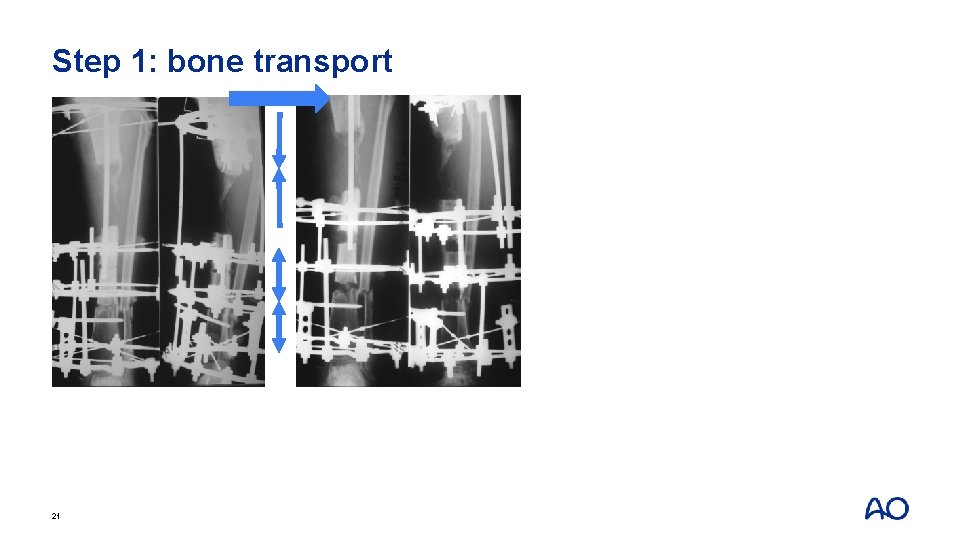
Step 1: bone transport Next step? • 24 How to manage the docking site and deformity
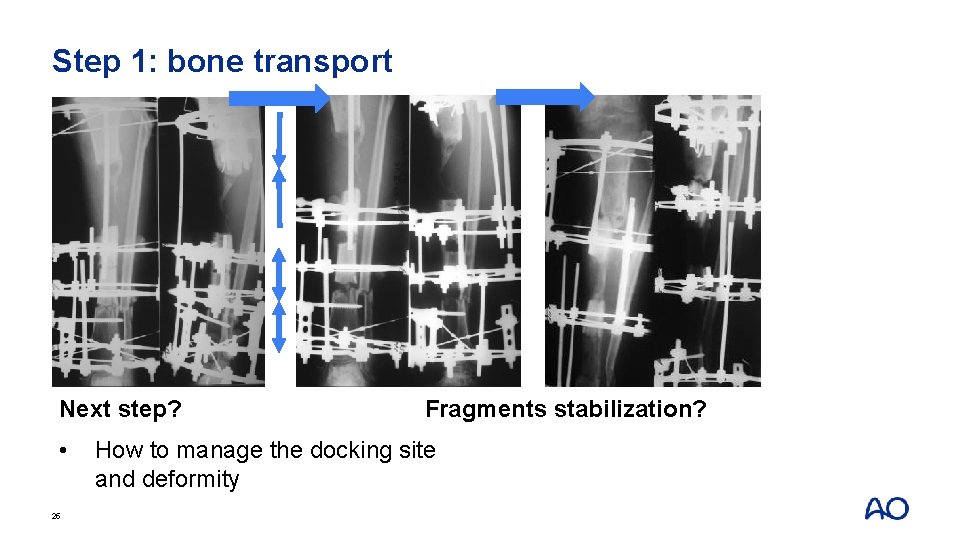
Step 1: bone transport Next step? • 25 Fragments stabilization? How to manage the docking site and deformity
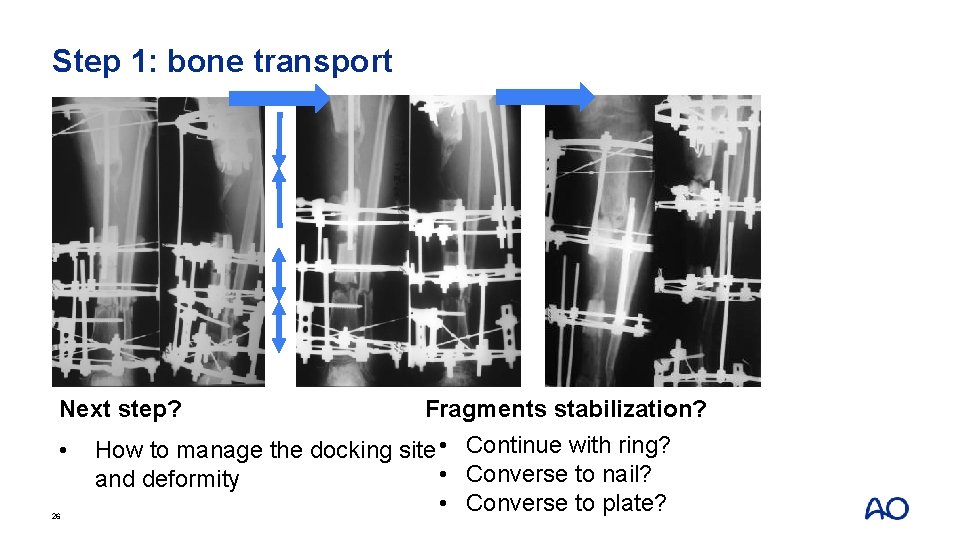
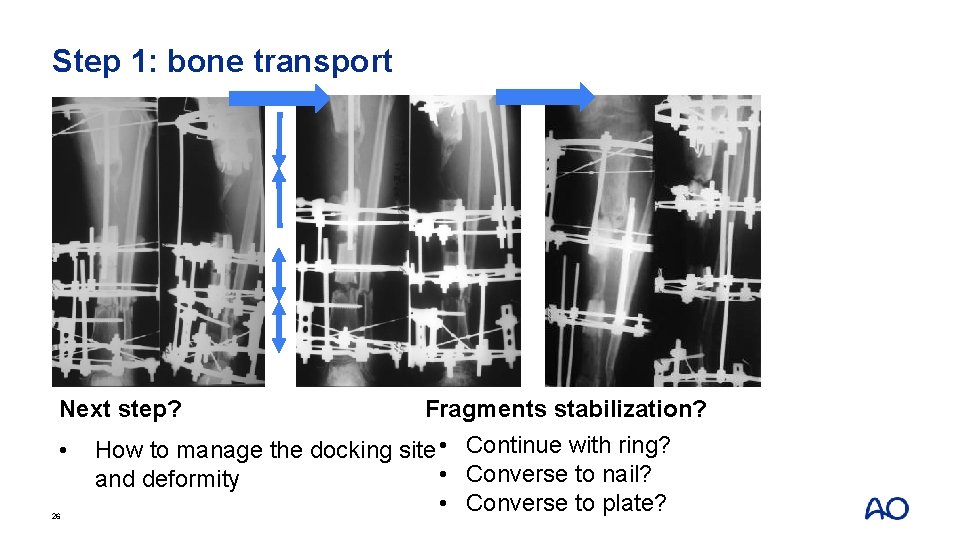
Step 1: bone transport Next step? • 26 Fragments stabilization? How to manage the docking site • Continue with ring? • Converse to nail? and deformity • Converse to plate?
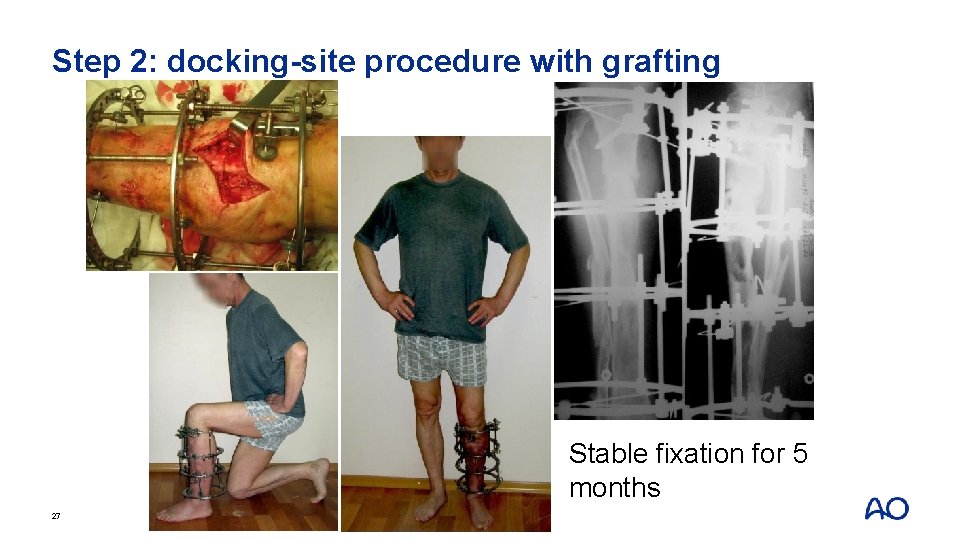
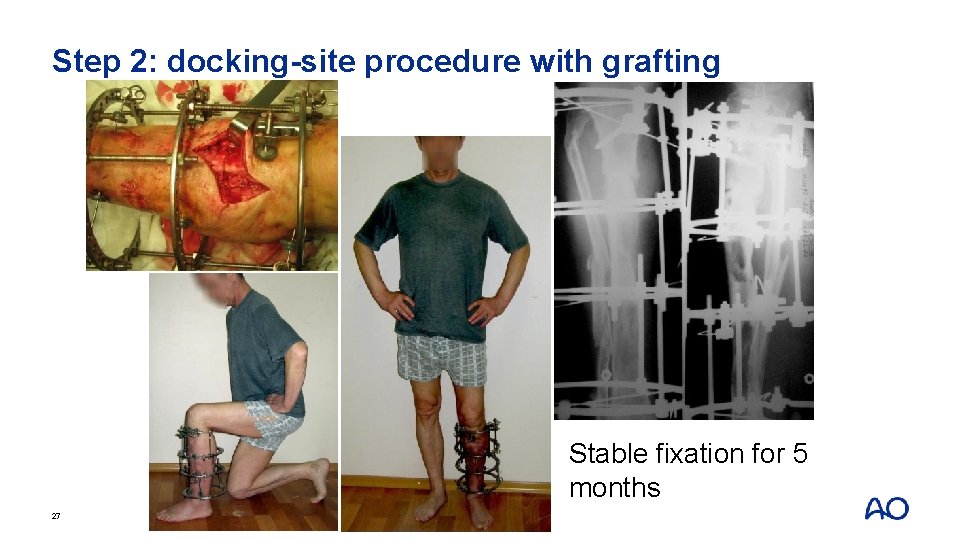
Step 2: docking-site procedure with grafting Stable fixation for 5 months 27
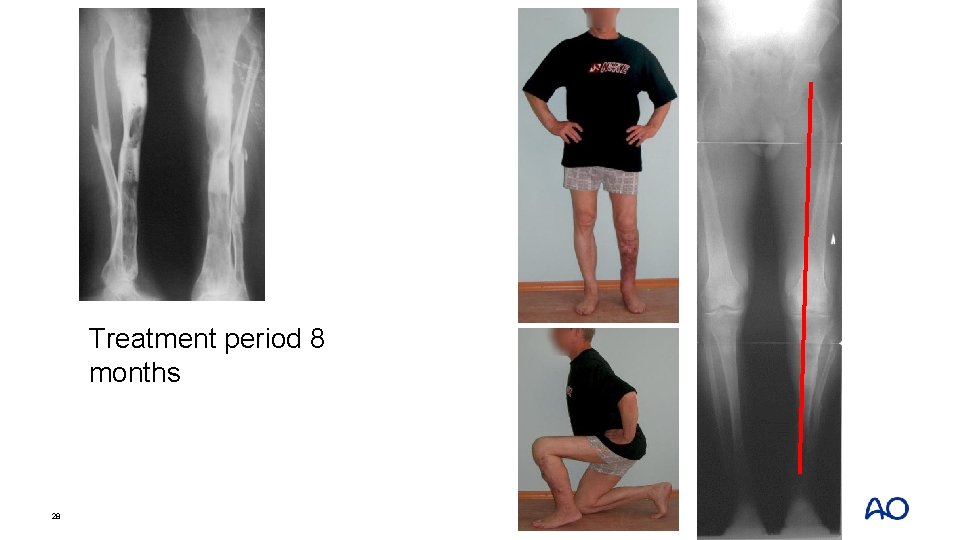
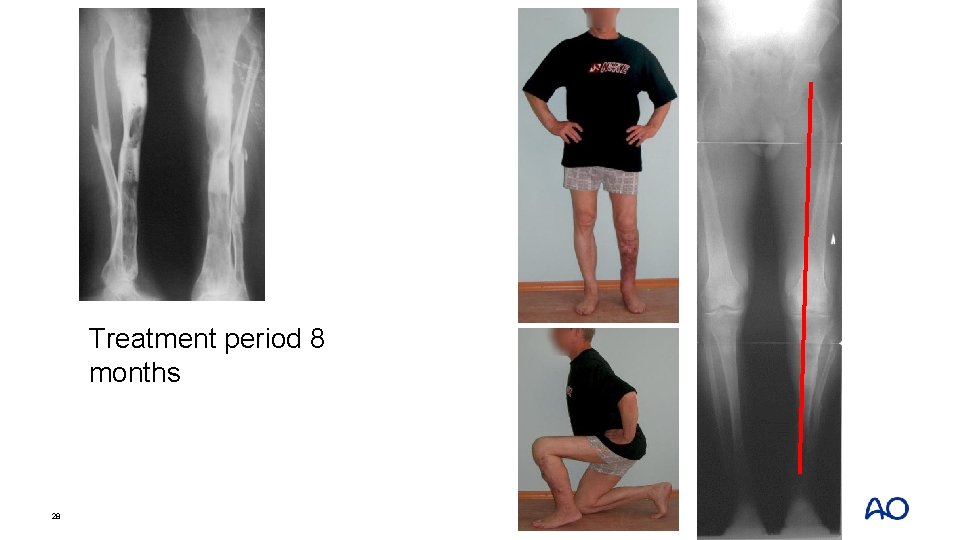
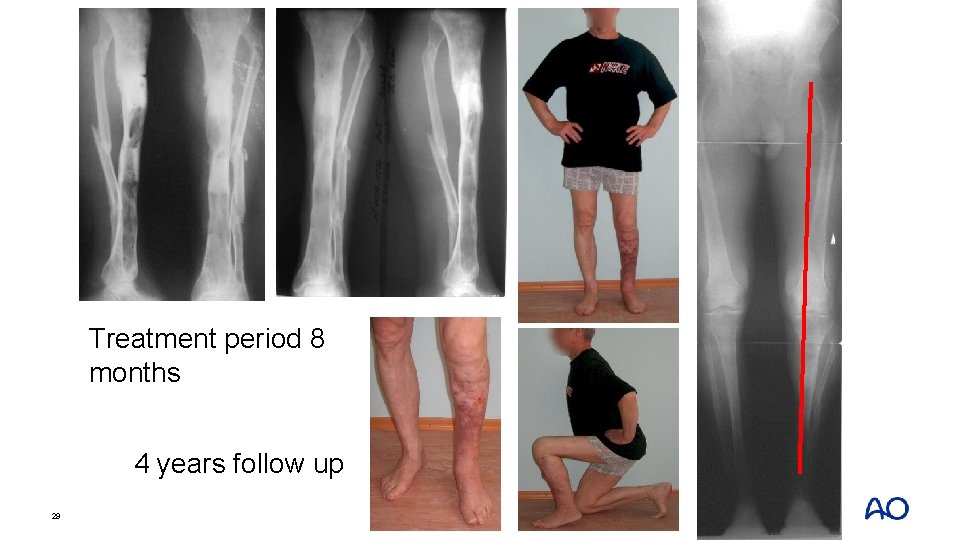
Treatment period 8 months 28
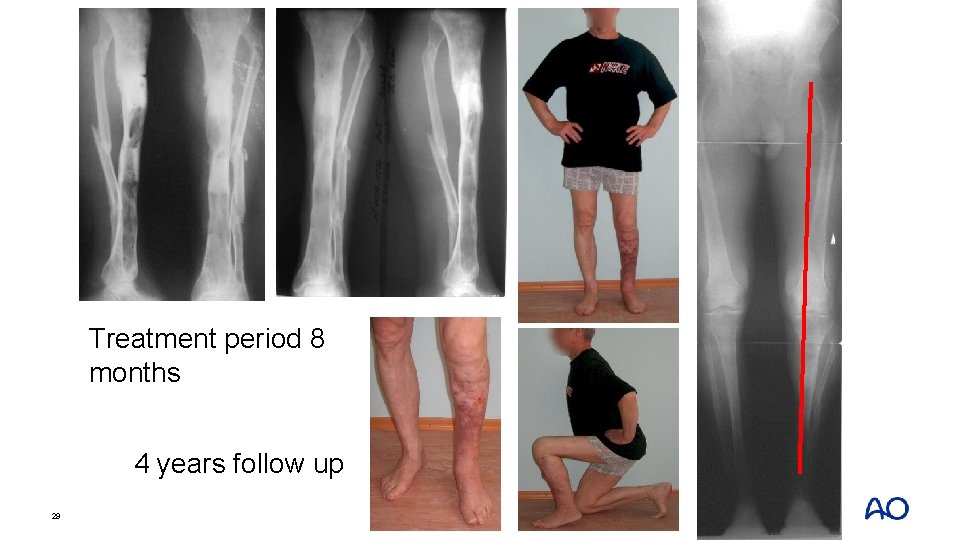
Treatment period 8 months 4 years follow up 29
Take-home messages • In case of bone defects, malunion, deformities, and shortening—different types of surgical decisions are available • Ring fixator can correct bone defect; shortening malunion and deformities in one system • Multilevel corticotomy can be used for long bone defect • Bone graft at docking site is really useful to achieve union 30
Case 3: Distal tibial injury with infection 31
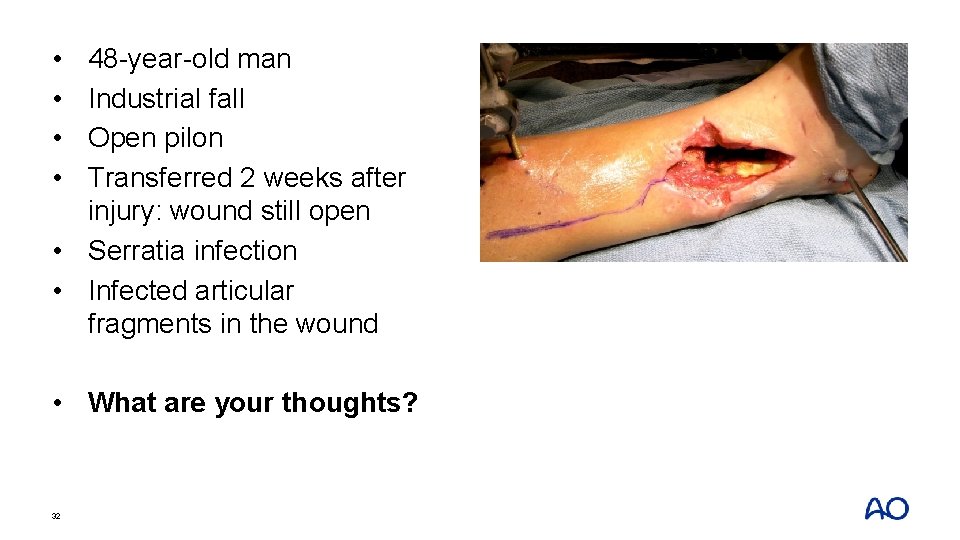
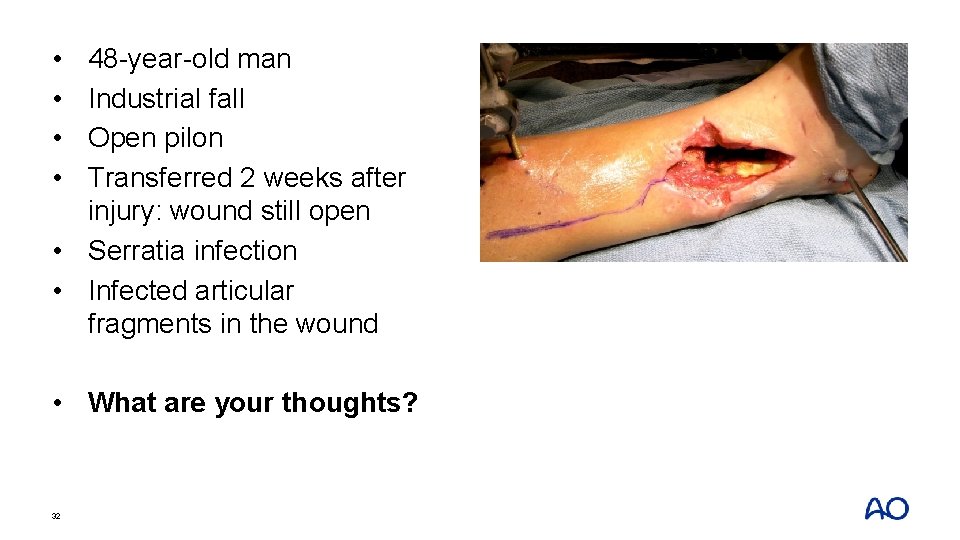
• • 48 -year-old man Industrial fall Open pilon Transferred 2 weeks after injury: wound still open • Serratia infection • Infected articular fragments in the wound • What are your thoughts? 32

• • 48 -year-old man Industrial fall Open pilon Transferred 2 weeks after injury: wound still open • Serratia infection • Infected articular fragments in the wound • What are your thoughts? 33
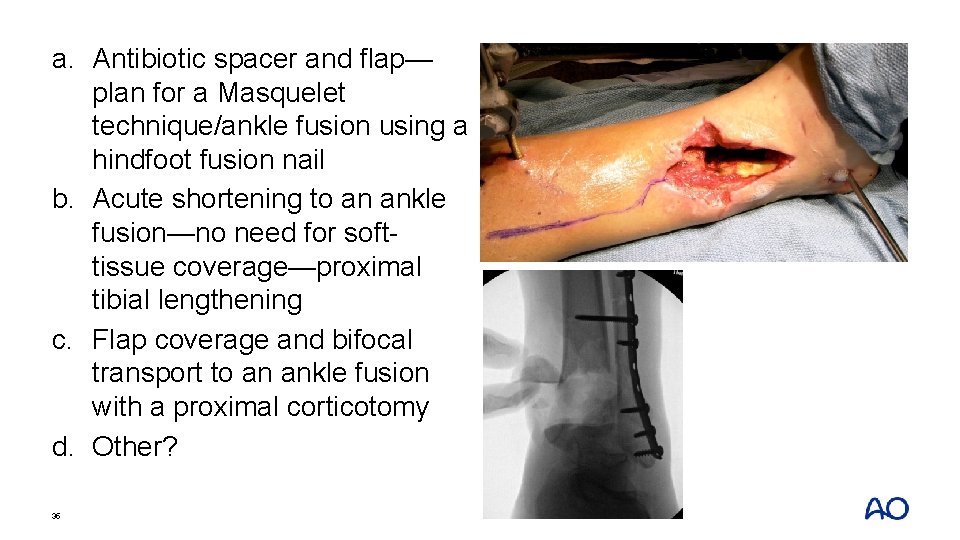
a. Antibiotic spacer and flap— plan for a Masquelet technique/ankle fusion using a hindfoot fusion nail b. Acute shortening to an ankle fusion—no need for softtissue coverage—proximal tibial lengthening c. Flap coverage and bifocal transport to an ankle fusion with a proximal corticotomy d. Other? 34
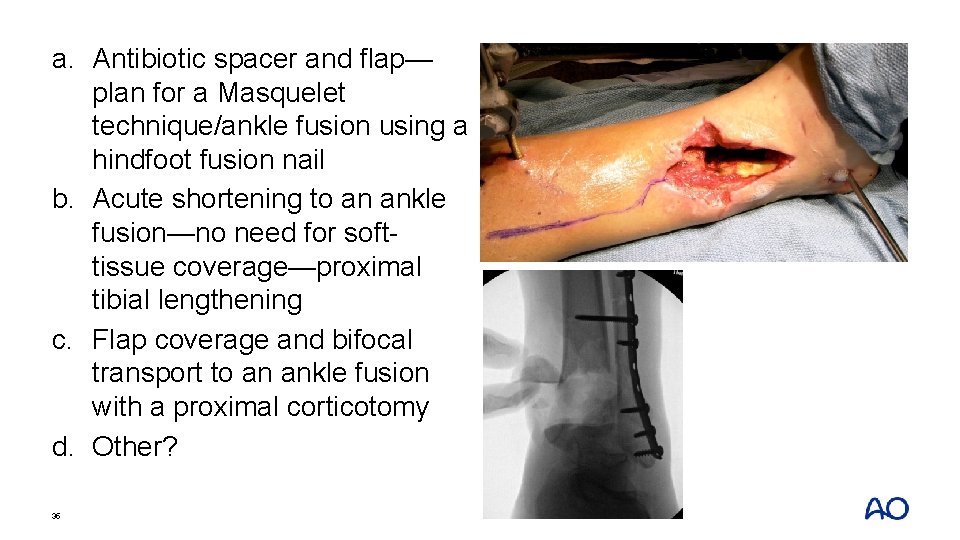
a. Antibiotic spacer and flap— plan for a Masquelet technique/ankle fusion using a hindfoot fusion nail b. Acute shortening to an ankle fusion—no need for softtissue coverage—proximal tibial lengthening c. Flap coverage and bifocal transport to an ankle fusion with a proximal corticotomy d. Other? 35
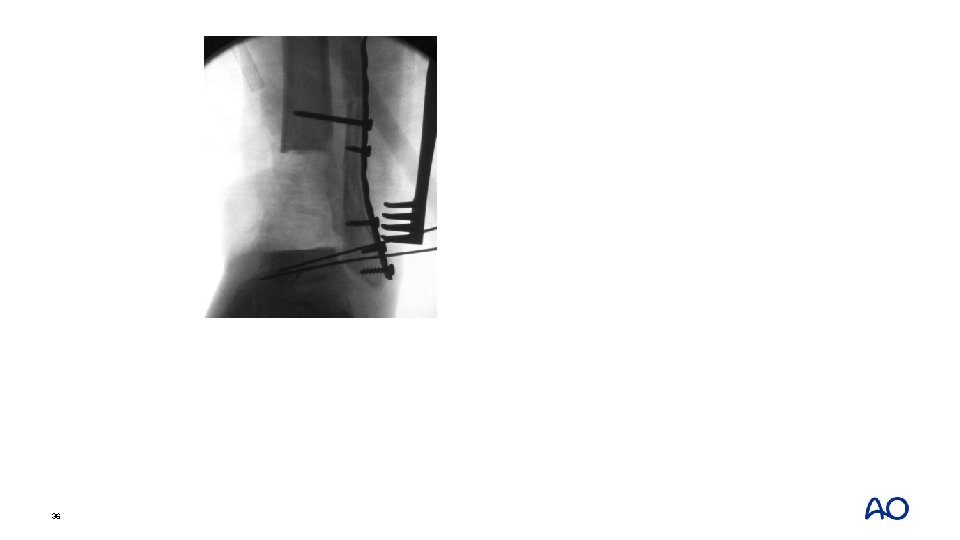
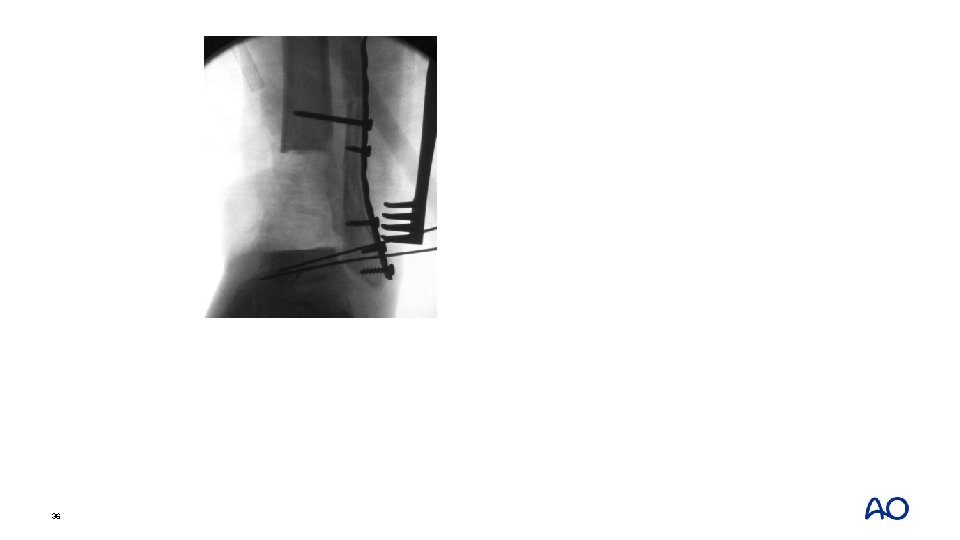
36
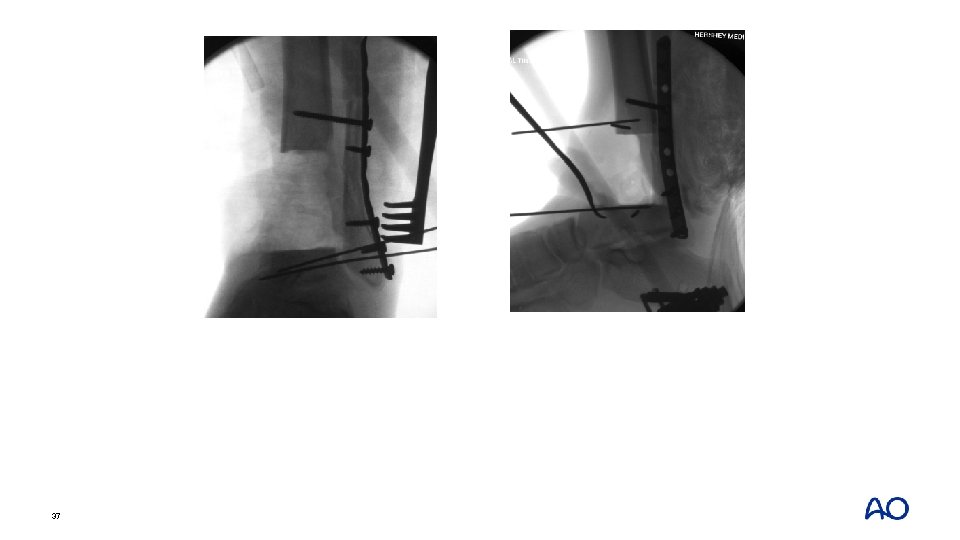
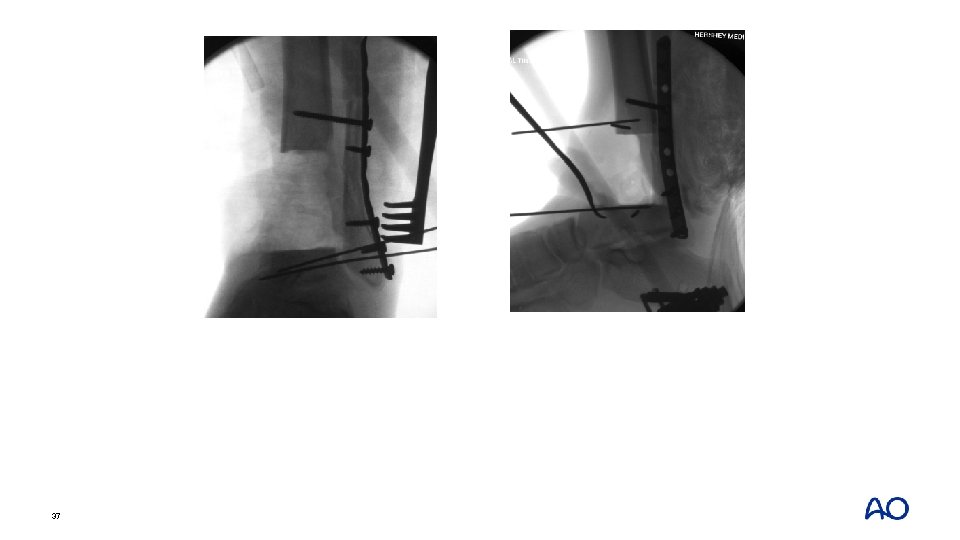
37
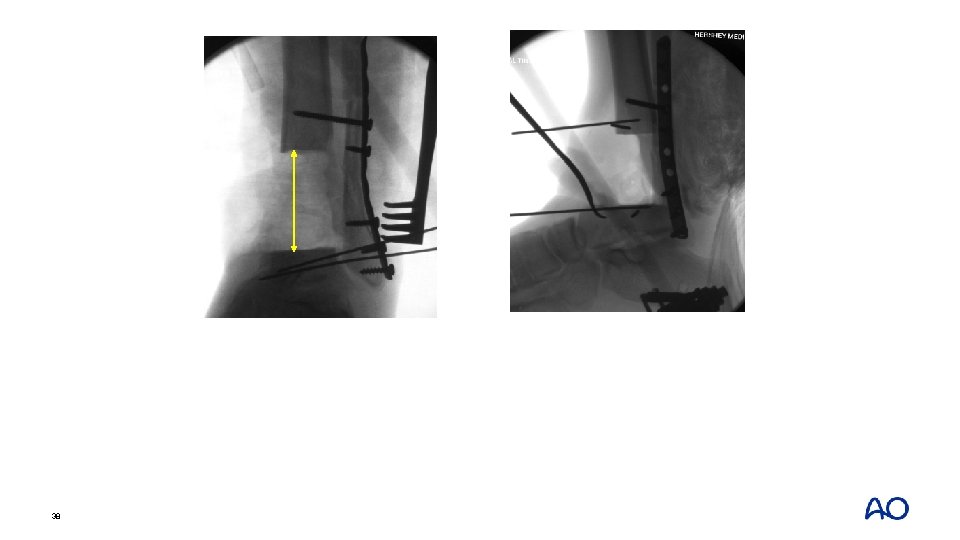
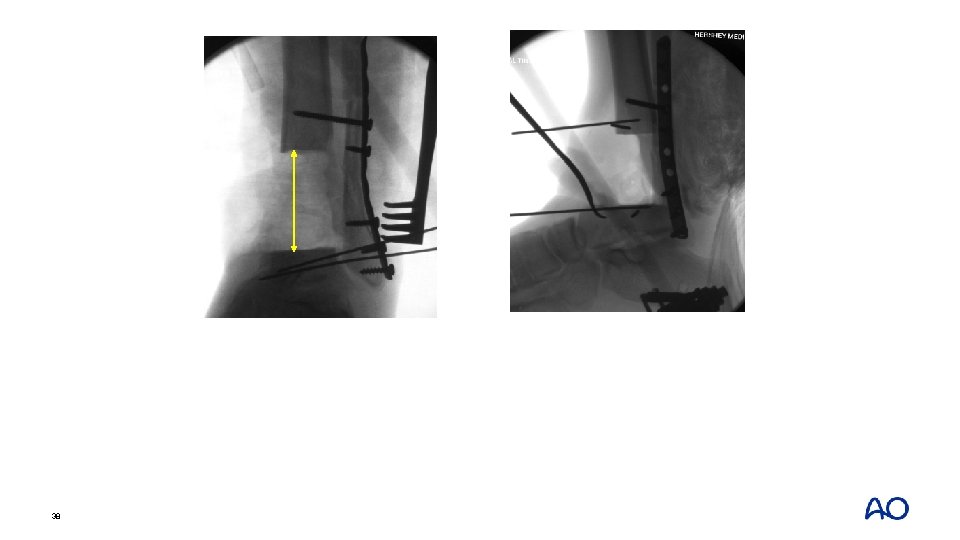
38
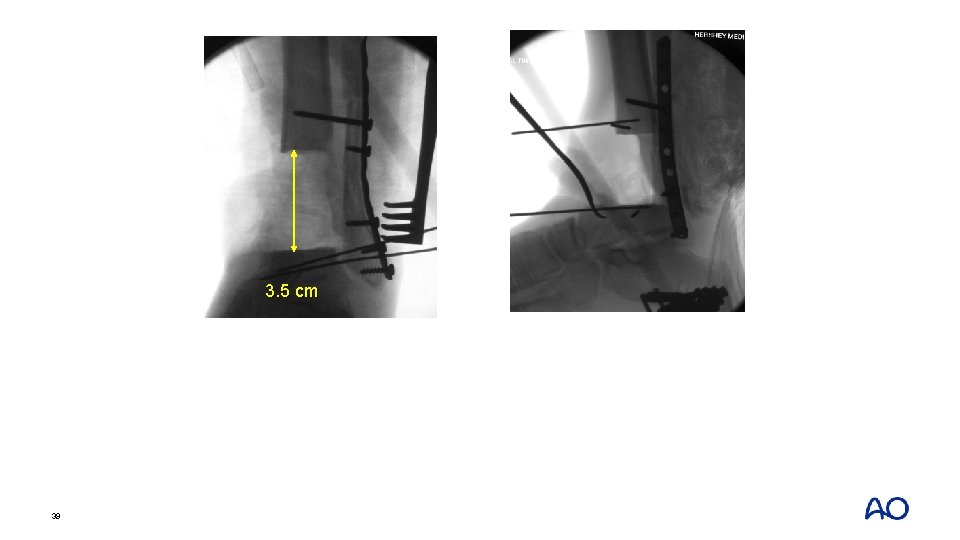
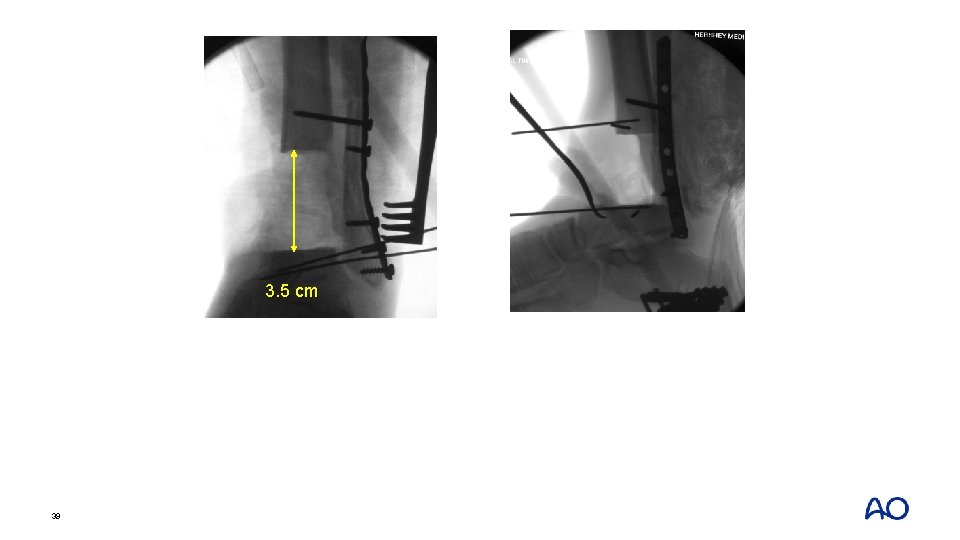
3. 5 cm 39
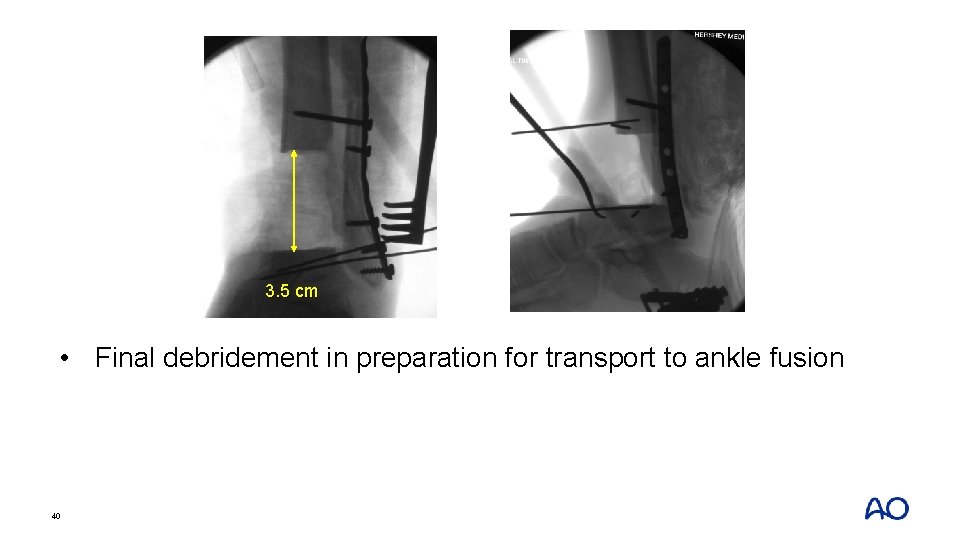
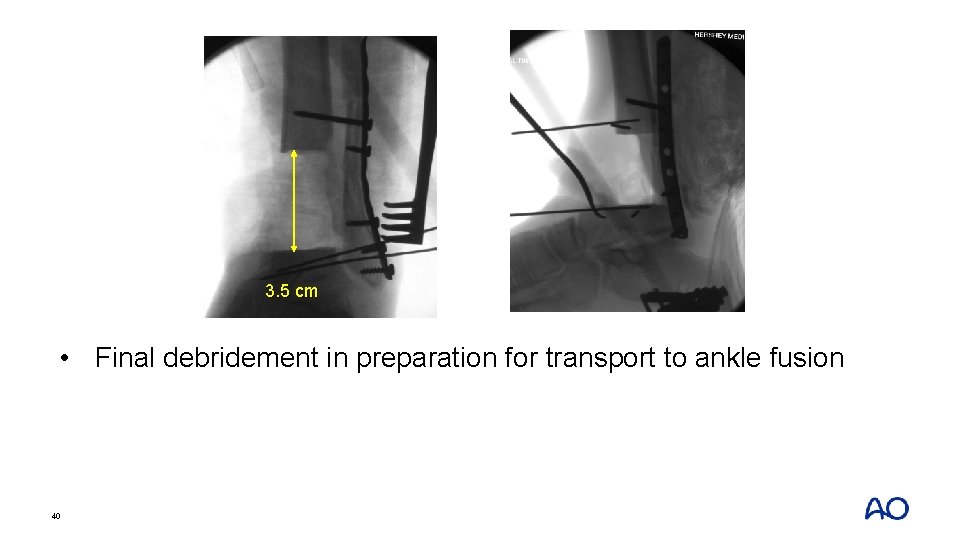
3. 5 cm • Final debridement in preparation for transport to ankle fusion 40
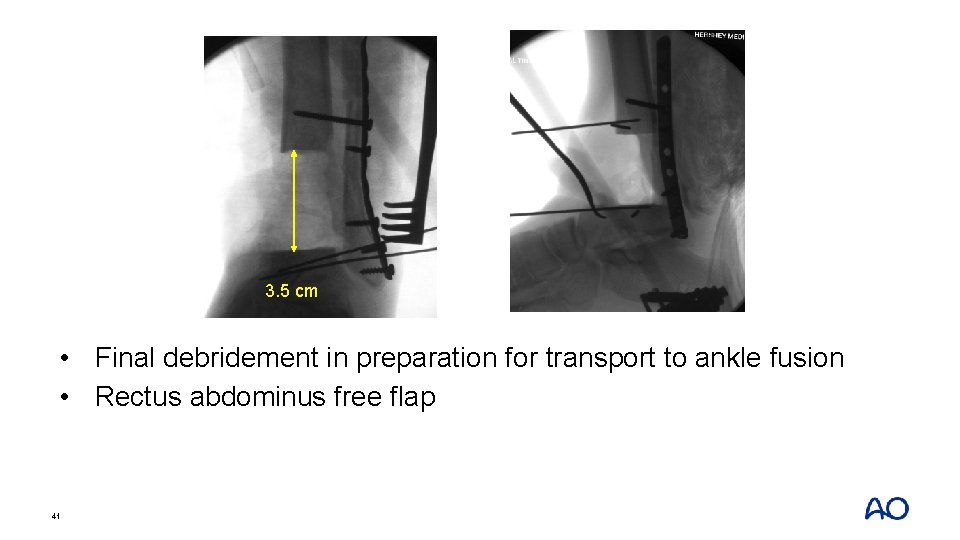
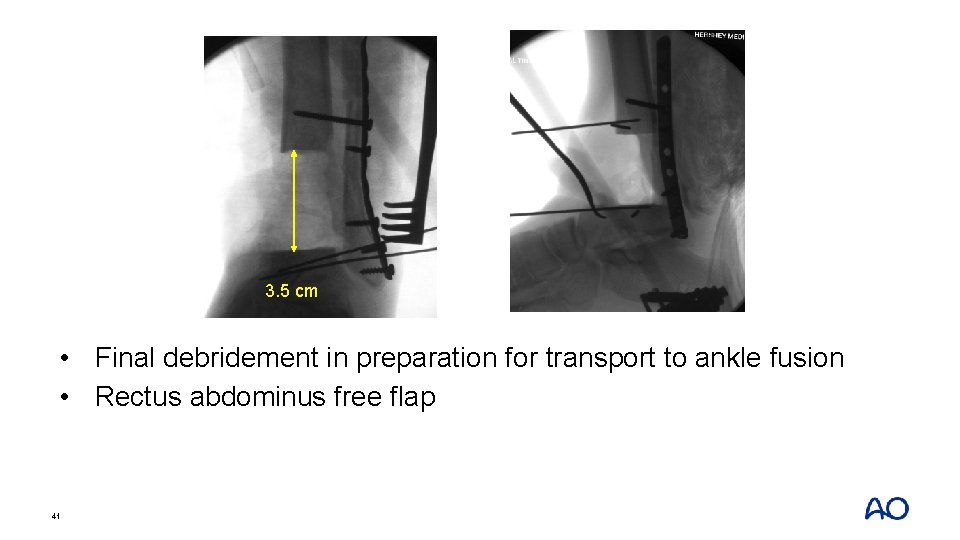
3. 5 cm • Final debridement in preparation for transport to ankle fusion • Rectus abdominus free flap 41
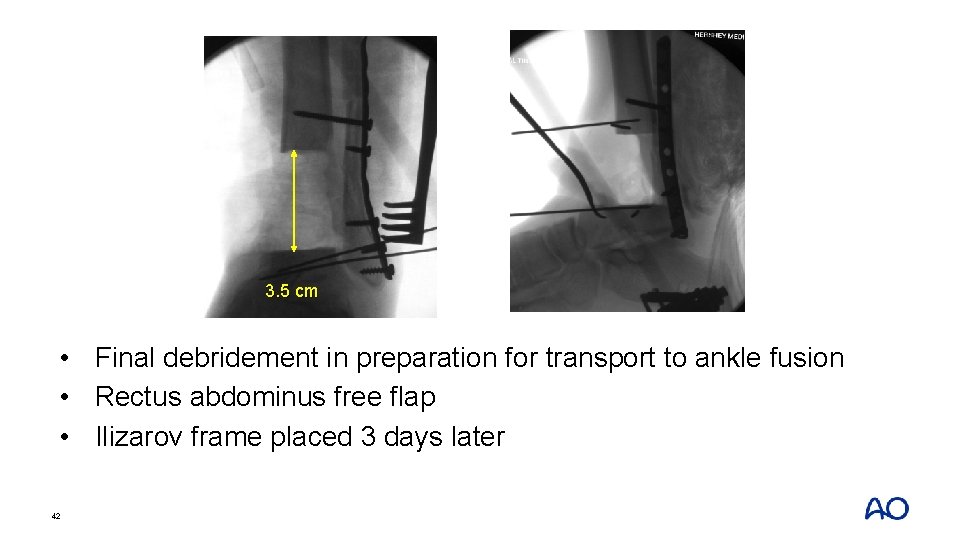
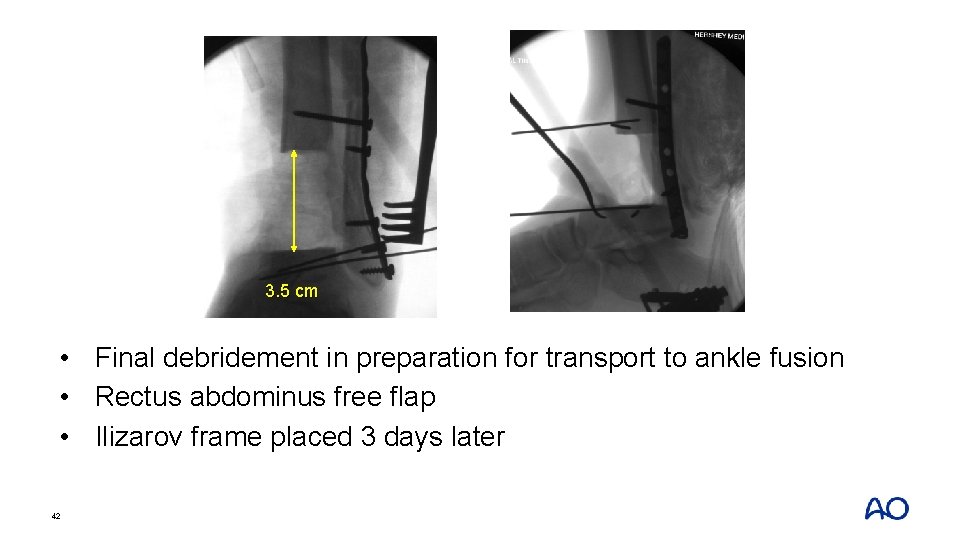
3. 5 cm • Final debridement in preparation for transport to ankle fusion • Rectus abdominus free flap • Ilizarov frame placed 3 days later 42

43
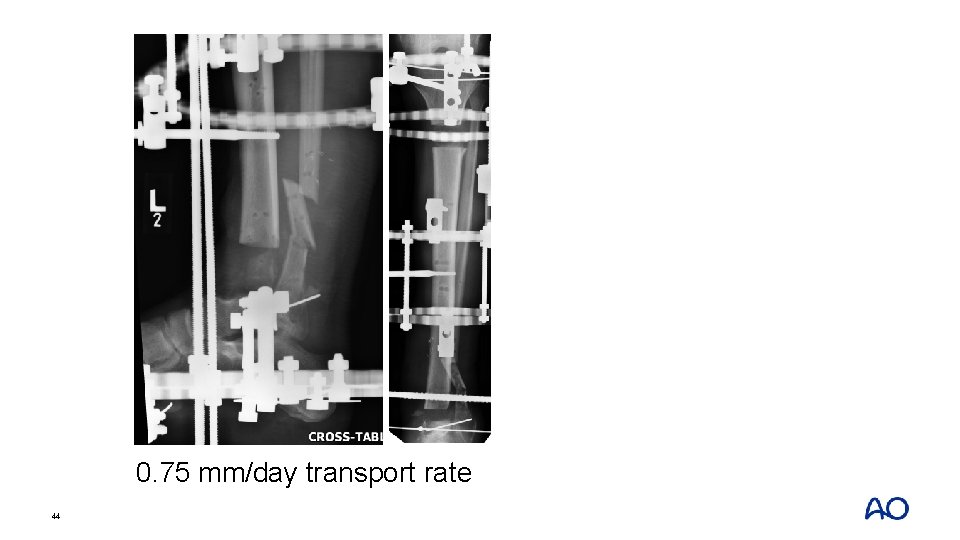
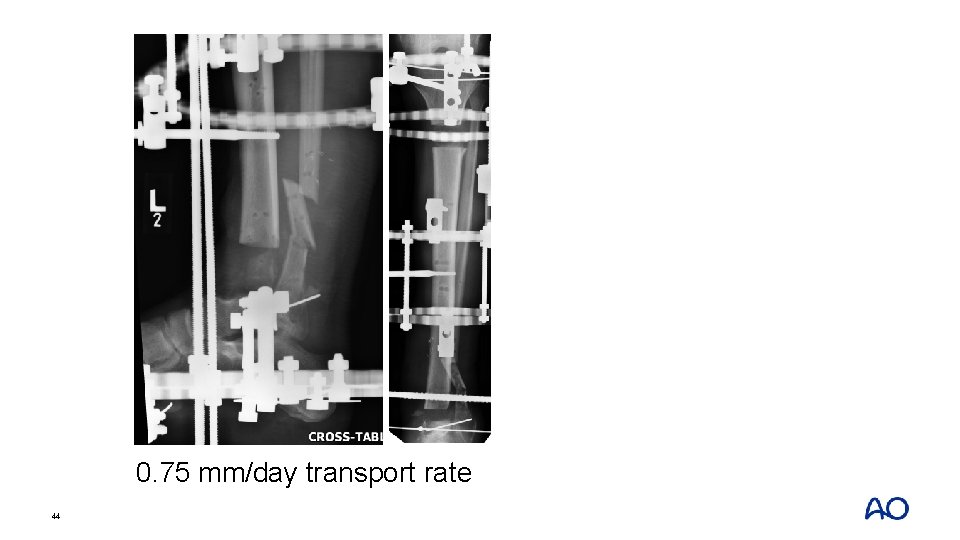
0. 75 mm/day transport rate 44
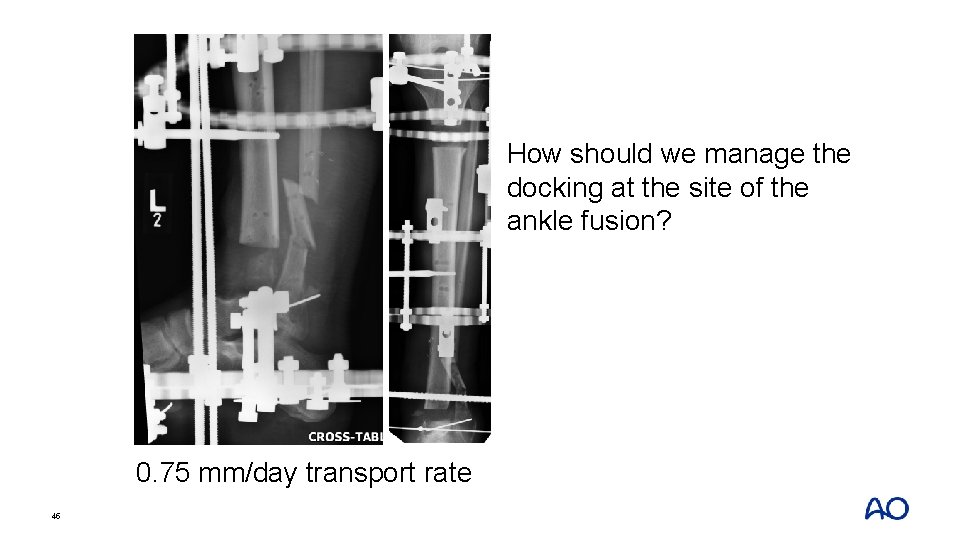
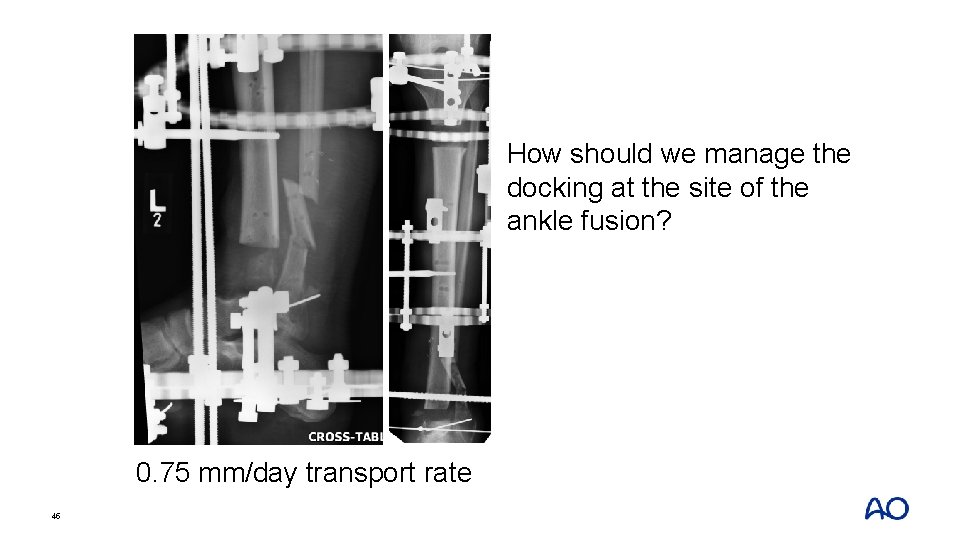
How should we manage the docking at the site of the ankle fusion? 0. 75 mm/day transport rate 45
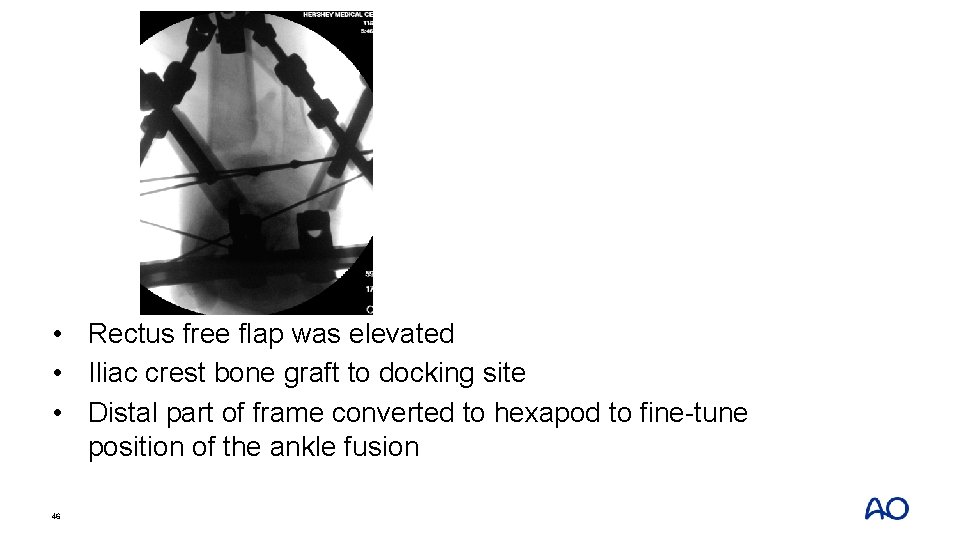
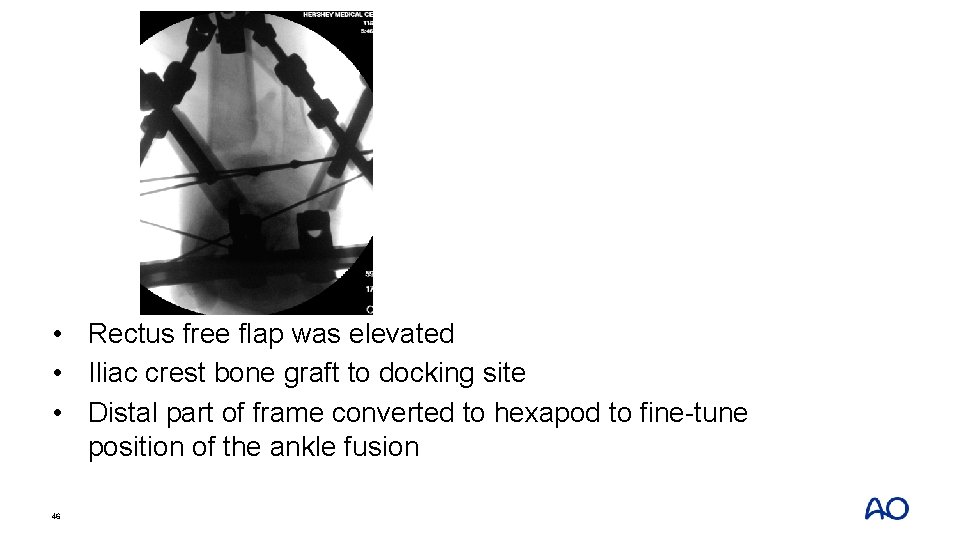
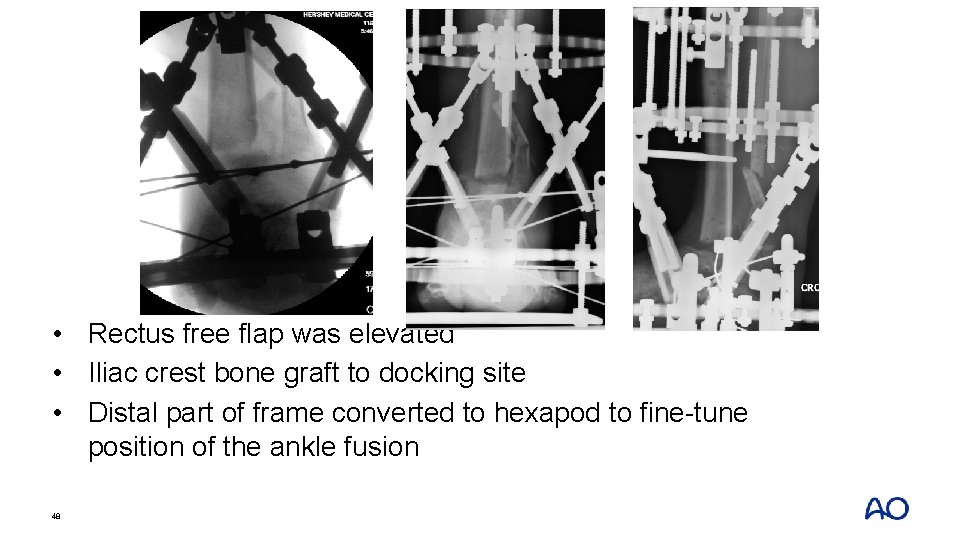
• Rectus free flap was elevated • Iliac crest bone graft to docking site • Distal part of frame converted to hexapod to fine-tune position of the ankle fusion 46
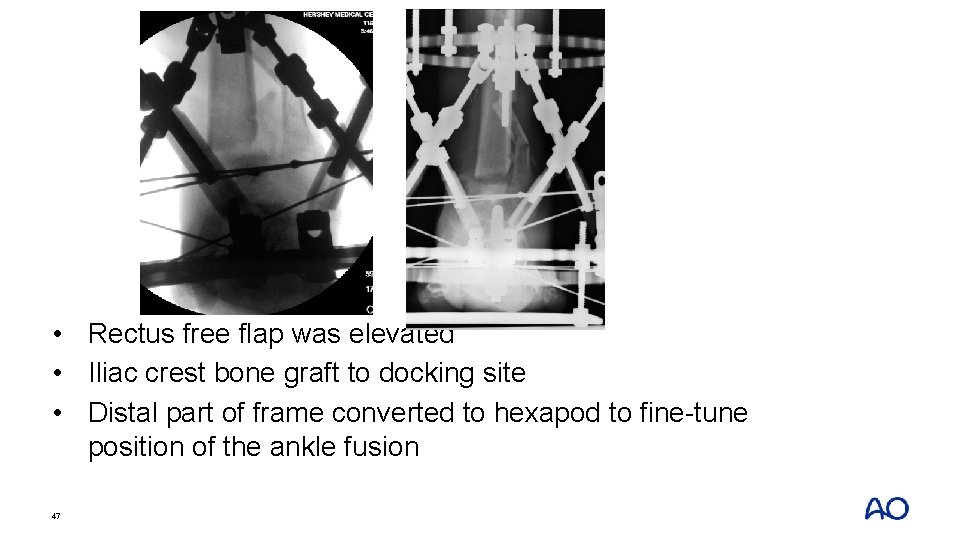
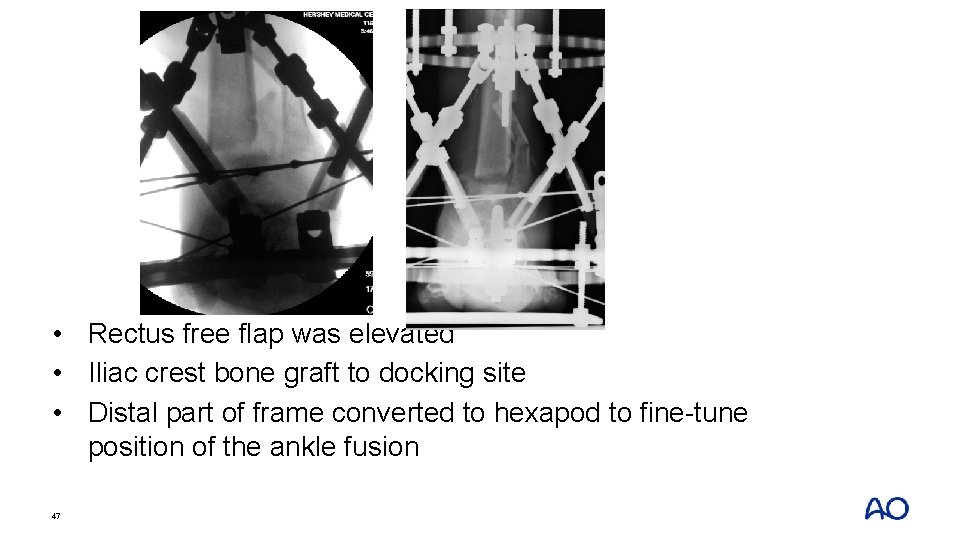
• Rectus free flap was elevated • Iliac crest bone graft to docking site • Distal part of frame converted to hexapod to fine-tune position of the ankle fusion 47
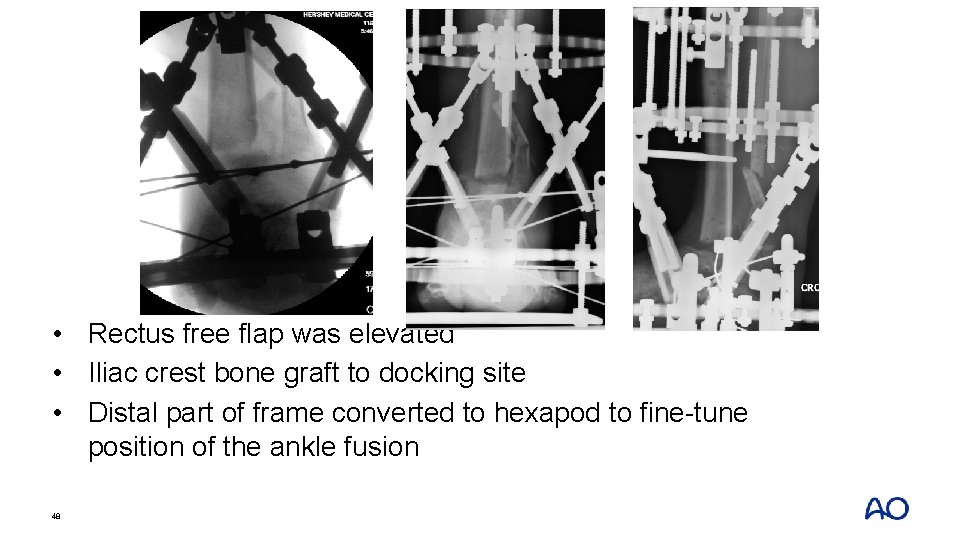
• Rectus free flap was elevated • Iliac crest bone graft to docking site • Distal part of frame converted to hexapod to fine-tune position of the ankle fusion 48
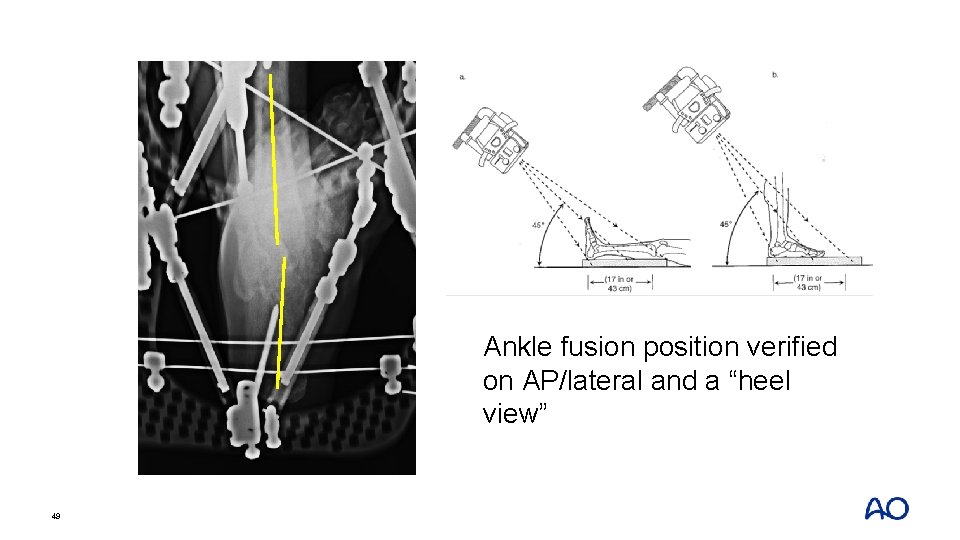
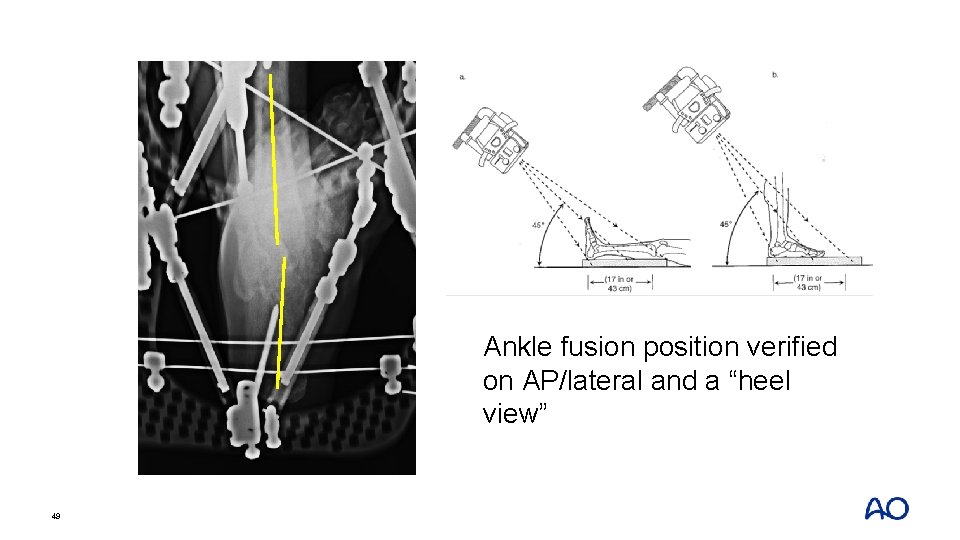
Ankle fusion position verified on AP/lateral and a “heel view” 49
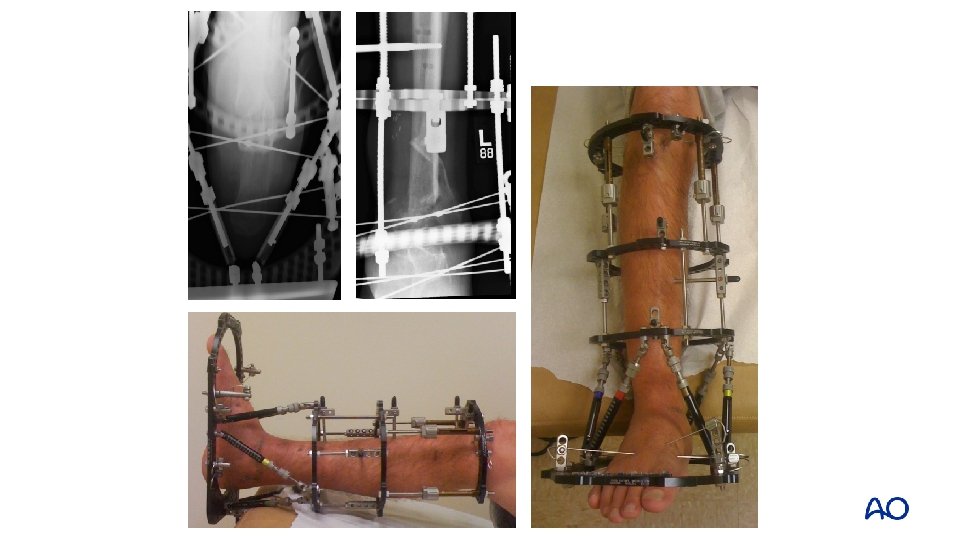

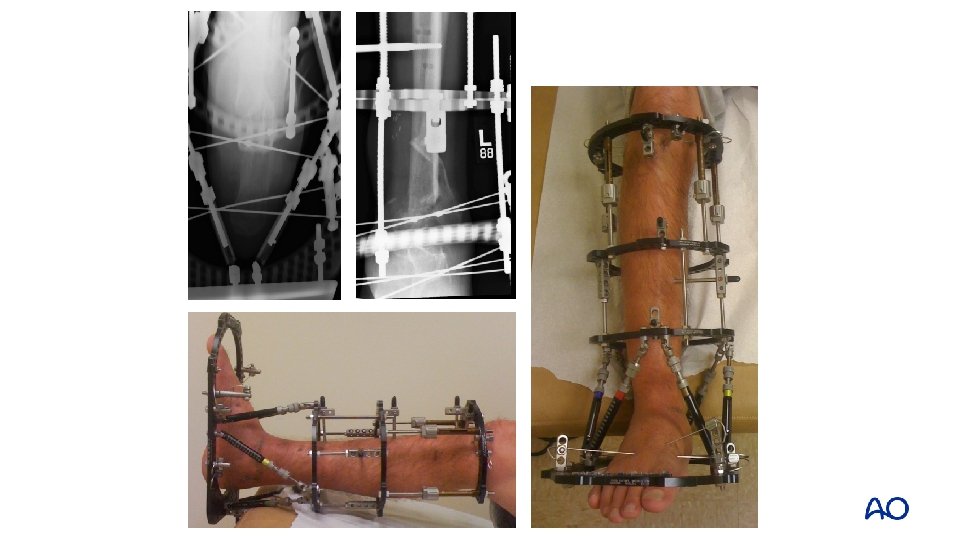
At 1 year 51
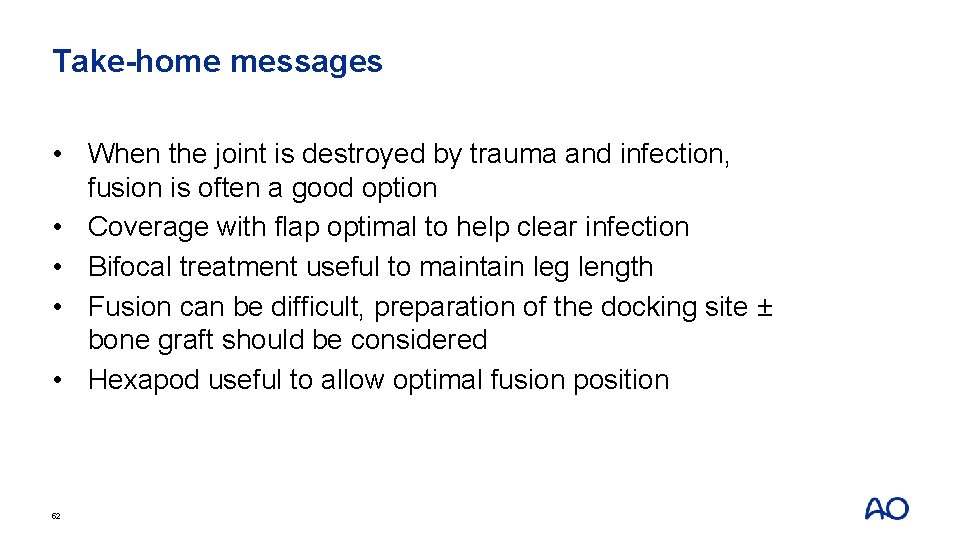
Take-home messages • When the joint is destroyed by trauma and infection, fusion is often a good option • Coverage with flap optimal to help clear infection • Bifocal treatment useful to maintain leg length • Fusion can be difficult, preparation of the docking site ± bone graft should be considered • Hexapod useful to allow optimal fusion position 52
Case 4: Pin tract infection and frame instability 53
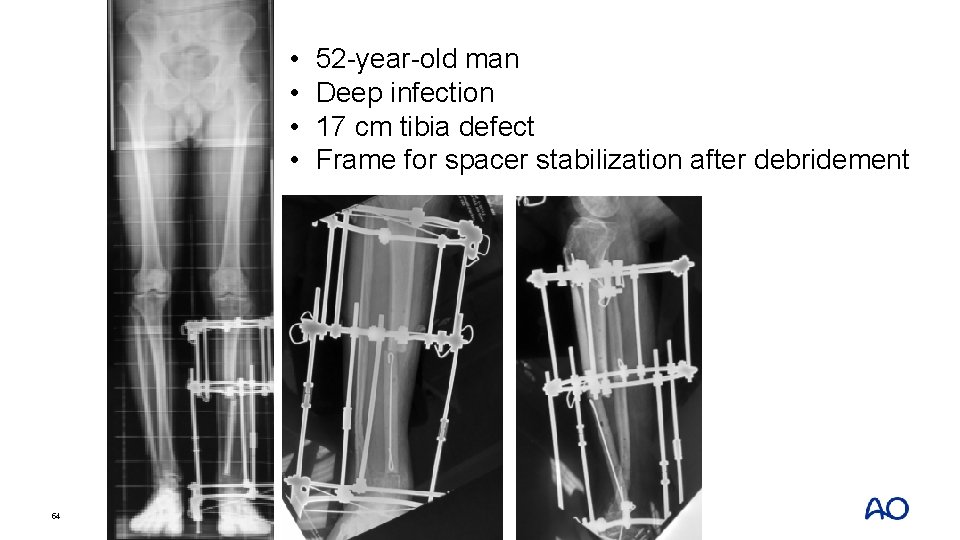
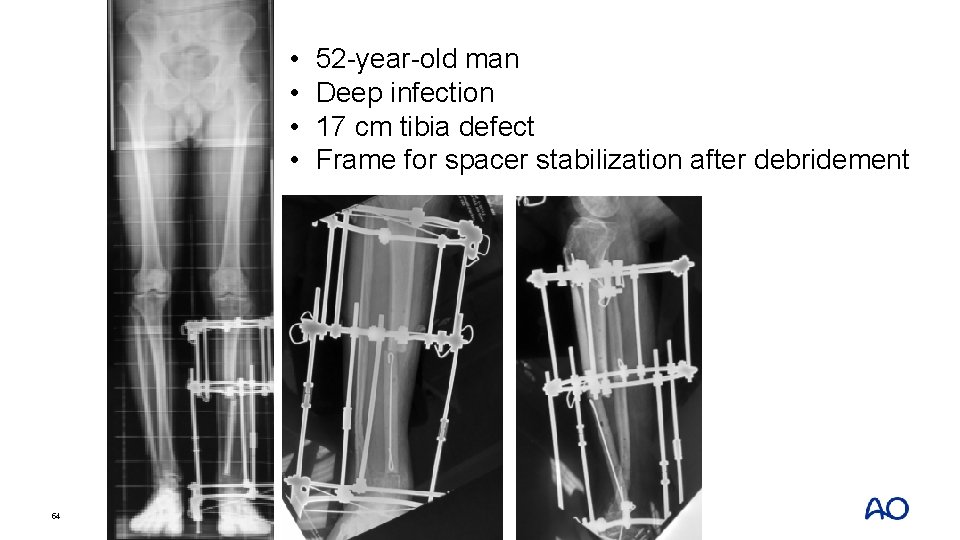
• • 54 52 -year-old man Deep infection 17 cm tibia defect Frame for spacer stabilization after debridement
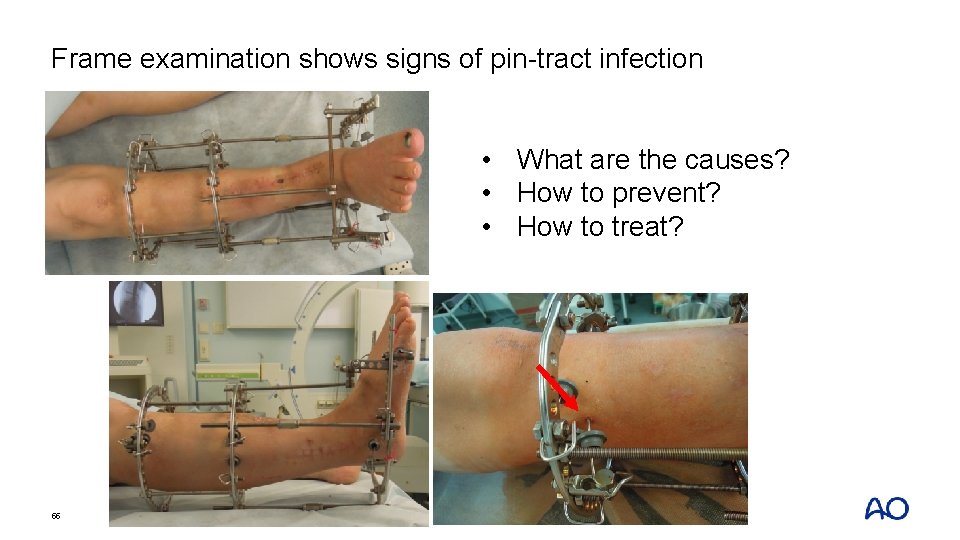
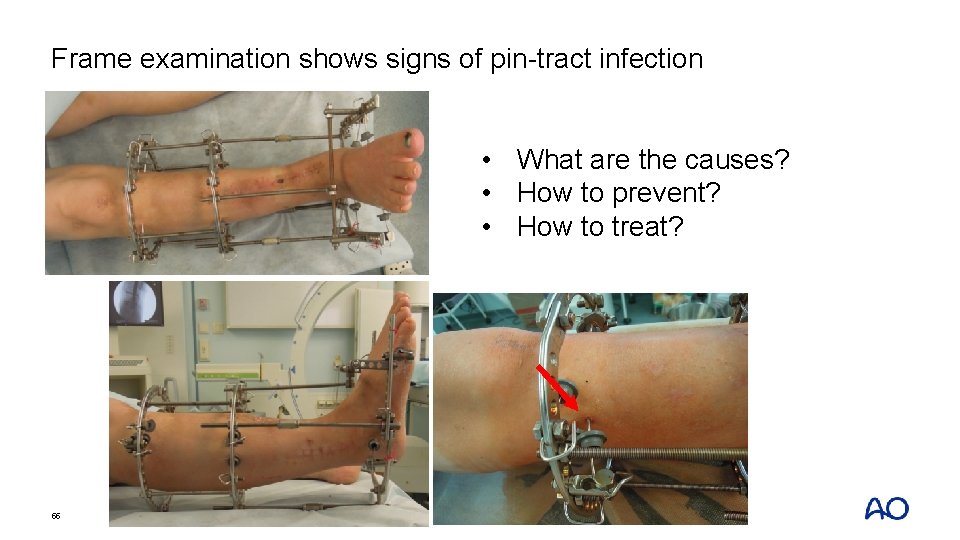
Frame examination shows signs of pin-tract infection • What are the causes? • How to prevent? • How to treat? 55
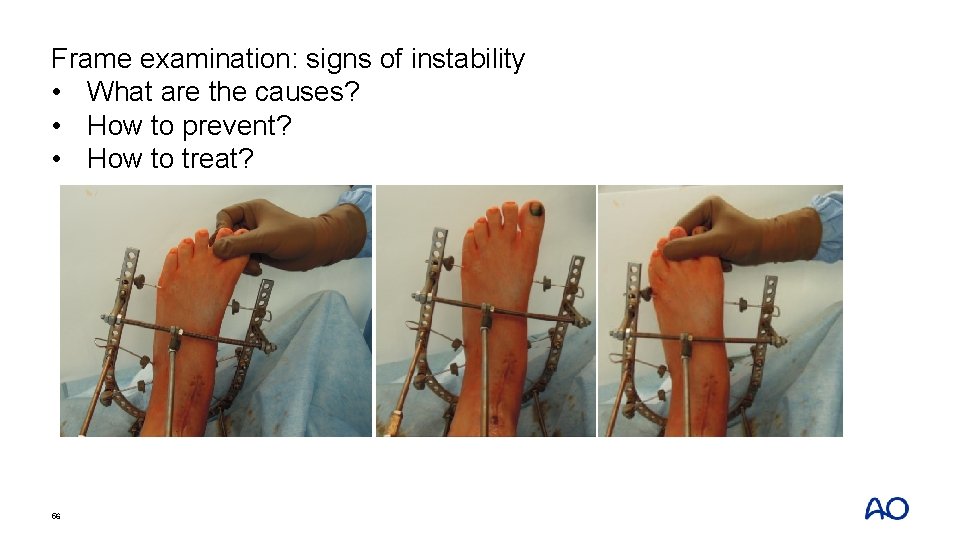
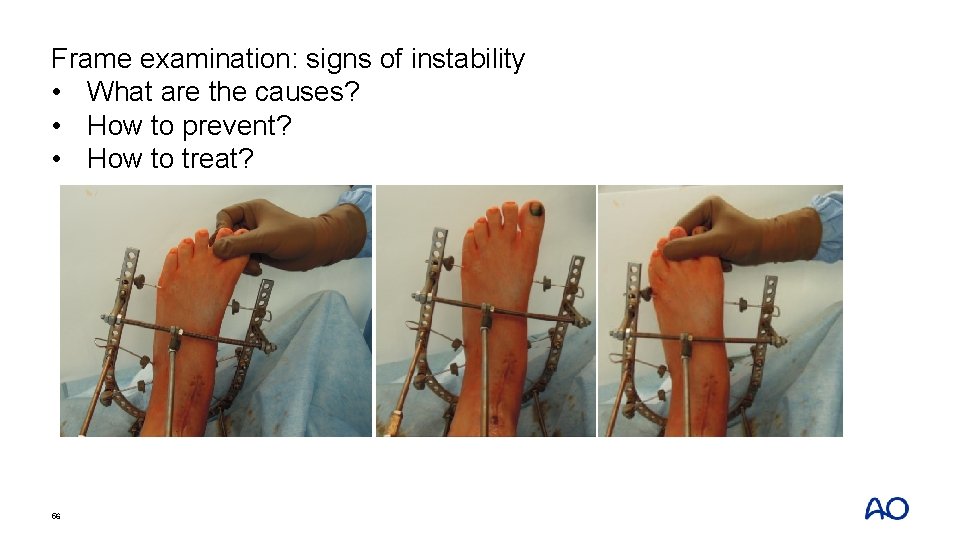
Frame examination: signs of instability • What are the causes? • How to prevent? • How to treat? 56
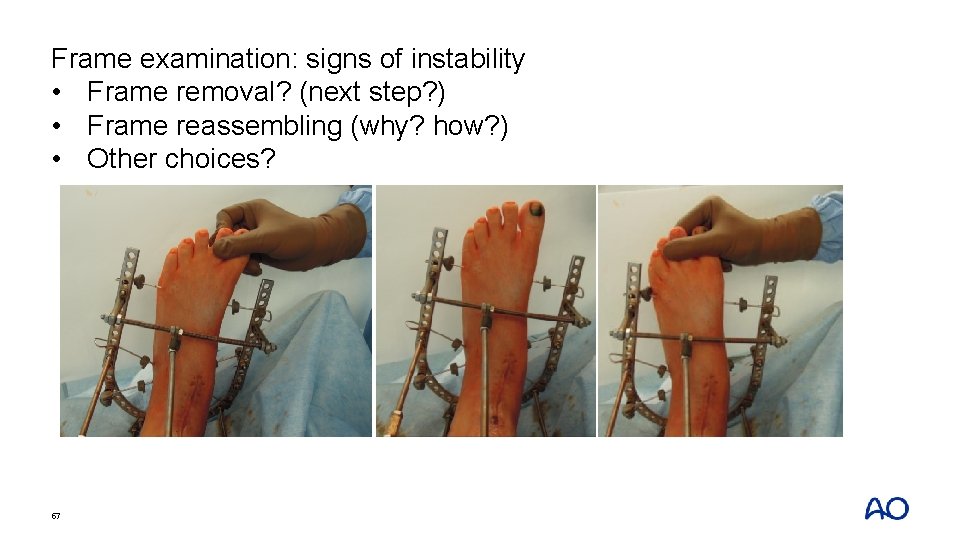
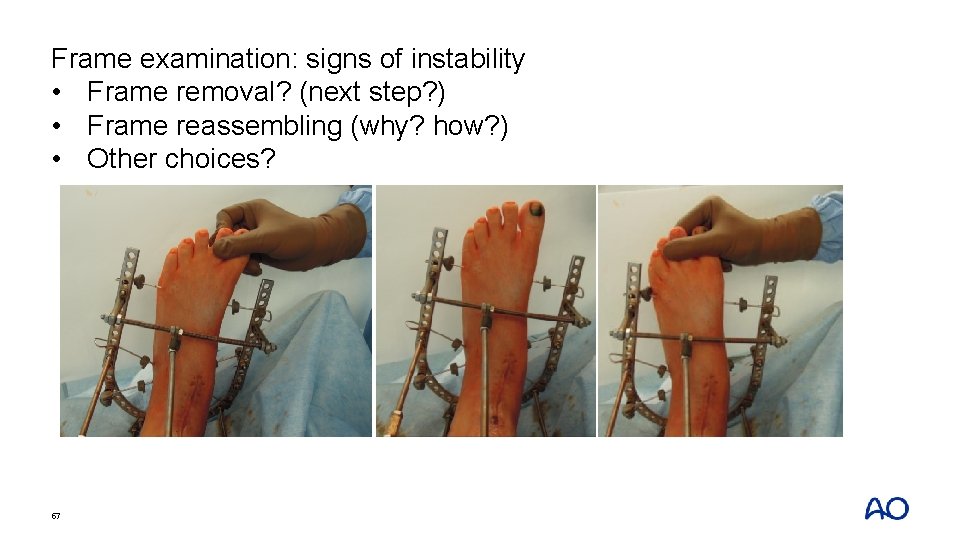
Frame examination: signs of instability • Frame removal? (next step? ) • Frame reassembling (why? how? ) • Other choices? 57
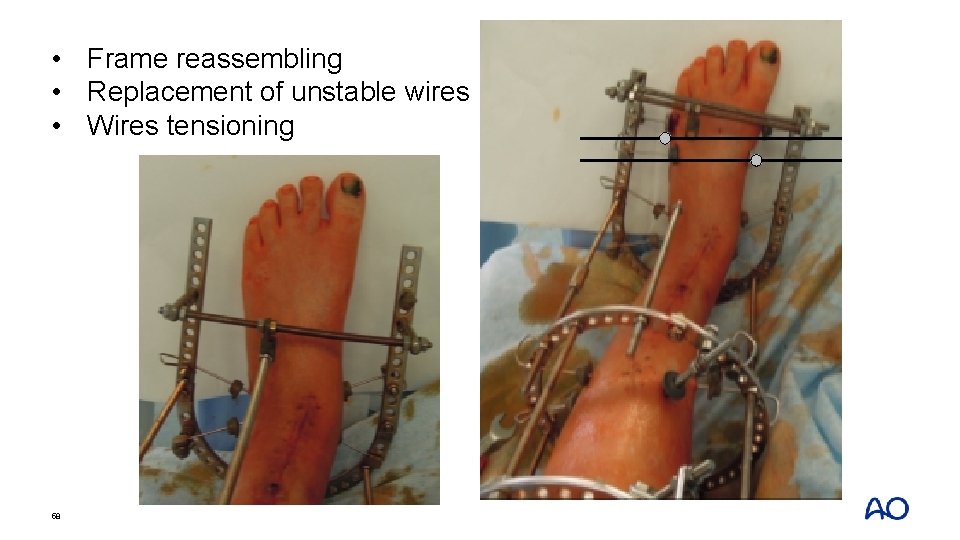
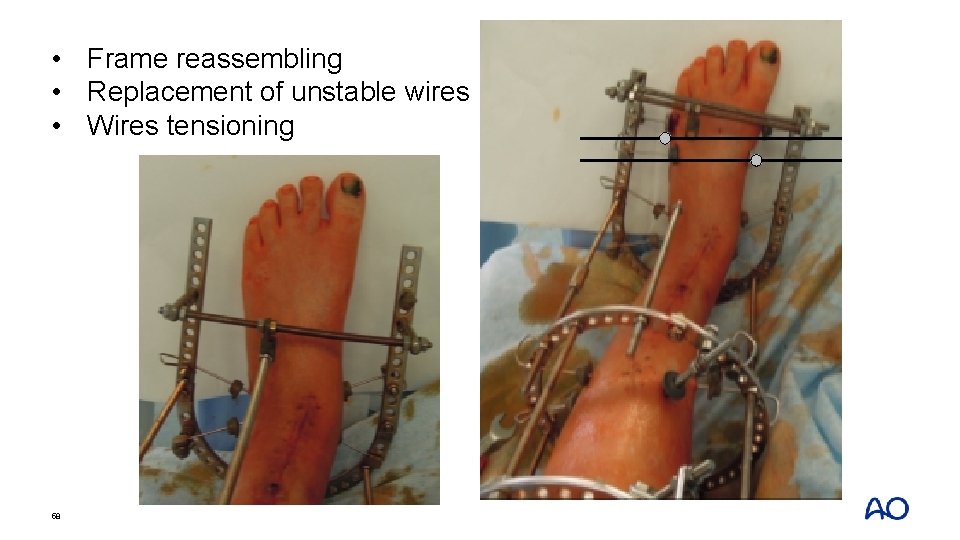
• Frame reassembling • Replacement of unstable wires • Wires tensioning 58
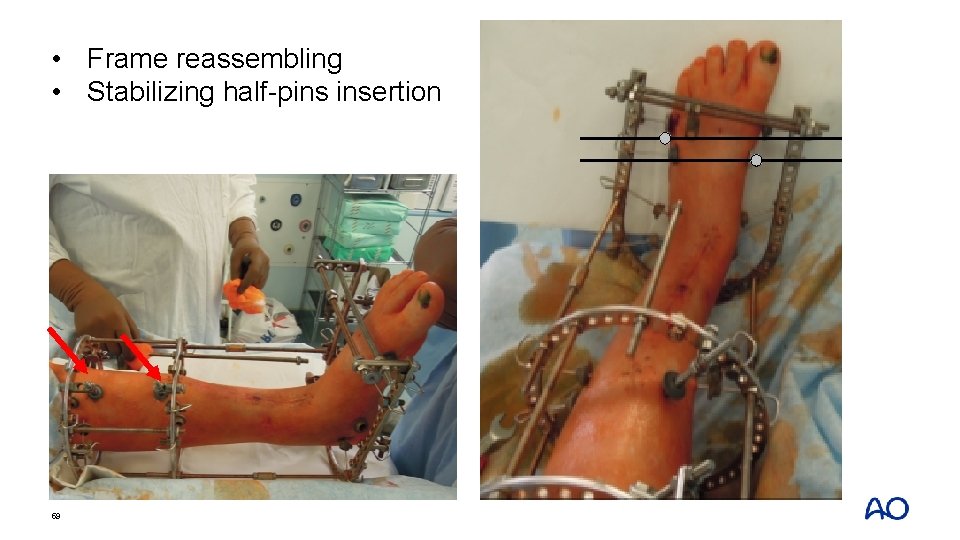
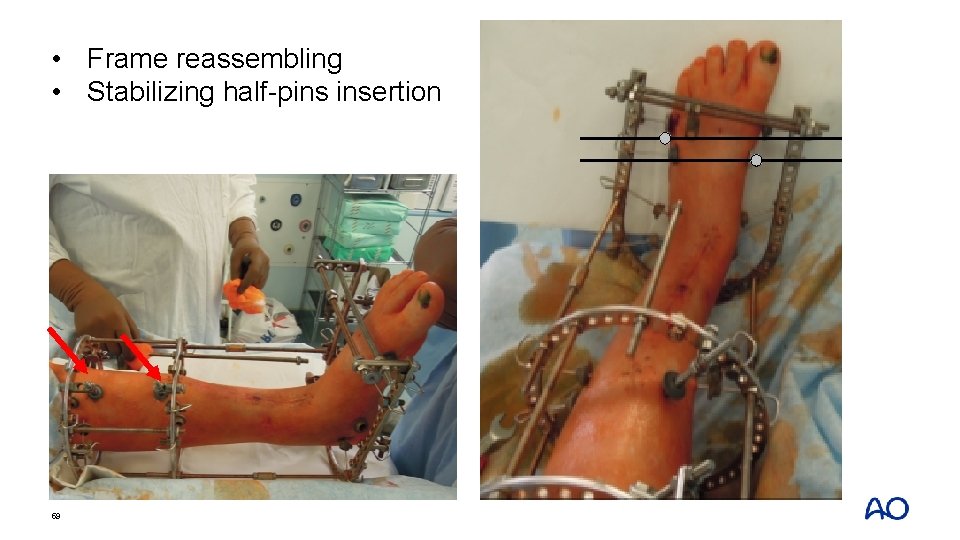
• Frame reassembling • Stabilizing half-pins insertion 59
Take-home messages • One of the causes of wire sites infection is unstable frame • Unstable frame will be infected frame soon (100%) • Needed level of stability depends on the purpose of using the frame (damage control orthopedics ≠ reconstructive surgery, needs more stability) • Proper level of stability must be provided with minimal number of wires, pins, and rings 60