Principles of External Fixation Roman Hayda MD Original



















- Slides: 70
Principles of External Fixation Roman Hayda, MD Original Authors: Alvin Ong, MD & Roman Hayda, MD; March 2004; New Author: Roman Hayda, MD; Revised November, 2008
Overview • • • Indications Advantages and disadvantages Mechanics Biology Complications
Indications • Definitive fx care: • Open fractures • Peri-articular fractures • Pediatric fractures • Temporary fx care • “Damage control” – Long bone fracture temporization • Pelvic ring injury • Periarticular fractures – Pilon fracture • • Malunion/nonunion Arthrodesis Osteomyelitis Limb deformity/length inequality • Congenital • Acquired

Advantages • • Minimally invasive Flexibility (build to fit) Quick application Complex 3 -C humerus fx Useful both as a temporizing or definitive stabilization device • Reconstructive and salvage applications
Disadvantages • Mechanical – – – Distraction of fracture site Inadequate immobilization Pin-bone interface failure Weight/bulk Refracture (pediatric femur) • Biologic May result in malunion/nonunion, loss of function – Infection (pin track) • May preclude conversion to IM nailing or internal fixation – Neurovascular injury – Tethering of muscle – Soft tissue contracture
Components of the Ex-fix • Pins • Clamps • Connecting rods
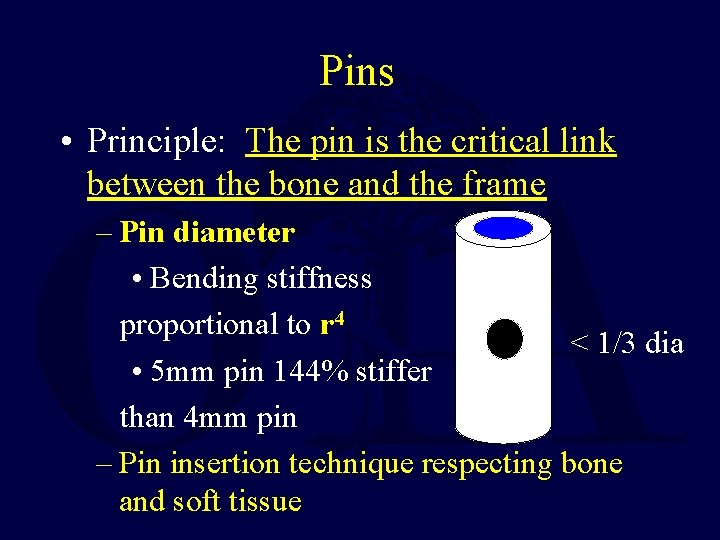
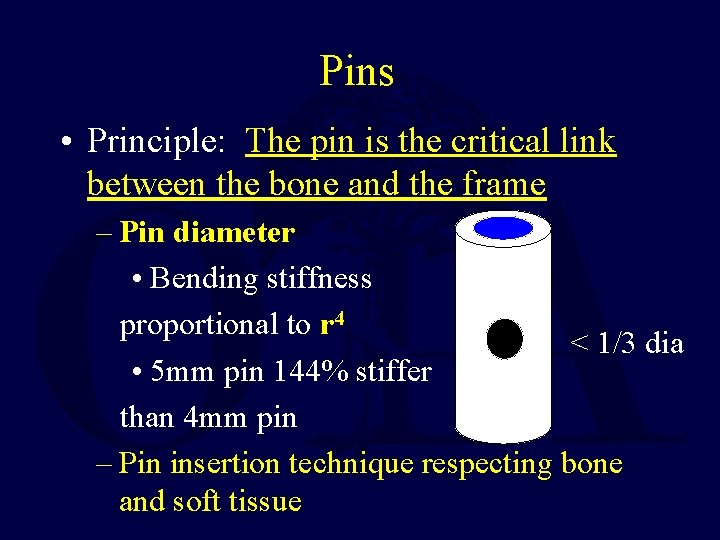
Pins • Principle: The pin is the critical link between the bone and the frame – Pin diameter • Bending stiffness proportional to r 4 < 1/3 dia • 5 mm pin 144% stiffer than 4 mm pin – Pin insertion technique respecting bone and soft tissue
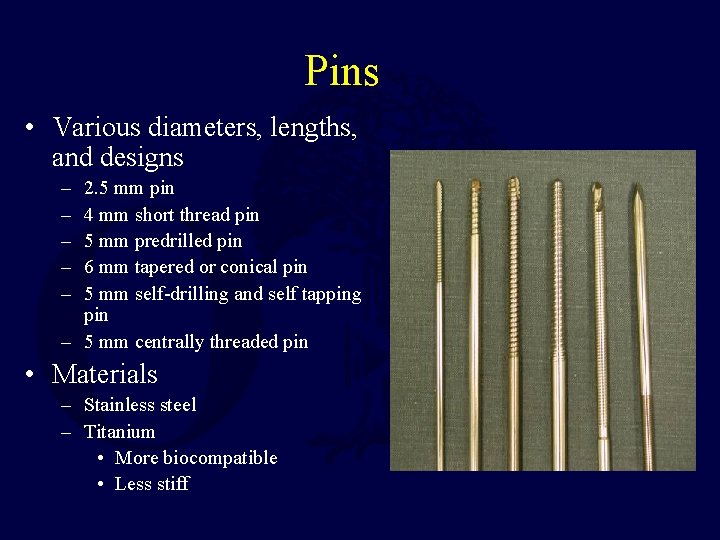
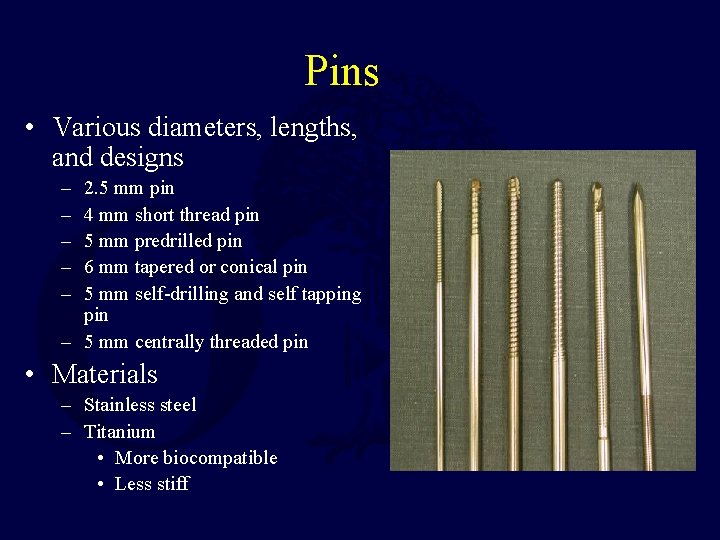
Pins • Various diameters, lengths, and designs – – – 2. 5 mm pin 4 mm short thread pin 5 mm predrilled pin 6 mm tapered or conical pin 5 mm self-drilling and self tapping pin – 5 mm centrally threaded pin • Materials – Stainless steel – Titanium • More biocompatible • Less stiff
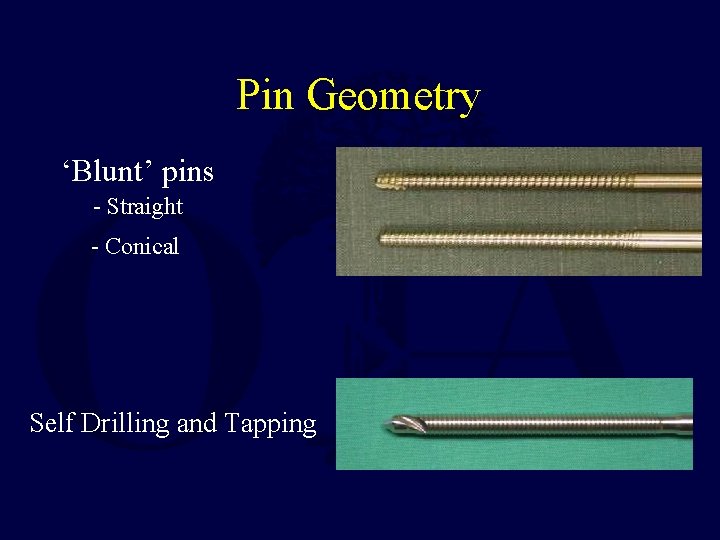
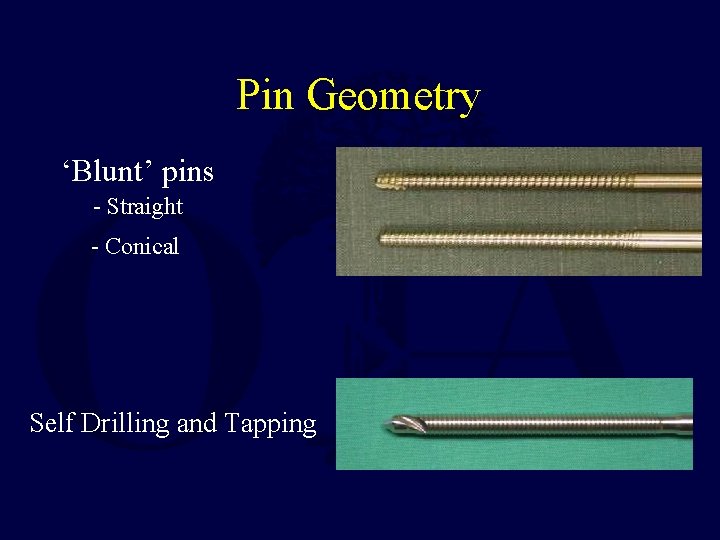
Pin Geometry ‘Blunt’ pins - Straight - Conical Self Drilling and Tapping

Pin coatings • Recent development of various coatings (Chlorohexidine, Silver, Hydroxyapatite) – Improve fixation to bone – Decrease infection – Moroni, JOT, ’ 02 • Animal study, HA pin 13 X higher extraction torque vs stainless and titanium and equal to insertion torque – Moroni, JBJS A, ’ 05 • 0/50 pts pin infection in tx of pertrochanteric fx
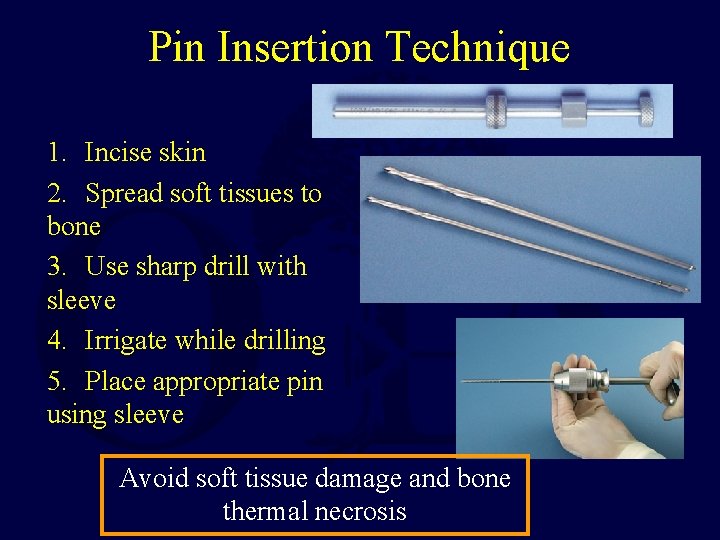
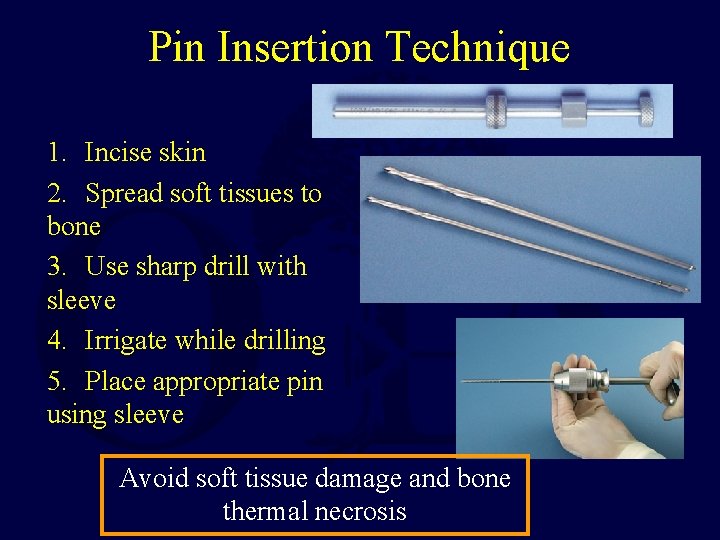
Pin Insertion Technique 1. Incise skin 2. Spread soft tissues to bone 3. Use sharp drill with sleeve 4. Irrigate while drilling 5. Place appropriate pin using sleeve Avoid soft tissue damage and bone thermal necrosis

Pin insertion • Self drilling pin considerations – Short drill flutes • thermal necrosis • stripping of near cortex with far cortex contact – Quick insertion – Useful for short term applications vs.
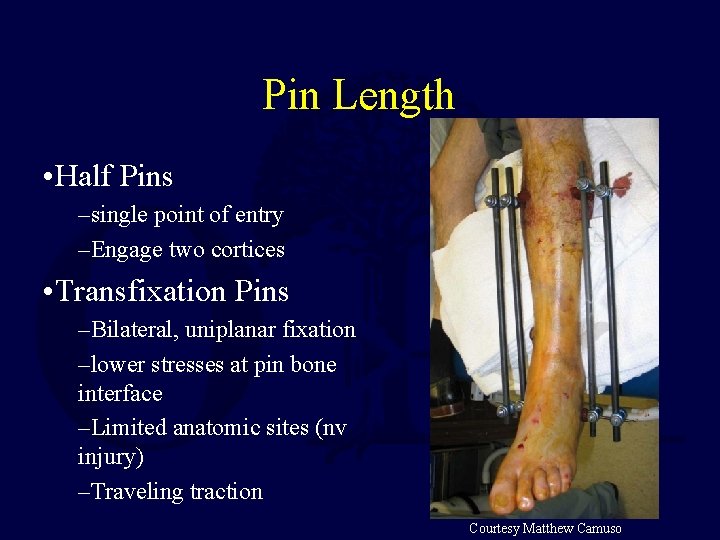
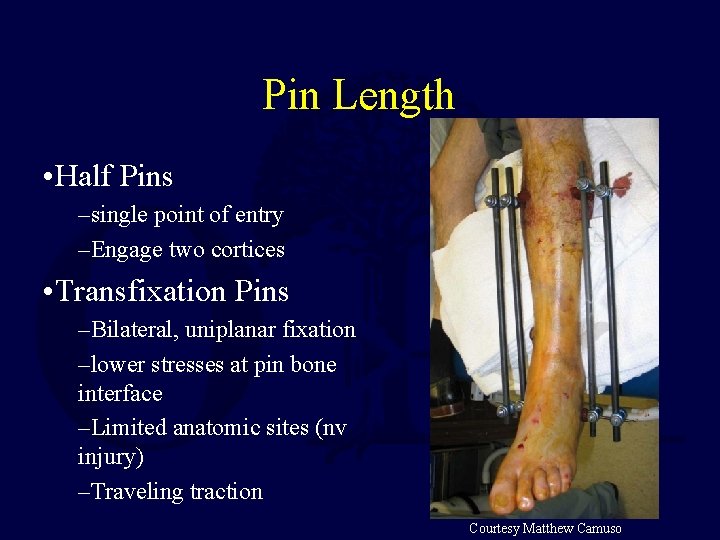
Pin Length • Half Pins –single point of entry –Engage two cortices • Transfixation Pins –Bilateral, uniplanar fixation –lower stresses at pin bone interface –Limited anatomic sites (nv injury) –Traveling traction Courtesy Matthew Camuso

Pin Diameter Guidelines • Femur – 5 or 6 mm • Tibia – 5 or 6 mm • Humerus – 5 mm • Forearm – 4 mm • Hand, Foot – 3 mm < 1/3 dia Slide courtesy Matthew Camuso

Clamps • Two general varieties: – Single pin to bar clamps – Multiple pin to bar clamps • Features: – Multi-planar adjustability – Open vs closed end • Principles – Must securely hold the frame to the pin – Clamps placed closer to bone increases the stiffness of the entire fixator construct

Connecting Rods and/or Frames • Options: – materials: • Steel • Aluminum • Carbon fiber – Design • Simple rod • Articulated • Telescoping • Principle – increased diameter = increased stiffness and strength – Stacked (2 parallel bars) = increased stiffness
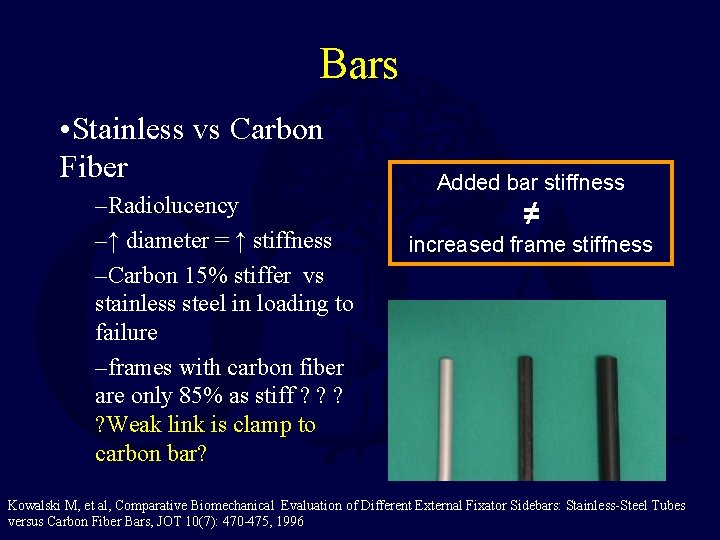
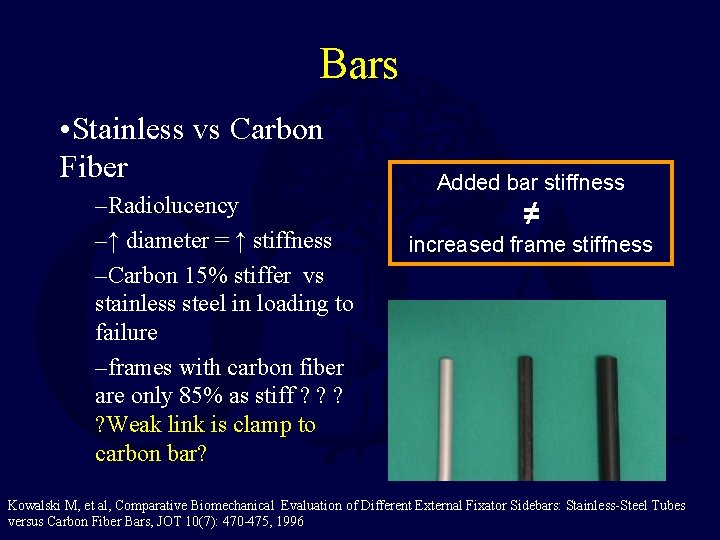
Bars • Stainless vs Carbon Fiber –Radiolucency –↑ diameter = ↑ stiffness –Carbon 15% stiffer vs stainless steel in loading to failure –frames with carbon fiber are only 85% as stiff ? ? ? ? Weak link is clamp to carbon bar? Added bar stiffness ≠ increased frame stiffness Kowalski M, et al, Comparative Biomechanical Evaluation of Different External Fixator Sidebars: Stainless-Steel Tubes versus Carbon Fiber Bars, JOT 10(7): 470 -475, 1996
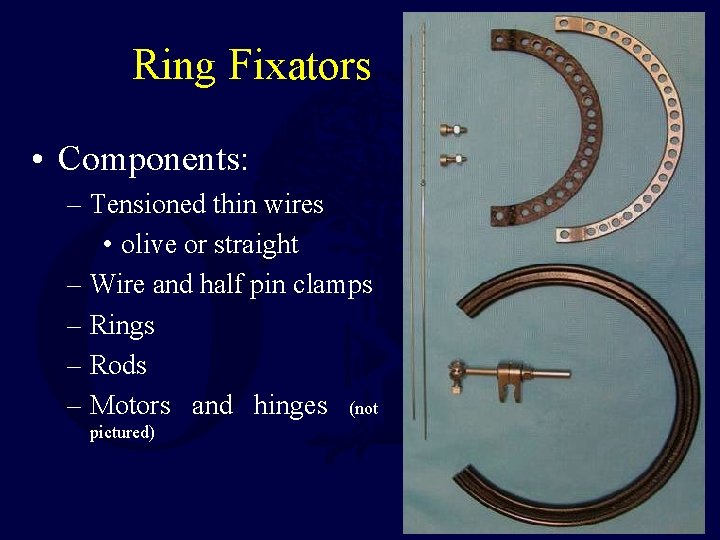
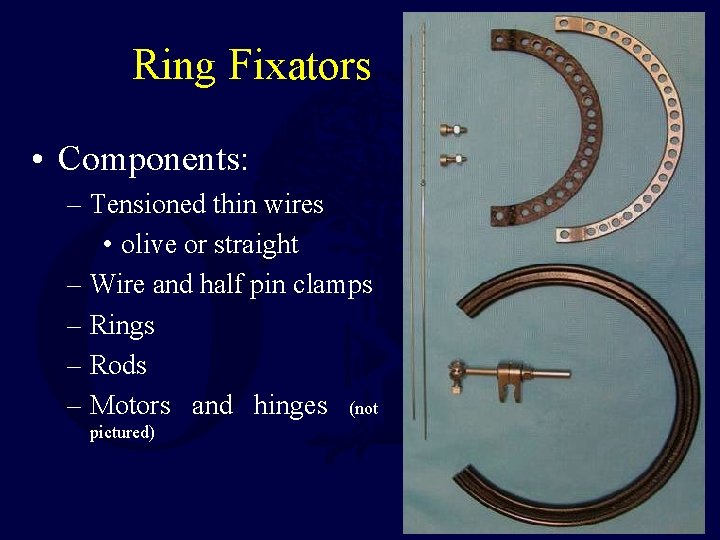
Ring Fixators • Components: – Tensioned thin wires • olive or straight – Wire and half pin clamps – Rings – Rods – Motors and hinges (not pictured)
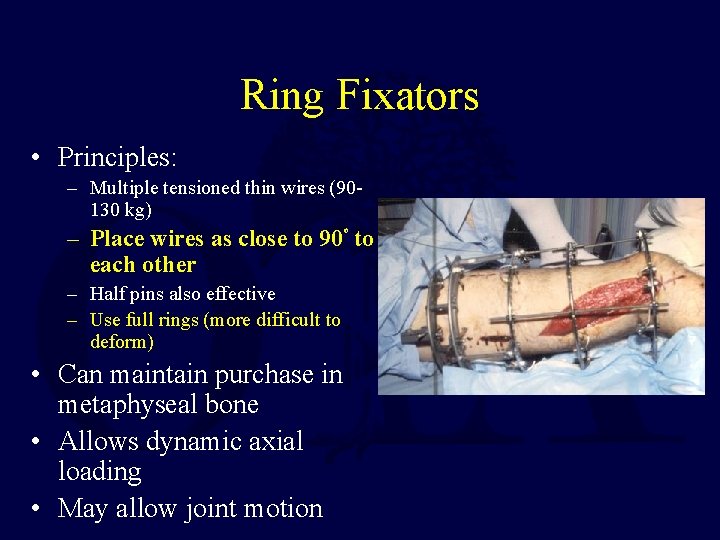
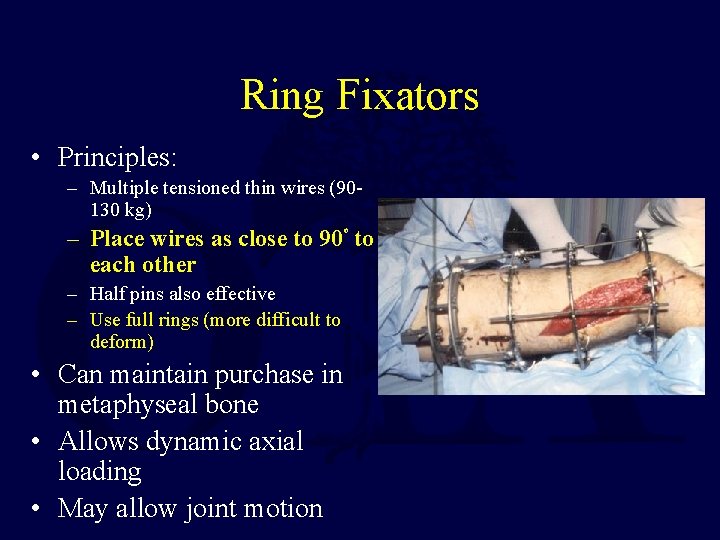
Ring Fixators • Principles: – Multiple tensioned thin wires (90130 kg) – Place wires as close to 90 to each other o – Half pins also effective – Use full rings (more difficult to deform) • Can maintain purchase in metaphyseal bone • Allows dynamic axial loading • May allow joint motion

Multiplanar Adjustable Ring Fixators • Application with wire or half pins • Adjustable with 6 degrees of freedom – Deformity correction • acute • chronic

• Type 3 A open tibia fracture with bone loss

• Following frame adjustment and bone grafting
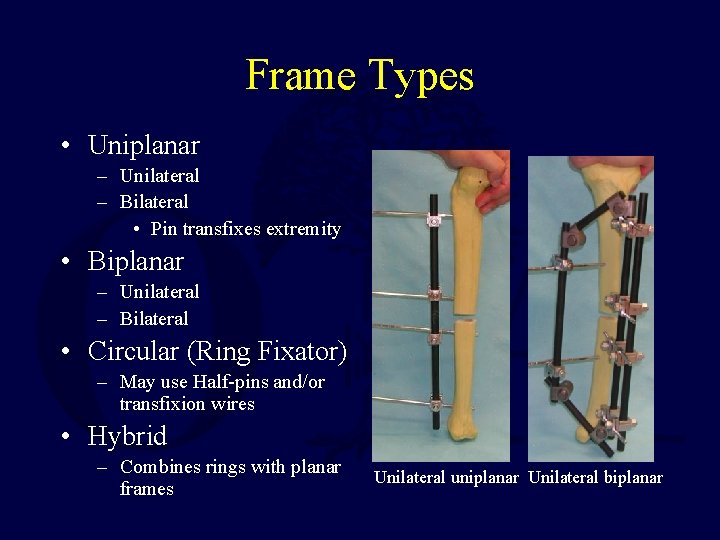
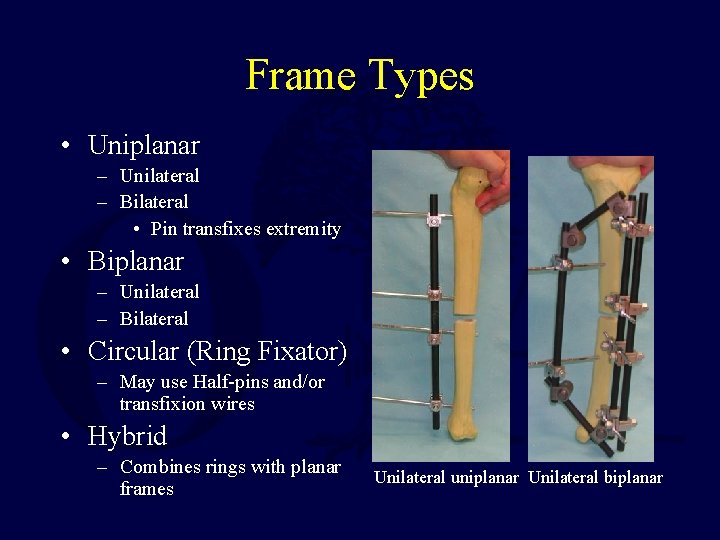
Frame Types • Uniplanar – Unilateral – Bilateral • Pin transfixes extremity • Biplanar – Unilateral – Bilateral • Circular (Ring Fixator) – May use Half-pins and/or transfixion wires • Hybrid – Combines rings with planar frames Unilateral uniplanar Unilateral biplanar

Hybrid Fixators • Combines the advantages of ring fixators in periarticular areas with simplicity of planar half pin fixators in diaphyseal bone From Rockwood and Green’s, 5 th Ed
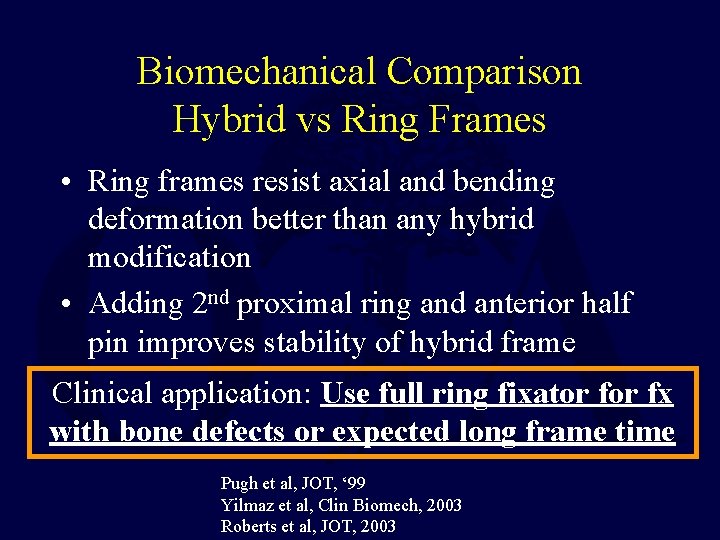
Biomechanical Comparison Hybrid vs Ring Frames • Ring frames resist axial and bending deformation better than any hybrid modification • Adding 2 nd proximal ring and anterior half pin improves stability of hybrid frame Clinical application: Use full ring fixator fx with bone defects or expected long frame time Pugh et al, JOT, ‘ 99 Yilmaz et al, Clin Biomech, 2003 Roberts et al, JOT, 2003
MRI Compatability • Issues: – Safety • Magnetic field displacing ferromagnetic object – Potential missile • Heat generation by induced fields – Image quality • Image distortion
MRI Compatibility • Stainless steel components (pins, clamps, rings) most at risk for attraction and heating • Titanium (pins), aluminum (rods, clamps, rings) and carbon fiber (rods, rings) demonstrate minimal heating and attraction • Almost all are safe if the components are not directly within the scanner (subject to local policy) • Consider use of MRI “safe” ex fix when area interest is spanned by the frame and use Kumar, JOR, 2006 titanium pins Davison, JOT, 2004 Cannada, CORR, 1995
Frame Types • Standard frame • Joint spanning frame: – Nonarticulated – Articulated frame • Distraction or Correction frame

Standard Frame • Standard Frame Design – Diaphyseal region – Allows adjacent joint motion – Stable
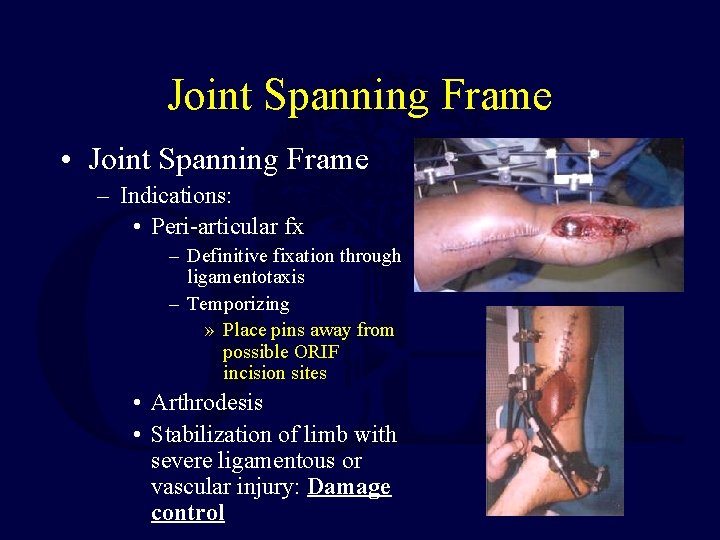
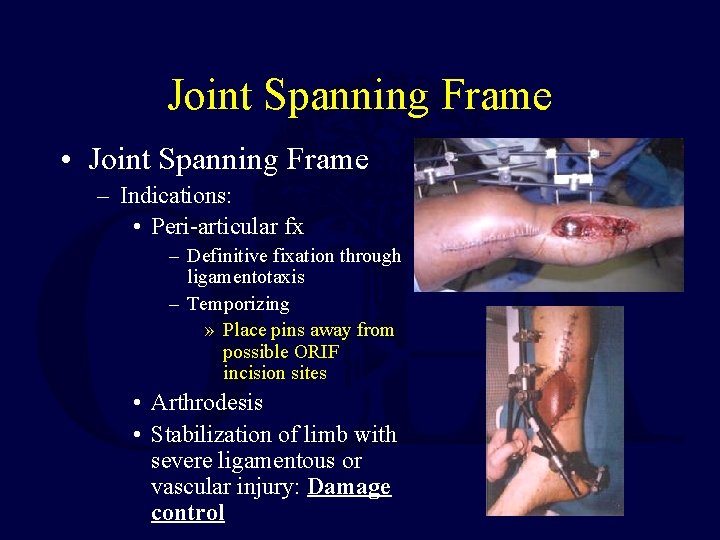
Joint Spanning Frame • Joint Spanning Frame – Indications: • Peri-articular fx – Definitive fixation through ligamentotaxis – Temporizing » Place pins away from possible ORIF incision sites • Arthrodesis • Stabilization of limb with severe ligamentous or vascular injury: Damage control
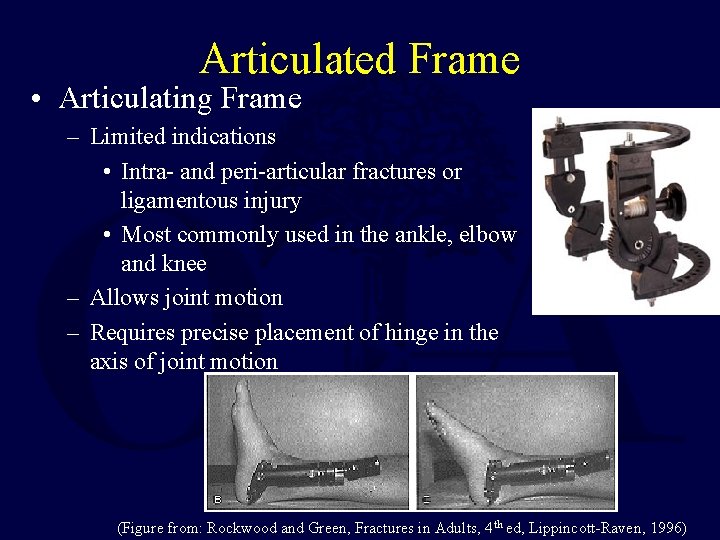
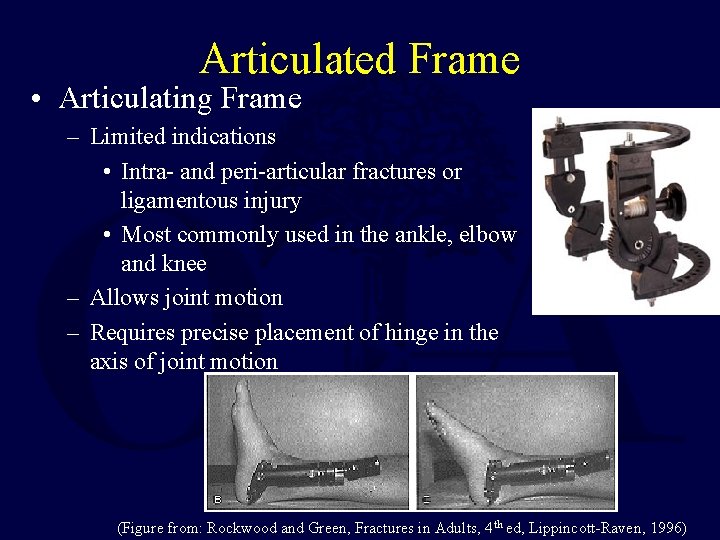
Articulated Frame • Articulating Frame – Limited indications • Intra- and peri-articular fractures or ligamentous injury • Most commonly used in the ankle, elbow and knee – Allows joint motion – Requires precise placement of hinge in the axis of joint motion (Figure from: Rockwood and Green, Fractures in Adults, 4 th ed, Lippincott-Raven, 1996)
Correction of Deformity or Defects • May use unilateral or ring frames • Simple deformities may use simple frames • Complex deformities require more complex frames • All require careful planning

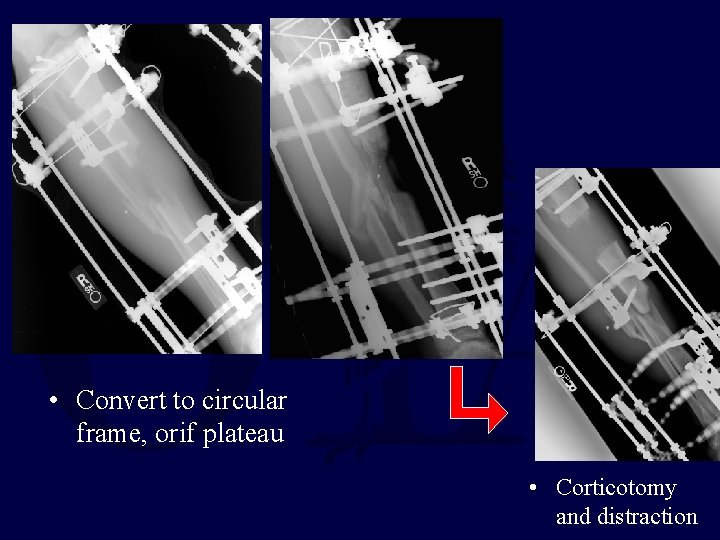
• 3 B tibia with segmental bone loss, 3 A plateau, temporary spanning ex fix
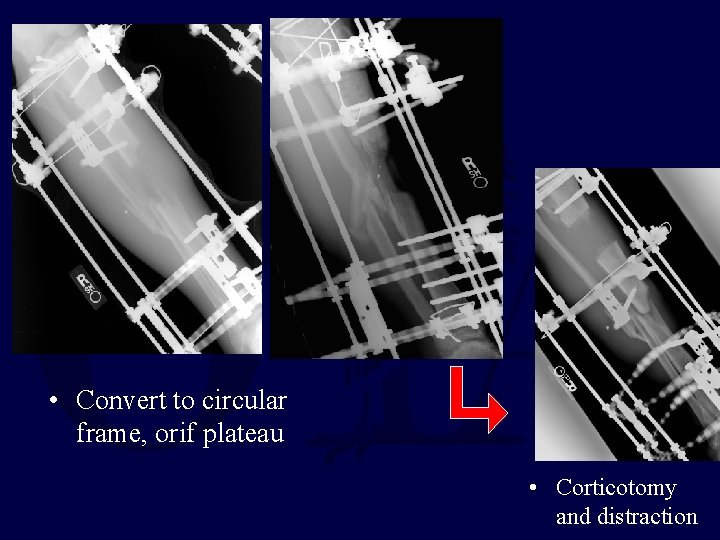
• Convert to circular frame, orif plateau • Corticotomy and distraction
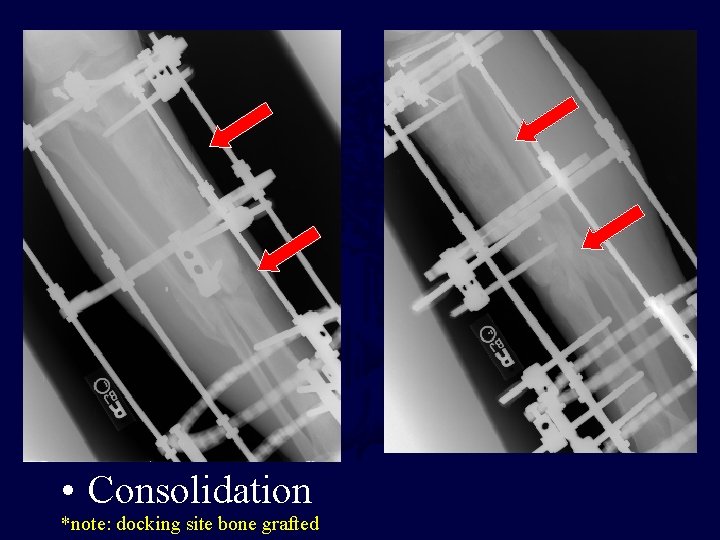
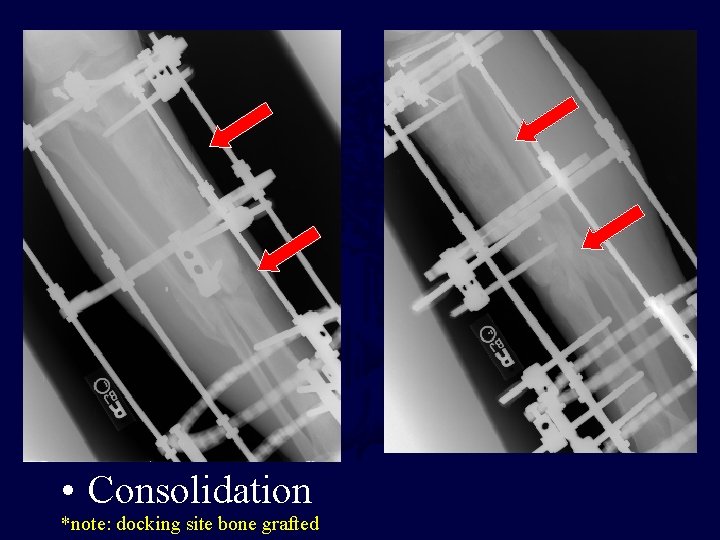
• Consolidation *note: docking site bone grafted

Healed
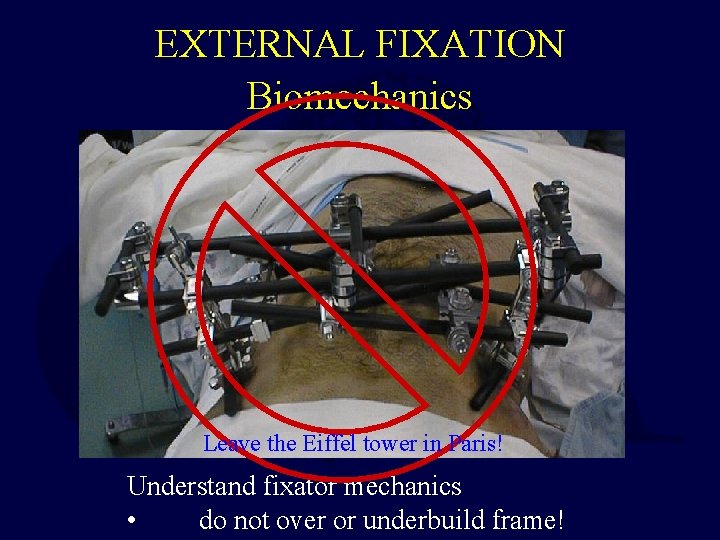
EXTERNAL FIXATION Biomechanics Leave the Eiffel tower in Paris! Understand fixator mechanics • do not over or underbuild frame!

Fixator Mechanics: Pin Factors • Larger pin diameter • Increased pin spread – on the same side of the fracture • Increased number of pins (both in and out of plane of construct)
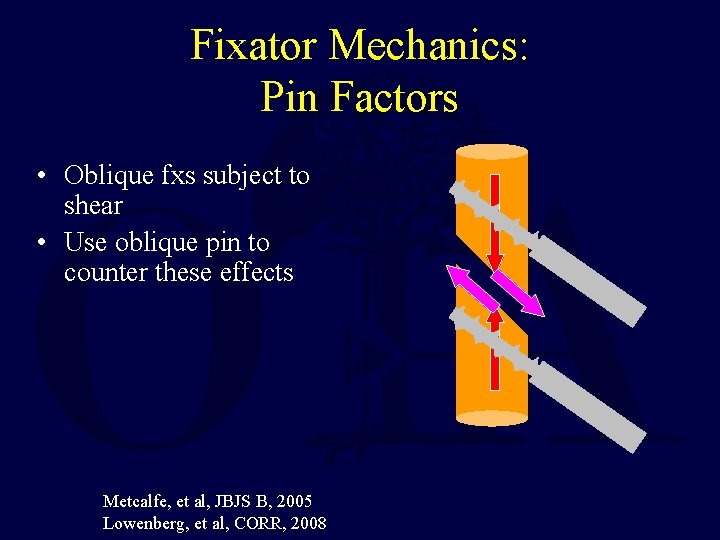
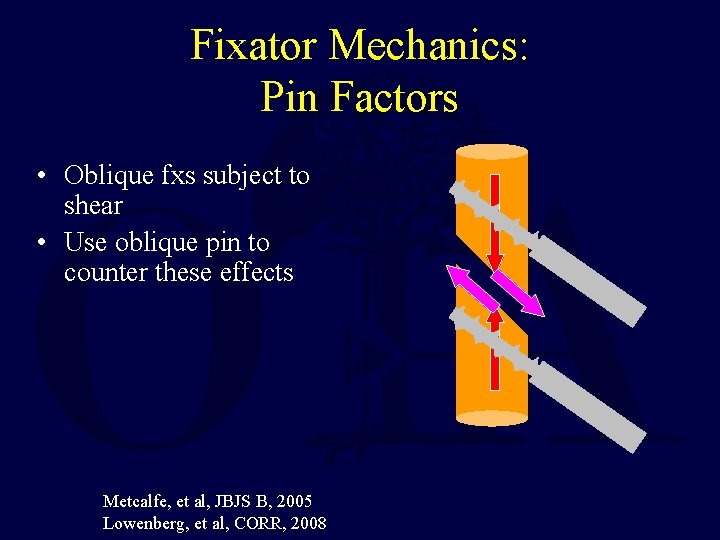
Fixator Mechanics: Pin Factors • Oblique fxs subject to shear • Use oblique pin to counter these effects Metcalfe, et al, JBJS B, 2005 Lowenberg, et al, CORR, 2008
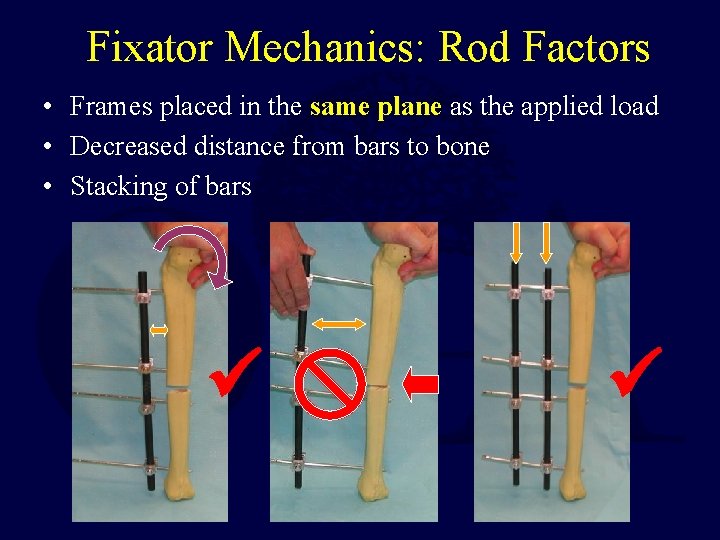
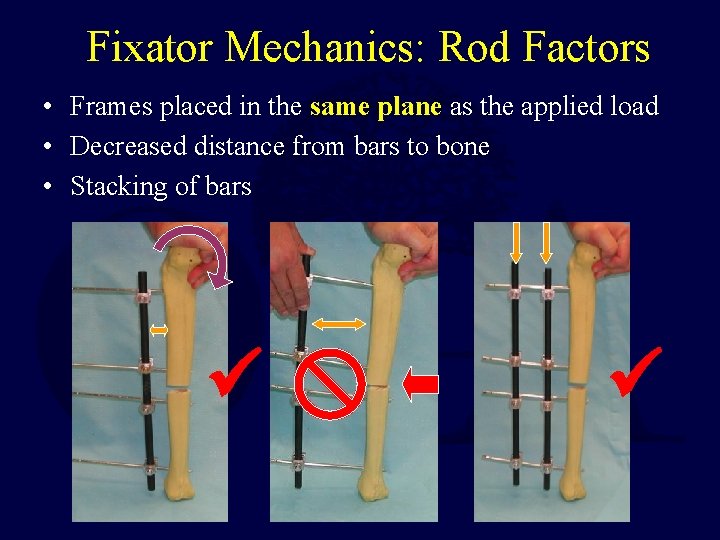
Fixator Mechanics: Rod Factors • Frames placed in the same plane as the applied load • Decreased distance from bars to bone • Stacking of bars
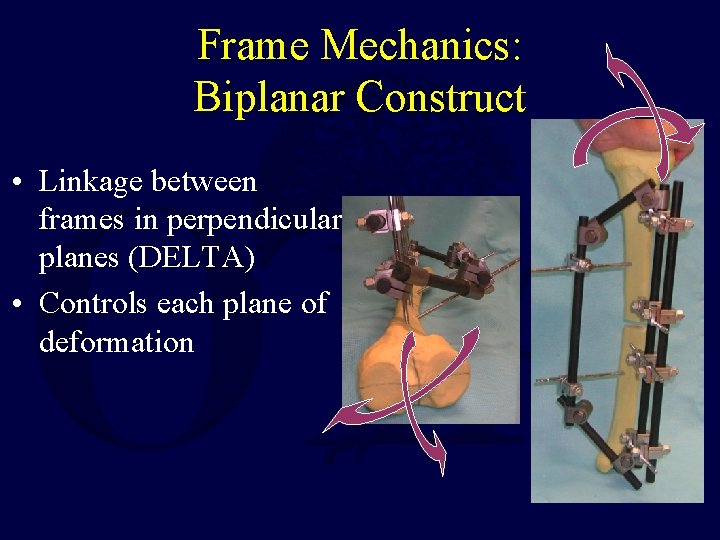
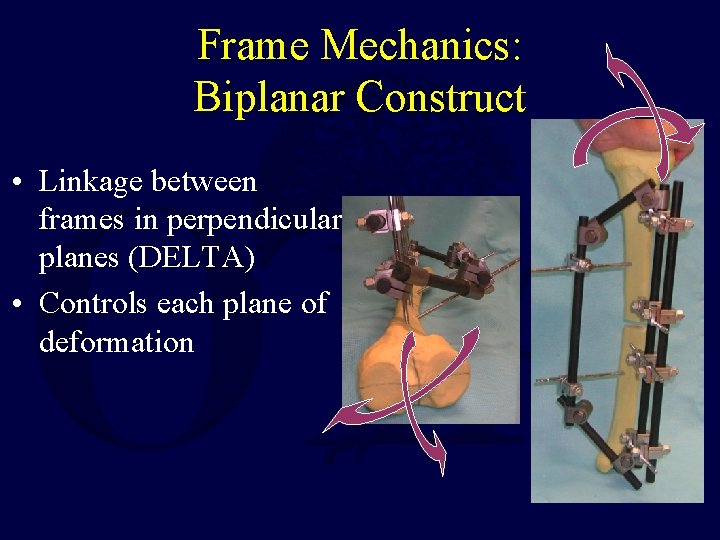
Frame Mechanics: Biplanar Construct • Linkage between frames in perpendicular planes (DELTA) • Controls each plane of deformation

Frame Mechanics: Ring Fixators • Spread wires to as o close to 90 as anatomically possible • Use at least 2 planes of wires/half pins in each major bone segment
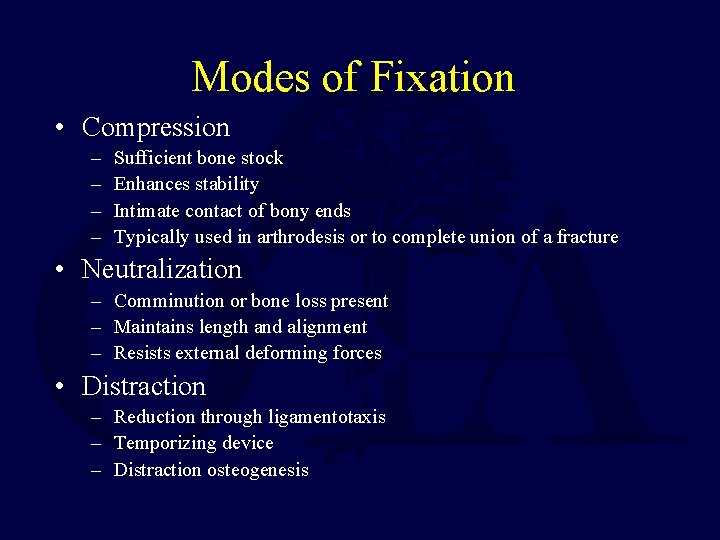
Modes of Fixation • Compression – – Sufficient bone stock Enhances stability Intimate contact of bony ends Typically used in arthrodesis or to complete union of a fracture • Neutralization – Comminution or bone loss present – Maintains length and alignment – Resists external deforming forces • Distraction – Reduction through ligamentotaxis – Temporizing device – Distraction osteogenesis
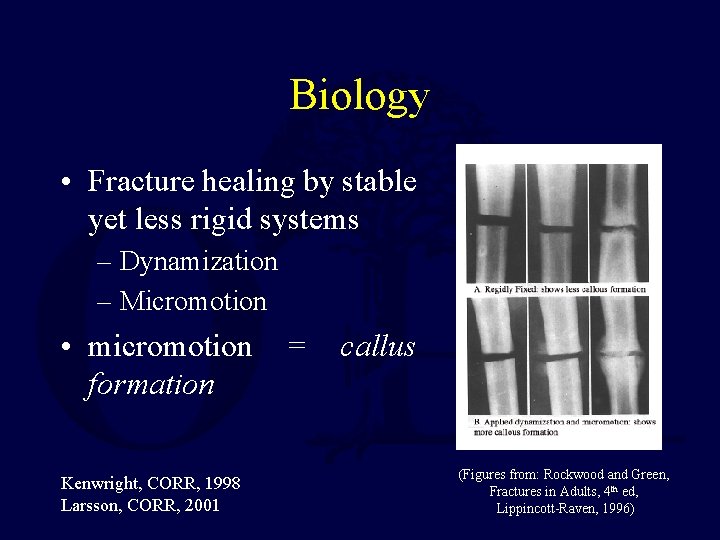
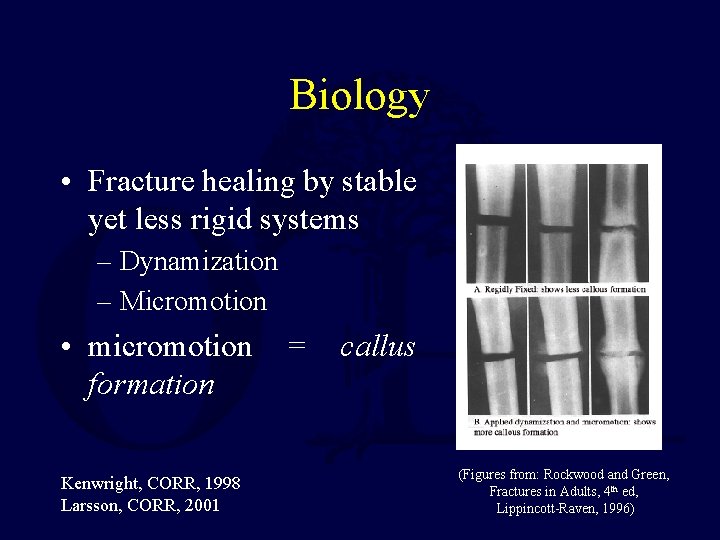
Biology • Fracture healing by stable yet less rigid systems – Dynamization – Micromotion • micromotion = callus formation Kenwright, CORR, 1998 Larsson, CORR, 2001 (Figures from: Rockwood and Green, Fractures in Adults, 4 th ed, Lippincott-Raven, 1996)
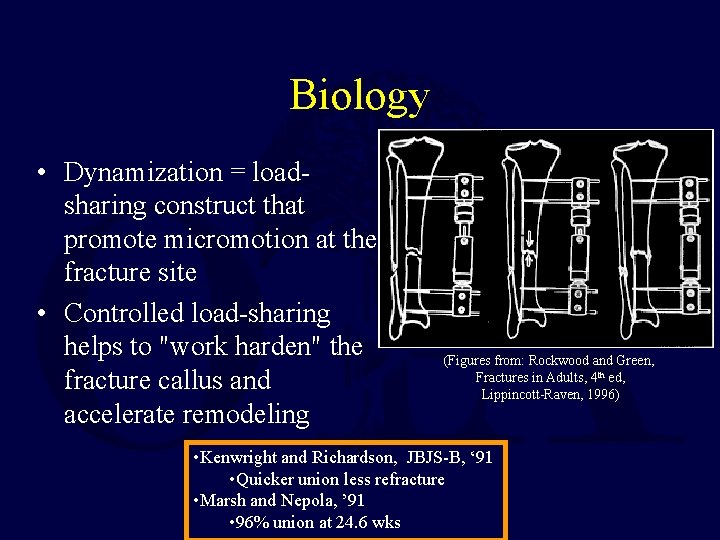
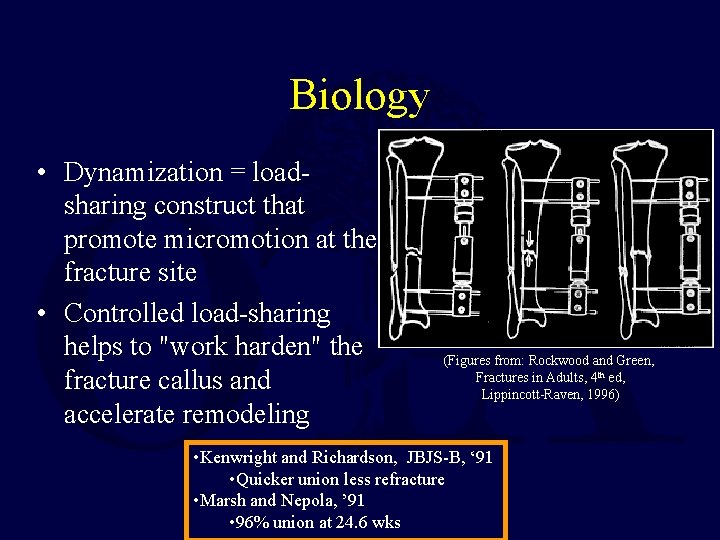
Biology • Dynamization = loadsharing construct that promote micromotion at the fracture site • Controlled load-sharing helps to "work harden" the fracture callus and accelerate remodeling (Figures from: Rockwood and Green, Fractures in Adults, 4 th ed, Lippincott-Raven, 1996) • Kenwright and Richardson, JBJS-B, ‘ 91 • Quicker union less refracture • Marsh and Nepola, ’ 91 • 96% union at 24. 6 wks
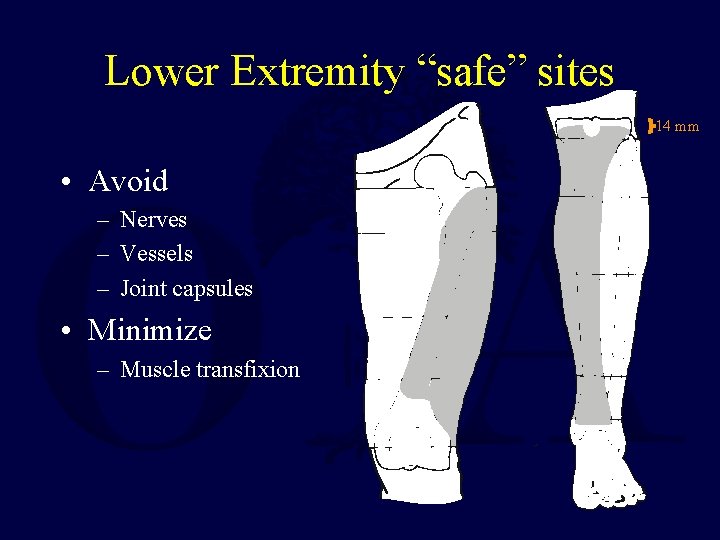
Anatomic Considerations • Fundamental knowledge of the anatomy is critical • Avoidance of major nerves, vessels and organs (pelvis) is mandatory • Avoid joints and joint capsules – Proximal tibial pins should be placed 14 mm distal to articular surface to avoid capsular reflection • Minimize muscle/tendon impalement (especially those with large excursions)
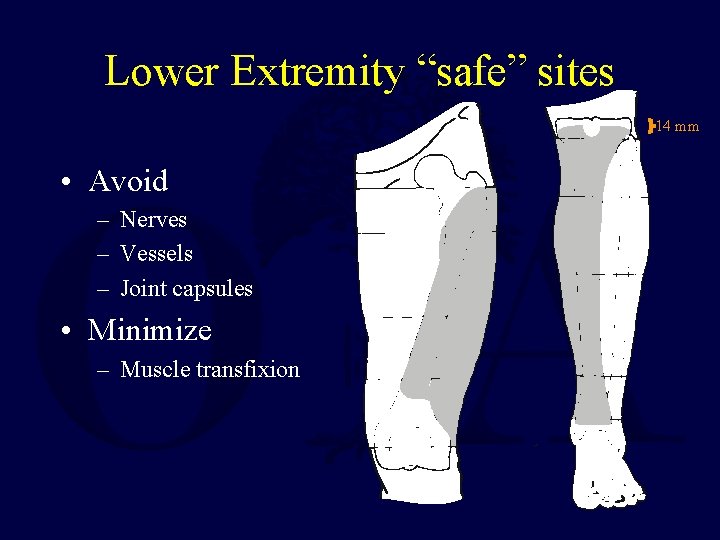
Lower Extremity “safe” sites 14 mm • Avoid – Nerves – Vessels – Joint capsules • Minimize – Muscle transfixion
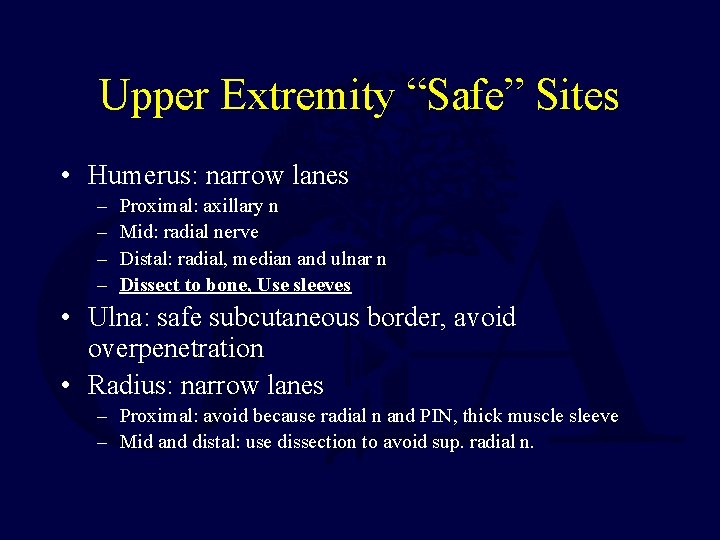
Upper Extremity “Safe” Sites • Humerus: narrow lanes – – Proximal: axillary n Mid: radial nerve Distal: radial, median and ulnar n Dissect to bone, Use sleeves • Ulna: safe subcutaneous border, avoid overpenetration • Radius: narrow lanes – Proximal: avoid because radial n and PIN, thick muscle sleeve – Mid and distal: use dissection to avoid sup. radial n.
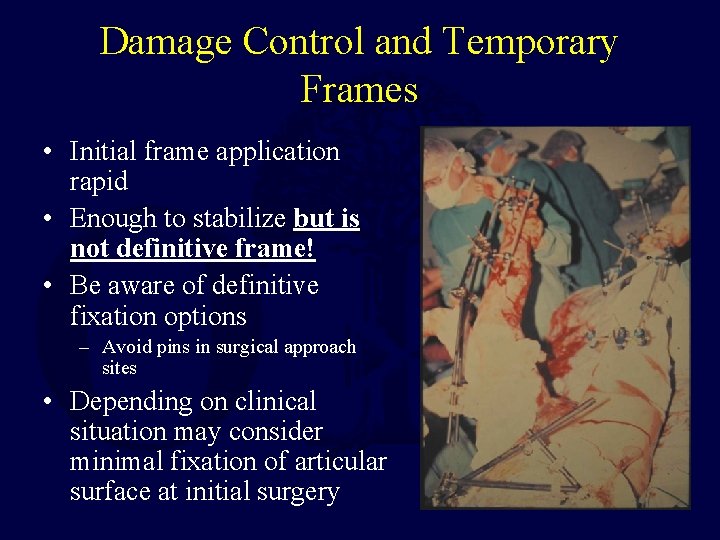
Damage Control and Temporary Frames • Initial frame application rapid • Enough to stabilize but is not definitive frame! • Be aware of definitive fixation options – Avoid pins in surgical approach sites • Depending on clinical situation may consider minimal fixation of articular surface at initial surgery
Conversion to Internal Fixation • Generally safe within 2 -3 wks – Bhandari, JOT, 2005 • Meta analysis: 6 femur, 9 tibia, all but one retrospective • Infection in tibia and femur <4% • Rods or plates appropriate • Use with caution with signs of pin irritation – Consider staged procedure • Remove and curette sites • Return following healing for definitive fixation – Extreme caution with established pin track infection – Maurer, ’ 89 • 77% deep infection with h/o pin infection
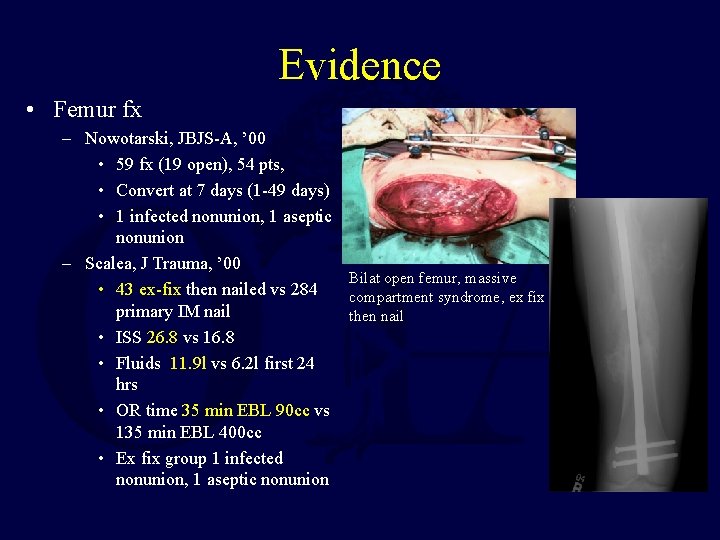
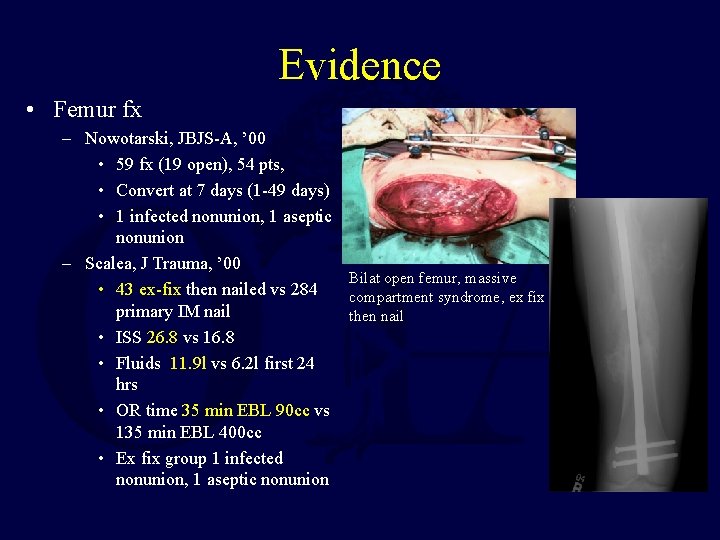
Evidence • Femur fx – Nowotarski, JBJS-A, ’ 00 • 59 fx (19 open), 54 pts, • Convert at 7 days (1 -49 days) • 1 infected nonunion, 1 aseptic nonunion – Scalea, J Trauma, ’ 00 Bilat open femur, massive • 43 ex-fix then nailed vs 284 compartment syndrome, ex fix primary IM nail then nail • ISS 26. 8 vs 16. 8 • Fluids 11. 9 l vs 6. 2 l first 24 hrs • OR time 35 min EBL 90 cc vs 135 min EBL 400 cc • Ex fix group 1 infected nonunion, 1 aseptic nonunion
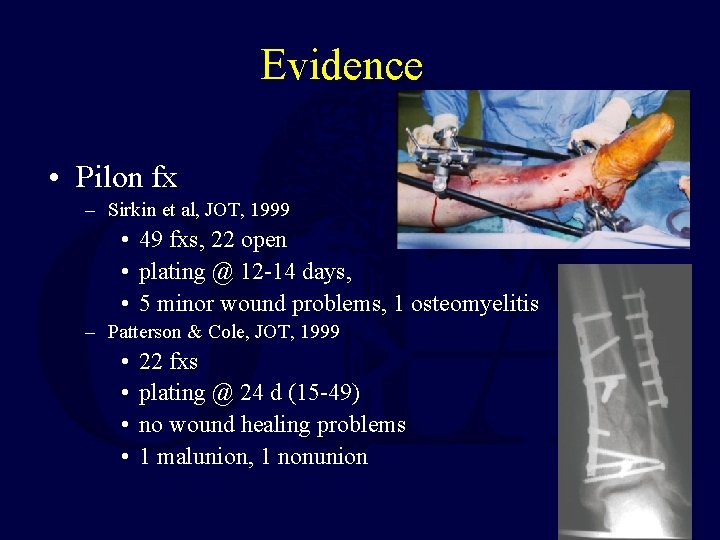
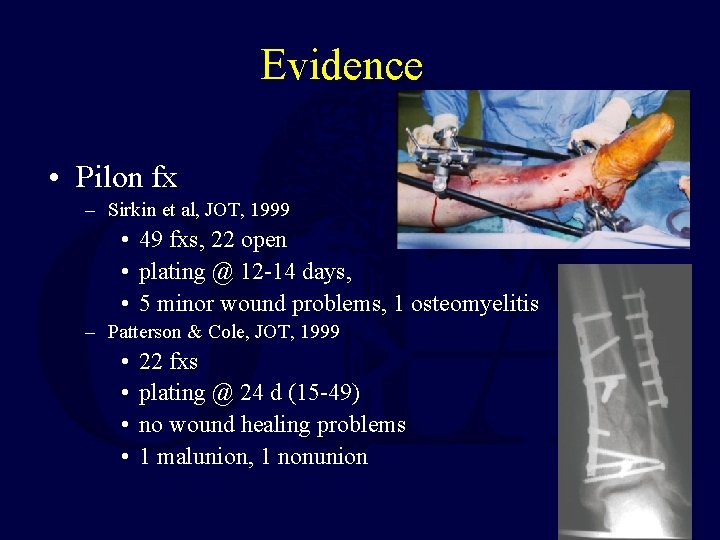
Evidence • Pilon fx – Sirkin et al, JOT, 1999 • 49 fxs, 22 open • plating @ 12 -14 days, • 5 minor wound problems, 1 osteomyelitis – Patterson & Cole, JOT, 1999 • • 22 fxs plating @ 24 d (15 -49) no wound healing problems 1 malunion, 1 nonunion
Complications • • • Pin-track infection/loosening Frame or Pin/Wire Failure Malunion Non-union Soft-tissue impalement Compartment syndrome
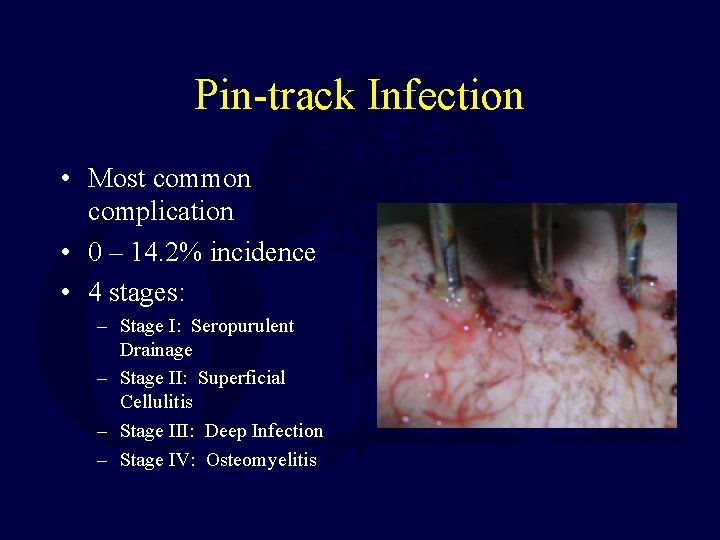
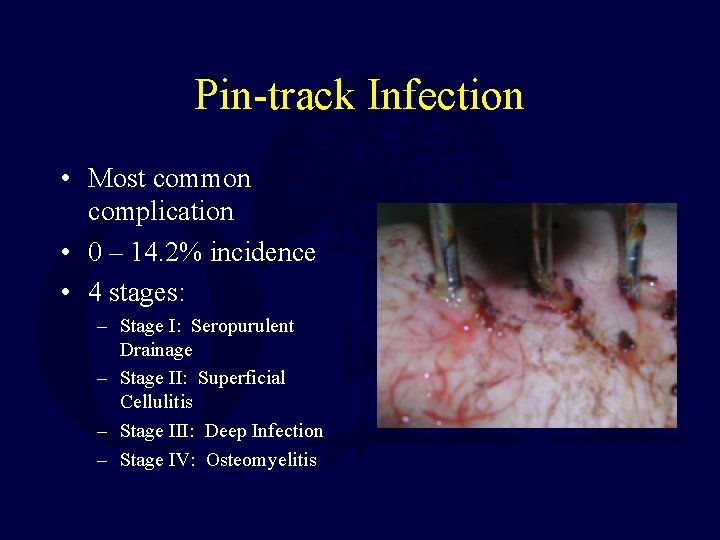
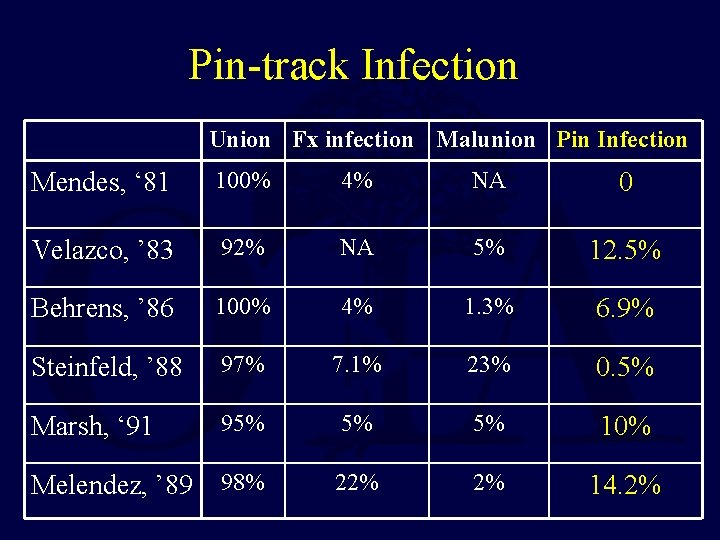
Pin-track Infection • Most common complication • 0 – 14. 2% incidence • 4 stages: – Stage I: Seropurulent Drainage – Stage II: Superficial Cellulitis – Stage III: Deep Infection – Stage IV: Osteomyelitis
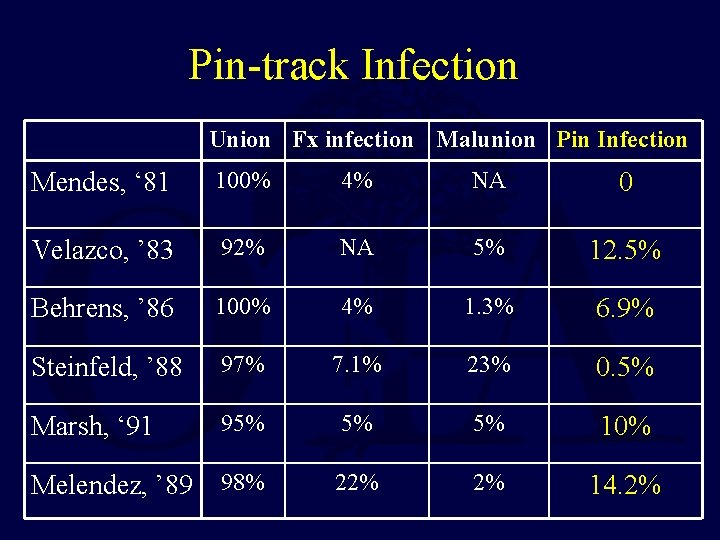
Pin-track Infection Union Fx infection Malunion Pin Infection Mendes, ‘ 81 100% 4% NA 0 Velazco, ’ 83 92% NA 5% 12. 5% Behrens, ’ 86 100% 4% 1. 3% 6. 9% Steinfeld, ’ 88 97% 7. 1% 23% 0. 5% Marsh, ‘ 91 95% 5% 5% 10% Melendez, ’ 89 98% 22% 2% 14. 2%
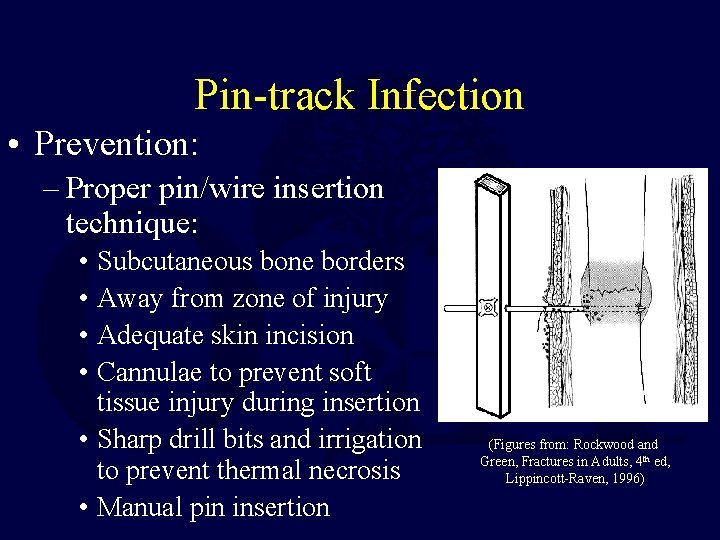
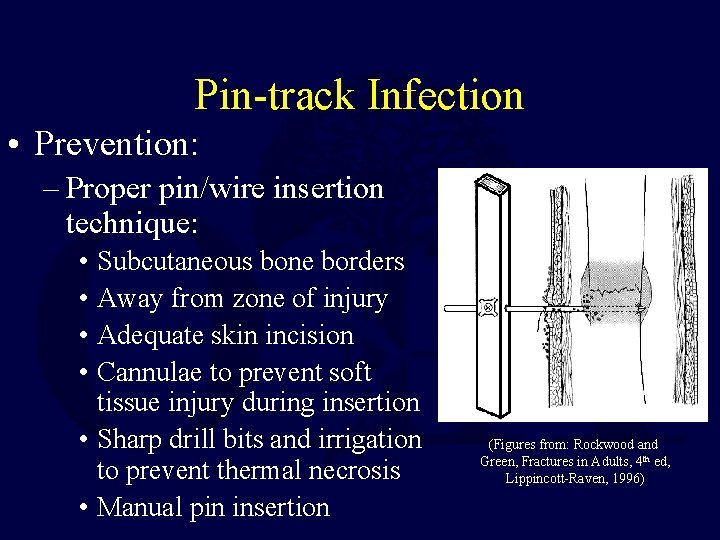
Pin-track Infection • Prevention: – Proper pin/wire insertion technique: • Subcutaneous bone borders • Away from zone of injury • Adequate skin incision • Cannulae to prevent soft tissue injury during insertion • Sharp drill bits and irrigation to prevent thermal necrosis • Manual pin insertion (Figures from: Rockwood and Green, Fractures in Adults, 4 th ed, Lippincott-Raven, 1996)

Pin-track Infection • Postoperative care: – Clean implant/skin interface – Saline – Gauze – Shower
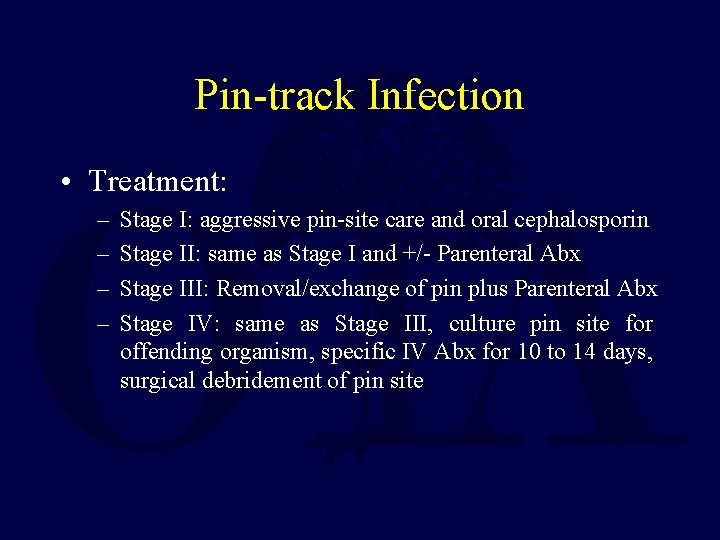
Pin-track Infection • Treatment: – – Stage I: aggressive pin-site care and oral cephalosporin Stage II: same as Stage I and +/- Parenteral Abx Stage III: Removal/exchange of pin plus Parenteral Abx Stage IV: same as Stage III, culture pin site for offending organism, specific IV Abx for 10 to 14 days, surgical debridement of pin site
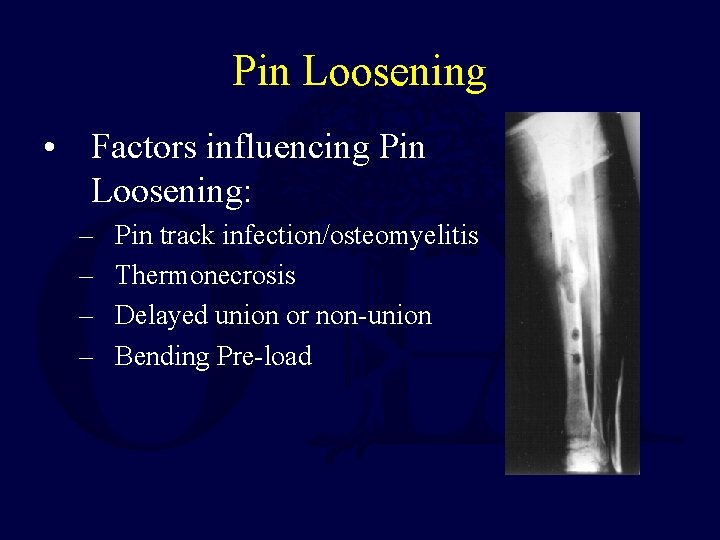
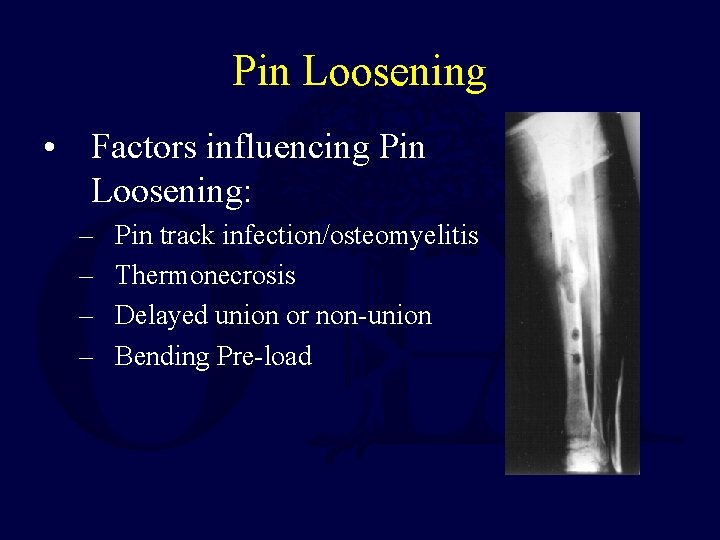
Pin Loosening • Factors influencing Pin Loosening: – – Pin track infection/osteomyelitis Thermonecrosis Delayed union or non-union Bending Pre-load
Pin Loosening • Prevention: – – – Proper pin/wire insertion techniques Radial preload Euthermic pin insertion Adequate soft-tissue release Bone graft early Pin coatings • Treatment: – Replace/remove loose pin
Frame Failure • Incidence: Rare • Theoretically can occur with recycling of old frames • However, no proof that frames can not be re -used

Malunion Intra-operative causes: – Due to poor technique • Prevention: – – Clear pre-operative planning Prep contralateral limb for comparison Use fluoroscopic and/or intra-operative films Adequate construct • Treatment: – Early: Correct deformity and adjust or re-apply frame prior to bony union – Late: Reconstructive correction of malunion

Malunion Post-operative causes: – Due to frame failure • Prevention: – Proper follow-up with both clinical and radiographic check-ups – Adherence to appropriate weight-bearing restrictions – Check and re-tighten frame at periodic intervals • Treatment: – Osteotomy/reconstruction
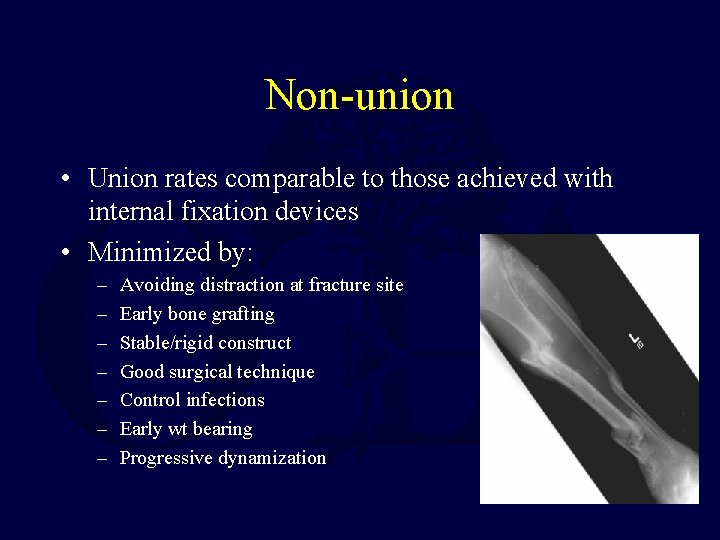
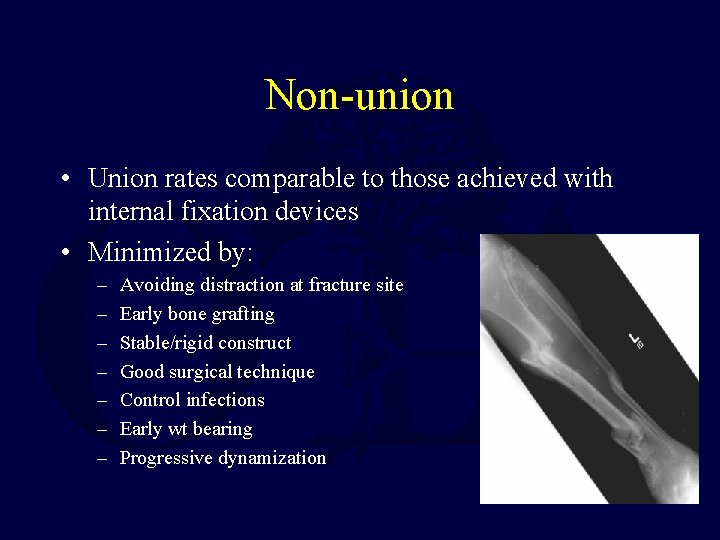
Non-union • Union rates comparable to those achieved with internal fixation devices • Minimized by: – – – – Avoiding distraction at fracture site Early bone grafting Stable/rigid construct Good surgical technique Control infections Early wt bearing Progressive dynamization
Soft-tissue Impalement • Tethering of soft tissues can result in: – Loss of motion – Scarring – Vessel injury • Prevention: – – Check ROM intra-operatively Avoid piercing muscle or tendons Position joint in NEUTRAL Early stretching and ROM exercises

Compartment Syndrome • Rare • Cause: – Injury related – pin or wire causing intracompartmental bleeding • Prevention: – Clear understanding of the anatomy – Good technique – Post-operative vigilance
Future Areas of Development • Pin coatings/sleeves – Reduce infection – Reduce pin loosening • Optimization of dynamization for fracture healing • Increasing ease of use/reduced cost
Construct Tips • • • Chose optimal pin diameter Use good insertion technique Place clamps and frames close to skin Frame in plane of deforming forces Stack frame (2 bars) Re-use/Recycle components (requires certified inspection). Plan ahead!
Summary • Multiple applications • Choose components and geometry suitable for particular application • Appropriate use can lead to excellent results • Recognize and correct complications early If you would like to volunteer as an author for the Resident Slide Project or recommend updates to any of the following slides, please send an email to ota@ota. org Return to General/Principles Index
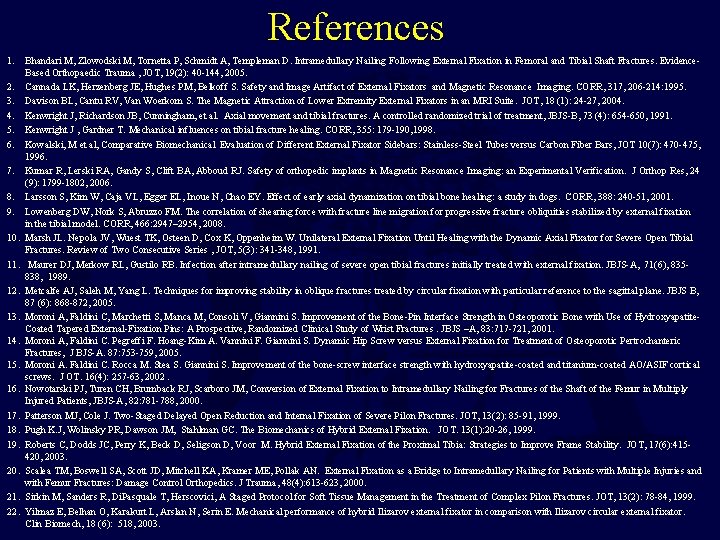
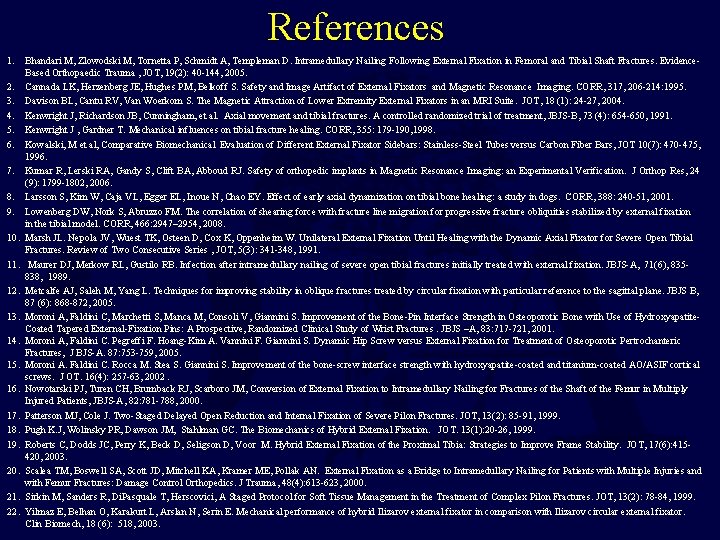
References 1. Bhandari M, Zlowodski M, Tornetta P, Schmidt A, Templeman D. Intramedullary Nailing Following External Fixation in Femoral and Tibial Shaft Fractures. Evidence. Based Orthopaedic Trauma , JOT, 19(2): 40 -144, 2005. 2. Cannada LK, Herzenberg JE, Hughes PM, Belkoff S. Safety and Image Artifact of External Fixators and Magnetic Resonance Imaging. CORR, 317, 206 -214: 1995. 3. Davison BL, Cantu RV, Van Woerkom S. The Magnetic Attraction of Lower Extremity External Fixators in an MRI Suite. JOT, 18 (1): 24 -27, 2004. 4. Kenwright J, Richardson JB, Cunningham, et al. Axial movement and tibial fractures. A controlled randomized trial of treatment, JBJS-B, 73 (4): 654 -650, 1991. 5. Kenwright J , Gardner T. Mechanical influences on tibial fracture healing. CORR, 355: 179 -190, 1998. 6. Kowalski, M et al, Comparative Biomechanical Evaluation of Different External Fixator Sidebars: Stainless-Steel Tubes versus Carbon Fiber Bars, JOT 10(7): 470 -475, 1996. 7. Kumar R, Lerski RA, Gandy S, Clift BA, Abboud RJ. Safety of orthopedic implants in Magnetic Resonance Imaging: an Experimental Verification. J Orthop Res, 24 (9): 1799 -1802, 2006. 8. Larsson S, Kim W, Caja VL, Egger EL, Inoue N, Chao EY. Effect of early axial dynamization on tibial bone healing: a study in dogs. CORR, 388: 240 -51, 2001. 9. Lowenberg DW, Nork S, Abruzzo FM. The correlation of shearing force with fracture line migration for progressive fracture obliquities stabilized by external fixation in the tibial model. CORR, 466: 2947– 2954, 2008. 10. Marsh JL. Nepola JV, Wuest TK, Osteen D, Cox K, Oppenheim W. Unilateral External Fixation Until Healing with the Dynamic Axial Fixator for Severe Open Tibial Fractures. Review of Two Consecutive Series , JOT, 5(3): 341 -348, 1991. 11. Maurer DJ, Merkow RL, Gustilo RB. Infection after intramedullary nailing of severe open tibial fractures initially treated with external fixation. JBJS-A, 71(6), 835838, 1989. 12. Metcalfe AJ, Saleh M, Yang L. Techniques for improving stability in oblique fractures treated by circular fixation with particular reference to the sagittal plane. JBJS B, 87 (6): 868 -872, 2005. 13. Moroni A, Faldini C, Marchetti S, Manca M, Consoli V, Giannini S. Improvement of the Bone-Pin Interface Strength in Osteoporotic Bone with Use of Hydroxyapatite. Coated Tapered External-Fixation Pins: A Prospective, Randomized Clinical Study of Wrist Fractures. JBJS –A, 83: 717 -721, 2001. 14. Moroni A, Faldini C. Pegreffi F. Hoang-Kim A. Vannini F. Giannini S. Dynamic Hip Screw versus External Fixation for Treatment of Osteoporotic Pertrochanteric Fractures, J BJS-A. 87: 753 -759, 2005. 15. Moroni A. Faldini C. Rocca M. Stea S. Giannini S. Improvement of the bone-screw interface strength with hydroxyapatite-coated and titanium-coated AO/ASIF cortical screws. J OT. 16(4): 257 -63, 2002. 16. Nowotarski PJ, Turen CH, Brumback RJ, Scarboro JM, Conversion of External Fixation to Intramedullary Nailing for Fractures of the Shaft of the Femur in Multiply Injured Patients, JBJS-A, 82: 781 -788, 2000. 17. Patterson MJ, Cole J. Two-Staged Delayed Open Reduction and Internal Fixation of Severe Pilon Fractures. JOT, 13(2): 85 -91, 1999. 18. Pugh K. J, Wolinsky PR, Dawson JM, Stahlman GC. The Biomechanics of Hybrid External Fixation. JOT. 13(1): 20 -26, 1999. 19. Roberts C, Dodds JC, Perry K, Beck D, Seligson D, Voor M. Hybrid External Fixation of the Proximal Tibia: Strategies to Improve Frame Stability. JOT, 17(6): 415420, 2003. 20. Scalea TM, Boswell SA, Scott JD, Mitchell KA, Kramer ME, Pollak AN. External Fixation as a Bridge to Intramedullary Nailing for Patients with Multiple Injuries and with Femur Fractures: Damage Control Orthopedics. J Trauma, 48(4): 613 -623, 2000. 21. Sirkin M, Sanders R, Di. Pasquale T, Herscovici, A Staged Protocol for Soft Tissue Management in the Treatment of Complex Pilon Fractures. JOT, 13(2): 78 -84, 1999. 22. Yilmaz E, Belhan O, Karakurt L, Arslan N, Serin E. Mechanical performance of hybrid Ilizarov external fixator in comparison with Ilizarov circular external fixator. Clin Biomech, 18 (6): 518, 2003.
 Roman hayda md
Roman hayda md External fiksasi
External fiksasi External fixation device nursing care
External fixation device nursing care Principles of internal fixation
Principles of internal fixation External-external trips
External-external trips Politheistic
Politheistic Roman republic vs roman empire
Roman republic vs roman empire Which phrase best defines a food chain?
Which phrase best defines a food chain? Oral fixation examples
Oral fixation examples Psychoanalysis
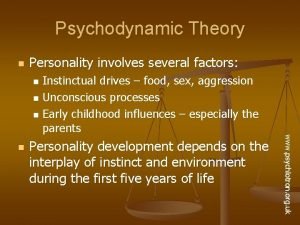
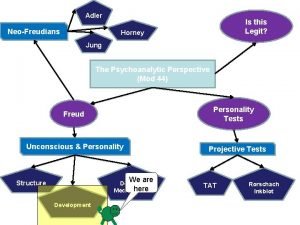
Psychoanalysis Sigmund freud psychodynamic approach
Sigmund freud psychodynamic approach Principle of suspension therapy
Principle of suspension therapy Behaviorist theory of personality
Behaviorist theory of personality Fixation in latency stage
Fixation in latency stage Phallic stage
Phallic stage Anal fixation
Anal fixation Nerf
Nerf Oral fixation examples
Oral fixation examples Freud’s psychoanalytic theory of personality
Freud’s psychoanalytic theory of personality Phallic fixation
Phallic fixation Sublimation defense mechanism example
Sublimation defense mechanism example Latent fixation
Latent fixation Fixation examples
Fixation examples Psychoanalytic
Psychoanalytic Les étapes de fixation des prix
Les étapes de fixation des prix Fixation in kinesiology
Fixation in kinesiology Phallic fixation
Phallic fixation Oral stage of development examples
Oral stage of development examples Erogenous zone theory
Erogenous zone theory Phallic fixation
Phallic fixation Fixation defense mechanism
Fixation defense mechanism Anal stage fixation
Anal stage fixation Tissue processing
Tissue processing Tissue processing steps in histopathology
Tissue processing steps in histopathology Stratified squamous non-keratinized epithelium
Stratified squamous non-keratinized epithelium Primary and supporting instruments
Primary and supporting instruments Phallic stage clipart
Phallic stage clipart Energy fixation
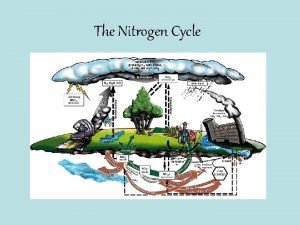
Energy fixation Nitrogen fixation is the conversion of
Nitrogen fixation is the conversion of Attitude instrument flying
Attitude instrument flying Disadvantages of 2's complement
Disadvantages of 2's complement Brand identity traps
Brand identity traps High nitrogen fertilizer numbers
High nitrogen fertilizer numbers Index.php?seccion=
Index.php?seccion= Modular externational fixation
Modular externational fixation Complement fixation test steps
Complement fixation test steps Reaction formation psych
Reaction formation psych Nitrogen fixation diagram
Nitrogen fixation diagram Unscramble fixation
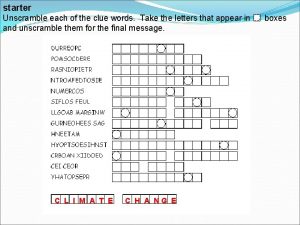
Unscramble fixation Nitrogen fixation
Nitrogen fixation Facet screw fixation
Facet screw fixation Complement fixation
Complement fixation Ventilation artificielle
Ventilation artificielle Les contraintes internes et externes de la fixation de prix
Les contraintes internes et externes de la fixation de prix Le triangle d'or du positionnement se compose
Le triangle d'or du positionnement se compose Original gospel manuscripts
Original gospel manuscripts Identify the type of congruence transformation
Identify the type of congruence transformation Thirteen colonies
Thirteen colonies Twitch original markz
Twitch original markz Who was the previous owner of oregon country
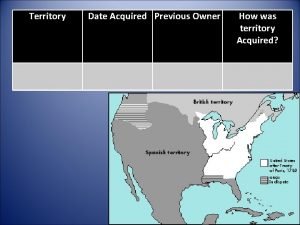
Who was the previous owner of oregon country Angular conformity
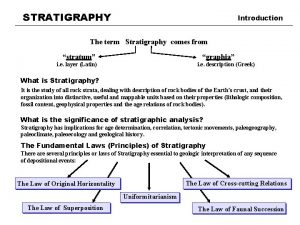
Angular conformity Characteristics of stonehenge
Characteristics of stonehenge Sugestões de oração inicial
Sugestões de oração inicial Do with their death bury their parents' strife translation
Do with their death bury their parents' strife translation Original oratory
Original oratory Metaphors in speech to the virginia convention
Metaphors in speech to the virginia convention Restate and paraphrase
Restate and paraphrase Theoriginalmarkz live stream
Theoriginalmarkz live stream Kringsatt af fjender
Kringsatt af fjender Original oratory
Original oratory Original nicene creed
Original nicene creed