Complement fixation test complement fixation test The complement

- Slides: 19

Complement fixation test
complement fixation test • The complement fixation test (CFT) was extensively used in syphilis serology after being introduced by Wasserman in 1909. • It took a number of decades before the CFT was adapted for routine use in virology. • CFT meet the following criteria ▫ It is convenient and rapid to perform ▫ The demand on equipment and reagents is small ▫ A large variety of test antigens are readily available
Principle of CFT • The complete fixation test (CFT) is used to detect the presence of specific antibodies in the patient’s serum. • This test is based on the use of complement, a Biologically labile serum factor that causes the immune cytolysis i. e. lysis of antibody coated cells.
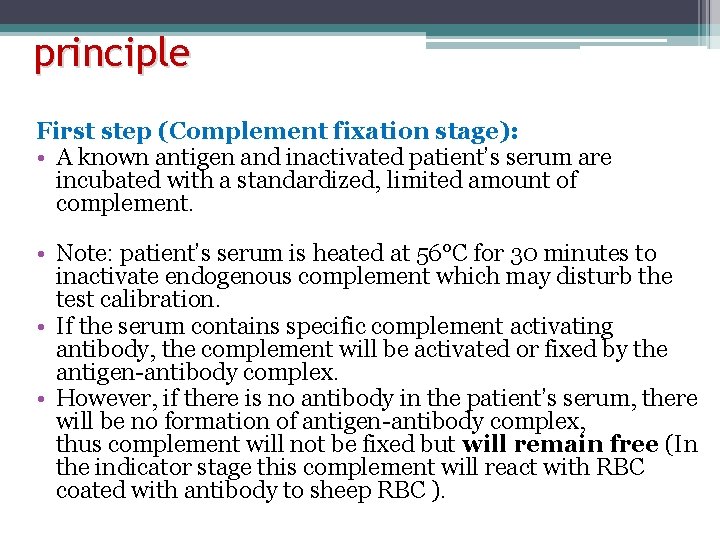
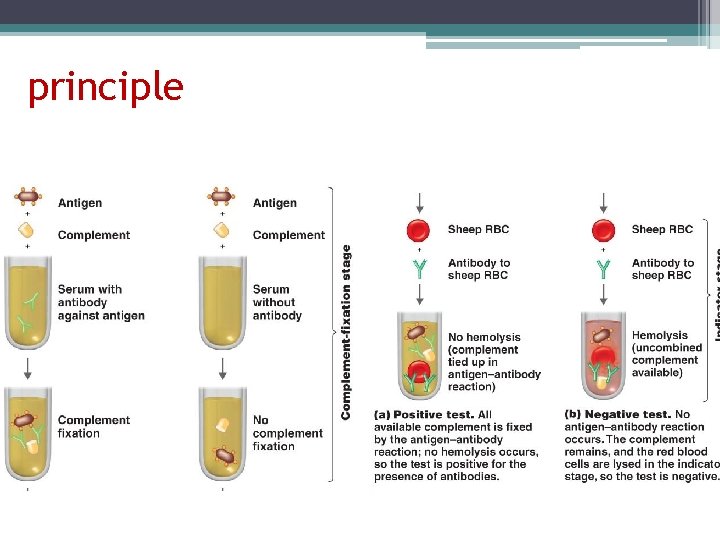
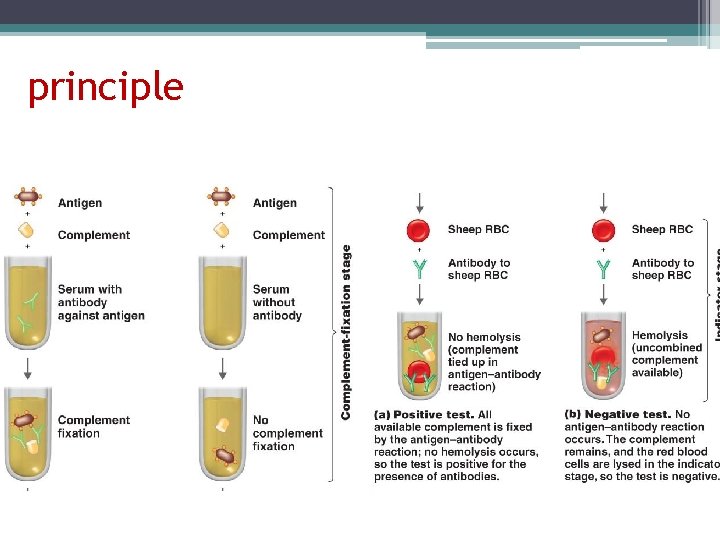
principle First step (Complement fixation stage): • A known antigen and inactivated patient’s serum are incubated with a standardized, limited amount of complement. • Note: patient’s serum is heated at 56°C for 30 minutes to inactivate endogenous complement which may disturb the test calibration. • If the serum contains specific complement activating antibody, the complement will be activated or fixed by the antigen-antibody complex. • However, if there is no antibody in the patient’s serum, there will be no formation of antigen-antibody complex, thus complement will not be fixed but will remain free (In the indicator stage this complement will react with RBC coated with antibody to sheep RBC ).
principle
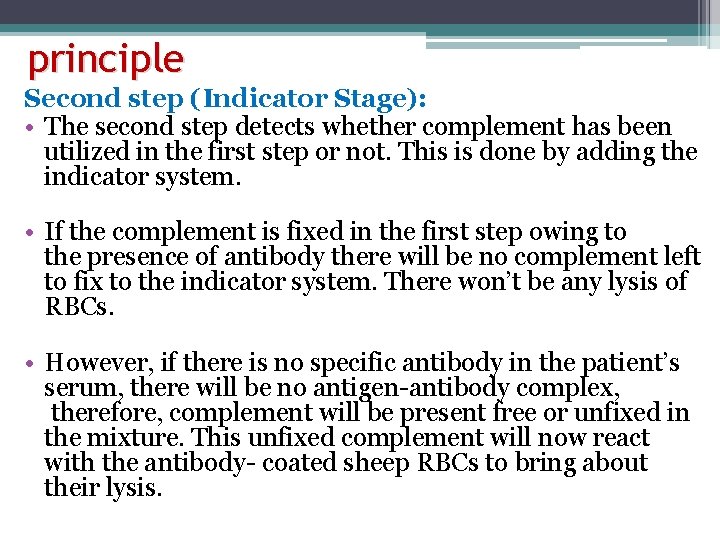
principle Second step (Indicator Stage): • The second step detects whether complement has been utilized in the first step or not. This is done by adding the indicator system. • If the complement is fixed in the first step owing to the presence of antibody there will be no complement left to fix to the indicator system. There won’t be any lysis of RBCs. • However, if there is no specific antibody in the patient’s serum, there will be no antigen-antibody complex, therefore, complement will be present free or unfixed in the mixture. This unfixed complement will now react with the antibody- coated sheep RBCs to bring about their lysis.
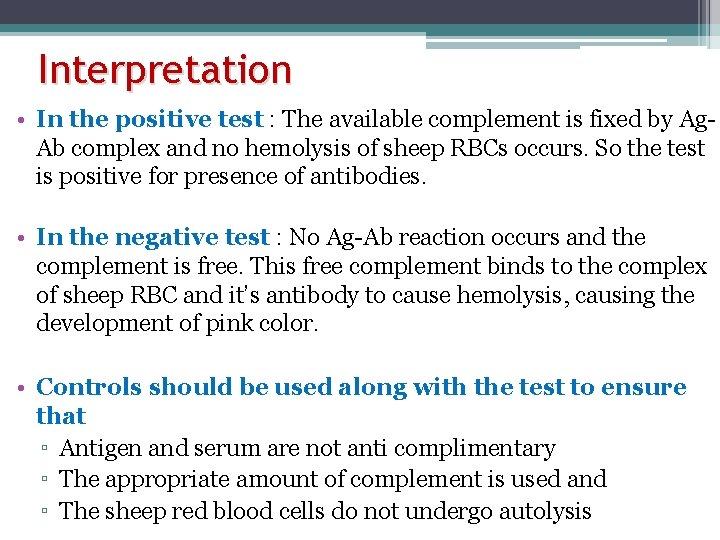
Interpretation • In the positive test : The available complement is fixed by Ag. Ab complex and no hemolysis of sheep RBCs occurs. So the test is positive for presence of antibodies. • In the negative test : No Ag-Ab reaction occurs and the complement is free. This free complement binds to the complex of sheep RBC and it’s antibody to cause hemolysis, causing the development of pink color. • Controls should be used along with the test to ensure that ▫ Antigen and serum are not anti complimentary ▫ The appropriate amount of complement is used and ▫ The sheep red blood cells do not undergo autolysis
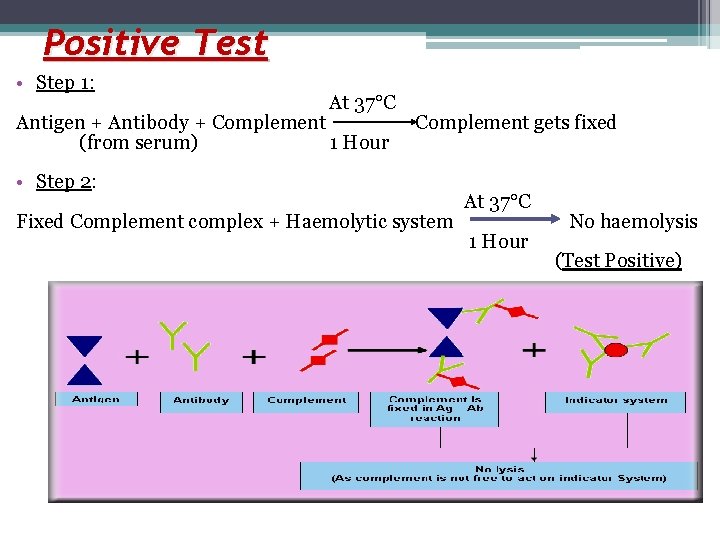
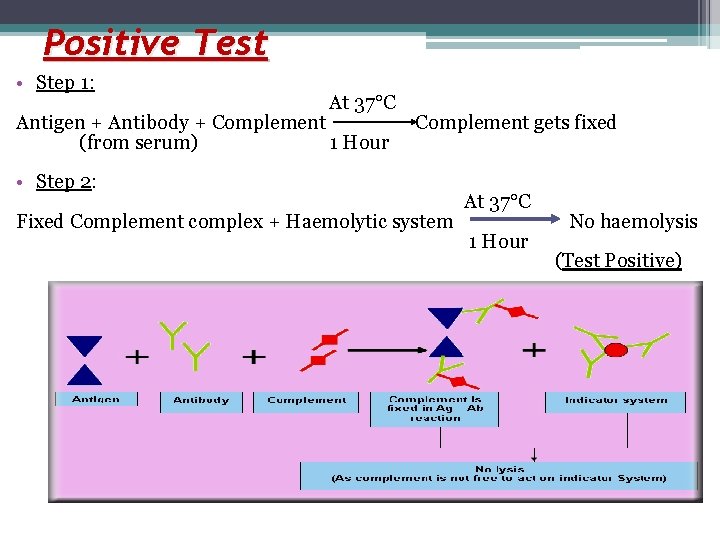
Positive Test • Step 1: At 37°C Antigen + Antibody + Complement gets fixed (from serum) 1 Hour • Step 2: At 37°C Fixed Complement complex + Haemolytic system No haemolysis 1 Hour (Test Positive)
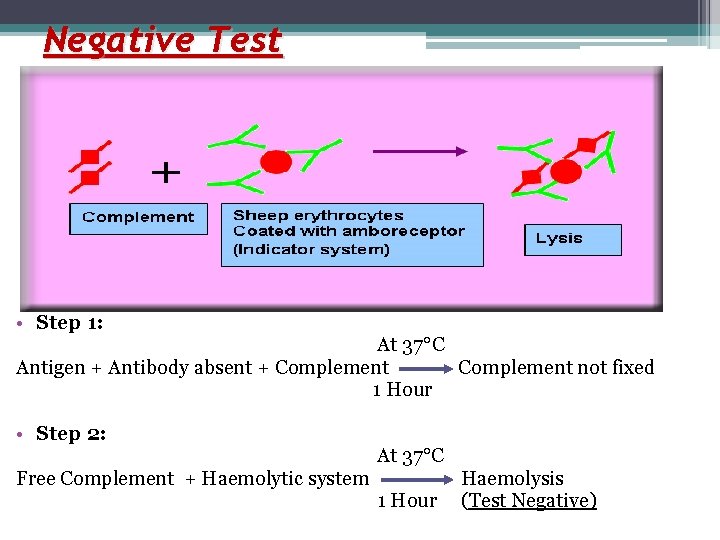
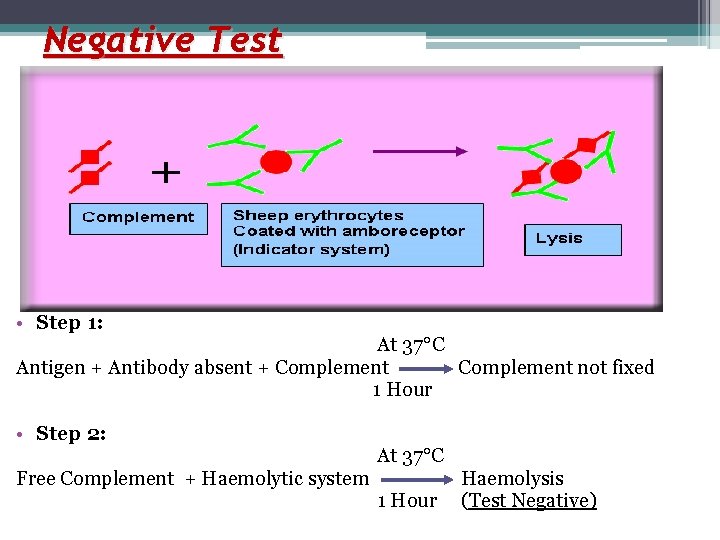
Negative Test • Step 1: At 37°C Antigen + Antibody absent + Complement not fixed 1 Hour • Step 2: At 37°C Free Complement + Haemolytic system Haemolysis 1 Hour (Test Negative)
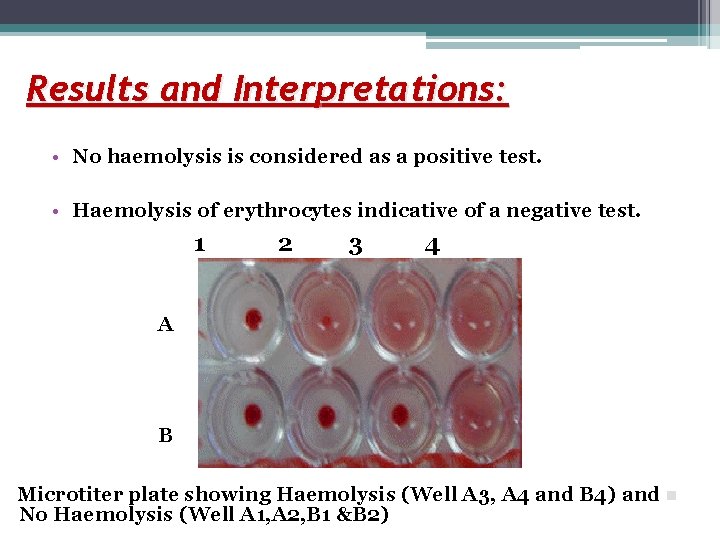
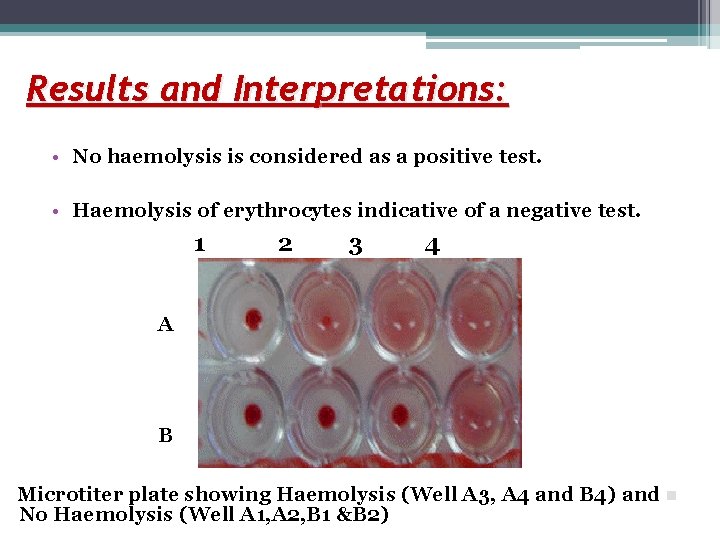
Results and Interpretations: • No haemolysis is considered as a positive test. • Haemolysis of erythrocytes indicative of a negative test. 1 2 3 4 A B Microtiter plate showing Haemolysis (Well A 3, A 4 and B 4) and n No Haemolysis (Well A 1, A 2, B 1 &B 2)
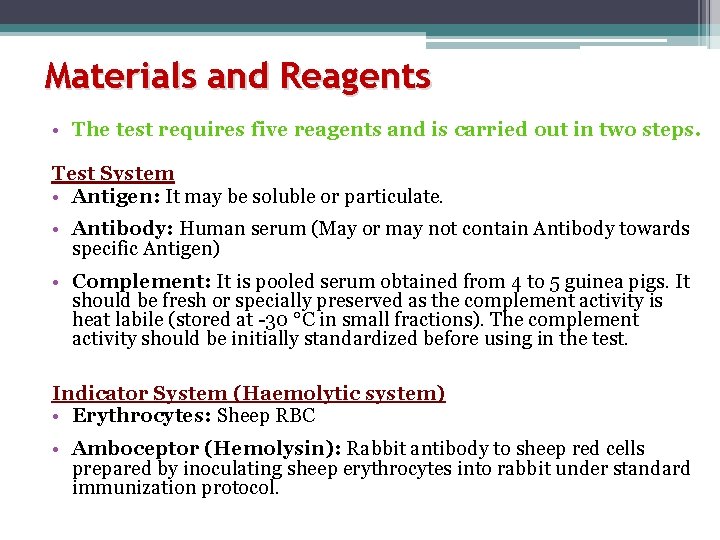
Materials and Reagents • The test requires five reagents and is carried out in two steps. Test System • Antigen: It may be soluble or particulate. • Antibody: Human serum (May or may not contain Antibody towards specific Antigen) • Complement: It is pooled serum obtained from 4 to 5 guinea pigs. It should be fresh or specially preserved as the complement activity is heat labile (stored at -30 °C in small fractions). The complement activity should be initially standardized before using in the test. Indicator System (Haemolytic system) • Erythrocytes: Sheep RBC • Amboceptor (Hemolysin): Rabbit antibody to sheep red cells prepared by inoculating sheep erythrocytes into rabbit under standard immunization protocol.
Advantages and disadvantages of CFT Advantages 1. Ability to screen against a large number of viral and bacterial infections at the same time. 2. Economical. Disadvantages 1. Not sensitive - cannot be used for immunity screening 2. Time consuming and labor intensive 3. Often non-specific e. g. cross-reactivity between HSV and VZV
Modifications of complement fixation test Indirect complement fixation test: • This modification is used when serums which don’t fix guinea pig complement is to be tested. • Seras of duck, turkey, parrot, horse, cat unable to fix guinea pig complement. • After step 1, standard antiserum to antigen which is known to fix complement is added to one set. • If antibodies were not present in the test serum then the antigen would react with the standard antiserum fixing the complement. • On the other hand if antibodies are present in the test serum the antigen would be utilized in the first step. So, no reaction would occur between the standard antiserum and the antigen and therefore no fixation of complement would cause lysis of sheep red blood cells. Thus in this case haemolysis indicates a positive result.
Congulating complement absorption test • Here horse complement which is non-haemolytic is used. • The indicator system used is sensitized sheep red blood cells mixed with bovine serum. • Bovine serum contains a beta globulin called conglutinin would also combine with this complement causing agglutination (conglutination) of the sheep red blood cells, indicating a negative result.
Immune adherence • When some bacteria (such as vibrio cholera or treponemapallidum) combine with their specific antibody in the presence of complement and some particles such as erythrocytes or platelets, they adhere to the erythrocytes or platelets. This is called immune adherence.
Immobilisation test • Here antigen is incubated with patient’s serum in presence of complement. • If specific antibody is present it would immobilize the antigen. Eg. Treponema palladium immobilization test, considered gold standard for the serodiagnosis of syphilis
Cytolytic tests • The incubation of a live bacterium with its specific antibody in the presence of complement leads to the lysis of the bacteria cells. • This is the basis of vibriocidal antibody test used to measure anticholera antibodies.
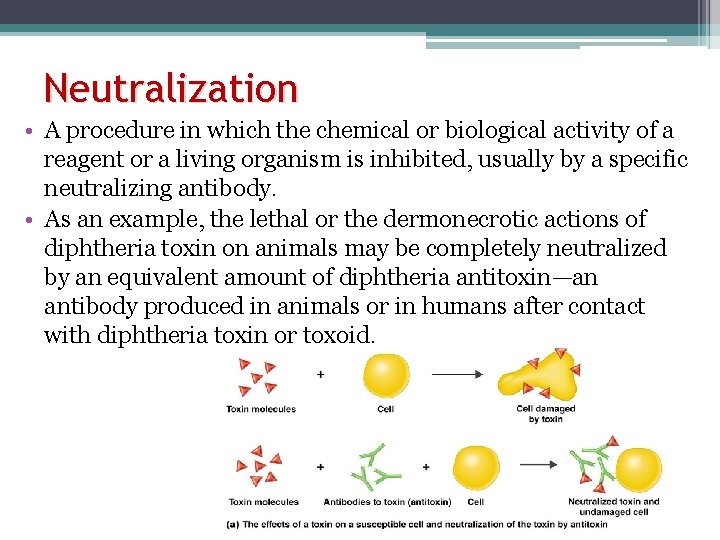
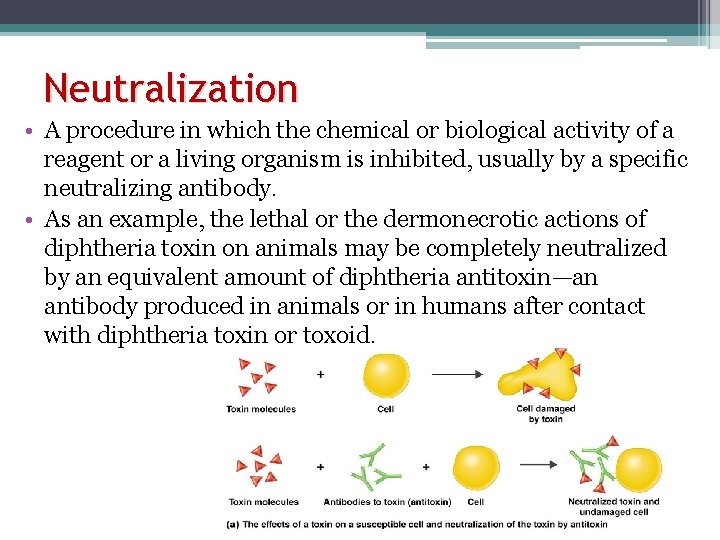
Neutralization • A procedure in which the chemical or biological activity of a reagent or a living organism is inhibited, usually by a specific neutralizing antibody. • As an example, the lethal or the dermonecrotic actions of diphtheria toxin on animals may be completely neutralized by an equivalent amount of diphtheria antitoxin—an antibody produced in animals or in humans after contact with diphtheria toxin or toxoid.
Neutralization • Lesser amounts of antitoxin provide intermediate degrees of inhibition. • These facts provide the basis for the Schick test for susceptibility to diphtheria. • Tetanus and botulinus toxins may be similarly inhibited by their specific antitoxins. • In contrast, the typical toxins of dysentery and other gram-negative bacteria are only slightly neutralized, even by large excesses of antibody.