Congenital Cyanotic Heart Disease Ghada ElShahed MD Assistant










- Slides: 39

Congenital Cyanotic Heart Disease Ghada El-Shahed, MD Assistant Professor of Cardiology
Cyonosis o It occurs when there is > 3 mg/dl reduced hemoglobin. o Central vs. peripheral cyanosis o Congenital Cyanotic Heart Disease >>> central cyanosis
Tetralogy of Fallot o 10 % of all CHD o. The commonest Congenital Cyanotic Heart Disease

PATHOLOGY
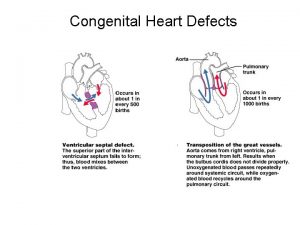
This malformation has 4 components: o VSD o Obstruction to RV outflow (Infundibular, valvular) o Overriding of the aorta o RV hypertrophy

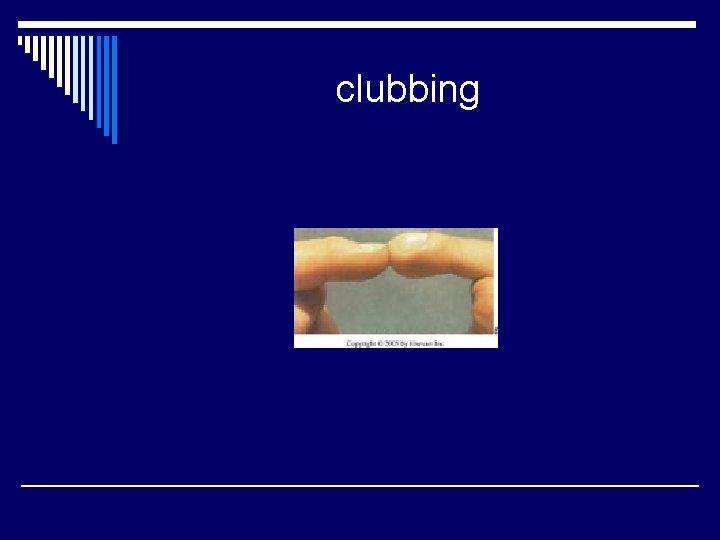
Clinical Picture o Cyanosis (onset < 1 year) o Clubbing ( > 1 year) o Effort intolerance o Squatting o Failure to thrive and delayed milestones o Cyanotic spells (hypoxic sells)
Physical signs General o Delayed development o Central cyanosis o Clubbing o Squatting position
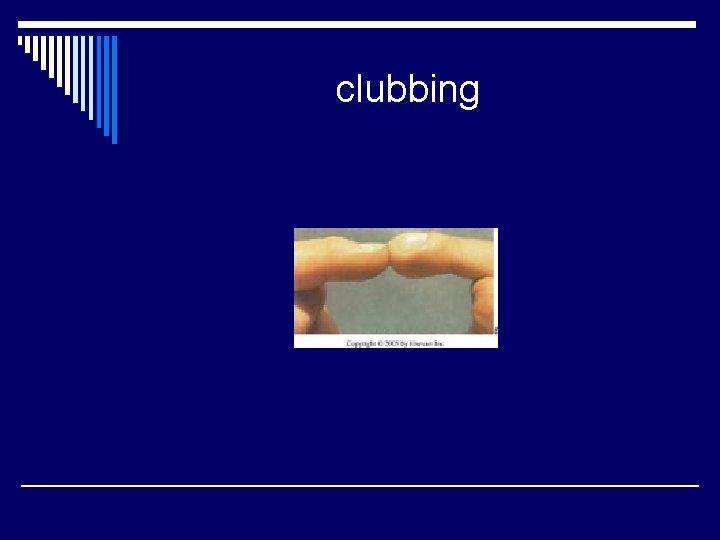
clubbing
Physical signs Local o Quiet precordium with no bulge o RV impulse : Lt. sternal border o Systolic thrill
auscultation o Loud single S 2 (aortic in origin) o Ejection systolic murmur (upper LSB) (intensity is inversely proportional to severity of obstruction) Very faint or absent during cyanotic spell o Continuous murmur: PDA or collaterals
Complications o Cyanotic spells o Polycythemia, coagulation disorders o Infective endocarditis o Paradoxical embolization o Brain abscess or infarction
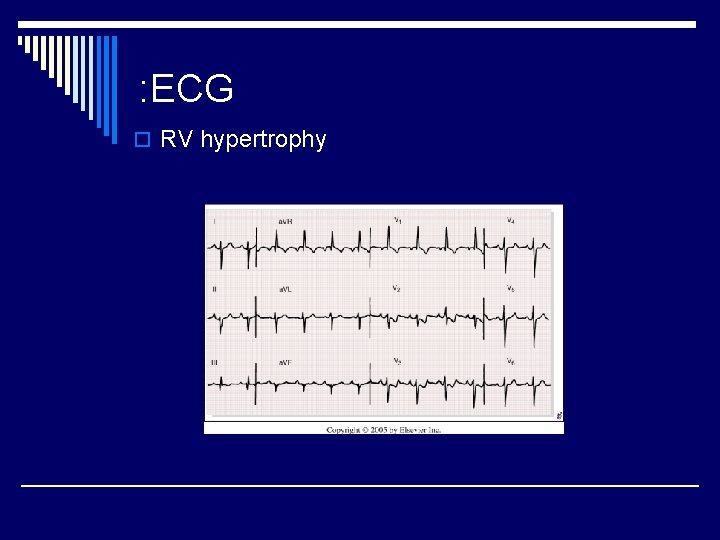
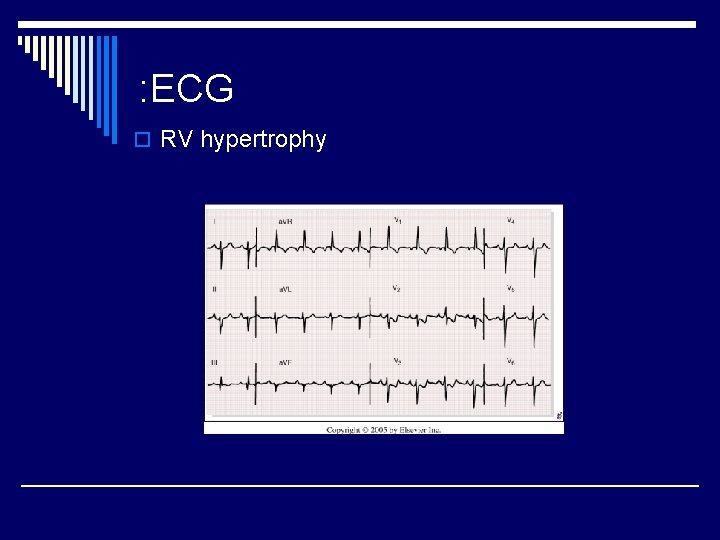
: ECG o RV hypertrophy
Chest X-ray o. Normal-sized boot shaped heart ( RV prominence + concavity at PA) o. Decreased pulmonary vascular markings o. Right-sided aortic arch

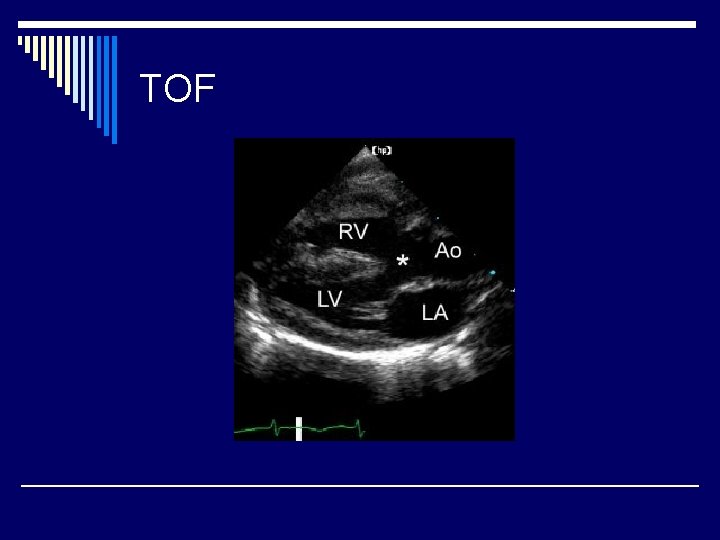
Echocardiography o. Diagnosis o. Decision-making o. Pre-and post-operative evaluation
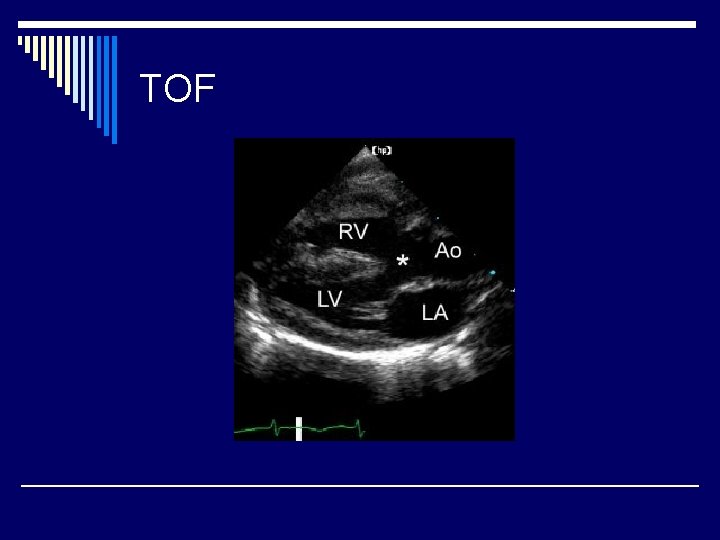
TOF

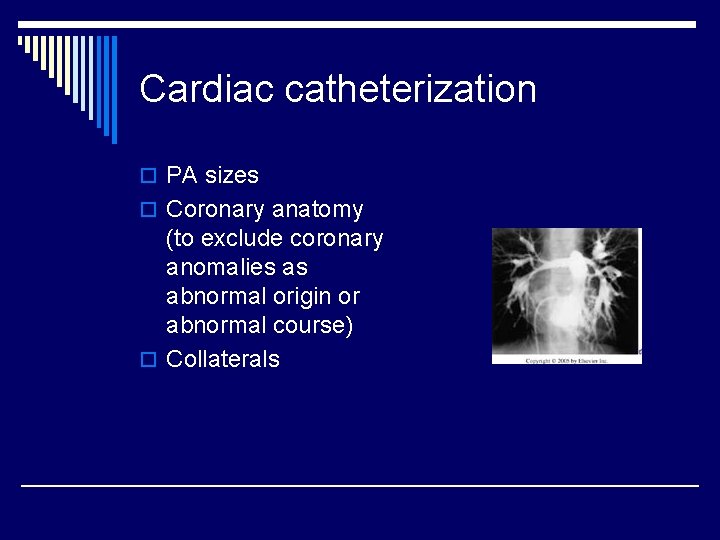
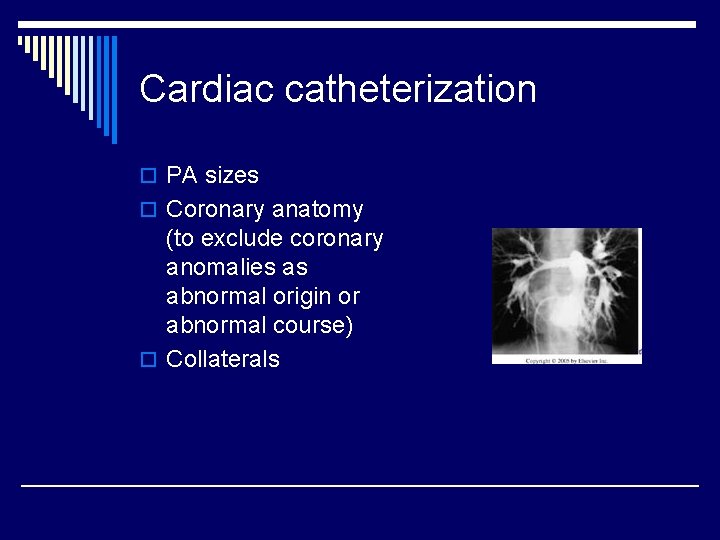
Cardiac catheterization o PA sizes o Coronary anatomy (to exclude coronary anomalies as abnormal origin or abnormal course) o Collaterals

Managemement
o Medical: --Infective endocarditis prophylaxis and treatment -- Treatment of cyanotic spell * Oxygen * Knee-chest position * Morphia * Correct acid-base balance * Fluids, vasopressors * Ventilation * Prevention of recurrence
Surgical treatment o Palliative: Shunt surgery o Corrective: VSD closure, Infundibular resection to relieve RVOT obstruction, trans-annular patch. o Choice: RVOT anatomy and PA sizes are the most important factors
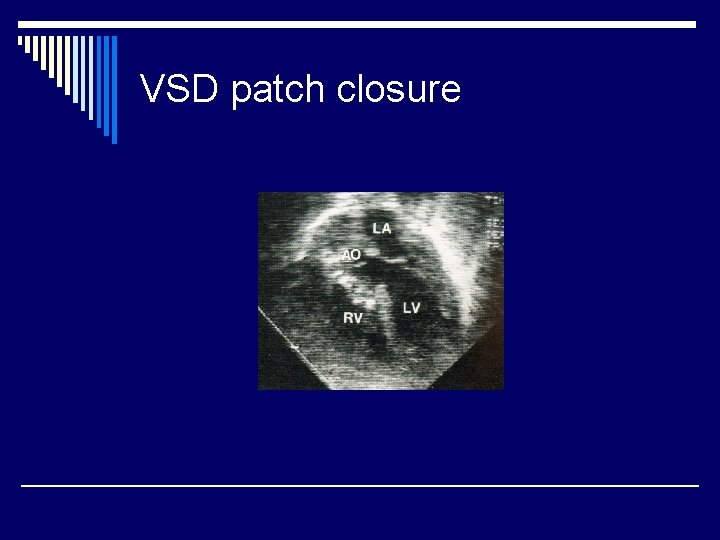
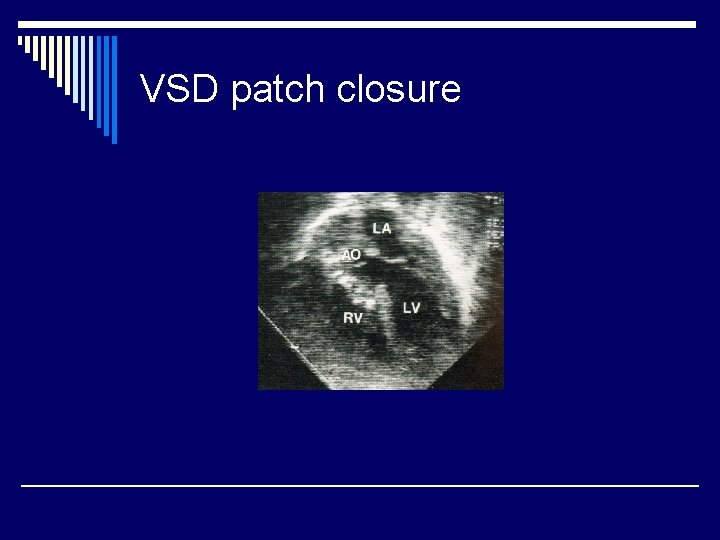
VSD patch closure
Transposition of the (great arteries (TGA


Eisenminger Syndrome ( (reversed shunt
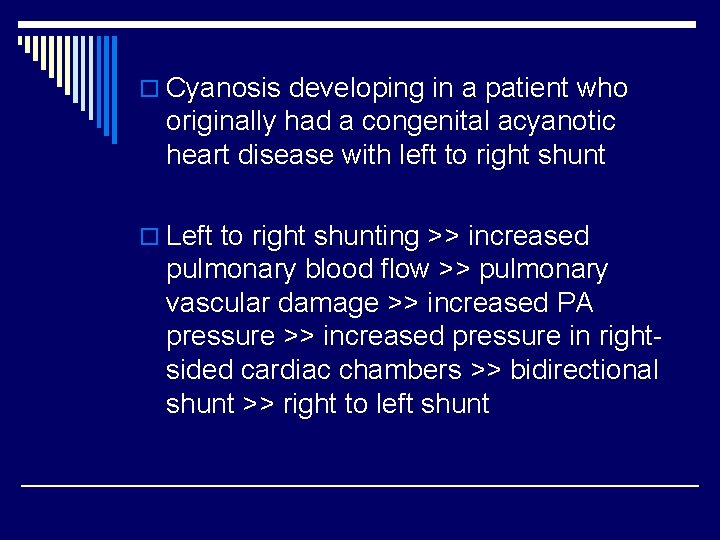
o Cyanosis developing in a patient who originally had a congenital acyanotic heart disease with left to right shunt o Left to right shunting >> increased pulmonary blood flow >> pulmonary vascular damage >> increased PA pressure >> increased pressure in rightsided cardiac chambers >> bidirectional shunt >> right to left shunt
VSD with reversed shunt o Decreased signs of hyperdynamic LV (due to decrease of shunt) o Diminished murmur >> absent o Signs of RV pressure overload o Cyanosis with effort >> at rest o Clubbing
o ECG: RV hypertrophy o Echo: RV enlargement Markedly increased RV pressure VSD flow is mainly right to left o Cardiac catheterization: Increased pulmonary vascular resistance o Corrective surgery is contra-indicated

Questions
The most common congenital : cyanotic heart disease is o TGA o Tetralogy of Fallot o Tricuspid atresia o Eisenminger disease
The most important investigation to diagnose Tetralogy of Fallot is o Cardiac catheterization o Echocardiography o ECG o Chest X-ray
Cyanosis in Tetralogy of Fallot is o Always present since birth o Never present since birth o Usually appears after birth
The second heart sound in Tetralogy of Fallot is o Widely split o Narrowly split o Very faint o Usually single
The treatment of Eisenminger disease is o. Urgent surgical defect closure o. Urgent defect closure by cardiac cathterization o. Medical treatment
o Discuss the clinical picture and the treatment options for a patient with Tetralogy of Fallot o Discuss the complications of uncorrected Tetralogy of Fallot and the detailed management of one of them

 Difference between cyanotic and acyanotic heart disease
Difference between cyanotic and acyanotic heart disease 5 cyanotic congenital heart disease
5 cyanotic congenital heart disease 5 terrible ts
5 terrible ts Pediatric knee chest position
Pediatric knee chest position Congenital heart disease pda
Congenital heart disease pda Congenital heart
Congenital heart Congenital heart defect
Congenital heart defect Canadian congenital heart alliance
Canadian congenital heart alliance Ghada jamal
Ghada jamal Ghada chahrour
Ghada chahrour Ghada kassab
Ghada kassab Ghada ramadan
Ghada ramadan Cyanotic spells
Cyanotic spells Patent ductus arteriosus pathophysiology
Patent ductus arteriosus pathophysiology Anoxic spell
Anoxic spell Communicable disease and non communicable disease
Communicable disease and non communicable disease Cvds
Cvds Coronary heart disease
Coronary heart disease Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Charyties
Charyties Heart disease
Heart disease Causes of valvular heart disease
Causes of valvular heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Mitral regurgitation symptoms
Mitral regurgitation symptoms Chronic rheumatic heart disease
Chronic rheumatic heart disease Antianginal drugs classification
Antianginal drugs classification Dopamine uses
Dopamine uses Heart disease cat
Heart disease cat Watch?v=0evgft8hgns
Watch?v=0evgft8hgns Fish mouth or buttonhole stenosis
Fish mouth or buttonhole stenosis Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Heart disease symptoms
Heart disease symptoms Rheumatic heart disease
Rheumatic heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Causes of valvular heart disease
Causes of valvular heart disease Heart disease data
Heart disease data Nyha classification
Nyha classification Rhuematic fever
Rhuematic fever Upper lobe venous diversion
Upper lobe venous diversion Pico question examples heart disease
Pico question examples heart disease