Complications of fractures 1 The general complications of




- Slides: 26
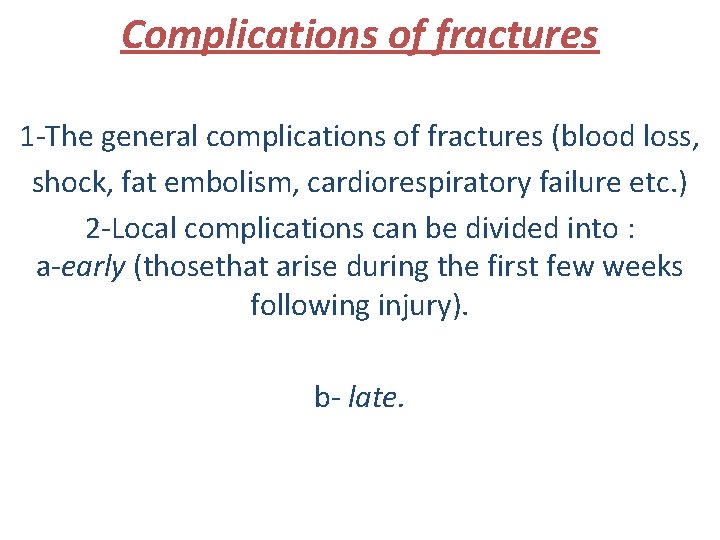
Complications of fractures 1 -The general complications of fractures (blood loss, shock, fat embolism, cardiorespiratory failure etc. ) 2 -Local complications can be divided into : a-early (thosethat arise during the first few weeks following injury). b- late.
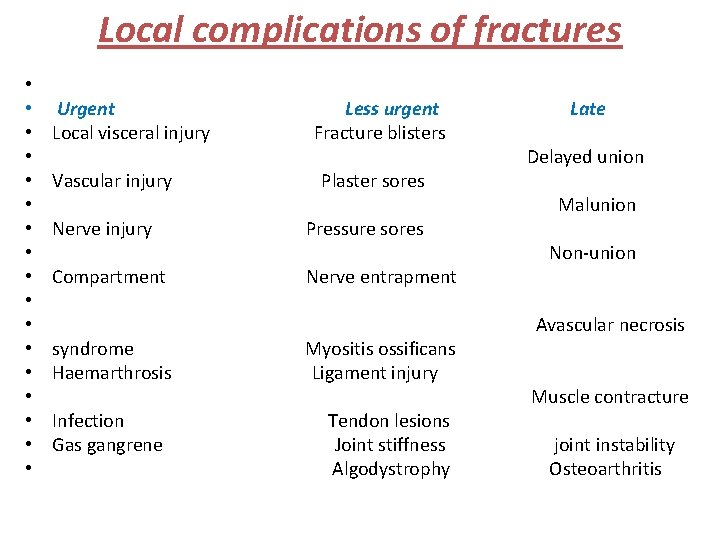
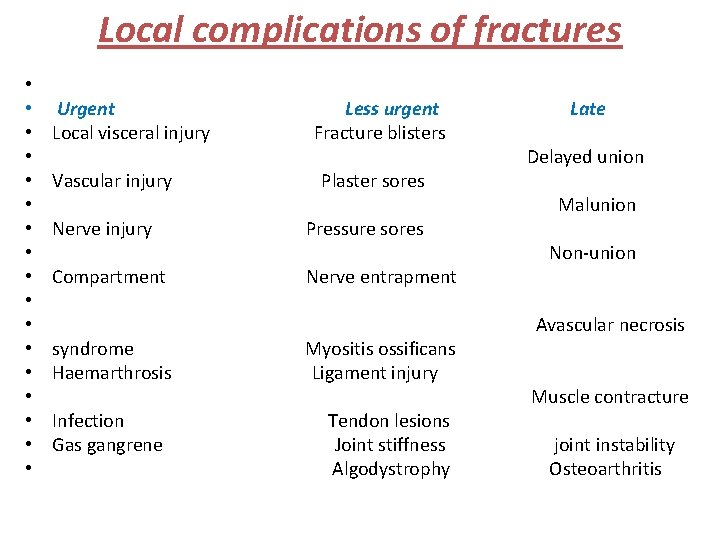
Local complications of fractures • • • • • Urgent Local visceral injury Vascular injury Less urgent Fracture blisters Plaster sores Nerve injury Pressure sores Compartment Nerve entrapment syndrome Haemarthrosis Infection Gas gangrene Myositis ossificans Ligament injury Tendon lesions Joint stiffness Algodystrophy Late Delayed union Malunion Non-union Avascular necrosis Muscle contracture joint instability Osteoarthritis
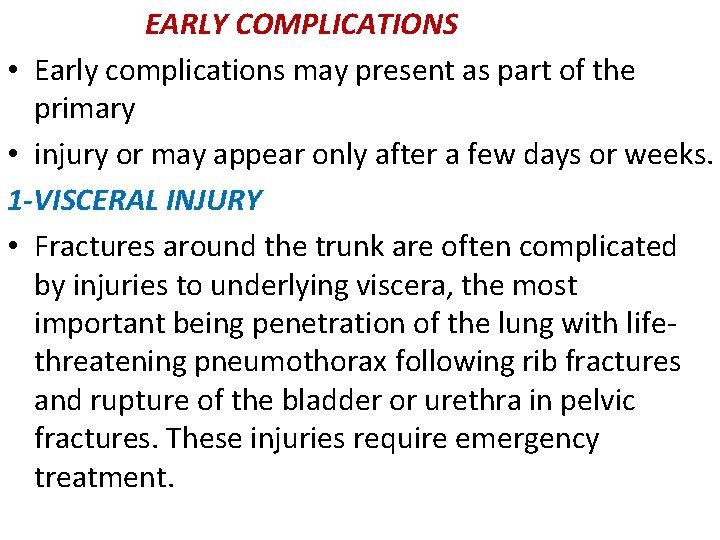
EARLY COMPLICATIONS • Early complications may present as part of the primary • injury or may appear only after a few days or weeks. 1 -VISCERAL INJURY • Fractures around the trunk are often complicated by injuries to underlying viscera, the most important being penetration of the lung with lifethreatening pneumothorax following rib fractures and rupture of the bladder or urethra in pelvic fractures. These injuries require emergency treatment.
2 -VASCULAR INJURY The fractures most often associated with damage to a major artery are those around the knee and elbow, and those of the humeral and femoral shafts. The artery may be cut, torn, compressed or contused, either by the initial injury or subsequently by jagged bone fragments. The effects vary from transient diminution of blood flow to profound ischaemia, tissue death and peripheral gangrene.
• Clinical features The patient may complain of paraesthesia or numbnessin the toes or the fingers. The injured limb is cold and pale, or slightly cyanosed, and the pulse is weak or absent. X-rays will probably show one of the ‘highrisk’fractures listed above. If a vascular injury is suspected an angiogram should be performed immediately; if it is positive, emergency treatment must be started without further delay. • Treatment All bandages and splints should be removed. The fracture is re-x-rayed and, if the position of the bones suggests that the artery is being compressed or kinked, prompt reduction is necessary. The circulation is then reassessed repeatedly over the next half hour. If there is no improvement, the vessels must be explored by operation preferably with the benefit of preoperative or peroperative angiography. A cut vessel can be sutured, or a segment may be replaced by a vein graft; if it is thrombosed, endarterectomy may restore the blood flow. If vessel repair is undertaken, stable fixation is a must and where it is practicable, the fracture should be fixed internally.

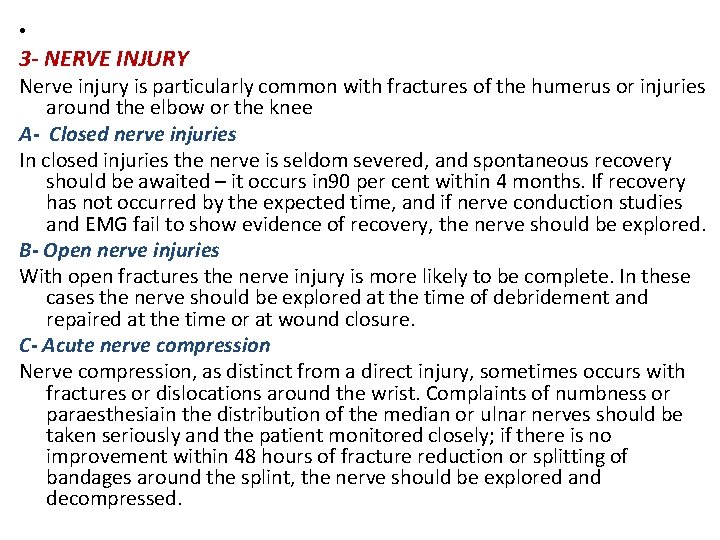
• 3 - NERVE INJURY Nerve injury is particularly common with fractures of the humerus or injuries around the elbow or the knee A- Closed nerve injuries In closed injuries the nerve is seldom severed, and spontaneous recovery should be awaited – it occurs in 90 per cent within 4 months. If recovery has not occurred by the expected time, and if nerve conduction studies and EMG fail to show evidence of recovery, the nerve should be explored. B- Open nerve injuries With open fractures the nerve injury is more likely to be complete. In these cases the nerve should be explored at the time of debridement and repaired at the time or at wound closure. C- Acute nerve compression Nerve compression, as distinct from a direct injury, sometimes occurs with fractures or dislocations around the wrist. Complaints of numbness or paraesthesiain the distribution of the median or ulnar nerves should be taken seriously and the patient monitored closely; if there is no improvement within 48 hours of fracture reduction or splitting of bandages around the splint, the nerve should be explored and decompressed.
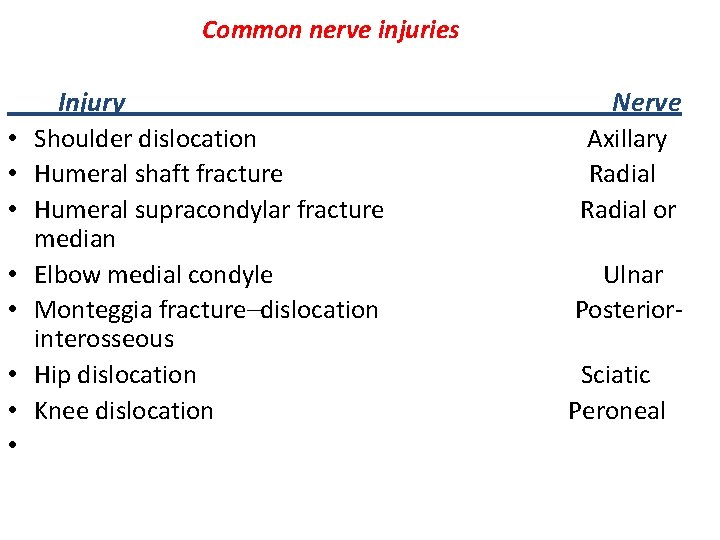
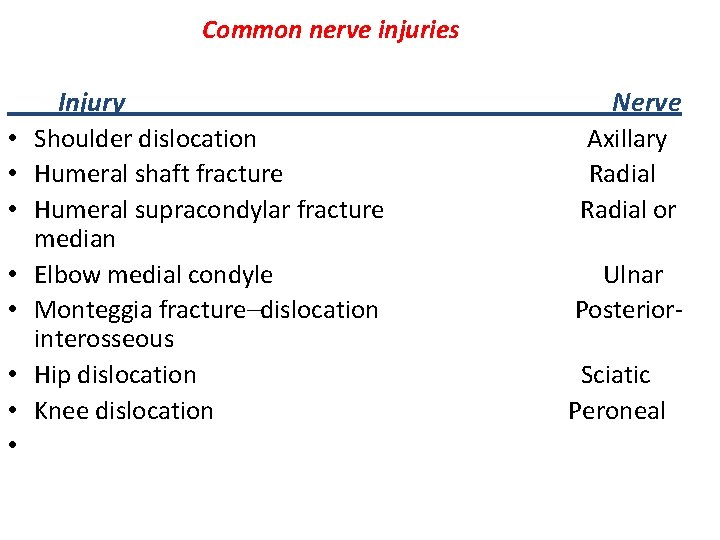
Common nerve injuries • • Injury Shoulder dislocation Humeral shaft fracture Humeral supracondylar fracture median Elbow medial condyle Monteggia fracture–dislocation interosseous Hip dislocation Knee dislocation Nerve Axillary Radial or Ulnar Posterior. Sciatic Peroneal
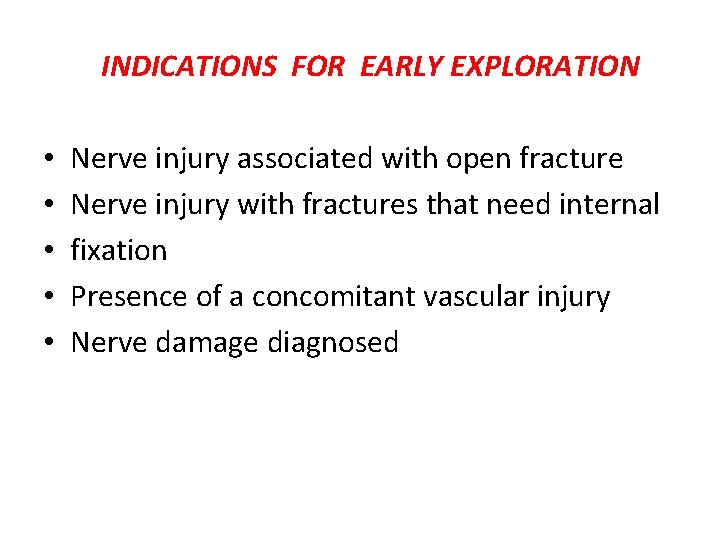
INDICATIONS FOR EARLY EXPLORATION • • • Nerve injury associated with open fracture Nerve injury with fractures that need internal fixation Presence of a concomitant vascular injury Nerve damage diagnosed
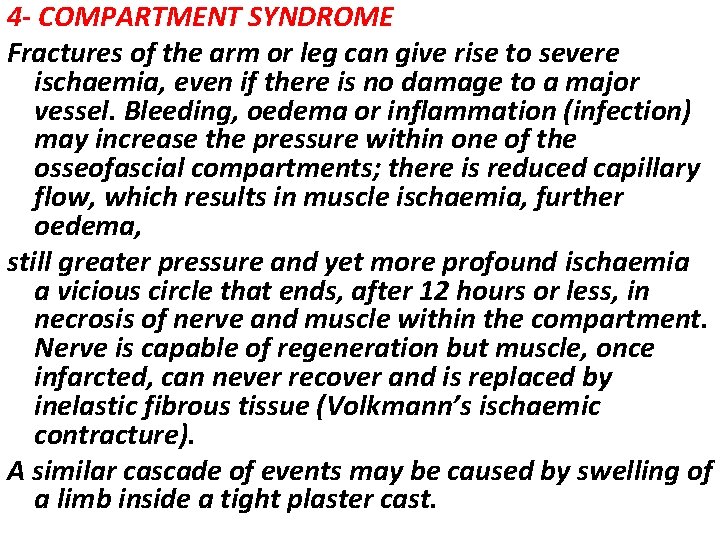
4 - COMPARTMENT SYNDROME Fractures of the arm or leg can give rise to severe ischaemia, even if there is no damage to a major vessel. Bleeding, oedema or inflammation (infection) may increase the pressure within one of the osseofascial compartments; there is reduced capillary flow, which results in muscle ischaemia, further oedema, still greater pressure and yet more profound ischaemia a vicious circle that ends, after 12 hours or less, in necrosis of nerve and muscle within the compartment. Nerve is capable of regeneration but muscle, once infarcted, can never recover and is replaced by inelastic fibrous tissue (Volkmann’s ischaemic contracture). A similar cascade of events may be caused by swelling of a limb inside a tight plaster cast.
Clinical features • High-risk injuries are fractures of the elbow, forearm bones, proximal third of the tibia, and also multiple fractures of the hand or foot, crush injuries and circumferential burns. Other precipitating factors are operation (usually for internal fixation) or infection. • The classic features of ischaemia are the five Ps: PAIN Paraesthesia Pallor Paralysis Pulselessness

• However in compartment syndrome the ischaemia occurs at the capillary level, so pulses may still be felt • and the skin may not be pale! The earliest of the ‘classic’features are pain (or a ‘bursting’ sensation), altered sensibility and paresis (or, more usually, weakness in active muscle contraction). • Ischaemic muscle is highly sensitive to stretch. If the limb is unduly painful, swollen or tense, the muscles (which may be tender) should be tested by stretching them. When the toes or fingers are passively hyperextended, there is increased pain in the calf or forearm. • Confirmation of the diagnosis can be made by measuring the intracompartmental pressures. So important is the need for early diagnosis that some surgeons advocate the use of continuous compartment pressure monitoring for high-risk injuries (e. g. fractures of the tibia and fibula) and especially forearm or leg fracture in patients who are unconscious. A split catheter is introduced into the compartment and the pressure is measured close to the level of the fracture. A differential pressure (ΔP) – the difference between diastolic pressure and compartment pressure – of less than 30 mm. Hg (4. 00 kilopascals) is an indication for immediate compartment decompression.
Treatment The threatened compartment (or compartments) must be promptly decompressed. Casts, bandages and dressings must be completely removed – merely splitting the plaster is utterly useless – and the limb should be nursed flat (elevating the limb causes a further decrease in end capillary pressure and aggravates the muscle ischaemia). The ΔP should be carefully monitored; if it falls below 30 mm. Hg, immediate open fasciotomy is performed. In the case of the leg, ‘fasciotomy’ means opening all four compartments through medial and lateral incisions. The wounds should be left open and inspected 2 days later:

5 -HAEMARTHROSIS Fractures involving a joint may cause acute haemarthrosis. The joint is swollen and tense and the patient resists any attempt at moving it. The blood should be aspirated before dealing with the fracture. 6 -INFECTION Open fractures may become infected; closed fractures hardly ever do unless they are opened by operation. Post-traumatic wound infection is now the most common cause of chronic osteitis.
LATE COMPLICTIONS 1 -DELAYED UNION • Causes A-BIOLOGICAL • Inadequate blood supply A badly displaced fracture of a long bone will cause tearing of both the periosteum and interruption of the intramedullary blood supply. The fracture edges will become necrotic and dependent on the formation of an ensheathing callus mass to bridge the break. If the zone of necrosis is extensive, as might occur in highly comminuted fractures, union may be hampered. • Severe damage to the soft tissues affects fracture healing by: (1) reducing the effectiveness of muscle splintage; (2) damaging the local blood supply and (3) diminishing or eliminating the osteogenic input from mesenchymal stem cells within muscle. • Periosteal stripping Over-enthusiastic stripping of periosteum during internal fixation is an avoidable cause of delayed union. • Infection Both biology and stability are hampered by active infection: not only is there bone lysis, necrosis and pus formation, but implants which are used to hold the fracture tend to loosen B- BIOMECHANICAL • Imperfect splintage Excessive traction (creating a fracture gap) or excessive movement at the fracture site will delay ossification in the callus. In the forearm and
• leg a single-bone fracture may be held apart by anntact fellow bone. • Over-rigid fixation Contrary to popular belief, rigid fixation delays rather than promotes fracture union. C-PATIENT RELATED • In a less than ideal world, there are patients who are: • • Immense • • Immoderate • • Immovable • • Impossible.
• Clinical features • • Fracture tenderness persists and, if the bone is subjectedto stress, pain may be acute. On x-ray, the fracture line remains visible and there is very little or incomplete callus formation or periosteal reaction. However, the bone ends are not sclerosed or atrophic. The appearances suggest that, although the fracture has not united, it eventually will. • Treatment • • CONSERVATIVE The two important principles are: (1) to eliminate any possible cause of delayed union and (2) to promote healing by providing the most appropriate environment. Immobilization (whether by cast or by internal fixation) should be sufficient to prevent shear at the fracture site, but fracture loading is an important stimulus to union and can be enhanced by: (1) encouraging muscular exercise and (2) by weightbearing in the cast or brace. The watchword is patience; however, there comes a point with every fracture where the illeffects of prolonged immobilization outweigh the advantages of non-operative treatment, or where the risk of implant breakage begins to loom. OPERATIVE Each case should be treated on its merits; however, if union is delayed for more than 6 months and there is no sign of callus formation, internal fixation and bone grafting are indicated.
2 -NON-UNION • In a minority of cases delayed union gradually turns into non-union – that is it becomes apparent that the fracture will never unite without intervention. • Movement can be elicited at the fracture site and pain diminishes; the fracture gap becomes a type of pseudoarthrosis. • X-ray The fracture is clearly visible but the bone on either side of it may show either exuberant callus or atrophy. This contrasting appearance has led to nonunion being divided into hypertrophic and atrophic types. In hypertrophic nonunion the bone ends are enlarged, suggesting that osteogenesis is still active but not quite capable of bridging the gap. In atrophic non-union, osteogenesis seems to have ceased. The bone ends are tapered or rounded with no suggestionof new bone formation.

Treatment • CONSERVATIVE Non-union is occasionally symptomless, needing no treatment or, at most, a removable splint. Even if symptoms are present, operation is not the onlyanswer; with hypertrophic non-union, functional bracing may be sufficient to induce union, but splintage often needs to be prolonged. Pulsed electromagnetic fields and low-frequency, pulsed ultrasound can also be used to stimulate union. • OPERATIVE 1 - With hypertrophic non-union and in the absence of deformity, very rigid fixation alone (internal or external) may lead to union. 2 -With atrophic non-union, fixation alone is not enough. Fibrous tissue in the fracture gap, as well as the hard, sclerotic bone ends is excised and bone grafts are packed around the fracture with internal or illizarov fixation
3 -MALUNION When the fragments join in an unsatisfactory position (unacceptable angulation, rotation or shortening) the fracture is said to be malunited. Causes are failure to reduce a fracture adequately, failure to hold reduction while healing proceeds, or gradual collapse of comminuted or osteoporotic bone. • Clinical features • The deformity is usually obvious, but sometimes the true extent of malunion is apparent only on x-ray. Rotational deformity of the femur, tibia, humerus or forearm may be missed unless the limb is compared with its opposite fellow. Rotational deformity of a metacarpal fracture is detected by asking the patient to flatten the fingers onto the palm and seeing whether the normal regular fan-shaped appearance I reproduced • X-rays are essential to check the position of the fracture while it is uniting. This is particularly important during the first 3 weeks, when the situation may change without warning. At this stage it is sometimes difficult to decide what constitutes ‘malunion’; acceptable norms differ from one site to another and these are discussed under the individual fractures
• Treatment • Incipient malunion may call for treatment even before the fracture has fully united; the decision on the need • for re-manipulation or correction may be extremely • difficult. A few guidelines are offered: • 1. In adults, fractures should be reduced as near to the anatomical position as possible. Angulation of more than 10– 15 degrees in a long bone or a noticeable rotational deformity may need correction by remanipulation, • or by osteotomy and fixation. • 2. In children, angular deformities near the bone ends (and especially if the deformity is in the same plane as that of movement of the nearby joint) will usually remodel with time; rotational deformities will not. • 3. In the lower limb, shortening of more than 2. 0 cm is seldom acceptable to the patient and a limb length equalizing procedure may be indicated. • 4. The patient’s expectations (often prompted bycosmesis) may be quite different from the surgeon’s; they are not to be ignored • 5. Very little is known of the long-term effects of small angular deformities on joint function. However, it seems likely that malalignment of more than 15 degrees in any plane may cause asymmetrical loading of the joint above or beloand the late development of secondary osteoarthritis; this applies particularly to the large weightbearing joints.
4 - AVASCULAR NECROSIS • Certain regions are notorious for their propensity tovdevelop ischaemia and bone necrosis after injury , They are: (1) the head of the femur (after fracture of the femoral neck or dislocation of the hip); (2) the proximal part of the scaphoid (after fracture through its waist); (3) the lunate (following dislocation) and (4) the body of the talus (after fracture of its neck). • Accurately speaking, this is an early complication of bone injury, because ischaemia occurs during the first few hours following fracture or dislocation. However, the clinical and radiological effects are not seen until weeks or even months later. • Clinical features There are no symptoms associated with avascular necrosis, but if the fracture fails to unite or if the bone collapses the patient may complain of pain. X-ray shows the characteristic increase in x-ray density, which occurs as a consequence of two factors: Disuse osteoporosis in the surrounding parts gives the impression of ‘increased density’ in the necrotic segment, and collapse of trabeculae compacts the bone and increases its density. Where normal bone meets the necrotic segment a zone of increased radiographic density may be produced by new bone formation.
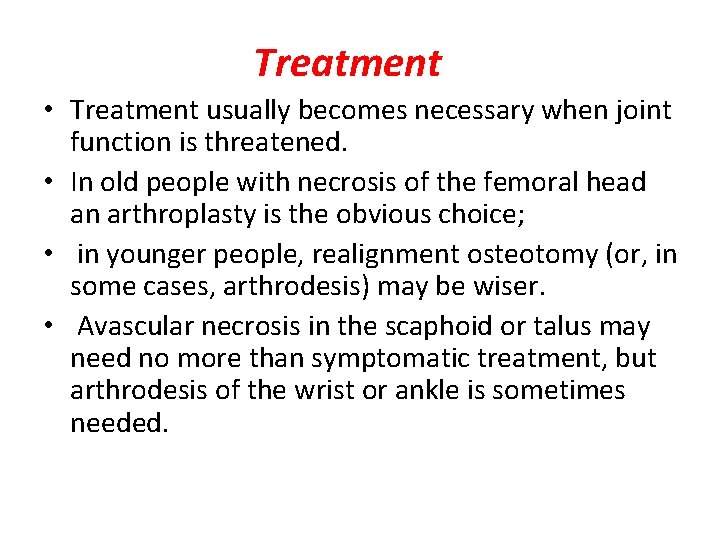
Treatment • Treatment usually becomes necessary when joint function is threatened. • In old people with necrosis of the femoral head an arthroplasty is the obvious choice; • in younger people, realignment osteotomy (or, in some cases, arthrodesis) may be wiser. • Avascular necrosis in the scaphoid or talus may need no more than symptomatic treatment, but arthrodesis of the wrist or ankle is sometimes needed.
 Perkins timetable fracture healing
Perkins timetable fracture healing Phlebitis vs infiltration
Phlebitis vs infiltration Fracture diacondylienne
Fracture diacondylienne Triradiate cartilage x ray
Triradiate cartilage x ray Panfacial fractures sequencing
Panfacial fractures sequencing Concentric glass fracture
Concentric glass fracture Types of fractures with pictures
Types of fractures with pictures Lisa kasman
Lisa kasman Fracture pubis
Fracture pubis Types of glass fractures
Types of glass fractures Daniel tibia
Daniel tibia Activity 14-1 glass fracture patterns answer key
Activity 14-1 glass fracture patterns answer key Tubular shaft of a long bone
Tubular shaft of a long bone Types of rib fractures
Types of rib fractures Fracture en bois vert
Fracture en bois vert Classification of open fractures
Classification of open fractures Ao classification of fractures
Ao classification of fractures Youtube
Youtube Primary bone vs secondary bone
Primary bone vs secondary bone Weber classification of ankle fractures
Weber classification of ankle fractures Irving olecranon fractures
Irving olecranon fractures Open fracture treatment
Open fracture treatment Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua