Complicated Encephalitis Dr Daniel Miller Emergency Medicine Dr

- Slides: 55
Complicated Encephalitis Dr Daniel Miller; Emergency Medicine Dr Joel Panthappattu; Kingston Family Practice Dr Beth Stefanchik; Nephrology Dr Jeremy Barnett; Critical Care / Moderator
www. crowdrise. com/ westchestermedicalcenter healthnetwork
Bias Disclosure Presenters have no direct financial relationship with any for-profit business entity in which the presentation topic is directly related to the business entity, or its products & services There are no disclosures by either speaker that are determined by the ACCME to be relevant relationships to be shared with the participants
Objectives Multidisciplinary review of a controversial subject with immediate impact on patient management & outcomes Evidence-based clinical practice criteria for evaluation & management of AMS associated with significant electrolyte abnormalities
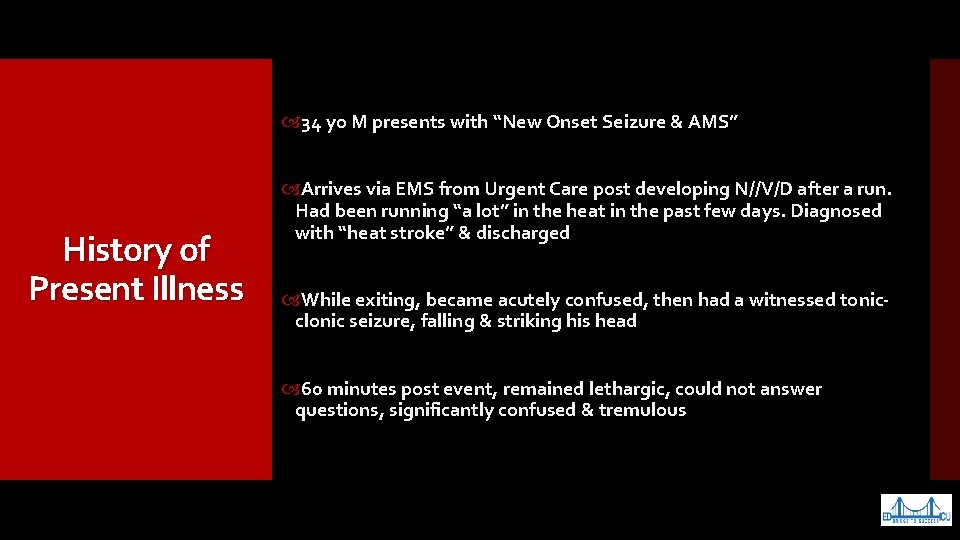
34 yo M presents with “New Onset Seizure & AMS” History of Present Illness Arrives via EMS from Urgent Care post developing N//V/D after a run. Had been running “a lot” in the heat in the past few days. Diagnosed with “heat stroke” & discharged While exiting, became acutely confused, then had a witnessed tonicclonic seizure, falling & striking his head 60 minutes post event, remained lethargic, could not answer questions, significantly confused & tremulous
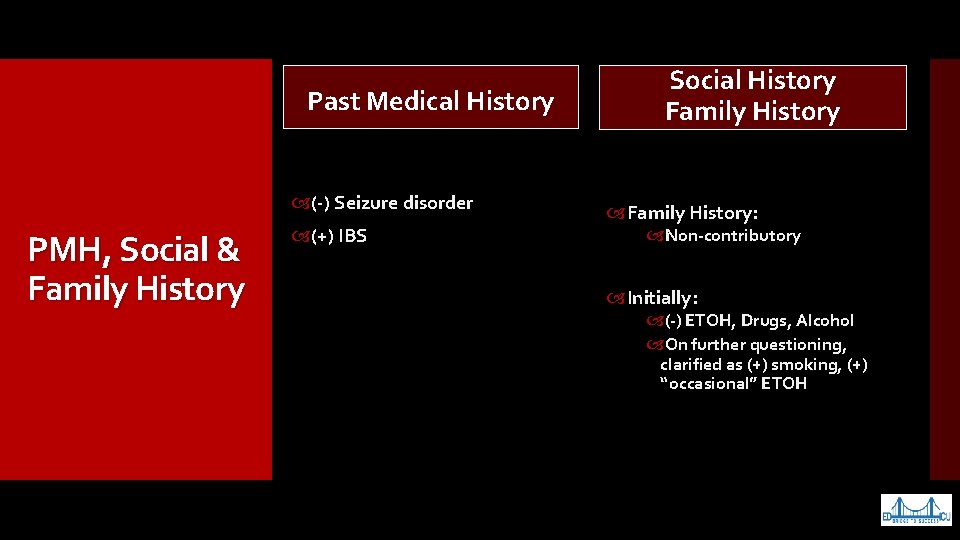
Past Medical History (-) Seizure disorder PMH, Social & Family History (+) IBS Social History Family History: Non-contributory Initially: (-) ETOH, Drugs, Alcohol On further questioning, clarified as (+) smoking, (+) “occasional” ETOH
Allergies NKDA Allergies & Medications Dicyclomine (Bentyl)
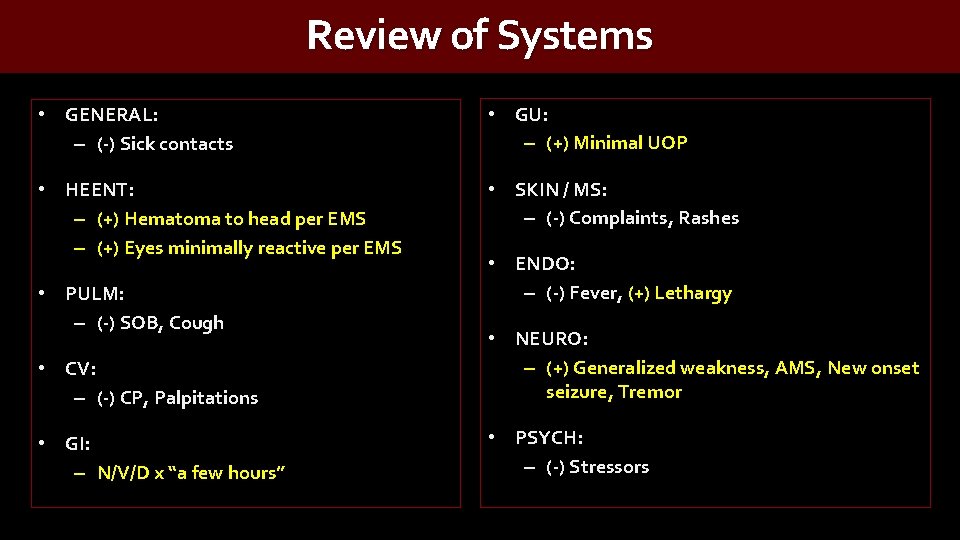
Review of Systems • GENERAL: – (-) Sick contacts • GU: – (+) Minimal UOP • HEENT: – (+) Hematoma to head per EMS – (+) Eyes minimally reactive per EMS • SKIN / MS: – (-) Complaints, Rashes • PULM: – (-) SOB, Cough • ENDO: – (-) Fever, (+) Lethargy • CV: – (-) CP, Palpitations • NEURO: – (+) Generalized weakness, AMS, New onset seizure, Tremor • GI: – N/V/D x “a few hours” • PSYCH: – (-) Stressors
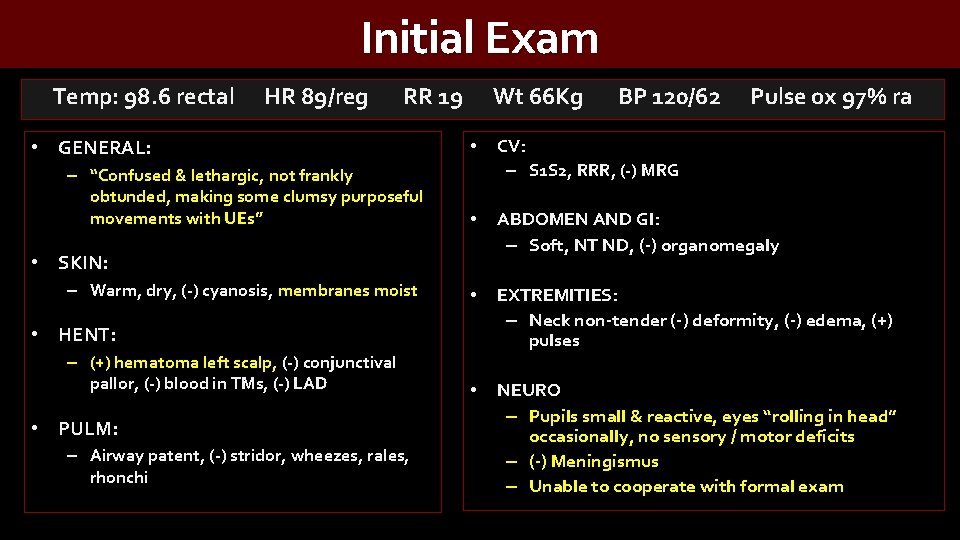
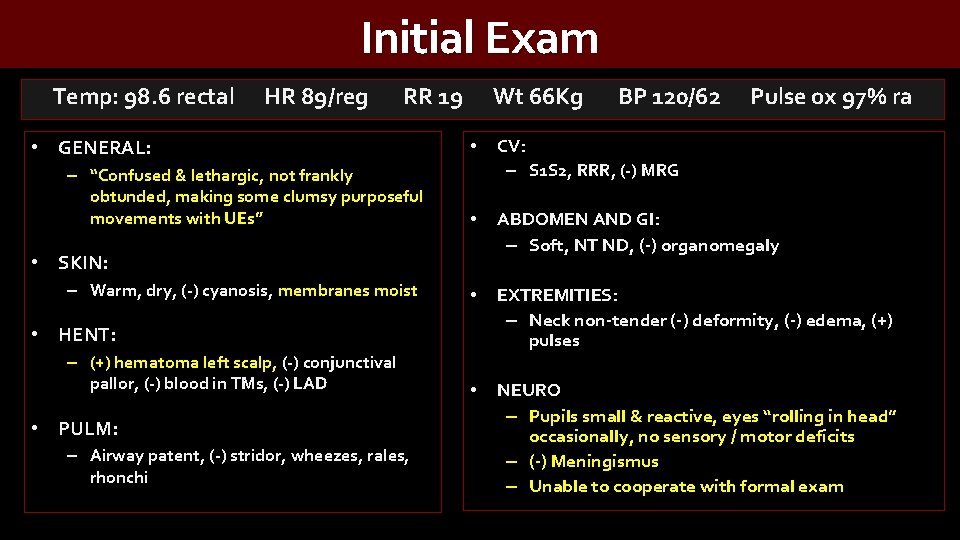
Initial Exam Temp: 98. 6 rectal HR 89/reg RR 19 Wt 66 Kg BP 120/62 Pulse ox 97% ra • GENERAL: – “Confused & lethargic, not frankly obtunded, making some clumsy purposeful movements with UEs” • CV: – S 1 S 2, RRR, (-) MRG • ABDOMEN AND GI: – Soft, NT ND, (-) organomegaly • EXTREMITIES: – Neck non-tender (-) deformity, (-) edema, (+) pulses • NEURO – Pupils small & reactive, eyes “rolling in head” occasionally, no sensory / motor deficits – (-) Meningismus – Unable to cooperate with formal exam • SKIN: – Warm, dry, (-) cyanosis, membranes moist • HENT: – (+) hematoma left scalp, (-) conjunctival pallor, (-) blood in TMs, (-) LAD • PULM: – Airway patent, (-) stridor, wheezes, rales, rhonchi
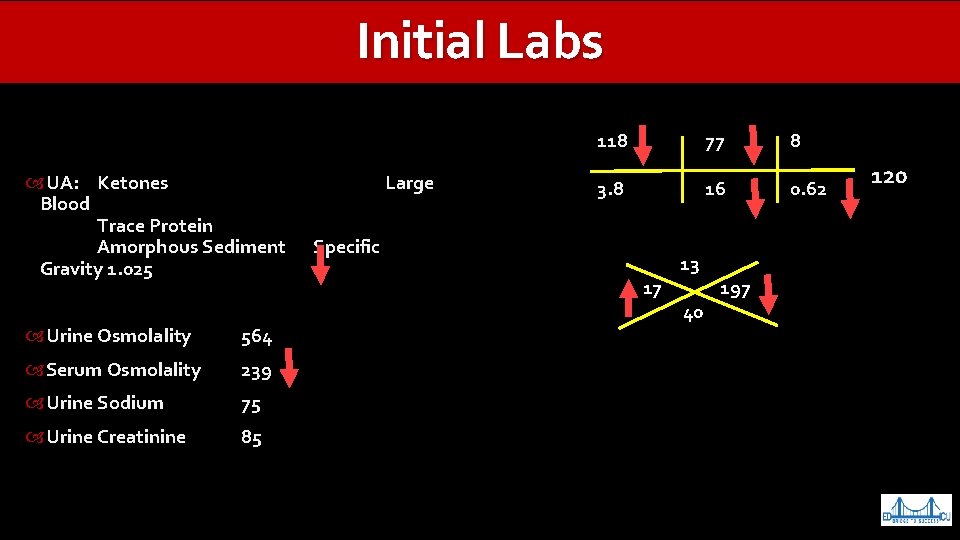
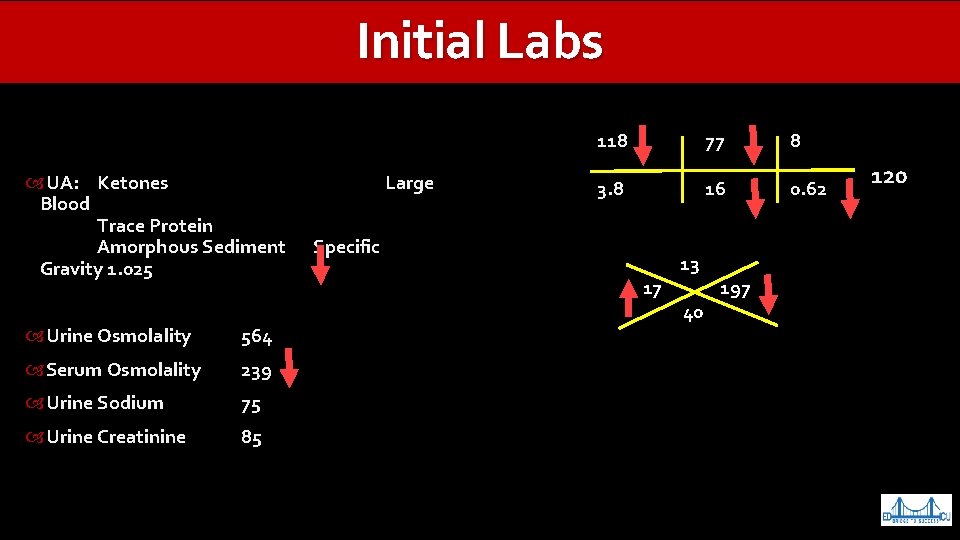
Initial Labs CK 630 Index 1. 4 UA: Troponin Ketones <0. 01 Large Blood Trace Protein Amorphous Sediment AST/ALT 69 / 34 Specific Gravity 1. 025 Albumin 4. 3 Urine Osmolality Calcium 8. 1 564 Serum Osmolality Alk Phos 40 239 Urine Sodium Anion Gap 25 75 Urine Creatinine 85 AG = Na - (Cl + HCO 3) AG = 118 – (77 + 16) = 25 118 77 8 3. 8 16 0. 62 13 17 197 40 120
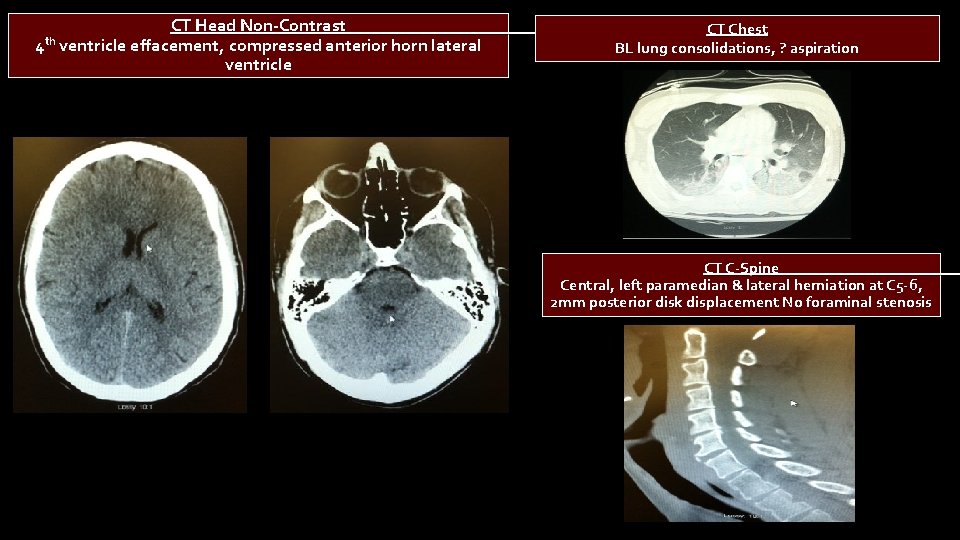
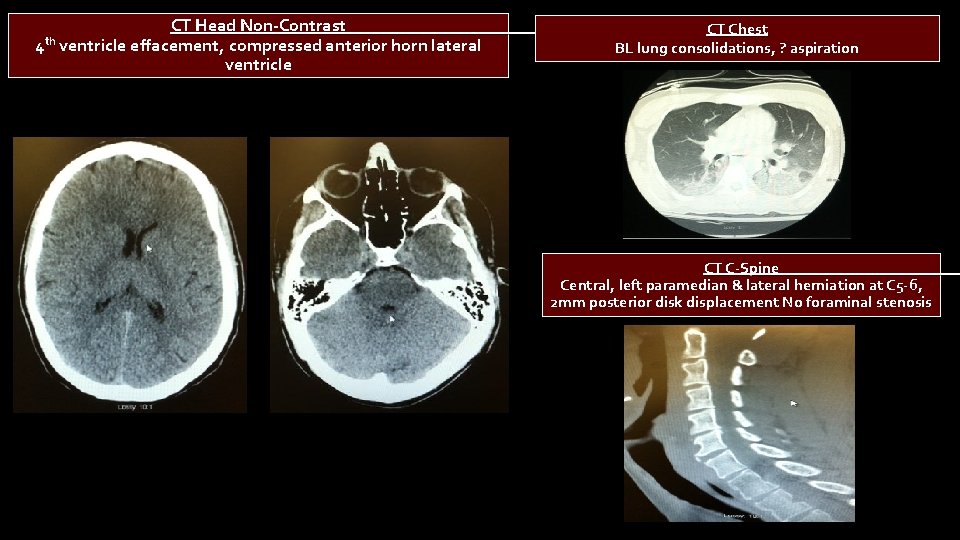
CT Head Non-Contrast CT Chest th 4 ventricle effacement, compressed anterior horn lateral BL lung consolidations, ? aspiration ventricle CT C-Spine Central, left paramedian & lateral herniation at C 5 -6, 2 mm posterior disk displacement No foraminal stenosis
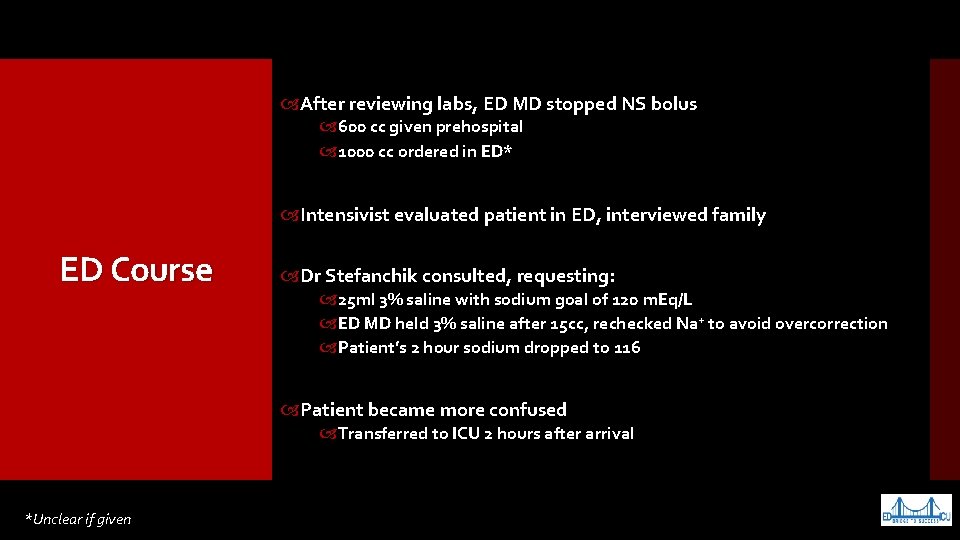
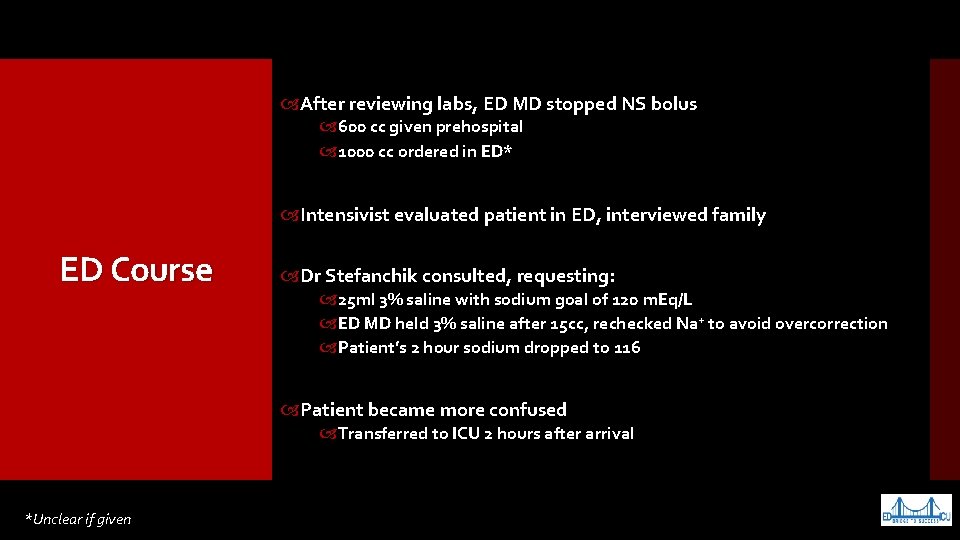
After reviewing labs, ED MD stopped NS bolus 600 cc given prehospital 1000 cc ordered in ED* Intensivist evaluated patient in ED, interviewed family ED Course Dr Stefanchik consulted, requesting: 25 ml 3% saline with sodium goal of 120 m. Eq/L ED MD held 3% saline after 15 cc, rechecked Na+ to avoid overcorrection Patient’s 2 hour sodium dropped to 116 Patient became more confused Transferred to ICU 2 hours after arrival *Unclear if given
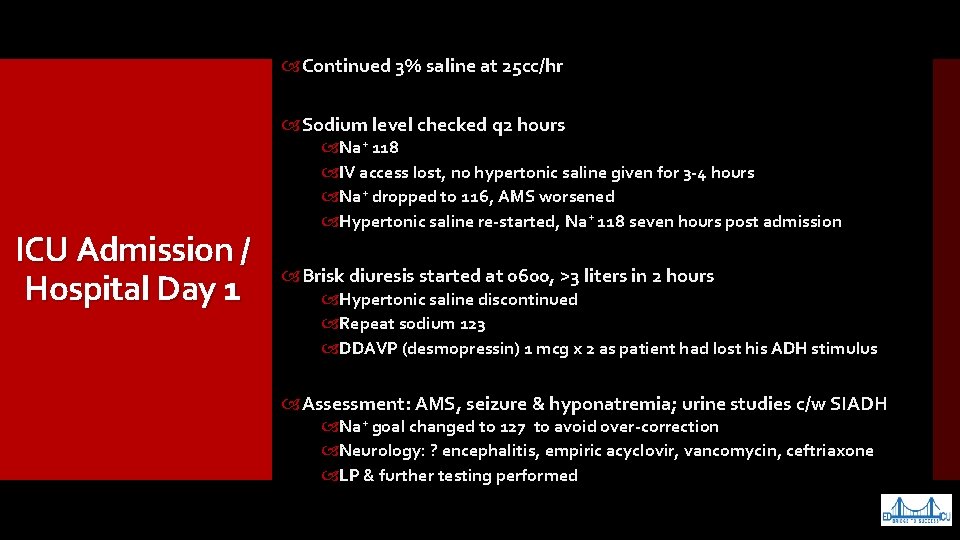
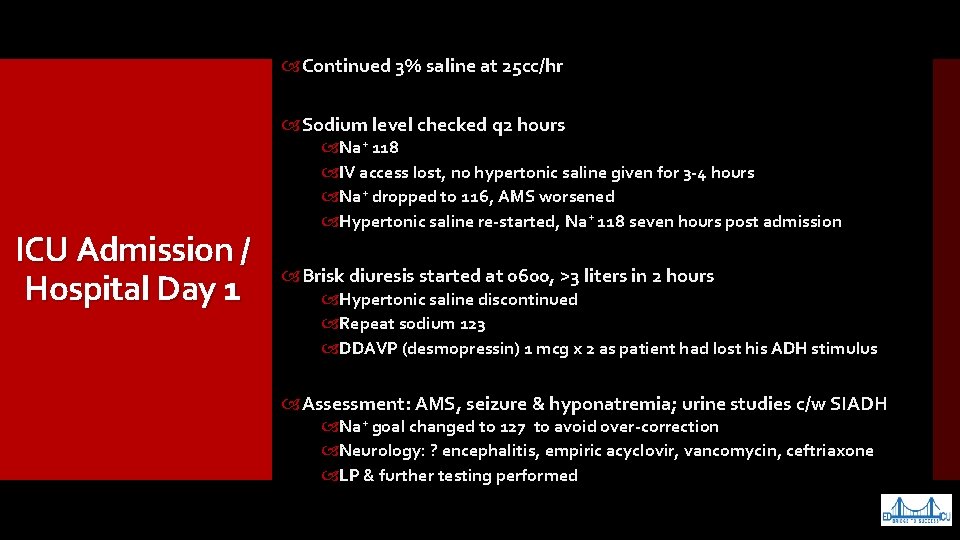
Continued 3% saline at 25 cc/hr Sodium level checked q 2 hours ICU Admission / Hospital Day 1 Na+ 118 IV access lost, no hypertonic saline given for 3 -4 hours Na+ dropped to 116, AMS worsened Hypertonic saline re-started, Na+ 118 seven hours post admission Brisk diuresis started at 0600, >3 liters in 2 hours Hypertonic saline discontinued Repeat sodium 123 DDAVP (desmopressin) 1 mcg x 2 as patient had lost his ADH stimulus Assessment: AMS, seizure & hyponatremia; urine studies c/w SIADH Na+ goal changed to 127 to avoid over-correction Neurology: ? encephalitis, empiric acyclovir, vancomycin, ceftriaxone LP & further testing performed
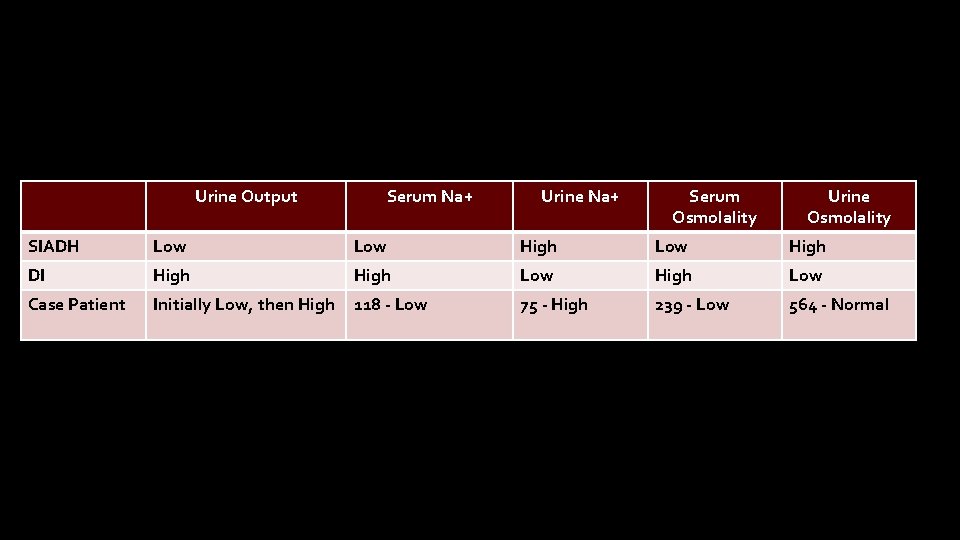
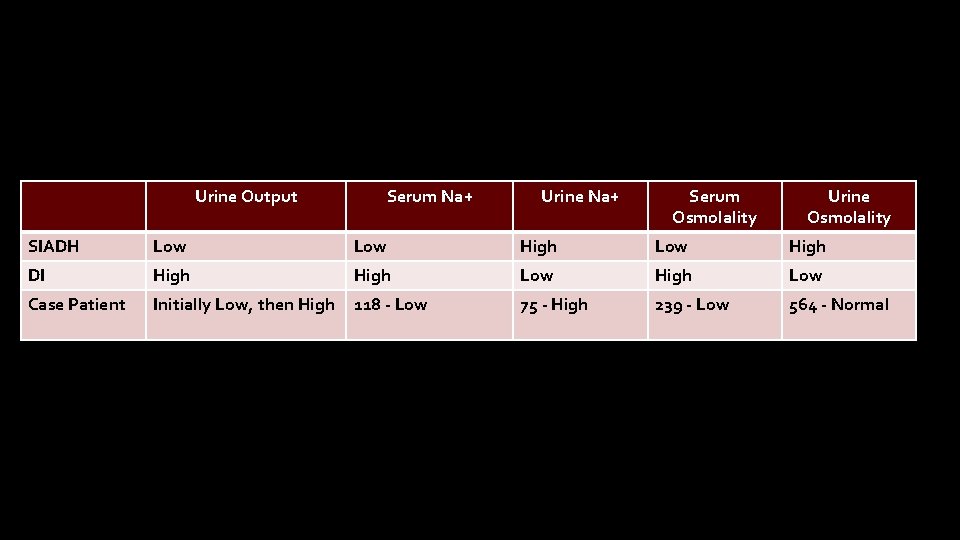
Worsening AMS, rhabdomyolysis, & transaminitis CPK 17, 837 m. L/min AST 424 / ALT 342 US: Cardiac: normal LVEDV Urine Output Serum Na+ Urine Na+ Orbital: Optic nerve sheath 0. 6 mm SIADH Low ICU Days 2 DI High EEG: High No seizure activity -3 Initially Low, then High Case Patient 118 - Low Serum Osmolality Urine Osmolality High Low High Low 75 - High 239 - Low 564 - Normal MRI: Patient combative, requiring sedation Likely diuresis secondary to resolving SIADH vs DI Sodium (134) & anion gap (13) normalizing
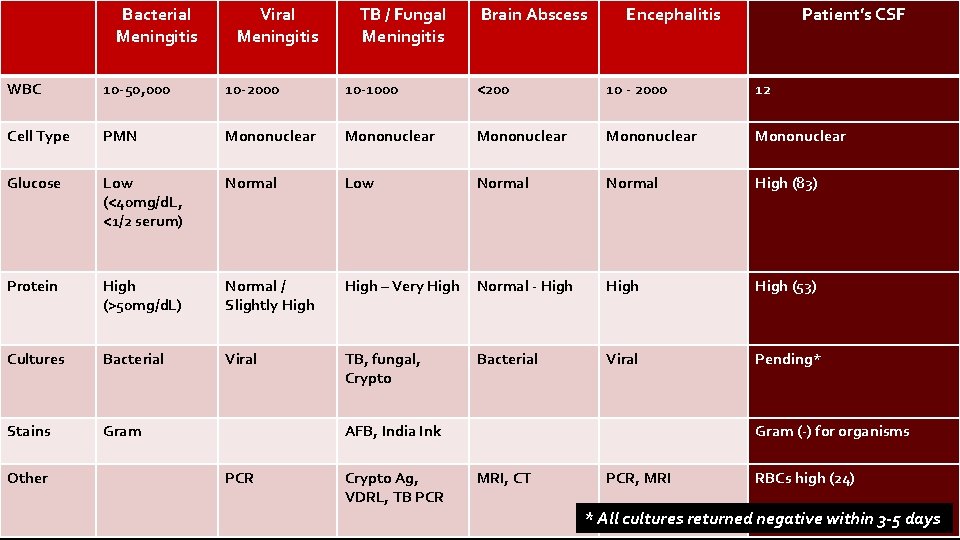
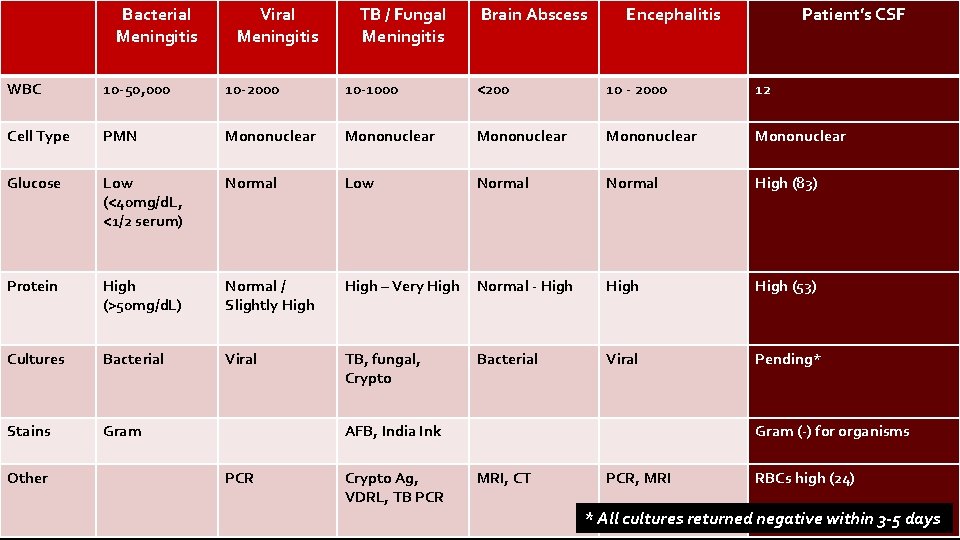
Bacterial Meningitis Viral Meningitis TB / Fungal Meningitis Brain Abscess MRI Brain Encephalitis Patient’s CSF WBC 10 -50, 000 10 -2000 10 -1000 <200 10 - 2000 12 Cell Type PMN Mononuclear Mononuclear Glucose Low (<40 mg/d. L, <1/2 serum) Normal Low Normal High (83) Protein High (>50 mg/d. L) Normal / Slightly High – Very High Normal - High (53) Cultures Bacterial Viral TB, fungal, Crypto Bacterial Viral Pending* Stains Gram Other AFB, India Ink PCR Crypto Ag, VDRL, TB PCR Gram (-) for organisms MRI, CT PCR, MRI RBCs high (24) * All cultures returned negative within 3 -5 days
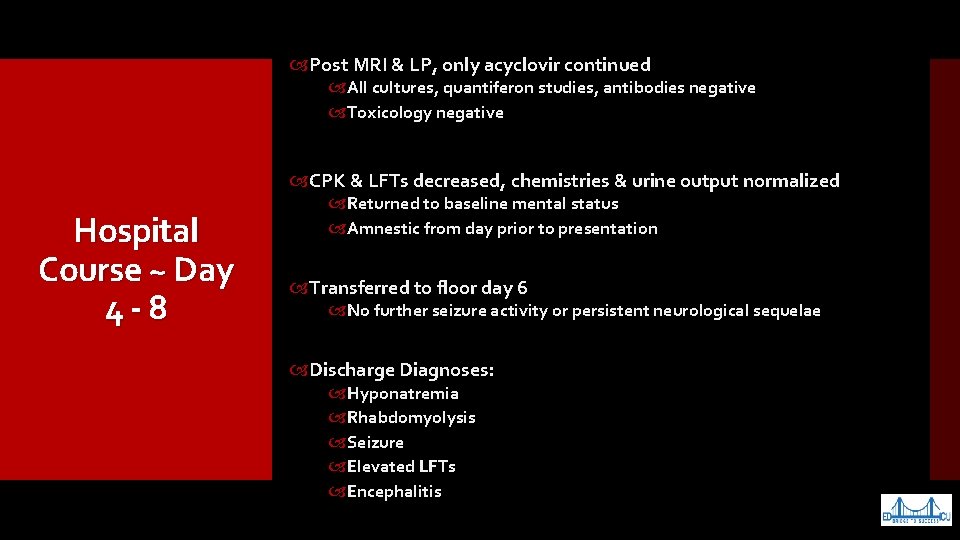
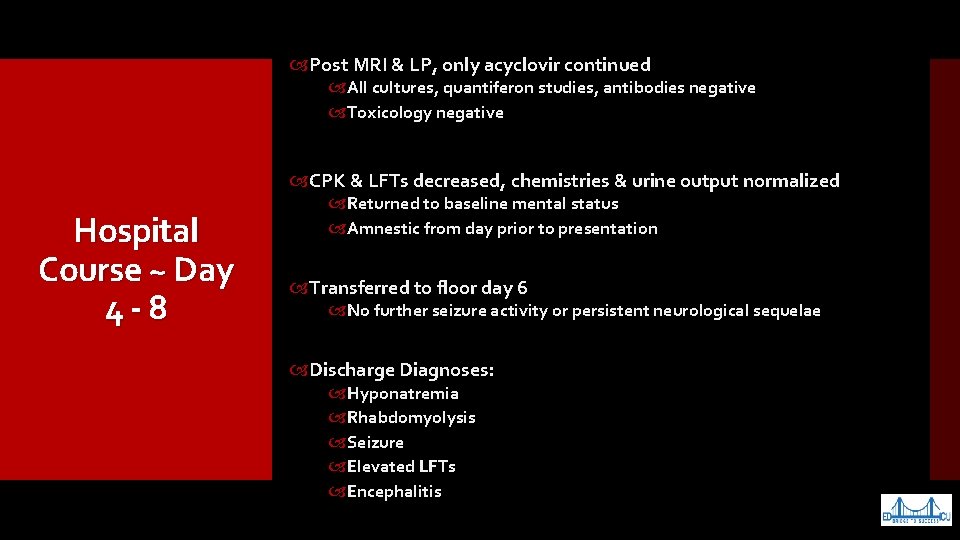
Post MRI & LP, only acyclovir continued All cultures, quantiferon studies, antibodies negative Toxicology negative CPK & LFTs decreased, chemistries & urine output normalized Hospital Course ~ Day 4 - 8 Returned to baseline mental status Amnestic from day prior to presentation Transferred to floor day 6 No further seizure activity or persistent neurological sequelae Discharge Diagnoses: Hyponatremia Rhabdomyolysis Seizure Elevated LFTs Encephalitis

Perfect Storm for SIADH Cerebral Infection / Inflammation Significant Exertion in Heat Rhabdomyolysis Traumatic Brain Injury Nicotine & Alcohol Usage Anticholinergic Medication
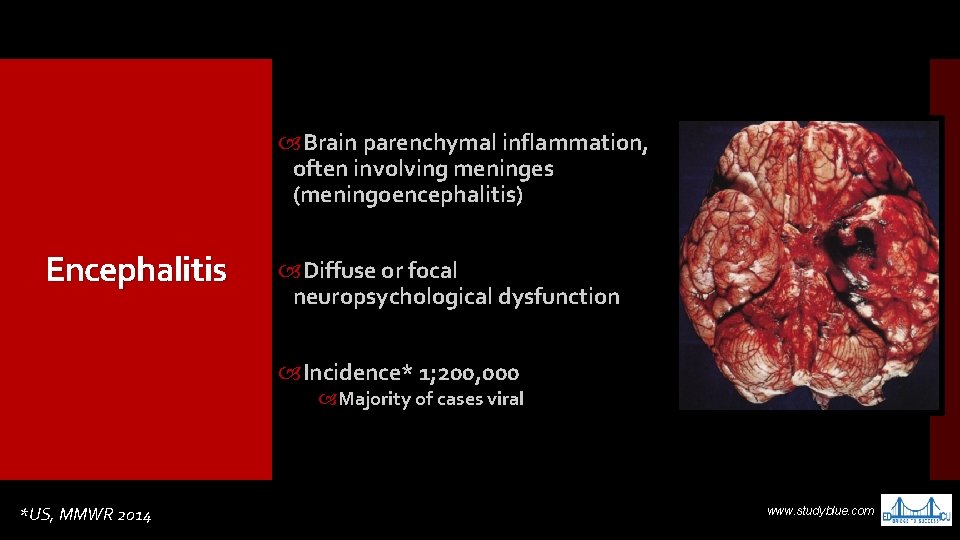
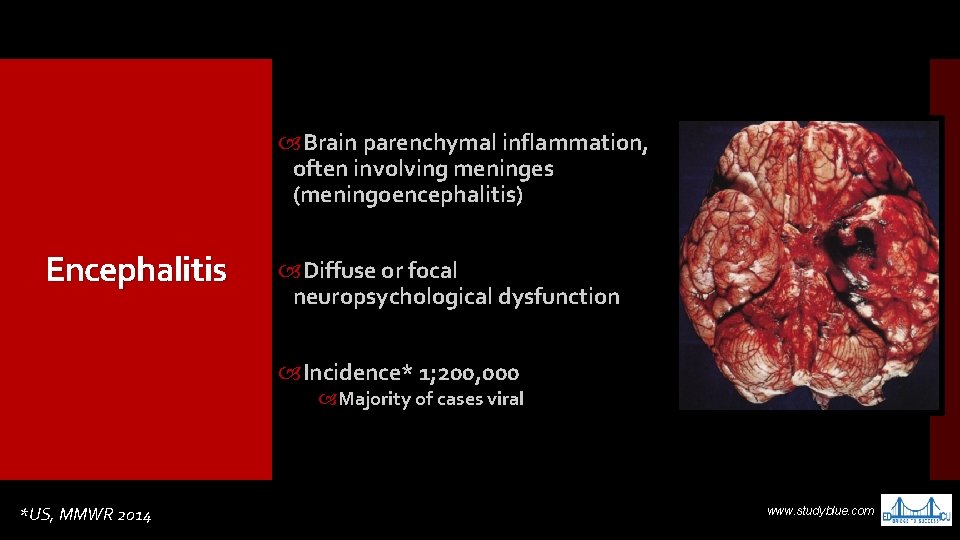
Brain parenchymal inflammation, often involving meninges (meningoencephalitis) Encephalitis Diffuse or focal neuropsychological dysfunction Incidence* 1; 200, 000 Majority of cases viral *US, MMWR 2014 www. studyblue. com
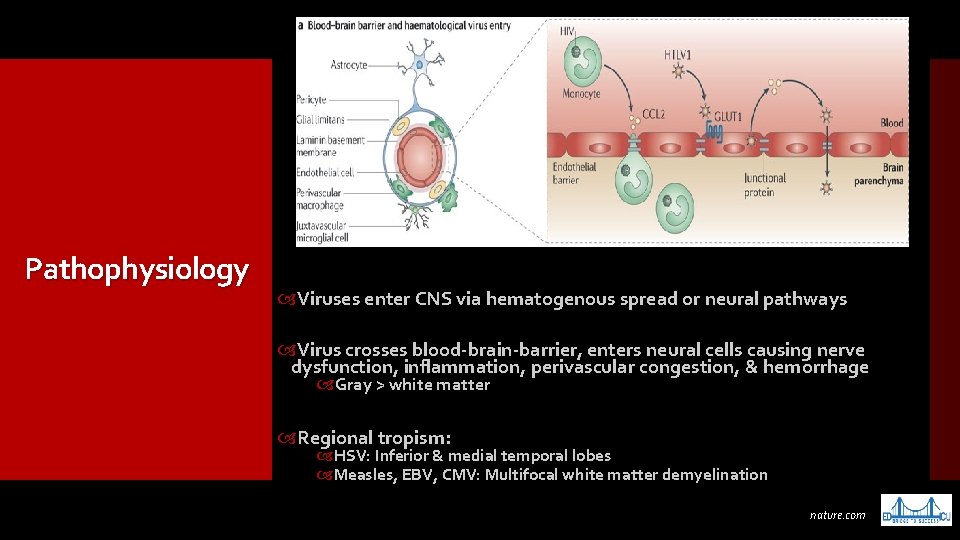
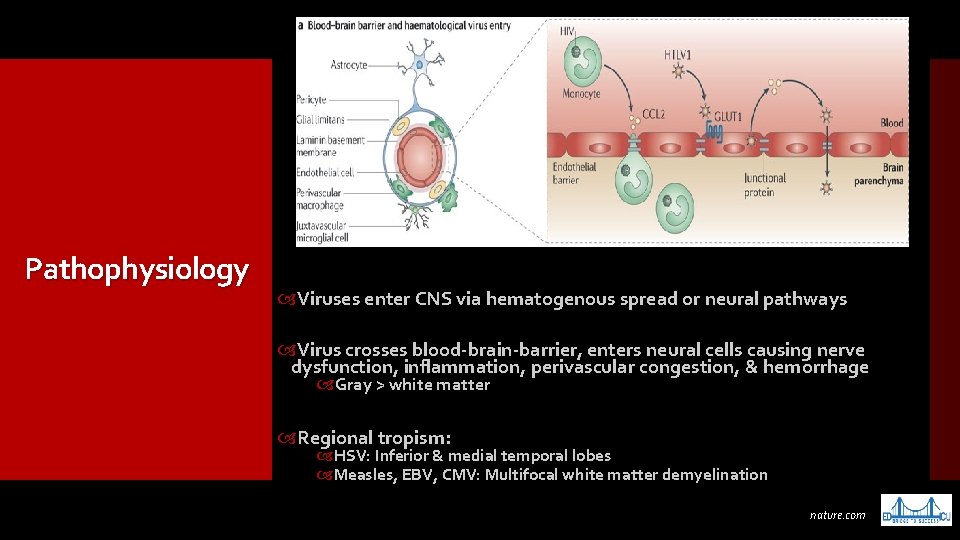
Pathophysiology Viruses enter CNS via hematogenous spread or neural pathways Virus crosses blood-brain-barrier, enters neural cells causing nerve dysfunction, inflammation, perivascular congestion, & hemorrhage Gray > white matter Regional tropism: HSV: Inferior & medial temporal lobes Measles, EBV, CMV: Multifocal white matter demyelination nature. com
Prognosis depends on viral virulence & patient’s health status US Incidence & Prognosis Poor outcomes: Age extremes, pre-existing neurologic condition, immunocompromised ~2, 000 viral encephalitis cases / yr HSV mortality 20 -75% 40 -95% with long-term disabilities cueflash. com
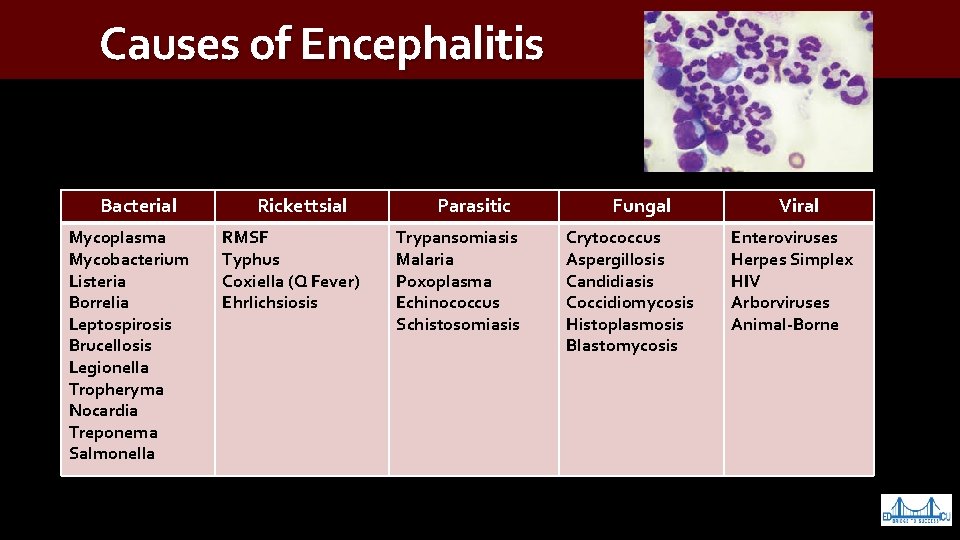
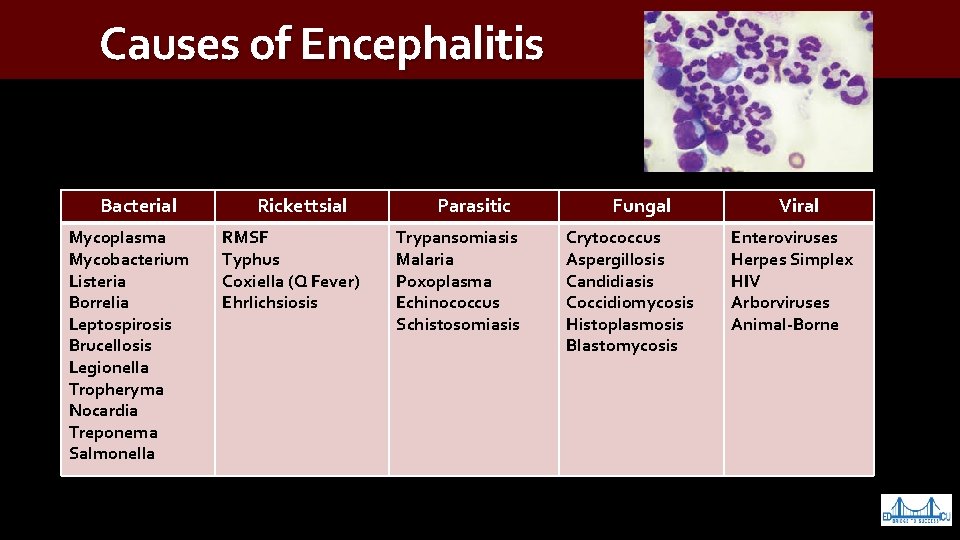
Causes of Encephalitis Bacterial Mycoplasma Mycobacterium Listeria Borrelia Leptospirosis Brucellosis Legionella Tropheryma Nocardia Treponema Salmonella Rickettsial RMSF Typhus Coxiella (Q Fever) Ehrlichsiosis Parasitic Trypansomiasis Malaria Poxoplasma Echinococcus Schistosomiasis Fungal Crytococcus Aspergillosis Candidiasis Coccidiomycosis Histoplasmosis Blastomycosis Viral Enteroviruses Herpes Simplex HIV Arborviruses Animal-Borne
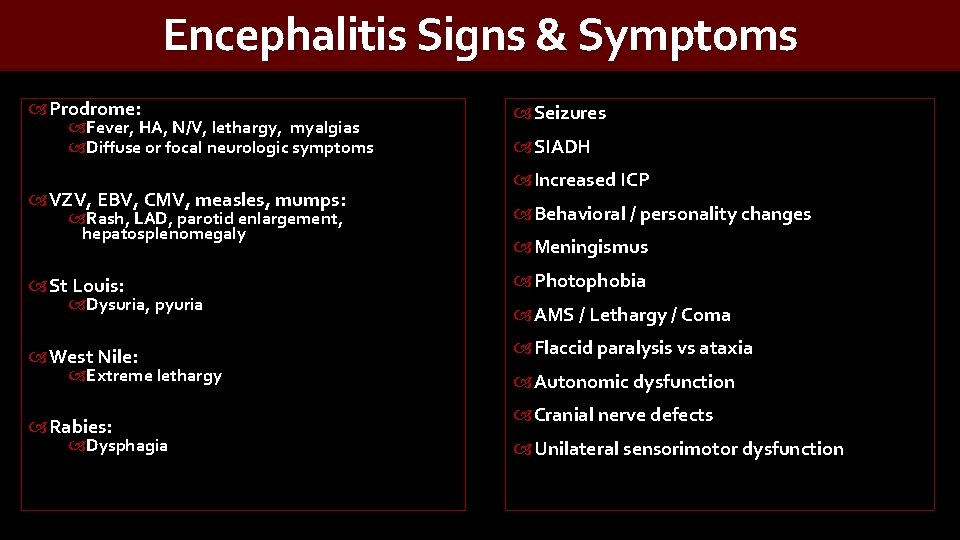
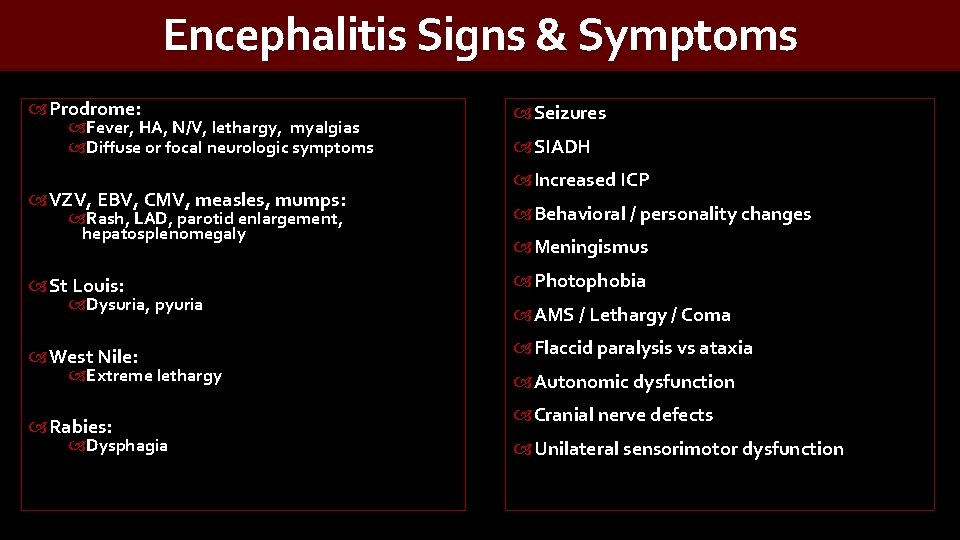
Encephalitis Signs & Symptoms Prodrome: Fever, HA, N/V, lethargy, myalgias Diffuse or focal neurologic symptoms VZV, EBV, CMV, measles, mumps: Rash, LAD, parotid enlargement, hepatosplenomegaly St Louis: Dysuria, pyuria West Nile: Extreme lethargy Rabies: Dysphagia Seizures SIADH Increased ICP Behavioral / personality changes Meningismus Photophobia AMS / Lethargy / Coma Flaccid paralysis vs ataxia Autonomic dysfunction Cranial nerve defects Unilateral sensorimotor dysfunction
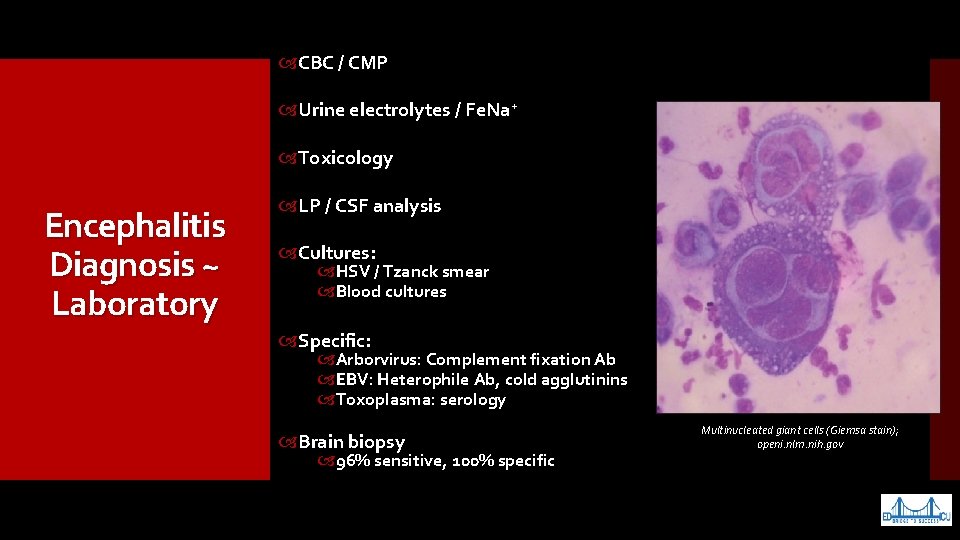
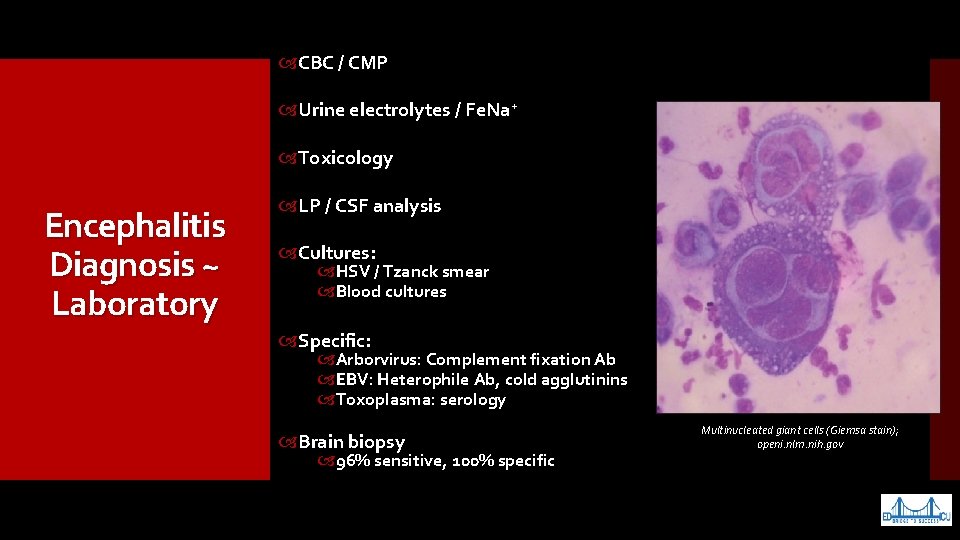
CBC / CMP Urine electrolytes / Fe. Na+ Toxicology Encephalitis Diagnosis ~ Laboratory LP / CSF analysis Cultures: HSV / Tzanck smear Blood cultures Specific: Arborvirus: Complement fixation Ab EBV: Heterophile Ab, cold agglutinins Toxoplasma: serology Brain biopsy 96% sensitive, 100% specific Multinucleated giant cells (Giemsa stain); openi. nlm. nih. gov
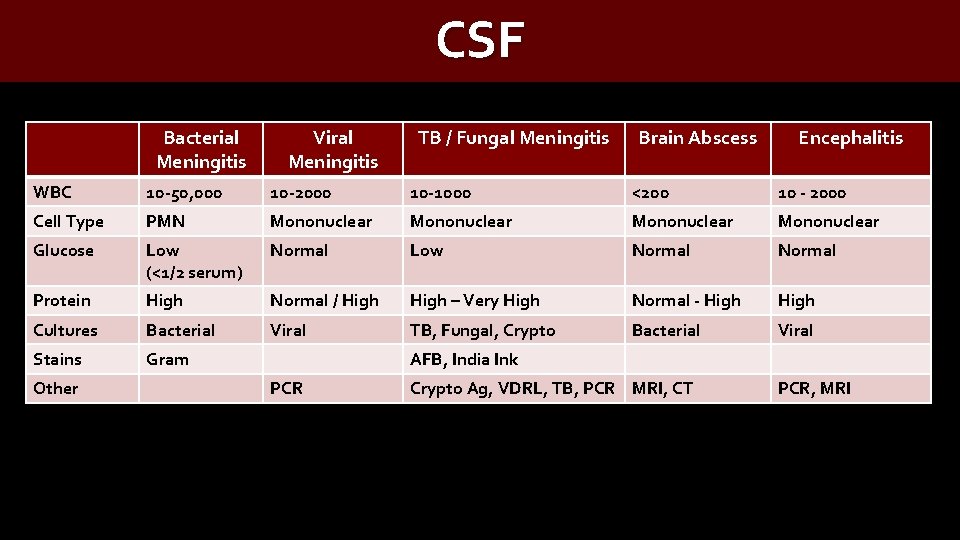
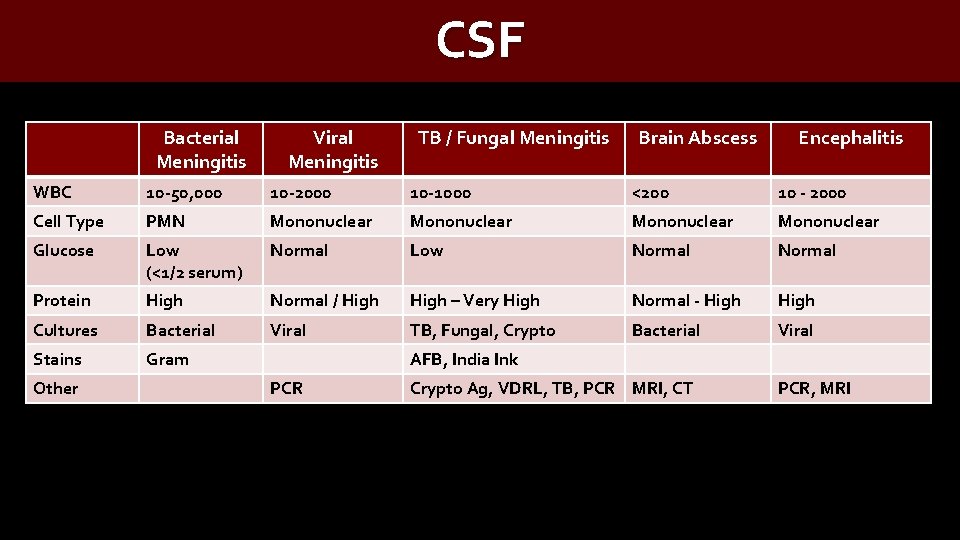
CSF Bacterial Meningitis Viral Meningitis TB / Fungal Meningitis Brain Abscess Encephalitis WBC 10 -50, 000 10 -2000 10 -1000 <200 10 - 2000 Cell Type PMN Mononuclear Glucose Low Normal (<1/2 serum) Low Normal Protein High Normal / High – Very High Normal - High Cultures Bacterial Viral TB, Fungal, Crypto Bacterial Viral Stains Gram Other AFB, India Ink PCR Crypto Ag, VDRL, TB, PCR MRI, CT PCR, MRI
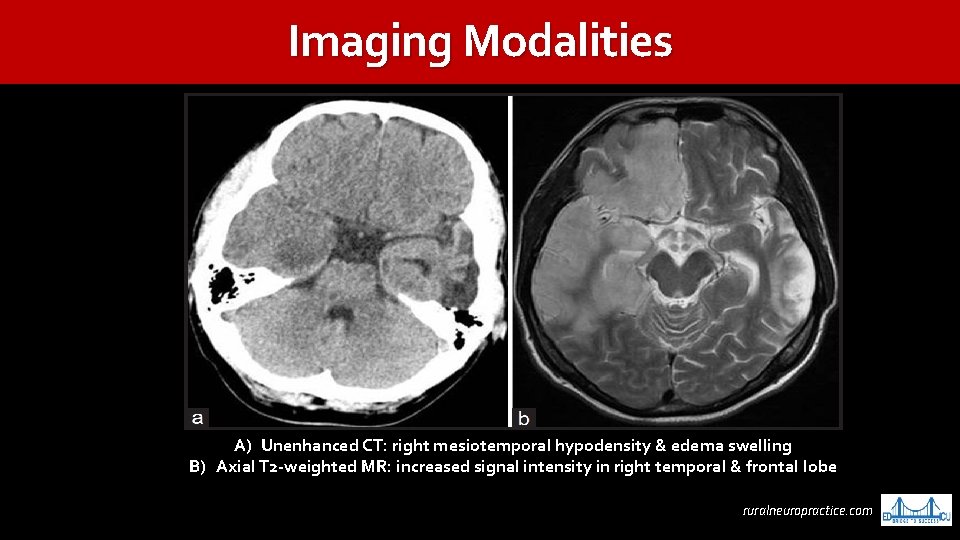
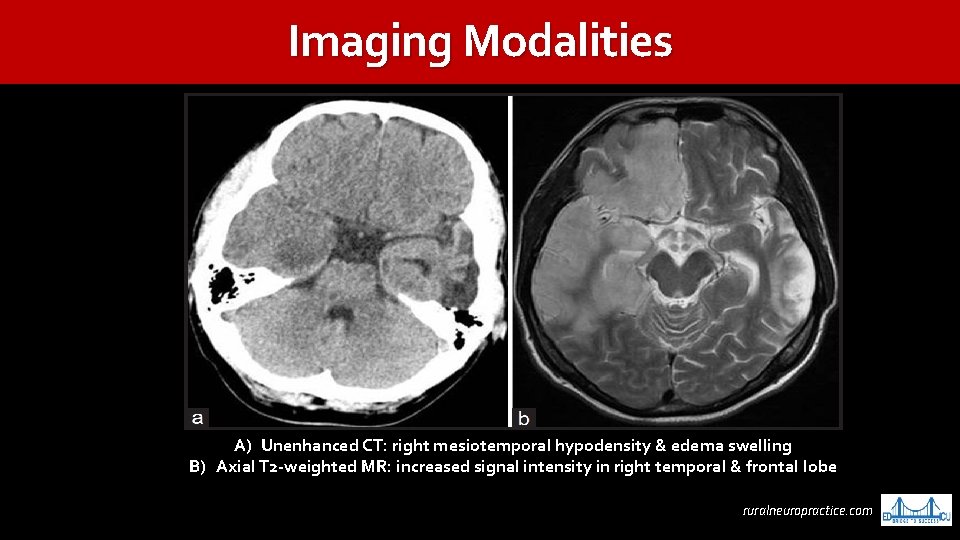
Imaging Modalities A) Unenhanced CT: right mesiotemporal hypodensity & edema swelling B) Axial T 2 -weighted MR: increased signal intensity in right temporal & frontal lobe ruralneuropractice. com
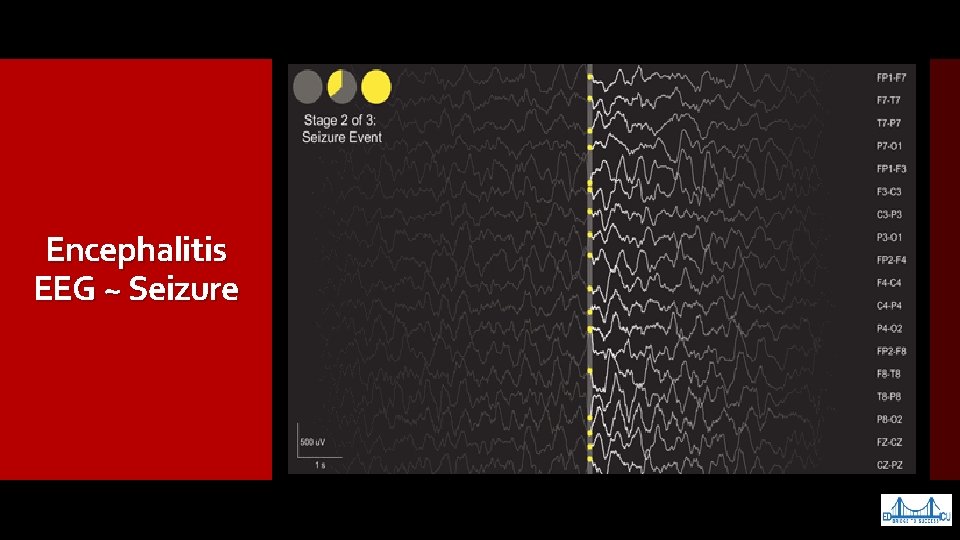
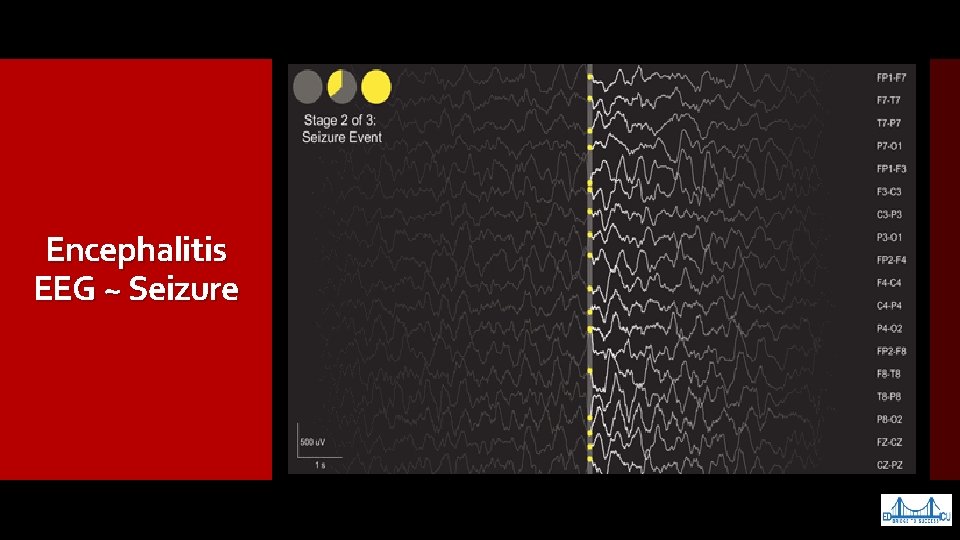
Encephalitis EEG ~ Seizure
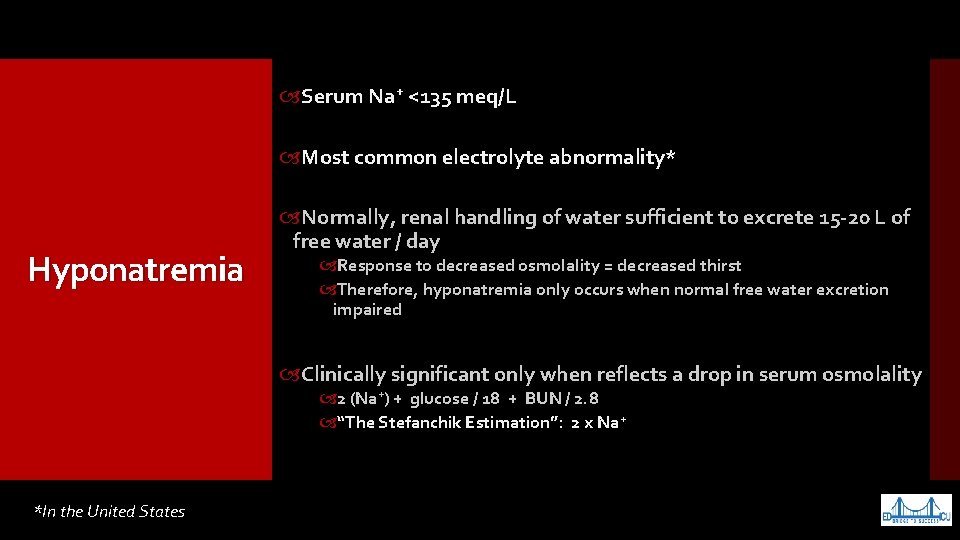
Serum Na+ <135 meq/L Most common electrolyte abnormality* Hyponatremia Normally, renal handling of water sufficient to excrete 15 -20 L of free water / day Response to decreased osmolality = decreased thirst Therefore, hyponatremia only occurs when normal free water excretion impaired Clinically significant only when reflects a drop in serum osmolality 2 (Na+) + glucose / 18 + BUN / 2. 8 “The Stefanchik Estimation”: 2 x Na+ *In the United States
Prevalence in hospitalized patients 2. 5 - 30% Usually hospital acquired / secondary to hypotonic IVF Other: postoperatively, stress, pain, & medications Hyponatremia Epidemiology (US) 20 -40% hospital-acquired hyponatremia is SIADH Must differentiate from hyponatremia in patients with limited capacity to excrete free water Hyponatremia Risk Factors: Age >30 yr Low body weight Males likely to develop mild-moderate, but not severe hyponatremia Females prone to drug-induced & exercise-induced hyponatremia
Profound when decrease in sodium very large or very rapid Hyponatremia Symptoms do not always correlate with severity or acuity Often asymptomatic if Na+ >125 or chronic emaze. com
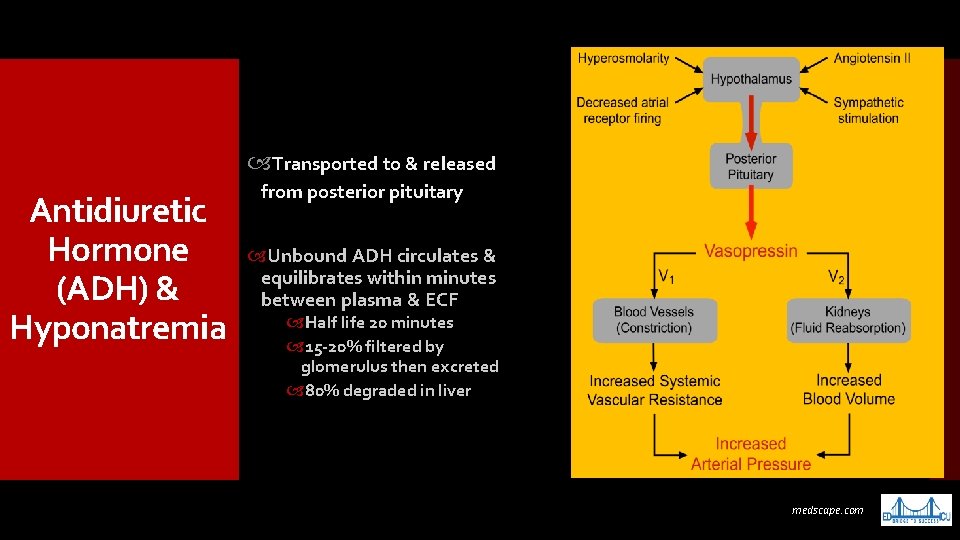
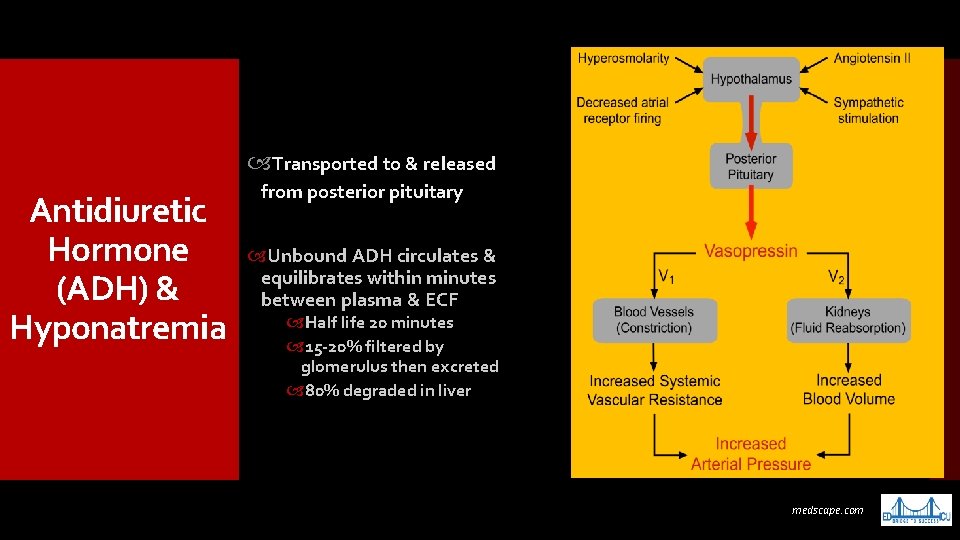
Transported to & released Antidiuretic Hormone (ADH) & Hyponatremia from posterior pituitary Unbound ADH circulates & equilibrates within minutes between plasma & ECF Half life 20 minutes 15 -20% filtered by glomerulus then excreted 80% degraded in liver medscape. com
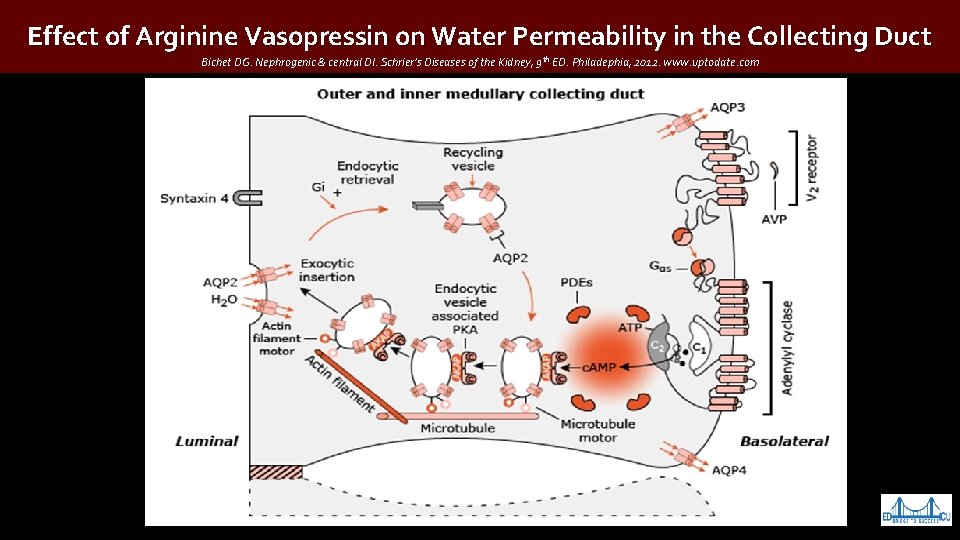
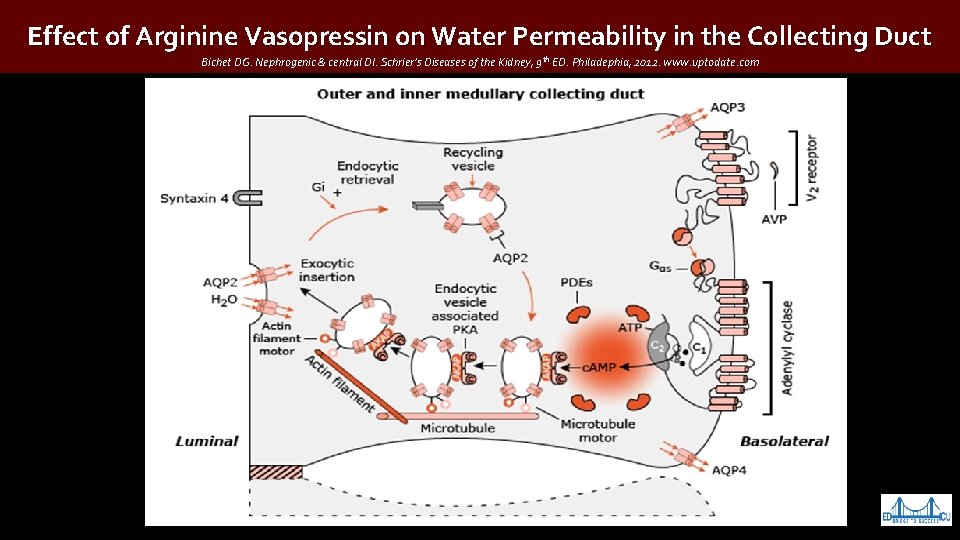
Effect of Arginine Vasopressin on Water Permeability in the Collecting Duct Bichet DG. Nephrogenic & central DI. Schrier’s Diseases of the Kidney, 9 th ED. Philadephia, 2012. www. uptodate. com
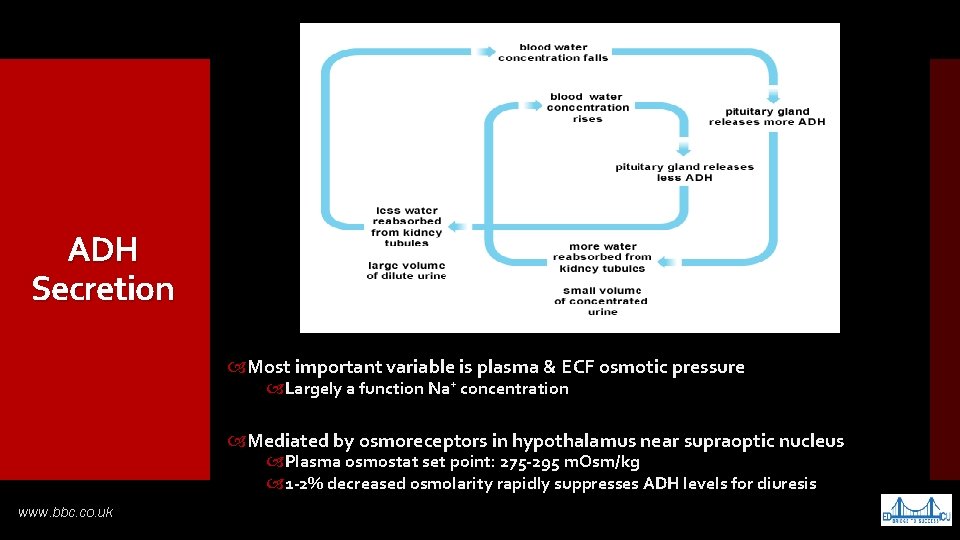
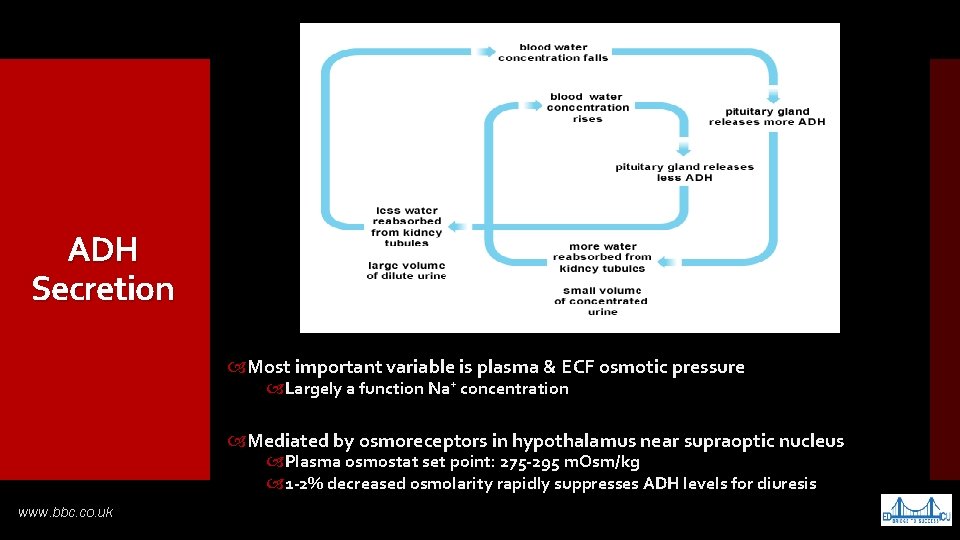
ADH Secretion Most important variable is plasma & ECF osmotic pressure Largely a function Na+ concentration Mediated by osmoreceptors in hypothalamus near supraoptic nucleus Plasma osmostat set point: 275 -295 m. Osm/kg 1 -2% decreased osmolarity rapidly suppresses ADH levels for diuresis www. bbc. co. uk
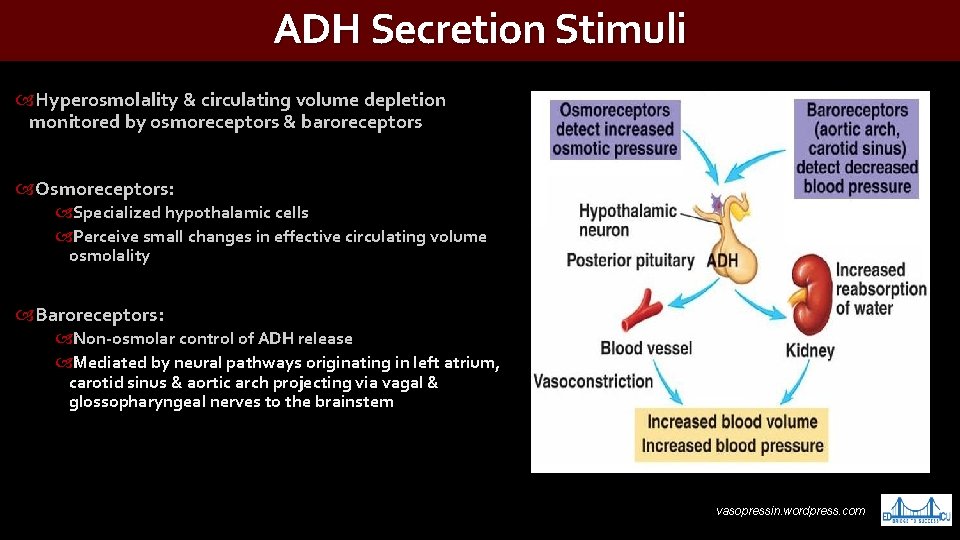
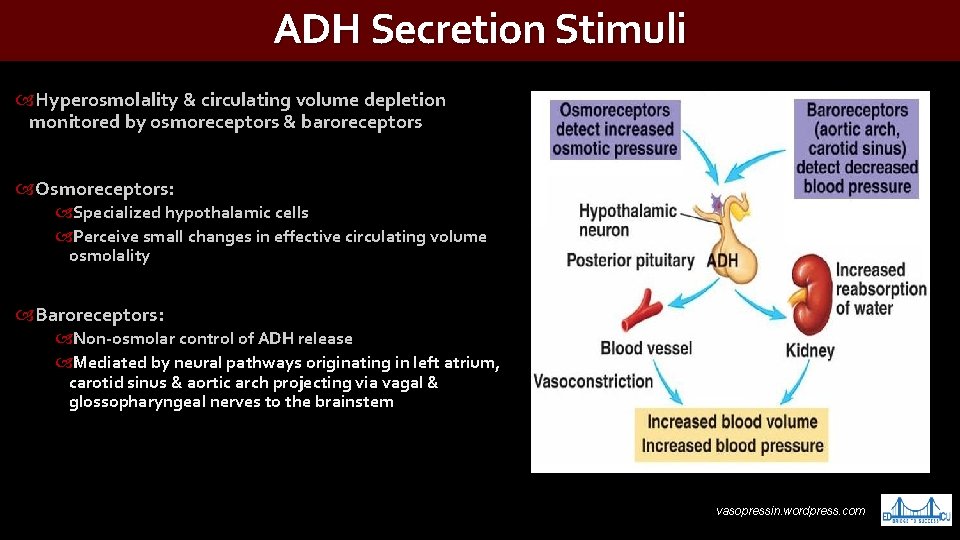
ADH Secretion Stimuli Hyperosmolality & circulating volume depletion monitored by osmoreceptors & baroreceptors Osmoreceptors: Specialized hypothalamic cells Perceive small changes in effective circulating volume osmolality Baroreceptors: Non-osmolar control of ADH release Mediated by neural pathways originating in left atrium, carotid sinus & aortic arch projecting via vagal & glossopharyngeal nerves to the brainstem vasopressin. wordpress. com
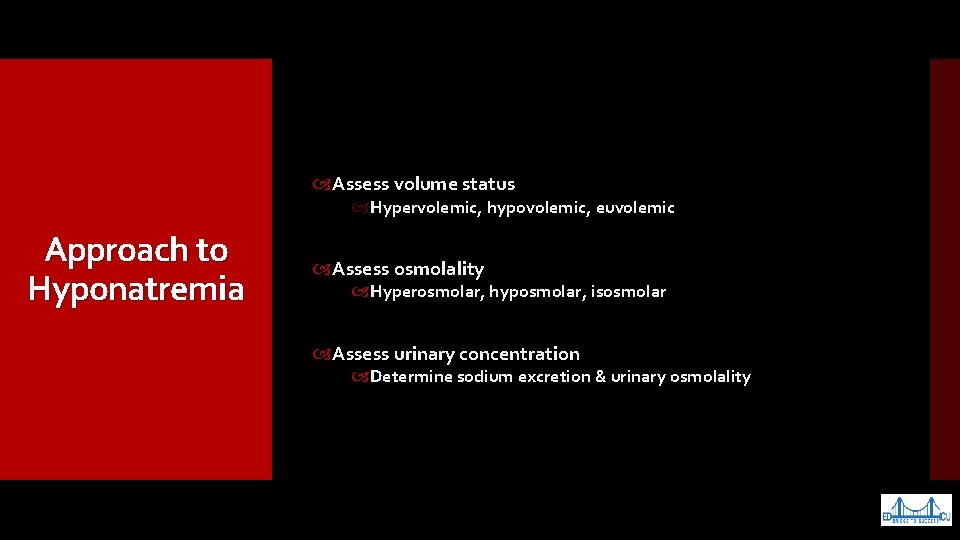
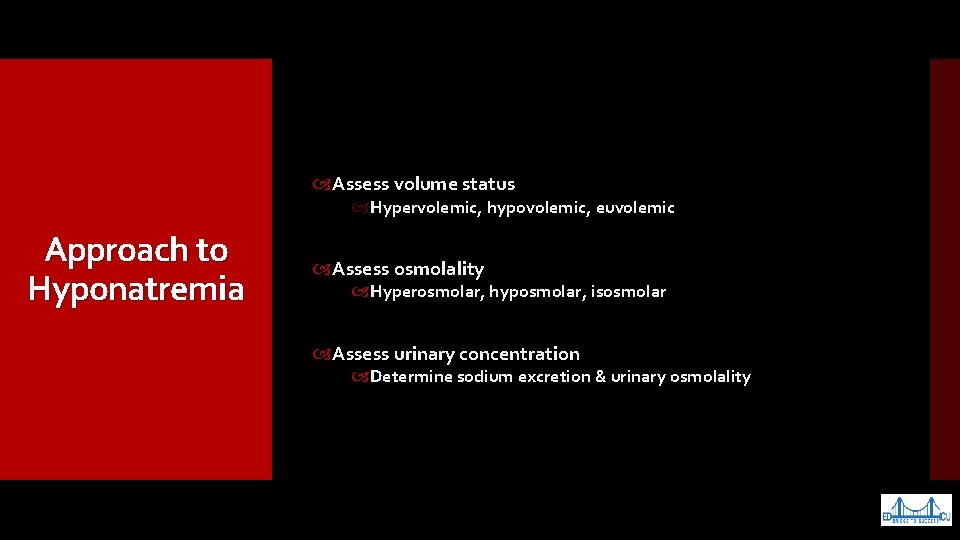
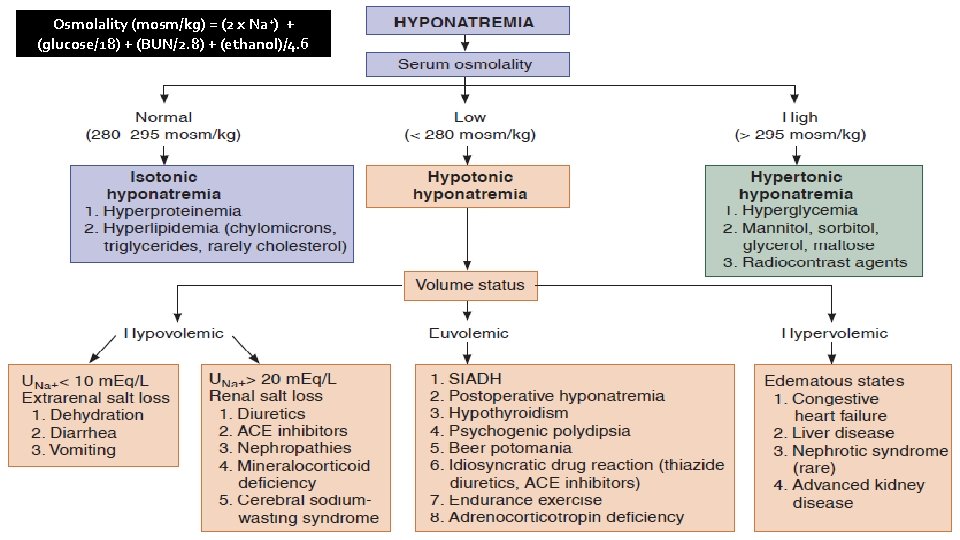
Assess volume status Hypervolemic, hypovolemic, euvolemic Approach to Hyponatremia Assess osmolality Hyperosmolar, hyposmolar, isosmolar Assess urinary concentration Determine sodium excretion & urinary osmolality
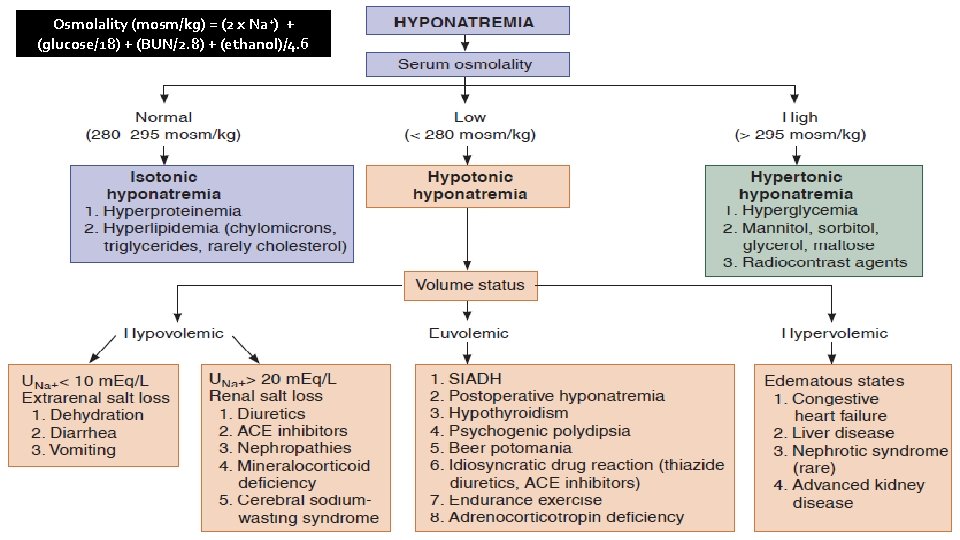
Osmolality (mosm/kg) = (2 x Na+) + (glucose/18) + (BUN/2. 8) + (ethanol)/4. 6 fff
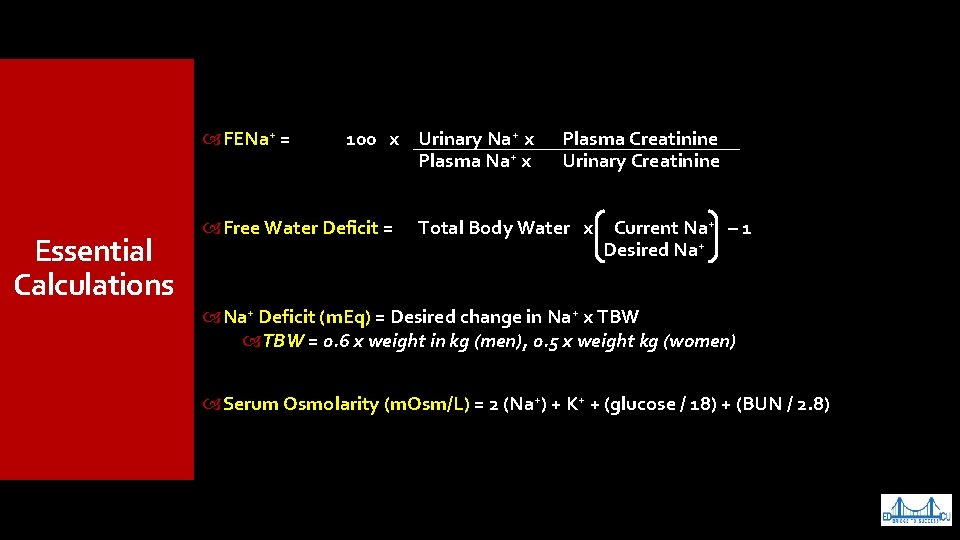
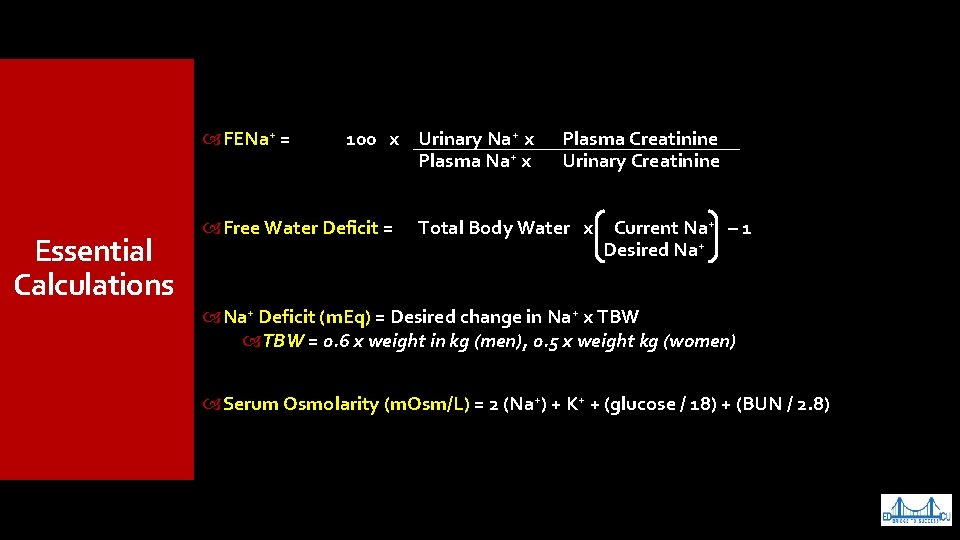
FENa+ = Essential Calculations 100 x Urinary Na+ x Plasma Na+ x Plasma Creatinine Urinary Creatinine Free Water Deficit = Total Body Water x Current Na+ – 1 Desired Na+ Deficit (m. Eq) = Desired change in Na+ x TBW = 0. 6 x weight in kg (men), 0. 5 x weight kg (women) Serum Osmolarity (m. Osm/L) = 2 (Na+) + K+ + (glucose / 18) + (BUN / 2. 8)
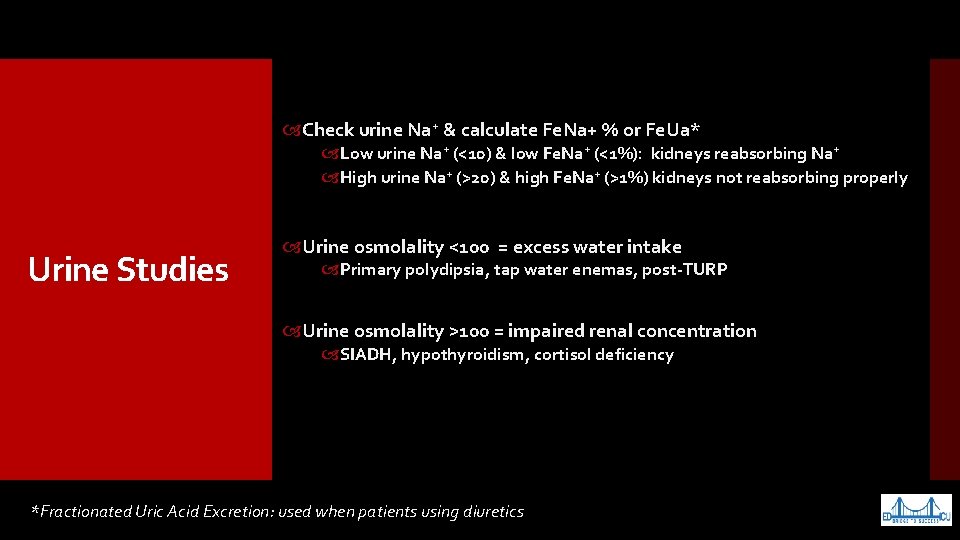
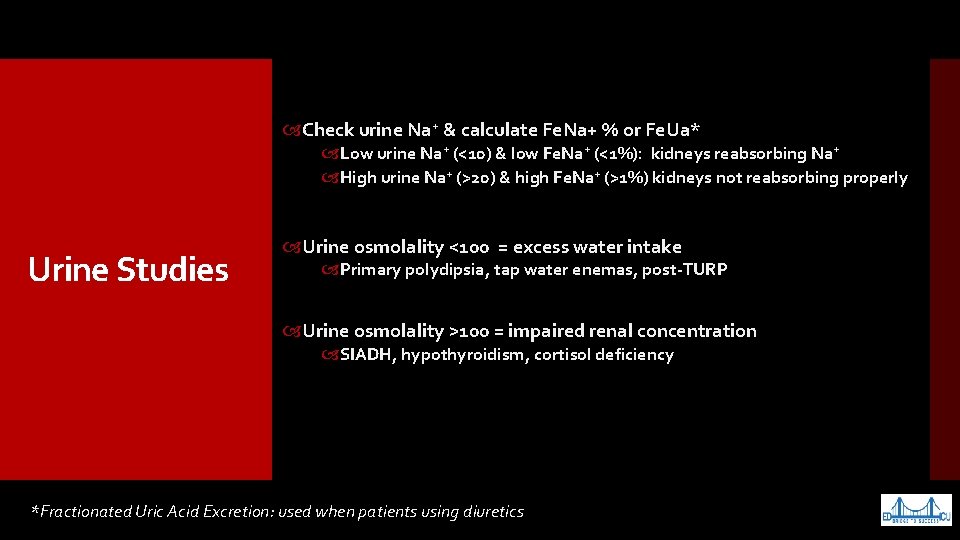
Check urine Na+ & calculate Fe. Na+ % or Fe. Ua* Low urine Na+ (<10) & low Fe. Na+ (<1%): kidneys reabsorbing Na+ High urine Na+ (>20) & high Fe. Na+ (>1%) kidneys not reabsorbing properly Urine Studies Urine osmolality <100 = excess water intake Primary polydipsia, tap water enemas, post-TURP Urine osmolality >100 = impaired renal concentration SIADH, hypothyroidism, cortisol deficiency *Fractionated Uric Acid Excretion: used when patients using diuretics
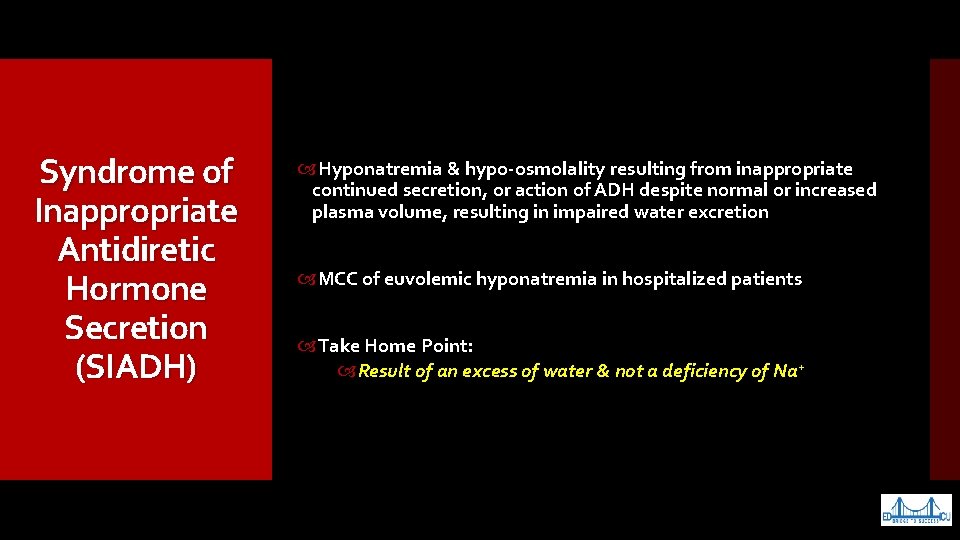
Syndrome of Inappropriate Antidiretic Hormone Secretion (SIADH) Hyponatremia & hypo-osmolality resulting from inappropriate continued secretion, or action of ADH despite normal or increased plasma volume, resulting in impaired water excretion MCC of euvolemic hyponatremia in hospitalized patients Take Home Point: Result of an excess of water & not a deficiency of Na+
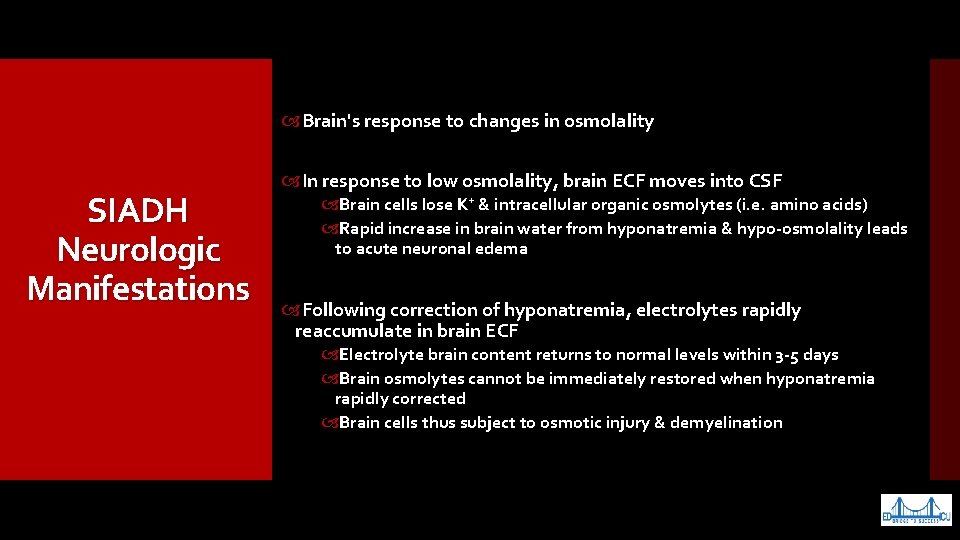
Brain's response to changes in osmolality SIADH Neurologic Manifestations In response to low osmolality, brain ECF moves into CSF Brain cells lose K+ & intracellular organic osmolytes (i. e. amino acids) Rapid increase in brain water from hyponatremia & hypo-osmolality leads to acute neuronal edema Following correction of hyponatremia, electrolytes rapidly reaccumulate in brain ECF Electrolyte brain content returns to normal levels within 3 -5 days Brain osmolytes cannot be immediately restored when hyponatremia rapidly corrected Brain cells thus subject to osmotic injury & demyelination
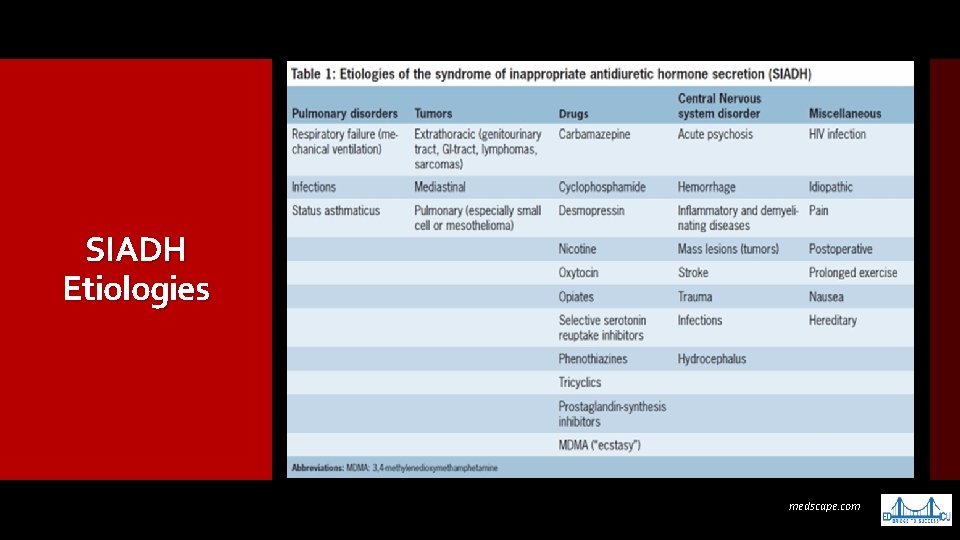
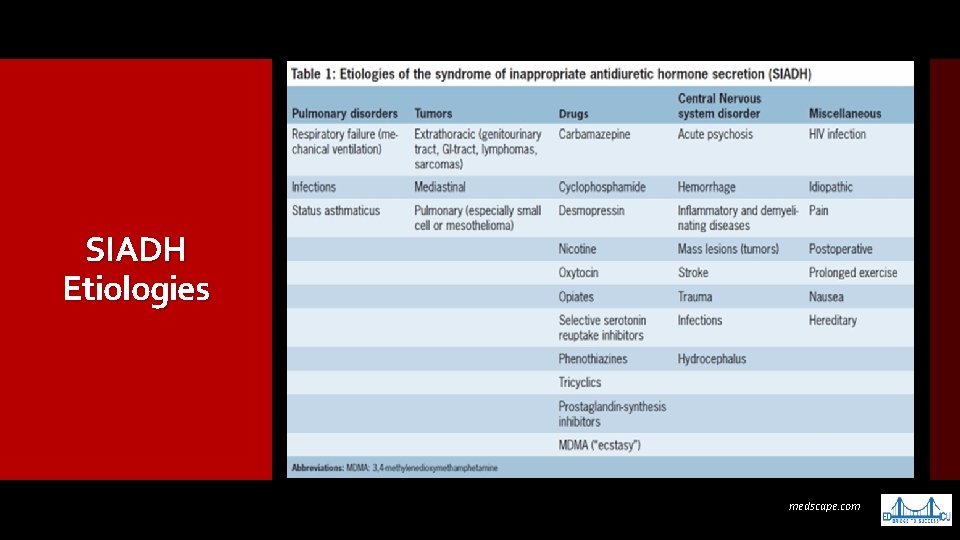
SIADH Etiologies medscape. com
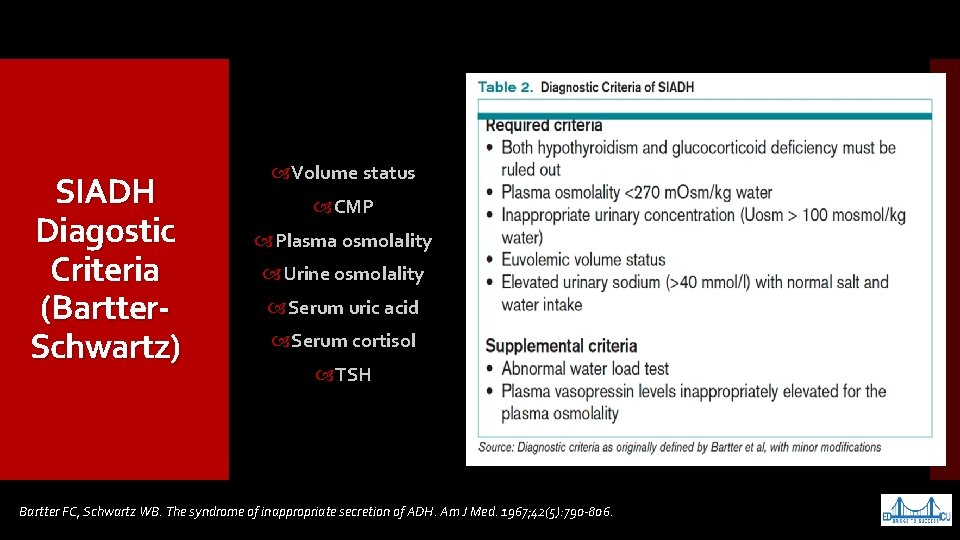
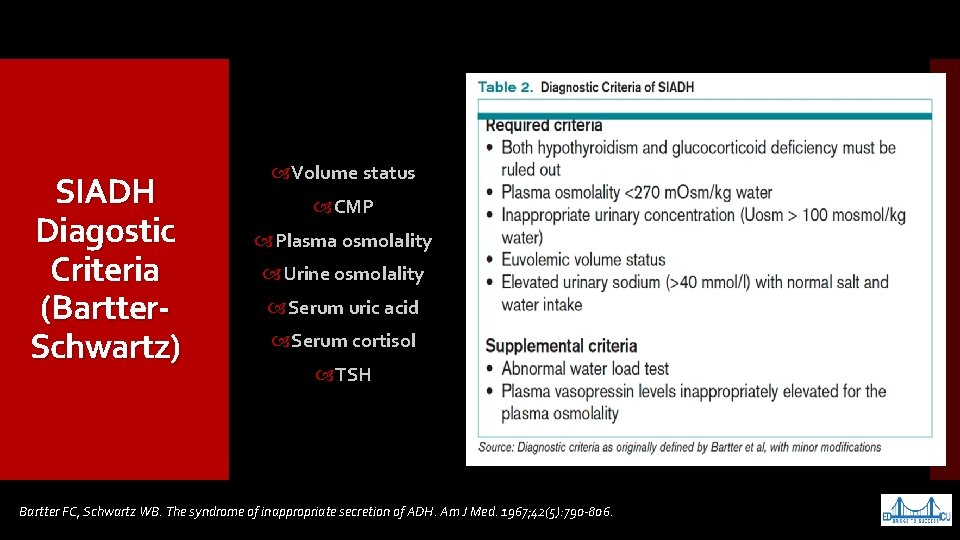
SIADH Diagostic Criteria (Bartter. Schwartz) Volume status CMP Plasma osmolality Urine osmolality Serum uric acid Serum cortisol TSH Bartter FC, Schwartz WB. The syndrome of inappropriate secretion of ADH. Am J Med. 1967; 42(5): 790 -806.
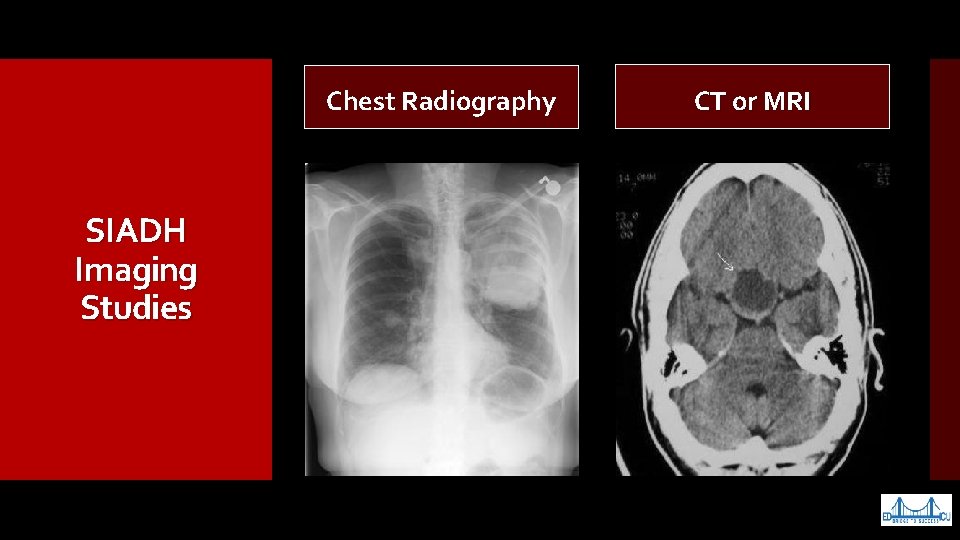
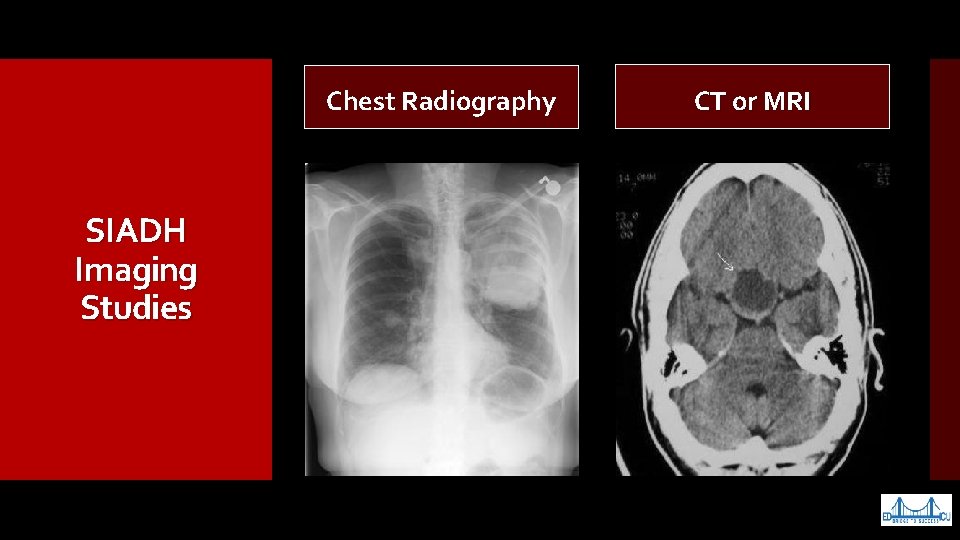
Chest Radiography SIADH Imaging Studies CT or MRI
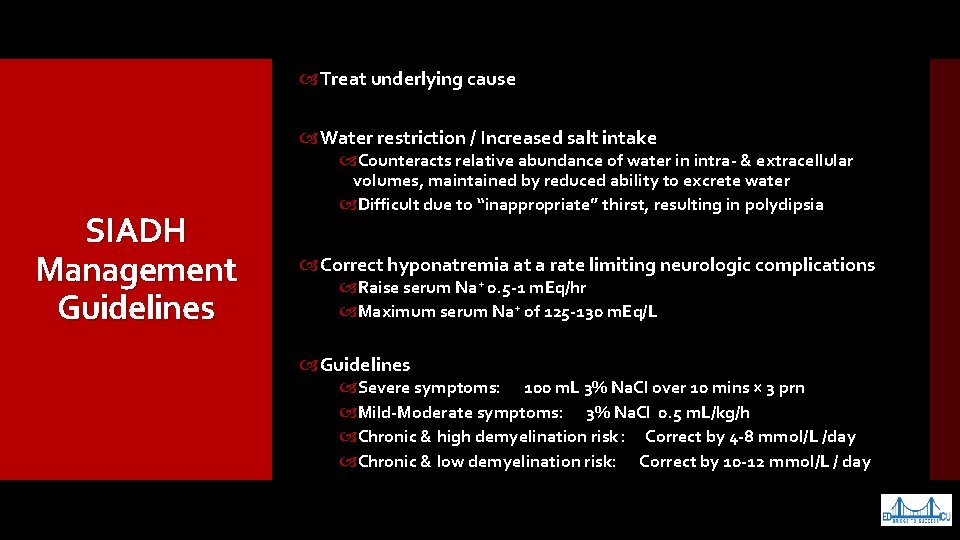
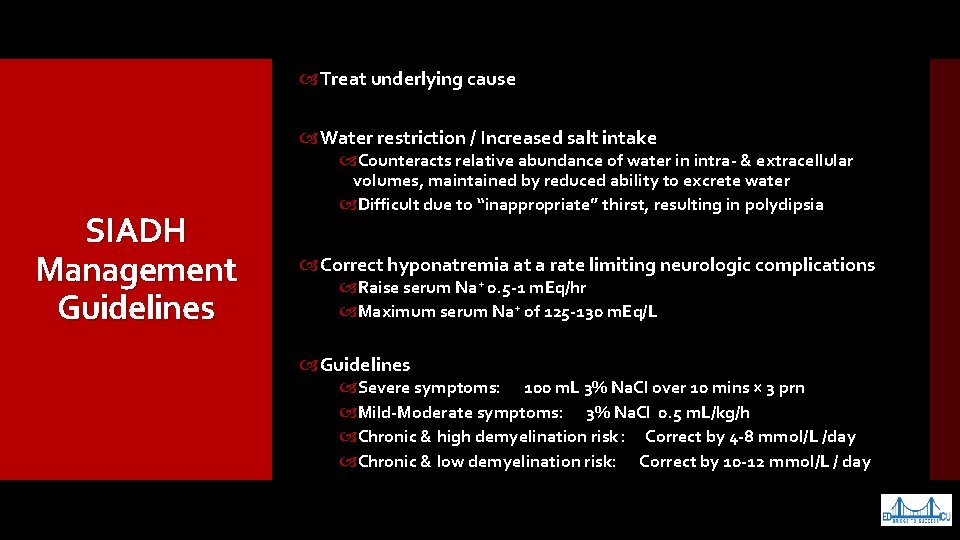
Treat underlying cause Water restriction / Increased salt intake SIADH Management Guidelines Counteracts relative abundance of water in intra- & extracellular volumes, maintained by reduced ability to excrete water Difficult due to “inappropriate” thirst, resulting in polydipsia Correct hyponatremia at a rate limiting neurologic complications Raise serum Na+ 0. 5 -1 m. Eq/hr Maximum serum Na+ of 125 -130 m. Eq/L Guidelines Severe symptoms: 100 m. L 3% Na. Cl over 10 mins × 3 prn Mild-Moderate symptoms: 3% Na. Cl 0. 5 m. L/kg/h Chronic & high demyelination risk : Correct by 4 -8 mmol/L /day Chronic & low demyelination risk: Correct by 10 -12 mmol/L / day
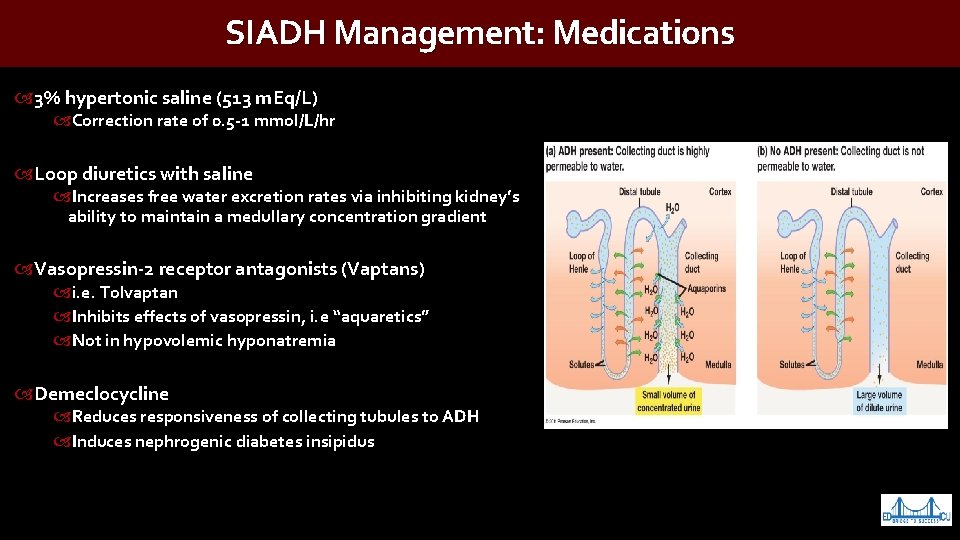
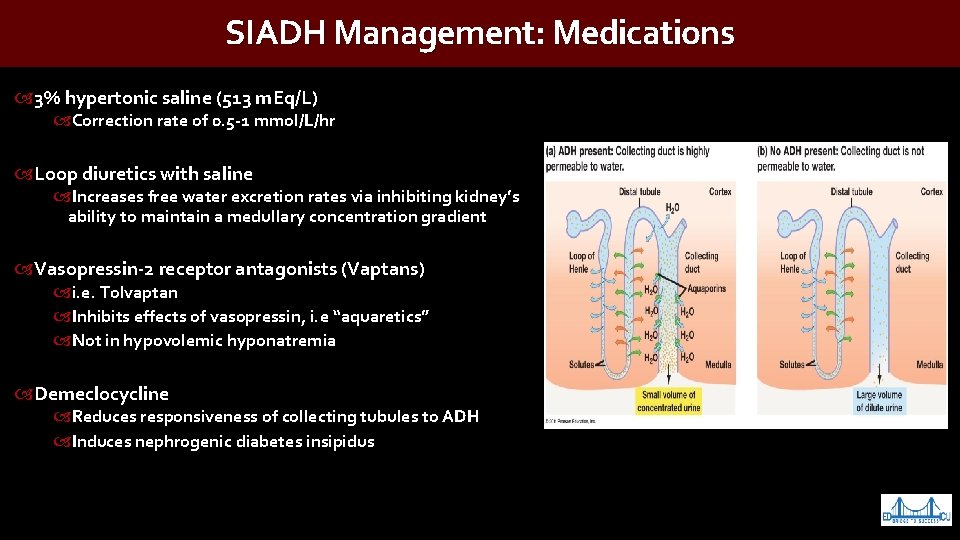
SIADH Management: Medications 3% hypertonic saline (513 m. Eq/L) Correction rate of 0. 5 -1 mmol/L/hr Loop diuretics with saline Increases free water excretion rates via inhibiting kidney’s ability to maintain a medullary concentration gradient Vasopressin-2 receptor antagonists (Vaptans) i. e. Tolvaptan Inhibits effects of vasopressin, i. e “aquaretics” Not in hypovolemic hyponatremia Demeclocycline Reduces responsiveness of collecting tubules to ADH Induces nephrogenic diabetes insipidus
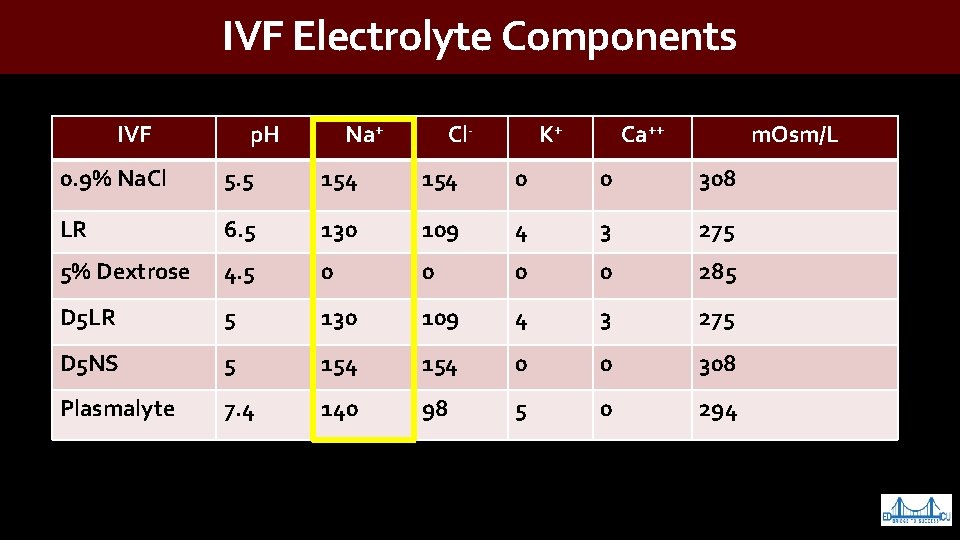
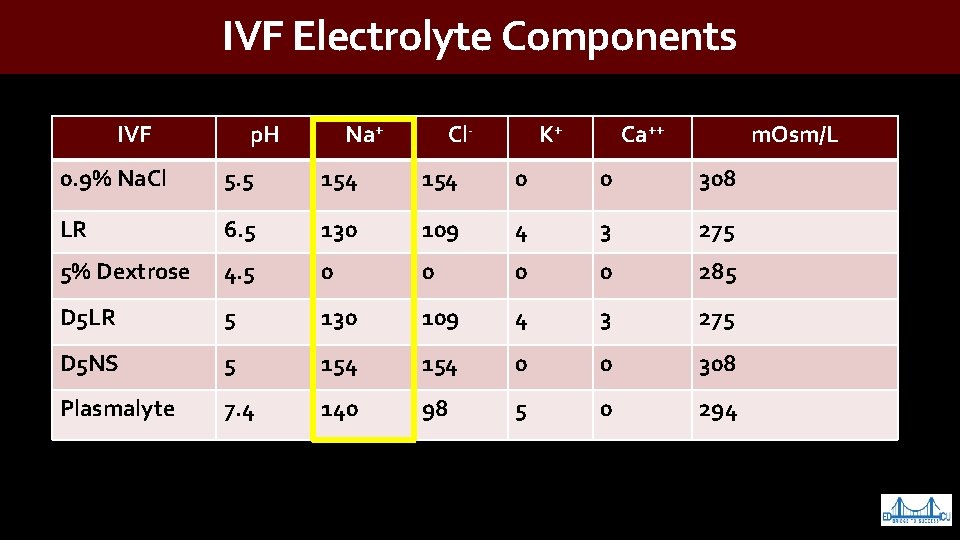
IVF Electrolyte Components IVF p. H Na+ Cl- K+ Ca++ m. Osm/L 0. 9% Na. Cl 5. 5 154 0 0 308 LR 6. 5 130 109 4 3 275 5% Dextrose 4. 5 0 0 285 D 5 LR 5 130 109 4 3 275 D 5 NS 5 154 0 0 308 Plasmalyte 7. 4 140 98 5 0 294
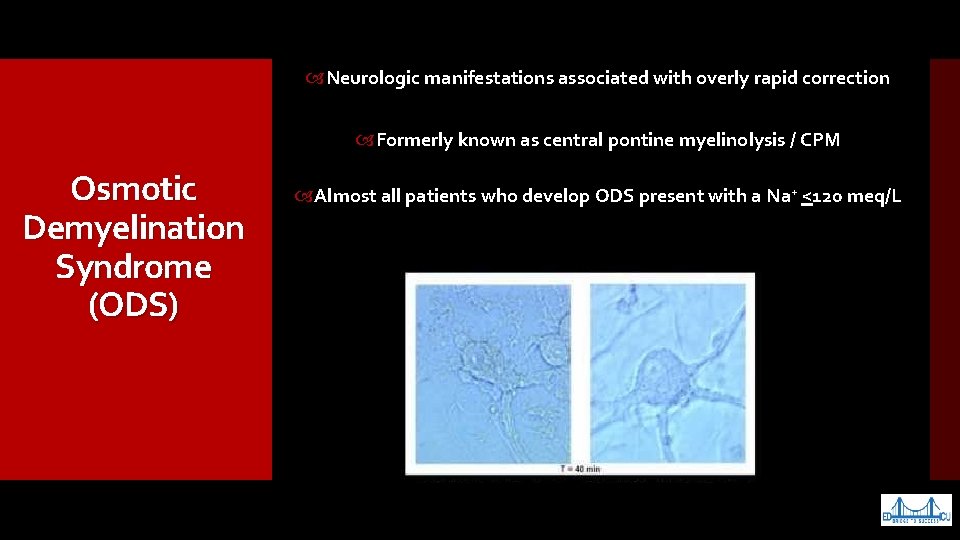
Neurologic manifestations associated with overly rapid correction Formerly known as central pontine myelinolysis / CPM Osmotic Demyelination Syndrome (ODS) Almost all patients who develop ODS present with a Na+ <120 meq/L
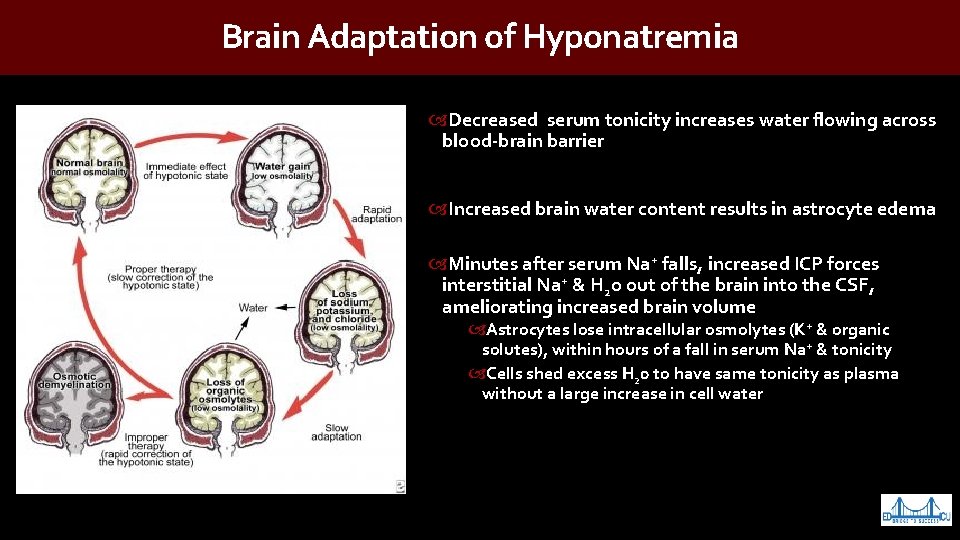
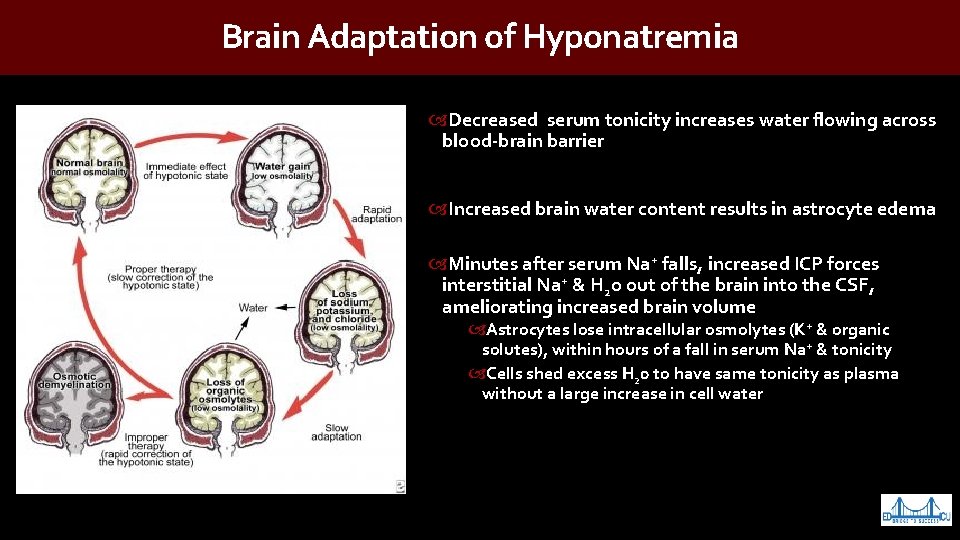
Brain Adaptation of Hyponatremia Decreased serum tonicity increases water flowing across blood-brain barrier Increased brain water content results in astrocyte edema Minutes after serum Na+ falls, increased ICP forces interstitial Na+ & H 2 o out of the brain into the CSF, ameliorating increased brain volume Astrocytes lose intracellular osmolytes (K+ & organic solutes), within hours of a fall in serum Na+ & tonicity Cells shed excess H 20 to have same tonicity as plasma without a large increase in cell water
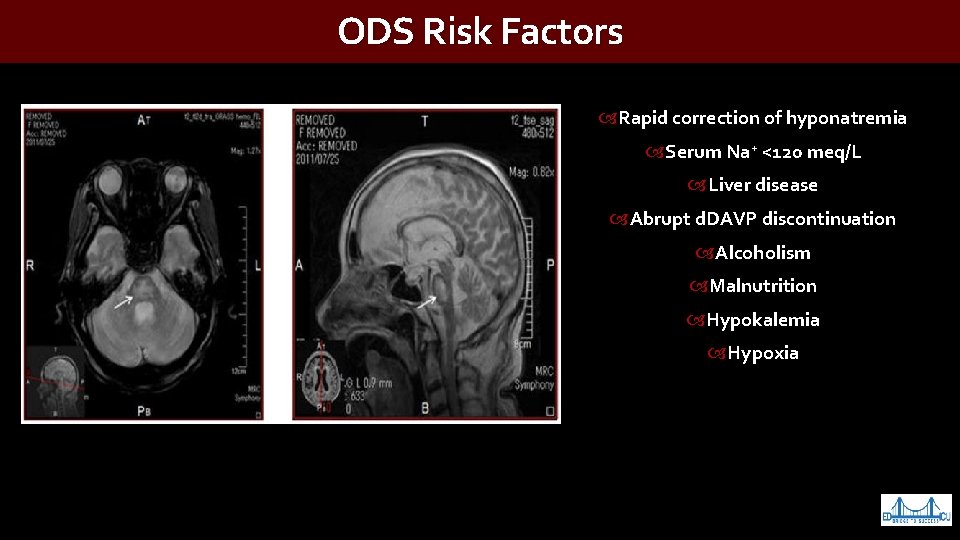
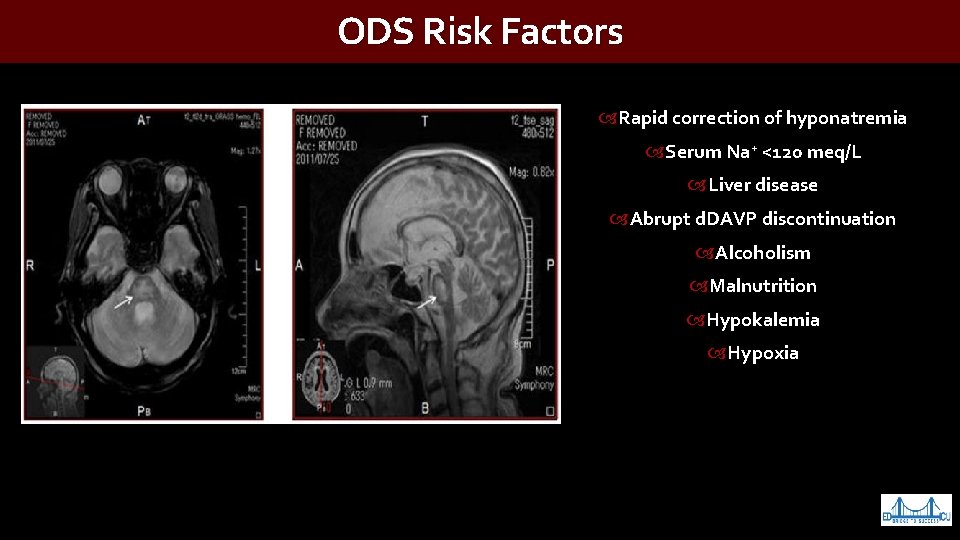
ODS Risk Factors Rapid correction of hyponatremia Serum Na+ <120 meq/L Liver disease Abrupt d. DAVP discontinuation Alcoholism Malnutrition Hypokalemia Hypoxia
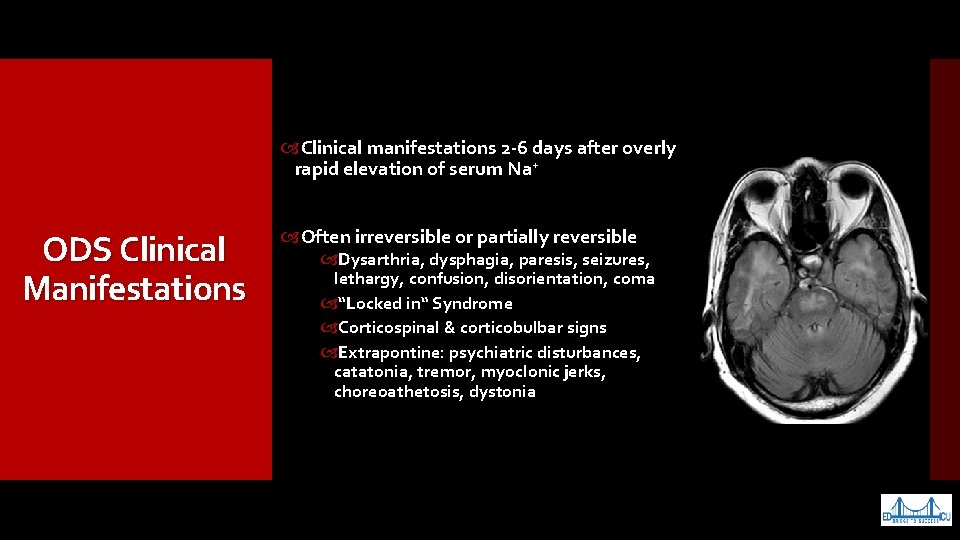
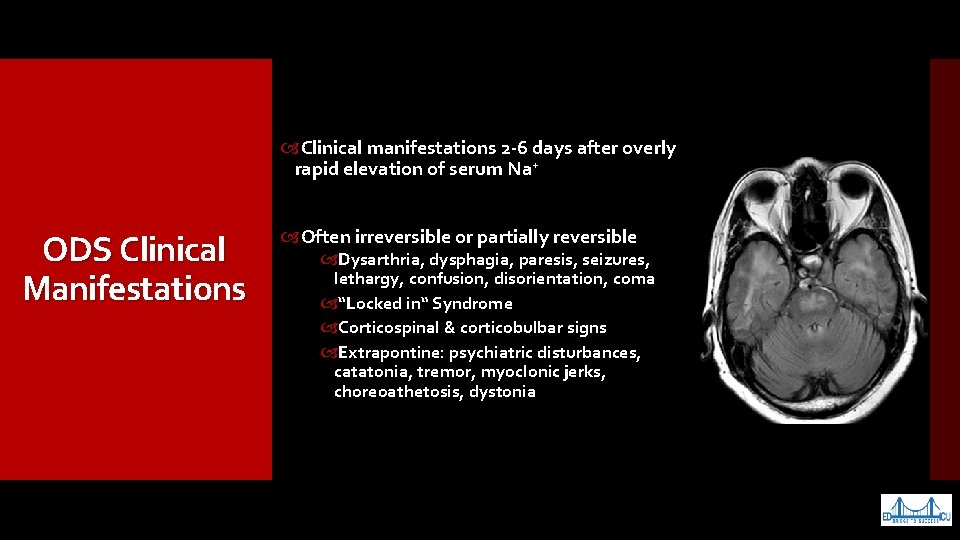
Clinical manifestations 2 -6 days after overly rapid elevation of serum Na+ ODS Clinical Manifestations Often irreversible or partially reversible Dysarthria, dysphagia, paresis, seizures, lethargy, confusion, disorientation, coma “Locked in“ Syndrome Corticospinal & corticobulbar signs Extrapontine: psychiatric disturbances, catatonia, tremor, myoclonic jerks, choreoathetosis, dystonia
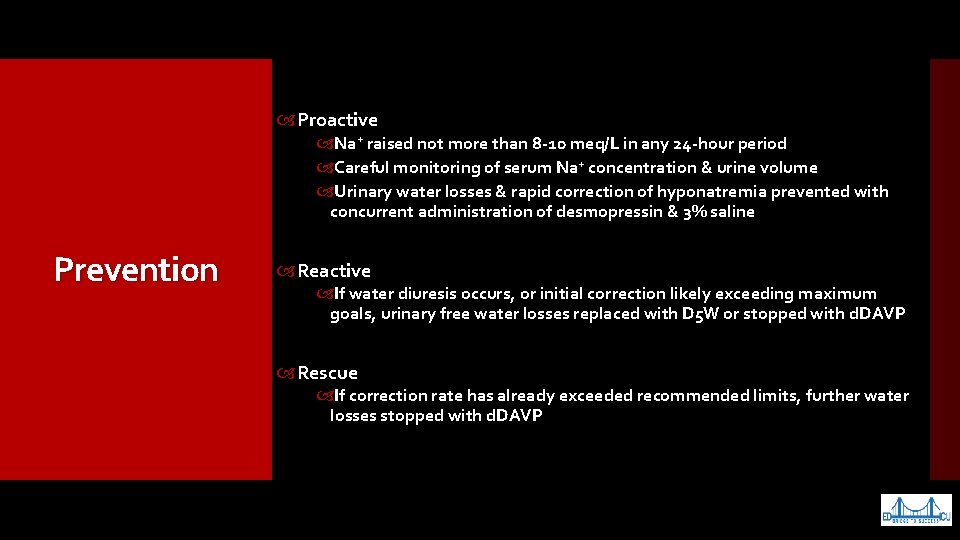
Proactive Na+ raised not more than 8 -10 meq/L in any 24 -hour period Careful monitoring of serum Na+ concentration & urine volume Urinary water losses & rapid correction of hyponatremia prevented with concurrent administration of desmopressin & 3% saline Prevention Reactive If water diuresis occurs, or initial correction likely exceeding maximum goals, urinary free water losses replaced with D 5 W or stopped with d. DAVP Rescue If correction rate has already exceeded recommended limits, further water losses stopped with d. DAVP
Minocycline Investigational Therapies Semisynthetic tetracycline Given concurrently with hypertonic saline reduces ODS severity Neuroprotective: Crosses blood-brain barrier, inhibits microglial activation, reducing microglial production of inflammatory cytokines Dexamethasone & myoinositol Rapidly restoration of organic osmolytes depleted in hyponatremia
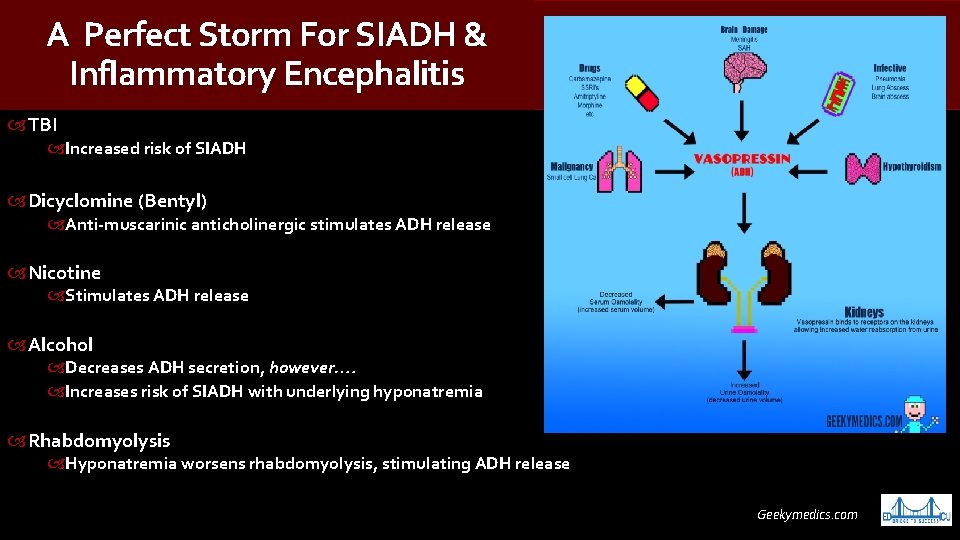
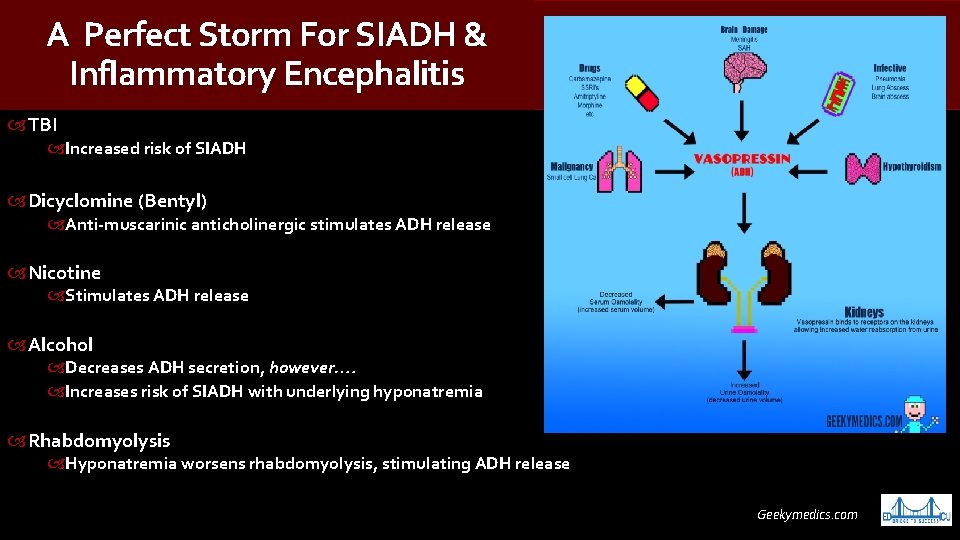
A Perfect Storm For SIADH & Inflammatory Encephalitis TBI Increased risk of SIADH Dicyclomine (Bentyl) Anti-muscarinic anticholinergic stimulates ADH release Nicotine Stimulates ADH release Alcohol Decreases ADH secretion, however…. Increases risk of SIADH with underlying hyponatremia Rhabdomyolysis Hyponatremia worsens rhabdomyolysis, stimulating ADH release Geekymedics. com
Tunkel AR, et al. The management of encephalitis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2008 Aug 1. 47(3): 30327. Bloch KC, Glaser C. Diagnostic approaches for patients with suspected encephalitis. Curr Infect Dis Rep. 2007 Jul. 9(4): 315 -22. Bartter FC, Schwartz WB. The syndrome of inappropriate secretion of antidiuretic hormone. Am J Med. 1967 May. 42(5): 790 -806. Sterns RH. Disorders of plasma sodium--causes, consequences, and correction. N Engl J Med. 2015 Jan 1. 372 (1): 55 -65. Verbalis JG, Berl T. Disorders of water balance. Brenner BM. Brenner & Rector's The Kidney. 8 th ed. Saunders; 2007. Vol 1: 459 -491. Elhassan EA. Hyponatremia: diagnosis, complications, and management including V 2 receptor antagonists. Curr Opin Nephrol Hypertens. 2011 Mar. 20(2): 161 -8. Kohen I, Voelker S, Manu P. Antipsychotic-induced hyponatremia: case report and literature review. Am J Ther. 2008 Sep-Oct. 15(5): 492 -4. Vitting KE, Gardenswartz MH, Zabetakis PM, et al. Frequency of hyponatremia and nonosmolar vasopressin release in the acquired immunodeficiency syndrome. JAMA. 1990 Feb 16. 263(7): 973 -8. Hoorn EJ, Lindemans J, Zietse R. Development of severe hyponatraemia in hospitalized patients: treatment-related risk factors and inadequate management. Nephrol Dial Transplant. 2006 Jan. 21(1): 70 -6. References Stelfox HT, Ahmed SB, Khandwala F, Zygun D, Shahpori R, Laupland K. The epidemiology of intensive care unit-acquired hyponatraemia and hypernatraemia in medical-surgical intensive care units. Crit Care. 2008. 12(6): R 162. Ayus JC, Varon J, Arieff AI. Hyponatremia, cerebral edema, & noncardiogenic pulmonary edema in marathon runners. Ann Intern Med. 2000 May 2. 132(9): 711 -4. Kumar S, Fowler M, Gonzalez-Toledo E, Jaffe SL. Central pontine myelinolysis, an update. Neurol Res. 2006 Apr. 28(3): 360 -6. https: //www. pharmacyjoe. com/why-normal-saline-makes-hyponatremia-worse-in-siadh/ Ellison DH, Berl T. Clinical practice. The syndrome of inappropriate antidiuresis. N Engl J Med. 2007 May 17. 356(20): 2064 -72. Spasovski G, Vanholder R, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Nephrol Dial Transplant. 2014 Feb 25. Danz M, Pöttgen K, et a; . Hyponatremia among Triathletes in the Ironman European Championship. N Engl J Med. 2016 Mar 10. 374 (10): 997 -8. Verbalis JG, Goldsmith SR, Greenberg A, Korzelius C, Schrier RW, Sterns RH, et al. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am J Med. 2013 Oct. 126 (10 Suppl 1): S 1 -42. Vachharajani TJ, Zaman F, Abreo KD. Hyponatremia in critically ill patients. J Intensive Care Med. 2003 Jan-Feb. 18(1): 3 -8. Dixon MB, Lien YH. Tolvaptan and its potential in the treatment of hyponatremia. Ther Clin Risk Manag. 2008 Dec. 4(6): 1149 -55. [Medline]. Ruzek KA, et al. Early diagnosis of central pontine myelinolysis with diffusion-weighted imaging. AJNR Am J Neuroradiol. 2004 Feb. 25(2): 210 -3. Pham PC, Pham PM, Pham PT. Vasopressin excess and hyponatremia. Am J Kidney Dis. 2006 May. 47(5): 727 -37. [Medline]. Sterns RH. The syndrome of inappropriate antidiuretic hormone secretion of unknown origin. Am J Kidney Dis. 1999 Jan. 33(1): 161 -3; discussion 163 -5.
Brain adaptations that reduce the cerebral edema associated with hyponatremia make the brain vulnerable to injury Summary & Recommendations Management of hyponatremia based on understanding CNS adaptations to altered serum osmolality Vigilance in evaluating & managing lab abnormalities Treatment varies by etiology, but cautious correction of sodium important to prevent osmotic demyelination
www. crowdrise. com/ westchestermedicalcenter healthnetwork