Common Allergy Symptoms Among Toddler CME for NURSES










- Slides: 48
Common Allergy Symptoms Among Toddler CME for NURSES Dr Intan Hakimah Ismail Consultant Paediatrician Paediatric Allergist and Immunologist Universiti Putra Malaysia
Overview – allergic disease • Prevalence • Definition • Clinical manifestations • Diagnosis
Allergic disease • Affects 30 -40% of people worldwide 1 • The 5 th leading chronic disease among all ages • The 3 rd common chronic disease among children under 18 years old; up to one child in three is affected • The prevalence is increasing in all regions of the world undergoing industrial development and westernization 1 WAO White Book on Allergy 2011/12
• Allergies affect people from the early stages of their life and continue until their late adult ages • A major global health issue
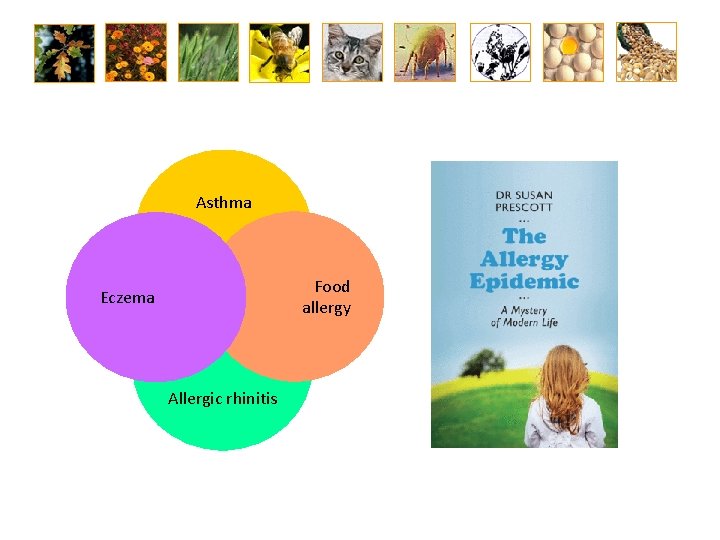
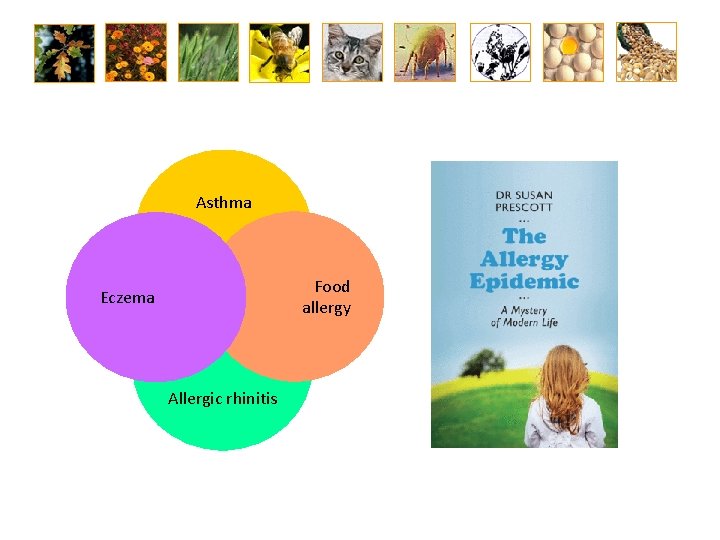
Asthma Food allergy Eczema Allergic rhinitis
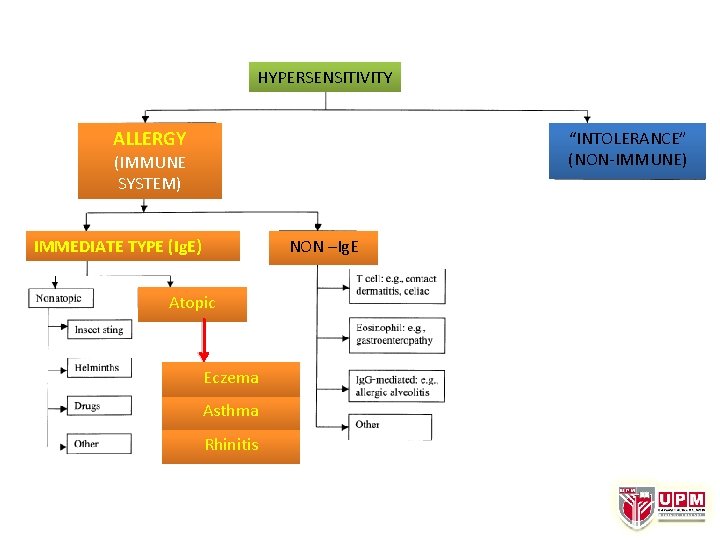
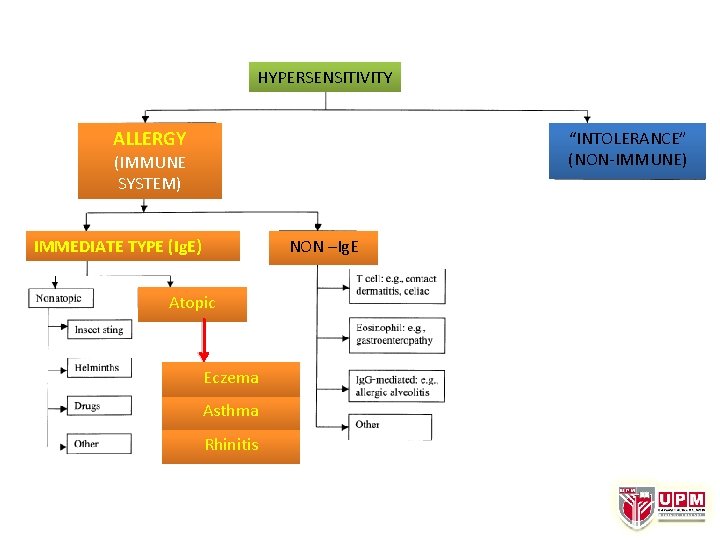
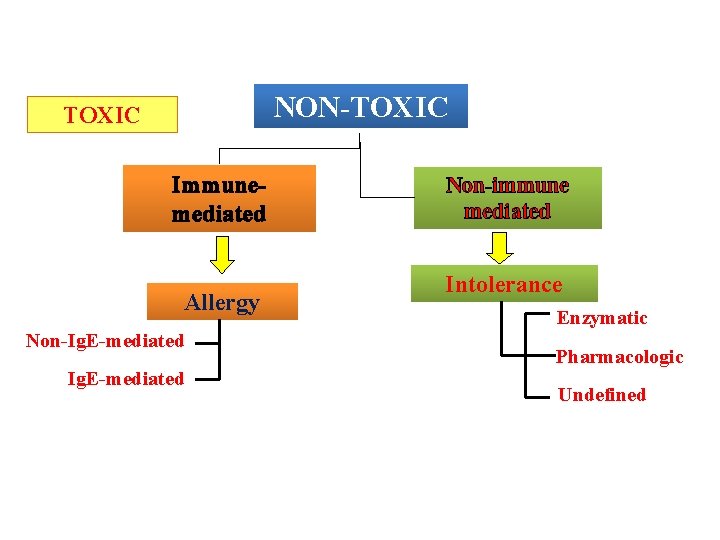
HYPERSENSITIVITY ALLERGY “INTOLERANCE” (NON-IMMUNE) (IMMUNE SYSTEM) IMMEDIATE TYPE (Ig. E) NON –Ig. E Atopic Eczema Asthma Rhinitis
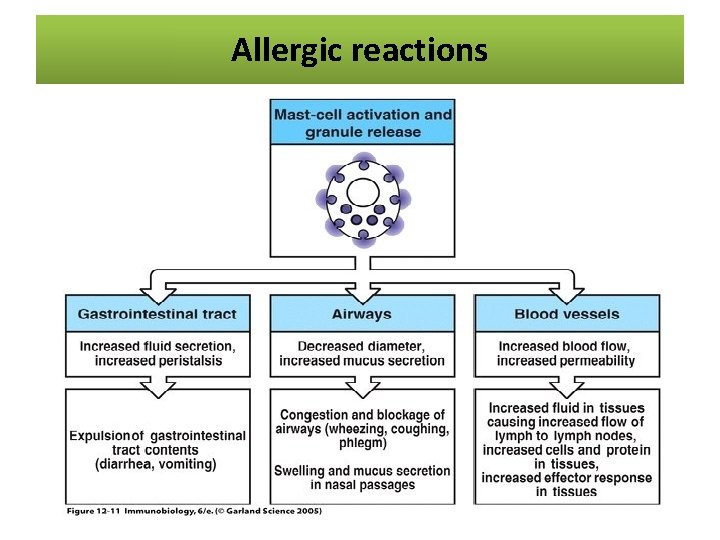
What causes allergic reactions? • Overactive immune system • Body believes a substance is harmful • Body wants to protect itself by fighting that substance off • Immune system releases chemicals and histamine, triggering the reaction
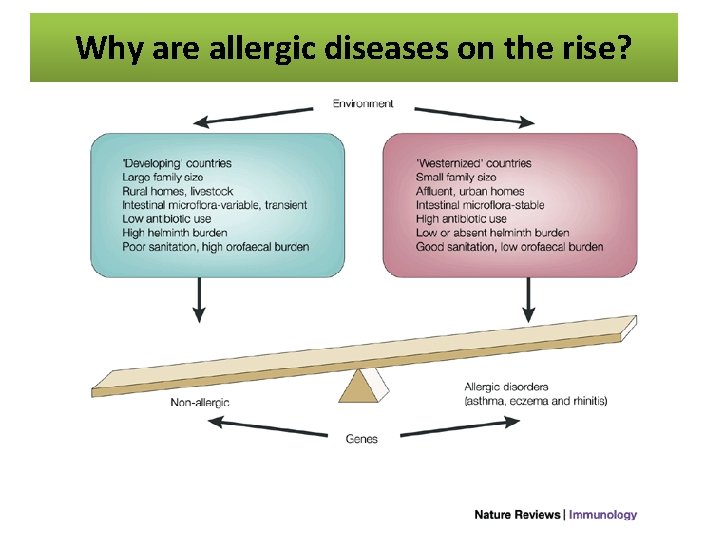
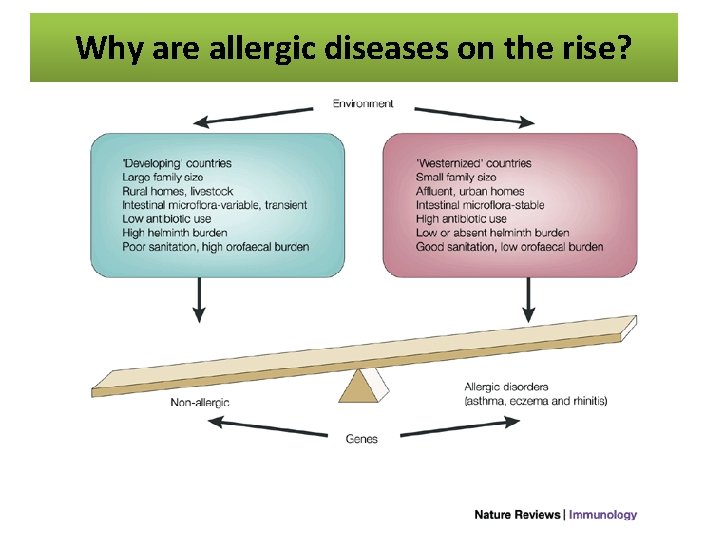
Why are allergic diseases on the rise?
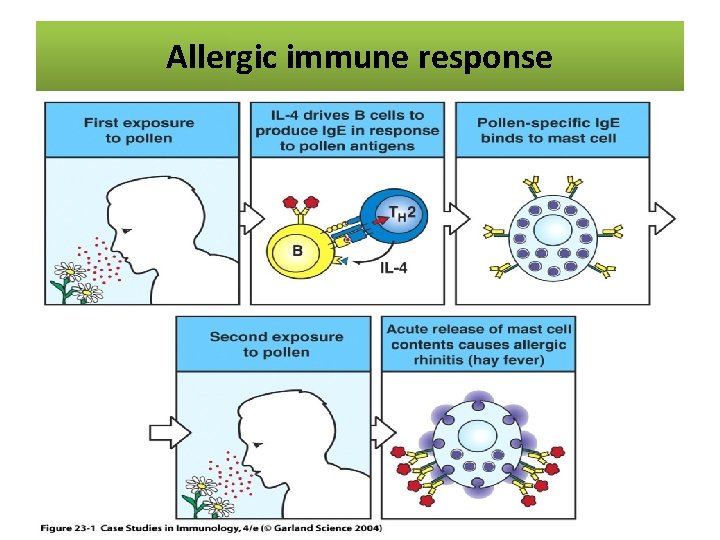
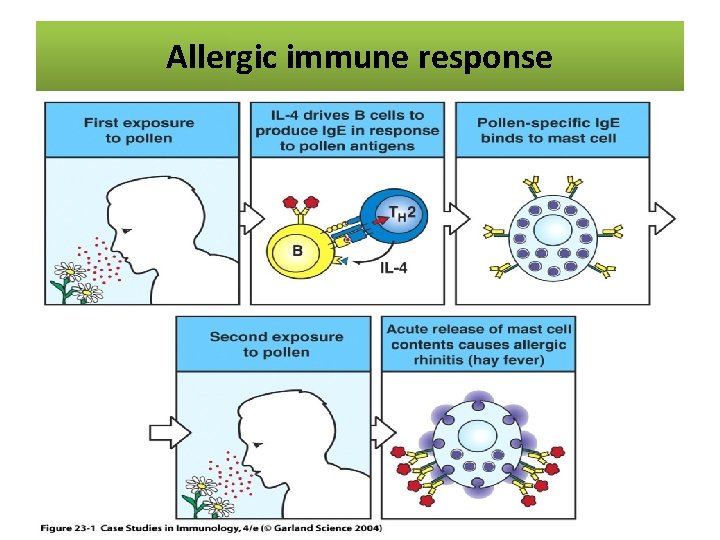
The allergic reaction Allergic immune response

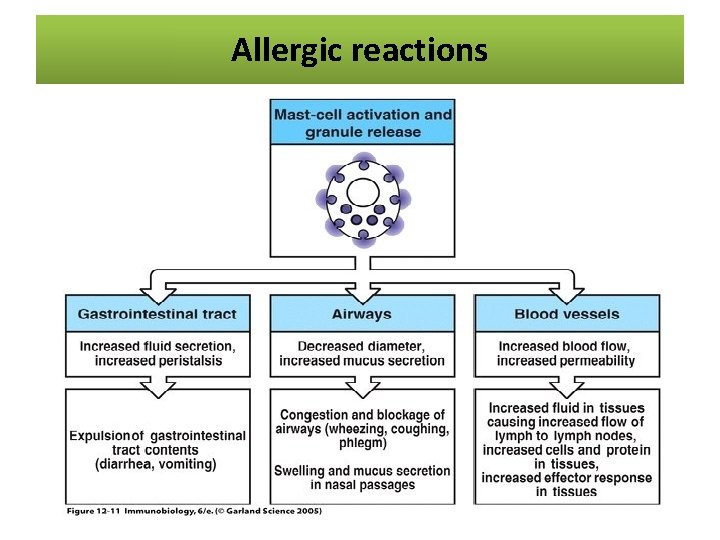
Allergic reactions
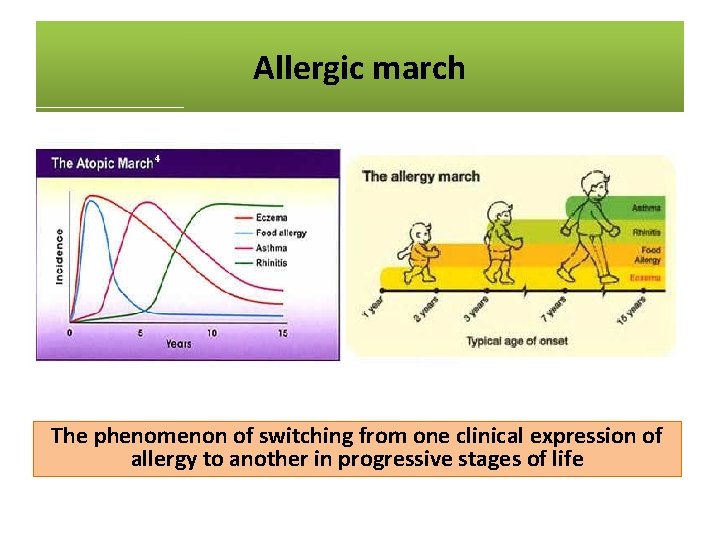
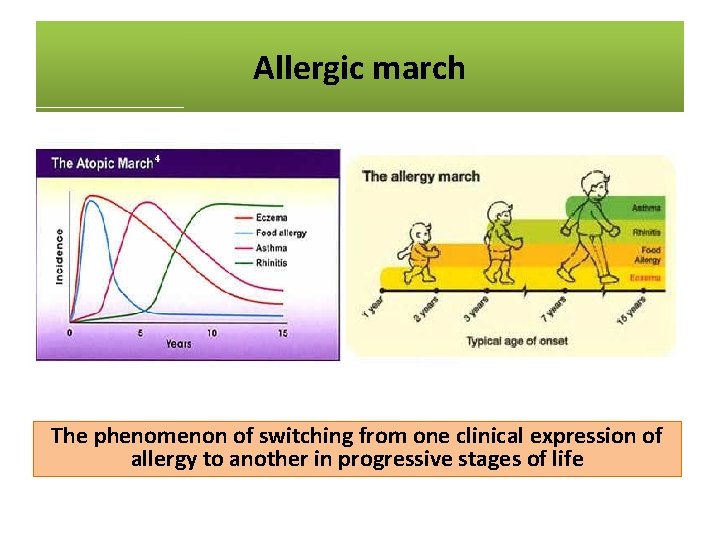
Allergic march The phenomenon of switching from one clinical expression of allergy to another in progressive stages of life
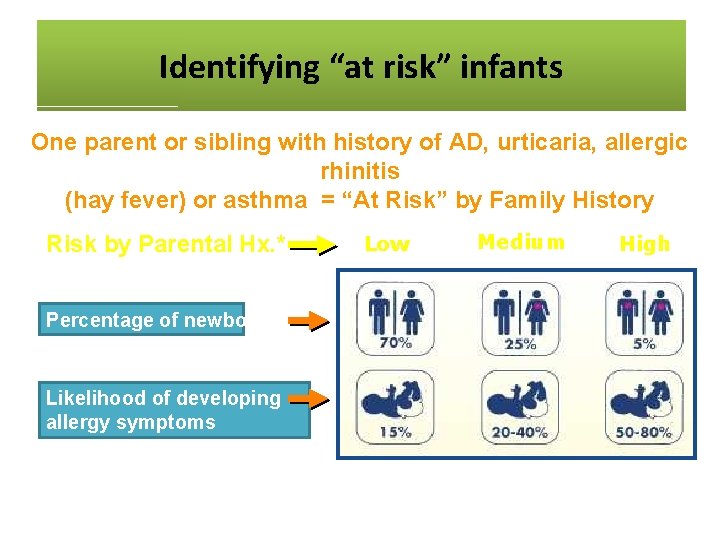
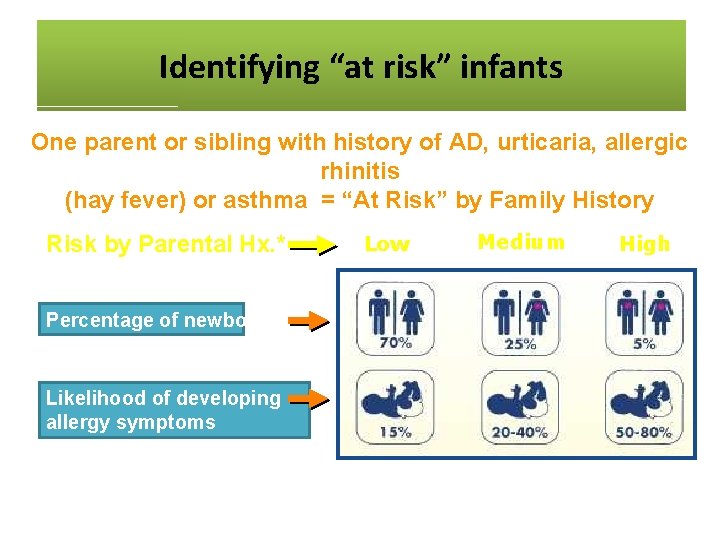
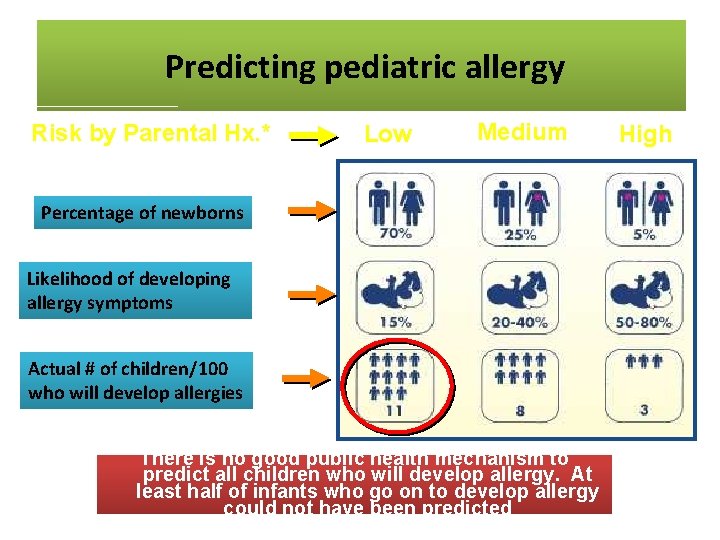
Identifying“At “at risk” Identifying Risk”infants Infants One parent or sibling with history of AD, urticaria, allergic rhinitis (hay fever) or asthma = “At Risk” by Family History Risk by Parental Hx. * Percentage of newborns Likelihood of developing allergy symptoms *Approximate numbers in developed countries. Adapted from 1. Bousquet J. et al. J Allergy Clin Immunol 1986; 78: 1019 -1022 2. Halken S et al. Allergy 2000; 55: 793 -802 3. Kjellman N. et al. Acta Paediatr Scan 1977; 66: 565 -71 4. Exl BM, Nutr Res 2001; 21: 355 -79 Low Medium High
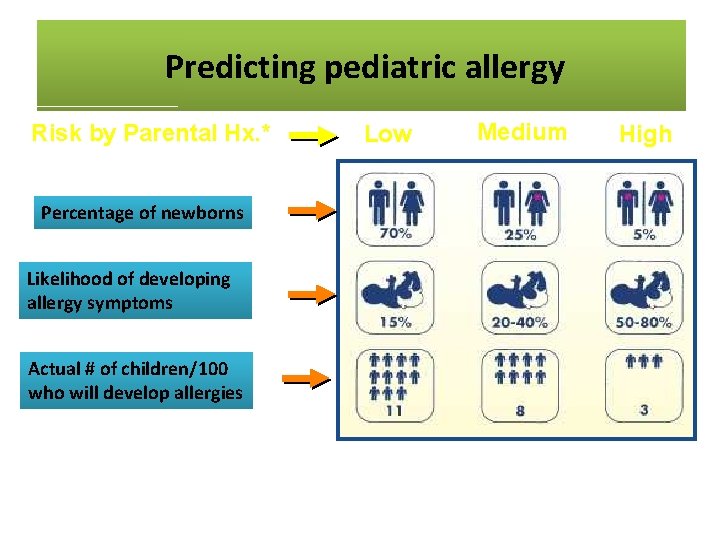
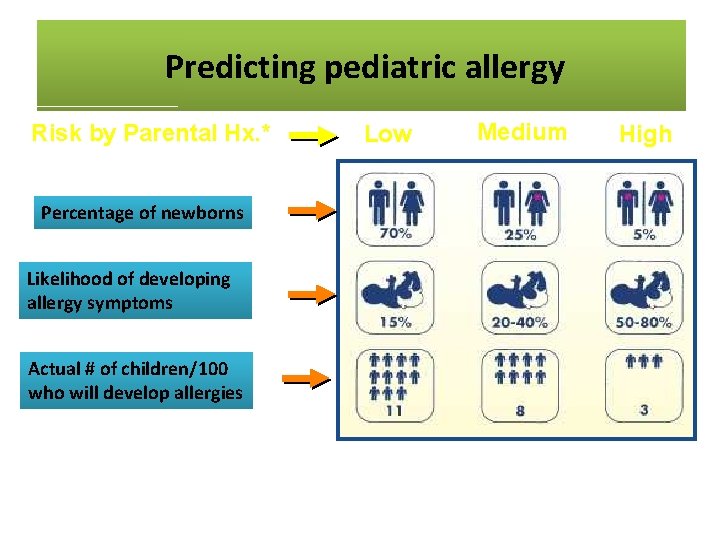
Predicting. Pediatric pediatric allergy Predicting Allergy Risk by Parental Hx. * Percentage of newborns Likelihood of developing allergy symptoms Actual # of children/100 who will develop allergies *Approximate numbers in developed countries Low Medium High
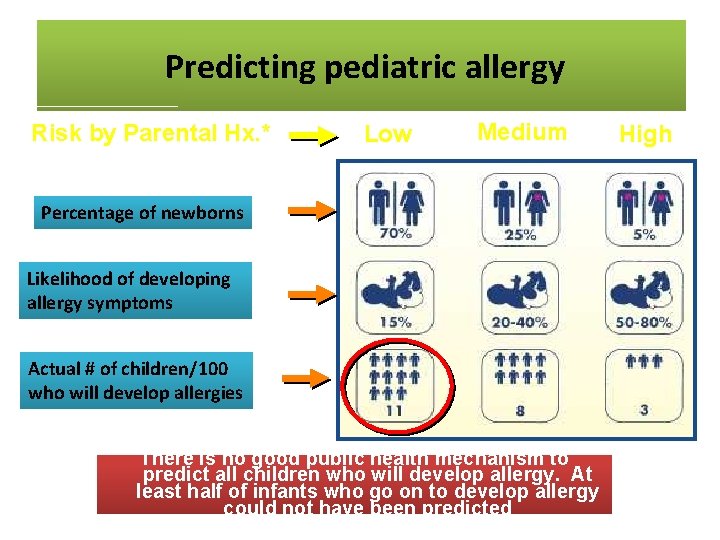
Predicting. Pediatric pediatric allergy Predicting Allergy Risk by Parental Hx. * Low Medium Percentage of newborns Likelihood of developing allergy symptoms Actual # of children/100 who will develop allergies There is no good public health mechanism to predict all children who will develop allergy. At least half of infants who go on to develop allergy *Approximate numbers in developed countries could not have been predicted High

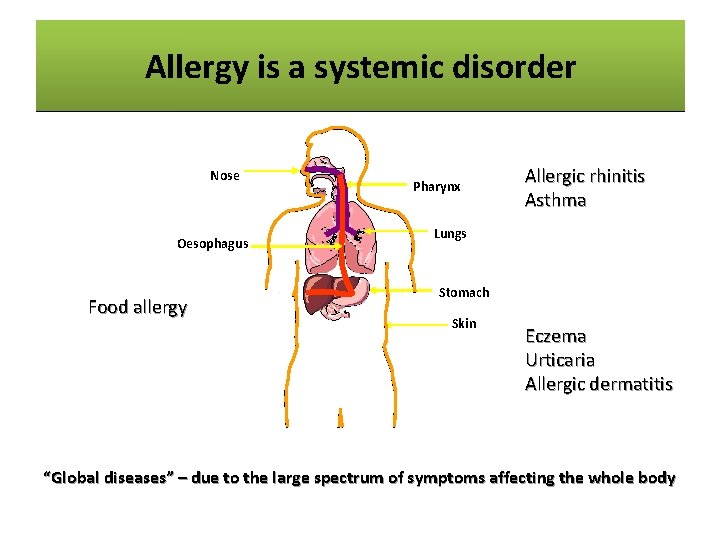
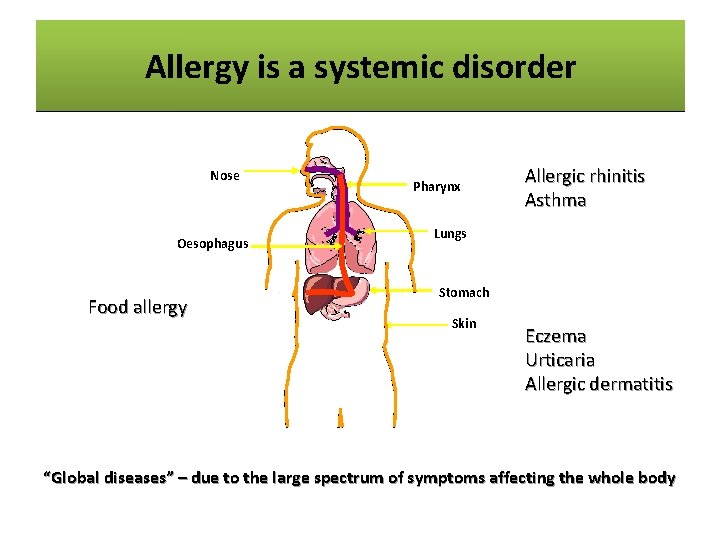
Allergyisisaasystemic disorder Allergy disorder Nose Oesophagus Food allergy Pharynx Allergic rhinitis Asthma Lungs Stomach Skin Eczema Urticaria Allergic dermatitis “Global diseases” – due to the large spectrum of symptoms affecting the whole body
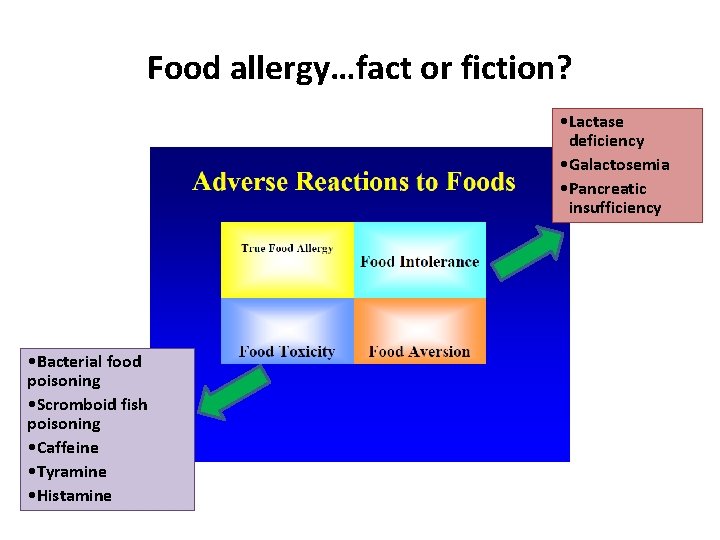
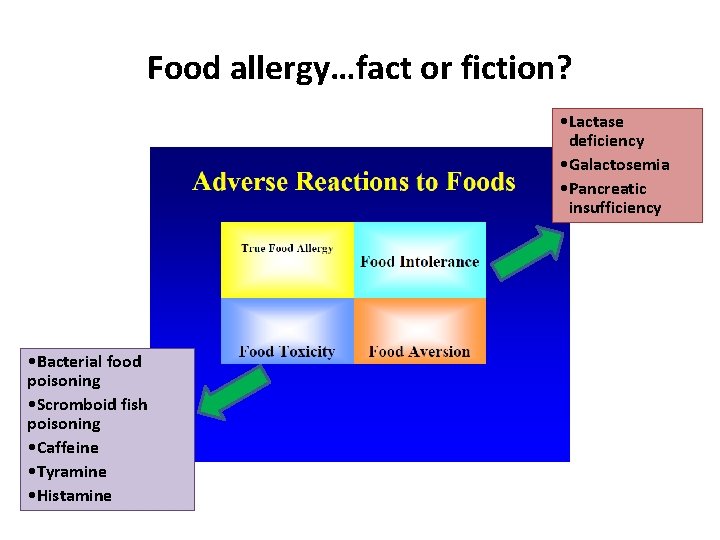
Food allergy…fact or fiction? • Lactase deficiency • Galactosemia • Pancreatic insufficiency • Bacterial food poisoning • Scromboid fish poisoning • Caffeine • Tyramine • Histamine
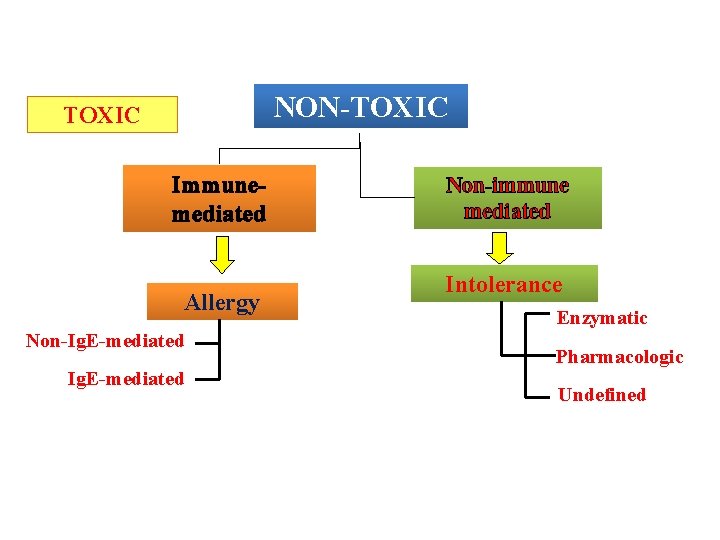
Adverse reactions to food NON-TOXIC Immunemediated Allergy Non-Ig. E-mediated Adverse Reactions to Food: Position Paper. Allergy 1995; 50: 623 -635 Non-immune mediated Intolerance Enzymatic Pharmacologic Undefined
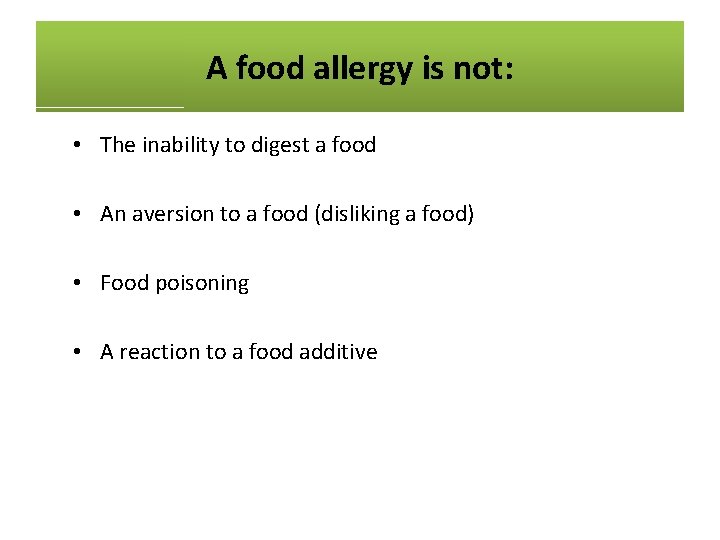
A food allergy is not: • The inability to digest a food • An aversion to a food (disliking a food) • Food poisoning • A reaction to a food additive

The“Big Eight”: The Eight”
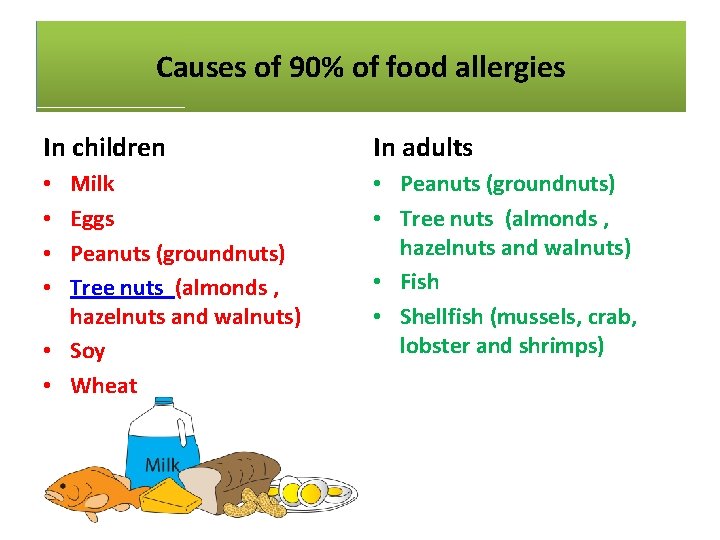
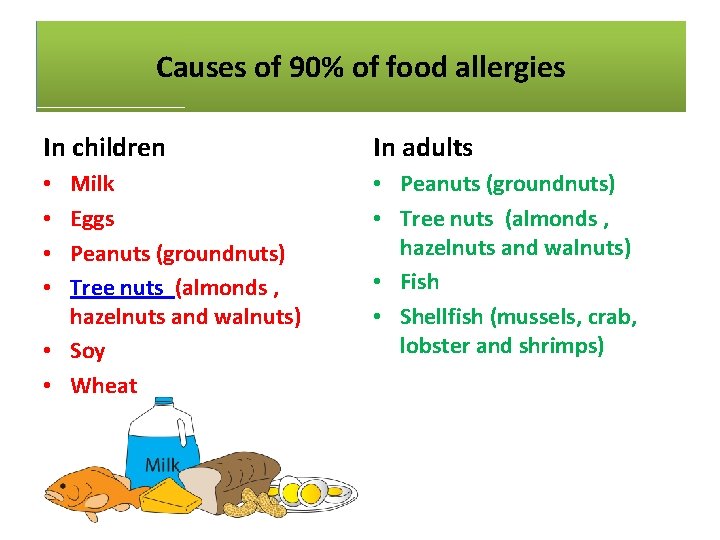
Causes 90%of of food allergies Causes of of 90% Food Allergies In children In adults Milk Eggs Peanuts (groundnuts) Tree nuts (almonds , hazelnuts and walnuts) • Soy • Wheat • Peanuts (groundnuts) • Tree nuts (almonds , hazelnuts and walnuts) • Fish • Shellfish (mussels, crab, lobster and shrimps) • •
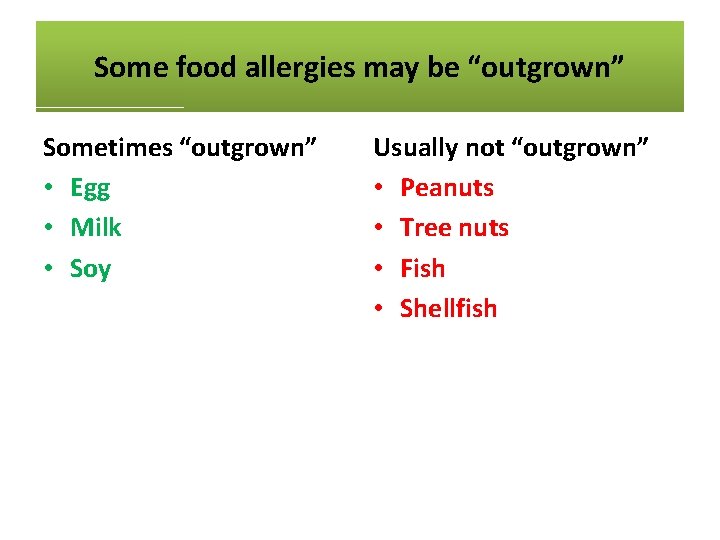
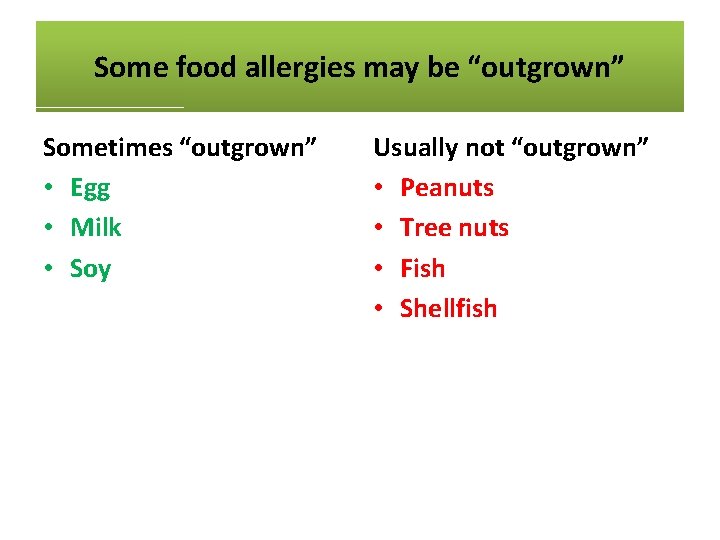
Some food allergies may be “outgrown” Sometimes “outgrown” • Egg • Milk • Soy Usually not “outgrown” • Peanuts • Tree nuts • Fish • Shellfish
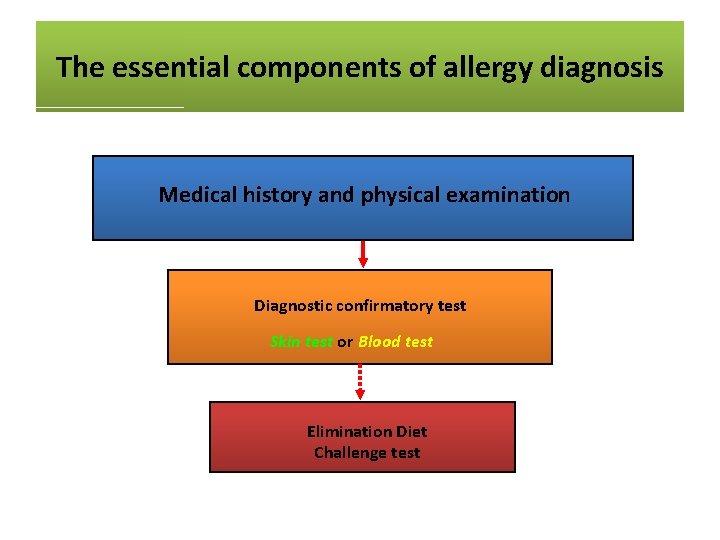
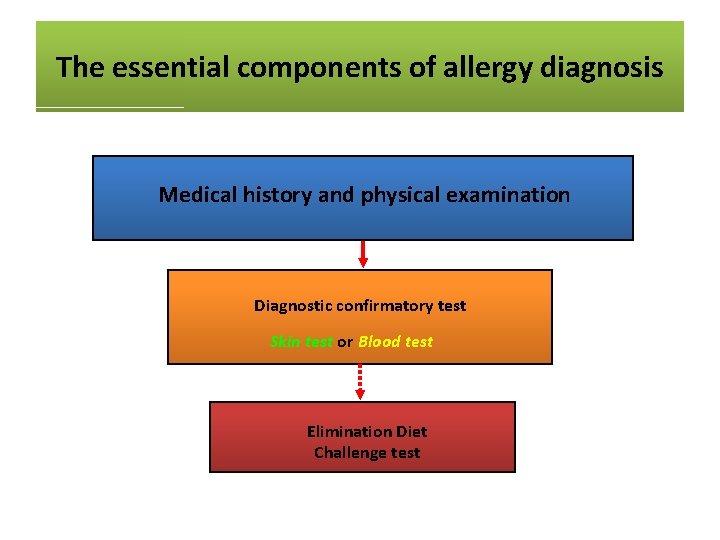
The essential components of allergy diagnosis Medical history and physical examination Diagnostic confirmatory test Skin test or Blood test Elimination Diet Challenge test
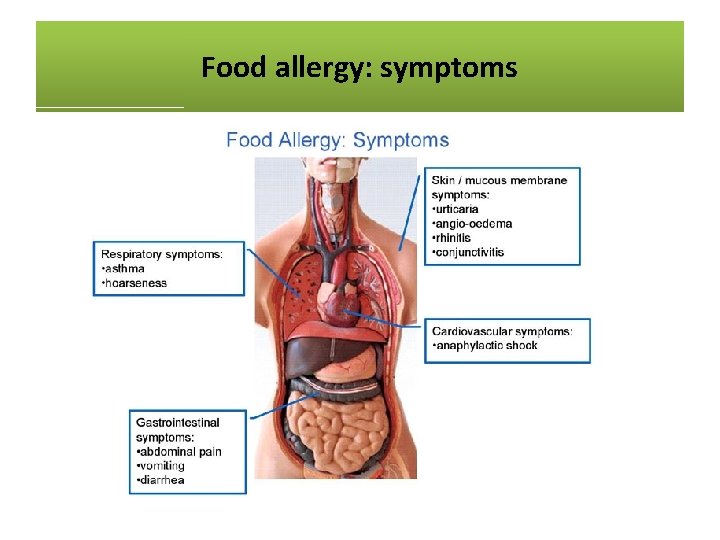
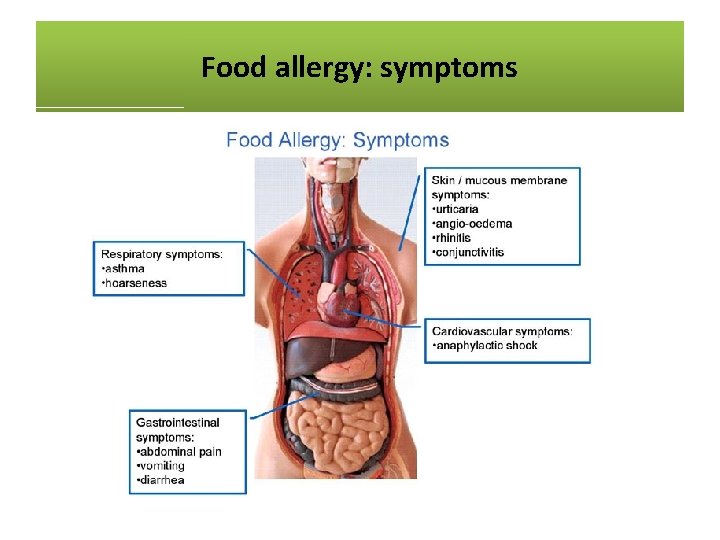
Food allergy: symptoms
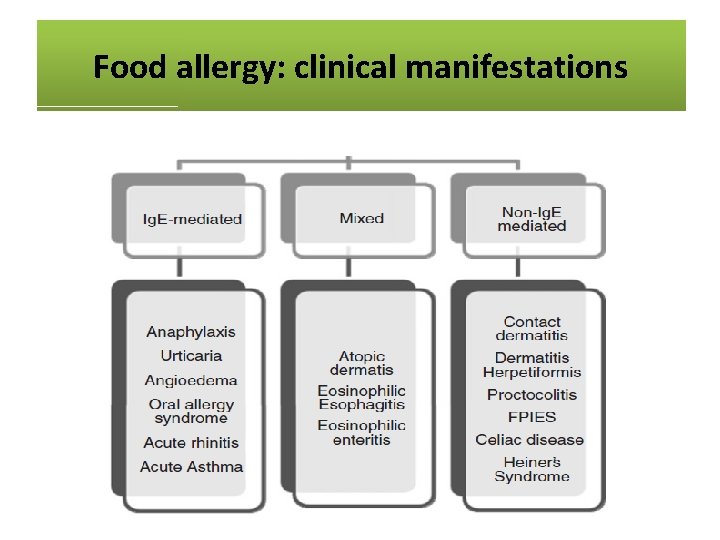
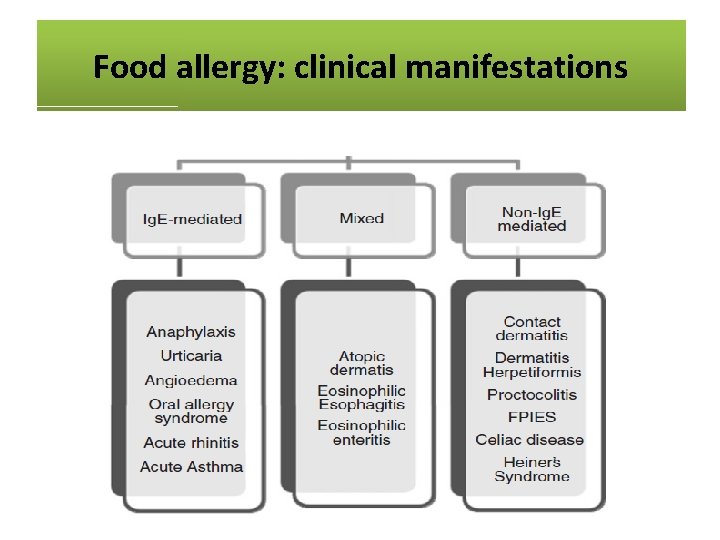
Food allergy: clinical manifestations

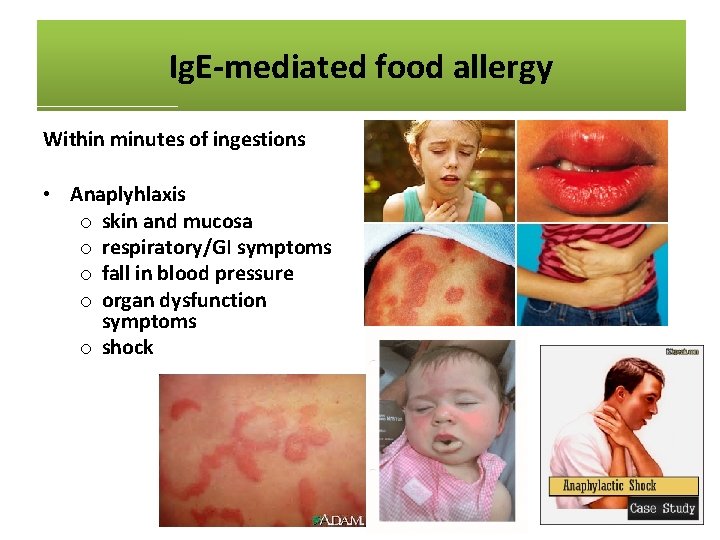
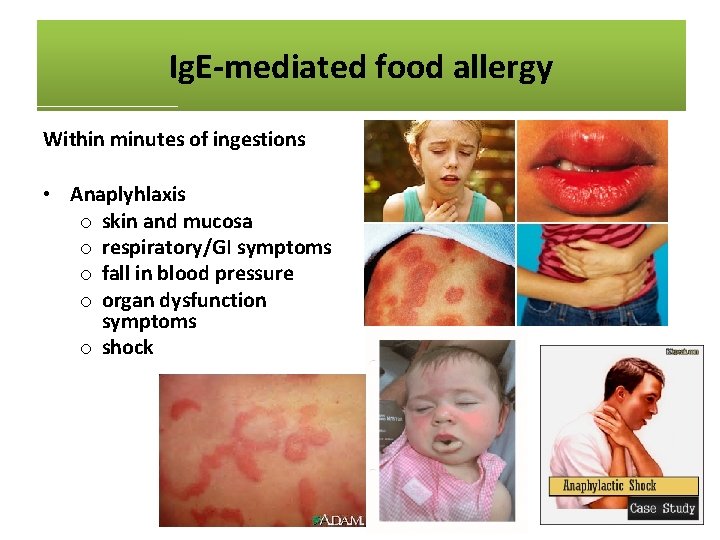
Ig. E-mediated food allergy Within minutes of ingestions • Anaplyhlaxis o skin and mucosa o respiratory/GI symptoms o fall in blood pressure o organ dysfunction symptoms o shock
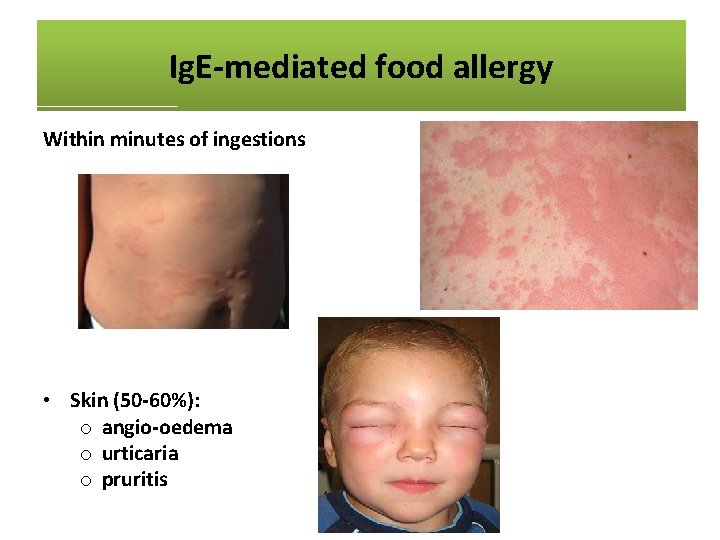
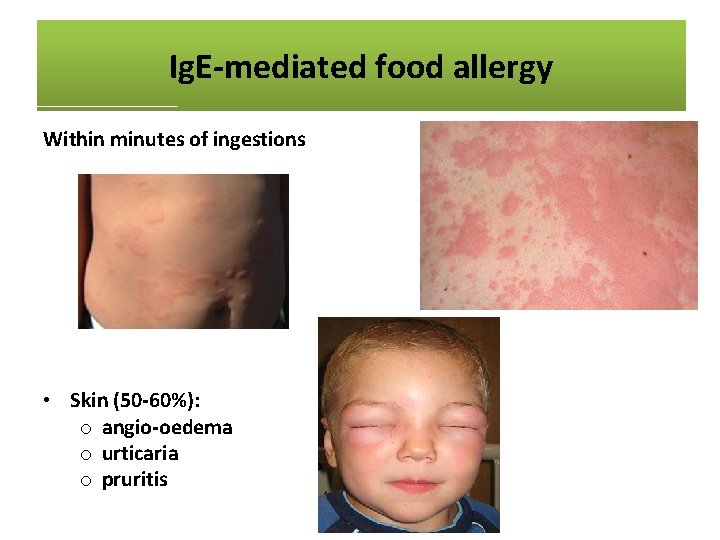
Ig. E-mediated food allergy Within minutes of ingestions • Anaplyhlaxis o skin and mucosa o respiratory/GI symptoms o fall in blood pressure o organ dysfunction symptoms o shock • Skin (50 -60%): o angio-oedema o urticaria o pruritis
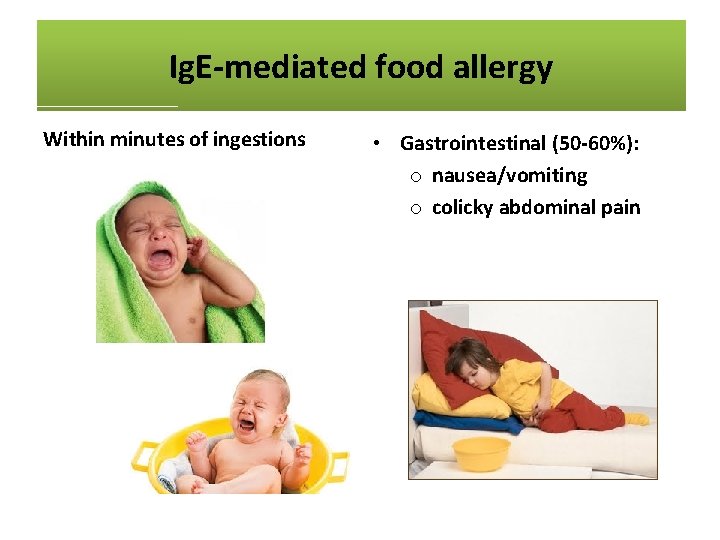
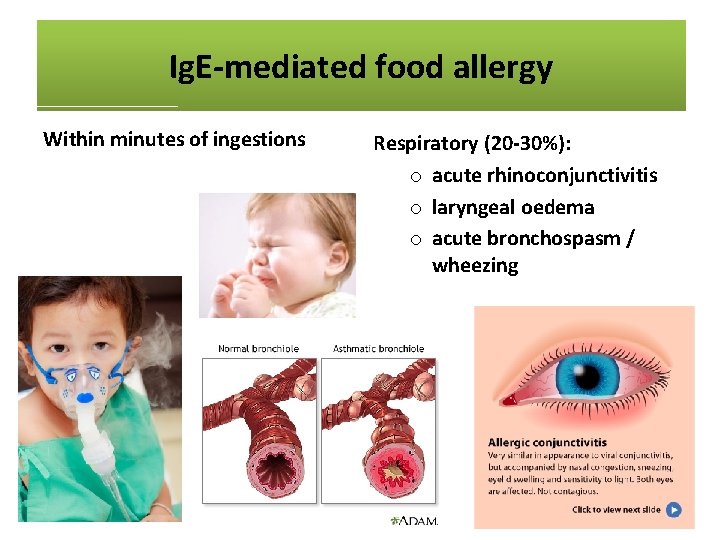
Ig. E-mediated food allergy Within minutes of ingestions • Anaplyhlaxis o skin and mucosa o respiratory/GI symptoms o fall in blood pressure o organ dysfunction symptoms o shock • Skin (50 -60%): o angio-oedema o urticaria o pruritis • Gastrointestinal (50 -60%): o nausea/vomiting o colicky abdominal pain • Respiratory (20 -30%): o acute rhinoconjunctivitis o laryngeal oedema o acute bronchospasm / wheezing
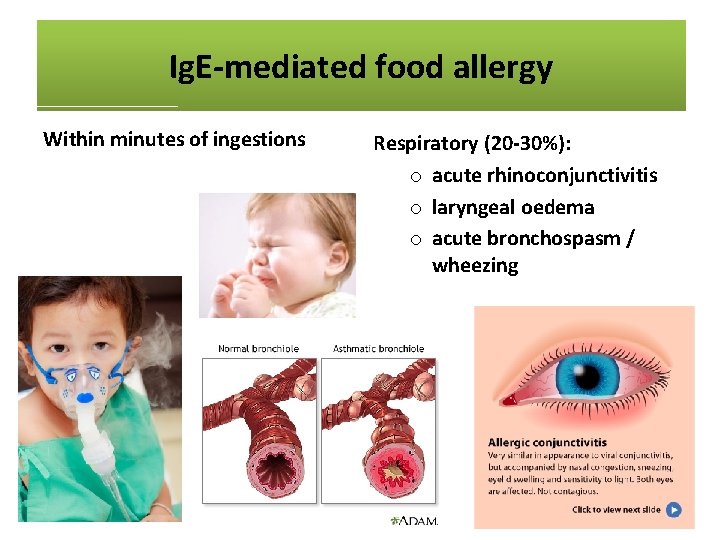
Ig. E-mediated food allergy Within minutes of ingestions • Anaplyhlaxis o skin and mucosa o respiratory/GI symptoms o fall in blood pressure o organ dysfunction symptoms o shock • Skin (50 -60%): o angio-oedema o urticaria o pruritis Respiratory (20 -30%): o acute rhinoconjunctivitis o laryngeal oedema o acute bronchospasm / wheezing

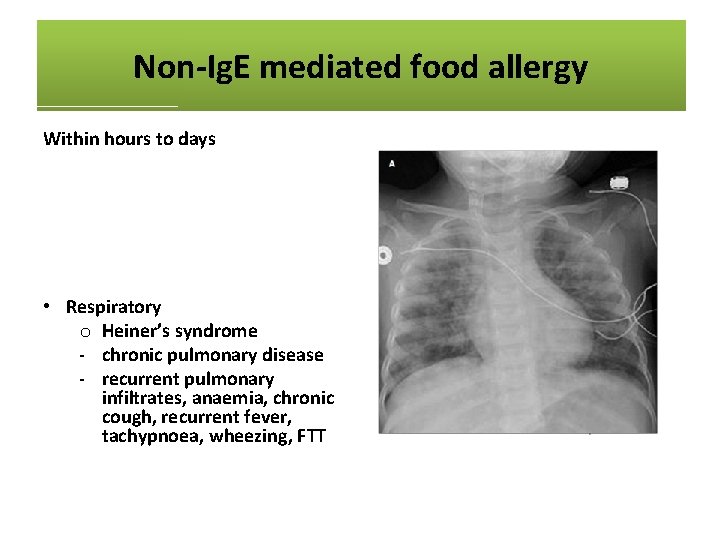
Non-Ig. E mediated food allergy Within hours to days • Skin o atopic dermatitis o contact dermatitis o dermatitis herpetiformis • Respiratory o Heiner’s syndrome - chronic pulmonary disease - recurrent pulmonary infiltrates, anaemia, chronic cough, recurrent fever, tachypnoea, wheezing, FTT • Gastrointestinal o chronic diarrhoea o iron deficiency anaemia o colic o food refusal and poor growth o gastro-oesophageal reflux disease (GORD) o blood in stool o constipation o enterocolitis / proctocolitis / gastroenteritis o eosinophilic oesophagitis / gastroenteritis

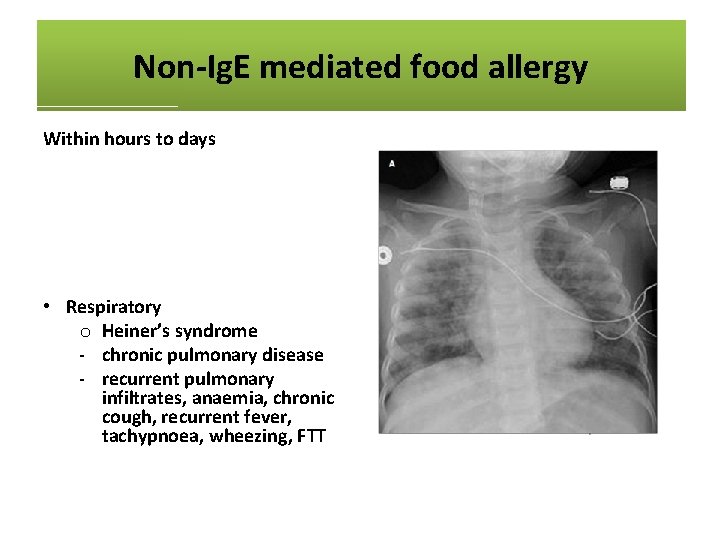
Non-Ig. E mediated food allergy Within hours to days • Skin o atopic dermatitis o contact dermatitis o dermatitis herpetiformis • Respiratory o Heiner’s syndrome - chronic pulmonary disease - recurrent pulmonary infiltrates, anaemia, chronic cough, recurrent fever, tachypnoea, wheezing, FTT • Gastrointestinal o chronic diarrhoea o iron deficiency anaemia o colic o food refusal and poor growth o gastro-oesophageal reflux disease (GORD) o blood in stool o constipation o enterocolitis / proctocolitis / gastroenteritis o eosinophilic oesophagitis / gastroenteritis
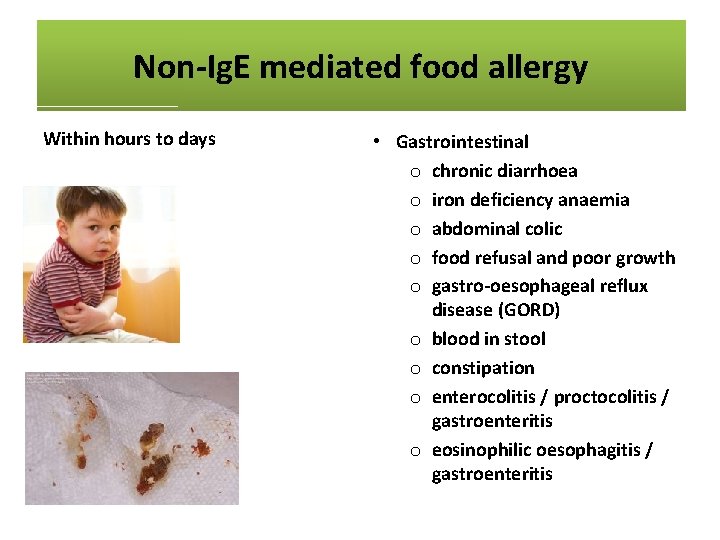
Non-Ig. E mediated food allergy Within hours to days • Skin o atopic dermatitis o contact dermatitis o dermatitis herpetiformis • Respiratory o Heiner’s syndrome - chronic pulmonary disease - recurrent pulmonary infiltrates, anaemia, chronic cough, recurrent fever, tachypnoea, wheezing, FTT • Gastrointestinal o chronic diarrhoea o iron deficiency anaemia o abdominal colic o food refusal and poor growth o gastro-oesophageal reflux disease (GORD) o blood in stool o constipation o enterocolitis / proctocolitis / gastroenteritis o eosinophilic oesophagitis / gastroenteritis

Eczema
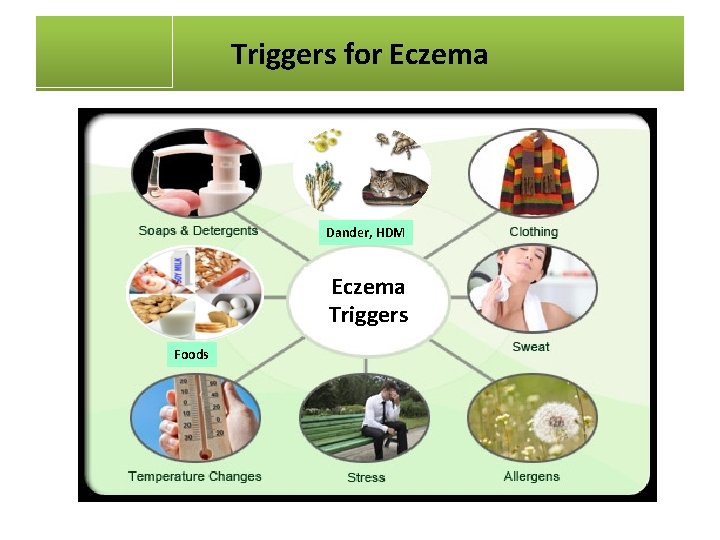
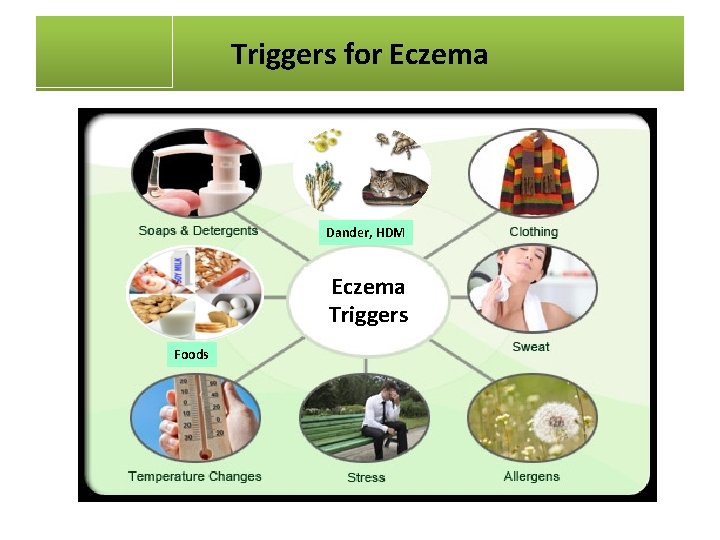
Triggers for Eczema Dander, HDM Eczema Triggers Foods
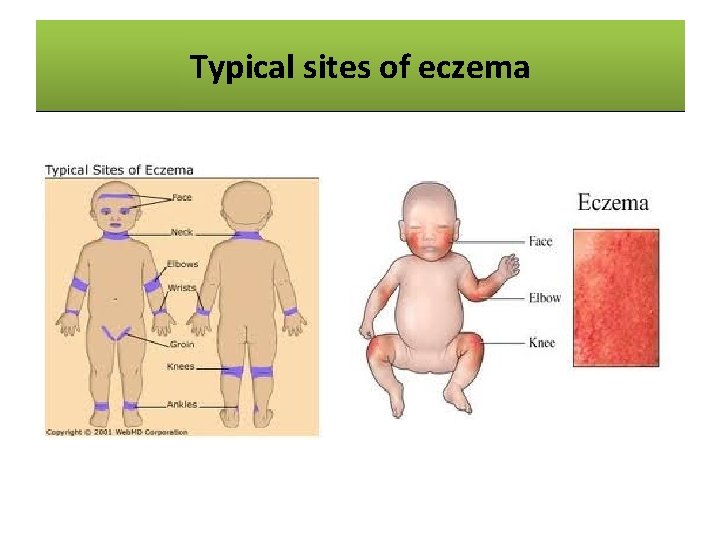
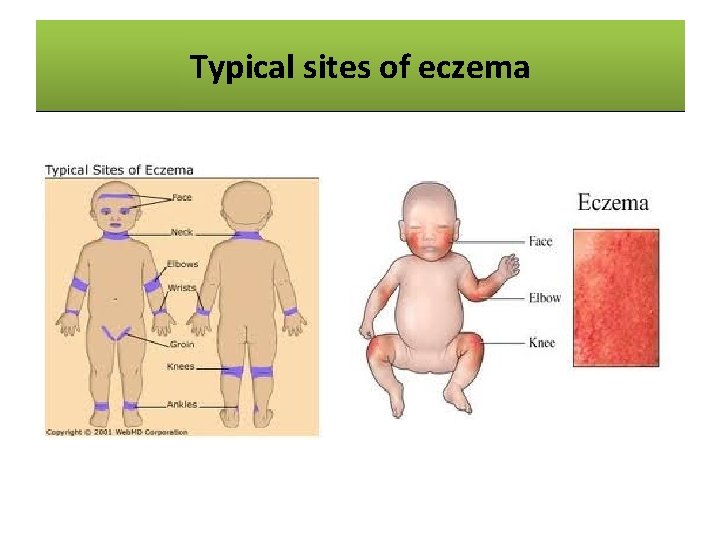
Typical sites eczema Common Sitesofof Eczema
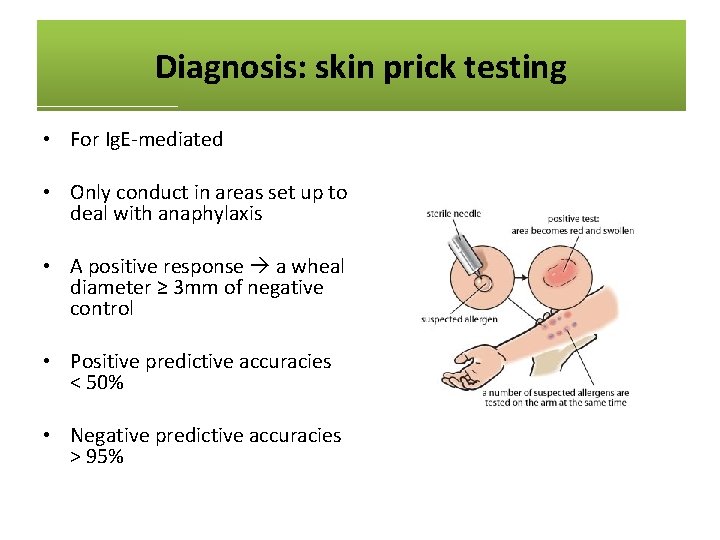
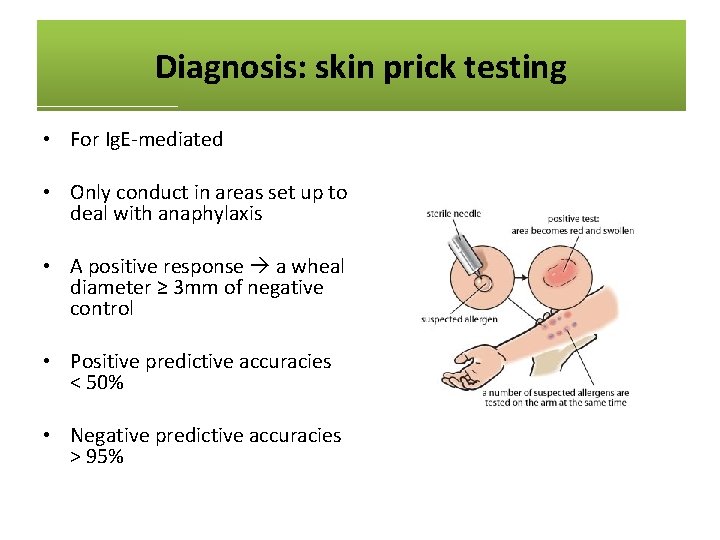
Diagnosis: skin prick testing • For Ig. E-mediated • Only conduct in areas set up to deal with anaphylaxis • A positive response a wheal diameter ≥ 3 mm of negative control • Positive predictive accuracies < 50% • Negative predictive accuracies > 95%

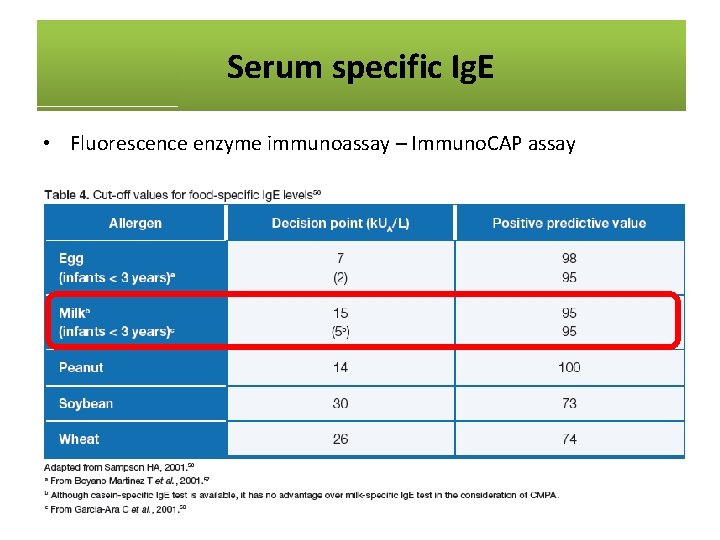
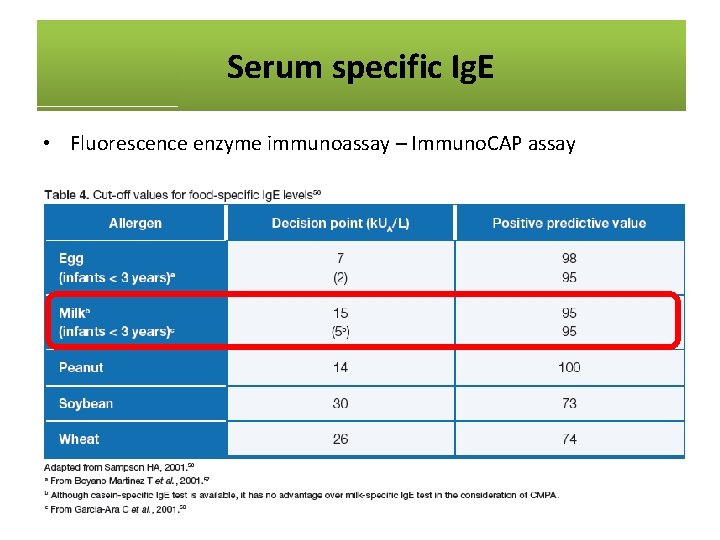
Serum specific Ig. E • Fluorescence enzyme immunoassay – Immuno. CAP assay
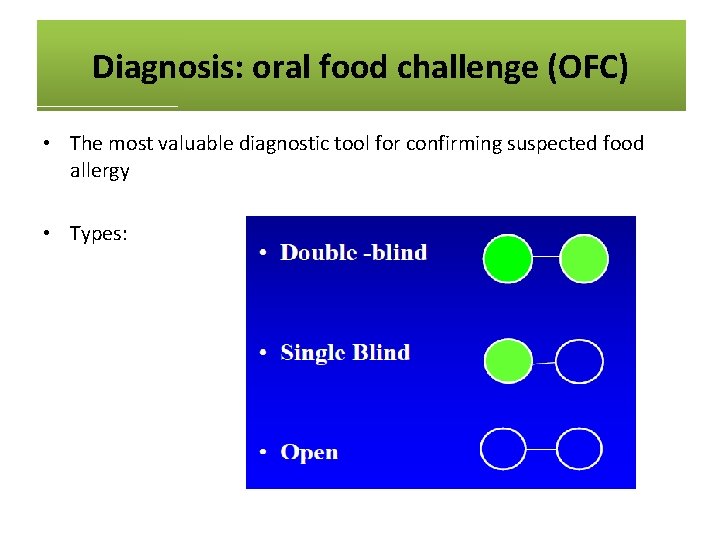
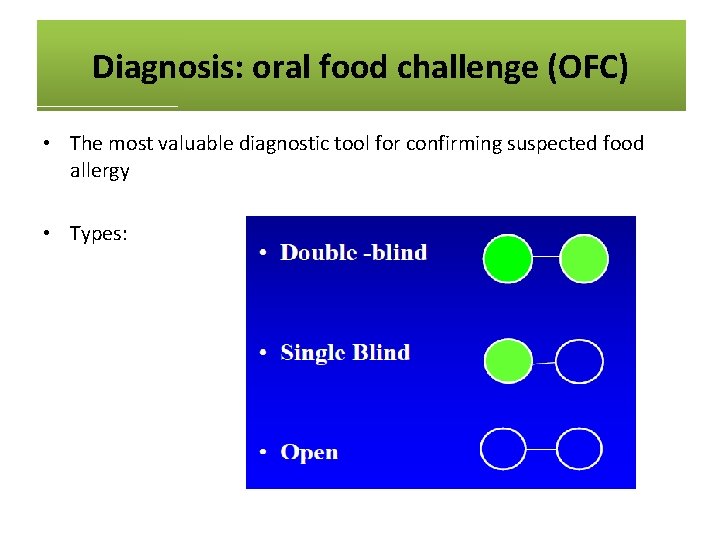
Diagnosis: oral food challenge (OFC) • The most valuable diagnostic tool for confirming suspected food allergy • Types:

Oral milk challenge
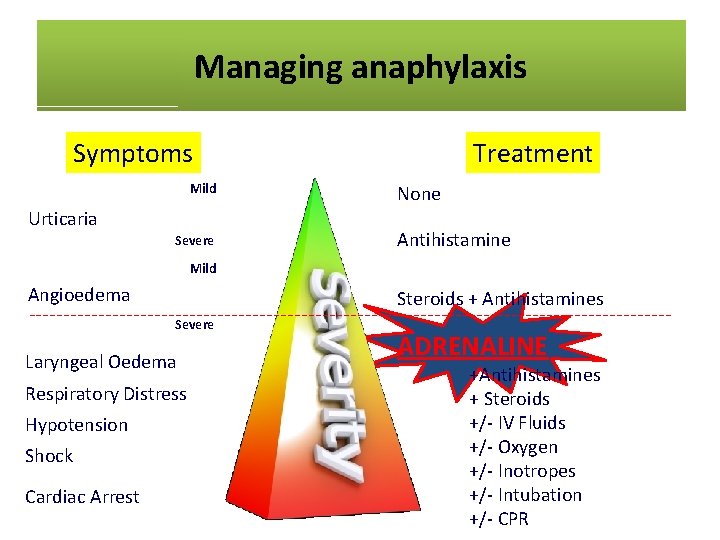
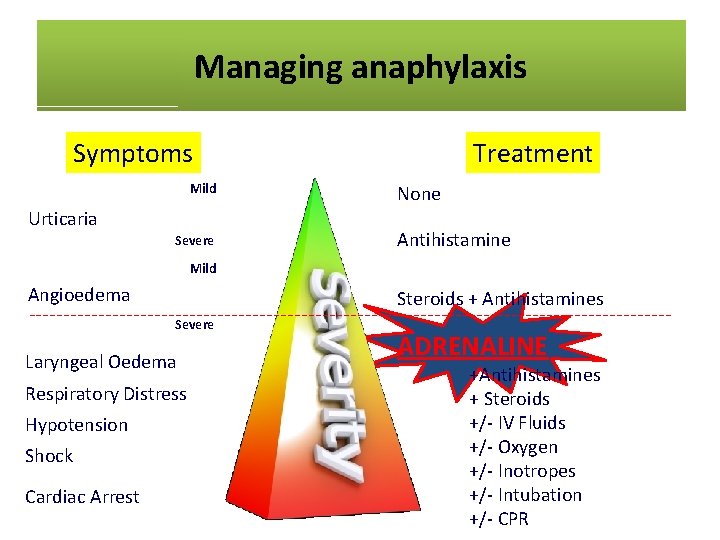
Managing anaphylaxis Symptoms Mild Urticaria Severe Treatment None Antihistamine Mild Angioedema Steroids + Antihistamines Severe Laryngeal Oedema Respiratory Distress Hypotension Shock Cardiac Arrest ADRENALINE +Antihistamines + Steroids +/- IV Fluids +/- Oxygen +/- Inotropes +/- Intubation +/- CPR
Management of food allergy • Dietary elimination and avoidance of protein allergen regardless of the clinical type – oral, inhalant or contact route • Nutritionally safe and balanced diet • Education • Pharmacotherapy • Immunotherapy (future)
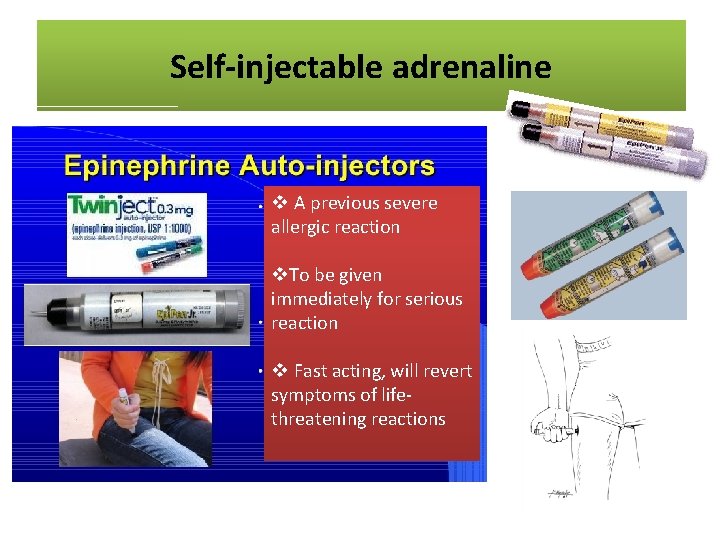
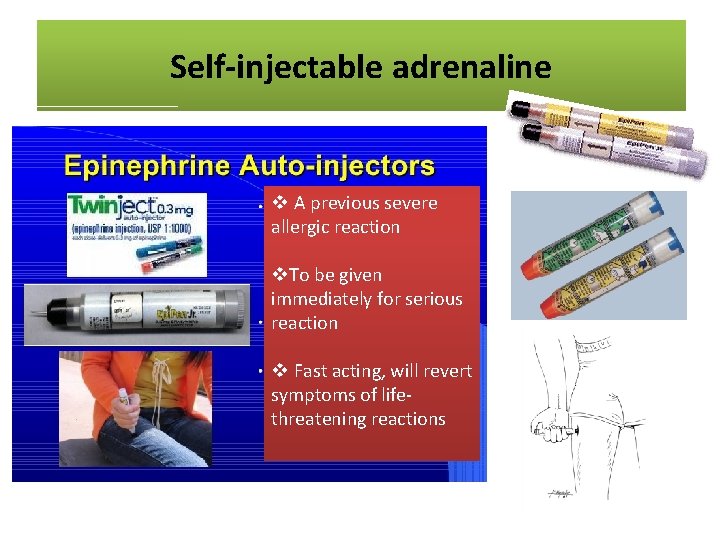
Self-injectableare adrenaline Medications Crucial v A previous severe allergic reaction v. To be given immediately for serious reaction v Fast acting, will revert symptoms of lifethreatening reactions
Eczema. Treatment treatment Eczema The goals are: • To control or prevent itching • To reduce or prevent inflammation • To prevent worsening of the condition • To clear secondary infection • To keep the skin well hydrated

Thank You
 Penicillin allergy cme
Penicillin allergy cme Latex allergy rash pictures
Latex allergy rash pictures What is breast tenderness in pregnancy
What is breast tenderness in pregnancy Brigance 5 year-old data sheet
Brigance 5 year-old data sheet Toddler dönemi nedir
Toddler dönemi nedir Baby fever chart
Baby fever chart Banajee list of toddler vocabulary
Banajee list of toddler vocabulary Toddler fracture
Toddler fracture Child observation samples
Child observation samples Antibiotics for uti in toddler
Antibiotics for uti in toddler Infant/toddler sensory profile score sheet
Infant/toddler sensory profile score sheet The webinar will begin shortly
The webinar will begin shortly Among the most common meters
Among the most common meters Forward contract definition
Forward contract definition Cme fec
Cme fec Phosrenal
Phosrenal Cme semi centralizada
Cme semi centralizada Lente intensificadora de imagem para cme
Lente intensificadora de imagem para cme Continuing medical education
Continuing medical education Nccpa self assessment cme
Nccpa self assessment cme Cme 2012
Cme 2012 Pedialink cme
Pedialink cme Cme tracking tool
Cme tracking tool Cbot market profile handbook pdf
Cbot market profile handbook pdf Www nyp org nursing news cme
Www nyp org nursing news cme Cme invite template
Cme invite template Cardiovillage free cme
Cardiovillage free cme Cmetask review
Cmetask review Cme weather derivatives
Cme weather derivatives Emory cme
Emory cme Allergic crease adalah
Allergic crease adalah Hibiclense
Hibiclense Keva allergy care
Keva allergy care Rhinitis allergy
Rhinitis allergy Allergy
Allergy Fruit latex allergy
Fruit latex allergy American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Contrast allergy premedication protocol acr
Contrast allergy premedication protocol acr Allergic rhinitis treatment guidelines
Allergic rhinitis treatment guidelines Latex fruit allergy
Latex fruit allergy Food allergy testing auckland
Food allergy testing auckland Allergy board review course
Allergy board review course Icd 10 ild
Icd 10 ild Macaulay allergy
Macaulay allergy Allergy asthma immunol res impact factor
Allergy asthma immunol res impact factor Latex allergy
Latex allergy Allergy
Allergy Hptv
Hptv Sfbb allergen chart
Sfbb allergen chart