Clinical pharmacology A N S PART II Cholinomimetic





- Slides: 71
Clinical pharmacology A N S PART II
Cholinomimetic drugs. .
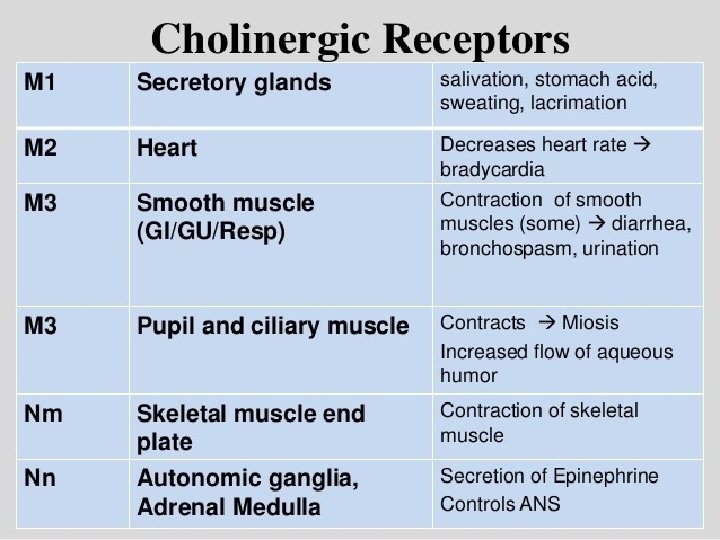
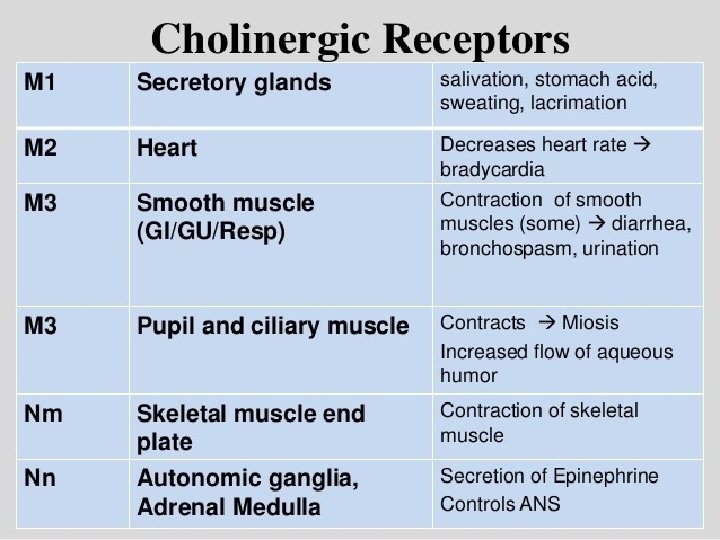
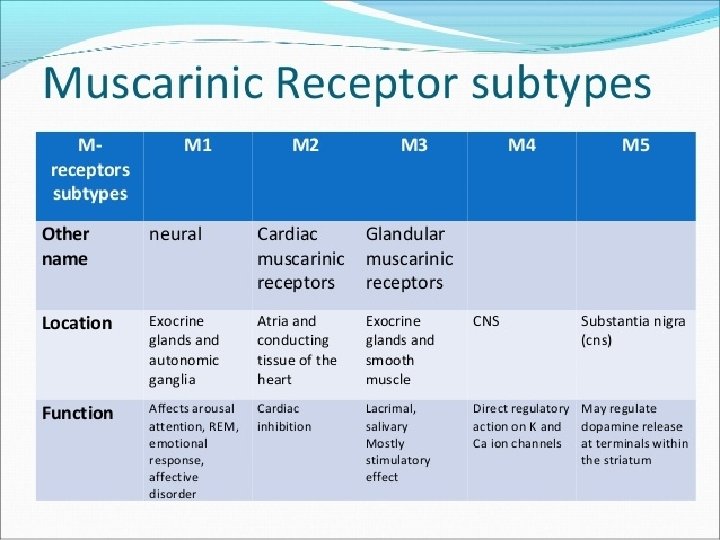
Cholinergic receptors.
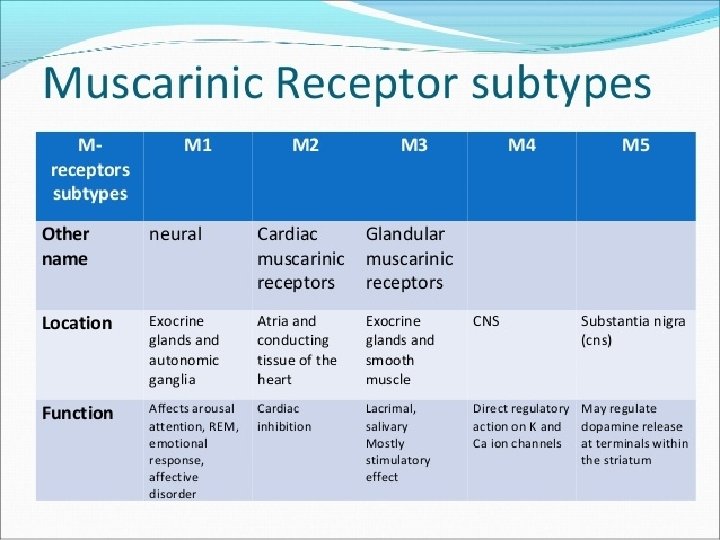
Cholinergic receptors.
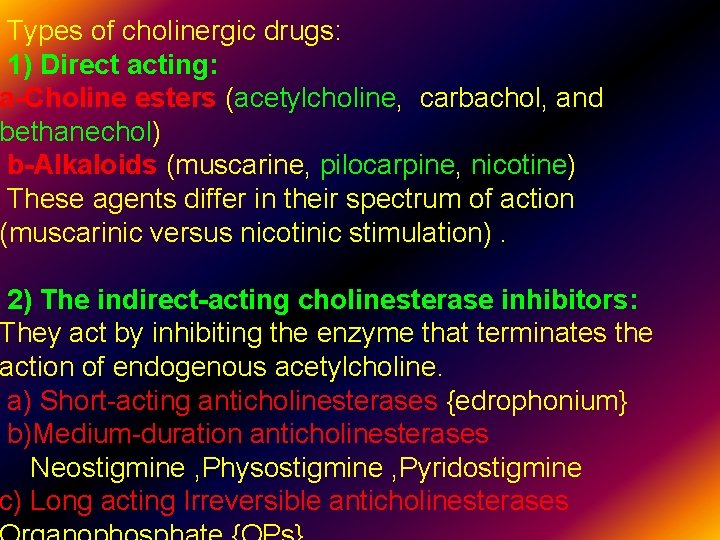
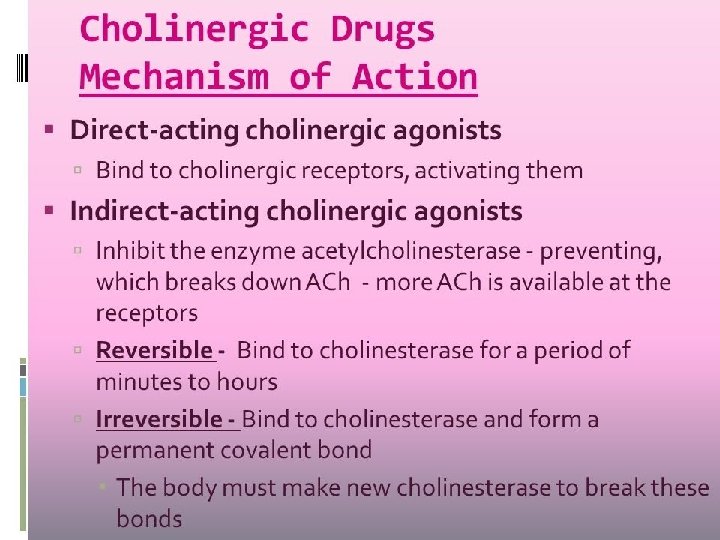
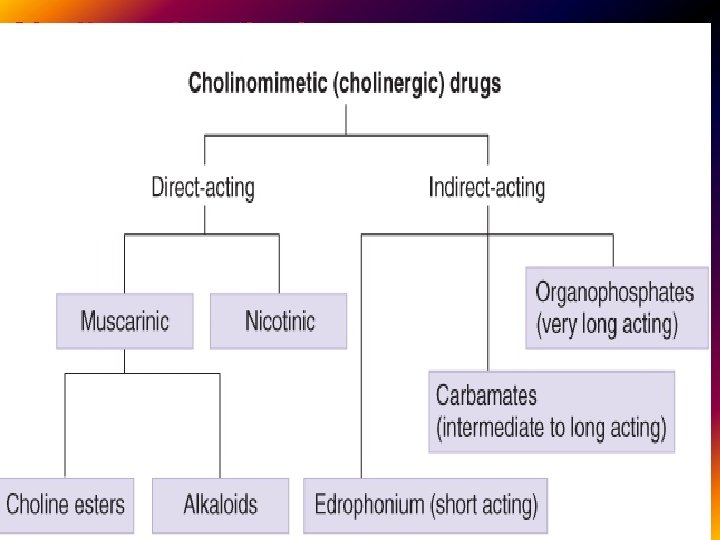
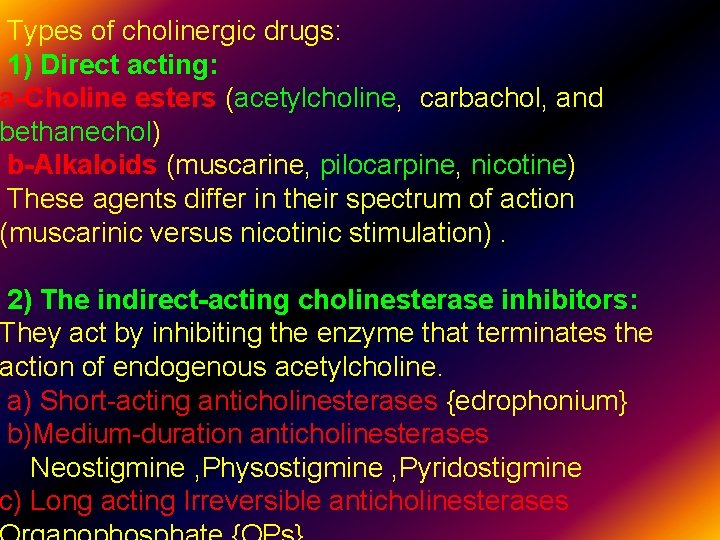
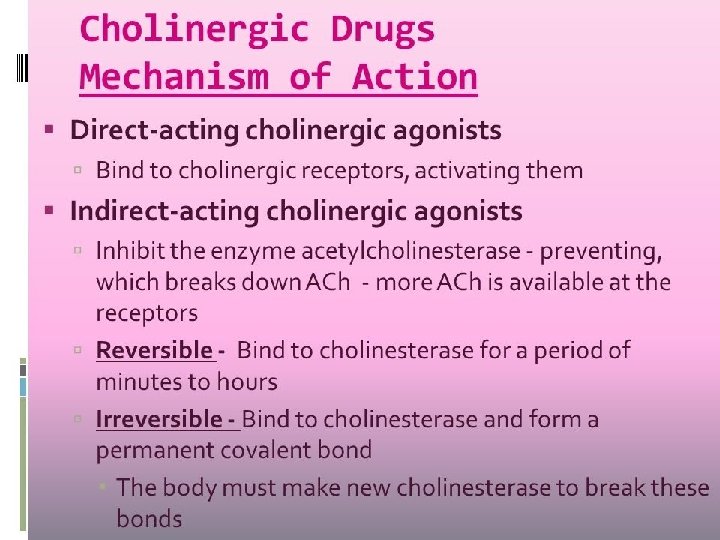
Types of cholinergic drugs: 1) Direct acting: a-Choline esters (acetylcholine, carbachol, and bethanechol) b-Alkaloids (muscarine, pilocarpine, nicotine) These agents differ in their spectrum of action (muscarinic versus nicotinic stimulation). 2) The indirect-acting cholinesterase inhibitors: They act by inhibiting the enzyme that terminates the action of endogenous acetylcholine. a) Short-acting anticholinesterases {edrophonium} b)Medium-duration anticholinesterases Neostigmine , Physostigmine , Pyridostigmine c) Long acting Irreversible anticholinesterases
Types of cholinergic drugs: 1) Direct acting: a-Choline esters (acetylcholine, carbachol, and bethanechol) It is non-selective .
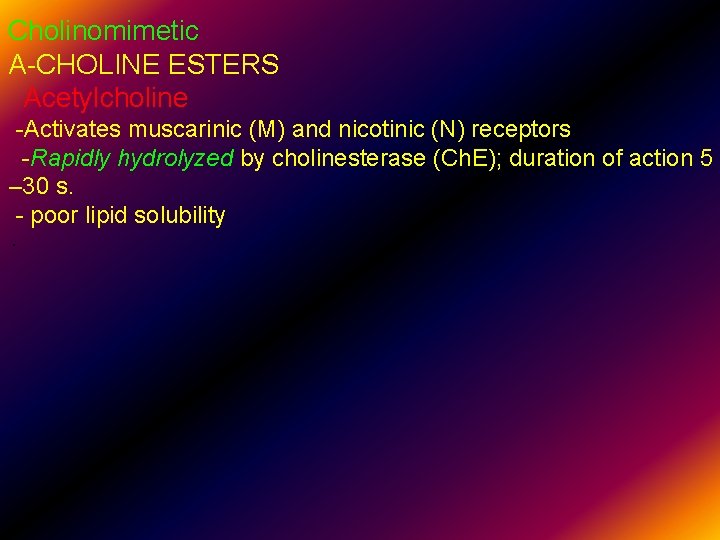
Cholinomimetic A-CHOLINE ESTERS Acetylcholine -Activates muscarinic (M) and nicotinic (N) receptors -Rapidly hydrolyzed by cholinesterase (Ch. E); duration of action 5 – 30 s. - poor lipid solubility.

Applications Drugs acting non – selectively Bethanechol Activate just M-R Uses : 1)Bladder and bowel atony, for example, after surgery or spinal cord injury or diabetic neuropathy of the bladder, or a side effect of anticholinergics 2) dry mouth Bethanechol is a powerful cholinergic agent which does not cross the blood - brain barrier (water soluble) Contraindication Use of bethanechol, as well as all other muscarinic receptor agonists, is contraindicated in patients with asthma, coronary
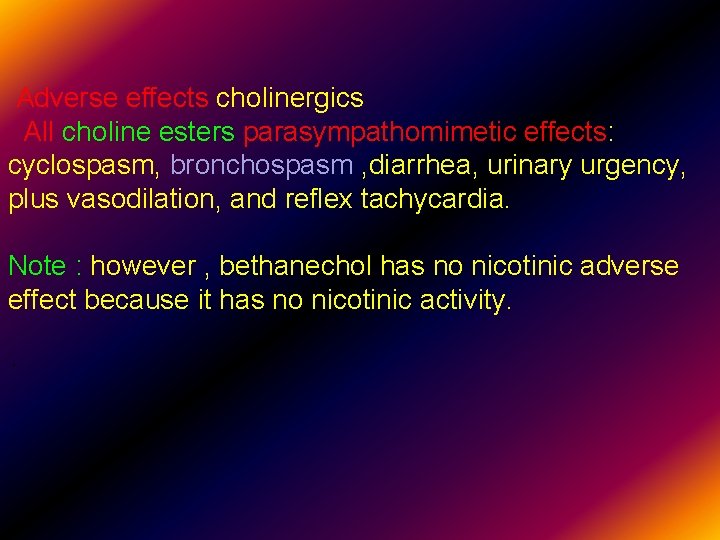
Adverse effects cholinergics All choline esters parasympathomimetic effects: cyclospasm, bronchospasm , diarrhea, urinary urgency, plus vasodilation, and reflex tachycardia. Note : however , bethanechol has no nicotinic adverse effect because it has no nicotinic activity. .
Applications drugs acting Selectively on M 1 -R 1) Citicoline (Somazina ) Citicoline is a water soluble Nootropic that is reported to help improve memory, increase attention span, enhance focus, concentration, and ADHD and Alzheimer’s. . In Alzheimer disease , amyloid formation may decrease the ability of M 1 receptors to transmit signals, leading to decreased cholinergic activity. It falls into the acetylcholine supplement category of Nootropics because this compound can
Cholinomimetic Drugs on M 2 -R There is no drug selectively acting on M 2 -receptors .
However Non selective Cholinomimetic Drugs act on Cardiovascular effects {Vagal stimulation}: M 2 -R These include cardiac slowing and a decrease in cardiac output. The latter action is due mainly to a decreased force of contraction of the atria. Generalized vasodilatation also occurs (a nitric oxidemediated effect), and these two effects combine to produce a sharp fall in arterial pressure. Atria Decrease in contractile force (negative inotropy ; ↓COP). Atrioventricular node : Decrease in conduction velocity (negative dromotropy), Ventricles small decrease in contractile force {Less cholinergic innervation}
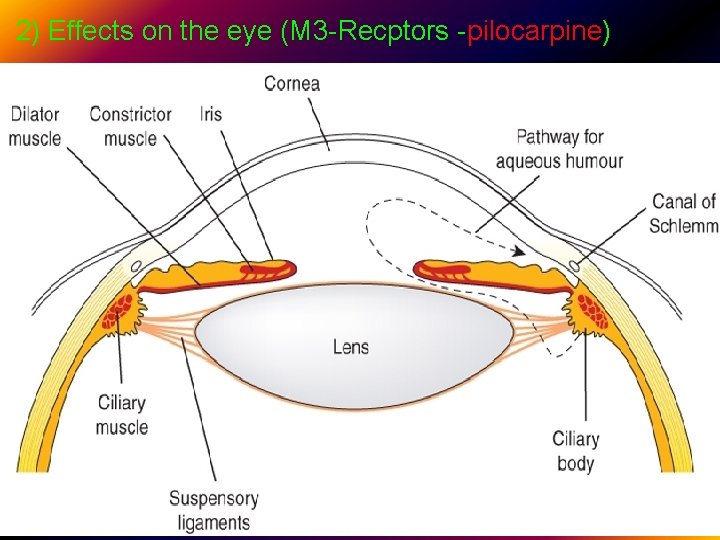
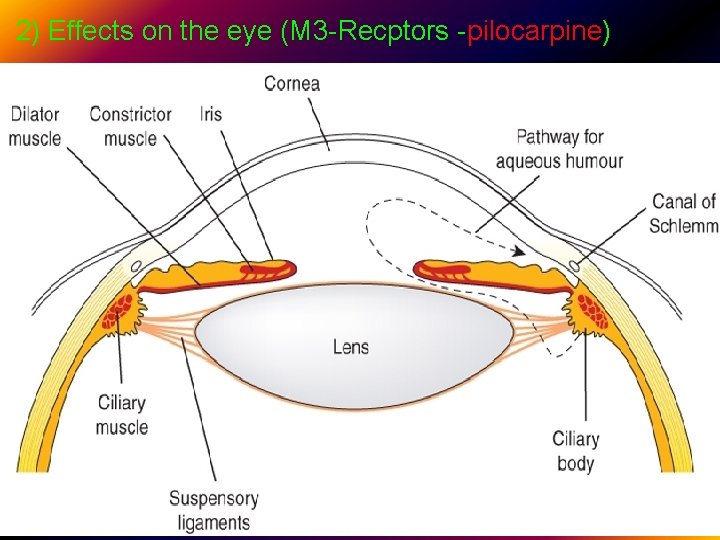
2) Effects on the eye (M 3 -Recptors -pilocarpine). .
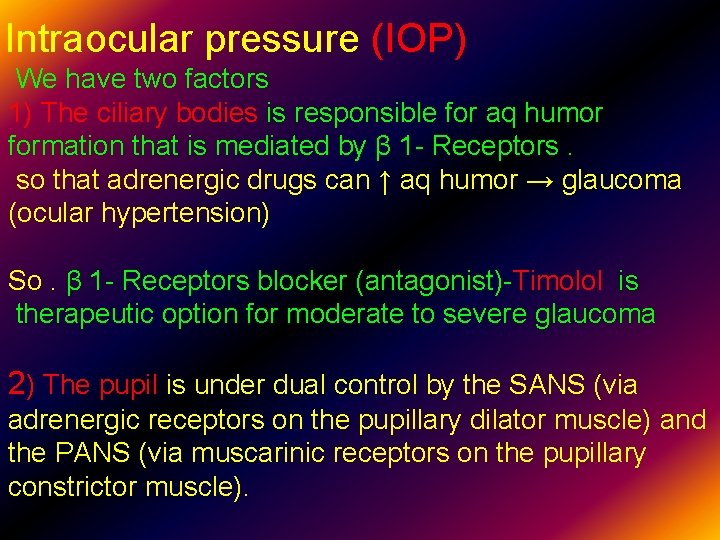
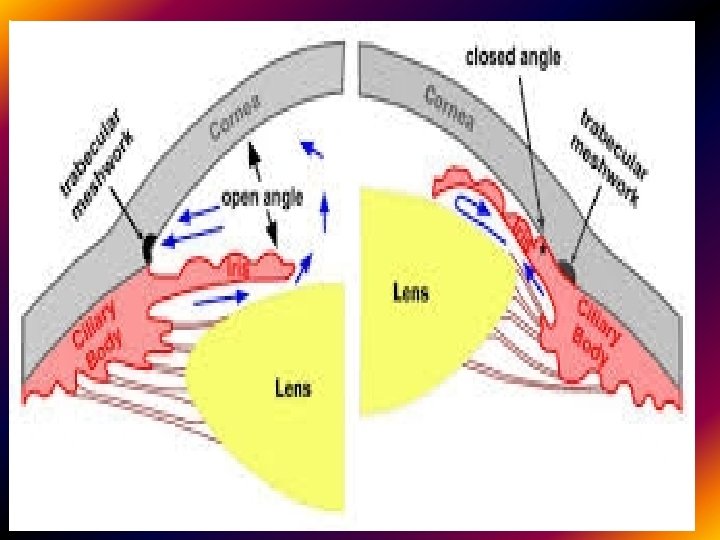
Intraocular pressure (IOP) We have two factors 1) The ciliary bodies is responsible for aq humor formation that is mediated by β 1 - Receptors. so that adrenergic drugs can ↑ aq humor → glaucoma (ocular hypertension) So. β 1 - Receptors blocker (antagonist)-Timolol is therapeutic option for moderate to severe glaucoma 2) The pupil is under dual control by the SANS (via adrenergic receptors on the pupillary dilator muscle) and the PANS (via muscarinic receptors on the pupillary constrictor muscle). .
Activation of the constrictor pupillae by muscarinic agonists M 3 -R (pilocarpine) →↓ folding of the iris tissue → ↑drainage →lowers the IOP Decreasing IOP is therapeutic strategy for mild to moderate glaucoma. .
Accommodation The ciliary muscle, which controls accommodation, is under primary control of muscarinic receptors (M 3 -R) innervated by the PANS, with insignificant contributions from the SANS. Contraction of the ciliary muscle in response to activation of muscarinic receptors {parasympathetic } causes relaxing the tension on the suspensory ligament of the lens, allowing the lens to bulge more and reducing its focal length. This parasympathetic reflex leads to accommodate the eye for near vision. .
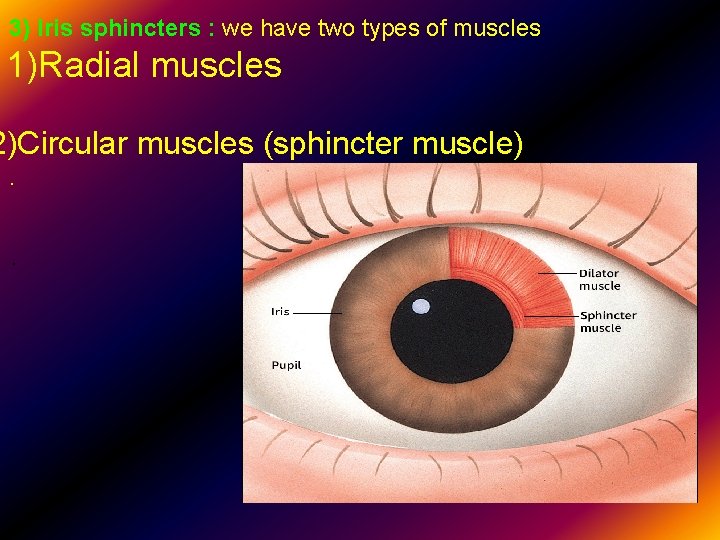
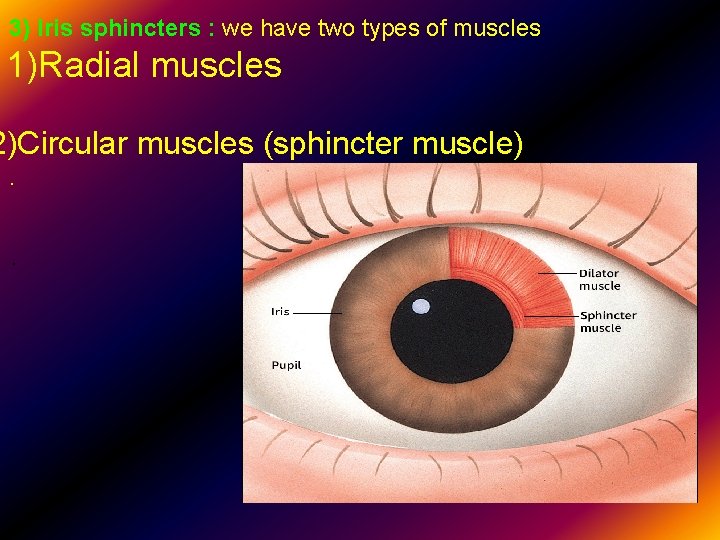
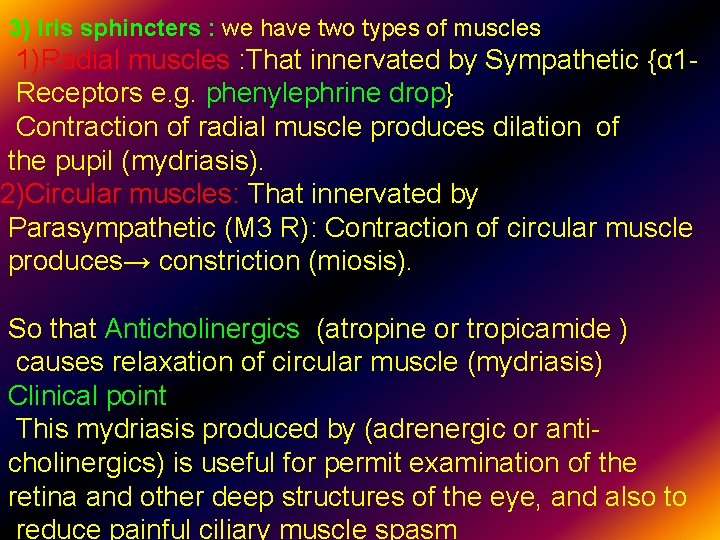
3) Iris sphincters : we have two types of muscles 1)Radial muscles 2)Circular muscles (sphincter muscle) . .
3) Iris sphincters : we have two types of muscles 1)Radial muscles : That innervated by Sympathetic {α 1 Receptors e. g. phenylephrine drop} Contraction of radial muscle produces dilation iof the pupil (mydriasis). 2)Circular muscles: That innervated by Parasympathetic (M 3 R): Contraction of circular muscle produces→ constriction (miosis). So that Anticholinergics (atropine or tropicamide ) causes relaxation of circular muscle (mydriasis) Clinical point This mydriasis produced by (adrenergic or anticholinergics) is useful for permit examination of the retina and other deep structures of the eye, and also to reduce painful ciliary muscle spasm

However , anti-cholinergic is associated with cycloplegia.
Autonomic neuropathy (DM) → mydriasis why? R/ Parasympathetic fibers travel with cranial nerve III, the oculo-motor nerve, to innervate the circular layer of muscle of the eye (sphincter pupillae) will be affected. Damage to this nerve typically cause mydriasis, because the sympathetic supply to the pupil, which causes mydriasis, remains unaffected, and therefore unopposed .
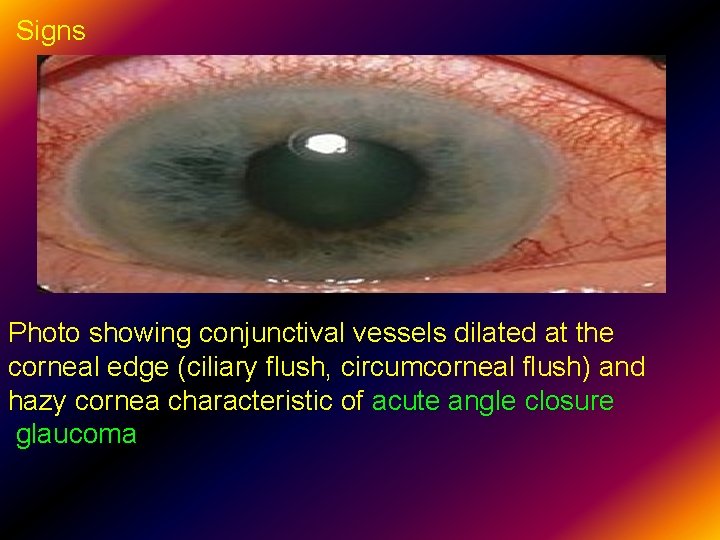
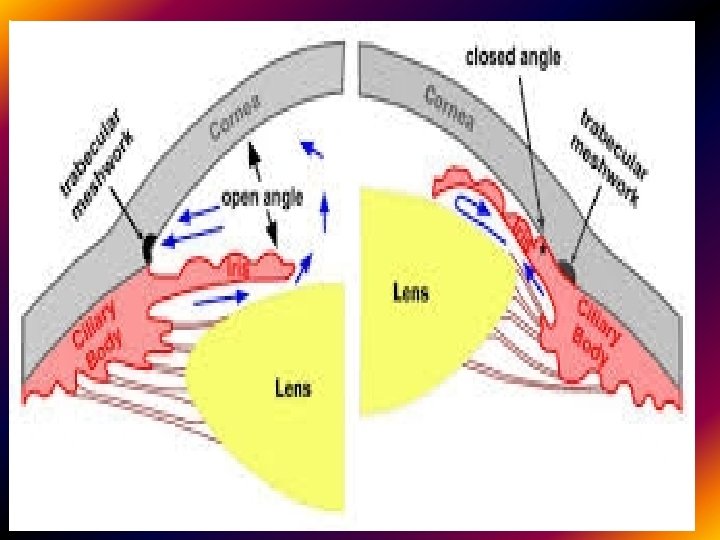
Glaucoma is an ocular disorders characterized by ↑↑ intraocular pressure + optic disc neuropathy. It is associated with increased fluid pressure in the eye (IOP above 21 mm. Hg {Normal 10 -21 mm. Hg} ). Untreated glaucoma can lead to permanent damage of the optic nerve and resultant blindness. Glaucoma can be roughly divided into two main categories, "open-angle" and "closed-angle" (or "angle closure") glaucoma. The angle refers to the area between the iris and cornea, through which fluid must flow to escape via the trabecular meshwork.
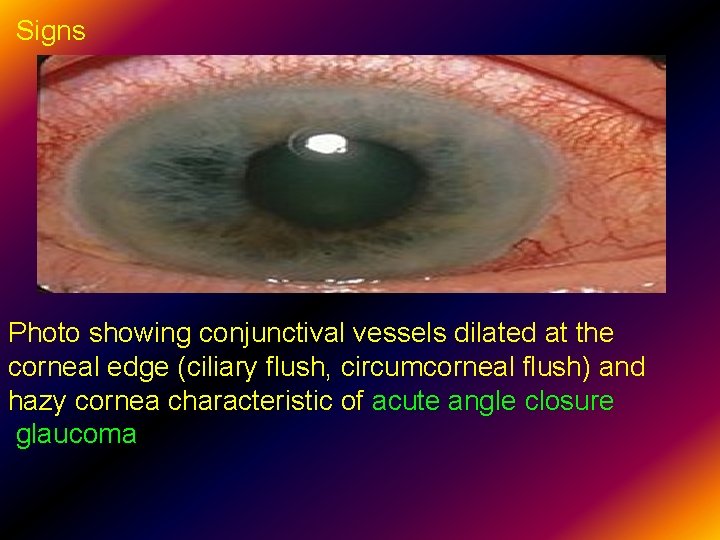
Signs Photo showing conjunctival vessels dilated at the corneal edge (ciliary flush, circumcorneal flush) and hazy cornea characteristic of acute angle closure glaucoma.
Dental considerations Adrenaline in local anesthetics can activate β 1 R in ciliray bodies leading to increase aqueous humor secretion with subsequent increase IOP; So we should be aware to restrict local anesthetics with adrenaline specially with closed angle glaucoma. It is OK if patient with open angle glaucome on treatment .
Applications Drugs acting on M 3 -R agonists 1)Pilocarpine is a drug that acts as a M 3 -receptor agonist that is used to treat glaucoma and Sjögren's syndrome. � • 2) Cevimeline • is a muscarinic agonist that is used for the •
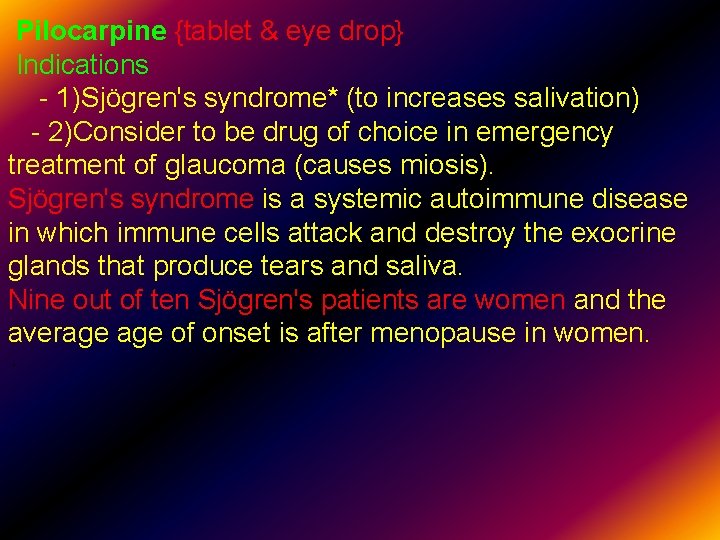
Pilocarpine {tablet & eye drop} Indications - 1)Sjögren's syndrome* (to increases salivation) - 2)Consider to be drug of choice in emergency treatment of glaucoma (causes miosis). Sjögren's syndrome is a systemic autoimmune disease in which immune cells attack and destroy the exocrine glands that produce tears and saliva. Nine out of ten Sjögren's patients are women and the average of onset is after menopause in women. .
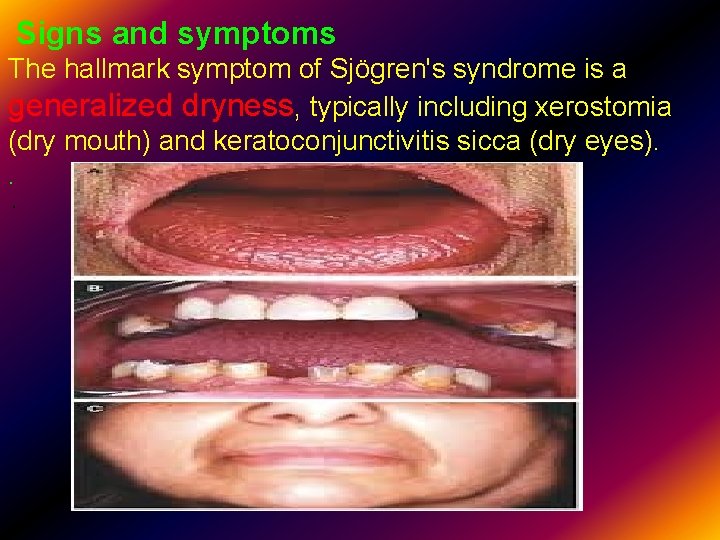
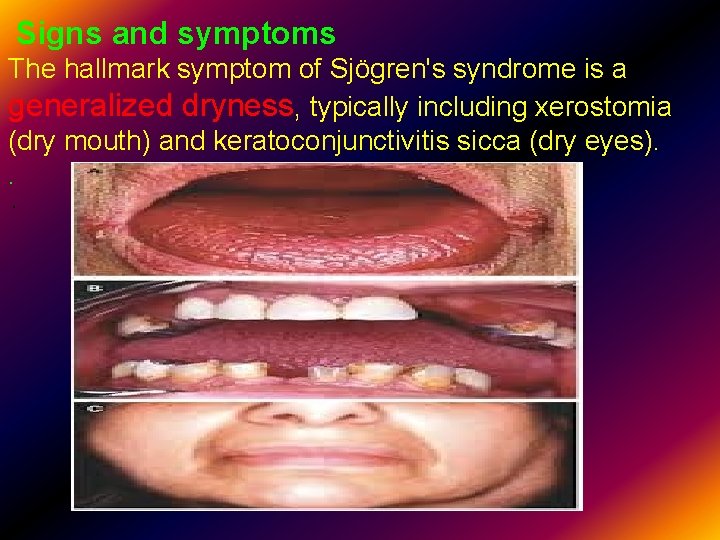
Signs and symptoms The hallmark symptom of Sjögren's syndrome is a generalized dryness, typically including xerostomia (dry mouth) and keratoconjunctivitis sicca (dry eyes). . .

Treatment There is no specific treatment to permanently restore gland secretion. Moisture replacement therapies such as artificial tears may stop the symptoms of dry eyes. Drugs are also available that help to stimulate salivary flow, such as pilocarpine drops and tab. For individuals with severe complications, corticosteroids (prednisolone 5 mg tab 2 tab TID) or immunosuppressant (azathioprine 50 mg once daily ) may be used. Also CMC oral gel 2% can be used.
Dental care Preventive dental treatment is also necessary , as the lack of saliva associated with xerostomia creates an ideal environment for the proliferation of bacteria that cause dental caries (cavities). Treatments include topical fluoride application to strengthen tooth enamel and frequent teeth cleanings Pharmacokinetics of Pilocarpine Oral, IM , Good lipid solubility, duration of action 30 min to 2 h . .
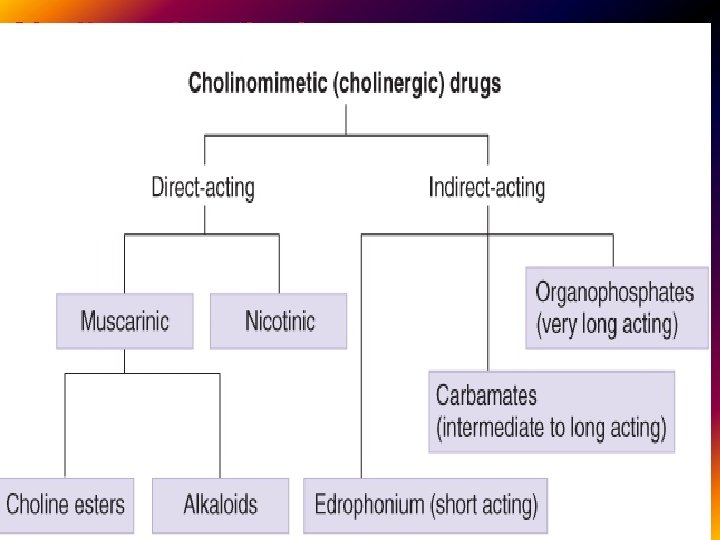
The Indirect-acting Cholinesterase Inhibitors They act by inhibiting the enzyme that terminates the action of endogenous acetylcholine 1)Reversible anticholinesterases Physostigmine -Action: Inhibitor of cholinesterase; amplifier of endogenously released Ach on M-receptors -Indications: -Reversal of severe atropine poisoning (IV) -occasionally used in acute glaucoma (topical). -Used in intestinal atony (increases their motility)Adverse effect: Generalized cholinergic stimulation plus CNS effects: seizures.
Neostigmine Action: Inhibitor of cholinesterase; amplifier of endogenously released Ach plus small direct nicotinic agonist action -Reversal of NM block caused by tubocurarine. - treatment of myasthenia Gravis. -Duration: 2– 4 h It differ from Physostigmine in 1) More polar(does not inter CNS) but orally active 2)Has greater effect on skeletal muscles {Why ? ? } Adverse effect: Generalized cholinergic stimulation.
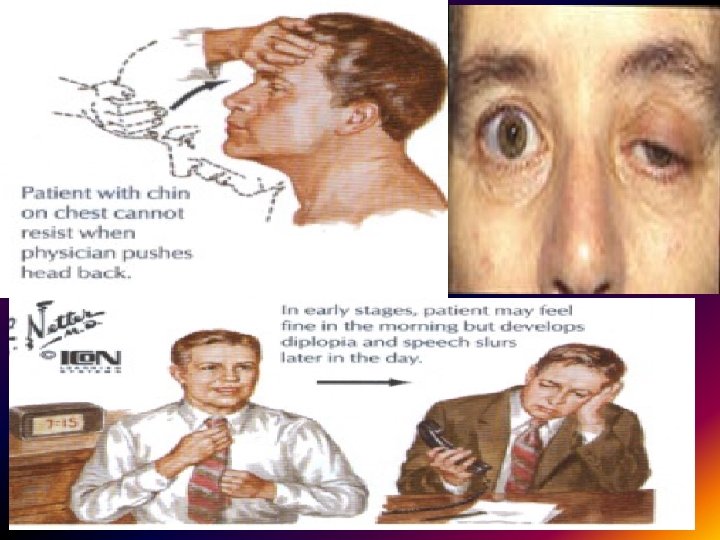
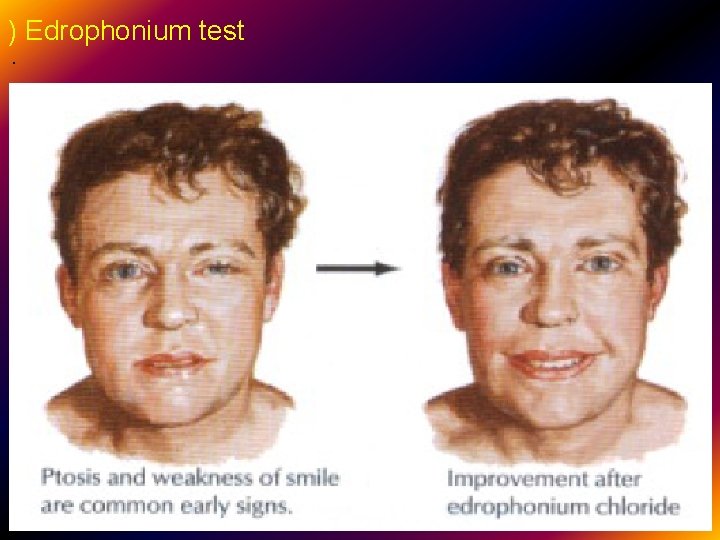
Short-acting anticholinesterases edrophonium The action of edrophonium is similar to Physostigmine, except that it is more rapidly absorbed and has short duration of action (10 -20 min) Used in diagnosis of myasthenia gravis {Tensilon test} *(I. V injection lead to rapid increase in muscle strength). Myasthenia gravis is an autoimmune neuromuscular disease ). Muscle weakness is caused by circulating antibodies that block acetylcholine receptors at the postsynaptic neuromuscular junction {skeletal m}, inhibiting the excitatory effects of acetylcholine on nicotinic receptors at neuromuscular junctions. .
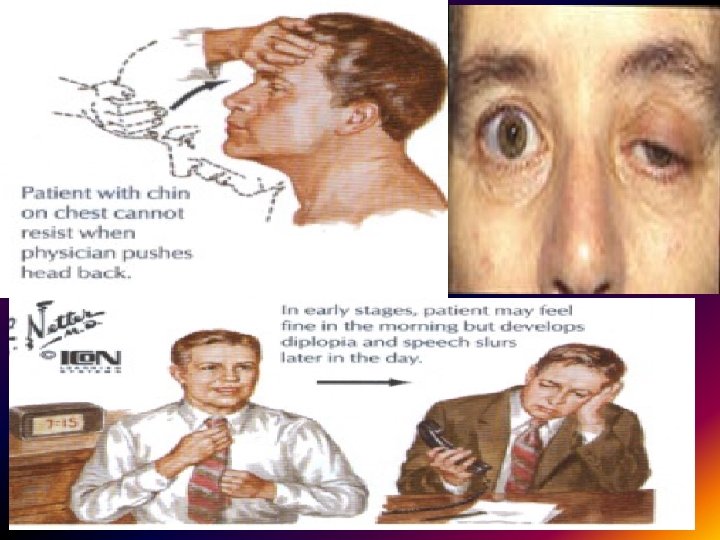
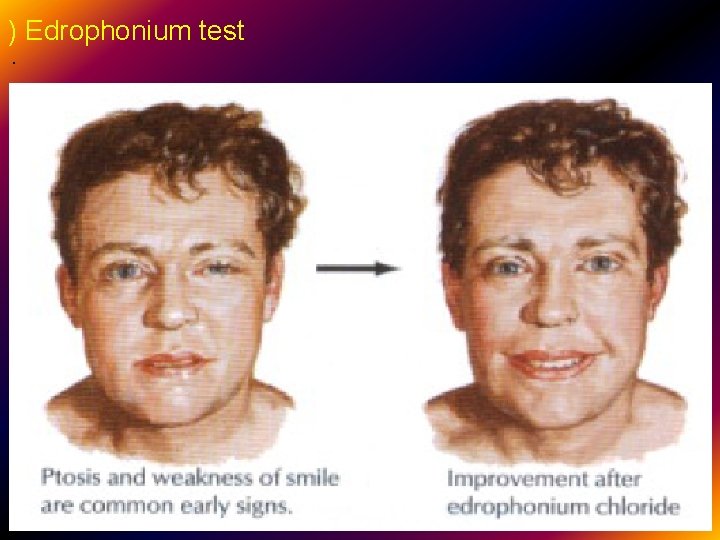
) Edrophonium test .
Medication 1) Acetylcholinesterase inhibitors: Neostigmine and pyridostigmine can improve muscle function by slowing the natural enzyme cholinesterase that degrades acetylcholine in the motor end plate. 2)Immunosuppressive drugs: prednisone, cyclosporin, mycophenolate and azathioprine may be used. 3)In some patients, the thymus gland is removed; very severely affected patients may benefit from administration of immunoglobulins and from plasmapheresis. .
Facial and masticatory muscles may be involved and complicate dental care and treatment. specially if you are anticipating significant oral surgery (wisdom tooth extractions, multiple tooth extractions . Dental considerations: These include 1) Identifying and managing myasthenic weakness or crisis. 2) Avoiding the potential of harmful drug interactions, monitoring oral side effects of drugs and therapies used to treat MG, and modifying dental treatment to accommodate altered muscle strength. 3) Morning dental work will minimize fatigue and take advantage of the typically greater muscle strength during the morning hours.
4) Best scheduled approximately 1 to 2 hours (4 following oral anticholinesterases medication ( Neostigmine or pyridostigmine ; Mestinon® ) so as to benefit from maximum therapeutic effect and decrease the risk of myasthenic weakness or crisis. 5) Dental treatment is usually done in a reclining position. 6) Frequent rest breaks during treatment. 7) Avoid aminoglycoside antibiotics. .
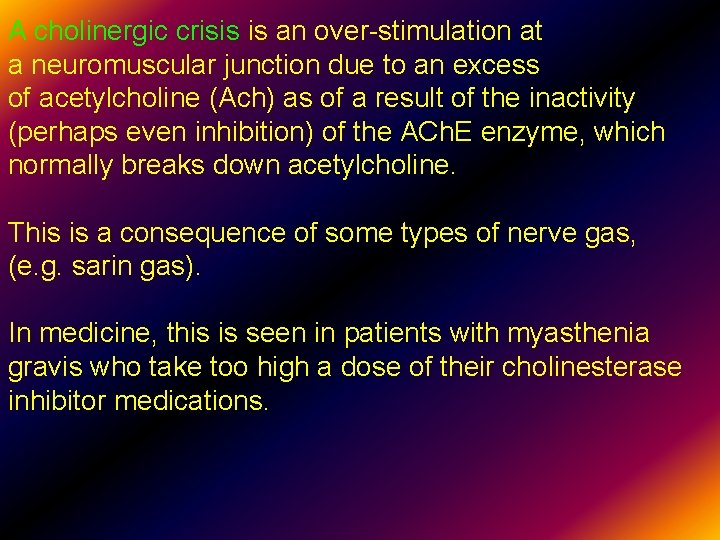
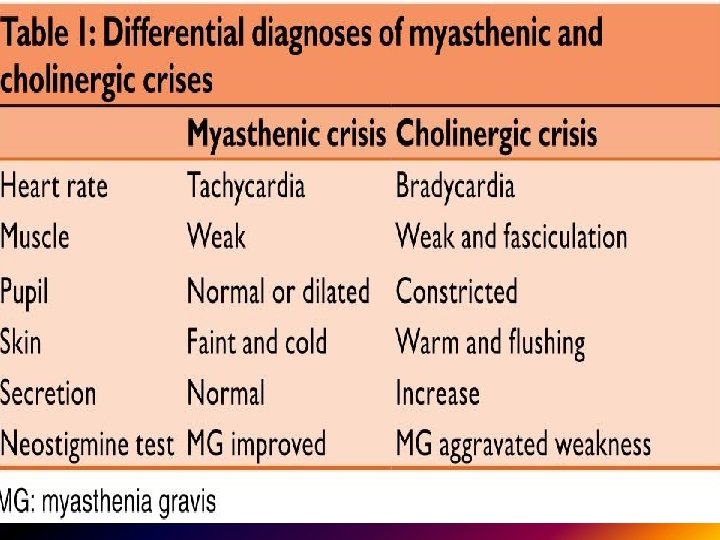
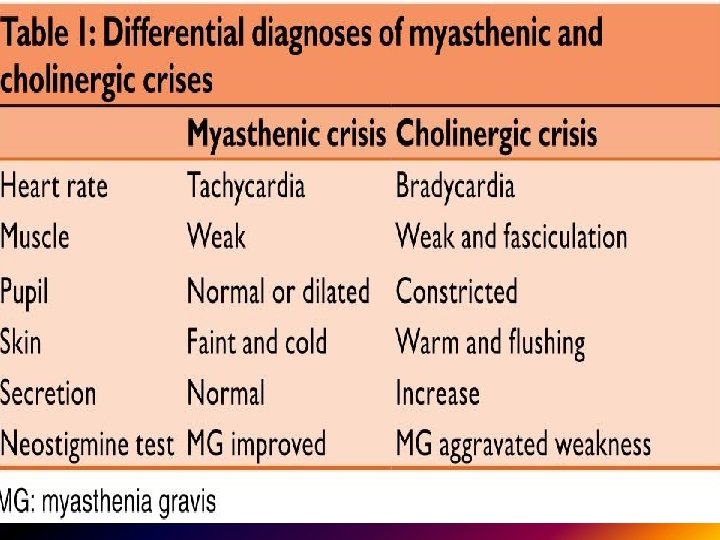
A cholinergic crisis is an over-stimulation at a neuromuscular junction due to an excess of acetylcholine (Ach) as of a result of the inactivity (perhaps even inhibition) of the ACh. E enzyme, which normally breaks down acetylcholine. This is a consequence of some types of nerve gas, (e. g. sarin gas). In medicine, this is seen in patients with myasthenia gravis who take too high a dose of their cholinesterase inhibitor medications. .
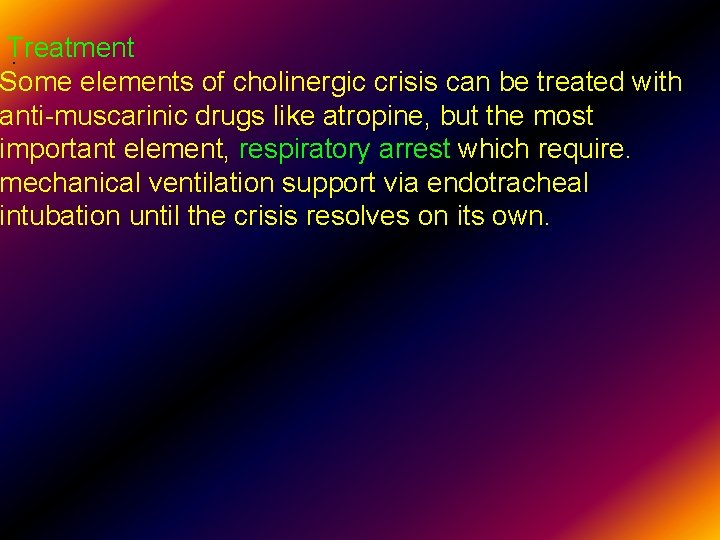
Treatment. Some elements of cholinergic crisis can be treated with anti-muscarinic drugs like atropine, but the most important element, respiratory arrest which require. mechanical ventilation support via endotracheal intubation until the crisis resolves on its own.
. Home work Differentiate between myasthenia gravis and Lambert – Eaton syndrome? And explain the effect of aminoglycosides on these diseases. .
2) Irreversible anticholinesterases Organophosphates are long-acting drugs; they form an extremely stable phosphate complex with the enzyme. Effects By inhibiting cholinesterase, these agents cause an increase in the concentration, half-life, and actions of acetylcholine in synapses where acetylcholine is released physiologically 1) Parathion Insecticide only 2) Permethrin 2. 5 -5% cream or lotion Scabicide and anti-head lice 3)Malathion (shampoo) Insecticide and scabicide* (topical).
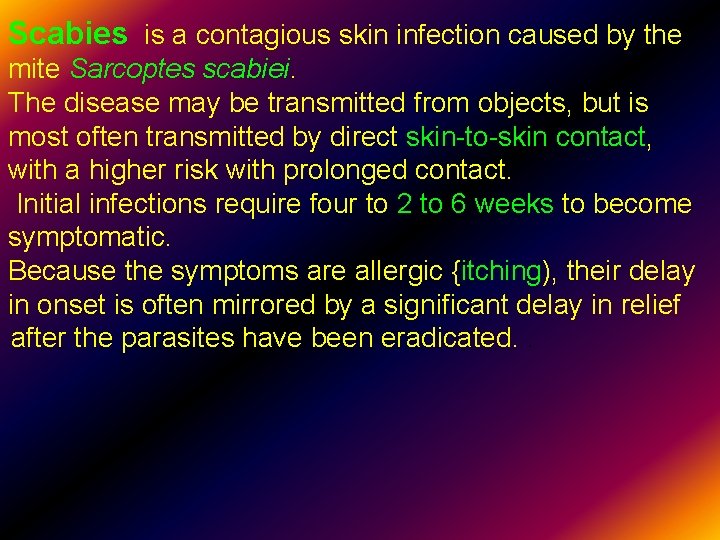
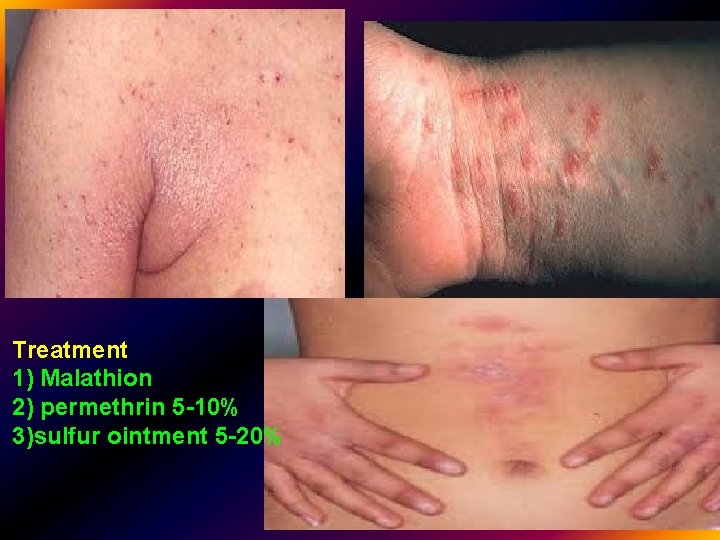
Scabies is a contagious skin infection caused by the mite Sarcoptes scabiei. The disease may be transmitted from objects, but is most often transmitted by direct skin-to-skin contact, with a higher risk with prolonged contact. Initial infections require four to 2 to 6 weeks to become symptomatic. Because the symptoms are allergic {itching), their delay in onset is often mirrored by a significant delay in relief after the parasites have been eradicated. .
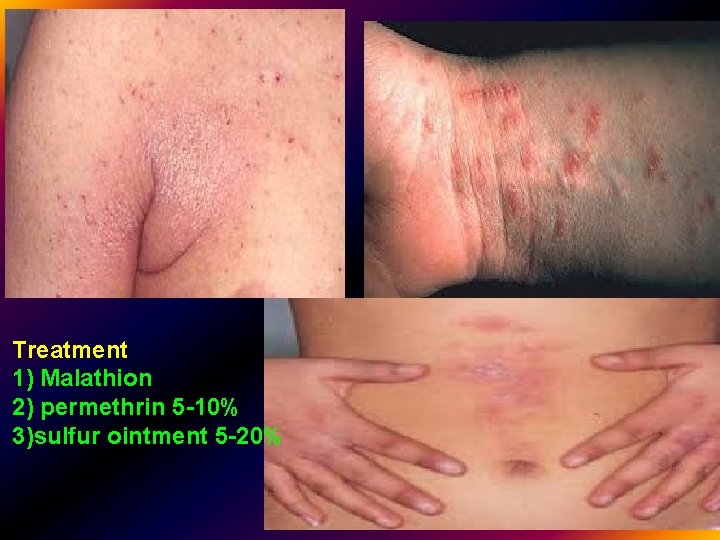
). . Treatment 1) Malathion 2) permethrin 5 -10% 3)sulfur ointment 5 -20%
3)Donepezil MOA : Cholinesterase inhibition plus variable other poorly understood effects used in Alzheimer's disease* Lipid soluble→ enter CNS. S. E : Nausea, vomiting Alzheimer’s Disease pathology – loss of cholinergic neurons and reduced synthesis of ACh
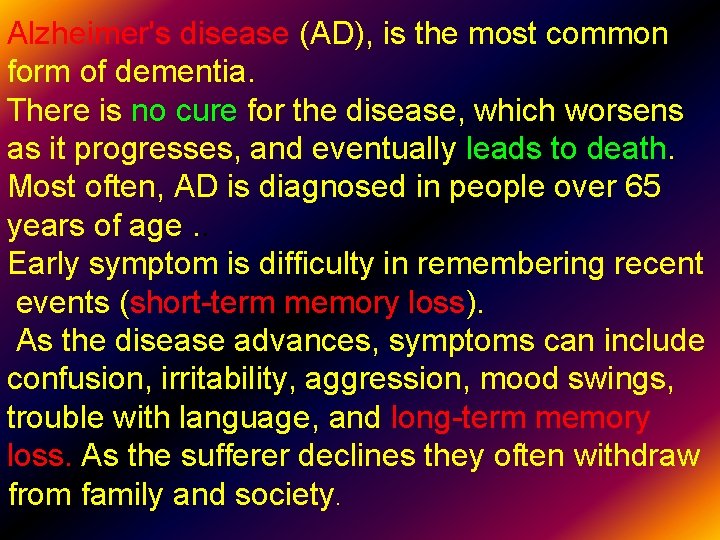
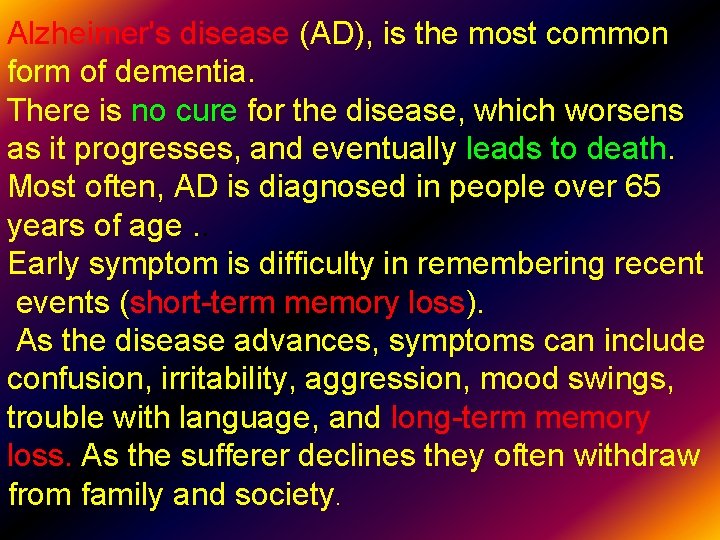
Alzheimer's disease (AD), is the most common form of dementia. There is no cure for the disease, which worsens as it progresses, and eventually leads to death. Most often, AD is diagnosed in people over 65 years of age. . Early symptom is difficulty in remembering recent events (short-term memory loss). As the disease advances, symptoms can include confusion, irritability, aggression, mood swings, trouble with language, and long-term memory loss. As the sufferer declines they often withdraw from family and society.
Anticholinesterases may improve cognitive function and memory in up to 40% of patients HW: Why women have more Alzheimer's disease than men ? . Management Five medications are currently used to treat the cognitive problems of AD: four are acetylcholinesterase inhibitors (tacrine, rivastigmine , and donepezil) and the other (memantine) is an NMDA receptor antagonist.
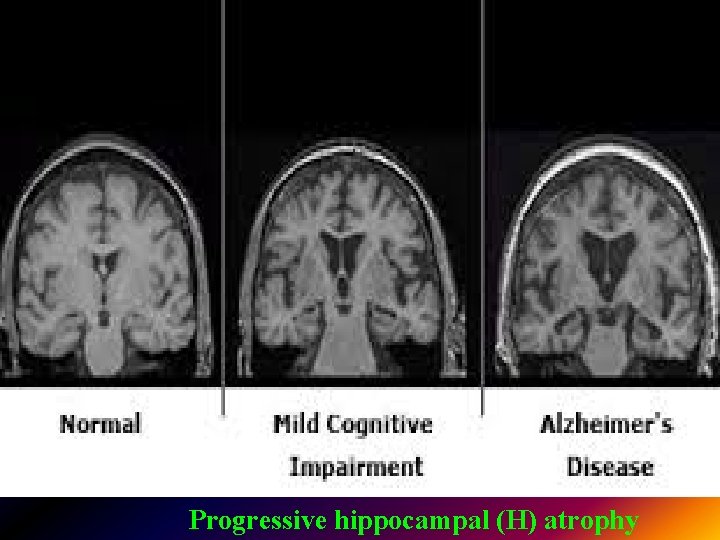
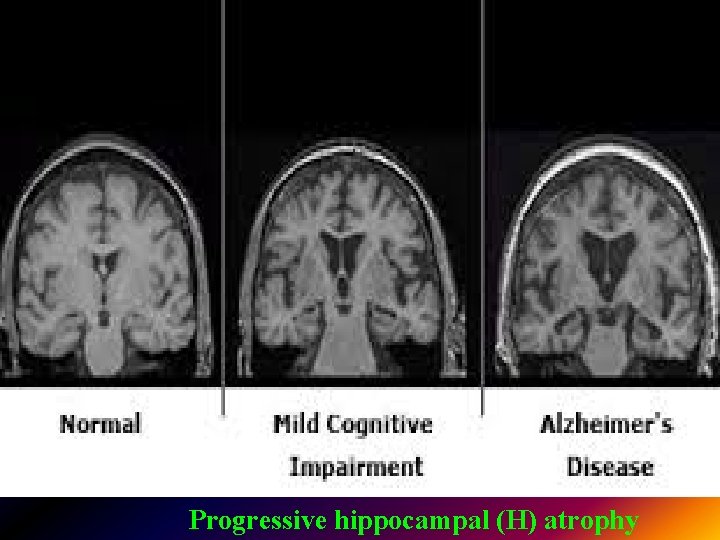
. Progressive hippocampal (H) atrophy
An organophosphate (organophosphorus). Organophosphates are the basis of many insecticides, herbicides, and nerve agents. Commonly used organophosphates have included parathion, malathion, methyl parathion, dichlorvos, Sarin, Tabun, and Soman. .
Toxicity by organophosphorus is due to A- Muscarinic effects (bradycardia, bronchoconstriction, excessive sweating, salivation, lacrimation, miosis, nausea, vomiting, abdominal cramps, urinary incontinence). B- Nicotinic effects (muscle twitches, neuromuscular blockade of diaphragm and intercostal muscles) C- CNS effects (restlessness, insomnia, tremors, confusion, convulsions, coma, death from respiratory failure).
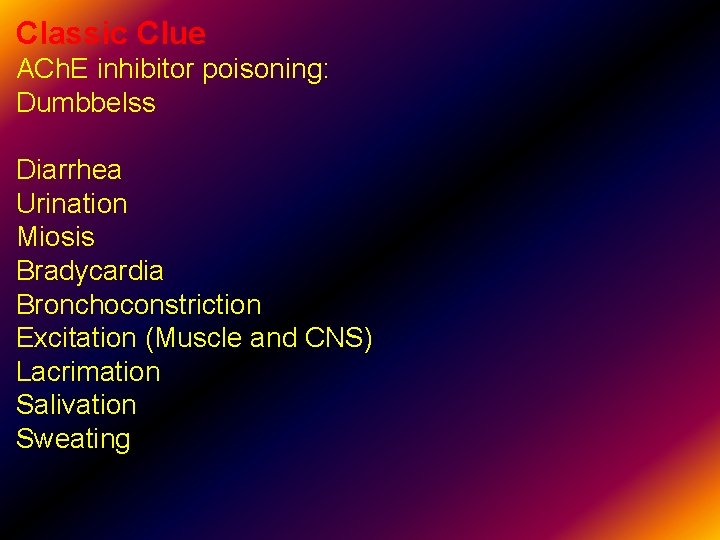
Classic Clue ACh. E inhibitor poisoning: Dumbbelss Diarrhea Urination Miosis Bradycardia Bronchoconstriction Excitation (Muscle and CNS) Lacrimation Salivation Sweating.
Management of organophosphorus Toxicity After standard protection of vital signs and oxygen therapy. the antidote of first choice is the antimuscarinic agent atropine , but this drug has no effect on the nicotinic signs of toxicity Nicotinic toxicity is treated by regenerating active cholinesterase. Immediately after binding to cholinesterase, most organophosphate inhibitors can be removed from the enzyme by the use of regenerator compounds such as pralidoxime and this may reverse both nicotinic and muscarinic signs.
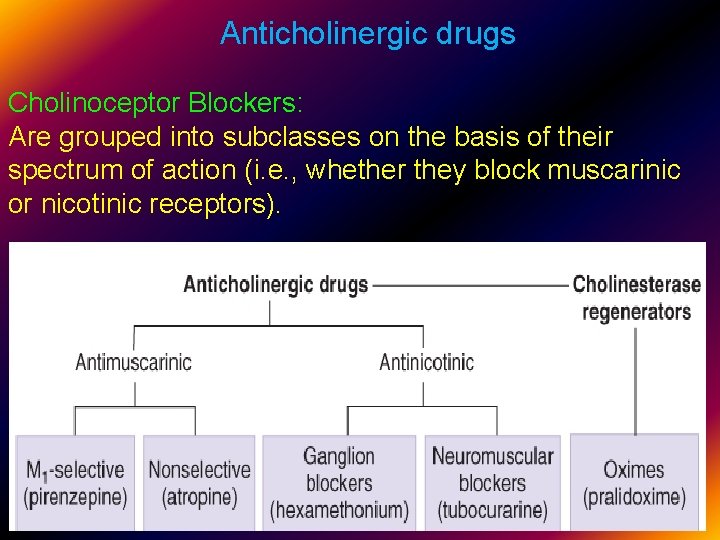
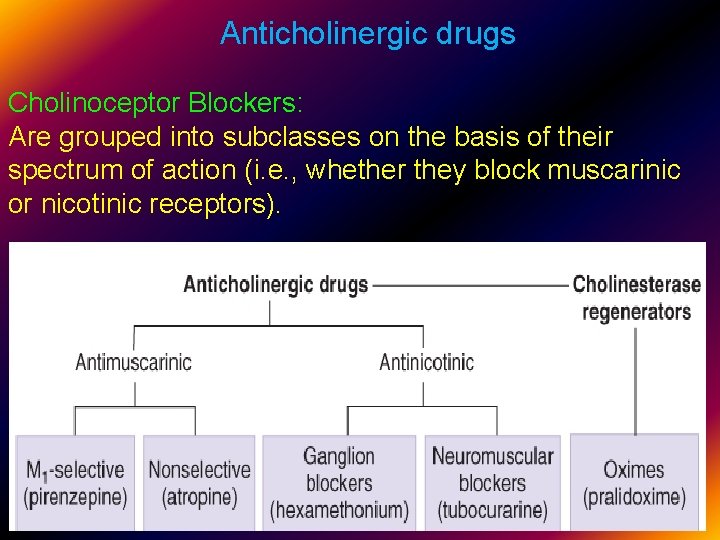
Anticholinergic drugs Cholinoceptor Blockers: Are grouped into subclasses on the basis of their spectrum of action (i. e. , whether they block muscarinic or nicotinic receptors). .
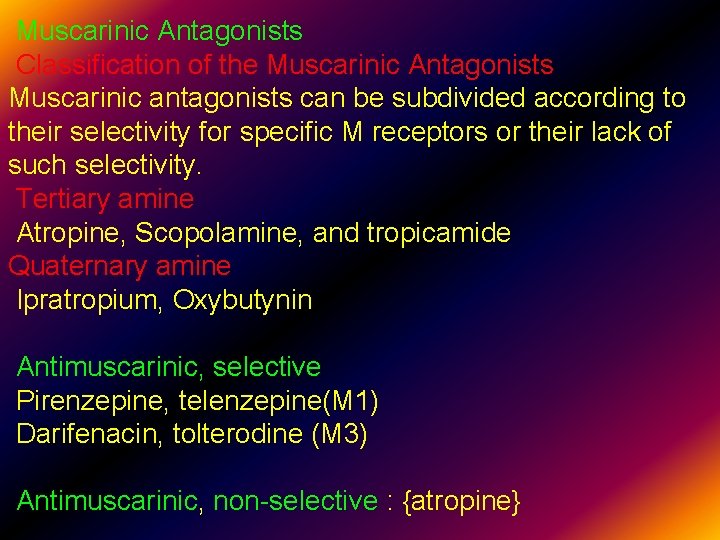
Muscarinic Antagonists Classification of the Muscarinic Antagonists Muscarinic antagonists can be subdivided according to their selectivity for specific M receptors or their lack of such selectivity. Tertiary amine Atropine, Scopolamine, and tropicamide Quaternary amine Ipratropium, Oxybutynin Antimuscarinic, selective Pirenzepine, telenzepine(M 1) Darifenacin, tolterodine (M 3) Antimuscarinic, non-selective : {atropine}
Drugs used for their effects on the CNS or the eye must be sufficiently lipid-soluble to cross lipid barriers. A major determinant of this property is the presence or absence of a permanently charged (quaternary) amine group in the drug molecule. This is because charged molecules are more polar and therefore less likely to penetrate a lipid barrier such as the blood-brain barrier or the cornea of the eye. .
Atropine is a nonselective muscarinic blocker. This alkaloid is found in Atropa belladonna and many other plants. Because it is a tertiary amine, atropine is relatively lipid-soluble and readily crosses membrane barriers. The elimination half-life is approximately 2 h, and the duration of action of normal doses is 4– 8 h except in the eye, where its t 1/2 =72 h &its effects last for 2 -3 weeks. Pharmacologic Effects : Atropine effects in order of increasing dose are: Decreased secretions (salivary, bronchiolar, sweat) Mydriasis and cycloplegia Hyperthermia. Tachycardia Urinary retention and constipation
Atropine poem: "dry as a bone, red as a beet, hot as a bare, blind as a bat, and mad as a hatter. Mechanism of Action The muscarinic blocking agents act like competitive pharmacologic antagonists; their blocking effects can be overcome by increased concentrations of muscarinic agonists (? ). Clinical uses of muscarinic antagonists {Effects} 1) The peripheral actions of muscarinic blockers are derived from cholinoceptor blockade. These include the ocular, gastrointestinal, genitourinary, and secretory effects. 2) CNS effects seen at therapeutic concentrations include sedation, & reduction of motion sickness. .
Peripheral effects: Effects on heart Cardiovascular effects at therapeutic doses include an initial slowing of heart rate {caused by central or presynaptic vagal effects} followed by the tachycardia and decreased atrioventricular conduction time. Arterial blood pressure is unaffected, because most resistance vessels have no cholinergic innervation. *Treatment of sinus bradycardia (e. g. after myocardial infarction): Effects on the CNS Atropine produces mainly excitatory effects on the CNS. At low doses, this causes mild restlessness; higher doses cause agitation and disorientation. .
Scopolamine (Buscopan ® ) is standard therapy for motion sickness; it is one of the most effective agents available for this condition. Cinnarazin (stugeron ®) also can be used. . .
Effects on the eye Topical use ( atropine )can cause mydriasis which causes a full visualization of the retina. , as indicated by the origin of the name belladonna ("beautiful lady") from the ancient cosmetic use of extracts of the Atropa belladonna plant to dilate the pupils. Intraocular pressure may rise; although this is unimportant in normal individuals, it can be dangerous in patients suffering from narrow-angle glaucoma. .
Bronchi Parenteral atropine has long been used to reduce airway secretions during general anesthesia. Ipratropium is a quaternary antimuscarinic agent used by inhalation to promote bronchodilation in asthma and chronic obstructive pulmonary disease (COPD). Tiotropium is a newer analog with a longer duration of action. . .

Effects on the gastrointestinal tract Gastrointestinal motility is inhibited by atropine. Gastrointestinal indications: 1)The M 1 -selective inhibitor pirenzepine for the treatment of peptic ulcer{inhibits gastric acid secretion}. 2)Muscarinic blockers (mebeverine {dusptaline® } ; stelabid ; Riabal and clidnium bromide {librax ® } can also be used to reduce cramping and hypermotility in transient diarrheas and irritable bowel syndrome {IBS}. . .
However , they delay gastric emptying and decrease esophageal and gastric emptying so it may leads to gastro-esophageal regurgitation Inhibition of secretions Salivary, lacrimal, bronchial and sweat glands are inhibited by very low doses of atropine. Gastric secretion is only slightly reduced Mucociliary clearance in the bronchi is inhibited. .

Bladder Oxybutynin (tablet and syrup) may be used to reduce urgency in mild cystitis and to reduce bladder spasms after urologic surgery. Tolterodine and darifenacin are promoted for the treatment of stress incontinence. Note: oxybutynin{Ditropan ®} has been also used to treat nocturnal enuresis and postmenopausal incontinence. . .
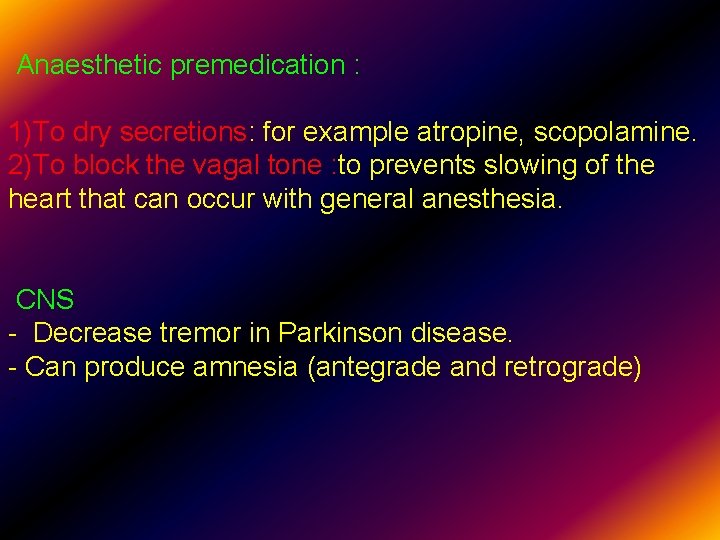
Anaesthetic premedication : 1)To dry secretions: for example atropine, scopolamine. 2)To block the vagal tone : to prevents slowing of the heart that can occur with general anesthesia. CNS - Decrease tremor in Parkinson disease. - Can produce amnesia (antegrade and retrograde) .
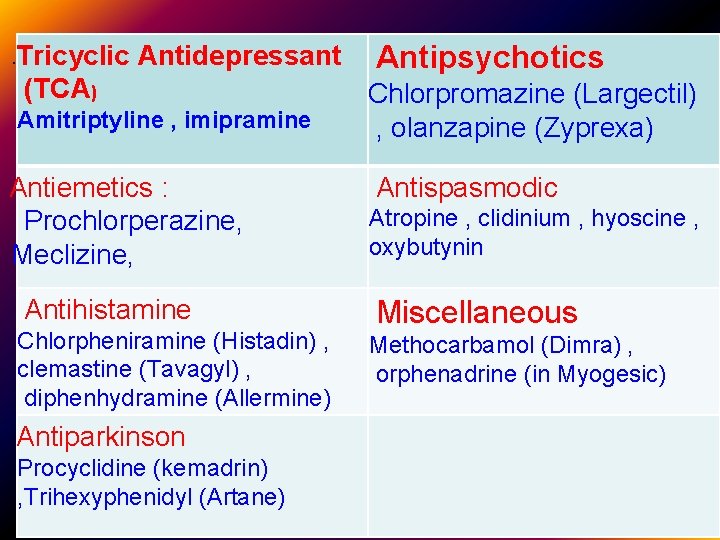
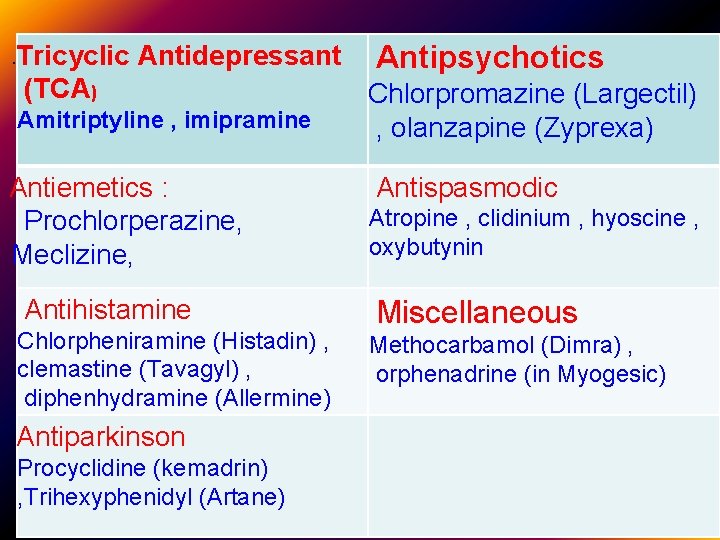
. Tricyclic Antidepressant (TCA) Amitriptyline , imipramine Antiemetics : Prochlorperazine, Meclizine, Antihistamine Chlorpheniramine (Histadin) , clemastine (Tavagyl) , diphenhydramine (Allermine) Antiparkinson Procyclidine (kemadrin) , Trihexyphenidyl (Artane) Antipsychotics Chlorpromazine (Largectil) , olanzapine (Zyprexa) Antispasmodic Atropine , clidinium , hyoscine , oxybutynin Miscellaneous Methocarbamol (Dimra) , orphenadrine (in Myogesic)
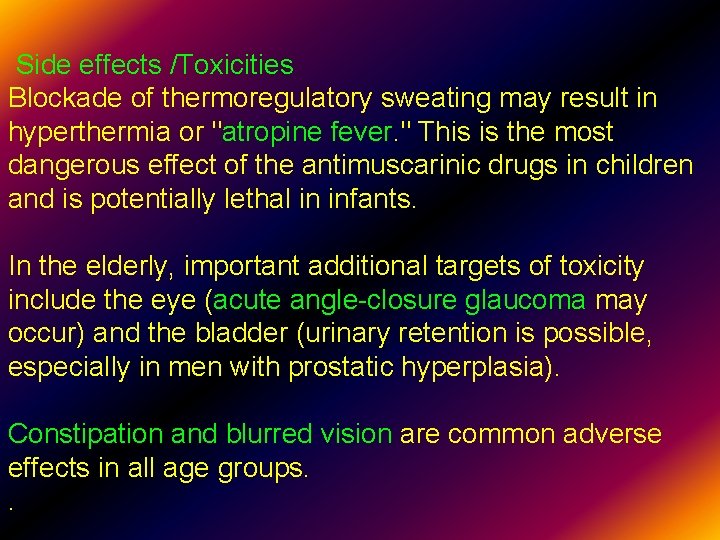
Side effects /Toxicities Blockade of thermoregulatory sweating may result in hyperthermia or "atropine fever. " This is the most dangerous effect of the antimuscarinic drugs in children and is potentially lethal in infants. In the elderly, important additional targets of toxicity include the eye (acute angle-closure glaucoma may occur) and the bladder (urinary retention is possible, especially in men with prostatic hyperplasia). Constipation and blurred vision are common adverse effects in all age groups. . .
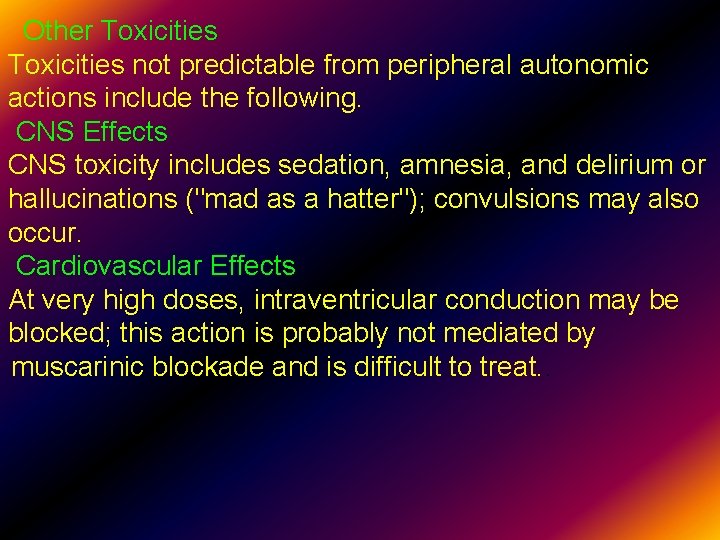
Other Toxicities not predictable from peripheral autonomic actions include the following. CNS Effects CNS toxicity includes sedation, amnesia, and delirium or hallucinations ("mad as a hatter"); convulsions may also occur. Cardiovascular Effects At very high doses, intraventricular conduction may be blocked; this action is probably not mediated by muscarinic blockade and is difficult to treat. .
 Basic & clinical pharmacology
Basic & clinical pharmacology Clinical pharmacology seminar
Clinical pharmacology seminar Dopamine synthesis
Dopamine synthesis Clinical pharmacology seminar
Clinical pharmacology seminar Clinical pharmacology powered by clinicalkey
Clinical pharmacology powered by clinicalkey Chronic gout
Chronic gout Clinical pharmacology
Clinical pharmacology Clinical pharmacology residency
Clinical pharmacology residency Glipizide interactions
Glipizide interactions Parasympathomimetic drugs
Parasympathomimetic drugs Cholinomimetic drugs classification
Cholinomimetic drugs classification Indirect acting cholinergic agonist
Indirect acting cholinergic agonist Focus on pharmacology
Focus on pharmacology First pass effect
First pass effect Mdi pharmacology
Mdi pharmacology Difference between tolerance and tachyphylaxis
Difference between tolerance and tachyphylaxis Objectives of pharmacology
Objectives of pharmacology Parkinson's disease definition
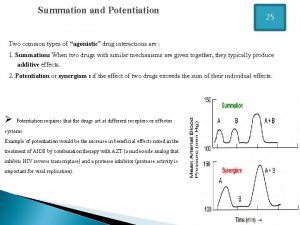
Parkinson's disease definition Potentiation example
Potentiation example Pharmacology of drugs acting on respiratory system
Pharmacology of drugs acting on respiratory system What is pharmacology
What is pharmacology Ion trapping
Ion trapping Define pharmacology
Define pharmacology Glomerular filtration
Glomerular filtration Rationale meaning in pharmacology
Rationale meaning in pharmacology Respiratory pharmacology quiz
Respiratory pharmacology quiz What is pharmacology
What is pharmacology If time permits quotes
If time permits quotes Mechanism of drug action
Mechanism of drug action What is ion trapping in pharmacology
What is ion trapping in pharmacology Potency vs efficacy
Potency vs efficacy Define pharmacology
Define pharmacology Pharmacology for veterinary technicians
Pharmacology for veterinary technicians Prostagalndins
Prostagalndins Pharmacology pay
Pharmacology pay Slidetodoc. com
Slidetodoc. com Alia drug testing
Alia drug testing Dosage regimen
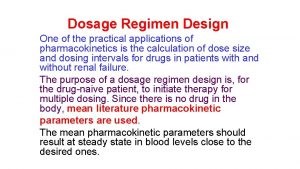
Dosage regimen Adrenal drugs pharmacology
Adrenal drugs pharmacology Loading dose formula in pharmacology
Loading dose formula in pharmacology Pharmacology chapter 1
Pharmacology chapter 1 Pharmacology module
Pharmacology module Tactcardia
Tactcardia First pass effect in pharmacology
First pass effect in pharmacology Pharmacology basics
Pharmacology basics Hagar conjugation
Hagar conjugation Concept of essential drugs
Concept of essential drugs Annual review of pharmacology and toxicology
Annual review of pharmacology and toxicology Pharmacology definition
Pharmacology definition Competitive antagonist
Competitive antagonist Chapter 15 diagnostic procedures and pharmacology
Chapter 15 diagnostic procedures and pharmacology Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals First pass effect in pharmacology
First pass effect in pharmacology Loading dose formula
Loading dose formula Estado estable
Estado estable Pharmacology tutor anderson
Pharmacology tutor anderson Venipuncture radiologic technologist
Venipuncture radiologic technologist First pass metabolism definition pharmacology
First pass metabolism definition pharmacology Npte pharmacology
Npte pharmacology Fish pharmacology
Fish pharmacology Chapter 30 principles of pharmacology
Chapter 30 principles of pharmacology Samyukti meaning
Samyukti meaning Toxicology and applied pharmacology
Toxicology and applied pharmacology What is ion trapping in pharmacology
What is ion trapping in pharmacology Pharmacology for nurses: a pathophysiological approach
Pharmacology for nurses: a pathophysiological approach Unit ratio definition
Unit ratio definition The part of a shadow surrounding the darkest part
The part of a shadow surrounding the darkest part Part part whole
Part part whole Part to part variation
Part to part variation Part by part technical description example
Part by part technical description example Addition symbol
Addition symbol Parts of bar counter
Parts of bar counter