CLASS 9 08092015 D Chemotherapy Indications In advanced









- Slides: 50
CLASS 9 08/09/2015
D. Chemotherapy Indications In advanced carcinoma breast. In postoperative period after simple mastectomy in stage III carcinoma breast with fixed axillary nodes. In inflammatory carcinoma of breast. In stage IV carcinoma breast with secondaries in bone, lungs, liver. In premenopausal age group with poorly differentiated tumours. All node positive patients
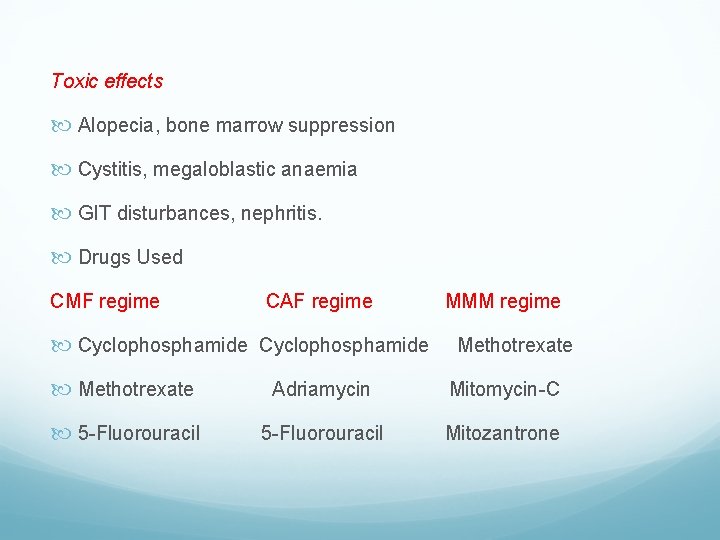
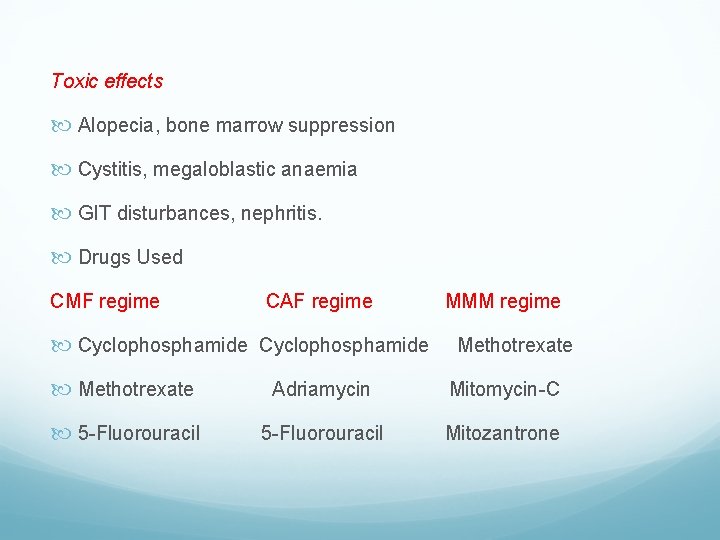
Toxic effects Alopecia, bone marrow suppression Cystitis, megaloblastic anaemia GIT disturbances, nephritis. Drugs Used CMF regime CAF regime Cyclophosphamide MMM regime Methotrexate Adriamycin Mitomycin-C 5 -Fluorouracil Mitozantrone
CMF and CAF are commonly used with monthly/ 3 weeks cycles for 6 months. Other anthracyclines like doxorubicin or epirubicin. Taxanes – act on G 2/M phase of cell cycle. It is commonly used in metastatic carcinoma of breast. Drugs are paclitaxel and docetaxel. Gemcitabine
Neoadjuvant chemotherapy is useful in large operable primary tumour to down stage. Hormone therapy is given after completion of chemotherapy for additive effect. Concurrent therapy of both (together) is not used at present. It is sequential – chemotherapy then hormone therapy.
Chemotherapy gives quicker and better response initially and so it is used early and later only hormone therapy is continued. Chemotherapy and radiotherapy can be given concurrently or as sandwich therapy. Presently one day dose of all drugs of the regimen used as a standard at 3 weekly cycles for 6 cycles for stage III CAF. For metastatic paclitaxel single day dose cycles or etoposide and cisplatin 3 days cycle– 6 cycles.
MANAGEMENT OF EARLY CARCINOMA BREAST Diagnosed by mammography or Stage I carcinoma breast. Aims of Treatment To achieve possible ‘cure’. Control of local disease in breast and axilla. Breast conservation, i. e. breast form and function. Prevention of distant metastasis. To prevent local recurrence
Modalities of Treatment Wide Excision QUART therapy. Patey’s operation or simple mastectomy with axillary clearance. Postoperative radiotherapy in high risk patients. Hormone therapy, i. e. Tamoxifen 10 mg BID. Sentinel node biopsy when required.
Regular follow-up often with radioisotope bone scan and CEA tumour marker.
BREAST CONSERVATIVE SURGERY Indications Lump < 4 cm Clinically negative axillary nodes Mammographically detected lesion Well differentiated tumour Adequate sized breast Tumour/breast size ratio is more

Radiotherapy is a must to breast and chest wall region (locally). QUART Therapy It is quadrantectomy, axillary dissection of level I and II nodes with separate axillary incision and post-operative radiotherapy to breast (5000 c. Gy) and axilla (1000 c. Gy). First it was started by Umberto Veronesi from Milan.
Skin Sparing Mastectomy (SSM) It is like a key-hole surgery of breast. Skin sparing/limited skin excision (5 -10%) will not alter/affect the recurrence rate. Indications are- central tumour/multicentral/extensive intraductal/T 1/not feasible for conservation. Excision of nipple-areola complex with very limited skin removal.
Indications for Total Mastectomy in early Breast Cancer When tumour is more than 4 cm. Multicentric tumour. Poorly differentiated tumour. Tumour margin is not clear of tumour after breast conservative surgery.
Management of Axillary Nodes when clinically not palpable Sentinel Lymph Node Biopsy (SLNB) is done. If node is positive for tumour then axillary dissection is done. But facility for SLNB is not available in most of the centres and so axillary dissection is done as a routine. Usually level I and II nodes - below the axillary vein are dissected.
Axillary sampling is done by separate curved incision between the outer border of pectoralis major and latissimus dorsi 6 cm below the apex of axilla. About 10 -15 nodes (level I) are sampled. Axillary sampling is not advocated now.
Endocrine manipulation– Ablation – Tamoxifen (receptor antagonist)- 20 mg/day for 5 years – Aromatase inhibitors- blocks oestrogen production. –Letrozole 2. 5 mg OD – LHRH agonists- Goserelin 3. 6 mg/28 day’s cycle for 2 years.
ADVANCED CARCINOMA BREAST Refers to • Locally inoperable (adherent to chest wall) tumour. • Inflammatory carcinoma of breast. • Fixed axillary lymph nodes, or supraclavicular lymph nodes, or opposite axillary nodes. • Bilateral carcinoma breast. • Metastatic carcinoma of breast, i. e. spread to bones, liver, lungs, brain.
Locally Advanced Carcinoma of Breast (LABC) • It means locally advanced tumour with muscle/chest wall involvement, extensive skin involvement or fixed axillary nodes. It will be T 3, T 4 a, T 4 b, T 4 c or T 4 d or N 2 or N 3. Treatment is always palliative by simple mastectomy, toilet mastectomy, chemotherapy and hormone therapy using tamoxifen. Palliation is to control pain, to prevent fungation or bleeding.
In inoperable fixed tumour chemotherapy is given initially. Later, after 3 -4 cycles of chemotherapy, when tumour size reduces and becomes operable, total mastectomy is done. Postoperative radiotherapy is given to breast field and axilla. Usually axillary dissection is not necessary in LACB. Only chemotherapy and radiotherapy to breast and axilla (without palliative mastectomy) also can be done in LACB. There is no role of breast conservative surgery for LACB. 5 year survival is 40% and 10 year survival is less than 25%.
Inflammatory carcinoma is T 4 d LACB. It is initially treated by chemotherapy or radiotherapy and later if tumour reduces in size total mastectomy with axillary clearance can be done. But most often it is inoperable. After surgery, chemotherapy and tamoxifen is given. 5 year survival for inflammatory carcinoma of breast is 25 -30%.
Metastatic Carcinoma of Breast It is blood spread into different places like bone, lungs and pleura, liver, soft tissues, brain and adrenals. It is evaluated by FNAC/incision biopsy, chest CT, LFT, U/S abdomen, CT abdomen, whole body bone scanning, CT brain, tissue study for ER/PR/HER-2 neu receptor status. Treatment concept in metastatic carcinoma of breast • To improve quality of life. • To relieve pain of secondaries like bone, lungs. • To relieve neurological problems like convulsions, space occupying cranial problems. • Other symptomatic relief.
Treatment strategy in metastatic carcinoma of breast • Chemotherapy- CMF, CAF, Taxanes in combination. • High dose of chemotherapy using cyclophosphamide, cisplatin, carmustine, melphalan is tried in view to get high response rate of 5570% along with bone marrow transplant. But toxic effects are often life threatening. Its advantages are now doubtful when compared to toxic effects. Haemopoietic growth factor also used along with chemotherapy to enhance the cell kill with less bone marrow toxicity.
It may also allow multiple high dose chemotherapy to increase the response rate. Radiotherapy is used in bone metastasis, brain secondaries, to prevent paraplegia in spine involvement, and advanced axillary nodes. It is also used in painful bone secondaries. Hormone therapy has got important role. Tamoxifen, oophorectomy, adrenalectomy, androgens, progestogens, aminoglutethimide are used.
Malignant pleural effusion • Respiratory distress and failure is the main feature • HRCT is ideal diagnostic tool • Treated by – Intercostal tube drainage – Pleurodesis using talc/tetracycline – Chemotherapy
Causes of death in carcinoma breast 1. Secondaries in lung—Haemoptysis, respiratory failure 2. Spine involvement—Quadriplegia 3. Secondaries in brain 4. Cancer cachexia
PROGNOSTIC FACTORS IN CARCINOMA BREAST Stage 5 yr survival I 90% II 70% III 40% IV 20%
Age: Younger the age worser the prognosis. Sex: Carcinoma male breast has got worser prognosis Lymph Node—as a Prognostic Factor • Number of nodes: > 2 carries poor prognosis • Location of nodes • Capsular invasion • Extranodal status • Size of the node: >2. 5 cm has poor prognosis • More than 4 nodes/level III (apical nodes)
Stage I and II has got better prognosis. Atrophic scirrhous has got best prognosis. Inflammatory carcinoma breast has worst prognosis. ER +ve tumours has got better prognosis. Differentiation also decides prognosis. Presence of elastic fibres in histology has got better prognosis. Tumour proliferation stages, growth factor and oncogene factors.
Erb. B 2 –Her-2/neu positive has got poor prognosis. Prognostic factors are classified as – • Host factors – Age; sex; menopausal status; family history; previous breast cancer; immunosuppression; nutrition. • Tumor factors – Tumour size; nuclear grade; staging; receptor status; DNA nature; spread etc.
Carcinoma breast in pregnancy Incidence is 3% Treatment is modified radical mastectomy (MRM) Chemotherapy can be given in 2 nd trimester with care Radiotherapy has no role As commonly ER negative, hormone therapy is not used When distressing secondaries are present termination of pregnancy may be required Women with breast cancer can become pregnant 2 years after the completion of therapy, as recurrence is more common in 2 years.
CARCINOMA OF MALE BREAST It is less than 1% of cases of breast cancers. Gynaecomastia and excess oestrogen are said to be the aetiological factors. Commonly associated with BRCA 2 gene mutation. Commonly it is infiltrating duct carcinoma. Presentation, spread, behaviour are same as carcinoma of female breast. Investigations and treatment are same as carcinoma female breast. Tamoxifen is very useful in carcinoma male breast. Carcinoma male breast has poorer prognosis when compared to carcinoma breast in females.
80% cases are ER positive. LHRH agonists are also often used. It works at hypothalamo-pituitary axis level. It produces reversible “chemical castration”. Goserelin 3. 6 mg/28 days for 2 years is the current recommendation. Bilateral orchidectomy which was earlier used is no longer commonly advocated.

FOLLOW UP AFTER THERAPY Clinical examination in detail at regular intervals. Yearly/two yearly mammography of treated and contralateral breast is a must. Bone scan/CT chest, abdomen/tumour marker are done only if there is clinical suspicion of spread/ metastases. There is no regular routine follow up method at present
BREAST RECONSTRUCTION Immediate reconstruction. In early stages of malignancies as well as in selected more advanced stages where the response to neo adjuvant chemo therapy has been good. Not advised in locally advanced disease. Delayed reconstruction (3 -9 months after surgery). Indications • Locally advanced disease. • Radiation needed in postoperative period. • Patient unfit for prolonged surgical procedure.
Advantages Allows for post op radiation without prosthesis exposure. Avoids fibrosis and fat necrosis where TRAM flap is used. Factors deciding the reconstruction • Amount of skin retained • Stage of the carcinoma • Earlier radiotherapy • Type of flap used
Methods of Reconstruction Oncoplastic techniques. Insertion of breast implants or expanders. They are best for small breasts. Healthy non irradiated overlying skin is the requirement. Flap with implant or expanders. Flap reconstruction— – Pedicled flap – TRAM flap. – Free flap – free TRAM flap into internal mammary artery.
Types Silicon gel implant under pectoralis major muscle. Expandible saline prosthesis with prior tissue expansion. If there is less skin or after radiotherapy—Latissimus dorsi musculocutaneous flap (LD flap) or contralateral transversus abdominis muscle flap (TRAM flap) is used. Superior gluteal flap based on superior gluteal vessels Ruben‘s flap using soft tissue pad overlying the iliac crest based on deep circumflex iliac vessels. External breast prosthesis which fits within the bra is a simpler cosmetic method.






Nipple is created using— Local breast flaps 3 months after breast reconstruction. Nipple sharing from contralateral nipple using composite graft. Skate flap: Local flap with deepithelialised donor site around the periphery over which a full thickness graft is applied. Nipple prosthesis can be fitted.
Areola pigmentation is created using (it is done 3 weeks after nipple creation)— Full thickness skin graft from non hairy skin lateral to labia majora, as the pigmentation of this graft matches that of the areola. From contralateral areola if reduction mammoplasty is done on that side. Tattooing – Colour tends to fade with time and may need to be repeated.

BREAST IMPLANTS
Technically simple. Achieve symmetry easily. Implant in submuscular plane is better whenever muscle is not removed during surgery. If muscle is removed as in radical mastectomy, then subcutaneous implant is placed. Silicon gel implants are used
Complications of breast implants • Pain, exposure of implant and rupture • Displacement, extrusion • Infection • Capsular contraction