Chapter 47 Management of Patients With Gastric and

- Slides: 52
Chapter 47 Management of Patients With Gastric and Duodenal Disorders Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
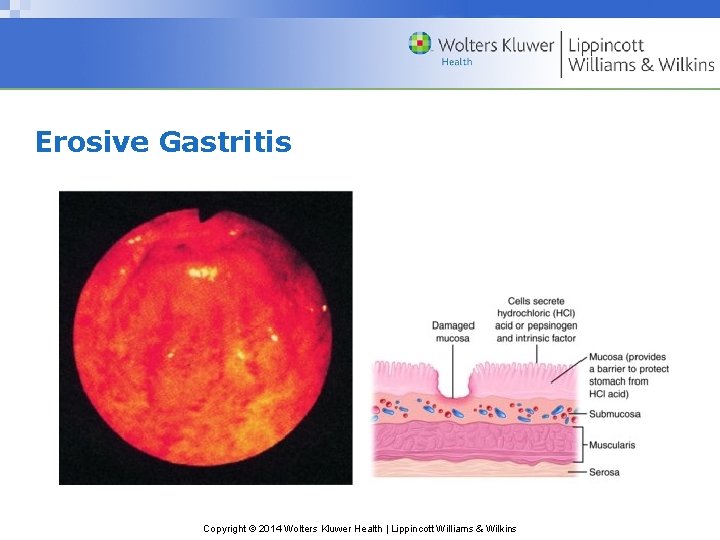
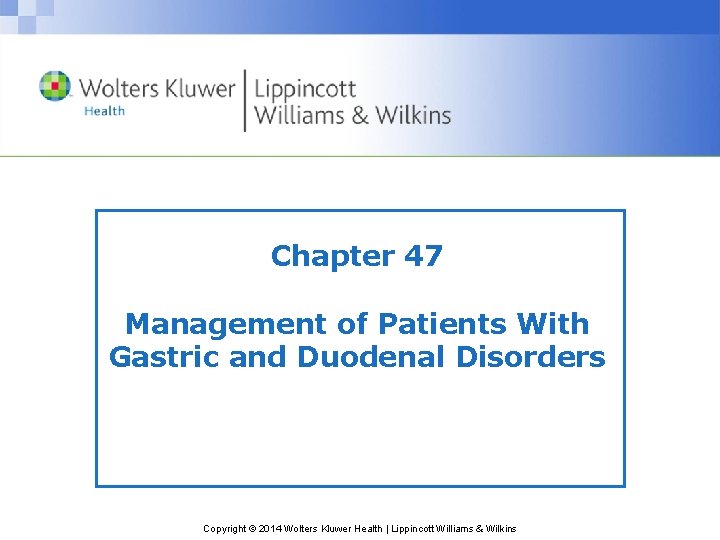
Gastritis • Inflammation of the stomach • A common GI problem • Acute: rapid onset of symptoms usually caused by dietary indiscretion. Other causes include medications, alcohol, bile reflux, and radiation therapy. Ingestion of strong acid or alkali may cause serious complications. • Chronic: prolonged inflammation due to benign or malignant ulcers of the stomach or by Helicobacter pylori. May also be associated with some autoimmune diseases, dietary factors, medications, alcohol, smoking, or chronic reflux of pancreatic secretions or bile. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Erosive Gastritis Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Gastritis—Assessment • History including presenting signs and symptoms • Dietary history and dietary associations with symptoms • 72 hour diet; diary may be helpful • Abdominal assessment Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Manifestations of Gastritis • Acute: abdominal discomfort, headache, lassitude, nausea, vomiting, hiccupping • Chronic: epigastric discomfort, anorexia, heartburn after eating, belching, sour taste in the mouth, nausea and vomiting, intolerance of some foods. May have vitamin deficiency due to malabsorption of B 12 • May be associated with achlorhydria, hypochlorhydria, or hyperchlorhydria • Diagnosis is usually by UGI X-ray or endoscopy and biopsy Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Gastritis—Diagnoses • Anxiety • Imbalanced nutrition • Risk for fluid volume imbalance • Deficient knowledge • Acute pain Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Gastritis—Planning • Major goals may include reduced anxiety, avoidance of irritating foods, adequate intake of nutrients, maintenance of fluid balance, increased awareness of dietary management, and relief of pain Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Medical Management of Gastritis • Acute – Refrain form alcohol and food until symptoms subside – If due to strong acid or alkali treatment to neutralize the agent, avoid emetics and lavage due to danger of perforation and damage to esophagus – Supportive therapy • Chronic – Modify diet, promote rest, reduce stress, avoid alcohol and NSAIDs – Pharmacologic therapy Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Interventions • Reduce anxiety; use calm approach and explain all procedures and treatments • Promote optimal nutrition; for acute gastritis, the patient should take no food or fluids by mouth. Introduce clear liquids and solid foods as prescribed. Evaluate and report symptoms. Discourage caffeinated beverages, alcohol, cigarette smoking. Refer for alcohol counseling and smoking cessation • Promote fluid balance; monitor I&O, for signs of dehydration, electrolyte imbalance, and hemorrhage • Measures to relieve pain: diet and medications Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
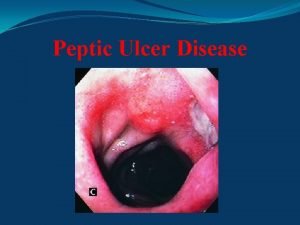
Peptic Ulcer • Erosion of a mucous membrane forms an excavation in the stomach, pylorus, duodenum, or esophagus • Associated with infection of H. pylori • Risk factors include excessive secretion of stomach acid, dietary factors, chronic use of NSAIDs, alcohol, smoking, and familial tendency • Manifestations include a dull gnawing pain or burning in the mid-epigastrium; heartburn and vomiting may occur • Treatment includes medications, lifestyle changes, and occasionally surgery Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins

Deep Peptic Ulcer Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question Is the following statement true or false? The most common site for peptic ulcer formation is the pylorus. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer False The most common site for peptic ulcer formation is not the pylorus. The most common site for peptic ulcer formation is the duodenum. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Peptic Ulcer—Assessment • Assess pain and methods used to relieve pain • Dietary intake and 72 hour diet diary • Lifestyle and habits such as cigarette and alcohol use • Medications; include use of NSAIDs • Sign and symptoms of anemia or bleeding • Abdominal assessment Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Peptic Ulcer—Diagnoses • Acute pain • Anxiety • Imbalanced nutrition • Deficient knowledge Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Collaborative Problems and Potential Complications • Hemorrhage • Perforation • Penetration • Pyloric obstruction (gastric outlet obstruction) Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Peptic Ulcer—Planning • Major goals for the patient may include relief of pain, reduced anxiety, maintenance of nutritional requirements, knowledge about the management and prevention of ulcer recurrence, and absence of complications Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Relieve Pain • Treat with prescription medications • Avoid aspirin, NSAIDs, and alcohol Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Anxiety • Assess anxiety • Calm manner • Explain all procedures and treatments • Help identify stressors • Explain various coping and relaxation methods such as biofeedback, hypnosis, and behavior modification Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Patient Education • Medication education • Dietary restrictions • Lifestyle changes Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Management of Potential Complications • Management of hemorrhage – Assess for evidence of bleeding, hematemesis or melena, and symptoms of shock/impending shock and anemia – Treatment includes IV fluids, NG, and saline or water lavage; oxygen, treatment of potential shock including monitoring of VS and UO; may require endoscopic coagulation or surgical intervention • Pyloric obstruction – Symptoms include nausea and vomiting, constipation, epigastric fullness, anorexia, and (later) weight loss – Insert NG tube to decompress the stomach, provide IV fluids and electrolytes. Balloon dilation or surgery may be required Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Management of Potential Complications • Management of perforation or penetration – Signs include severe upper abdominal pain that may be referred to the shoulder, vomiting and collapse, tender board-like abdomen, and symptoms of shock or impending shock – Patient requires immediate surgery Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question What is the best time to teach a client to take proton pump inhibitors? A. 30 minutes before a meal B. With a meal C. Immediately after the meal D. One to three hours after a meal Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer A. 30 minutes before a meal The best time for a client to take a proton pump inhibitor is before a meal. It is a delayed-release medication that is to be swallowed whole and taken before a meal. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Obesity • Obesity is body mass indices (BMI) above 30 mg/m 2 • 66% of all adults are overweight or obese • Obesity-related mortality rates are 30% greater for every gain of 5 kg/m 2 of body mass beyond a BMI of 25 kg/m 2 • Increased risk for disease, disorders, low self-esteem, impaired body image, depression, and diminished quality of life Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Obesity Management • Lifestyle modifications • Pharmacotherapy • Bariatric surgery Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Bariatric Surgery • Morbid obesity: persons more than two times IBW, BMI exceeds 30 kg/m 2, or more than 100 pounds greater than IBW; high risk for health complications • Surgery is preformed only after nonsurgical methods have failed • Selection factors include body weight, patient history, failure to lose weight using other means, absence of endocrine disorders, and psychological stability Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
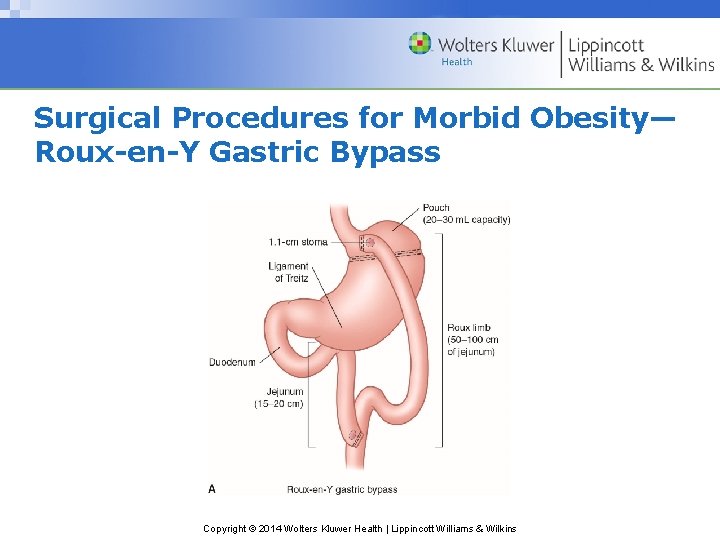
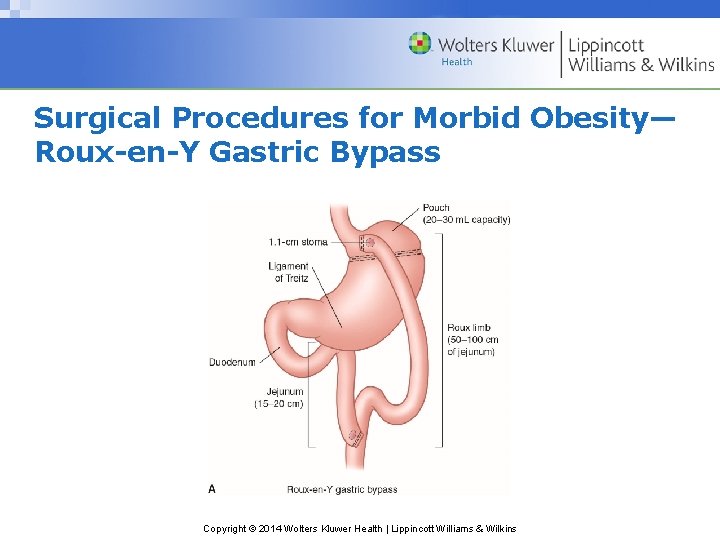
Surgical Procedures for Morbid Obesity— Roux-en-Y Gastric Bypass Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
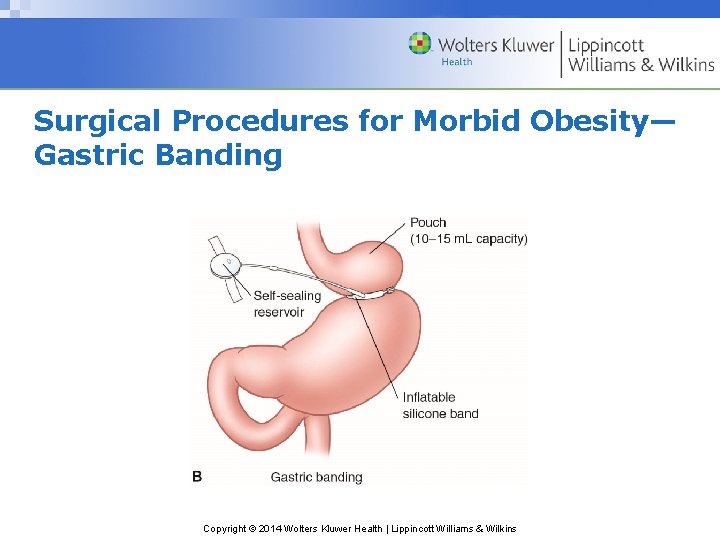
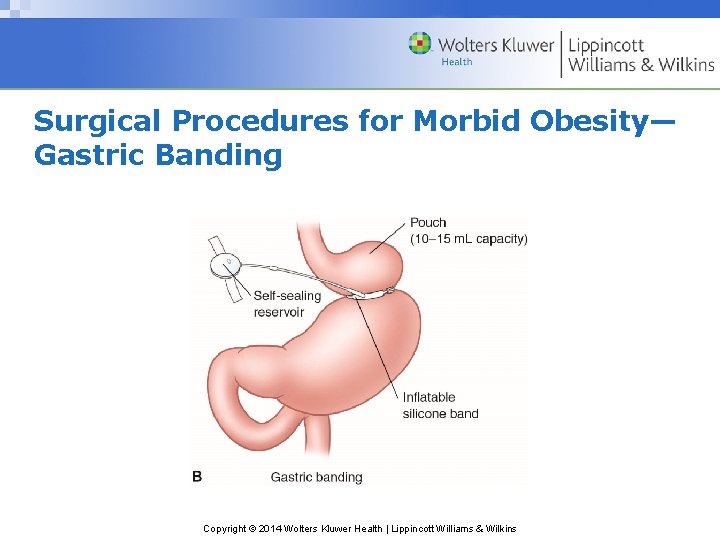
Surgical Procedures for Morbid Obesity— Gastric Banding Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
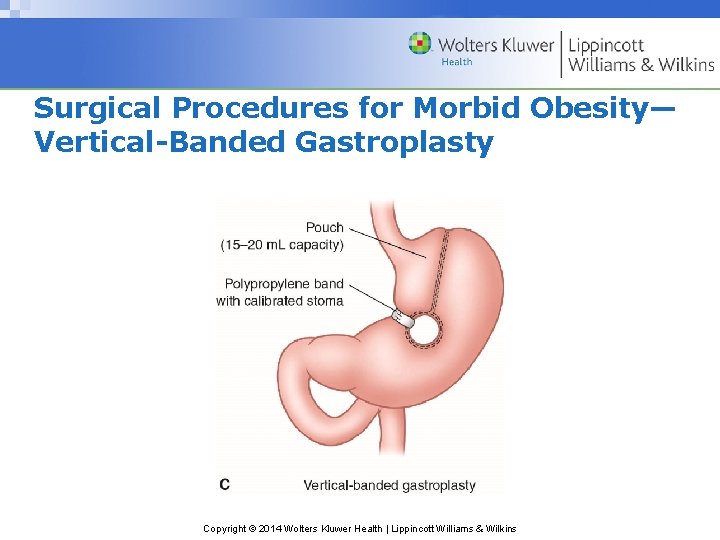
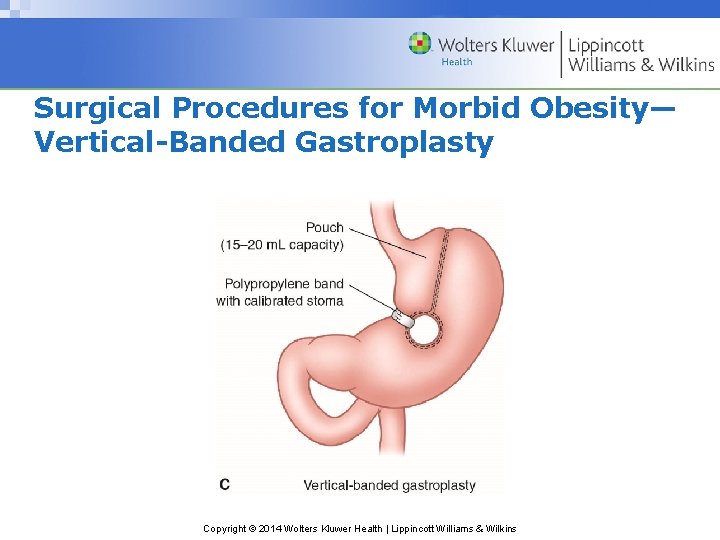
Surgical Procedures for Morbid Obesity— Vertical-Banded Gastroplasty Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
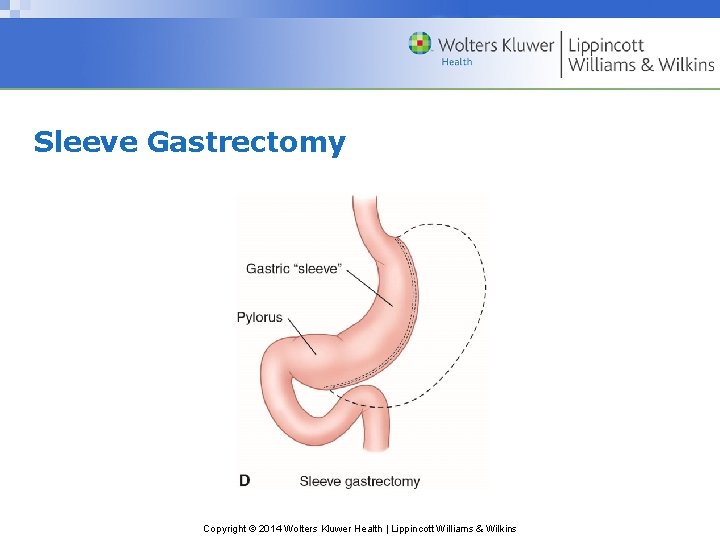
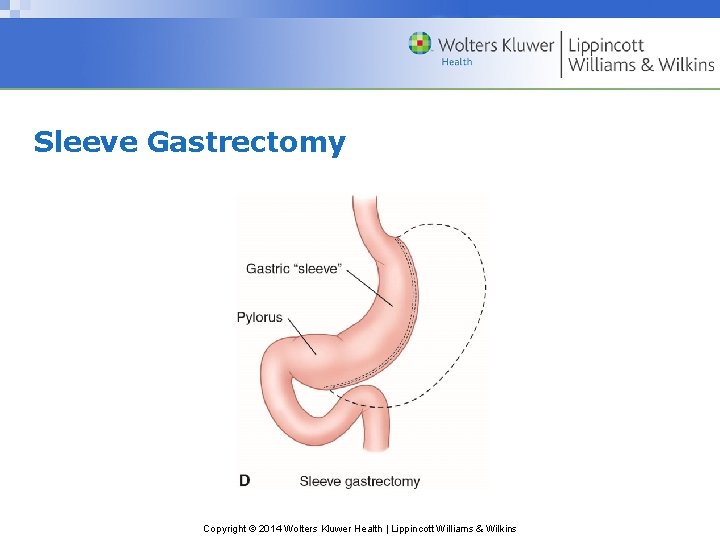
Sleeve Gastrectomy Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
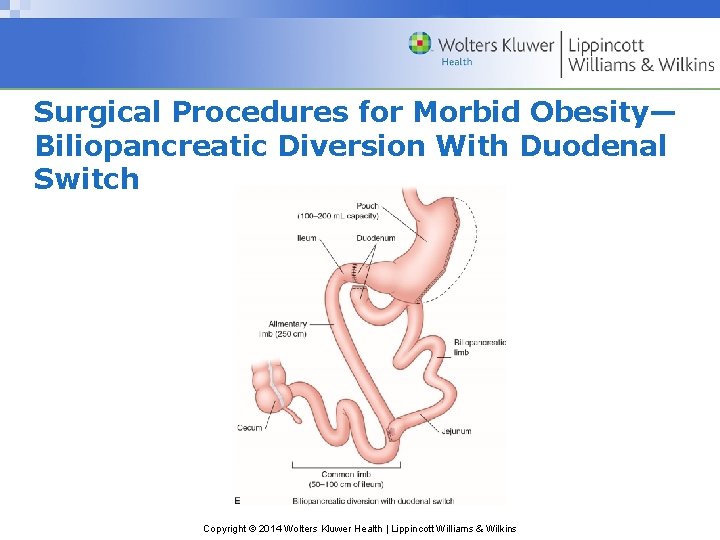
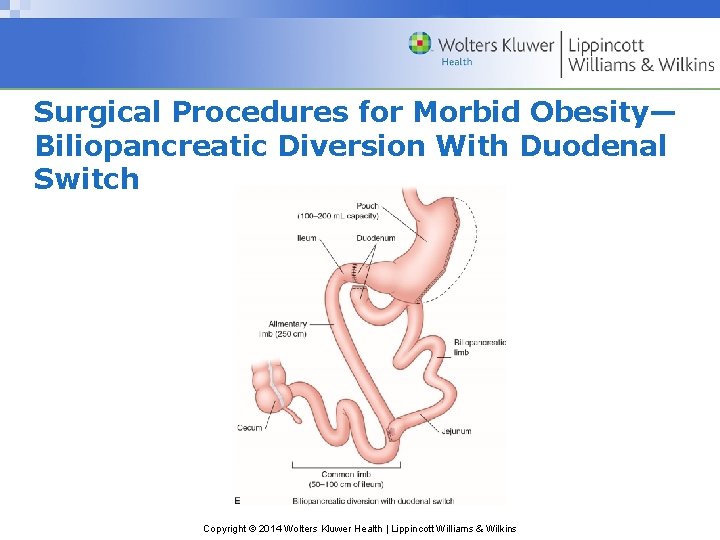
Surgical Procedures for Morbid Obesity— Biliopancreatic Diversion With Duodenal Switch Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Care of the Patient Undergoing Bariatric Surgery • Preoperative care; evaluation and counseling • Postoperative care is similar to gastric resection, but the patient is at greater risk for complications because of obesity • Postoperative diet: six small feedings totaling 600 to 800 calories per day • Patients require psychosocial interventions to modify their eating behaviors • Follow-up care • Education regarding long-term effects Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Collaborative Problems and Potential Complications • Hemorrhage • Bile reflux • Dumping syndrome • Dysphagia • Bowel or gastric outlet obstruction Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Question Is the following statement true or false? The average weight loss after bariatric surgery is 60% of previous body weight. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Answer True The average weight loss after bariatric surgery is 60% of previous body weight. Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
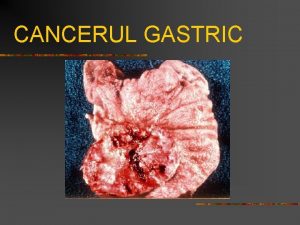
Gastric Cancer • Incidence is deceasing, but accounts for more than 10, 000 deaths in U. S. annually • Increased incidence in men, Native Americans, Hispanic Americans, and African Americans • Risk factors include diet, chronic inflammation of the stomach, H. pylori infection, pernicious anemia, smoking, achlorhydria, gastric ulcers, previous subtotal gastrectomy, and genetics • Manifestations include pain relieved by antacids, dyspepsia, early satiety, weight loss, abdominal pain, loss or decrease in appetite, bloating after meals, nausea, and vomiting. Diagnosis of the disease is often late • Treatment is surgical removal of the tumor if possible, and palliative care if the tumor is unresectable or metastasized Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Gastric Cancer—Assessment • Dietary history and nutritional status • Risk factors and smoking and alcohol history • Social support, individual and family coping • Resources • Physical assessment, including assessment of the abdomen Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Gastric Cancer—Diagnoses • Anxiety • Imbalanced nutrition • Pain • Anticipatory grieving • Deficient knowledge Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Gastric Cancer—Planning • Major goals include reduced anxiety, optimal nutrition, relief of pain, adjustment to the diagnosis, and anticipated lifestyle changes Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Anxiety • Provide a relaxed, nonthreatening atmosphere • Allow patient to express fears and concerns • Provide support and encourage family support • Promote positive coping measures • Explain treatments and procedures • Referral to support persons such as social worker or clergy Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Promote Optimal Nutrition • Encourage small, frequent meals of non-irritating foods • Provide foods high in calories and vitamins A and C and iron • Provide diet and education for potential dumping syndrome after gastric resection • Six small feedings low in carbohydrates and sugar, with fluids between, not with, meals • Assessment includes I&O, daily weights, assessment for signs of dehydration, and nutritional status Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Other Interventions • Pain – Administer analgesic as prescribed – Nonpharmacologic pain relief measures • Psychosocial support – Allow patient to express fears concern and grief – Allow patient to participate in decisions – Include family members and significant others – Referral or involvement of other support persons as needed • Patient education Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Gastric Surgery—Assessment • Patient and family knowledge • Nutritional status • Abdominal assessment • Postoperatively assess for potential complications Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Gastric Surgery—Diagnoses • Anxiety • Pain • Deficient knowledge • Imbalanced nutrition Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Collaborative Problems and Potential Complications • Hemorrhage • Dietary deficiencies • Bile reflux • Dumping syndrome Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Nursing Process: The Care of the Patient With Gastric Surgery—Planning • Major goals include reduced anxiety, increased knowledge, optimal nutrition, management of complications that can interfere with nutrition, relief of pain, avoidance of hemorrhage and steatorrhea, and enhanced self-care skills at home Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Interventions • Provide interventions to reduce anxiety • Pain – Administer analgesics as prescribed so patient may perform pulmonary care, leg exercises, and ambulation activities – Position in Fowler’s position – Maintain function of NG tube • Patient education • Individualized nutritional care and support Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Care and Prevention of Complications • Gastric retention – May require reinstatement of NPO and Ng suction; use low-pressure suction • Bile reflux – Agents that bind with bile acid: cholestyramine • Malabsorption of vitamins and minerals – Supplementation of iron and other nutrients – Parenteral administration of vitamin B 12 because of a lack of intrinsic factor Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Care and Prevention of Complications • Dumping syndrome – Caused by rapid passage of food into the jejunum and drawing of fluid into the jejunum caused by hypertonic intestinal contents – Causes vasomotor and GI symptoms with reactive hypoglycemia – Avoid fluid with meals – Avoid high carbohydrate and sugar intake • Steatorrhea – Reduce fat intake and administer loperamide Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Dietary Self-Management • To delay stomach emptying and dumping syndrome, assume low Fowler’s position after meals; lie down for 20 to 30 minutes • Take antispasmodics as prescribed • Avoid fluid with meals • Meals should contain more dry items than liquid items • Eat fat as tolerated but keep carbohydrate intake low and avoid concentrated carbohydrates • Eat small, frequent meals • Take dietary supplements as prescribed; vitamins, medium-chain triglycerides, and B 12 injections Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
Tumors of the Small Intestine • 64% malignant • Higher rates of cancer among older adults, African Americans, and men • May be asymptomatic or present with pain, occult bleeding, weight loss, nausea, vomiting, and intestinal obstruction • Assessment includes CBC, bilirubin, carcinoembryonic antigen (CEA) • Diagnose by upper GI radiograph or abdominal CT • Treat with surgery and chemotherapy Copyright © 2014 Wolters Kluwer Health | Lippincott Williams & Wilkins
 Enema
Enema When performing the rapid extrication technique
When performing the rapid extrication technique Lifting and moving patients
Lifting and moving patients Straddle slide technique
Straddle slide technique Nursing management of duodenal ulcer
Nursing management of duodenal ulcer Management of patients with neurologic trauma
Management of patients with neurologic trauma Management of patients with neurologic trauma
Management of patients with neurologic trauma Cva
Cva Dope mnemonic emt
Dope mnemonic emt Chapter 58 care of patients with liver problems
Chapter 58 care of patients with liver problems Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Niche on lesser curvature
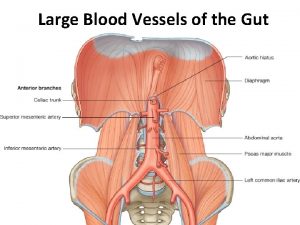
Niche on lesser curvature Inferior pancreaticoduodenal artery
Inferior pancreaticoduodenal artery Megalocephalitis
Megalocephalitis Types of gastric ulcer
Types of gastric ulcer A muscular bag secretes gastric juice and mixes food around
A muscular bag secretes gastric juice and mixes food around Differentiate between gastric gavage and lavage
Differentiate between gastric gavage and lavage Wendylett sheets 1 carer
Wendylett sheets 1 carer Fowler position
Fowler position Patients rights and responsibilities nabh
Patients rights and responsibilities nabh Safe staffing ratios benefiting nurses and patients
Safe staffing ratios benefiting nurses and patients Medicare improvements for patients and providers act
Medicare improvements for patients and providers act Ems lifting and moving patients
Ems lifting and moving patients Gastric glands
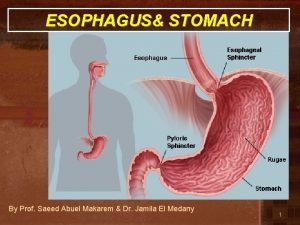
Gastric glands Ulcer
Ulcer Gastric folds
Gastric folds Parts of stomach
Parts of stomach Function if stomach
Function if stomach Sportello unico previdenziale
Sportello unico previdenziale Vomiting case presentation
Vomiting case presentation Bifurcation of common iliac artery vertebral level
Bifurcation of common iliac artery vertebral level Posterolateral abdominal wall
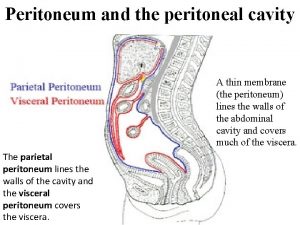
Posterolateral abdominal wall What is the peritoneal cavity
What is the peritoneal cavity Gastric ulcer
Gastric ulcer Hpilora
Hpilora Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Ge junction histology
Ge junction histology Enteropancreatic reflex
Enteropancreatic reflex What is the role of gastric juice
What is the role of gastric juice Gastric lavage for tb
Gastric lavage for tb Tubular spine surgery in mumbai
Tubular spine surgery in mumbai Borrmann classification of gastric cancer
Borrmann classification of gastric cancer Tablou clinic ulcer gastric
Tablou clinic ulcer gastric Medany el makarem
Medany el makarem Give an example for
Give an example for Gastric folds
Gastric folds Goose neck deformity
Goose neck deformity Cardiac orifice
Cardiac orifice Stomatch parts
Stomatch parts Function of stomach
Function of stomach Which bacteria gives protection against gastric injury
Which bacteria gives protection against gastric injury Pepsin renin
Pepsin renin Gastric outlet obstruction
Gastric outlet obstruction