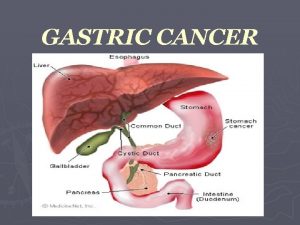
GASTRIC CANCER GASTRIC CANCER 4 5 th position








- Slides: 23
GASTRIC CANCER
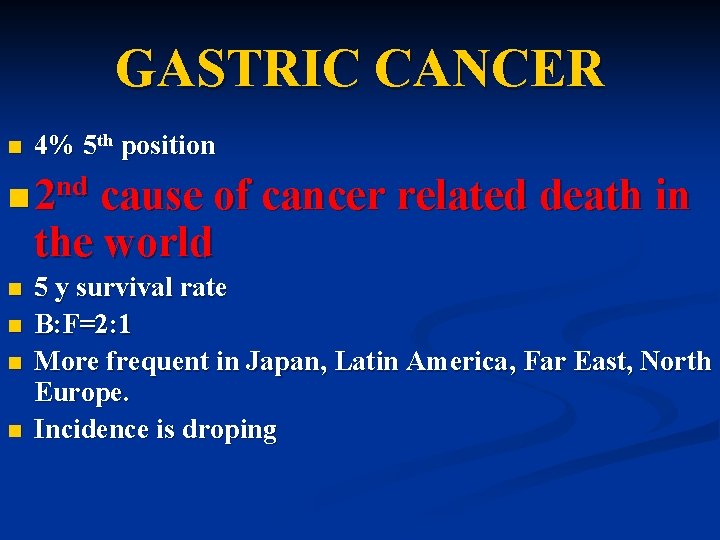
GASTRIC CANCER 4% 5 th position nd n 2 cause of n cause of cancer related death in the world n 2 n n 5 y survival rate B: F=2: 1 More frequent in Japan, Latin America, Far East, North Europe. Incidence is droping
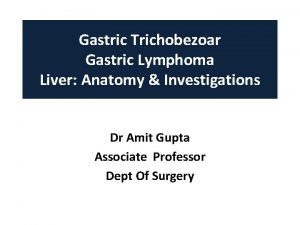
Pathology n Adenocarcinoma 90% n Sarcoma n Limfoma
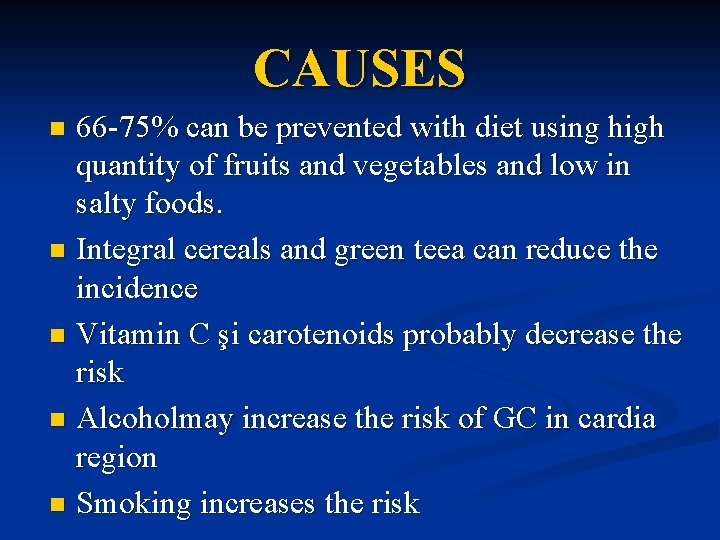
CAUSES 66 -75% can be prevented with diet using high quantity of fruits and vegetables and low in salty foods. n Integral cereals and green teea can reduce the incidence n Vitamin C şi carotenoids probably decrease the risk n Alcoholmay increase the risk of GC in cardia region n Smoking increases the risk n
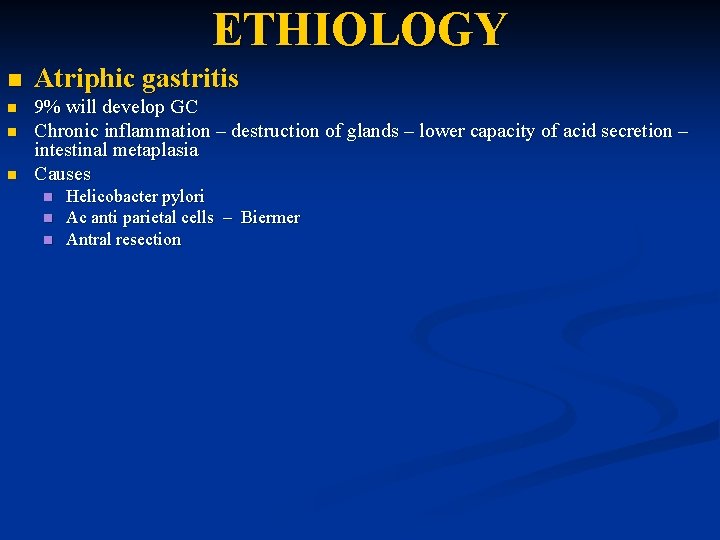
ETHIOLOGY n Atriphic gastritis n 9% will develop GC Chronic inflammation – destruction of glands – lower capacity of acid secretion – intestinal metaplasia Causes n n n Helicobacter pylori Ac anti parietal cells – Biermer Antral resection
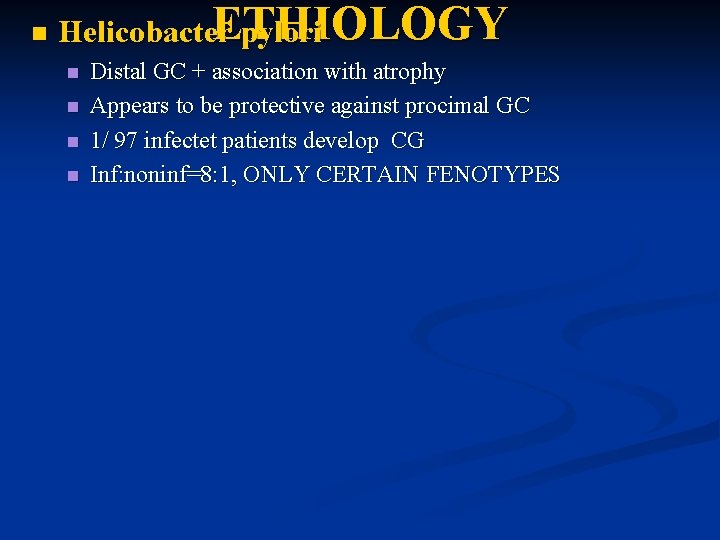
n ETHIOLOGY Helicobacter pylori n n Distal GC + association with atrophy Appears to be protective against procimal GC 1/ 97 infectet patients develop CG Inf: noninf=8: 1, ONLY CERTAIN FENOTYPES
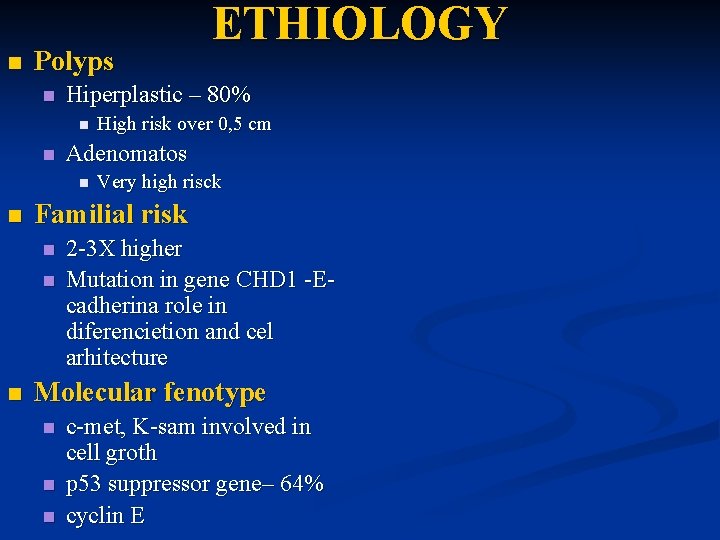
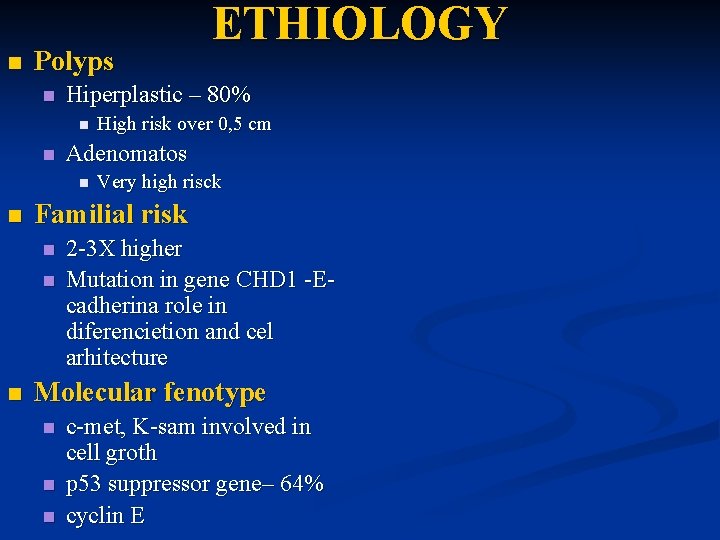
n Polyps n Hiperplastic – 80% n n Very high risck Familial risk n n n High risk over 0, 5 cm Adenomatos n n ETHIOLOGY 2 -3 X higher Mutation in gene CHD 1 -Ecadherina role in diferencietion and cel arhitecture Molecular fenotype n n n c-met, K-sam involved in cell groth p 53 suppressor gene– 64% cyclin E

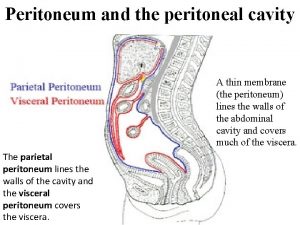
n n PATHOLOGY Intestinal n n Atrophy – metaplasia displasia – adenoma cancer Difuz – linitis plastica n Submucosal invasion
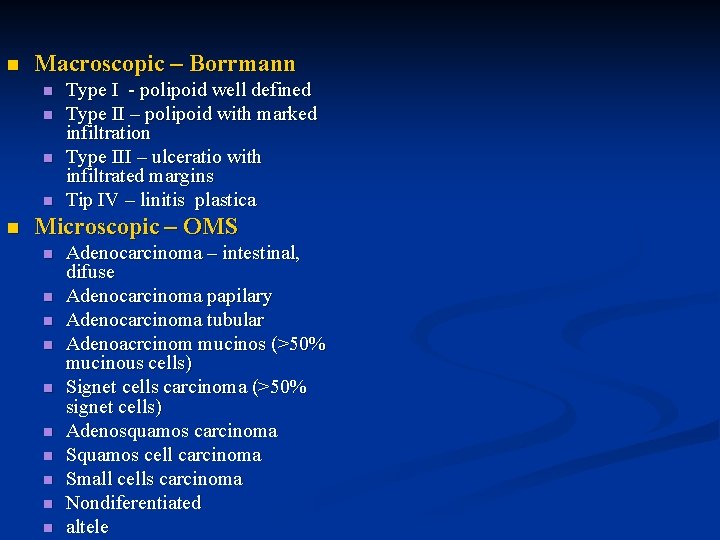
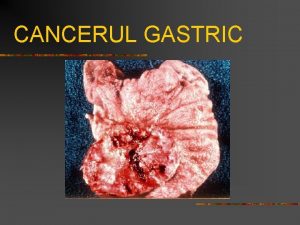
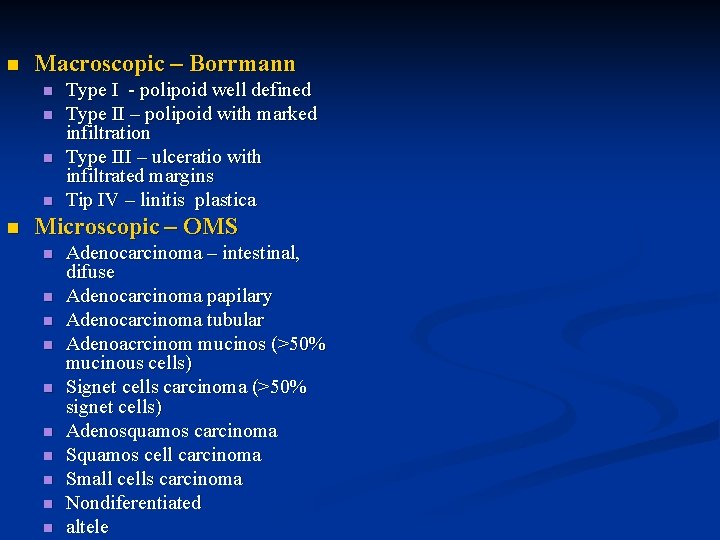
n Macroscopic – Borrmann n n Type I - polipoid well defined Type II – polipoid with marked infiltration Type III – ulceratio with infiltrated margins Tip IV – linitis plastica Microscopic – OMS n n n n n Adenocarcinoma – intestinal, difuse Adenocarcinoma papilary Adenocarcinoma tubular Adenoacrcinom mucinos (>50% mucinous cells) Signet cells carcinoma (>50% signet cells) Adenosquamos carcinoma Squamos cell carcinoma Small cells carcinoma Nondiferentiated altele


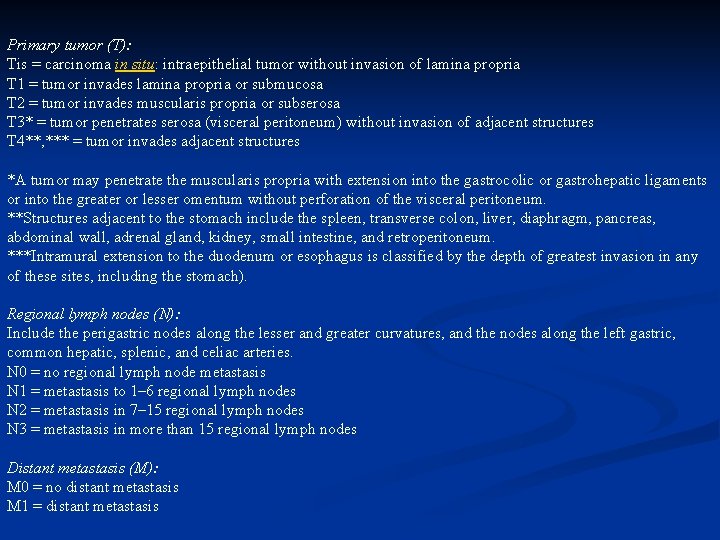
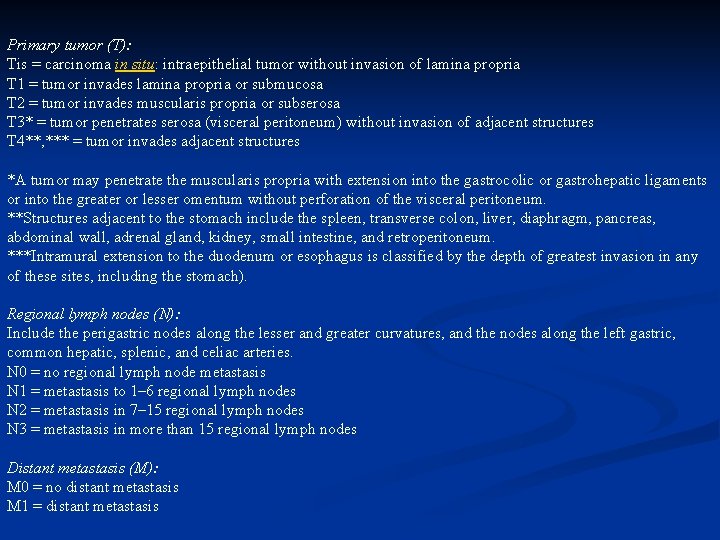
Primary tumor (T): Tis = carcinoma in situ: intraepithelial tumor without invasion of lamina propria T 1 = tumor invades lamina propria or submucosa T 2 = tumor invades muscularis propria or subserosa T 3* = tumor penetrates serosa (visceral peritoneum) without invasion of adjacent structures T 4**, *** = tumor invades adjacent structures *A tumor may penetrate the muscularis propria with extension into the gastrocolic or gastrohepatic ligaments or into the greater or lesser omentum without perforation of the visceral peritoneum. **Structures adjacent to the stomach include the spleen, transverse colon, liver, diaphragm, pancreas, abdominal wall, adrenal gland, kidney, small intestine, and retroperitoneum. ***Intramural extension to the duodenum or esophagus is classified by the depth of greatest invasion in any of these sites, including the stomach). Regional lymph nodes (N): Include the perigastric nodes along the lesser and greater curvatures, and the nodes along the left gastric, common hepatic, splenic, and celiac arteries. N 0 = no regional lymph node metastasis N 1 = metastasis to 1– 6 regional lymph nodes N 2 = metastasis in 7– 15 regional lymph nodes N 3 = metastasis in more than 15 regional lymph nodes Distant metastasis (M): M 0 = no distant metastasis M 1 = distant metastasis
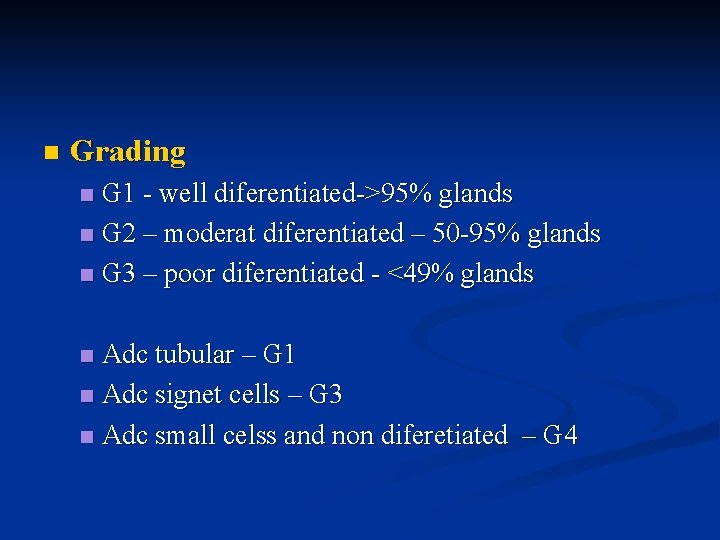
n Grading G 1 - well diferentiated->95% glands n G 2 – moderat diferentiated – 50 -95% glands n G 3 – poor diferentiated - <49% glands n Adc tubular – G 1 n Adc signet cells – G 3 n Adc small celss and non diferetiated – G 4 n

CLINICA PRESENTATION n Subjectiv n n Objectiv n n n n n General neoplastic simptoms Dispepsia UGI bleeding Tumor palpable Hepatomegaly, ascites, jaundice, splenomagaly Sister Mary Joseph – sign (umbilkical nodule) Virchow sign – left supraclavicular LN Krukenberg –ovarian MTS Blumer – rectal palpable mass Trousseau – migrating flebitis Leser-Trelat – seborheic keratitis Lab n n n Anemia Ocult bleeding ACE, CA 19. 9
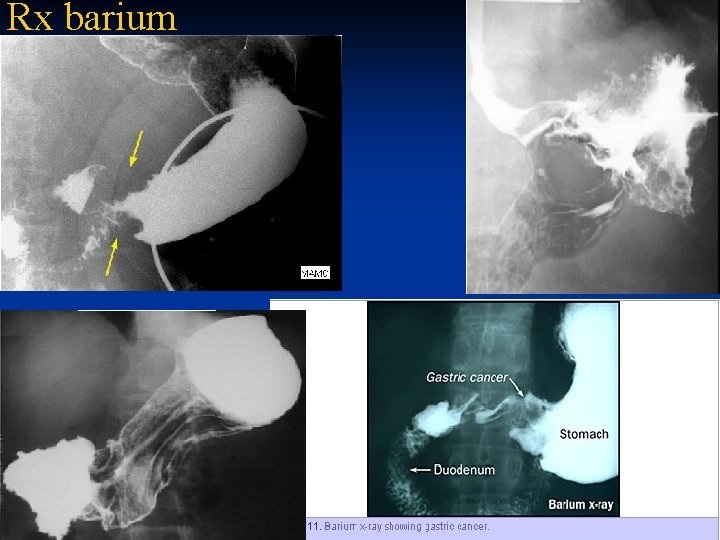
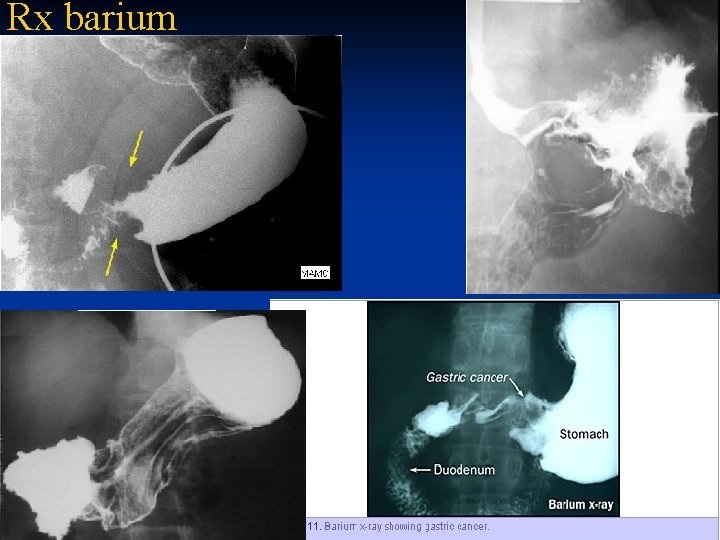
Rx barium

CT, MRI, echoendoscopy+biopsy brush citology, laparoscopy, lapro echography

COMPLICATIONS n Bleeding n Perforation n Obstruction n Penetration
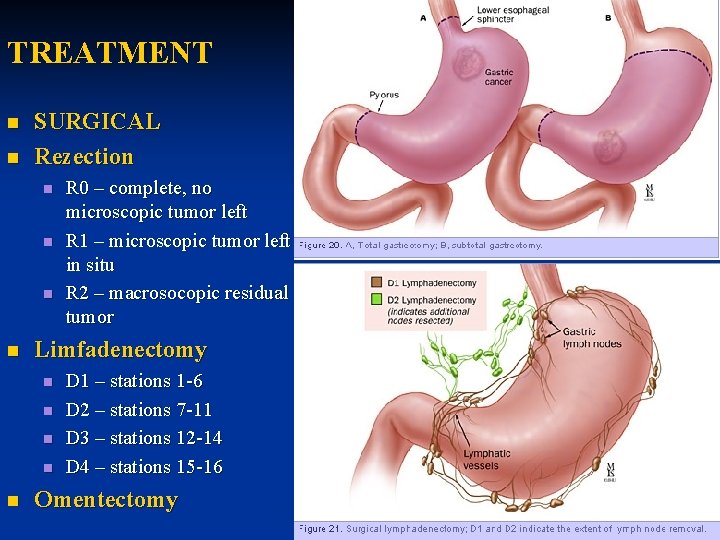
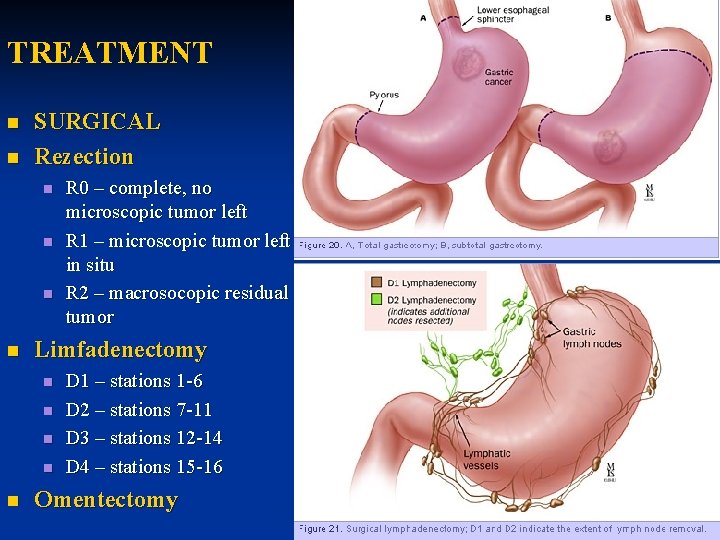
TREATMENT n n SURGICAL Rezection n n Limfadenectomy n n n R 0 – complete, no microscopic tumor left R 1 – microscopic tumor left in situ R 2 – macrosocopic residual tumor D 1 – stations 1 -6 D 2 – stations 7 -11 D 3 – stations 12 -14 D 4 – stations 15 -16 Omentectomy
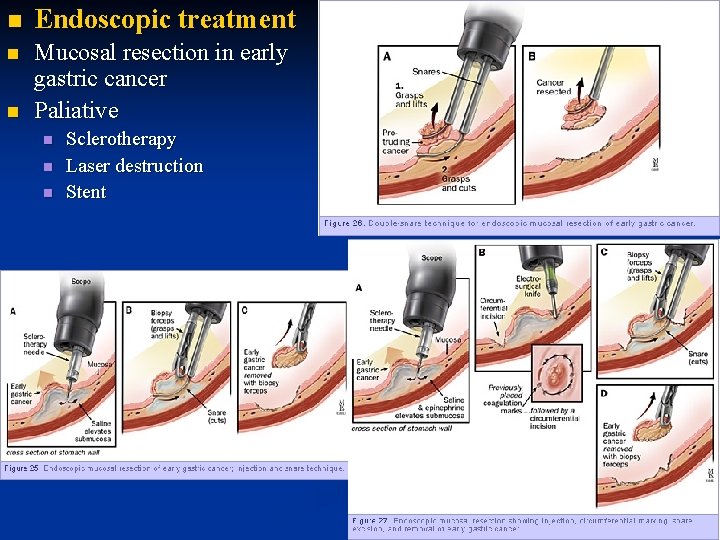
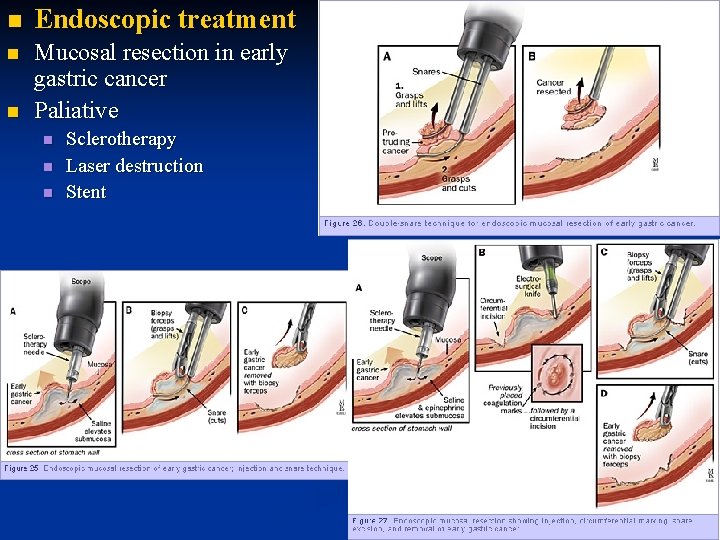
n Endoscopic treatment n Mucosal resection in early gastric cancer Paliative n n Sclerotherapy Laser destruction Stent


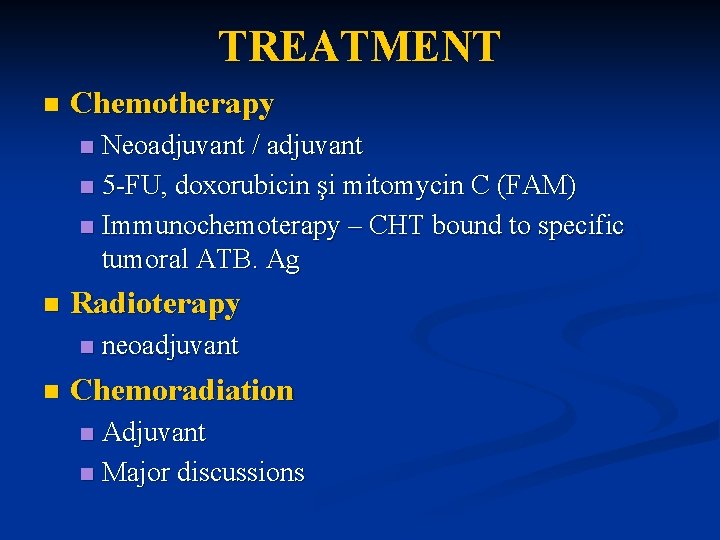
TREATMENT n Chemotherapy Neoadjuvant / adjuvant n 5 -FU, doxorubicin şi mitomycin C (FAM) n Immunochemoterapy – CHT bound to specific tumoral ATB. Ag n n Radioterapy n n neoadjuvant Chemoradiation Adjuvant n Major discussions n
 Second position
Second position Borrmann classification
Borrmann classification Subtotal gastrectomy
Subtotal gastrectomy Stomach cancer symotoms
Stomach cancer symotoms Fundamental position vs anatomical position
Fundamental position vs anatomical position Fundamental position definition
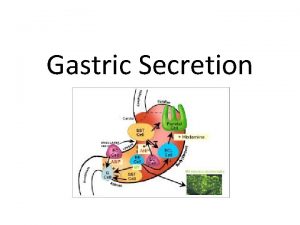
Fundamental position definition Chief cells secrete
Chief cells secrete Types of gastric ulcer
Types of gastric ulcer Sportello unico previdenziale
Sportello unico previdenziale Lymphatic drainage of stomach diagram
Lymphatic drainage of stomach diagram Erythrocytopenia prefix root suffix
Erythrocytopenia prefix root suffix Gastric secretion
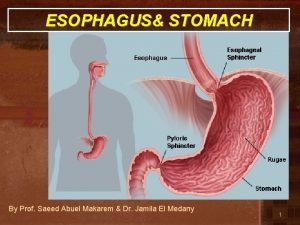
Gastric secretion Where is the stomach located at
Where is the stomach located at Aditus to lesser sac
Aditus to lesser sac Duodenal ulcer anatomy
Duodenal ulcer anatomy Transverse mesocolon
Transverse mesocolon Stomach ulcer definition
Stomach ulcer definition Heineke mikulicz pyloroplasty
Heineke mikulicz pyloroplasty Her2 gastric
Her2 gastric Chapter 15 elimination and gastric intubation
Chapter 15 elimination and gastric intubation Secretion of gastric juice
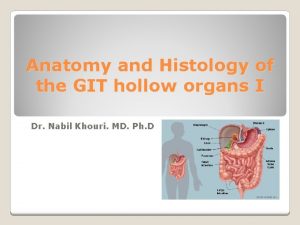
Secretion of gastric juice Compartments of the abdomen
Compartments of the abdomen Gastric folds
Gastric folds Duodemum
Duodemum