Chapter 11 Lecture Outline See separate Power Point



- Slides: 75
Chapter 11 Lecture Outline See separate Power. Point slides for all figures and tables pre-inserted into Power. Point without notes. Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display.
I. Endocrine Glands and Hormones

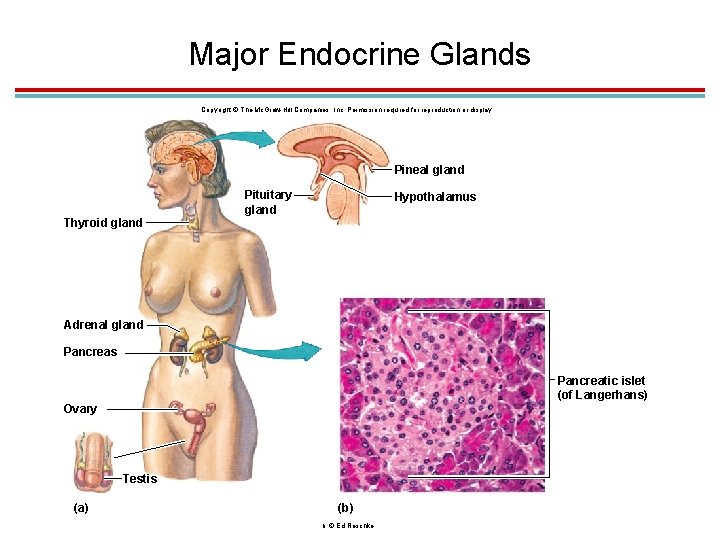
1. Endocrine Glands 1. Ductless 2. Secrete hormones into the blood 3. Hormones are carried to target cells having receptors for those hormones. 4. Many organs secrete hormones other than those discussed in this chapter such as the heart, liver, kidneys, and adipose tissue. 5. Neurohormones are secreted by specialized cells of the hypothalamus 6. Hormones help regulate body metabolism, growth, and reproduction
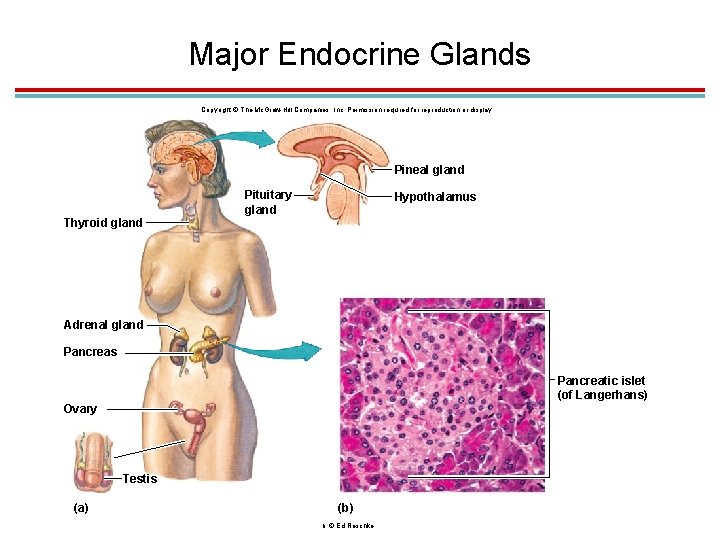
Major Endocrine Glands Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Pineal gland Thyroid gland Pituitary gland Hypothalamus Adrenal gland Pancreas Pancreatic islet (of Langerhans) Ovary Testis (a) (b) b: © Ed Reschke
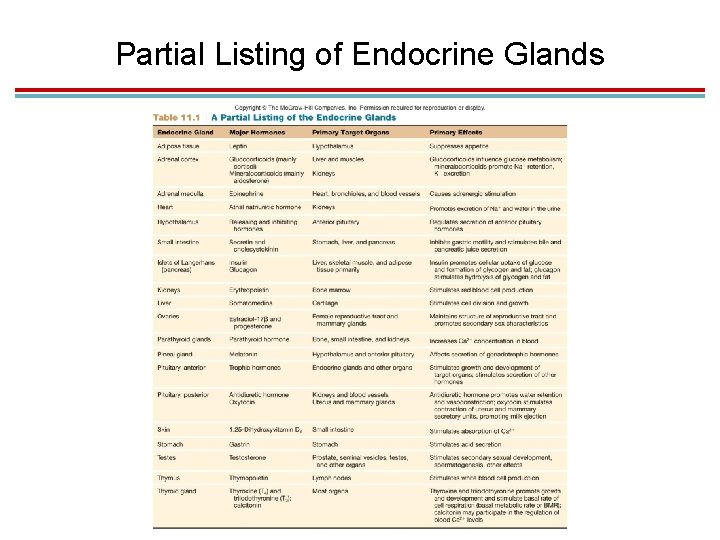
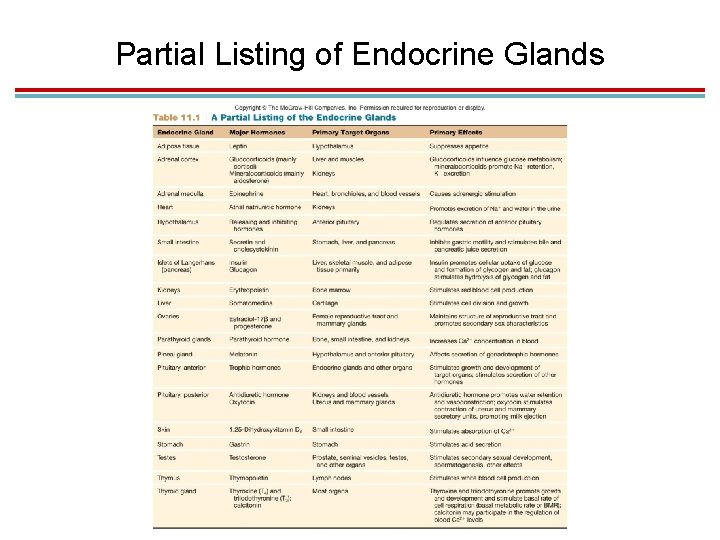
Partial Listing of Endocrine Glands
1. Chemical Classification of Hormones 1. ______, derived from tyrosine and tryptophan 1. Examples: hormones from the adrenal medulla, thyroid, and pineal glands 2. Polypeptides and proteins 1. Examples: antidiuretic hormone, insulin, and growth hormone
Chemical Classification of Hormones, cont 1. Glycoproteins are long polypeptides bound to a carbohydrate. 1. Examples: follicle-stimulating and luteinizing hormones 2. ____ are lipids derived from cholesterol 1. Examples: testosterone, estradiol, progesterone, cortisol 2. Secreted by adrenal cortex and gonads
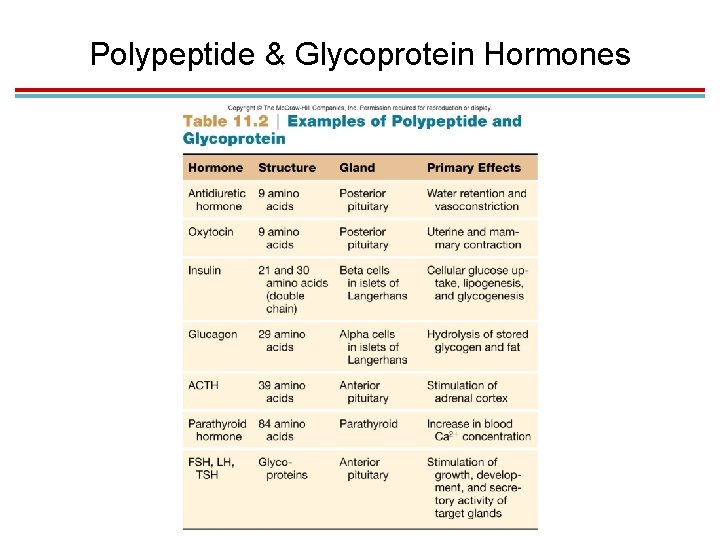
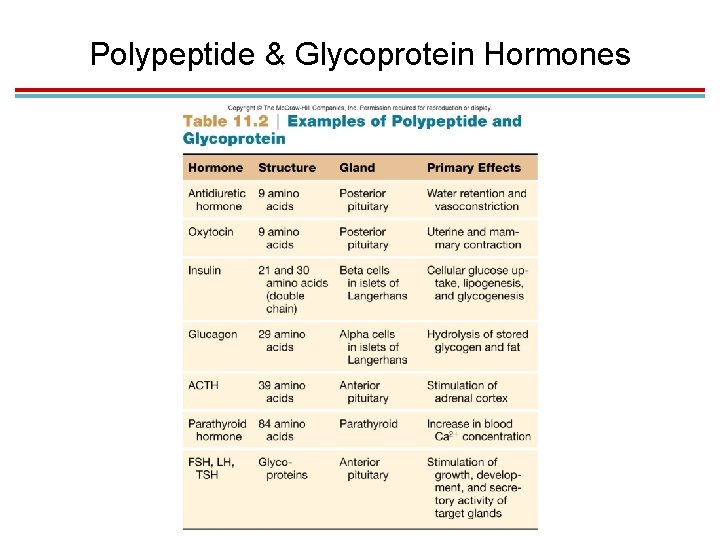
Polypeptide & Glycoprotein Hormones
1. Hormone Classifications by action 1. Polar hormones: water soluble 1. Cannot pass through plasma membranes 2. Must be injected if used as a drug 3. Includes polypeptides, glycoproteins, catecholamines, norepinephrine, and epinephrine 2. Nonpolar: insoluble in water 1. Often called lipophilic hormones 2. Can enter target cells directly 3. Include steroids, thyroid hormone, and melatonin 4. Can be taken orally in pill form
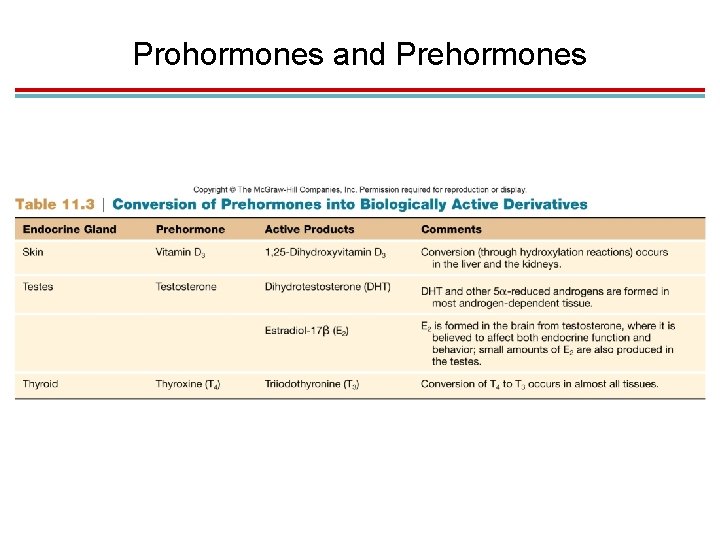
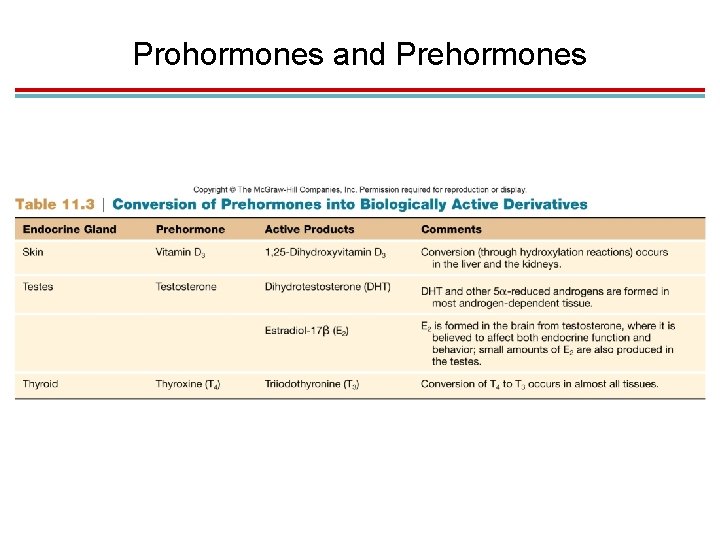
1. Prohormones and Prehormones 1. Prohormones are inactive hormones that must be cut and spliced together to be active. 1. Example: insulin 2. Prehormones are inactive prohormones that must be modified within their target cells.
Prohormones and Prehormones
1. Common Aspects of Neural & Endocrine Regulation 1. Hormones and neurotransmitters both interact with specific receptors. 2. Binding to a receptor causes a change within the cell. 3. There are mechanisms to turn off target cell activity; the signal is either removed or inactivated. 4. Neurotransmitters and hormones have many similarities 5. Some hormones can also be neurotransmitters in the CNS
II. Mechanisms of Hormone Action
Introduction 1. Hormones bind to receptors on or in target cells. 1. Binding is highly specific. 2. Hormones bind to receptors with a high affinity. 3. Hormones bind to receptors with a low capacity; saturating the receptors with hormone molecules 2. _____ hormone receptors are in the cytoplasm or nucleus 3. Water-soluble hormone receptors are on the outer surface of the plasma membrane
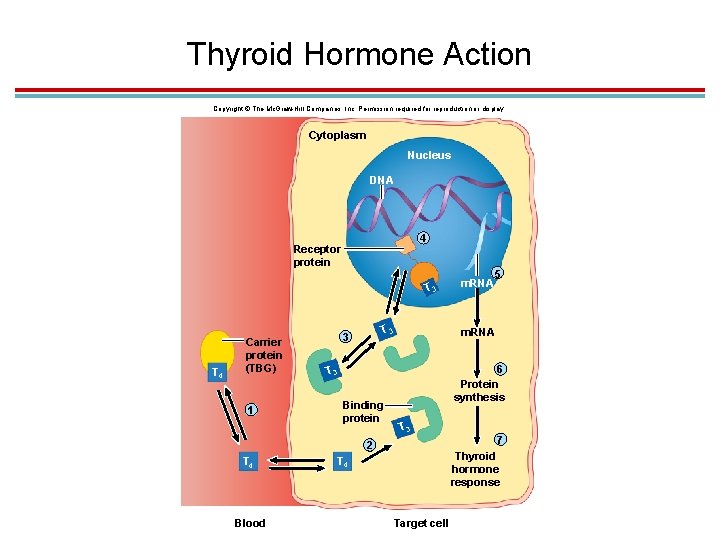
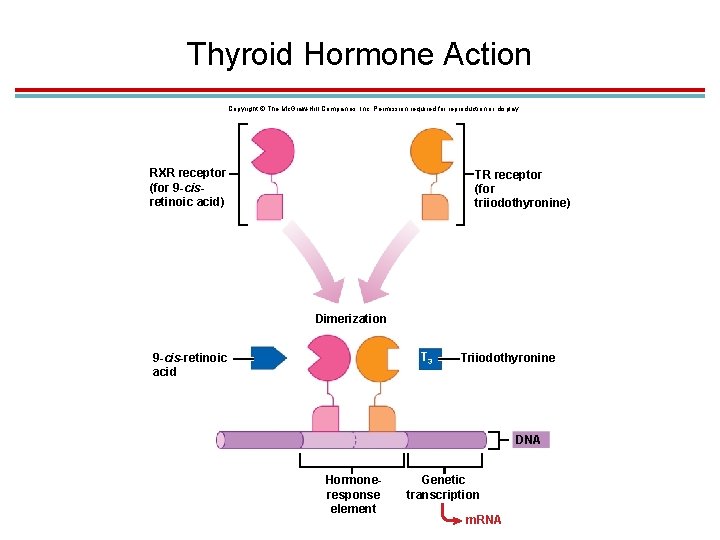
Thyroid Hormone Action 1. _____ (T 4) travels to target cells on thyroxine-binding globulin (TBG). 2. Some T 3 is also released, but is not bonded to a carrier; “free iodine” 3. Inside the target cell, T 4 is converted to T 3. 4. Receptor proteins are located inside the nucleus bound to DNA.
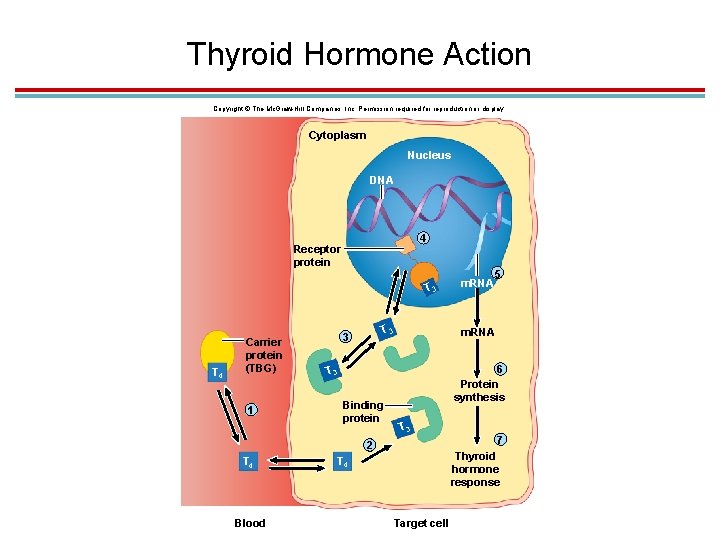
Thyroid Hormone Action Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Cytoplasm Nucleus DNA 4 Receptor protein T 3 T 4 Carrier protein (TBG) 1 T 3 3 6 Protein synthesis T 3 7 2 T 4 Blood 5 m. RNA T 3 Binding protein m. RNA Thyroid hormone response T 4 Target cell
Thyroid Hormone Action, cont 1. The hormone response element on the DNA has two half-sites, one for a T 3 receptor and one for a 9 -cis-retinoic acid receptor (a Vit A derivative). 2. Binding of these molecules forms a heterodimer because there are two different receptors 3. The binding of T 3 will cause corepressor proteins to be removed and coactivator proteins to be recruited. 4. Vitamin D action in the cell is similar.
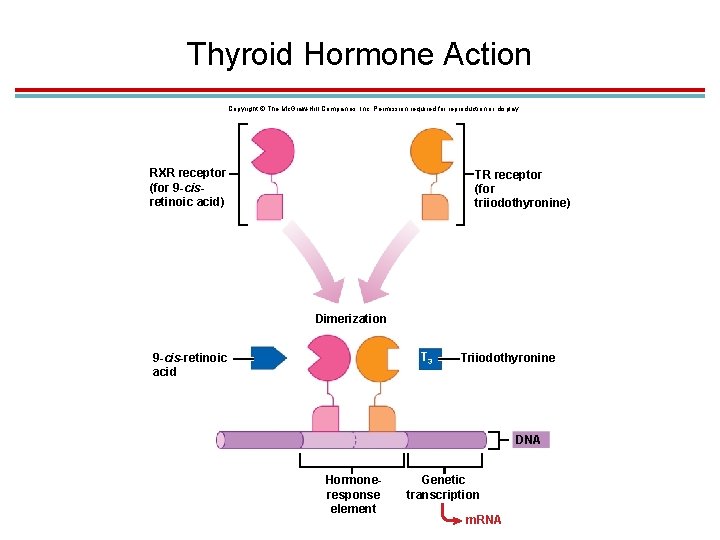
Thyroid Hormone Action Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. RXR receptor (for 9 -cisretinoic acid) TR receptor (for triiodothyronine) Dimerization T 3 9 -cis-retinoic acid Triiodothyronine DNA Hormoneresponse element Genetic transcription m. RNA
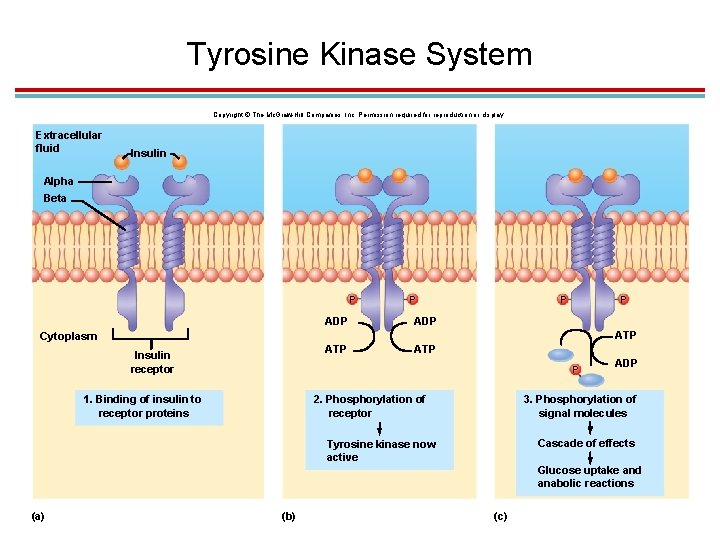
Tyrosine Kinase System 1. Insulin and growth factors uses this system 2. The receptor is also the enzyme tyrosine kinase. 3. The ligand-binding site is on the outside of the cell, and the enzyme faces the cytoplasm. 4. The enzyme portion is activated via phosphorylation. 5. The activated receptor phosphorylates insulin receptor substrate molecules. 6. This activates a cascade of enzymatic activity.
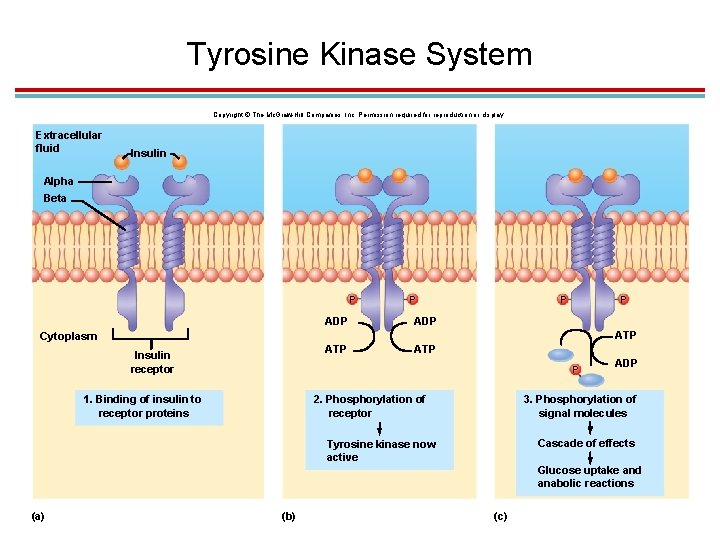
Tyrosine Kinase System Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Extracellular fluid Insulin Alpha Beta P ADP ATP Cytoplasm ATP Insulin receptor ATP P 1. Binding of insulin to receptor proteins 2. Phosphorylation of receptor ADP 3. Phosphorylation of signal molecules Cascade of effects Tyrosine kinase now active Glucose uptake and anabolic reactions (a) (b) (c)
III. Pituitary Gland
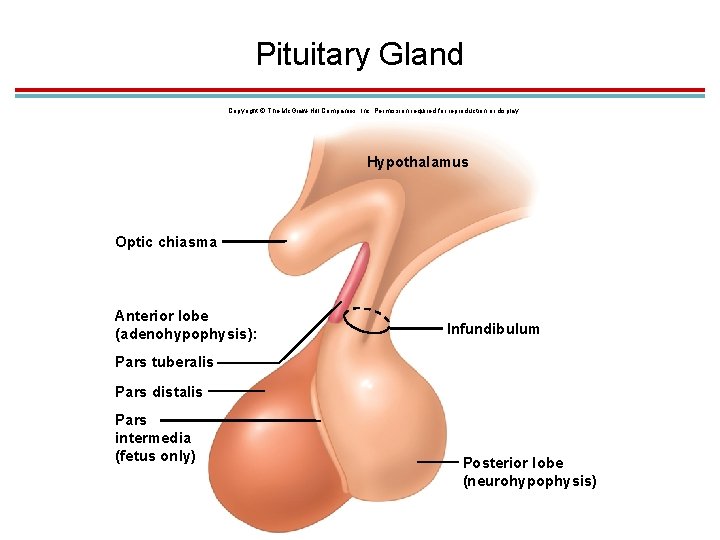
1. Introduction 1. The pituitary gland is attached to the hypothalamus by the infundibulum 2. Divided into an anterior lobe (________) and a posterior lobe (neurohypophysis) 1. The anterior pituitary is glandular epithelium with two parts – pars distalis and pars tuberalis 2. The posterior pituitary is nervous tissue and also called the pars nervosa
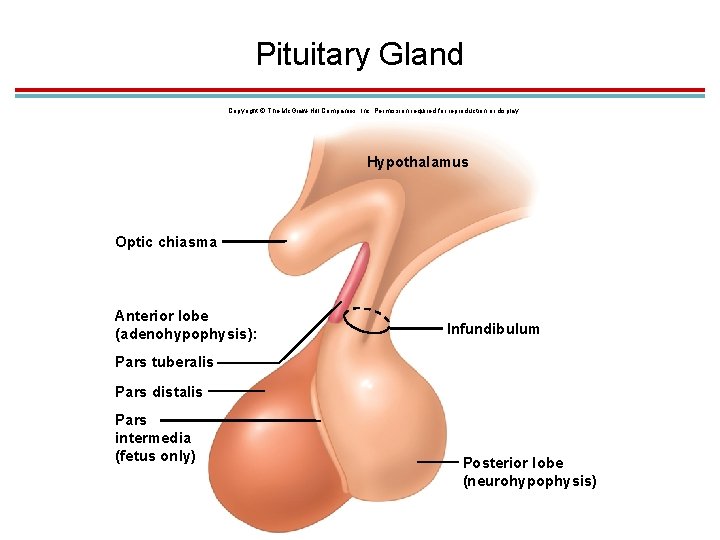
Pituitary Gland Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Hypothalamus Optic chiasma Anterior lobe (adenohypophysis): Infundibulum Pars tuberalis Pars distalis Pars intermedia (fetus only) Posterior lobe (neurohypophysis)
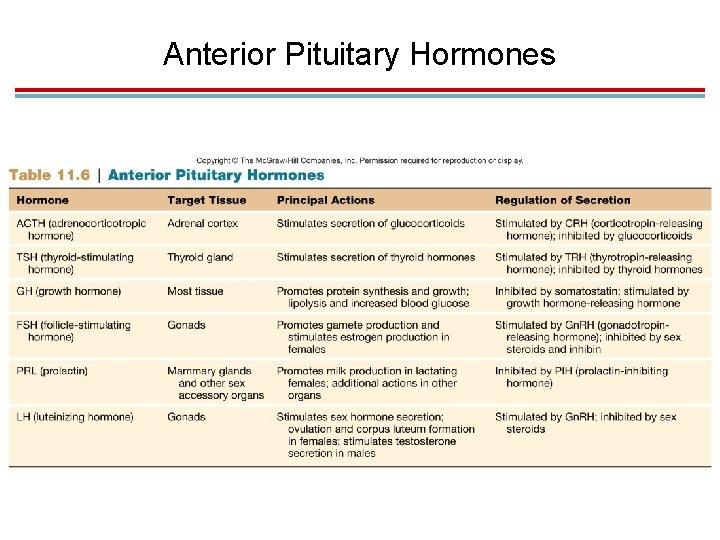
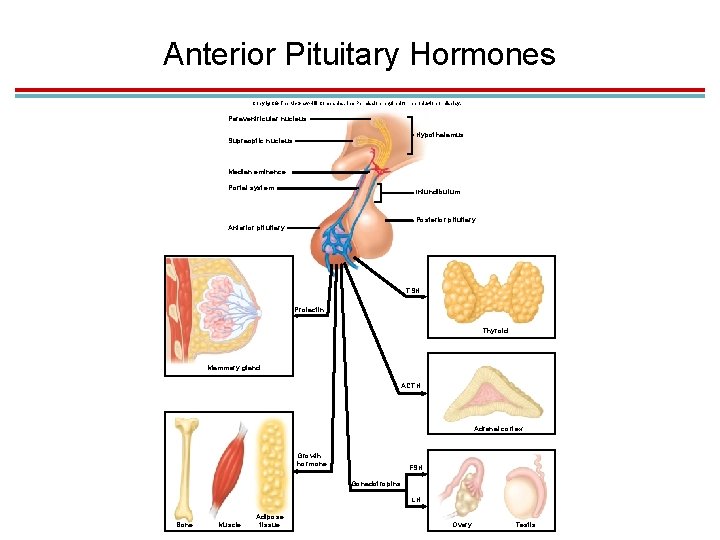
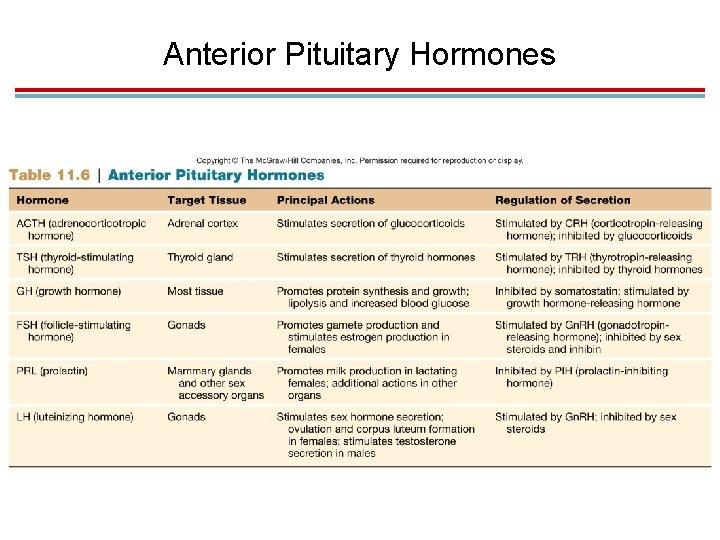
1. Pituitary Hormones 1. Secreted by the anterior lobe 2. Trophic hormones stimulate hormone secretion in other glands: 1. Growth hormone (GH) 2. Thyroid-stimulating hormone (TSH) 3. Adrenocorticotropic hormone (ACTH) 4. Follicle-stimulating hormone (FSH) 5. Luteinizing hormone (LH) – in the male, it is interstitial cell stimulating hormone (ICSH) 6. Prolactin (PRL)
Anterior Pituitary Hormones
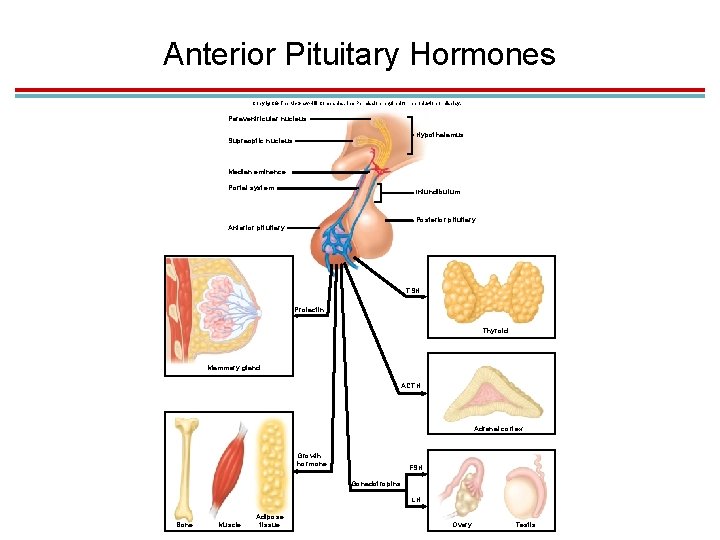
Anterior Pituitary Hormones Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Paraventricular nucleus Hypothalamus Supraoptic nucleus Median eminence Portal system Infundibulum Posterior pituitary Anterior pituitary TSH Prolactin Thyroid Mammary gland ACTH Adrenal cortex Growth hormone FSH Gonadotropins LH Bone Muscle Adipose tissue Ovary Testis
1. Posterior Pituitary Hormones 1. Stores and releases two hormones made in the hypothalamus: 1. Antidiuretic hormone (ADH), which promotes the retention of water in the kidneys (also called arginine vasopressin – AVP) 2. ____, which stimulates contractions in childbirth and milk let-down in lactation
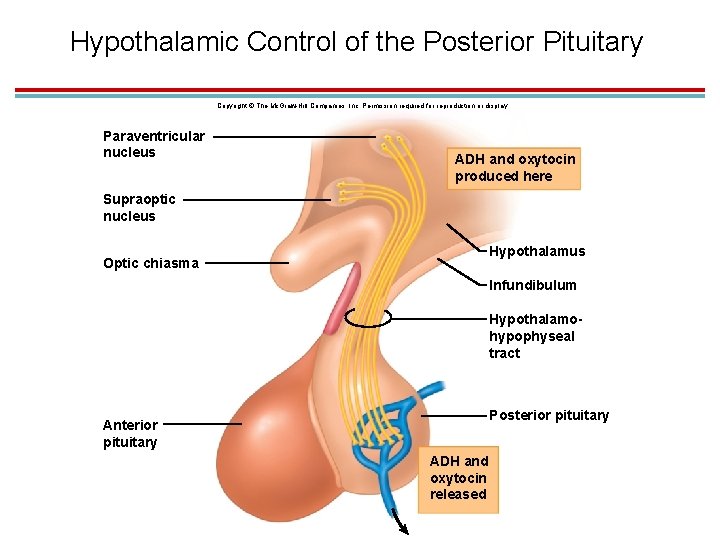
1. Hypothalamic Control of the Posterior Pituitary 1. ADH and oxytocin are produced by the supraoptic and paraventricular nuclei of the hypothalamus, respectively 2. They are transported along axons of the hypothalamo-hypophyseal tract to the posterior pituitary where they are stored. 3. Release is controlled by neuroendocrine reflexes. 1. ADH is stimulated by an increase in blood osmolality 2. Oxytocin is stimulated by suckling
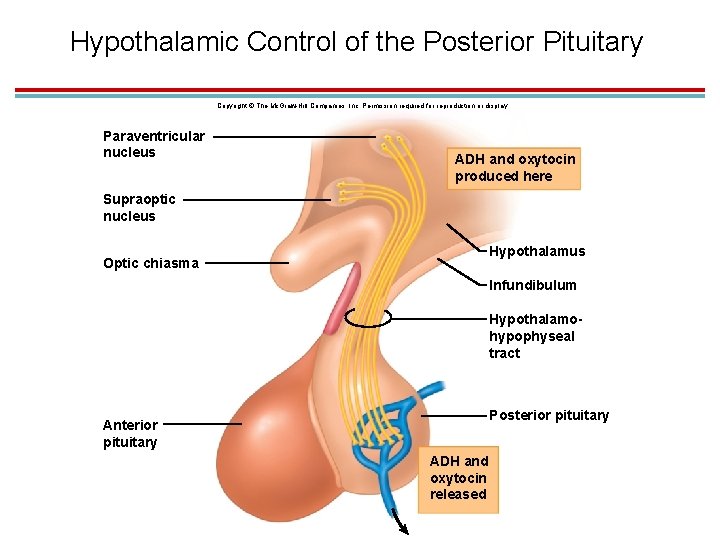
Hypothalamic Control of the Posterior Pituitary Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Paraventricular nucleus ADH and oxytocin produced here Supraoptic nucleus Hypothalamus Optic chiasma Infundibulum Hypothalamohypophyseal tract Posterior pituitary Anterior pituitary ADH and oxytocin released
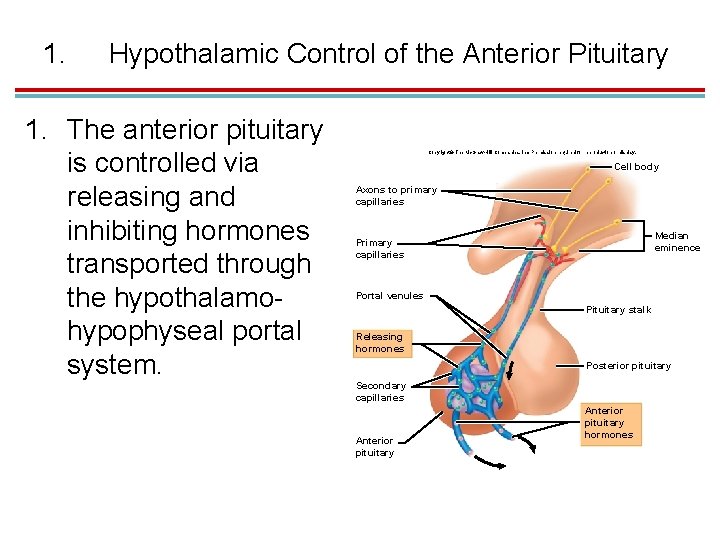
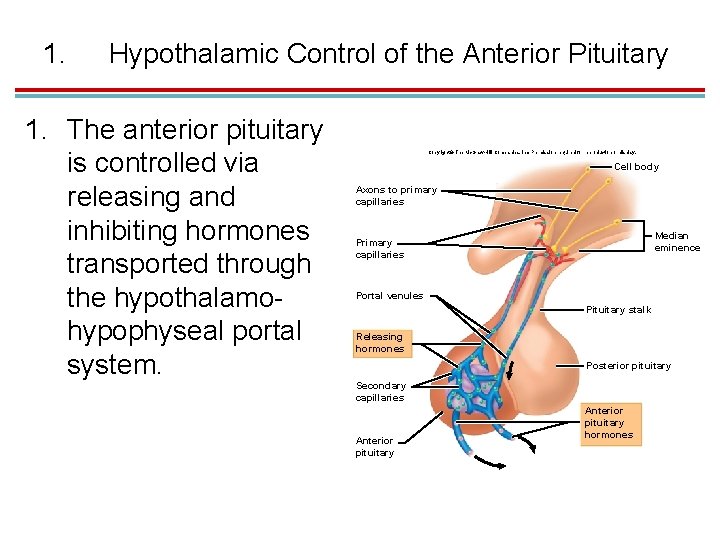
1. Hypothalamic Control of the Anterior Pituitary 1. The anterior pituitary is controlled via releasing and inhibiting hormones transported through the hypothalamohypophyseal portal system. Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Cell body Axons to primary capillaries Median eminence Primary capillaries Portal venules Pituitary stalk Releasing hormones Posterior pituitary Secondary capillaries Anterior pituitary hormones
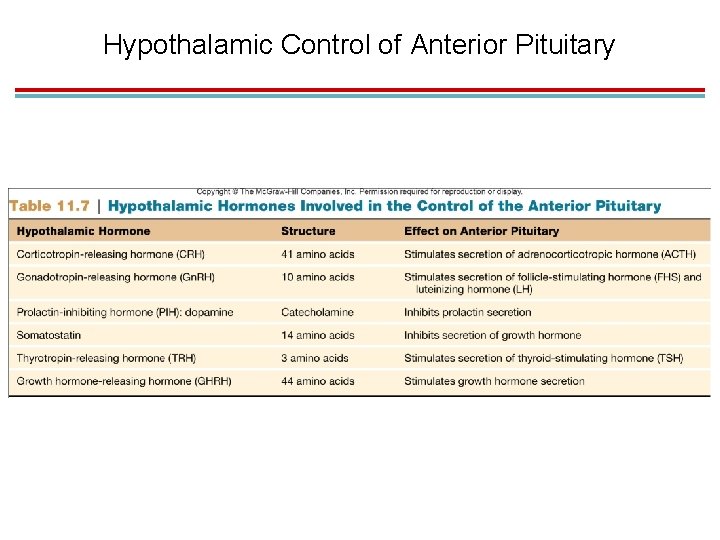
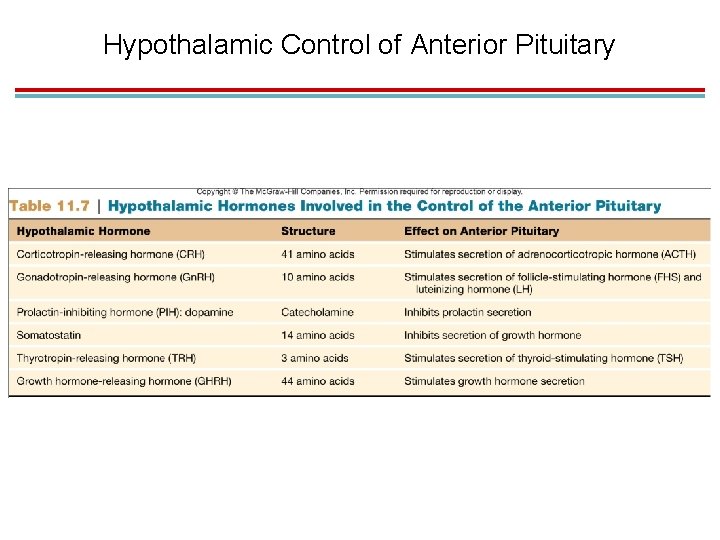
Hypothalamic Control of Anterior Pituitary, cont 1. Releasing and inhibiting hormones 1. Corticotropin-releasing hormone (CRH) 2. Gonadotropin-releasing hormone (GRH) 3. Prolactin-inhibiting hormone (PIH) (dopamine) 4. Somatostatin 5. Thyrotropin-releasing hormone (TRH) 6. Growth hormone−releasing hormone (GHRH)
Hypothalamic Control of Anterior Pituitary
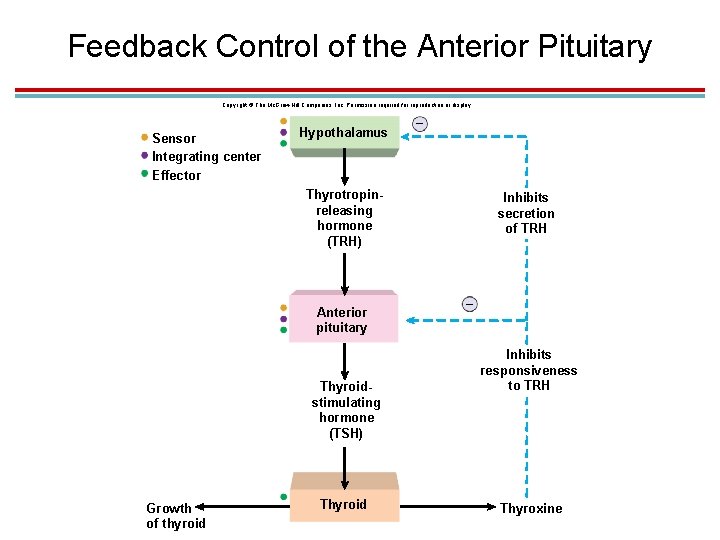
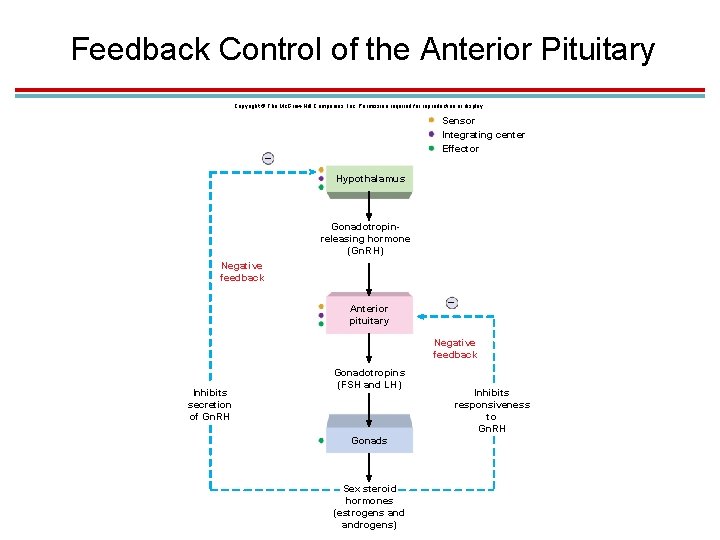
1. Feedback control of the anterior pituitary 1. The final product regulates secretion of pituitary hormones – negative feedback inhibition 2. The relationship between the hypothalamus, anterior pituitary, , and the target tissue is called an axis 3. Inhibition can occur at the pituitary gland level, inhibiting response to hypothalamic hormones. 4. Inhibition can occur at the hypothalamus level, inhibiting secretion of releasing hormones.
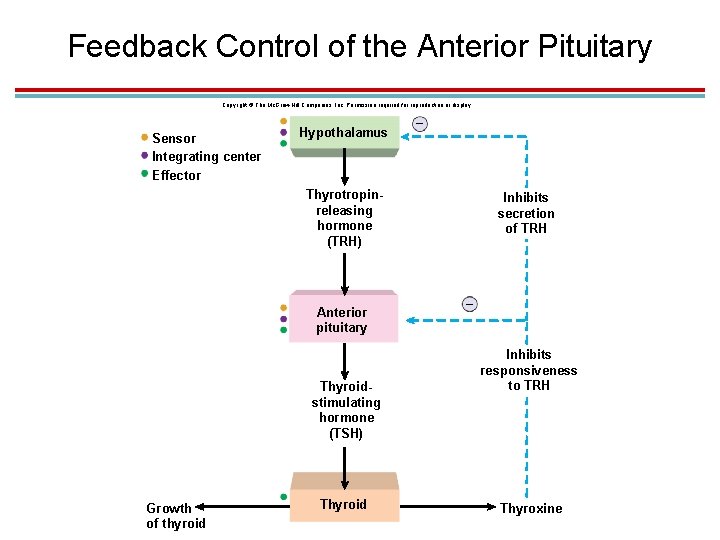
Feedback Control of the Anterior Pituitary Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Sensor Integrating center Effector Hypothalamus – Thyrotropinreleasing hormone (TRH) Anterior pituitary Thyroidstimulating hormone (TSH) Growth of thyroid Thyroid Inhibits secretion of TRH – Inhibits responsiveness to TRH Thyroxine
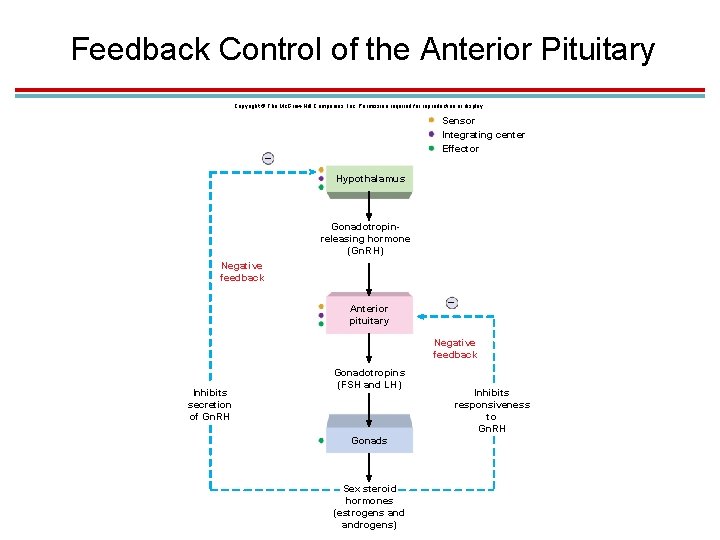
Feedback Control of the Anterior Pituitary Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Sensor Integrating center Effector – Hypothalamus Gonadotropinreleasing hormone (Gn. RH) Negative feedback Anterior pituitary – Negative feedback Inhibits secretion of Gn. RH Gonadotropins (FSH and LH) Gonads Sex steroid hormones (estrogens androgens) Inhibits responsiveness to Gn. RH
1. Higher Brain Controls 1. Since the hypothalamus receives input from higher brain regions, emotions can alter hormone secretion. 1. At least 26 brain regions and olfactory neurons send axons to the Gn. RH-producing neurons. 2. Stressors increase CRH production as part of the pituitary-adrenal axis 3. Circadian rhythms

IV. Adrenal Glands
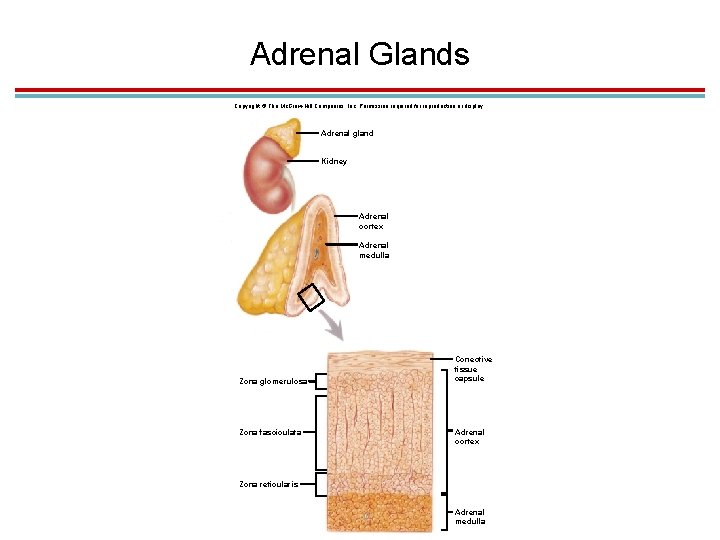
1. Structure of the Adrenal Glands 1. Found atop the kidneys 2. Consist of an outer adrenal cortex and an inner adrenal medulla that function as separate glands 1. The adrenal medulla is neural tissue and secretes epinephrine and norepinephrine in response to sympathetic neural stimulation. 2. The adrenal cortex is glandular epithelium and secretes steroid hormones in response to ACTH; three layers – zona glomerulosa, zona fasciculata, and zona reticularis
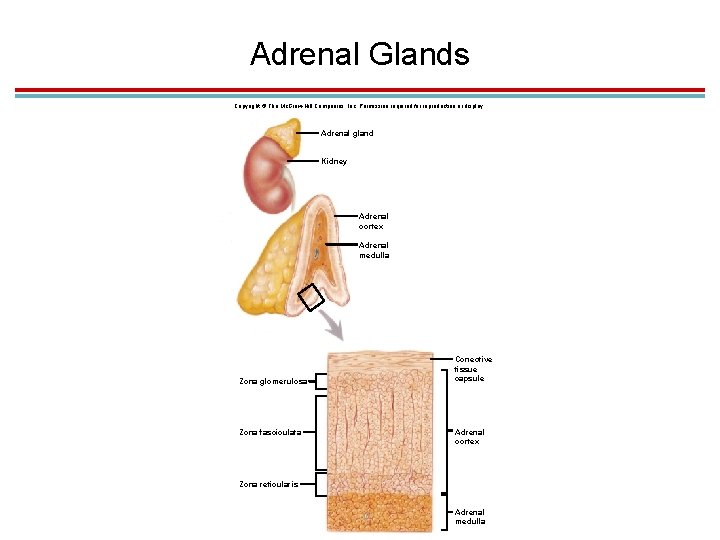
Adrenal Glands Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Adrenal gland Kidney Adrenal cortex Adrenal medulla Zona glomerulosa Zona fasciculata Conective tissue capsule Adrenal cortex Zona reticularis Adrenal medulla
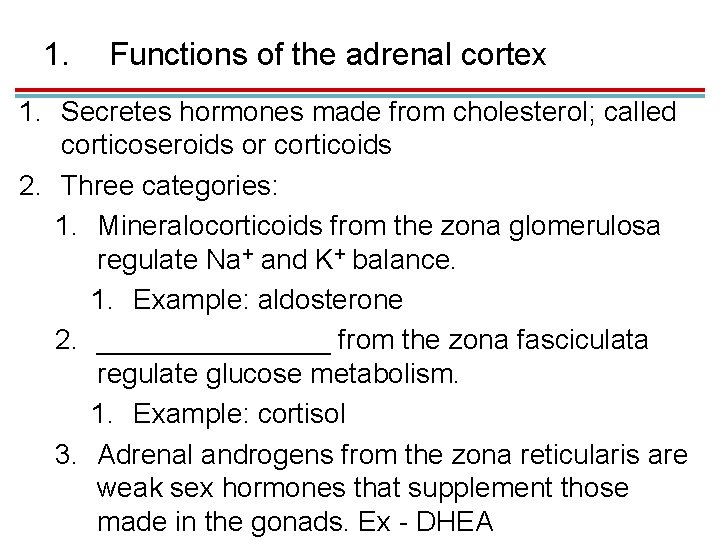
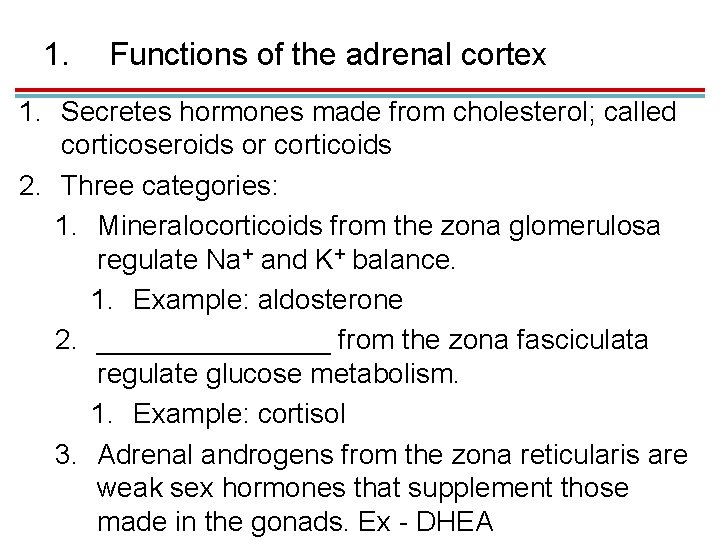
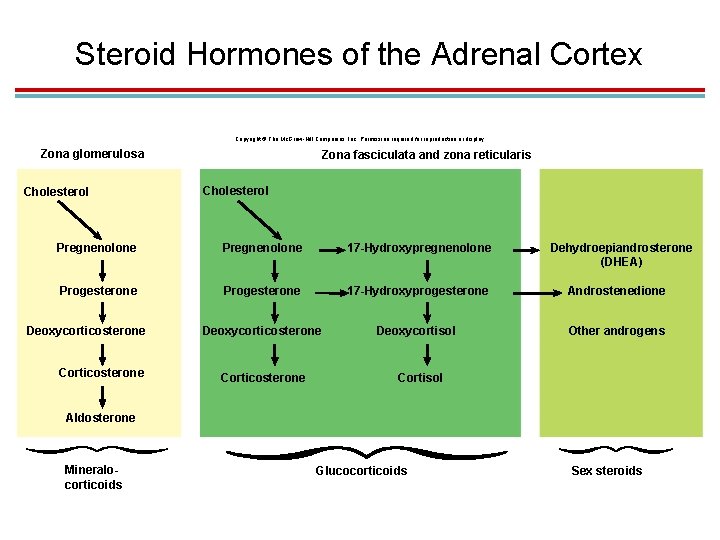
1. Functions of the adrenal cortex 1. Secretes hormones made from cholesterol; called corticoseroids or corticoids 2. Three categories: 1. Mineralocorticoids from the zona glomerulosa regulate Na+ and K+ balance. 1. Example: aldosterone 2. ________ from the zona fasciculata regulate glucose metabolism. 1. Example: cortisol 3. Adrenal androgens from the zona reticularis are weak sex hormones that supplement those made in the gonads. Ex - DHEA
3. Functions of cortisol (hydrocortisone) 1. Stimulates protein degradation 2. Stimulates gluconeogenesis and inhibits glucose utilization to raise blood glucose levels 3. Stimulates lipolysis 1. Exogenous glucocorticoids are used medically to suppress immune response and inhibit inflammation; can have many negative side effects
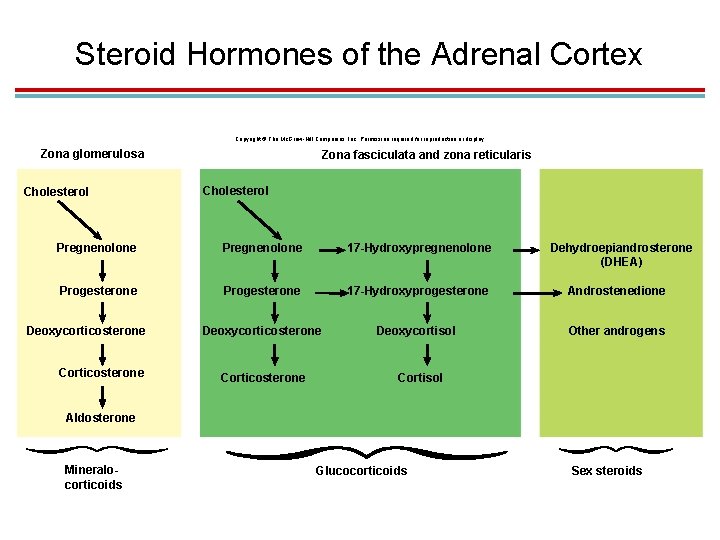
Steroid Hormones of the Adrenal Cortex Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Zona glomerulosa Cholesterol Zona fasciculata and zona reticularis Cholesterol Pregnenolone 17 -Hydroxypregnenolone Progesterone 17 -Hydroxyprogesterone Androstenedione Deoxycorticosterone Deoxycortisol Other androgens Deoxycorticosterone Corticosterone Dehydroepiandrosterone (DHEA) Cortisol Aldosterone Mineralocorticoids Glucocorticoids Sex steroids
1. Functions of the Adrenal Medulla 1. Epinephrine and norepinephrine 1. Activated with sympathetic response 2. Have effects similar to sympathetic innervation but lasting 10 times longer 3. Increase cardiac output, respiratory rate, and mental alertness; dilate coronary blood vessels; elevate metabolic rates
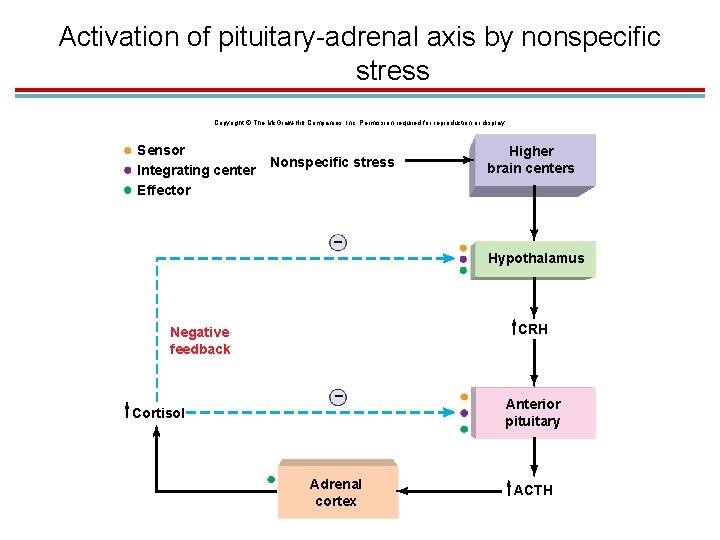
1. Stress and the Adrenal Gland 1. Stress increases secretion of ACTH, which results in increased glucocorticoid release. 2. The stress hormones are glucocorticoids, epinephrine, and CRH 3. Called the general adaptation syndrome (GAS). 1. Good for proper recovery after stress, such as an illness or trauma. 2. Cortisol helps inhibit the immune system so it does not overrespond.
Stress and the Adrenal Gland, cont 1. Chronic stress leads to an increased risk of illness. 1. Cortisol may act on higher brain regions, contributing to depression and anxiety and memory. 2. By stimulating the liver to release glucose, insulin receptors may become resistant, making it harder to treat people with diabetes.
1. Stages of GAS 1. Alarm reaction – activates the adrenal glands 2. Stage of resistance – readjustments in response 3. Stage of exhaustion – may lead to sickness or death 1. GAS effects 1. Stimulates growth of adrenal glands 2. Atrophy of lymphatic tissue of spleen, lymph nodes, and thymus 3. Formation of bleeding peptic ulcers
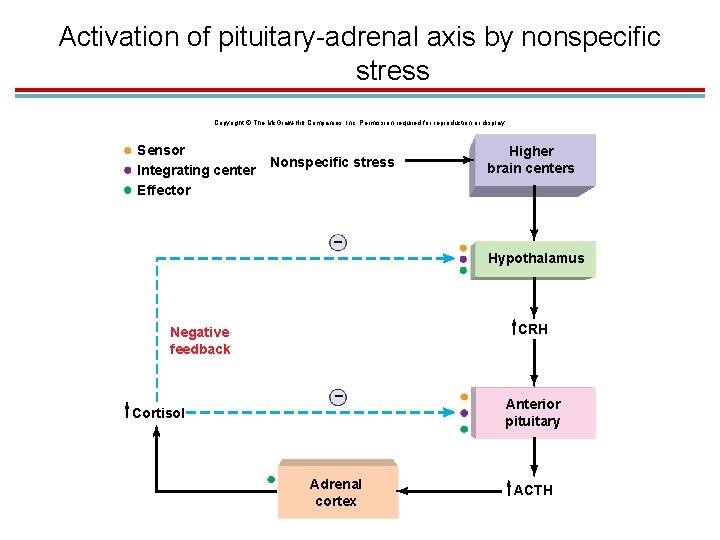
Activation of pituitary-adrenal axis by nonspecific stress Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Sensor Integrating center Effector Nonspecific stress Higher brain centers – Hypothalamus CRH Negative feedback – Cortisol Adrenal cortex Anterior pituitary ACTH
V. Thyroid and Parathyroid Glands
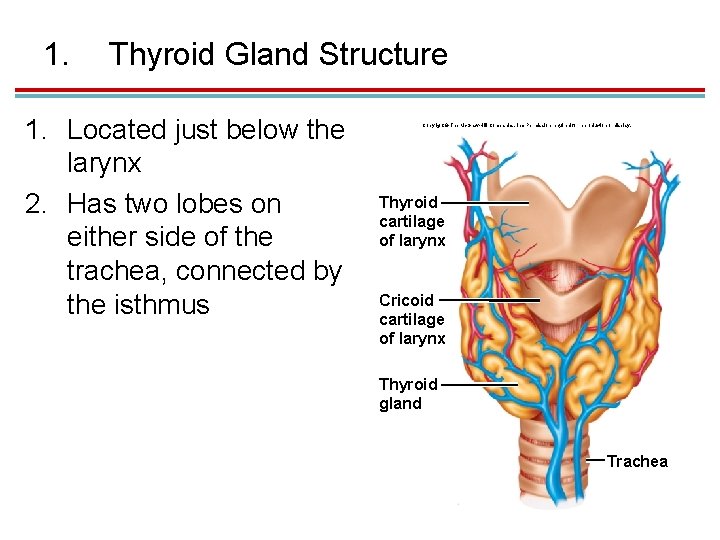
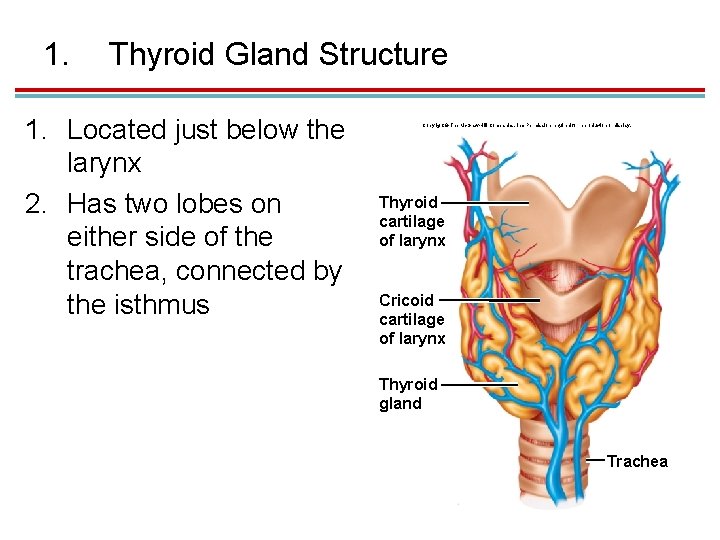
1. Thyroid Gland Structure 1. Located just below the larynx 2. Has two lobes on either side of the trachea, connected by the isthmus Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Thyroid cartilage of larynx Cricoid cartilage of larynx Thyroid gland Trachea
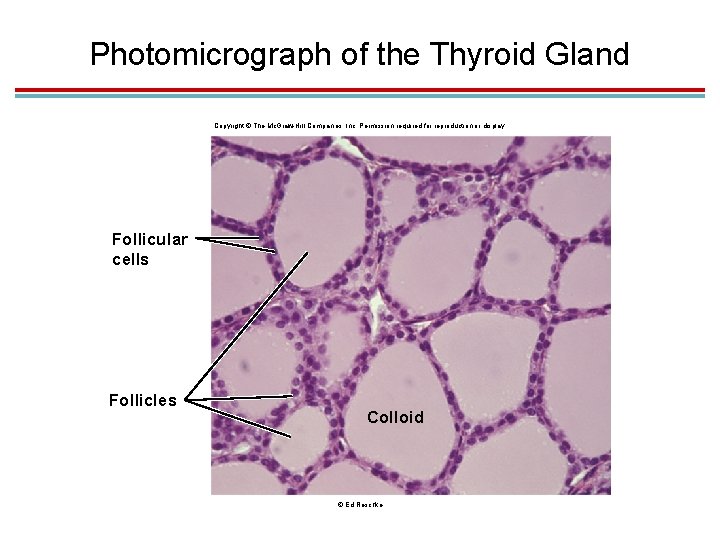
1. Microscopic Thyroid Gland Structure 1. Consists of hollow spaces called thyroid follicles lined with simple cuboidal epithelium composed of follicular cells that produce thyroxine 2. Interior of the follicles is filled with a fluid called colloid. 3. Outside of the follicles are parafollicular cells that secrete calcitonin
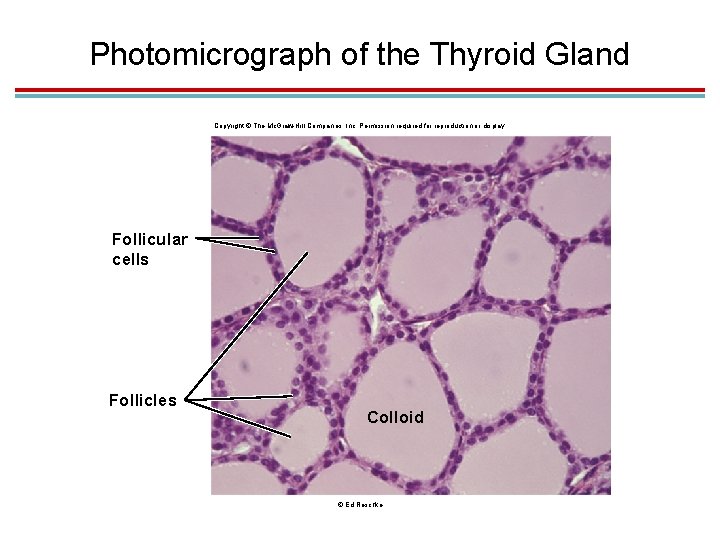
Photomicrograph of the Thyroid Gland Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Follicular cells Follicles Colloid © Ed Reschke

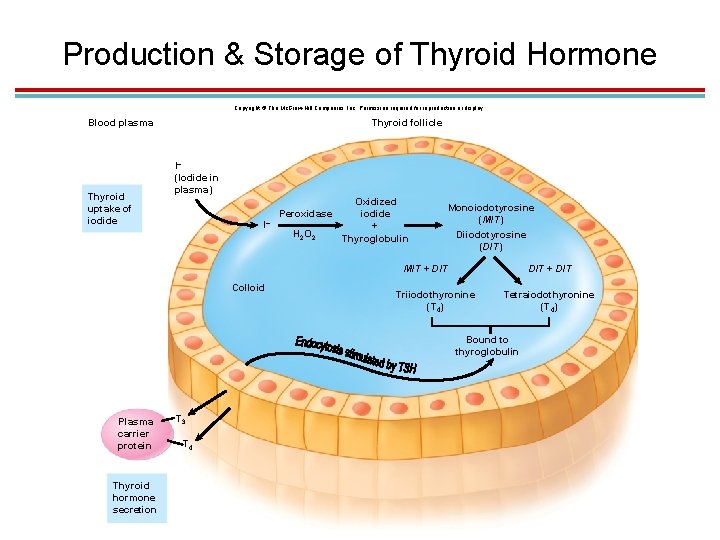
1. Production & Action of Thyroid Hormone 1. Thyroglobulin is made by the follicular cells. 1. Thyroid follicles actively accumulate iodide (I-) and secrete it into the colloid. 2. The iodine is attached to tyrosines within the thyroglobulin molecule. 1. One iodine produces monoiodotyrosine (MIT). 2. Two iodines produce diiodotyrosine (DIT).
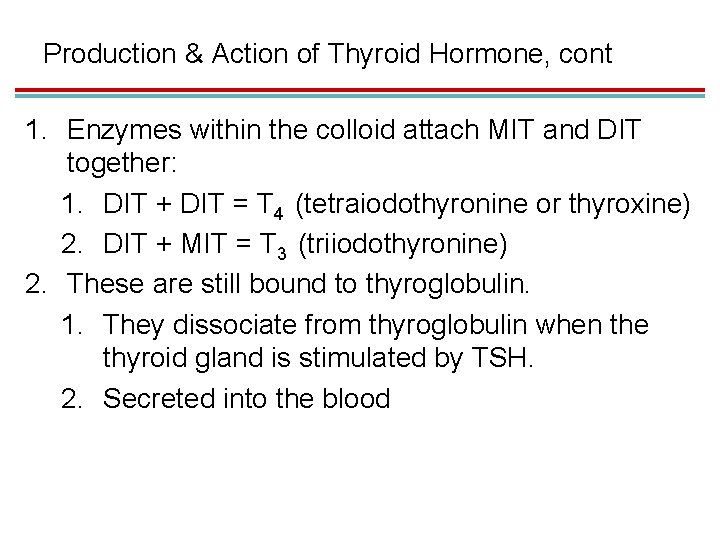
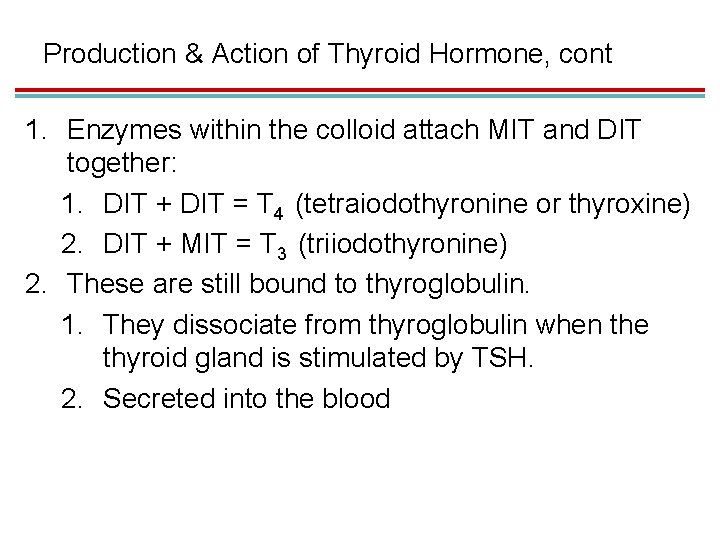
Production & Action of Thyroid Hormone, cont 1. Enzymes within the colloid attach MIT and DIT together: 1. DIT + DIT = T 4 (tetraiodothyronine or thyroxine) 2. DIT + MIT = T 3 (triiodothyronine) 2. These are still bound to thyroglobulin. 1. They dissociate from thyroglobulin when the thyroid gland is stimulated by TSH. 2. Secreted into the blood
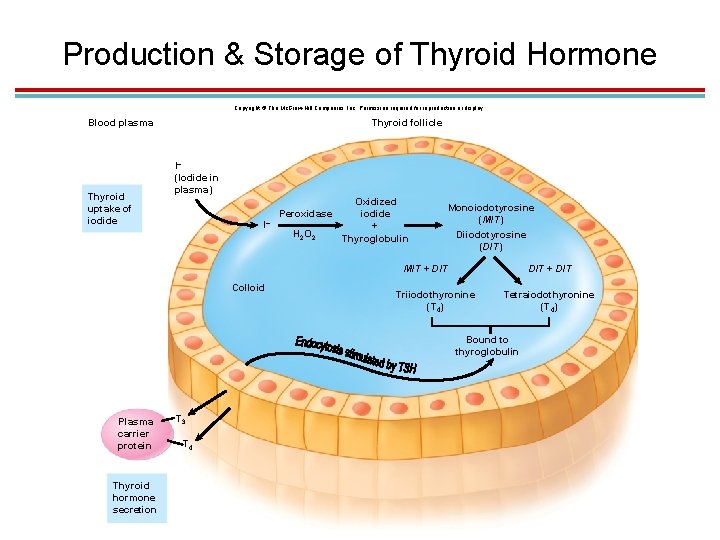
Production & Storage of Thyroid Hormone Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Blood plasma Thyroid uptake of iodide Thyroid follicle I– (Iodide in plasma) I– Peroxidase H 2 O 2 Oxidized iodide + Thyroglobulin Monoiodotyrosine (MIT) Diiodotyrosine (DIT) MIT + DIT Colloid DIT + DIT Triiodothyronine (T 4) Tetraiodothyronine (T 4) Bound to thyroglobulin Plasma carrier protein Thyroid hormone secretion T 3 T 4
1. 1. 2. 3. 4. Action of Thyroid Hormone Stimulates protein synthesis Promotes maturation of the nervous system Increases rates of cellular respiration Elevates basal metabolic rate
1. Calcitonin 1. Made by the parafollicular cells 2. Inhibits dissolution of calcium from bone and stimulates excretion of calcium in the kidneys to lower blood calcium levels
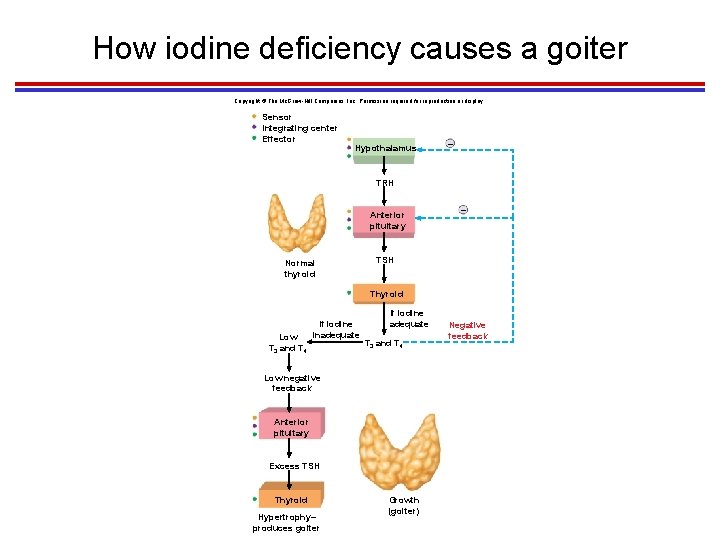
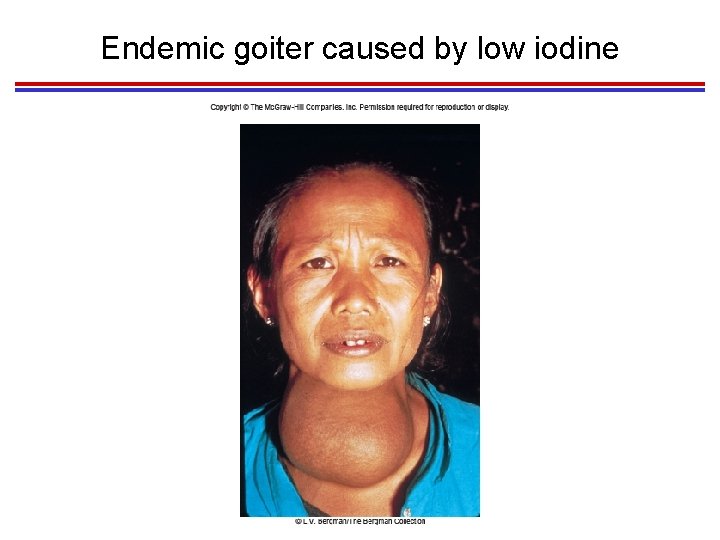
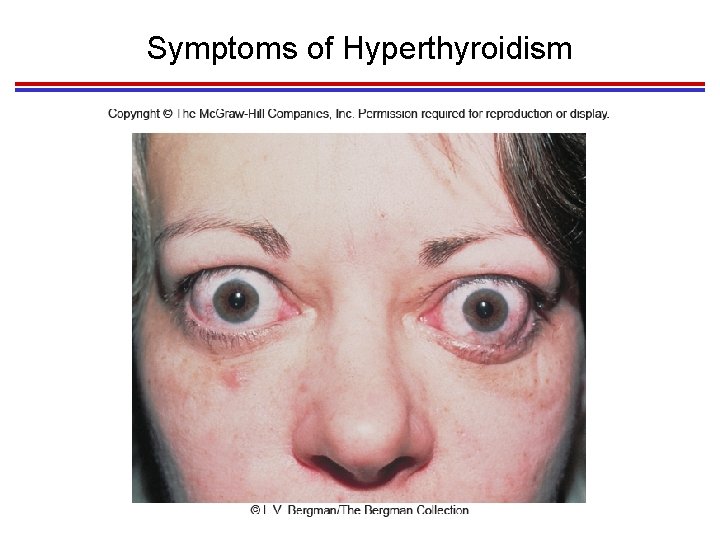
1. Diseases of the Thyroid 1. Iodine deficiency leads to overstimulation of the thyroid gland (no negative feedback on pituitary gland) and growth of a goiter. 2. It also leads to hypothyroidism: low metabolic rates, weight gain and lethargy, poor adaptation to cold stress, and myxedema (accumulation of fluids in subcutaneous connective tissues). 3. Grave’s Disease – hyperthyroidism 4. Cretinism results from hypothyroidism during pregnancy to about 6 months after birth
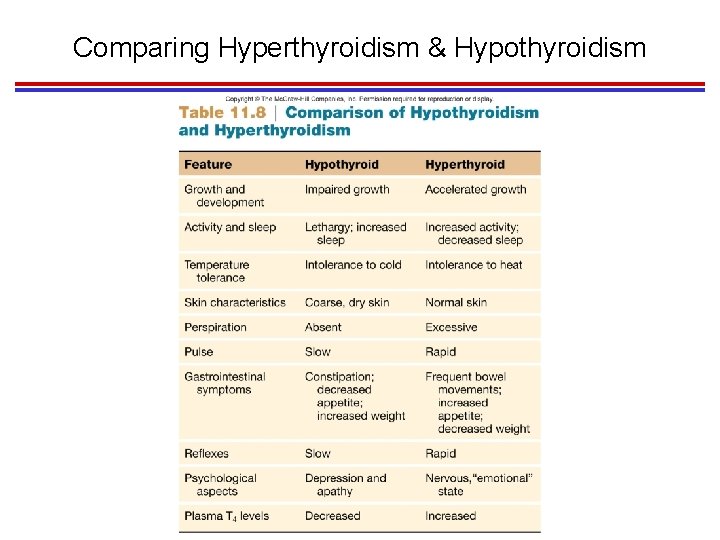
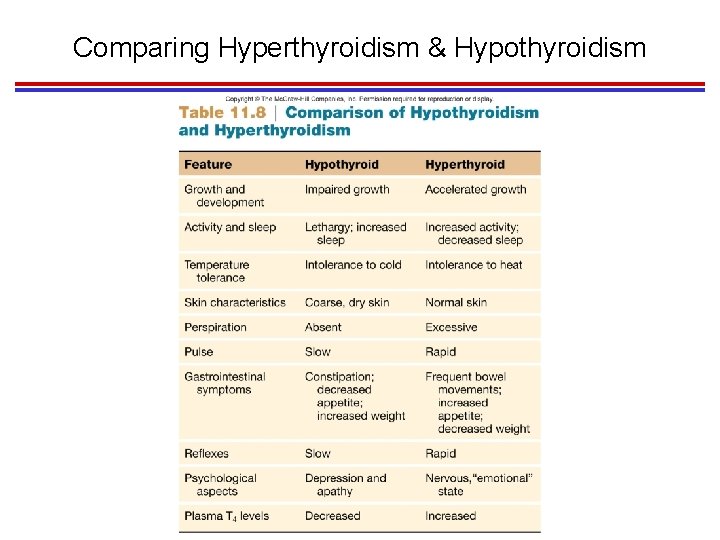
Comparing Hyperthyroidism & Hypothyroidism
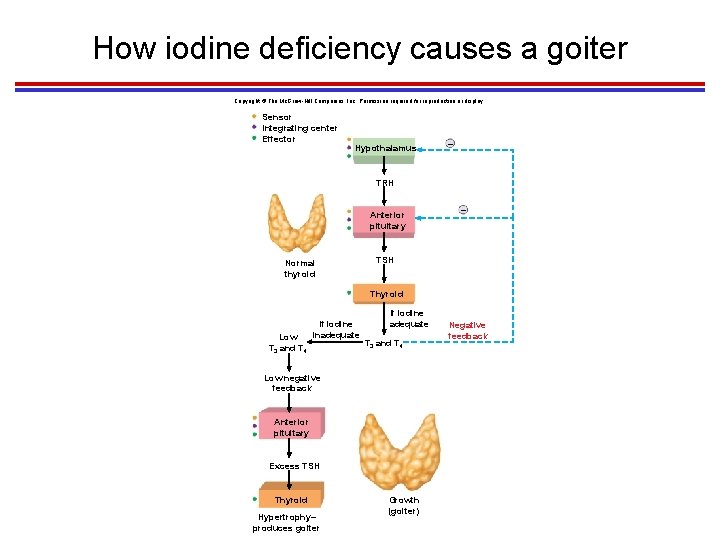
How iodine deficiency causes a goiter Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Sensor Integrating center Effector Hypothalamus – TRH Anterior pituitary Normal thyroid – TSH Thyroid Low T 3 and T 4 If iodine inadequate If iodine adequate T 3 and T 4 Low negative feedback Anterior pituitary Excess TSH Thyroid Hypertrophy– produces goiter Growth (goiter) Negative feedback
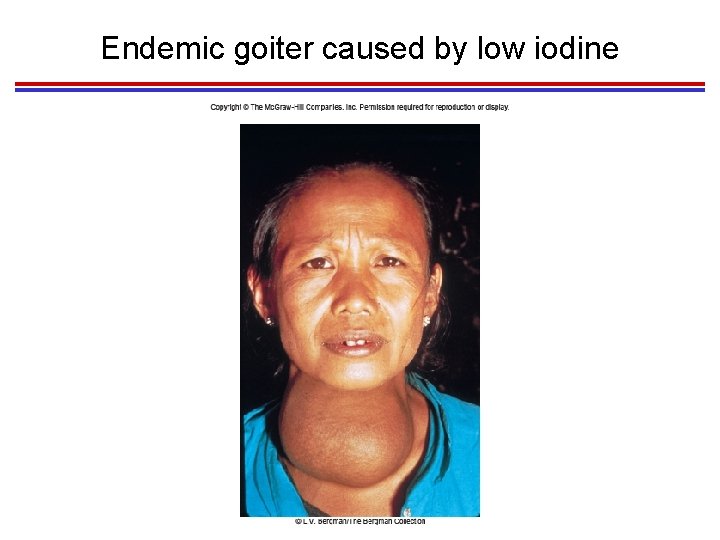
Endemic goiter caused by low iodine
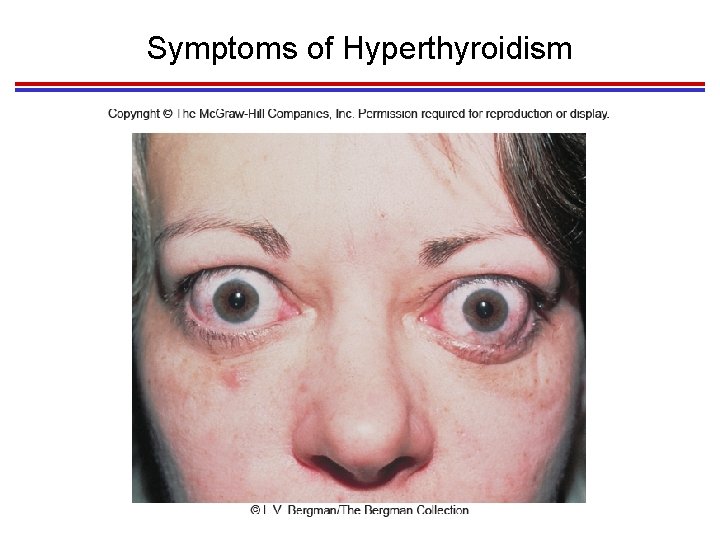
Symptoms of Hyperthyroidism
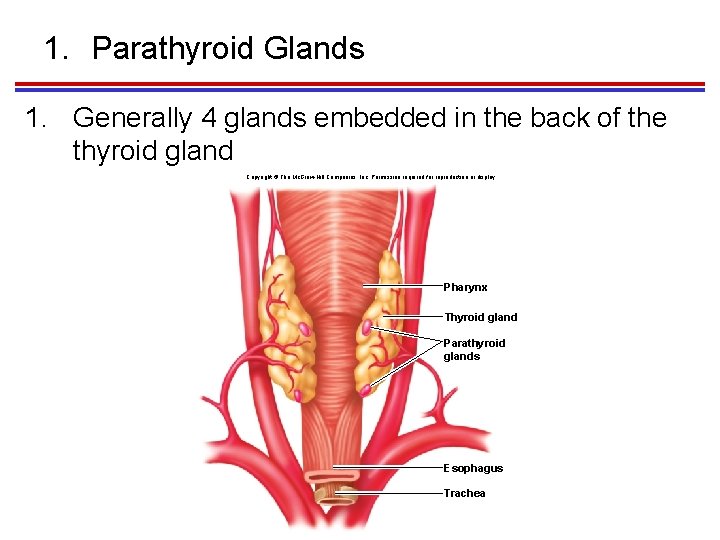
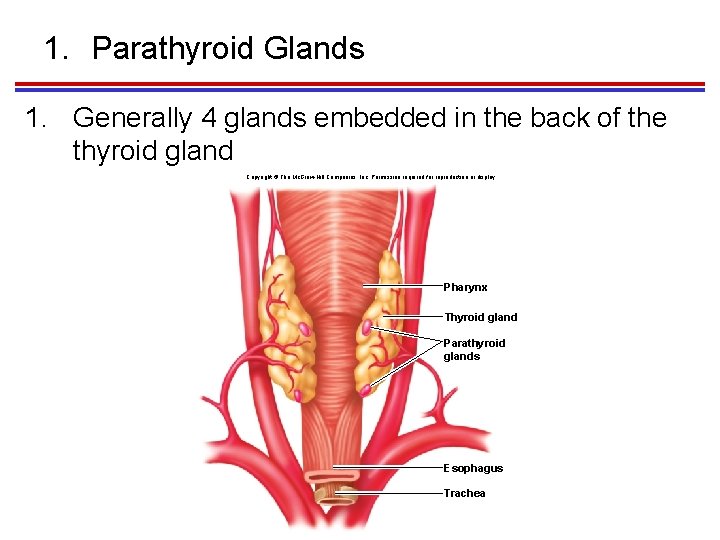
1. Parathyroid Glands 1. Generally 4 glands embedded in the back of the thyroid gland Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Pharynx Thyroid gland Parathyroid glands Esophagus Trachea
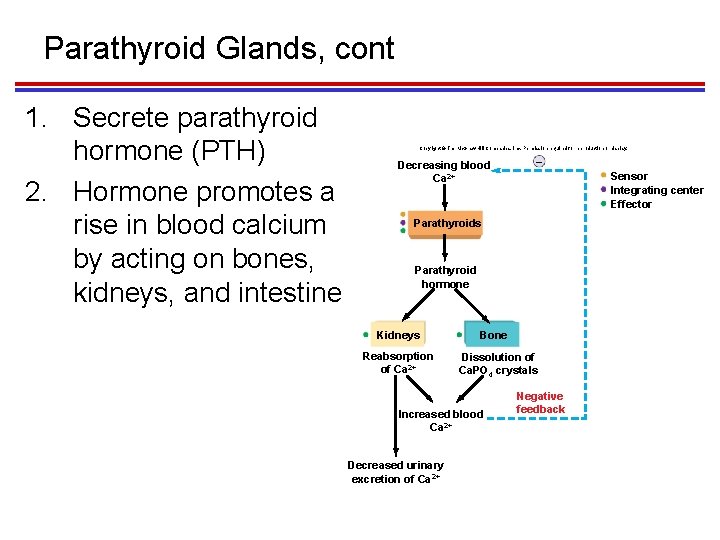
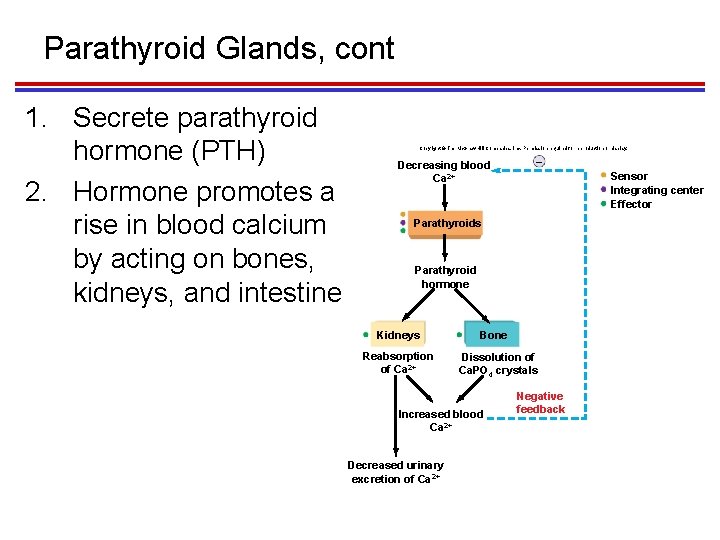
Parathyroid Glands, cont 1. Secrete parathyroid hormone (PTH) 2. Hormone promotes a rise in blood calcium by acting on bones, kidneys, and intestine Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Decreasing blood Ca 2+ – Sensor Integrating center Effector Parathyroids Parathyroid hormone Kidneys Reabsorption of Ca 2+ Bone Dissolution of Ca. PO 4 crystals Increased blood Ca 2+ Decreased urinary excretion of Ca 2+ Negative feedback
VI. Pancreas and Other Endocrine Glands
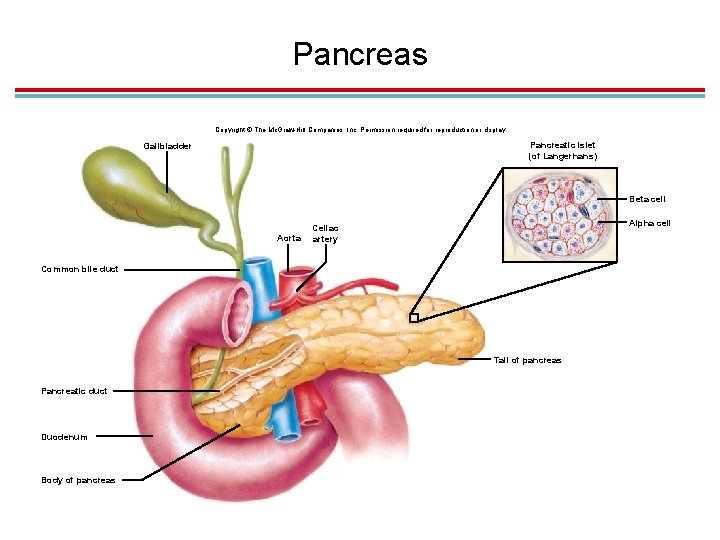
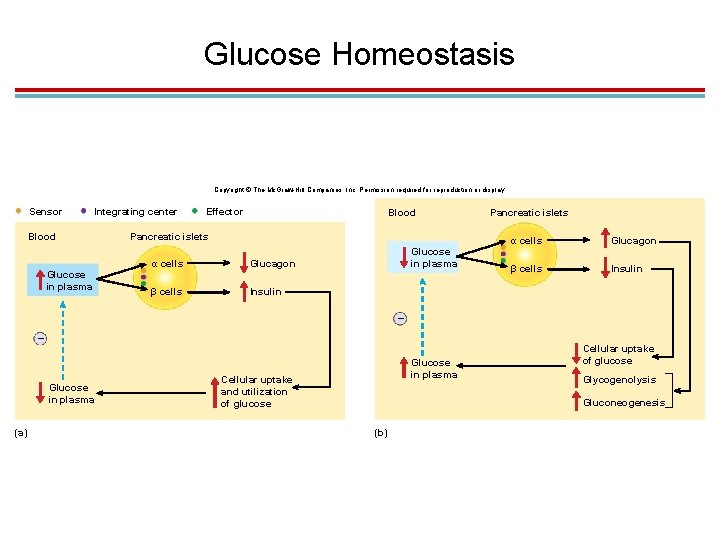
1. Pancreas 1. The pancreas is both an endocrine and an exocrine gland. 2. Endocrine cells are located in pancreatic islets (islets of Langerhans). 1. Alpha cells: glucagon 2. Beta cells: insulin
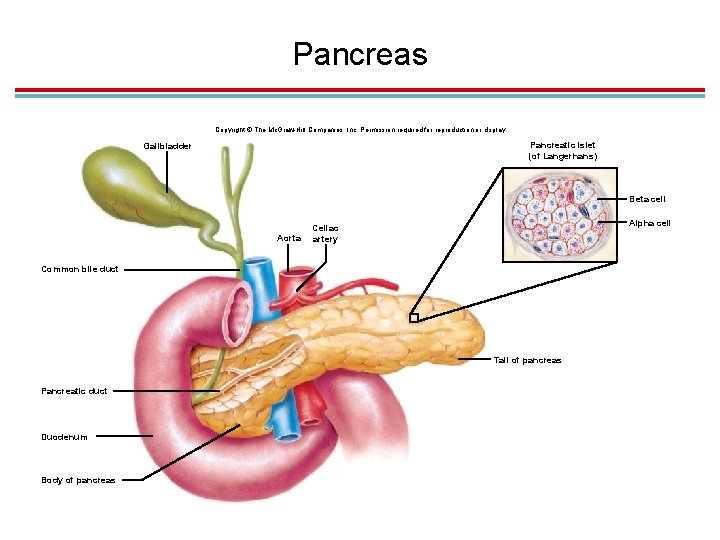
Pancreas Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Pancreatic islet (of Langerhans) Gallbladder Beta cell Aorta Alpha cell Celiac artery Common bile duct Tail of pancreas Pancreatic duct Duodenum Body of pancreas
1. Insulin 1. Primary hormone regulating plasma glucose concentration. 2. Insulin is secreted by beta cells when blood glucose levels rise after a sugary or carbohydrate meal. 3. Its purpose is to lower blood glucose levels to the “normal” range.
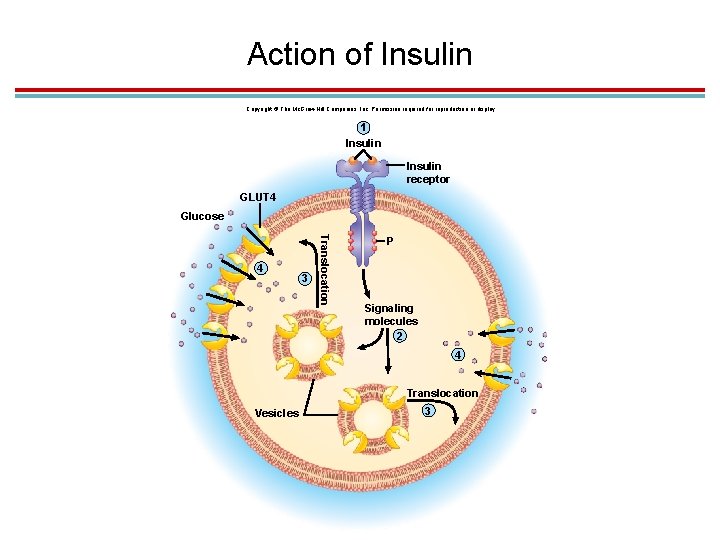
1. Action of Insulin 1. Insulin binds to receptors on target cells. 1. Vesicles with GLUT 4 carrier proteins bind to membrane. 2. Glucose diffuses through GLUT 4 channels by facilitated diffusion 3. Occurs in adipose tissue, skeletal muscle, and the liver. 2. Indirectly stimulates the enzyme glycogen synthase in liver and skeletal muscles to promote sugar storage 3. Stimulates adipose tissue to store fat
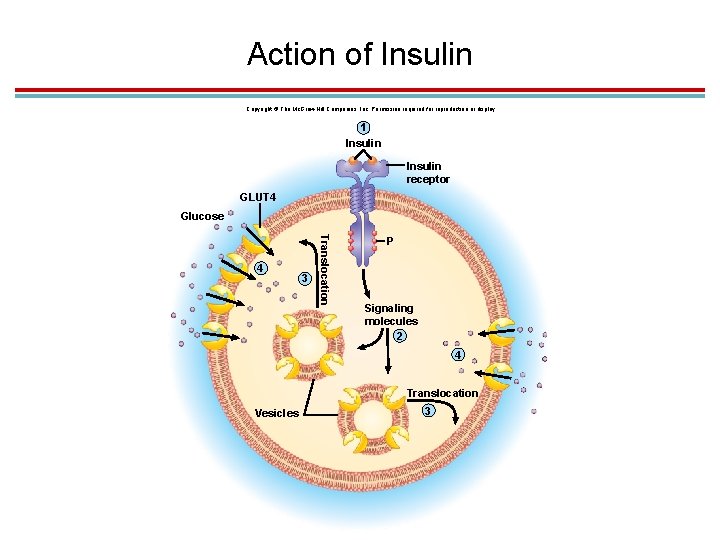
Action of Insulin Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. 1 Insulin receptor GLUT 4 Glucose 3 Translocation 4 P Signaling molecules 2 4 Translocation Vesicles 3
1. Glucagon 1. Antagonistic to insulin 2. Secreted by alpha cells when blood glucose levels are low 3. Purpose is to raise blood glucose levels to a “normal” range
1. Action of Glucagon 1. Stimulates liver to hydrolyze glycogen into glucose and release it into the blood 2. Stimulates gluconeogenesis, conversion of noncarbohydrates into glucose 3. Stimulates lipolysis in adipose tissue so fat is released and used as a fuel source instead of glucose
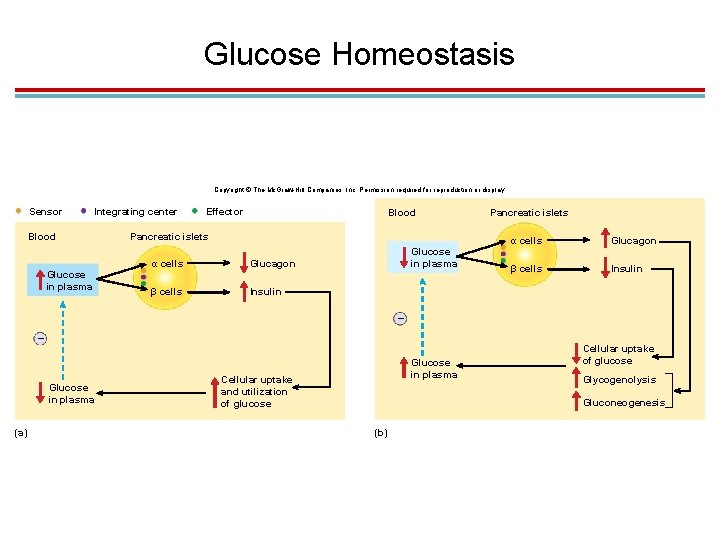
Glucose Homeostasis Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. Sensor Integrating center Blood Glucose in plasma Effector Blood Pancreatic islets α cells Glucagon β cells Insulin Glucose in plasma Pancreatic islets α cells Glucagon β cells Insulin – – Glucose in plasma (a) Glucose in plasma Cellular uptake and utilization of glucose Cellular uptake of glucose Glycogenolysis Gluconeogenesis (b)
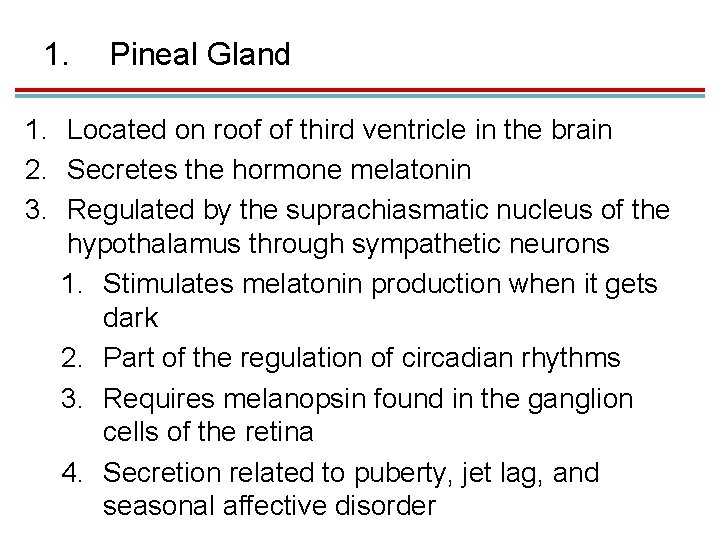
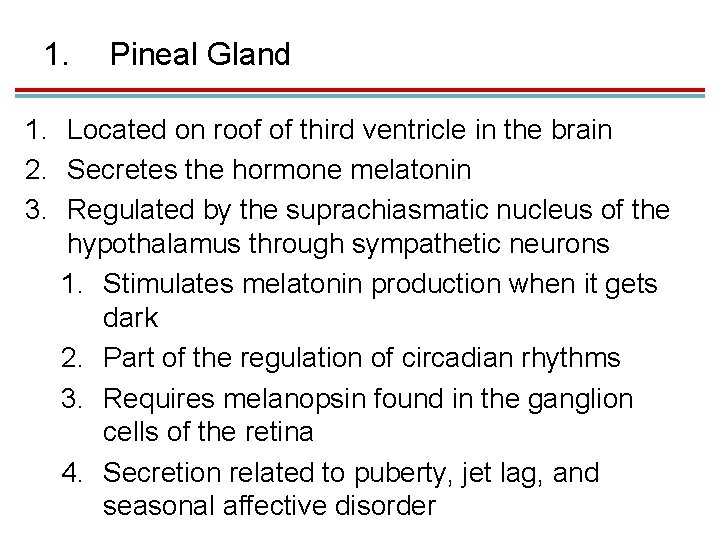
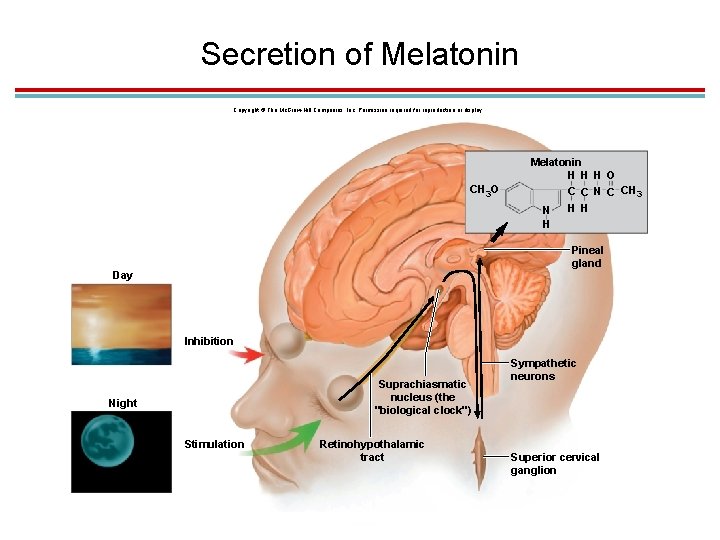
1. Pineal Gland 1. Located on roof of third ventricle in the brain 2. Secretes the hormone melatonin 3. Regulated by the suprachiasmatic nucleus of the hypothalamus through sympathetic neurons 1. Stimulates melatonin production when it gets dark 2. Part of the regulation of circadian rhythms 3. Requires melanopsin found in the ganglion cells of the retina 4. Secretion related to puberty, jet lag, and seasonal affective disorder
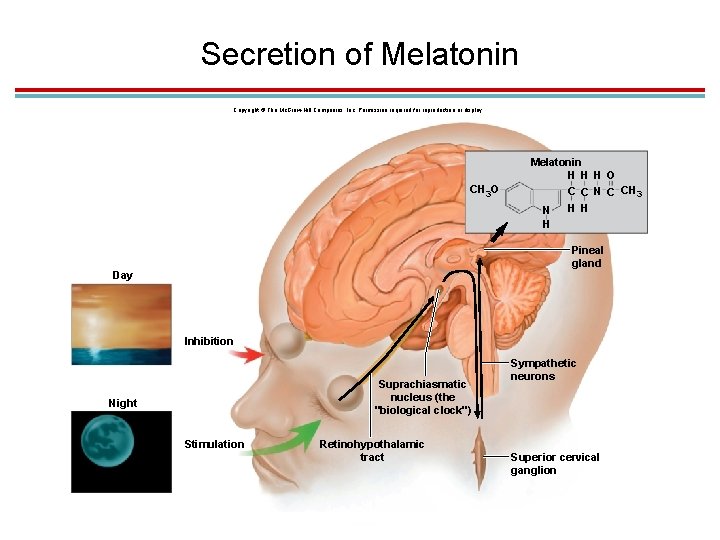
Secretion of Melatonin Copyright © The Mc. Graw-Hill Companies, Inc. Permission required for reproduction or display. CH 3 O Melatonin H H H O C C N C CH 3 H H N H Pineal gland Day Inhibition Suprachiasmatic nucleus (the "biological clock") Night Stimulation Retinohypothalamic tract Sympathetic neurons Superior cervical ganglion
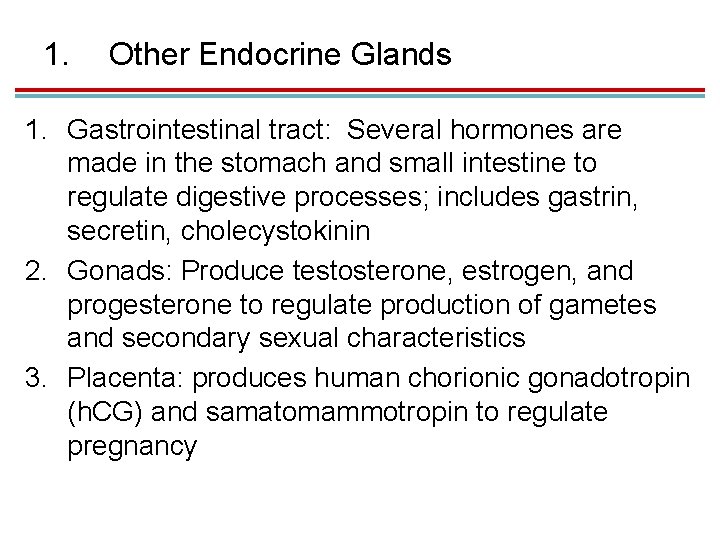
1. Other Endocrine Glands 1. Gastrointestinal tract: Several hormones are made in the stomach and small intestine to regulate digestive processes; includes gastrin, secretin, cholecystokinin 2. Gonads: Produce testosterone, estrogen, and progesterone to regulate production of gametes and secondary sexual characteristics 3. Placenta: produces human chorionic gonadotropin (h. CG) and samatomammotropin to regulate pregnancy