Chapter 15 Lecture Outline See separate Power Point




- Slides: 48
Chapter 15 Lecture Outline See separate Power. Point slides for all figures and tables preinserted into Power. Point without notes. Copyright © Mc. Graw-Hill Education. Permission required for reproduction or display. 1
Introduction • The heart pumps 7, 000 liters of blood through the body each day • The heart contracts 2. 5 billion times in an average lifetime • The heart pumps blood through the blood vessels in this order: arteries arterioles capillaries venules veins back to heart • The heart and all blood vessels make up the cardiovascular system 2
15. 1: Overview of the Cardiovascular System • “Cardiovascular” refers to both heart and blood vessels • Pumping action of heart transports blood through blood vessels Blood vessels form 2 circuits: Pulmonary Circuit: • Transports oxygen-poor blood from heart to lungs, and back to heart • In lungs, blood picks up O 2 and drops off CO 2 Systemic Circuit: • Transports oxygen-rich blood from heart to all body cells, and back to heart • Blood delivers nutrients to cells, and removes wastes 3
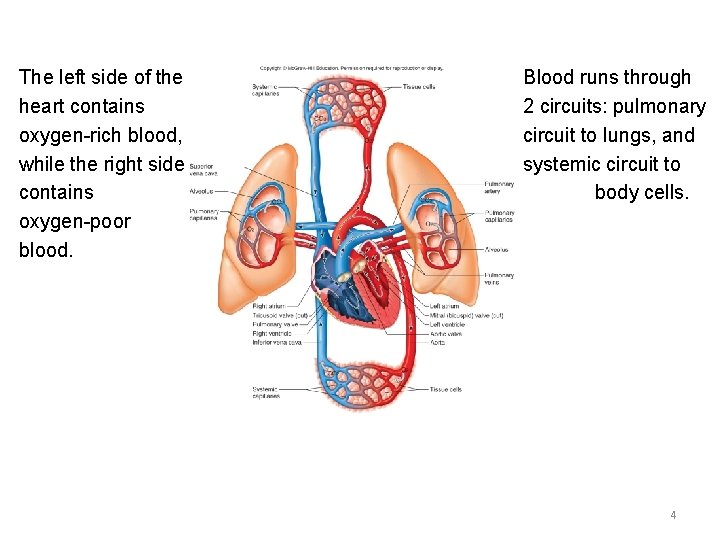
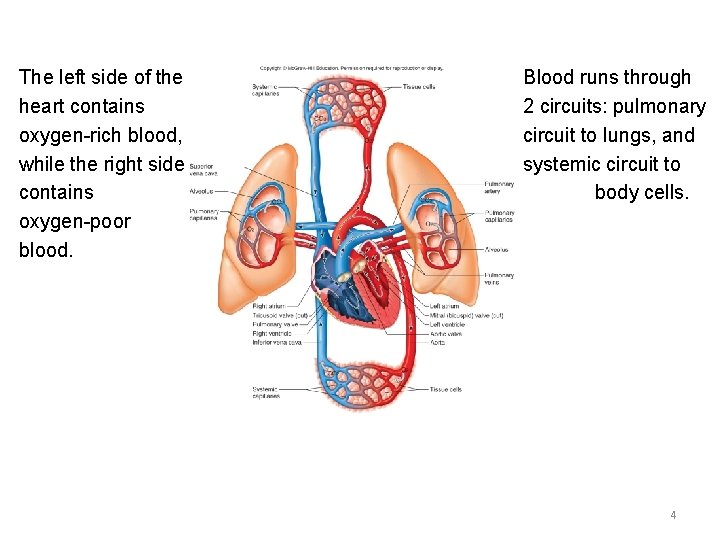
The left side of the heart contains oxygen-rich blood, while the right side contains oxygen-poor blood. Blood runs through 2 circuits: pulmonary circuit to lungs, and systemic circuit to body cells. 4
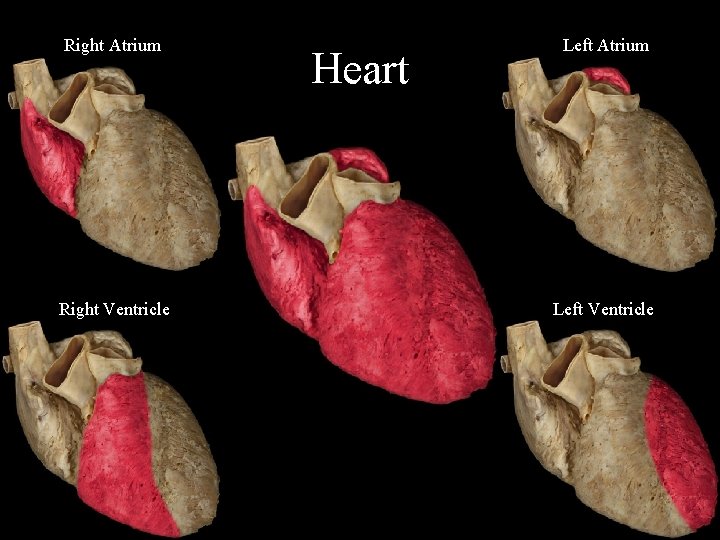
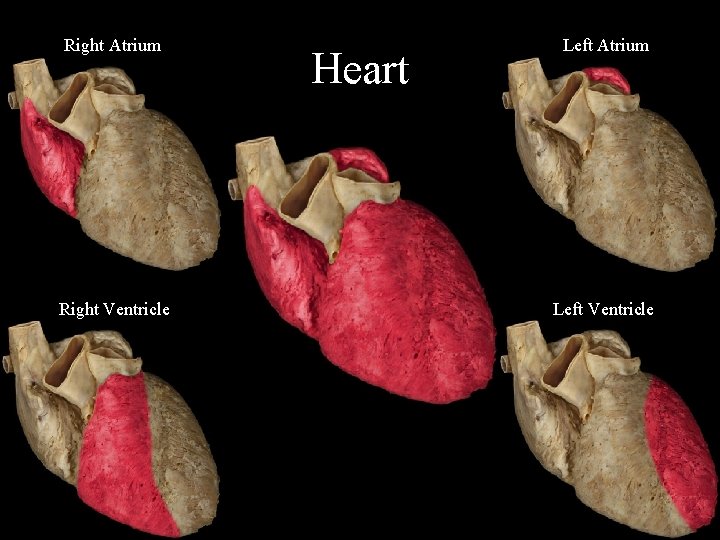
Right Atrium Right Ventricle Heart Left Atrium Left Ventricle
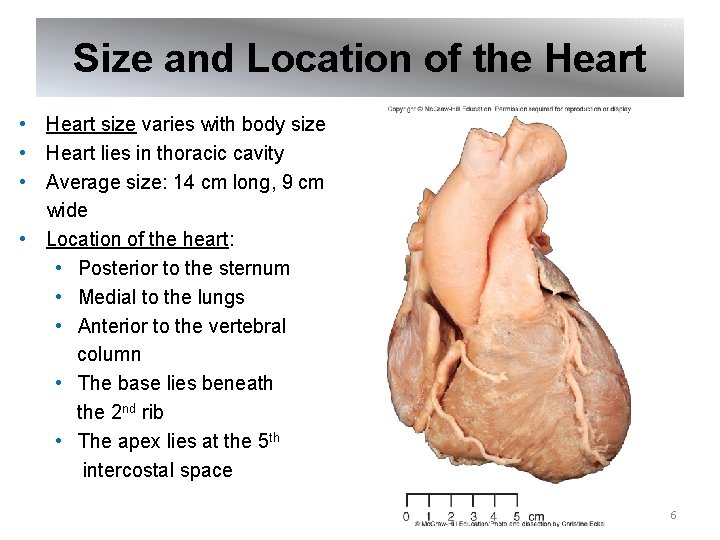
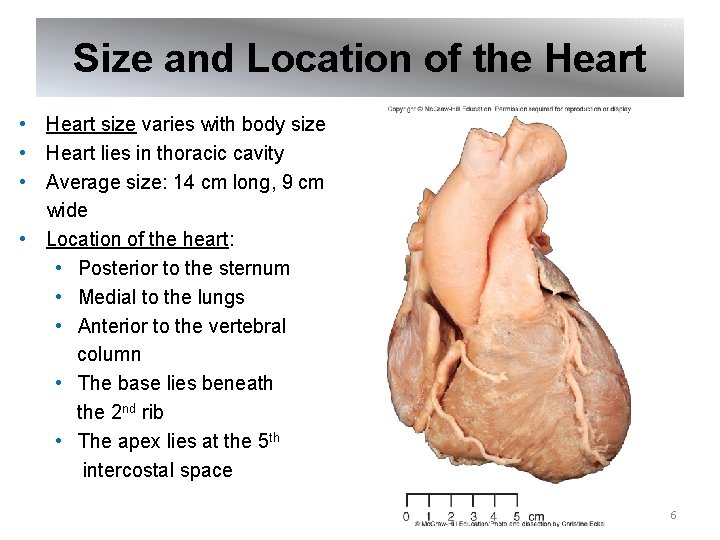
Size and Location of the Heart • Heart size varies with body size • Heart lies in thoracic cavity • Average size: 14 cm long, 9 cm wide • Location of the heart: • Posterior to the sternum • Medial to the lungs • Anterior to the vertebral column • The base lies beneath the 2 nd rib • The apex lies at the 5 th intercostal space 6
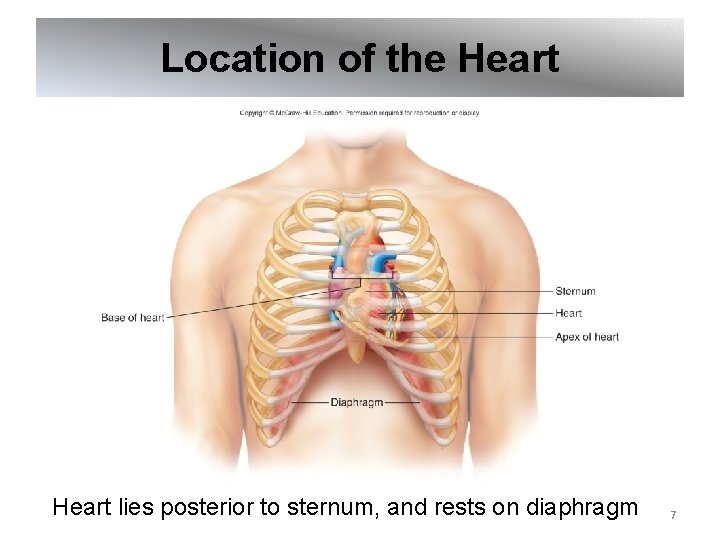
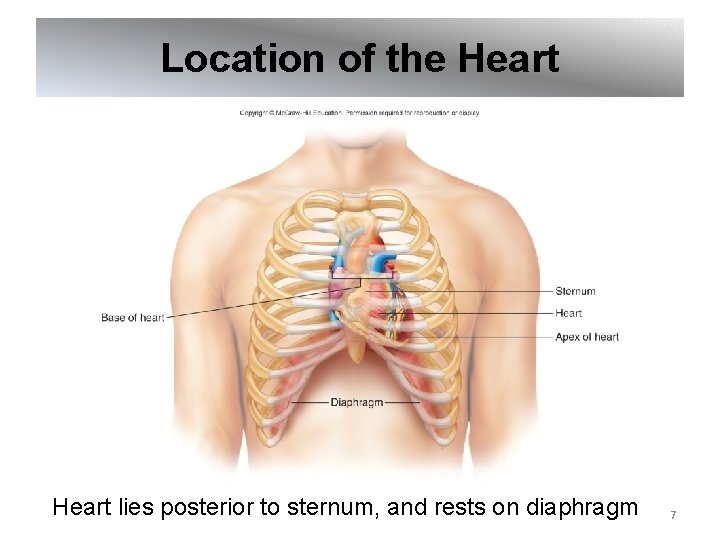
Location of the Heart lies posterior to sternum, and rests on diaphragm 7

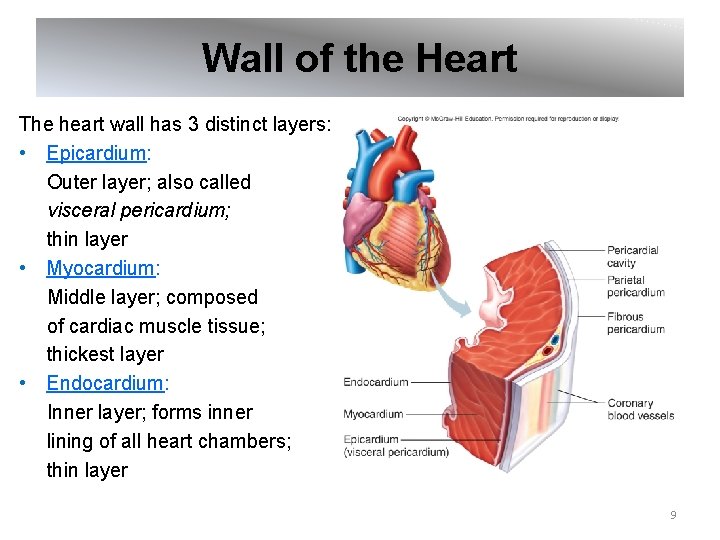
Coverings of the Heart Pericardium: Covering over heart and Large blood vessels • Fibrous pericardium: Outer layer, that surrounds double-layered serous membrane • Parietal pericardium: Deep to fibrous pericardium; outer layer of serous membrane • Visceral pericardium: Inner layer of serous membrane; attached to surface of heart; also called the epicardium 8
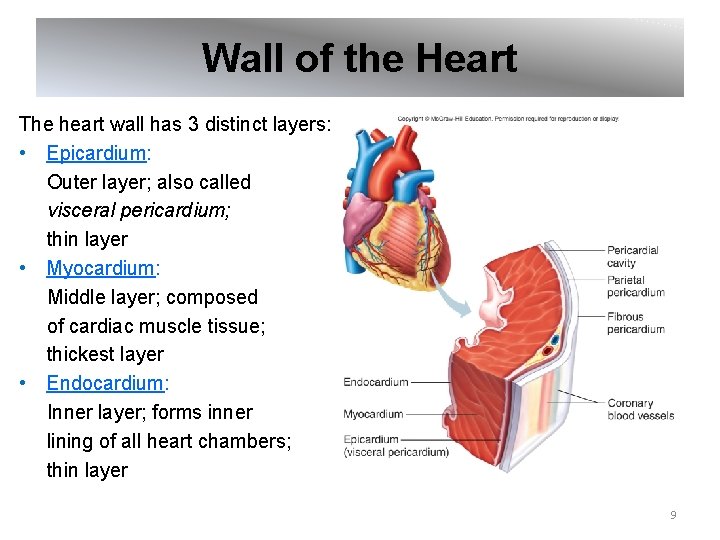
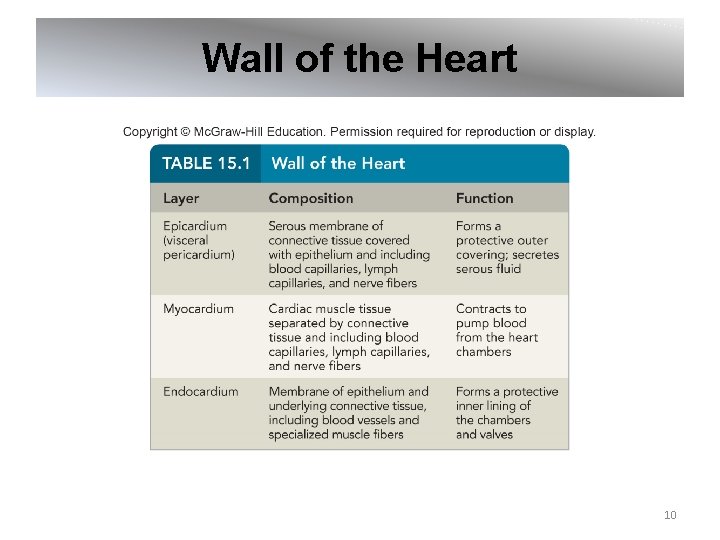
Wall of the Heart The heart wall has 3 distinct layers: • Epicardium: Outer layer; also called visceral pericardium; thin layer • Myocardium: Middle layer; composed of cardiac muscle tissue; thickest layer • Endocardium: Inner layer; forms inner lining of all heart chambers; thin layer 9
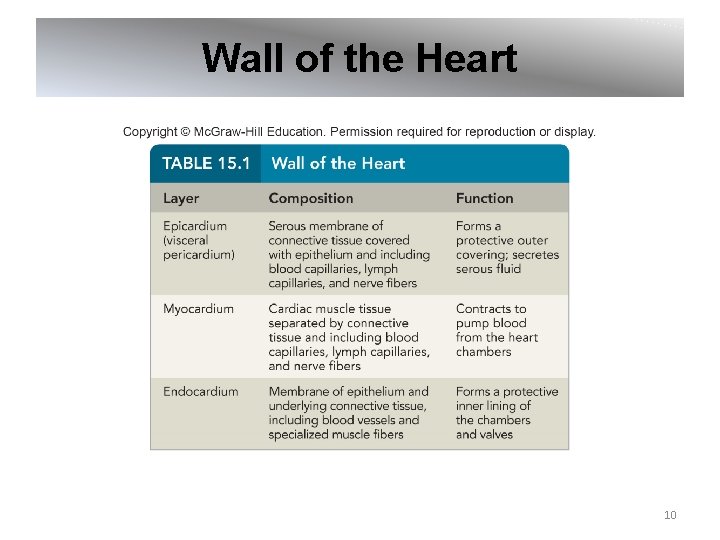
Wall of the Heart 10
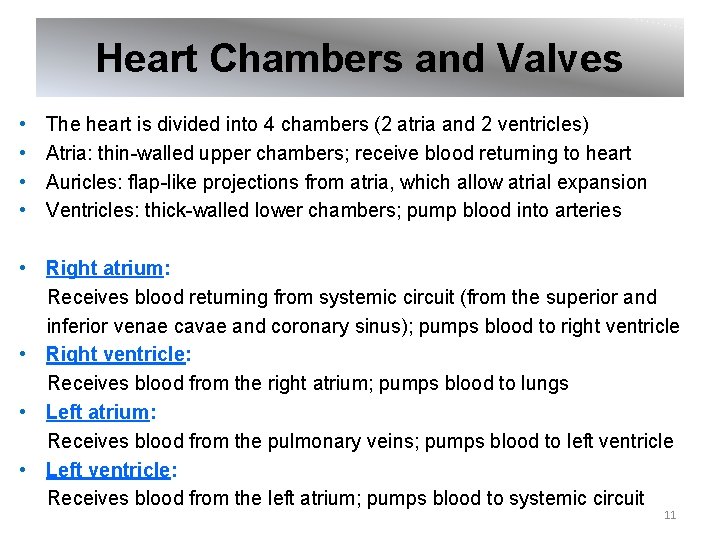
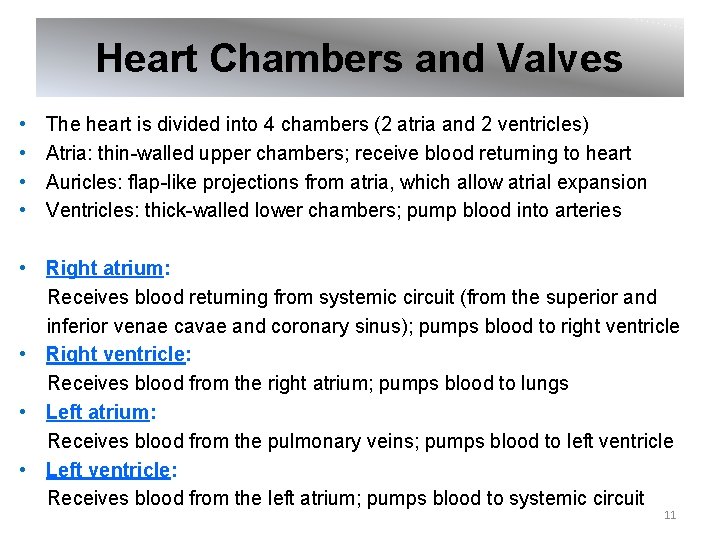
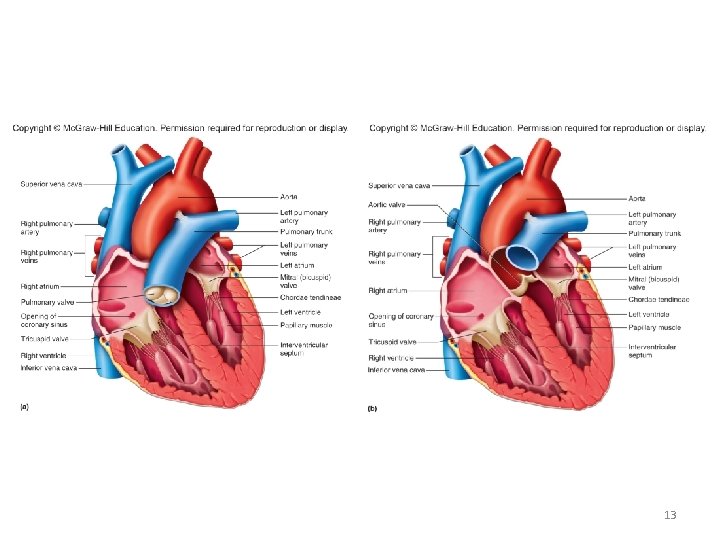
Heart Chambers and Valves • • The heart is divided into 4 chambers (2 atria and 2 ventricles) Atria: thin-walled upper chambers; receive blood returning to heart Auricles: flap-like projections from atria, which allow atrial expansion Ventricles: thick-walled lower chambers; pump blood into arteries • Right atrium: Receives blood returning from systemic circuit (from the superior and inferior venae cavae and coronary sinus); pumps blood to right ventricle • Right ventricle: Receives blood from the right atrium; pumps blood to lungs • Left atrium: Receives blood from the pulmonary veins; pumps blood to left ventricle • Left ventricle: Receives blood from the left atrium; pumps blood to systemic circuit 11
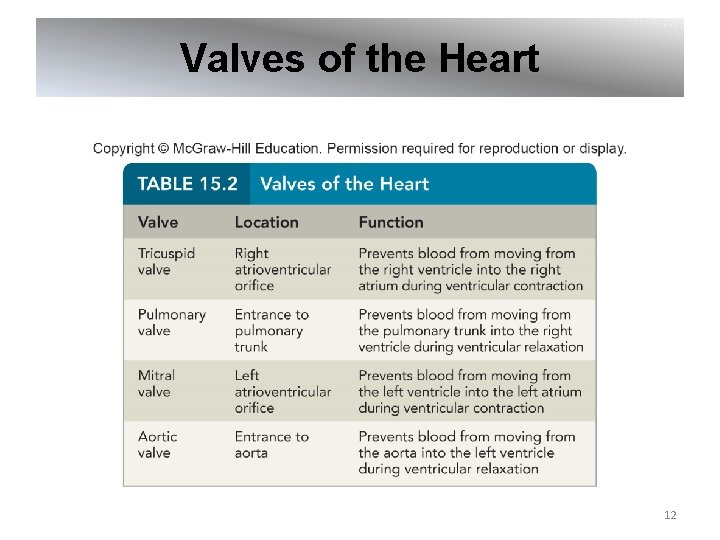
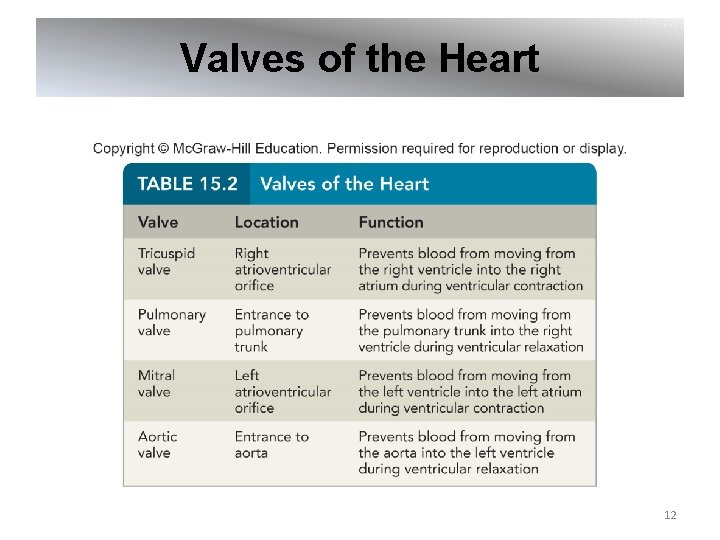
Valves of the Heart 12
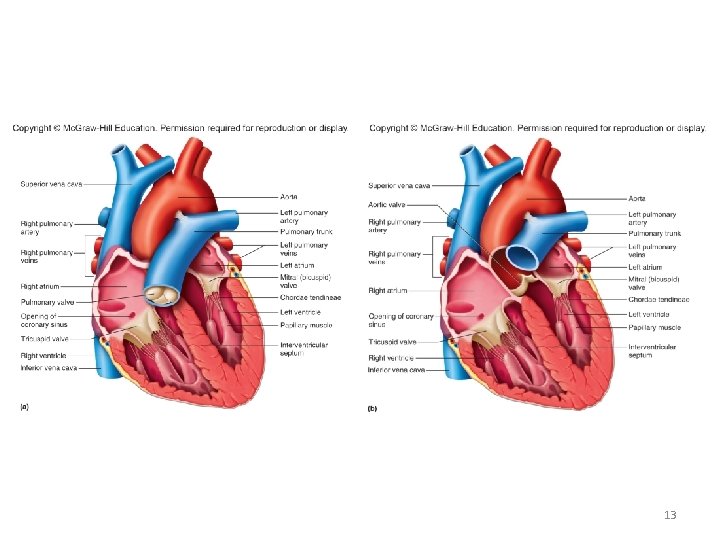
13
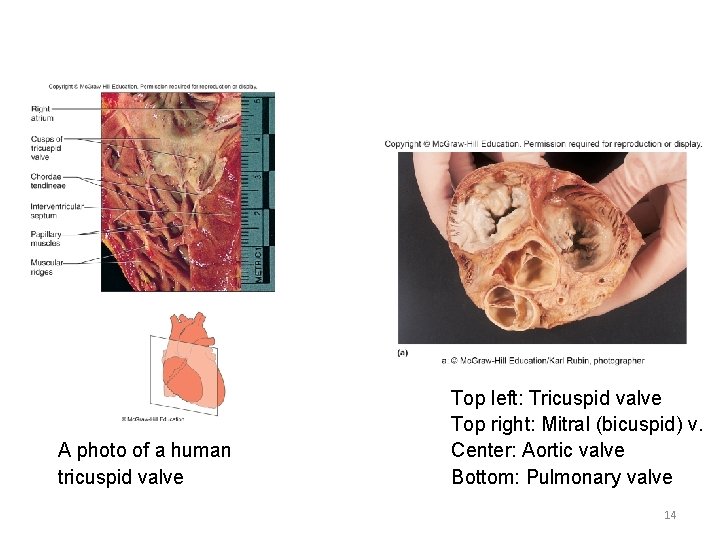
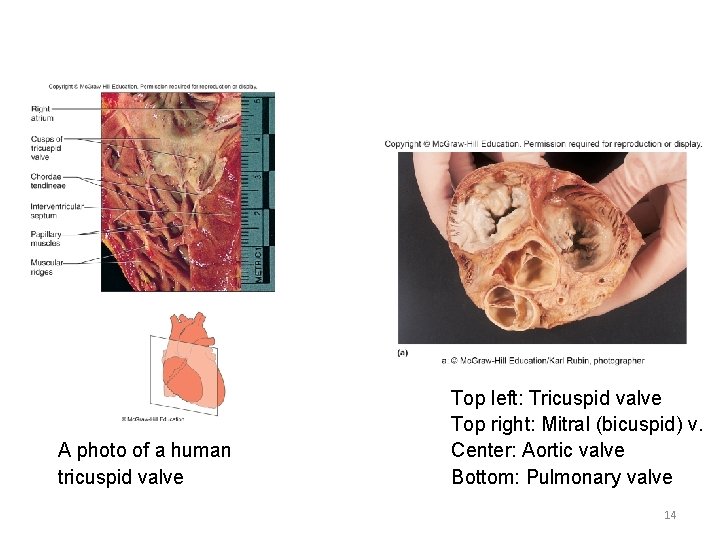
A photo of a human tricuspid valve Top left: Tricuspid valve Top right: Mitral (bicuspid) v. Center: Aortic valve Bottom: Pulmonary valve 14
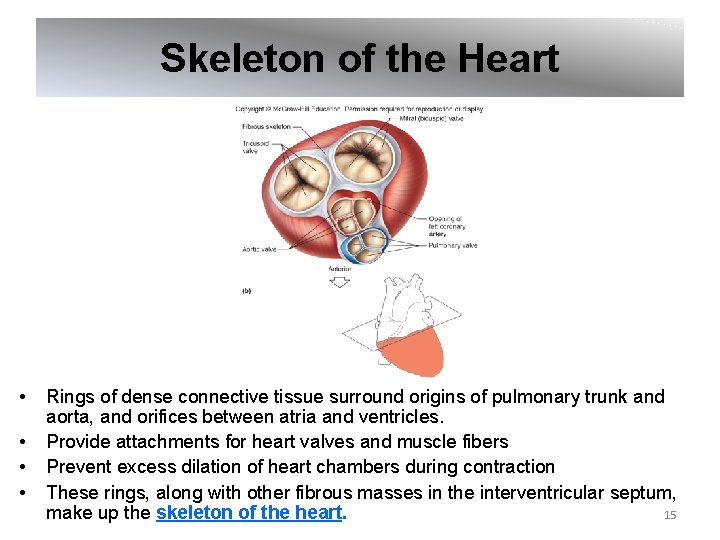
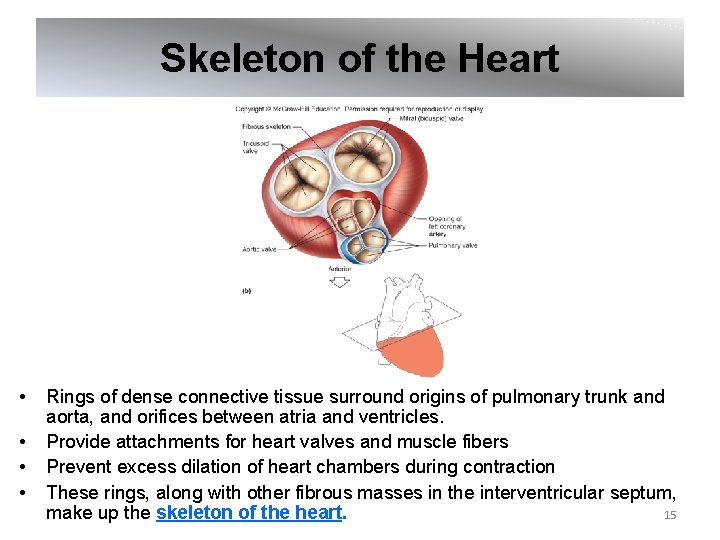
Skeleton of the Heart • • Rings of dense connective tissue surround origins of pulmonary trunk and aorta, and orifices between atria and ventricles. Provide attachments for heart valves and muscle fibers Prevent excess dilation of heart chambers during contraction These rings, along with other fibrous masses in the interventricular septum, 15 make up the skeleton of the heart.
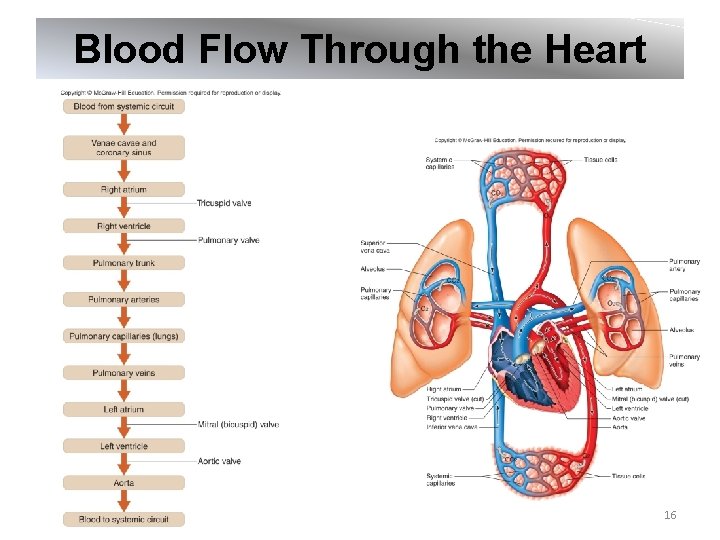
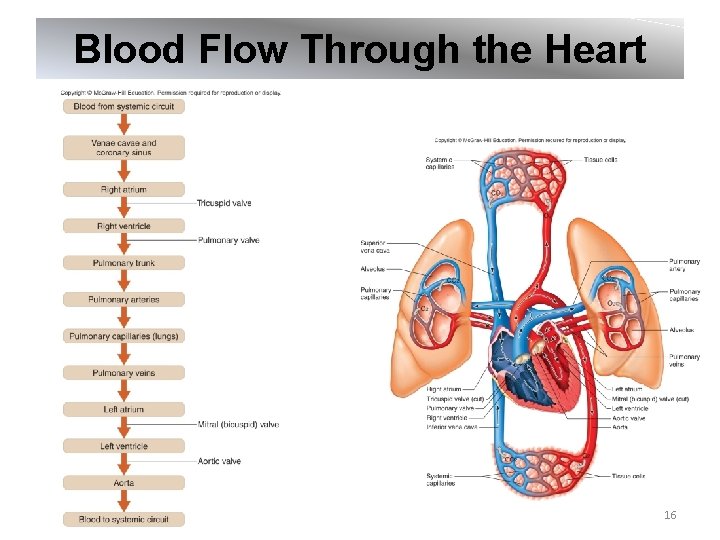
Blood Flow Through the Heart 16
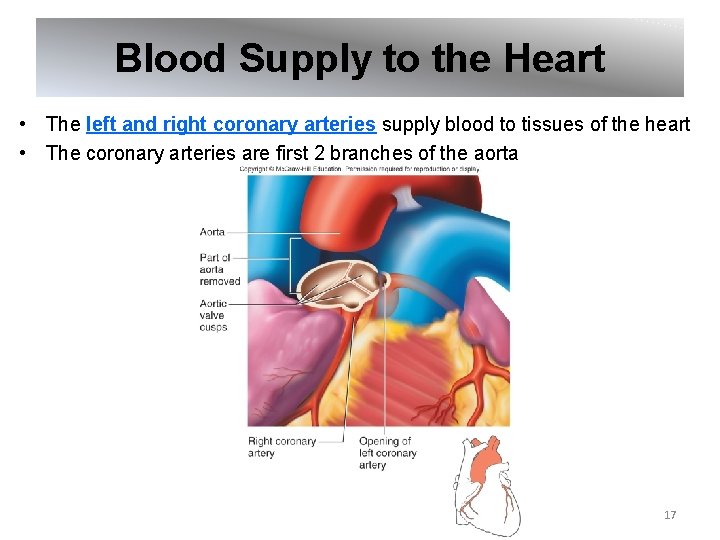
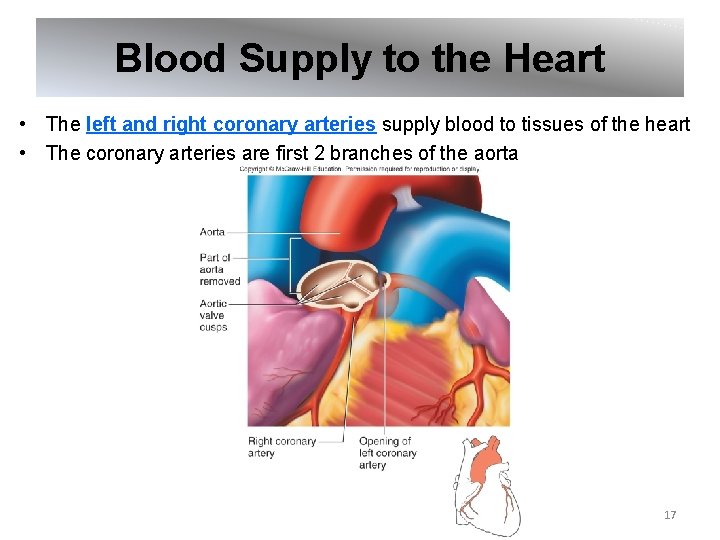
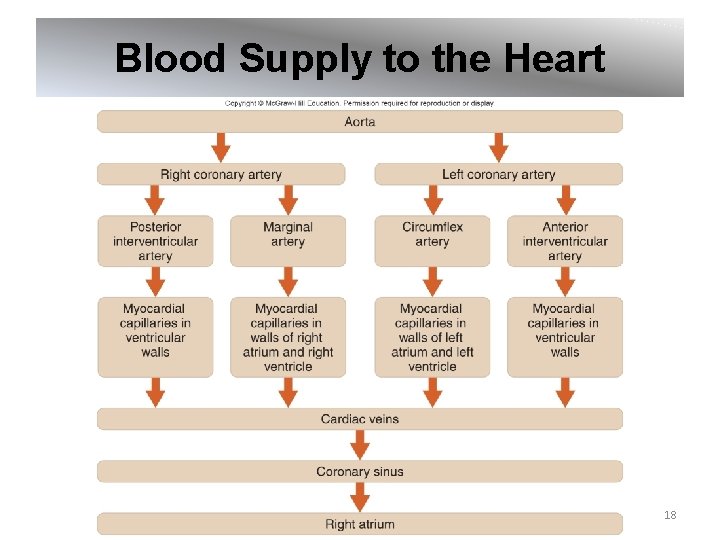
Blood Supply to the Heart • The left and right coronary arteries supply blood to tissues of the heart • The coronary arteries are first 2 branches of the aorta 17
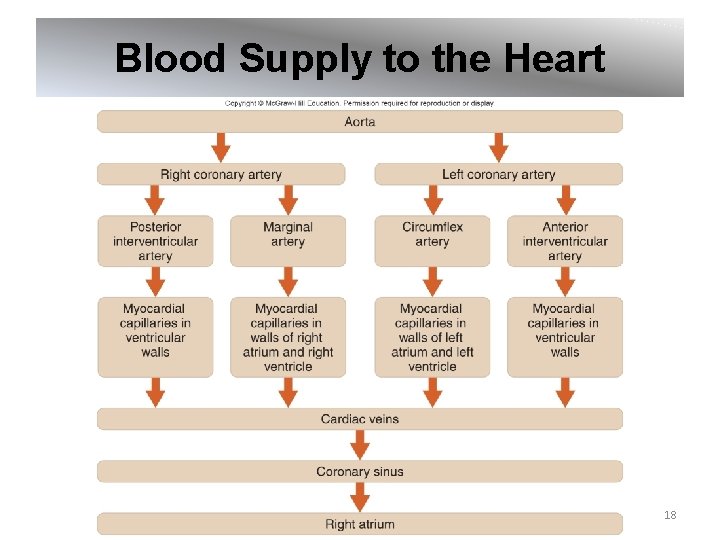
Blood Supply to the Heart 18
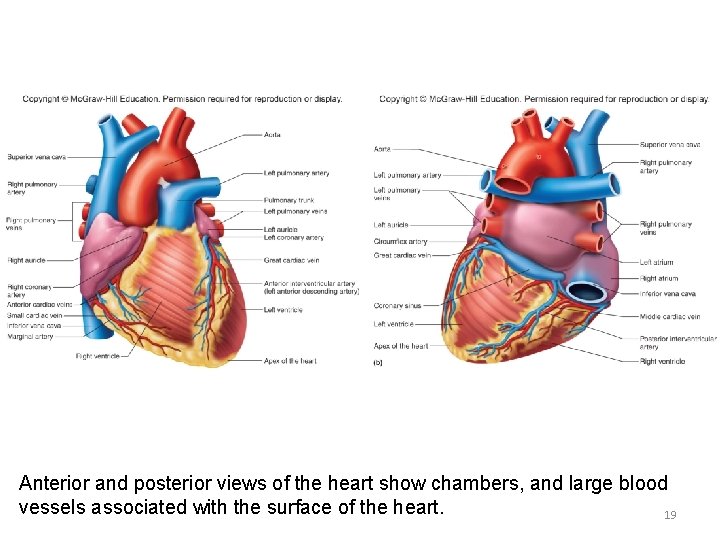
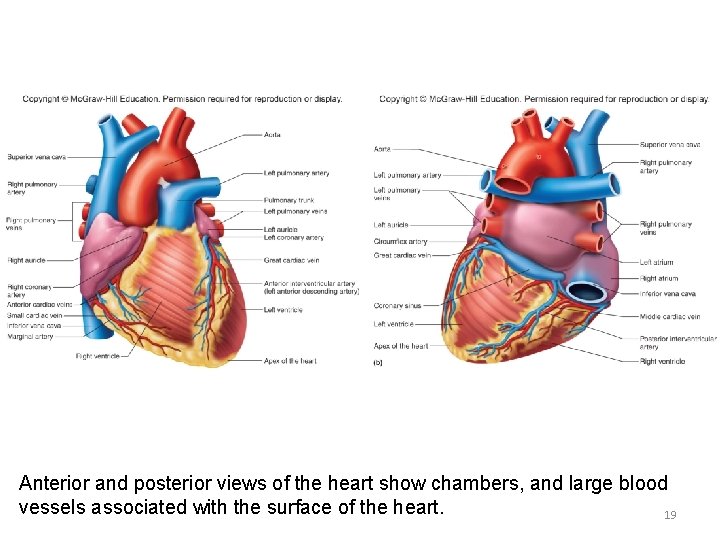
Anterior and posterior views of the heart show chambers, and large blood vessels associated with the surface of the heart. 19
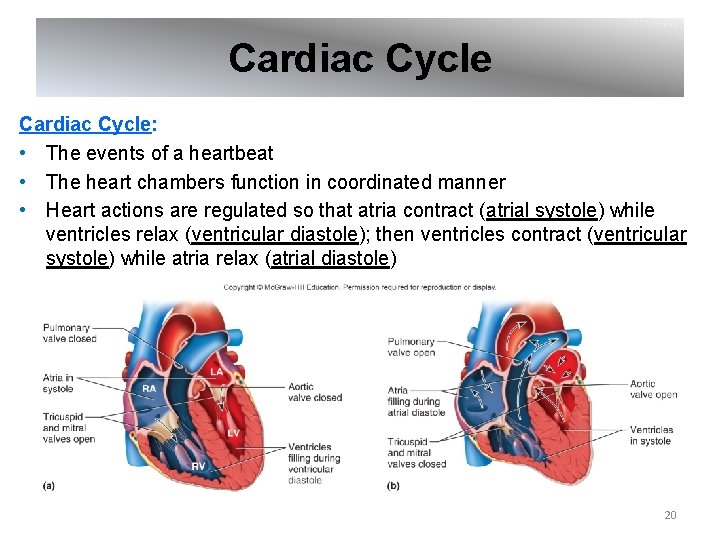
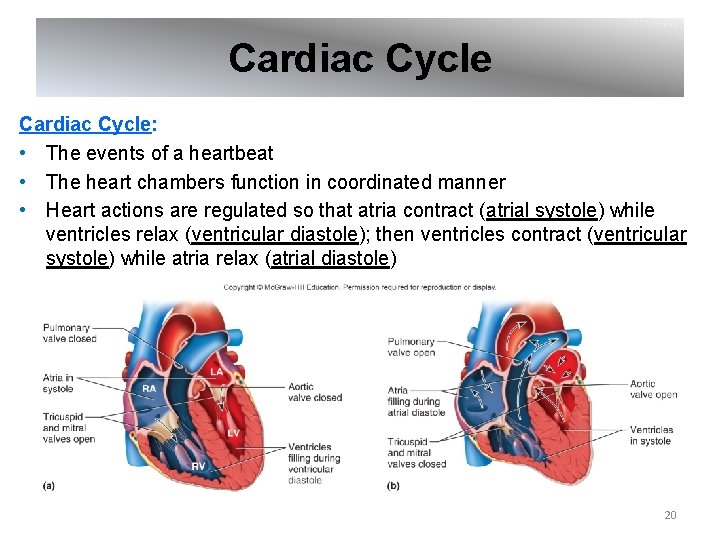
Cardiac Cycle: • The events of a heartbeat • The heart chambers function in coordinated manner • Heart actions are regulated so that atria contract (atrial systole) while ventricles relax (ventricular diastole); then ventricles contract (ventricular systole) while atria relax (atrial diastole) 20
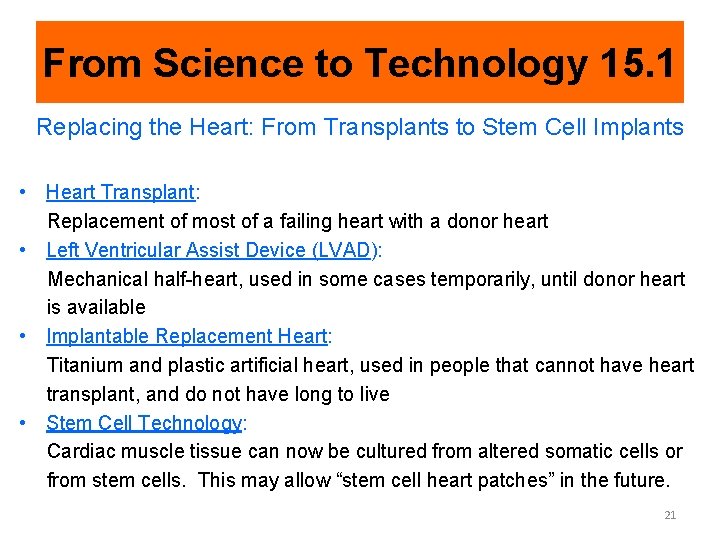
From Science to Technology 15. 1 Replacing the Heart: From Transplants to Stem Cell Implants • Heart Transplant: Replacement of most of a failing heart with a donor heart • Left Ventricular Assist Device (LVAD): Mechanical half-heart, used in some cases temporarily, until donor heart is available • Implantable Replacement Heart: Titanium and plastic artificial heart, used in people that cannot have heart transplant, and do not have long to live • Stem Cell Technology: Cardiac muscle tissue can now be cultured from altered somatic cells or from stem cells. This may allow “stem cell heart patches” in the future. 21
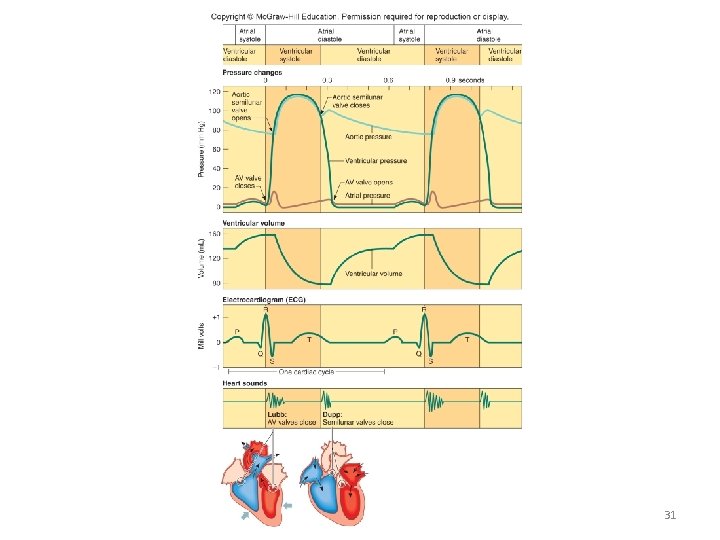
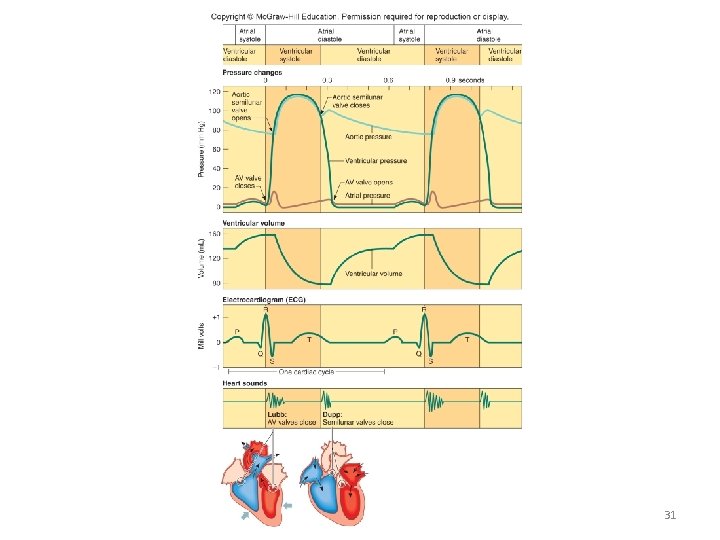
Cardiac Cycle • During a cardiac cycle, the pressure in the heart chambers rises and falls • Pressure changes open and close the valves • During atrial systole and ventricular diastole: • The ventricles are relaxed • The A-V valves open and the semilunar valves close • About 70% of blood flows passively from atria into ventricles • Atrial systole pushes remaining 30% of blood into the ventricles, causing ventricular pressure to increase • During ventricular systole and atrial diastole: • The A-V valves close • The chordae tendineae prevent the cusps of the valves from bulging too far backward into the atria • The atria relax • Blood flows into atria from venae cavae and pulmonary veins • The ventricular pressure increases and opens the semilunar valves • Blood flows into the pulmonary trunk and aorta 22
Heart Sounds • A heart beat through a stethoscope sounds like “lubb-dupp” • Sounds are due to closing of heart valves, and vibrations associated with a sudden slowing of blood flow during contraction/relaxation of chambers • “Lubb”: • The first heart sound • Occurs during ventricular systole • Associated with closing of the A-V valves • “Dupp”: • The second heart sound • Occurs during ventricular diastole • Associated with closing of the pulmonary and aortic semilunar valves • Murmur: Abnormal heart sound derived from incomplete closure of cusps of a valve 23
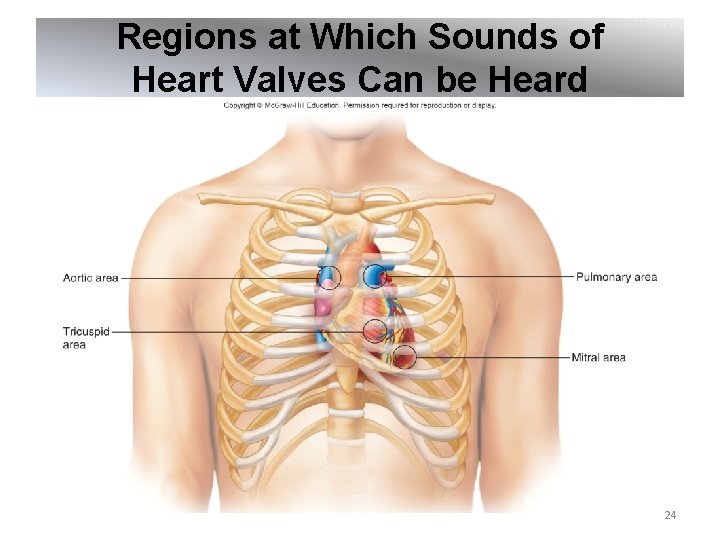
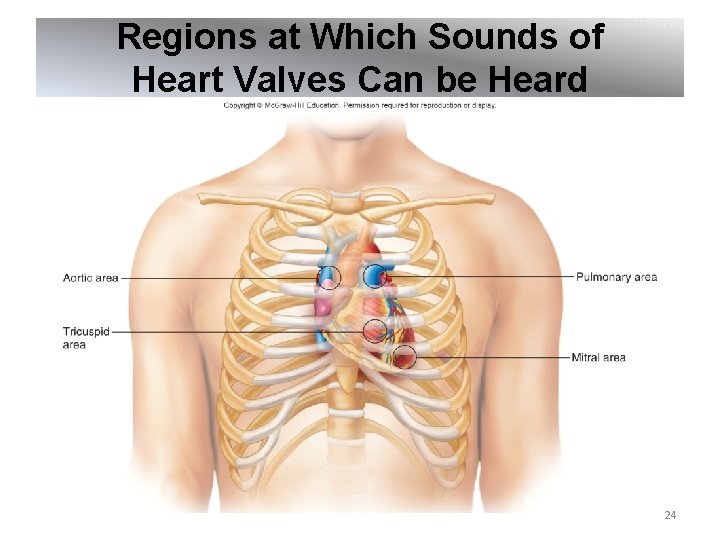
Regions at Which Sounds of Heart Valves Can be Heard 24
Cardiac Muscle • Cardiac muscle cells form branching networks • Intercalated discs between cells contain gap junctions, so action potentials can be spread through a network of cells • Cardiac muscle fibers form a functional syncytium: A mass of merging cells that function as a unit • 2 such masses exist in the heart: • In the atrial walls; called the atrial syncytium • In the ventricular walls; called the ventricular syncytium 25

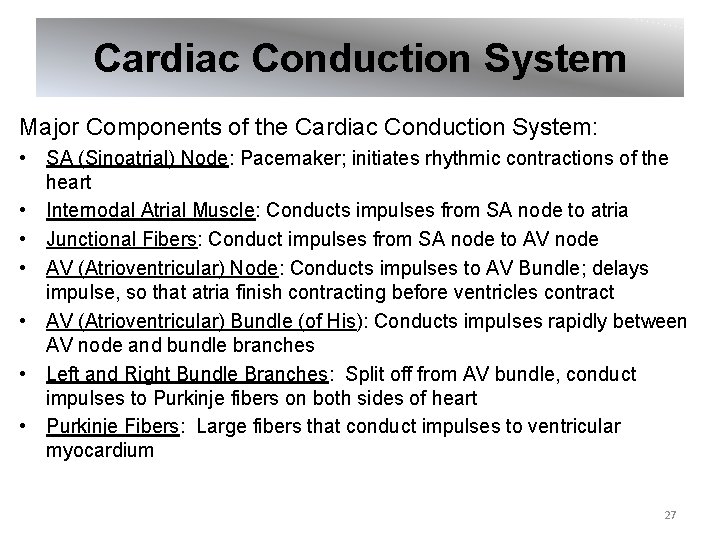
Cardiac Conduction System: • A group of clumps and strands of specialized cardiac muscle tissue, which initiates and distributes impulses throughout the myocardium • Coordinates the events of the cardiac cycle 26
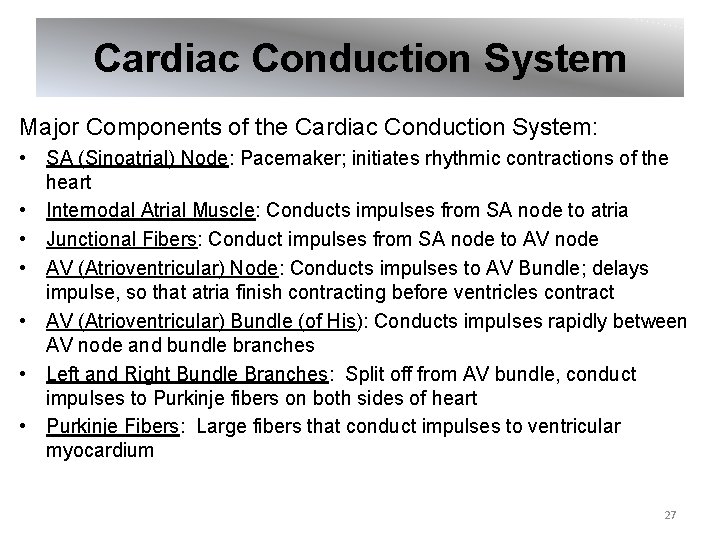
Cardiac Conduction System Major Components of the Cardiac Conduction System: • SA (Sinoatrial) Node: Pacemaker; initiates rhythmic contractions of the heart • Internodal Atrial Muscle: Conducts impulses from SA node to atria • Junctional Fibers: Conduct impulses from SA node to AV node • AV (Atrioventricular) Node: Conducts impulses to AV Bundle; delays impulse, so that atria finish contracting before ventricles contract • AV (Atrioventricular) Bundle (of His): Conducts impulses rapidly between AV node and bundle branches • Left and Right Bundle Branches: Split off from AV bundle, conduct impulses to Purkinje fibers on both sides of heart • Purkinje Fibers: Large fibers that conduct impulses to ventricular myocardium 27
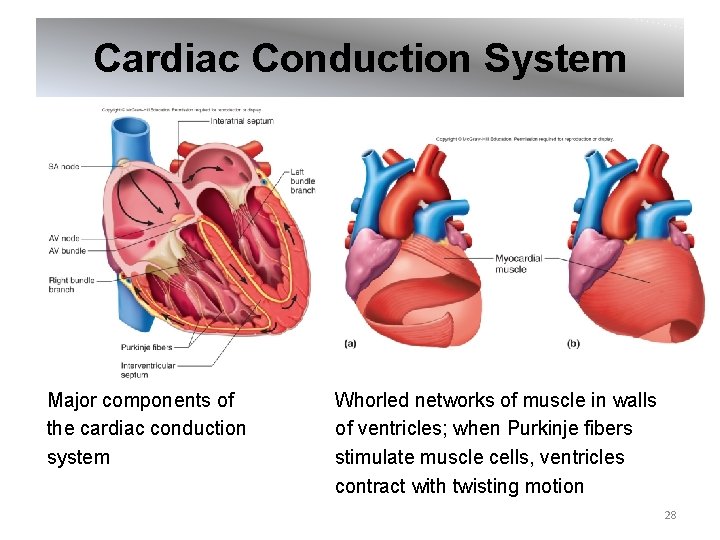
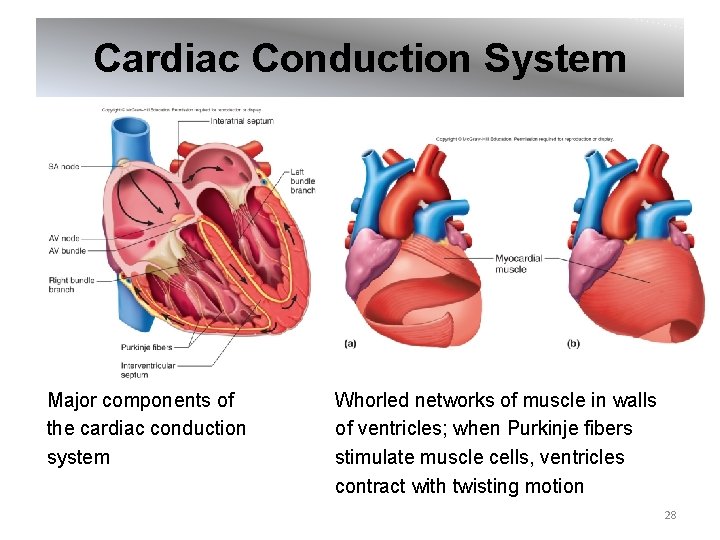
Cardiac Conduction System Major components of the cardiac conduction system Whorled networks of muscle in walls of ventricles; when Purkinje fibers stimulate muscle cells, ventricles contract with twisting motion 28
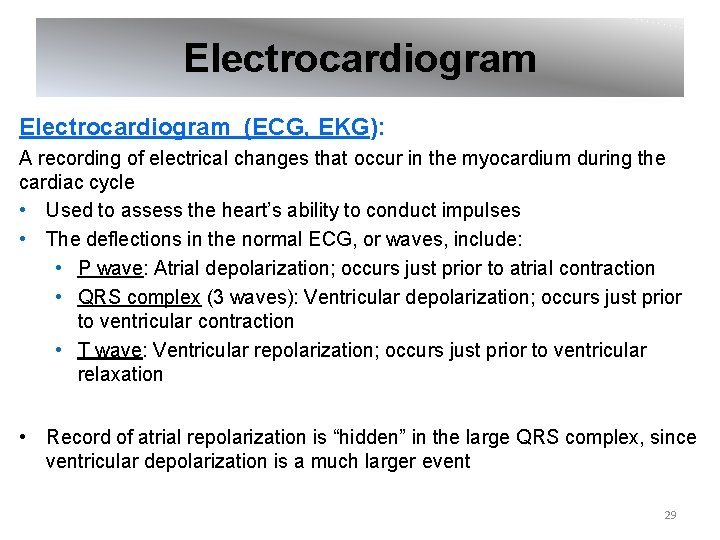
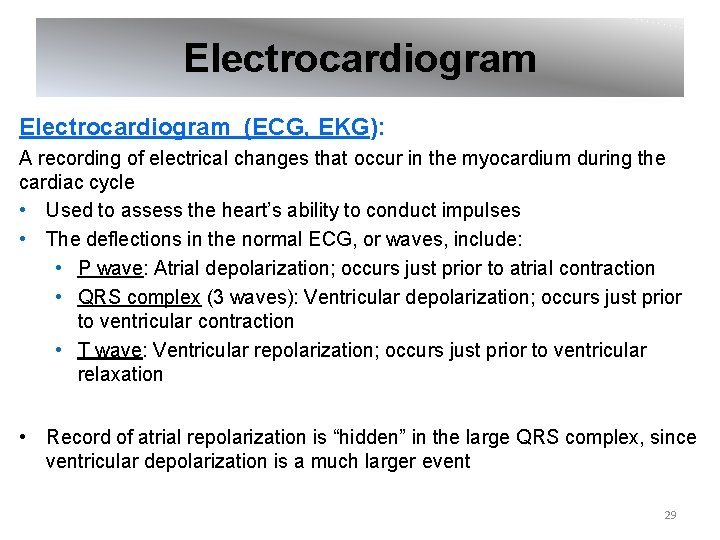
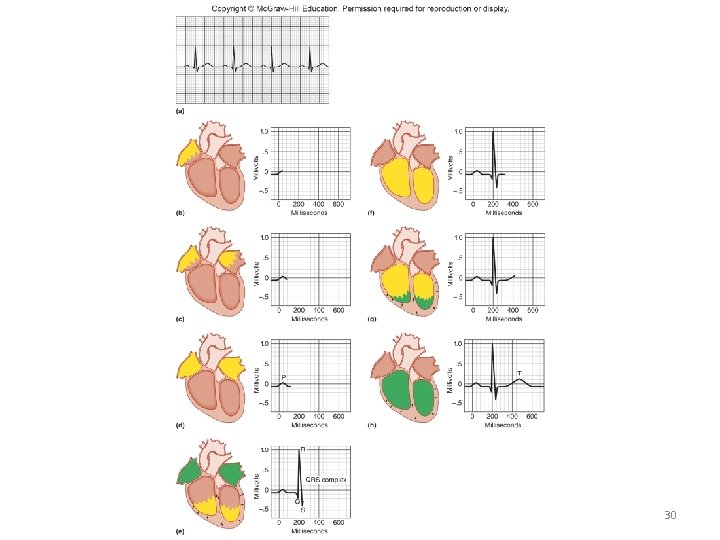
Electrocardiogram (ECG, EKG): A recording of electrical changes that occur in the myocardium during the cardiac cycle • Used to assess the heart’s ability to conduct impulses • The deflections in the normal ECG, or waves, include: • P wave: Atrial depolarization; occurs just prior to atrial contraction • QRS complex (3 waves): Ventricular depolarization; occurs just prior to ventricular contraction • T wave: Ventricular repolarization; occurs just prior to ventricular relaxation • Record of atrial repolarization is “hidden” in the large QRS complex, since ventricular depolarization is a much larger event 29
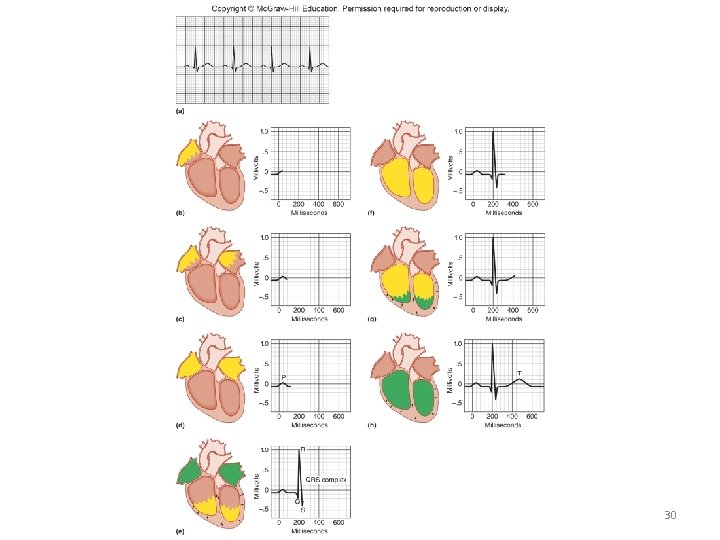
30
31
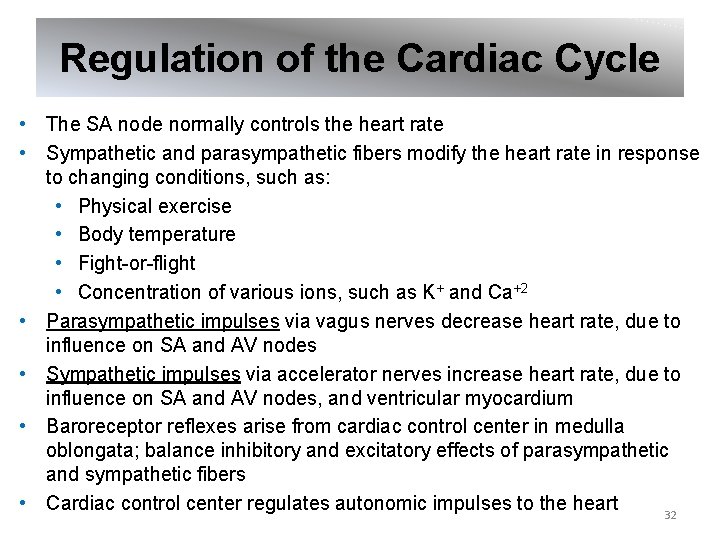
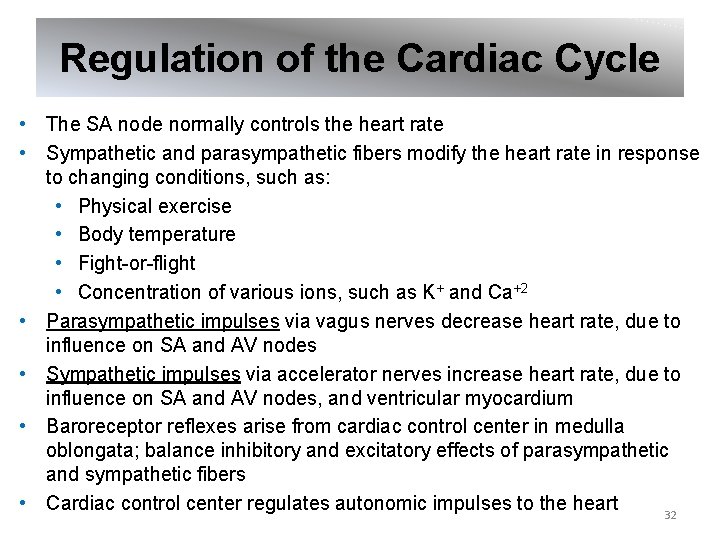
Regulation of the Cardiac Cycle • The SA node normally controls the heart rate • Sympathetic and parasympathetic fibers modify the heart rate in response to changing conditions, such as: • Physical exercise • Body temperature • Fight-or-flight • Concentration of various ions, such as K+ and Ca+2 • Parasympathetic impulses via vagus nerves decrease heart rate, due to influence on SA and AV nodes • Sympathetic impulses via accelerator nerves increase heart rate, due to influence on SA and AV nodes, and ventricular myocardium • Baroreceptor reflexes arise from cardiac control center in medulla oblongata; balance inhibitory and excitatory effects of parasympathetic and sympathetic fibers • Cardiac control center regulates autonomic impulses to the heart 32
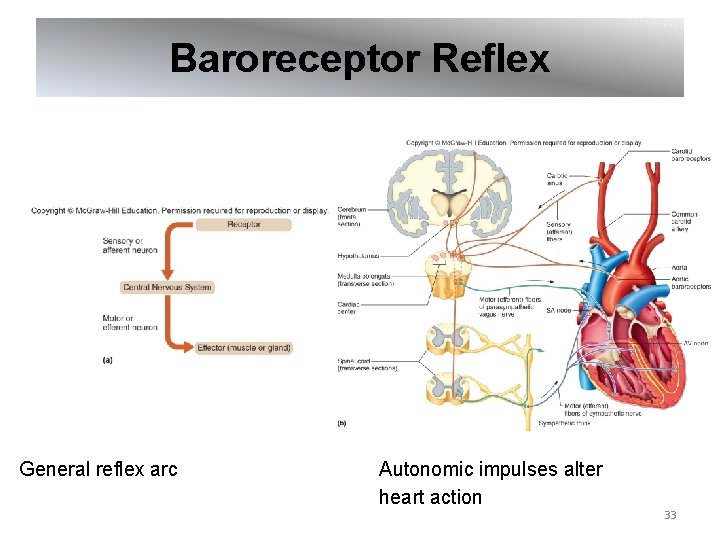
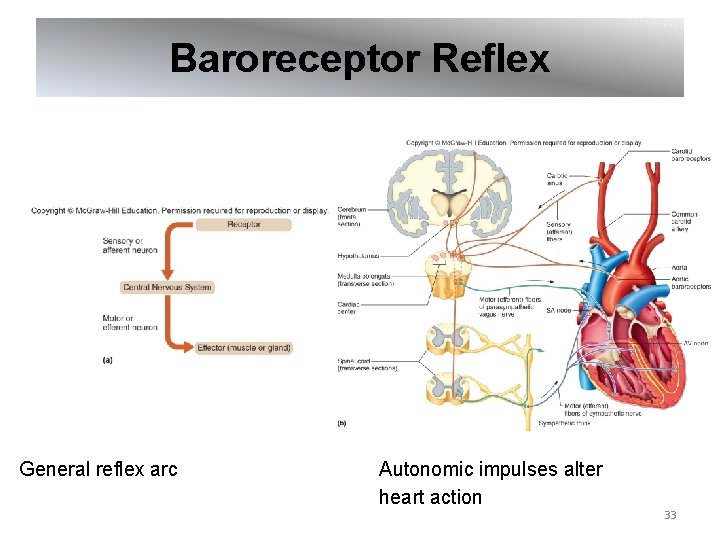
Baroreceptor Reflex General reflex arc Autonomic impulses alter heart action 33
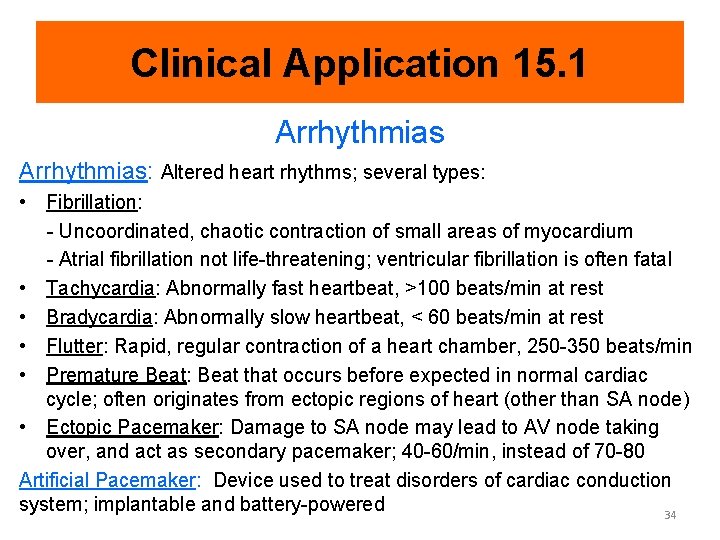
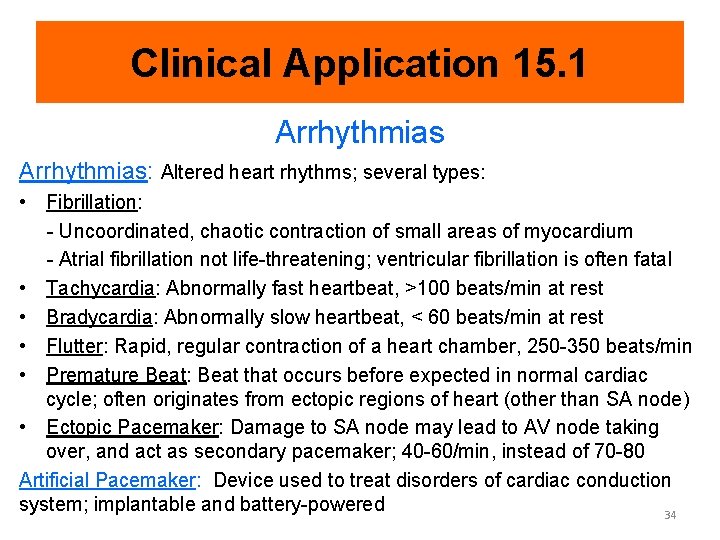
Clinical Application 15. 1 Arrhythmias: Altered heart rhythms; several types: • Fibrillation: - Uncoordinated, chaotic contraction of small areas of myocardium - Atrial fibrillation not life-threatening; ventricular fibrillation is often fatal • Tachycardia: Abnormally fast heartbeat, >100 beats/min at rest • Bradycardia: Abnormally slow heartbeat, < 60 beats/min at rest • Flutter: Rapid, regular contraction of a heart chamber, 250 -350 beats/min • Premature Beat: Beat that occurs before expected in normal cardiac cycle; often originates from ectopic regions of heart (other than SA node) • Ectopic Pacemaker: Damage to SA node may lead to AV node taking over, and act as secondary pacemaker; 40 -60/min, instead of 70 -80 Artificial Pacemaker: Device used to treat disorders of cardiac conduction system; implantable and battery-powered 34
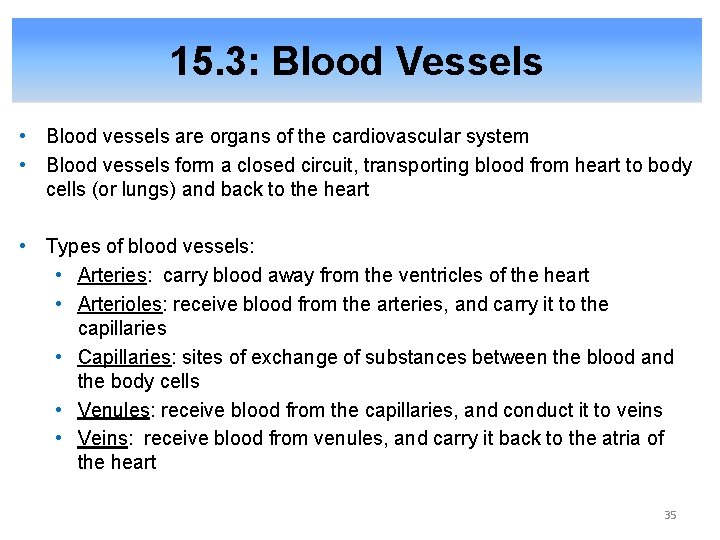
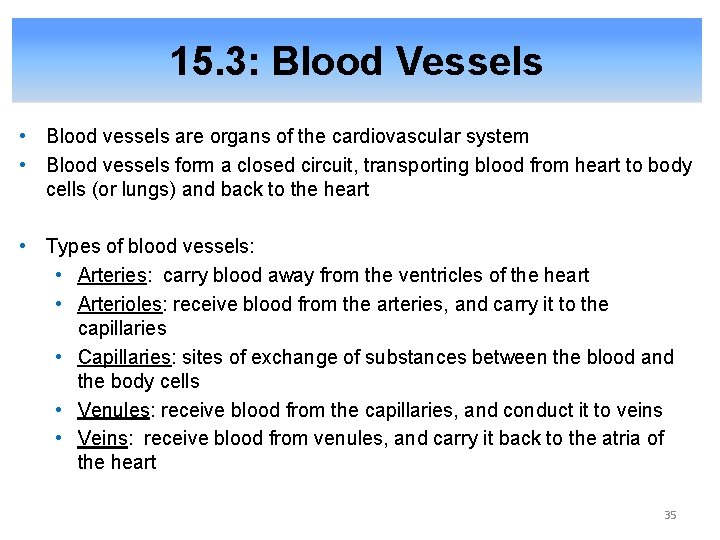
15. 3: Blood Vessels • Blood vessels are organs of the cardiovascular system • Blood vessels form a closed circuit, transporting blood from heart to body cells (or lungs) and back to the heart • Types of blood vessels: • Arteries: carry blood away from the ventricles of the heart • Arterioles: receive blood from the arteries, and carry it to the capillaries • Capillaries: sites of exchange of substances between the blood and the body cells • Venules: receive blood from the capillaries, and conduct it to veins • Veins: receive blood from venules, and carry it back to the atria of the heart 35
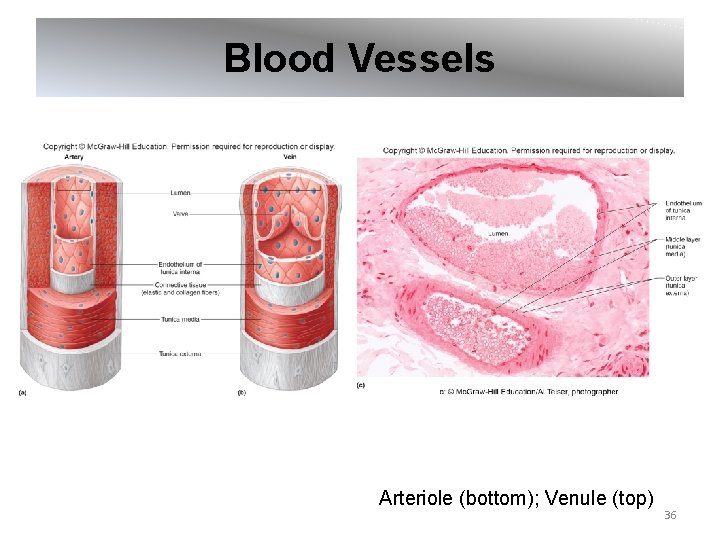
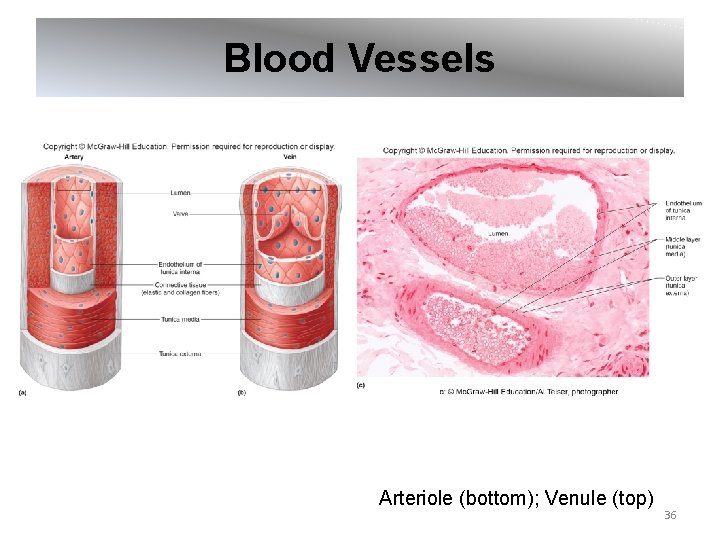
Blood Vessels Arteriole (bottom); Venule (top) 36
From Science to Technology 15. 2 Altering Angiogenesis • Angiogenesis: Formation of new blood vessels • Angiogenesis is mainly controlled by Vascular Endothelial Growth Factor (VEGF) • Angiogenesis is regulated in the body, since excess, deficient, or inappropriate blood vessel formation cause common diseases • Promoting angiogenesis: - Body secretes VEGF in response to blocked coronary artery - If this is not sufficient, VEGF may be able to be delivered in time-release capsules • Preventing angiogenesis: - Tumors secrete VEGF to nourish themselves - Antiangiogenesis drugs are used to treat cancer and age-related macular degeneration 37
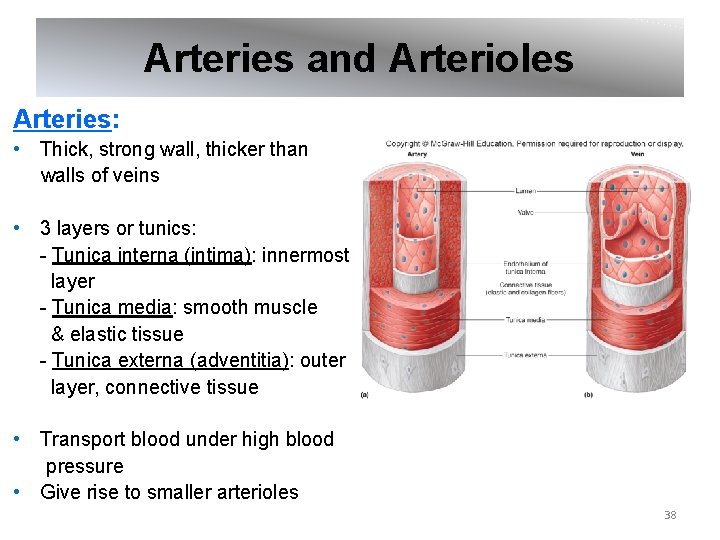
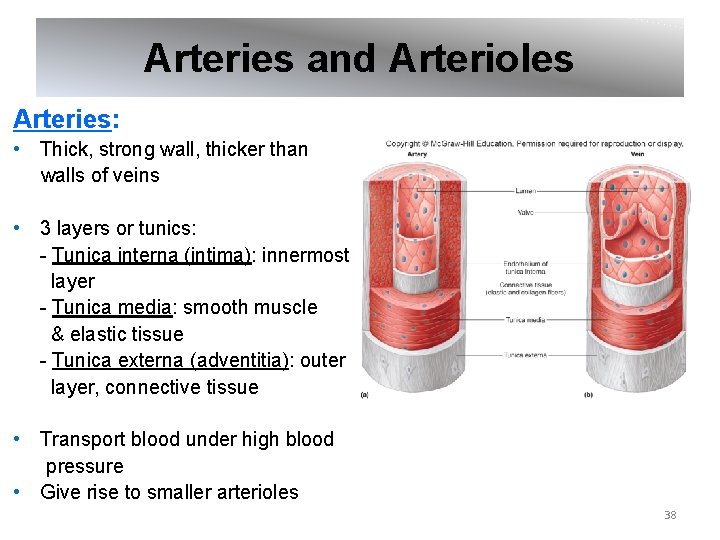
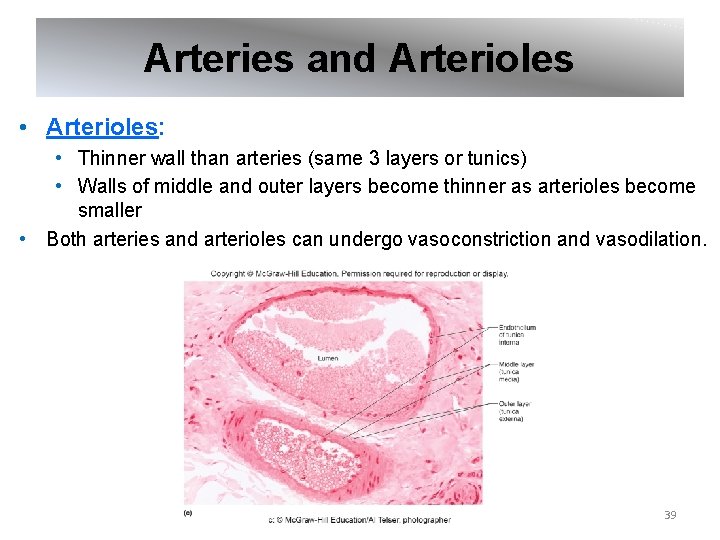
Arteries and Arterioles Arteries: • Thick, strong wall, thicker than walls of veins • 3 layers or tunics: - Tunica interna (intima): innermost layer - Tunica media: smooth muscle & elastic tissue - Tunica externa (adventitia): outer layer, connective tissue • Transport blood under high blood pressure • Give rise to smaller arterioles 38
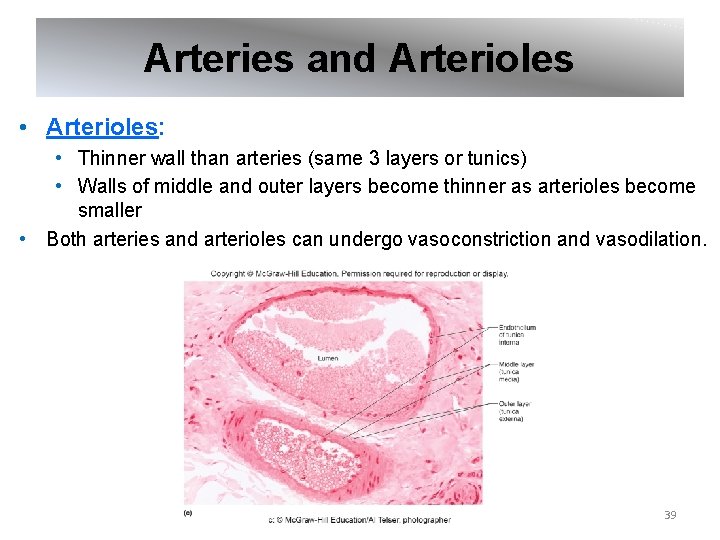
Arteries and Arterioles • Arterioles: • Thinner wall than arteries (same 3 layers or tunics) • Walls of middle and outer layers become thinner as arterioles become smaller • Both arteries and arterioles can undergo vasoconstriction and vasodilation. 39
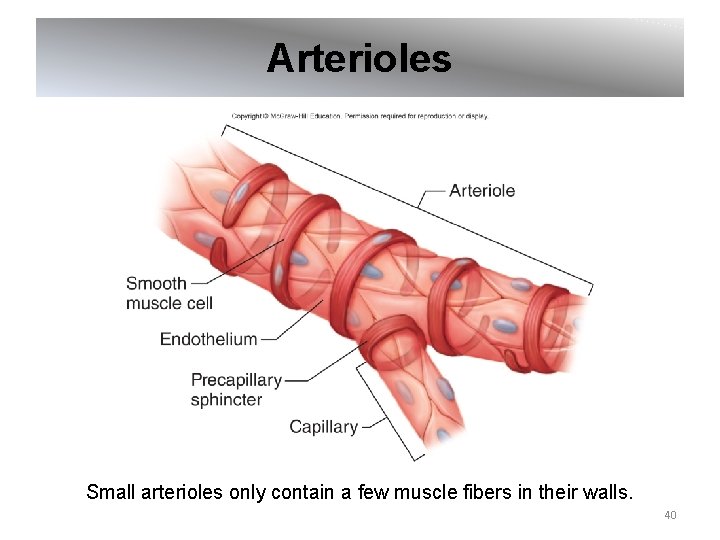
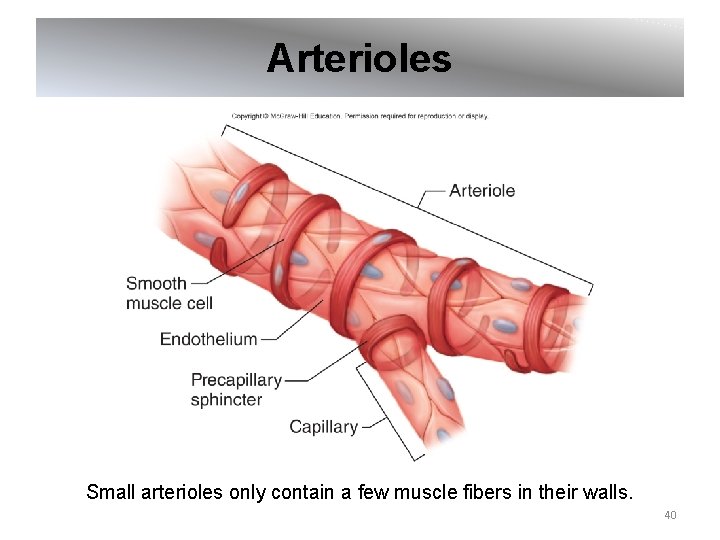
Arterioles Small arterioles only contain a few muscle fibers in their walls. 40
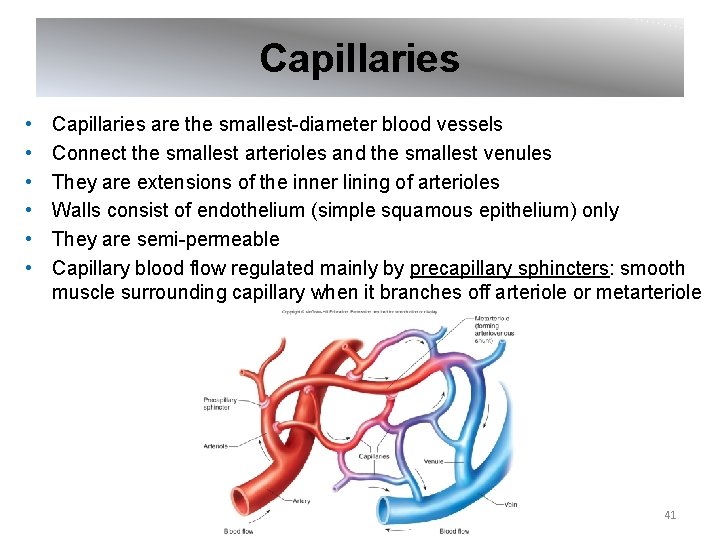
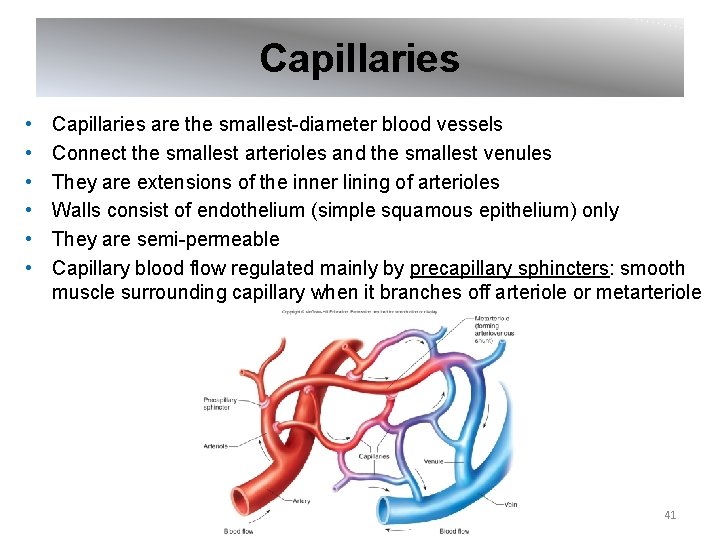
Capillaries • • • Capillaries are the smallest-diameter blood vessels Connect the smallest arterioles and the smallest venules They are extensions of the inner lining of arterioles Walls consist of endothelium (simple squamous epithelium) only They are semi-permeable Capillary blood flow regulated mainly by precapillary sphincters: smooth muscle surrounding capillary when it branches off arteriole or metarteriole 41

Capillary Structure & Permeability Substances are exchanged by diffusion. Openings in walls of capillaries are thin slits found where endothelial cells overlap. Sizes of openings vary among tissues; permeability varies with size of slits. 42
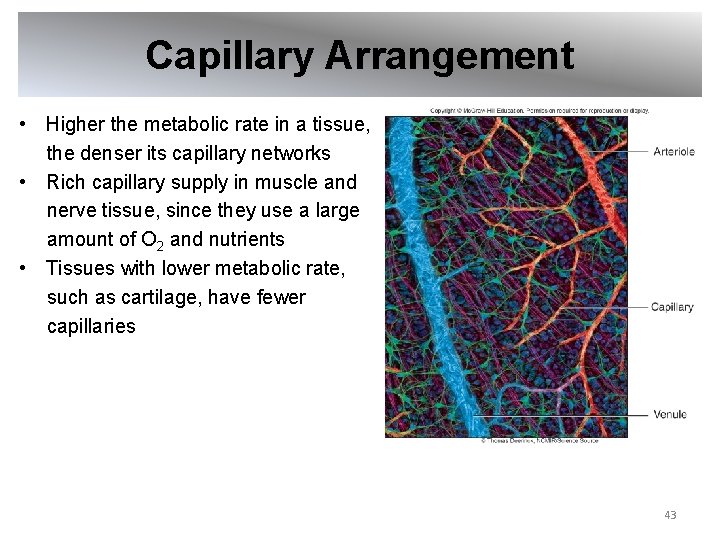
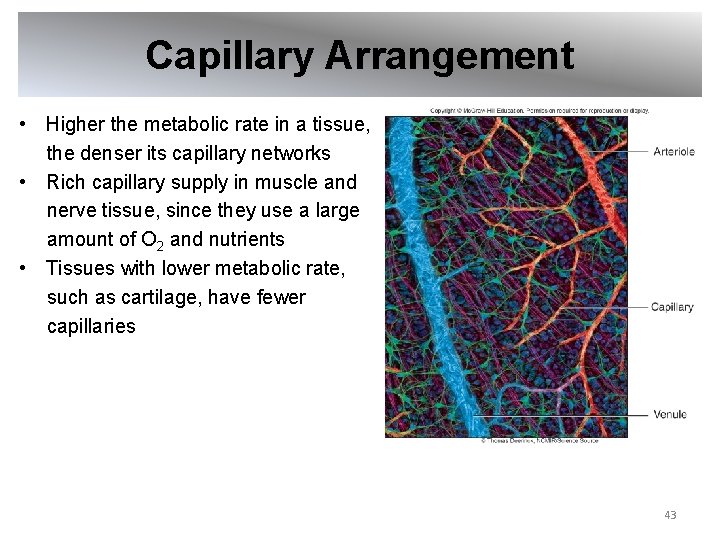
Capillary Arrangement • Higher the metabolic rate in a tissue, the denser its capillary networks • Rich capillary supply in muscle and nerve tissue, since they use a large amount of O 2 and nutrients • Tissues with lower metabolic rate, such as cartilage, have fewer capillaries 43

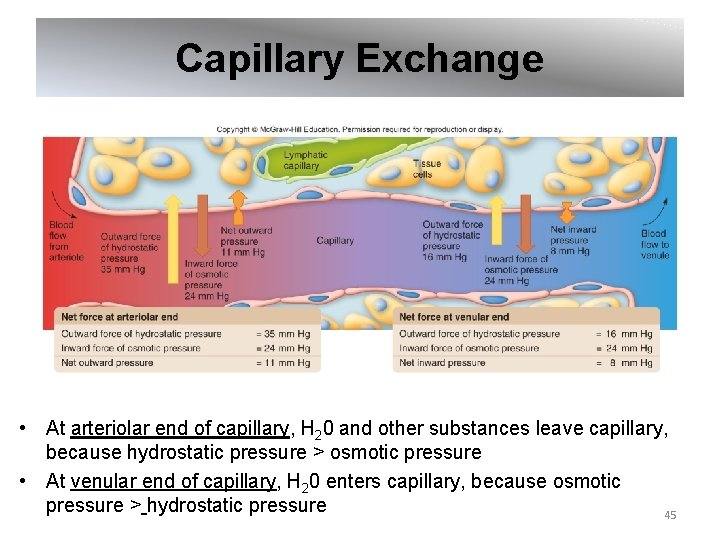
Capillary Exchange Capillaries exchange gases, nutrients, and metabolic byproducts between blood and tissue around cells. Exchange occurs by these methods: Diffusion: • Most important method of transfer • Lipid-soluble substances diffuse through cell membrane; water-soluble substances diffuse through membrane channels and slits Filtration: • Hydrostatic pressure forces molecules through membrane • Pressure is derived from ventricular contraction Osmosis: • Presence of impermeant solute, such as plasma proteins, inside capillaries creates osmotic pressure • Osmotic pressure draws water into capillaries, opposing filtration 44
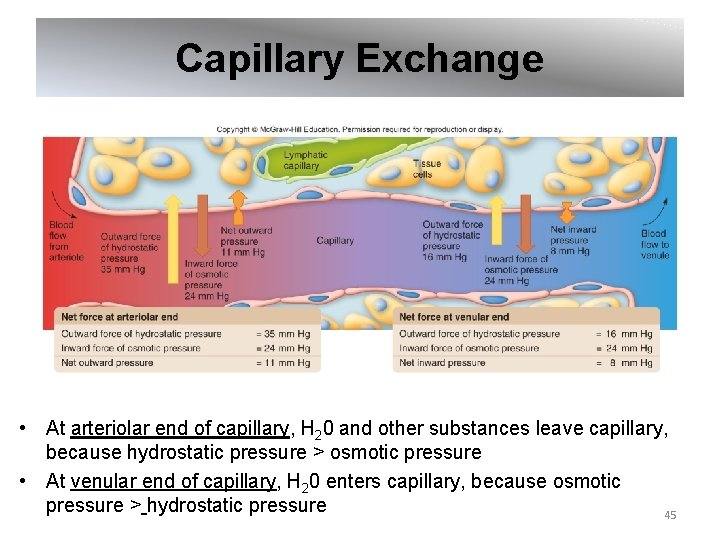
Capillary Exchange • At arteriolar end of capillary, H 20 and other substances leave capillary, because hydrostatic pressure > osmotic pressure • At venular end of capillary, H 20 enters capillary, because osmotic pressure > hydrostatic pressure 45
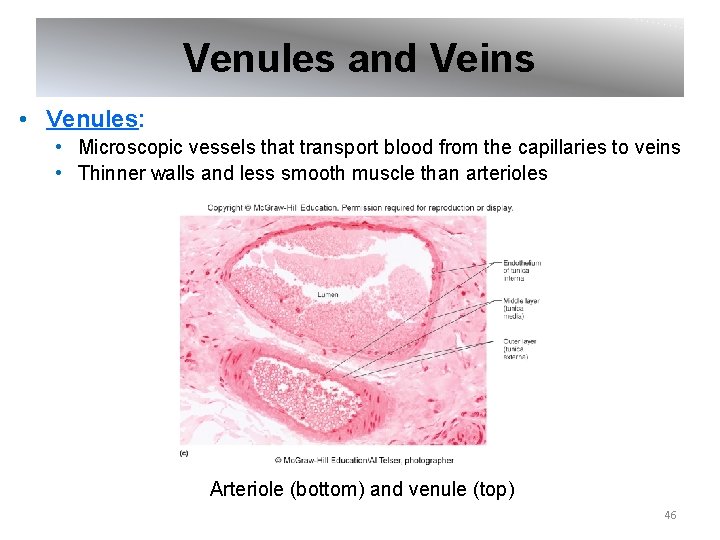
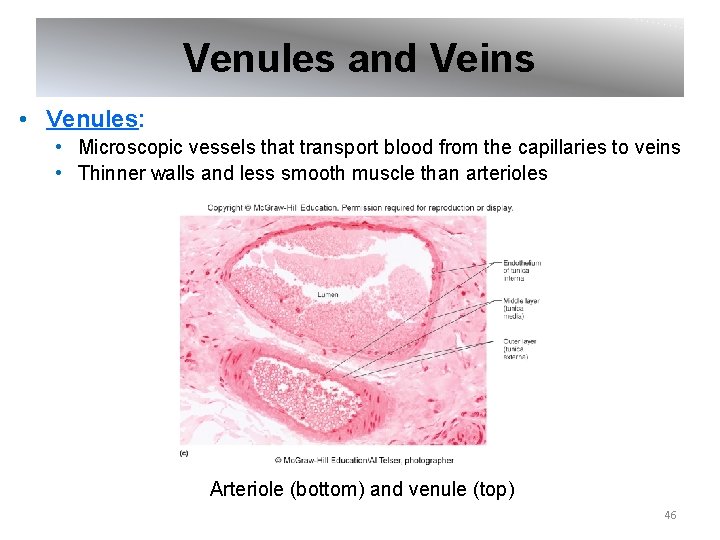
Venules and Veins • Venules: • Microscopic vessels that transport blood from the capillaries to veins • Thinner walls and less smooth muscle than arterioles Arteriole (bottom) and venule (top) 46
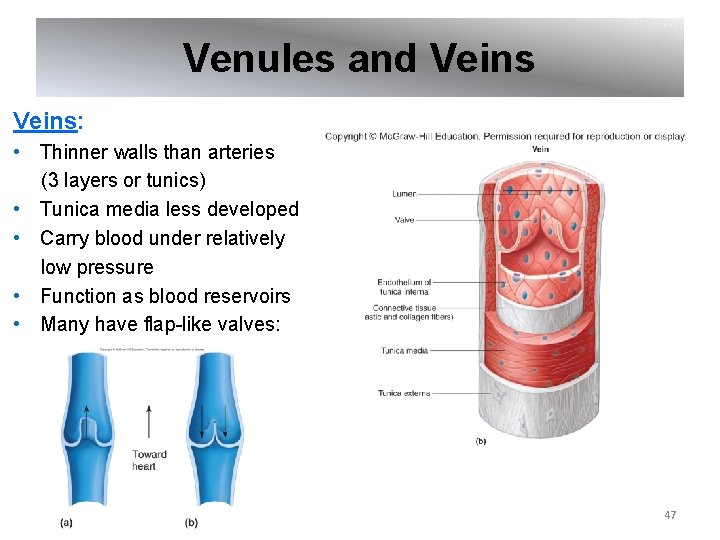
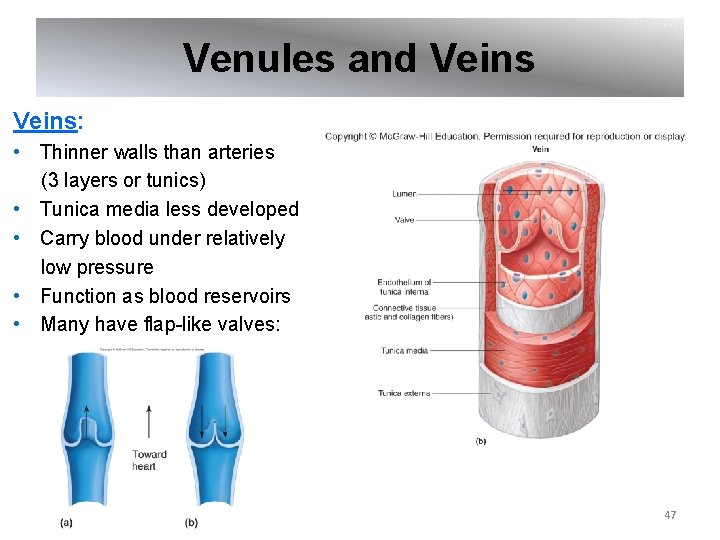
Venules and Veins: • Thinner walls than arteries (3 layers or tunics) • Tunica media less developed • Carry blood under relatively low pressure • Function as blood reservoirs • Many have flap-like valves: 47
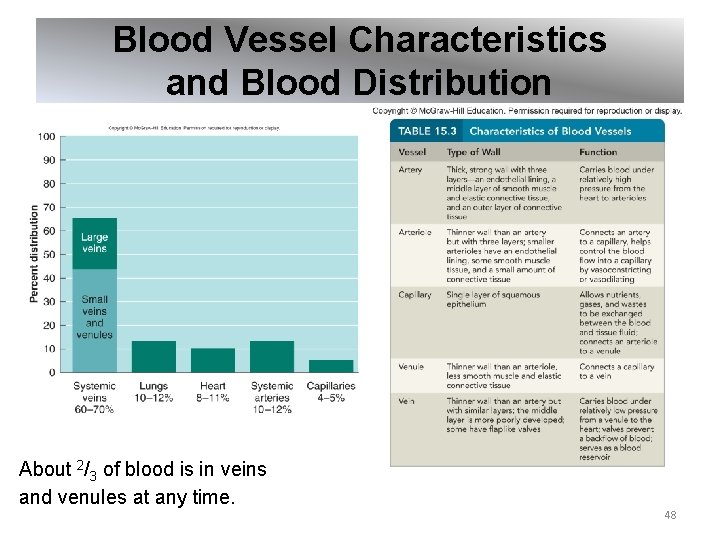
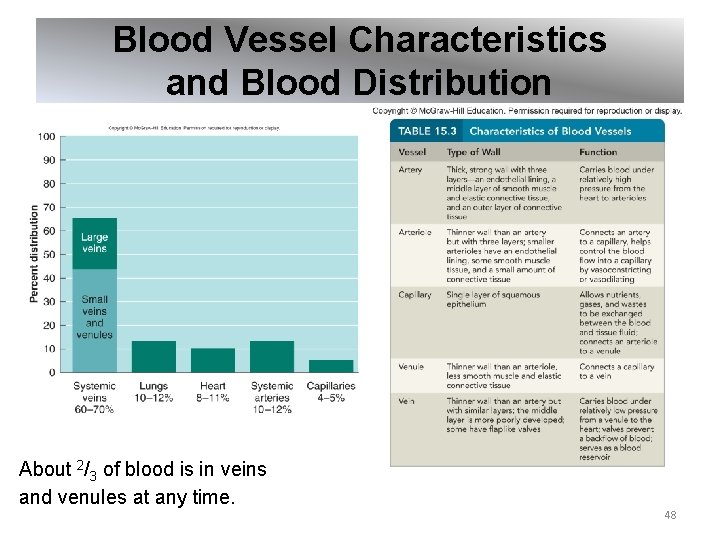
Blood Vessel Characteristics and Blood Distribution About 2/3 of blood is in veins and venules at any time. 48