CH 4 PULMONARY ASPERGILLOSIS CT ASPECTS AND ANATOMO

- Slides: 28
CH 4 PULMONARY ASPERGILLOSIS: CT ASPECTS AND ANATOMO RADIOLOGICAL CORRELATION F. Z. Belhoussine 1, M. Boubbou 1, B. Alami 1 , S. Boumezaoued 2, M. Serraj 2, Y. Wadouni 3, M. Smahi 3, S. Tizniti 1 Department of Radiology 1, CHU Hassan II, Fez Department of Pulmonary Medecine 2, CHU Hassan II, Fez Department of Thoracic Surgery 3, CHU Hassan II, Fez
INTRODUCTION Pulmonary aspergillosis is a hot topic. These infections are not unusual, especially in the context of chronic obstructive pulmonary and immune depressed about. The diagnosis can be strongly evoked in front of several radiological imaging. CT is more sensitive than plain films in the detection of occult or small lesion and more accurate in delineating the extent of disease and number of aspergillomas. Confident diagnosis is difficult, it is based on cytological and histological.
OBJECTIVES: Show the interest of the scanner in the diagnosis of pulmonary aspergillosis. Show radiological aspects of different forms. Underpin suggestive radiological aspects.
BACKGROUND Pulmonary aspergillosis is a mycotic infection caused most of the times by Aspergillus Fumigatus, an ubiquitous soil fungus acquired by inhaling its spores. When we talk about aspergillosis we are referring to a spectrum of radiologic and clinical manifestations that depend directly of the immunological state of the patient and the virulence of the organism. We can distinguish 4 types of pulmonary aspergillosis. • Aspergilloma (saprophytic aspergillosis) • Allergic bronchopulmonary aspergillosis (ABPA) • Semi-invasive or chronic necrotizing aspergillosis • Invasive aspergillosis (which can be divided into airway invasive and angioinvasive forms).
MATERIALS AND METHODS: A retrospective study involving 30 patients collected for department of radiology and lung diseases over 3 years. Median age is 41 years (22 - 67 years). Chest CT scan was performed without injection of contrast and fine reformatted reconstructions in all patients. Bell in front of a picture, another acquisition in the prone position was performed. Histological confirmation was performed in all patients.
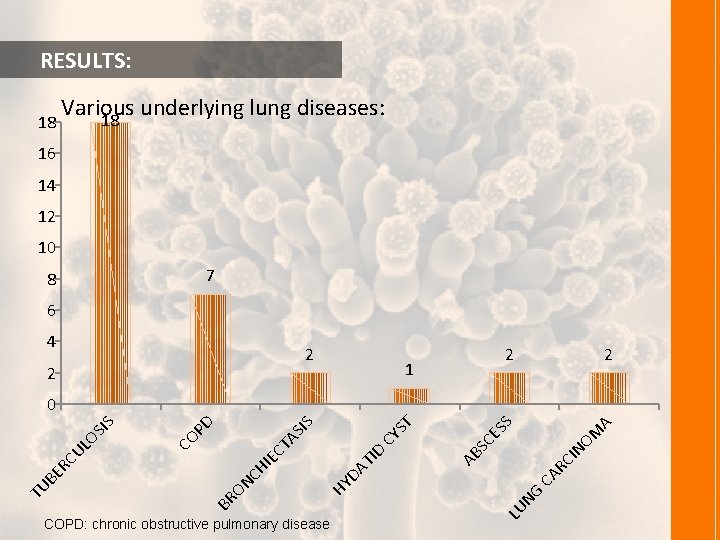
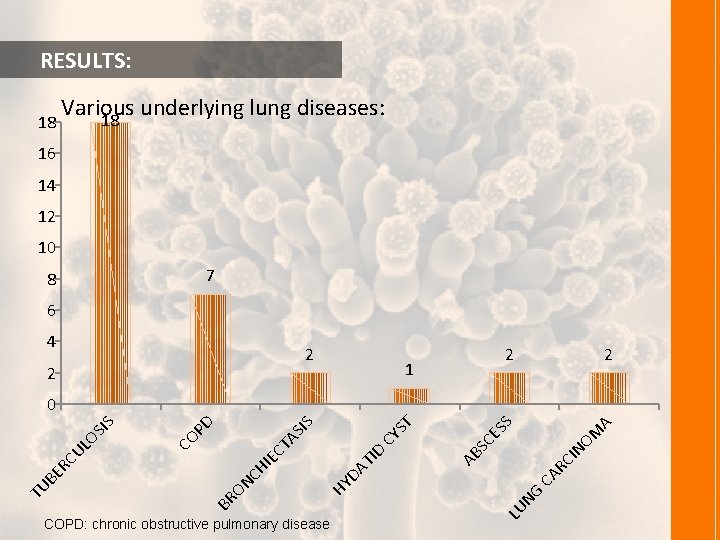
RESULTS: 18 Various underlying lung diseases: 18 16 14 12 10 7 8 6 4 2 2 2 1 2 M NO CI AR C NG LU COPD: chronic obstructive pulmonary disease A ES S SC AB ST D TI DA HY ON CH IE CT CY AS IS PD CO BR TU BE RC UL OS IS 0
RESULTS: radiographic and CT findings were abnormal in all patients. A preoperative diagnosis of aspergilloma considering : Their radiological examination in 20 cases. Radiological examination and isolation of Aspergillus fumigatus, in the bronchial aspirate in 2 cases. A postoperative diagnosis of aspergilloma in 8 cases.
RESULTS: The spectrum of CT finding were: Aspergilloma with air crescent sign in 7 cases. Bronchectasis in 4 cases. Chronic consolidation in 15 cases. Multiples nodules with progressive cavitation 18 cases. Hydropneumothorax in 2 cases. Abcess in 1 case. Lung destruction in 3 cases.
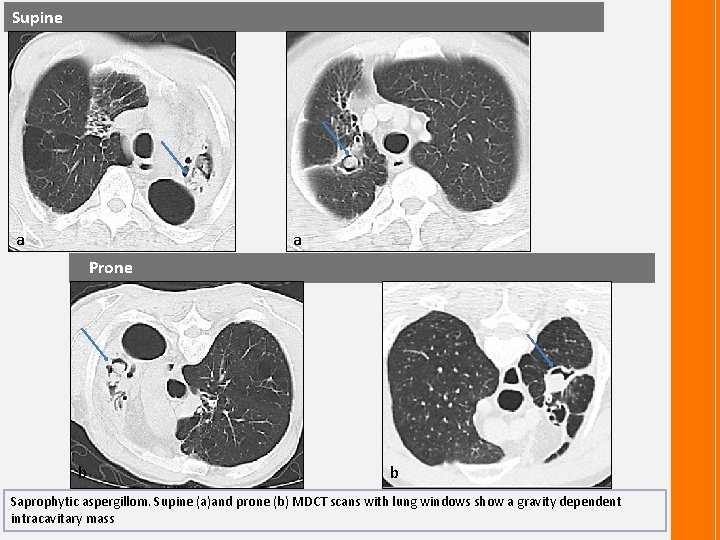
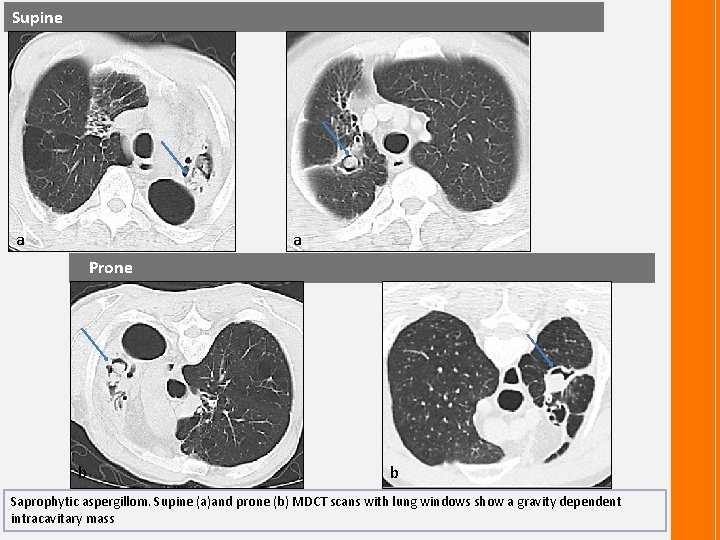
Supine a a Prone b b Saprophytic aspergillom. Supine (a)and prone (b) MDCT scans with lung windows show a gravity dependent intracavitary mass
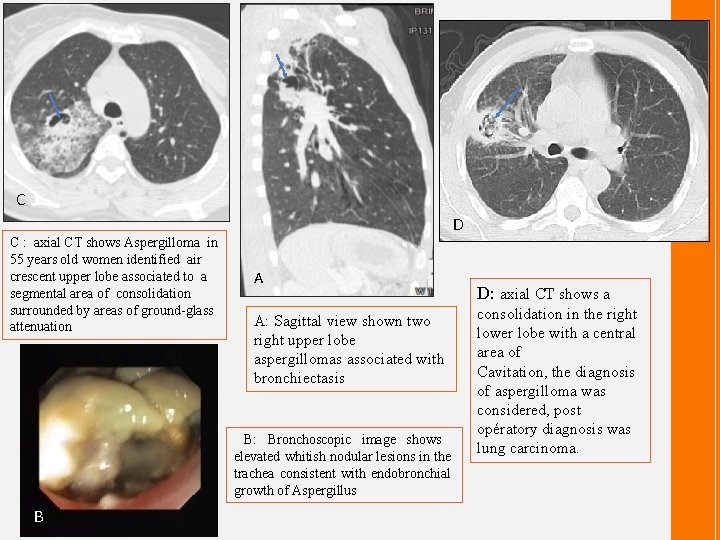
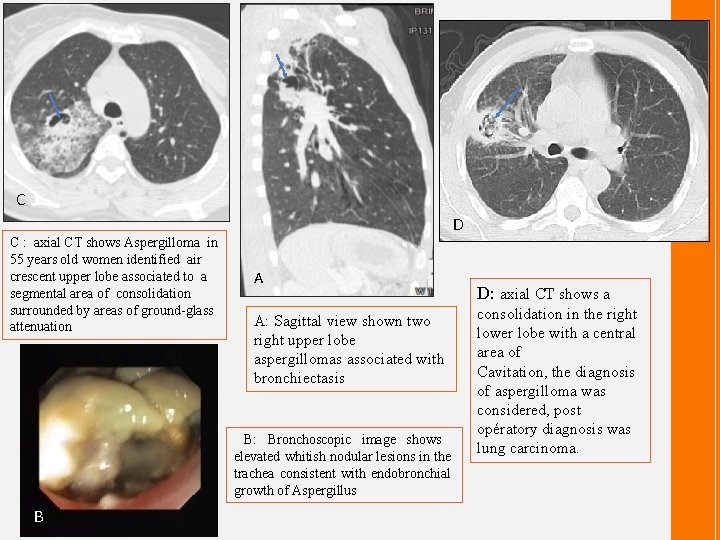
C D C : axial CT shows Aspergilloma in 55 years old women identified air crescent upper lobe associated to a segmental area of consolidation surrounded by areas of ground-glass attenuation A A: Sagittal view shown two right upper lobe aspergillomas associated with bronchiectasis B: Bronchoscopic image shows elevated whitish nodular lesions in the trachea consistent with endobronchial growth of Aspergillus B D: axial CT shows a consolidation in the right lower lobe with a central area of Cavitation, the diagnosis of aspergilloma was considered, post opératory diagnosis was lung carcinoma.
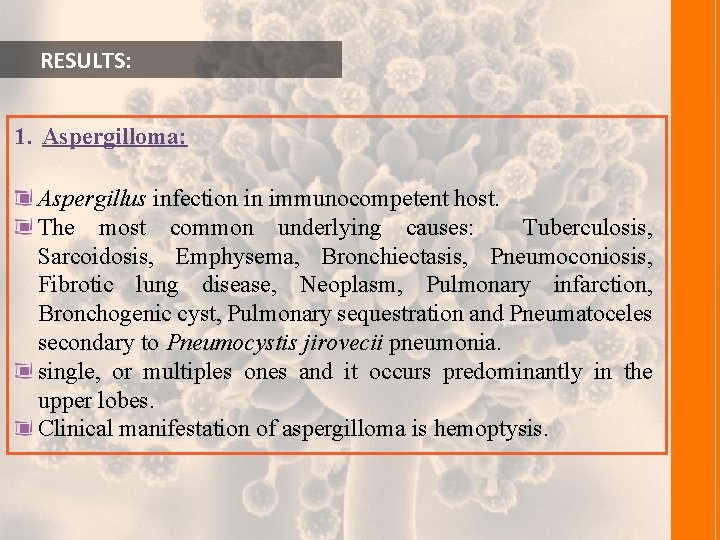
RESULTS: 1. Aspergilloma: Aspergillus infection in immunocompetent host. The most common underlying causes: Tuberculosis, Sarcoidosis, Emphysema, Bronchiectasis, Pneumoconiosis, Fibrotic lung disease, Neoplasm, Pulmonary infarction, Bronchogenic cyst, Pulmonary sequestration and Pneumatoceles secondary to Pneumocystis jirovecii pneumonia. single, or multiples ones and it occurs predominantly in the upper lobes. Clinical manifestation of aspergilloma is hemoptysis.
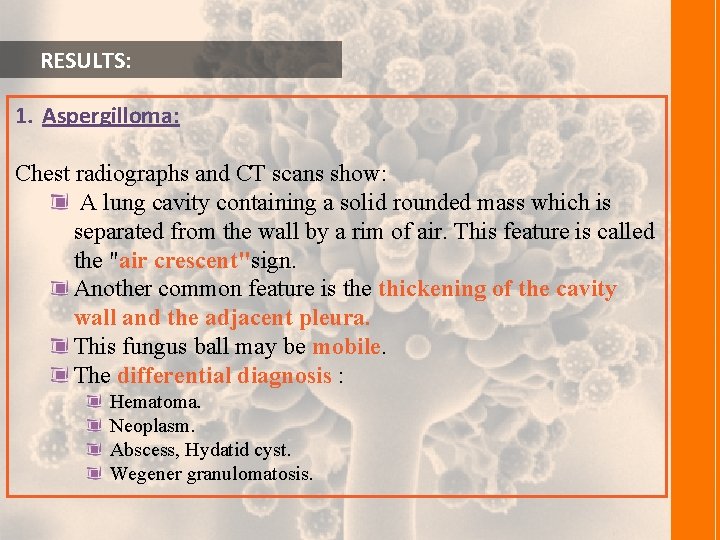
RESULTS: 1. Aspergilloma: Chest radiographs and CT scans show: A lung cavity containing a solid rounded mass which is separated from the wall by a rim of air. This feature is called the "air crescent"sign. Another common feature is the thickening of the cavity wall and the adjacent pleura. This fungus ball may be mobile. The differential diagnosis : Hematoma. Neoplasm. Abscess, Hydatid cyst. Wegener granulomatosis.

Chest radiography: Postero anterior radiographs chest shows Upper lobe opacity surrounded by air crescent: fungus ball within a cavity. CT: * a ^ b c Chest CT « a » axial « b » coronal shows a fungus ball within cavity air cresecent Surrounded this cavity, the Chest CT shows also bronchiesctasis « * » associated and multiples basal centrilobular nodules « ^ » .
RESULTS: 2. Allergic bronchopulmonary aspergillosis (ABPA): Characterized by the presence of fleeting dense plugs of mucus, hyphaes and eosinophils in lung parenchyma due to deposition of immune complexes and inflammatory cells within the segmental and subsegmental bronchi. ABPA represents a hypersensitivity reaction to Aspergillus occurring almost exclusively in long-standing bronchial asthma patients and occasionally as a complication of cystic fibrosis.
RESULTS: 2. Allergic bronchopulmonary aspergillosis (ABPA): Clinically : wheezing, cough and fever. Eosinophilia and elevated serum Ig. E levels are typically found and they can suggest the diagnosis. Initial radiologic manifestations: Transitory pulmonary opacities (deposition of immune complexes and inflammatory cells in the alveoli). An irreversible damage occurs to the bronchi with dilatation, wall thickening and mucus plugging. CT findings: tubular or saccular finger-in-glove areas of increased opacity in a bronchial distribution representing mucus plugging within bronchiectasis, predominantly involving the upper lobes.
RESULTS: 2. Allergic bronchopulmonary aspergillosis (ABPA): The diagnosis is made by a combination of criteria: Episodic asthma exacerbations. Transient or fixed pulmonary infiltrates. Central bronchiectasis. Peripheral blood eosinophilia. Elevated serum Ig. E levels. Positive Aspergillus precipitins.
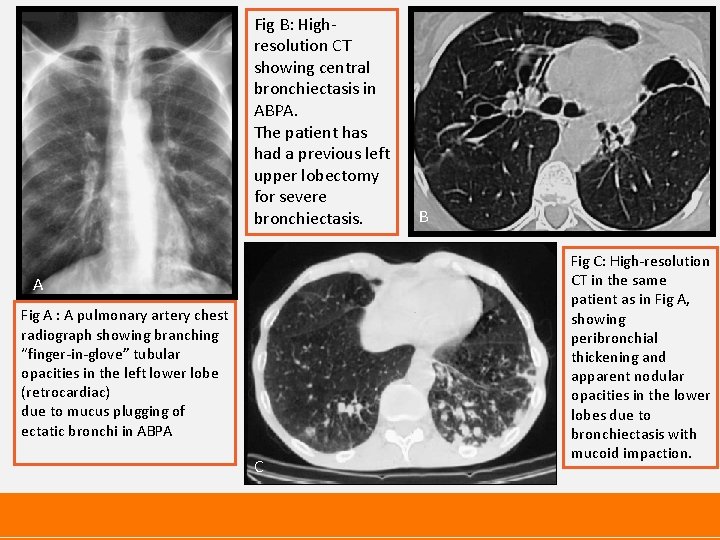
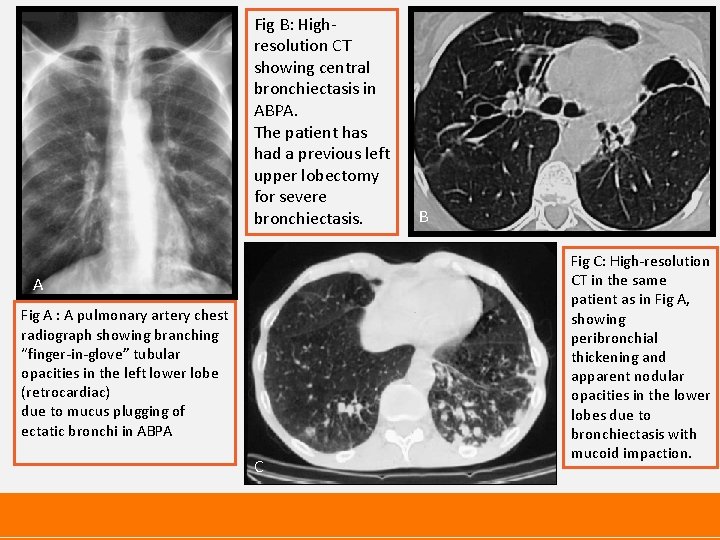
Fig B: Highresolution CT showing central bronchiectasis in ABPA. The patient has had a previous left upper lobectomy for severe bronchiectasis. A Fig A : A pulmonary artery chest radiograph showing branching “finger-in-glove” tubular opacities in the left lower lobe (retrocardiac) due to mucus plugging of ectatic bronchi in ABPA C B Fig C: High-resolution CT in the same patient as in Fig A, showing peribronchial thickening and apparent nodular opacities in the lower lobes due to bronchiectasis with mucoid impaction.
RESULTS: 3. Chronic necrotizing pulmonary aspergillosis (CNPA) or semi-invasive aspergillosis: Local and more indolent form of invasive pulmonary aspergillosis. Patients with a chronic disease that predispose them to infection. Histologically: Presence of tissue necrosis and granulomatous inflammation similar to that seen in reactivated tuberculosis.
RESULTS: 3. Chronic necrotizing pulmonary aspergillosis (CNPA) or semi-invasive aspergillosis: Clinically: Chronic productive cough or with hemoptysis, which varies from severe to trivial. Radiologically: chronic consolidation. Multiples nodules with progressive cavitation in one or both upper lobes. Non-specific, most commonly mimicking those of mycobacterial infection. lesions are more peripheral, associate pleural thickening and mayprogress to form a bronchopleural fistula.
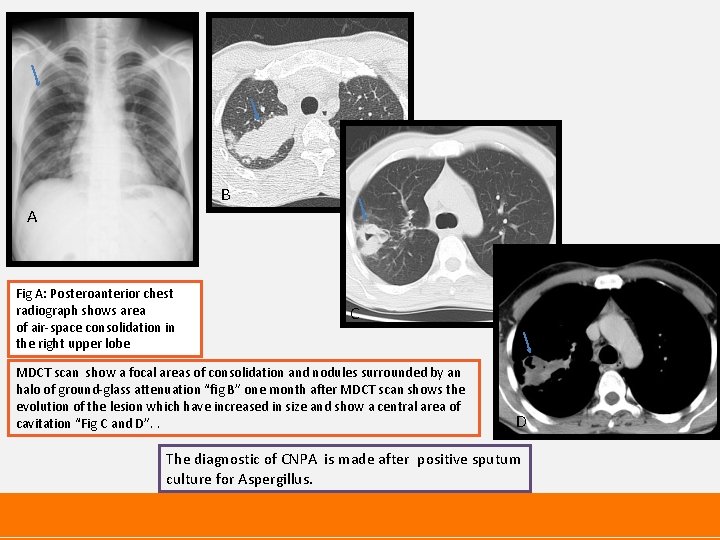
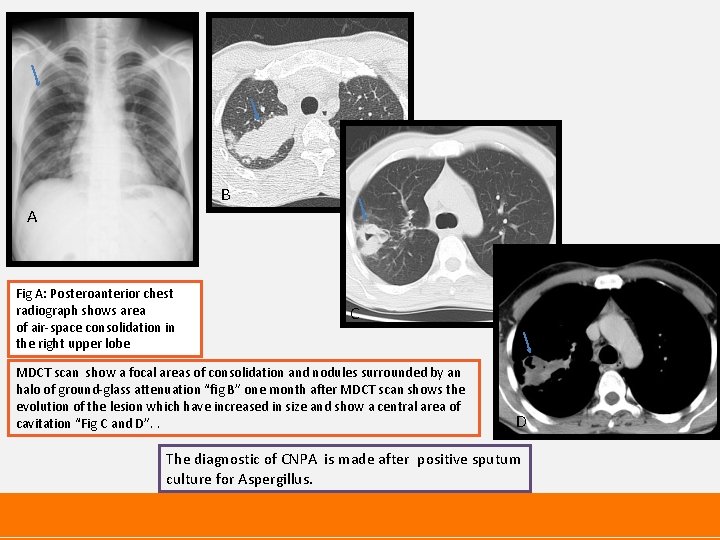
B A Fig A: Posteroanterior chest radiograph shows area of air-space consolidation in the right upper lobe C MDCT scan show a focal areas of consolidation and nodules surrounded by an halo of ground-glass attenuation “fig B” one month after MDCT scan shows the evolution of the lesion which have increased in size and show a central area of cavitation “Fig C and D”. . D The diagnostic of CNPA is made after positive sputum culture for Aspergillus.
RESULTS: 4. Invasive pulmonary aspergillosis (IPA): Mortality : of up to 85%. Occurs in severe immunocompromised patients, especially in those with neutropenia due to hematologic malignancies, chemotherapy or immunosuppressive therapy. Depending on the route of spread we can discern two kinds of invasive aspergillosis: Angioinvasive. Airway invasive. which can even coexist in the same patient. However, this is just a histological and etiopathogenical distinction as, in the clinical practice, this is not relevant for therapy.
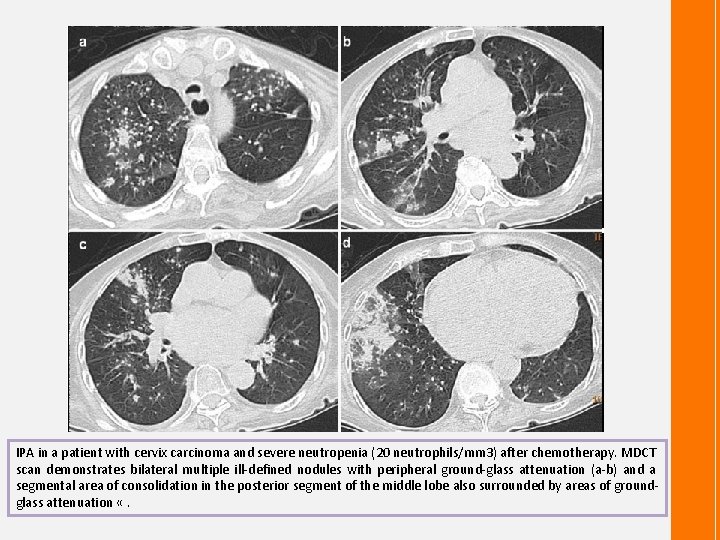
RESULTS: 4. Invasive pulmonary aspergillosis (IPA): a. Angioinvasive aspergillosis Is histologically characterized by invasion of small to mediumsized vessels by fungal hyphae. This results in thrombus formation and vascular occlusion with the consequent tissue necrosis and systemic dissemination. CT scans shows: Early IPA: Small nodules and/or small pleuralbased, wedge-shaped consolidations with a surrounding halo of ground-glass attenuation (halo sign). The halo sign represents alveolar hemorrhage. As the disease progresses the nodules may cavitate, the necrotic parenchyma detaches from the adjacent lung forming an air crescent similar to that seen in aspergilloma. In the right clinical context, nodules or consolidations surrounded by a ground-glass halo, progressing to cavitation or air crescent formation are considered typical of angio invasive aspergillosis.
RESULTS: 4. Invasive pulmonary aspergillosis (IPA): b. Invasive aspergillosis of the airways : 14%-34% of cases of invasive aspergillosis. Includes bronchitis and bronchiolitis, bronchopneumonia and lobar pneumonia without evidence of vascular invasion. Surrounding the involved airway there is often a variably sized zone of hemorrhage and/or organizing pneumonia.
RESULTS: 4. Invasive pulmonary aspergillosis (IPA): b. Invasive aspergillosis of the airways : In the majority of cases, radiographic findings of invasive aspergillosis of the airways appear as: Patchy peribronchial consolidation. Centrilobular nodules. Areas of tree-in-bud pattern. These features are non-specific and are indistinguishable from those of bronchopneumonia caused by other microorganisms.
RESULTS: 4. Invasive pulmonary aspergillosis (IPA): b. Invasive aspergillosis of the airways : This uncommon manifestation affects almost exclusively lung transplant recipients and AIDS patients. Patients experience cough, dyspnea and hemoptysis but they can also be asymptomatic. CT scans are usually normal; sometimes a non-specific tracheal wall thickening is the only evident finding. Bronchoscopy and fungal culture of the sputum proportionate a definitive diagnosis.
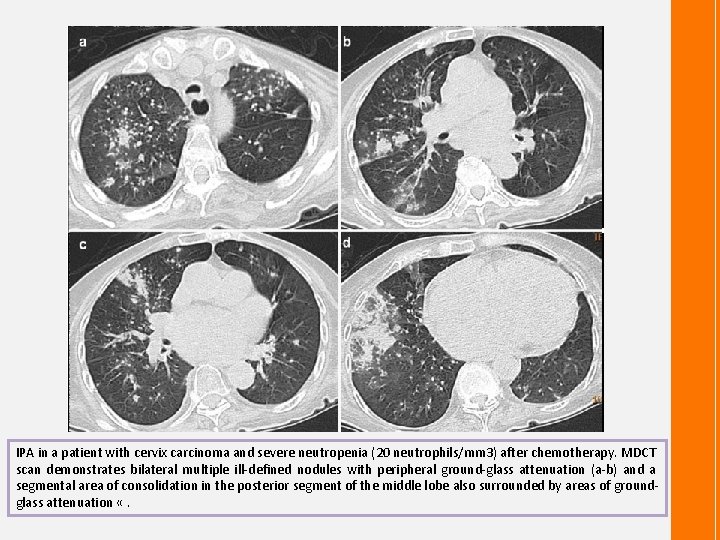
IPA in a patient with cervix carcinoma and severe neutropenia (20 neutrophils/mm 3) after chemotherapy. MDCT scan demonstrates bilateral multiple ill-defined nodules with peripheral ground-glass attenuation (a-b) and a segmental area of consolidation in the posterior segment of the middle lobe also surrounded by areas of groundglass attenuation «.
CONCLUSION: Computed tomography has become a key consideration in the diagnosis of pulmonary aspergillosis and this in front of suggestive radiological aspects. It also determines therapeutic.
Bibliography: 1 - KOREN. L, ALONSO. S, Sanchez-Nistal. M. A, Mandich. D, Daimiel. I, Ayala. G; Pulmonary aspergillosis; a spectrum of CT findings. ECR 2012: 1 -22. 2 - Caillot D, Couaillier JF, Bernard A, et al. Increasing volume and changing characteristics of invasive pulmonary aspergillosis on sequential thoracic computed tomography scans in patients with netropenia. J Clin Oncol 2001: 19: 253 -259. 3 - Franquet T, Müller N, Giménez A, Guembe P, De La Torre J, Bagué S. Spectrum of Pulmonary Aspergillosis: Histologic, Clinical, and Radiologic Findings. Radio. Graphics 2001; 21: 825 -837. 4 - R. Grech, A. Mizzi, S. Grech; Birkirkara/MT, BIRKIRKARA/MT. The protean radiological appearances of pulmonary Aspergillus infections. ECR 2011: 1 -18. 5 - Presse Med. 2001 Apr 7; 30(13): 621 -5. Role of computed tomography in pulmonary aspergillosis. 20 cases Adil A, el Amraoui F, Kadiri R. Service Central de Radiologie, CHU Ibn Rochd, Casablanca, Maroc. 6 - Ali Nawaz Khan, FRCP, FRCR, Carolyn Jones, MRCP, FRCR, and Sumaira Macdonald, MRCP FRCR. Bronchopulmonary Aspergillosis: A Review. Curr Probl Diagn Radiol, July/August 2003. p 156 -168.
 Doc for invasive aspergillosis
Doc for invasive aspergillosis Aspergillosis
Aspergillosis Aspergillosis
Aspergillosis Aspergillosis
Aspergillosis Aspergillosis symptoms
Aspergillosis symptoms What is the physiology of respiration
What is the physiology of respiration Pulmonary artery and aorta
Pulmonary artery and aorta Structure of bronchiole
Structure of bronchiole Difference between right and left bronchus
Difference between right and left bronchus Aorta and pulmonary artery
Aorta and pulmonary artery Aorta and pulmonary artery
Aorta and pulmonary artery Aortic orifice
Aortic orifice Circulatory system diagram
Circulatory system diagram Pulmonary volumes and capacities
Pulmonary volumes and capacities Total anomalous pulmonary venous return
Total anomalous pulmonary venous return Thorax cavity
Thorax cavity Pulmonary circulation pathway
Pulmonary circulation pathway Neurogenic shock
Neurogenic shock Fibrous pericardium
Fibrous pericardium Hypoventilation causes
Hypoventilation causes Pulmonary surfactant function
Pulmonary surfactant function Cvs xray
Cvs xray Flow volume loop obstructive
Flow volume loop obstructive V/q scan pulmonary embolism
V/q scan pulmonary embolism Pulmonary embolism test
Pulmonary embolism test Medslide
Medslide Complications of empyema
Complications of empyema Mediastinal surface
Mediastinal surface Windpipe cells
Windpipe cells