Trial of posaconazole therapy for chronic pulmonary aspergillosis
- Slides: 1
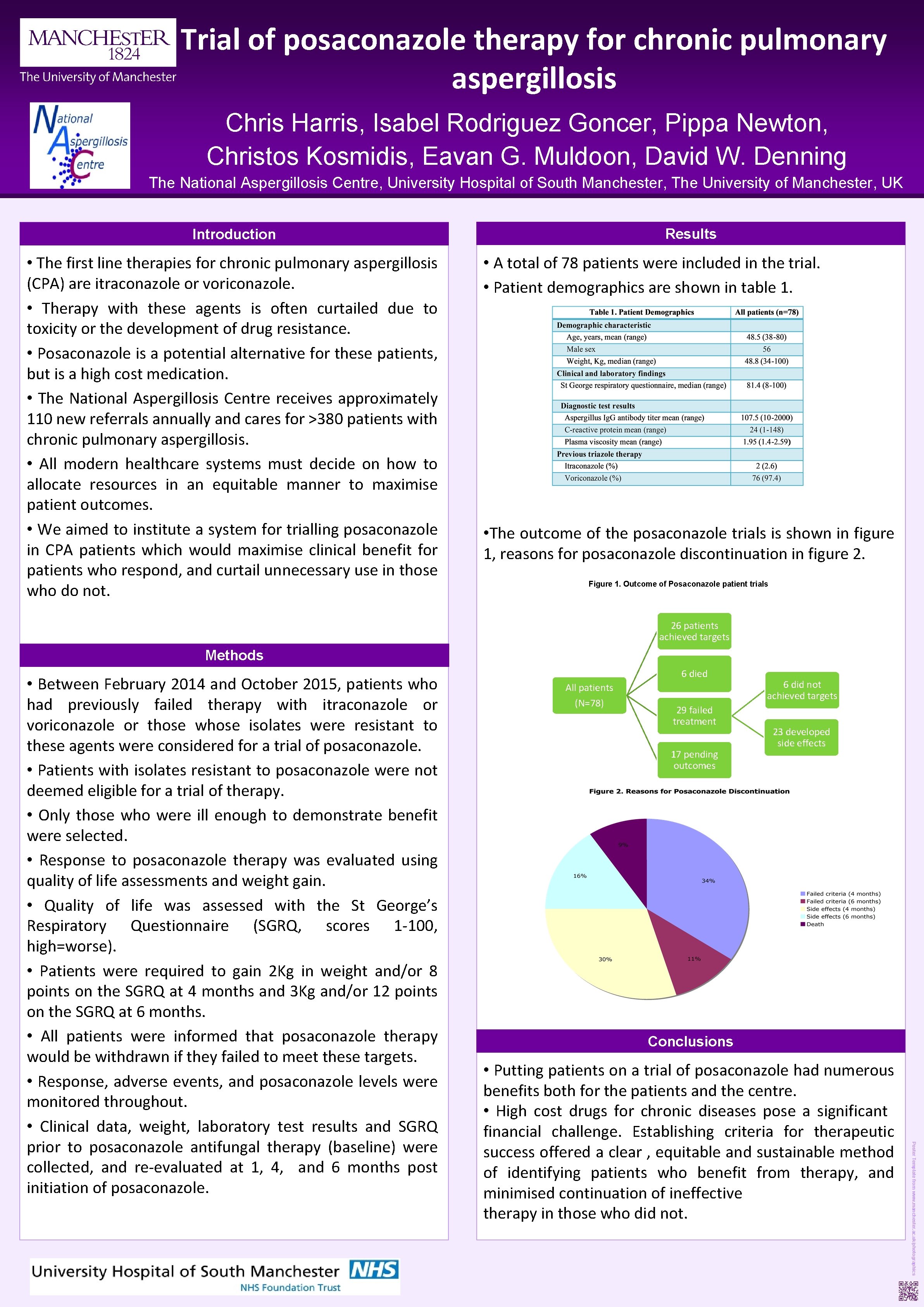
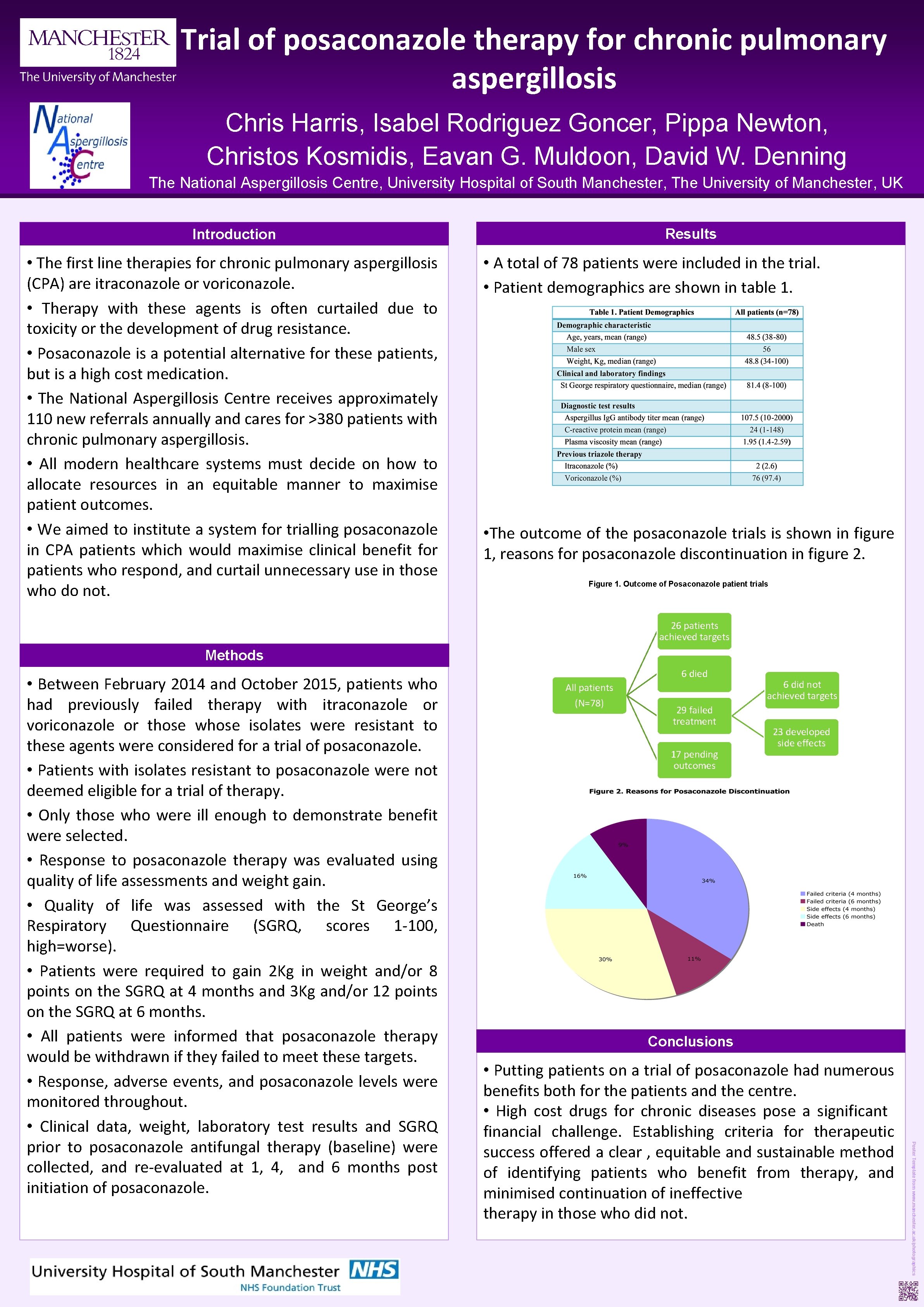
Trial of posaconazole therapy for chronic pulmonary aspergillosis Chris Harris, Isabel Rodriguez Goncer, Pippa Newton, Christos Kosmidis, Eavan G. Muldoon, David W. Denning The National Aspergillosis Centre, University Hospital of South Manchester, The University of Manchester, UK Results Introduction • The first line therapies for chronic pulmonary aspergillosis (CPA) are itraconazole or voriconazole. • Therapy with these agents is often curtailed due to toxicity or the development of drug resistance. • Posaconazole is a potential alternative for these patients, but is a high cost medication. • The National Aspergillosis Centre receives approximately 110 new referrals annually and cares for >380 patients with chronic pulmonary aspergillosis. • All modern healthcare systems must decide on how to allocate resources in an equitable manner to maximise patient outcomes. • We aimed to institute a system for trialling posaconazole in CPA patients which would maximise clinical benefit for patients who respond, and curtail unnecessary use in those who do not. • A total of 78 patients were included in the trial. • Patient demographics are shown in table 1. • The outcome of the posaconazole trials is shown in figure 1, reasons for posaconazole discontinuation in figure 2. Figure 1. Outcome of Posaconazole patient trials 26 patients achieved targets Methods All patients (N=78) 29 failed treatment 17 pending outcomes 6 did not achieved targets 23 developed side effects Conclusions • Putting patients on a trial of posaconazole had numerous benefits both for the patients and the centre. • High cost drugs for chronic diseases pose a significant financial challenge. Establishing criteria for therapeutic success offered a clear , equitable and sustainable method of identifying patients who benefit from therapy, and minimised continuation of ineffective therapy in those who did not. Poster Template from www. manchester. ac. uk/photographics • Between February 2014 and October 2015, patients who had previously failed therapy with itraconazole or voriconazole or those whose isolates were resistant to these agents were considered for a trial of posaconazole. • Patients with isolates resistant to posaconazole were not deemed eligible for a trial of therapy. • Only those who were ill enough to demonstrate benefit were selected. • Response to posaconazole therapy was evaluated using quality of life assessments and weight gain. • Quality of life was assessed with the St George’s Respiratory Questionnaire (SGRQ, scores 1 -100, high=worse). • Patients were required to gain 2 Kg in weight and/or 8 points on the SGRQ at 4 months and 3 Kg and/or 12 points on the SGRQ at 6 months. • All patients were informed that posaconazole therapy would be withdrawn if they failed to meet these targets. • Response, adverse events, and posaconazole levels were monitored throughout. • Clinical data, weight, laboratory test results and SGRQ prior to posaconazole antifungal therapy (baseline) were collected, and re-evaluated at 1, 4, and 6 months post initiation of posaconazole. 6 died