Care of the Neonate with Congenital Heart Disease

- Slides: 43
Care of the Neonate with Congenital Heart Disease Sylvia del Castillo, MD Clinical Associate Professor of Pediatrics USC Keck School of Medicine February 3, 2020
Objectives • To understand the differences in presentation of left vs. right sided obstructive congenital heart lesions • To recognize the signs of cardiogenic or obstructive shock in a newborn • To recognize the presentation and management of different types of congenital heart disease • To present all of this to you in one hour…. . 2
Left vs. Right Sided Lesions • IT’S ALL ABOUT THE DUCT!!! (well, most of the time) • Always remember, the PDA either sends blood to the lungs (right sided lesion) or to the body (left sided lesion) • Oxygen stimulates the duct to CLOSE • PGE 1 is essential for maintaining systemic or pulmonary perfusion until surgical repair/palliation – Side effects of PGE 1: • Apnea with subsequent bradycardia • Hypotension • Fever 3
Left Sided Lesions • • • Coarctation of the Aorta Interruption of the Aortic Arch Critical Aortic Stenosis Shone’s Complex Hypoplastic Left Heart Syndrome 4
Left sided lesions Physical Exam extremely important!!! • – – – – Presence of a murmur Capillary refill Upper and lower extremity blood pressure Pulses Oxygen saturations (pre vs post ductal) Level of consciousness Urine output 5
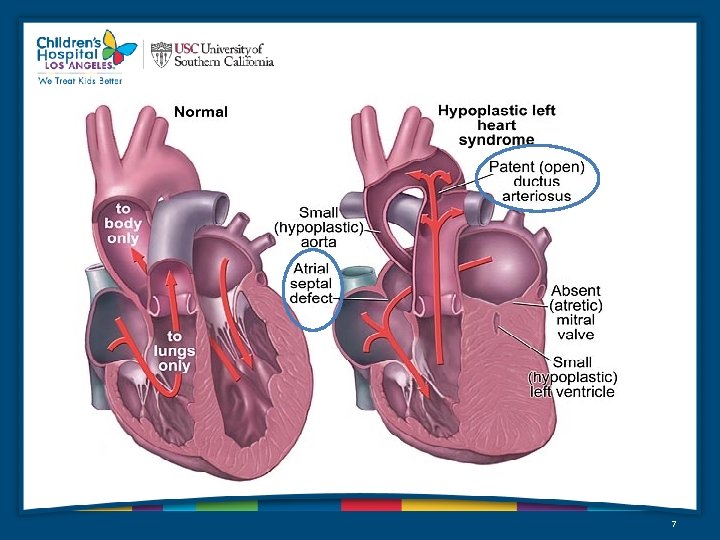
Hypoplastic Left Heart Syndrome • Defined as a spectrum of cardiac malformations – – – – Most central anatomic feature is aortic valve atresia Results in hypoplasia of the ascending aorta and the aortic arch LV is hypoplastic or even absent Systemic blood flow maintained by the RV via the Pulmonary Artery and PDA Fourth most common CHD presenting in infancy (7. 5% of newborns) 25% of cardiac deaths in the first week of life 15% of cardiac deaths in the first month of life Occurs 2 X as often in boys as in girls 6
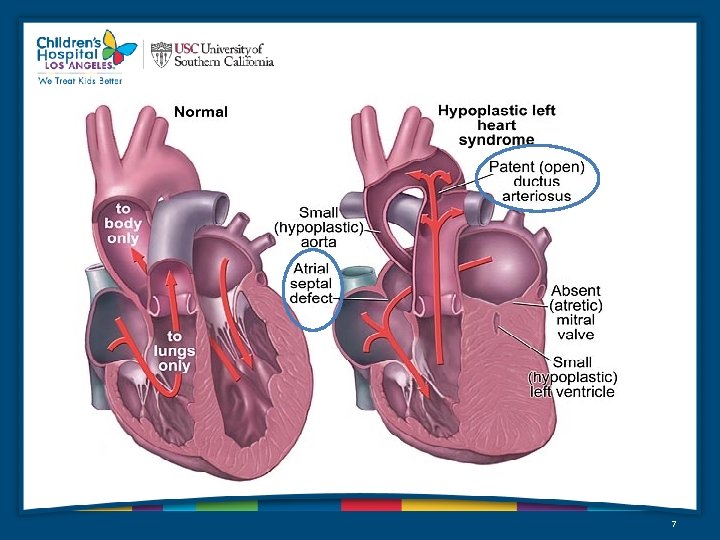
7
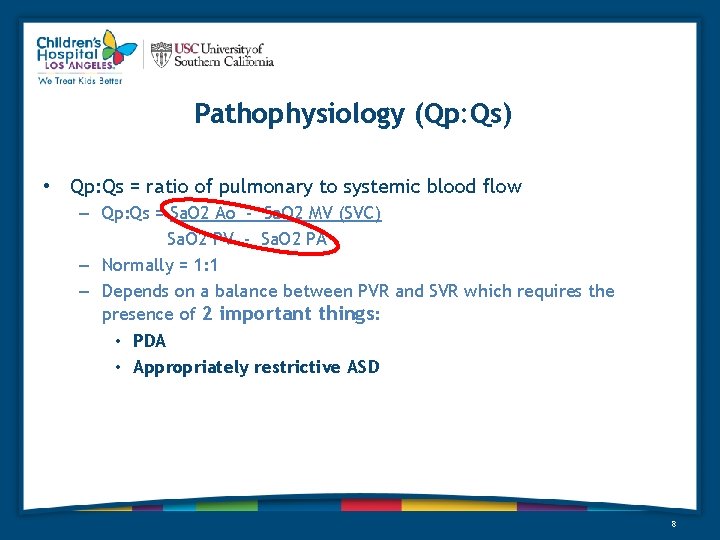
Pathophysiology (Qp: Qs) • Qp: Qs = ratio of pulmonary to systemic blood flow – Qp: Qs = Sa. O 2 Ao - Sa. O 2 MV (SVC) Sa. O 2 PV - Sa. O 2 PA – Normally = 1: 1 – Depends on a balance between PVR and SVR which requires the presence of 2 important things: • PDA • Appropriately restrictive ASD 8
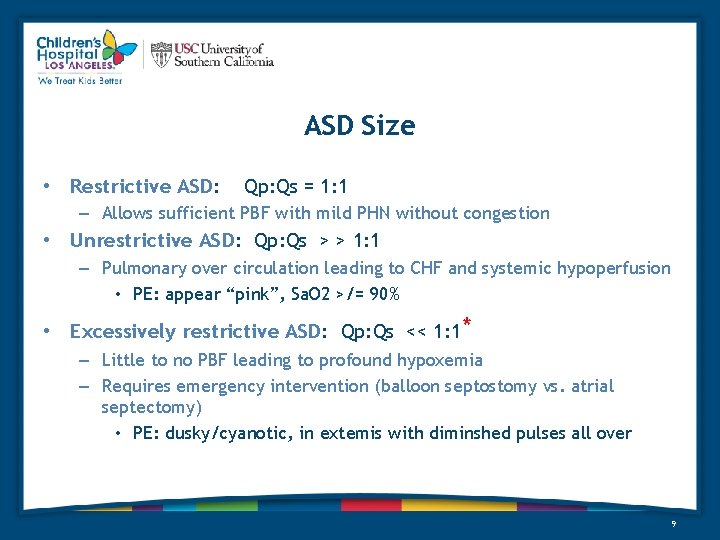
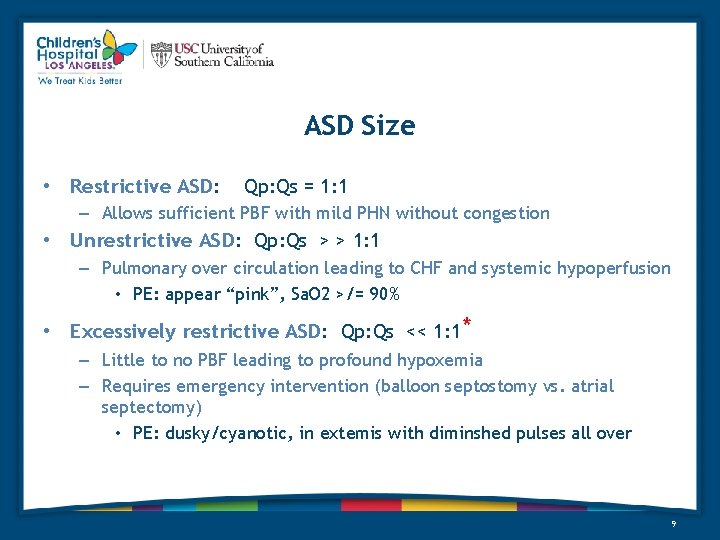
ASD Size • Restrictive ASD: Qp: Qs = 1: 1 – Allows sufficient PBF with mild PHN without congestion • Unrestrictive ASD: Qp: Qs > > 1: 1 – Pulmonary over circulation leading to CHF and systemic hypoperfusion • PE: appear “pink”, Sa. O 2 >/= 90% • Excessively restrictive ASD: Qp: Qs << 1: 1* – Little to no PBF leading to profound hypoxemia – Requires emergency intervention (balloon septostomy vs. atrial septectomy) • PE: dusky/cyanotic, in extemis with diminshed pulses all over 9
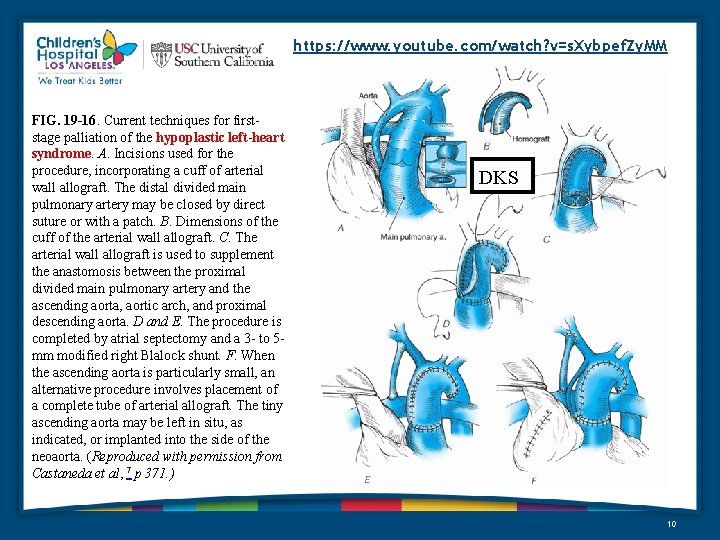
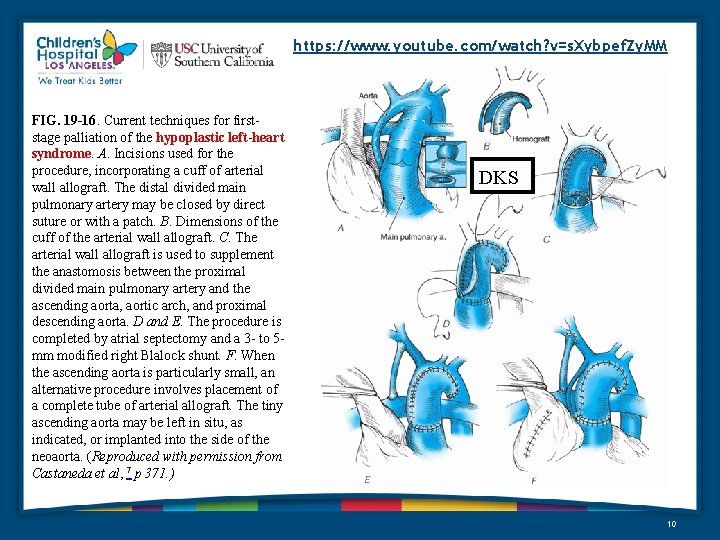
https: //www. youtube. com/watch? v=s. Xybpef. Zy. MM FIG. 19 -16. Current techniques for firststage palliation of the hypoplastic left-heart syndrome. A. Incisions used for the procedure, incorporating a cuff of arterial wall allograft. The distal divided main pulmonary artery may be closed by direct suture or with a patch. B. Dimensions of the cuff of the arterial wall allograft. C. The arterial wall allograft is used to supplement the anastomosis between the proximal divided main pulmonary artery and the ascending aorta, aortic arch, and proximal descending aorta. D and E. The procedure is completed by atrial septectomy and a 3 - to 5 mm modified right Blalock shunt. F. When the ascending aorta is particularly small, an alternative procedure involves placement of a complete tube of arterial allograft. The tiny ascending aorta may be left in situ, as indicated, or implanted into the side of the neoaorta. (Reproduced with permission from Castaneda et al, 7 p 371. ) DKS 10
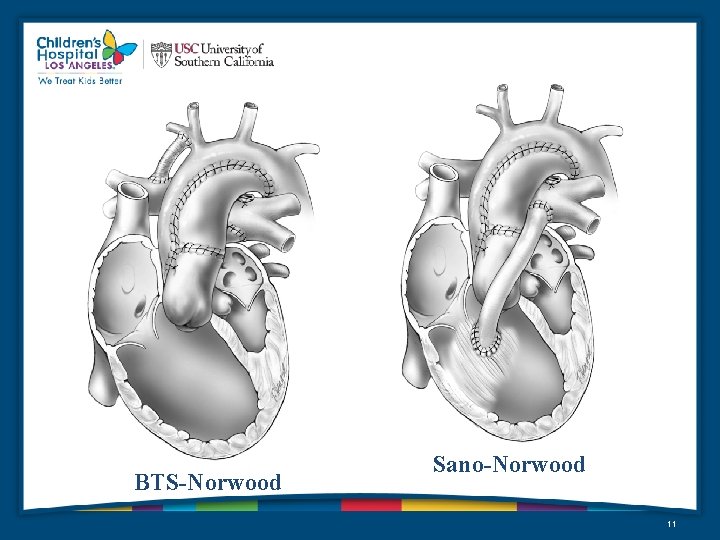
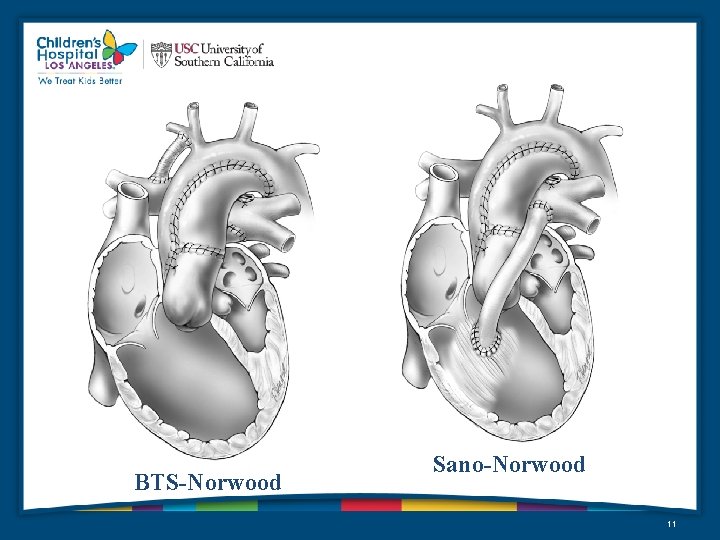
BTS-Norwood Sano-Norwood 11
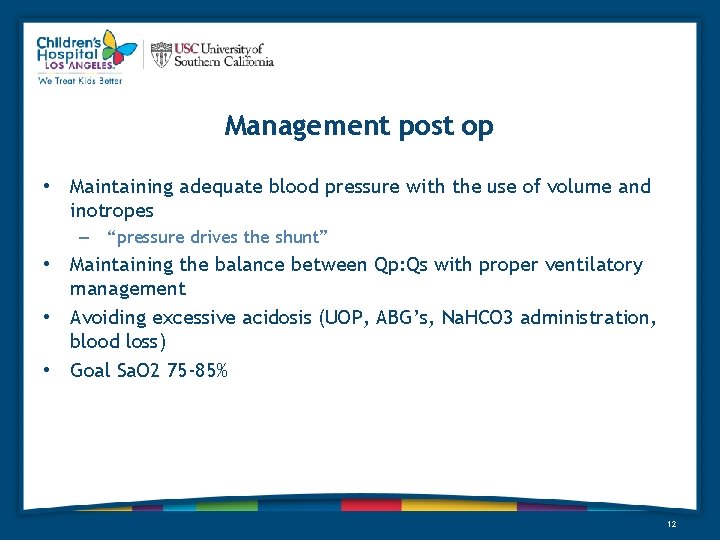
Management post op • Maintaining adequate blood pressure with the use of volume and inotropes – “pressure drives the shunt” • Maintaining the balance between Qp: Qs with proper ventilatory management • Avoiding excessive acidosis (UOP, ABG’s, Na. HCO 3 administration, blood loss) • Goal Sa. O 2 75 -85% 12
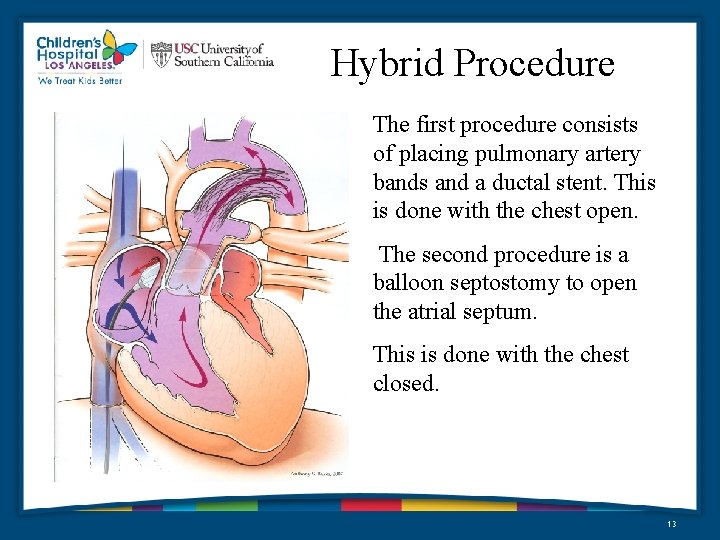
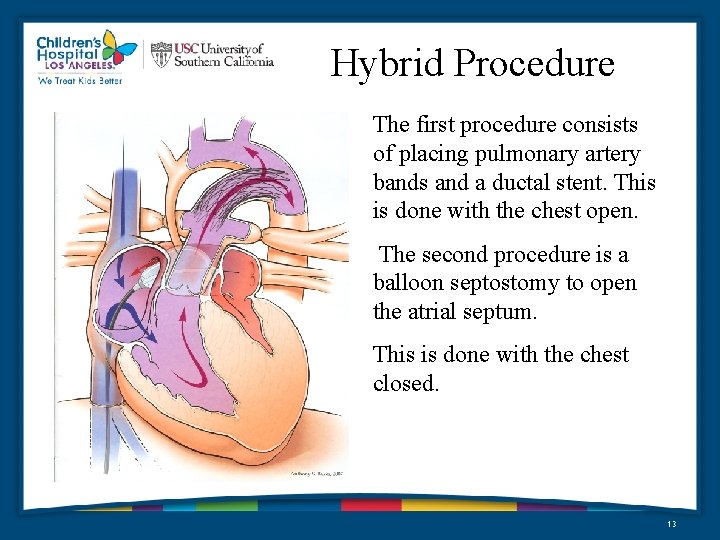
Hybrid Procedure The first procedure consists of placing pulmonary artery bands and a ductal stent. This is done with the chest open. The second procedure is a balloon septostomy to open the atrial septum. This is done with the chest closed. 13
Right Sided/Other Lesions • • • Total Anomalous Pulmonary Venous Return D-Transposition of the Great Arteries Ebstein’s anomaly Tricuspid Atresia Pulmonary Atresia 14
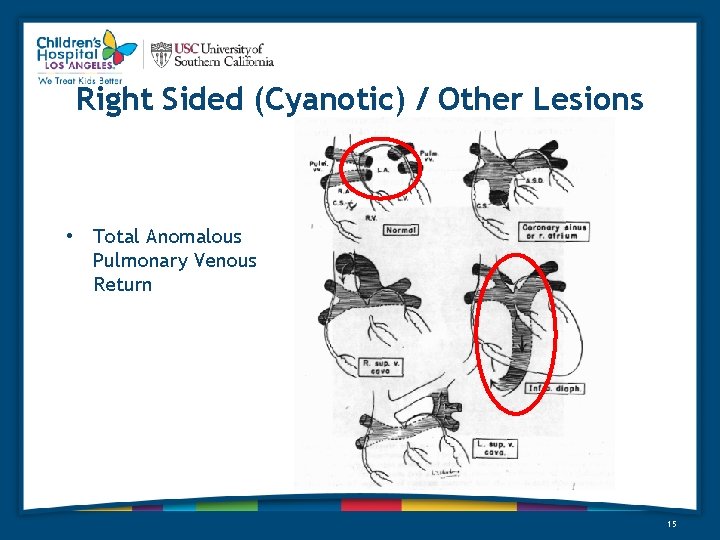
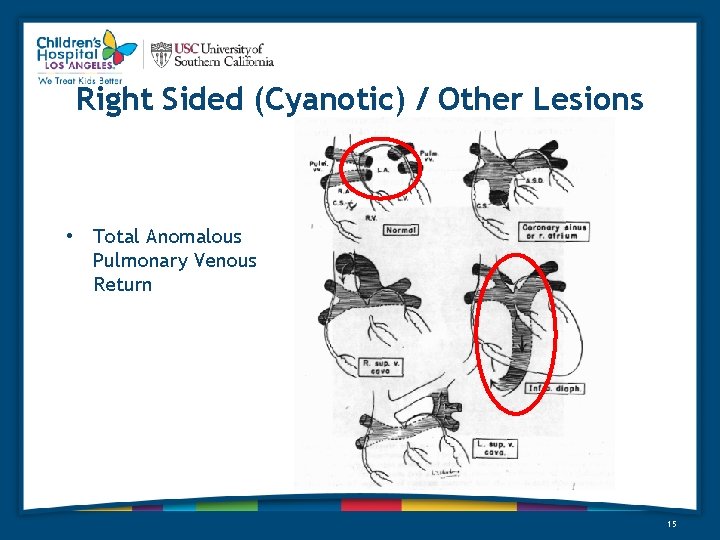
Right Sided (Cyanotic) / Other Lesions • Total Anomalous Pulmonary Venous Return 15
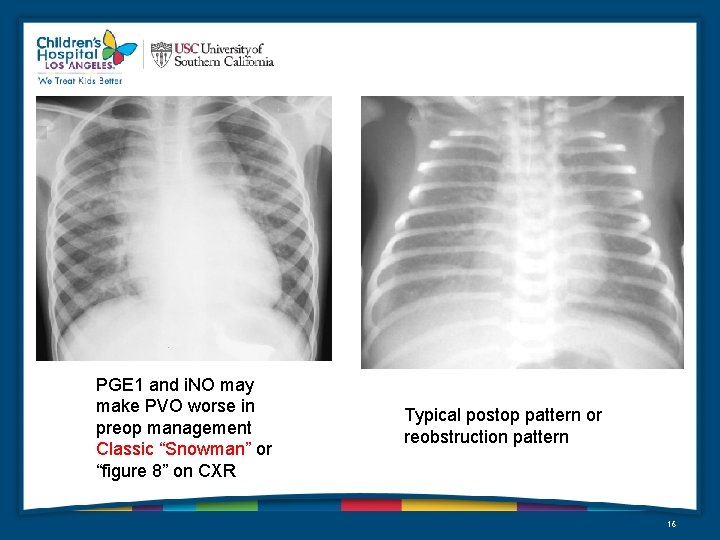
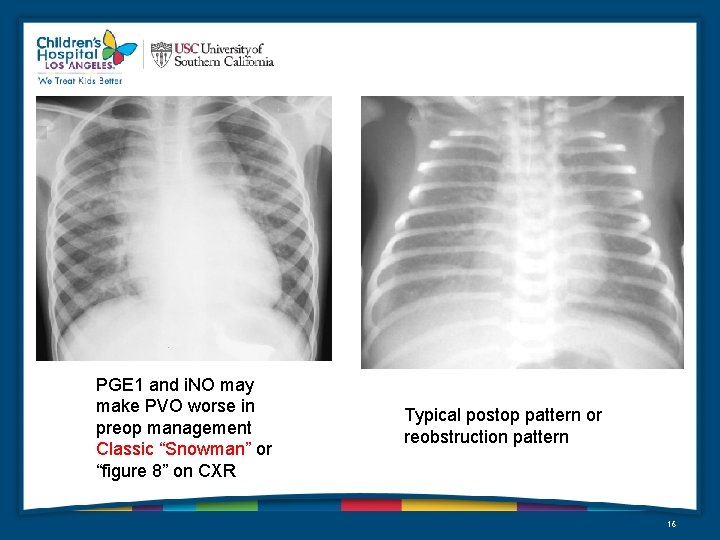
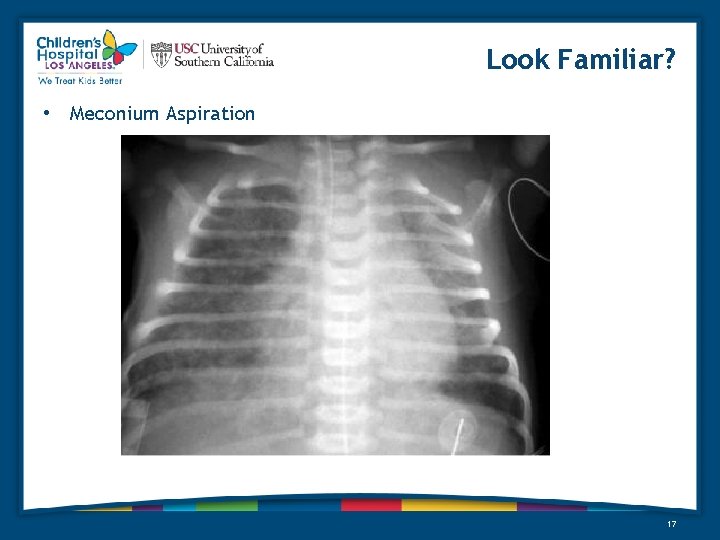
PGE 1 and i. NO may make PVO worse in preop management Classic “Snowman” or “figure 8” on CXR Typical postop pattern or reobstruction pattern 16
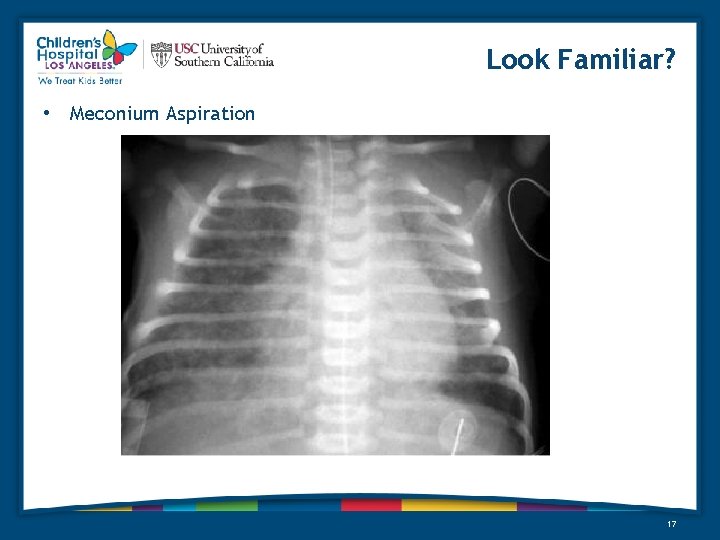
Look Familiar? • Meconium Aspiration 17
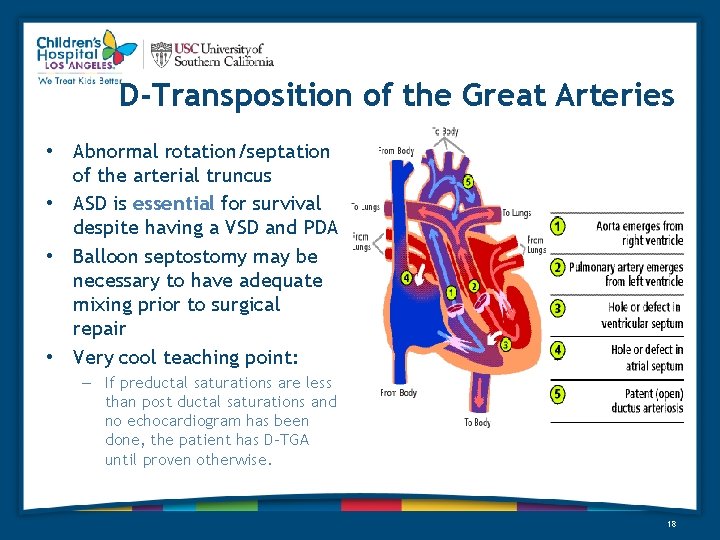
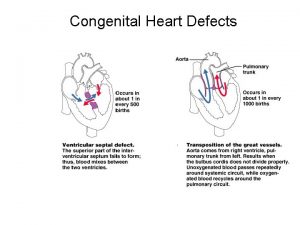
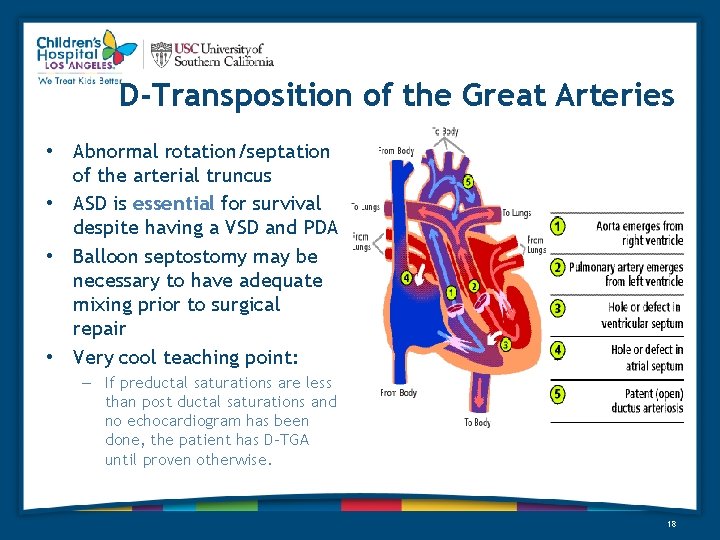
D-Transposition of the Great Arteries • Abnormal rotation/septation of the arterial truncus • ASD is essential for survival despite having a VSD and PDA • Balloon septostomy may be necessary to have adequate mixing prior to surgical repair • Very cool teaching point: – If preductal saturations are less than post ductal saturations and no echocardiogram has been done, the patient has D-TGA until proven otherwise. 18
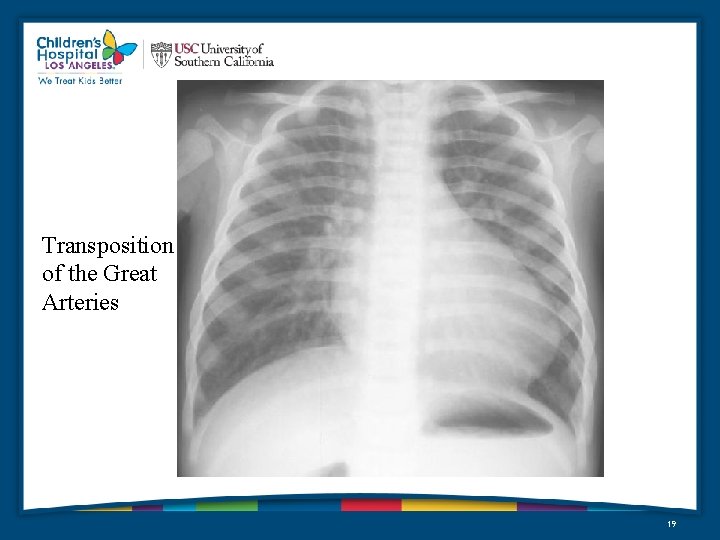
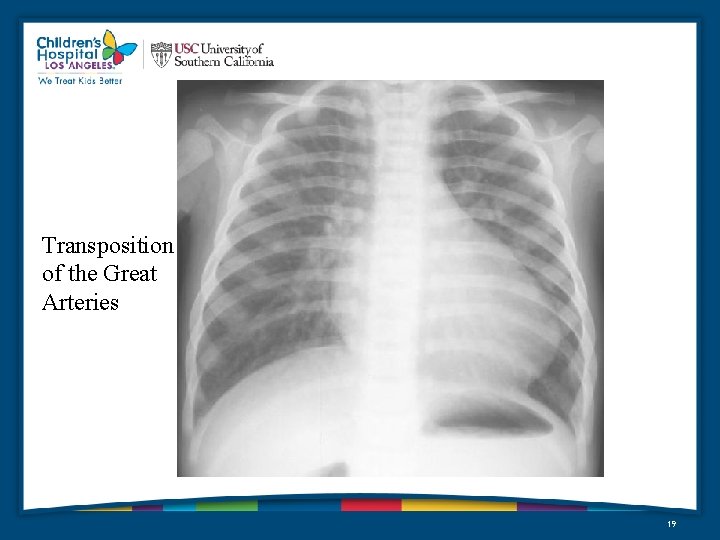
Transposition of the Great Arteries 19
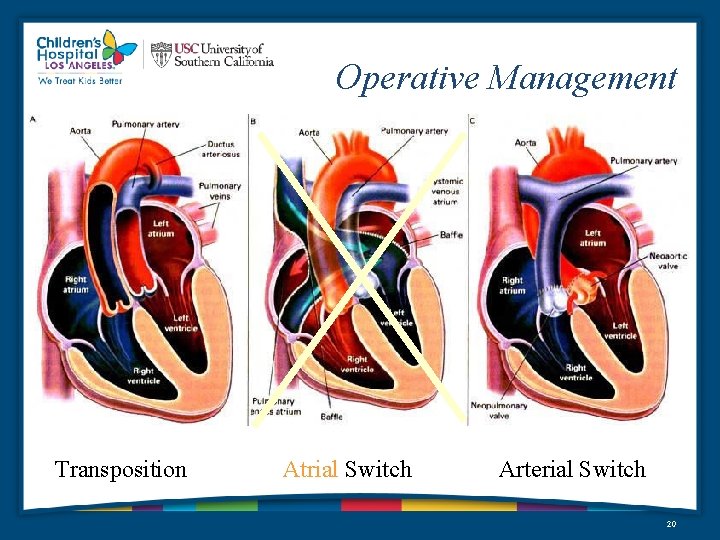
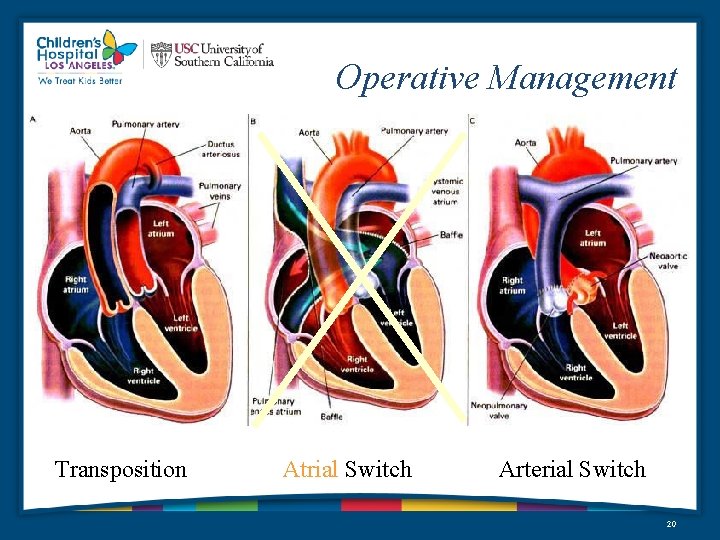
Operative Management Transposition Atrial Switch Arterial Switch 20
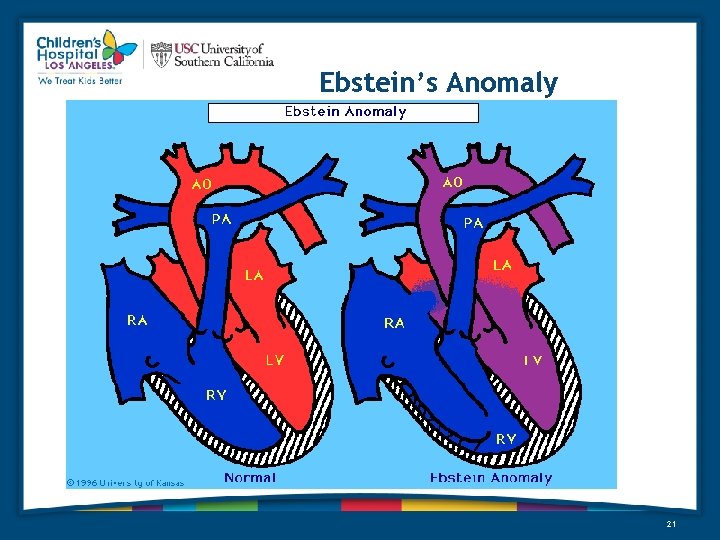
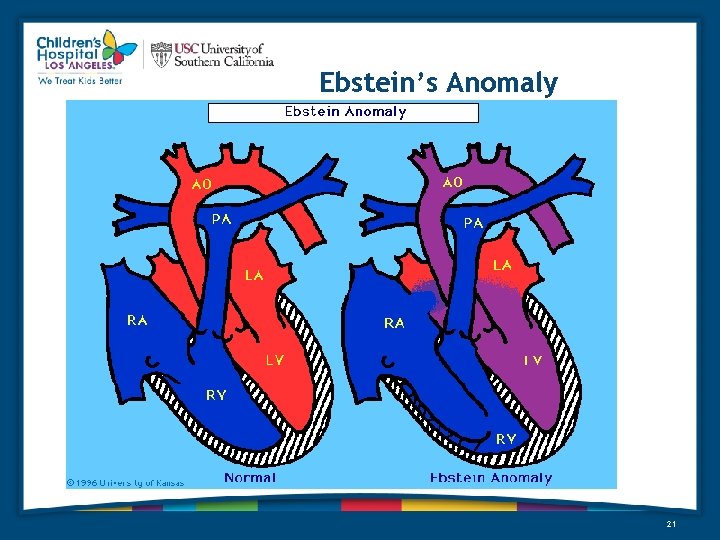
Ebstein’s Anomaly 21
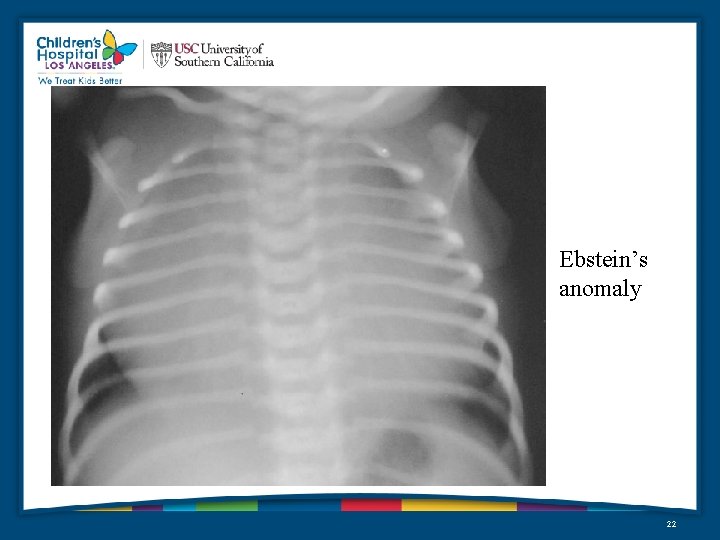
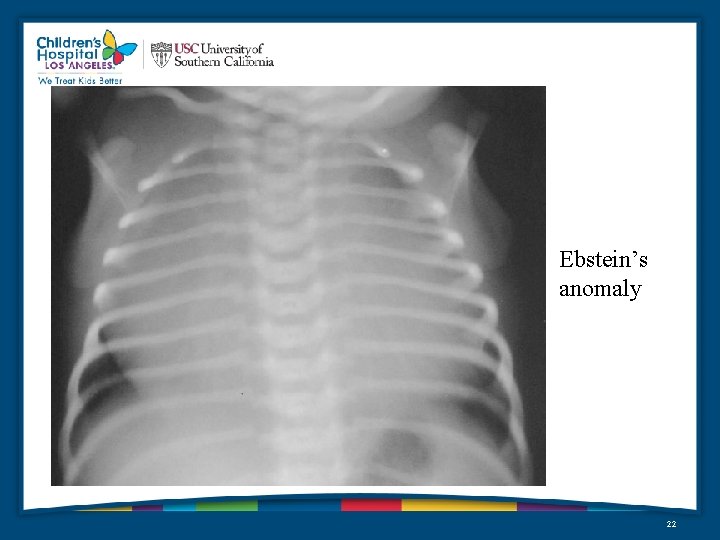
Ebstein’s anomaly 22
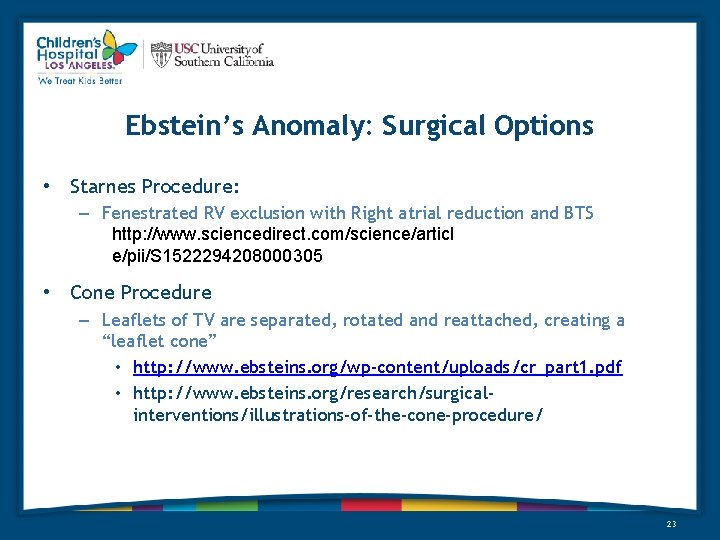
Ebstein’s Anomaly: Surgical Options • Starnes Procedure: – Fenestrated RV exclusion with Right atrial reduction and BTS http: //www. sciencedirect. com/science/articl e/pii/S 1522294208000305 • Cone Procedure – Leaflets of TV are separated, rotated and reattached, creating a “leaflet cone” • http: //www. ebsteins. org/wp-content/uploads/cr_part 1. pdf • http: //www. ebsteins. org/research/surgicalinterventions/illustrations-of-the-cone-procedure/ 23
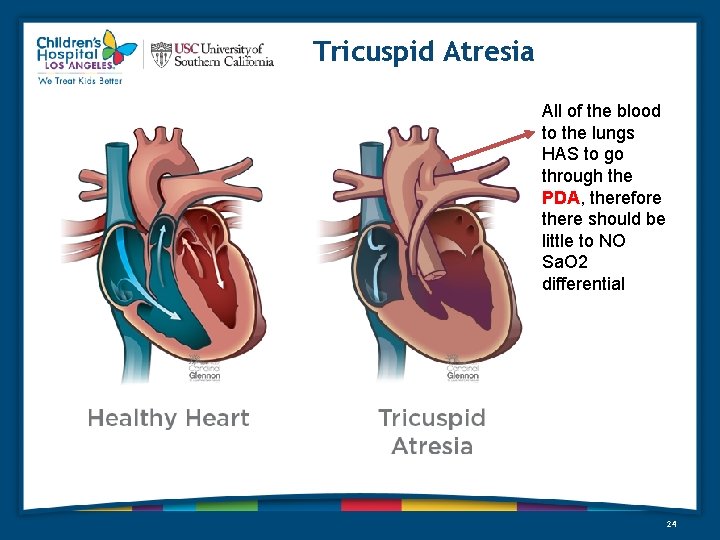
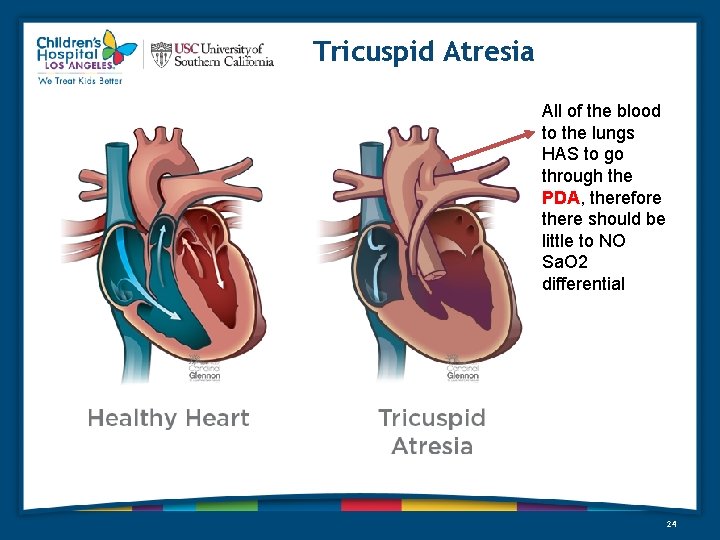
Tricuspid Atresia All of the blood to the lungs HAS to go through the PDA, therefore there should be little to NO Sa. O 2 differential 24
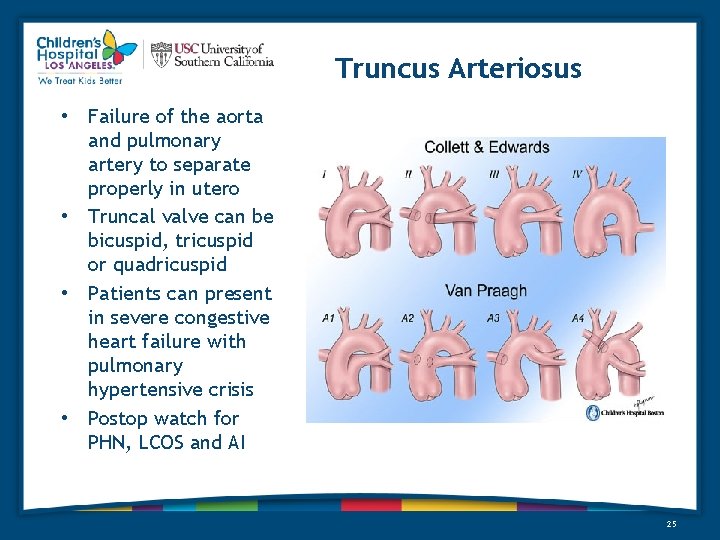
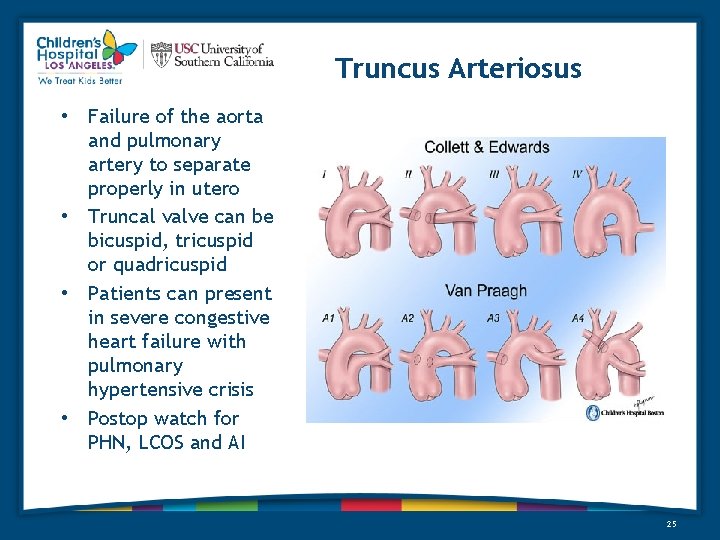
Truncus Arteriosus • Failure of the aorta and pulmonary artery to separate properly in utero • Truncal valve can be bicuspid, tricuspid or quadricuspid • Patients can present in severe congestive heart failure with pulmonary hypertensive crisis • Postop watch for PHN, LCOS and AI 25
What Should Scare You • • Pulmonary Hypertension Thrombosed Shunt Restrictive Atrial Septum Arrhythmias 26
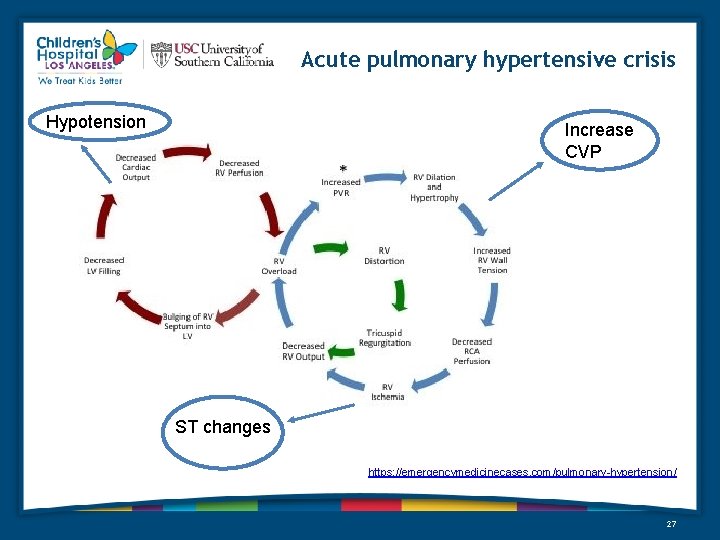
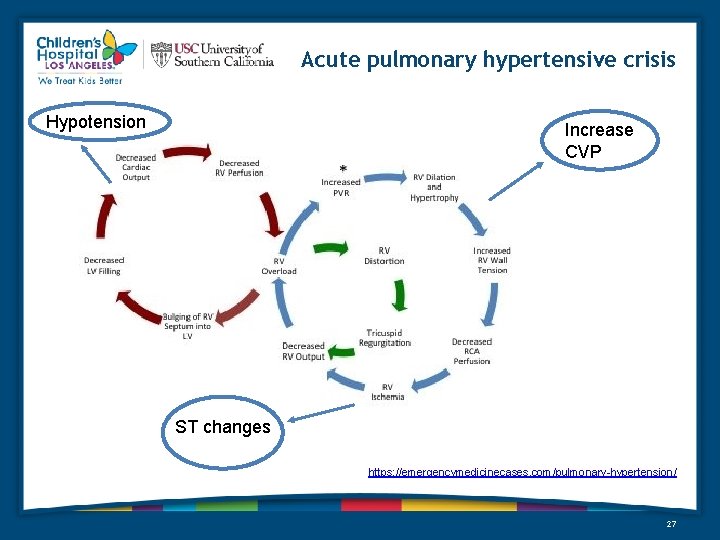
Acute pulmonary hypertensive crisis Hypotension Increase CVP ST changes https: //emergencymedicinecases. com/pulmonary-hypertension/ 27
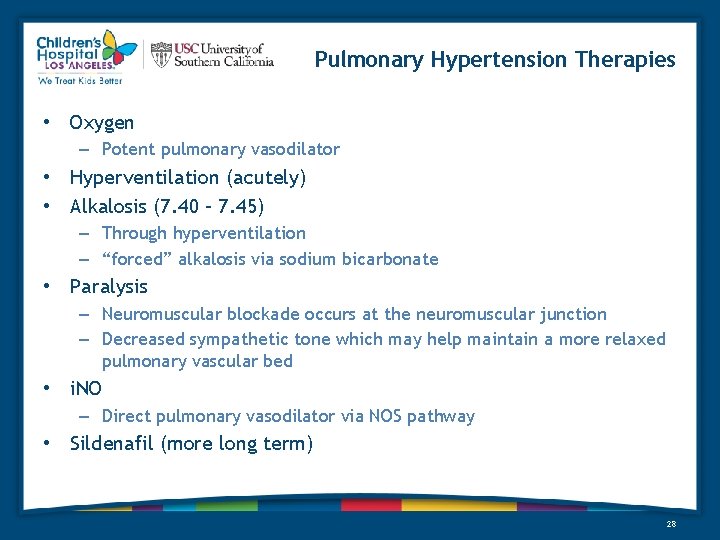
Pulmonary Hypertension Therapies • Oxygen – Potent pulmonary vasodilator • Hyperventilation (acutely) • Alkalosis (7. 40 – 7. 45) – Through hyperventilation – “forced” alkalosis via sodium bicarbonate • Paralysis – Neuromuscular blockade occurs at the neuromuscular junction – Decreased sympathetic tone which may help maintain a more relaxed pulmonary vascular bed • i. NO – Direct pulmonary vasodilator via NOS pathway • Sildenafil (more long term) 28
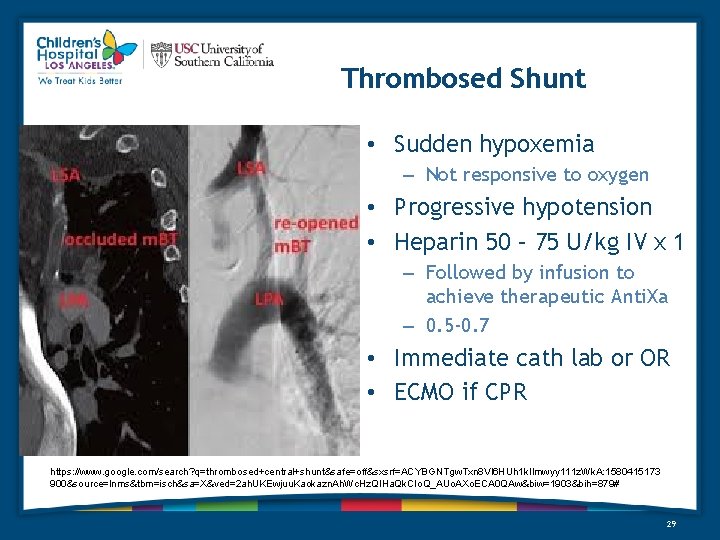
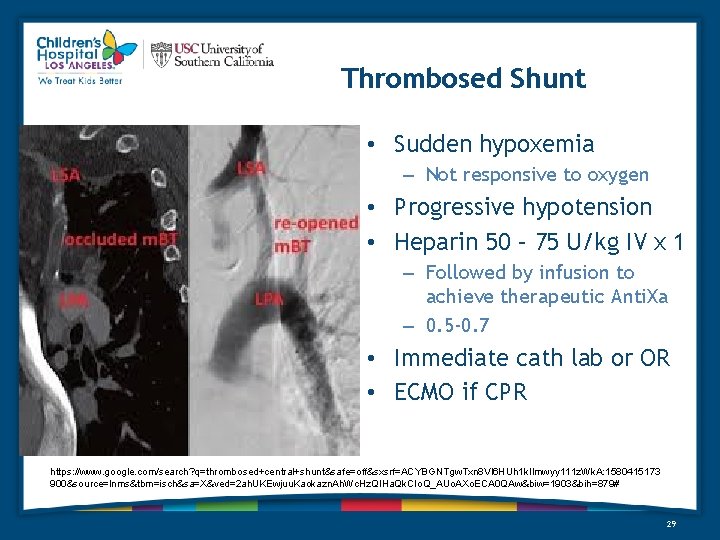
Thrombosed Shunt • Sudden hypoxemia – Not responsive to oxygen • Progressive hypotension • Heparin 50 – 75 U/kg IV x 1 – Followed by infusion to achieve therapeutic Anti. Xa – 0. 5 -0. 7 • Immediate cath lab or OR • ECMO if CPR https: //www. google. com/search? q=thrombosed+central+shunt&safe=off&sxsrf=ACYBGNTgw. Txn 8 Vl 6 HUh 1 k. Ilmwyy 111 z. Wk. A: 1580415173 900&source=lnms&tbm=isch&sa=X&ved=2 ah. UKEwjuu. Kaokazn. Ah. Wc. Hz. QIHa. Qk. CIo. Q_AUo. AXo. ECA 0 QAw&biw=1903&bih=879# 29
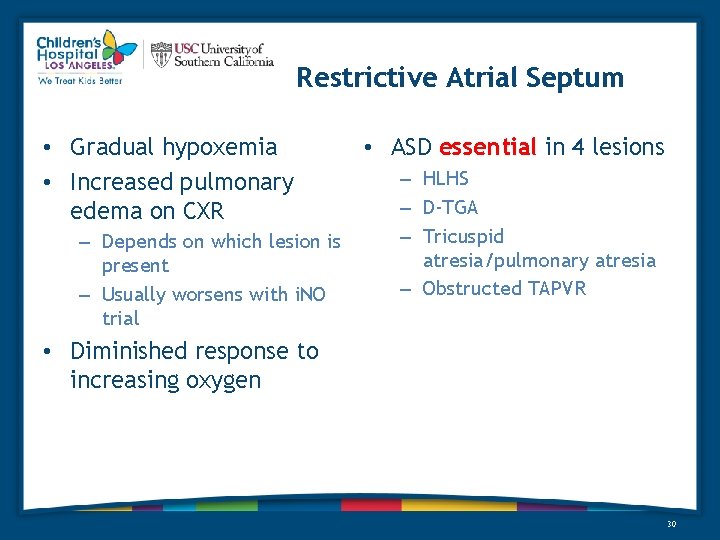
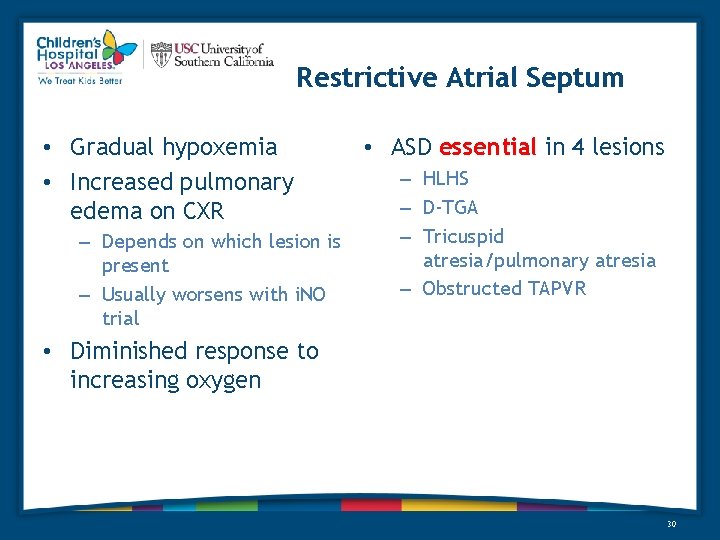
Restrictive Atrial Septum • Gradual hypoxemia • Increased pulmonary edema on CXR – Depends on which lesion is present – Usually worsens with i. NO trial • ASD essential in 4 lesions – HLHS – D-TGA – Tricuspid atresia/pulmonary atresia – Obstructed TAPVR • Diminished response to increasing oxygen 30
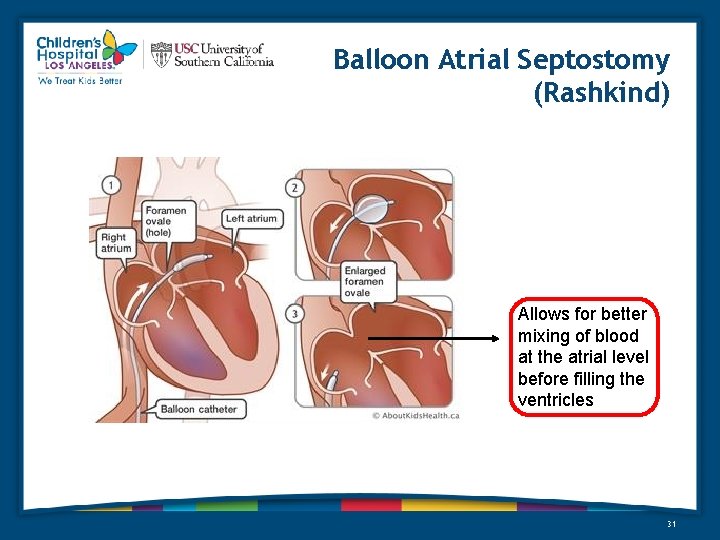
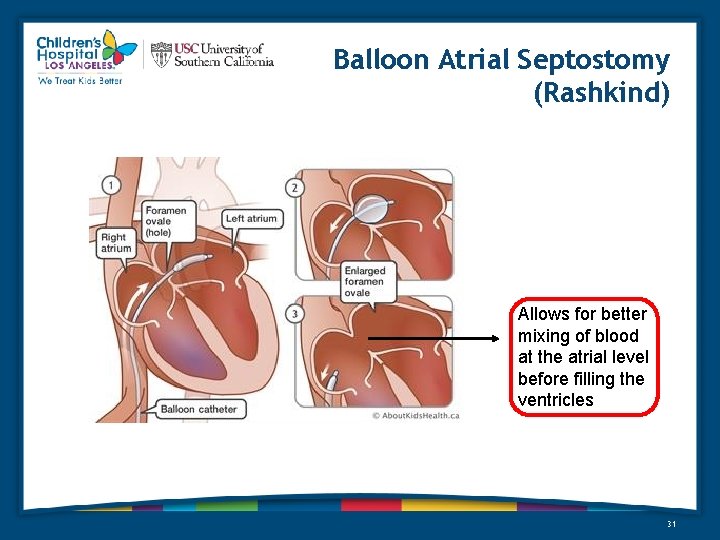
Balloon Atrial Septostomy (Rashkind) Allows for better mixing of blood at the atrial level before filling the ventricles 31
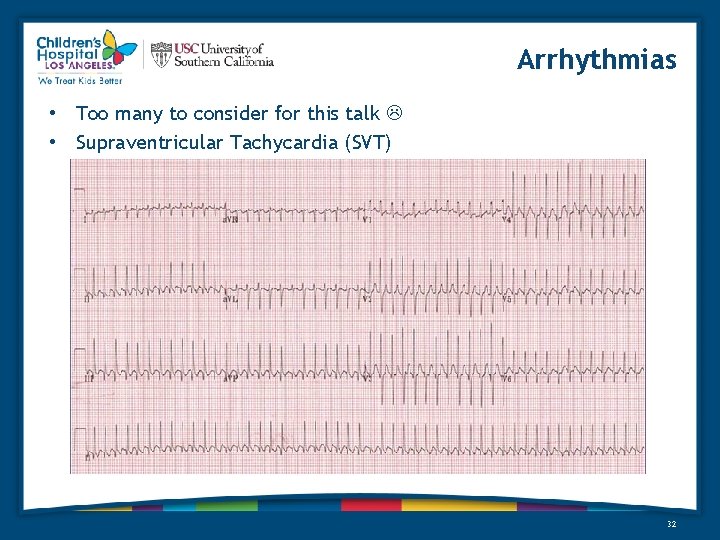
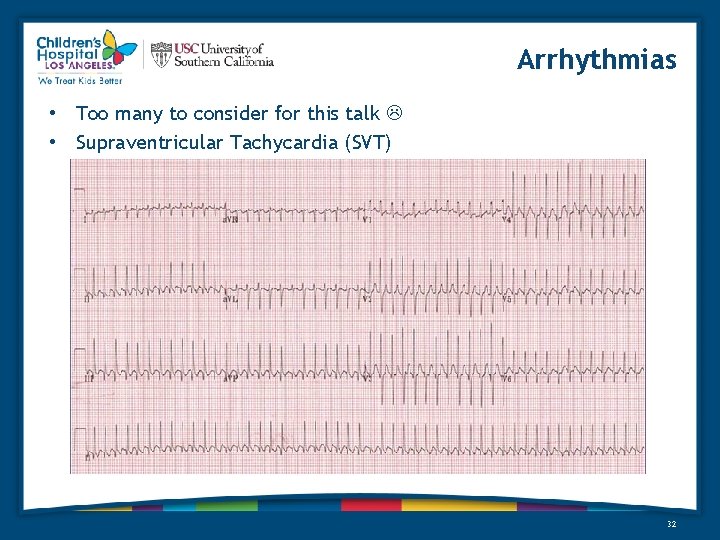
Arrhythmias • Too many to consider for this talk • Supraventricular Tachycardia (SVT) 32
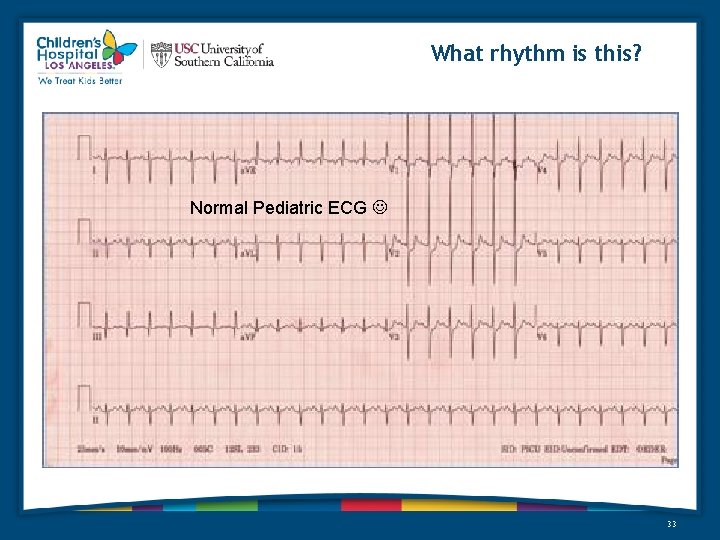
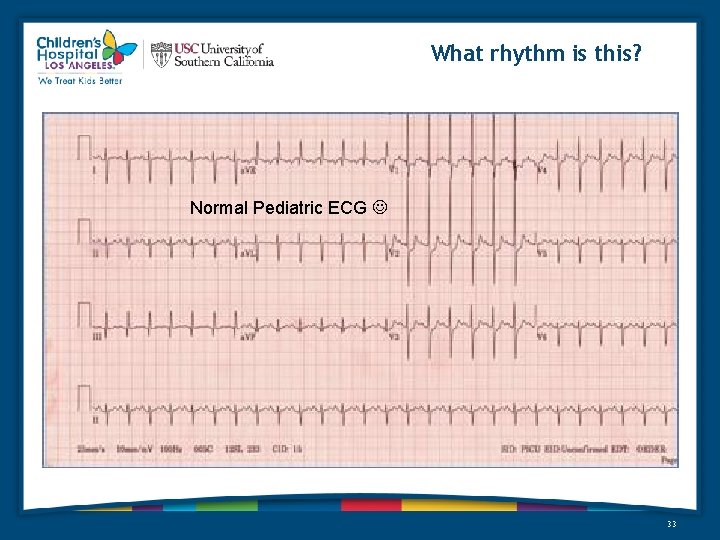
What rhythm is this? Normal Pediatric ECG 33
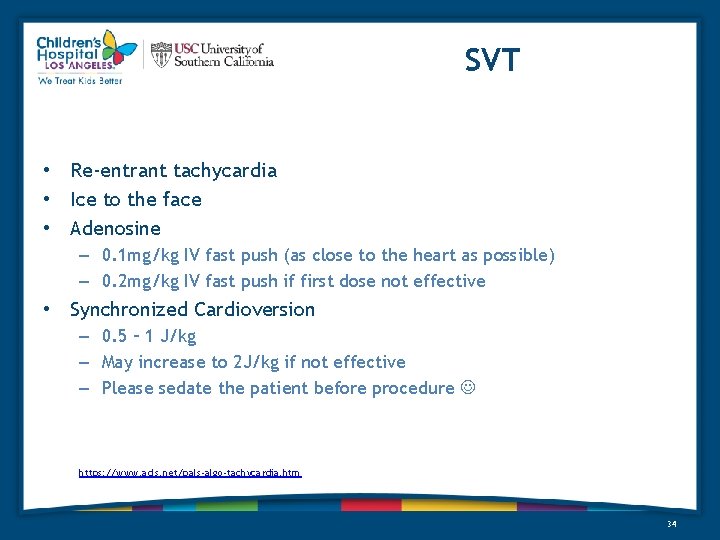
SVT • Re-entrant tachycardia • Ice to the face • Adenosine – 0. 1 mg/kg IV fast push (as close to the heart as possible) – 0. 2 mg/kg IV fast push if first dose not effective • Synchronized Cardioversion – 0. 5 – 1 J/kg – May increase to 2 J/kg if not effective – Please sedate the patient before procedure https: //www. acls. net/pals-algo-tachycardia. htm 34

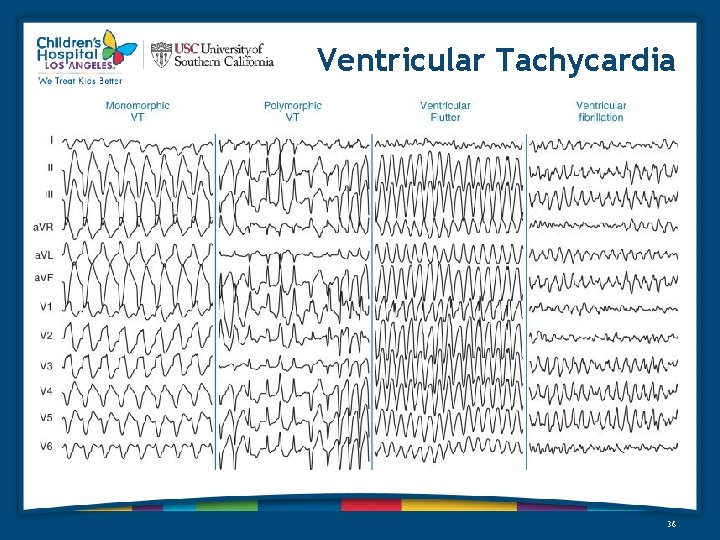
Ventricular Tachycardia 35
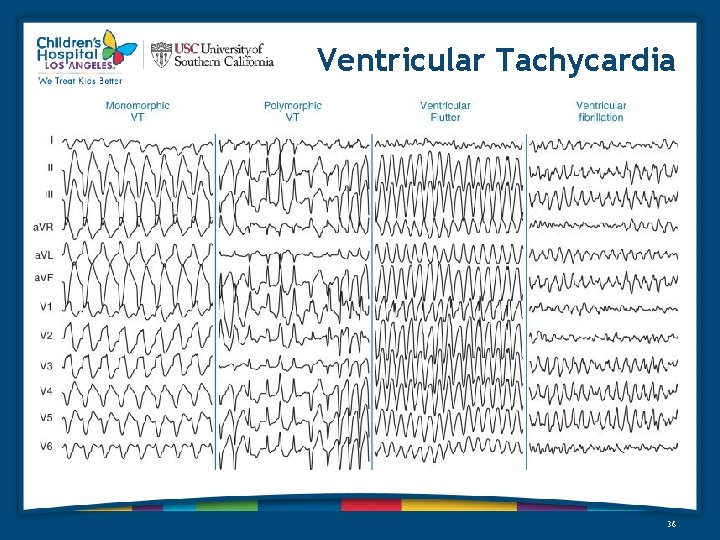
Ventricular Tachycardia 36
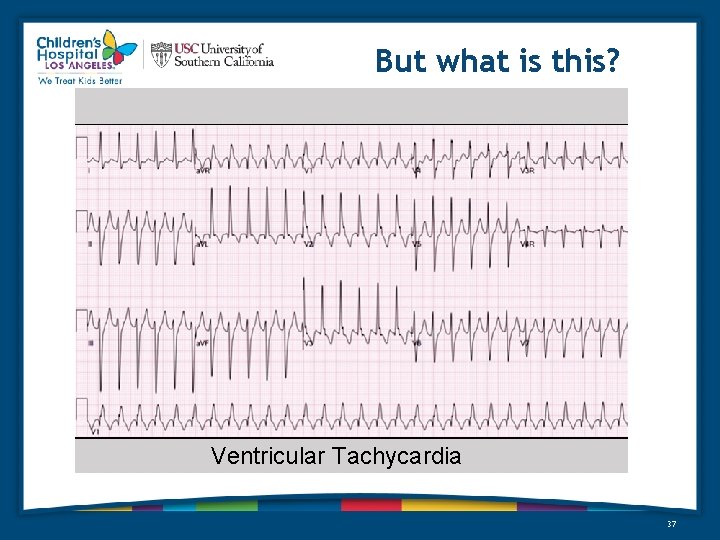
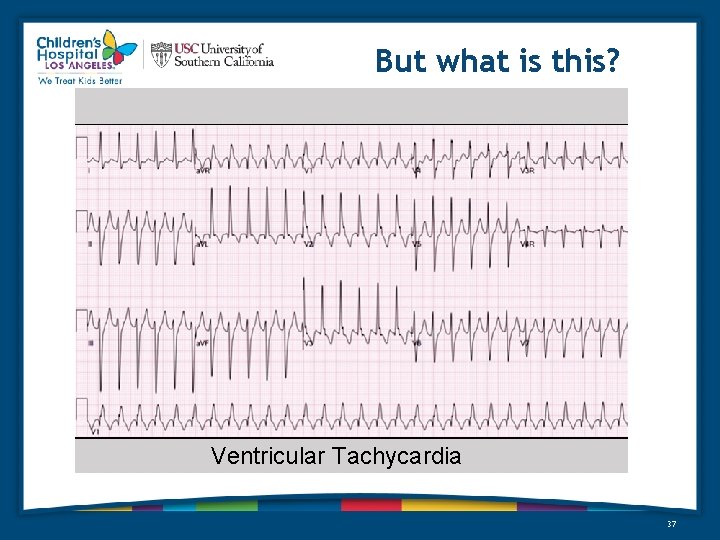
But what is this? Ventricular Tachycardia 37
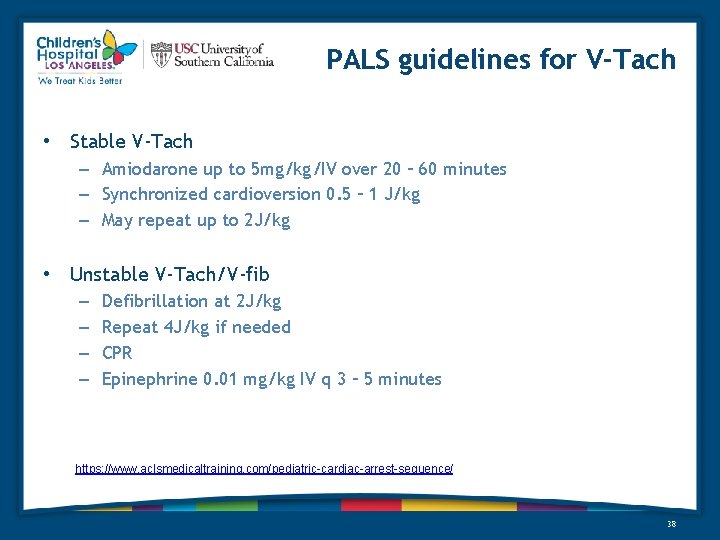
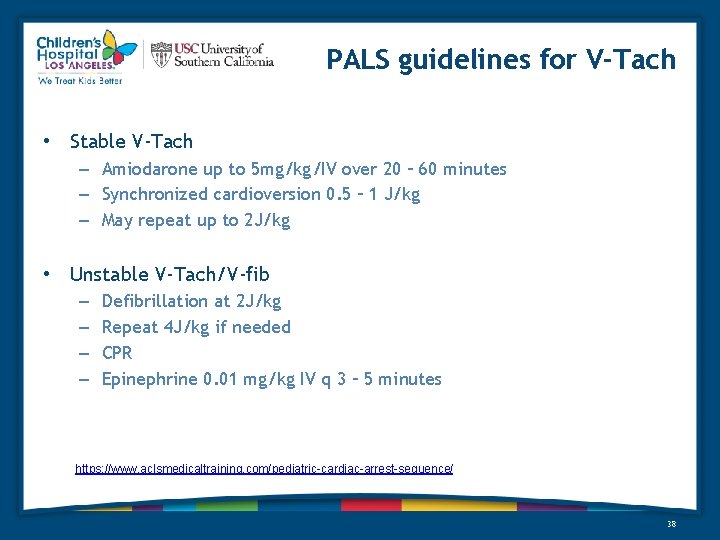
PALS guidelines for V-Tach • Stable V-Tach – Amiodarone up to 5 mg/kg/IV over 20 – 60 minutes – Synchronized cardioversion 0. 5 – 1 J/kg – May repeat up to 2 J/kg • Unstable V-Tach/V-fib – – Defibrillation at 2 J/kg Repeat 4 J/kg if needed CPR Epinephrine 0. 01 mg/kg IV q 3 – 5 minutes https: //www. aclsmedicaltraining. com/pediatric-cardiac-arrest-sequence/ 38
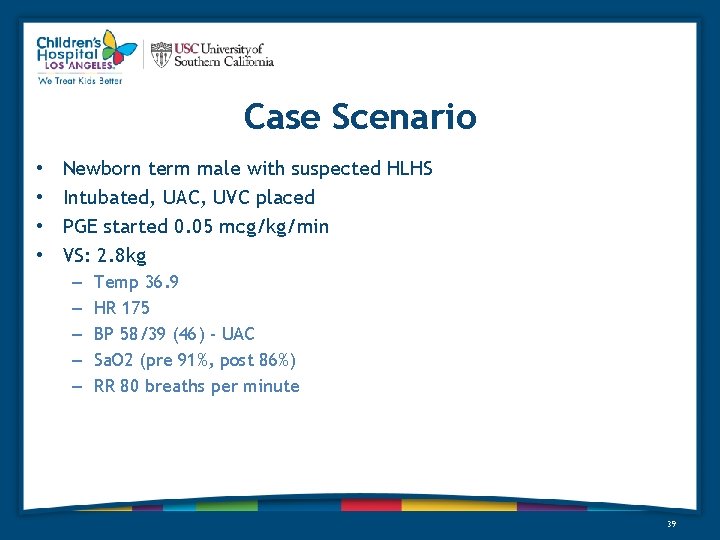
Case Scenario • • Newborn term male with suspected HLHS Intubated, UAC, UVC placed PGE started 0. 05 mcg/kg/min VS: 2. 8 kg – – – Temp 36. 9 HR 175 BP 58/39 (46) - UAC Sa. O 2 (pre 91%, post 86%) RR 80 breaths per minute 39
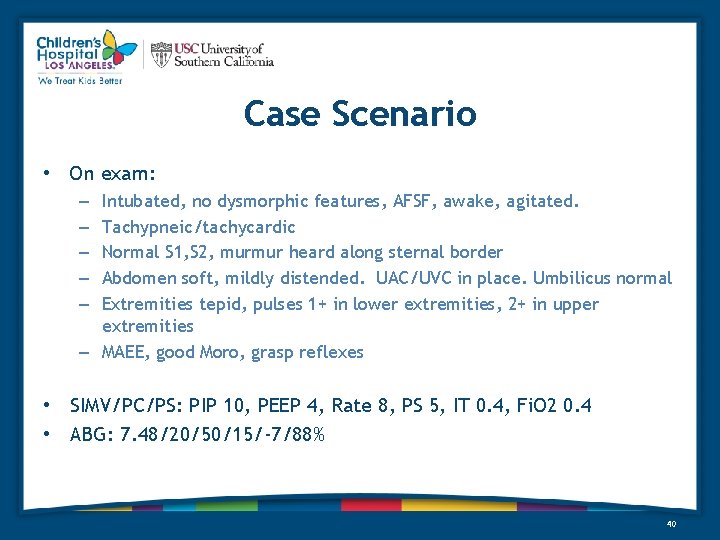
Case Scenario • On exam: Intubated, no dysmorphic features, AFSF, awake, agitated. Tachypneic/tachycardic Normal S 1, S 2, murmur heard along sternal border Abdomen soft, mildly distended. UAC/UVC in place. Umbilicus normal Extremities tepid, pulses 1+ in lower extremities, 2+ in upper extremities – MAEE, good Moro, grasp reflexes – – – • SIMV/PC/PS: PIP 10, PEEP 4, Rate 8, PS 5, IT 0. 4, Fi. O 2 0. 4 • ABG: 7. 48/20/50/15/-7/88% 40
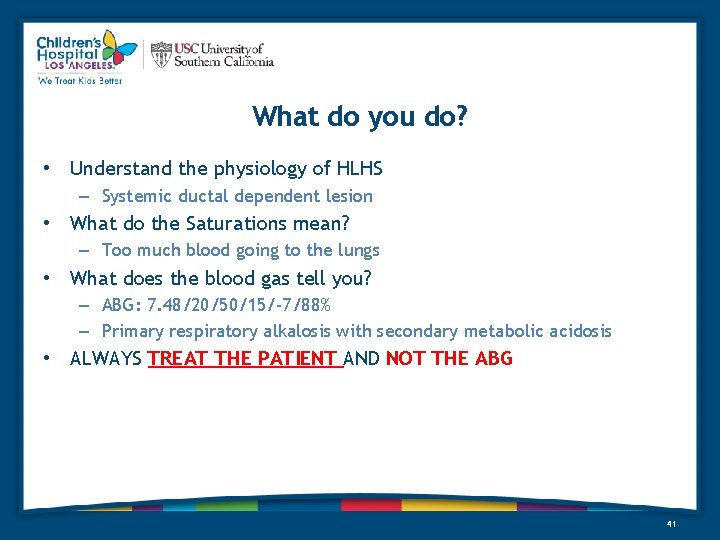
What do you do? • Understand the physiology of HLHS – Systemic ductal dependent lesion • What do the Saturations mean? – Too much blood going to the lungs • What does the blood gas tell you? – ABG: 7. 48/20/50/15/-7/88% – Primary respiratory alkalosis with secondary metabolic acidosis • ALWAYS TREAT THE PATIENT AND NOT THE ABG 41
Summary • Understand the physiology of pulmonary (right sided) vs systemic (left sided) ductal dependent lesions • Trust your physical exam (always feel for pulses in all extremities) • Acute hypoxemia in a shunted patient = shunt thrombosis until proven otherwise • Pay attention to pre and post ductal saturation differentials – (do NOT need pre and post ductal saturations in right sided ductal dependent lesions) • Oxygen can either really help, or really hurt a patient, depending on their anatomy and physiology 42
THANK YOU 43
 Difference between cyanotic and acyanotic heart disease
Difference between cyanotic and acyanotic heart disease Cyanotic vs acyanotic
Cyanotic vs acyanotic Tet spell
Tet spell Farah garmany
Farah garmany Grimace reflex
Grimace reflex Definition of high risk neonates
Definition of high risk neonates Petechiae neonate
Petechiae neonate Neonate skull
Neonate skull Canadian congenital heart alliance
Canadian congenital heart alliance Congenital heart
Congenital heart Congenital heart defect
Congenital heart defect Primary secondary tertiary care nursing
Primary secondary tertiary care nursing Communicable disease and non communicable disease
Communicable disease and non communicable disease Heart disease symptoms
Heart disease symptoms Pico question examples heart disease
Pico question examples heart disease Ronaldo heart
Ronaldo heart Feline
Feline Heart disease data
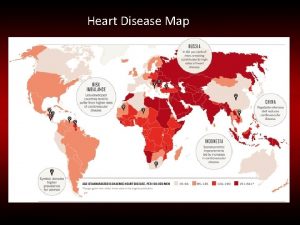
Heart disease data Rheumatic heart disease
Rheumatic heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Mitral stenosis severity
Mitral stenosis severity Terrible t's cyanotic heart disease
Terrible t's cyanotic heart disease Upper lobe venous diversion
Upper lobe venous diversion Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Dopamine uses
Dopamine uses Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Right sided heart failure
Right sided heart failure Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Causes of valvular heart disease
Causes of valvular heart disease Preload and afterload
Preload and afterload Site:slidetodoc.com
Site:slidetodoc.com Heart disease
Heart disease Heart disease
Heart disease Coronary heart disease
Coronary heart disease Antianginal drugs classification
Antianginal drugs classification Strepsore
Strepsore Rheumatic heart disease causes
Rheumatic heart disease causes Ischemic heart disease
Ischemic heart disease Pac ekg
Pac ekg Nyha classifications
Nyha classifications Cvds
Cvds Vijaya's echo criteria
Vijaya's echo criteria кагами-огата
кагами-огата Congenital pneumonia
Congenital pneumonia