2 INCIDENCE 2 nd most common malignancy in




- Slides: 46

2
INCIDENCE • 2 nd most common malignancy in children after leukemia. • 20% of all childhood malignancy 3
Etiology &Predisposing factors 1 -Unkown 2 - Environmental factors( diet, smoking, alcohol Radiation). 3 - Immunosuppression ( transplant. , AIDS) 4 - Mutation or deletion of specific genes 5 - Irradiation 4
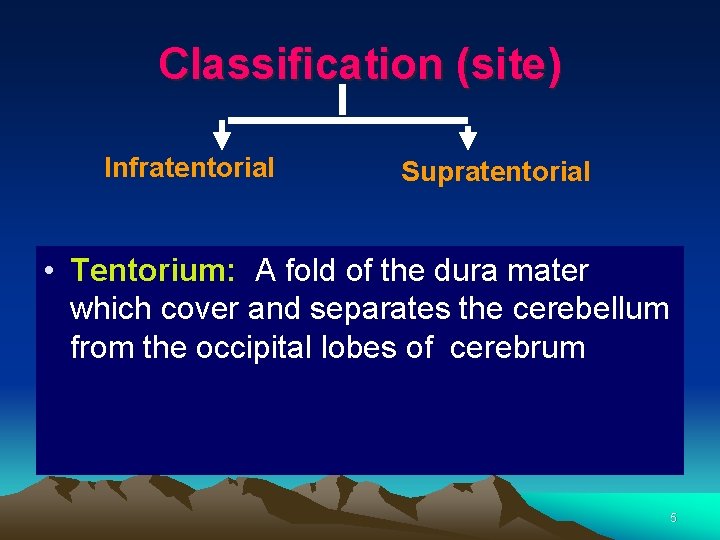
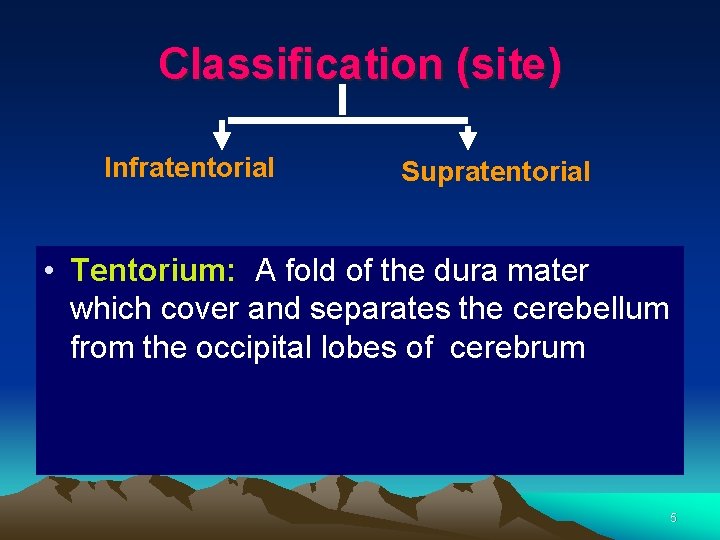
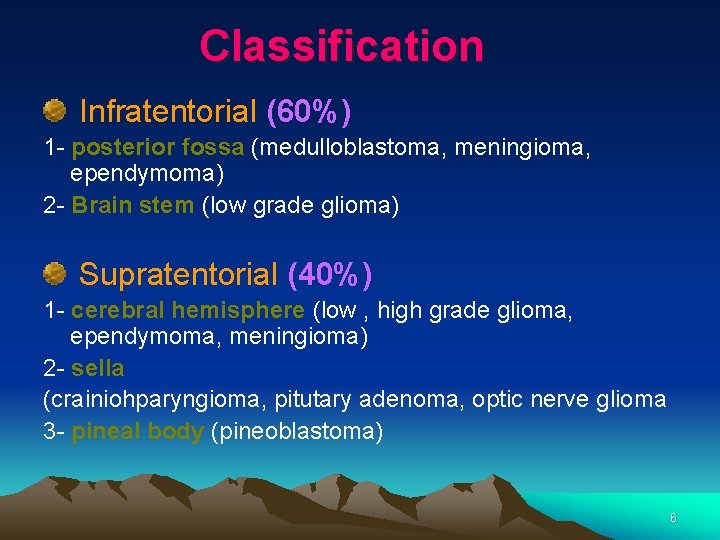
Classification (site) Infratentorial Supratentorial • Tentorium: A fold of the dura mater which cover and separates the cerebellum from the occipital lobes of cerebrum 5
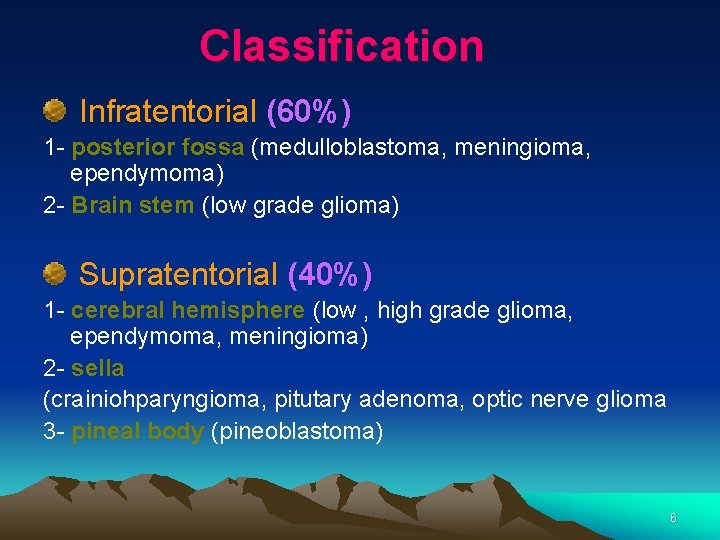
Classification Infratentorial (60%) 1 - posterior fossa (medulloblastoma, meningioma, ependymoma) 2 - Brain stem (low grade glioma) Supratentorial (40%) 1 - cerebral hemisphere (low , high grade glioma, ependymoma, meningioma) 2 - sella (crainiohparyngioma, pitutary adenoma, optic nerve glioma 3 - pineal body (pineoblastoma) 6
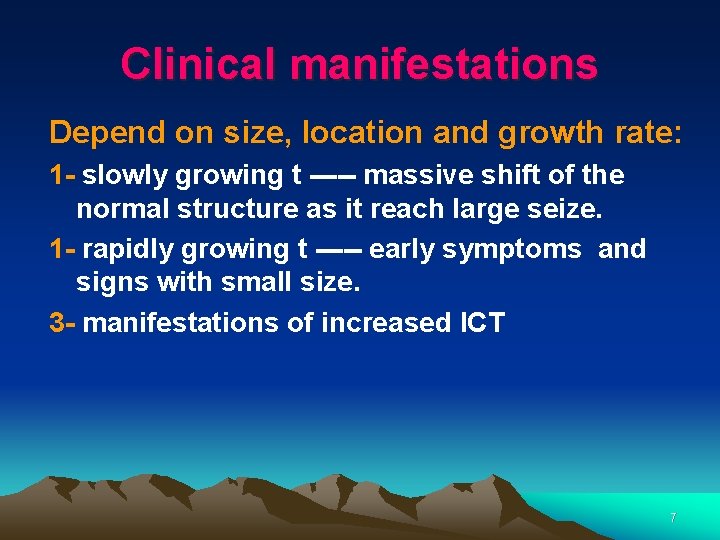
Clinical manifestations Depend on size, location and growth rate: 1 - slowly growing t ----- massive shift of the normal structure as it reach large seize. 1 - rapidly growing t ----- early symptoms and signs with small size. 3 - manifestations of increased ICT 7
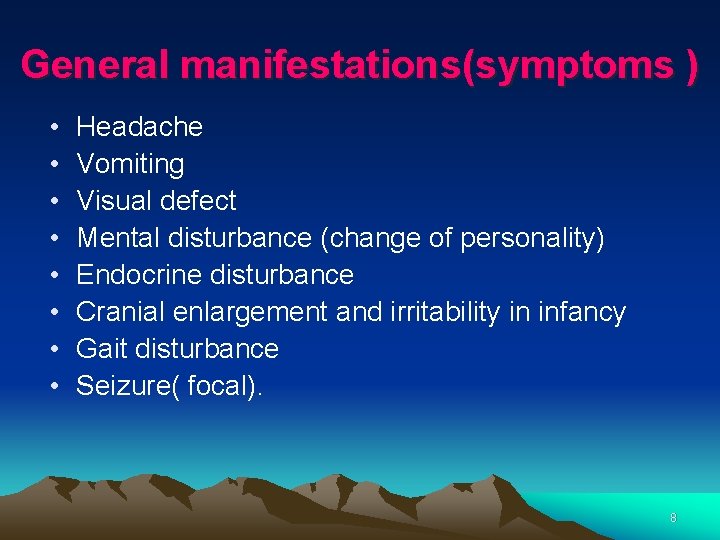
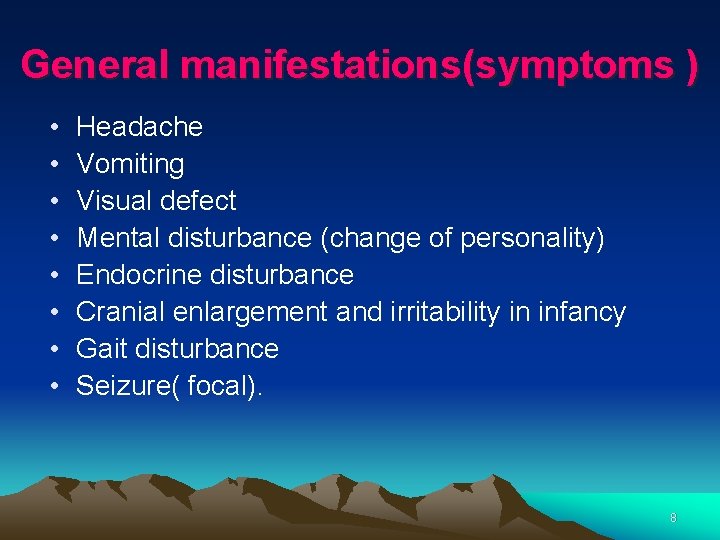
General manifestations(symptoms ) • • Headache Vomiting Visual defect Mental disturbance (change of personality) Endocrine disturbance Cranial enlargement and irritability in infancy Gait disturbance Seizure( focal). 8
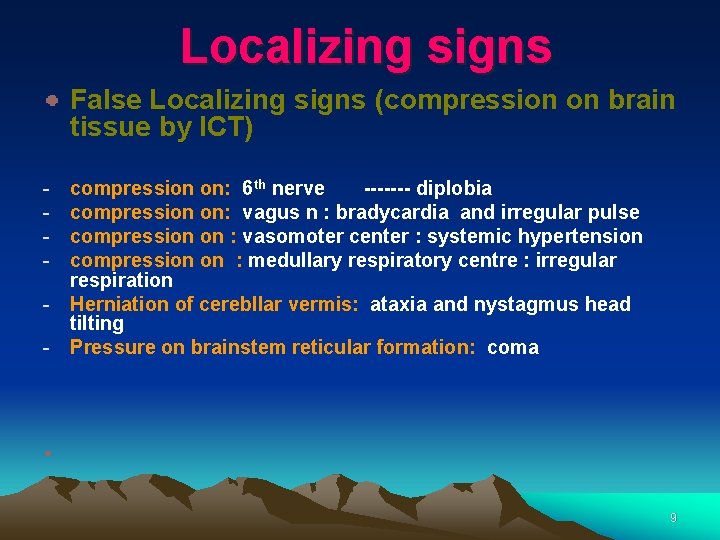
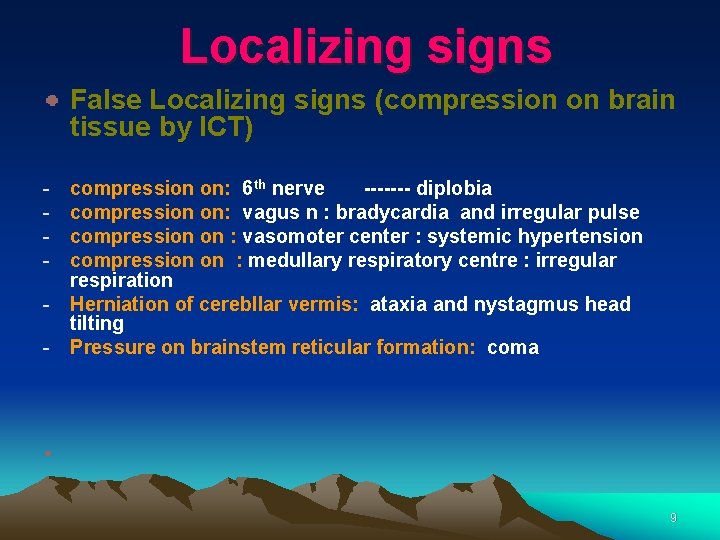
Localizing signs False Localizing signs (compression on brain tissue by ICT) - compression on: 6 th nerve ------- diplobia compression on: vagus n : bradycardia and irregular pulse compression on : vasomoter center : systemic hypertension compression on : medullary respiratory centre : irregular respiration Herniation of cerebllar vermis: ataxia and nystagmus head tilting Pressure on brainstem reticular formation: coma 9
10
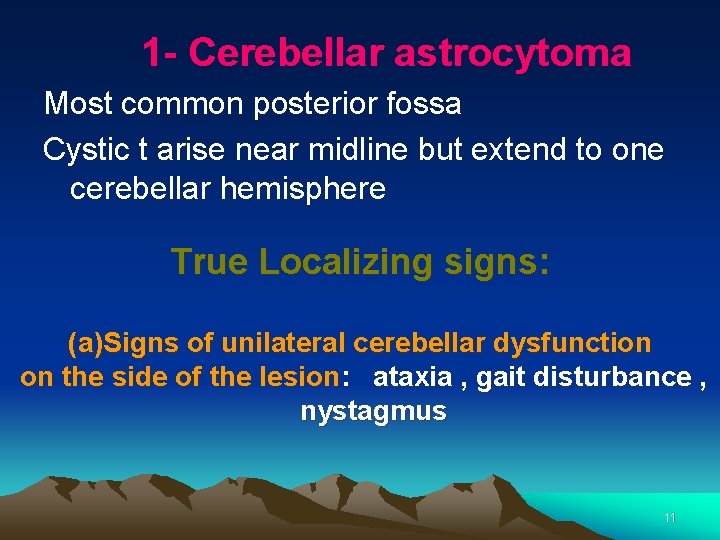
1 - Cerebellar astrocytoma Most common posterior fossa Cystic t arise near midline but extend to one cerebellar hemisphere True Localizing signs: (a)Signs of unilateral cerebellar dysfunction on the side of the lesion: ataxia , gait disturbance , nystagmus 11
(b) Cerebellar fits : seizure like states due to pressure on vital structure in the brainstem loss of consciousness , neck retraction, dilatation of the pupils and respiratory irregularity. (c) Hydrocephalus and s, s of increased ICT: obstruction of aqueduct of sylvius or fourth ventricle. 12

Treatment 1 - surgery • 2 - chemotherapy • 3 - radiotherapy • 13
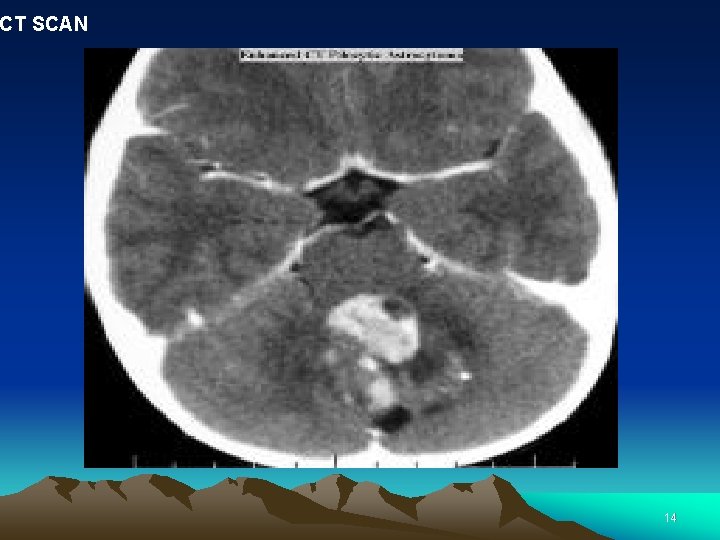
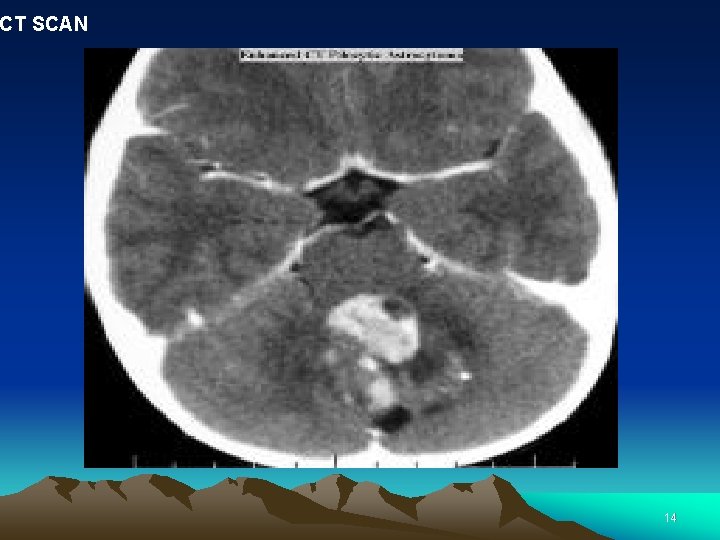
CT SCAN 14
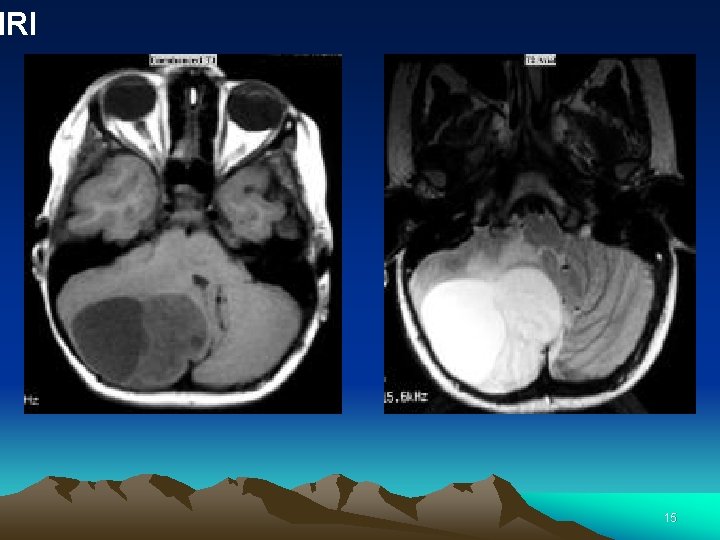
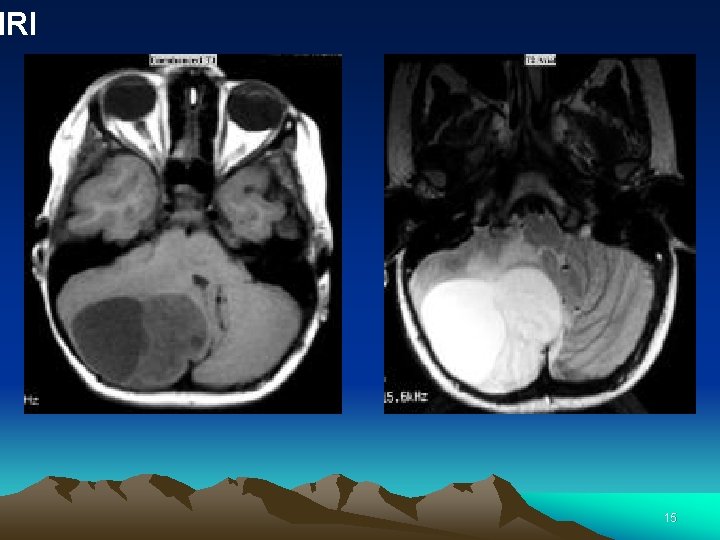
MRI 15
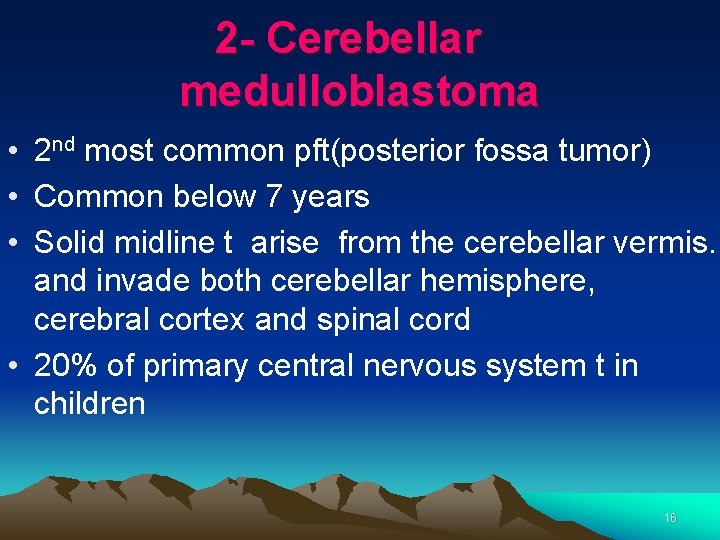
2 - Cerebellar medulloblastoma • 2 nd most common pft(posterior fossa tumor) • Common below 7 years • Solid midline t arise from the cerebellar vermis. and invade both cerebellar hemisphere, cerebral cortex and spinal cord • 20% of primary central nervous system t in children 16
True Localizing signs: • ataxia , hydrocephalus and signs of increased ICT other symptoms: Hydrocephalus 17
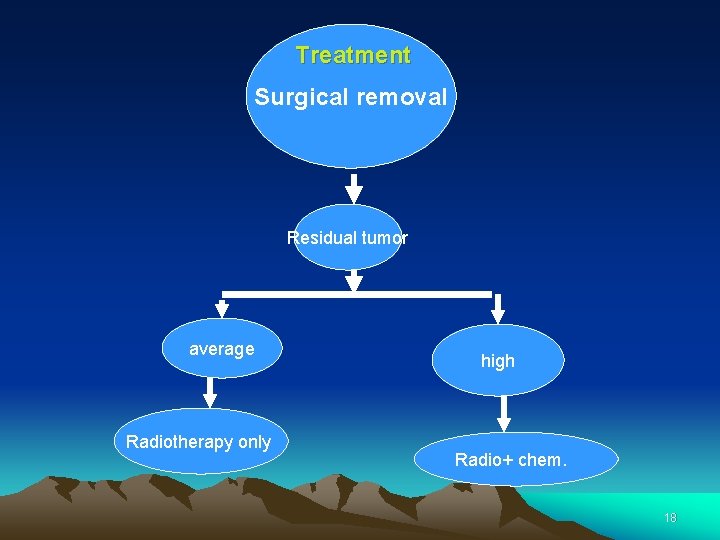
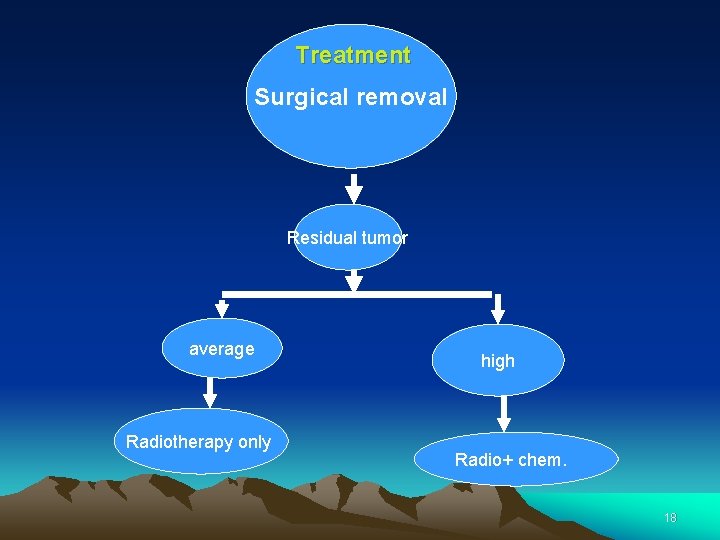
Treatment Surgical removal Residual tumor average Radiotherapy only high Radio+ chem. 18
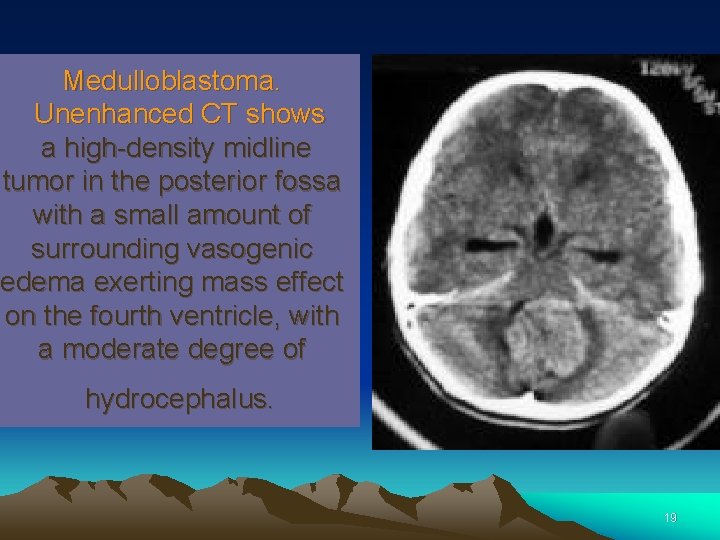
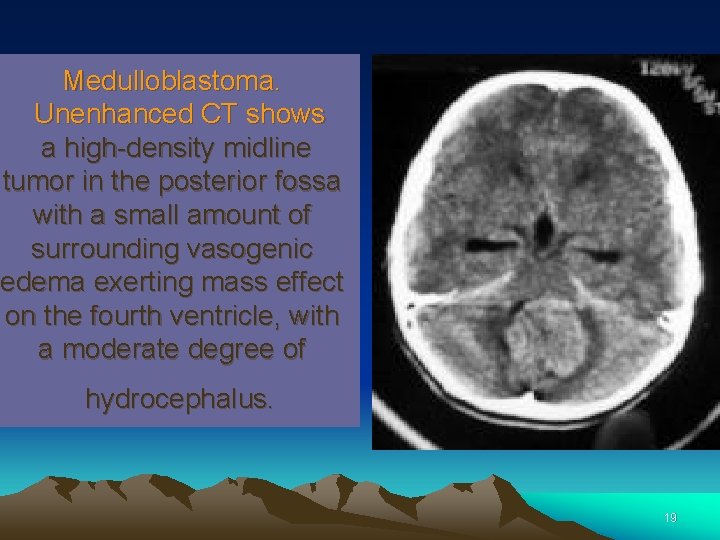
Medulloblastoma. Unenhanced CT shows a high-density midline tumor in the posterior fossa with a small amount of surrounding vasogenic edema exerting mass effect on the fourth ventricle, with a moderate degree of hydrocephalus. 19
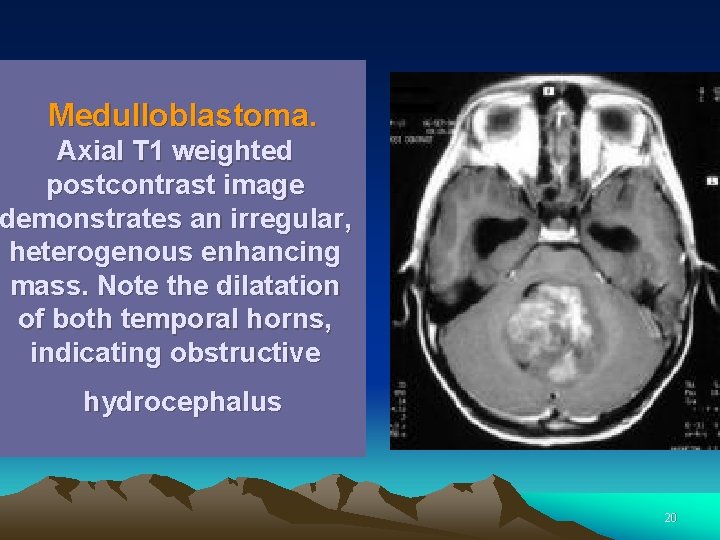
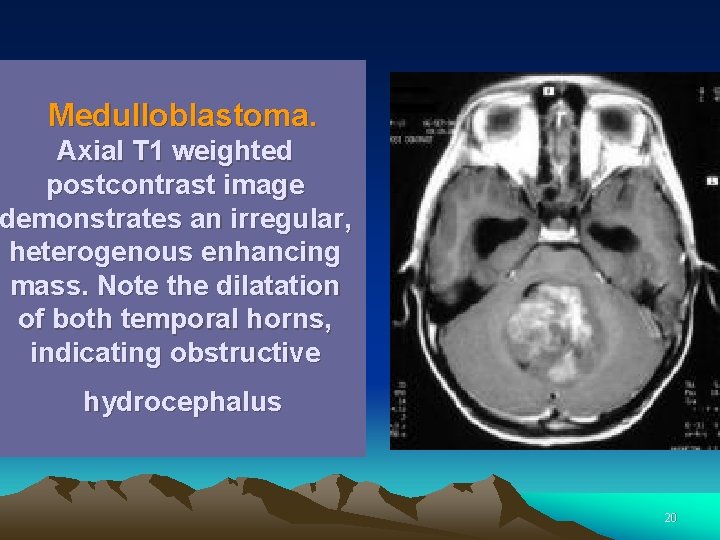
Medulloblastoma. Axial T 1 weighted postcontrast image demonstrates an irregular, heterogenous enhancing mass. Note the dilatation of both temporal horns, indicating obstructive hydrocephalus 20
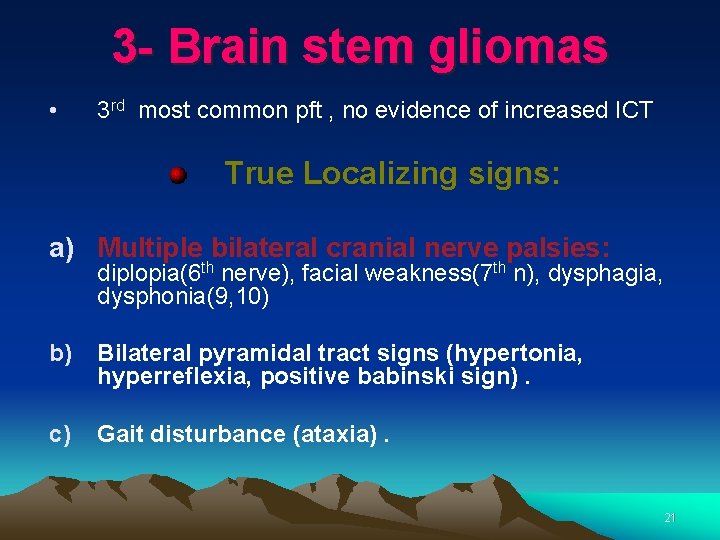
3 - Brain stem gliomas • 3 rd most common pft , no evidence of increased ICT True Localizing signs: a) Multiple bilateral cranial nerve palsies: diplopia(6 th nerve), facial weakness(7 th n), dysphagia, dysphonia(9, 10) b) Bilateral pyramidal tract signs (hypertonia, hyperreflexia, positive babinski sign). c) Gait disturbance (ataxia). 21
Treatment (palliative) Surgery: not usually possible (near to vital structure, limited room for expansion) Radiotherapy : limited field radiation Chemotherapy : not improve survival 22
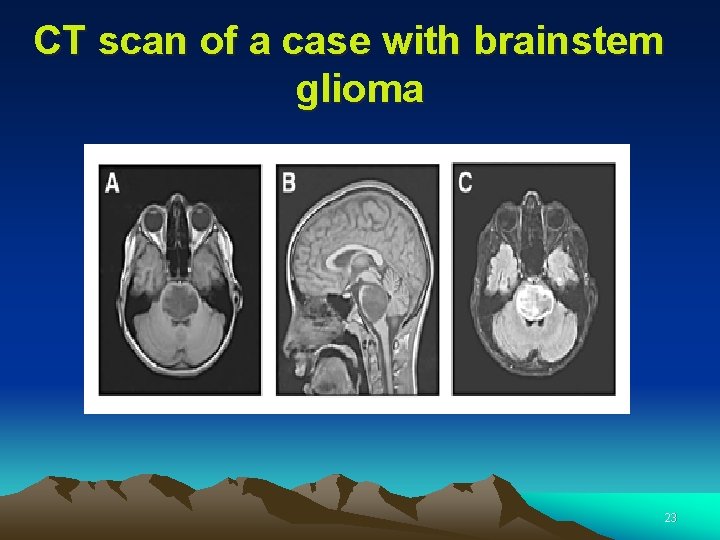
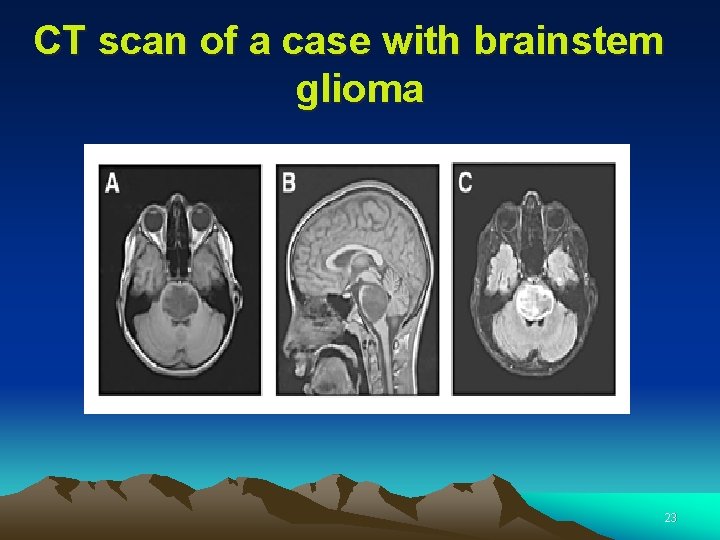
CT scan of a case with brainstem glioma 23

4 - Ependymomas • Arise from the floor of the 4 th ventricle • Early obstruction to CSF flow early signs of increased ICT • Calcification 24
Grades 3, 4 Treatment Surgery (debalking) radiotherapy chemotherapy 25
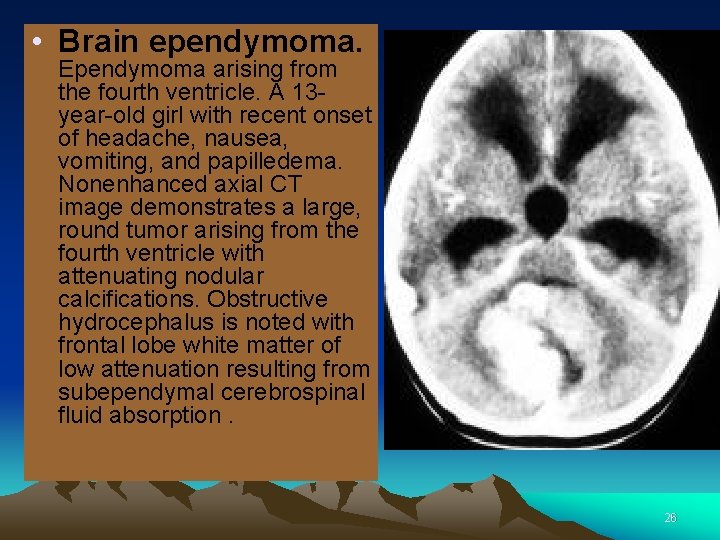
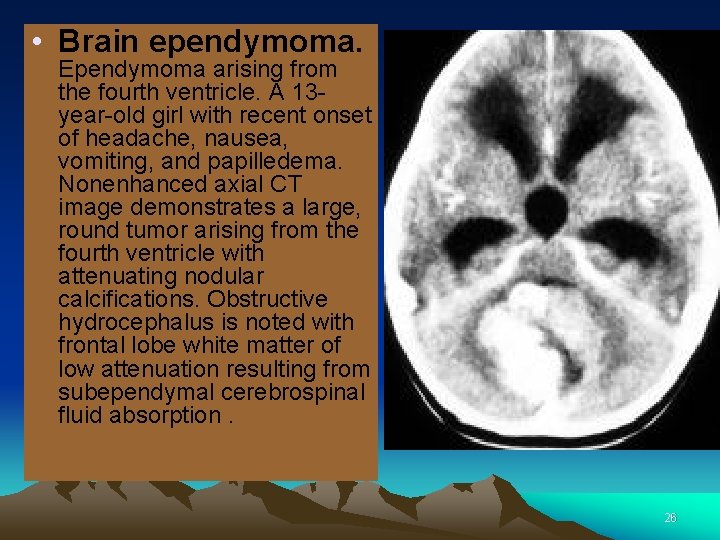
• Brain ependymoma. Ependymoma arising from the fourth ventricle. A 13 year-old girl with recent onset of headache, nausea, vomiting, and papilledema. Nonenhanced axial CT image demonstrates a large, round tumor arising from the fourth ventricle with attenuating nodular calcifications. Obstructive hydrocephalus is noted with frontal lobe white matter of low attenuation resulting from subependymal cerebrospinal fluid absorption. 26
27
1 -Craniopharyngioma • the most Supratentorial t • Slowly growing (benign histology but malignant behavior) • Consist of cystic and solid areas with calcification • arising from remnants of the craniopharyngeal duct • May be confined to sella turcica or extend to compress optic nerve system 28
C/P • Progressive visual loss • Increased ICT • Endocrine disorders : short stature and growth failure. X ray skull: calcification of intra or supra sellar location and increased ICT 29
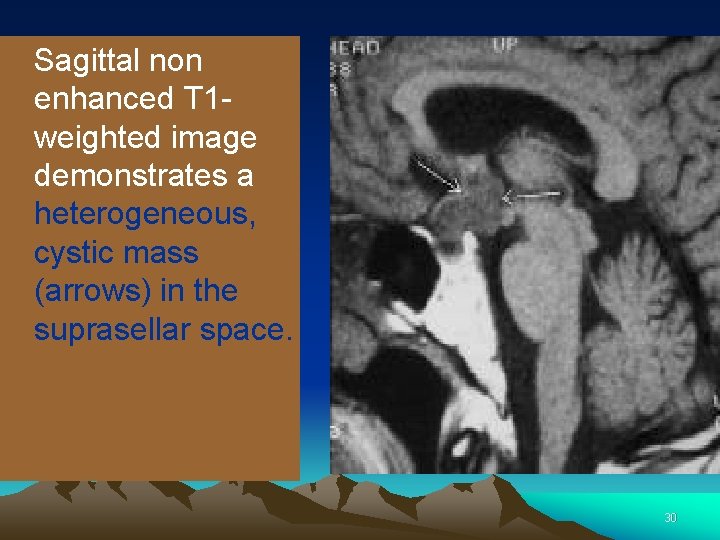
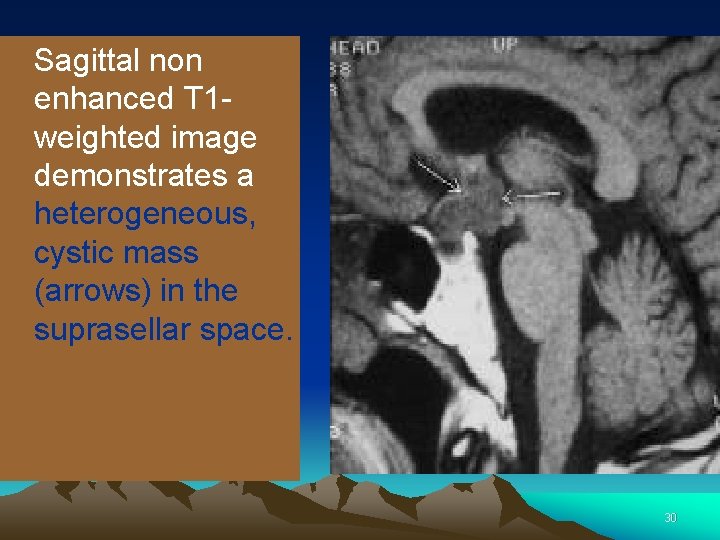
Sagittal non enhanced T 1 weighted image demonstrates a heterogeneous, cystic mass (arrows) in the suprasellar space. 30
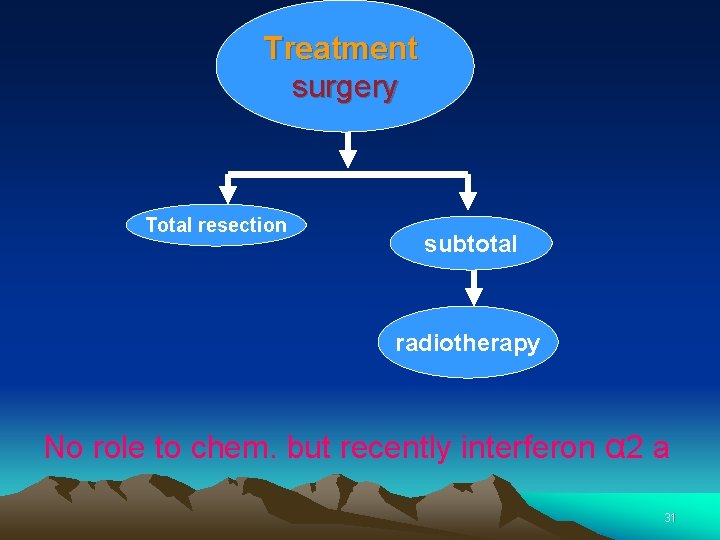
Treatment surgery Total resection subtotal radiotherapy No role to chem. but recently interferon α 2 a 31
2 - CHOROID PLEXUS PAPILLOMA • Most common prior to 3 yr of age. • It usually arises from choroid plexus of a lateral ventricle (less commonly 3 rd and 4 th ventricles )-- increased CSF production --- hydrocephalus. • Ct scan detect the tumor mass and hydrocephalus. • Malignant choroid plexus carcinoma is extremely vascular and invasive. • Treatment : mainly surgical resection. 32
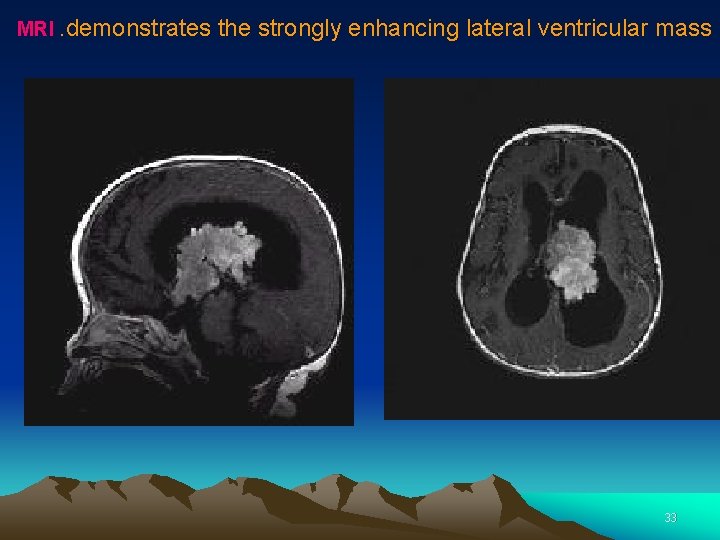
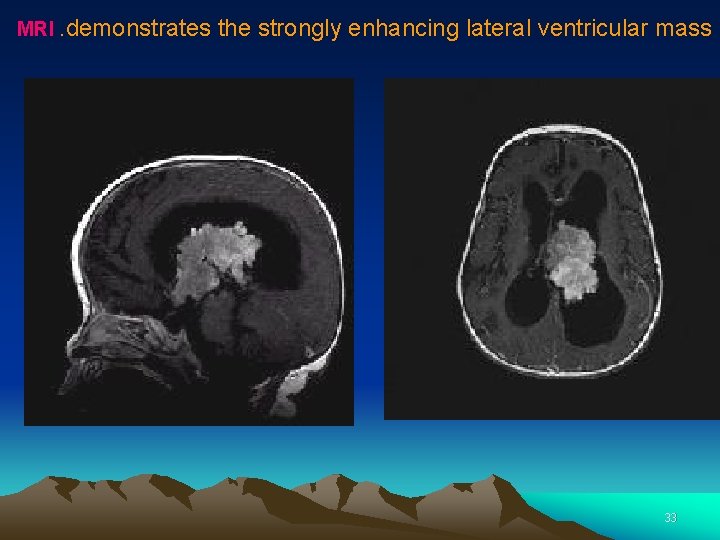
MRI. demonstrates the strongly enhancing lateral ventricular mass 33
3 - LEUKEMIA • It may invade : A. Leptomeninges ----- increased intracranial pressure B. Brain parenchyma (Focal signs). c. CNS Hge 34
4 - Cerebral cortex tumors Cerebral ASTROCYTOMA • They are located in the cerebral hemisphere The true localizing signs (according to the site of the tumor ) are : A. Frontal lobe tumor * irritative ( early) lesion : • chronic focal convulsion of opposite side. Destructive lesion : • personality changes: lethargic, irritable, forgetful Progressive motor weakness of UMNL type in the 35 opposite side of the body
b. Parietal lobe tumor * Irritative lesion : fits of opposite side of body. • destructive lesion: loss of cortical sensation. • C. Occipital lobe tumor • Irritative lesion : visual hallucination ( flashes of light). destructive lesion : visual affection. D. Temporal lobe tumor * Irritative lesion : epilepsy. *destructive lesion: loss of hearing, 36
5 - PITUTARY T • Pituitary adenomas are divided into 2 categories by their size : v. Microadenomas: < 1 cm are rarely damage the rest of the pituitary or neighboring tissues. They produce symptoms because of the excessive amounts of hormone they secrete. • Macroadenomas: >1 cm. have they cause symptoms of damage of the normal pituitary tissue or nearby nerves especially the optic nerve and manifestation of hormonal secretion 37
Manifestation of pitutary t A. hormonal manifestations • gigantism or acromegaly. • cushing syndrome. • hypopituitarism. B. Neurological manifestations (compression of adjacent structures ) 38
treatment Surgical removal Radiation therapy using high-doses of x-rays to kill tumor cells 39
40
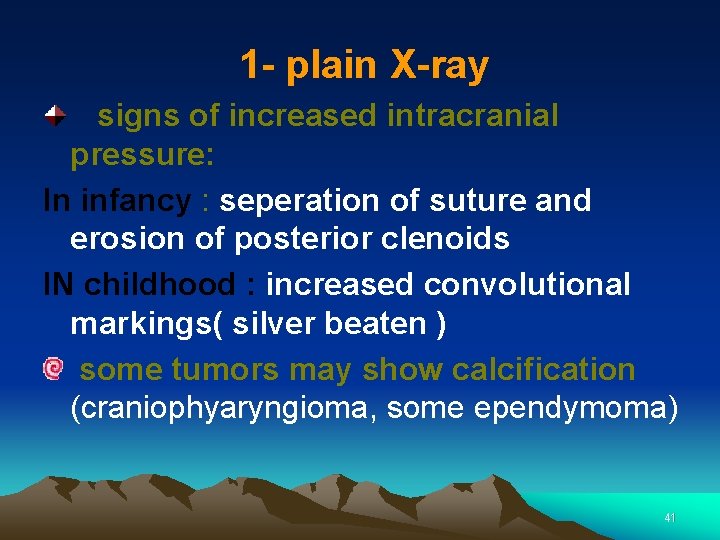
1 - plain X-ray signs of increased intracranial pressure: In infancy : seperation of suture and erosion of posterior clenoids IN childhood : increased convolutional markings( silver beaten ) some tumors may show calcification (craniophyaryngioma, some ependymoma) 41
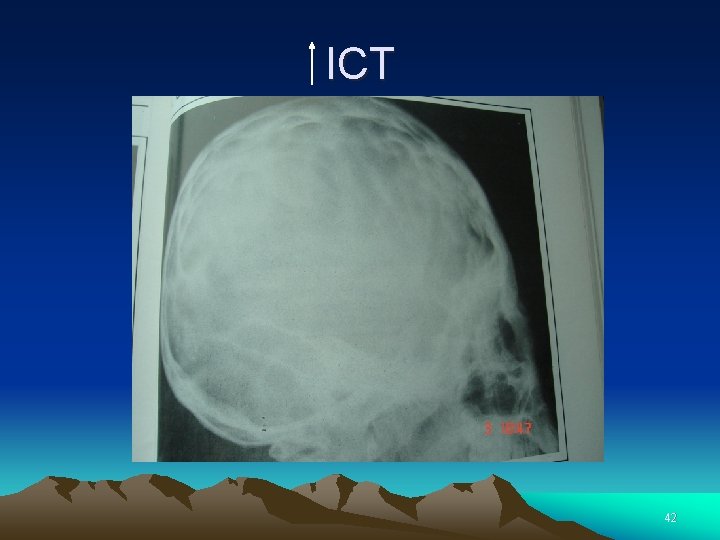
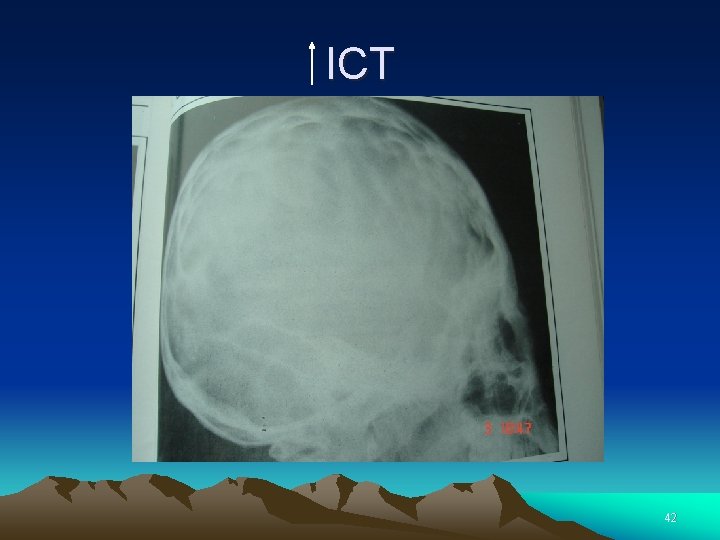
ICT 42
2 - CT SCAN • Detect 95% of brain tumors even without contrast. • Not useful in posterior fossa t ---MRI. • Useful than MRI in (calcified t and unstable patients) 3 - MRI 43
4 -Biopsy • The only test that can absolutely make a diagnosis of a brain tumor is a biopsy. • A needle biopsy: Tissue is removed using the needle, which is frequently guided by CT scanning. 44
Spread of brain tumor • Local: confined to: one hemisphere in one part of brain (infra/supratentorial); meninges; invading/encroaching on ventricular system • Regional crossing midline or tentorium invades bone, blood vessel, nerves, spinal cord • Distant circulating cells in CSF; extension to nasal cavity, nasopharynx, posterior pharynx; outside CNS 45

46