Update in Clinical Psychopharmacology Peter A De Maria


- Slides: 52
Update in Clinical Psychopharmacology Peter A. De. Maria, Jr. , M. D. , FASAM Tuttleman Counseling Services Temple University Clinical Associate Professor of Psychiatry Temple University School of Medicine Philadelphia, PA
Disclosures • I have no actual or potential conflict of interest in relation to this educational activity or presentation. • Use of trade versus generic drug names • Off-label use of drugs.
Treatment Planning 1. Medication 2. Psychotherapy 3. Combined medication and psychotherapy
Referral for Psychopharmacologic Evaluation/Treatment 1. When to refer 2. Preparing the patient 3. What to expect 4. The challenge of split treatment – Communication – Dynamics – Ethics – Legal issues 5. What to expect
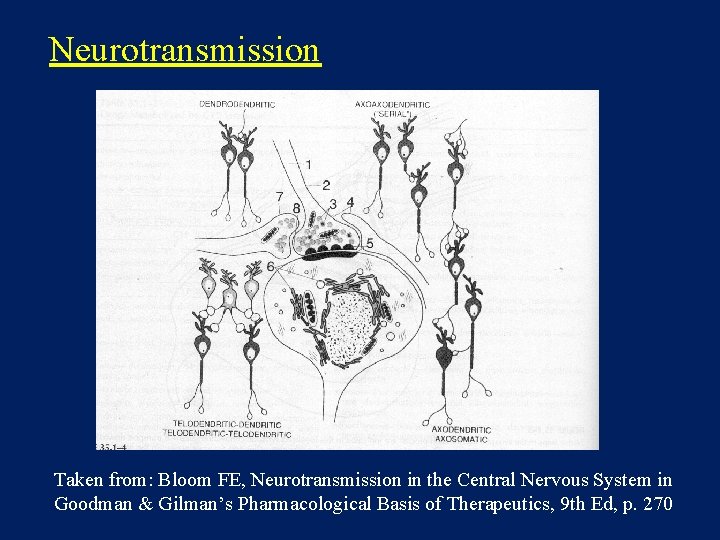
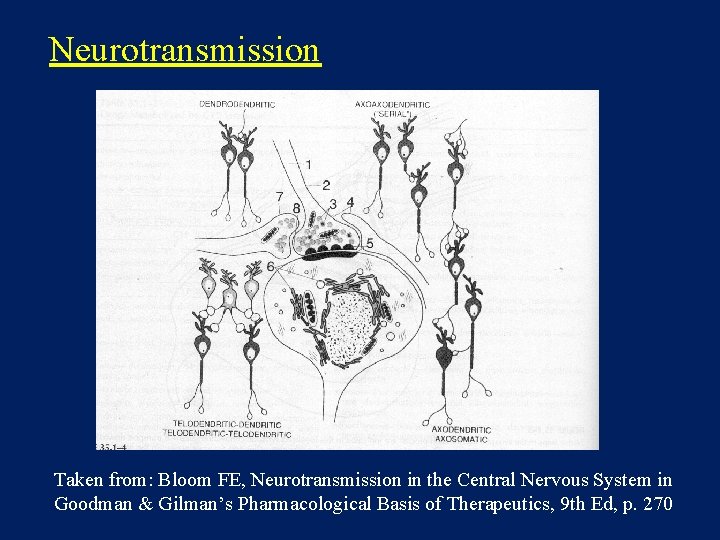
Neurotransmission Taken from: Bloom FE, Neurotransmission in the Central Nervous System in Goodman & Gilman’s Pharmacological Basis of Therapeutics, 9 th Ed, p. 270
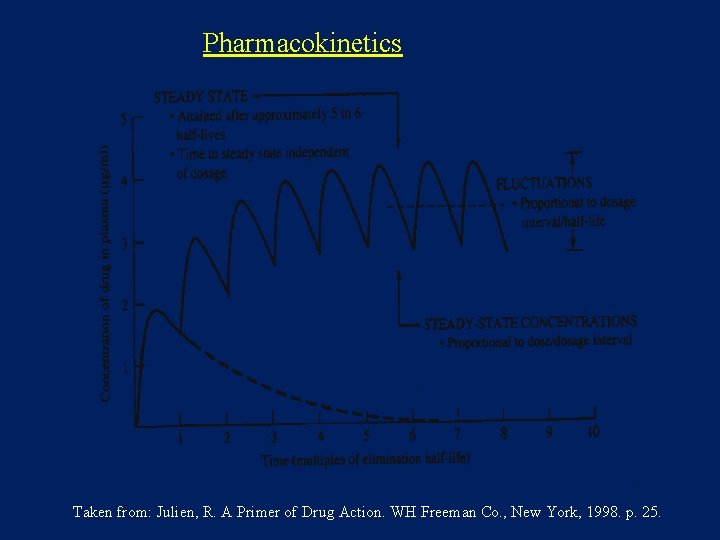
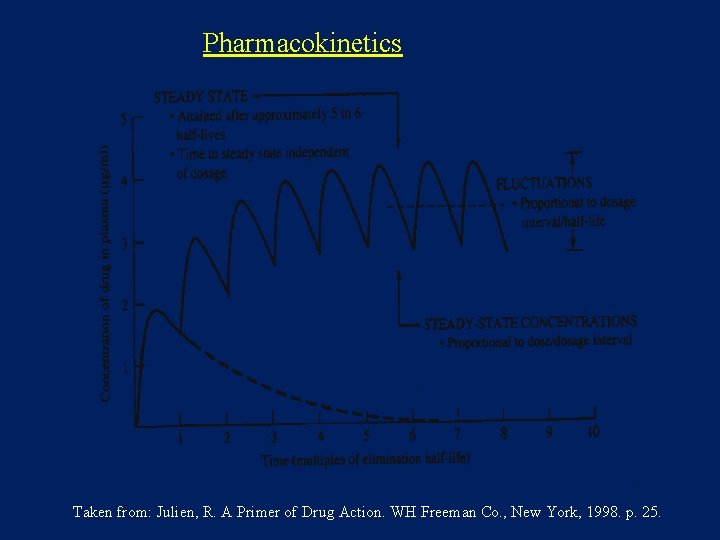
Pharmacokinetics Taken from: Julien, R. A Primer of Drug Action. WH Freeman Co. , New York, 1998. p. 25.
Drug Interactions · Synergism (e. g. alcohol + sedative) · Induction of enzymes and increased metabolism · Inhibition of enzymes and delayed metabolism · In vitro versus clinical significance FDA approval vs. clinical use (“Off-label use”)
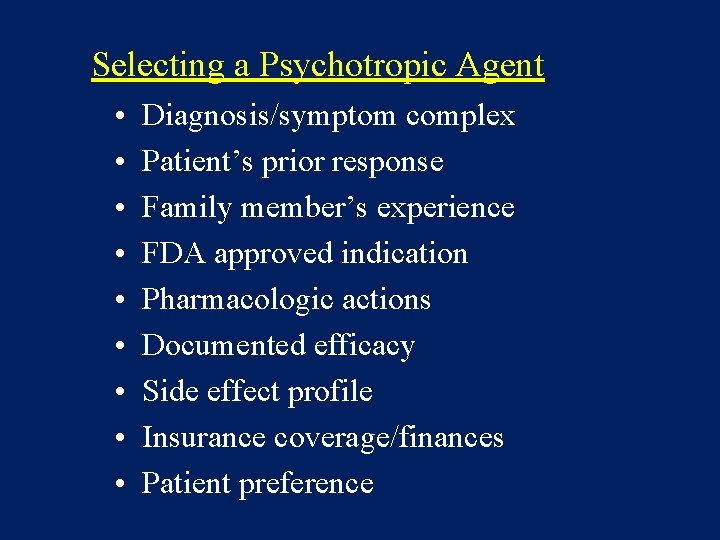
Selecting a Psychotropic Agent • • • Diagnosis/symptom complex Patient’s prior response Family member’s experience FDA approved indication Pharmacologic actions Documented efficacy Side effect profile Insurance coverage/finances Patient preference
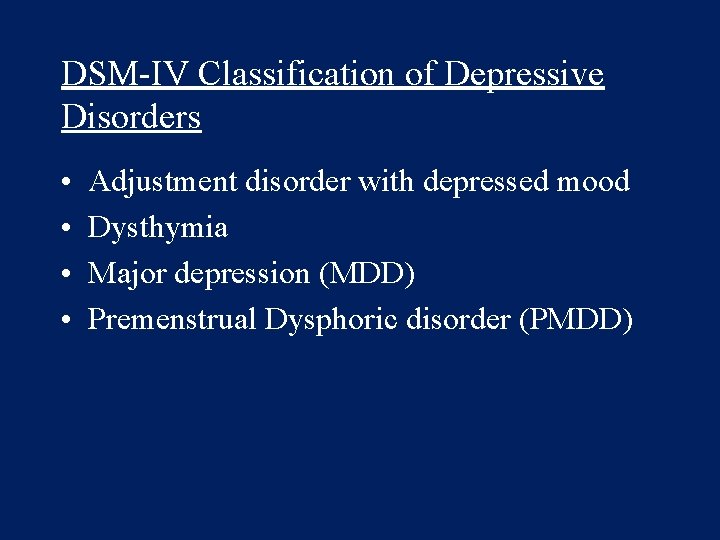
DSM-IV Classification of Depressive Disorders • • Adjustment disorder with depressed mood Dysthymia Major depression (MDD) Premenstrual Dysphoric disorder (PMDD)
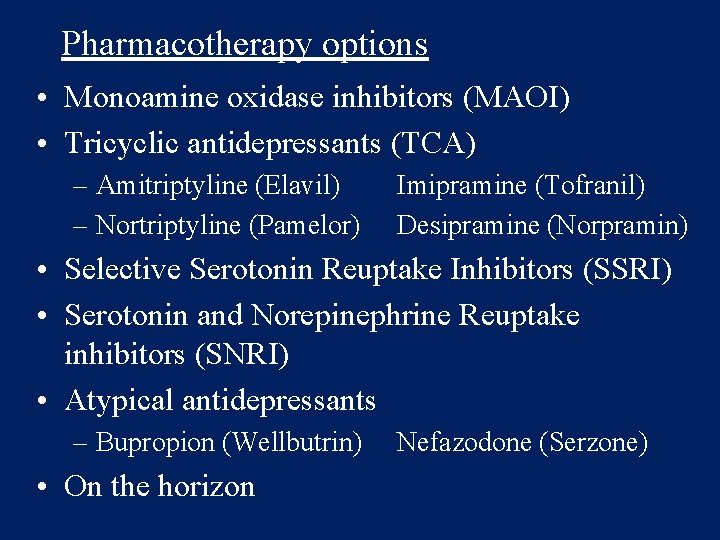
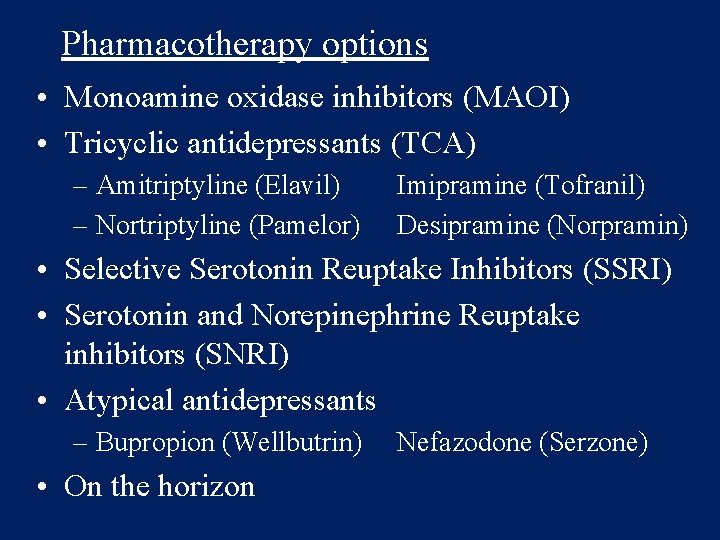
Pharmacotherapy options • Monoamine oxidase inhibitors (MAOI) • Tricyclic antidepressants (TCA) – Amitriptyline (Elavil) – Nortriptyline (Pamelor) Imipramine (Tofranil) Desipramine (Norpramin) • Selective Serotonin Reuptake Inhibitors (SSRI) • Serotonin and Norepinephrine Reuptake inhibitors (SNRI) • Atypical antidepressants – Bupropion (Wellbutrin) • On the horizon Nefazodone (Serzone)
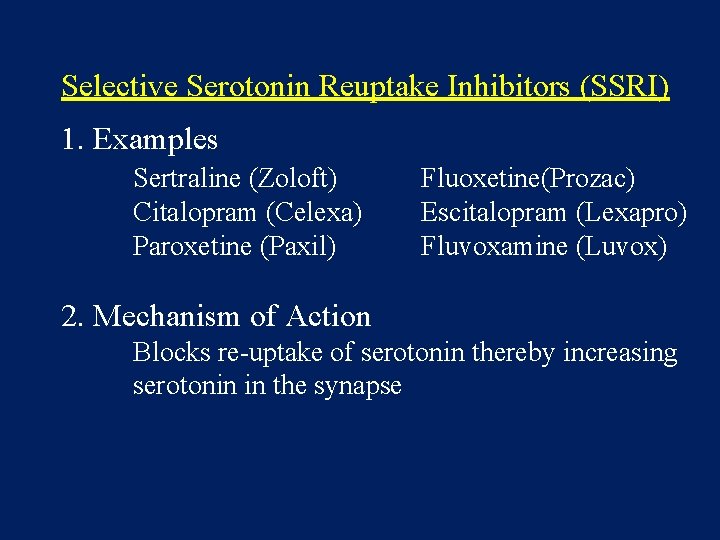
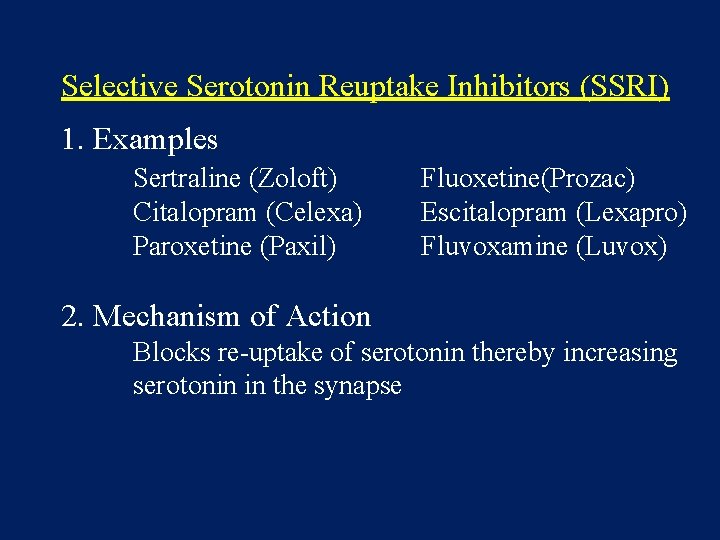
Selective Serotonin Reuptake Inhibitors (SSRI) 1. Examples Sertraline (Zoloft) Citalopram (Celexa) Paroxetine (Paxil) Fluoxetine(Prozac) Escitalopram (Lexapro) Fluvoxamine (Luvox) 2. Mechanism of Action Blocks re-uptake of serotonin thereby increasing serotonin in the synapse
SSRI - FDA Approved Indications Therapeutic Response • Can take between 2 and 8 weeks • Response is gradual • Others may notice the response before the patient does
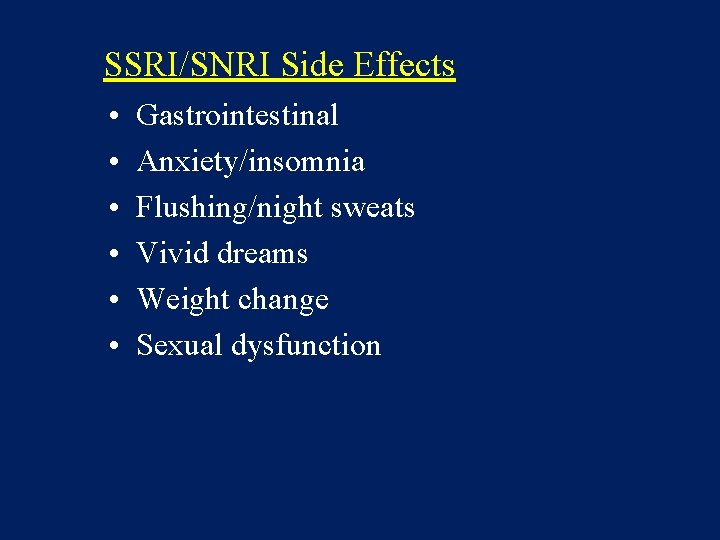
SSRI/SNRI Side Effects • • • Gastrointestinal Anxiety/insomnia Flushing/night sweats Vivid dreams Weight change Sexual dysfunction
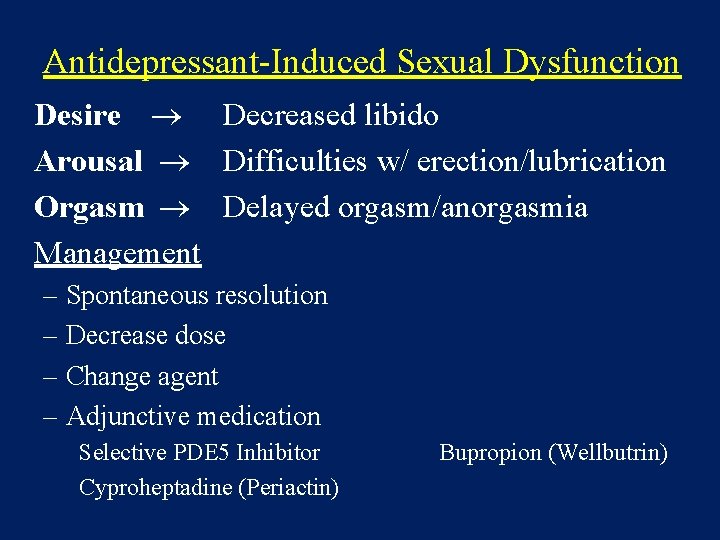
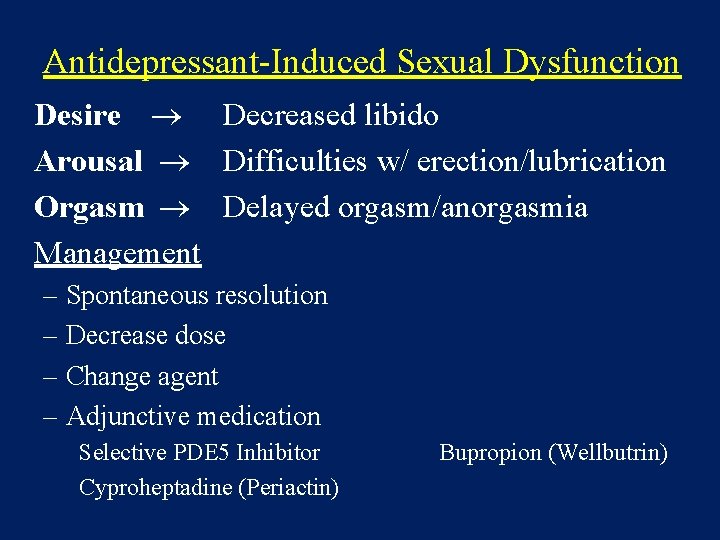
Antidepressant-Induced Sexual Dysfunction Desire Decreased libido Arousal Difficulties w/ erection/lubrication Orgasm Delayed orgasm/anorgasmia Management – Spontaneous resolution – Decrease dose – Change agent – Adjunctive medication Selective PDE 5 Inhibitor Cyproheptadine (Periactin) Bupropion (Wellbutrin)
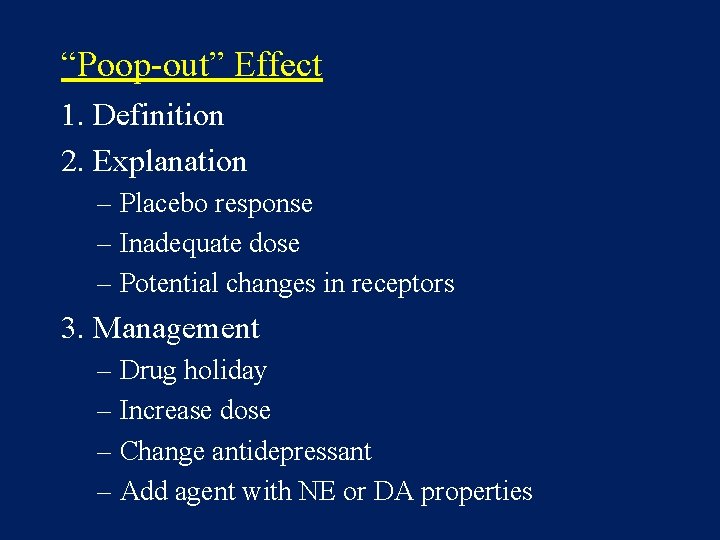
“Poop-out” Effect 1. Definition 2. Explanation – Placebo response – Inadequate dose – Potential changes in receptors 3. Management – Drug holiday – Increase dose – Change antidepressant – Add agent with NE or DA properties
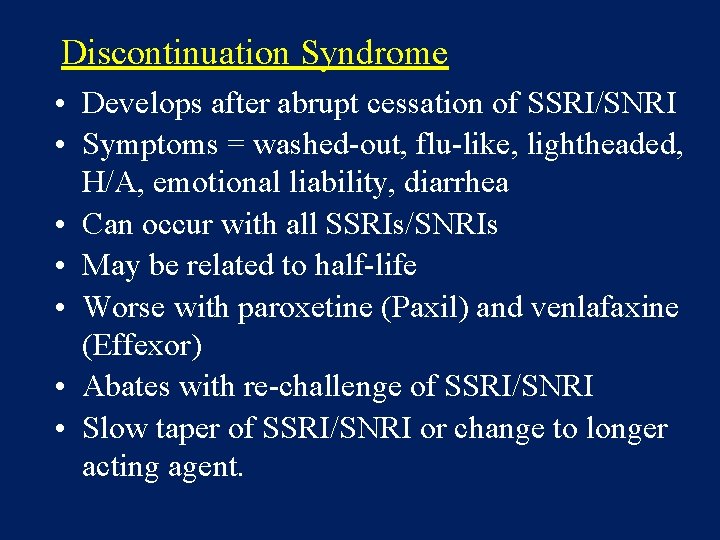
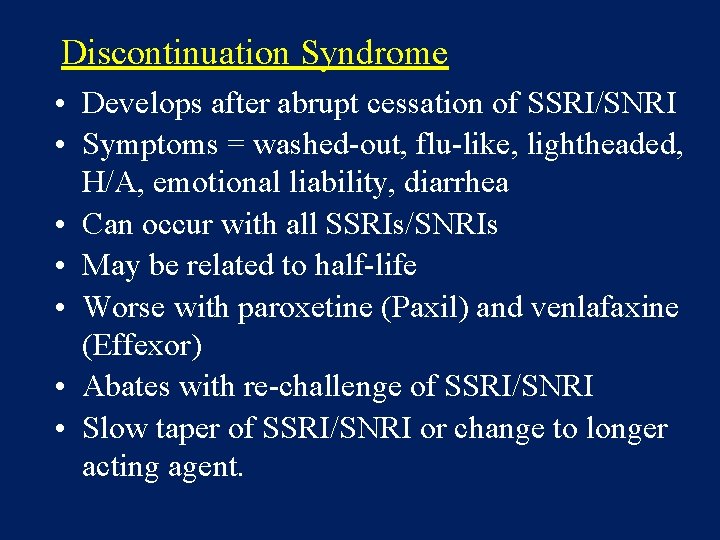
Discontinuation Syndrome • Develops after abrupt cessation of SSRI/SNRI • Symptoms = washed-out, flu-like, lightheaded, H/A, emotional liability, diarrhea • Can occur with all SSRIs/SNRIs • May be related to half-life • Worse with paroxetine (Paxil) and venlafaxine (Effexor) • Abates with re-challenge of SSRI/SNRI • Slow taper of SSRI/SNRI or change to longer acting agent.
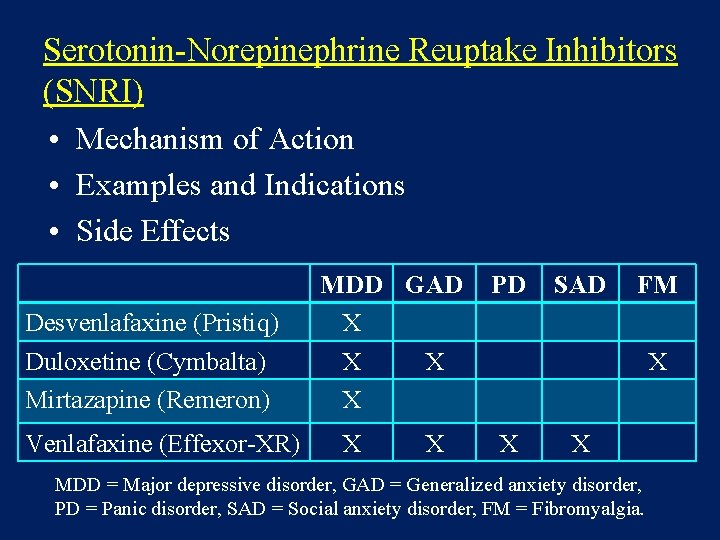
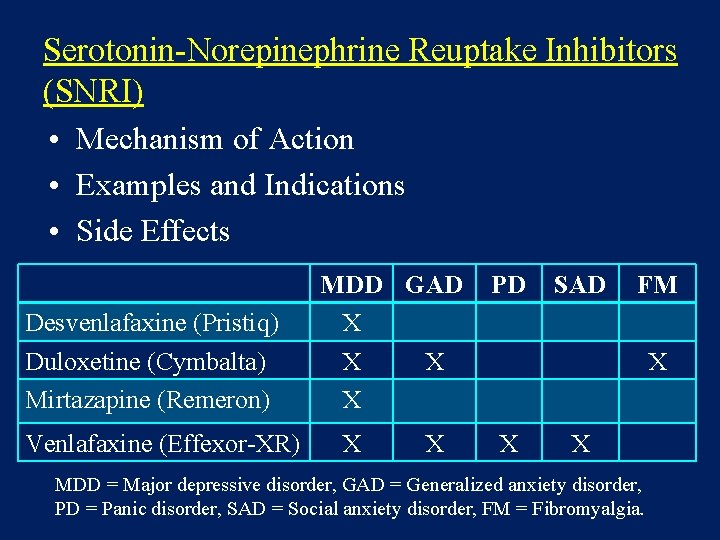
Serotonin-Norepinephrine Reuptake Inhibitors (SNRI) • Mechanism of Action • Examples and Indications • Side Effects Desvenlafaxine (Pristiq) Duloxetine (Cymbalta) Mirtazapine (Remeron) Venlafaxine (Effexor-XR) MDD GAD X X X PD SAD FM X X X MDD = Major depressive disorder, GAD = Generalized anxiety disorder, PD = Panic disorder, SAD = Social anxiety disorder, FM = Fibromyalgia.
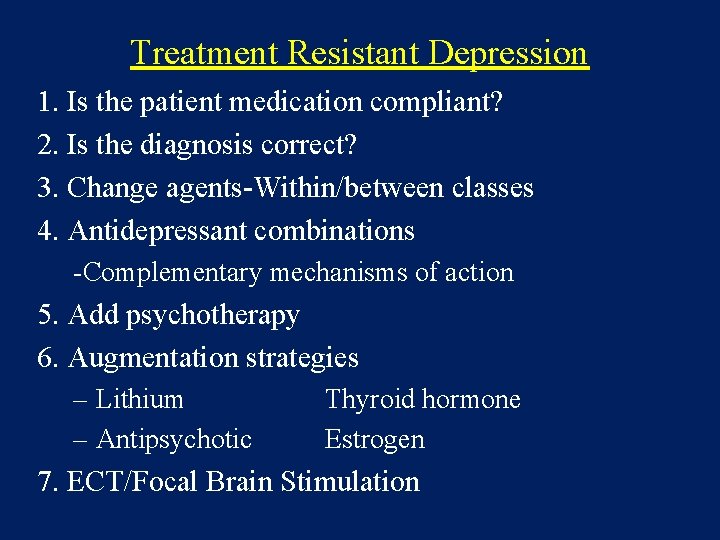
Treatment Resistant Depression 1. Is the patient medication compliant? 2. Is the diagnosis correct? 3. Change agents-Within/between classes 4. Antidepressant combinations -Complementary mechanisms of action 5. Add psychotherapy 6. Augmentation strategies – Lithium – Antipsychotic Thyroid hormone Estrogen 7. ECT/Focal Brain Stimulation
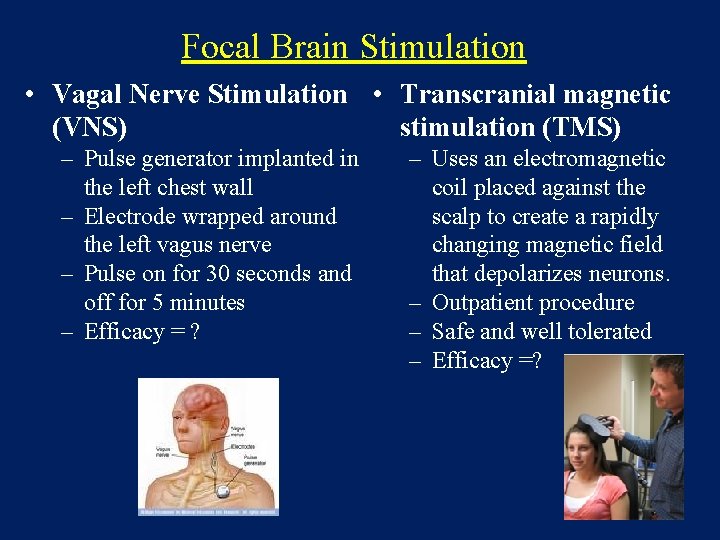
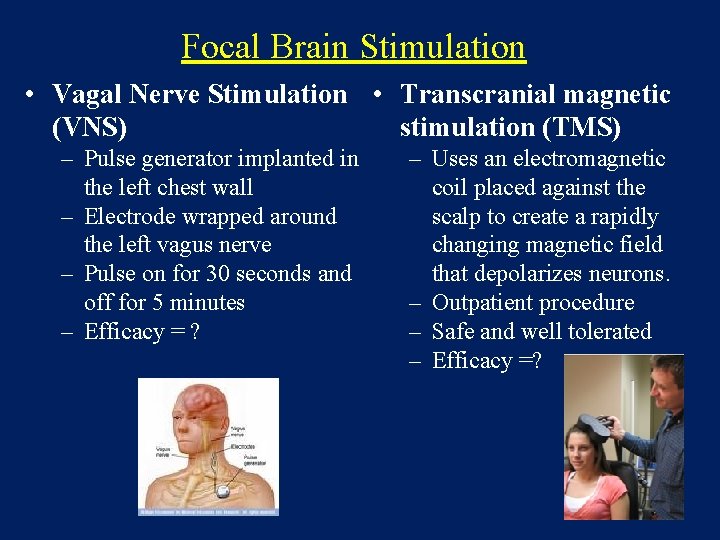
Focal Brain Stimulation • Vagal Nerve Stimulation • Transcranial magnetic (VNS) stimulation (TMS) – Pulse generator implanted in the left chest wall – Electrode wrapped around the left vagus nerve – Pulse on for 30 seconds and off for 5 minutes – Efficacy = ? – Uses an electromagnetic coil placed against the scalp to create a rapidly changing magnetic field that depolarizes neurons. – Outpatient procedure – Safe and well tolerated – Efficacy =?
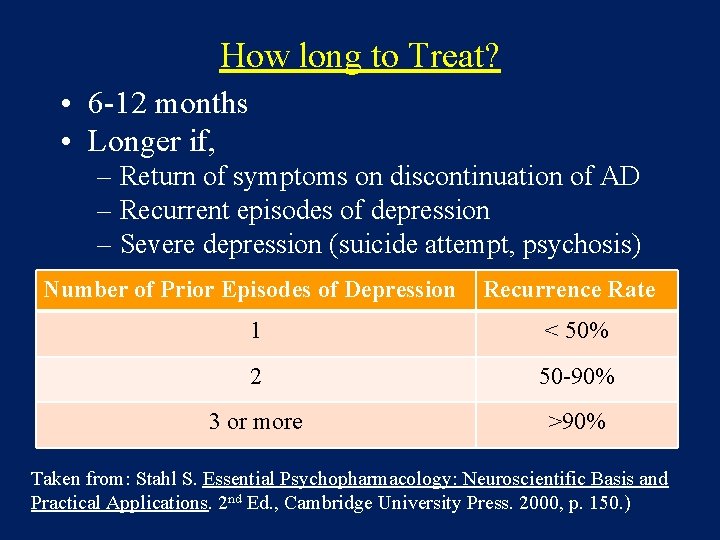
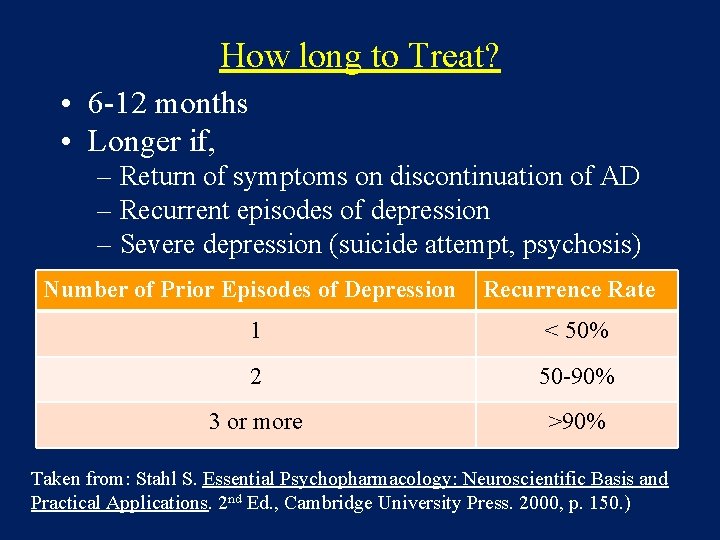
How long to Treat? • 6 -12 months • Longer if, – Return of symptoms on discontinuation of AD – Recurrent episodes of depression – Severe depression (suicide attempt, psychosis) Number of Prior Episodes of Depression Recurrence Rate 1 < 50% 2 50 -90% 3 or more >90% Taken from: Stahl S. Essential Psychopharmacology: Neuroscientific Basis and Practical Applications. 2 nd Ed. , Cambridge University Press. 2000, p. 150. )
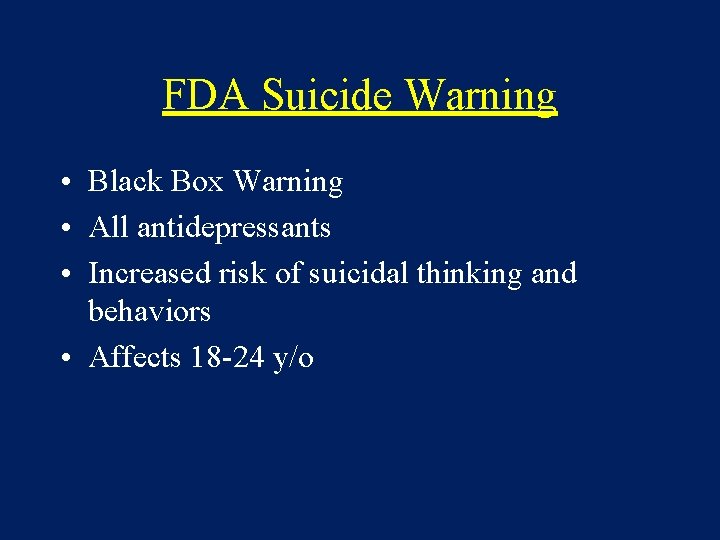
FDA Suicide Warning • Black Box Warning • All antidepressants • Increased risk of suicidal thinking and behaviors • Affects 18 -24 y/o
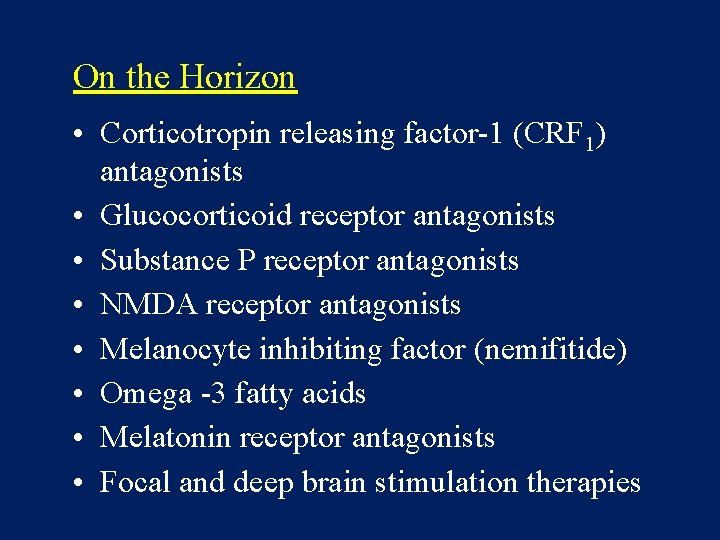
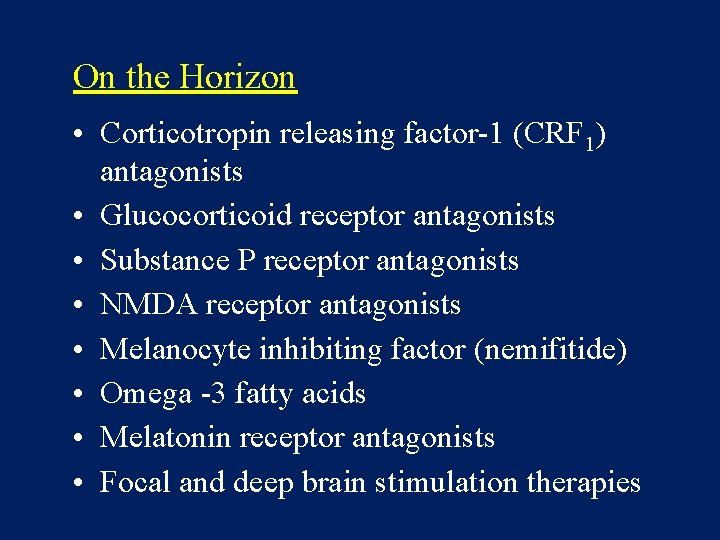
On the Horizon • Corticotropin releasing factor-1 (CRF 1) antagonists • Glucocorticoid receptor antagonists • Substance P receptor antagonists • NMDA receptor antagonists • Melanocyte inhibiting factor (nemifitide) • Omega -3 fatty acids • Melatonin receptor antagonists • Focal and deep brain stimulation therapies
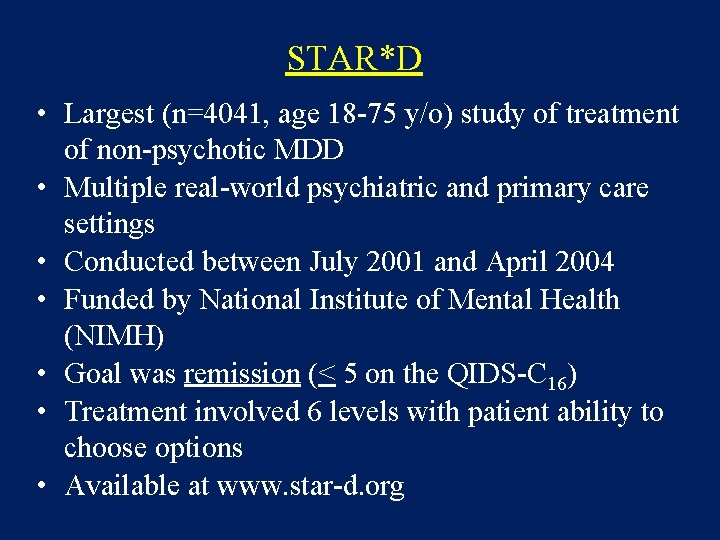
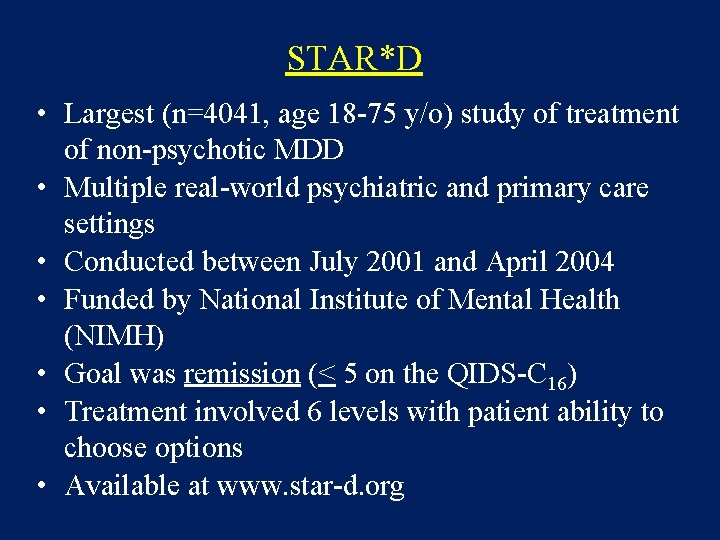
STAR*D • Largest (n=4041, age 18 -75 y/o) study of treatment of non-psychotic MDD • Multiple real-world psychiatric and primary care settings • Conducted between July 2001 and April 2004 • Funded by National Institute of Mental Health (NIMH) • Goal was remission (< 5 on the QIDS-C 16) • Treatment involved 6 levels with patient ability to choose options • Available at www. star-d. org
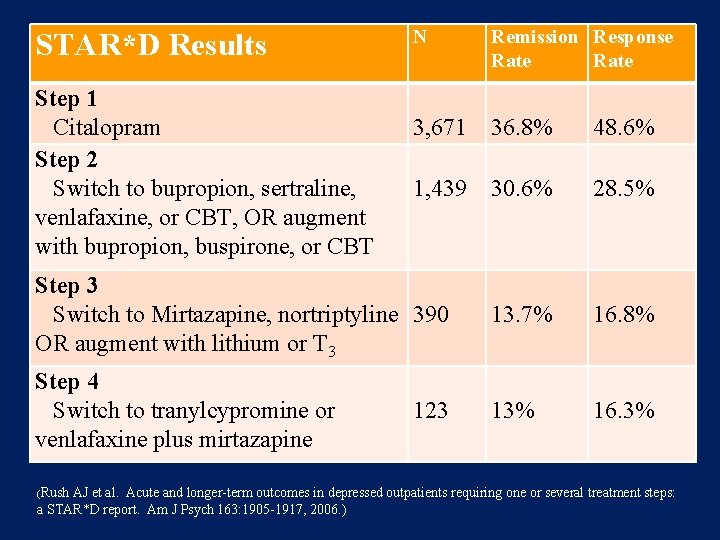
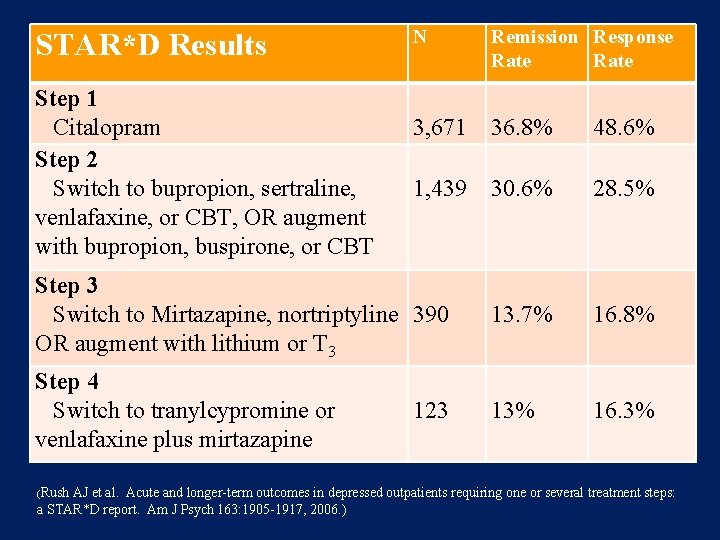
N Remission Response Rate 3, 671 36. 8% 48. 6% 1, 439 30. 6% 28. 5% Step 3 Switch to Mirtazapine, nortriptyline 390 OR augment with lithium or T 3 13. 7% 16. 8% Step 4 Switch to tranylcypromine or venlafaxine plus mirtazapine 13% 16. 3% STAR*D Results Step 1 Citalopram Step 2 Switch to bupropion, sertraline, venlafaxine, or CBT, OR augment with bupropion, buspirone, or CBT (Rush 123 AJ et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psych 163: 1905 -1917, 2006. )
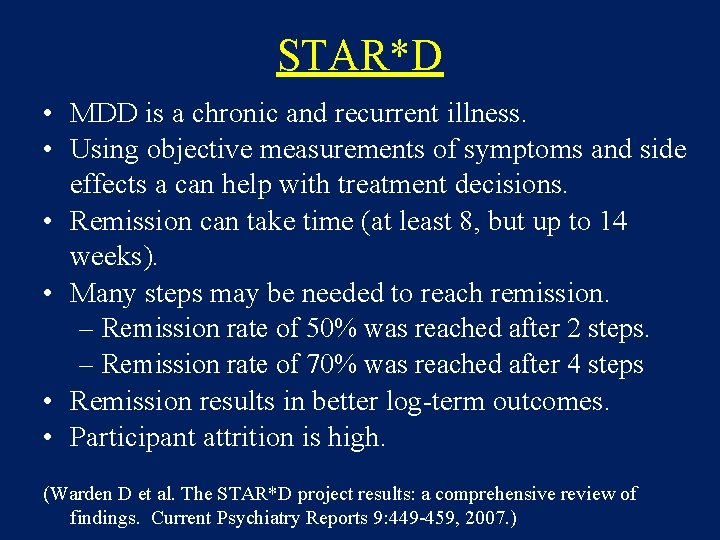
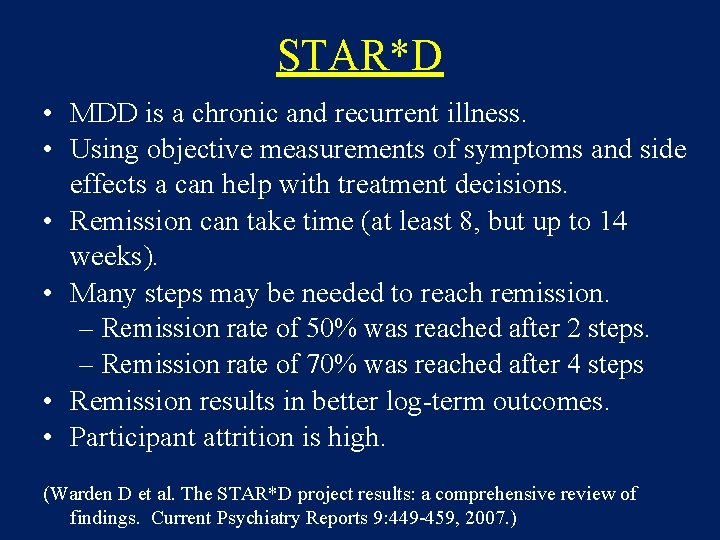
STAR*D • MDD is a chronic and recurrent illness. • Using objective measurements of symptoms and side effects a can help with treatment decisions. • Remission can take time (at least 8, but up to 14 weeks). • Many steps may be needed to reach remission. – Remission rate of 50% was reached after 2 steps. – Remission rate of 70% was reached after 4 steps • Remission results in better log-term outcomes. • Participant attrition is high. (Warden D et al. The STAR*D project results: a comprehensive review of findings. Current Psychiatry Reports 9: 449 -459, 2007. )

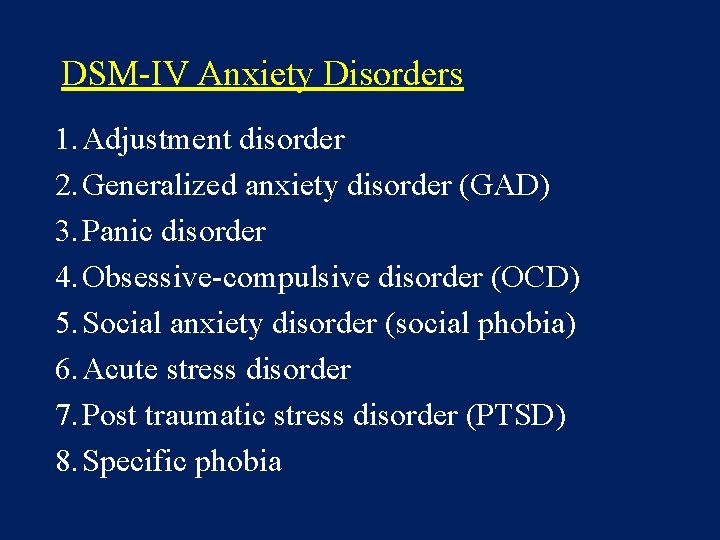
DSM-IV Anxiety Disorders 1. Adjustment disorder 2. Generalized anxiety disorder (GAD) 3. Panic disorder 4. Obsessive-compulsive disorder (OCD) 5. Social anxiety disorder (social phobia) 6. Acute stress disorder 7. Post traumatic stress disorder (PTSD) 8. Specific phobia
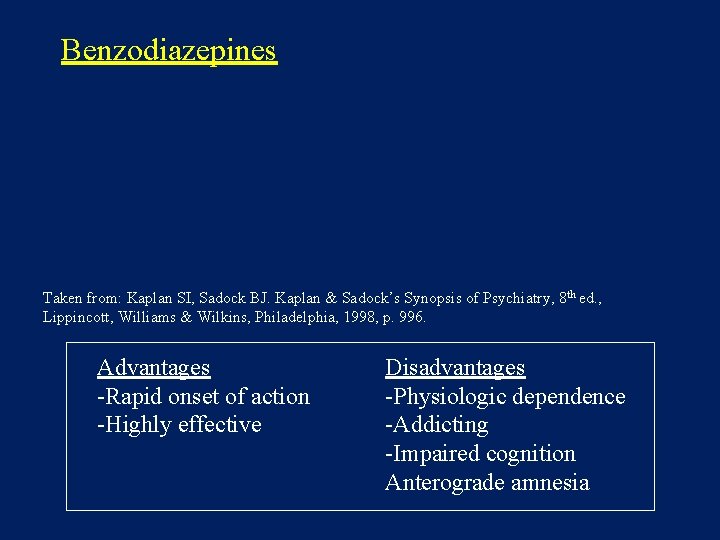
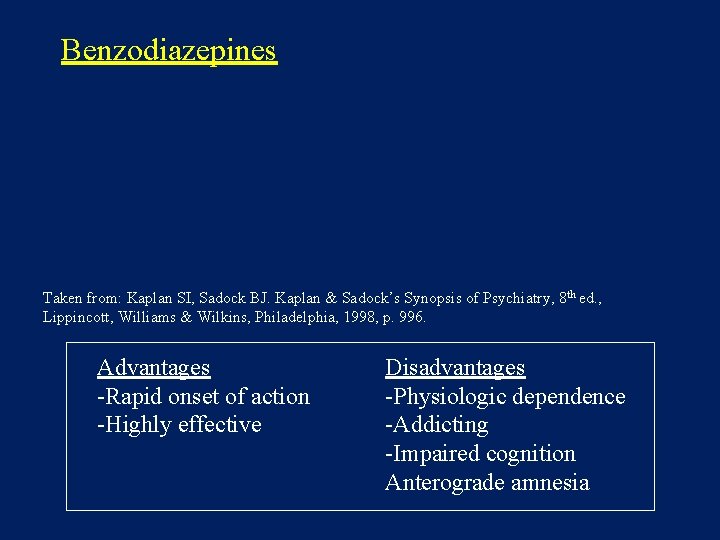
Benzodiazepines Taken from: Kaplan SI, Sadock BJ. Kaplan & Sadock’s Synopsis of Psychiatry, 8 th ed. , Lippincott, Williams & Wilkins, Philadelphia, 1998, p. 996. Advantages -Rapid onset of action -Highly effective Disadvantages -Physiologic dependence -Addicting -Impaired cognition Anterograde amnesia
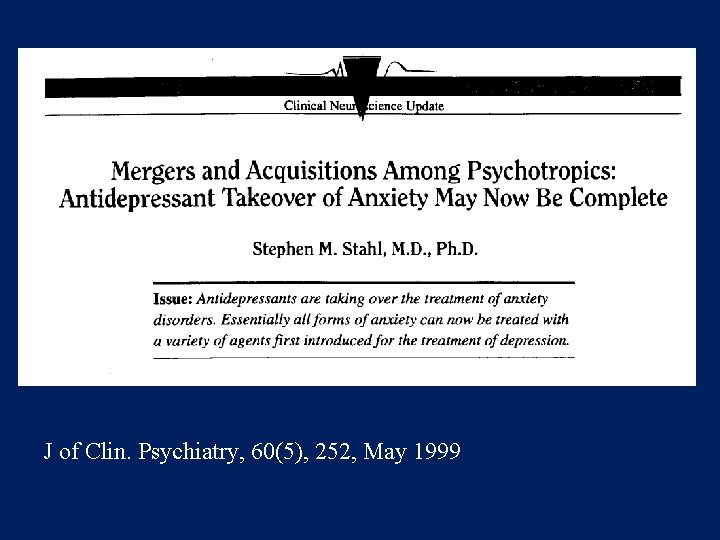
J of Clin. Psychiatry, 60(5), 252, May 1999
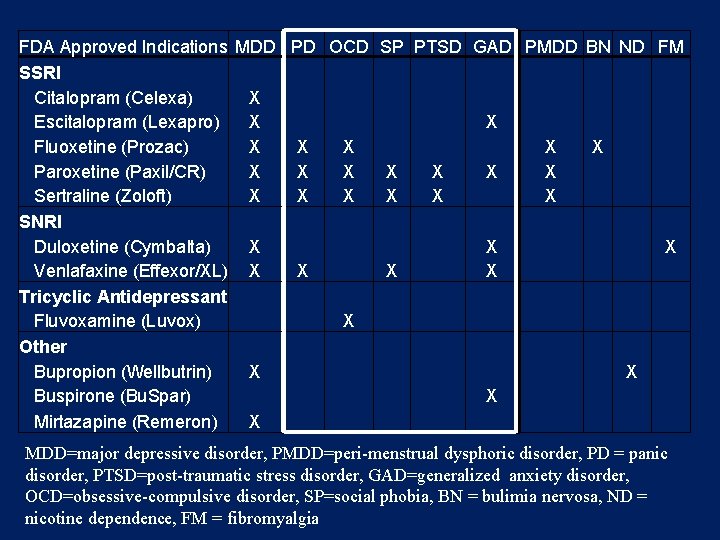
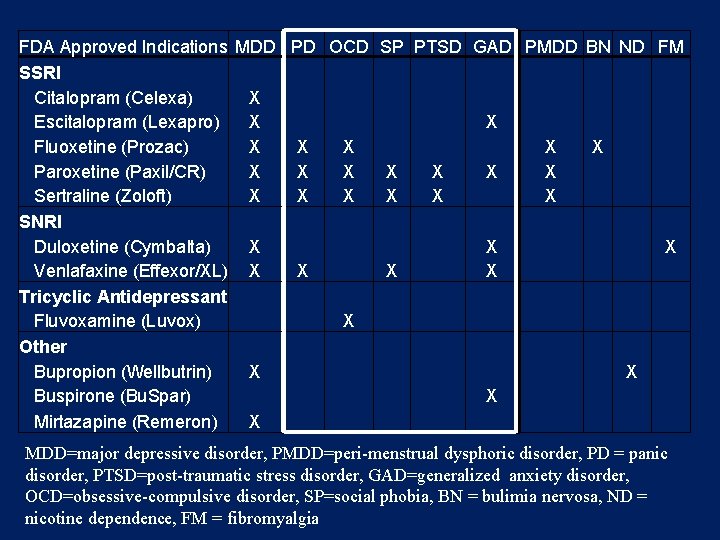
FDA Approved Indications MDD PD OCD SP PTSD GAD PMDD BN ND FM SSRI Citalopram (Celexa) X Escitalopram (Lexapro) X Fluoxetine (Prozac) X X X Paroxetine (Paxil/CR) X X X X Sertraline (Zoloft) X X X X SNRI Duloxetine (Cymbalta) X X Venlafaxine (Effexor/XL) X X X X Tricyclic Antidepressant Fluvoxamine (Luvox) X Other Bupropion (Wellbutrin) X X Buspirone (Bu. Spar) X Mirtazapine (Remeron) X MDD=major depressive disorder, PMDD=peri-menstrual dysphoric disorder, PD = panic disorder, PTSD=post-traumatic stress disorder, GAD=generalized anxiety disorder, OCD=obsessive-compulsive disorder, SP=social phobia, BN = bulimia nervosa, ND = nicotine dependence, FM = fibromyalgia
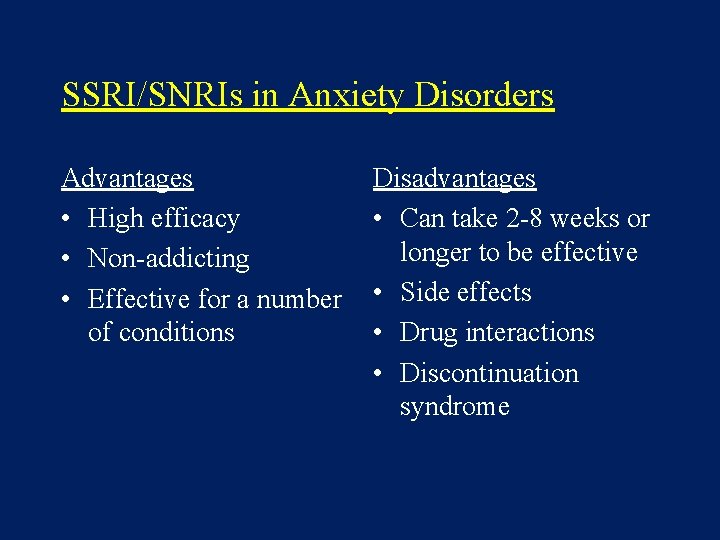
SSRI/SNRIs in Anxiety Disorders Advantages • High efficacy • Non-addicting • Effective for a number of conditions Disadvantages • Can take 2 -8 weeks or longer to be effective • Side effects • Drug interactions • Discontinuation syndrome
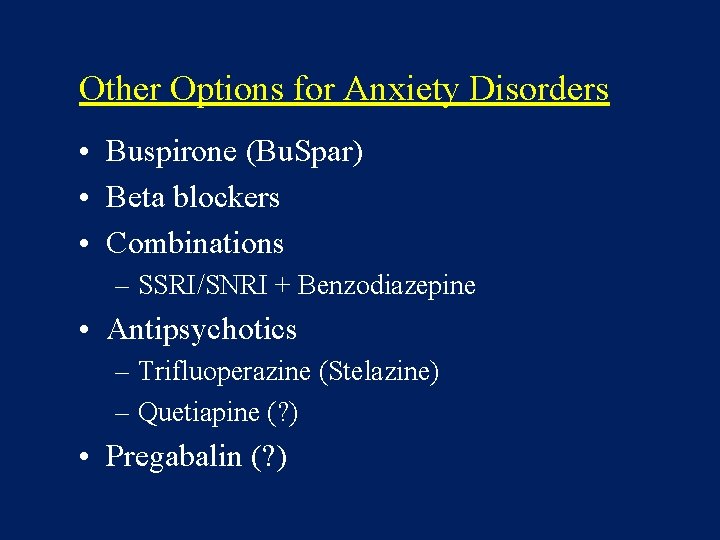
Other Options for Anxiety Disorders • Buspirone (Bu. Spar) • Beta blockers • Combinations – SSRI/SNRI + Benzodiazepine • Antipsychotics – Trifluoperazine (Stelazine) – Quetiapine (? ) • Pregabalin (? )
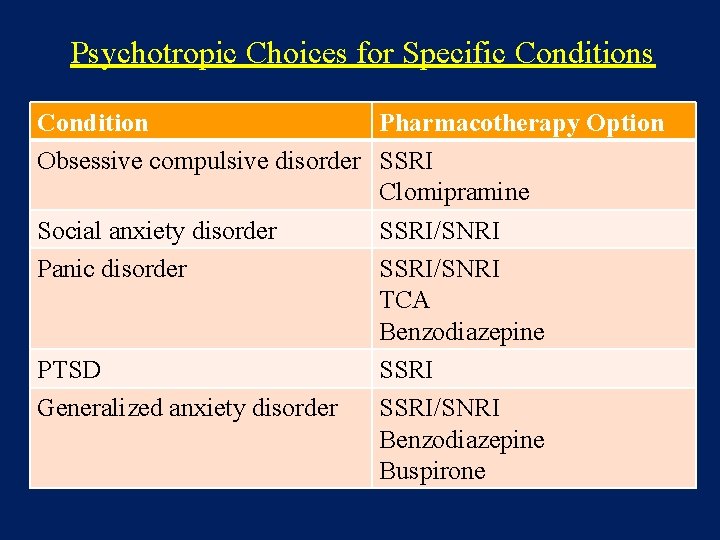
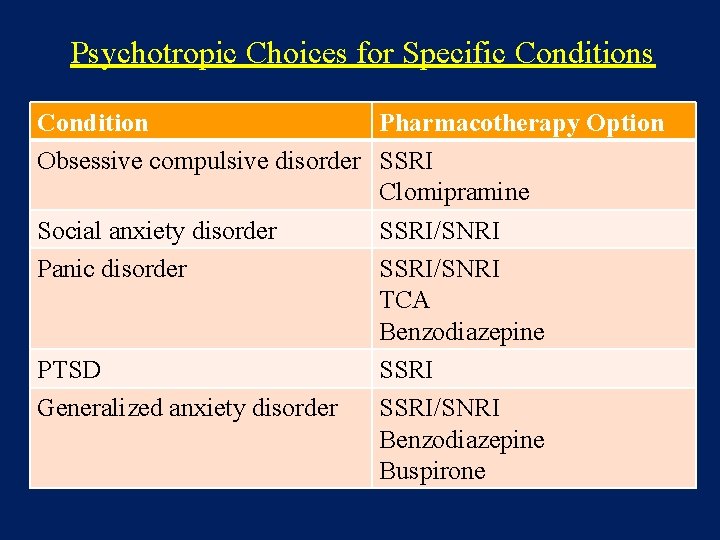
Psychotropic Choices for Specific Conditions Condition Pharmacotherapy Option Obsessive compulsive disorder SSRI Clomipramine Social anxiety disorder SSRI/SNRI Panic disorder SSRI/SNRI TCA Benzodiazepine PTSD SSRI Generalized anxiety disorder SSRI/SNRI Benzodiazepine Buspirone
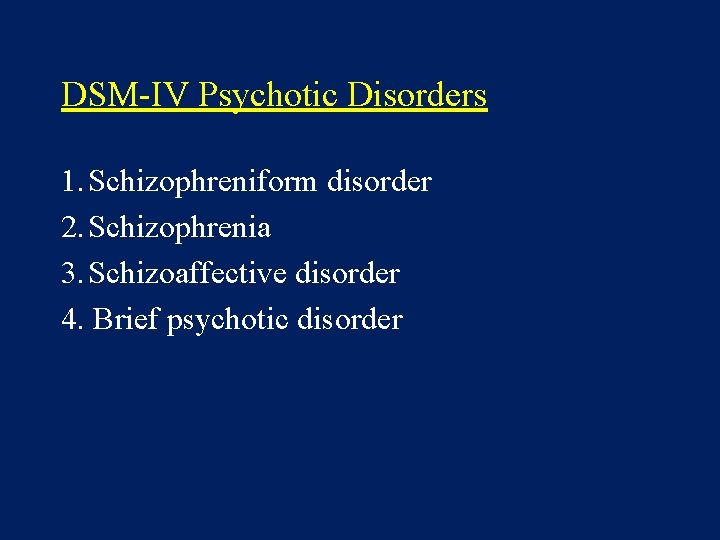
DSM-IV Psychotic Disorders 1. Schizophreniform disorder 2. Schizophrenia 3. Schizoaffective disorder 4. Brief psychotic disorder
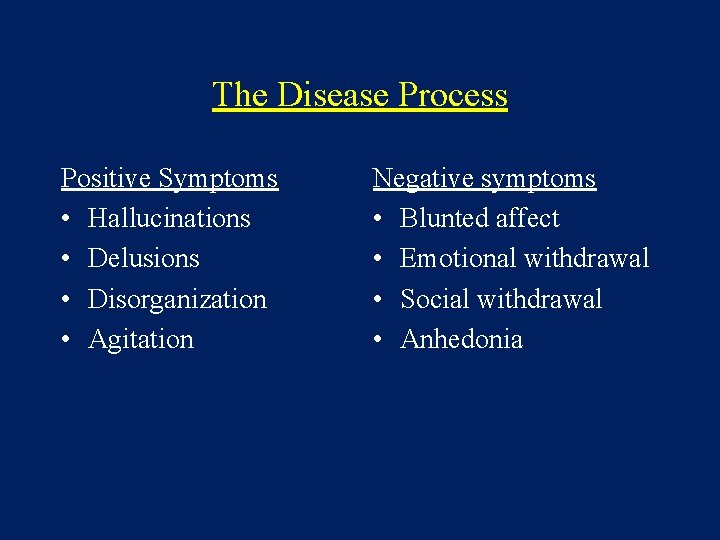
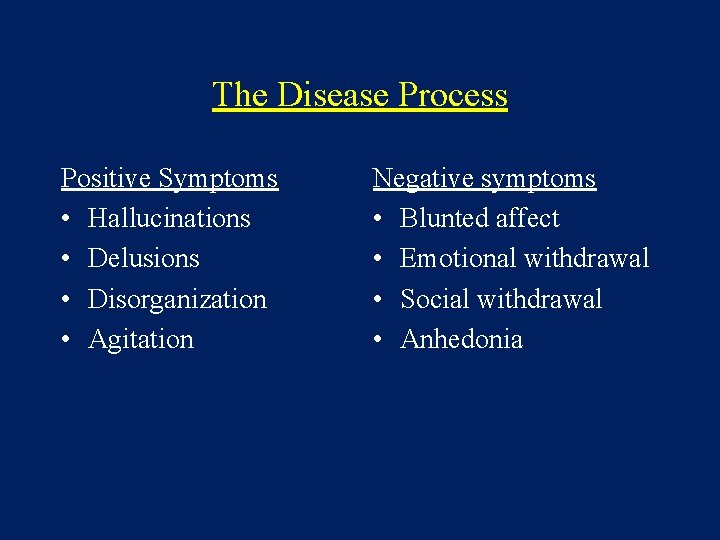
The Disease Process Positive Symptoms • Hallucinations • Delusions • Disorganization • Agitation Negative symptoms • Blunted affect • Emotional withdrawal • Social withdrawal • Anhedonia
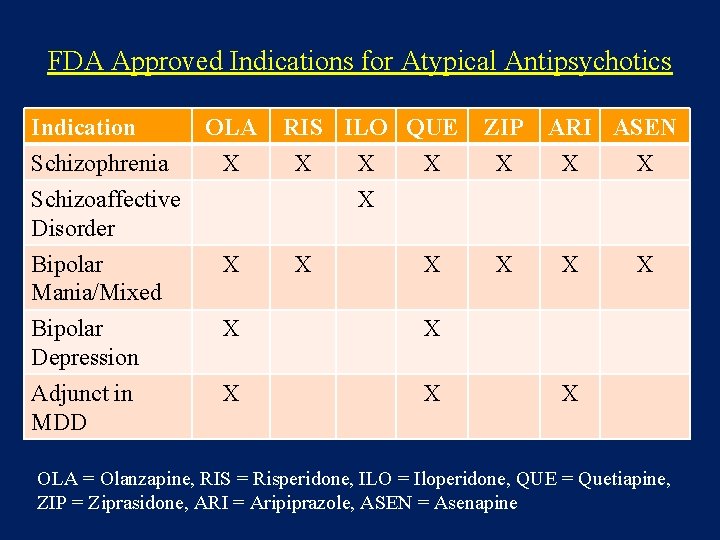
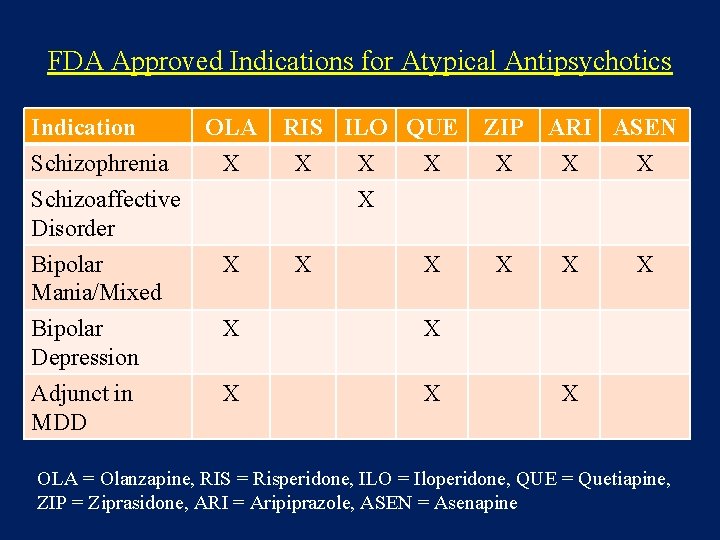
FDA Approved Indications for Atypical Antipsychotics Indication Schizophrenia Schizoaffective Disorder OLA X RIS ILO QUE X X Bipolar Mania/Mixed X X X Bipolar Depression X X Adjunct in MDD X X ZIP X X ARI ASEN X X X OLA = Olanzapine, RIS = Risperidone, ILO = Iloperidone, QUE = Quetiapine, ZIP = Ziprasidone, ARI = Aripiprazole, ASEN = Asenapine
Atypical (2 nd Generation) Antipsychotics HL=haloperidol (Haldol), CPZ=chlorpromazine (Thorazine), CLZ=clozapine (Clozaril), RIS=risperidone (Risperdal), OLZ=olanzapine (Zyprexa), QTP=quetiapine (Seroquel), ZIP=ziprasidone (Geodon) (Taken from: Jam, MW. Advances in the treatment of psychosis: a multidisciplinary continuing education program. Power-Pak CE, New York, NY 2001, p. 8. )
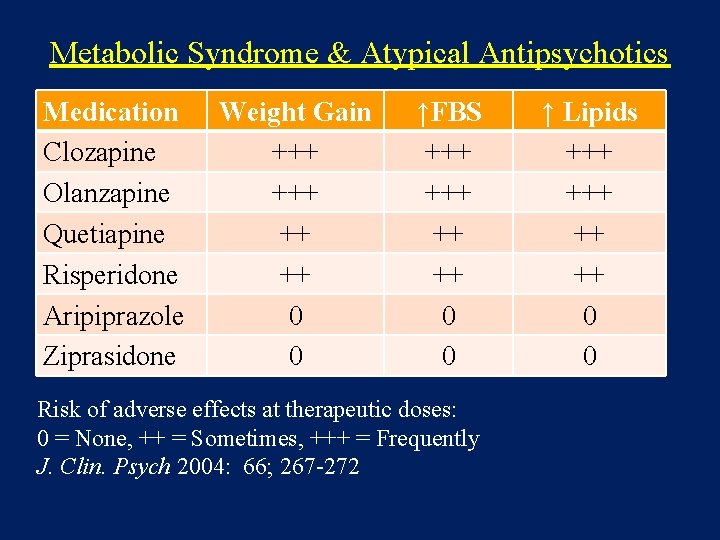
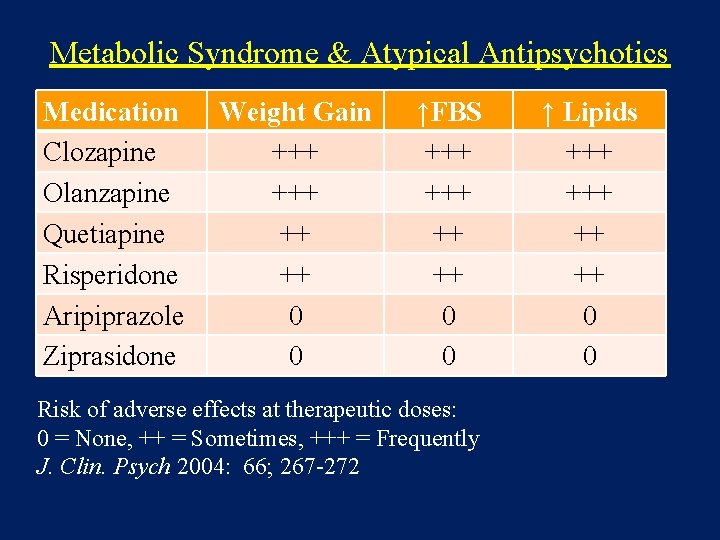
Metabolic Syndrome & Atypical Antipsychotics Medication Clozapine Olanzapine Quetiapine Risperidone Aripiprazole Ziprasidone Weight Gain +++ ++ ++ 0 0 ↑FBS +++ ++ ++ 0 0 Risk of adverse effects at therapeutic doses: 0 = None, ++ = Sometimes, +++ = Frequently J. Clin. Psych 2004: 66; 267 -272 ↑ Lipids +++ ++ ++ 0 0
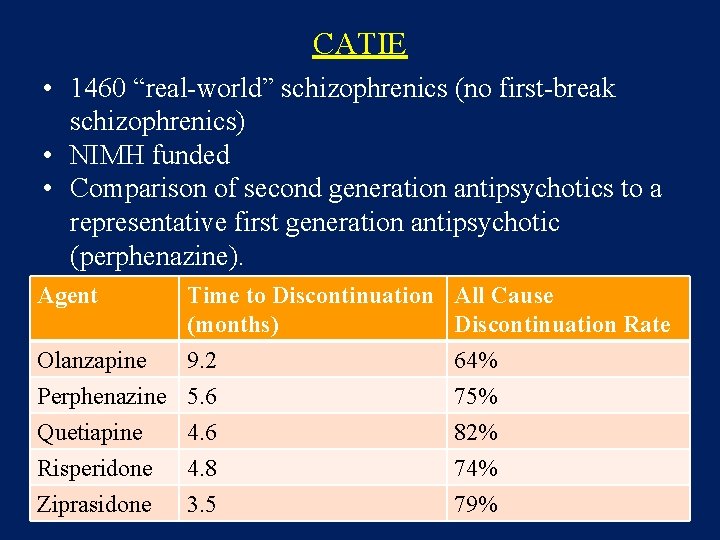
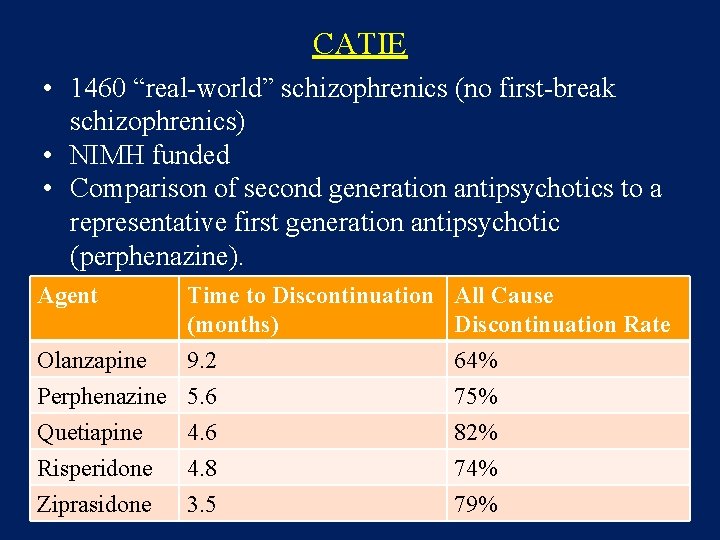
CATIE • 1460 “real-world” schizophrenics (no first-break schizophrenics) • NIMH funded • Comparison of second generation antipsychotics to a representative first generation antipsychotic (perphenazine). Agent Time to Discontinuation All Cause (months) Discontinuation Rate Olanzapine Perphenazine Quetiapine Risperidone Ziprasidone 9. 2 5. 6 4. 8 3. 5 64% 75% 82% 74% 79%
CATIE • Overall findings: – Discontinuation rates for all agents were high. – Olanzapine was the most efficacious medication, however, it was associated with the greatest weight gain, and the worst metabolic profiles. – For those patients changing drugs due to tolerability, olanzapine and risperidone were more efficacious second choice drugs. – Ziprasidone had a better metabolic profile.
DSM-IV Mood Disorders Bipolar disorder (manic-depressive disorder) · Bipolar I (recurrent major depression and mania) · Bipolar II (recurrent major depression with hypomania) · Specifiers q Rapid cycling (more than 4 episodes in a 12 month period) q Seasonal pattern Cyclothymia
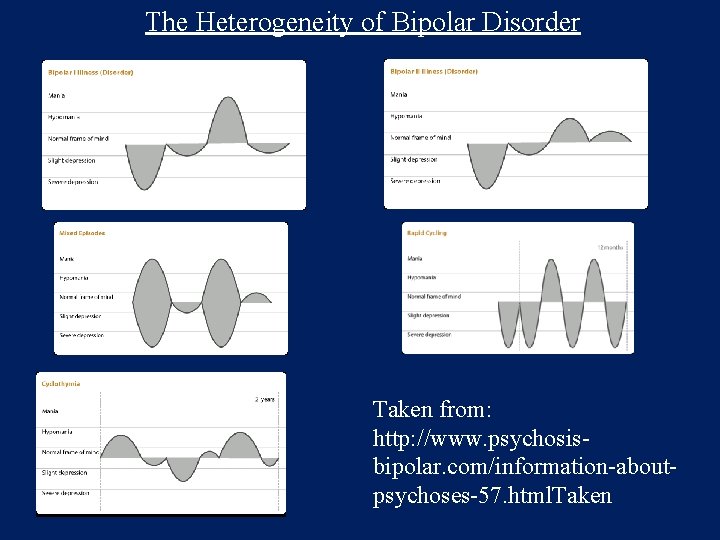
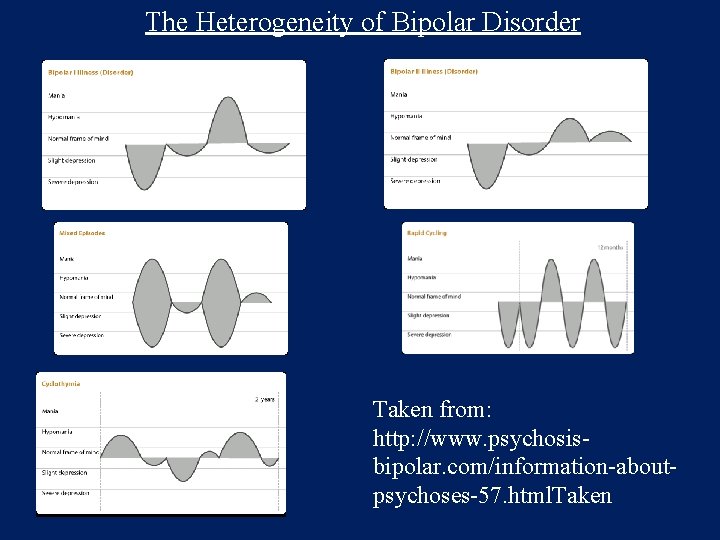
The Heterogeneity of Bipolar Disorder Taken from: http: //www. psychosisbipolar. com/information-aboutpsychoses-57. html. Taken
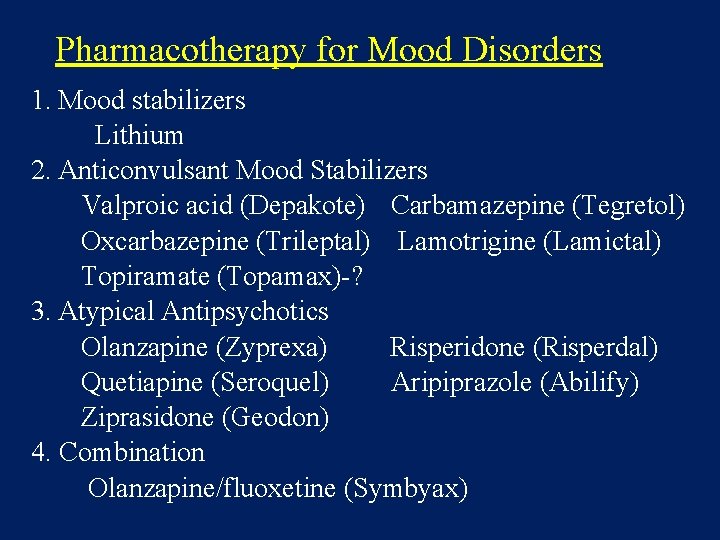
Pharmacotherapy for Mood Disorders 1. Mood stabilizers Lithium 2. Anticonvulsant Mood Stabilizers Valproic acid (Depakote) Carbamazepine (Tegretol) Oxcarbazepine (Trileptal) Lamotrigine (Lamictal) Topiramate (Topamax)-? 3. Atypical Antipsychotics Olanzapine (Zyprexa) Risperidone (Risperdal) Quetiapine (Seroquel) Aripiprazole (Abilify) Ziprasidone (Geodon) 4. Combination Olanzapine/fluoxetine (Symbyax)
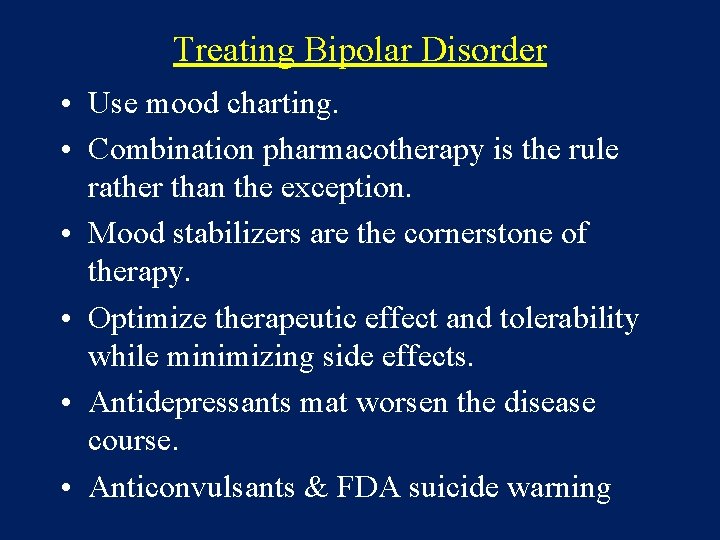
Treating Bipolar Disorder • Use mood charting. • Combination pharmacotherapy is the rule rather than the exception. • Mood stabilizers are the cornerstone of therapy. • Optimize therapeutic effect and tolerability while minimizing side effects. • Antidepressants mat worsen the disease course. • Anticonvulsants & FDA suicide warning
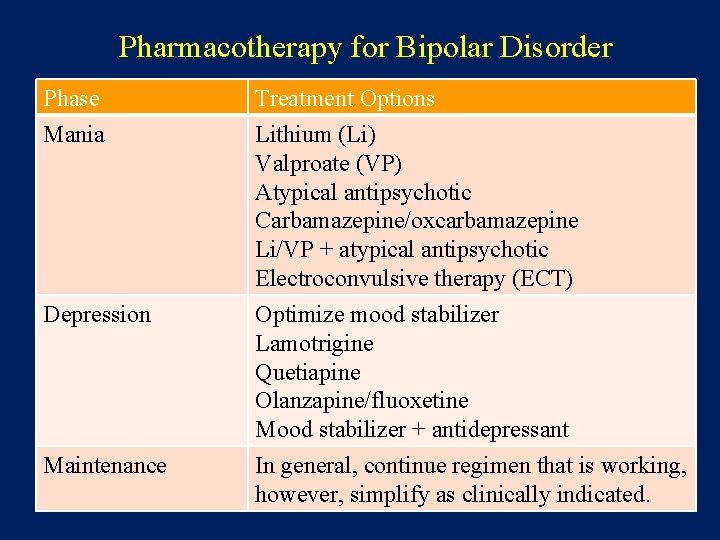
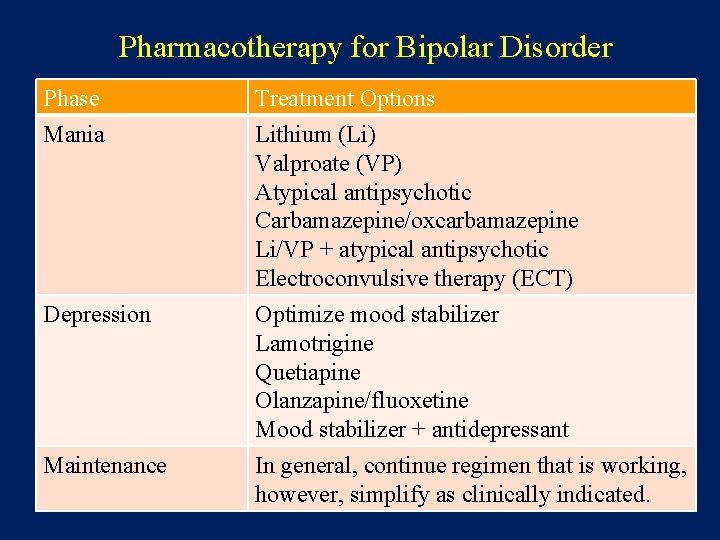
Pharmacotherapy for Bipolar Disorder Phase Mania Treatment Options Lithium (Li) Valproate (VP) Atypical antipsychotic Carbamazepine/oxcarbamazepine Li/VP + atypical antipsychotic Electroconvulsive therapy (ECT) Depression Optimize mood stabilizer Lamotrigine Quetiapine Olanzapine/fluoxetine Mood stabilizer + antidepressant Maintenance In general, continue regimen that is working, however, simplify as clinically indicated.
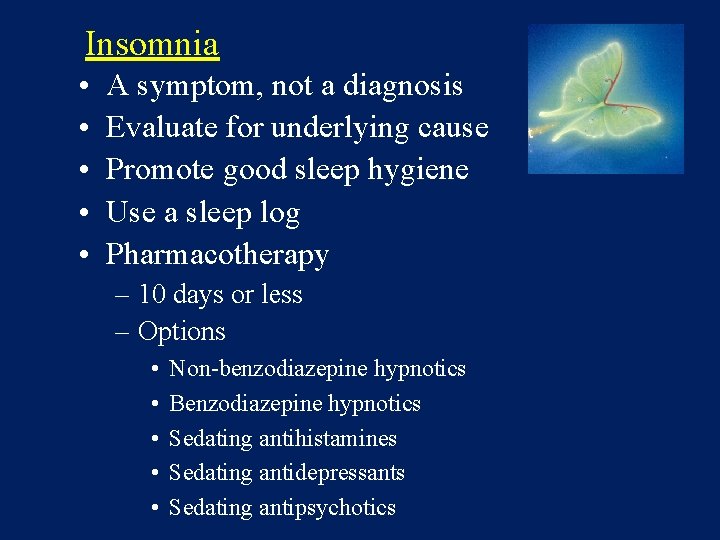
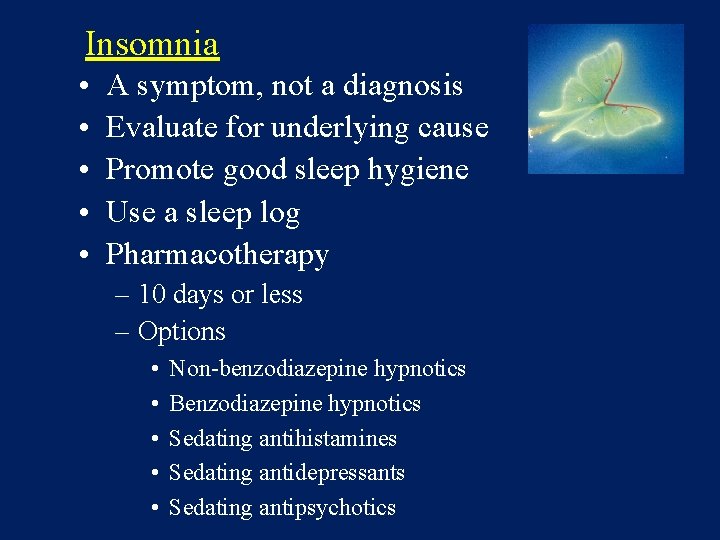
Insomnia • • • A symptom, not a diagnosis Evaluate for underlying cause Promote good sleep hygiene Use a sleep log Pharmacotherapy – 10 days or less – Options • • • Non-benzodiazepine hypnotics Benzodiazepine hypnotics Sedating antihistamines Sedating antidepressants Sedating antipsychotics
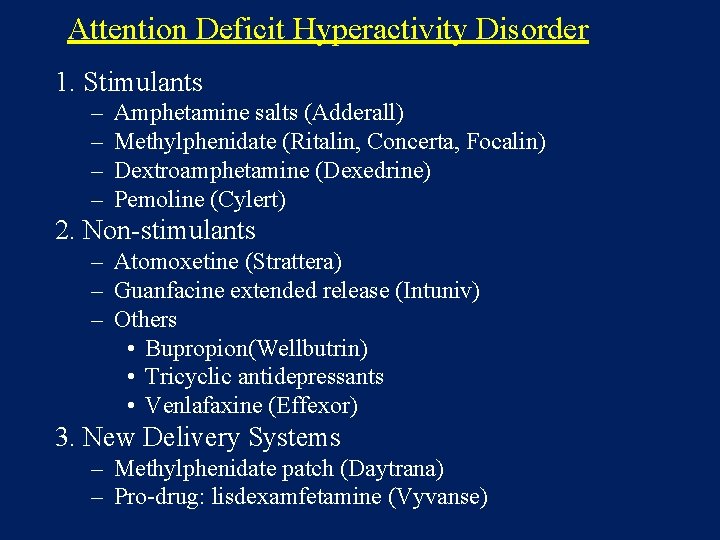
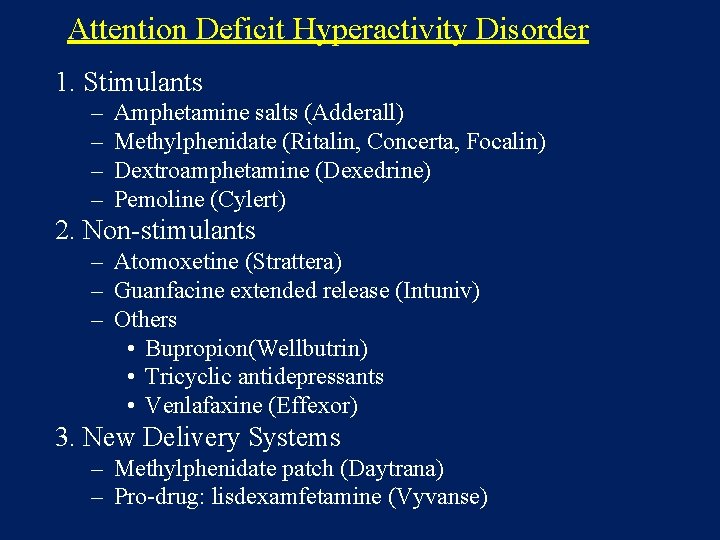
Attention Deficit Hyperactivity Disorder 1. Stimulants – – Amphetamine salts (Adderall) Methylphenidate (Ritalin, Concerta, Focalin) Dextroamphetamine (Dexedrine) Pemoline (Cylert) 2. Non-stimulants – Atomoxetine (Strattera) – Guanfacine extended release (Intuniv) – Others • Bupropion(Wellbutrin) • Tricyclic antidepressants • Venlafaxine (Effexor) 3. New Delivery Systems – Methylphenidate patch (Daytrana) – Pro-drug: lisdexamfetamine (Vyvanse)
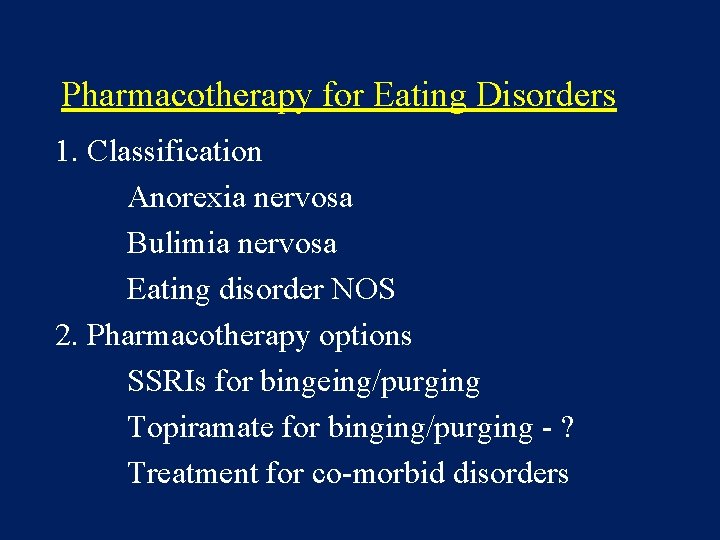
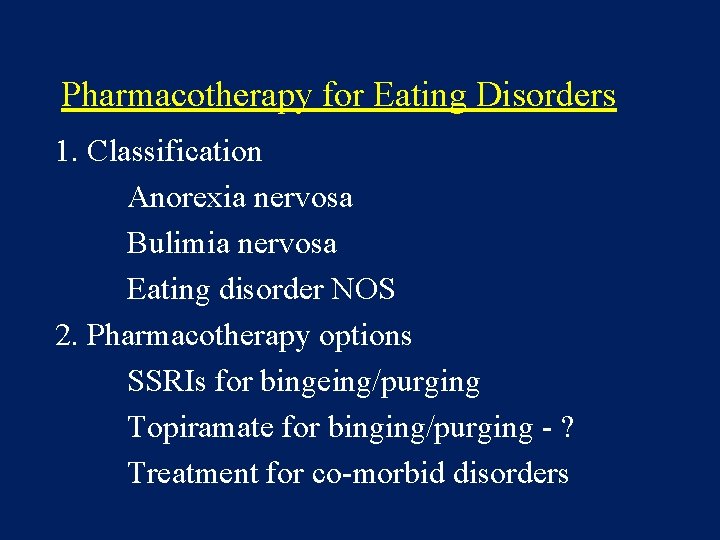
Pharmacotherapy for Eating Disorders 1. Classification Anorexia nervosa Bulimia nervosa Eating disorder NOS 2. Pharmacotherapy options SSRIs for bingeing/purging Topiramate for binging/purging - ? Treatment for co-morbid disorders
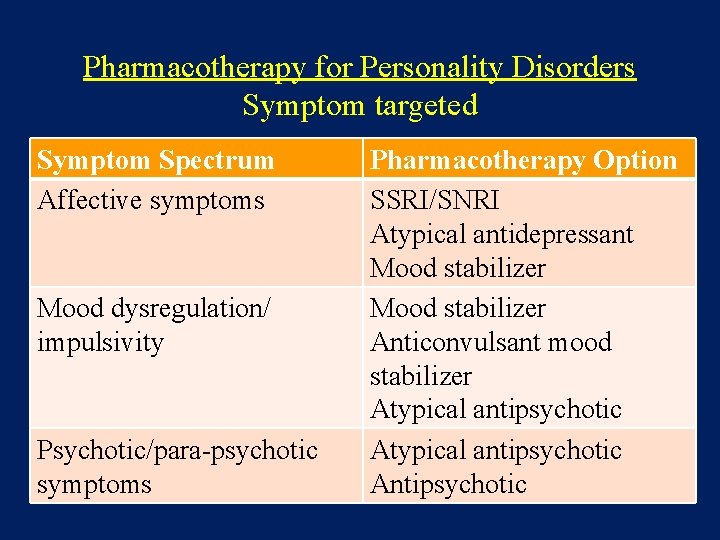
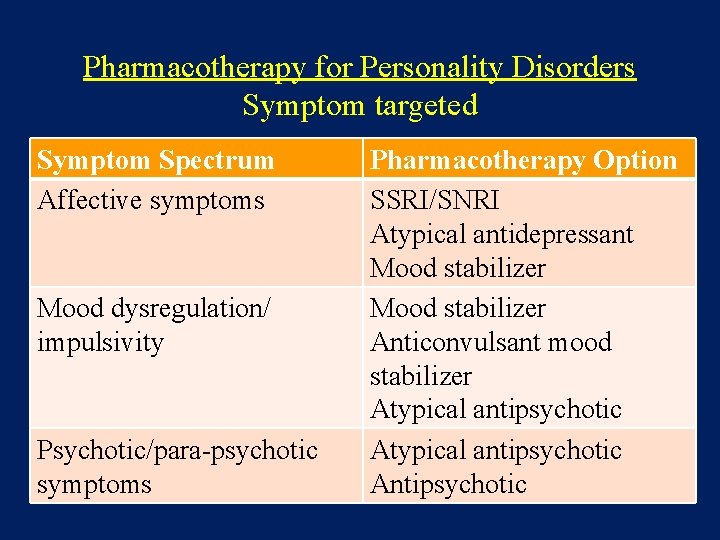
Pharmacotherapy for Personality Disorders Symptom targeted Symptom Spectrum Affective symptoms Mood dysregulation/ impulsivity Psychotic/para-psychotic symptoms Pharmacotherapy Option SSRI/SNRI Atypical antidepressant Mood stabilizer Anticonvulsant mood stabilizer Atypical antipsychotic Antipsychotic
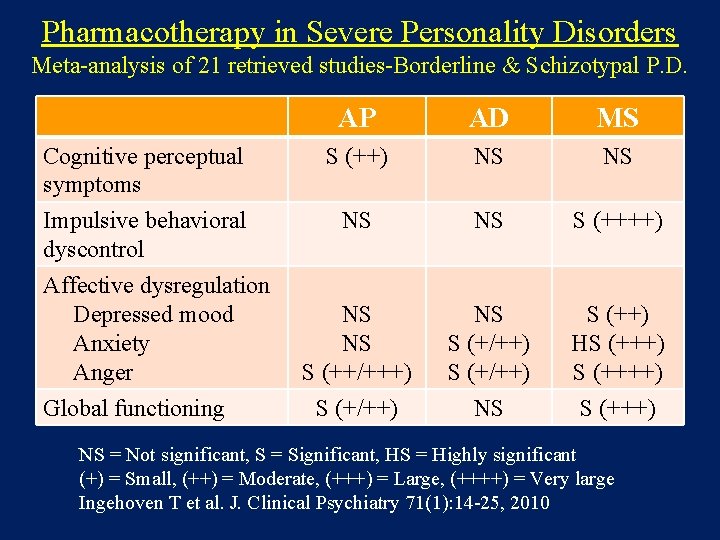
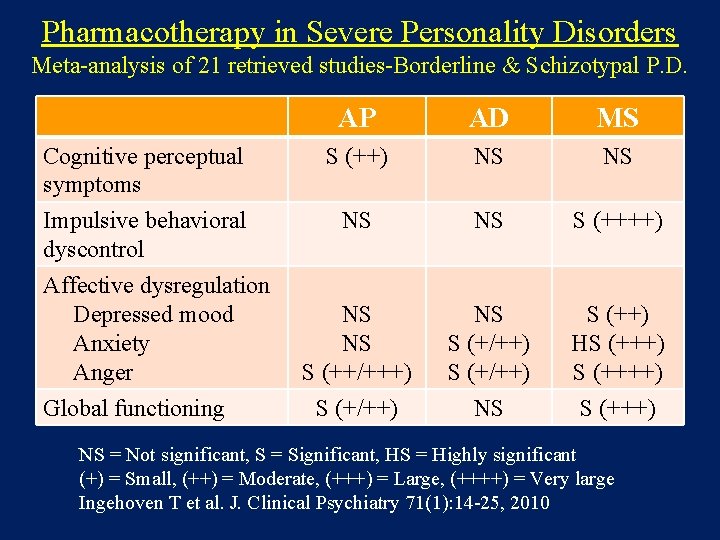
Pharmacotherapy in Severe Personality Disorders Meta-analysis of 21 retrieved studies-Borderline & Schizotypal P. D. AP AD MS Cognitive perceptual symptoms S (++) NS NS Impulsive behavioral dyscontrol NS NS S (++++) NS NS S (++/+++) S (+/++) NS S (++) HS (+++) Affective dysregulation Depressed mood Anxiety Anger Global functioning NS = Not significant, S = Significant, HS = Highly significant (+) = Small, (++) = Moderate, (+++) = Large, (++++) = Very large Ingehoven T et al. J. Clinical Psychiatry 71(1): 14 -25, 2010
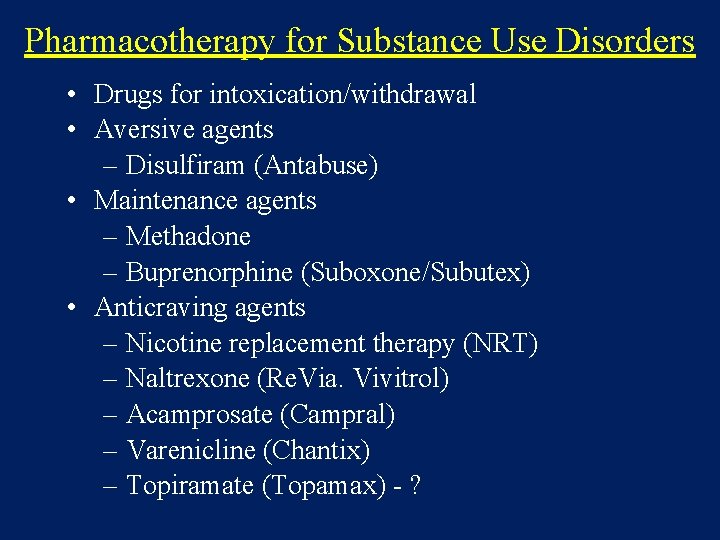
Pharmacotherapy for Substance Use Disorders • Drugs for intoxication/withdrawal • Aversive agents – Disulfiram (Antabuse) • Maintenance agents – Methadone – Buprenorphine (Suboxone/Subutex) • Anticraving agents – Nicotine replacement therapy (NRT) – Naltrexone (Re. Via. Vivitrol) – Acamprosate (Campral) – Varenicline (Chantix) – Topiramate (Topamax) - ?

 Ms program in clinical psychopharmacology
Ms program in clinical psychopharmacology Deferred update and immediate update
Deferred update and immediate update Nei master psychopharmacology
Nei master psychopharmacology Cosmetic psychopharmacology
Cosmetic psychopharmacology Cosmetic psychopharmacology
Cosmetic psychopharmacology Biological basis for understanding psychopharmacology
Biological basis for understanding psychopharmacology Maria felicia de jesús sacramentado maría teresa arminda
Maria felicia de jesús sacramentado maría teresa arminda Peter de maria
Peter de maria [email protected]
[email protected] Fidelity quarterly market update q1 2018
Fidelity quarterly market update q1 2018 Kb2533623
Kb2533623 Deferred update
Deferred update Project status examples
Project status examples Apollo gx55 database update
Apollo gx55 database update Data redundancy and update anomalies
Data redundancy and update anomalies Www sab update
Www sab update Stfms
Stfms Modul komitmen sakti
Modul komitmen sakti Mentor update yorkshire
Mentor update yorkshire Location update procedure
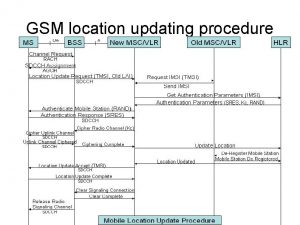
Location update procedure Leslie intervention update
Leslie intervention update Microsoft security essential tidak bisa update
Microsoft security essential tidak bisa update Position update formula
Position update formula Flash player update
Flash player update Noc update
Noc update Windows update herstellen
Windows update herstellen Chocolate uncountable
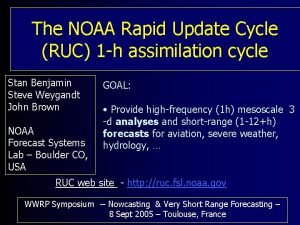
Chocolate uncountable Rapid update cycle
Rapid update cycle Zechariah 4:8
Zechariah 4:8 Unity connection to the update server failed
Unity connection to the update server failed Microsoft update
Microsoft update Food product knowledge training
Food product knowledge training Update debrecen
Update debrecen Oracle release management
Oracle release management Sudo dpkg-reconfigure slapd
Sudo dpkg-reconfigure slapd Nwcg iqcs
Nwcg iqcs Apache server
Apache server Covid update today
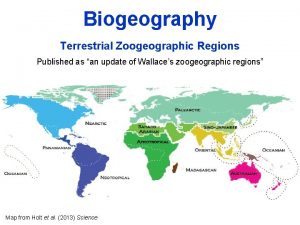
Covid update today An update of wallace’s zoogeographic regions of the world
An update of wallace’s zoogeographic regions of the world Aplikasi siha offline
Aplikasi siha offline Raksha tpa query reply
Raksha tpa query reply Microsoft update
Microsoft update Recovery techniques based on immediate update
Recovery techniques based on immediate update Routing area update
Routing area update Language windows 10
Language windows 10 Microsoft update
Microsoft update Injector update
Injector update Chrome update
Chrome update Application screen update false
Application screen update false Swhp coverage update center
Swhp coverage update center Firmware fiberhome
Firmware fiberhome Publishing swansea
Publishing swansea Mike intervention update
Mike intervention update