TRAUMA AND EMERGENCY IN OPHTHALMOLOGY Prof Dr Raciha












- Slides: 47
TRAUMA AND EMERGENCY IN OPHTHALMOLOGY Prof. Dr. Raciha Beril Küçümen 2016 -2017 Educational Year
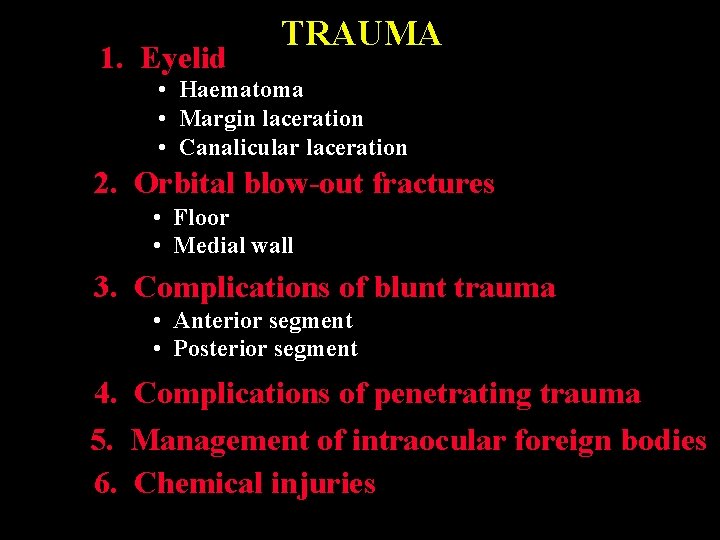
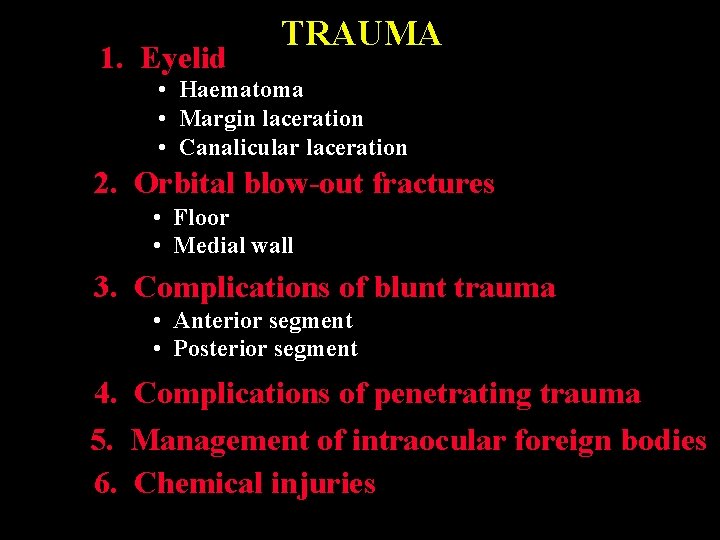
1. Eyelid TRAUMA • Haematoma • Margin laceration • Canalicular laceration 2. Orbital blow-out fractures • Floor • Medial wall 3. Complications of blunt trauma • Anterior segment • Posterior segment 4. Complications of penetrating trauma 5. Management of intraocular foreign bodies 6. Chemical injuries
How to examine History : type of traumatic event, time of onset, nature of symptoms Time, place and type of injury Patients’ history of eye conditions, drug allergies and tetanus immunization Pearl: don’t delay prompt treatment for a detailed hx in an obvious injury (eg. Chemical burn) Visual Acuity Testing
How to examine External examination Palpation: orbital rims in blunt injury? Penlight inspection: signs of perforation, depth of AC, uveal prolapsus, hyphema Lid eversion: foreign body, chemical burn – Pearl: don’t manipulate eyelids in injury of the globe ? Fluorescein staining: foreign body sensation, hx of blunt or sharp injury. Topical anesthesia: relieve discomfort • Pearl: Don’t prescribe! Prolonged use can result in corneal ulceration and inadvertant injury Pupillary reactions: optic nerve injury Ocular motility testing: • Restricted in orbital hematoma. • Vertical restriction in blowout fracture. • Limitation of eye movements, bruit, proptosis: carotid-cavernous fistula
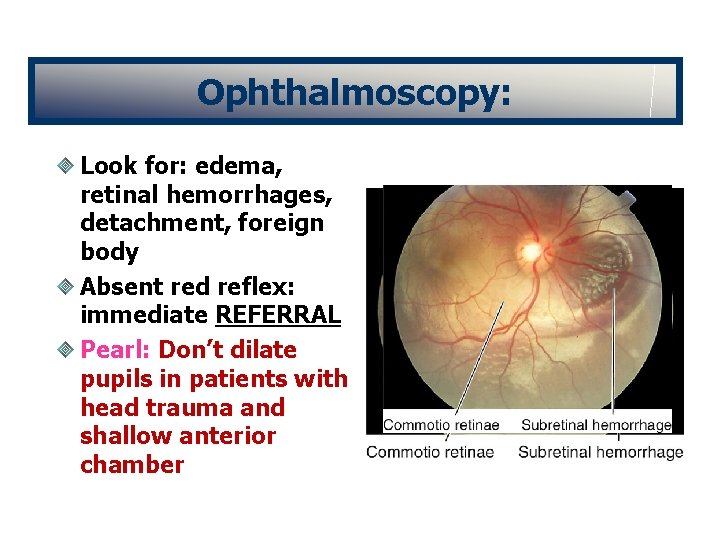
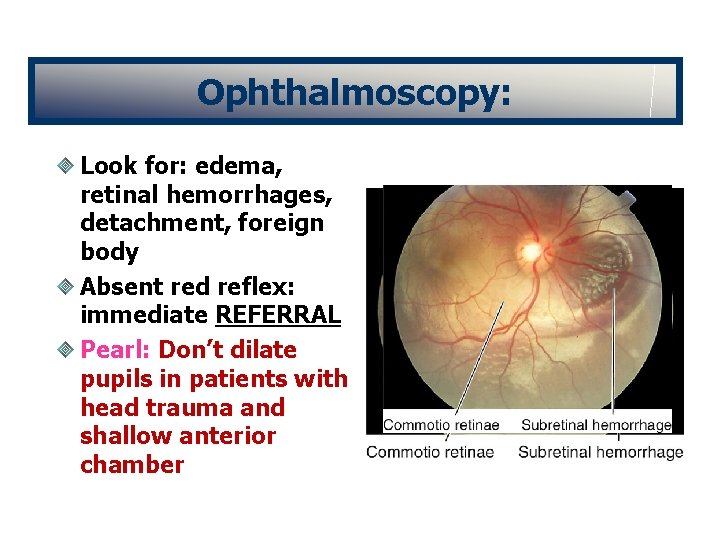
Ophthalmoscopy: Look for: edema, retinal hemorrhages, detachment, foreign body Absent red reflex: immediate REFERRAL Pearl: Don’t dilate pupils in patients with head trauma and shallow anterior chamber
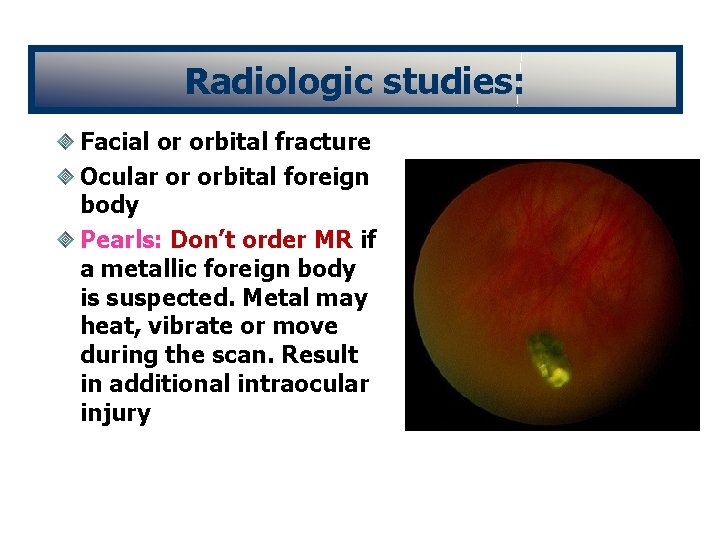
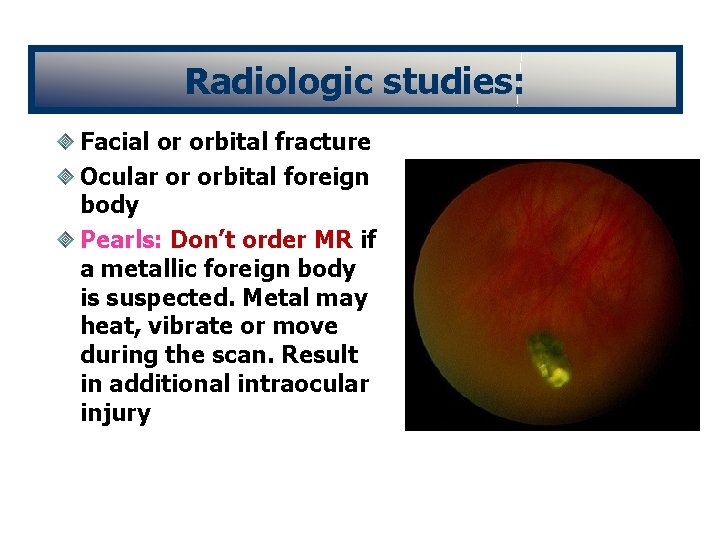
Radiologic studies: Facial or orbital fracture Ocular or orbital foreign body Pearls: Don’t order MR if a metallic foreign body is suspected. Metal may heat, vibrate or move during the scan. Result in additional intraocular injury
Definitions and Classification in Ocular Trauma Eyewall: sclera and cornea Closed globe injury: no full thickness wound of eyewall Open globe injury: full thickness wound of eyewall Contusion: no wound, injury results from changes in the shape of the globe (eg. Angle recession) Lamellar laceration: partial-thickness wound Rupture: full-thickness wound of the eyewall caused by a blunt object Laceration: full-thickness wound of the eyewall caused by a sharp object Penetrating injury: entrance wound Perforating injury: entrance and exit wounds
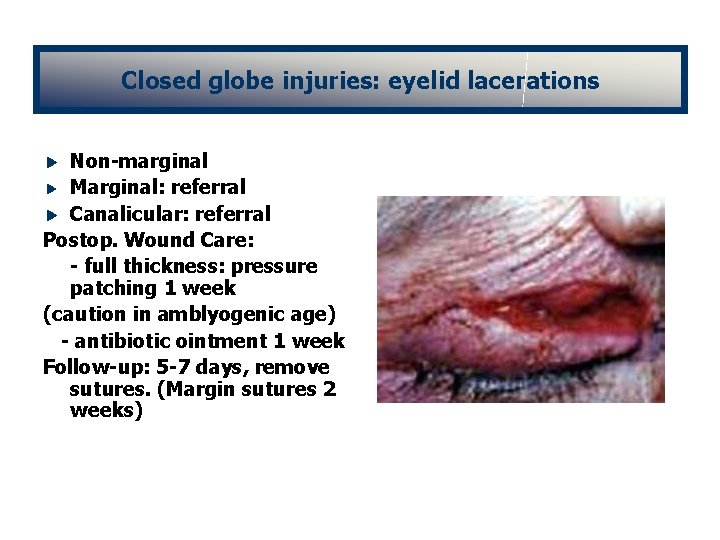
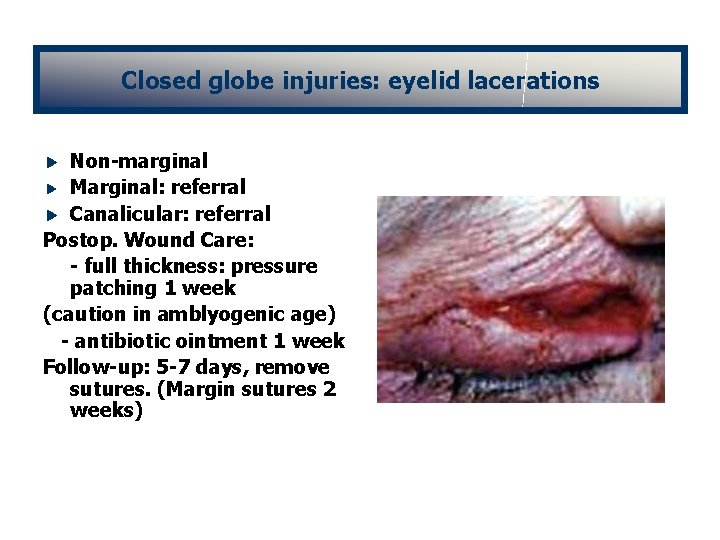
Closed globe injuries: eyelid lacerations Non-marginal Marginal: referral Canalicular: referral Postop. Wound Care: - full thickness: pressure patching 1 week (caution in amblyogenic age) - antibiotic ointment 1 week Follow-up: 5 -7 days, remove sutures. (Margin sutures 2 weeks)

Lid margin laceration Carefully align to prevent notching Align with 6 -0 black silk suture Close tarsal plate with fine absorbable suture Place additional marginal silk sutures Close skin with multiple interrupted 6 -0 black silk sutures
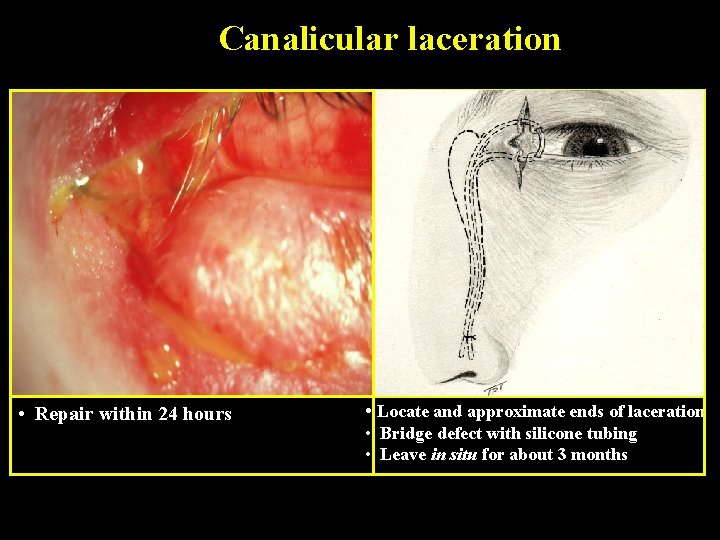
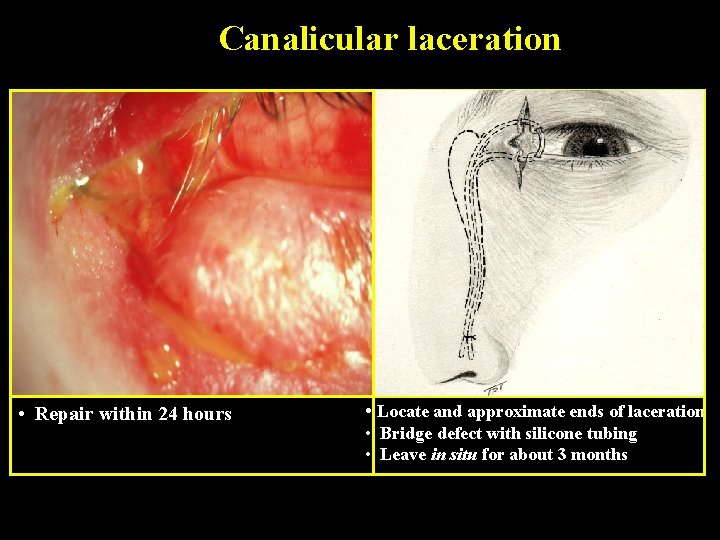
Canalicular laceration • Repair within 24 hours • Locate and approximate ends of laceration • Bridge defect with silicone tubing • Leave in situ for about 3 months
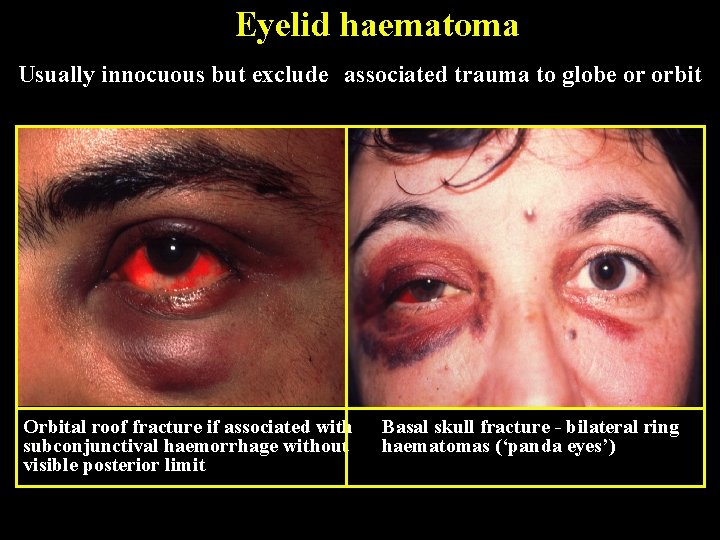
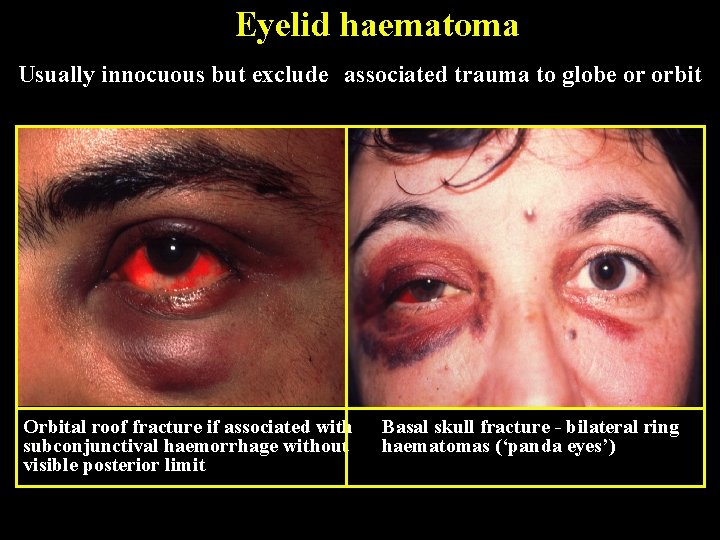
Eyelid haematoma Usually innocuous but exclude associated trauma to globe or orbit Orbital roof fracture if associated with subconjunctival haemorrhage without visible posterior limit Basal skull fracture - bilateral ring haematomas (‘panda eyes’)
Closed globe injuries: orbital trauma Orbital blowout fractures Traumatic optic neuropathy Orbital hemorrhage and compartment syndrome Mild-moderate IOP elevations: glaucoma medications and observation Severe: lateral canthotomy and cantolysis surgical decompression
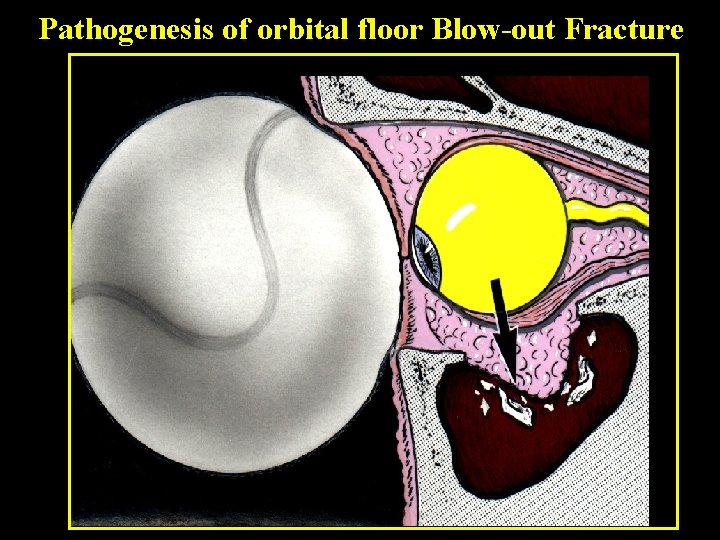
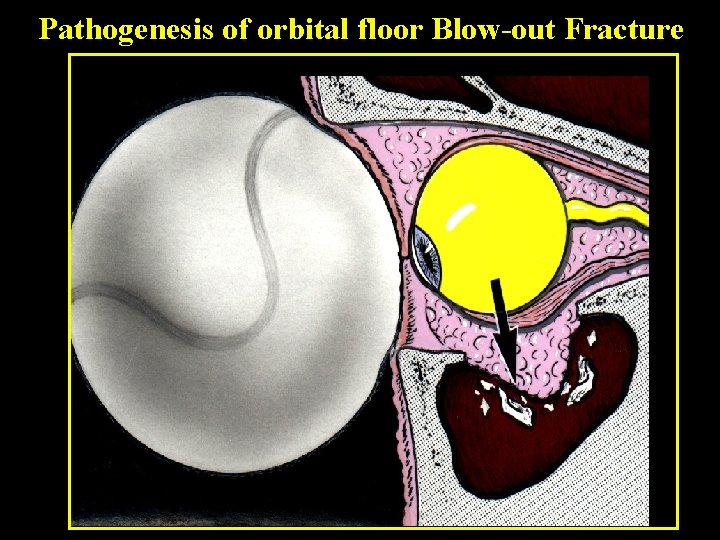
Pathogenesis of orbital floor Blow-out Fracture
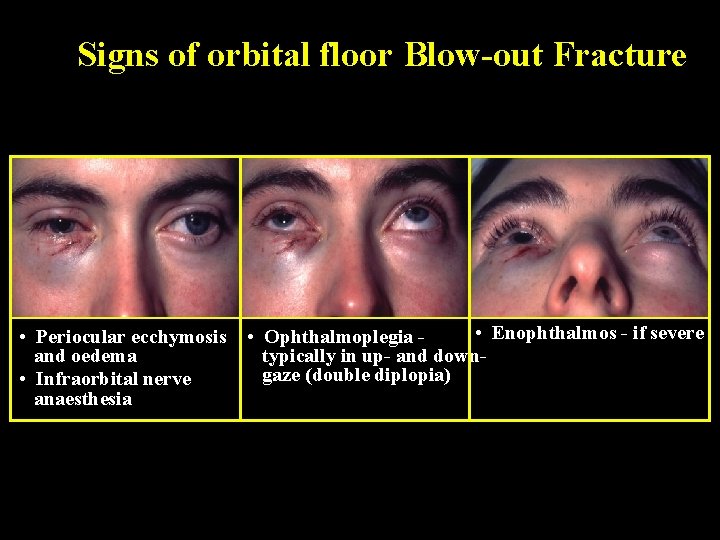
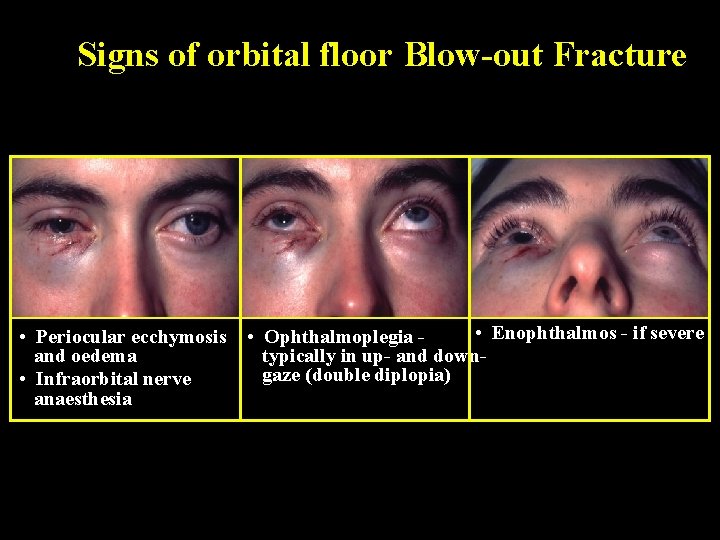
Signs of orbital floor Blow-out Fracture • Periocular ecchymosis and oedema • Infraorbital nerve anaesthesia • Enophthalmos - if severe • Ophthalmoplegia typically in up- and downgaze (double diplopia)
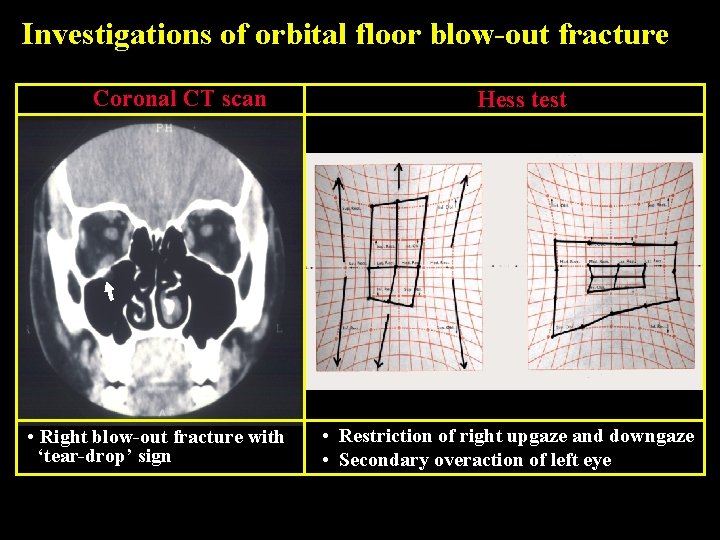
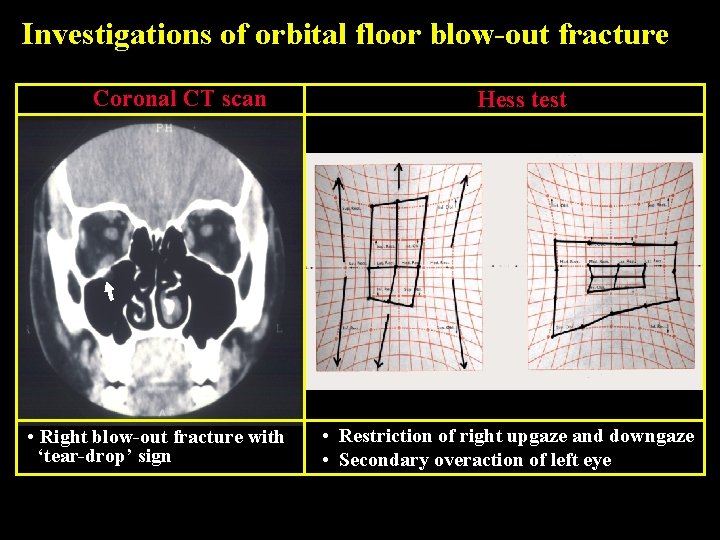
Investigations of orbital floor blow-out fracture Coronal CT scan • Right blow-out fracture with ‘tear-drop’ sign Hess test • Restriction of right upgaze and downgaze • Secondary overaction of left eye
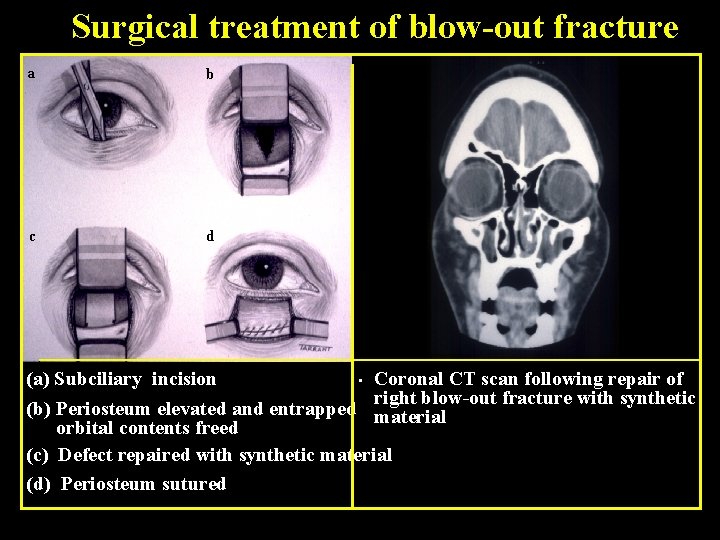
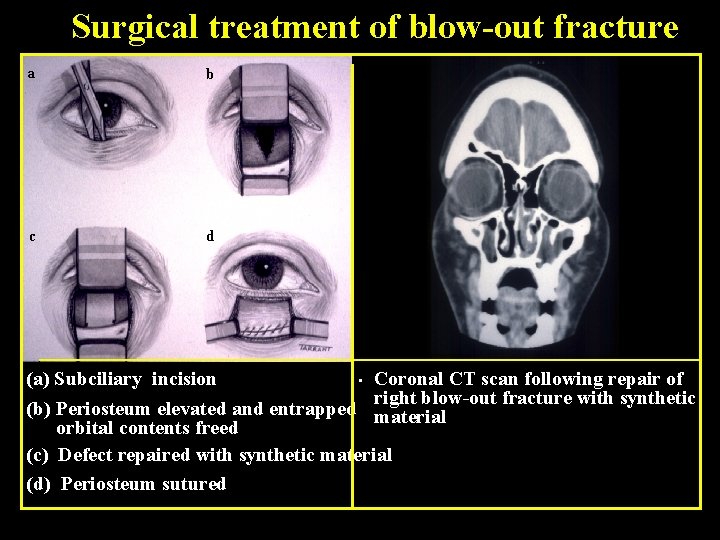
Surgical treatment of blow-out fracture a b c d (a) Subciliary incision • Coronal CT scan following repair of right blow-out fracture with synthetic (b) Periosteum elevated and entrapped material orbital contents freed (c) Defect repaired with synthetic material (d) Periosteum sutured
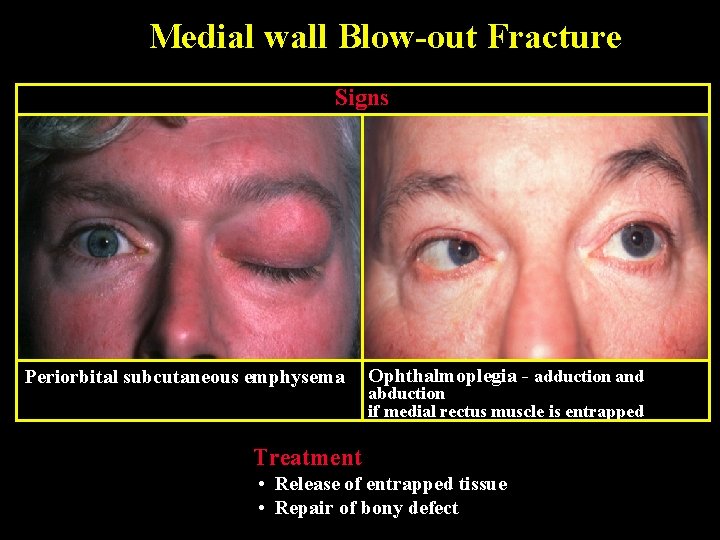
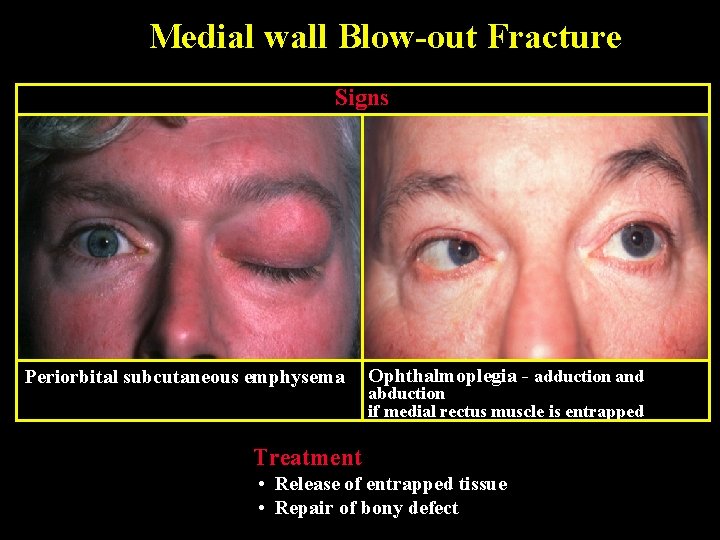
Medial wall Blow-out Fracture Signs Periorbital subcutaneous emphysema Ophthalmoplegia - adduction and abduction if medial rectus muscle is entrapped Treatment • Release of entrapped tissue • Repair of bony defect
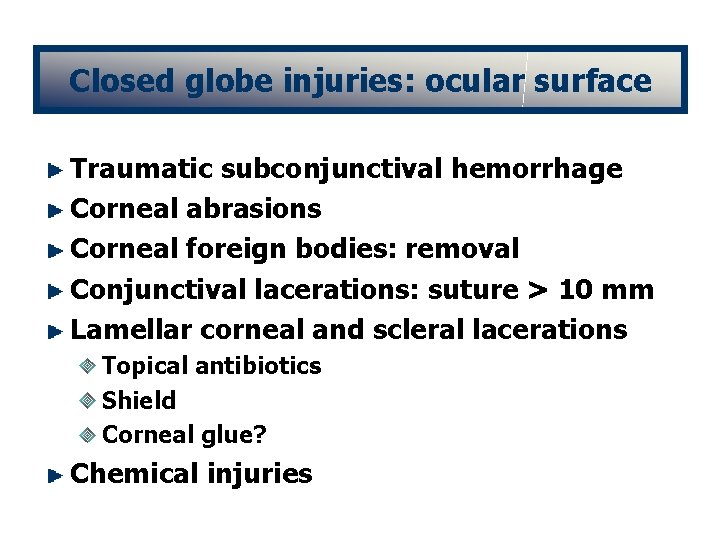
Closed globe injuries: ocular surface Traumatic subconjunctival hemorrhage Corneal abrasions Corneal foreign bodies: removal Conjunctival lacerations: suture > 10 mm Lamellar corneal and scleral lacerations Topical antibiotics Shield Corneal glue? Chemical injuries
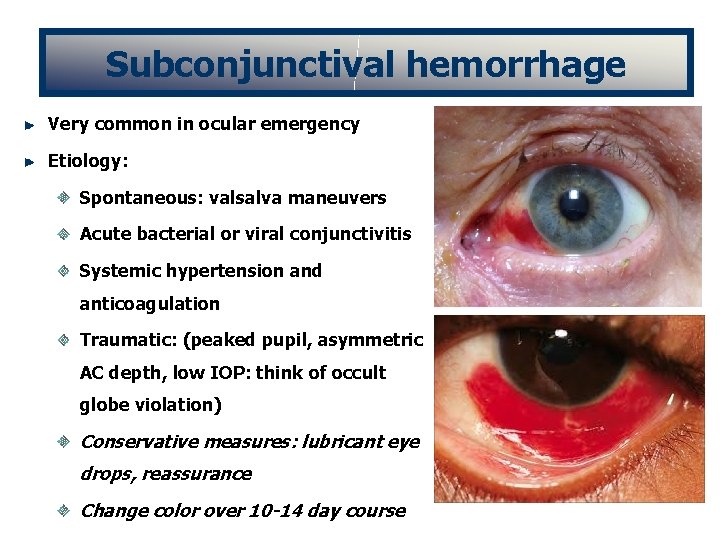
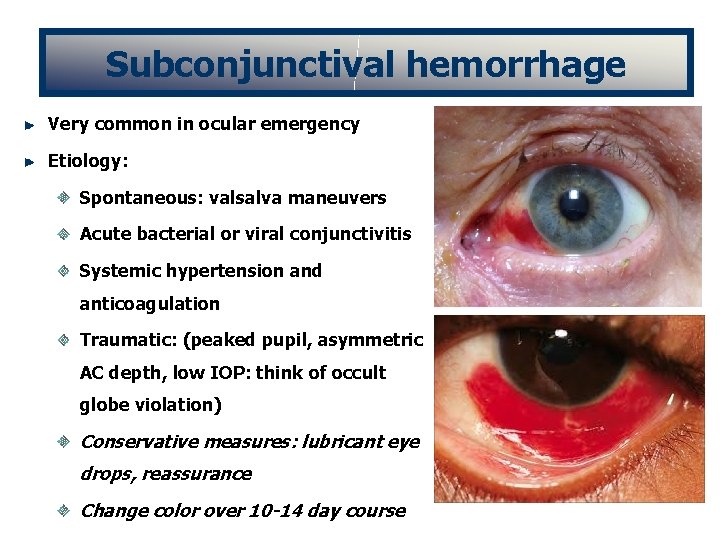
Subconjunctival hemorrhage Very common in ocular emergency Etiology: Spontaneous: valsalva maneuvers Acute bacterial or viral conjunctivitis Systemic hypertension and anticoagulation Traumatic: (peaked pupil, asymmetric AC depth, low IOP: think of occult globe violation) Conservative measures: lubricant eye drops, reassurance Change color over 10 -14 day course


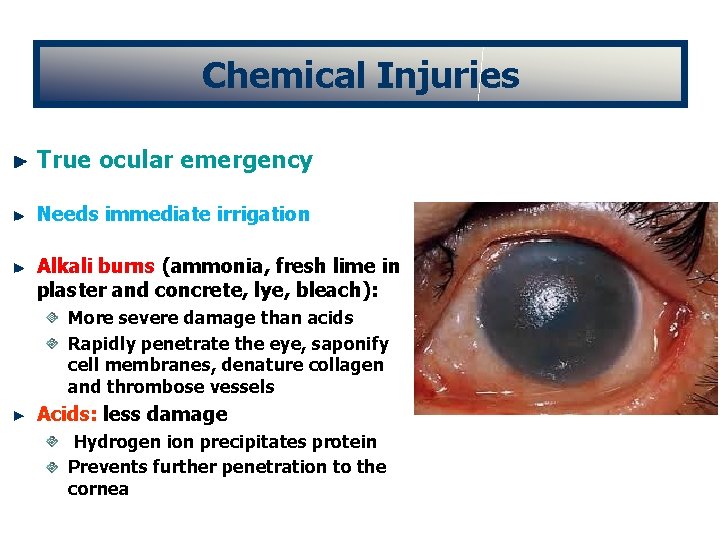
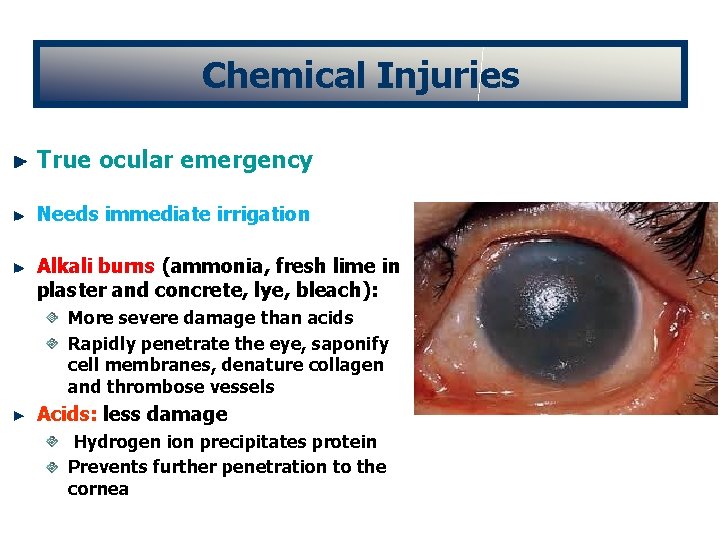
Chemical Injuries True ocular emergency Needs immediate irrigation Alkali burns (ammonia, fresh lime in plaster and concrete, lye, bleach): More severe damage than acids Rapidly penetrate the eye, saponify cell membranes, denature collagen and thrombose vessels Acids: less damage Hydrogen ion precipitates protein Prevents further penetration to the cornea
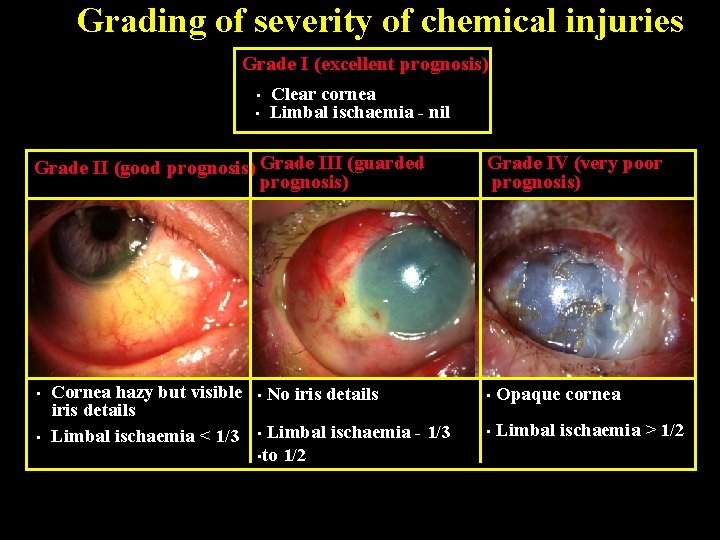
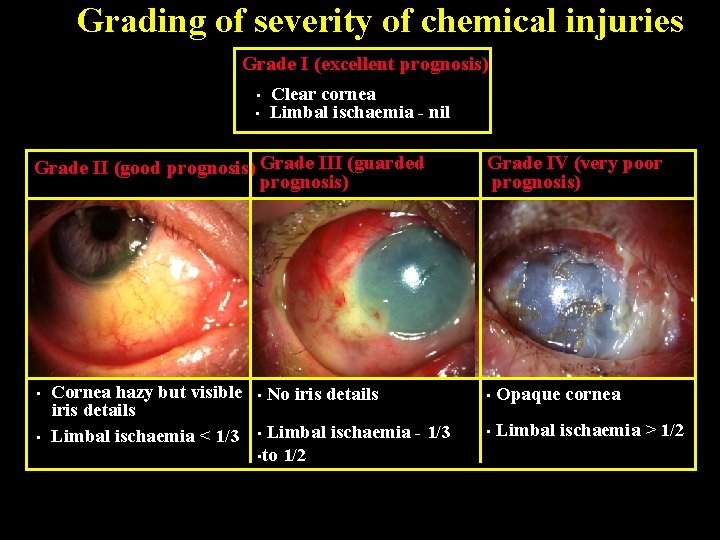
Grading of severity of chemical injuries Grade I (excellent prognosis) • • Clear cornea Limbal ischaemia - nil Grade II (good prognosis) Grade III (guarded prognosis) • • Cornea hazy but visible iris details Limbal ischaemia < 1/3 • No iris details Limbal ischaemia - 1/3 • to 1/2 • Grade IV (very poor prognosis) • Opaque cornea • Limbal ischaemia > 1/2

Medical Treatment of Severe Injuries 1. Copious irrigation ( 15 -30 min ) - to restore normal p. H 2. Topical steroids ( first 7 -10 days ) - to reduce inflammation 3. Topical and systemic ascorbic acid - to enhance collagen production 4. Topical citric acid - to inhibit neutrophil activity 5. Topical and systemic tetracycline - to inhibit collagenase and neutrophil activity
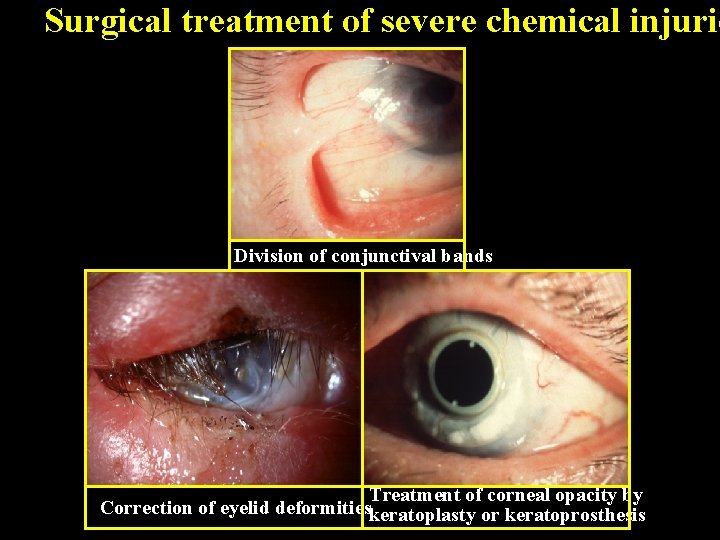
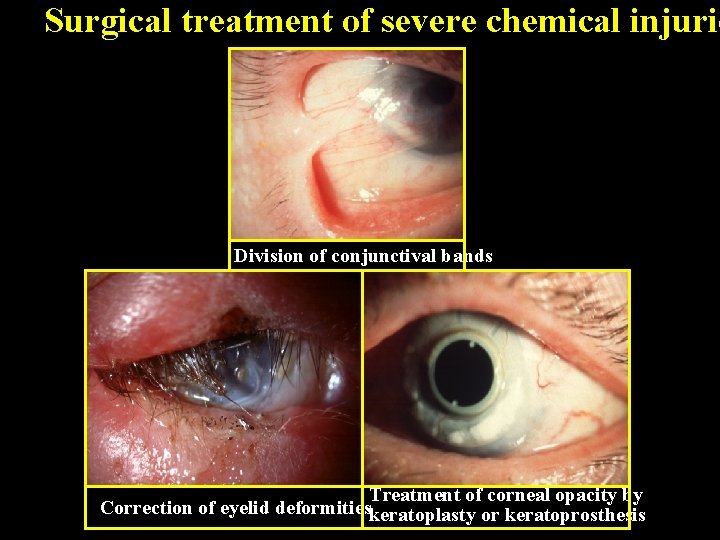
Surgical treatment of severe chemical injurie Division of conjunctival bands Treatment of corneal opacity by Correction of eyelid deformitieskeratoplasty or keratoprosthesis
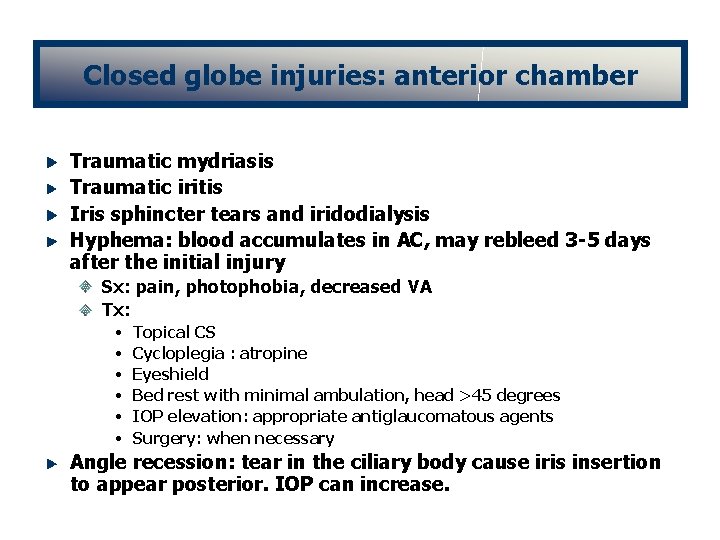
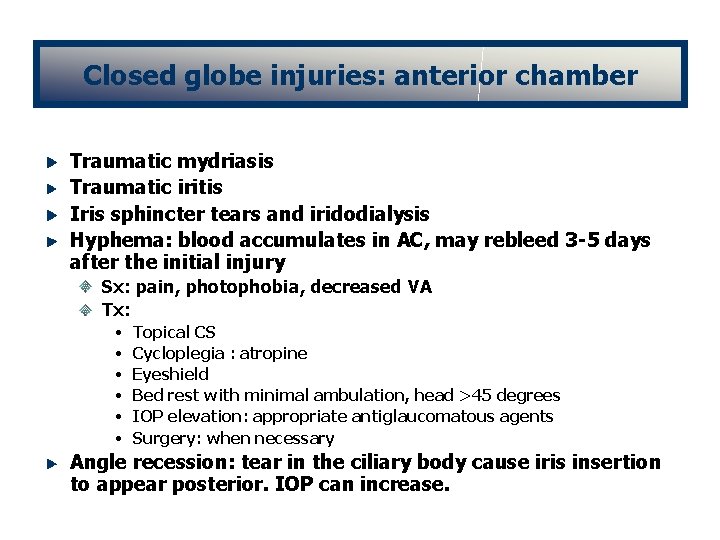
Closed globe injuries: anterior chamber Traumatic mydriasis Traumatic iritis Iris sphincter tears and iridodialysis Hyphema: blood accumulates in AC, may rebleed 3 -5 days after the initial injury Sx: pain, photophobia, decreased VA Tx: • • • Topical CS Cycloplegia : atropine Eyeshield Bed rest with minimal ambulation, head >45 degrees IOP elevation: appropriate antiglaucomatous agents Surgery: when necessary Angle recession: tear in the ciliary body cause iris insertion to appear posterior. IOP can increase.
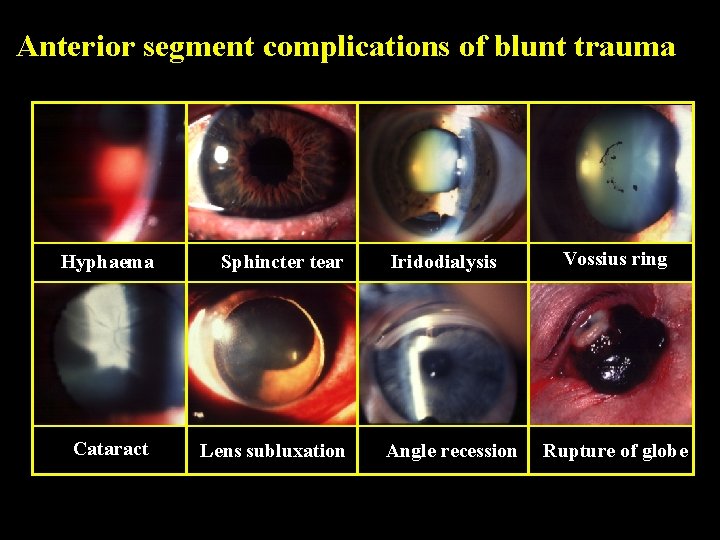
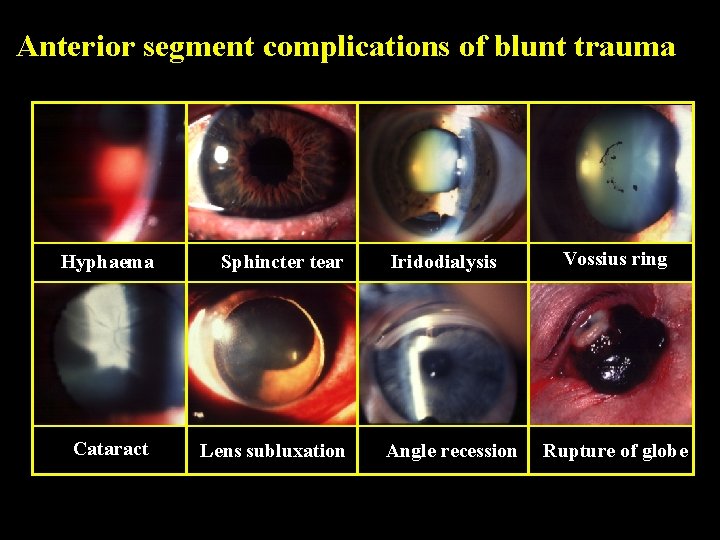
Anterior segment complications of blunt trauma Hyphaema Sphincter tear Cataract Lens subluxation Iridodialysis Angle recession Vossius ring Rupture of globe


Closed globe injuries: lens Lens subluxation and dislocation Phacoanaphylactic uveitis Traumatic cataract Lens-induced glaucoma

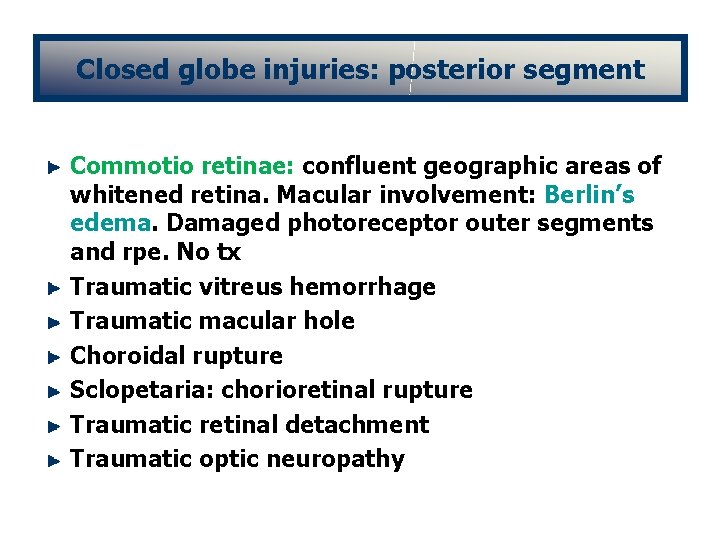
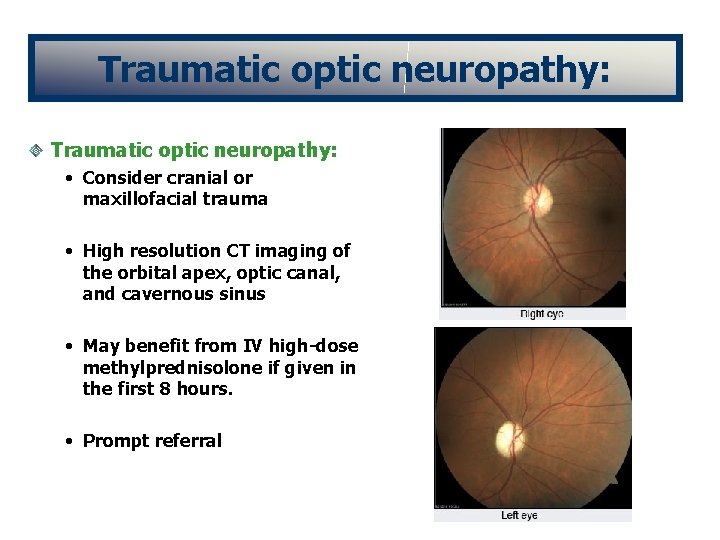
Closed globe injuries: posterior segment Commotio retinae: confluent geographic areas of whitened retina. Macular involvement: Berlin’s edema. Damaged photoreceptor outer segments and rpe. No tx Traumatic vitreus hemorrhage Traumatic macular hole Choroidal rupture Sclopetaria: chorioretinal rupture Traumatic retinal detachment Traumatic optic neuropathy
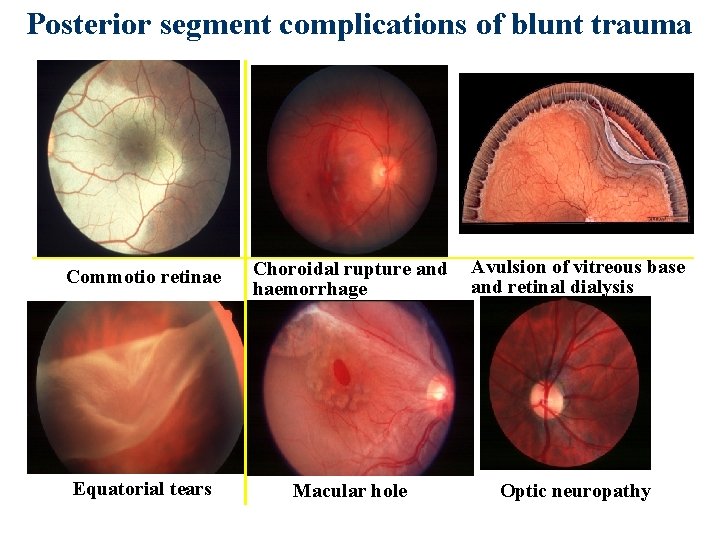
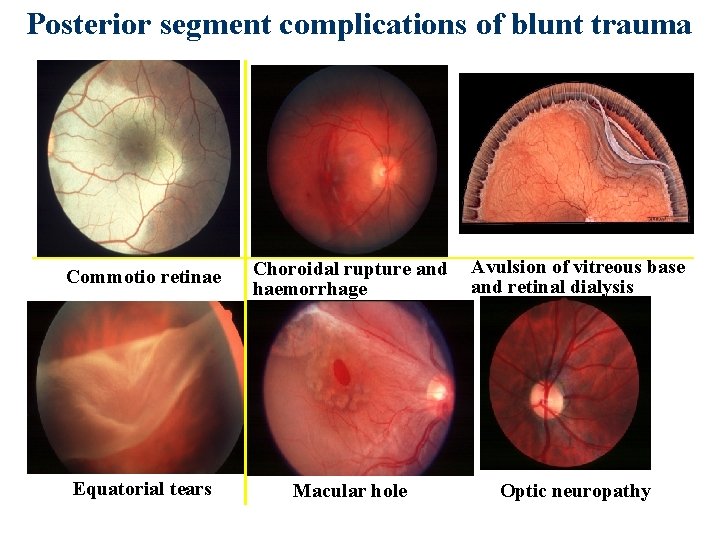
Posterior segment complications of blunt trauma Commotio retinae Choroidal rupture and haemorrhage Avulsion of vitreous base and retinal dialysis Equatorial tears Macular hole Optic neuropathy


Open globe injuries: ruptures and lacerations Subconjunctival hemorrhage: 360 degrees Profound chemosis Relative asymmetry in the AC: Shallow often with peaking of the iris towards the wound Deep AC: in full-thickness injury of posterior segment Transillumination defects of the iris Traumatic cataract, lens dislocation Hyphema Vitreous hemorrhage
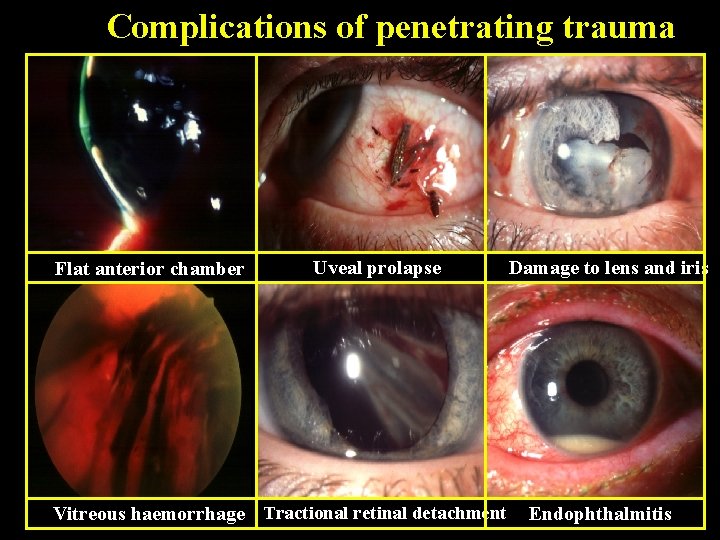
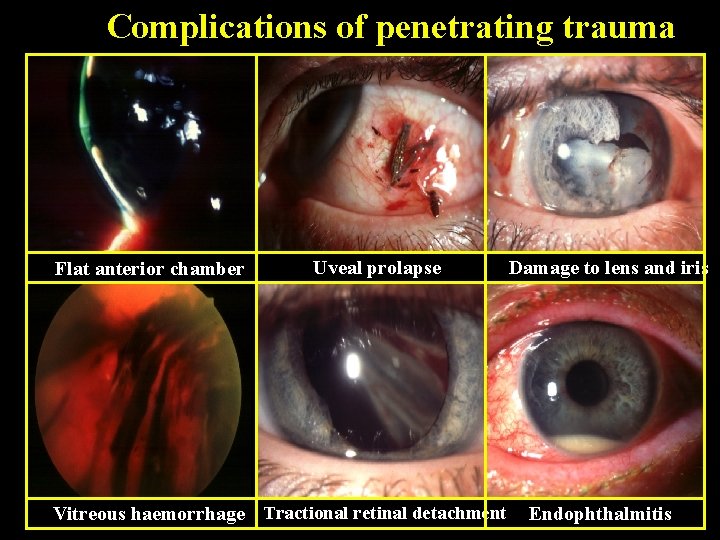
Complications of penetrating trauma Flat anterior chamber Uveal prolapse Vitreous haemorrhage Tractional retinal detachment Damage to lens and iris Endophthalmitis

Delayed complications of ocular injury Traumatic iritis Traumatic cataract Delayed trauma related glaucoma Retinal detachment Metallosis bulbi: intraocular foreign bodies should be removed! Traumatic endophthalmitis Sympathetic ophthalmia: least common, most feared Bilateral granulomatous uveitis after injury to the eye
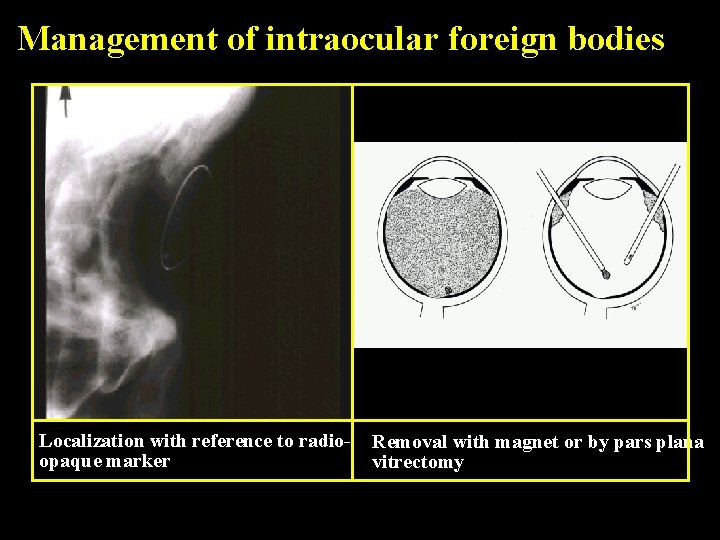
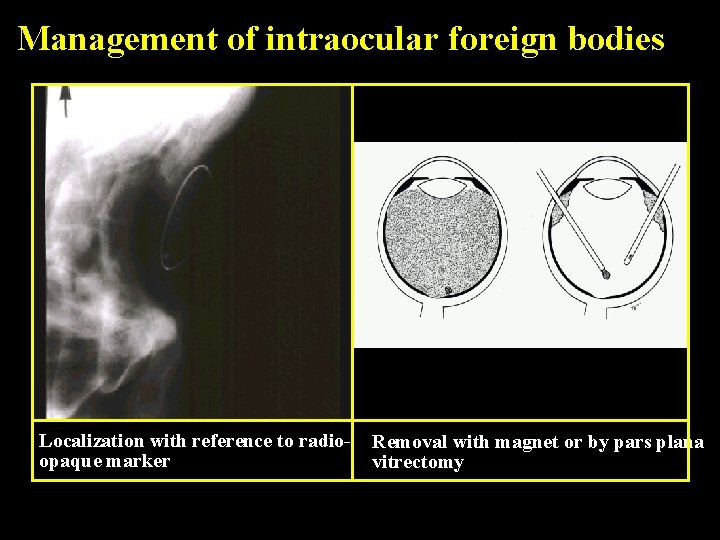
Management of intraocular foreign bodies Localization with reference to radioopaque marker Removal with magnet or by pars plana vitrectomy

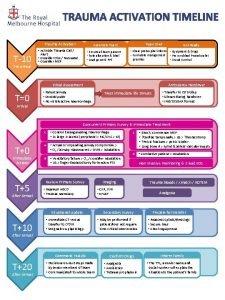
Management or Referral True emergency: initiate treatment within minutes! Chemical burns: • Immediate and profuse irrigation. • Referral to an ophthalmologist
Urgent situation: require therapy within a few hours Penetrating injuries of the globe: • • X-ray or CT scan Eye shield Don’t patch, don’t apply ointment REFERRAL Conjunctival or corneal foreign bodies: • • Topical anesthesia Cotton-tipped applicator Irrigation If remains embbedded: REFERRAL
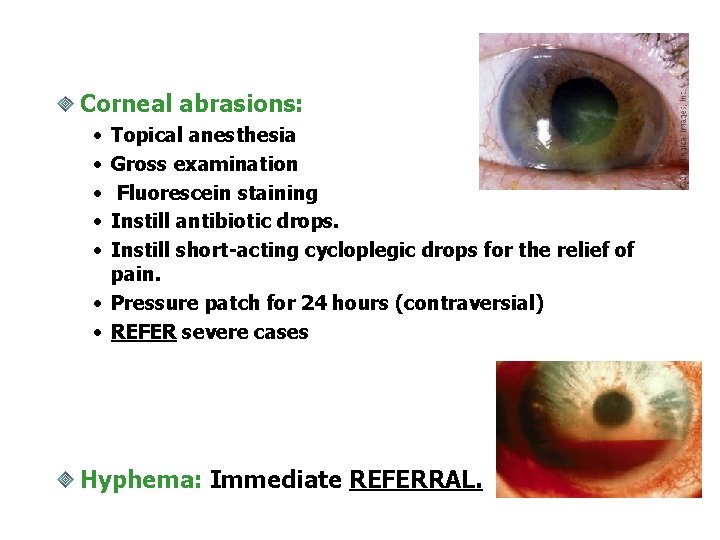
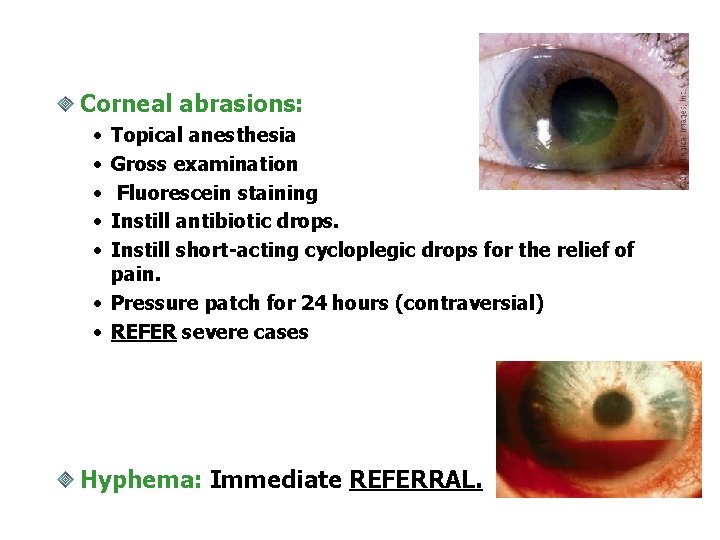
Corneal abrasions: • • • Topical anesthesia Gross examination Fluorescein staining Instill antibiotic drops. Instill short-acting cycloplegic drops for the relief of pain. • Pressure patch for 24 hours (contraversial) • REFER severe cases Hyphema: Immediate REFERRAL.
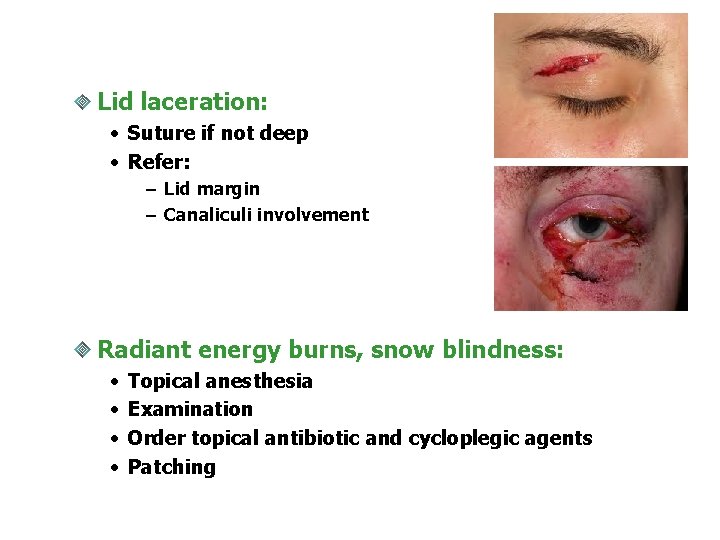
Lid laceration: • Suture if not deep • Refer: – Lid margin – Canaliculi involvement Radiant energy burns, snow blindness: • • Topical anesthesia Examination Order topical antibiotic and cycloplegic agents Patching
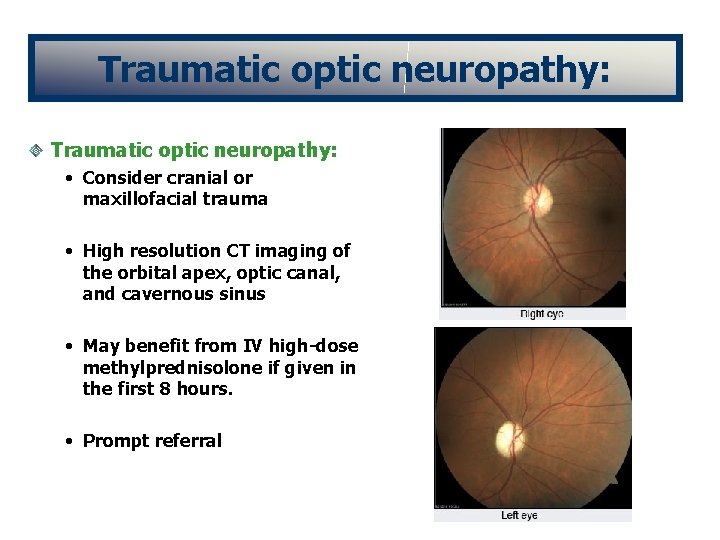
Traumatic optic neuropathy: • Consider cranial or maxillofacial trauma • High resolution CT imaging of the orbital apex, optic canal, and cavernous sinus • May benefit from IV high-dose methylprednisolone if given in the first 8 hours. • Prompt referral
Semiurgent condition: refer to an ophthalmologist within 1 -2 days Orbital fracture Subconjunctival hemorrhage: unless globe rupture or intraocular hemorrhage is suspected

The End
 Dr glaukomflecken
Dr glaukomflecken Glaukomflecken cataract
Glaukomflecken cataract Iridodialysis
Iridodialysis Emergency management of maxillofacial trauma
Emergency management of maxillofacial trauma Chapter 31 ophthalmology and otolaryngology
Chapter 31 ophthalmology and otolaryngology Vanderbilt ophthalmology residency
Vanderbilt ophthalmology residency St john's hospital
St john's hospital National tb control program
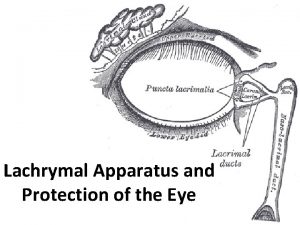
National tb control program Lacrim/o combining form
Lacrim/o combining form Mr luke anderson ophthalmology
Mr luke anderson ophthalmology Kreiger eye institute
Kreiger eye institute Ubc ophthalmology
Ubc ophthalmology Ophthalmology code of ethics
Ophthalmology code of ethics Ophthalmology
Ophthalmology Ubc ophthalmology
Ubc ophthalmology Miosis
Miosis Sump syndrome
Sump syndrome Veterinary ophthalmology
Veterinary ophthalmology Jama ophthalmology impact factor
Jama ophthalmology impact factor British journal of ophthalmology
British journal of ophthalmology Online journal of ophthalmology
Online journal of ophthalmology Asia-pacific academy of ophthalmology
Asia-pacific academy of ophthalmology Ophthalmology case study
Ophthalmology case study 16710-17
16710-17 Alan bird ophthalmology
Alan bird ophthalmology Ophthalmology lecture
Ophthalmology lecture Trauma awareness and treatment center utah
Trauma awareness and treatment center utah Triune brain theory and trauma
Triune brain theory and trauma Limbic system and trauma
Limbic system and trauma Tarn database
Tarn database Trauma recovery and empowerment model
Trauma recovery and empowerment model Uccs veterans health and trauma clinic
Uccs veterans health and trauma clinic Vicarious felidae
Vicarious felidae Trauma gestig behindert
Trauma gestig behindert Trauma thorax
Trauma thorax Tscyc screening form
Tscyc screening form Trauma sensitief lesgeven
Trauma sensitief lesgeven 4 r's trauma informed care
4 r's trauma informed care Trauma informed care lgbtq
Trauma informed care lgbtq Dental mobility classification
Dental mobility classification Miemss trauma decision tree
Miemss trauma decision tree Examples of little t trauma
Examples of little t trauma Trauma bonding definition
Trauma bonding definition Trauma timeline
Trauma timeline Dr anita ravi
Dr anita ravi Golden hour of trauma
Golden hour of trauma Trauma-informed care cheat sheet
Trauma-informed care cheat sheet Nethercutt emergency center
Nethercutt emergency center