Systemic versus Catheter Directed Lysis for Acute Arterial

- Slides: 23
Systemic versus Catheter Directed Lysis for Acute Arterial Thrombosis Kenneth Rosenfield, MD, MHCDS

Kenneth Rosenfield, MD • Consultant – Abbott Vascular – Capture Vascular – Cardinal Health – CRUZAR Systems – Endospan – Inspire. MD – MD Insider – Micell – Shockwave – Silk Road – Surmodics – Valcare • • Financial Disclosures Equity • Research or Fellowship Support – Contego – NIH – Embolitech – Atrium – MDInsider – Janacare – PQ Bypass – Primacea – Vortex Board Member – VIVA Physicians (Not For Profit 501(c) 3 Organization) • www. vivapvd. com
Acute Limb Ischemia • Cause – sudden decrease in blood flow to limb • Arterial – embolization (Afib, Atheroembolism, Iatrogenic) (15%) – thrombosis (clot superimposed on PAOD (80%) – slow from cardiogenic shock; obstruction from devices…eg. ECMO; hypercoagulable state) – Compromised flow …eg. Dissection or plaque rupture • Venous – Thrombosis and Phlegmasia
Symptoms – 6 P’s • • • Pain Pallor Polar (cool) Paresthesias Pulselessness Paralysis
Arterial Thrombosis in other organs • • Renal Mesenteric Cerebral Coronary!
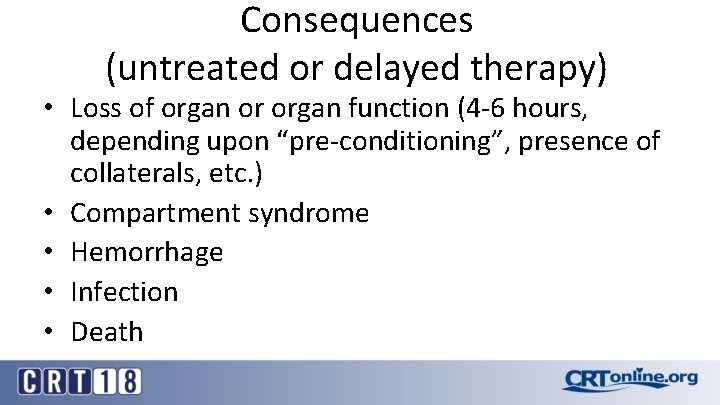
Consequences (untreated or delayed therapy) • Loss of organ or organ function (4 -6 hours, depending upon “pre-conditioning”, presence of collaterals, etc. ) • Compartment syndrome • Hemorrhage • Infection • Death
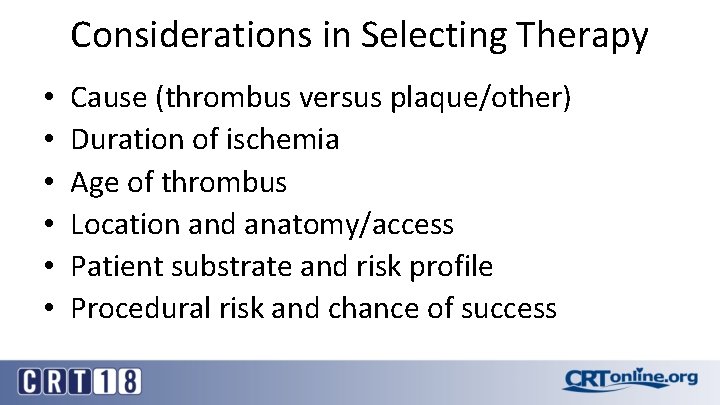
Considerations in Selecting Therapy • • • Cause (thrombus versus plaque/other) Duration of ischemia Age of thrombus Location and anatomy/access Patient substrate and risk profile Procedural risk and chance of success
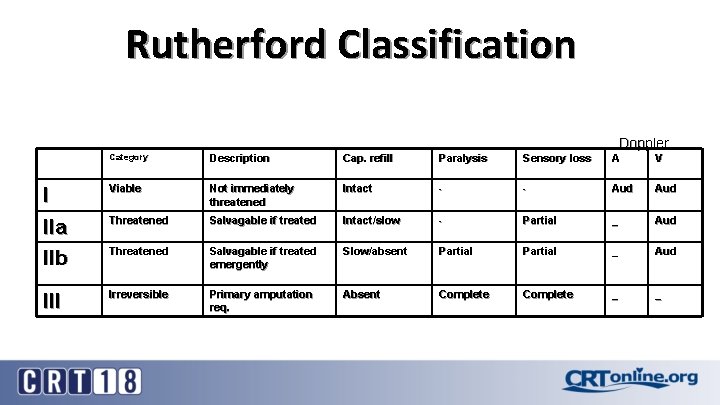
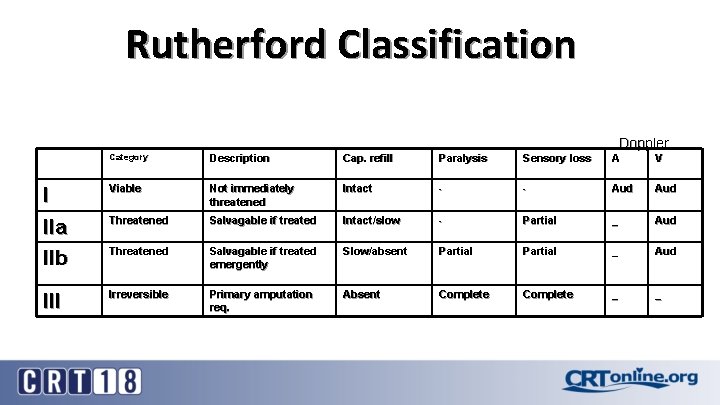
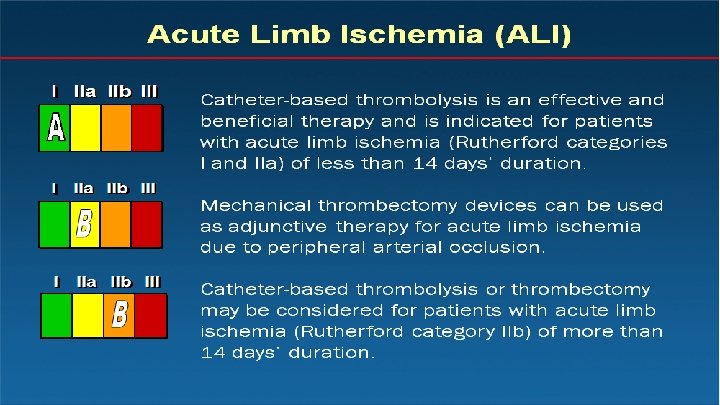
Rutherford Classification Doppler Category Description Cap. refill Paralysis Sensory loss A V I IIa IIb Viable Not immediately threatened Intact - - Aud Threatened Salvagable if treated Intact/slow - Partial _ Aud Threatened Salvagable if treated emergently Slow/absent Partial _ Aud III Irreversible Primary amputation req. Absent Complete _ _
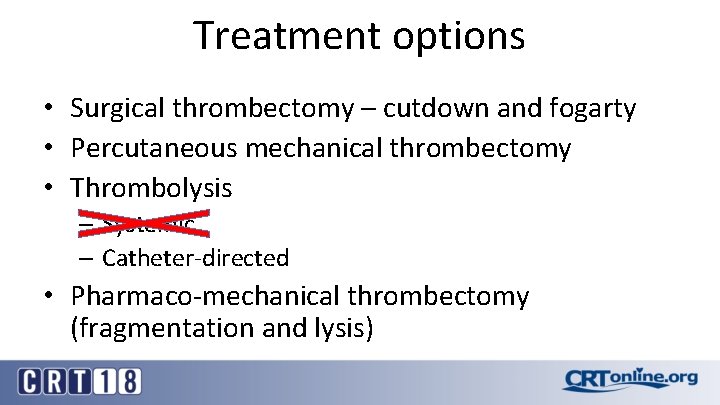
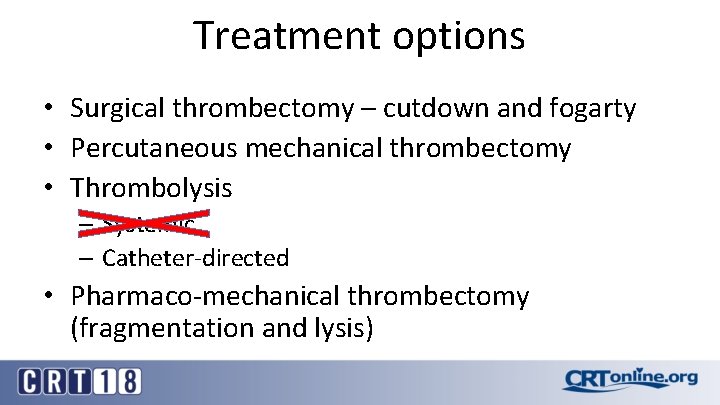
Treatment options • Surgical thrombectomy – cutdown and fogarty • Percutaneous mechanical thrombectomy • Thrombolysis – Systemic – Catheter-directed • Pharmaco-mechanical thrombectomy (fragmentation and lysis)
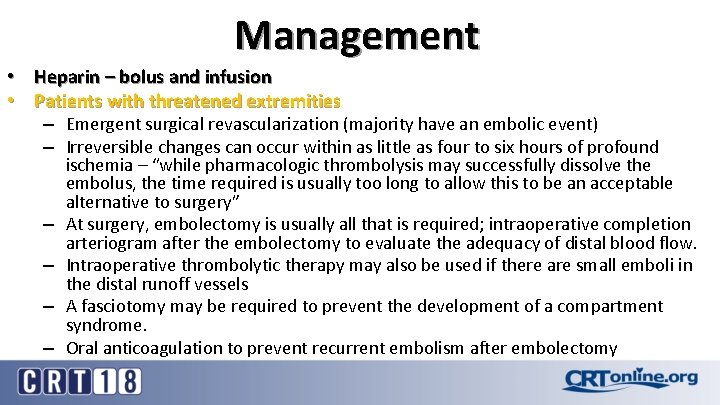
Management • Heparin – bolus and infusion • Patients with threatened extremities – Emergent surgical revascularization (majority have an embolic event) – Irreversible changes can occur within as little as four to six hours of profound – – ischemia – “while pharmacologic thrombolysis may successfully dissolve the embolus, the time required is usually too long to allow this to be an acceptable alternative to surgery” At surgery, embolectomy is usually all that is required; intraoperative completion arteriogram after the embolectomy to evaluate the adequacy of distal blood flow. Intraoperative thrombolytic therapy may also be used if there are small emboli in the distal runoff vessels A fasciotomy may be required to prevent the development of a compartment syndrome. Oral anticoagulation to prevent recurrent embolism after embolectomy
Management • Patients with viable extremities – Intra-arterial thrombolysis is an alternative to surgical therapy in patients with ischemic but viable extremities – Thrombolytic therapy vs. surgery • TOPAS and STILE trials
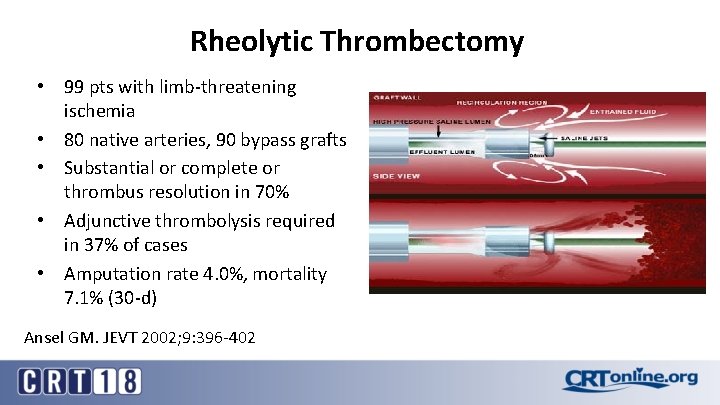
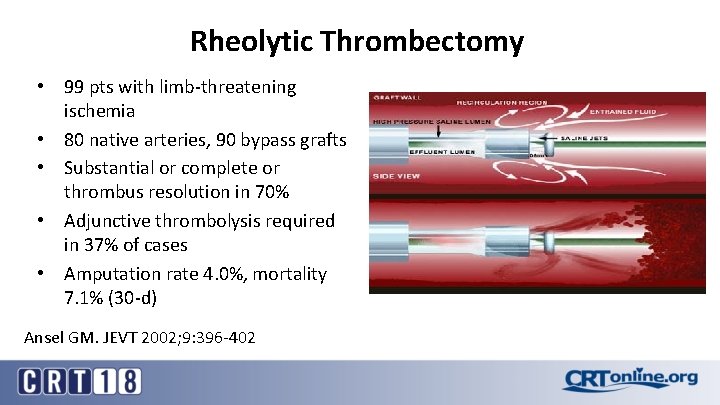
Rheolytic Thrombectomy • 99 pts with limb-threatening ischemia • 80 native arteries, 90 bypass grafts • Substantial or complete or thrombus resolution in 70% • Adjunctive thrombolysis required in 37% of cases • Amputation rate 4. 0%, mortality 7. 1% (30 -d) Ansel GM. JEVT 2002; 9: 396 -402
CDT versus surgical thrombectomy CDT • Less invasive • Potentially more rapid reperfusion • ? more complete (side branches and distal bed) • Reduced infection • Reduced LOS • Reduced cost • Identify culprit lesion (although intra-op angio now feasible in most hospitals)
Percutaneous mechanical thrombectomy • Fragmentation and aspiration – Penumbra – Angiojet – Jed-i • Direct aspiration – Large bore catheter – Flow-triever
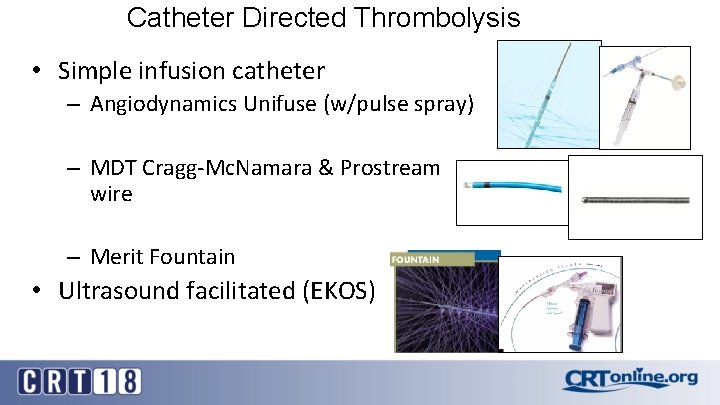
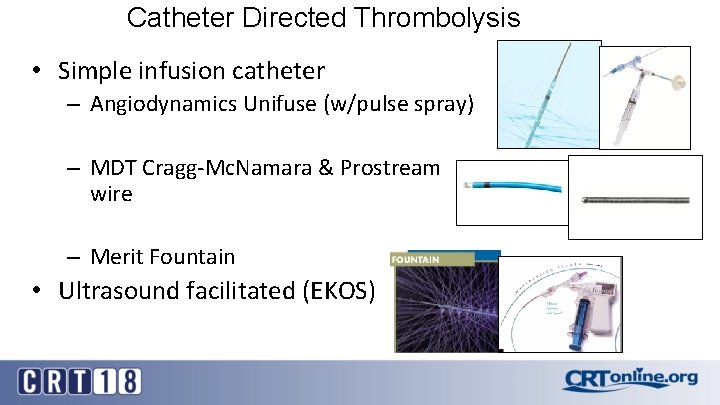
Catheter Directed Thrombolysis • Simple infusion catheter – Angiodynamics Unifuse (w/pulse spray) – MDT Cragg-Mc. Namara & Prostream wire – Merit Fountain • Ultrasound facilitated (EKOS)
Catheter Directed Thrombolysis • Ultrasound facilitated (EKOS) – BTG-EKOS
Catheter Directed Thrombolysis • Dosing – t. PA 0. 25 -1 mg/hr – Retevase 0. 25 -1 mg/hr • Duration – 30 min (pulse-spray and dwell) – Up to 24 hrs (general guideline)
Contraindications to Thrombolytic Therapy Absolute • Previous hemorrhagic stroke • Active bleeding diathesis • Intracranial tumor Relative Major • • • Major surgery or trauma within 10 days Uncontrolled HTN Puncture of non-compressible vessel Serious and uncorrected GI bleed Pregnancy Must consider each patient individually
Surgery versus thrombolysis for initial management of acute limb ischaemia Cochrane Database Syst Rev. 2013 Jun 6; (6): CD 002784. doi: 10. 1002/14651858. CD 002784. pub 2. Berridge DC 1, Kessel DO, Robertson I.
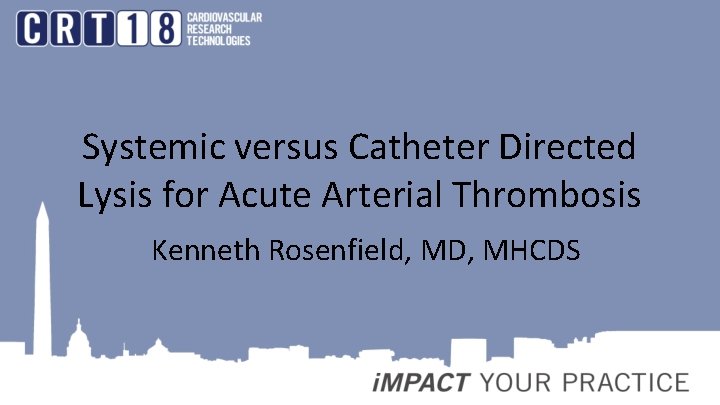
Cochrane analysis • Five trials - 1283 participants • no significant difference in limb salvage or death at 30 days, six months or one year between initial surgery and initial thrombolysis • Stroke more frequent at 30 days in thrombolysis participants (1. 3%) compared to surgery participants (0%) (OR) 6. 41; 95% confidence interval (CI) 1. 57 to 26. 22) • Major hemorrhage more likely at 30 days in thrombolysis participants (8. 8%) compared to surgery participants (3. 3%) (OR 2. 80; 95% CI 1. 70 to 4. 60) • distal embolization more likely at 30 days in thrombolysis participants (12. 4%) compared to surgery participants (0%) (OR 8. 35; 95% CI 4. 47 to 15. 58). • Participants treated by initial thrombolysis underwent a less severe degree of intervention (OR 5. 37; 95%CI 3. 99 to 7. 22) and displayed equivalent overall survival compared to initial surgery (OR 0. 87; 95% CI 0. 61 to 1. 25).
Authors’ conclusions • Universal initial treatment with either surgery or thrombolysis cannot be advocated on the available evidence. • no overall difference in limb salvage or death at one year between initial surgery and initial thrombolysis. • Thrombolysis may be associated with a higher risk of ongoing limb ischemia and hemorrhagic complications including stroke • Higher risk of complications must bebalanced against risks of surgery in each patient
Summary: Arterial Thrombolysis • Catheter-directed thrombolysis remains a useful treatment for native artery and graft occlusion • Thrombolysis is a complementary technique with surgery • Critical to identify & correct underlying stenotic lesion • Decreased hemorrhagic complications are possible with mechanical thrombectomy