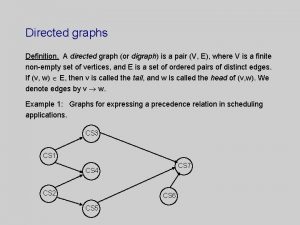
Concerns with Catheter Directed TPA for the Treatment











- Slides: 31
Concerns with Catheter Directed TPA for the Treatment of PEs
Concerns • Triage / Processes • Parallels with catheter-directed CVA treatments • Review of the catheter-directed PE literature
Triage • Massive / Shock -> Thrombolysis • Submassive • No RV strain -> Routine Anticoagulation
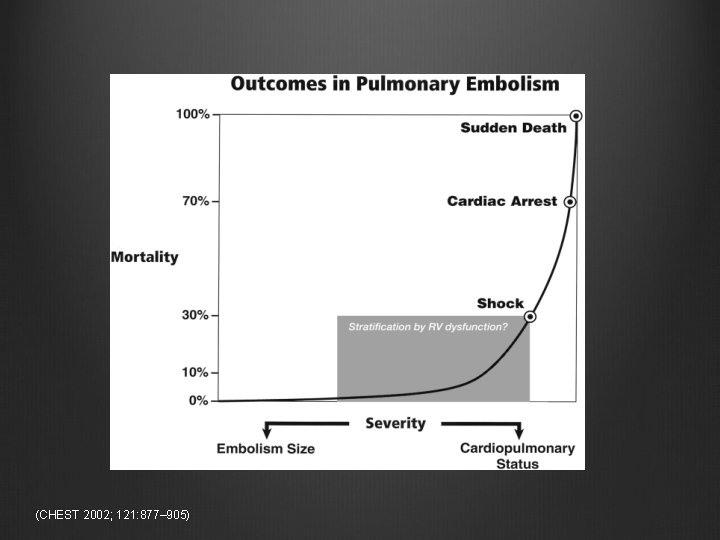
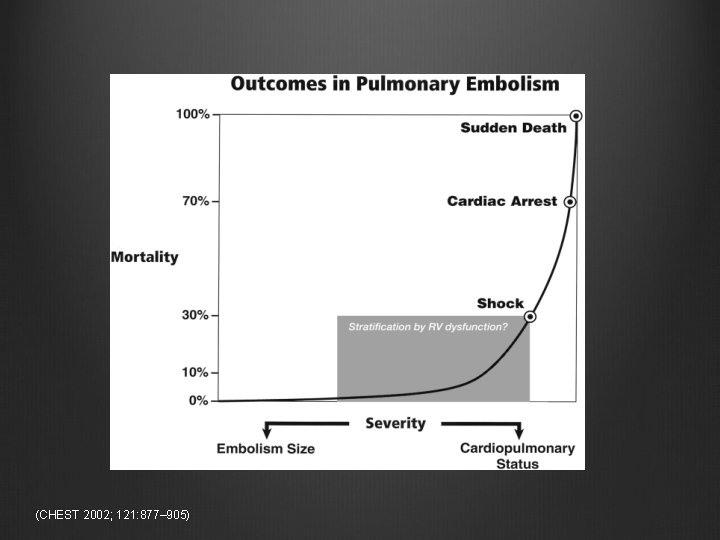
(CHEST 2002; 121: 877– 905)


“Golden Hour” “In fatal cases, it has long been recognized that two thirds of those patients will die within 1 h of presentation and that anatomically massive PE will only account for one half of those deaths, with the remainder attributed to smaller submassive or recurrent emboli. ” (CHEST 2002; 121: 877– 905)
Judgment “…thrombolytic therapy in this population should be individualized and benefits and risks (of bleeding) should be carefully weighed on a case -by-case basis. ” Tapson. Uptodate.
Who is called first matters.

Death may decide when doctors disagree

Code PE Why do we have “code stroke” and “code STEMI” protocols?
Parallels (http: //digiphotomag. com/articles/many-traveled-roads-an-interview-with-harvey-stein/)
Parallels Catheterdirected treatment of CVAs Cather-directed treatment of PEs

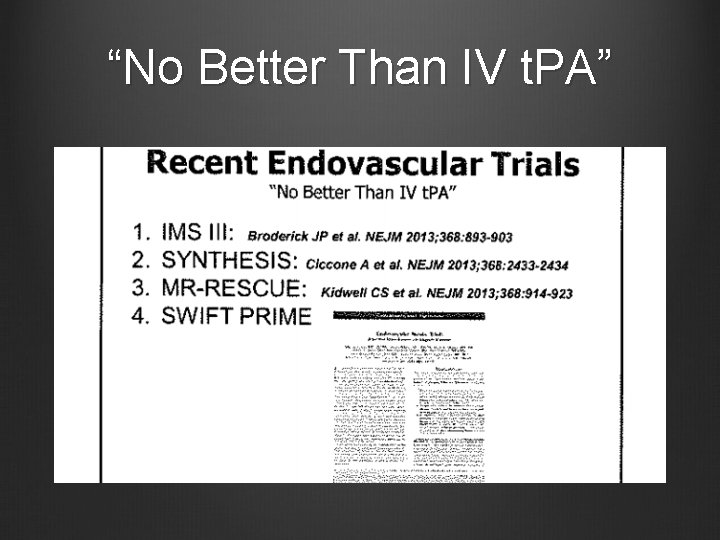
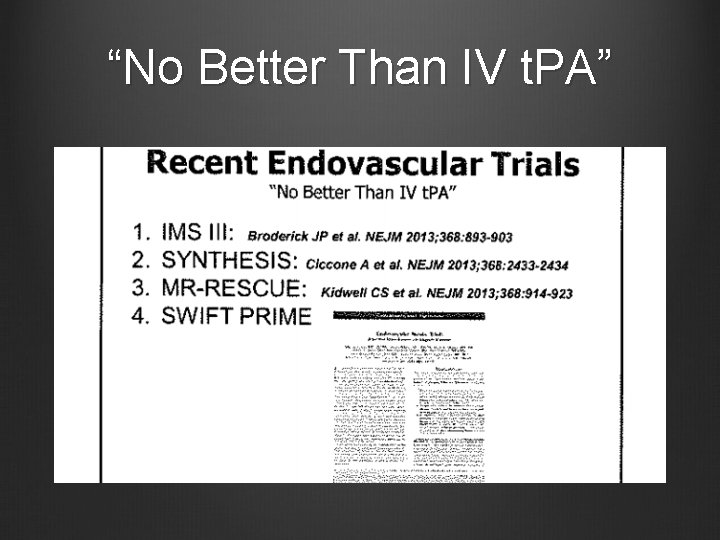
“No Better Than IV t. PA”

Too Slow • “The time from symptom onset to endovascular treatment start was too long (1 -3 hours) and this delay places [intraarterial therapy] at a significant disadvantage. ” Barreto, Endovascular Therapy for Acute Ischemic Stroke -- An Update
AHA Stroke Guidelines • “Patients eligible for intravenous rt. PA should receive intravenous rt. PA even if intra-arterial treatments are being considered (Class I; Level of Evidence A). ” • “…thrombectomy devices can be useful in achieving recanalization alone or in combination with pharmacological fibrinolysis in carefully selected patients (Class IIa; Level of Evidence B). Their ability to improve patient outcomes has not yet been established. These devices should continue to be studied in randomized controlled trials to determine the efficacy of such treatments in improving patient outcomes. ” http: //stroke. ahajournals. org/content/44/3/870. full

Triage Parallel “We did have one patient several years ago who was sent to the cath lab and did not receive IV t. PA when she was a candidate. ”
DVT Parallel • Catheter-directed treatment of DVT versus anticoagulation • Mortality unchanged • Blood transfusions, PEs, ICH, length of stay, and IVC filter placements all significantly higher • Three times more hospital charges (http: //archinte. jamanetwork. com/article. aspx? article. ID=1889011)

Systemic Thrombolysis for Submassive PE • No mortality benefit • More bleeding including ICH • Less decompensation n engl j med 370; 15 nejm. org april 10, 2014 Journal of Thrombosis and Haemostasis, 10: 751– 759 JAMA. 2014; 311(23): 2414 -2421. doi: 10. 1001/jama. 2014. 5990
ULTIMA • Nonblinded, industry-involved trial 59 patients (out of 304 screened) • Ultrasound Catheter TPA up to 4 hrs vs heparin • Required RV/LV ratio > 1. 0 • Not powered for survival or bleeding complications. • RV/LV ratio improved faster with intervention • Heparin group “caught up” by 90 days
Natural PE Course • “Most patients with PE treated with anti-coagulation alone will achieve embolus resolution at 4 weeks. ” • “The feared consequence of resultant chronic thromboembolic pulmonary hypertension occurs only 0. 1% to 3. 8% of patients with PE” • “Mortality after submassive PE is uncommon” (Circulation. 2014; 129: 420 -421)
ULTIMAtely Meh? • Small, not blinded, industry-involved • ULTIMA shows that US facilitated TPA compared to heparin rapidly improves RV size. • IVC / RV improvement not significantly different at 90 days. • No survival or bleeding data
Seattle-II • Industry-funded, not (yet? ) published • US Catheter directed TPA • No comparison group • No ICH. Major bleeding 11. 3% • Many patients required two catheters. • RV/LV ratio acutely improved • 1 death due to PE (0. 5%). 3 total deaths (2%). http: //www. medscape. com/viewarticle/823571#

Seattle Pee-eww? • Industry-funded. Not published. • No comparison group. • Although no ICH reported, major bleeding appears as high as systemic t. PA. 11. 3% vs 11. 5%. • Apparently only shows short-term RV improvement.
ACCP Guidelines • “In patients with acute PE when a thrombolytic agent is used, we suggest administration through a peripheral vein over a pulmonary artery catheter. ” • “In patients with acute PE associated with hypotension and who have (i) contraindications to thrombolysis, (ii) failed thrombolysis, or (iii) shock that is likely to cause death before systemic thrombolysis can take effect (eg, within hours), if appropriate expertise and resources are available, we suggest catheter-assisted thrombus removal over no such intervention. ” • “In patients with acute PE who are treated with anticoagulants, we recommend against the use of an IVC filter. ” http: //journal. publications. chestnet. org/issue. aspx? journalid=99&issueid=23443&direction=P

Chronic thromboembolic pulmonary hypertension? • 40% never diagnosed with DVT or PE • 0. 57% incidence in patient’s with PE • Only 10/170 (5. 8%) with symptoms actually have CTEPH • “Because of the very low incidence of CTEPH after PE, the implementation of extensive follow-up programs for the detection of CTEPH after acute PE seems to be unnecessary. ” Haematologica. Jun 2010; 95(6): 970– 975.
Chronic RV Dysfunction? • 159 heparin vs 19 TPA • Neither 6 minute walks nor NYHA scores were significantly different between heparin and thrombolysis. • RV hypokinesis no difference between the two groups (7% vs 6%) • Subgroup analysis showed that heparin only group 27% had “increase in RVSP” and 46% had symptoms. However, more t. PA patients had RVSP > 40 (11% vs 7%). (Chest / 136 / 5 / November, 2009)
Conclusions PE with RV strain (like a STEMI) often is an emergency which requires a clear, single pathway. Time consumed trying to tease out who owns these patients is dangerous. Critical care medicine should hold primary responsibility for these patients.

Conclusions Our history with CVAs should be a lesson to us. Despite initial promising studies, large trials of catheter-directed therapy have shown no benefit over standard of care. Wake. Med’s premature journey down this pathway last time wasteful and dangerous.
Conclusions Although catheter directed thrombolysis for submassive PEs may show some promise, these early industry-supported studies have shown no meaningful long term improvement over routine care. Catheter-directed thrombolysis should remain an option in patients who have contraindications or fail systemic therapy.
 Gan dunnington md
Gan dunnington md Syntax directed definition and syntax directed translation
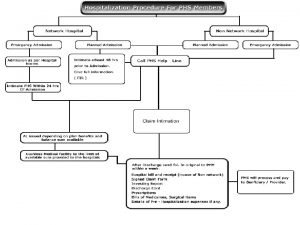
Syntax directed definition and syntax directed translation Paramount health insurance philippines
Paramount health insurance philippines Tpa handbook
Tpa handbook Pengertian q
Pengertian q Tpa spanish
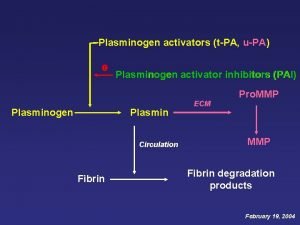
Tpa spanish Tpa upa
Tpa upa Tpa best presentation award
Tpa best presentation award Aul4s
Aul4s California tpa
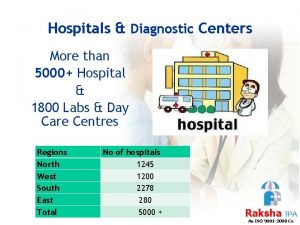
California tpa Raksha tpa claim
Raksha tpa claim Transfer of physical assets
Transfer of physical assets Raksha tpa intimation
Raksha tpa intimation Super shuttle tampa
Super shuttle tampa Lifeline tpa
Lifeline tpa 1800226655
1800226655 Gica marker
Gica marker Htpothalamus
Htpothalamus Thematic concerns
Thematic concerns Health concerns
Health concerns Joys and concerns prayer
Joys and concerns prayer Layout
Layout Addressing concerns and earning commitment
Addressing concerns and earning commitment Macbeth study questions acts 1-5 answers
Macbeth study questions acts 1-5 answers Escalating concerns
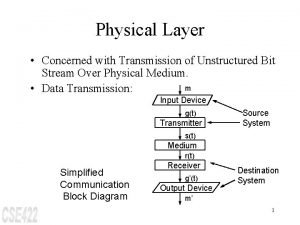
Escalating concerns The physical layer concerns with
The physical layer concerns with Southwest airlines code of ethics
Southwest airlines code of ethics Java9s
Java9s Gmc raising concerns flowchart
Gmc raising concerns flowchart When a choice concerns matters of personal value or taste
When a choice concerns matters of personal value or taste Pietro molla
Pietro molla Ddd gui
Ddd gui