Paramount Health Services TPA P Ltd In conjunction




- Slides: 21
Paramount Health Services (TPA) P. Ltd. , In conjunction with UNITED INDIA INSURANCE CO LTD. Presents New Dimensions In Health Insurance For Dr. B. R. Ambedkar National Institute of Technology, Jalandhar.

Group Mediclaim PARAMOUNT AS A TPA - EFFICIENT LINK This insurance scheme is to provide adequate insurance coverage to the students for expenses related to hospitalization due to illness, disease or injury. Service Provider (PHS)

Programme. Highlights Benefit Details Enrollment in the program Cashless Hospitalization Process Reimbursement Claim Process
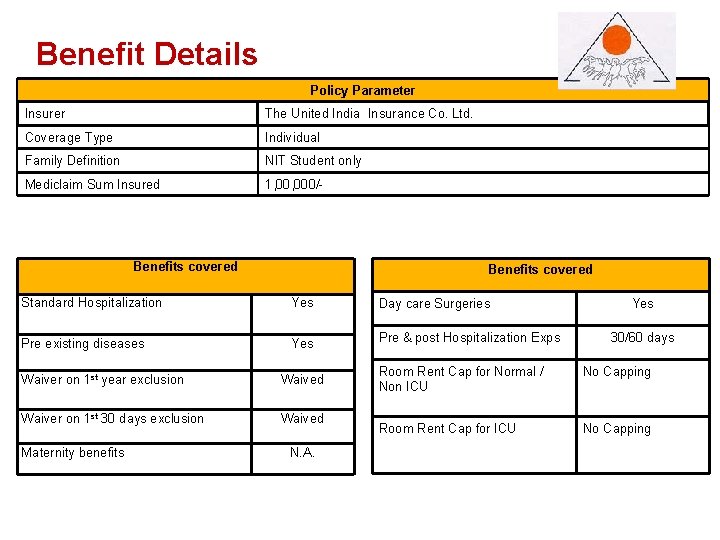
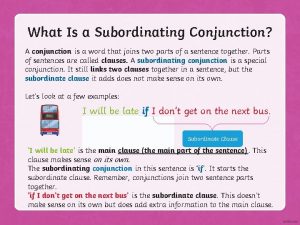
Benefit. Details Policy Parameter Insurer The United India Insurance Co. Ltd. Coverage Type Individual Family Definition NIT Student only Mediclaim Sum Insured 1, 000/- Benefits covered Standard Hospitalization Yes Day care Surgeries Pre existing diseases Yes Pre & post Hospitalization Exps Waiver on 1 st year exclusion Waived Waiver on 1 st 30 days exclusion Waived Maternity benefits N. A. Yes 30/60 days Room Rent Cap for Normal / Non ICU No Capping Room Rent Cap for ICU No Capping
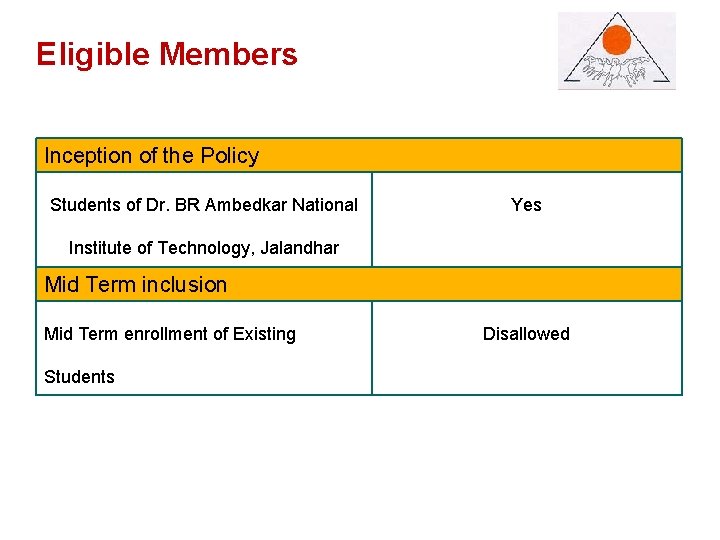
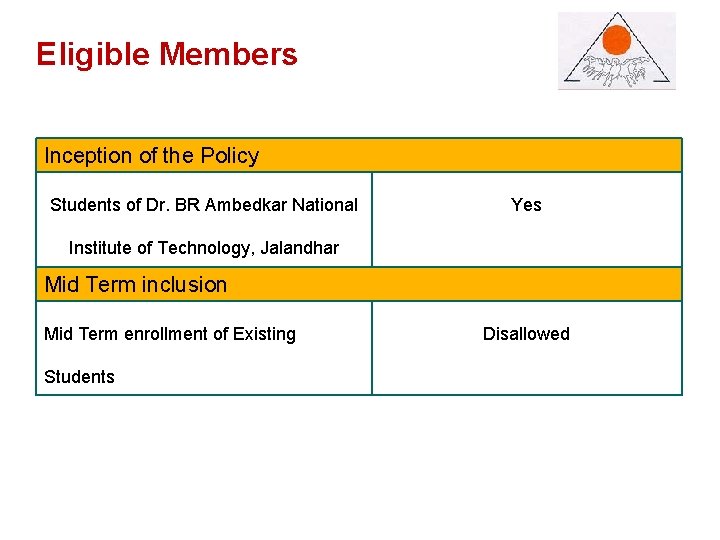
Eligible. Members Inception of the Policy Students of Dr. BR Ambedkar National Yes Institute of Technology, Jalandhar Mid Term inclusion Mid Term enrollment of Existing Students Disallowed
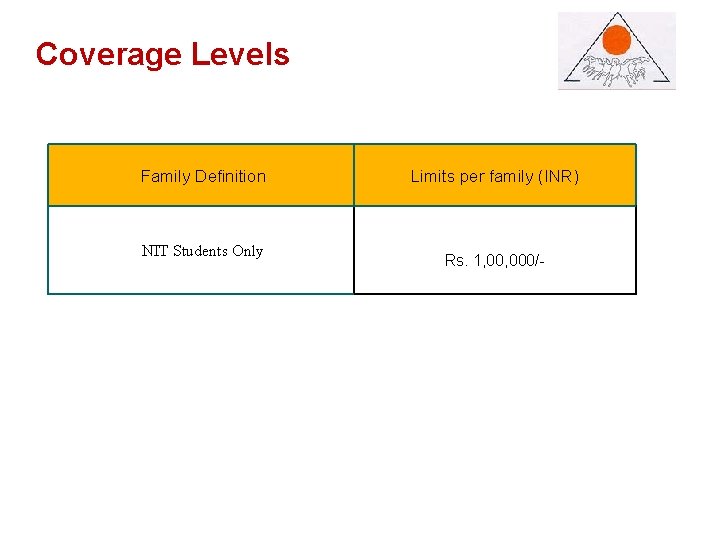
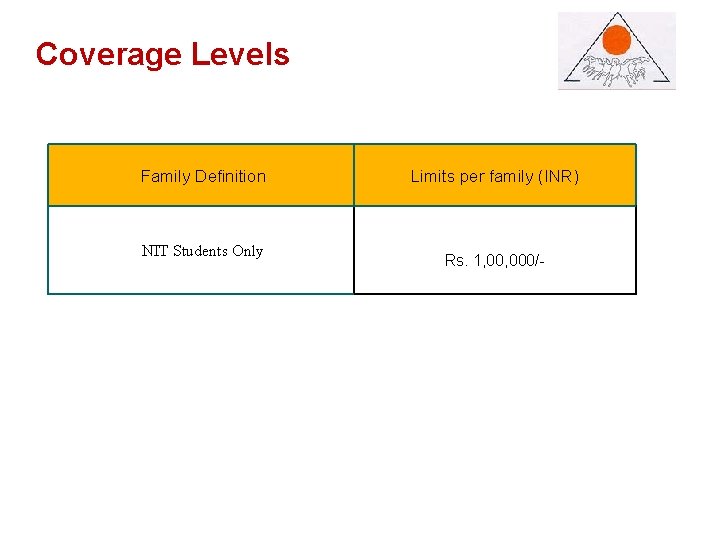
Coverage. Levels Family Definition NIT Students Only Limits per family (INR) Rs. 1, 000/- Back
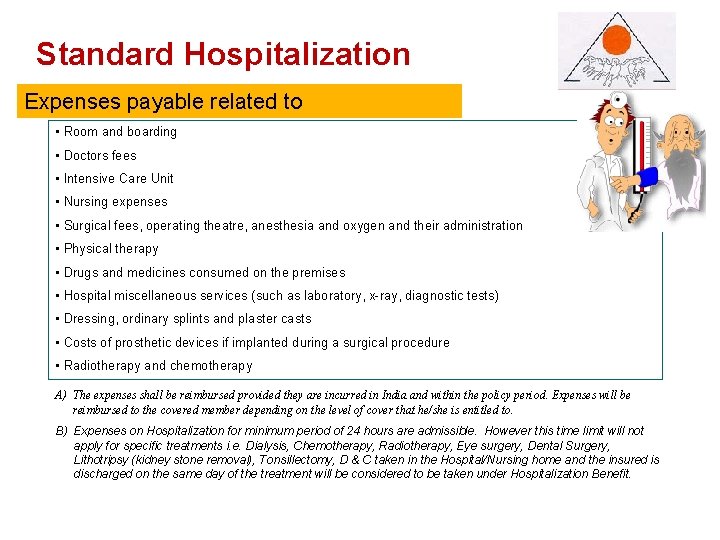
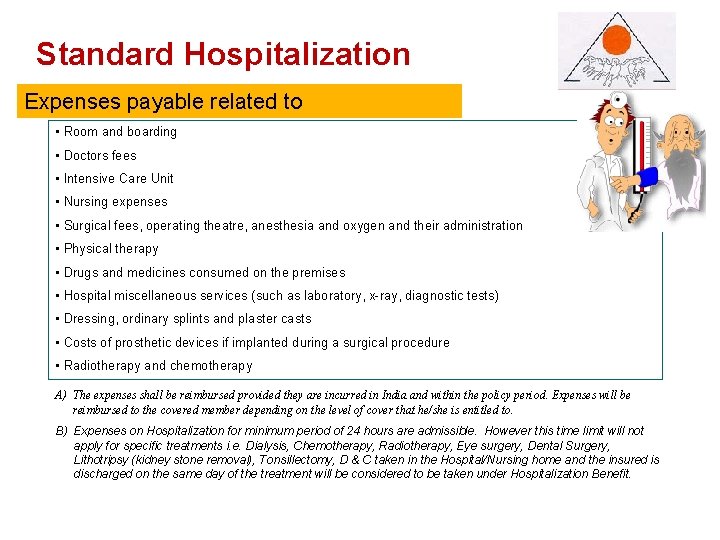
Standard. Hospitalization Expenses payable related to • Room and boarding • Doctors fees • Intensive Care Unit • Nursing expenses • Surgical fees, operating theatre, anesthesia and oxygen and their administration • Physical therapy • Drugs and medicines consumed on the premises • Hospital miscellaneous services (such as laboratory, x-ray, diagnostic tests) • Dressing, ordinary splints and plaster casts • Costs of prosthetic devices if implanted during a surgical procedure • Radiotherapy and chemotherapy A) The expenses shall be reimbursed provided they are incurred in India and within the policy period. Expenses will be reimbursed to the covered member depending on the level of cover that he/she is entitled to. B) Expenses on Hospitalization for minimum period of 24 hours are admissible. However this time limit will not apply for specific treatments i. e. Dialysis, Chemotherapy, Radiotherapy, Eye surgery, Dental Surgery, Lithotripsy (kidney stone removal), Tonsillectomy, D & C taken in the Hospital/Nursing home and the insured is discharged on the same day of the treatment will be considered to be taken under Hospitalization Benefit. Back

Customized. Benefits Pre existing diseases Definition Any Pre-Existing ailments such as diabetes, hypertension, etc or related ailments for which care, treatment or advice was recommended by or received from a Doctor or which was first manifested prior to the commencement date of the Insured Person’s first Health Insurance policy with the Insurer √ Covered First 30 day waiting period Definition Any Illness diagnosed or diagnosable within 30 days of the effective date of the Policy Period if this is the first Health Policy taken by the Policyholder with the Insurer. If the Policyholder renews the Health Policy with the Insurer and increases the Limit of Indemnity, then this exclusion shall apply in relation to the amount by which the Limit of Indemnity has been increased X Waived Off First Year Waiting period Definition During the first year of the operation of the policy the expenses on treatment of diseases such as Cataract, Benign Prostatic Hypertrophy, Hysterectomy for Menorrhagia or Fibromyoma, Hernia, Hydrocele, Congenital Internal Diseases, Fistula in anus, Piles, Sinusitis and related disorders are not payable. If these diseases are pre- existing at the time of proposal they will not be covered even during subsequent period or renewal too Back
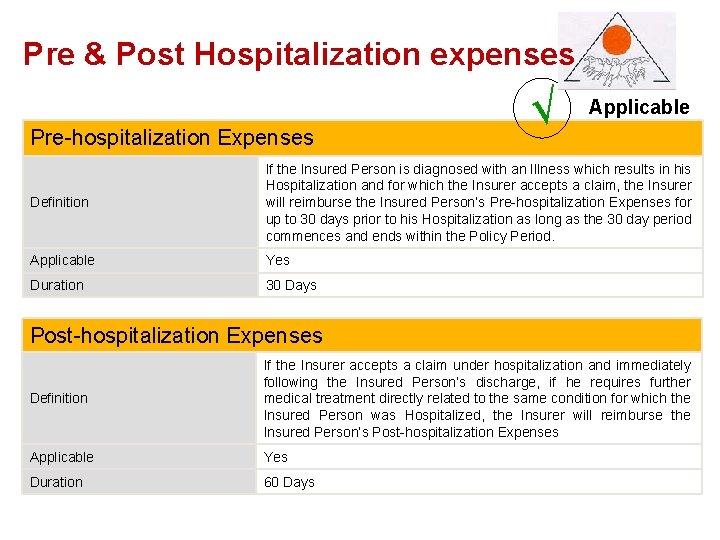
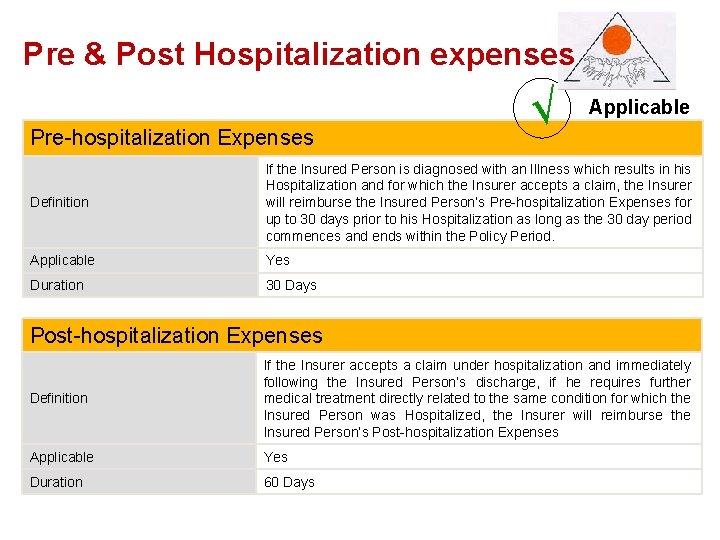
Pre Pre&&Post. Hospitalizationexpenses Pre-hospitalization Expenses √ Applicable Definition If the Insured Person is diagnosed with an Illness which results in his Hospitalization and for which the Insurer accepts a claim, the Insurer will reimburse the Insured Person’s Pre-hospitalization Expenses for up to 30 days prior to his Hospitalization as long as the 30 day period commences and ends within the Policy Period. Applicable Yes Duration 30 Days Post-hospitalization Expenses Definition If the Insurer accepts a claim under hospitalization and immediately following the Insured Person’s discharge, if he requires further medical treatment directly related to the same condition for which the Insured Person was Hospitalized, the Insurer will reimburse the Insured Person’s Post-hospitalization Expenses Applicable Yes Duration 60 Days
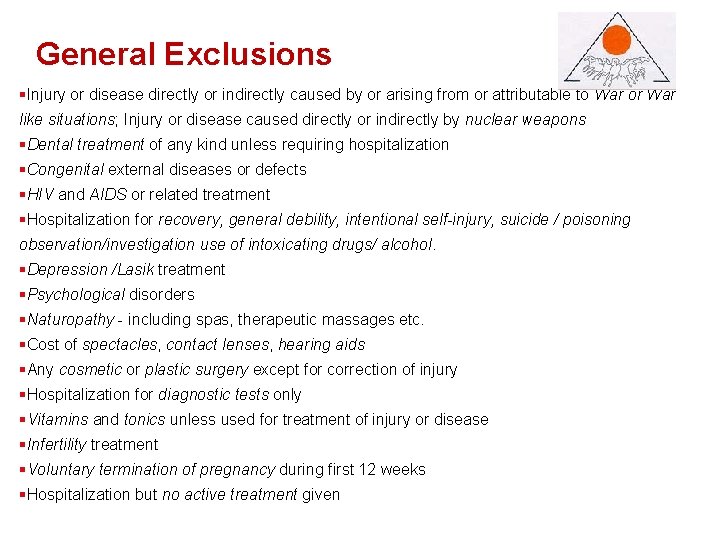
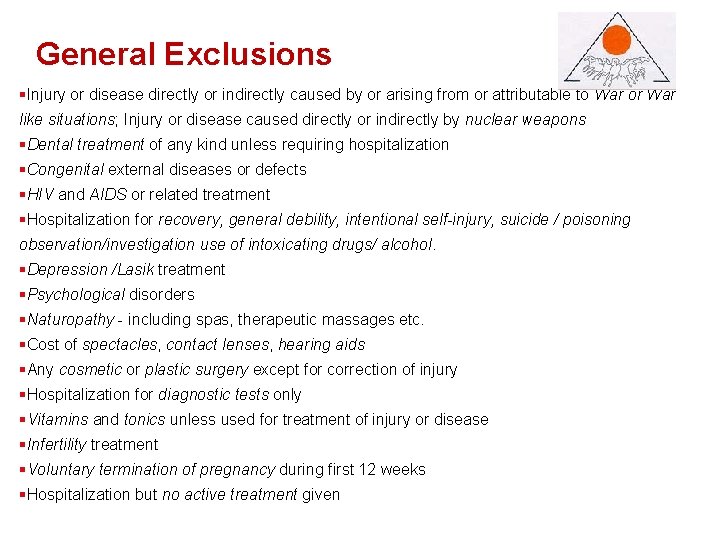
General. Exclusions §Injury or disease directly or indirectly caused by or arising from or attributable to War or War like situations; Injury or disease caused directly or indirectly by nuclear weapons §Dental treatment of any kind unless requiring hospitalization §Congenital external diseases or defects §HIV and AIDS or related treatment §Hospitalization for recovery, general debility, intentional self-injury, suicide / poisoning observation/investigation use of intoxicating drugs/ alcohol. §Depression /Lasik treatment §Psychological disorders §Naturopathy - including spas, therapeutic massages etc. §Cost of spectacles, contact lenses, hearing aids §Any cosmetic or plastic surgery except for correction of injury §Hospitalization for diagnostic tests only §Vitamins and tonics unless used for treatment of injury or disease §Infertility treatment §Voluntary termination of pregnancy during first 12 weeks §Hospitalization but no active treatment given Back
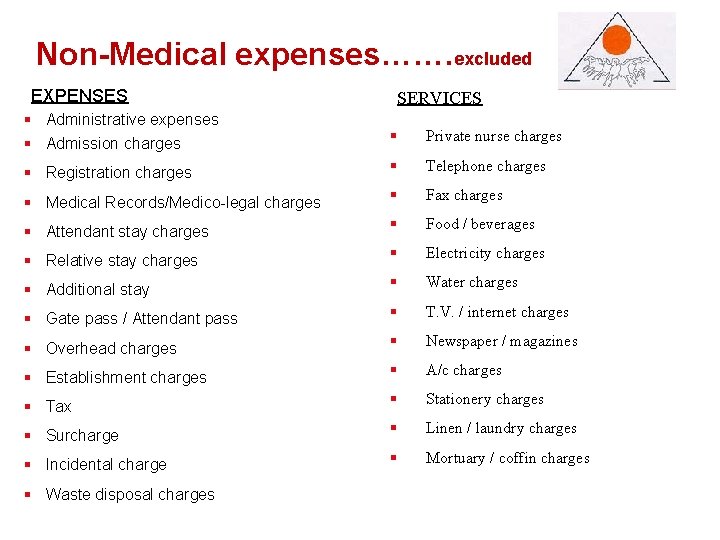
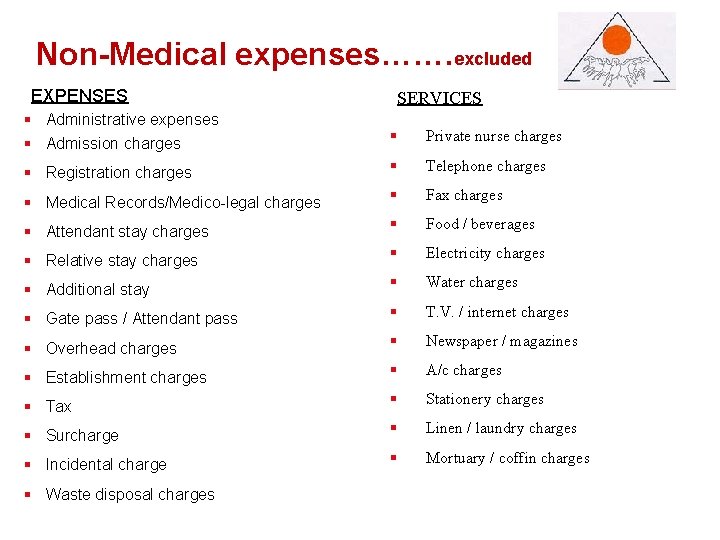
Non-Medicalexpenses……. excluded EXPENSES SERVICES § Administrative expenses § Admission charges § Private nurse charges § Registration charges § Telephone charges § Medical Records/Medico-legal charges § Fax charges § Attendant stay charges § Food / beverages § Relative stay charges § Electricity charges § Additional stay § Water charges § Gate pass / Attendant pass § T. V. / internet charges § Overhead charges § Newspaper / magazines § Establishment charges § A/c charges § Tax § Stationery charges § Surcharge § Linen / laundry charges § Incidental charge § Mortuary / coffin charges § Waste disposal charges
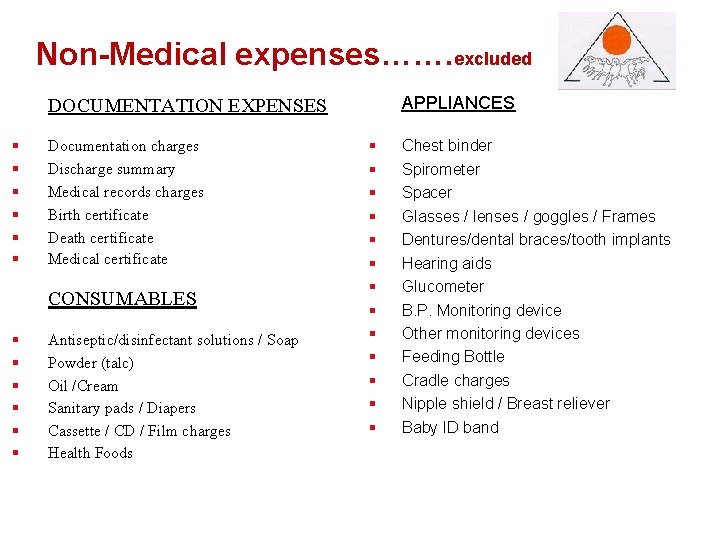
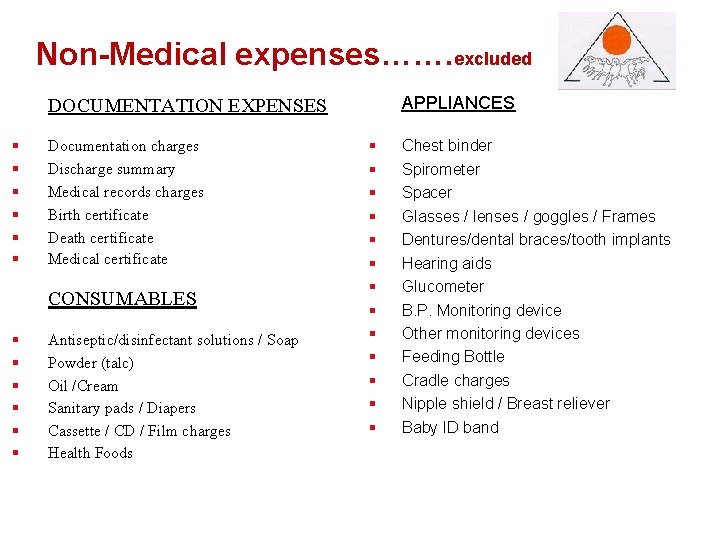
Non-Medicalexpenses……. excluded APPLIANCES DOCUMENTATION EXPENSES § § § Documentation charges Discharge summary Medical records charges Birth certificate Death certificate Medical certificate CONSUMABLES § § § Antiseptic/disinfectant solutions / Soap Powder (talc) Oil /Cream Sanitary pads / Diapers Cassette / CD / Film charges Health Foods § § § § Chest binder Spirometer Spacer Glasses / lenses / goggles / Frames Dentures/dental braces/tooth implants Hearing aids Glucometer B. P. Monitoring device Other monitoring devices Feeding Bottle Cradle charges Nipple shield / Breast reliever Baby ID band
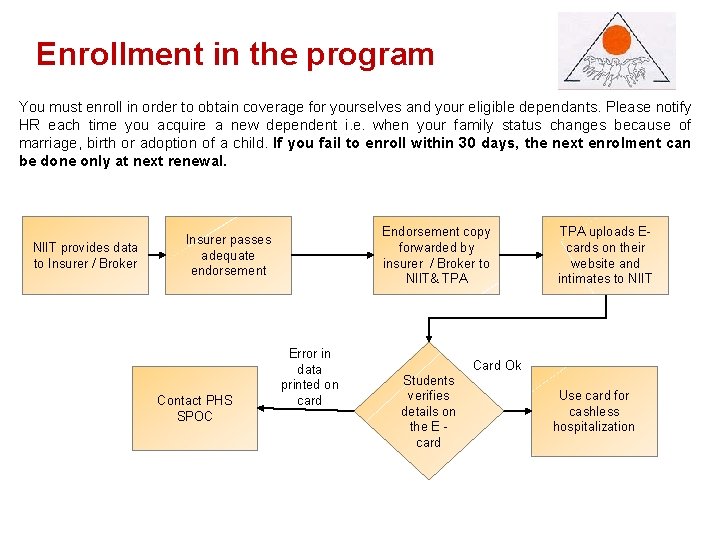
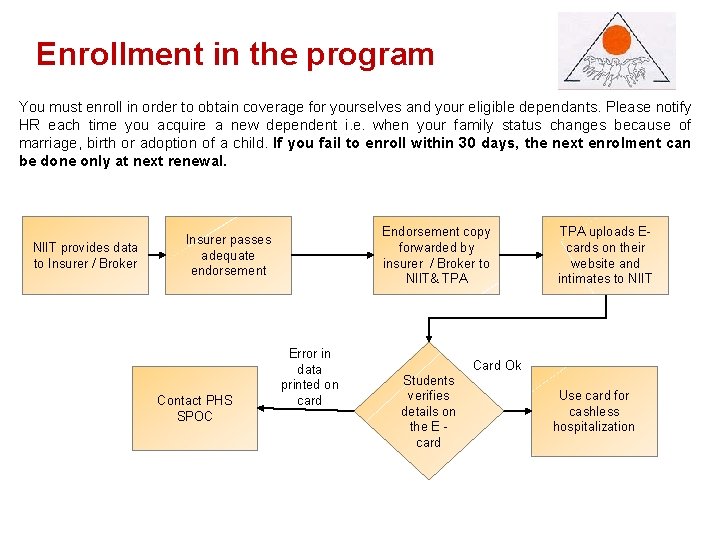
Enrollmentin inthe theprogram You must enroll in order to obtain coverage for yourselves and your eligible dependants. Please notify HR each time you acquire a new dependent i. e. when your family status changes because of marriage, birth or adoption of a child. If you fail to enroll within 30 days, the next enrolment can be done only at next renewal. NIIT provides data to Insurer / Broker Endorsement copy forwarded by insurer / Broker to NIIT& TPA Insurer passes adequate endorsement Contact PHS SPOC Error in data printed on card Students verifies details on the E card TPA uploads Ecards on their website and intimates to NIIT Card Ok Use card for cashless hospitalization Back
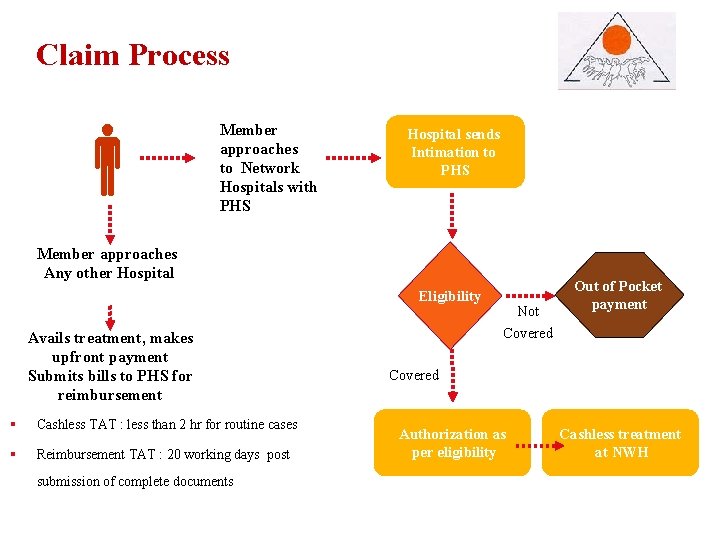
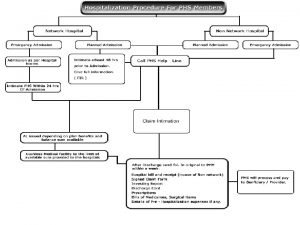
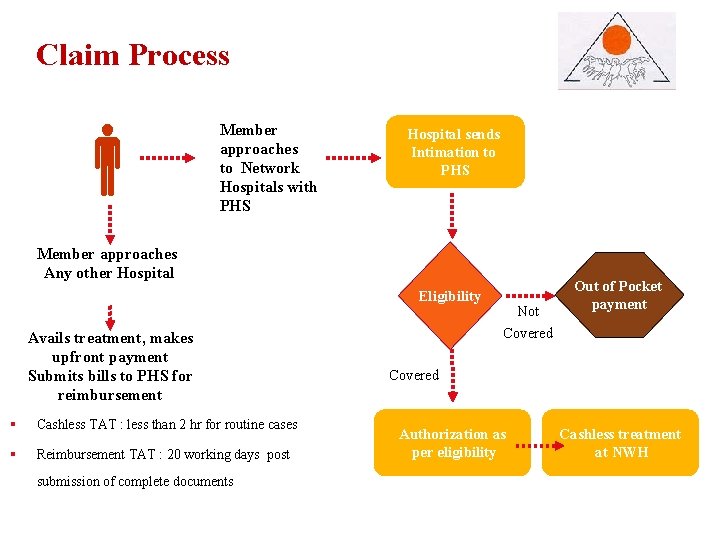
Claim. Process Member approaches to Network Hospitals with PHS Hospital sends Intimation to PHS Member approaches Any other Hospital Eligibility Avails treatment, makes upfront payment Submits bills to PHS for reimbursement § Cashless TAT : less than 2 hr for routine cases § Reimbursement TAT : 20 working days post submission of complete documents Not Covered Out of Pocket payment Covered Authorization as per eligibility Cashless treatment at NWH Back
Cashless. Hospitalization Cashless hospitalization means the Insurer may authorize upon a Policyholder’s request for direct settlement of eligible services and it’s according charges between a Network Hospital and the Insurer. In such cases the Insurer will directly settle all eligible amounts with the Network Hospital and the Insured Person may not have to pay any deposits at the commencement of the treatment or bills after the end of treatment to the extent as these services are covered under the Policy. List of hospitals in the TPA’s network eligible for cashless hospitalization Website: www. paramounttpa. com 24 X 7 Customer Service Center: - 1800226655 +91 -41637594 -95 -96 (Hotline) +91 -41637592, 42890921, 42890927 (Fax)

Reimbursement. Claim. Process Admission procedure In case you choose a non-network hospital you will have to liaise directly for admission. However you are advised to follow the pre authorization procedure to ensure eligibility for reimbursement of hospitalization expenses from the insurer. Discharge procedure In case of non network hospital, you will be required to clear the bill and submit a claim to insurer for reimbursement. Please ensure that you collect all necessary documents such as – discharge summary, investigation reports etc. for submitting your claim. Submission of hospitalization claim After the hospitalization is complete and the patient has been discharged from the hospital, you must submit the final claim within 15 days from the date of discharge from the hospital. (Applicable in case of Non Network hospital) Claims Process Claim Docs Back
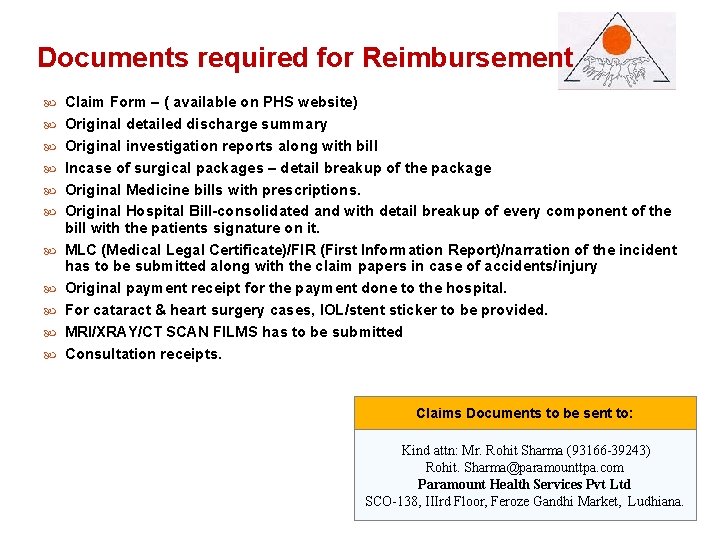
Documentsrequiredfor for. Reimbursement Claim Form – ( available on PHS website) Original detailed discharge summary Original investigation reports along with bill Incase of surgical packages – detail breakup of the package Original Medicine bills with prescriptions. Original Hospital Bill-consolidated and with detail breakup of every component of the bill with the patients signature on it. MLC (Medical Legal Certificate)/FIR (First Information Report)/narration of the incident has to be submitted along with the claim papers in case of accidents/injury Original payment receipt for the payment done to the hospital. For cataract & heart surgery cases, IOL/stent sticker to be provided. MRI/XRAY/CT SCAN FILMS has to be submitted Consultation receipts. Claims Documents to be sent to: Kind attn: Mr. Rohit Sharma (93166 -39243) Rohit. Sharma@paramounttpa. com Paramount Health Services Pvt Ltd Back SCO-138, IIIrd Floor, Feroze Gandhi Market, Ludhiana.
Pointsto to. Remember Cashless request must be reached within 24 hours of hospitalization. For re-imbursement cases, Intimation should be received within 24 hrs of admission in the hospital. Bills and documents to be submitted within 30 days from Date of Discharge of the hospital for reimbursement. For Pre-Post Claim, the maximum time allowed for submission of claim is with in 67 days of discharge from the Hospital. Carry your office ID card & E Card (PHS) at the time of admission at network hospitals. In case of emergency kindly refer your PHS ID, Organization Name and your Roll no. at the time of admission. Take a pre approval from PHS for all the elective cases/planned hospitalizations Sign on the final bill at the time of discharge from the hospital after checking For any other assistance call the Account Manager (Mr. Rohit Sharma ).
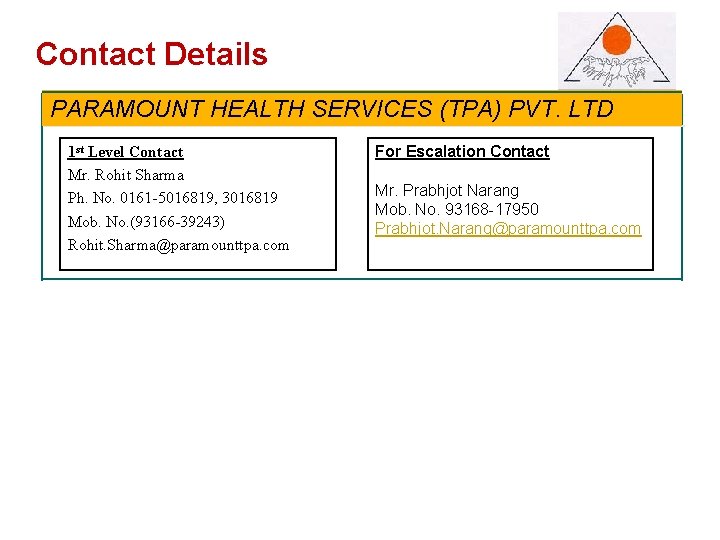
Contact. Details PARAMOUNT HEALTH SERVICES (TPA) PVT. LTD 1 st Level Contact Mr. Rohit Sharma Ph. No. 0161 -5016819, 3016819 Mob. No. (93166 -39243) Rohit. Sharma@paramounttpa. com For Escalation Contact Mr. Prabhjot Narang Mob. No. 93168 -17950 Prabhjot. Narang@paramounttpa. com Proceed
Take Care… Do take care of your own & family’s health so that You do not need to use this Claims Process Claim Docs Back
Take Care… Thank You for kind presence Paramount – Your Link to Good Health Claims Process Claim Docs Back
 Paramount preauth form
Paramount preauth form Paramount health insurance preauth form
Paramount health insurance preauth form Raksha health insurance tpa pvt ltd
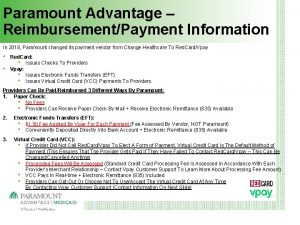
Raksha health insurance tpa pvt ltd Paramount advantage providers
Paramount advantage providers Paramount portal
Paramount portal Words that are subordinating conjunctions
Words that are subordinating conjunctions Paramount lighting setup
Paramount lighting setup Metro goldwyn mayer columbia pictures
Metro goldwyn mayer columbia pictures Paramount triple sec
Paramount triple sec Les hazlewood
Les hazlewood Kapgrow corporate advisory services pvt. ltd
Kapgrow corporate advisory services pvt. ltd Jagruti technical services pvt ltd photos
Jagruti technical services pvt ltd photos Jagruti technical services pvt ltd photos
Jagruti technical services pvt ltd photos Indo asia leisure services ltd
Indo asia leisure services ltd Indivirtus healthcare services pvt ltd
Indivirtus healthcare services pvt ltd Ravensdown shipping
Ravensdown shipping Feathers management
Feathers management Advanced facility management services
Advanced facility management services Acl audit exchange
Acl audit exchange Team plus hr services pvt ltd
Team plus hr services pvt ltd Dotcom services india pvt ltd
Dotcom services india pvt ltd Prudent broking
Prudent broking