SYSTEMIC SCLEROSIS Pathogenesis Vasculopathy Activated endothelial cells release
- Slides: 29
SYSTEMIC SCLEROSIS
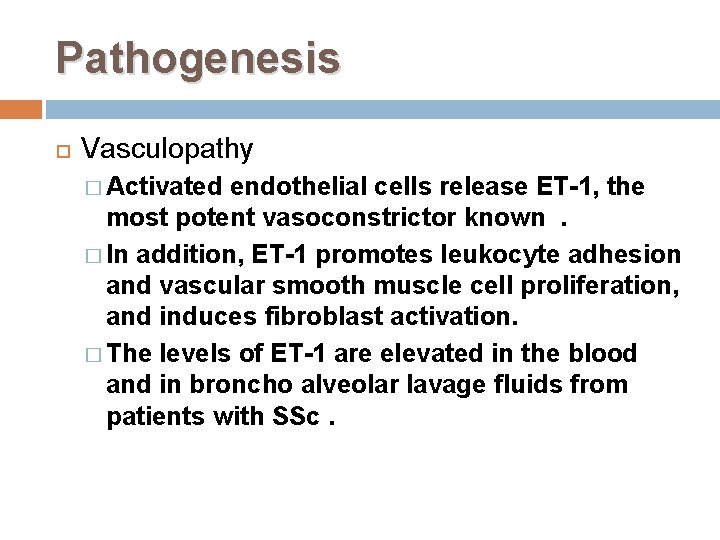
Pathogenesis Vasculopathy � Activated endothelial cells release ET-1, the most potent vasoconstrictor known. � In addition, ET-1 promotes leukocyte adhesion and vascular smooth muscle cell proliferation, and induces fibroblast activation. � The levels of ET-1 are elevated in the blood and in broncho alveolar lavage fluids from patients with SSc.
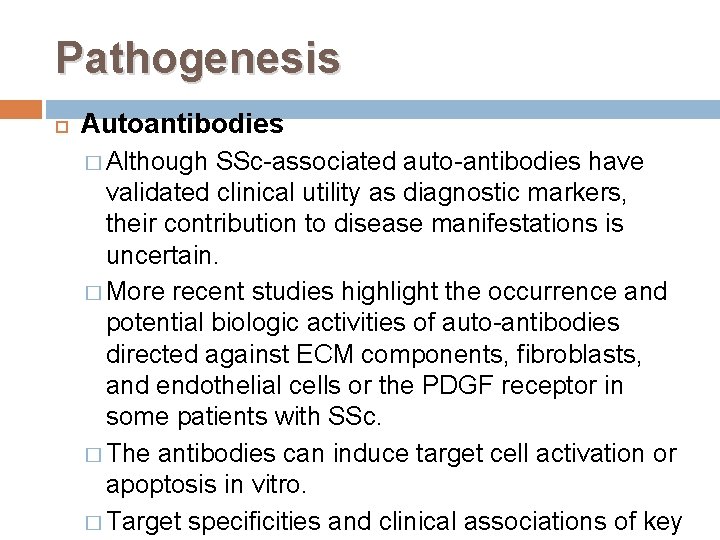
Pathogenesis Autoantibodies � Although SSc-associated auto-antibodies have validated clinical utility as diagnostic markers, their contribution to disease manifestations is uncertain. � More recent studies highlight the occurrence and potential biologic activities of auto-antibodies directed against ECM components, fibroblasts, and endothelial cells or the PDGF receptor in some patients with SSc. � The antibodies can induce target cell activation or apoptosis in vitro. � Target specificities and clinical associations of key
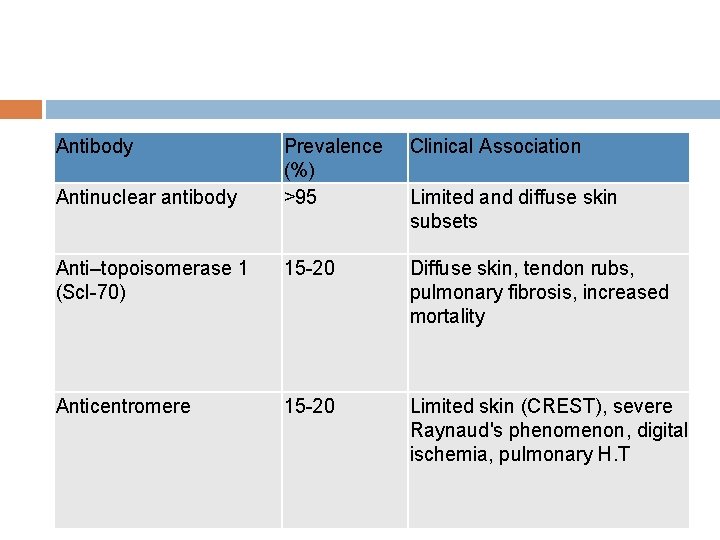
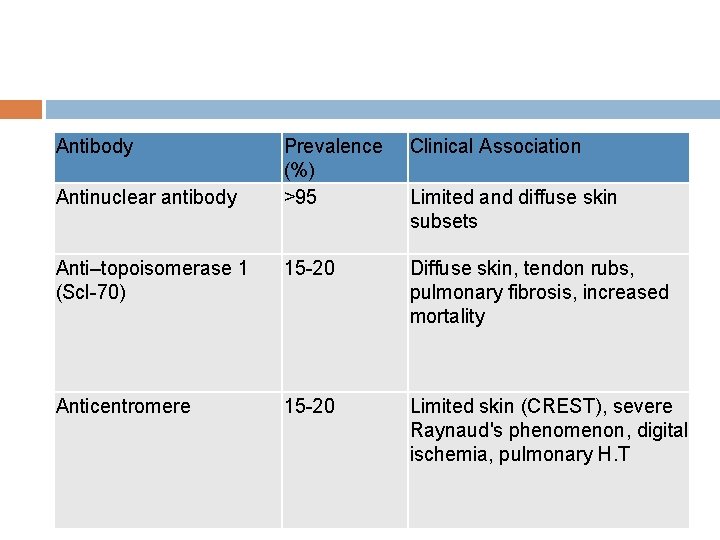
Antibody Prevalence (%) >95 Clinical Association Anti–topoisomerase 1 (Scl-70) 15 -20 Diffuse skin, tendon rubs, pulmonary fibrosis, increased mortality Anticentromere 15 -20 Limited skin (CREST), severe Raynaud's phenomenon, digital ischemia, pulmonary H. T Antinuclear antibody Limited and diffuse skin subsets
Pathogenesis Platelet derived growth factor � Platelet-Derived Growth Factor(PDGFs) are disulfide-bonded hetero dimeric proteins consisting of an A and a B chain that act mainly on stromal cells and regulate the wound healing process. � Originally isolated from platelets, PDGF isoforms also are produced by macrophages, endothelial cells, and fibroblasts. PDGF is a potent fibroblast mitogen and chemo-attractant for fibroblasts; induces the synthesis of collagen, fibronectin, and proteoglycans; and stimulates the secretion of TGF-β 1 and IL-6. � Fibroblasts from patients with SSc show elevated expression of PDGF and PDGF-β receptor and PDGF levels are increased in broncho-alveolar lavage fluid. � Serum antibodies to the PDGF receptor from patients with SSc induce fibroblast activation in vitro; however, stimulatory antibodies to the PDGF receptor are not specific for SSc and have been detected in the sera of patients with graft-versushost disease as well.
Pathogenesis Interferon-γ IFN-γ, produced primarily by Th 1 lymphocytes, is a major negative regulator of collagen gene expression and fibroblast activation and abrogates stimulation induced by TGF-β. IFN-γ also is a potent inhibitor of fibroblast proliferation, fibroblast-mediated matrix contraction, and myofibroblast trans-differentiation. Significantly, some studies have shown that fibroblasts from patients with SSc are resistant to the inhibitory effects of IFN-γ Clinical trials of IFN-γ in SSc have shown a modest and inconsistent improvement in skin fibrosis.
CLINICAL FEATURES Fatigue and lethargy are common throughout the illness, although usually more pronounced in its early phases. Reactive depression is a frequent accompaniment to this often relentless and disfiguring disorder. Patients often feel isolated or depressed, and support groups can provide an invaluable service to them.
SKIN MANIFESTATIONS Skin thickening and hardening are the hallmarks of SSc. In patients with limited cutaneous SSc, skin changes generally are restricted to the hands and face, with some extension to the neck and forearms, and are generally preceded by Raynaud's phenomenon. Different patterns of skin involvement can develop. In some cases, there is puffiness and swelling of the skin, especially over the digits. In other cases, the skin changes are more atrophic with tightened fingers and loss of subcutaneous tissue. Complications of digital ischemia including pitting scars and ulceration occur Careful assessment of the extent of skin involvement is the best clinical technique for detecting the patient at risk for life-threatening internal organ involvement.
Raynaud's phenomenon It is classically manifest by episodic pallor of the digits followed by cyanosis, suffusion, and/or pain and tingling. This blanching reflects digital arterial vasospasm, the cyanosis the de-oxygenation of static venous blood, and the redness reactive hyper-aemia following the return of blood flow. Continuous blanching, blueness, or pain is not Raynaud's phenomenon and to have implications for autoimmune rheumatic disease the phenomenon must be biphasic and episodic. Important clues to secondary Raynaud's on clinical evaluation are: The development of Raynaud's either in very young children or after the age of 45 years; � Severe symptoms occurring all year round; � Digital ulcerations, which rarely, if ever occur in primary Raynaud's; �
Systemic features of disease
Gastrointestinal tract Mouth : Tight skin, Dental caries : Esophagus Dysmobility/oesophageal spasm, Dysphagia diagnosed Barium swallow treated Protonpump inhibitors Reflux oesophagitis Heartburn treated Elevate head of bed Stricture Dysphagia Endoscopy, Avoid late meals Stomach: Gastric paresis, NSAID-related ulcer, Early satiety treated by proton pump inhibitor& prokinetic. Small bowel: Hypomotility, Stasis, Bacterial overgrowth , NSAID enteropathy, Pseudo-obstruction , Pneumatosis intestinalis
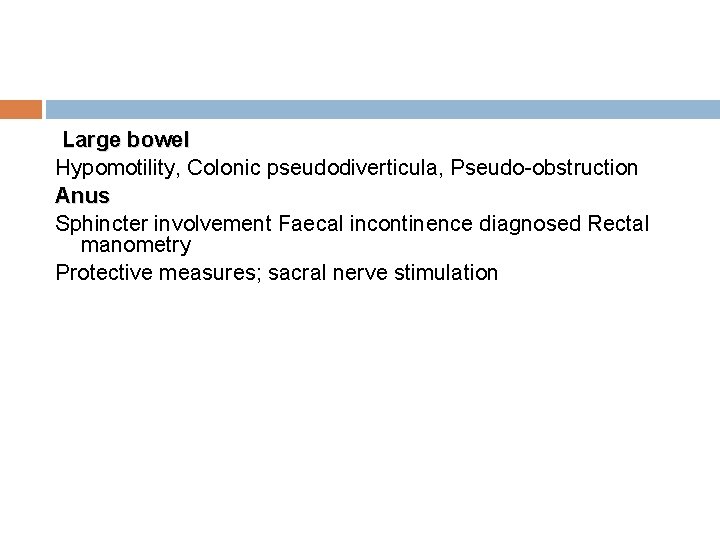
Large bowel Hypomotility, Colonic pseudodiverticula, Pseudo-obstruction Anus Sphincter involvement Faecal incontinence diagnosed Rectal manometry Protective measures; sacral nerve stimulation
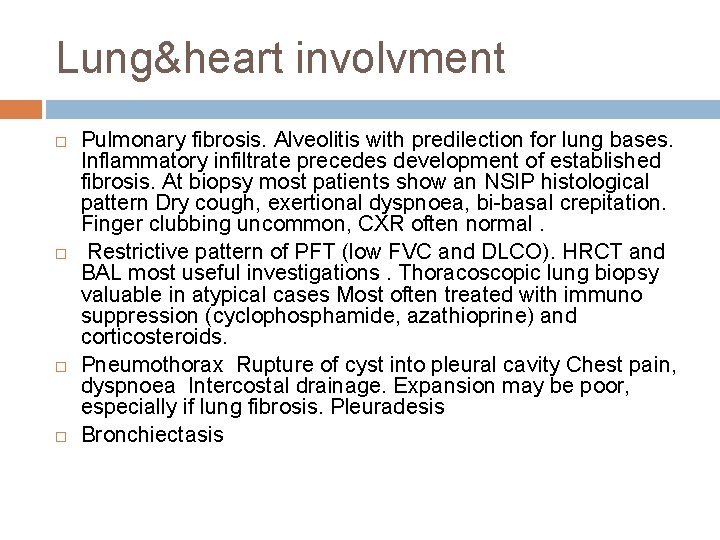
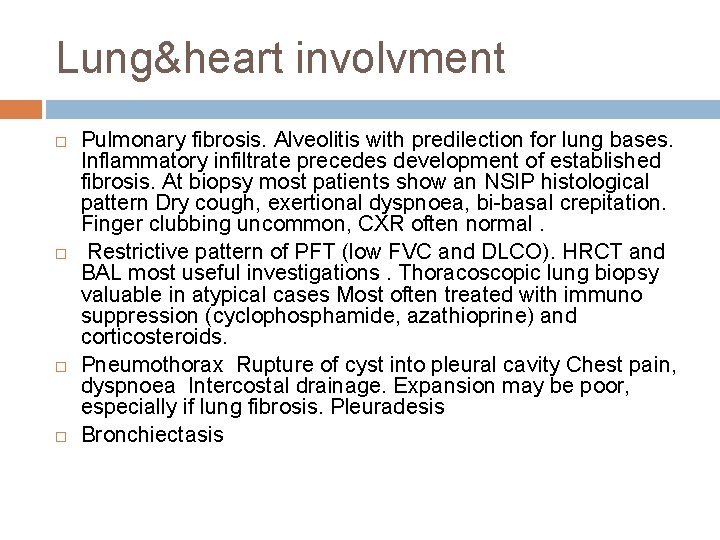
Lung&heart involvment Pulmonary fibrosis. Alveolitis with predilection for lung bases. Inflammatory infiltrate precedes development of established fibrosis. At biopsy most patients show an NSIP histological pattern Dry cough, exertional dyspnoea, bi-basal crepitation. Finger clubbing uncommon, CXR often normal. Restrictive pattern of PFT (low FVC and DLCO). HRCT and BAL most useful investigations. Thoracoscopic lung biopsy valuable in atypical cases Most often treated with immuno suppression (cyclophosphamide, azathioprine) and corticosteroids. Pneumothorax Rupture of cyst into pleural cavity Chest pain, dyspnoea Intercostal drainage. Expansion may be poor, especially if lung fibrosis. Pleuradesis Bronchiectasis
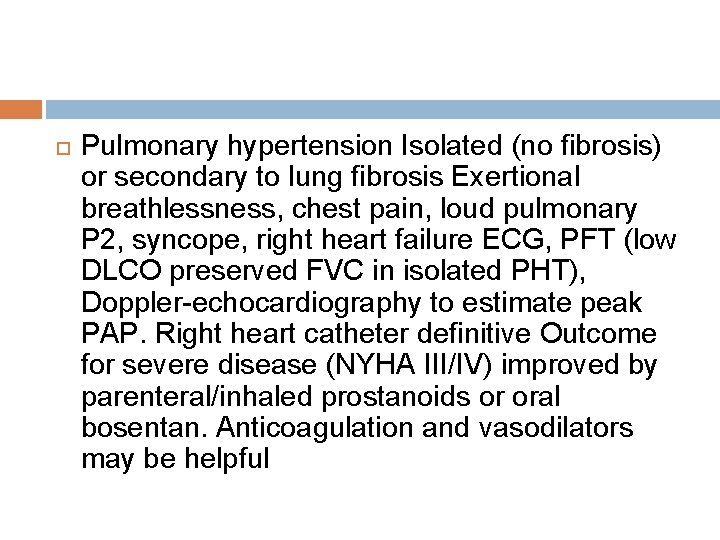
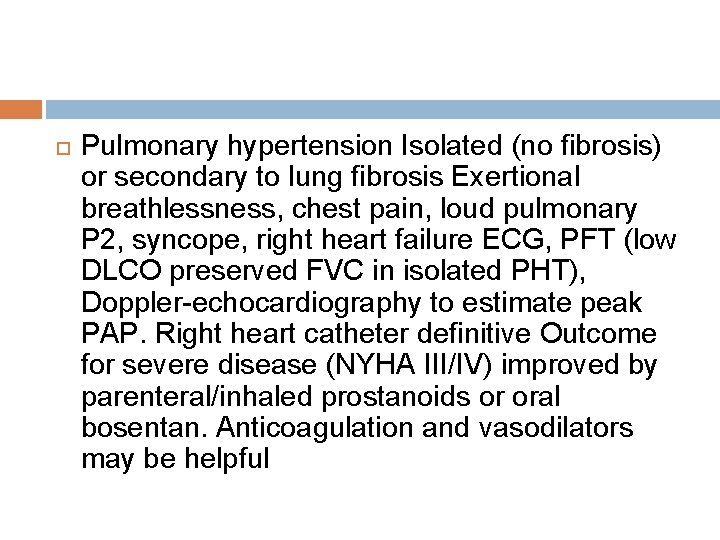
Pulmonary hypertension Isolated (no fibrosis) or secondary to lung fibrosis Exertional breathlessness, chest pain, loud pulmonary P 2, syncope, right heart failure ECG, PFT (low DLCO preserved FVC in isolated PHT), Doppler-echocardiography to estimate peak PAP. Right heart catheter definitive Outcome for severe disease (NYHA III/IV) improved by parenteral/inhaled prostanoids or oral bosentan. Anticoagulation and vasodilators may be helpful
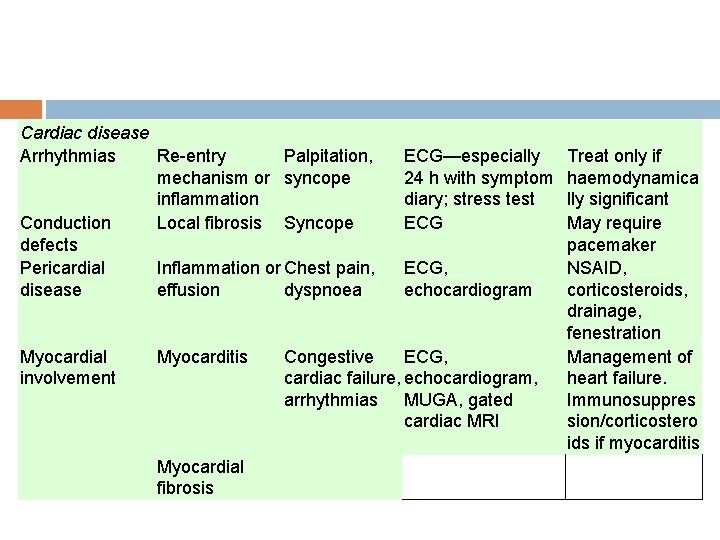
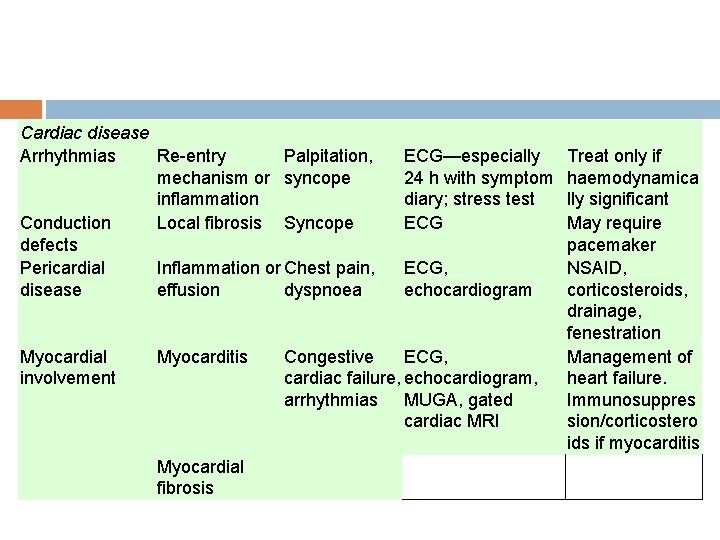
Cardiac disease Arrhythmias Re-entry Palpitation, mechanism or syncope inflammation Conduction Local fibrosis Syncope defects Pericardial Inflammation or Chest pain, disease effusion dyspnoea Myocardial involvement Myocarditis Myocardial fibrosis ECG—especially 24 h with symptom diary; stress test ECG, echocardiogram Congestive ECG, cardiac failure, echocardiogram, arrhythmias MUGA, gated cardiac MRI Treat only if haemodynamica lly significant May require pacemaker NSAID, corticosteroids, drainage, fenestration Management of heart failure. Immunosuppres sion/corticostero ids if myocarditis
MUSCULOSKELETAL INVOLVEMENT Joints � The fibrotic process of SSc commonly affects the tendons (causing tendon friction rubs), ligaments, and joint capsules, restricting movement. In addition, fibrosis is found in the synovium, but frank arthritis and joint destruction are uncommon. � Arthralgia is common, especially in the early stage of the diffuse cutaneous form of SSc
Skeletal Muscle Involvement muscle weakness and atrophy may result from disuse secondary to joint contractures or chronic disease, about 20% of SSc patients develop a true myopathy characterized by mild chronic weakness and atrophy, minimal elevation of creatine phosphokinase, subtle abnormalities on electromyography, and modest noninflammatory histologic alterations with focal replacement of myofibrils with collagen and perimysial and epimysial fibrosis.
Renal disease q q q characterized pattern of renal involvement in systemic sclerosis is an acute or subacute renal hypertensive crisis. This generally occurs in patients with diffuse systemic sclerosis criteria to diagnose scleroderma renal crisis: 1 -abrupt onset of arterial hypertension greater than 160/90 mm. Hg; 2 - hypertensive retinopathy of at least grade III severity; 3 - and rapid deterioration of renal function and elevated plasma renin activity. Other typical features include the presence of a microangiopathic haemolytic blood film and hypertensive encephalopathy, often complicated by generalized
Patients usually present with the clinical features of severe hypertension, including head aches, visual disturbances, hypertensive encephalopathy (especially seizures), and pulmonary oedema. Occasionally a similar pattern of renal dysfunction occurs without hypertension (normotensive renal crisis), suggesting that the pathological features are not simply the end-organ consequences of raised arterial pressure Management of renal systemic sclerosis requires a high index of suspicion to enable early diagnosis and treatment of the renal crisis. Creatinine clearance or isotope glomerular filtration rate should be checked twice yearly in diffuse cutaneous systemic sclerosis for the first 5 years and annually thereafter
Blood pressure should be well controlled (often antihypertensive treatments also help Raynaud's symptoms) and in diffuse cutaneous systemic sclerosis the use of angiotensin-converting enzyme inhibitors is particularly appropriate since there is some anecdotal evidence that they protect from hypertensive crisis. High-dose corticosteroids have now been formally demonstrated in a case–control study to increase the risk of renal crisis in diffuse cutaneous systemic sclerosis and doses above 20 mg prednisolone equivalent daily should be avoided
Once diagnosed, an acute renal crisis in systemic sclerosis must be treated as a medical emergency. The patient should be admitted immediately and reasonable control of the blood pressure is a priority. Hypertension should be treated with angiotensinconverting enzyme inhibitors (captopril or enalapril up to maximum dose) and calcium-channel blockers (starting with long-acting nifedipine initially), aiming to reduce both diastolic and systolic pressure by 20 mm. Hg in the first 48 h and ultimately maintaining diastolic pressure at 80– 90 mm. Hg. Intravenous prostacyclin, which is believed to help the microvascular lesion without precipitating hypotension, is often administered from diagnosis.
Renal function should be closely monitored by twice-weekly creatinine clearance and daily serum creatinine estimations. Regular full blood counts, clotting screening, and estimations of fibrin degradation product are important to monitor the degree of microangiopathic haemolytic anaemia, which often reflects the activity of the disease process. Short-term haemodialysis should be given if necessary and peritoneal dialysis often works well if long-term renal replacement therapy is needed.
TREATMENT management and outcome of scleroderma renal crisis has been transformed by the judicious use of ACE inhibitor Morbidity from Raynaud's phenomenon and esophagitis has been markedly reduced. Progress also has been made in treating PAH, and more recent reports indicate that immuno-suppression using cyclophosphamide may slow the progression of interstitial lung disease complicating SSc. Despite these positive developments, no SSc therapy to date has been proved to be effective in altering the natural history of the disease.
The choice and evaluation of any treatment regimen for SSc is challenging because the disease is complex, and its pathogenesis is poorly understood; it is heterogeneous in its extent, severity, and rate of progression. Treatment typically includes a combination of agents targeting the immune, vascular, and fibrotic processes underlying the pathogenesis of SSc. Therapy must be tailored to the individual patient, however, carefully taking into consideration disease subset and duration, rate of progression, and pattern and severity of internal organ involvement. Careful baseline assessment of organ-based complications and long-term follow-up are essential.
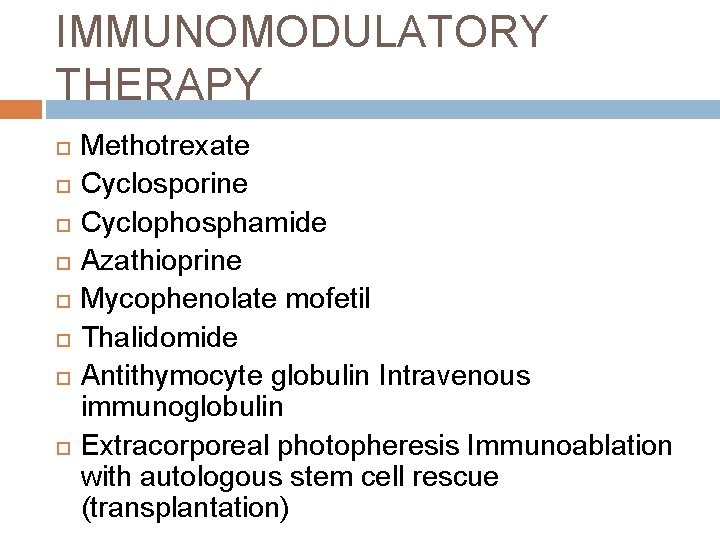
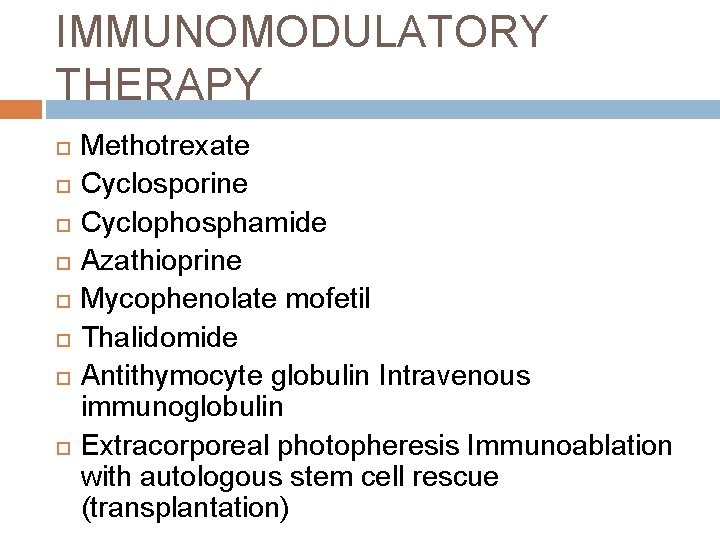
IMMUNOMODULATORY THERAPY Methotrexate Cyclosporine Cyclophosphamide Azathioprine Mycophenolate mofetil Thalidomide Antithymocyte globulin Intravenous immunoglobulin Extracorporeal photopheresis Immunoablation with autologous stem cell rescue (transplantation)
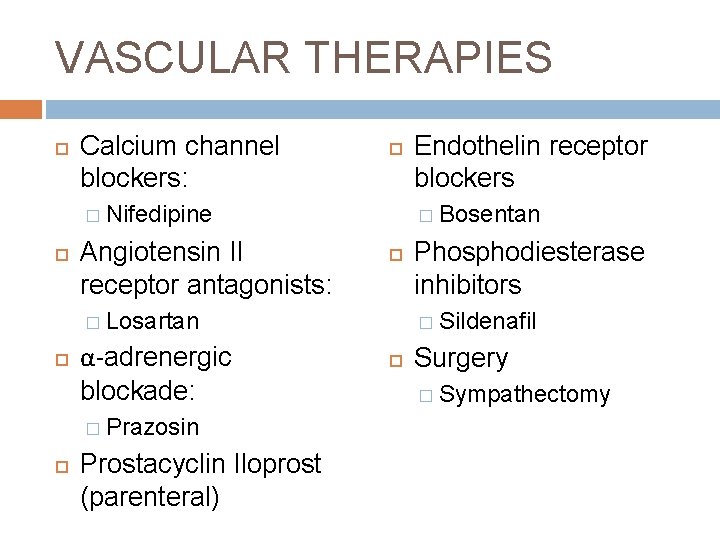
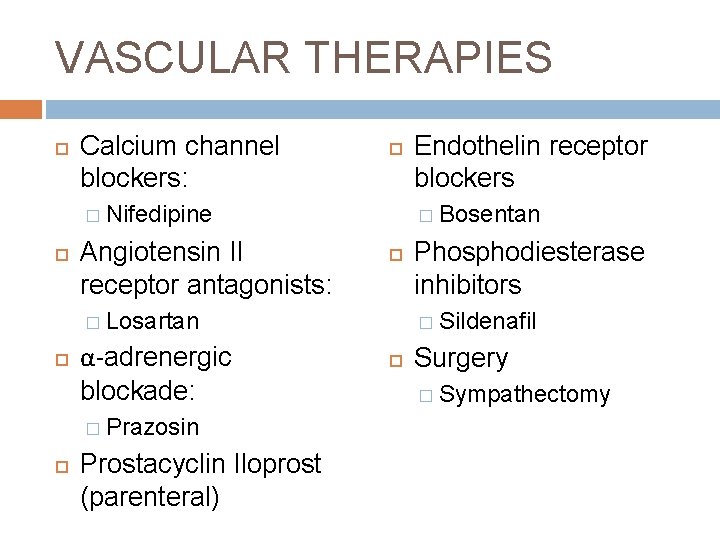
VASCULAR THERAPIES Calcium channel blockers: � Nifedipine Angiotensin II receptor antagonists: � Bosentan � Losartan α-adrenergic blockade: � Prazosin Prostacyclin Iloprost (parenteral) Endothelin receptor blockers Phosphodiesterase inhibitors � Sildenafil Surgery � Sympathectomy
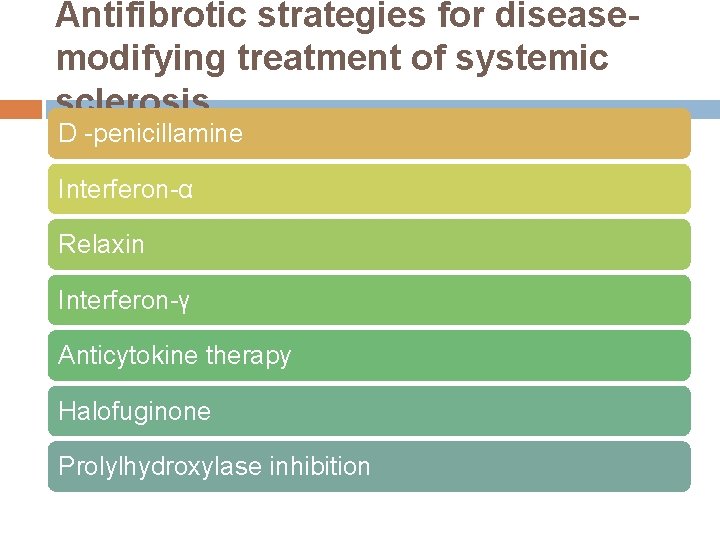
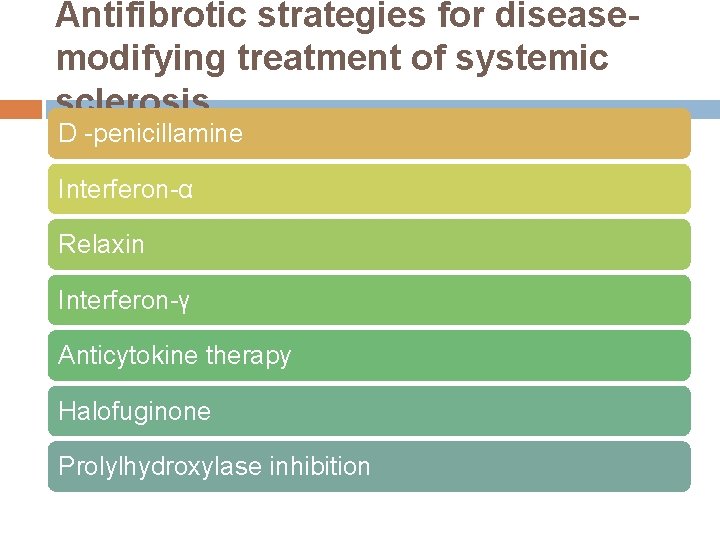
Antifibrotic strategies for diseasemodifying treatment of systemic sclerosis D -penicillamine Interferon-α Relaxin Interferon-γ Anticytokine therapy Halofuginone Prolylhydroxylase inhibition
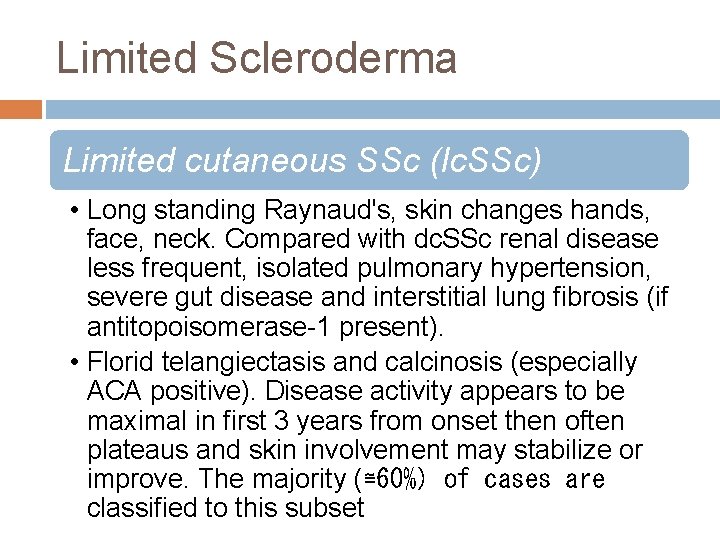
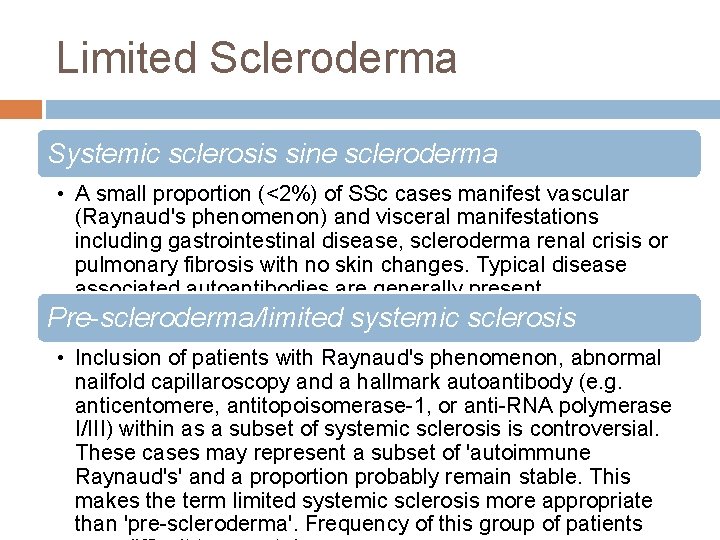
Limited Scleroderma Limited cutaneous SSc (lc. SSc) • Long standing Raynaud's, skin changes hands, face, neck. Compared with dc. SSc renal disease less frequent, isolated pulmonary hypertension, severe gut disease and interstitial lung fibrosis (if antitopoisomerase-1 present). • Florid telangiectasis and calcinosis (especially ACA positive). Disease activity appears to be maximal in first 3 years from onset then often plateaus and skin involvement may stabilize or improve. The majority (≅60%) of cases are classified to this subset
Limited Scleroderma Systemic sclerosis sine scleroderma • A small proportion (<2%) of SSc cases manifest vascular (Raynaud's phenomenon) and visceral manifestations including gastrointestinal disease, scleroderma renal crisis or pulmonary fibrosis with no skin changes. Typical disease associated autoantibodies are generally present Pre-scleroderma/limited systemic sclerosis • Inclusion of patients with Raynaud's phenomenon, abnormal nailfold capillaroscopy and a hallmark autoantibody (e. g. anticentomere, antitopoisomerase-1, or anti-RNA polymerase I/III) within as a subset of systemic sclerosis is controversial. These cases may represent a subset of 'autoimmune Raynaud's' and a proportion probably remain stable. This makes the term limited systemic sclerosis more appropriate than 'pre-scleroderma'. Frequency of this group of patients