Supporting Dementia Patients and their Caregivers in the
- Slides: 27
Supporting Dementia Patients and their Caregivers in the Home Robert Burns MD and Linda Olivia Nichols, Ph. D Memphis Caregiver Center, VA Memphis Professors, Preventive and Internal Medicine University of Tennessee Health Science Center ©AAHCM
Disclosure � Robert Burns, M. D. and Linda O. Nichols, Ph. D. have no actual or potential conflict of interest in relation to these presentations ©AAHCM
Objectives � Discuss what a Family-Centered approach to home based dementia care would look like � Review national guidelines for dementia care and clinical outcomes � Briefly review evidence for drug based and non-drug regimens for treatment � Discuss strategies for helping caregivers manage patient behaviors and their own stress ©AAHCM
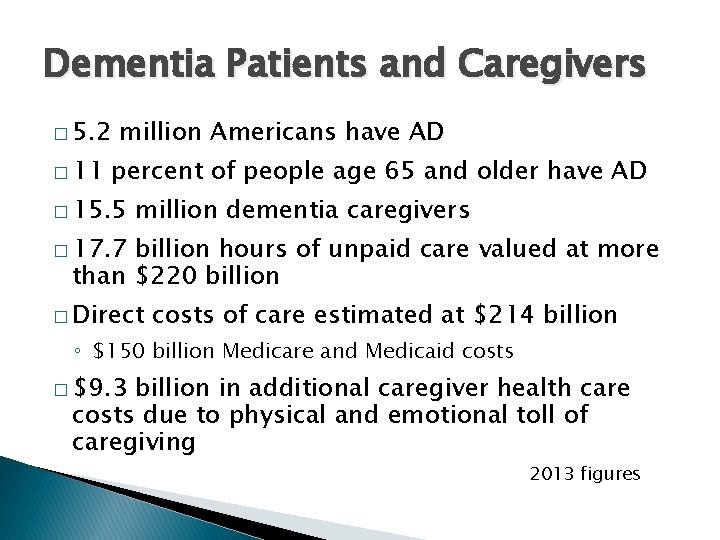
Dementia Patients and Caregivers � 5. 2 � 11 million Americans have AD percent of people age 65 and older have AD � 15. 5 million dementia caregivers � 17. 7 billion hours of unpaid care valued at more than $220 billion � Direct costs of care estimated at $214 billion ◦ $150 billion Medicare and Medicaid costs � $9. 3 billion in additional caregiver health care costs due to physical and emotional toll of caregiving 2013 figures
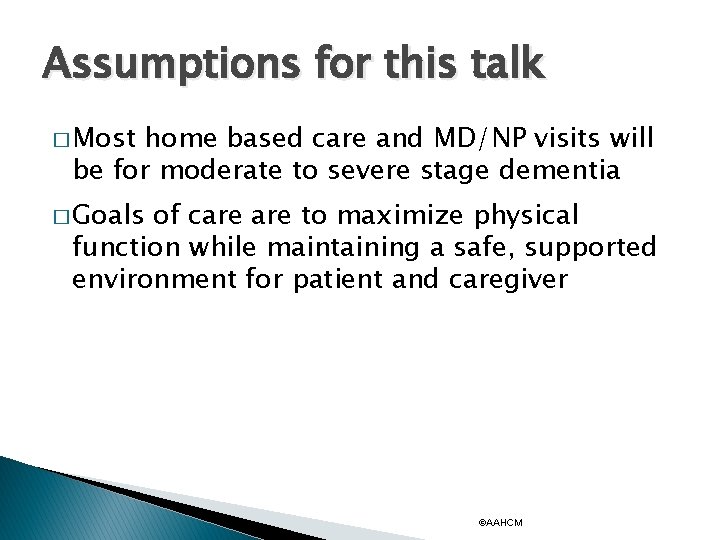
Assumptions for this talk � Most home based care and MD/NP visits will be for moderate to severe stage dementia � Goals of care to maximize physical function while maintaining a safe, supported environment for patient and caregiver ©AAHCM
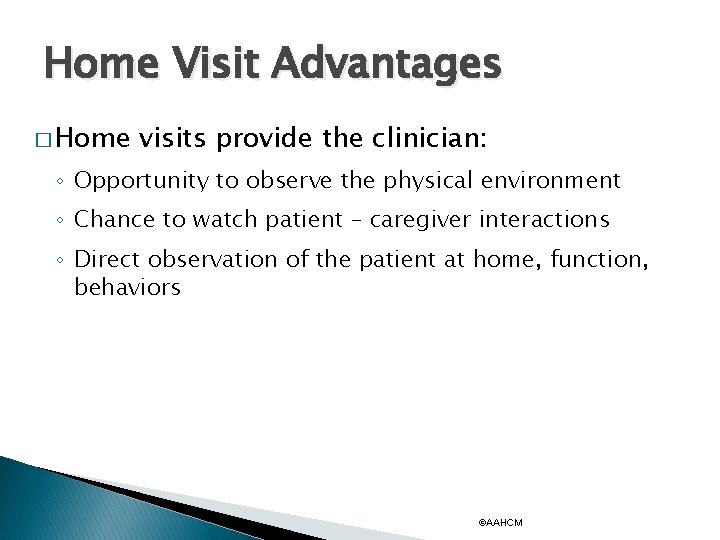
Home Visit Advantages � Home visits provide the clinician: ◦ Opportunity to observe the physical environment ◦ Chance to watch patient – caregiver interactions ◦ Direct observation of the patient at home, function, behaviors ©AAHCM
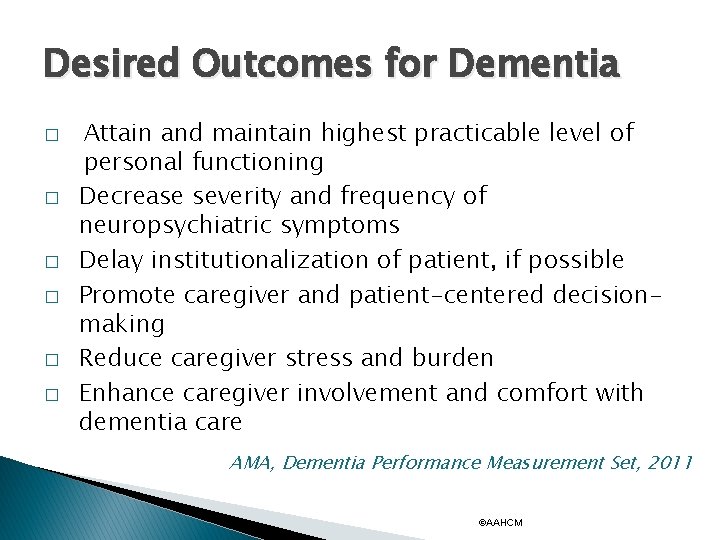
Desired Outcomes for Dementia � � � Attain and maintain highest practicable level of personal functioning Decrease severity and frequency of neuropsychiatric symptoms Delay institutionalization of patient, if possible Promote caregiver and patient-centered decisionmaking Reduce caregiver stress and burden Enhance caregiver involvement and comfort with dementia care AMA, Dementia Performance Measurement Set, 2011 ©AAHCM
Family Centered Dementia Care Plans � For moderate to severe stage dementia, focus will be on: ◦ Presentation of non-specific symptoms ◦ Developing a care plan when discussing diagnosis of “dementia” ◦ Easing guilt and worry and supporting the caregiver ©AAHCM
Family Centered Dementia Care Plans Treatment Plans � � � Essential features of effective chronic disease management programs tailored to individual Involvement of patient and/or family in customizing approach for patient Treatment plans customized for patient’s treatment preferences more likely to yield satisfied, adherent patients and families ©AAHCM
Family Centered Dementia Care Plans Treatment Plans � Utilize evidence based management of the dementia patient ◦ Data driven guidelines and protocols for assessment and drug utilization ◦ Evidence based behavioral interventions ◦ Team members to help educate caregivers �HMO disease specific phone support �HH nurse education ◦ When utilized, improve outcomes across disease conditions ©AAHCM
Self-Management Support � For dementia patients, management and education falls to primary caregivers � Emphasis on acquisition of skills, not just knowledge, especially important in managing difficult behaviors, and caregiver self care � Team members with specific skills for targeting skills and behavioral training ◦ MD/NP directed education of caregiver ◦ Telephone support ©AAHCM
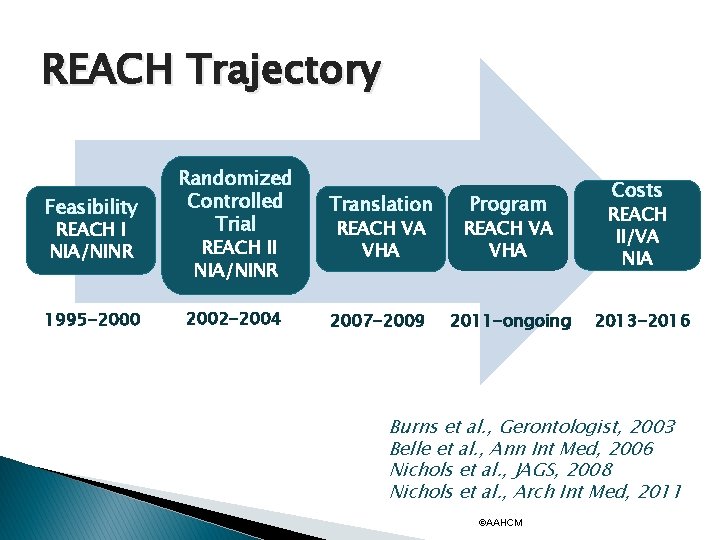
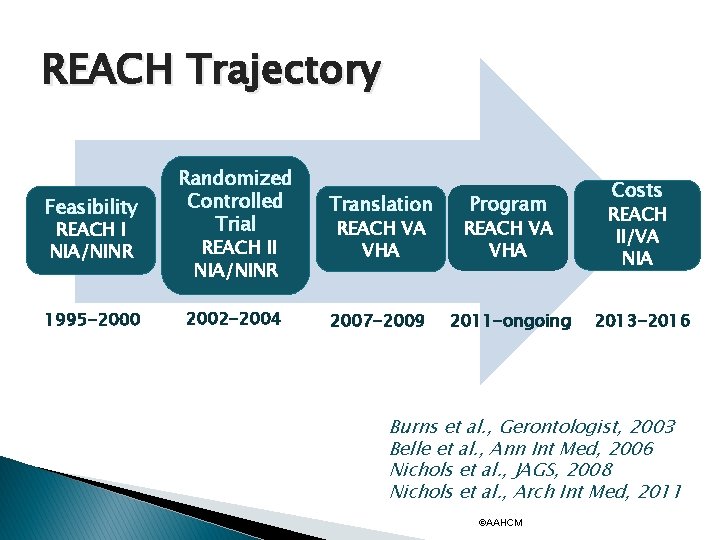
REACH Trajectory Feasibility REACH I NIA/NINR 1995 -2000 Randomized Controlled Trial Translation REACH VA VHA REACH II/VA NIA 2002 -2004 2007 -2009 2011 -ongoing 2013 -2016 REACH II NIA/NINR Program Costs Burns et al. , Gerontologist, 2003 Belle et al. , Ann Int Med, 2006 Nichols et al. , JAGS, 2008 Nichols et al. , Arch Int Med, 2011 ©AAHCM
Evidence Based Management Includes � Discussion of diagnosis and stage of illness with the caregiver � Limited benefit of cognitive enhancing drugs (ACh. EI and NMDA antagonists) � Discussion of risks/benefits of drug treatment of behavioral and psychological symptoms � Benefit of behavioral interventions and caregiver support ©AAHCM
Conclusions � � Home care visits can improve care of dementia patients by allowing provider to see patient environment and interactions Assessment of patient function and behaviors can allow a tailored, patient specific intervention Skills training of caregiver improves quality of life for both members of dyad Promotion of caregiver and patient-centered decision-making enhances success of caregiving ©AAHCM
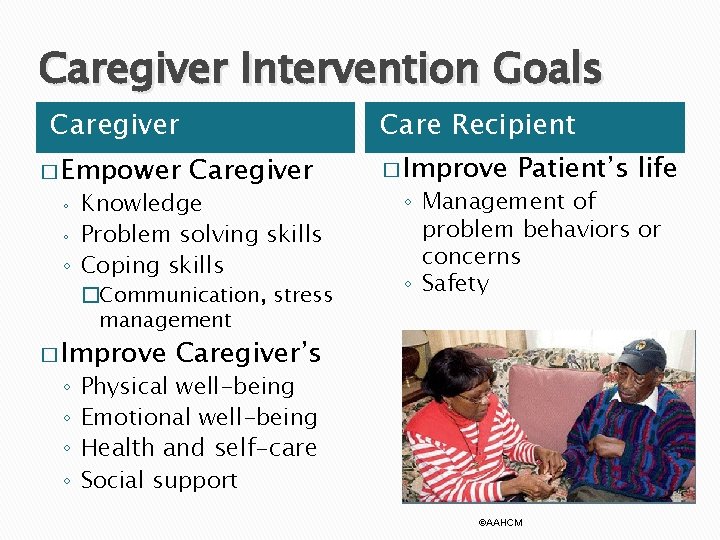
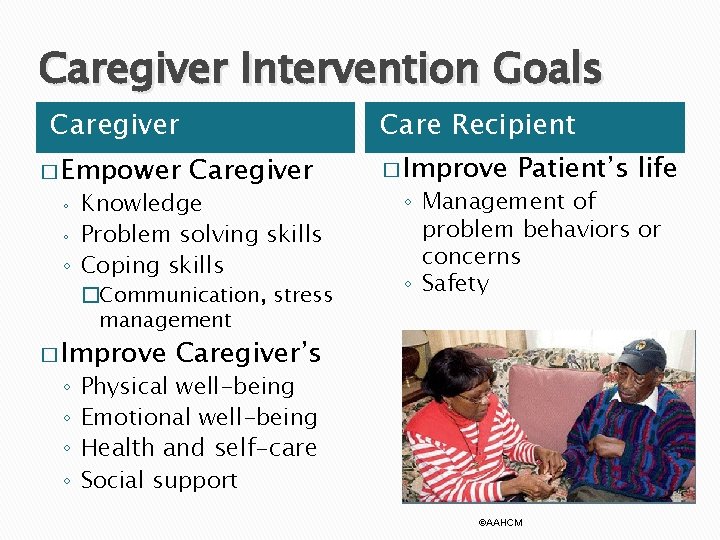
Caregiver Intervention Goals Caregiver � Empower Care Recipient Caregiver Knowledge ◦ Problem solving skills ◦ Coping skills ◦ �Communication, stress management � Improve ◦ ◦ � Improve Patient’s life ◦ Management of problem behaviors or concerns ◦ Safety Caregiver’s Physical well-being Emotional well-being Health and self-care Social support ©AAHCM
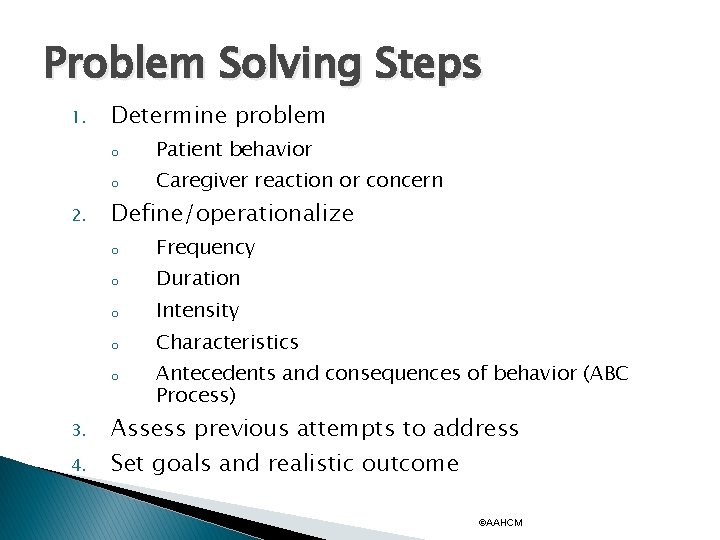
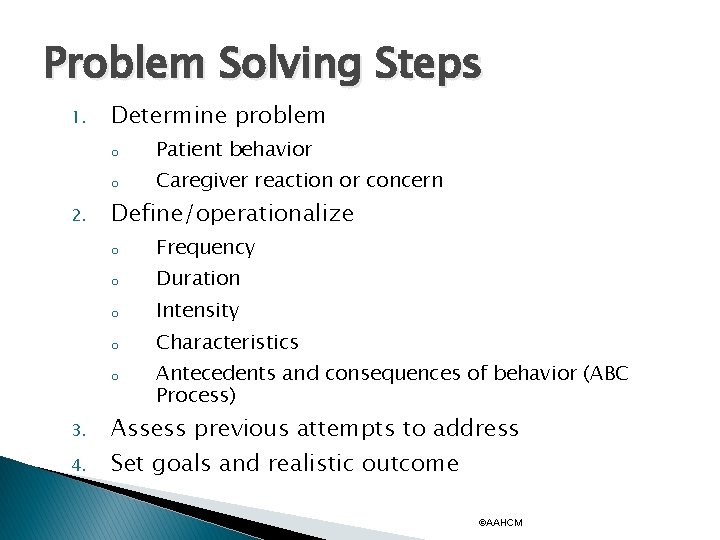
Problem Solving Steps 1. 2. Determine problem o Patient behavior o Caregiver reaction or concern Define/operationalize o Frequency o Duration o Intensity o Characteristics o 3. 4. Antecedents and consequences of behavior (ABC Process) Assess previous attempts to address Set goals and realistic outcome ©AAHCM
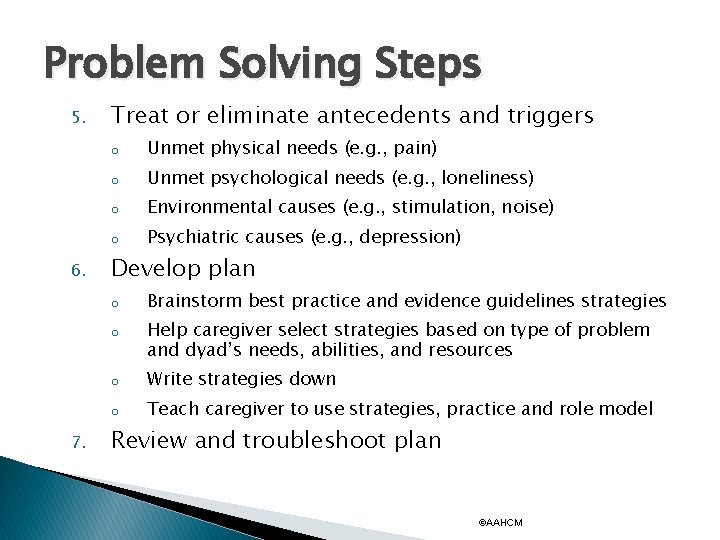
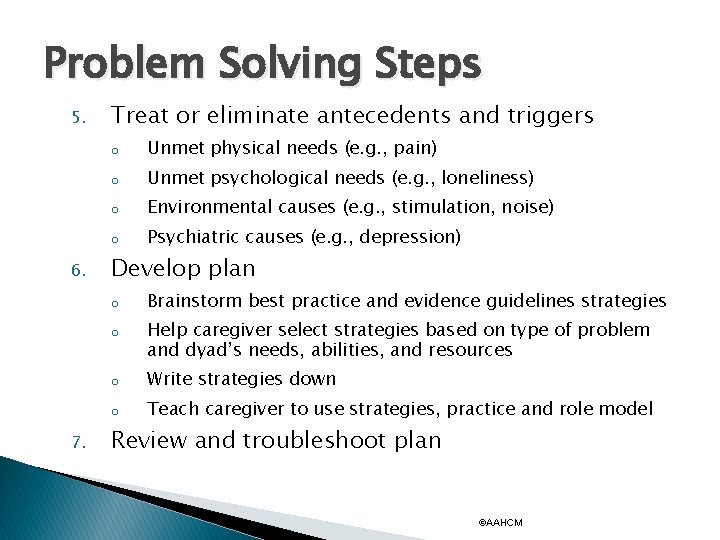
Problem Solving Steps 5. 6. Treat or eliminate antecedents and triggers o Unmet physical needs (e. g. , pain) o Unmet psychological needs (e. g. , loneliness) o Environmental causes (e. g. , stimulation, noise) o Psychiatric causes (e. g. , depression) Develop plan o o 7. Brainstorm best practice and evidence guidelines strategies Help caregiver select strategies based on type of problem and dyad’s needs, abilities, and resources o Write strategies down o Teach caregiver to use strategies, practice and role model Review and troubleshoot plan ©AAHCM
Problem Solving – Define Problem � Problem: Confusion, agitation, dependence, decreased mobility, falls � Operationalize: ◦ When does it happen? ◦ Where does it happen? ◦ How often does it happen? ◦ Is anyone around? ◦ Is the patient hurt? ©AAHCM
Problem Solving – Goals � Problem: Wandering � What would make it better: ◦ Keep from wandering �Adapt environment to reduce exit-seeking ◦ Make wandering safe �Identification/GPS �Safe wandering paths ©AAHCM
Problem Solving – Possible Solutions � Problems: Increased dependence in dressing, unable to choose appropriate and clean clothing, increased agitation � Possible solutions: ◦ ◦ ◦ ◦ Medication Attendant Lay out clothes Simplify tasks Limit choices Cue, prompt Modify environment ©AAHCM
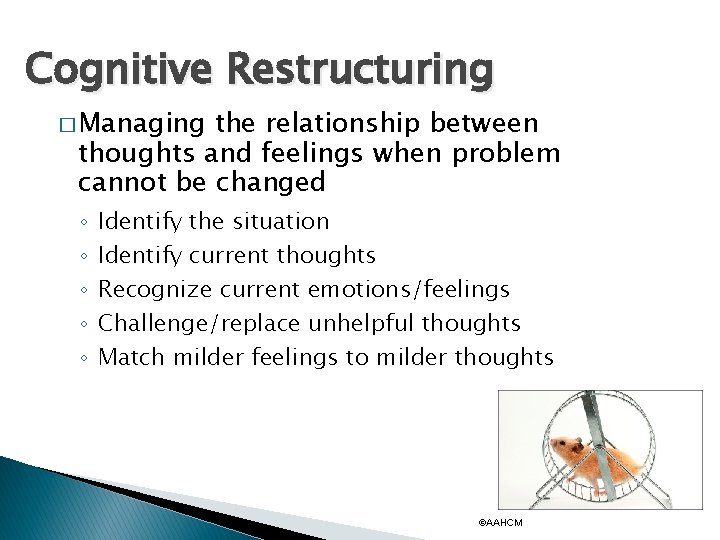
Cognitive Restructuring � Managing the relationship between thoughts and feelings when problem cannot be changed ◦ ◦ ◦ Identify the situation Identify current thoughts Recognize current emotions/feelings Challenge/replace unhelpful thoughts Match milder feelings to milder thoughts ©AAHCM
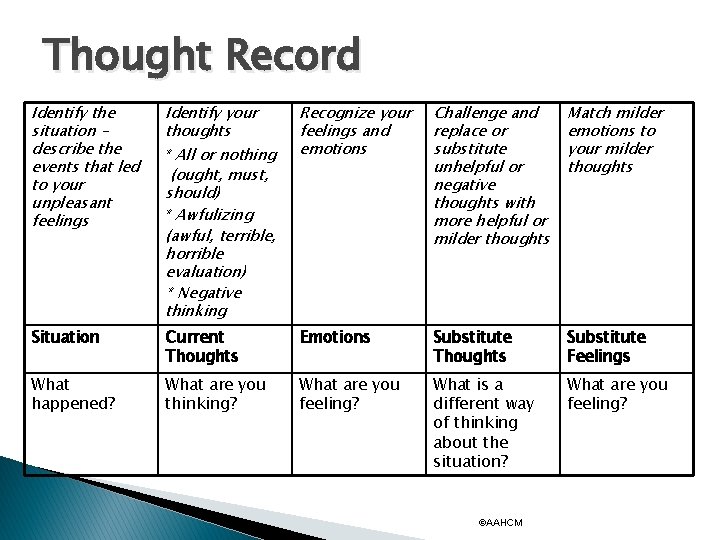
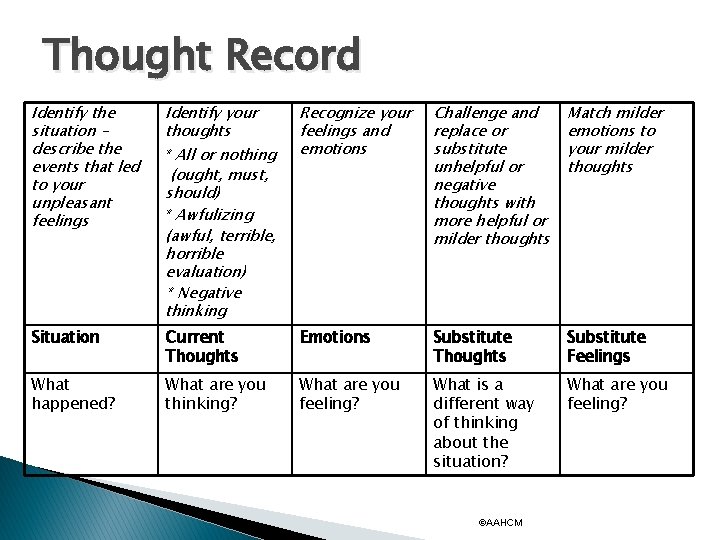
Thought Record Identify the situation – describe the events that led to your unpleasant feelings Identify your thoughts Recognize your feelings and emotions Challenge and replace or substitute unhelpful or negative thoughts with more helpful or milder thoughts Match milder emotions to your milder thoughts Situation Current Thoughts Emotions Substitute Thoughts Substitute Feelings What happened? What are you thinking? What are you feeling? What is a different way of thinking about the situation? What are you feeling? * All or nothing (ought, must, should) * Awfulizing (awful, terrible, horrible evaluation) * Negative thinking ©AAHCM
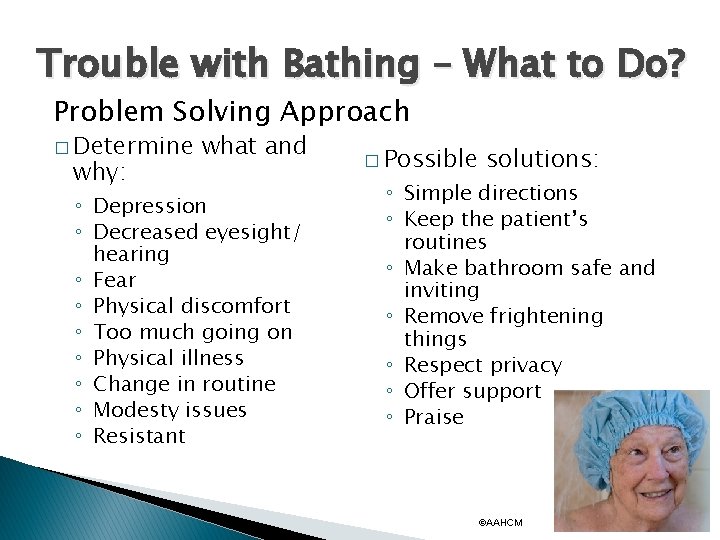
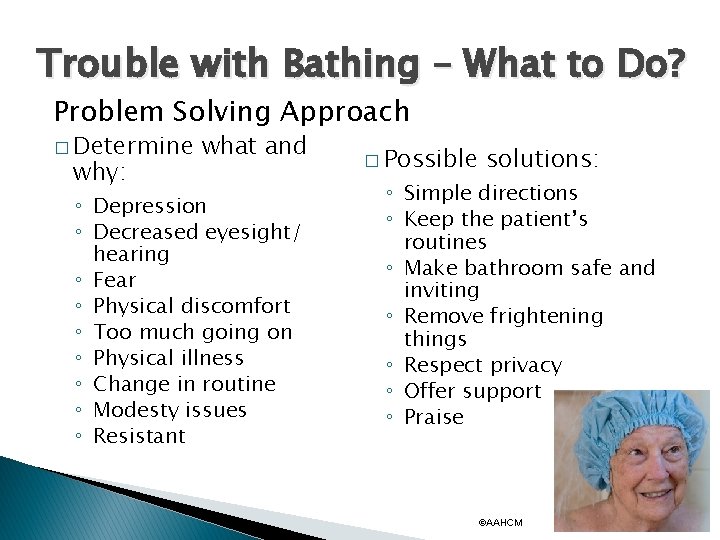
Trouble with Bathing – What to Do? Problem Solving Approach � Determine why: what and ◦ Depression ◦ Decreased eyesight/ hearing ◦ Fear ◦ Physical discomfort ◦ Too much going on ◦ Physical illness ◦ Change in routine ◦ Modesty issues ◦ Resistant � Possible solutions: ◦ Simple directions ◦ Keep the patient’s routines ◦ Make bathroom safe and inviting ◦ Remove frightening things ◦ Respect privacy ◦ Offer support ◦ Praise ©AAHCM
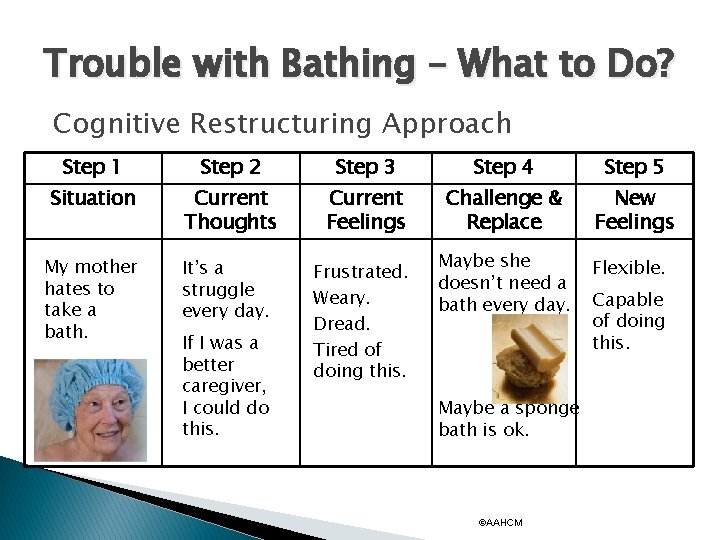
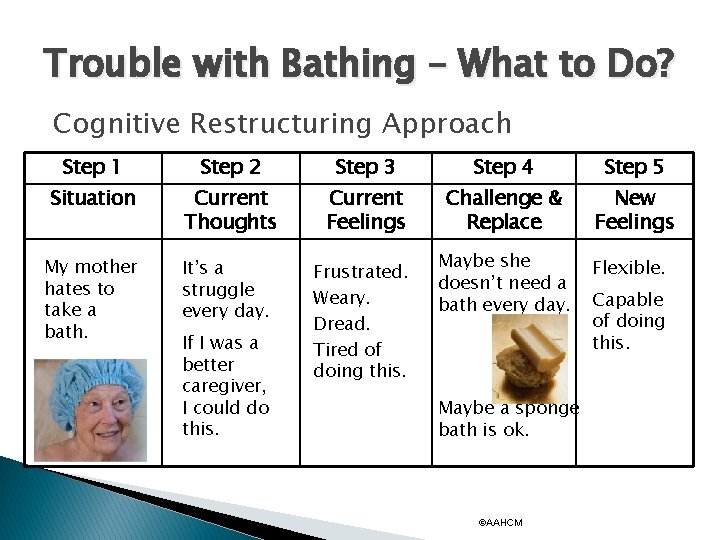
Trouble with Bathing – What to Do? Cognitive Restructuring Approach Step 1 Step 2 Step 3 Step 4 Step 5 Situation Current Thoughts Current Feelings Challenge & Replace New Feelings My mother hates to take a bath. It’s a struggle every day. Frustrated. Weary. Dread. Tired of doing this. If I was a better caregiver, I could do this. Maybe she doesn’t need a bath every day. Maybe a sponge bath is ok. ©AAHCM Flexible. Capable of doing this.
Stress Management/Relaxation Exercises � ◦ Signal Breath ◦ Music ◦ Stretching ◦ Guided Imagery/Visualization ◦ Pleasant Events ©AAHCM
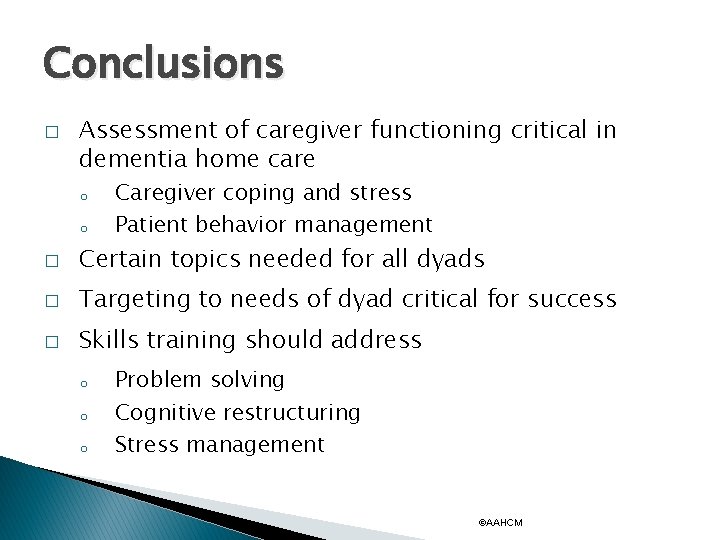
Conclusions � Assessment of caregiver functioning critical in dementia home care o o Caregiver coping and stress Patient behavior management � Certain topics needed for all dyads � Targeting to needs of dyad critical for success � Skills training should address o o o Problem solving Cognitive restructuring Stress management ©AAHCM
Questions? Contact Us linda. nichols@va. gov rburns 1@uthsc. edu ©AAHCM
 Moving and handling dementia patients
Moving and handling dementia patients Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Pediatric first aid for teachers
Pediatric first aid for teachers Professional boundaries for in home caregivers
Professional boundaries for in home caregivers Zone of helpfulness
Zone of helpfulness Vagus nerve theory
Vagus nerve theory Caregivers guide to medication
Caregivers guide to medication Idaho caregiver alliance
Idaho caregiver alliance 3 zones of space and awareness dementia
3 zones of space and awareness dementia Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease Chapter 49 confusion and dementia
Chapter 49 confusion and dementia Confusion dementia and alzheimer disease chapter 19
Confusion dementia and alzheimer disease chapter 19 Confusion dementia and alzheimer's disease
Confusion dementia and alzheimer's disease If a resident with ad shows violent behavior the na should
If a resident with ad shows violent behavior the na should Difference between dementia and delirium
Difference between dementia and delirium Francisco fernandez md
Francisco fernandez md Types of amnesia
Types of amnesia Dementia treatments and interventions near patterson
Dementia treatments and interventions near patterson Bookcase analogy dementia
Bookcase analogy dementia Dementia pugilistica
Dementia pugilistica Enriched model of dementia care
Enriched model of dementia care Glycogen storage disease mnemonic
Glycogen storage disease mnemonic Dementia 2015
Dementia 2015 Tom kitwood enriched model of dementia care
Tom kitwood enriched model of dementia care Reversible dementia
Reversible dementia Reversible dementia
Reversible dementia Barbara's story dementia
Barbara's story dementia Fast score for dementia
Fast score for dementia