Dealing with Dementia Clients Clinicians and Caregivers Presented







- Slides: 46
Dealing with Dementia: Clients, Clinicians, and Caregivers

Presented by: Dr. Kim Mc. Cullough, P. H. D. , CCCSLP Walt Greenslade, B. A. , Graduate Clinician *Information and slides adapted from materials collected by Cindy Woodson and Suzanne Sprague
True or False: 1. Memory loss is a natural part of aging. 2. Alzheimer’s disease is not fatal. 3. Vitamin E is a possible treatment for slowing the progression of Alzheimer’s disease. 4. Drinking out of aluminum cans or cooking in aluminum pots and pans can lead to Alzheimer’s disease. 5. Aspartame (Nutrasweet) causes memory loss.
True or False (Cont. ): 6. Flu shots increase risk of Alzheimer’s disease. 7. There are therapies available to stop the progression of Alzheimer's disease. 8. Approximately 5% of the population is likely to inherit Alzheimer’s disease from their family. 9. For the majority (95%) of cases of Alzheimer’s disease, there is no known cause. 10. Alzheimer’s disease was first discovered in 1906 by Dr. Alois Alzheimer.
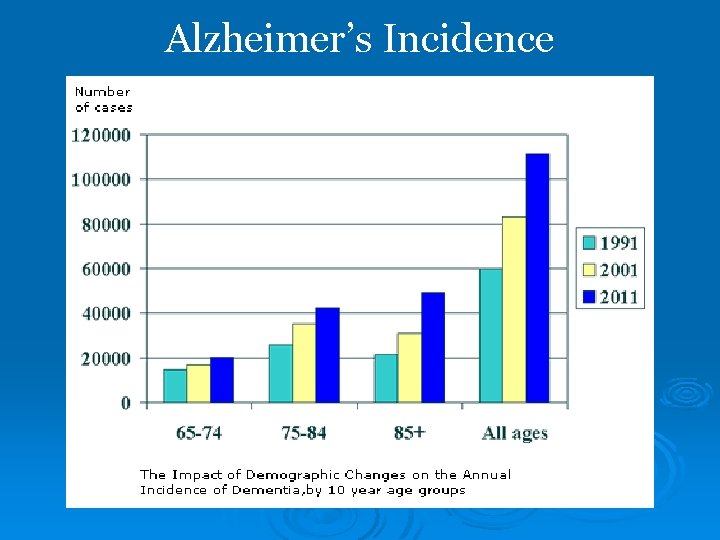
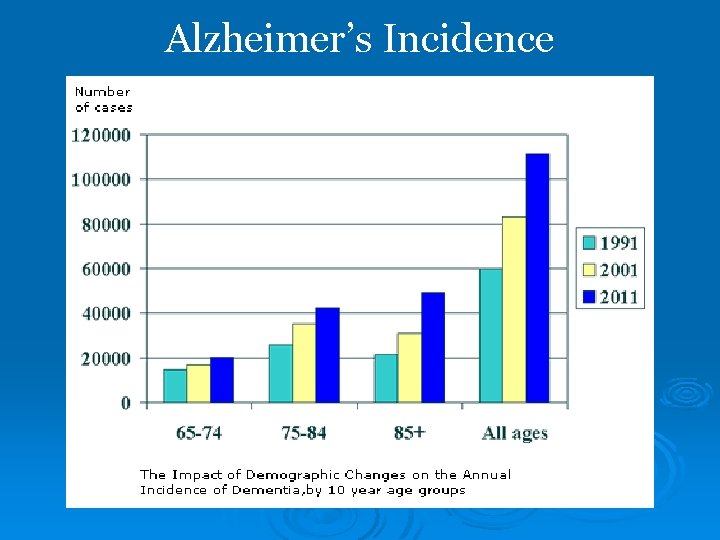
Alzheimer’s Incidence
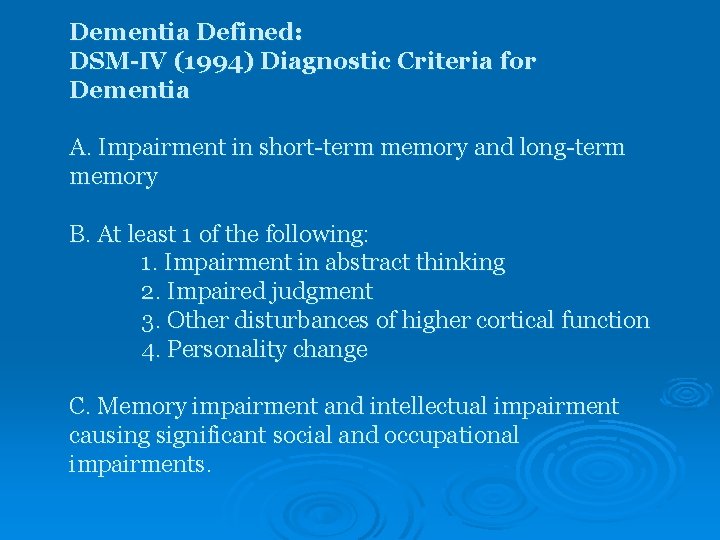
Dementia Defined: DSM-IV (1994) Diagnostic Criteria for Dementia A. Impairment in short-term memory and long-term memory B. At least 1 of the following: 1. Impairment in abstract thinking 2. Impaired judgment 3. Other disturbances of higher cortical function 4. Personality change C. Memory impairment and intellectual impairment causing significant social and occupational impairments.
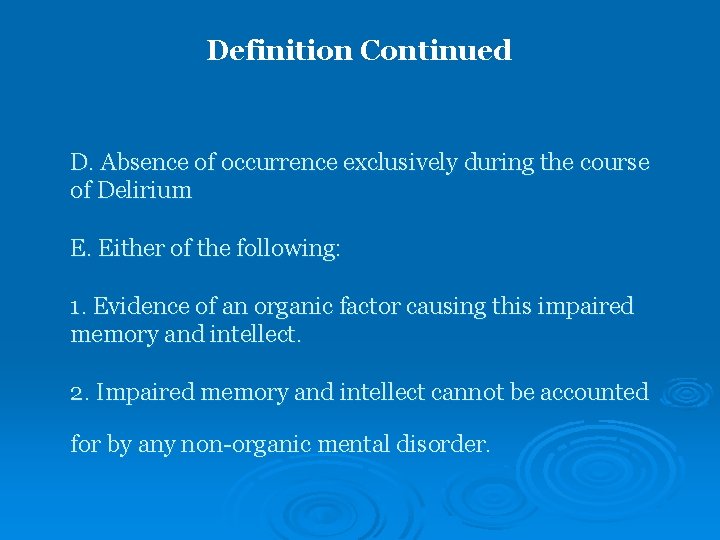
Definition Continued D. Absence of occurrence exclusively during the course of Delirium E. Either of the following: 1. Evidence of an organic factor causing this impaired memory and intellect. 2. Impaired memory and intellect cannot be accounted for by any non-organic mental disorder.
Dementia vs. Delirium • Usually a transient condition • Rapid Onset (a few hours to a few days) • Characterized by confusion, disordered thinking, disorientation, agitation, hyperactivity, distractibility, and sometimes delusions and hallucinations
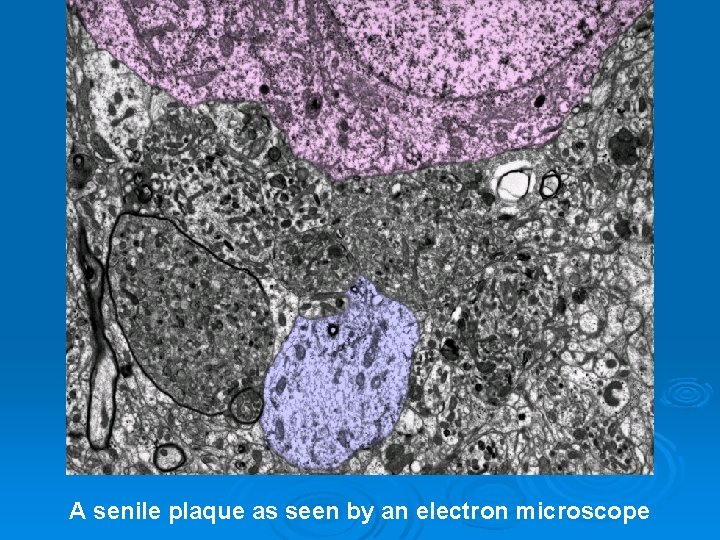
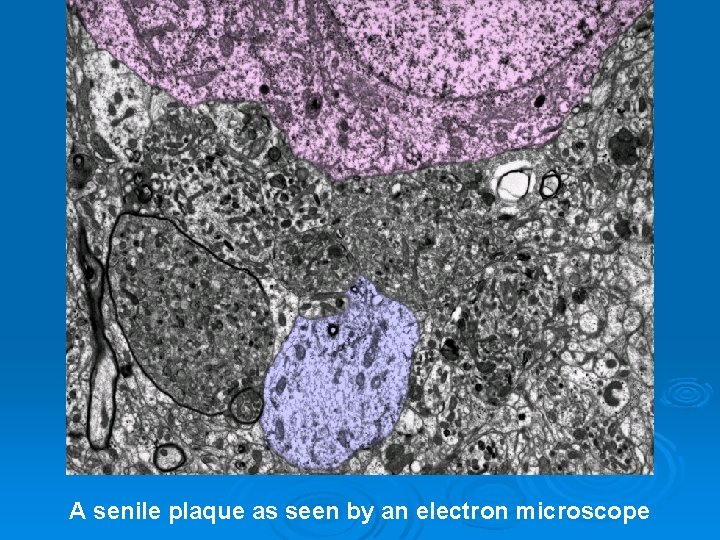
A senile plaque as seen by an electron microscope
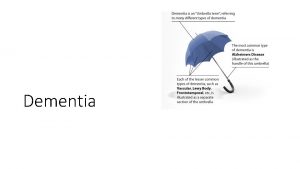
Types of dementia – reversible and irreversible Irreversible: • Alzheimer’s • Pick’s Disease • Lewy Body Disease • Vascular dementia • Huntington’s Chorea Reversible: • Brain Tumor • Depression • Hypothyroidism • Drug Interactions • Nutrition Deficits
Huntington’s Chorea Video Clip
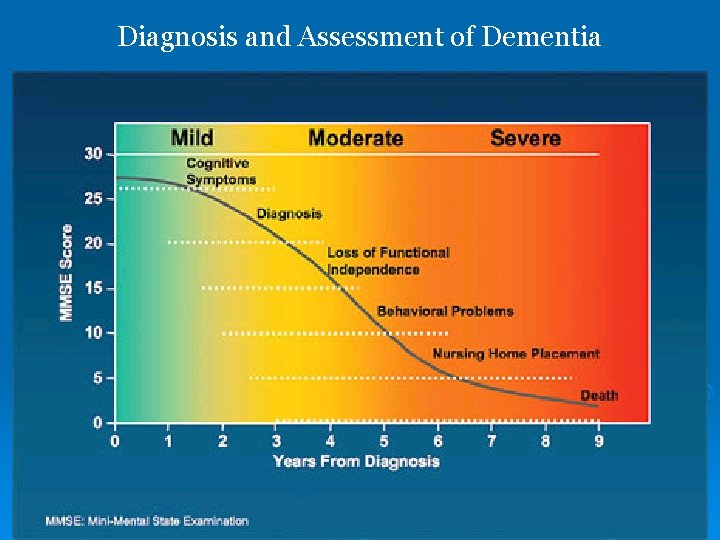
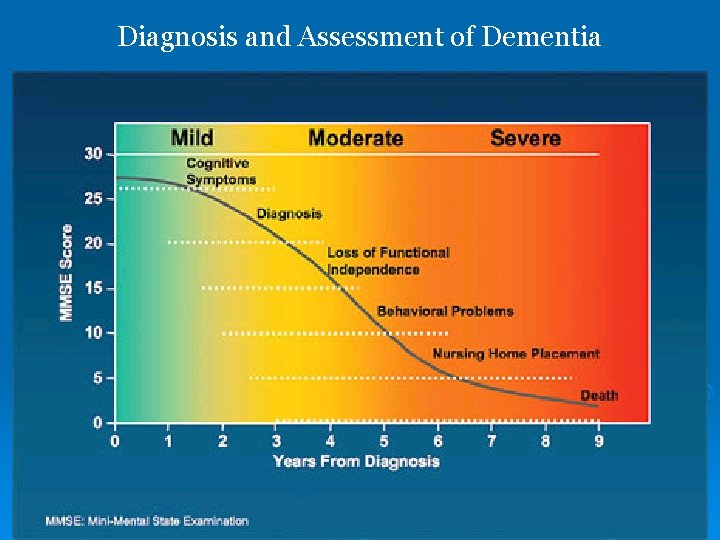
Diagnosis and Assessment of Dementia
Diagnosis and Assessment of Dementia How is Dementia Diagnosed? • Patient History • Physical Examination • Neurological Evaluations • Cognitive and Neuropsychological Tests • Brain Scans • Rating Scales
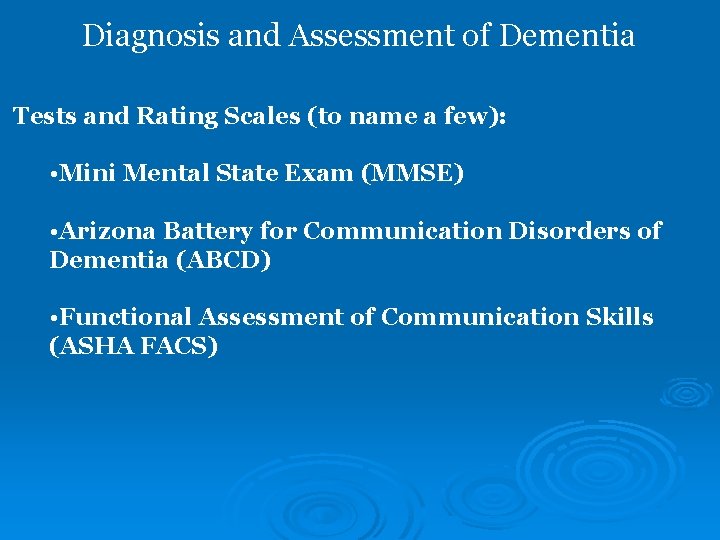
Diagnosis and Assessment of Dementia Tests and Rating Scales (to name a few): • Mini Mental State Exam (MMSE) • Arizona Battery for Communication Disorders of Dementia (ABCD) • Functional Assessment of Communication Skills (ASHA FACS)
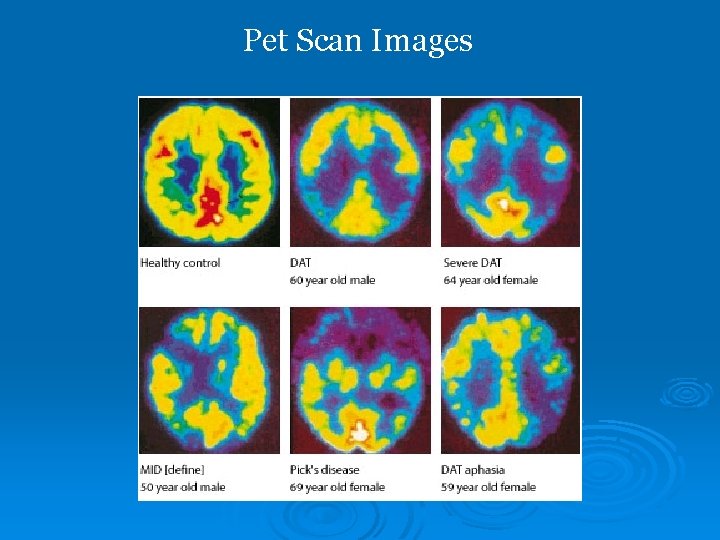
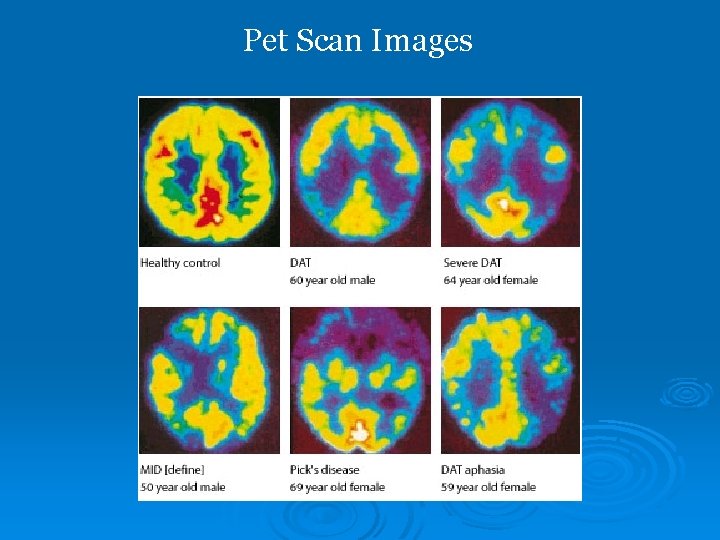
Pet Scan Images
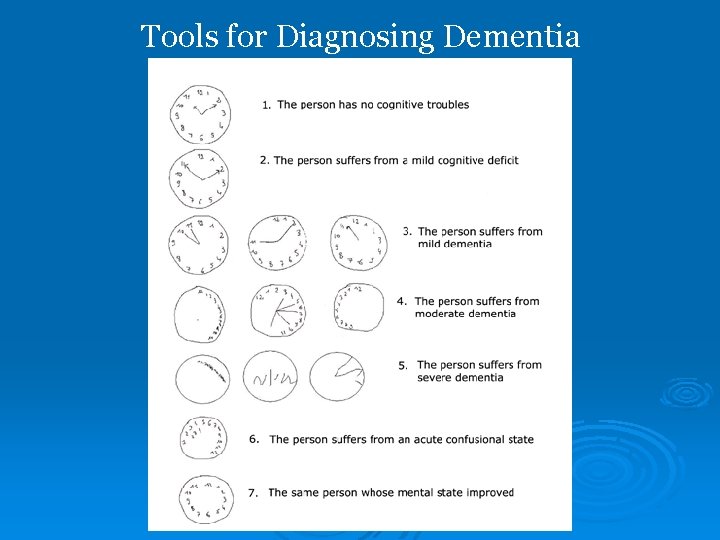
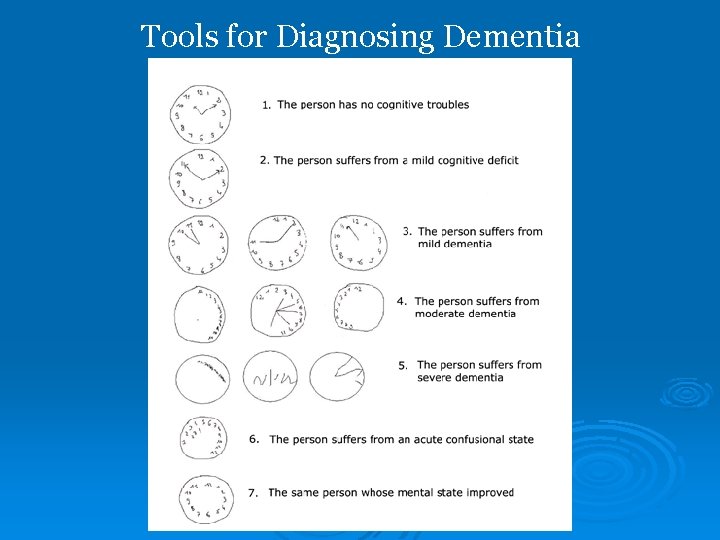
Tools for Diagnosing Dementia




Pharmacological Treatment of Dementia Cognex, Aricept, Exelon, Razadyne, & Namenda Q: What do they do? A: With the exception of Namenda, they all block an enzyme in the brain that helps to remove Acetylcholine - a chemical messenger in the brain. People with AD typically have low levels of this helpful chemical messenger, so keeping this at higher levels helps to slow the progression of AD. Q: What are the side effects? A: Generally, cholinesterase inhibitors are well tolerated. Symptoms such as nausea, vomiting, loss of appetite, diarrhea, sleeplessness, and abnormal dreams are the most commonly reported side effects.
Pharmacological Treatment of Dementia Q: What about Namenda? A: Namenda essentially works to keep the neurons in the brain firing smoothly. It targets specific types of neurons and keeps them from over firing. When these neurons fire too often, the chemical result is an increase in free radicals that contribute to damage of surrounding brain tissue. Q: What are the side effects? The most commonly reported side effects are: constipation, dizziness, headache, and general pain.
Pharmacological Treatment of Dementia Q: Are there any new drugs coming out soon? A: It’s difficult to say what will actually make it to the market, but there are several promising new treatments on the later stages of clinical trials. One such drug attacks the formation of the plaques that form as a result of AD. However, there is still no miracle cure for AD coming out in the foreseeable future. *Vaccines!? !? !? WHERE DO I SIGN UP? ?
Therapy + Drugs A study done by Requena et al. looked at 86 individuals with dementia over the course of a year (2004). Ø Cahn-Weiner et al. found no statistically significant differences between a group receiving both Ch. EIs and cognitive stimulation and a control group (2003). Ø Another study of interest that specifically looks at the combined effects of Ch. EIs and cognitive intervention was done by Chapman et al. in 2004. Ø

The Role of the SLP for Persons with Cognitive-Communication Impairments • Identification/assessment • Intervention • Inter-professional collaboration • Case management • Education/advocacy
Treatment Goals A Model for Treatment (adapted from Tomoeda, 2001 Arksha) 1. Improve orientation, attention, and association 2. Reduce demands on episodic and working memory systems 3. Increase reliance on spared recognition and procedural/habit memory systems 4. Provide sensory stimulation to evoke positive fact memory, action, and emotion
Treatment Options for SLPs • Spaced Retrieval Training (SRT) – focuses on strengths and existing memory function • Small Group Therapy- includes compensatory strategies for enabling communication – no interruptions when they’re talking, etc. (Includes Reminiscence therapy and Breakfast Club) • Memory notebooks – compensatory strategy for coping with memory loss. • Validation Therapy
Available Evidence: Dementia Ø Interventions Identified: Ø 1. Validation Therapy Ø 2. Reality Orientation Therapy Ø 3. Reminiscence Therapy Ø 4. Sensory Stimulation Ø 5. Spaced Retrieval Training
Dementia: Validation Therapy Ø Results? Ø Qualitative descriptions of improved mood, communicative interactions from staff, family members (Brack, 1997; Touzinsky, 1998) Ø Changes in behavior: l l l Reduced physically & verbally aggressive behavior (Toseland, 1997) Increased smiling, eye contact, touching, talking, showing leadership and physical participation during VT sessions (Brack, 1997) Increased initiation & verbal interaction after VT for 2/3 participants (Morton & Bleathman, 1991)
Dementia: Validation Therapy Ø Clinical Application: Ø Anecdotal evidence that VT has a generally positive effect on facilitating communication, increasing verbal interactions and decreasing some problem behaviors. Ø Rationale/principles of VT could be taught to family members & caregivers to increase meaningful communication in individuals with AD.
Dementia: Reality Orientation Therapy Ø Results? Ø Reduced depression and anxiety (Spector et al. , 2001) Ø Gains in orientation and language over control group, but same gains demonstrated by ‘social interaction’ group (Gerber et al. , 1991) Ø 4/6 studies reported significant differences in MMSE scores between control & treatment groups after ROT
Dementia: Reality Orientation Therapy Ø Clinical Application: Ø In general, formal ROT can have positive effects on cognitive functioning of individuals with very mild or mildmoderate AD Ø Positive relationship between duration of treatment and cognitive outcomes
Dementia: Reminiscence Therapy Ø Results? Ø Generally positive results of group RT across all studies, on cognition, affect, behavior and functioning of moderatesevere patients Ø Group RT had a greater effect on patients in hospital setting vs. community day-care setting (Head et al. , 1990) Ø Individuals who attended day care (regardless if they received RT or not) improved on cognitive measures vs. control group who did not attend day care (Nomura, 2002)
Dementia: Reminiscence Therapy Ø Clinical Application: Ø Fair amount of certainty that group RT has positive effects on mood, communication and cognition of individuals with dementia Ø Difficult to tease apart what aspect of RT is contributing most to improvements: sensory stimulation, social interaction, positive interactions with trained facilitators, etc.
Dementia: Sensory Stimulation: Memory Wallets & Notebooks Results? Generally positive effects observed on meaningfulness of utterances during conversations between individuals with AD and caregivers, nurses’ assistants, other dementia patients Ø More on-topic, factual statements produced; fewer ambiguous, nonsensical utterances Ø Variability in performance as a function of severity level Ø Some subjects still showed wallet use at followup testing up to 30 months later (Bourgeois, 1990; Ø Ø Bourgeois, 1992)
Dementia: Sensory Stimulation: Memory Wallets & Notebooks Clinical Application Ø Use of memory wallets/notebooks contributed to improved ‘conversations’ between AD patients and others, Ø BUT ‘conversation’ consisted of patient being asked a question, and having him/her read the statement in the notebook Ø Need a sense of how individuals with AD would perform without printed material in front of them to refer to for answers Ø
Dementia: Spaced Retrieval Training Ø What are the results? Ø Large majority of the participants learned some or all of the target information and/or behaviors Ø Maintenance of learned information or behaviors reported in 12 studies Ø Generalization reported in six studies Ø Object-name associations Ø Face-name associations Ø Cue-behavior associations
Dementia: Spaced Retrieval Training Clinical Application: Ø Individuals with mild to severe dementia who have the ability to engage in structured training tasks have been shown to benefit from SRT Ø SRT sessions conducted weekly or more frequently Ø Improvement in the acquisition, retention and generalization of trained information and/or skills Ø No change in global cognitive functioning or general memory function as a result of training Ø
Caregiver Information • Caregivers spend 40 to 100 hours weekly with each person suffering from AD • Challenges include: • Social isolation • Feelings of guilt • High emotions • Coping skills • Lack of knowledge about AD and its treatments • Approximately 90% of caregivers report that they are affected emotinally, frustrated, and/or drained *(Adapted from Schluterman, K. , Alzheimer’s Disease Overview)
Caregiver Information
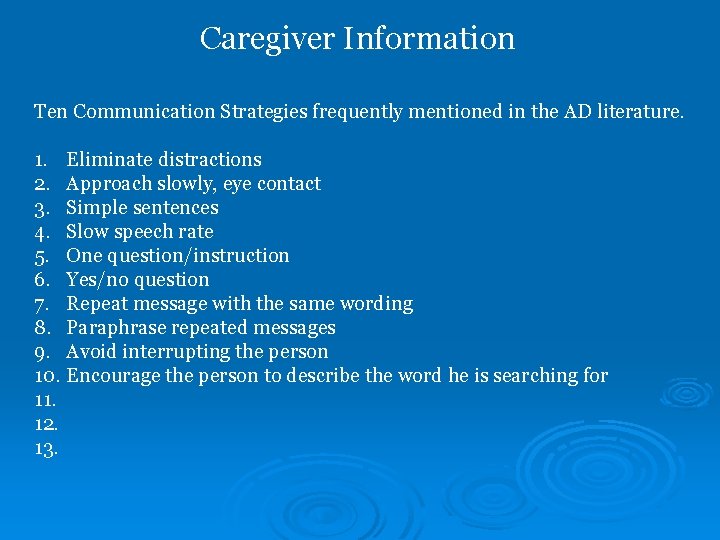
Caregiver Information Ten Communication Strategies frequently mentioned in the AD literature. 1. Eliminate distractions 2. Approach slowly, eye contact 3. Simple sentences 4. Slow speech rate 5. One question/instruction 6. Yes/no question 7. Repeat message with the same wording 8. Paraphrase repeated messages 9. Avoid interrupting the person 10. Encourage the person to describe the word he is searching for 11. 12. 13.
Caregiver Information Fewer communication breakdowns occurred with these strategies: More communication breakdowns occurred with these strategies: No clear difference in communication breakdown occurred with these strategies:
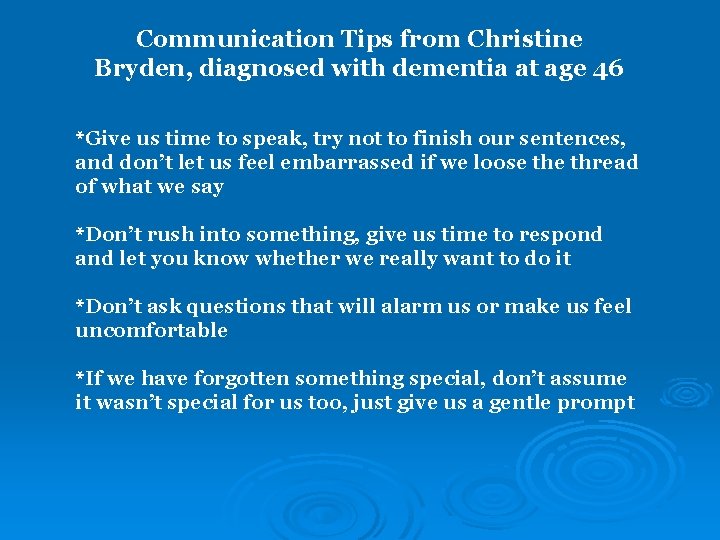
Communication Tips from Christine Bryden, diagnosed with dementia at age 46 *Give us time to speak, try not to finish our sentences, and don’t let us feel embarrassed if we loose thread of what we say *Don’t rush into something, give us time to respond and let you know whether we really want to do it *Don’t ask questions that will alarm us or make us feel uncomfortable *If we have forgotten something special, don’t assume it wasn’t special for us too, just give us a gentle prompt
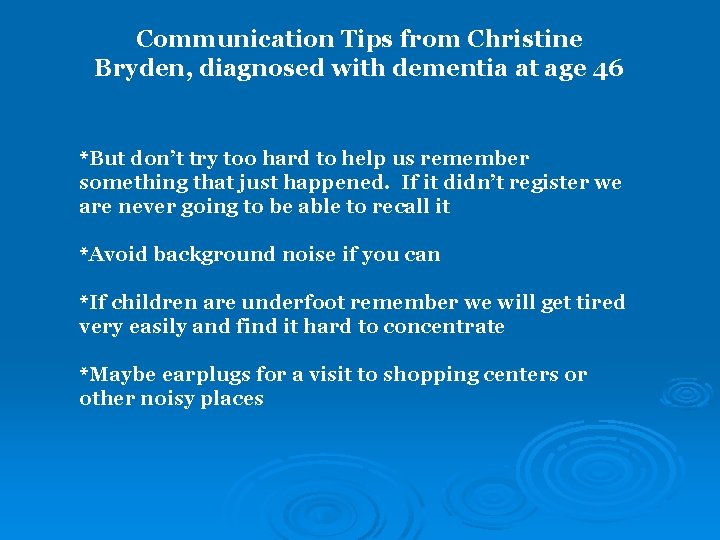
Communication Tips from Christine Bryden, diagnosed with dementia at age 46 *But don’t try too hard to help us remember something that just happened. If it didn’t register we are never going to be able to recall it *Avoid background noise if you can *If children are underfoot remember we will get tired very easily and find it hard to concentrate *Maybe earplugs for a visit to shopping centers or other noisy places

Environmental Factors: Positive and Negative Visual Auditory Tactile/Olfactory Space
References American Speech-Language-Hearing Association. (2005). The roles of speech-language pathologists working with individuals with dementia: Technical report. Rockville, MD: Author. Bottino, M. C. , Carvalho, A. M. , Alvarez, A. M. , Avila, R. , Zukauskas, P. R. , Bustamante, E. Z. , Adrade, F. C. , Hototian, S. R. , Saffi, F. , & Camargo, H. P. (2005). Cognitive rehabilitation combined with drug treatment in Alzheimer’s disease patients: A pilot study. Clinical Rehabilitation, 19, 861 -869. Bourgeois, M. S. , (1991). Communication Treatment for Adults with Dementia. Journal of Speech and Hearing Research, 34, 831 -844. Bourgeois, M. S. , (1992). Evaluating Memory Wallets in Conversations With Persons With Dementia. Journal of Speech and Hearing Research, 35, 1344 -1357. Bourgeois, M. S. , Camp, C. , Rose, M. , White, B. , Malone, M. , Carr, J. , Rovine, M. (2003). A comparison of training strategies to enhance the use of external aids by persons with dementia. Journal of Communication Disorders, 361 -378. Camp, C. J. , & Stevens, A. B. (1990). Spaced-retrieval: A memory intervention for dementia of the Alzheimer’s type. Clinical Gerontologist, 10(11), 58 -61. Camp, C. J. , Foss, J. W. , O’Hanlon, A. M. , & Stevens, A. B. (1996). Memory interventions for persons with dementia. Applied Cognitive Psychology, 10, 193 -210. Cahn-Weiner, D. A. , Malloy, P. F. , Rebok, G. W. , & Ott, B. R. (2003). Results of a randomized placebocontrolled study of memory training for mildly impaired Alzheimer’s disease patients. Applied Neuropsychology, 10, 215 -223.
References Chapman, S. B. , Weiner, M. F. , Rackley, A. , Hynan, L. S. , & Zeintz, J. (2004). Effects of cognitive-communication stimulation for Alzheimer’s disease patients treated with donepezil. Journal of Speech, Language, and Hearing Research, 47, 1149 -1163. Kimball, J. W. (2004, December 9). Enzymes. Retrieved November 16, 2006, from http: //users. rcn. com/jkimball. ma. ultranet/Biology. Pages/E/Enzymes. html Reese, P. B. (2000). The Source for Alzheimer’s & Dementia. Lingui. Systems, East Moline, IL. Small, J. A. , Gutman, G. , Makela, S. & Hillhouse, B. (2003). Effectiveness of communication strategies used by caregivers of persons with alzhimer’s disease during activities of daily living. Journal of Speech, Language, and Hearing Research, 46, 353 -367.
 Pediatric first aid for teachers
Pediatric first aid for teachers Zone of helpfulness
Zone of helpfulness Boundaries for caregivers
Boundaries for caregivers Vagus nerve theory
Vagus nerve theory Caregivers guide to medication
Caregivers guide to medication Idaho caregiver alliance
Idaho caregiver alliance Sabre helps its clients through dashboards and analytics
Sabre helps its clients through dashboards and analytics Web essentials
Web essentials Positive physical approach
Positive physical approach Chapter 19 confusion dementia and alzheimer's disease
Chapter 19 confusion dementia and alzheimer's disease Chapter 49 confusion and dementia
Chapter 49 confusion and dementia Confusion dementia and alzheimer disease chapter 19
Confusion dementia and alzheimer disease chapter 19 Confusion dementia and alzheimer's disease
Confusion dementia and alzheimer's disease A helpful way for an na to respond to hallucinations is to
A helpful way for an na to respond to hallucinations is to Difference between dementia and delirium
Difference between dementia and delirium Moving and handling dementia patients
Moving and handling dementia patients Francisco fernandez md
Francisco fernandez md Difference between delirium and dementia table
Difference between delirium and dementia table Dementia treatments and interventions near patterson
Dementia treatments and interventions near patterson Todays public relations departments
Todays public relations departments Recruitment cold calling script
Recruitment cold calling script Déontologie
Déontologie étude de flux
étude de flux Typologie des clients insatisfaits
Typologie des clients insatisfaits Ibm thin clients
Ibm thin clients How to schedule appointments with clients
How to schedule appointments with clients Trauma-informed questions for clients
Trauma-informed questions for clients Assessment questions social work
Assessment questions social work Nudge for clients
Nudge for clients Existential therapy from a multicultural perspective
Existential therapy from a multicultural perspective Characteristics of professional ethics
Characteristics of professional ethics Basic assumptions of adlerian theory
Basic assumptions of adlerian theory Counseling multicultural clients
Counseling multicultural clients Prospecting and qualifying
Prospecting and qualifying Two basic requirements for a healthy scalp
Two basic requirements for a healthy scalp Clients needs assessment
Clients needs assessment Gnutella file sharing
Gnutella file sharing Thin client nachteile
Thin client nachteile How should you handle tardy clients
How should you handle tardy clients Idt therapy
Idt therapy Ece 450
Ece 450 Appipay service en ligne
Appipay service en ligne Chapter 5 lesson 1 dealing with anxiety and depression
Chapter 5 lesson 1 dealing with anxiety and depression Chapter 5 lesson 1 dealing with anxiety and depression
Chapter 5 lesson 1 dealing with anxiety and depression Jekyll and hyde symbolism
Jekyll and hyde symbolism Romeo and juliet themes
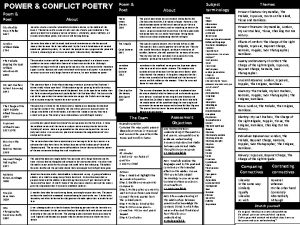
Romeo and juliet themes How is power presented in ozymandias and london
How is power presented in ozymandias and london