SEMINAR PRESENTER AKSHATHA MANJUNATH MODERATOR DR ARAVIND ANATOMY
























- Slides: 76
SEMINAR PRESENTER: AKSHATHA MANJUNATH MODERATOR: DR ARAVIND
• ANATOMY • PHYSIOLOGY • URINARY INCONTINENCE • BLADDER IN SPINAL INJURY AND MANAGEMENT • BLADDER INJURY IN ORTHOPAEDICS • POSTOPERATIVE URINARY RETENTION

ANATOMY �Smooth muscle chamber �Behind the pubic bones �In women, inferior to the uterus �In men, superior to the prostate gland � 2 parts : the body and the neck


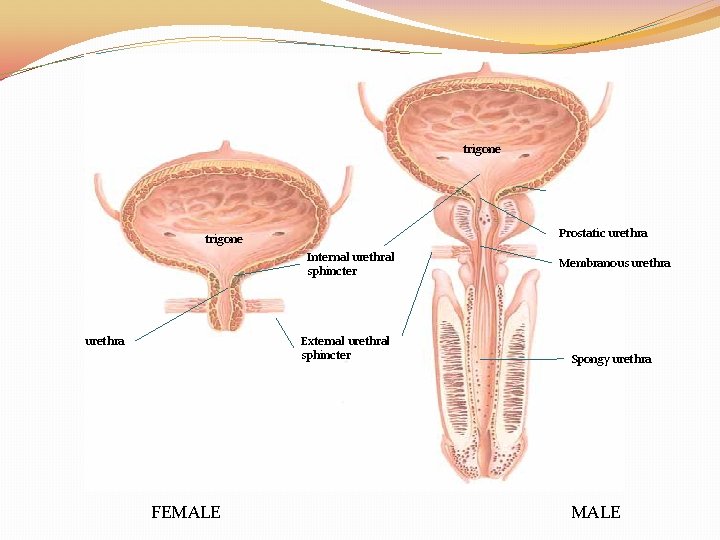
THE SPHINCTERS �Bladder neck is 2 to 3 cms long and its wall is composed of detrusor muscle interlaced with a large amount of elastic tissue. This is the INTERNAL SPHINCTER. �Keeps the bladder neck and posterior urethra empty of urine �Prevents emptying of the bladder until pressure in the body reaches critical threshold
THE SPHINCTERS �The urethra passes through the urogenital diaphragm, which contains a layer of muscle called the EXTERNAL SPHINCTER. �A voluntary skeletal muscle and used to prevent urination even when involuntary controls are attempting to empty the bladder
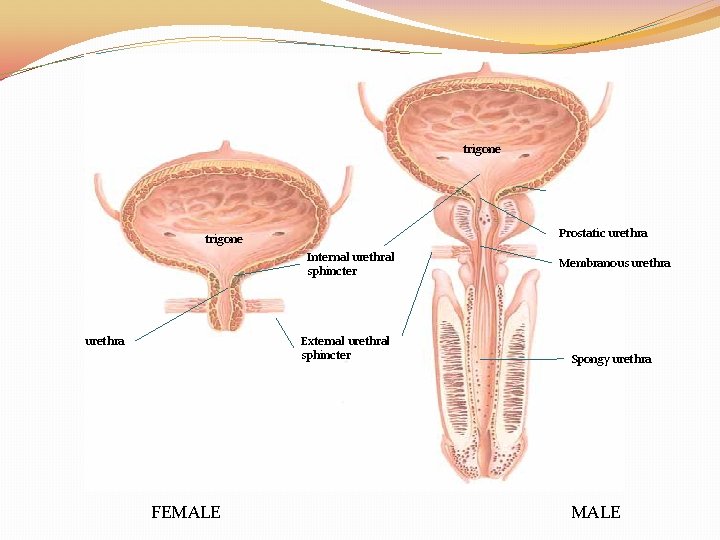
trigone Prostatic urethra trigone Internal urethral sphincter urethra External urethral sphincter FEMALE Membranous urethra Spongy urethra MALE
PHYSIOLOGY

MICTURITION �“process by which the urinary bladder empties when it becomes filled” �Spinal reflex facilitated and inhibited by higher brain centers , and subject to voluntary facilitation and inhibition
FILLING OF THE BLADDER �The walls of the ureters contain smooth muscle arranged in spiral , longitudinal and circular bundles �Regular peristaltic contractions (1 to 5 times/min) move urine from renal pelvis to the bladder
FILLING OF THE BLADDER �Enhanced by parasympathetic stimulation and inhibited by sympathetic stimulation �Thus urine enters the bladder in spurts synchronous with each peristaltic wave
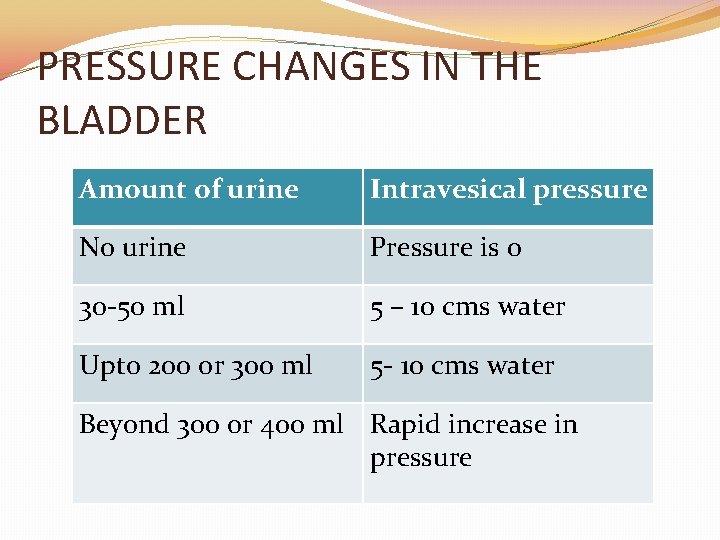
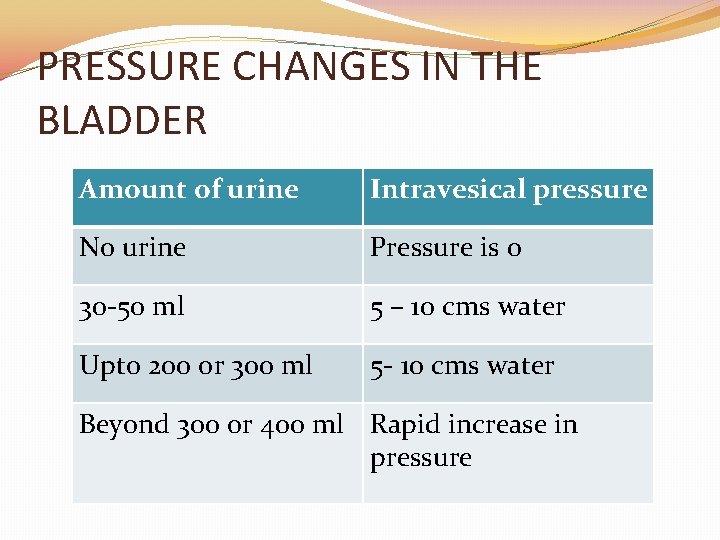
PRESSURE CHANGES IN THE BLADDER Amount of urine Intravesical pressure No urine Pressure is 0 30 -50 ml 5 – 10 cms water Upto 200 or 300 ml 5 - 10 cms water Beyond 300 or 400 ml Rapid increase in pressure
The first urge to void : around 150 ml. A marked sense of fullness : about 400 ml.
EMPTYING OF THE BLADDER When the bladder is only partially full �the micturition contractions usually relax spontaneously after a fraction of a minute, �the detrusor stops contracting �pressure falls back to baseline. As the bladder continues to fill, �the reflexes become more frequent �greater detrusor contractions.
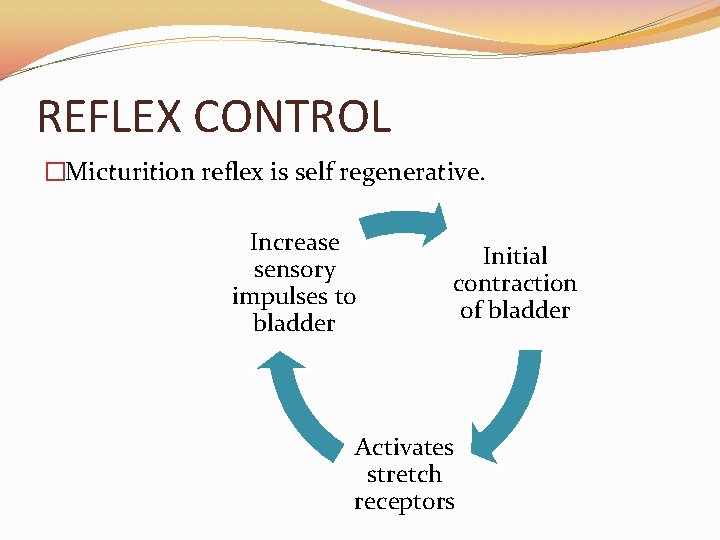
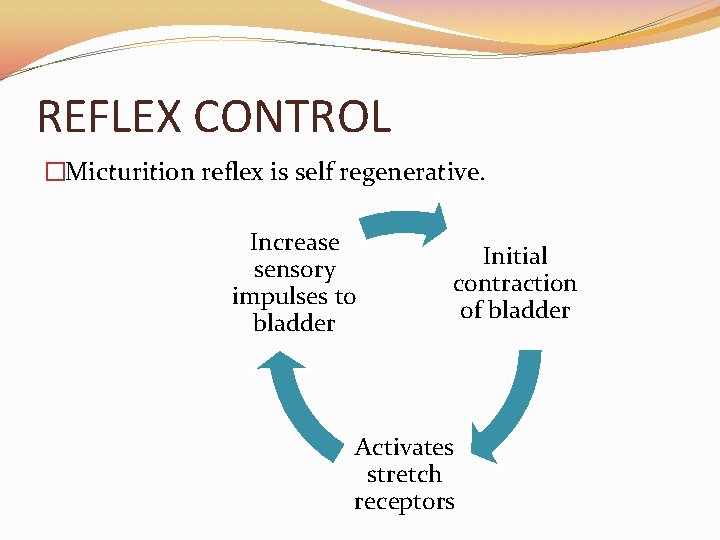
REFLEX CONTROL �Micturition reflex is self regenerative. Increase sensory impulses to bladder Initial contraction of bladder Activates stretch receptors
REFLEX CONTROL Thus the micturition reflex is a single complete cycle of 1. Progressive and rapid increase of pressure 2. A period of sustained pressure 3. Return of pressure to basal tone of the bladder
FACILITATION OR INHIBITION OF MICTURITION BY THE BRAIN �Strong facilitatory and inhibitory centres in the brain stem , located mainly in the pons. �Several centers located in the cerebral cortex that are mainly inhibitory but can become excitatory.


MECHANISM OF VOLUNTARY URINATION Person voluntarily contracts abdominal muscles Increases pressure in bladder and allows extra urine to enter bladder neck under pressure Stimulates stretch receptors Excites the micturition reflex and simultaneously inhibits external sphincter
MECHANISM OF VOLUNTARY URINATION �After urination, female urethra empties by gravity �Male urethra empties by contractions of the bulbocavernous muscle �Ordinarily all the urine is emptied with rarely more than 5 to 10 ml left

URINARY INCONTINENCE

DEFINITION “any involuntary loss of urine”

TYPES �Anatomic or genuine stress incontinence �True urge incontinence �Mixed incontinence �Neuropathic incontinence �Congenital incontinence �False or overflow incontinence �Traumatic incontinence �Fistulous incontinence �Unconscious or unaware incontinence
Anatomic or genuine stress incontinence “the involuntary leakage of urine during increase in abdominal pressure in absence of detrusor contraction” Ø Essentially intact sphincter mechanism Ø Weak pelvic floor support Ø Anatomic abnormality Symptom is the complaint of involuntary leakage on exertion, sneezing or coughing

True urge incontinence “Detrusor instability with normal sphincteric component” ØNormal anatomy ØNo neuropathy ØSphincteric instability is less common Symptom is the complaint of involuntary leakage accompanied by or immediately preceded by urgency
Mixed urinary incontinence “involuntary leakage of urine associated with urgency and also with exertion, coughing or sneezing”
False or overflow incontinence �Result of obstructive or neuropathic lesion �Not true incontinence

Neuropathic incontinence �Depends on nerve lesion �Can be of three types § Active ie detrusor hyperreflexia § Passive ie sphincter atony § Combination of active and passive
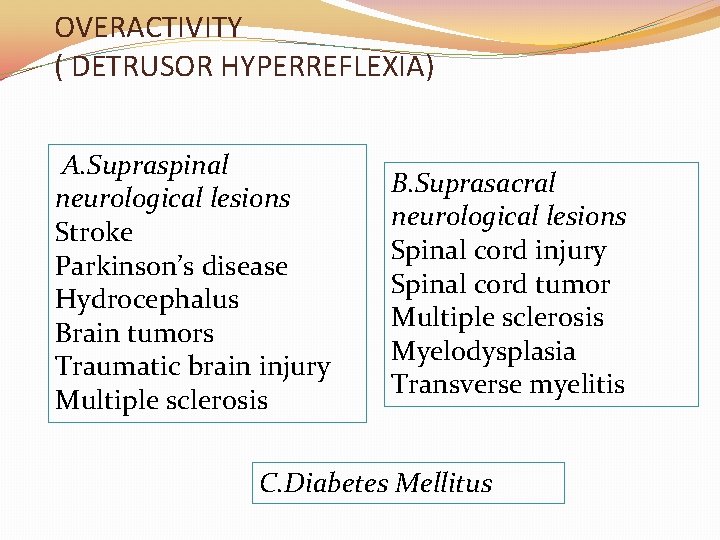
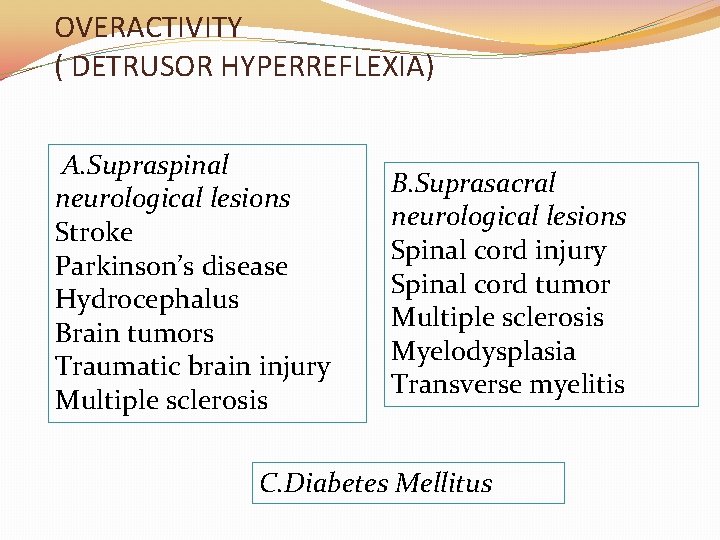
OVERACTIVITY ( DETRUSOR HYPERREFLEXIA) A. Supraspinal neurological lesions Stroke Parkinson’s disease Hydrocephalus Brain tumors Traumatic brain injury Multiple sclerosis B. Suprasacral neurological lesions Spinal cord injury Spinal cord tumor Multiple sclerosis Myelodysplasia Transverse myelitis C. Diabetes Mellitus

OTHER POSSIBLE MECHANISMS �A suprasacral spinal cord injury or lesion might cause decreased bladder compliance �Trauma to the external sphincter during a pelvic fracture or repair of it can cause neuropathic incontinence
CAUSES OF TRANSIENT INCONTINENCE �Delirium �Infection �Atrophic vaginitis/urethritis �Psychological �Pharmacologic �Excess urine production �Restricted mobility �Stool impaction
DIAGNOSTIC EVALUATION: HISTORY Ask for: �Characteristics? �Severity of incontinence? �Impact on quality of life? �Any neurological conditions? �Previous surgeries? �Any radiation received? �Medication history? �Obstetric history ?
DIAGNOSTIC EVALUATION: PHYSICAL EXAMINATION �Neurological examination �Abdominal examination �Rectal examination �Pelvic examination in women

DIAGNOSTIC EVALUATION: TESTS FOR MICTURITION �Micturition diary �Pad testing �Dye testing �Uroflowmetry �Urodynamic testing
MANAGEMENT A. Treat the underlying cause B. Rehabilitative techniques § behavioural modification: decreasing fluid intake, dietary and lifestyle changes, voiding by the clock § pelvic floor muscle training: with biofeedback or electrical stimulation

C. Oral pharmacologic Treatment § Antimuscarinics § Musculotropic relaxants § Tricyclical antidepressants
D. Intravesical or intradetrusor therapies § intravesical agents: capsaicin and resiniferatoxin § intra detrusor agents: botulinum toxin
E. SURGICAL TREATMENT FOR DETRUSOR FOR SPHINCTER OVERACTIVITY/ DYSFUNCTION: LOW COMPLAINCE § midurethral sling § Sacral nerve neuromodulation § pubovaginal sling § Denervation § urethral/colposuspe procedures nsion § Augmentation cystoplasty § artificial urinary § Autoaugmentation of sphincter the bladder

BLADDER IN SPINAL CORD INJURY LMN BLADDER UMN BLADDER Flaccid bladder/ overflow incontinence/ autonomous bladder Spastic bladder/ urge incontinence / automatic bladder Lesion at conus medullaris or cauda equina ( t 12 or below) Lesion above conus medullaris or cauda equina ( t 11 or above) Overdistension : destruction of Oversensitive: Sensory nerve sensory nerve fibres intact No inhibition of pudendal nerve, external sphincter contracted Inhibition of pudendal nerve, external sphincter relaxes



LMN BLADDER No reflex activity No urge to urinate , small amounts of urine leak continuously 1. Alpha 1 adrenergic blockers 2. Anticholinergic medication 3. Intermittent self catheterisation 4. Physiotherapy UMN BLADDER Reflex arc is intact Uncontrollable urge to urinate, accidental urination 1. Anticholinergic agents 2. Antispasmodic medications 3. Tricyclic antidepressants 4. Protective devices like bed pads and adult diapers 5. Physiotherapy
BLADDER MANAGEMENT Stimulated Voiding �Crede This method involves manually pressing down on the bladder. �Tapping The area over the bladder is tapped with the fingertips or the side of the hand, lightly and repeatedly, to stimulate detrusor muscle contractions and voiding. �Valsalva This method involves increasing pressure inside the abdomen by bearing down as if you were going to have a bowel movement.
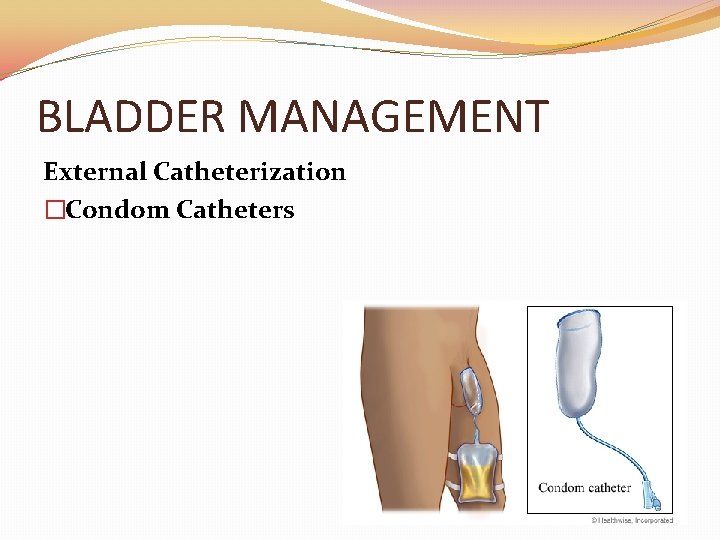
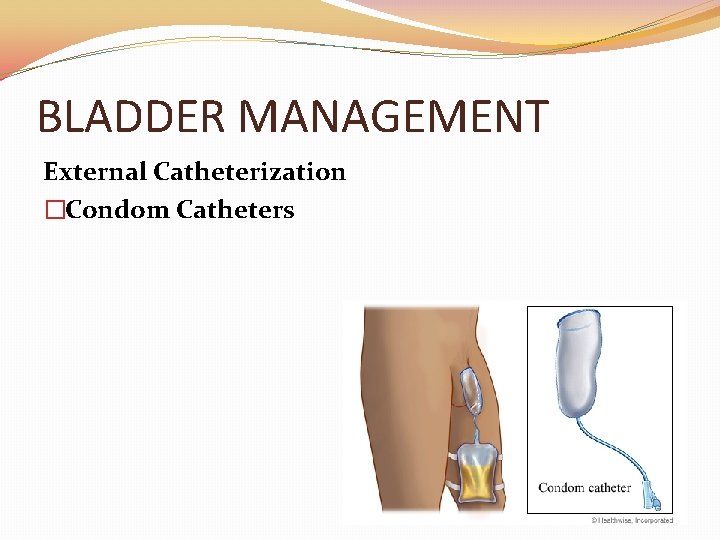
BLADDER MANAGEMENT External Catheterization �Condom Catheters
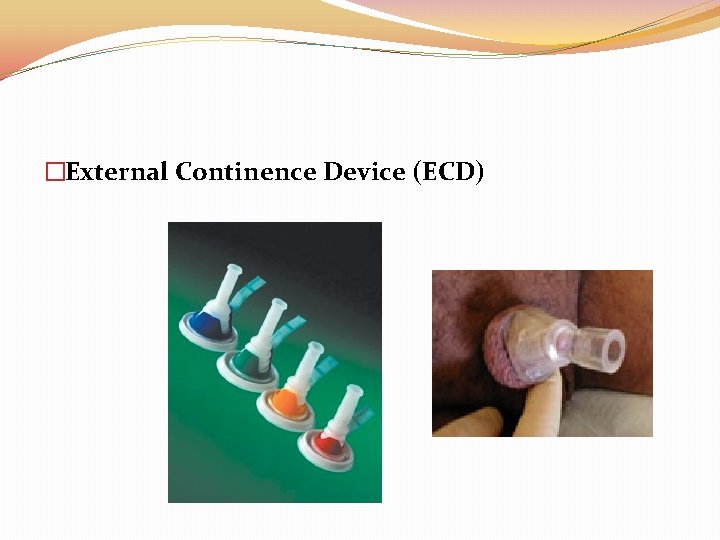
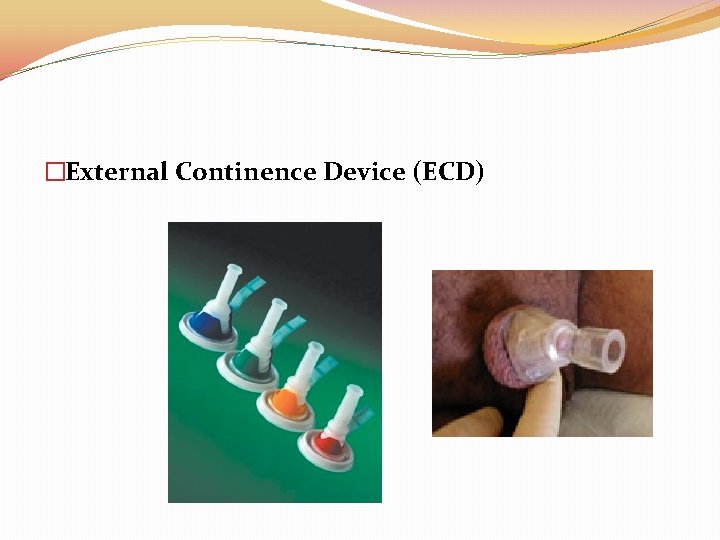
�External Continence Device (ECD)
BLADDER MANAGEMENT �Intermittent Catheterization


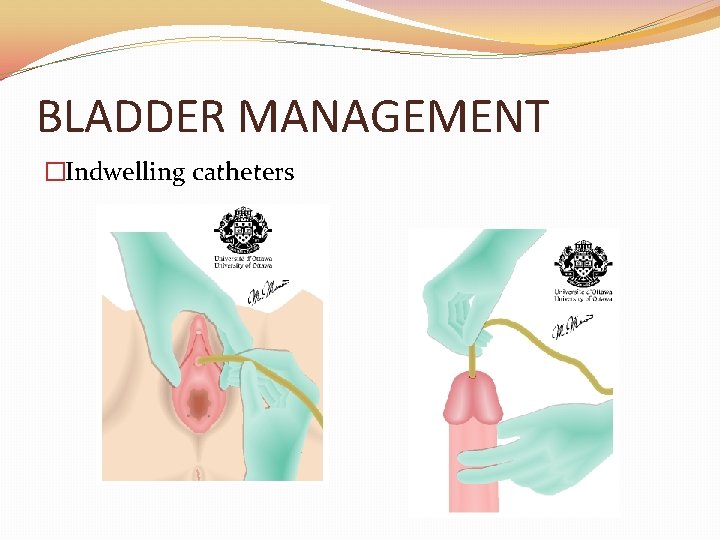
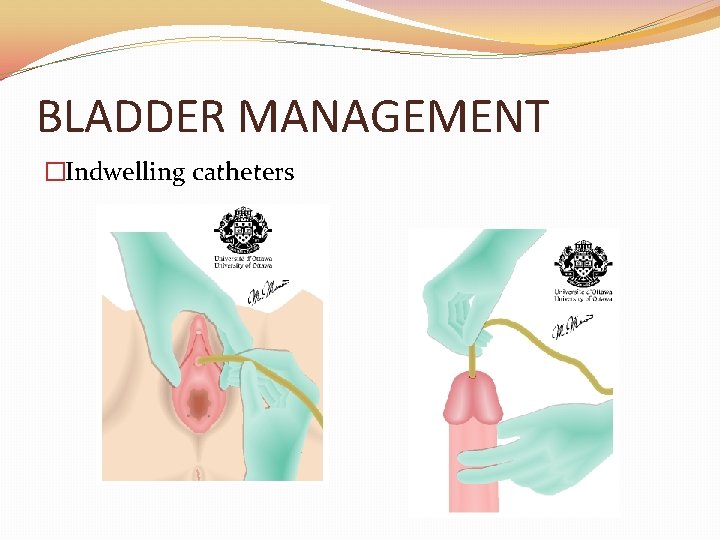
BLADDER MANAGEMENT �Indwelling catheters
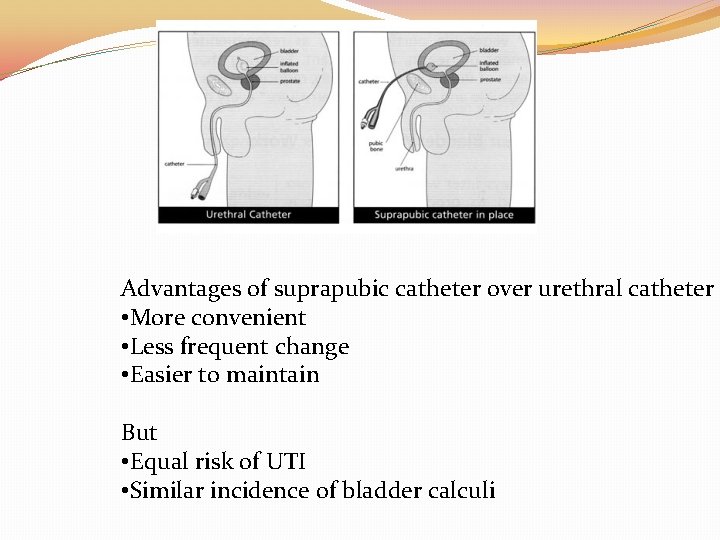
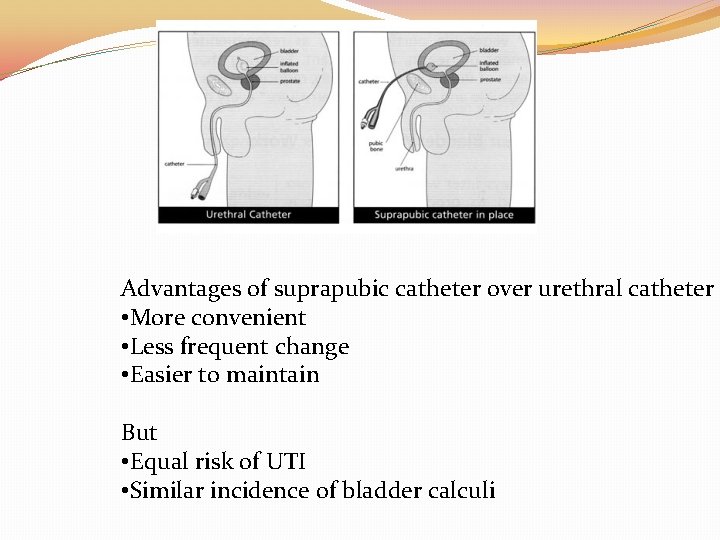
Advantages of suprapubic catheter over urethral catheter • More convenient • Less frequent change • Easier to maintain But • Equal risk of UTI • Similar incidence of bladder calculi
BLADDER INJURY IN ORTHOPAEDICS
�Approximately 10% of patients with pelvic fractures also have significant bladder injuries. �Related to its degree of distension �Related to the severity of the fracture
MECHANISM OF INJURY 1. Pelvic fracture �Usually extraperitoneal ruptures (89%-100%). �Due to a direct burst injury or the shearing force of the deforming pelvic ring. �Associated with fractures of the anterior pubic arch or direct laceration by the bony fragments �Anterolateral aspect is typically perforated by bony spicules. �Forceful disruption of the pelvis and/or the puboprostatic ligaments also tears the wall of the bladder.

MECHANISM OF INJURY 2. Orthopedic pins and screws can perforate the urinary bladder, particularly during internal fixation of pelvic fractures. 3. Thermal injuries to the bladder wall may occur during the setting of cement substances used to seat arthroplasty prosthetics.
CLNICAL FEATURES A triad of symptoms is often present �gross hematuria �suprapubic pain or tenderness �difficulty or inability to void
WHEN TO SUSPECT BLADDER INJURY? �Abdominal distension, guarding, or rebound tenderness. �Absent bowel sounds �Signs of peritoneal irritation �If blood is present at the urethral meatus, suspect a urethral injury.
WHAT NEXT? �STEP ONE Foley’s catheter �STEP TWO x ray/ CT scan/cystography

MANAGEMENT �Simple catheter drainage (ie, urethral or suprapubic). �Leave the catheter in for 7 -10 days and then obtain a cystogram. � Approximately 85% of the time, the laceration is sealed and the catheter is removed for a voiding trial. �Almost all extraperitoneal bladder injuries heal within 3 weeks.

MANAGEMENT �If the patient is taken to the operating room for associated injuries, extraperitoneal ruptures may be repaired concomitantly if the patient is stable. �Most, if not all, intraperitoneal bladder ruptures require surgical exploration.
POST OPERATIVE URINARY RETENTION
FACTORS AFFECTING RETENTION �AGE �GENDER �TYPE OF SURGERY �DURATION OF SURGERY �CO MORBIDITIES �DRUGS IN PEROPERATIVE PERIOD �INTRAOPERATIVE FLUIDS �ANESTHESIA
DIAGNOSIS Three methods have been used to diagnose POUR: �history and physical examination �the need for bladder catheterization, and, �ultrasonographic assessment

CLINICAL CRITERIA �Patient discomfort, sensation of a full bladder, palpable, distended bladder �Inability to void with bladder distension �Inability to void urine for 12 h after induction of anesthesia with 500 ml urine drained on catheterization �Inability to void 8 h after the end of surgery, and the bladder is distended or the patient is uncomfortable
�Inability to void in 8 h after removal of Foley catheter �Need of catheterization in 24 h �Unable to empty the bladder in 10 h, discomfort, and palpable bladder �Catheterization in 48 h after the end of the surgery �Parturient unable to void spontaneously and with a residual volume greater than 500 ml (measured by catheterization) were categorized as urinary retention
ULTRASOUND ASSESSMENT �Inability to void with bladder volume >600 ml in 30 hrs �Residual volume >500 ml
ADVERSE EFFECTS OF RETENTION �Autonomic response �Infection �Bladder distension and adverse effects on urodynamics
PREVENTION �Fluid restriction in high risk patients �Avoid epinephrine administration �Long acting local anesthetic �Multimodal analgesia �Alpha agonists
TREATMENT �PHARMACOLOGICAL �Alpha receptor agonists �Muscarinic agonists �Naloxone �CATHETERISATION
WHOM TO CATHETERISE? �Bladder volume > 600 ml FOR HOW LONG? �Low risk patients: 1 day �High risk patients : 5 day
INDWELLING OR INTERMITTENT CATHETERISATION? �Duration of retention : no significant difference �Risk of infection : no significant difference �Duration of hospital stay: longer in indwelling catheter.
Thank you….
 Vitrectimy
Vitrectimy Aravind chennuru
Aravind chennuru Preethi aravind
Preethi aravind Webinar introduction script sample
Webinar introduction script sample Umur andira tiktok
Umur andira tiktok Moderator examples
Moderator examples Moderator
Moderator Yang hu lancaster
Yang hu lancaster Extraneous variable definition
Extraneous variable definition Moderator tom
Moderator tom Assalamualaikum greetings
Assalamualaikum greetings Dm80 moderator
Dm80 moderator Regulator moderator war
Regulator moderator war Liking scale 1-5
Liking scale 1-5 Ce este bazinul hidrografic brainly
Ce este bazinul hidrografic brainly Constant moderator
Constant moderator Tugas moderator adalah
Tugas moderator adalah Intel svt closed chassis adapter
Intel svt closed chassis adapter Mediator vs moderator in research
Mediator vs moderator in research Cara moderator
Cara moderator Moderator show
Moderator show Continuous moderator
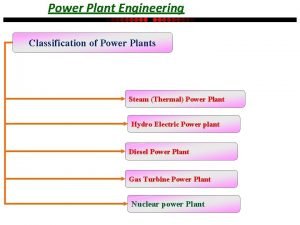
Continuous moderator Classification of power plant
Classification of power plant Kwantitatieve observatie
Kwantitatieve observatie Moderator examples
Moderator examples Presenter logo
Presenter logo Asm cluster
Asm cluster Presenter name
Presenter name Presenter position
Presenter position Mitel presenter
Mitel presenter Site:slidetodoc.com
Site:slidetodoc.com Nous allons vous présenter notre exposé
Nous allons vous présenter notre exposé Name presentation
Name presentation Portrait d'une femme ezra pound
Portrait d'une femme ezra pound Text presenter
Text presenter Younique presenter ms name
Younique presenter ms name Uno telefoni
Uno telefoni Presenter's name
Presenter's name Mitel presenter
Mitel presenter Company presenter
Company presenter It2teach
It2teach Fern presenter
Fern presenter Presenter name
Presenter name Presenter title
Presenter title Adobe presenter
Adobe presenter Mitel presenter
Mitel presenter Chèn video vào adobe presenter
Chèn video vào adobe presenter Presenter name
Presenter name Name
Name Ubiquitous presenter
Ubiquitous presenter Name/title of presenter
Name/title of presenter Insert presenter
Insert presenter Rashmi choudhary presenter
Rashmi choudhary presenter Name/title of presenter
Name/title of presenter Presentation by name
Presentation by name Title of presenter
Title of presenter Mindfulschools
Mindfulschools Presenter media
Presenter media Presenter media
Presenter media Presenter's name
Presenter's name Presenter media
Presenter media Presenters name
Presenters name By name title date
By name title date Cover letter for news presenter
Cover letter for news presenter Ai presenter
Ai presenter Sales presenter
Sales presenter Classroom presenter
Classroom presenter Name of the presenter
Name of the presenter Paper presenter
Paper presenter Presenters name
Presenters name Company presenter
Company presenter Social media presenter
Social media presenter Ppt presenter based solutions
Ppt presenter based solutions Presenter verb
Presenter verb Presenter alternatives
Presenter alternatives Asos presenter
Asos presenter Presenter media
Presenter media