Regulation of respiration Overall Control of Activity of
- Slides: 57
Regulation of respiration
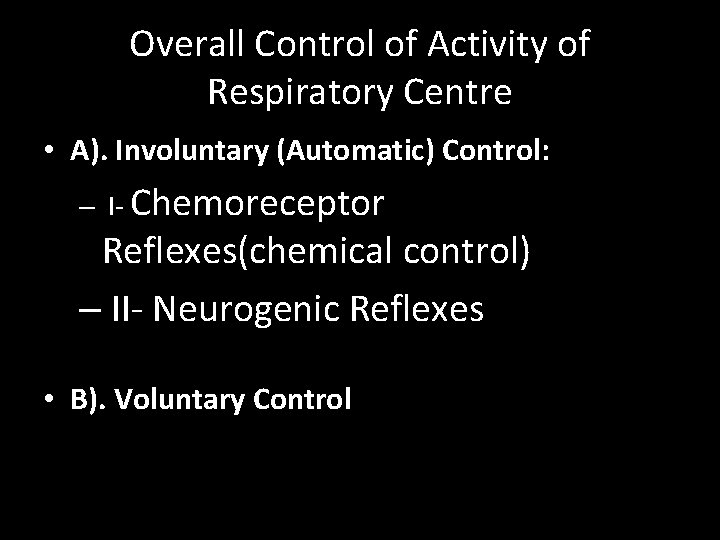
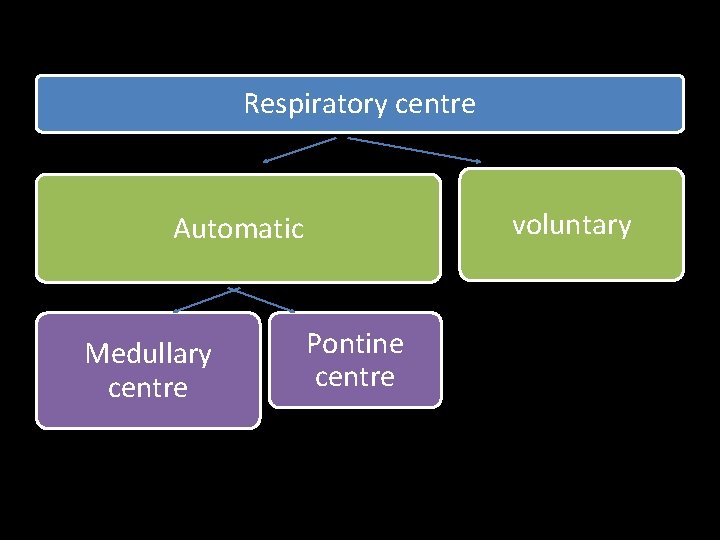
Overall Control of Activity of Respiratory Centre • A). Involuntary (Automatic) Control: – I- Chemoreceptor Reflexes(chemical control) – II- Neurogenic Reflexes • B). Voluntary Control
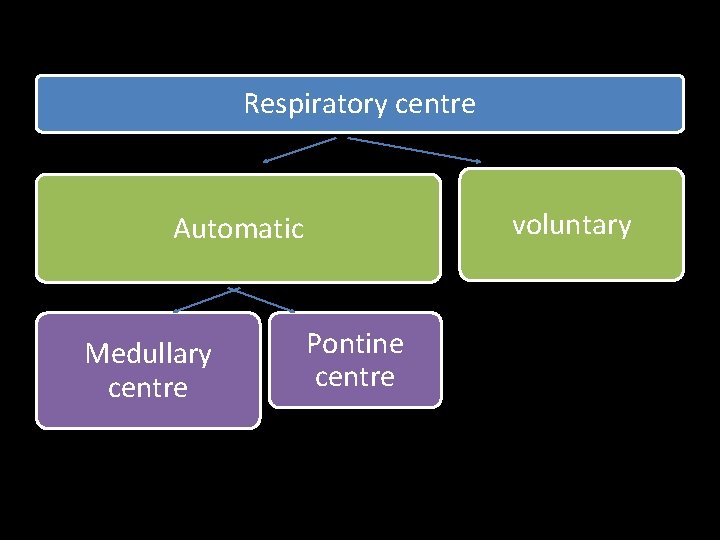
Respiratory centre voluntary Automatic Medullary centre Pontine centre
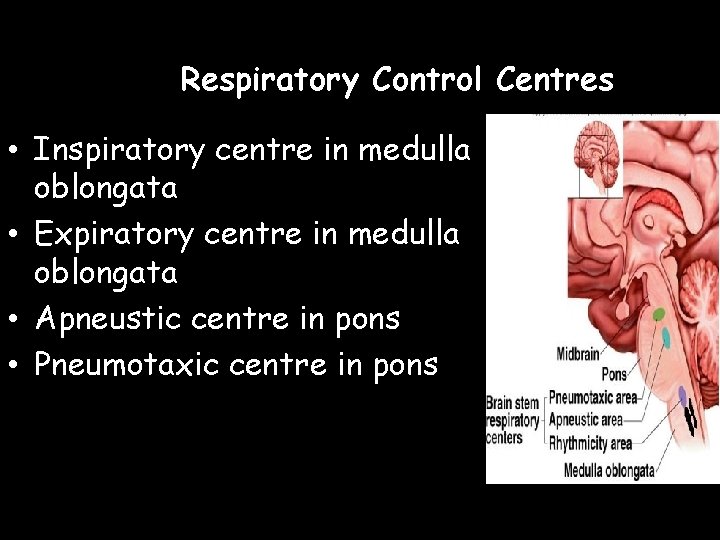
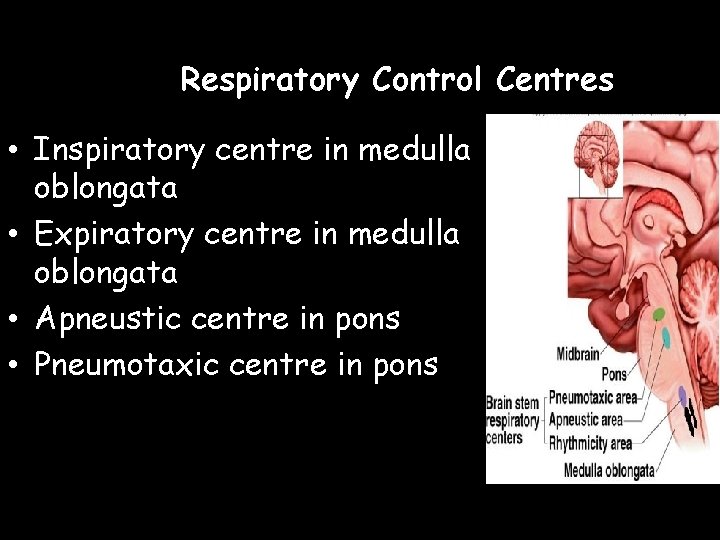
Respiratory Control Centres • Inspiratory centre in medulla oblongata • Expiratory centre in medulla oblongata • Apneustic centre in pons • Pneumotaxic centre in pons
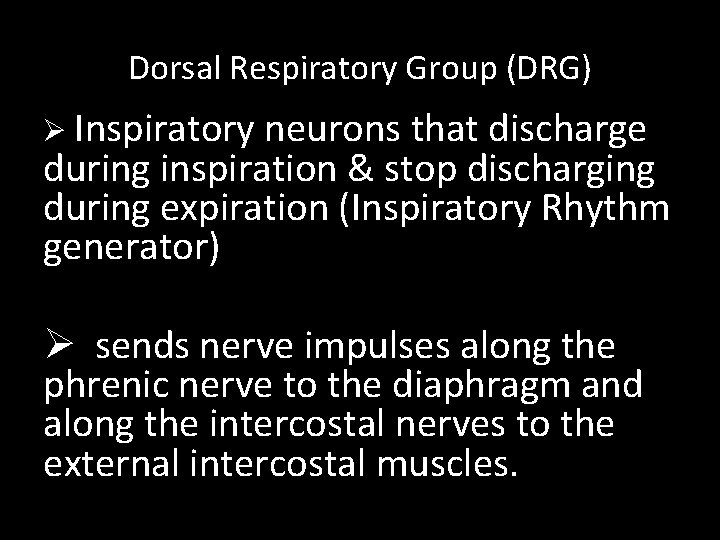
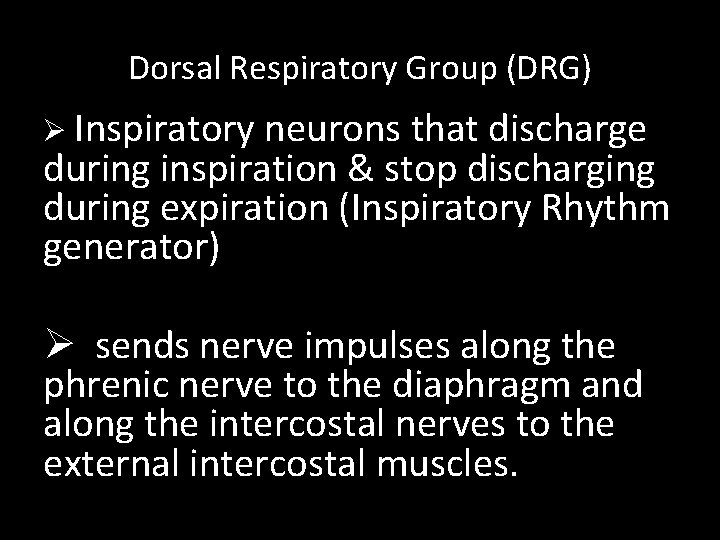
Dorsal Respiratory Group (DRG) Ø Inspiratory neurons that discharge during inspiration & stop discharging during expiration (Inspiratory Rhythm generator) Ø sends nerve impulses along the phrenic nerve to the diaphragm and along the intercostal nerves to the external intercostal muscles.
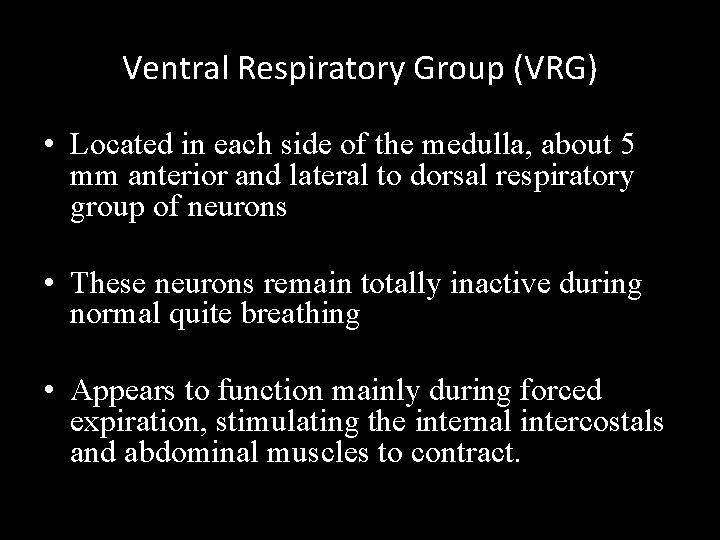
Ventral Respiratory Group (VRG) • Located in each side of the medulla, about 5 mm anterior and lateral to dorsal respiratory group of neurons • These neurons remain totally inactive during normal quite breathing • Appears to function mainly during forced expiration, stimulating the internal intercostals and abdominal muscles to contract.
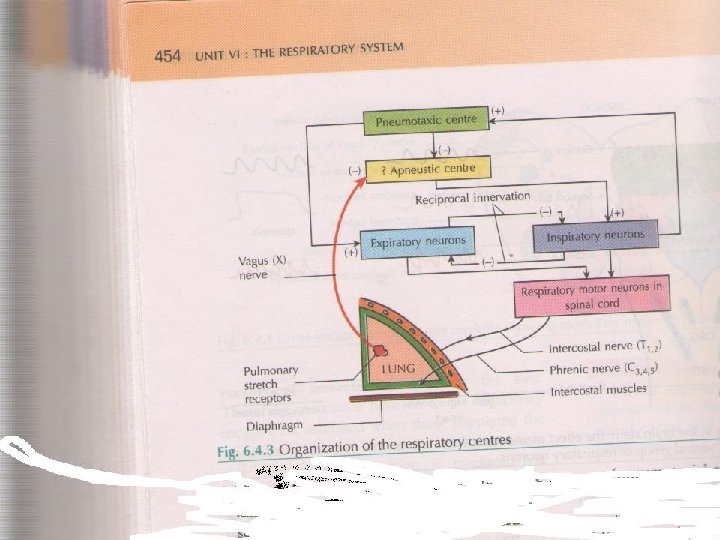
Pontine Respiratory Centers 1 - Apneustic Center (APC): . It receives inhibitory impulses from: - Lung stretch receptors. - Pneumotaxic center (PNC). . When APC is inhibited , inspiration will stop which will turn off the excitation of inspiratory muscles and allow elastic recoil of the lung to cause expiration.
2 - Pneumotaxic Center (PNC): . PNC lies in upper pons. . It controls SWITCH OFF point of inspiration by sending inhibitory impulse to APC. . PNC by switching off inspiration will limit the duration of inspiration.
Control of Respiration • The inspiratory centre in medulla sets breathing rhythm • connected to diaphragm via phrenic nerves and to intercostal muscles via intercostal • Impulses stimulate contraction and inspiration follows • When impulses cease, muscles relax and expiration occurs • Cycle repeats approx. 12 -15 times per minute (autorhythmic neurones).
• Expiration results from passive recoil of the lungs (& muscles) • Neurones of expiratory centre (Ventral Respiratory Group) are inactive during quiet breathing but are activated during forced/laboured breathing. • Expiratory centre contains both inspiratory and expiratory neurones and is activated during forced breathing. • =stimulates contraction of internal intercostals and abdominal muscles. Furthermore VRG increases inspiratory activity.
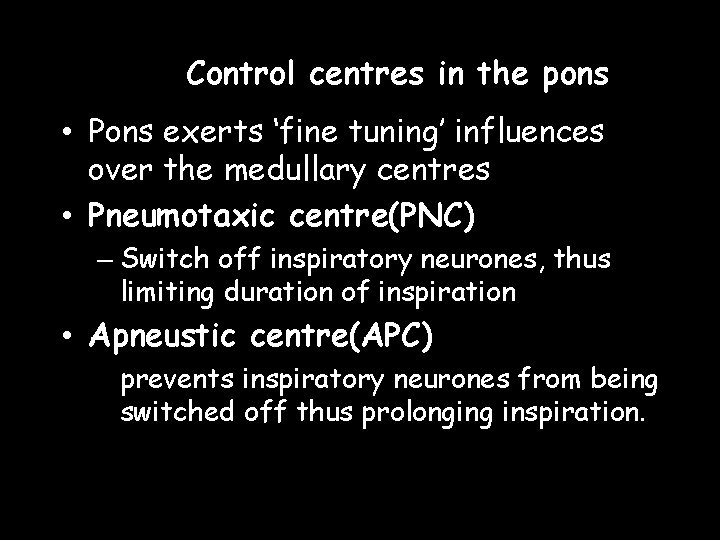
Control centres in the pons • Pons exerts ‘fine tuning’ influences over the medullary centres • Pneumotaxic centre(PNC) – Switch off inspiratory neurones, thus limiting duration of inspiration • Apneustic centre(APC) prevents inspiratory neurones from being switched off thus prolonging inspiration.
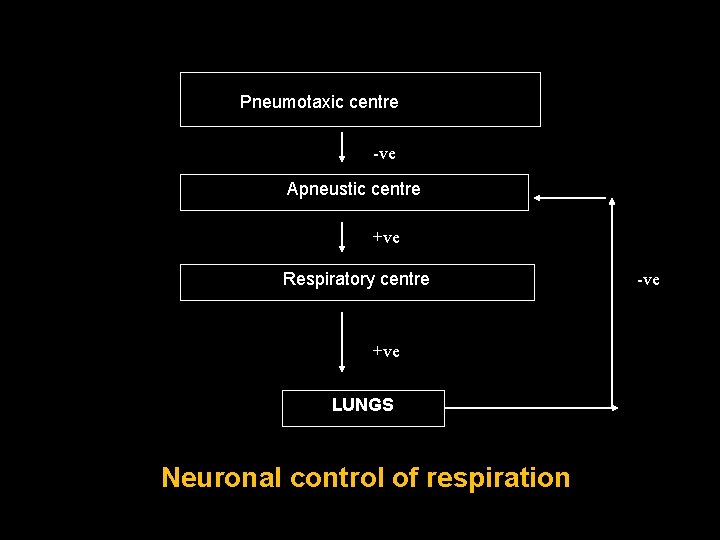
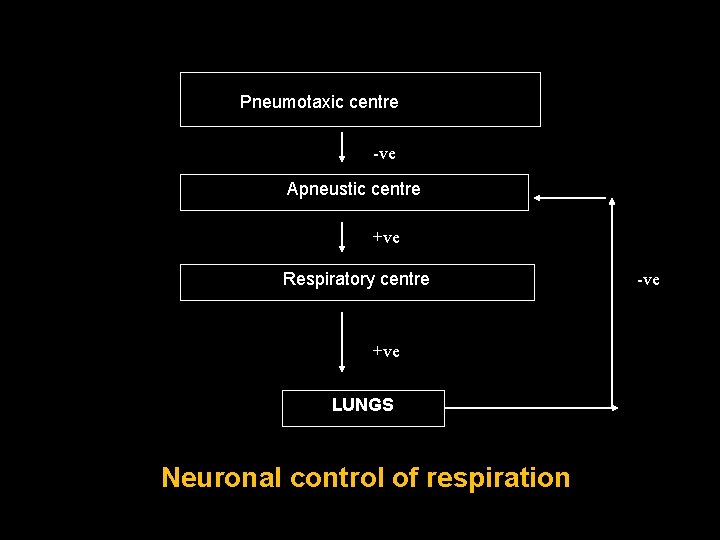
Pneumotaxic centre -ve Apneustic centre +ve Respiratory centre +ve LUNGS Neuronal control of respiration -ve
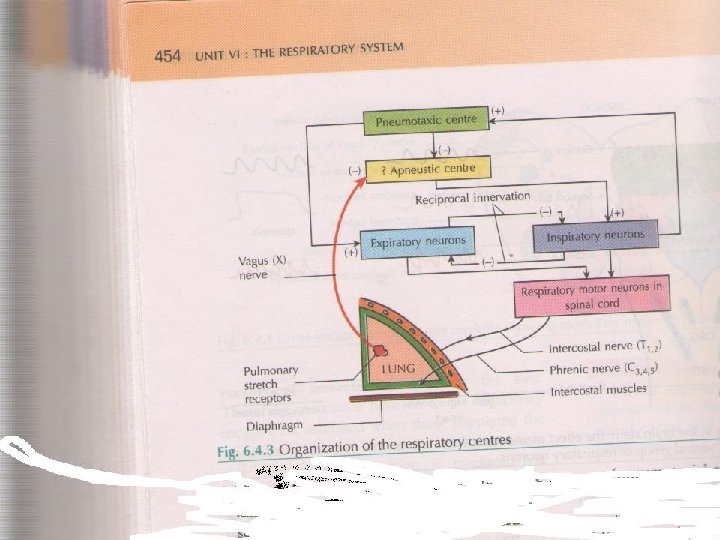
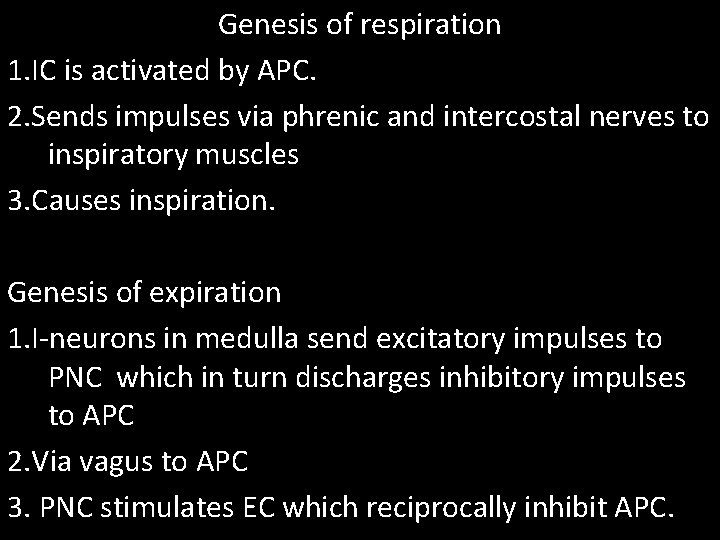
Genesis of respiration 1. IC is activated by APC. 2. Sends impulses via phrenic and intercostal nerves to inspiratory muscles 3. Causes inspiration. Genesis of expiration 1. I-neurons in medulla send excitatory impulses to PNC which in turn discharges inhibitory impulses to APC 2. Via vagus to APC 3. PNC stimulates EC which reciprocally inhibit APC.
Genesis of Rhythmic Respiration -APC sends continuous regular discharge of signals exciting inspiratory neurons of DRG. -DRG sends impulses down the spinal cord to diaphragm and external intercostals muscles causing inspiration and stimulation of stretch receptors in the lungs which will inhibit APC and DRG via vagus. -At the same time , PNC inhibits APC to switch off inspiration. This stops inspiration and brings expiration
Factors affecting rate and depth of respiration • Hering – Breuer reflex – Stretch receptors in bronchi and bronchioles – When stimulated, send inhibitory impulses along vagus nerve to inspiration centre – Inspiration is inhibited and expiration occurs – Prevents over inflation of lungs
J-receptor Reflex • Pulmonary emboli or oedema →juxtapulmonary -capillaries receptors →vagal afferent to respiratory centre → rapid shallow respiration • These receptors are responsible for the sensation of air hunger (Dyspnea; shortness of breath)
• Voluntary Control – Control from cerebral cortex (breath-holding, speech etc. ) • Chemical regulation – Central chemoreceptors in medulla sensitive to changes in H+ conc or PCO 2 in CSF – Peripheral chemoreceptors in aortic and carotid bodies are sensitive to changes in H+, PCO 2 and PO 2
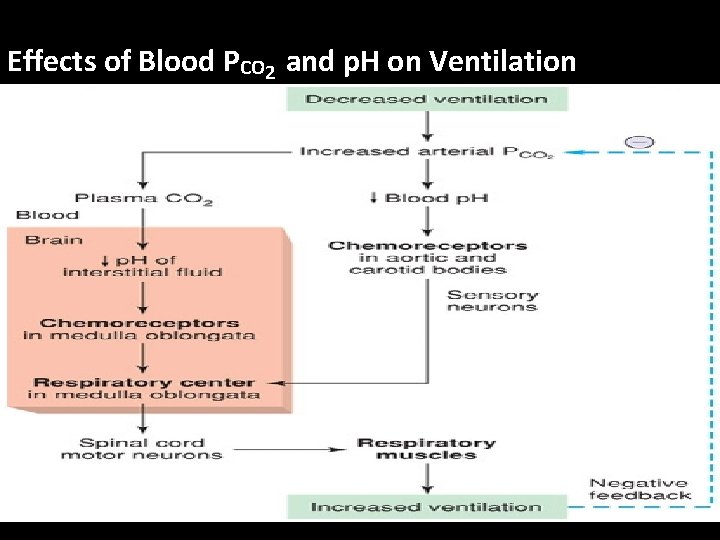
Chemical Regulation of Respiration It is the basic mechanism for regulation of breathing. -Increase arterial PCO 2 -Increase arterial H ion -Decrease arterial PO 2 Stimulate respiratory chemoreceptors Increase activity of respiratory center and Increase pulmonary ventilation.
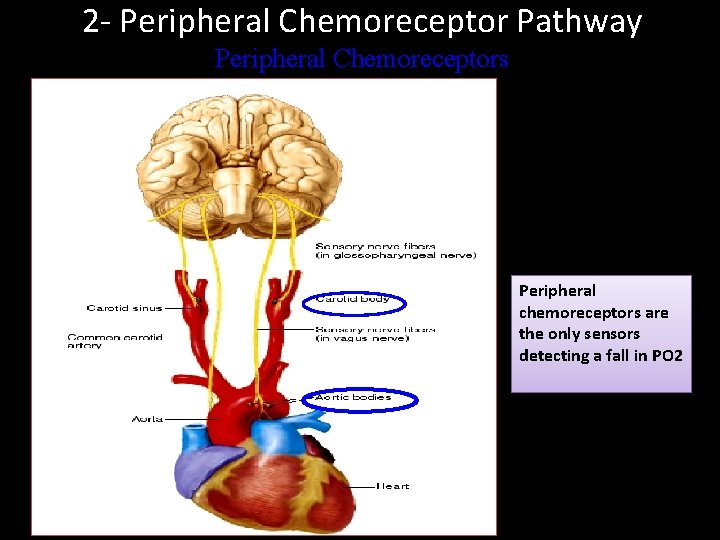
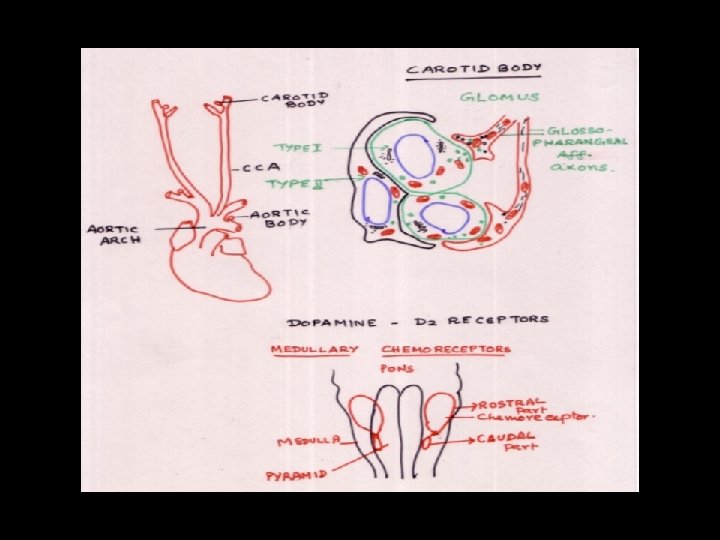
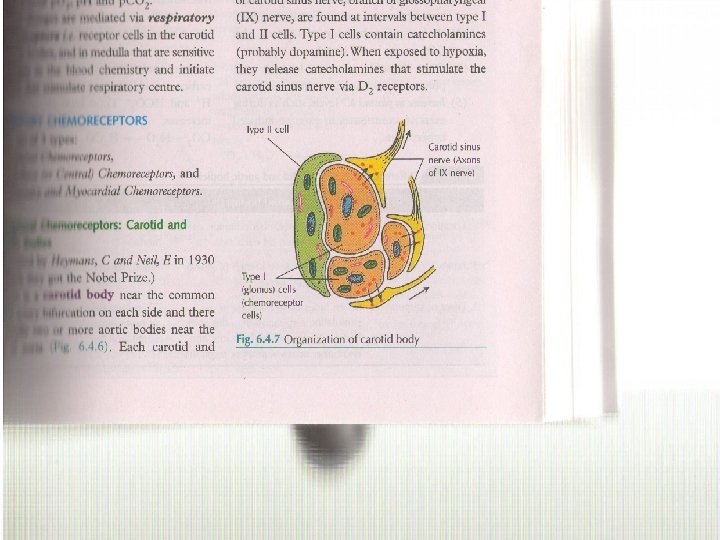
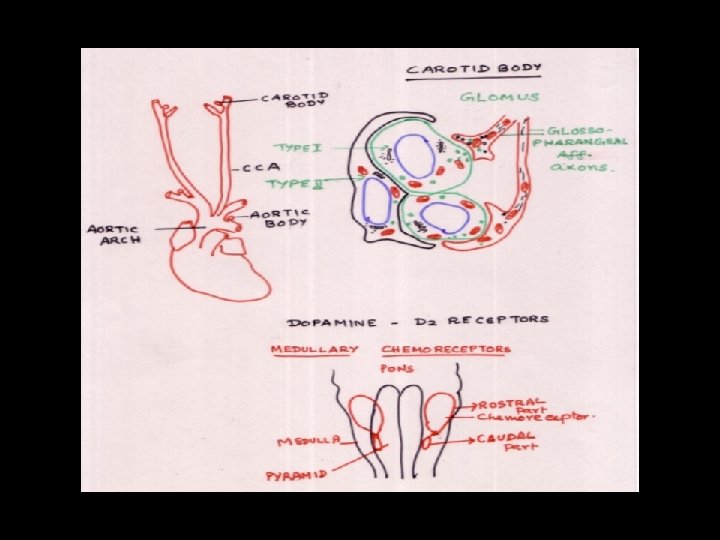
Chemoreceptors. Peripheral Site: Aortic bodies: over aortic arch Carotid bodies: at bifurcation of each common carotid artery. Innervation: Carotid bodies: glossopharyngeal nerve Aortic bodies: vagus nerve
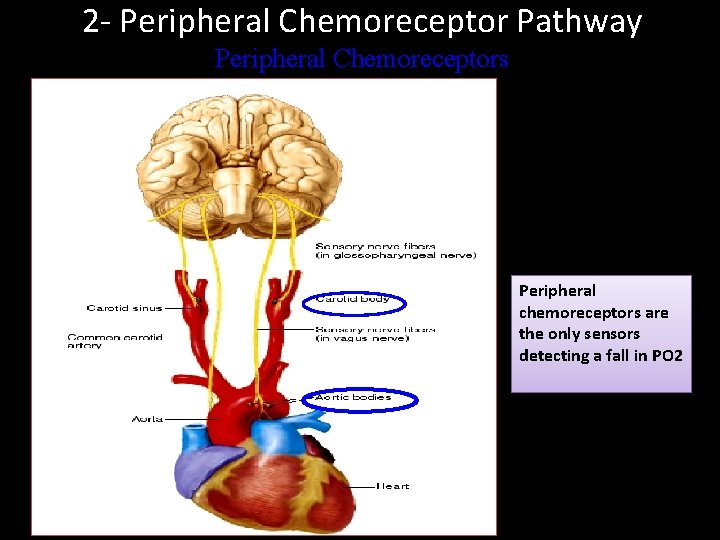
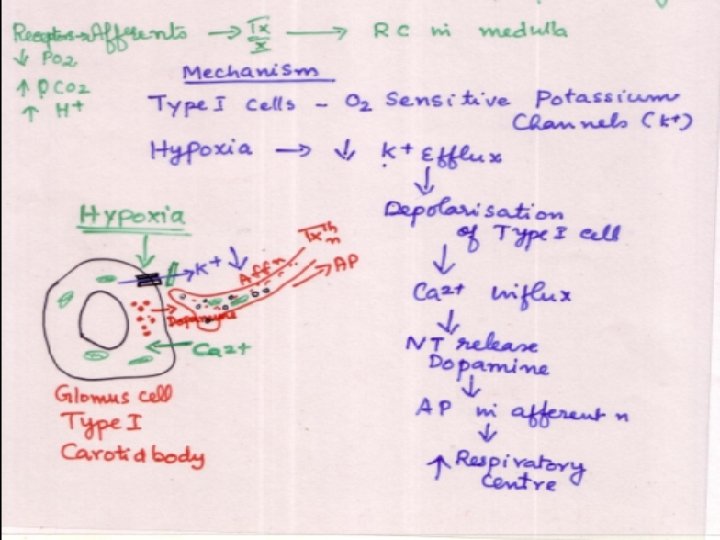
2 - Peripheral Chemoreceptor Pathway Peripheral Chemoreceptors Peripheral chemoreceptors are the only sensors detecting a fall in PO 2
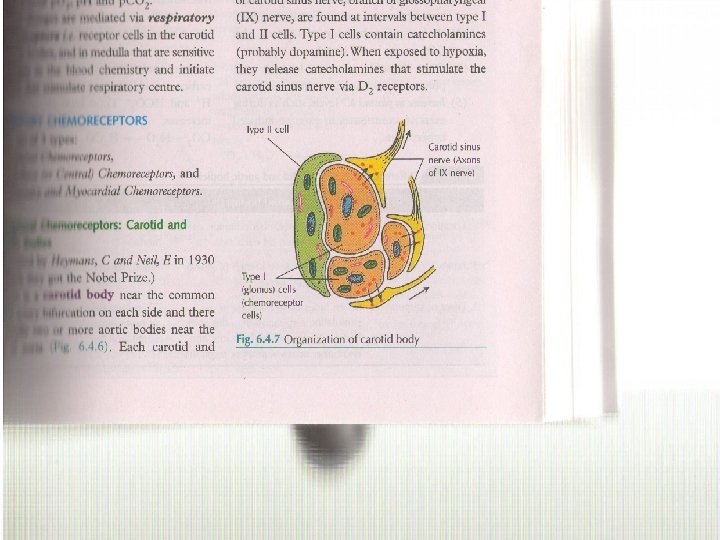
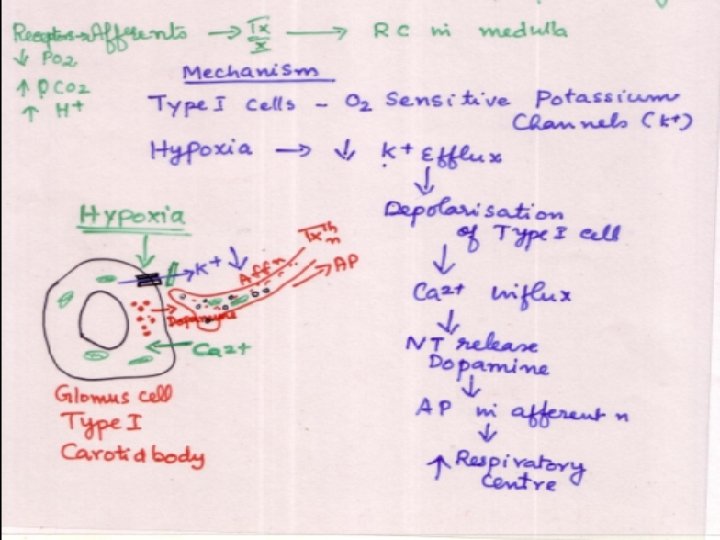
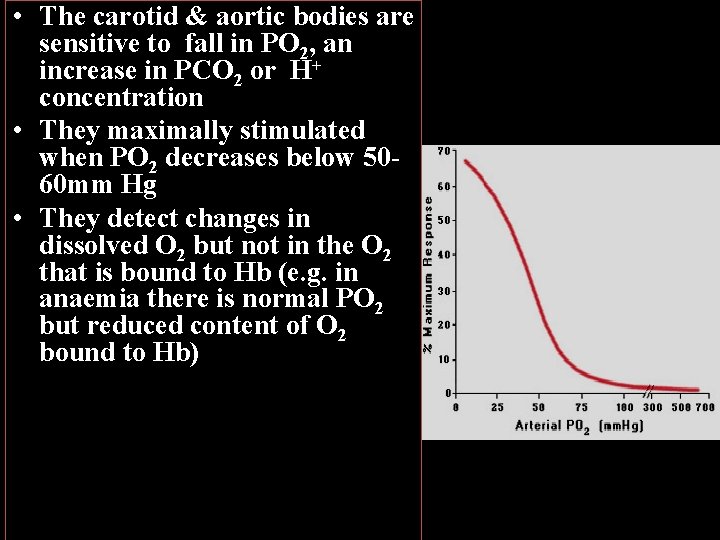
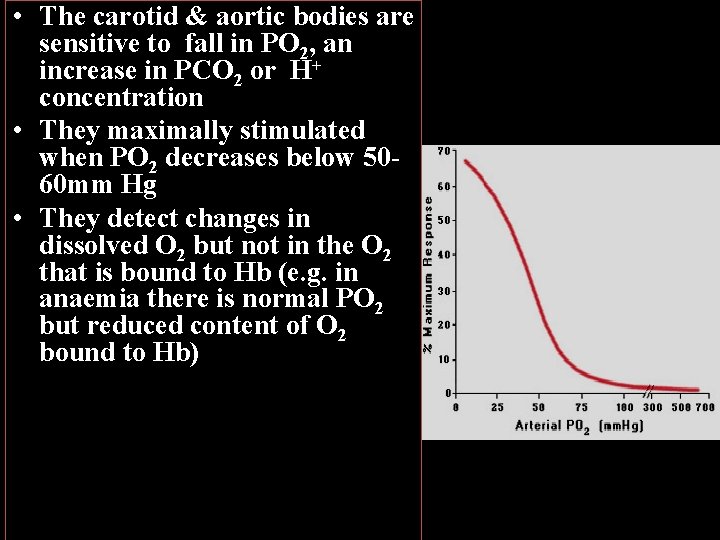
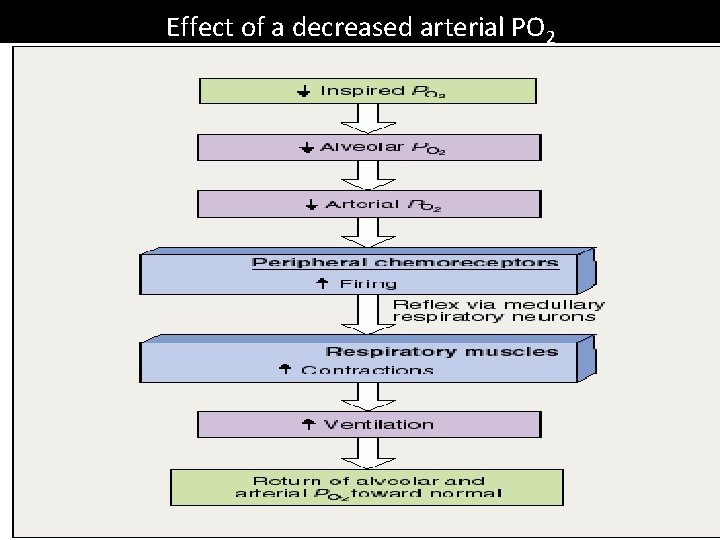
• The carotid & aortic bodies are sensitive to fall in PO 2, an increase in PCO 2 or H+ concentration • They maximally stimulated when PO 2 decreases below 5060 mm Hg • They detect changes in dissolved O 2 but not in the O 2 that is bound to Hb (e. g. in anaemia there is normal PO 2 but reduced content of O 2 bound to Hb)
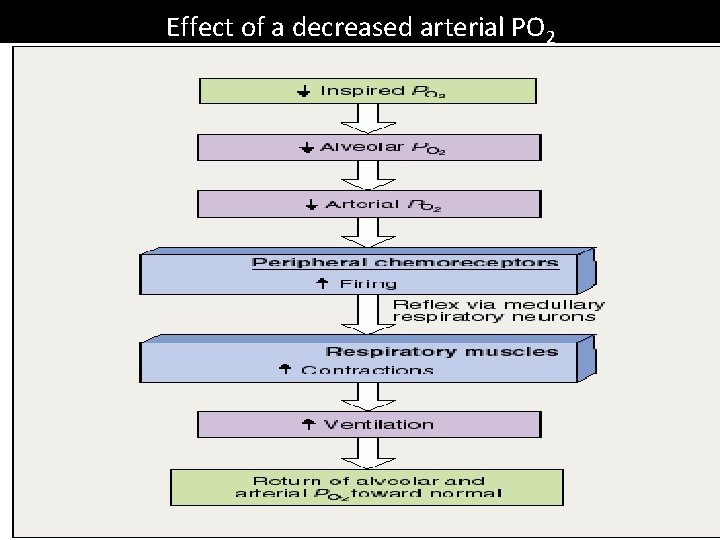
Effect of a decreased arterial PO 2
Central Chemoreceptors Site: Located bilaterally just beneath central surface of medulla. Stimulus: 1 - Response to H ion ( primary stimulus). 2 - Response to PCO 2. 3 - Response to Po 2.
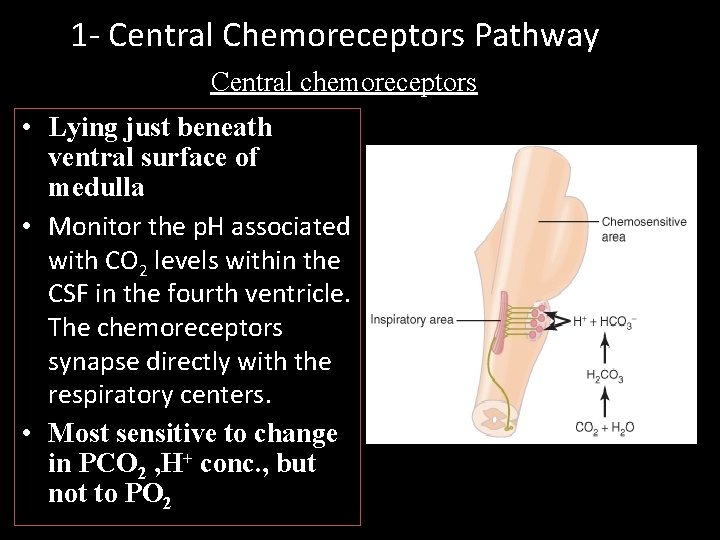
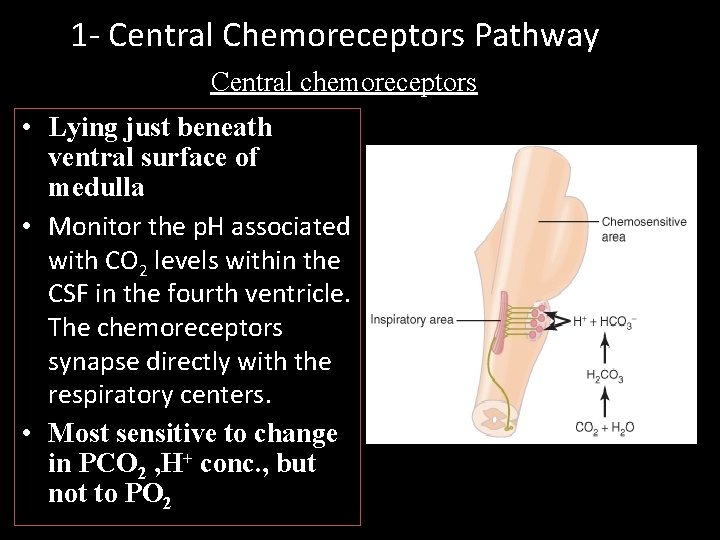
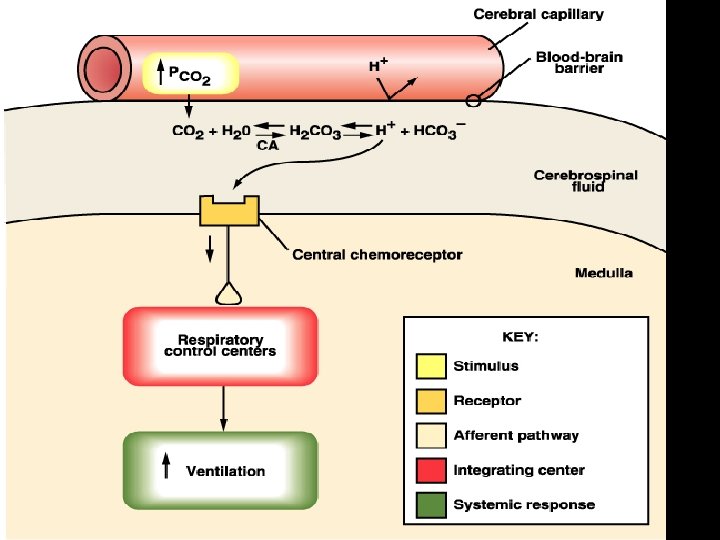
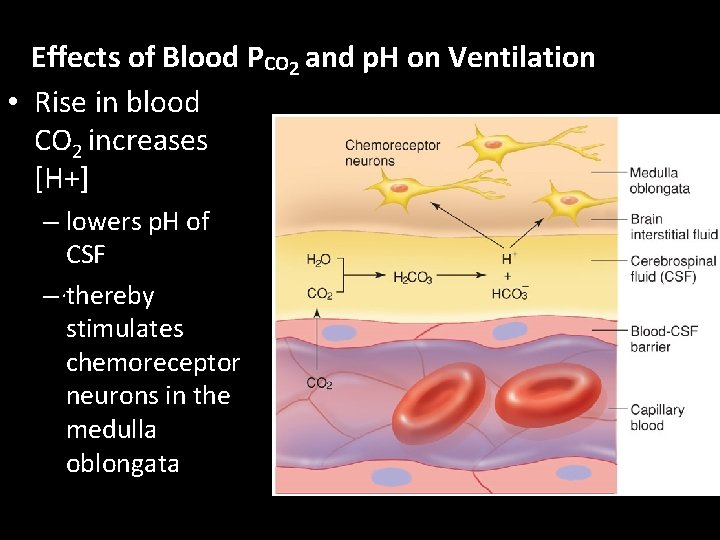
1 - Central Chemoreceptors Pathway Central chemoreceptors • Lying just beneath ventral surface of medulla • Monitor the p. H associated with CO 2 levels within the CSF in the fourth ventricle. The chemoreceptors synapse directly with the respiratory centers. • Most sensitive to change in PCO 2 , H+ conc. , but not to PO 2
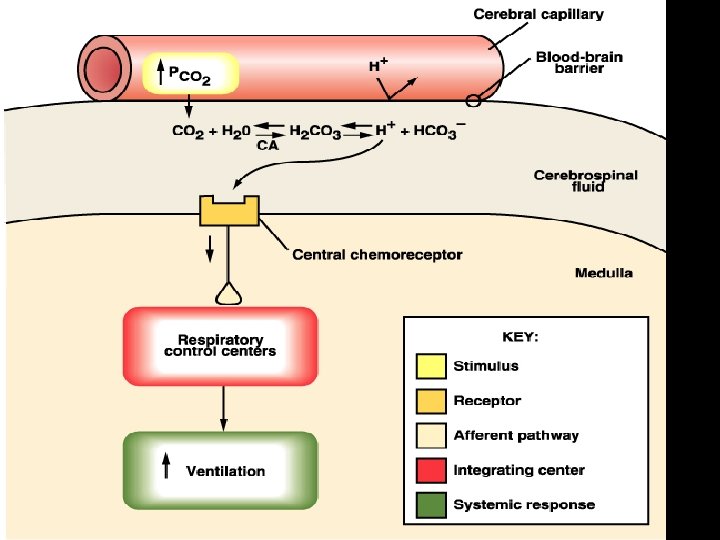
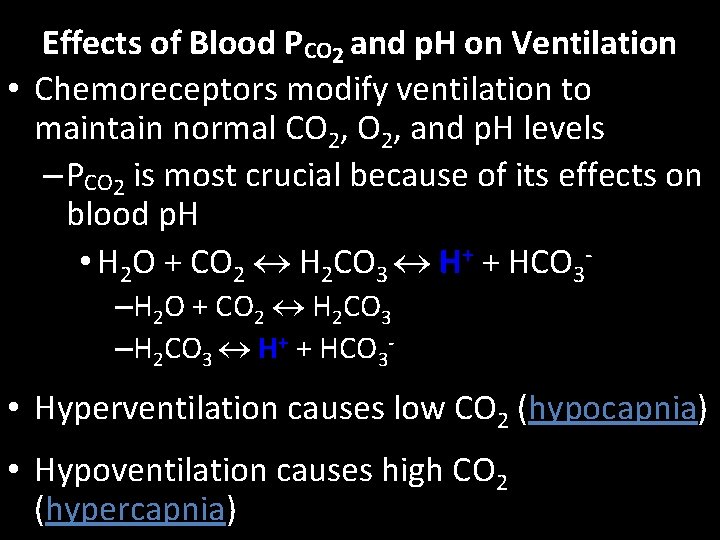
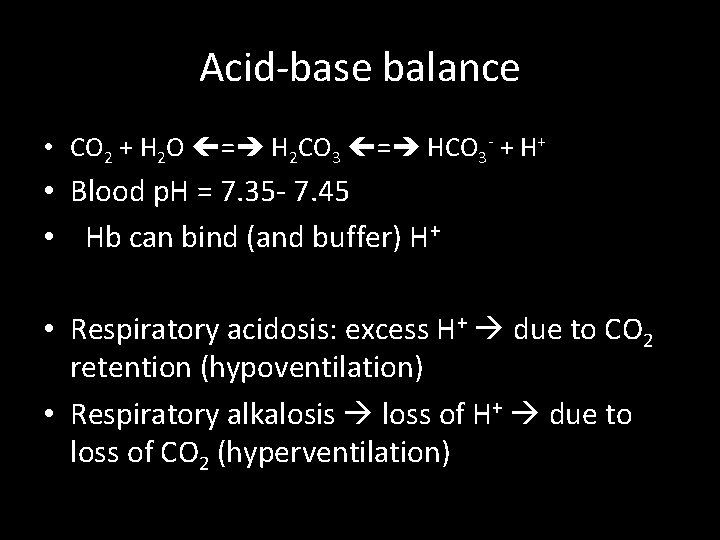
Effects of Blood PCO 2 and p. H on Ventilation • Chemoreceptors modify ventilation to maintain normal CO 2, and p. H levels – PCO 2 is most crucial because of its effects on blood p. H • H 2 O + CO 2 H 2 CO 3 H+ + HCO 3–H 2 O + CO 2 H 2 CO 3 –H 2 CO 3 H+ + HCO 3 - • Hyperventilation causes low CO 2 (hypocapnia) • Hypoventilation causes high CO 2 (hypercapnia)
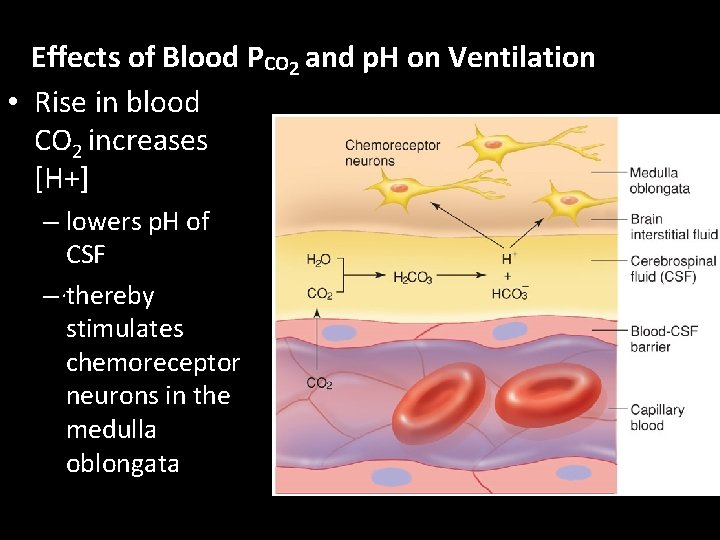
Effects of Blood PCO 2 and p. H on Ventilation • Rise in blood CO 2 increases [H+] – lowers p. H of CSF –. thereby stimulates chemoreceptor neurons in the medulla oblongata
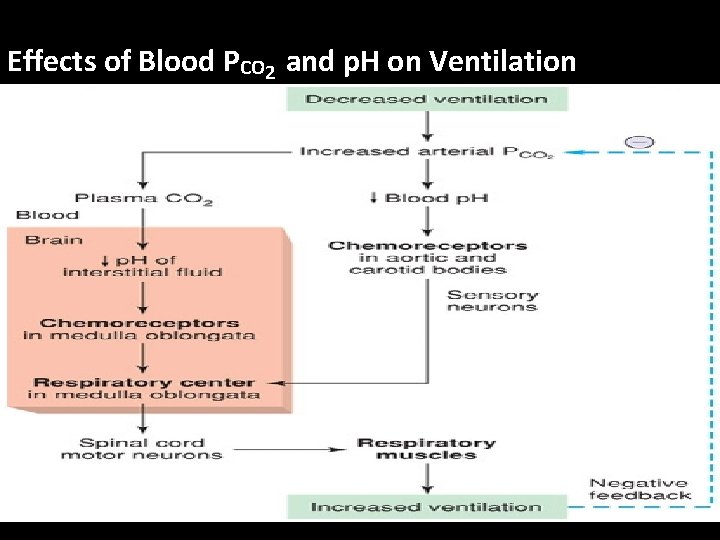
Effects of Blood PCO 2 and p. H on Ventilation
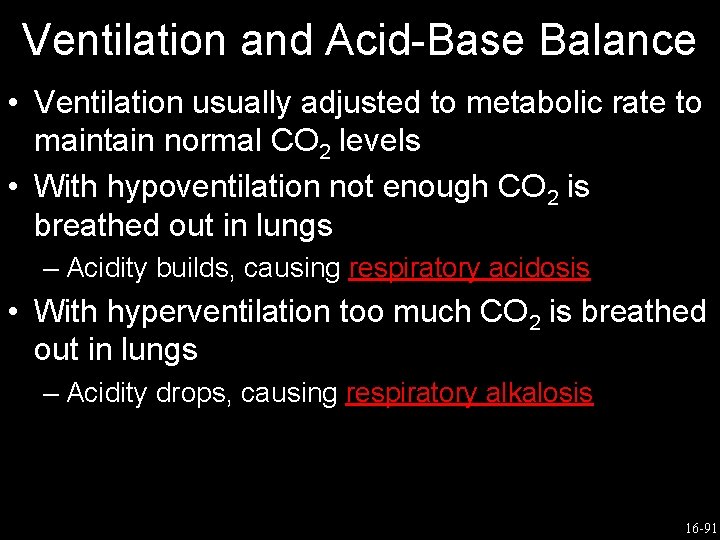
Acid-base balance • CO 2 + H 2 O = H 2 CO 3 = HCO 3 - + H+ • Blood p. H = 7. 35 - 7. 45 • Hb can bind (and buffer) H+ • Respiratory acidosis: excess H+ due to CO 2 retention (hypoventilation) • Respiratory alkalosis loss of H+ due to loss of CO 2 (hyperventilation)
Ventilation and Acid-Base Balance • Ventilation usually adjusted to metabolic rate to maintain normal CO 2 levels • With hypoventilation not enough CO 2 is breathed out in lungs – Acidity builds, causing respiratory acidosis • With hyperventilation too much CO 2 is breathed out in lungs – Acidity drops, causing respiratory alkalosis 16 -91
• Respiratory acidosis (p. H < 7. 35) caused by failure of pulmonary ventilation, CO 2 retention, excess fatty acids in diabetics, accumulation of latic acid) – hypercapnia: PCO 2 > 43 mm. Hg • CO 2 easily crosses blood-brain barrier • in CSF the CO 2 reacts with water and releases H+ • central chemoreceptors strongly stimulate inspiratory center – “wash out” CO 2 pushes reaction to the left CO 2 (expired) + H 2 O H 2 CO 3 HCO 3 - + H+ – so hyperventilation reduces H+ (reduces acid)
Respiratory alkalosis (p. H > 7. 45) hypocapnia: PCO 2 < 37 mm. Hg Hypoventilation ( CO 2), pushes reaction to the right CO 2 + H 2 O H 2 CO 3 HCO 3 - + H+ + (increases acid), lowers p. H to normal H p. H imbalances can have metabolic causes uncontrolled diabetes mellitus fat oxidation causes ketoacidosis
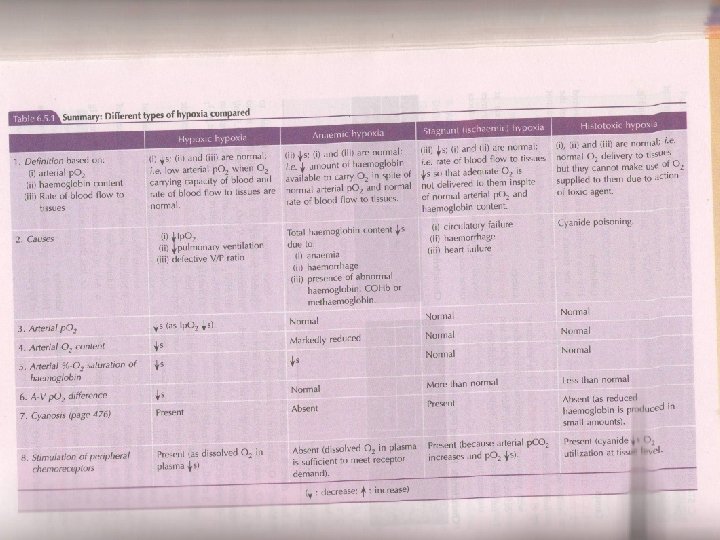
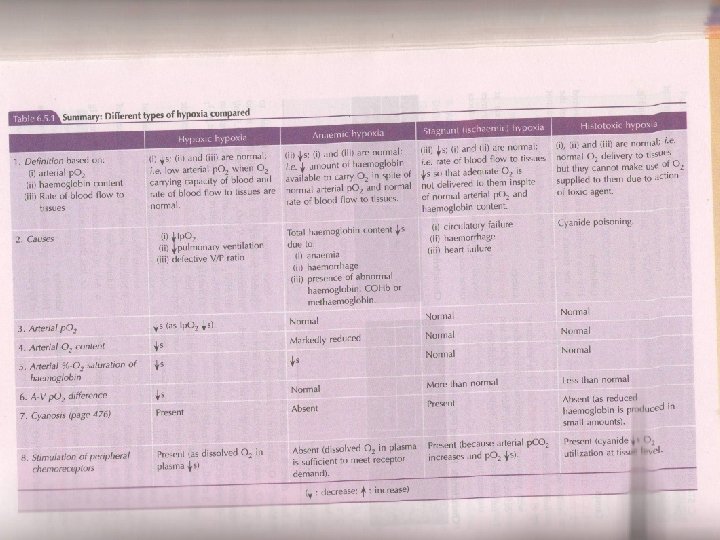
Hypoxic hypoxia • Inadequate PO 2 in arterial blood (Pa. O 2). May results from: • Inadequate PO 2 in inspired air • Major hypoventilation • Inadequate alveolar – capillary transfer
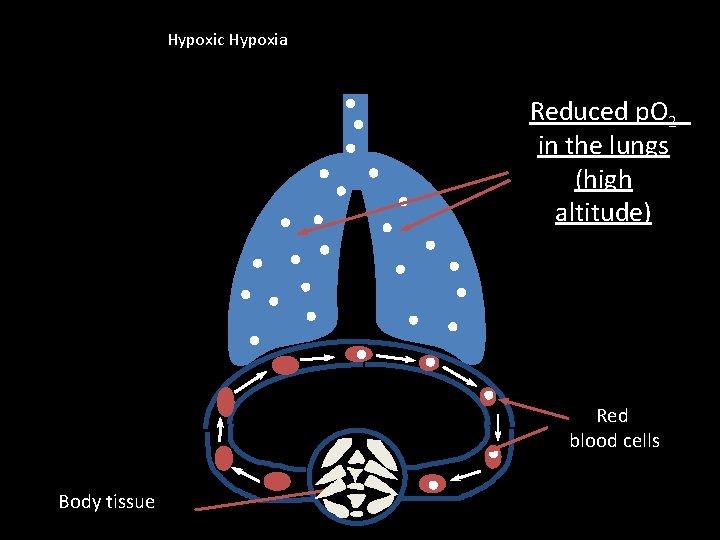
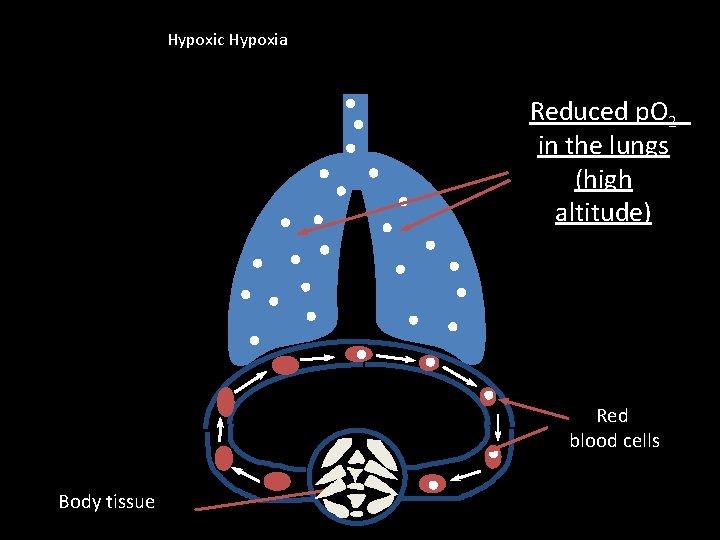
Hypoxic Hypoxia Reduced p. O 2 in the lungs (high altitude) Red blood cells Body tissue
• • • Partial pressure of oxygen –decreases 0 xygen carrying capacity –normal Oxygen content in blood-decreases Blood flow rate and tissue utilization –normal A-V 0 f oxygen decreases Cyanosis is present
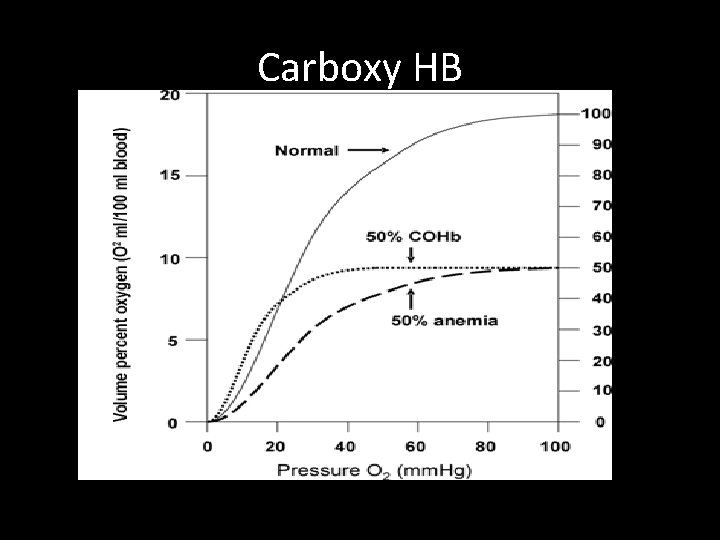
Anaemic Hypoxia • Pa. O 2 normal but concentration of functional haemoglobin is reduced. • Possible causes of anaemia: – – – Deficiencies of iron, vitamin B 12, folate or copper Kidney disease affecting production of erythropoietin Excessive blood loss Hereditary spherocytosis (RBCs have short life span) Carbon monoxide poisoning
• • • Partial pressure of oxygen –normal 0 xygen carrying capacity –decreases Oxygen content in blood-decreases Blood flow rate and tissue utilization –normal A-V 0 f oxygen -normal Cyanosis is not present
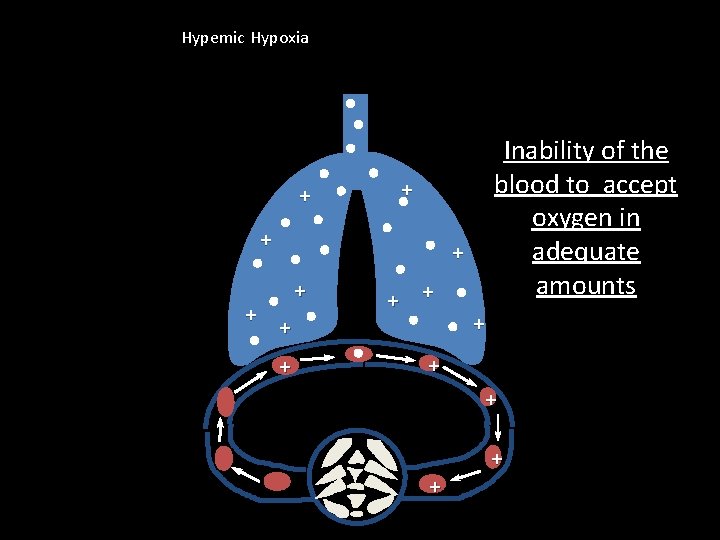
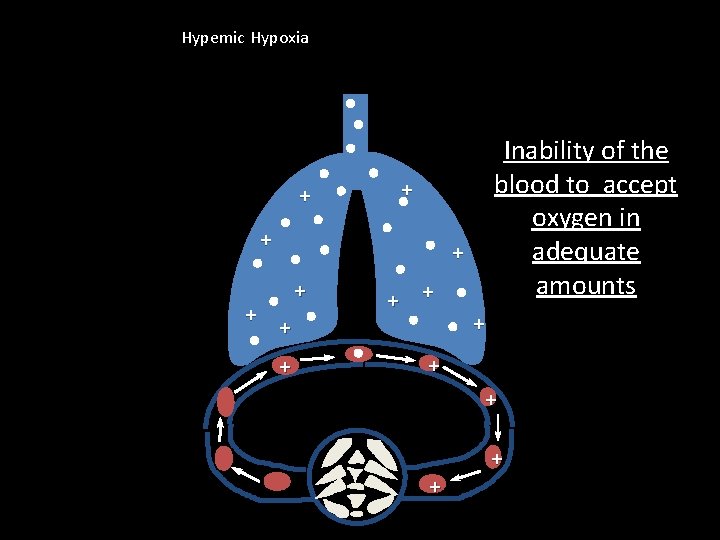
Hypemic Hypoxia + + + Inability of the blood to accept oxygen in adequate amounts + + + + +
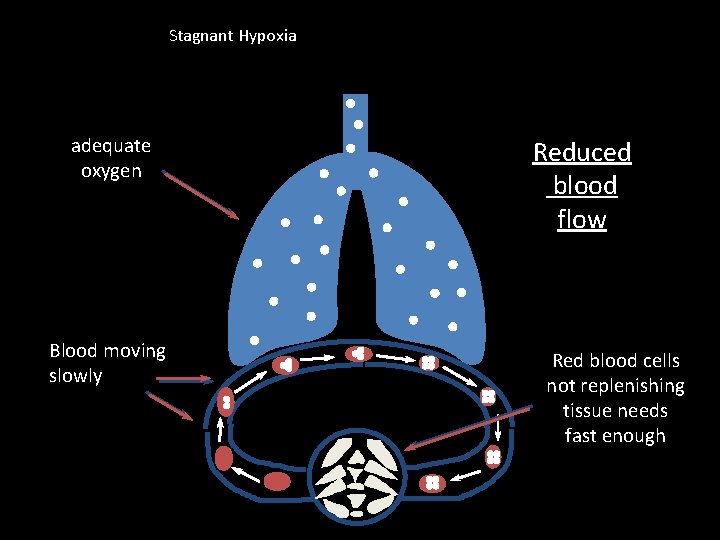
Stagnant hypoxia • Reduction in supply of oxygen to tissues produced by a reduced blood flow i. e. circulatory failure (e. g. angina, claudication etc. ) • Pa. O 2 (and Pa. CO 2) may be normal but delivery is not. Initially tissue oxygenation is maintained by increasing the degree of oxygen extraction from the blood, but as tissue perfusion worsens this becomes insufficient and tissue hypoxia occurs.
• Partial pressure of oxygen –normal 0 xygen carrying capacity –normal Oxygen content in blood-normal • Blood flow rate–decreases • tissue utilization- normal • A-V 0 f oxygen decreases • Cyanosis is present
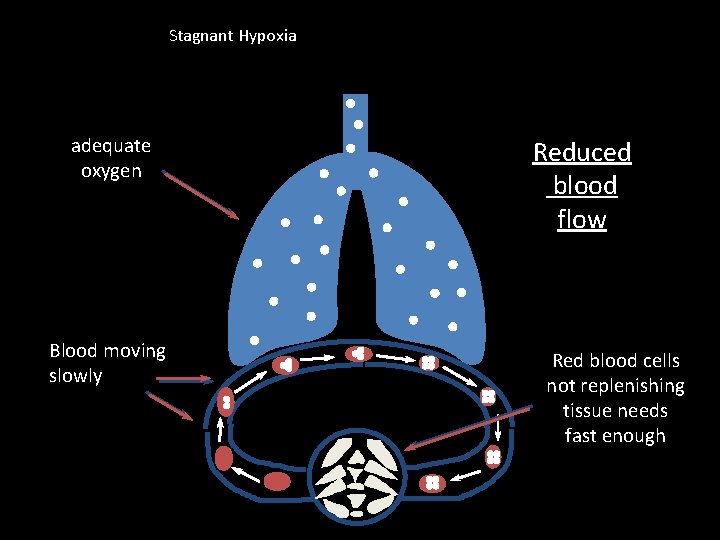
Stagnant Hypoxia adequate oxygen Blood moving slowly Reduced blood flow Red blood cells not replenishing tissue needs fast enough
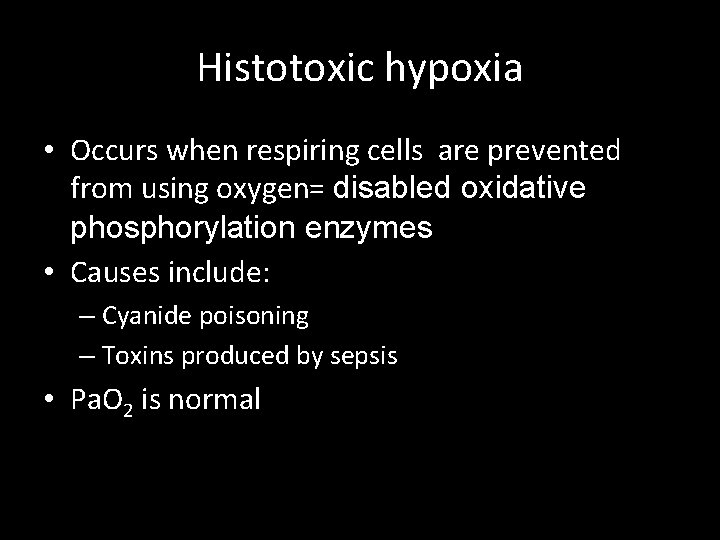
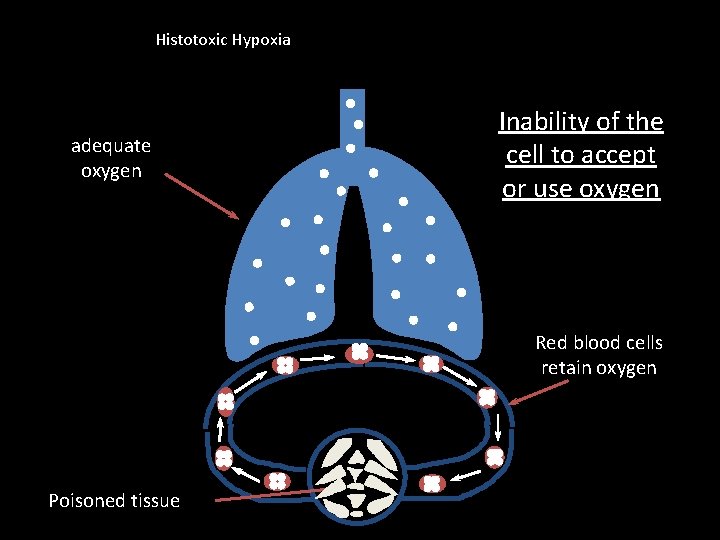
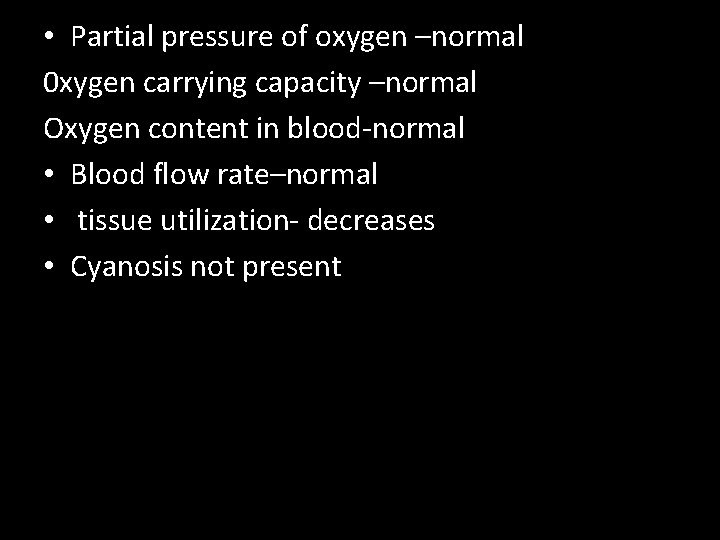
Histotoxic hypoxia • Occurs when respiring cells are prevented from using oxygen= disabled oxidative phosphorylation enzymes • Causes include: – Cyanide poisoning – Toxins produced by sepsis • Pa. O 2 is normal
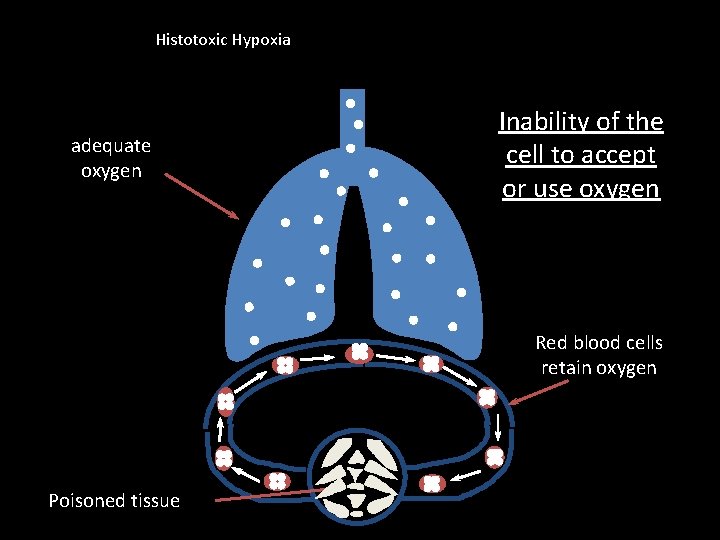
Histotoxic Hypoxia adequate oxygen Inability of the cell to accept or use oxygen Red blood cells retain oxygen Poisoned tissue
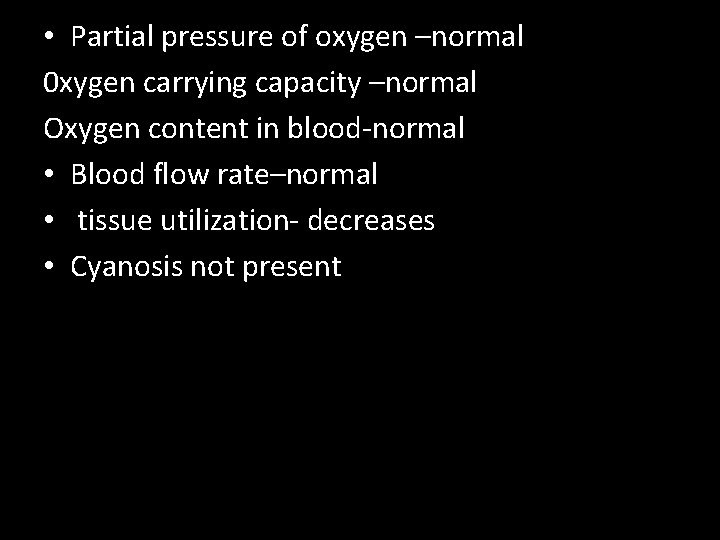
• Partial pressure of oxygen –normal 0 xygen carrying capacity –normal Oxygen content in blood-normal • Blood flow rate–normal • tissue utilization- decreases • Cyanosis not present
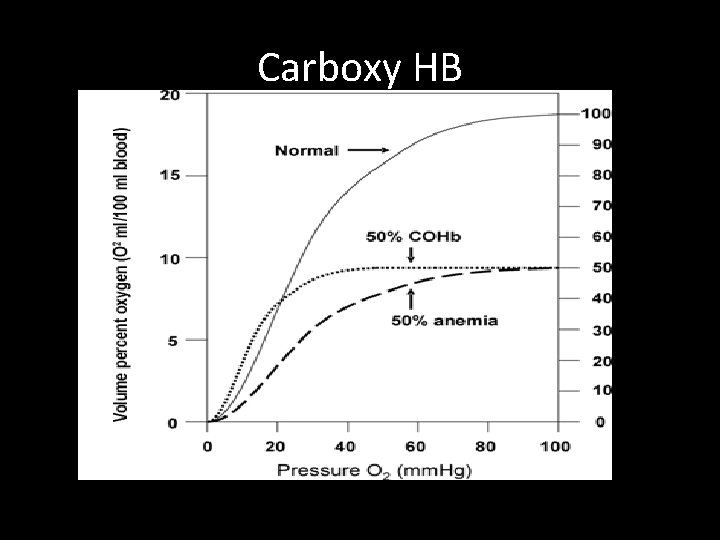
Carboxy HB
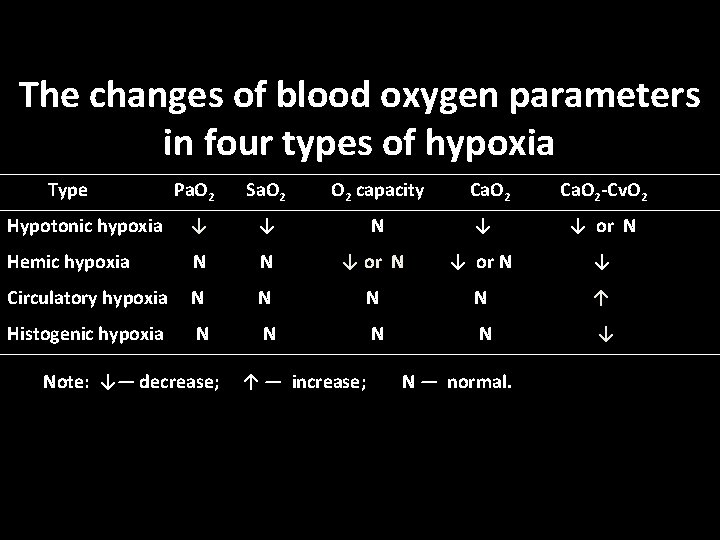
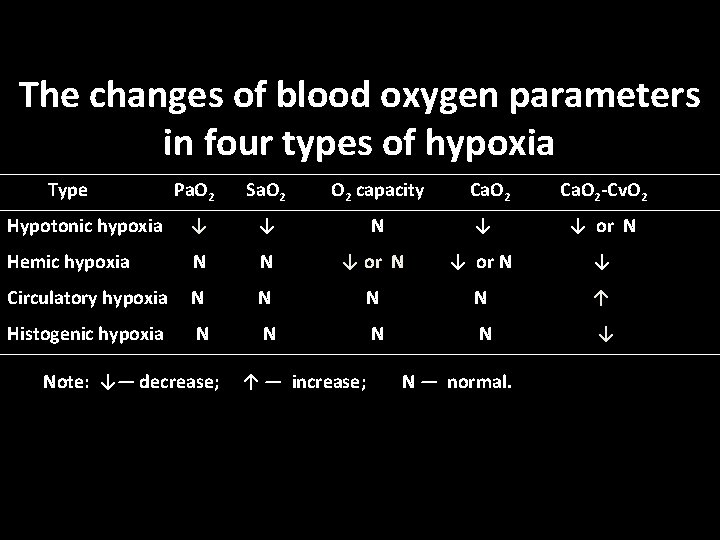
The changes of blood oxygen parameters in four types of hypoxia Type Pa. O 2 Sa. O 2 capacity Hypotonic hypoxia ↓ ↓ N ↓ ↓ or N Hemic hypoxia N N ↓ or N ↓ Circulatory hypoxia N N ↑ Histogenic hypoxia N N ↓ Note: ↓— decrease; ↑ — increase; Ca. O 2 N — normal. Ca. O 2 -Cv. O 2
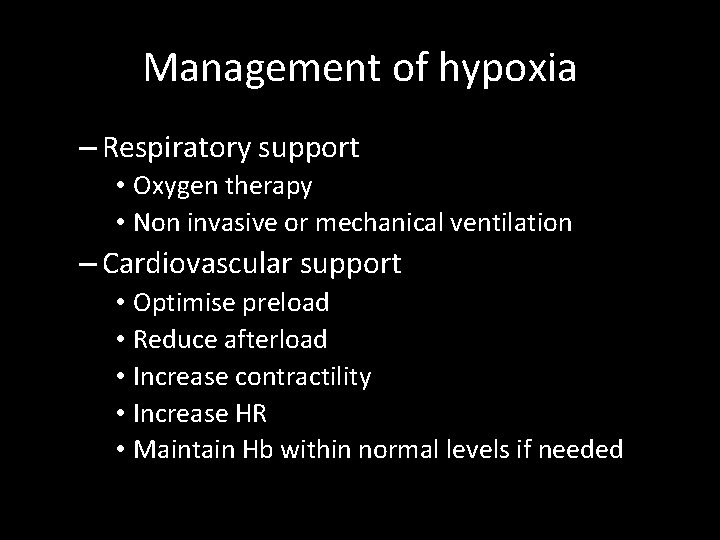
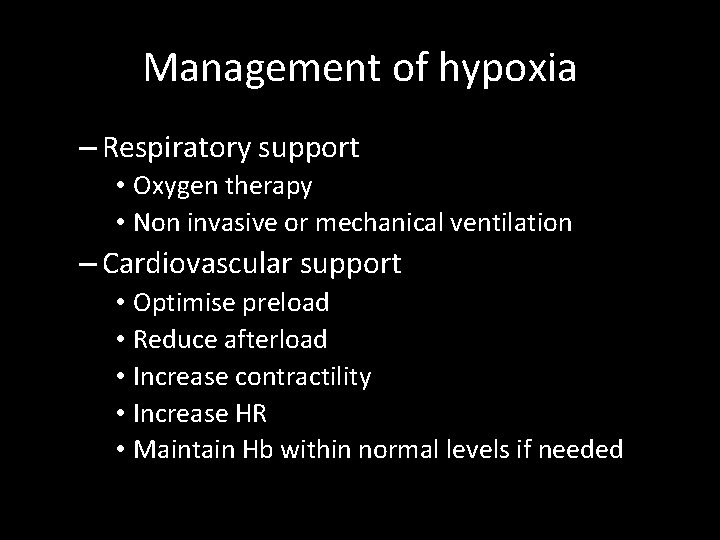
Management of hypoxia – Respiratory support • Oxygen therapy • Non invasive or mechanical ventilation – Cardiovascular support • Optimise preload • Reduce afterload • Increase contractility • Increase HR • Maintain Hb within normal levels if needed
• • • Effects of hyoxia On respiration Stimulate PC to increase respiration On cvs Drowsiness , depression, headache, emotional outbursts Headache Cvs Increase BP and HR (stimulation of VMC) Treatment Oxygen therapy
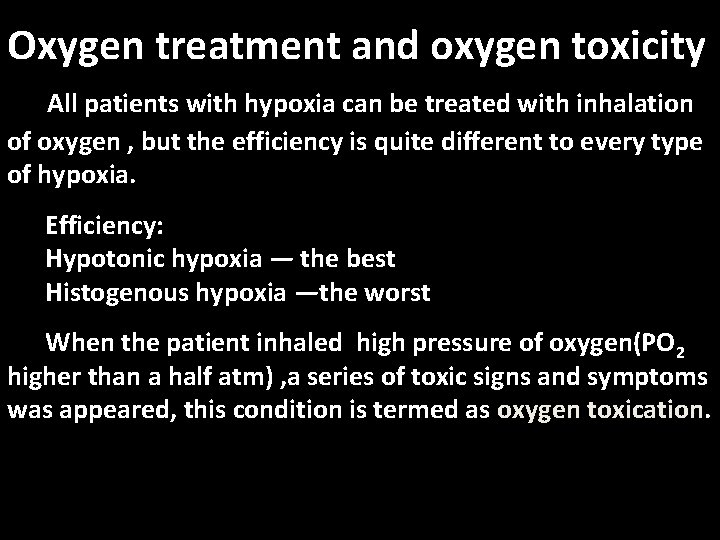
Oxygen treatment and oxygen toxicity All patients with hypoxia can be treated with inhalation of oxygen , but the efficiency is quite different to every type of hypoxia. Efficiency: Hypotonic hypoxia — the best Histogenous hypoxia —the worst When the patient inhaled high pressure of oxygen(PO 2 higher than a half atm) , a series of toxic signs and symptoms was appeared, this condition is termed as oxygen toxication.
Oxygen toxication: 1. Pulmonary oxygen toxication 2. Cerebral oxygen toxication The mechanisms of oxygen toxicity: Reactive oxygen species or oxygen free radicals.
Cyanosis • Bluish discoluration of skin and or mucus membrane due to presence of atleast 5 gm of reduced Hb/100 ml of blood. • Sites • Mucous membrane • Lips • Earlobes nail beds and tips of nose • Occurence • Total amt of Hb • Degree of Hb unsaturation • State of capillary circulation
• Types • Central cyanosis • Peripheral cyanosis
 Overall reaction of cellular respiration
Overall reaction of cellular respiration What are the net products of the krebs cycle
What are the net products of the krebs cycle Neural regulation of respiration flow chart
Neural regulation of respiration flow chart Internal respiration vs external respiration
Internal respiration vs external respiration The nose serves all the following functions except
The nose serves all the following functions except Enzyme regulation
Enzyme regulation Reactants products and leftovers
Reactants products and leftovers Debye huckel limiting law
Debye huckel limiting law Aoa and aon examples
Aoa and aon examples Form content and use
Form content and use Activity 1 activity 2
Activity 1 activity 2 Activity 2 identifying the pattern
Activity 2 identifying the pattern Activity 2:
Activity 2: Production activity control
Production activity control Lesson quiz 7-5 deviance and social control
Lesson quiz 7-5 deviance and social control Production activity control
Production activity control Production activity control
Production activity control Activity level control
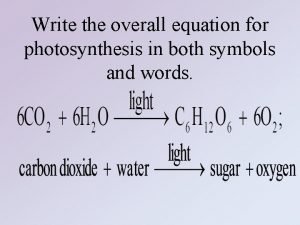
Activity level control Write the overall equation for photosynthesis
Write the overall equation for photosynthesis Purpose of discussion
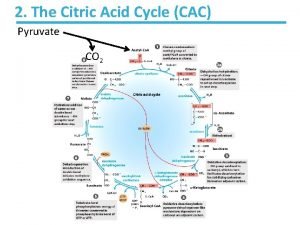
Purpose of discussion Citric acid cycle overall reaction
Citric acid cycle overall reaction Testing overall ability
Testing overall ability Overall expression
Overall expression What is the overall message of romeo and juliet
What is the overall message of romeo and juliet Molecularity of reaction
Molecularity of reaction The overall heat transfer coefficient
The overall heat transfer coefficient Menentukan materialitas audit
Menentukan materialitas audit Shell side reynolds number
Shell side reynolds number The overall heat transfer coefficient
The overall heat transfer coefficient Glycolysis overall reaction
Glycolysis overall reaction The overall reaction in a commercial heat pack
The overall reaction in a commercial heat pack Overall rate law of a reaction
Overall rate law of a reaction Chapter 7 business management
Chapter 7 business management Retail strategic planning
Retail strategic planning New venture fitness drinks concept statement
New venture fitness drinks concept statement What is an overall state of well-being or total health
What is an overall state of well-being or total health Overall cas progress
Overall cas progress Overall cas progress
Overall cas progress Citric acid cycle overall reaction
Citric acid cycle overall reaction Glycolysis overall reaction
Glycolysis overall reaction Theme is the message
Theme is the message Securing information systems
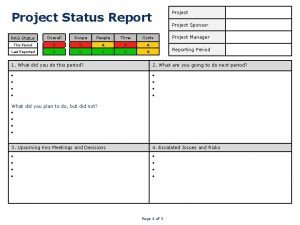
Securing information systems Overall rag status
Overall rag status Wavelike describes melodic
Wavelike describes melodic Clearly trivial threshold
Clearly trivial threshold Overall force acting on an object
Overall force acting on an object Overall compositie
Overall compositie The general goal of science is to
The general goal of science is to Project overall status
Project overall status Overall equipment effectiveness
Overall equipment effectiveness What is the mood in literature
What is the mood in literature Overall plan or structure of music
Overall plan or structure of music The line of a dress or the garment's overall shape
The line of a dress or the garment's overall shape What are the characteristics of a short story
What are the characteristics of a short story First screen feasibility analysis example
First screen feasibility analysis example A carefully developed overall approach to leading
A carefully developed overall approach to leading Overall reaction of glycolysis
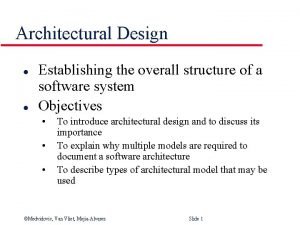
Overall reaction of glycolysis What is a overall structure
What is a overall structure