Rapidly Progressive Crescentic GlomerulonephritisRPGN Is a syndrome associated



- Slides: 58
Rapidly Progressive (Crescentic) Glomerulonephritis(RPGN) - Is a syndrome associated with severe glomerular injury, but does not denote a specific etiologic form of glomerulonephritis. - It is characterized by rapid and progressive loss of renal function associated with severe oliguria and signs of nephritic syndrome
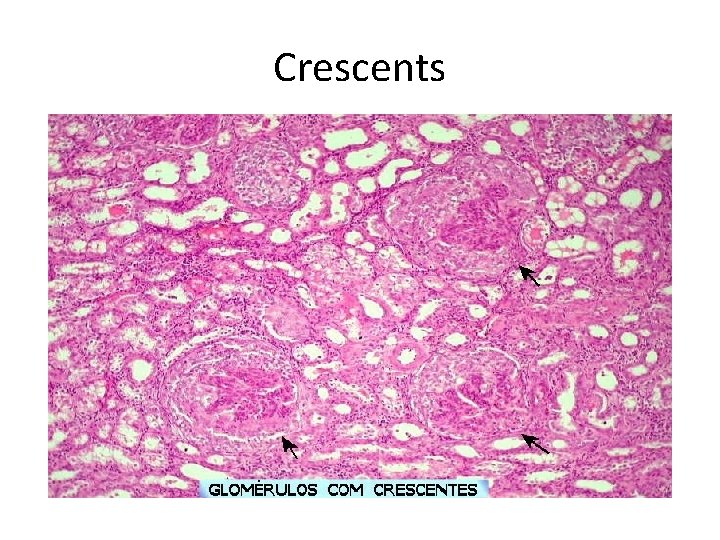
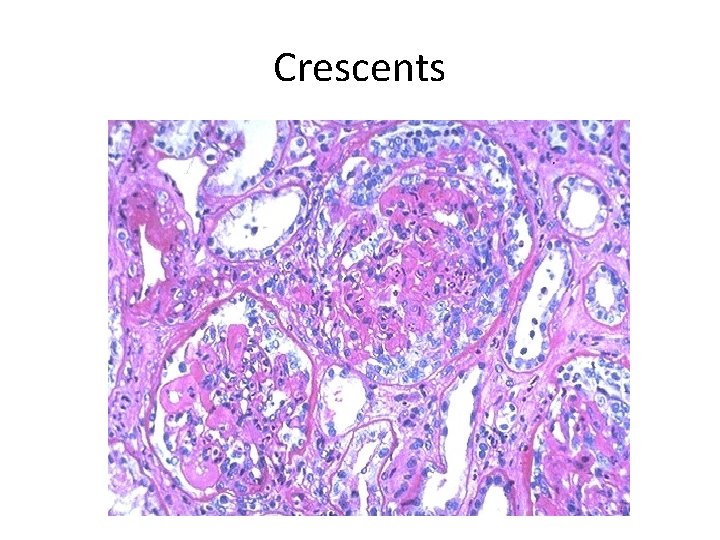
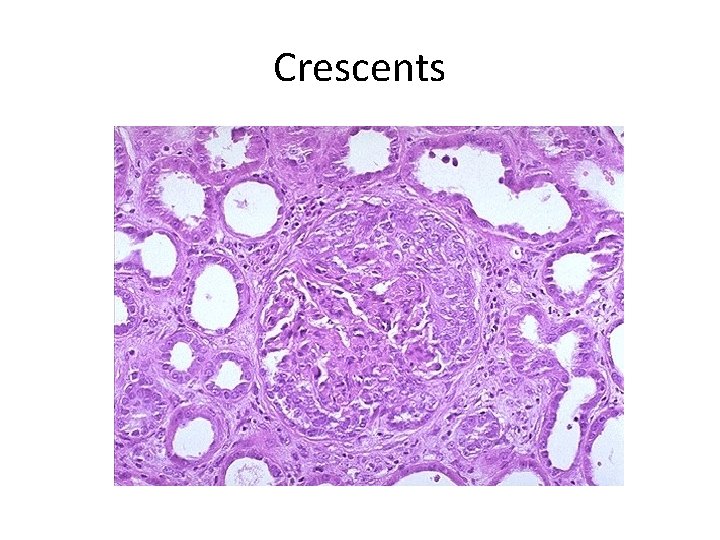
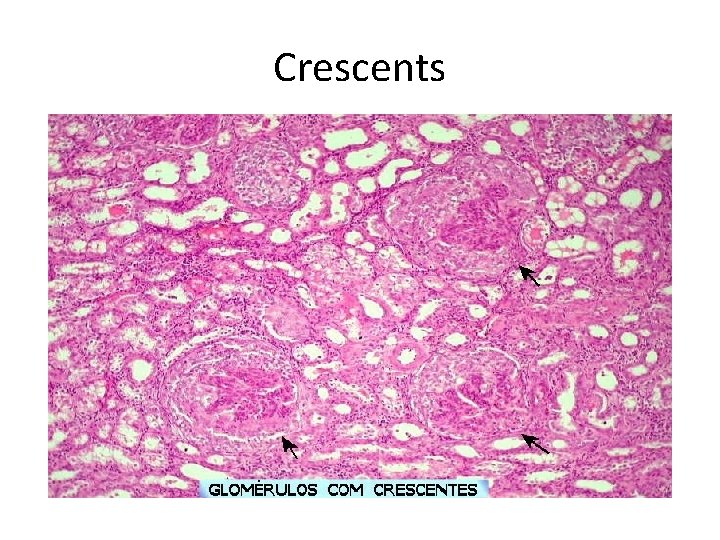
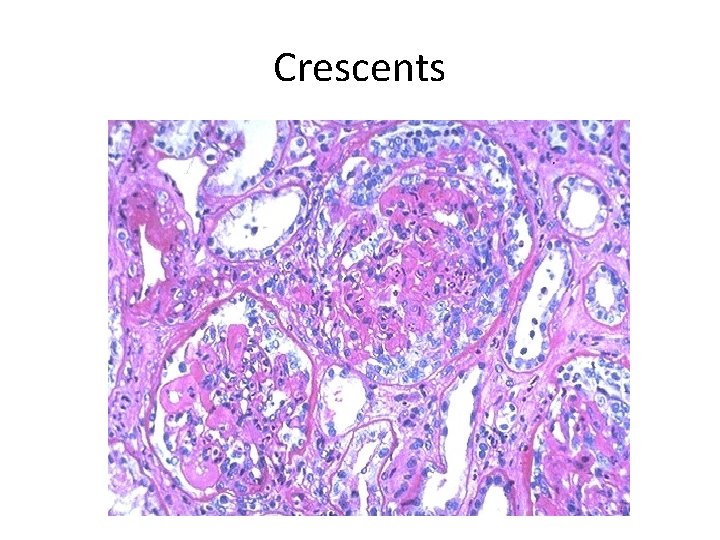
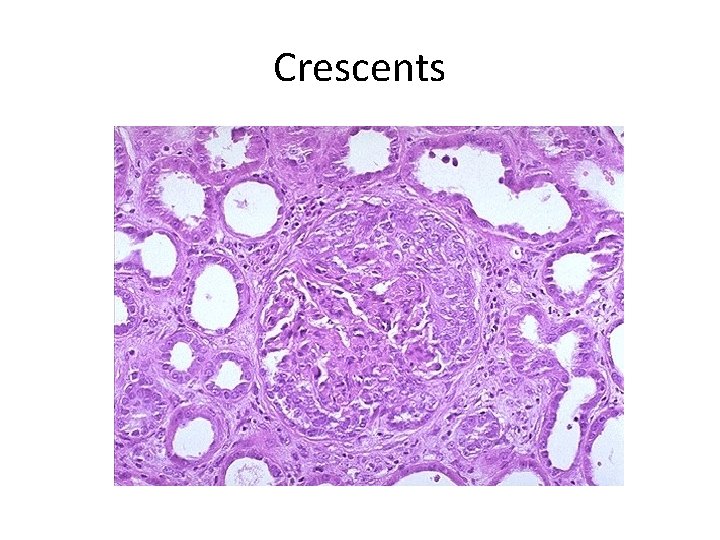
- If untreated, death from renal failure occurs within weeks to months. - The most common histologic picture is the presence of crescents in most of the glomeruli and these are produced a. predominantly by the proliferation of the parietal epithelial cells lining Bowman capsule and b. by the infiltration of monocytes and macrophages.
Crescents
Crescents
Crescents
Classification and Pathogenesis. - RPGN may be caused by a number of different diseases, some restricted to the kidney and others systems. - Although no single mechanism can explain all cases, but in most cases the glomerular injury is immunologically mediated.
classification - RPGN is classified into three groups on the basis of immunologic findings and In each group the disease may be a. Associated with a known disorder, b. or it may be idiopathic - The common denominator in all types of RPGN is severe glomerular injury.
1. Anti-GBM antibody-mediated disease: - Characterized by linear deposits of Ig. G and, in many cases, C 3 in the Glomerular basement membrane(GBM) - In some of these patients, the anti. GBM antibodies cross-react with pulmonary alveolar basement membranes to produce the clinical
- The antigen common to the alveoli and GBM is a peptide within the noncollagenous domain of the α 3 chain of collagen type IV - What triggers the formation of these antibodies is unclear in most patients. - Exposure to viruses or hydrocarbon solvents (found in paints and dyes) and drugs has been implicated in some patients
2. Diseases caused by immune complex deposition. - RPGN can be a complication of any of the immune complex nephritides, including : I. Idiopathic II. Secondary to a. Postinfectious glomerulonephritis, b. Lupus nephritis, c. Ig. A nephropathy,
- In this group, immunofluorescence studies reveal the granular pattern of staining characteristic of immune complex deposition. - These patients usually cannot be helped by plasmapheresis, and they require treatment for the underlying disease.
3. Pauci-immune RPGN, - Defined by the lack of detectable anti. GBM antibodies or immune complexes by immunofluorescence and electron microscopy and can be 1. Idiopathic - More than 90% of idiopathic cases have c-ANCAs or p-ANCAs in the sera
2. Most commonly the patients have circulating antineutrophil cytoplasmic antibodies (ANCAs) that produce cytoplasmic (c) or perinuclear (p) staining pattern and are known to play a role in some vasculitides - This type of RPGN may be a component of a systemic vasculitis such as granulomatosis with polyangiitis (formerly called Wegener granulomatosis) or microscopic
-. - The presence of circulating ANCAs in both idiopathic crescentic glomerulonephritis and cases that occur as a component of systemic vasculitis, and the similar pathologic features in either setting, have led to the idea that these disorders are pathogenetically related
- According to this concept, all cases of crescentic glomerulonephritis of the pauci-immune type are manifestations of small-vessel vasculitis or polyangiitis, which is limited to glomerular and perhaps peritubular capillaries in cases of idiopathic crescentic glomerulonephritis.
Morphology Light microscope - The histologic picture is dominated by distinctive crescents - Crescents are formed by proliferation of parietal cells and by migration of monocytes and macrophages into the urinary space. - Neutrophils and lymphocytes may be present.
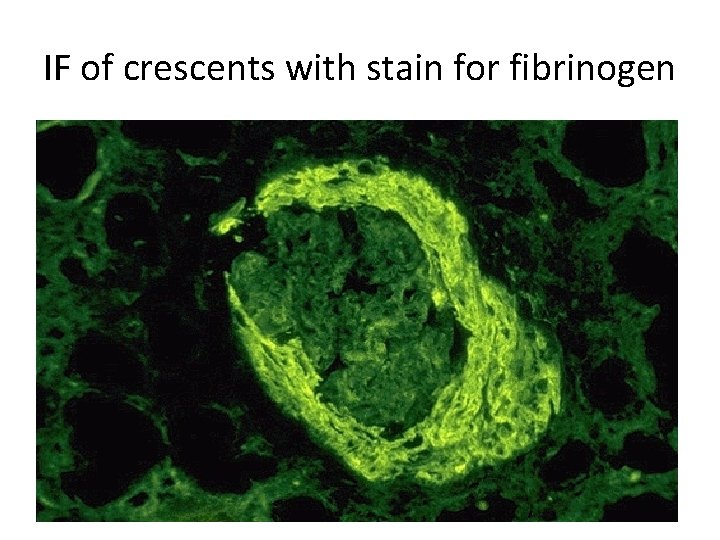
- Fibrin strands are frequently prominent between the cellular layers in the crescents; indeed, as the escape of procoagulant factors, fibrin and cytokines into Bowman space may contribute to crescent formation
- By immunofluorescence microscopy, 1. Goodpasture syndrome cases show linear GBM fluorescence for Ig. G and C 3 2. immune complex-mediated group show granular immune deposits; 3. Pauci-immune cases have little or no deposition of immune reactants
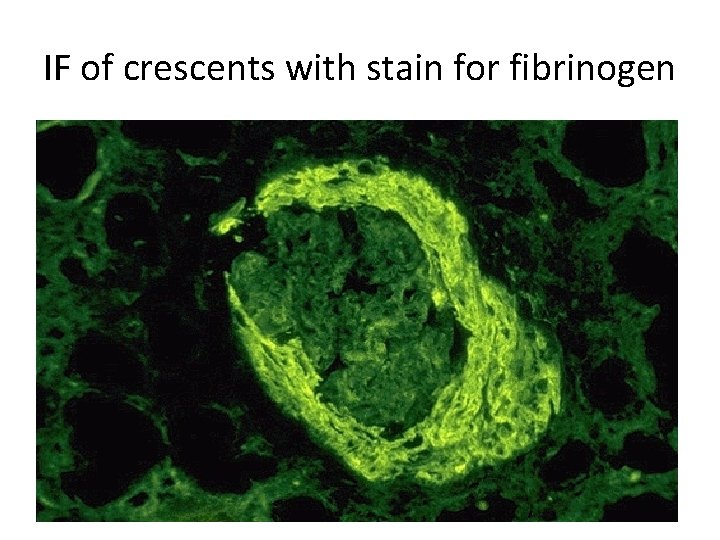
IF of crescents with stain for fibrinogen
Electron microscopy - Ruptures in the GBM in the three groups - Shows discloses deposits in those cases due to immune complex deposition (type II). Note: - In time, most crescents undergo organization and fibrosis
Clinical Course. - The renal manifestations of all forms of crescentic glomerulonephritis include: a. Hematuria with red blood cell casts in the urine, b. Moderate proteinuria occasionally reaching the nephrotic range, c. Variable hypertension
Clinical course - The renal involvement is usually progressive over a matter of weeks and culminates in severe oliguria. - Recovery of renal function may follow early intensive plasmapheresis combined with steroids and cytotoxic agents in Goodpasture syndrome. which can reverse both pulmonary hemorrhage and renal failure
- Other forms of RPGN also respond well to steroids and cytotoxic agents, However, despite therapy, many patients eventually require chronic dialysis or transplantation, particularly if the disease is discovered at a late stage. Note: Serum analyses for anti-GBM antibodies, antinuclear antibodies, and ANCAs are helpful in the diagnosis of
Nephrotic Syndrome - The manifestations of the syndrome include: 1. Massive proteinuria, with the daily loss of 3. 5 m or more of protein (less in children) 2. Hypoalbuminemia, with plasma albumin levels less than 3 m/d. L 3. Generalized edema 4. Hyperlipidemia and lipiduria
- Increased permeability resulting from either structural or physicochemical alterations in this barrier allows proteins to escape from the plasma into the urinary space, resulting in proteinuria. - Heavy proteinuria depletes serum albumin levels at a rate beyond the compensatory synthetic capacity of the liver, resulting in hypoalbuminemia. -
- Increased renal catabolism of filtered albumin also contributes to the hypoalbuminemia. - The edema is a consequence of decreased intravascular colloid osmotic pressure. - Edema is soft and pitting, and is most marked in the periorbital regions and dependent portions of the body. .
- The largest proportion of protein lost in the urine is albumin, but globulins are also excreted in some diseases. - The ratio of low- to high-molecularweight proteins in the urine in various cases of nephrotic syndrome is a manifestation of the selectivity of proteinuria
a. A highly selective proteinuria - Consists mostly of low-molecularweight proteins (albumin, and transferrin), b. A poorly selective proteinuria - Consists of higher molecular-weight globulins in addition to albumin.
The genesis of the hyperlipidemia is complex. - Most patients with nephrotic syndrome have a. Increased blood levels of cholesterol, triglyceride, very-low-density lipoprotein, Lp(a) lipoprotein, and apoprotein, and b. there is a decrease in high-density lipoprotein concentration in some patients.
• These defects are due to a combination of: a. increased synthesis of lipoproteins in the liver b. Abnormal transport of circulating lipid particles, c. and decreased lipid catabolism
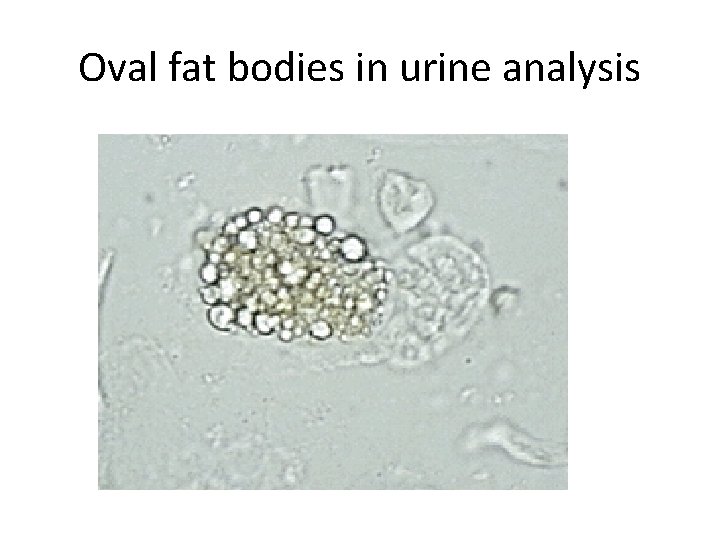
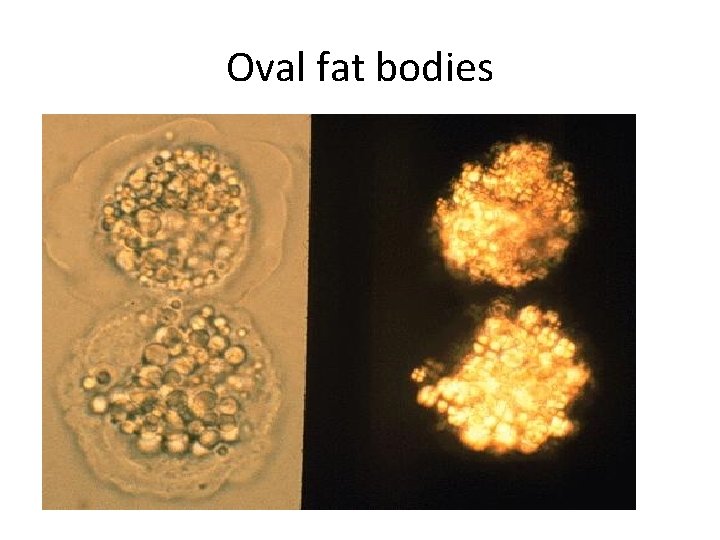
- Lipiduria follows the hyperlipidemia, because lipoproteins also leak across the glomerular capillary wall. - The lipid appears in the urine either as free fat or as oval fat bodies, representing lipoprotein resorbed by tubular epithelial cells and then shed along with injured tubular cells from the basement membrane.
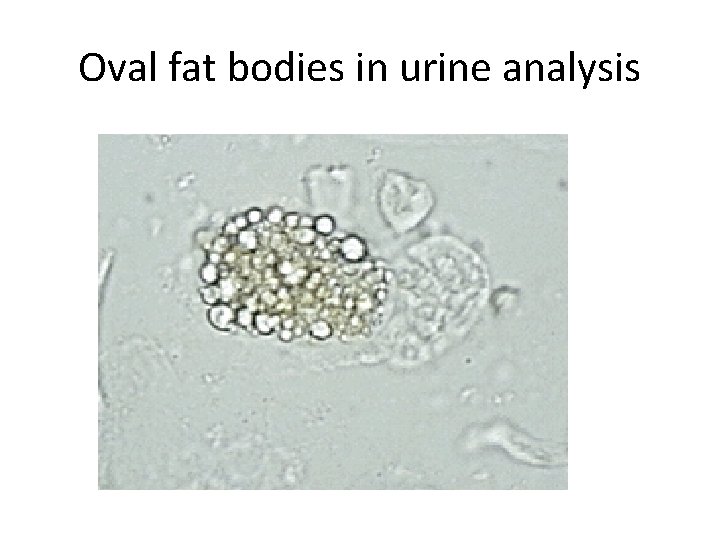
Oval fat bodies in urine analysis
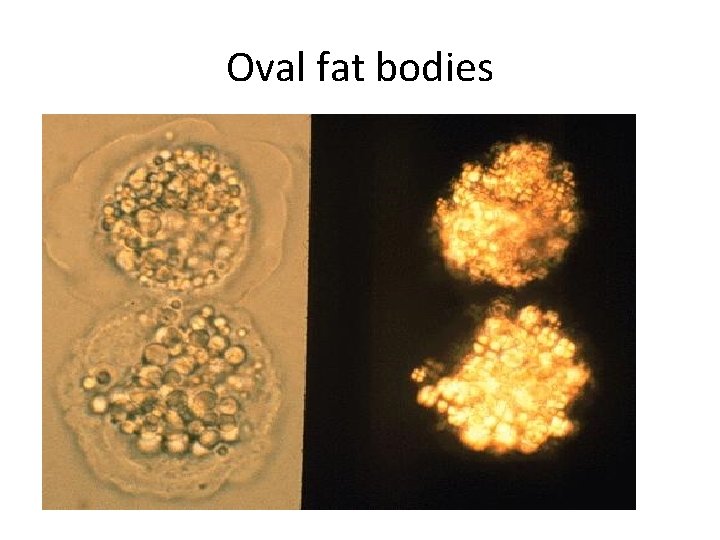
Oval fat bodies
Other manifestations I. Nephrotic patients are vulnerable to infection, especially staphylococcal and pneumococcal infections, probably due to loss of immunoglobulins in the urine. II. Thrombotic and thromboembolic complications due to loss of endogenous anticoagulants (e. g. , antithrombin III) in the urine.
III. Renal vein thrombosis, - is a consequence of this hypercoagulable state, particularly in patients with membranous nephropathy
Causes of Nephrotic syndrome - The incidences of the several causes of the nephrotic syndrome vary according to age and geography. 1. In children younger than 17 years in North America, nephrotic syndrome is almost always caused by a lesion primary to the kidney; 2. Among adults, in contrast, it is often associated with a systemic disease.
- The most frequent systemic causes of the nephrotic syndrome are a. Diabetes, b. Amyloidosis, c. SLE.
• The most important of the primary glomerular lesions are a. Minimal-change disease : is most common in children in North America b. Membranous glomerulopathy, is most common in older adults : c. Focal segmental glomerulosclerosis: occurs at all ages
• Other less common causes of nephrotic syndrome include: a. Membranoproliferative glomerulonephritides b. Ig. A nephropathy
1. Membranous Nephropathy - Membranous nephropathy is characterized by diffuse thickening of the glomerular capillary wall due to the accumulation of deposits containing Immunoglobulins (Ig) along the subepithelial side of the basement membrane.
1. Primary in 75% of cases 2. Secondary to systemic disease in 25% of case a. Drugs such as penicillamine, captopril, gold, nonsteroidal antiinflammatory drugs (NSAIDs b. Underlying malignant tumors - particularly carcinomas of the lung and colon, and melanoma
c. SLE d. Infections such as chronic hepatitis B, hepatitis C, syphilis, schistosomiasis, malaria
Pathogenesis. • Membranous nephropathy is a form of chronic immune complex-mediated disease. - The antigens may be a. endogenous which may be renal or non renal such as self nuclear antigens in SLE b. exogenous such as those derived from hepatitis B virus
Pathogenesis Primary (also called idiopathic) membranous nephropathy, - Is now considered to be an autoimmune disease linked to certain HLA alleles such as HLA-DQA 1 and caused in most cases by antibodies to a renal autoantigen. - In many adult cases the autoantigen is the phospholipase A 2 receptor.
- How does the glomerular capillary wall become leaky in membranous nephropathy? There is a paucity of neutrophils, monocytes, or platelets in glomeruli. - The presence of complement and corroborating experimental work suggest that the complement C 5 b-C 9 membrane attack complex has an important role.
- It is postulated that C 5 b-C 9 activates glomerular epithelial and mesangial cells, inducing them to liberate proteases and oxidants, which cause capillary wall injury and increased protein leakage.
- A subclass of Ig. G, Ig. G 4, which differs from other Ig. G subclasses in being a poor activator of the classical complement pathway, is the principal immunoglobulin deposited in cases of primary membranous nephropathy. - How Ig. G 4 may activate the complement system is not clear.
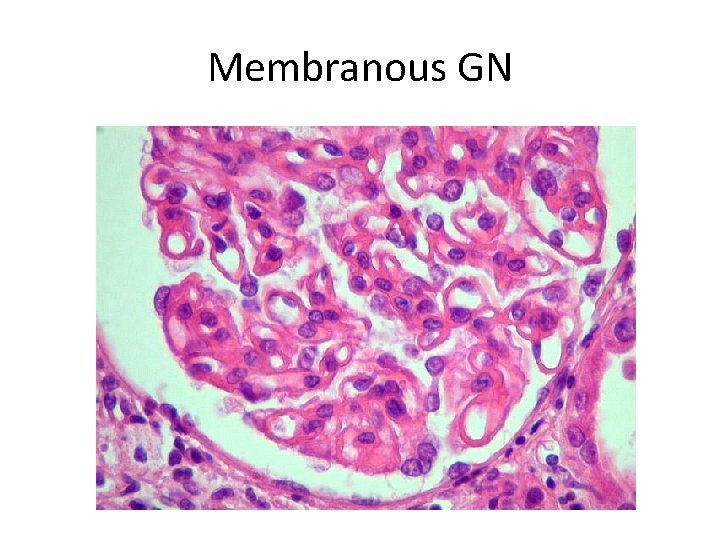
Morphology Light microscopy - The glomeruli either appear normal in the early stages of the disease or exhibit uniform, diffuse thickening of the glomerular capillary wall

Membranous GN
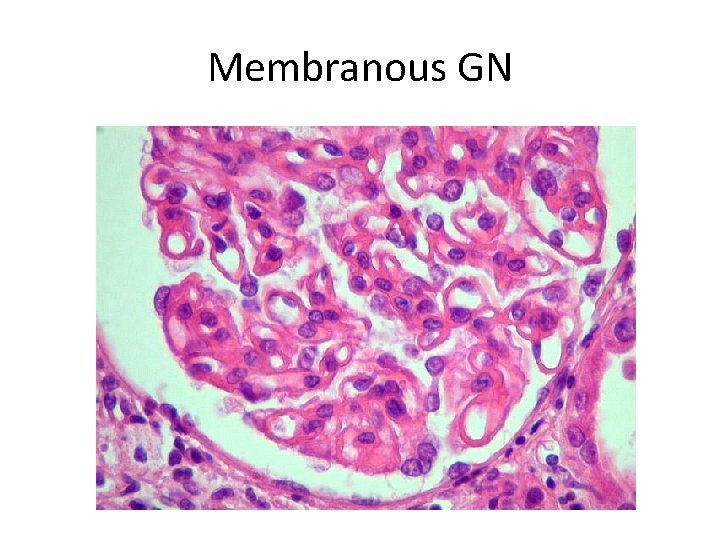
Membranous GN
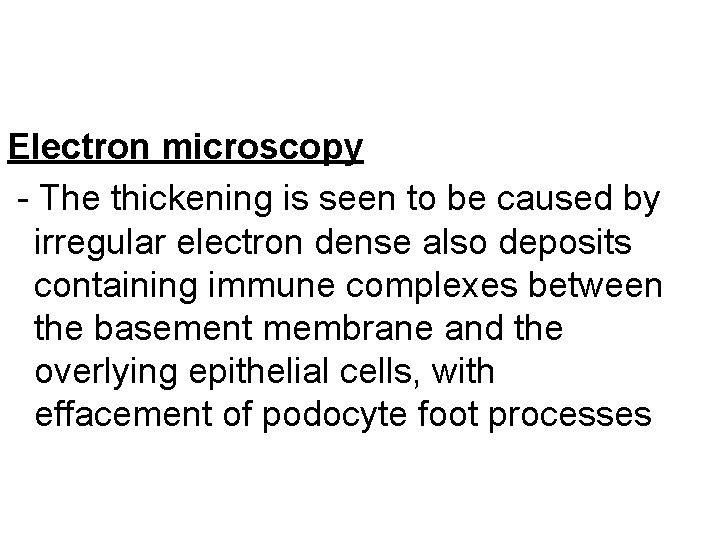
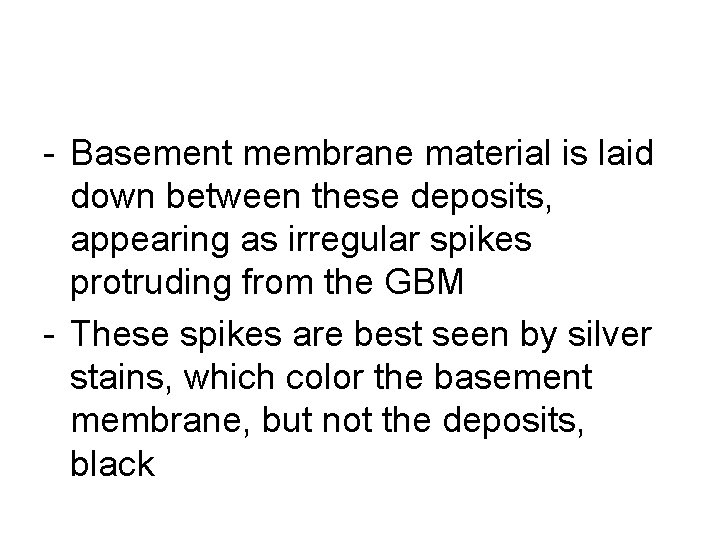
Electron microscopy - The thickening is seen to be caused by irregular electron dense also deposits containing immune complexes between the basement membrane and the overlying epithelial cells, with effacement of podocyte foot processes
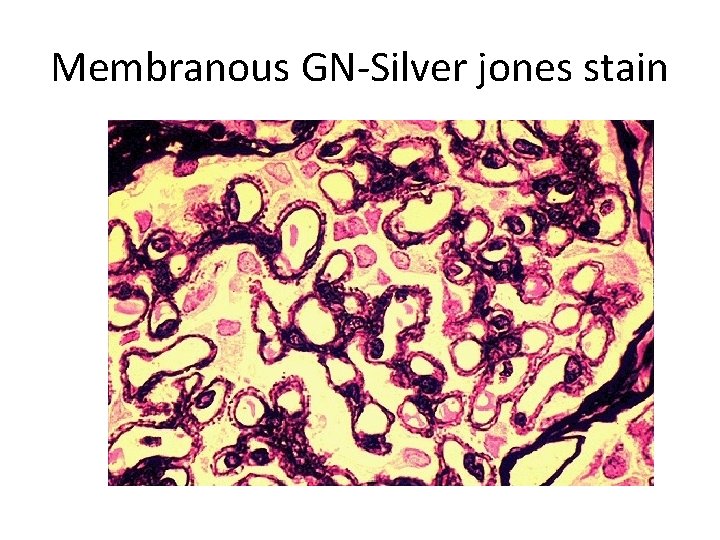
- Basement membrane material is laid down between these deposits, appearing as irregular spikes protruding from the GBM - These spikes are best seen by silver stains, which color the basement membrane, but not the deposits, black

Membranous GN-Silver jones stain
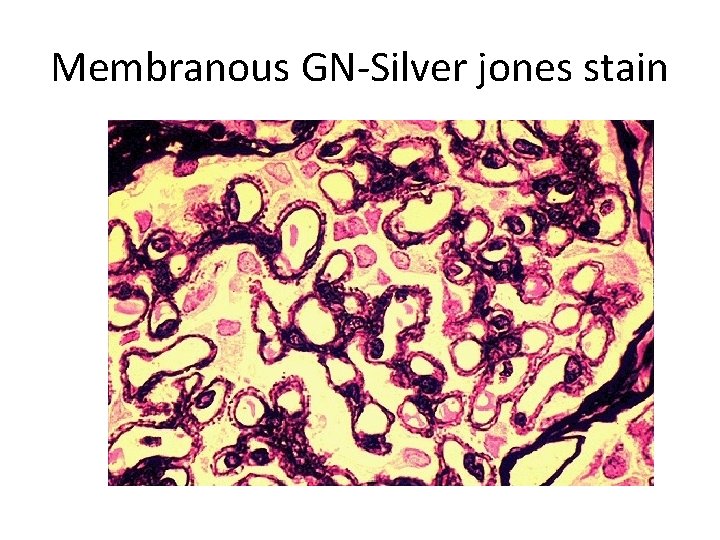
Membranous GN-Silver jones stain

- In time, these spikes thicken to produce domelike protrusions and eventually close over the immune deposits, burying them within a markedly thickened, irregular membrane.
Immunofluorescence microscopy - Demonstrates that the granular deposits contain both immunoglobulins and complement.
- The epithelial cells of the proximal tubules contain protein reabsorption droplets, and there may be considerable interstitial mononuclear cell inflammation.
 Extracapillary
Extracapillary What is passive
What is passive Past perfect and past progressive
Past perfect and past progressive Past perfect progressive objasnjenje
Past perfect progressive objasnjenje Active phagocytes that increase rapidly acute infection
Active phagocytes that increase rapidly acute infection While viewing a slide of rapidly moving sperm cells
While viewing a slide of rapidly moving sperm cells Plyometrics involves moving a weight as rapidly as possible
Plyometrics involves moving a weight as rapidly as possible Chapter 15 infection control
Chapter 15 infection control Pare cooking definition
Pare cooking definition Talk rapidly
Talk rapidly Which of the following gases will effuse the most rapidly
Which of the following gases will effuse the most rapidly To beat rapidly to incorporate air and increase volume.
To beat rapidly to incorporate air and increase volume. Which compounds solubility decreases most rapidly
Which compounds solubility decreases most rapidly When air rapidly expands its temperature normally
When air rapidly expands its temperature normally Corporations developed rapidly in the 1830s
Corporations developed rapidly in the 1830s Which rock weathers most rapidly when exposed to acid rain
Which rock weathers most rapidly when exposed to acid rain L
L What is zero circle in surveying
What is zero circle in surveying The root jur means law. what does the word perjury mean?
The root jur means law. what does the word perjury mean? Bar pilots association
Bar pilots association Spinal meninges and associated structures
Spinal meninges and associated structures Rfc 5116
Rfc 5116 Colors associated with time
Colors associated with time Out group homogeneity
Out group homogeneity Psychodynamic perspective
Psychodynamic perspective One weakness associated with the entity theory is that
One weakness associated with the entity theory is that Alyssa's extended family is staying at the lake house
Alyssa's extended family is staying at the lake house Sfrs in 8051
Sfrs in 8051 Immediacy definition in communication
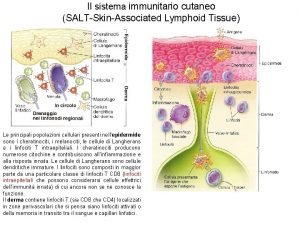
Immediacy definition in communication Salt skin associated lymphoid tissue
Salt skin associated lymphoid tissue Cyclical unemployment is closely associated with
Cyclical unemployment is closely associated with Flank defence in marketing
Flank defence in marketing Write the terms associated with ipde process
Write the terms associated with ipde process Laser alignment
Laser alignment It is a large hanging barrel drum
It is a large hanging barrel drum What is my three word location
What is my three word location Write the terms associated with ipde process
Write the terms associated with ipde process In neurons, efferent is to ______ as afferent is to ______.
In neurons, efferent is to ______ as afferent is to ______. What encompasses all activities associated with the flow
What encompasses all activities associated with the flow Kaysville city power
Kaysville city power Biosafety of recombinant adeno associated virus vectors
Biosafety of recombinant adeno associated virus vectors Chapter 17 oral pathology short answer questions
Chapter 17 oral pathology short answer questions Name something associated with china
Name something associated with china Four parts of ireland
Four parts of ireland Ivan pavlov is most closely associated with
Ivan pavlov is most closely associated with Professor yashpal committee
Professor yashpal committee Symbol for associated with
Symbol for associated with Knightley v johns
Knightley v johns Big data analytics is usually associated with
Big data analytics is usually associated with Encompasses all activities associated with the flow
Encompasses all activities associated with the flow Primary taste cortex
Primary taste cortex All the mental activities associated with thinking
All the mental activities associated with thinking Natural resources and associated problems
Natural resources and associated problems Loosely associated statements example
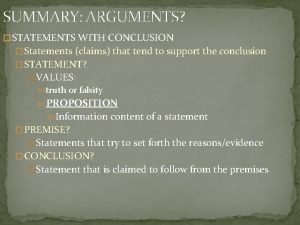
Loosely associated statements example Status withdrawal theory example
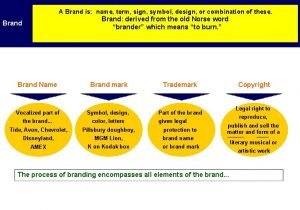
Status withdrawal theory example Name, term symbol, design and the like refer to
Name, term symbol, design and the like refer to Post office related words
Post office related words Sfr in 8051
Sfr in 8051 The mental activities associated with thinking
The mental activities associated with thinking