Radiological Category Gastrointestinal Principal Modality 1 MRI Principal
- Slides: 39
Radiological Category: Gastrointestinal Principal Modality (1): MRI Principal Modality (2): CT Case Report 679 Submitted by: Joshua Franklin, M. D. Faculty reviewer: Varaha Tammisetti M. D The University of Texas Medical School at Houston Date accepted: 1 March 2010
Case History A 67 year old hispanic male presented to his primary care physician complaining of dark urine for 6 weeks and 3 weeks of acholic stools with nausea and vomiting after fatty meals. The patient denies abdominal pain, fever, and loss of appetite. After a CT performed as an outpatient was found to be abnormal, the patient was told he may need surgery, prompting his presentation to the Memorial Hermann emergency department. The patient underwent CT during his initial admission to Memorial Hermann and an MRI was obtained approximated one month later. Select images from these examinations are presented.
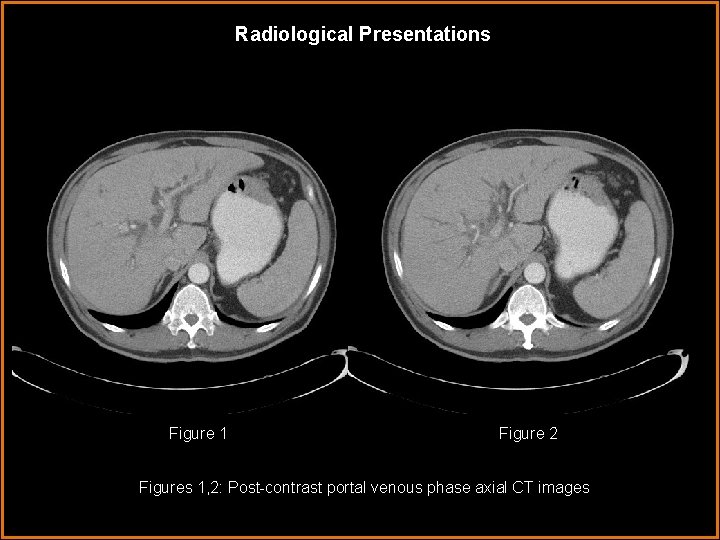
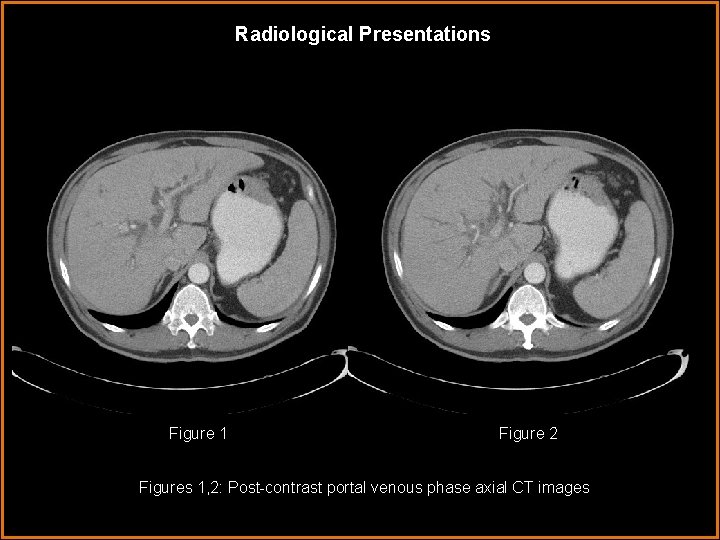
Radiological Presentations Figure 1 Figure 2 Figures 1, 2: Post-contrast portal venous phase axial CT images
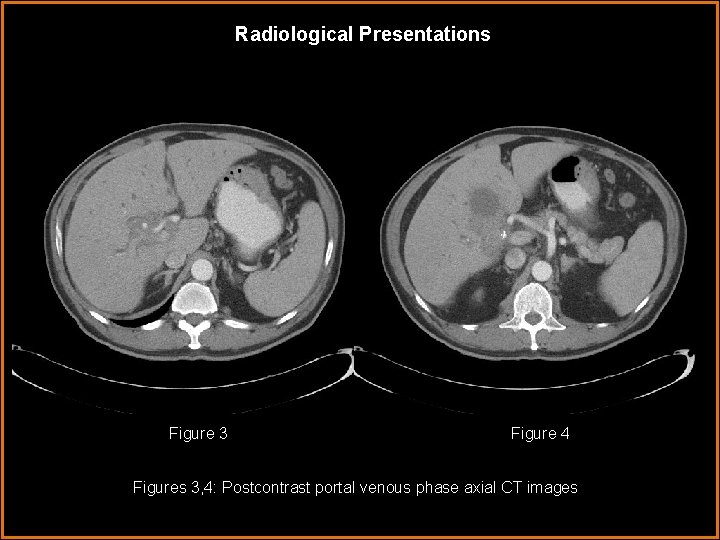
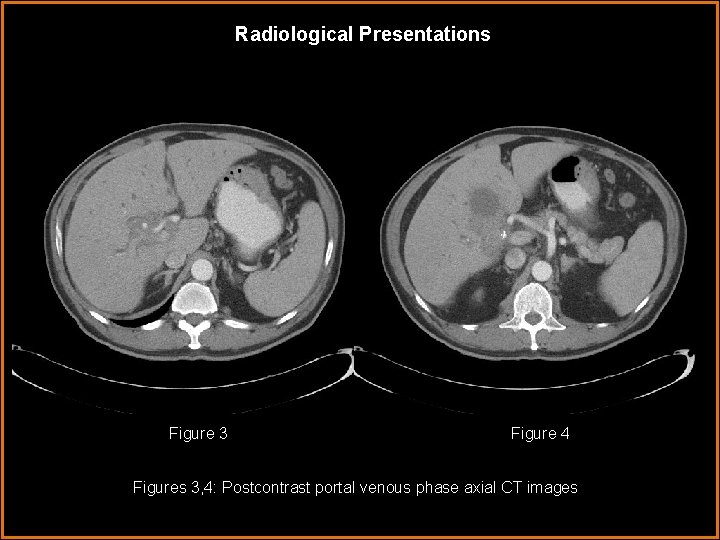
Radiological Presentations Figure 3 Figure 4 Figures 3, 4: Postcontrast portal venous phase axial CT images
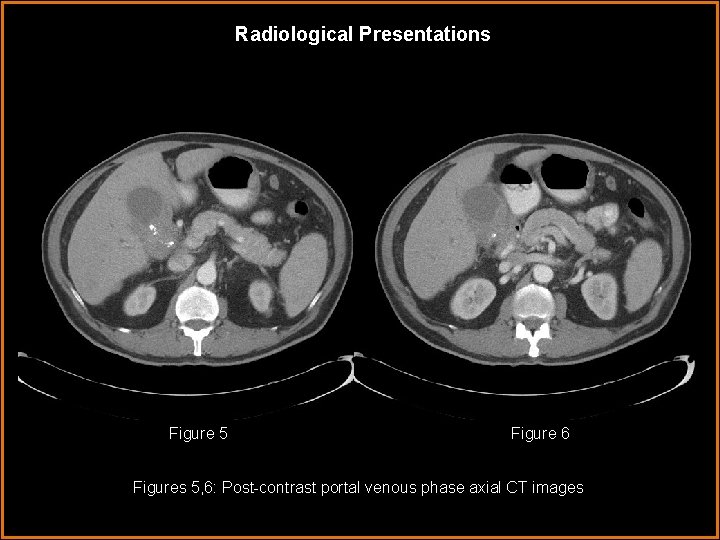
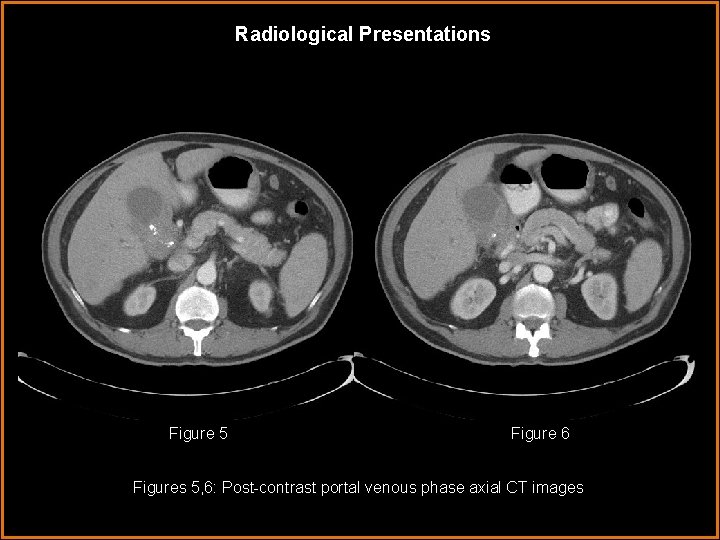
Radiological Presentations Figure 5 Figure 6 Figures 5, 6: Post-contrast portal venous phase axial CT images
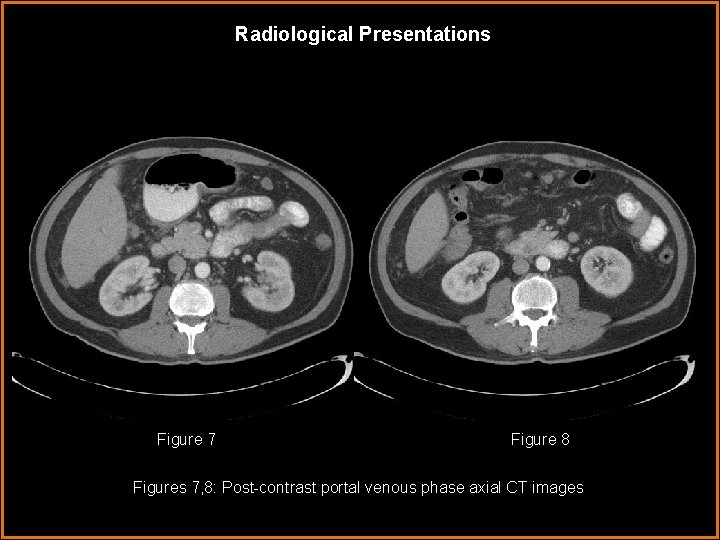
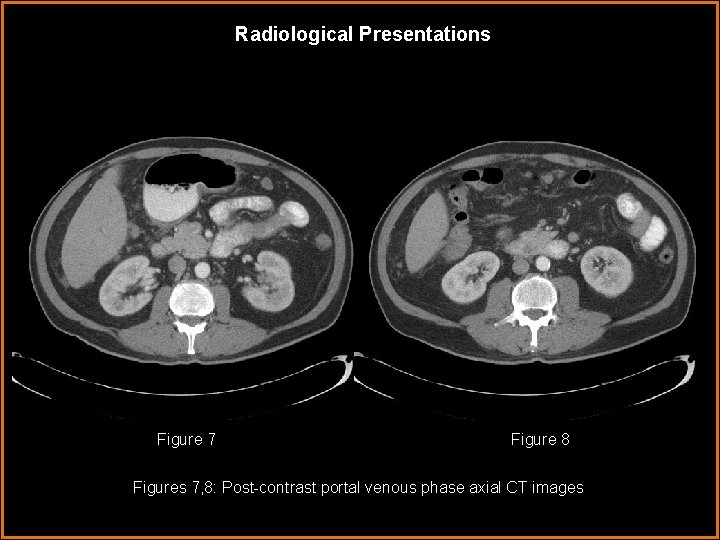
Radiological Presentations Figure 7 Figure 8 Figures 7, 8: Post-contrast portal venous phase axial CT images
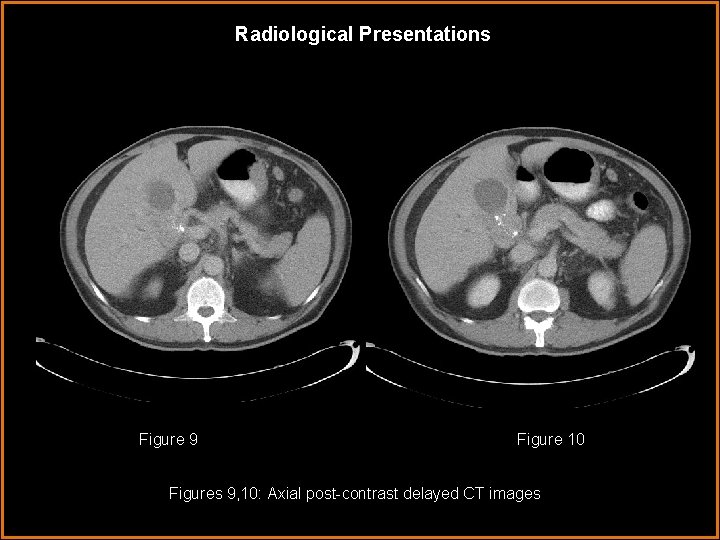
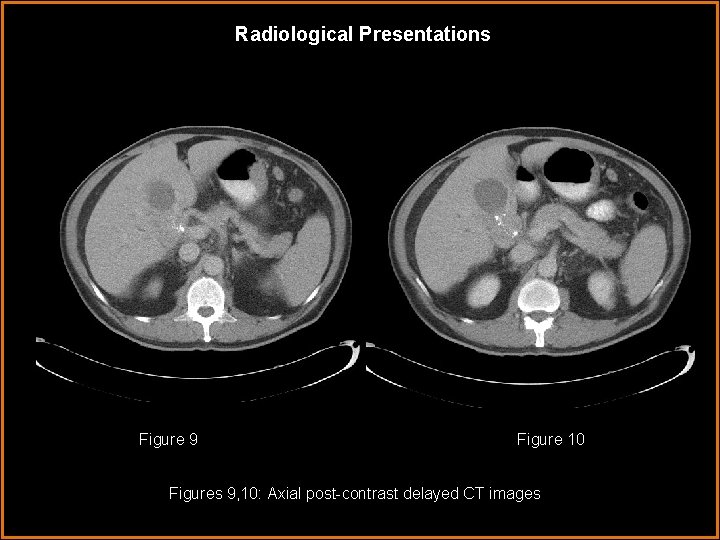
Radiological Presentations Figure 9 Figure 10 Figures 9, 10: Axial post-contrast delayed CT images
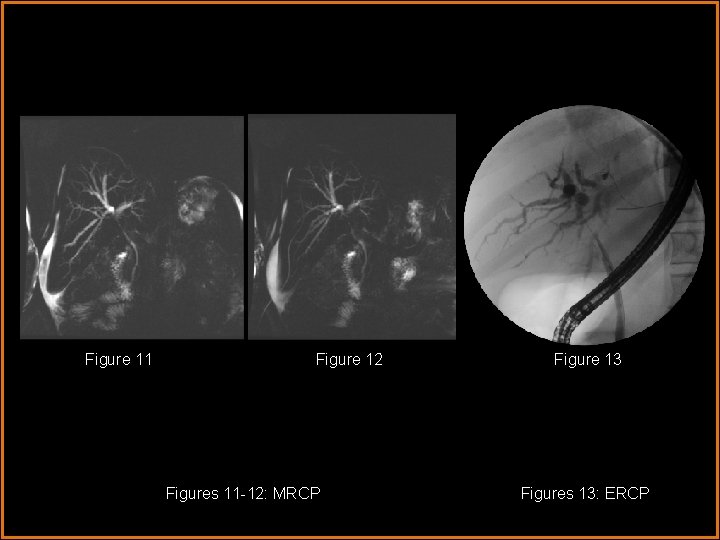
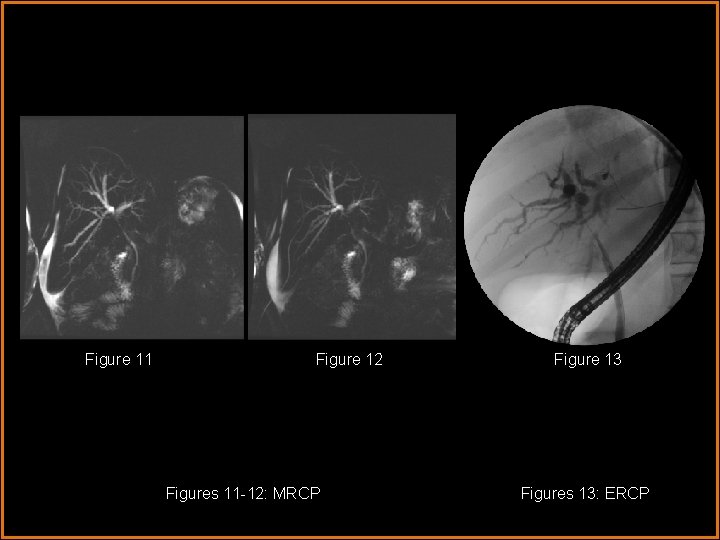
Figure 11 Figure 12 Figures 11 -12: MRCP Figure 13 Figures 13: ERCP
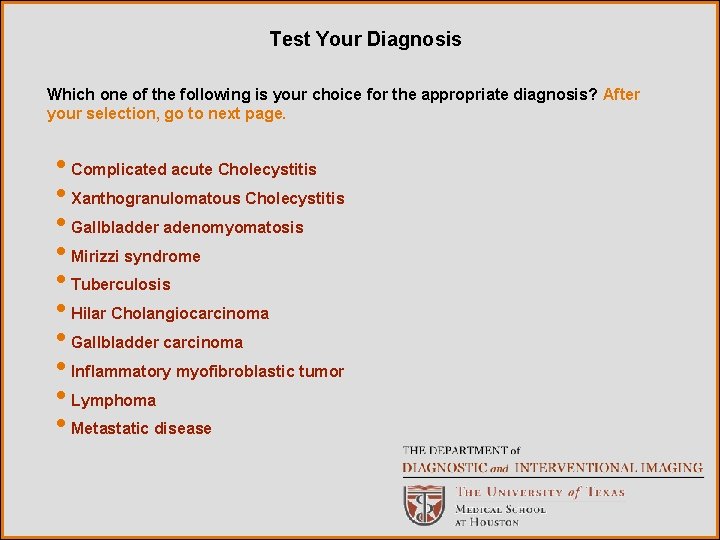
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Complicated acute Cholecystitis • Xanthogranulomatous Cholecystitis • Gallbladder adenomyomatosis • Mirizzi syndrome • Tuberculosis • Hilar Cholangiocarcinoma • Gallbladder carcinoma • Inflammatory myofibroblastic tumor • Lymphoma • Metastatic disease
Additional History Bile duct washings from ERCP: benign epithelial cells
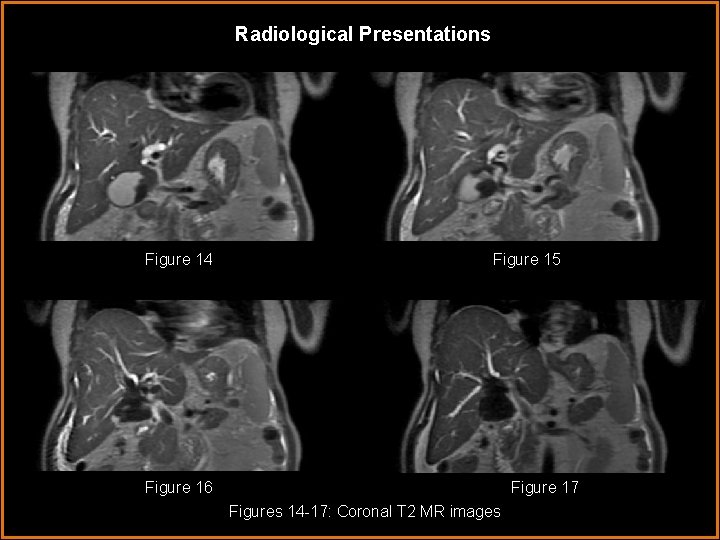
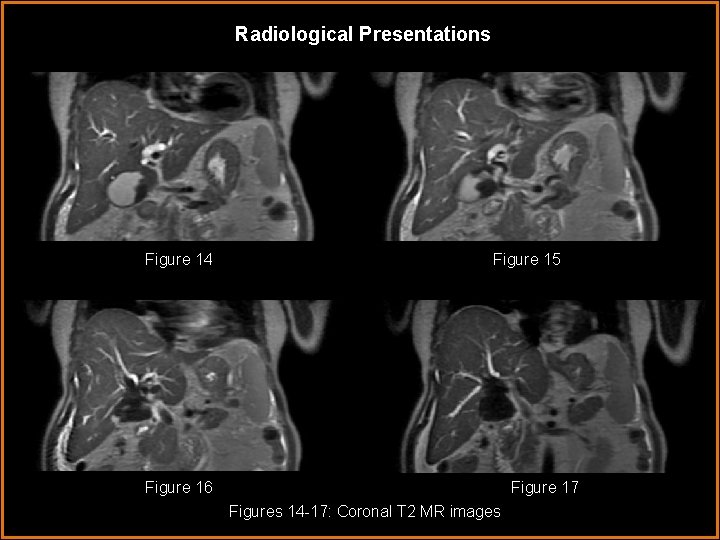
Radiological Presentations Figure 14 Figure 15 Figure 16 Figure 17 Figures 14 -17: Coronal T 2 MR images
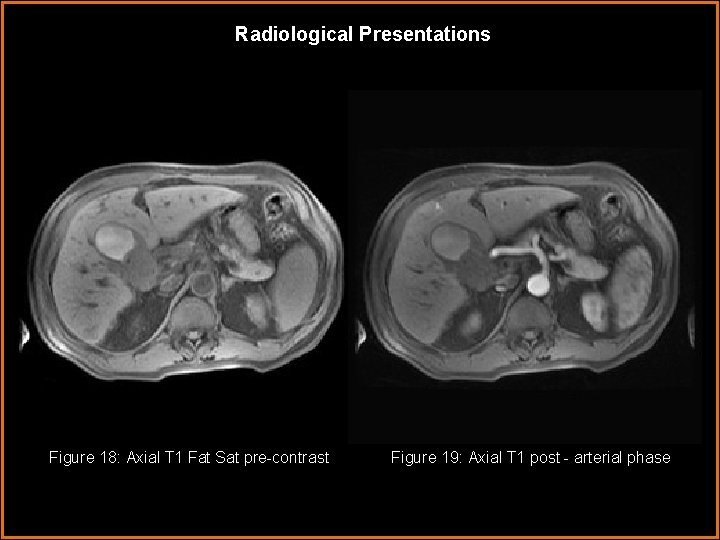
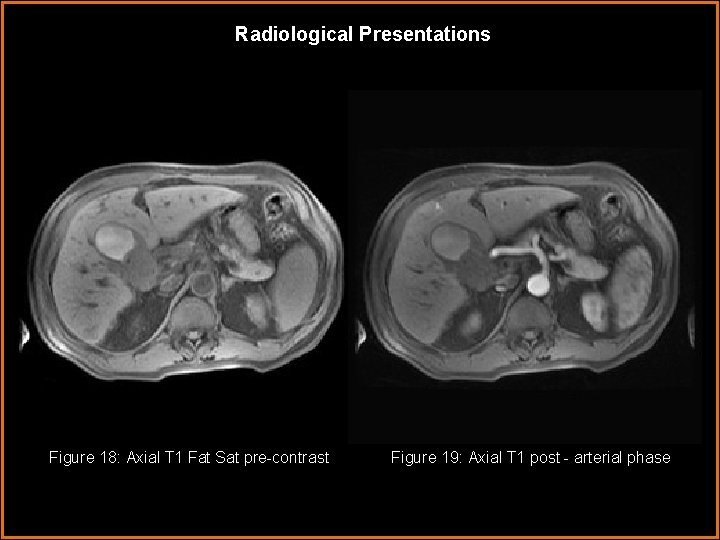
Radiological Presentations Figure 18: Axial T 1 Fat Sat pre-contrast Figure 19: Axial T 1 post - arterial phase
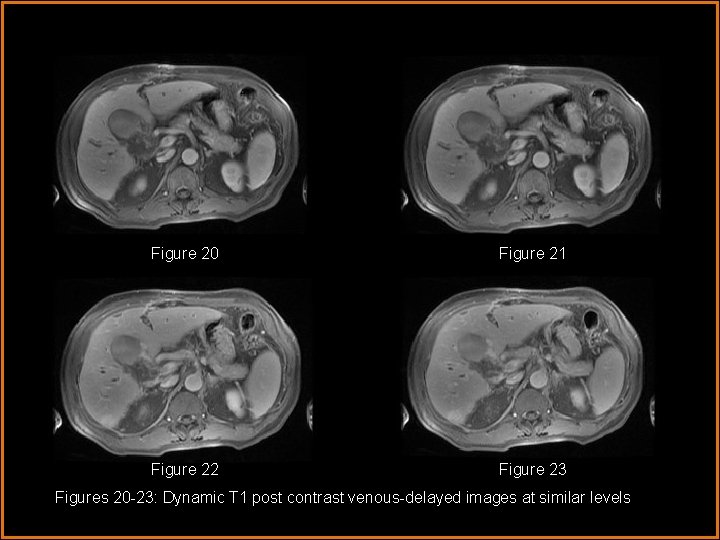
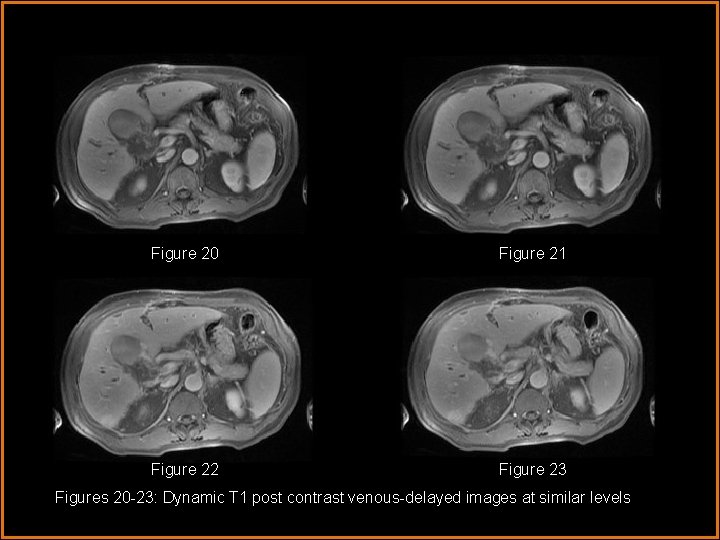
Figure 20 Figure 21 Figure 22 Figure 23 Figures 20 -23: Dynamic T 1 post contrast venous-delayed images at similar levels
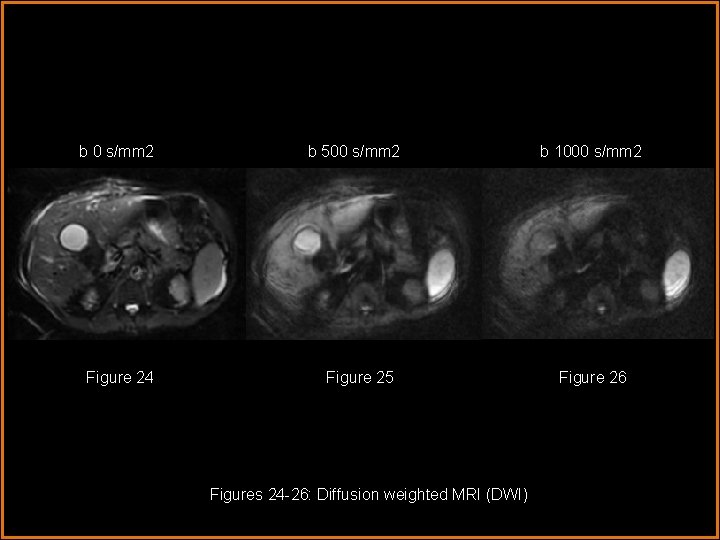
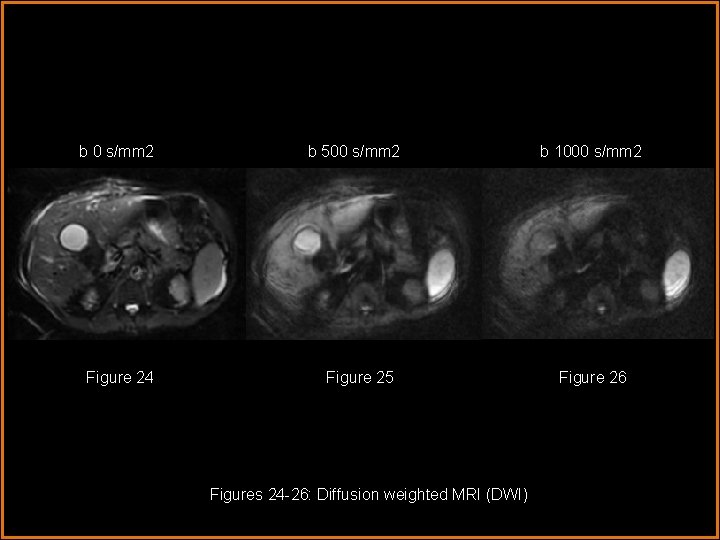
b 0 s/mm 2 Figure 24 b 500 s/mm 2 Figure 25 Figures 24 -26: Diffusion weighted MRI (DWI) b 1000 s/mm 2 Figure 26
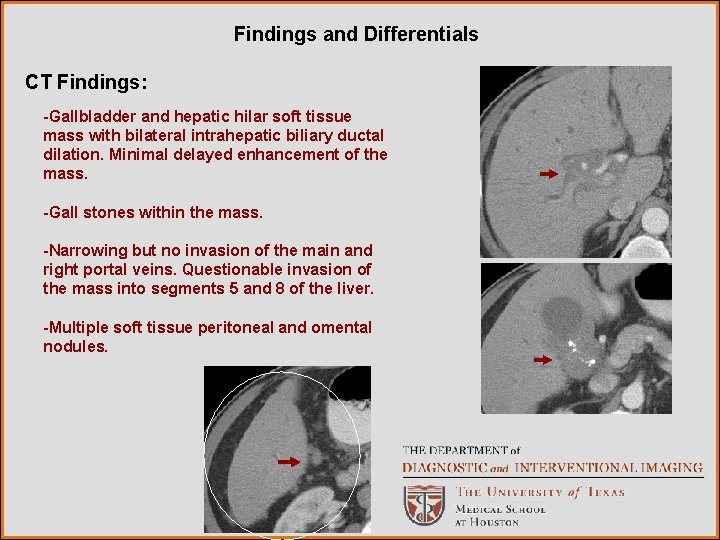
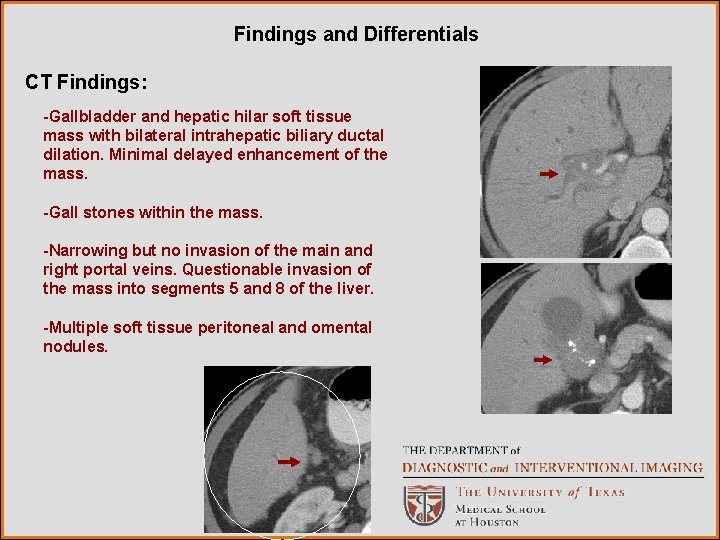
Findings and Differentials CT Findings: -Gallbladder and hepatic hilar soft tissue mass with bilateral intrahepatic biliary ductal dilation. Minimal delayed enhancement of the mass. -Gall stones within the mass. -Narrowing but no invasion of the main and right portal veins. Questionable invasion of the mass into segments 5 and 8 of the liver. -Multiple soft tissue peritoneal and omental nodules.
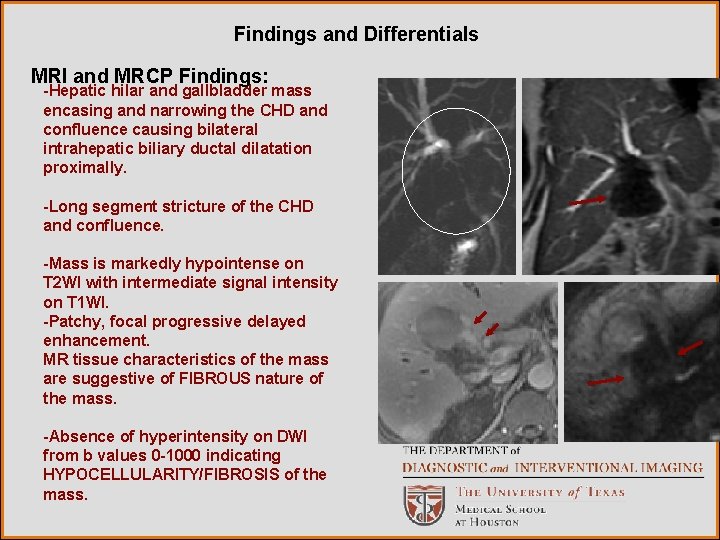
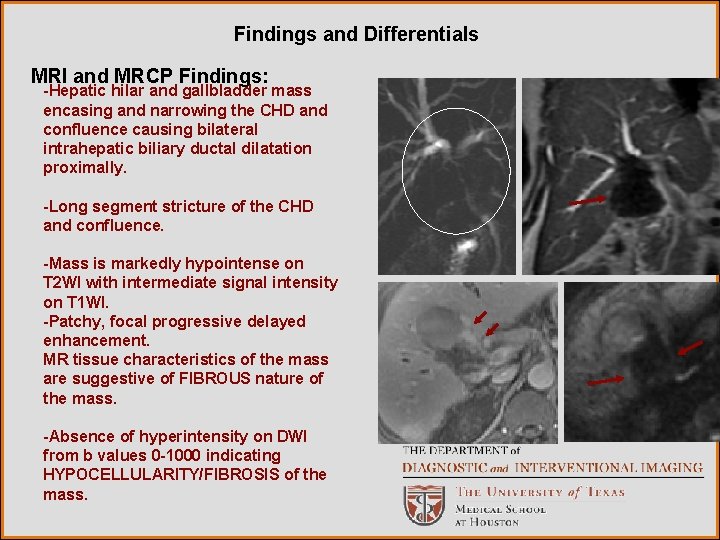
Findings and Differentials MRI and MRCP Findings: -Hepatic hilar and gallbladder mass encasing and narrowing the CHD and confluence causing bilateral intrahepatic biliary ductal dilatation proximally. -Long segment stricture of the CHD and confluence. -Mass is markedly hypointense on T 2 WI with intermediate signal intensity on T 1 WI. -Patchy, focal progressive delayed enhancement. MR tissue characteristics of the mass are suggestive of FIBROUS nature of the mass. -Absence of hyperintensity on DWI from b values 0 -1000 indicating HYPOCELLULARITY/FIBROSIS of the mass.
Findings and Differentials: • Hilar Cholangiocarcinoma • Gallbladder carcinoma • Xanthogranulomatous Cholecystitis • Lymphoma • Inflammatory myofibroblastic tumor
Discussion Masses involving the hepatic hilum and gallbladder fossa are uncommon but not rare. The major and relatively common differential diagnoses in this case are cholangiocarcinoma and gallbladder carcinoma. Rarely, certain benign processes with similar presentations, such as chronic xanthogranulomatous cholecystitis and inflammatory pseudotumor may also be included in the differential. Specifically, these benign processes may be considered in the setting of biliary washings negative for malignancy and atypical MR findings demonstrating an entirely fibrous mass and no restricted diffusion. It must noted, however, that negative biliary washings do not exclude malignancy.
Discussion Differential: Hilar Cholangiocarcinoma (Klatskin tumor): Cholangiocarcinoma comprises up to 15% of primary hepatic tumors making it the 2 nd most common neoplasm of the liver. Pathologically, the tumors are usually adenocarcinomas with abundant fibrous stroma. 1, 2, 3 Mass forming cholangiocarcinomas are most commonly hypodense on CT, moderately hypointense on T 1 weighted MR images and variably hyperintense on T 2 weighted MR images. They characteristically demonstrate early peripheral rim enhancement as well as delayed and persistent enhancement. These imaging findings and enhancement characteristics are thought to be related to the fibrous nature of these tumors. 1, 2, 3 The fibrosis in these tumors is generally located centrally, with T 2 hyperintense viable tumor at the periphery. The marked T 2 hypointensity in this patient is atypical for cholangiocarcinoma.
Discussion Gallbladder carcinoma: Gallbladder carcinoma is the 6 th most common gastrointestinal malignancy in the United States. The primary histology of gallbladder cancer is adenocarcinoma, making up approximately 90% of cases. On CT, gallbladder carcinoma presents as an heterogenous, iso- to hypoattenuating mass with areas of necrosis and calcification. Calcifications may be related to gallstones, calcifications of the gallbladder wall as seen in porcelain gallbladder, or calcified mucinous content. 4 On MRI, gallbladder carcinoma typically demonstrates heterogeneous T 2 hyperintensity and iso- to hypointense signal on T 1 weighted images. Viable tumor typically displays irregular early enhancement. 4, 5 Extension of gallbladder carcinoma beyond the gallbladder occurs very frequently, being seen in the majority of cases on presentation. The most common form of spread is direct extension. Up to 65% of cases present with extension into the liver. Lymphatic, hematogenous, intraperitoneal, and intraductal spread also occur. Biliary ductal involvement is also very common being seen in up to 38% of cases. 4
Discussion Other rare malignancies that may involve the biliary system include nonhodgkins lymphoma, metastatic disease (most commonly colon cancer), primary and metastatic biliary melanoma, and even carcinoid. The radiological appearances of these tumors overlap substantially with cholangiocarcinoma and gallbladder carcinoma preventing accurate diagnosis before histopathological evaluation. 3, 4
Discussion Xanthogranulomatous cholecystits (XGC): XGC is an uncommon form of chronic cholecystitis that may simulate gallbladder carcinoma radiologically. Pathologically, XGC is characterized by intramural nodules, severe proloferative fibrosis, and foamy histiocytes. The pathological basis for this entity is not completely understood; however, the initiating factor is believed to be bile extravasation into the gallbladder wall. This extravastion may occur either when Rokitansky-Aschoff sinuses dilate and rupture or when there is mucosal ulceration in the setting of chronic gallbladder obstruction and inflammation, which is usually related to cholelithiasis. Acute and chronic inflammatory cells accumulate along bile pigment containing foamy histiocytes resulting in poorly defined xanthogranulomata that appear as yellow-gray nodules within the gallbladder wall on gross inspection. 6 -8 On CT, XGC may present with focal or diffuse gallbladder wall thickening, heterogeneous gallbladder wall enhancement, and/or hypoattenuating nodules or bands in the gallbladder wall corresponding with xanthogranulomas or intramural abscesses. . Infiltration may be seen into the pericholecystic fat and there may be involvement of adjacent organs such as the liver. Intrahepatic ductal dilatation may also be seen, but is uncommon. 6 -10
Discussion Unfortunately most of the CT findings of XGC may also be seen with gallbladder carcinoma making differentiating the two entities difficult if not impossible. Chun et. al 6 found that hypoattenuating nodules in >60% of the thickened gallbladder wall and a continuously enhancing mucosal line were statistically significantly more common in XGC compared to gallbladder carcinoma. Despite the significant difference, these findings were still seen in 35 -40% of gallbladder carcinoma cases in the study confirming that obtaining a tissue diagnosis is still necessary. On MRI, the low attenuation nodules of XGC seen on CT appear as areas of T 1 hypointensity and variable intensity on T 2 weighted images. Those foci which demonstrate very high T 2 signal and do not enhance correspond with intramural abscesses whereas those foci with slightly high T 2 signal and strong delayed enhancement correspond with xanthogranulomas on pathology. 9
Discussion Inflammatory myofibroblastic tumor (IMT), also known as inflammatory pseudotumor, is a benign, pseudosarcomatous lesion, which is often mistaken for malignancy. IMTs are composed of benign myofibroblastic cells with a prominent inflammatory cell infiltrate and has the potential for persistent local growth and recurrence. The pathogenesis is not completely understood with current theories suggesting an exaggerated response to tissue injury as well as infectious and immunologic processes. 11, 12 Although most commonly found in the lungs and upper respiratory tracts of children and young adults, IMTs have also been described less commonly in other locations including the liver parenchyma and biliary tree. The 2 described patterns of hepatobiliary IMT are hepatic masses and periportal soft tissue masses. The clinical presentation of IMT is very nonspecific and highly depends upon the site involved. Patients with hepatobiliary IMT can present with biliary obstruction and jaundice; however, If there is no biliary obstruction, patients may present only with nonspecific constitutional symptoms. 12 Someren classified IMTs according to predominating cell type: (a) xanthogranuloma type IMT, (b) plasma cell granuloma type IMT, and (c) hyalinized sclerosing type IMT. Furthermore, there is evidence that IMT lesions evolve toward the sclerosing type (with a decrease in cellular content and an increase in fibrosis).
Discussion The imaging findings of inflammatory myofibroblastic tumors are nonspecific. As in cholangiocarcinoma, IMT may present as a mass or periportal soft tissue infiltration. 11 In one series of 7 patients, biliary IMTs presented as subtle infiltrating hilar soft tissue masses with one patient having a hilar mass inseparable from a gallbladder fossa mass. 13 The appearance of IMTs on MRI is variable, with lesions being iso- to hypointense relative to liver on T 1 w images and iso- to hyperintense on T 2 w images. 11, 12, 14 The variable appearance on MR is most likely related to the variable amounts of fibrosis and cellularity within different lesions. 12 Most commonly, IMTs demonstrate a delayed and persistent enhancement pattern without significant early arterial enhancement due to a high degree of fibrosis. 11, 12, 14 While IMT may be considered in the differential of a hepatobiliary mass, authors are seemingly in agreement that there are no findings specific to the diagnosis to allow it to be distinguished from cholangiocarcinoma or lymphoma. However, awareness of this entity could potentially alter surgical approach if the mass is repeatedly negative for malignancy. There have been very few case reports of this rare entity.
Discussion Radiological approach to the differential: In the case presented here, there is an illdefined hilar mass with delayed enhancement in the porta hepatis, which also involves the body and neck of the gallbladder. On MRI, the mass is markedly T 2 hypointense and has intermediate T 1 intensity. Thre is associated intrahepatic ductal dilatation, and there are scattered peritoneal nodules. The primary radiological differential considerations are cholangiocarcinoma and gallbladder carcinoma. Although the mass is more hypointense on T 2 WI than expected, it is in the right location for Klatskin tumor and demonstrates the typical delayed enhancement pattern. The presence of peritoneal nodules is also concerning for malignancy with intraperitoneal metastasis. Gallbladder carcinoma can also present similarly, but the lesion’s markedly T 2 hypointense MRI signal and lack of arterial enhancement are atypical. Also, with a mass this size, one would expect contiguous extension/invasion into the liver if the diagnosis were gallbladder carcinoma.
Discussion While not excluded, this is not a typical presentation for uncomplicated Xanthogranulomatous cholecystitis. XGC has a varied presentation and appearance but there are no specific findings such as intramural hypoattenuating nodules to suggest the diagnosis. However, XGC has known association with gallbladder carcinoma and therefore XGC complicated by gallbladder carcinoma can also be considered. Other rare entities such as biliary lymphoma and metastatic disease are also in the differenital, however, as previously discussed, there are no specific radiologic findings of these processes to allow diagnosis without biopsy. Inflammatory myofibroblastic tumor is another rare differential consideration. Again, the mass is more hypointense on T 2 WI than expected, however this could indicate increased fibrotic content and evolution to the sclerotic type. The delayed enhancement is an expected finding in IMT. As described previously, however, there are no described findings to differentiate IMT and cholangiocarcinoma radiologically.
Discussion Overall for a hilar mass with such an appearance, even if there are radiological findings that suggest benignity, rarely if ever are they convincing enough to avoid surgical intervention. The role of imaging in this setting is for therapeutic planning and to assess resectability. Awareness of benign entities might limit the surgical approach if the mass is repeatedly negative for malignancy. Future directions of imaging for the evaluation of inflammatory fibroblastic tumors might include the potenital role of diffusion weighted MR imaging and also the significance of marked T 2 hypointensity (which can vary with stage of fibrosis). While cholangiocarcinoma would be expected to restrict diffusion, no restricted diffusion was seen in our case.
Discussion • Surgery performed: Open cholecystectomy attempted, but only partial resection of the gallbladder and mass could be performed. • Operative findings (excerpt): “-The entire hilum was covered with adhesions from the omentum and the duodenum that had stuck against the gallbladder. -The gallbladder was a matted mass of big nodules that simulated a carcinomatosis and there was extensive involvement of the gallbladder. -Cholecystectomy was extremely difficult because of the desmoplastic inflammatory reaction. -There were protruding, hard nodular masses in the gallbladder, which was sent for biopsy once more, and they were negative for carcinoma. ”
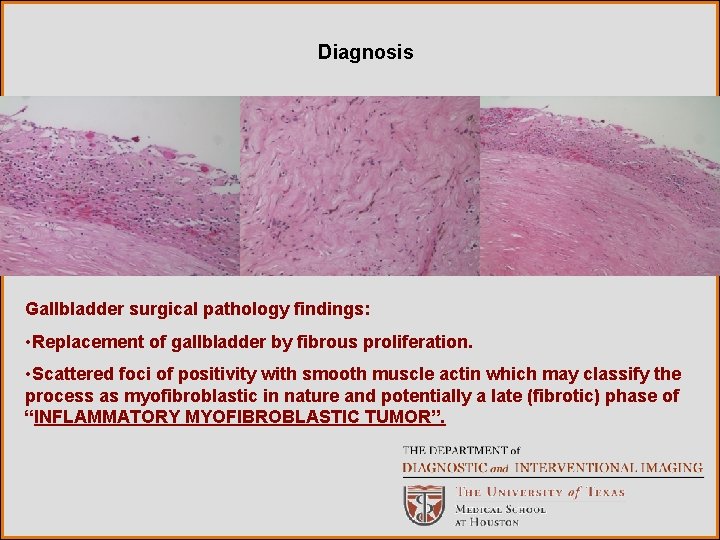
Diagnosis Relevant Pathologic Findings: 1. Bile duct washings from ERCP: benign epithelial cells 2. CT guided FNA samples of the mass: dense fibrosis, dystrophic calcs, and rare atypical cells 3. Peritoneal nodules : Benign fibrogranulomatous peritonitis. Bile within histiocytic giant cells suggests xanthogranulomatous cholecystitis with rupture and secondary bile peritonitis with similar fibrogranulomatous reaction to bile. 4. Gallbladder from open cholecystectomy: Replacement of gallbladder by fibrous proliferation. Scattered foci of positivity with smooth muscle actin which may classify the process as myofibroblastic in nature and potentially a late (fibrotic) phase of inflammatory myofibroblastic tumor.
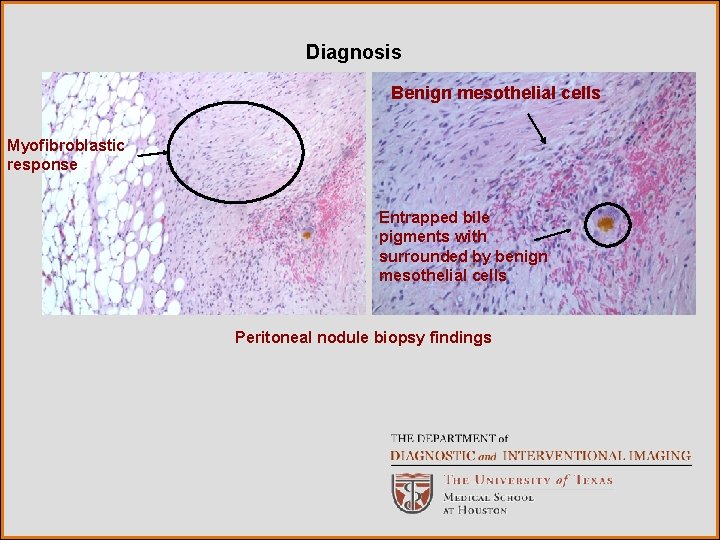
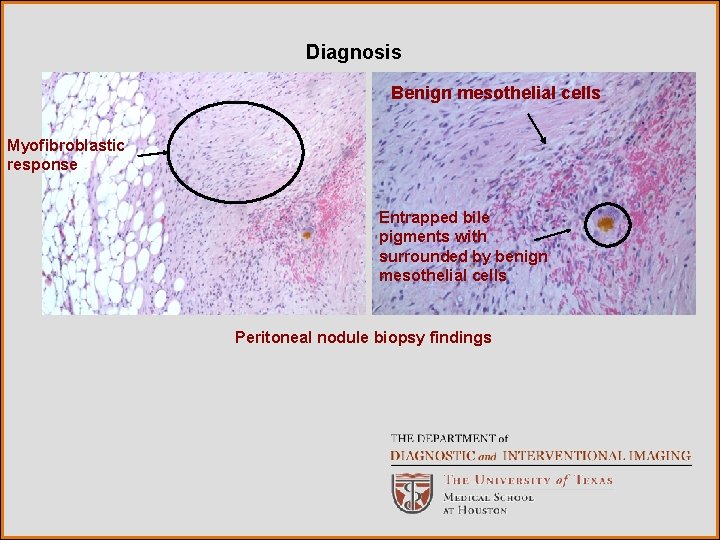
Diagnosis Benign mesothelial cells Myofibroblastic response Entrapped bile pigments with surrounded by benign mesothelial cells Peritoneal nodule biopsy findings
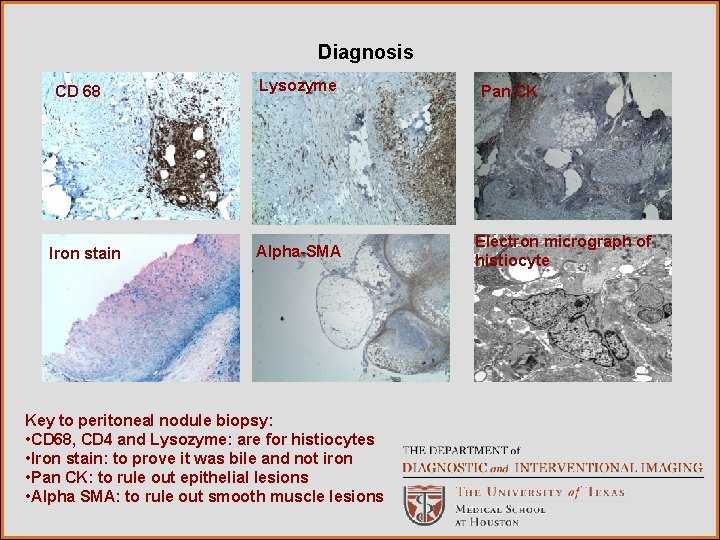
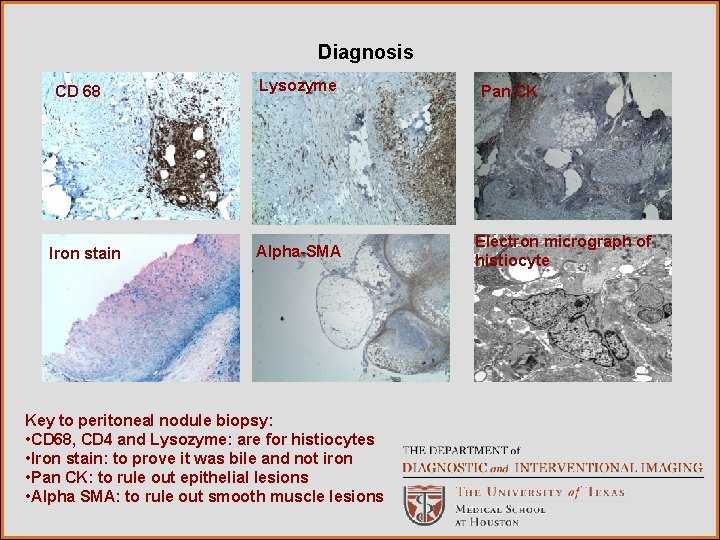
Diagnosis CD 68 Iron stain Lysozyme Alpha-SMA Key to peritoneal nodule biopsy: • CD 68, CD 4 and Lysozyme: are for histiocytes • Iron stain: to prove it was bile and not iron • Pan CK: to rule out epithelial lesions • Alpha SMA: to rule out smooth muscle lesions Pan CK Electron micrograph of histiocyte
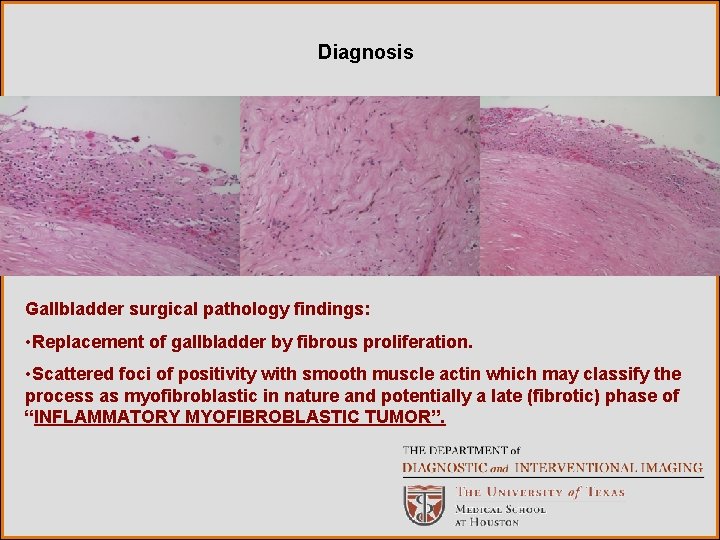
Diagnosis Gallbladder surgical pathology findings: • Replacement of gallbladder by fibrous proliferation. • Scattered foci of positivity with smooth muscle actin which may classify the process as myofibroblastic in nature and potentially a late (fibrotic) phase of “INFLAMMATORY MYOFIBROBLASTIC TUMOR”.
16 months later………. .
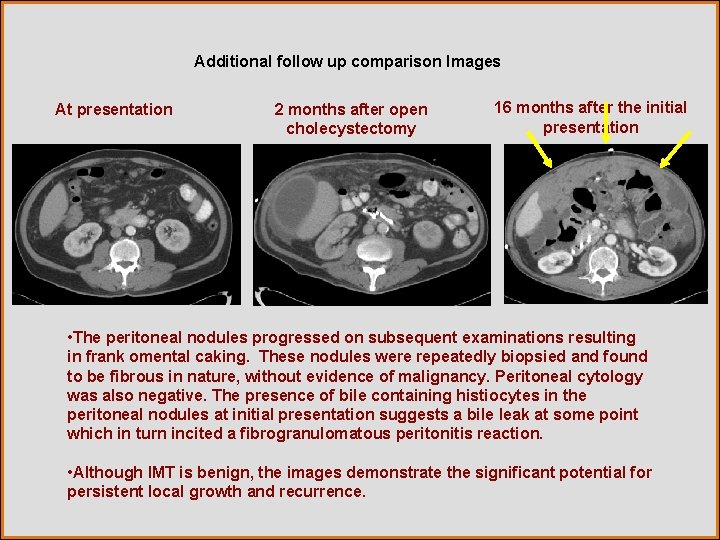
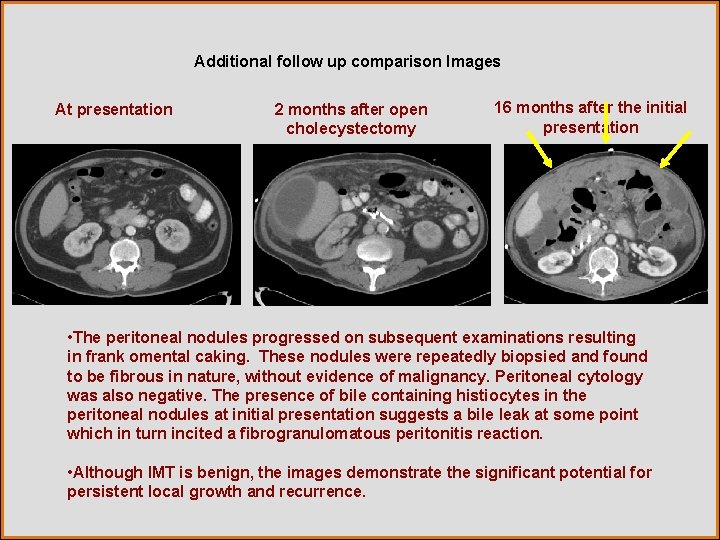
Additional follow up comparison Images At presentation 2 months after open cholecystectomy 16 months after the initial presentation • The peritoneal nodules progressed on subsequent examinations resulting in frank omental caking. These nodules were repeatedly biopsied and found to be fibrous in nature, without evidence of malignancy. Peritoneal cytology was also negative. The presence of bile containing histiocytes in the peritoneal nodules at initial presentation suggests a bile leak at some point which in turn incited a fibrogranulomatous peritonitis reaction. • Although IMT is benign, the images demonstrate the significant potential for persistent local growth and recurrence.
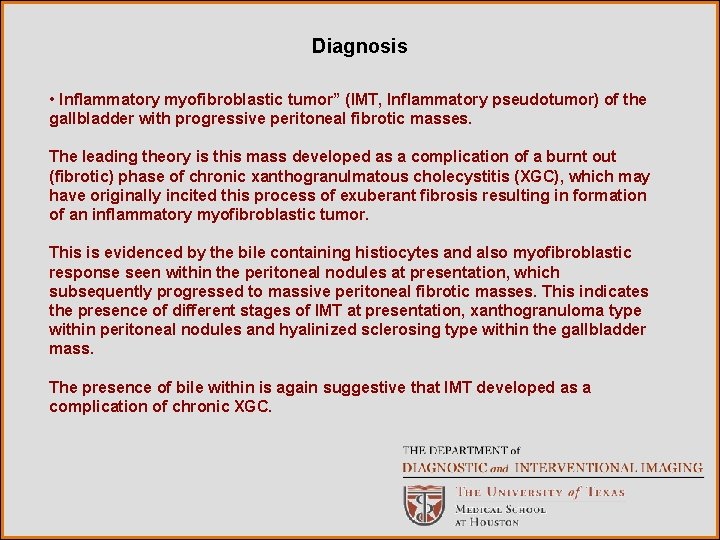
Diagnosis • Inflammatory myofibroblastic tumor” (IMT, Inflammatory pseudotumor) of the gallbladder with progressive peritoneal fibrotic masses. The leading theory is this mass developed as a complication of a burnt out (fibrotic) phase of chronic xanthogranulmatous cholecystitis (XGC), which may have originally incited this process of exuberant fibrosis resulting in formation of an inflammatory myofibroblastic tumor. This is evidenced by the bile containing histiocytes and also myofibroblastic response seen within the peritoneal nodules at presentation, which subsequently progressed to massive peritoneal fibrotic masses. This indicates the presence of different stages of IMT at presentation, xanthogranuloma type within peritoneal nodules and hyalinized sclerosing type within the gallbladder mass. The presence of bile within is again suggestive that IMT developed as a complication of chronic XGC.
References 1. Han JK, Choi BI, Kim AH, An SK, Lee JW, Kim TK, Kim SW. Cholangiocarcinoma: Pictoral essay of CT and cholangiographic findings. Radio. Graphics 2002; 22: 173– 187. 2. Worawattanakul S, Semelka RC, Noone TC, Calvo BF, Kelekis NL, Woosley JT. Cholangiocarcinoma: Spectrum of appearances on MR images using current techniques. Magnetic Resonance Imaging 1998; 16: 993– 1003. 3. Menias CO, Surabhi VR, Prasad SR, Wang HL, Narra VR, Chintapalli KN. Mimics of Cholangiocarcinoma: Spectrum of disease. Radio. Graphics 2008; 28: 1115– 1129. 4. Levy AD, Murakata LA, Rohrmann CA. Gallbladder Carcinoma: Radiologic. Pathologic Correlation. Radio. Graphics 2001; 21: 295– 314. 5. Catalano OA, Sahani DV, Kalva SP, Cushing MS, Hahn PF, Brown JJ, Edelman RR. MR Imaging of the Gallbladder: A Pictorial Essay. Radio. Graphics 2008; 28: 135– 155.
References 6. Chun KA, Ha KH, Yu ES, Shinn KS, Kim KW, Lee DH, Kang SW, Auh, YH. Xanthogranulomatous Cholecystitis: CT Features with Emphasis on Differentiation from Gallbladder Carcinoma. Radiology 1997; 203: 93 -97. 7. Parra JA, Acinas O, Bueno J, Guezmes A, Fernandez MA, Farinas MC. Xanthogranulomatous Cholecystitis: Clinical, Sonographic, and CT Findings in 26 Patients. AJR 2000; 174: 979– 983. 8. Levy AD, Murakata LA, Abbott RM, Rohrmann CA. From the Archives of the AFIP Benign Tumors and Tumorlike Lesions of the Gallbladder and Extrahepatic Bile Ducts: Radiologic-Pathologic Correlation. Radio. Graphics 2002; 22: 387– 413. 9. Shuto R, Kiyosue H, Komatsu E, Matsumoto S, Kawano K, Kondo Y, Yokoyama S, Mori H. CT and MR imaging findings of xanthogranulomatous cholecystitis: correlation with pathologic findings. Eur Radiol 2004; 14: 440– 446.
References 10. Goshima S, Chang S, Wang JH, Kanematsu M, Bae KT, Federle MP. Xanthogranulomatous cholecystitis: Diagnostic performance of CT to differentiate from gallbladder cancer. Eur J Radiol (2009), doi: 10. 1016/j. ejrad. 2009. 04. 017 11. Behranwala KA, Straker P, Wan A, Fisher C, Thompson JN. Inflammatory myofibroblastic tumour of the gallbladder. World Journal of Surgical Oncology 2005, 3: 24 doi: 10. 1186/1477 -7819 -3 -24 12. Venkataraman S, Semelka RC, Braga L, Danet IM, Woosley JT. Inflammatory Myofibroblastic Tumor of the Hepatobiliary System: Report of MR Imaging Appearance in Four Patients. Radiology 2003; 227: 758– 763. 13. Tublin ME, Moser AJ, Marsh JW, Gamblin TC. Biliary Inflammatory Pseudotumor: Imaging Features in Seven Patients. AJR 2007; 188: W 44–W 48. 14. Yan FH, Zhou KR, Jiang YP, Shi WB. Inflammatory pseudotumor of the liver: 13 cases of MRI findings. World J Gastroentero, 2001; 7(3): 422 – 424. Acknowledgements for the slides: Dr. Brown and Dr. Trujillo, Department of Pathology, University of Texas HSC, Houston, TX.
 Erate category 2 eligible equipment
Erate category 2 eligible equipment Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Mri principal
Mri principal Intestinal villus
Intestinal villus Gastrointestinal tract
Gastrointestinal tract Gastrointestinal tract
Gastrointestinal tract Pneumatic reduction of intussusception
Pneumatic reduction of intussusception Rins anatomia
Rins anatomia Dr sigid djuniawan
Dr sigid djuniawan Gastrointestinal medical terminology breakdown
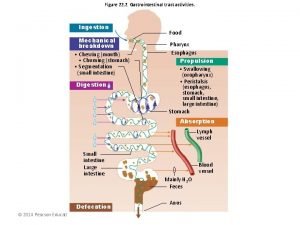
Gastrointestinal medical terminology breakdown Peristalsis and segmentation
Peristalsis and segmentation Motilidad gastrointestinal
Motilidad gastrointestinal Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Ashraf radwan
Ashraf radwan Sinal de lichtenberg medicina legal
Sinal de lichtenberg medicina legal Palpation percussion auscultation
Palpation percussion auscultation Embriologia del sistema gastrointestinal
Embriologia del sistema gastrointestinal Metformin and constipation
Metformin and constipation Borborygmi
Borborygmi Dumping syndrome signs
Dumping syndrome signs Chapter 15 the gastrointestinal system
Chapter 15 the gastrointestinal system Gastrointestinal tüp aracılığıyla ilaç uygulama
Gastrointestinal tüp aracılığıyla ilaç uygulama Pankreatik polipeptid
Pankreatik polipeptid Foregut midgut hindgut
Foregut midgut hindgut Gastrointestinal tract
Gastrointestinal tract What is alimentary canal
What is alimentary canal Orgaos anexos
Orgaos anexos Gastrointestinal hormones
Gastrointestinal hormones Medium modality
Medium modality Modality in software engineering
Modality in software engineering Cardinality and modality
Cardinality and modality Modality
Modality Tom arbuthnot
Tom arbuthnot Epistemic modality
Epistemic modality Crow's foot notation
Crow's foot notation Swd modality
Swd modality Modality stats
Modality stats