Radiological Category Gastrointestinal Principal Modality 1 CT Principal


- Slides: 13

Radiological Category: Gastrointestinal Principal Modality (1): CT Principal Modality (2): MRI Case Report 715 Submitted by: Jesse Proett, M. D. Faculty reviewer: Venkateswar Surabhi, M. D The University of Texas Medical School at Houston Date accepted: 5 April 2010
Case History 17 yo girl with worsening abdominal pain, nausea, and vomiting for several weeks.

Radiological Presentations CECT
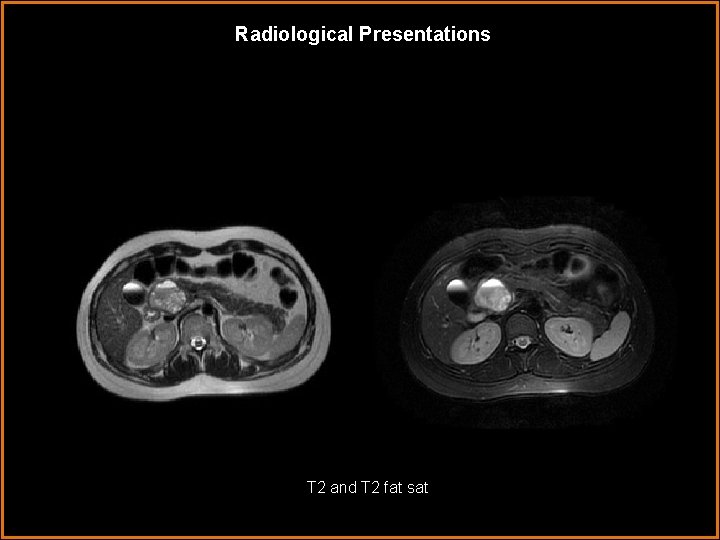
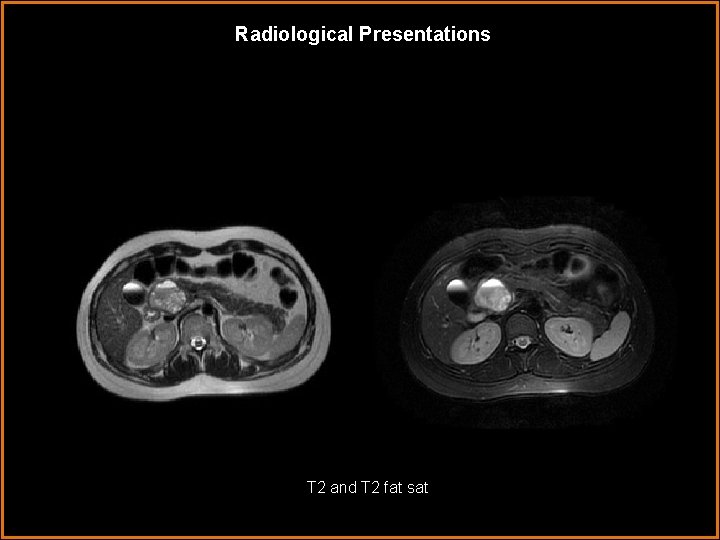
Radiological Presentations T 2 and T 2 fat sat
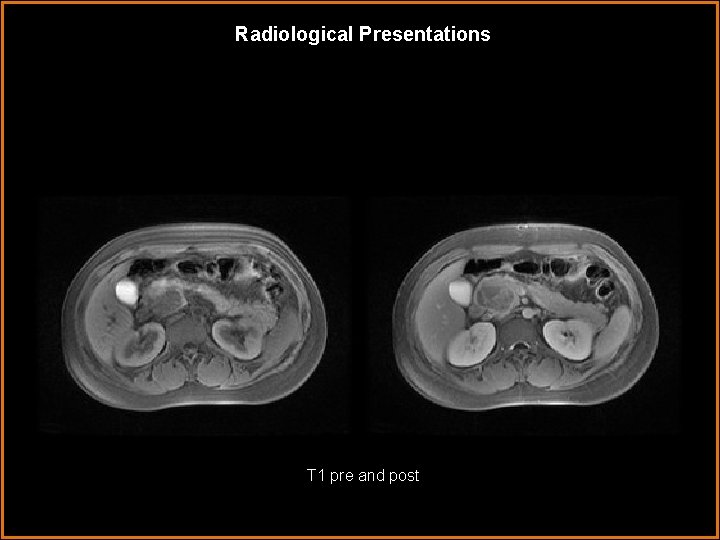
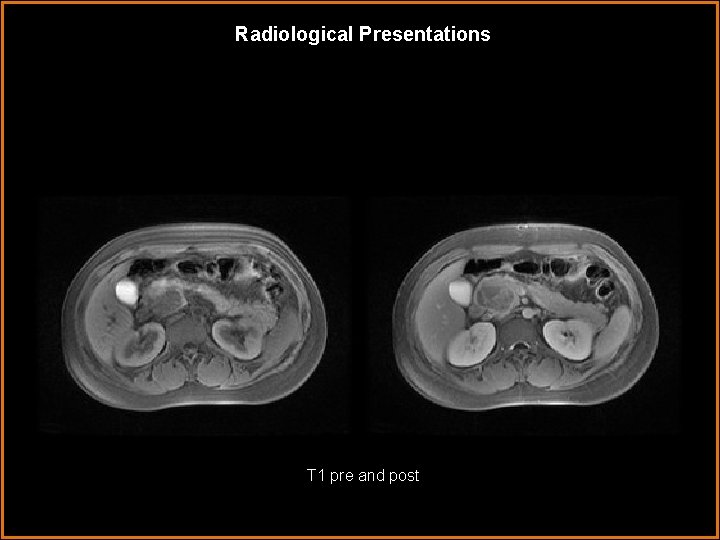
Radiological Presentations T 1 pre and post
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Solid Pseudopapillary Tumor of the Pancreas • Pancreaticoblastoma • Teratoma • Nonfunctioning Neuroendocrine Tumor • Hemorrhagic Pseudocyst • Serous Microcystic Adenoma • Mucinous Cystic Neoplasm
Findings and Differentials Findings: CT: There is a large pacreatic head mass with heterogeneous attenuation. Solid and cystic portions are noted surrounded by a sharply demarcated enhancing capsule. No calcifications, internal septations or central scar is identified. MRI: Mass shows high and low intensity signal on T 1 and T 2 weighted images with predominantly hyperintense features on T 2. It is well circumscribed with a distinct T 2 hypointense fibrous capsule. Pre-contrast T 1 images show areas of high signal corresponding with low signal on T 2 representing hemorrhage. There is early intense enhancement of the capsule and mild heterogeneous central enhancement of the solid portions. The internal enhancement is less intense than the normal pancreatic parenchyma. No pancreatic duct dilatation is present. Differentials: • Solid Pseudopapillary Tumor of the Pancreas
Discussion There is a wide differential for solid and cystic masses of the pancreas. However, history, patient demographics, and key findings on CT and MRI can help narrow this down to the most likely diagnosis. Ultimately, microscopic evaluation of the mass is necessary to make a definitive diagnosis. Without a history of pancreatitis, a hemorrhagic pancreatic pseudocyst is not likely even though this is the most common cystic lesion of the pancreas. Serous microcystic adenoma, mucinous cystic neoplasm, and nonfunctioning neuroendocrine tumors such as cystic islet cell tumors are rarely seen in patients younger than 30 years of age. Additionally, contrast enhancement of islet cell tumors typically show greater enhancement compared to normal pactreatic parenchyma. No calcification or fat associated with the mass rules out the possibility of a teratoma.
Discussion The last differential left on the list is a pancreaticoblastoma (PB) which is a rare aggressive tumor having similar morphologic and enhancement features to that of solid pseudopapillary tumors (SPT). The cystic components of PB is due to liquifaction necrosis. Intratumoral hemorrhage has never been reported with PB, but is a predominant feature of SPT. Also, PB is more aggressive and almost always presents with liver metastases initially. It would be difficult to definitively rule out PB, but the features mentioned above help differentiate PB from SPT.
Discussion Solid Pseudopapillary Tumor (SPT) is a rare pancreatic mass representing only 0. 13 -2. 7% of all pancreatic tumors. These tumors are overwhelmingly seen in young women under 30 years of age with a mean age between 23 -27 yrs and a male to female ratio of 1: 9. 5. SPT was first described in 1959 by Dr Franz who affectionately named it Franz’s tumor. Since then it has assumed many different names including solid and cystic tumor, solid and papillary epithelial neoplasm (SPEN), papillary cystic neoplasm, papillary cystic epithelial neoplasm, papillary cystic tumor, and of course Franz tumor. This cornucopia of names made it confusing and in 1996 the WHO renamed it solid pseudopapillary tumor (SPT) of the pancreas based on its origin in the exocrine pancreas. Grossly SPT is a large encapsulated mass composed of a mixture of cystic, solid and hemorrhagic components. The characteristic features are the capsule and hemorrhagic areas which are rarely found in other pancreatic tumors. Because of its exocrine origin SPT rarely causes pancreatic duct obstruction or dilatation. SPT can be found anywhere along the pancreas with a slight predilection for the pancreatic tail reported in a few case series.
Discussion Characteristic Imaging Features of SPT CT: Typical features of SPT on CT are a large well-defined encapsulated mass with solid and cystic components caused by hemorrhage. Calcification are often seen along the periphery. Enhancement of the capsule and solid structures within the mass are also characteristic. MRI: The appearance on MRI classically shows a well-defined mass with a low signal capsule on T 2 weighted images. The tumor will have a mix of high and low signal intensity on T 1 and T 2 weighted images. The areas of high signal on T 1 and low or inhomogeneous signal on T 2 help identify hemorrhage which is the key finding in SPT that helps differentiate it from most other pancreatic tumors. The enhancement pattern shows early peripheral enhancement of the capsule and solid portions with progressive fill-in of the tumor.
Diagnosis Solid Pseudopapillary Tumor of the Pancreas
References Cantisani V et al: MR Imaging features of solid pseudopapillary tumor of the pancreas in adult and pediatric patients. AJR. 181: 395 -401, 2003 Choi JY et al: Solid pseudopapillary tumor of the pancreas: Typical and atypical manifestations. AJR. 187: 178 -186, 2006 Madan AK et al: Solid and papillary epithelial neoplasm of the pancreas. Journal Surgical Oncology. 85(4): 193 -198, 2004 Yu CC et al: Clinicopathologic study of solid and pseudopapillary tumor of pancreas: Emphysis on magnetic resonance imaging findings. World Journal Gastroenterology. 13(12): 1811 -1815, 2007 Buetow PC et al: Solid and papillary epithelial neoplasm of the pancreas: imagingpathologic correlationon 56 cases. Radiology. 199(3): 707 -711, 1996 Choi BI et al: Solid and papillary neoplasms of the pancreas: CT findings. Radiology. 166(2): 413 -416. 1988
 Erate pa
Erate pa Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Nutrition focused physical findings
Nutrition focused physical findings Gastrointestinal medical terminology breakdown
Gastrointestinal medical terminology breakdown Why does metformin cause gastrointestinal problems
Why does metformin cause gastrointestinal problems Chemotrypsinogen
Chemotrypsinogen Gastrointestinal diagram
Gastrointestinal diagram Sigid djuniawan
Sigid djuniawan Po ilaç uygulama
Po ilaç uygulama Embryology
Embryology Structure of alimentary canal
Structure of alimentary canal