Radiological Category Gastrointestinal Principal Modality 1 CT Principal

- Slides: 17
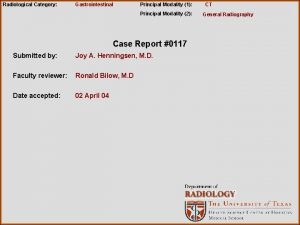
Radiological Category: Gastrointestinal Principal Modality (1): CT Principal Modality (2): Fluoroscopy Case Report #0481 Submitted by: Kiran Chang, M. D. Faculty reviewer: Venkateswar Surabhi, M. D. Date accepted: 06 March 2008
Case History 60 yr old male with chronic abdominal pain
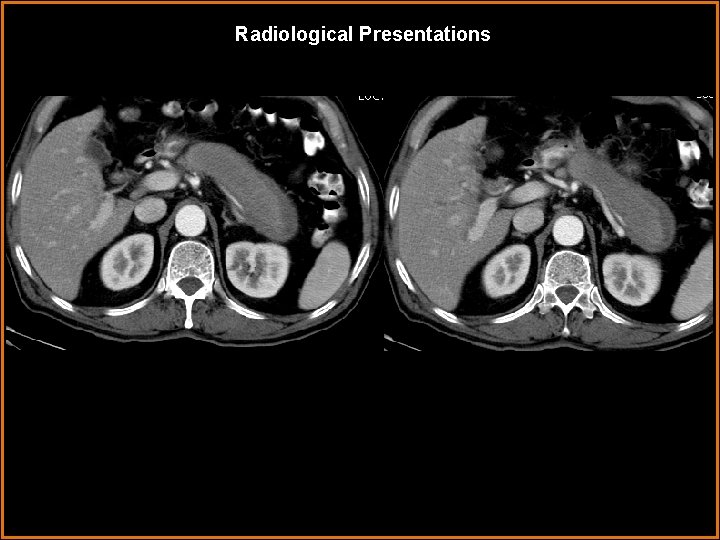
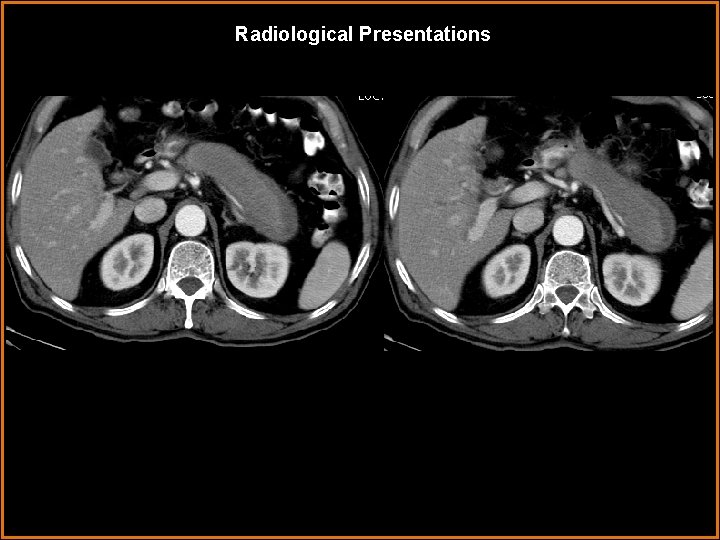
Radiological Presentations
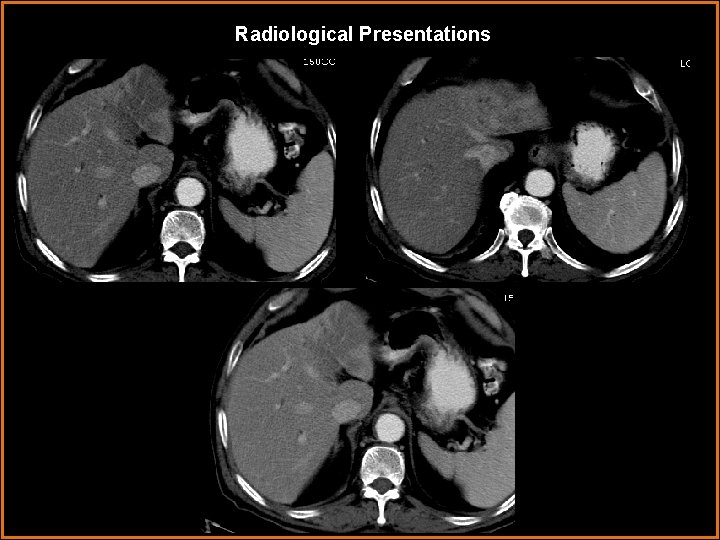
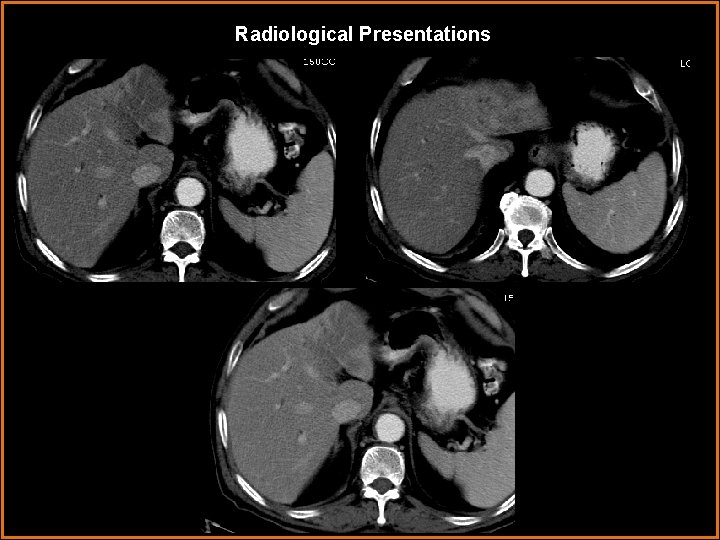
Radiological Presentations
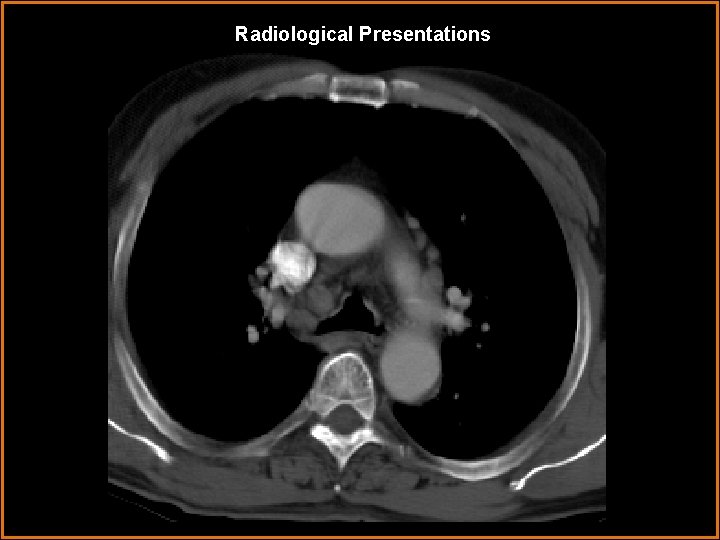
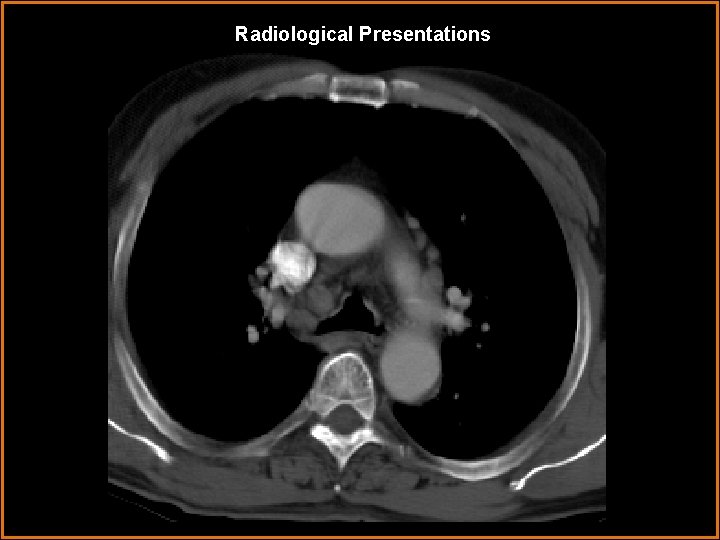
Radiological Presentations
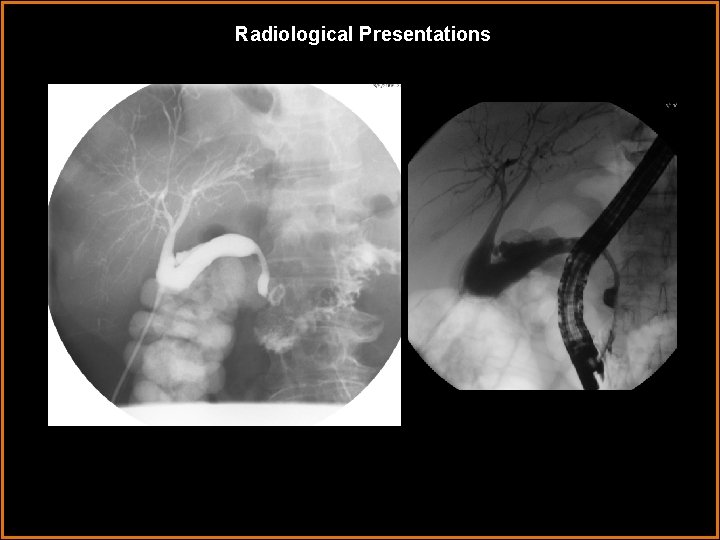
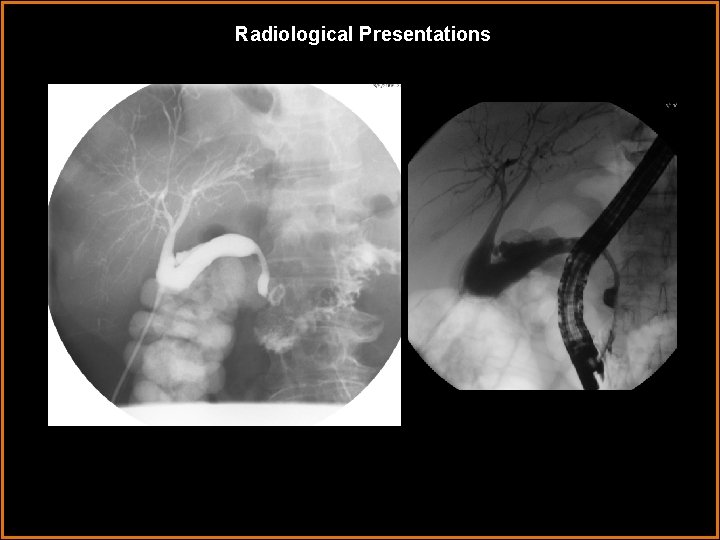
Radiological Presentations
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • cholangiocarcinoma • pancreatic malignancy • autoimmune hepatitis • autoimmune pancreatitis
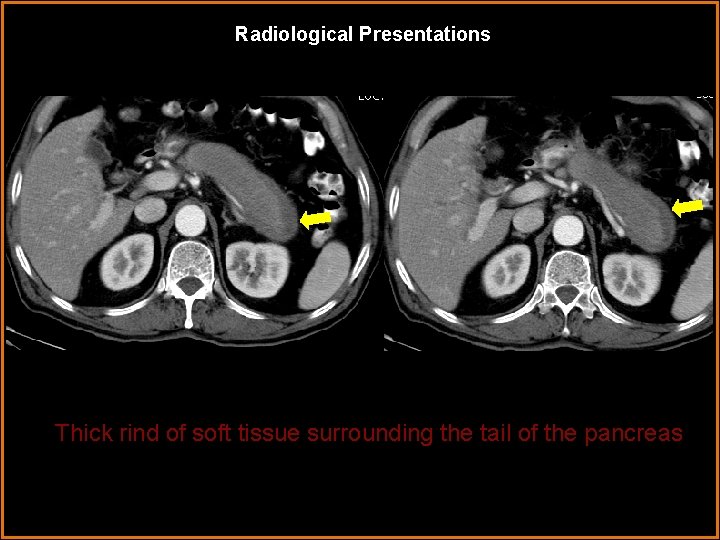
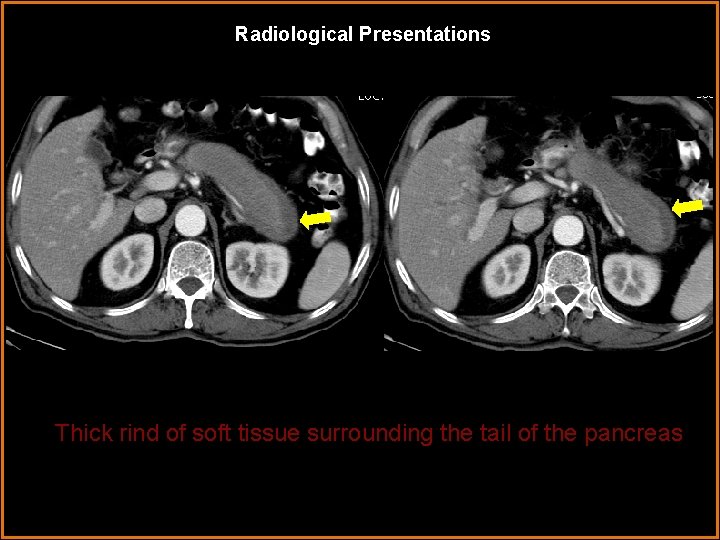
Radiological Presentations Thick rind of soft tissue surrounding the tail of the pancreas
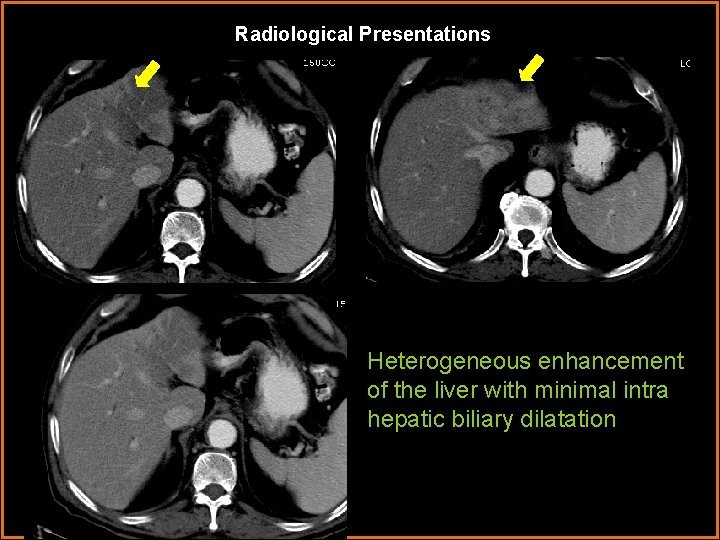
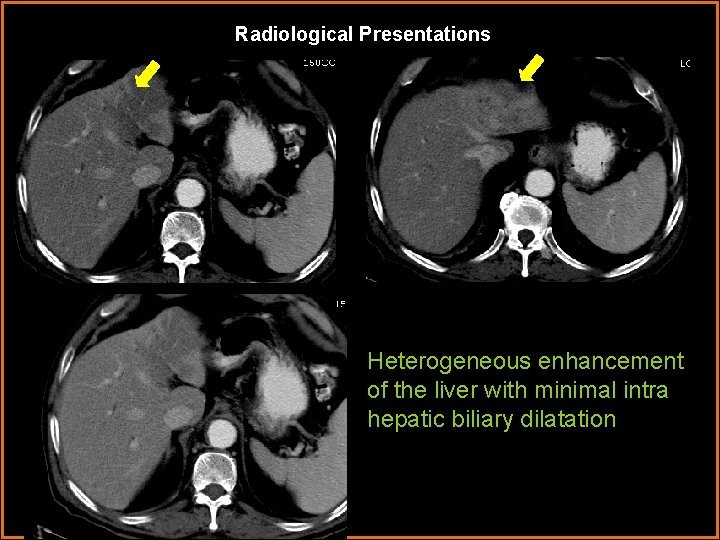
Radiological Presentations Heterogeneous enhancement of the liver with minimal intra hepatic biliary dilatation
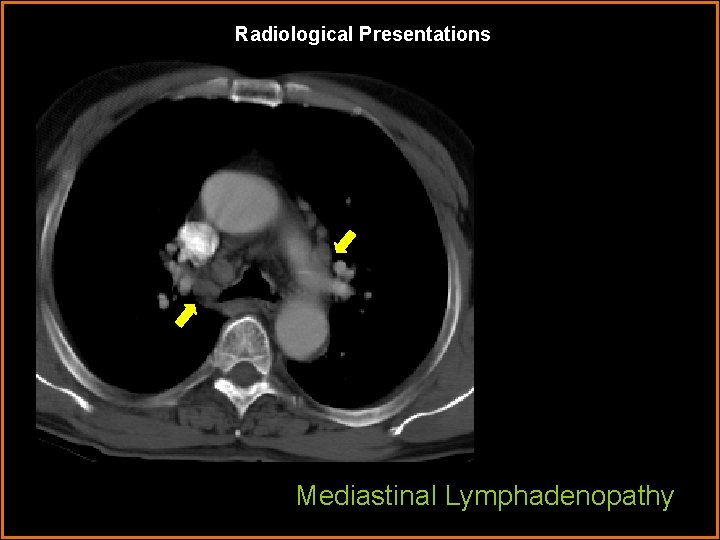
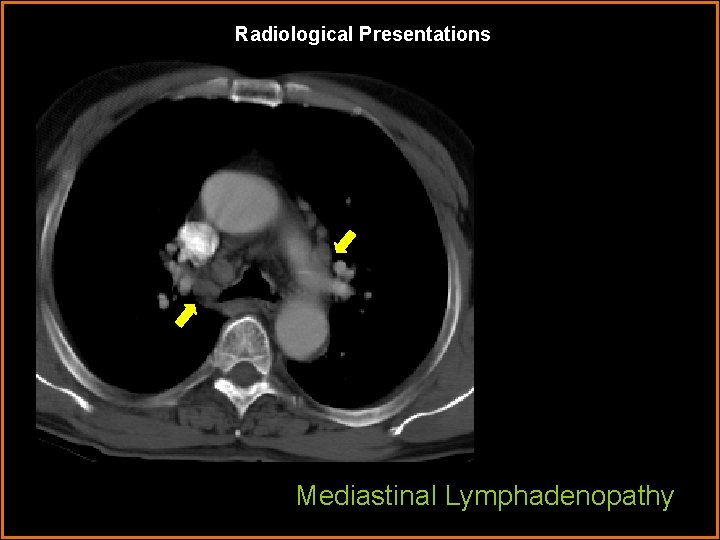
Radiological Presentations Mediastinal Lymphadenopathy
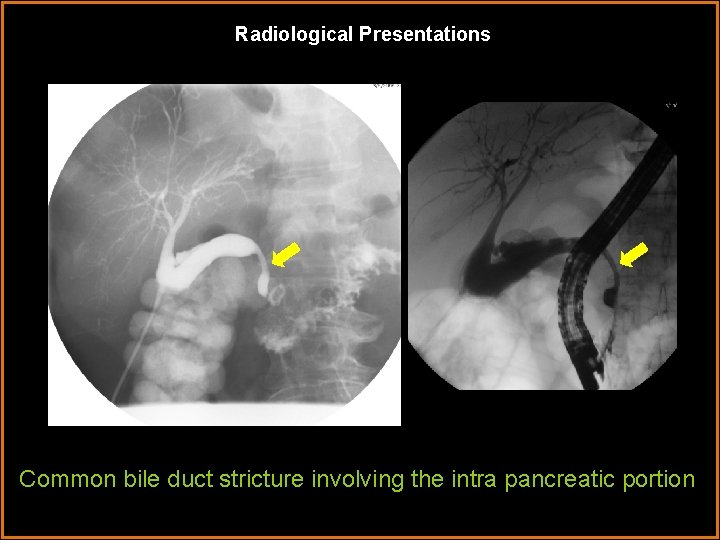
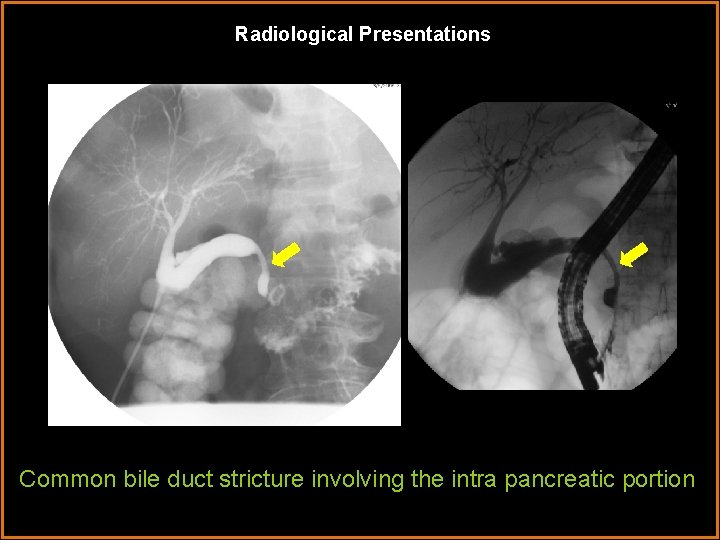
Radiological Presentations Common bile duct stricture involving the intra pancreatic portion
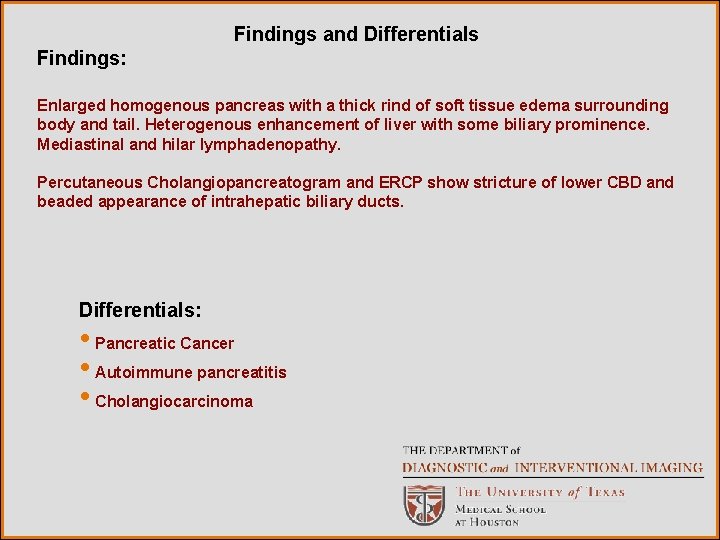
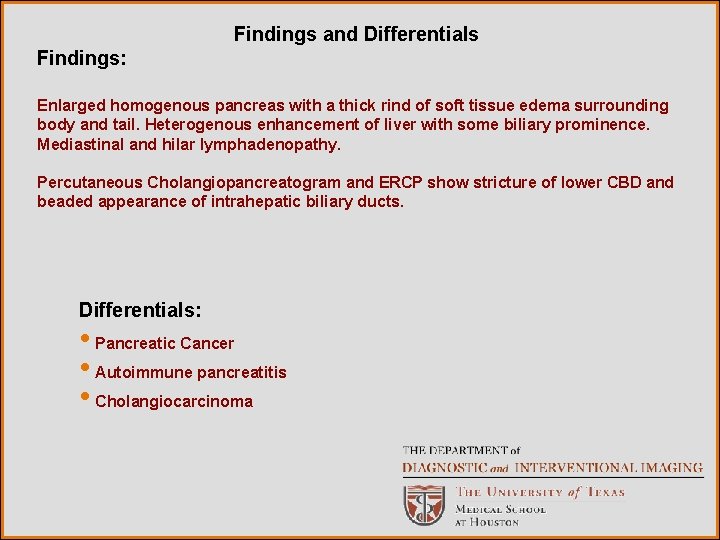
Findings and Differentials Findings: Enlarged homogenous pancreas with a thick rind of soft tissue edema surrounding body and tail. Heterogenous enhancement of liver with some biliary prominence. Mediastinal and hilar lymphadenopathy. Percutaneous Cholangiopancreatogram and ERCP show stricture of lower CBD and beaded appearance of intrahepatic biliary ducts. Differentials: • Pancreatic Cancer • Autoimmune pancreatitis • Cholangiocarcinoma
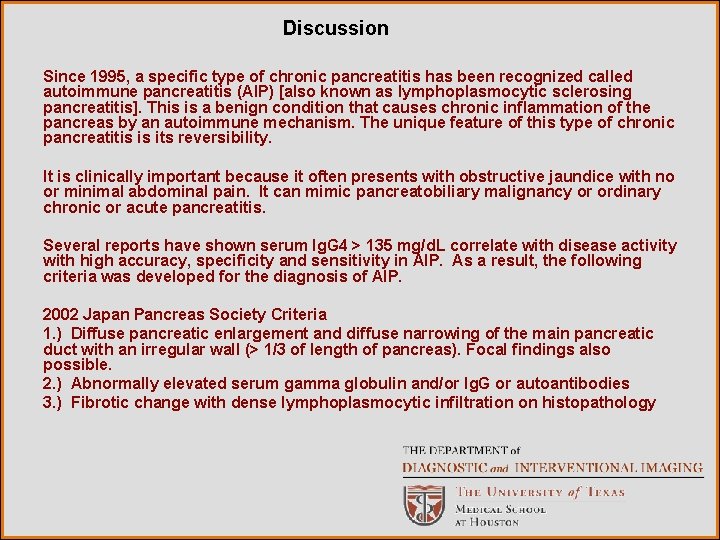
Discussion Since 1995, a specific type of chronic pancreatitis has been recognized called autoimmune pancreatitis (AIP) [also known as lymphoplasmocytic sclerosing pancreatitis]. This is a benign condition that causes chronic inflammation of the pancreas by an autoimmune mechanism. The unique feature of this type of chronic pancreatitis is its reversibility. It is clinically important because it often presents with obstructive jaundice with no or minimal abdominal pain. It can mimic pancreatobiliary malignancy or ordinary chronic or acute pancreatitis. Several reports have shown serum Ig. G 4 > 135 mg/d. L correlate with disease activity with high accuracy, specificity and sensitivity in AIP. As a result, the following criteria was developed for the diagnosis of AIP. 2002 Japan Pancreas Society Criteria 1. ) Diffuse pancreatic enlargement and diffuse narrowing of the main pancreatic duct with an irregular wall (> 1/3 of length of pancreas). Focal findings also possible. 2. ) Abnormally elevated serum gamma globulin and/or Ig. G or autoantibodies 3. ) Fibrotic change with dense lymphoplasmocytic infiltration on histopathology
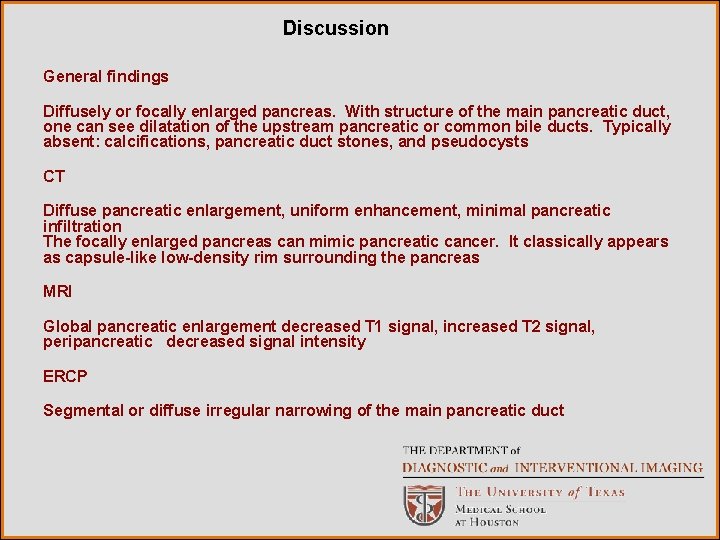
Discussion General findings Diffusely or focally enlarged pancreas. With structure of the main pancreatic duct, one can see dilatation of the upstream pancreatic or common bile ducts. Typically absent: calcifications, pancreatic duct stones, and pseudocysts CT Diffuse pancreatic enlargement, uniform enhancement, minimal pancreatic infiltration The focally enlarged pancreas can mimic pancreatic cancer. It classically appears as capsule-like low-density rim surrounding the pancreas MRI Global pancreatic enlargement decreased T 1 signal, increased T 2 signal, peripancreatic decreased signal intensity ERCP Segmental or diffuse irregular narrowing of the main pancreatic duct
Discussion Focal involvement of pancreas in AIP may mimic pancreatic cancer, therefore fine needle aspiration may sometimes be necessary to distinguish. CT findings more often seen in pancreatic cancer than in autoimmune pancreatitis are: 1. ) Significant dilatation of the main pancreatic duct proximal to the narrowed segment 2. ) Atrophy of the pancreatic parenchyma proximal to the mass or focal enlargement 3. ) Involvement of the major peripancreatic vessels, particularly arterial involvement. In patients with segmental narrowing of the main pancreatic duct due to AIP, the main pancreatic duct proximal to the segmental narrowing typically shows minimal or no dilatation. Extrapancreatic Manifestations Associated with AIP • Biliary strictures • Sclerosing cholangitis • Sialoadenitis • Retroperitoneal fibrosis • Hilar or abdominal lymphadenopathy • Chronic thyroiditis • Interstitial nephritis • Inflammatory bowel disease

Diagnosis Autoimmune pancreatitis Associated with extra pancreatic manifestations 1. Primary sclerosing cholangitis 2. Hilar lypmhadenopathy 3. CBD stricture
References Kawamoto, S, Siegelman, S, Hruban, R, Fishman, E. “Lymphoplasmocytic Sclerosing Pancreatitis (Autoimmune Pancreatitis): Evaluation with Multidetector CT. ” Radio. Graphics 2008; 28: 157 -170. Kim, KP, Kim, MH, Song, MH, Lee, SS, Seo, DW, Lee, SK. “Autoimmune Chronic Pancreatitis. ” Am J Gastroenterol 2004; 99: 1605 -1616.
 E-rate category 1 vs category 2
E-rate category 1 vs category 2 Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Gastrointestinal medical terminology breakdown
Gastrointestinal medical terminology breakdown Nursing diagnosis for pud
Nursing diagnosis for pud Gastrointestinal tract
Gastrointestinal tract Ashraf radwan
Ashraf radwan Nutrition focused physical findings
Nutrition focused physical findings Why does metformin cause gastrointestinal problems
Why does metformin cause gastrointestinal problems Malrotasi traktus gastrointestinal
Malrotasi traktus gastrointestinal Upper gi bleeding management
Upper gi bleeding management Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Sublingual ilaç uygulaması
Sublingual ilaç uygulaması Cloaca
Cloaca Alimentary canal in order
Alimentary canal in order Espectro equimótico
Espectro equimótico