Quality Payment Program Medicare Access and Chip Reauthorization

- Slides: 54
Quality Payment Program Medicare Access and Chip Reauthorization Act of 2015 (MACRA) Paul A. Martin DO FACOFP dist. CMO/VP Grandview/Southview Medical Centers
Quality Payment Program Which current physician payment adjustment will sunset after December 31, 2018? A. Medicare Shared Savings Program (MSSP) B. Comprehensive Primary Care Initiative (CPCI) C. EHR Meaningful Use program (MU) D. Comprehensive Primary Care Plus (CPC+) 102
Quality Payment Program By not participating in the MIPS Quality Payment Program in the 2017 transition year, what negative payment adjustment would eligible physicians incur? A. Negative. 5% payment adjustment B. Negative 4% payment adjustment C. Negative 1% payment adjustment D. Negative 9% payment adjustment 103
Quality Payment Program MACRA Background
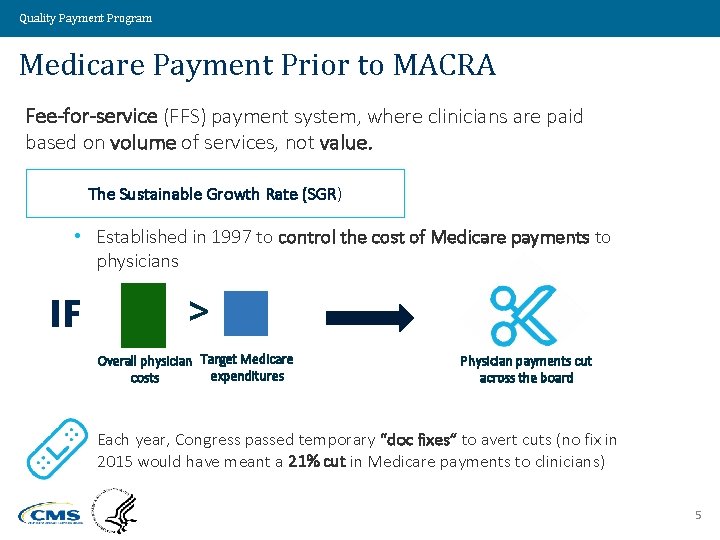
Quality Payment Program Medicare Payment Prior to MACRA Fee-for-service (FFS) payment system, where clinicians are paid based on volume of services, not value. The Sustainable Growth Rate (SGR) • Established in 1997 to control the cost of Medicare payments to physicians IF > Overall physician Target Medicare expenditures costs Physician payments cut across the board Each year, Congress passed temporary “doc fixes” to avert cuts (no fix in 2015 would have meant a 21% cut in Medicare payments to clinicians) 5
Quality Payment Program MACRA Background Goal – Move physician payment from volume-based to value-based • Signed into law April 2015 • Supported by organized medicine • Passed with over 90 percent support in both the House and Senate • Rare example of bi-partisan legislation - Strong indication Medicare value-based payment is here to stay Value Driven. Health Care. Solutions. 6
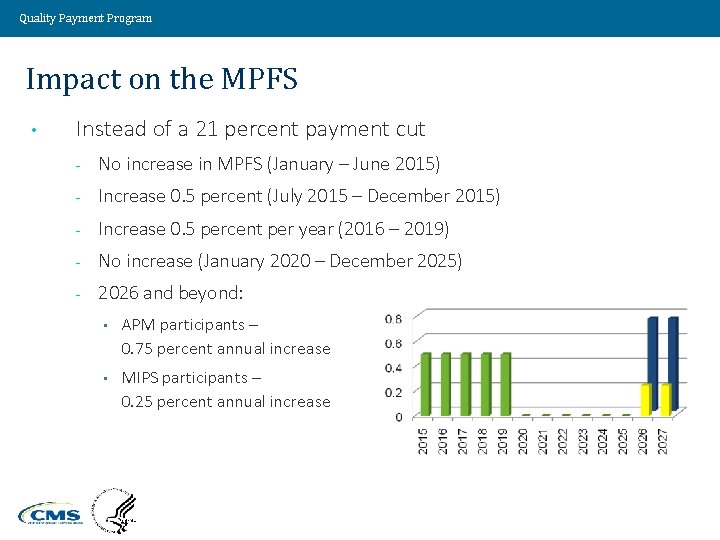
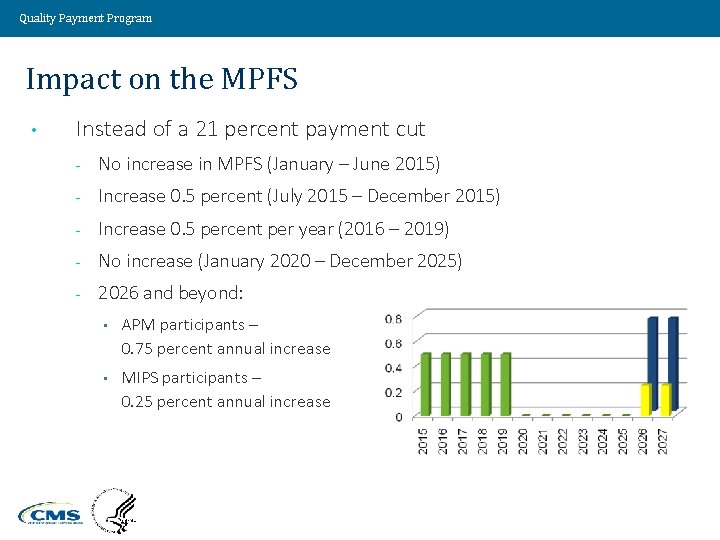
Quality Payment Program Impact on the MPFS • Instead of a 21 percent payment cut - No increase in MPFS (January – June 2015) - Increase 0. 5 percent (July 2015 – December 2015) - Increase 0. 5 percent per year (2016 – 2019) - No increase (January 2020 – December 2025) - 2026 and beyond: • APM participants – 0. 75 percent annual increase • MIPS participants – 0. 25 percent annual increase Value Driven. Health Care. Solutions. 7
Quality Payment Program Impact on Current Medicare Payment Adjustments • • Sunsets current payment adjustments after December 31, 2018 - Physician Quality Reporting System (PQRS) - EHR Meaningful Use (MU) program - Value-based Payment Modifier (VBM) Some features of PQRS, MU, and VBM are part of the new MIPS criteria Value Driven. Health Care. Solutions. 8
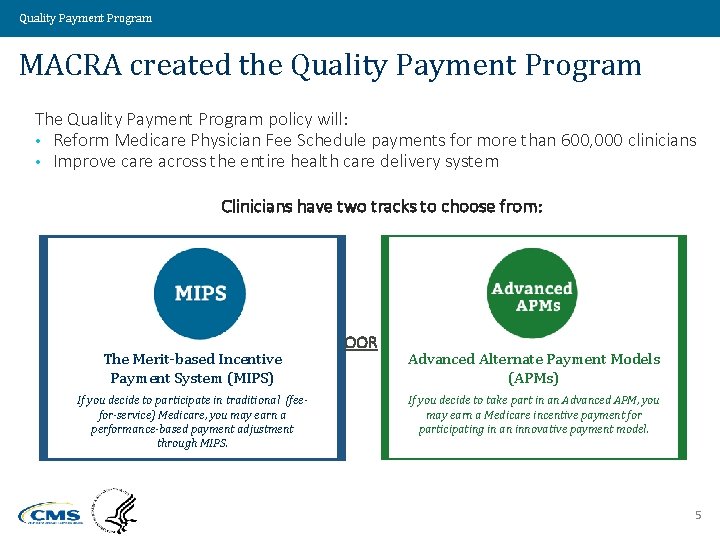
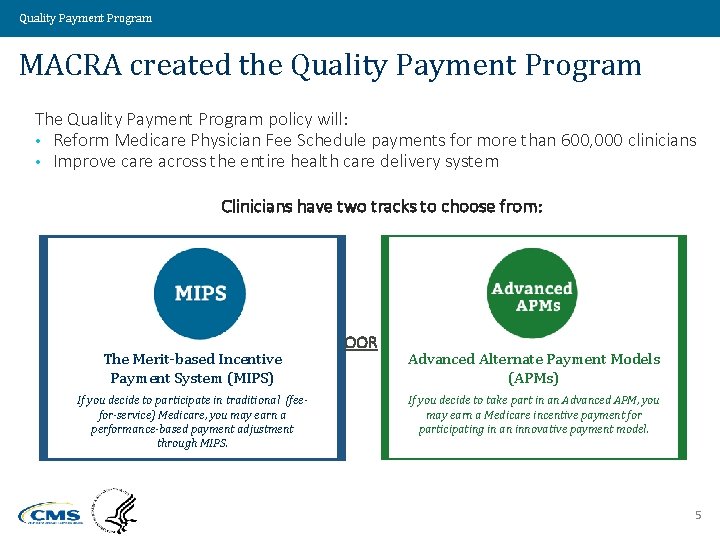
Quality Payment Program MACRA created the Quality Payment Program The Quality Payment Program policy will: • Reform Medicare Physician Fee Schedule payments for more than 600, 000 clinicians • Improve care across the entire health care delivery system Clinicians have two tracks to choose from: The Merit-based Incentive Payment System (MIPS) If you decide to participate in traditional (feefor-service) Medicare, you may earn a performance-based payment adjustment through MIPS. OOR Advanced Alternate Payment Models (APMs) If you decide to take part in an Advanced APM, you may earn a Medicare incentive payment for participating in an innovative payment model. 5
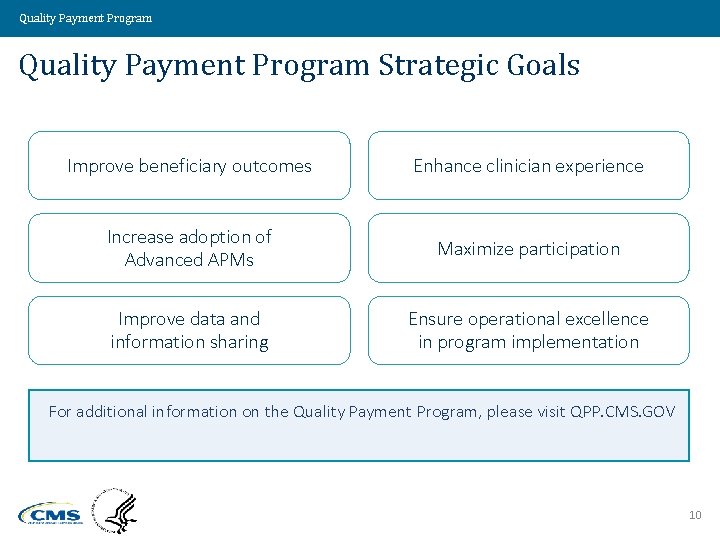
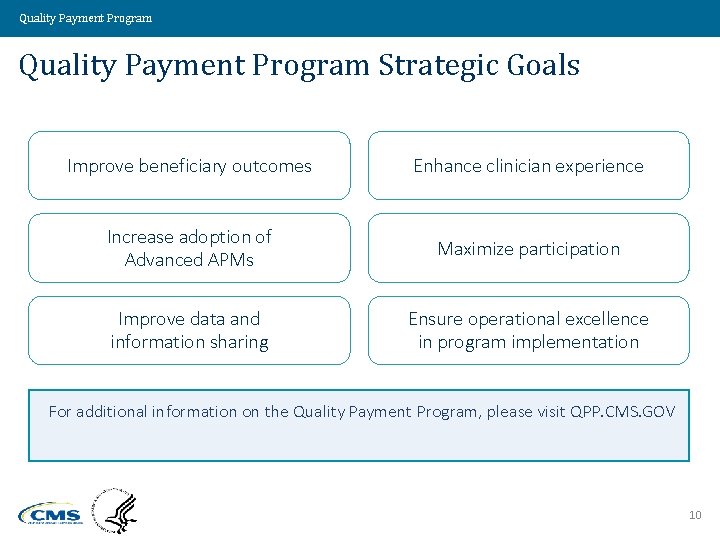
Quality Payment Program Strategic Goals Improve beneficiary outcomes Enhance clinician experience Increase adoption of Advanced APMs Maximize participation Improve data and information sharing Ensure operational excellence in program implementation For additional information on the Quality Payment Program, please visit QPP. CMS. GOV 10
Quality Payment Program 11
Quality Payment Program Alternative Payment Models (APMS)
Quality Payment Program What are APMs? • Payment approachs that incent clinicians to provide highquality, cost-effective care • Examples: - Medicare Shared Savings Program (MSSP) - CMS Innovation Center Models - CMS Demonstration Programs Value Driven. Health Care. Solutions. 13
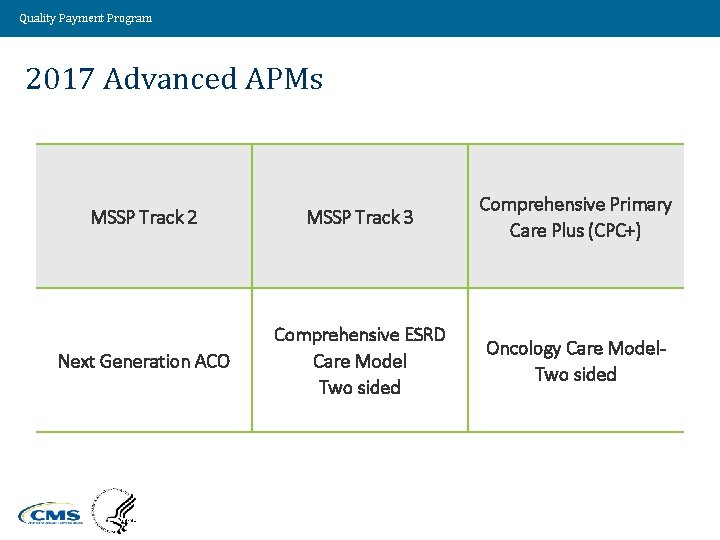
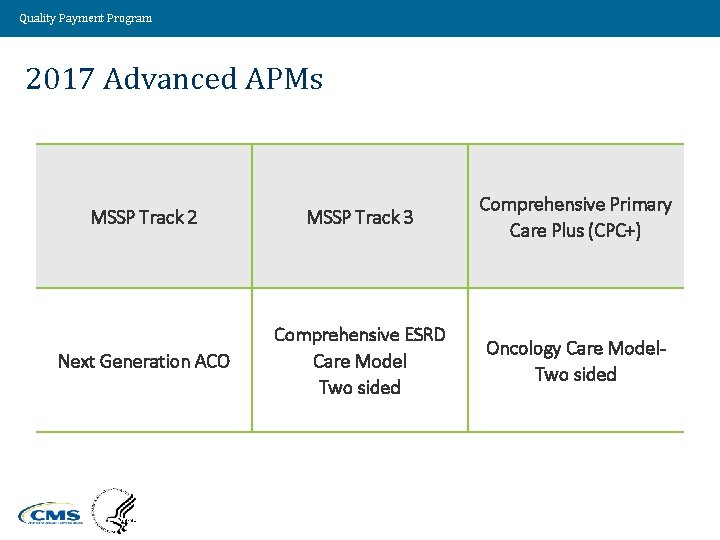
Quality Payment Program 2017 Advanced APMs MSSP Track 2 MSSP Track 3 Comprehensive Primary Care Plus (CPC+) Next Generation ACO Comprehensive ESRD Care Model Two sided Oncology Care Model. Two sided Value Driven. Health Care. Solutions. 14
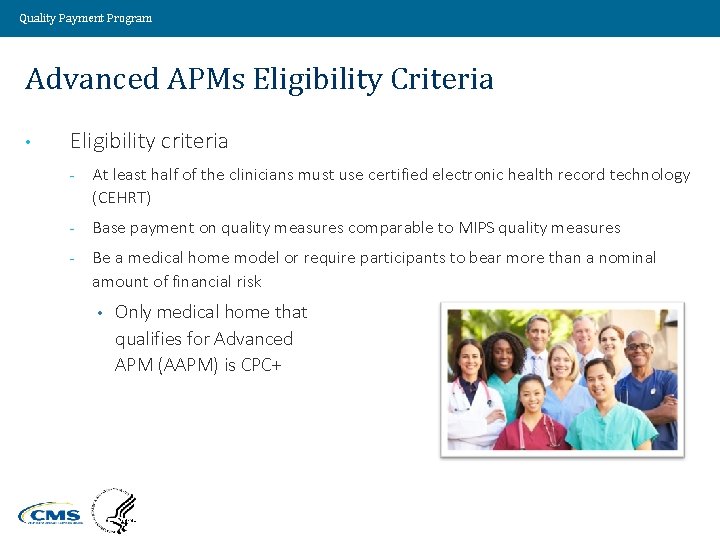
Quality Payment Program Advanced APMs Eligibility Criteria • Eligibility criteria - At least half of the clinicians must use certified electronic health record technology (CEHRT) - Base payment on quality measures comparable to MIPS quality measures - Be a medical home model or require participants to bear more than a nominal amount of financial risk • Only medical home that qualifies for Advanced APM (AAPM) is CPC+ Value Driven. Health Care. Solutions. 15
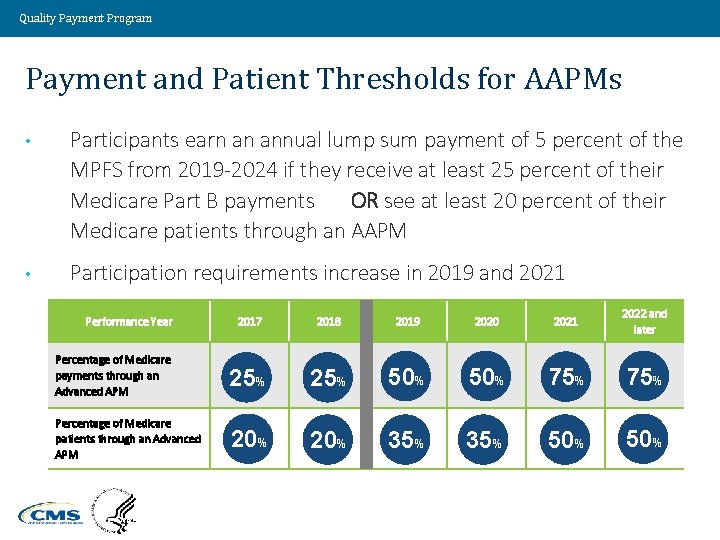
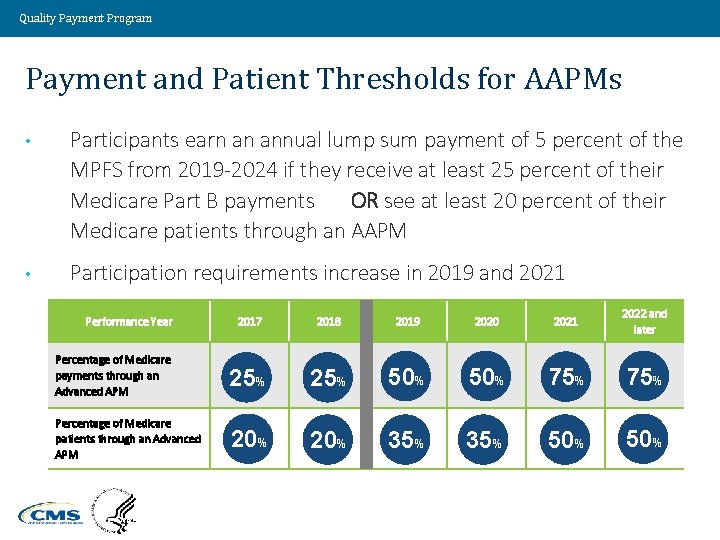
Quality Payment Program Payment and Patient Thresholds for AAPMs • Participants earn an annual lump sum payment of 5 percent of the MPFS from 2019 -2024 if they receive at least 25 percent of their Medicare Part B payments OR see at least 20 percent of their Medicare patients through an AAPM • Participation requirements increase in 2019 and 2021 2017 2018 2019 2020 2021 2022 and later Percentage of Medicare payments through an Advanced APM 25% 50% 75% Percentage of Medicare patients through an Advanced APM 20% 35% 50% Performance Year Value Driven. Health Care. Solutions. 16
Quality Payment Program Merit-Based Incentive Payment System (MIPS)
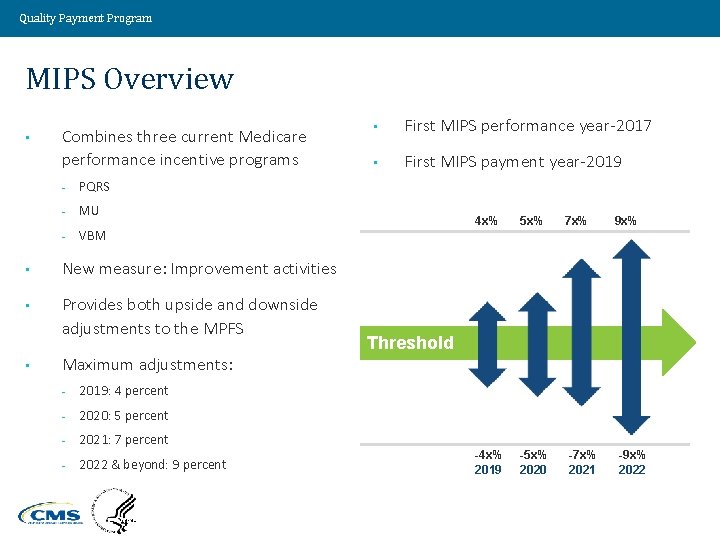
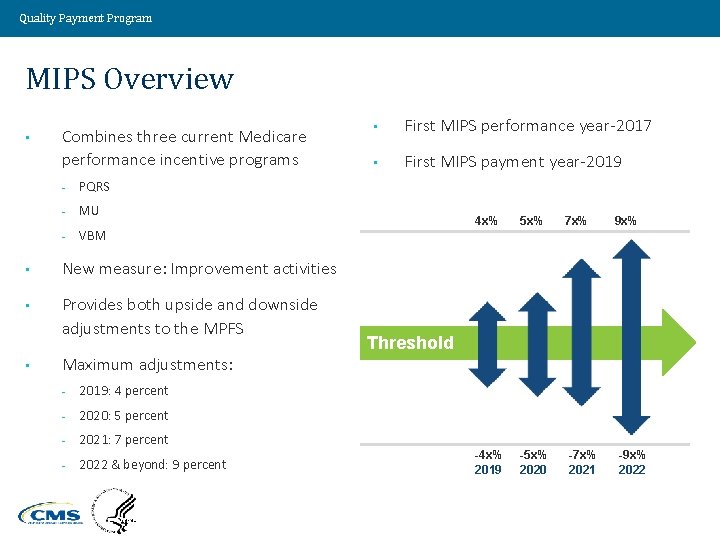
Quality Payment Program MIPS Overview • Combines three current Medicare performance incentive programs - PQRS - MU - VBM • New measure: Improvement activities • Provides both upside and downside adjustments to the MPFS • • First MIPS performance year-2017 • First MIPS payment year-2019 4 x% 5 x% -4 x% 2019 -5 x% 2020 7 x% 9 x% Threshold Maximum adjustments: - 2019: 4 percent - 2020: 5 percent - 2021: 7 percent - 2022 & beyond: 9 percent Value Driven. Health Care. Solutions. -7 x% 2021 -9 x% 2022 18
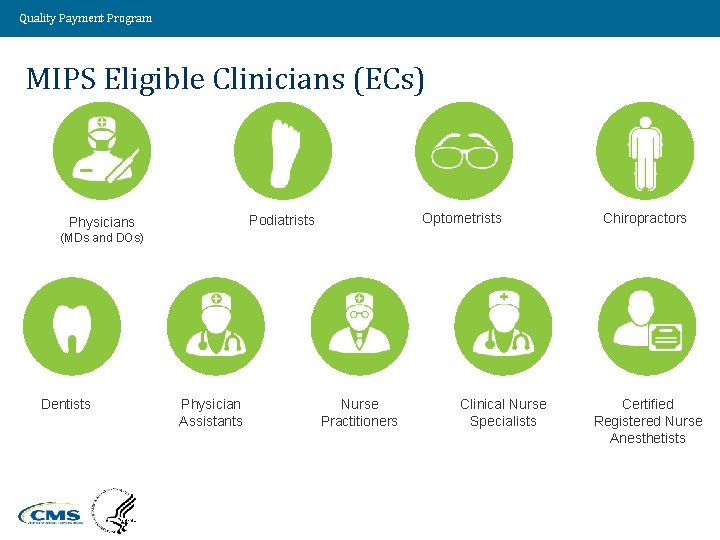
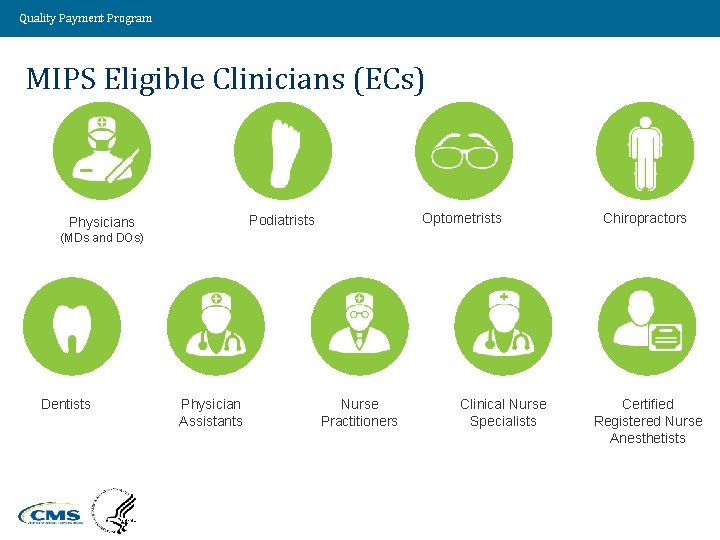
Quality Payment Program MIPS Eligible Clinicians (ECs) Optometrists Podiatrists Physicians Chiropractors (MDs and DOs) Dentists Physician Assistants Value Driven. Health Care. Solutions. Nurse Practitioners Clinical Nurse Specialists Certified Registered Nurse Anesthetists 19
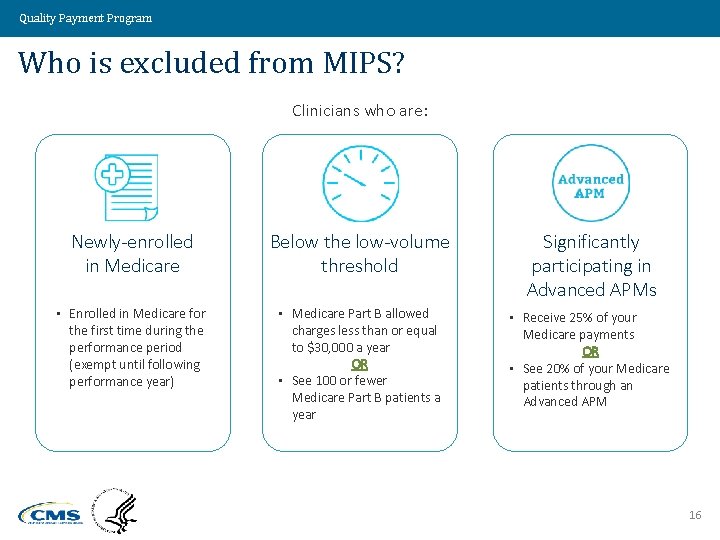
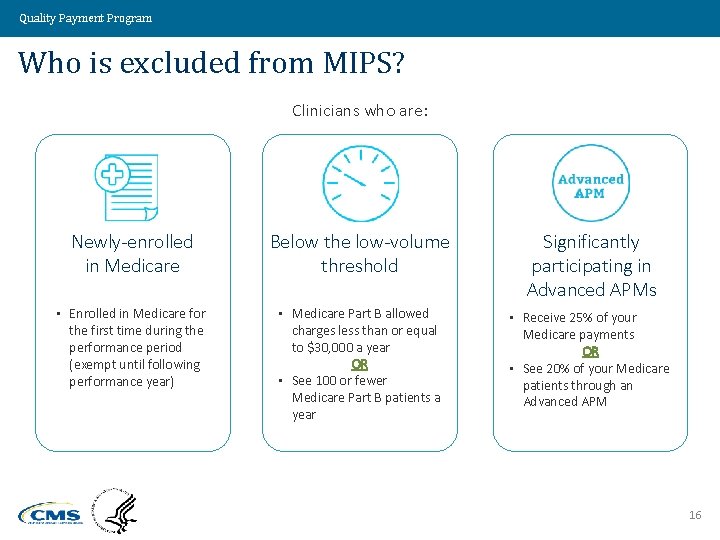
Quality Payment Program Who is excluded from MIPS? Clinicians who are: Newly-enrolled in Medicare Below the low-volume threshold Significantly participating in Advanced APMs • Enrolled in Medicare for the first time during the performance period (exempt until following performance year) • Medicare Part B allowed charges less than or equal to $30, 000 a year OR • See 100 or fewer Medicare Part B patients a year • Receive 25% of your Medicare payments OR • See 20% of your Medicare patients through an Advanced APM 16
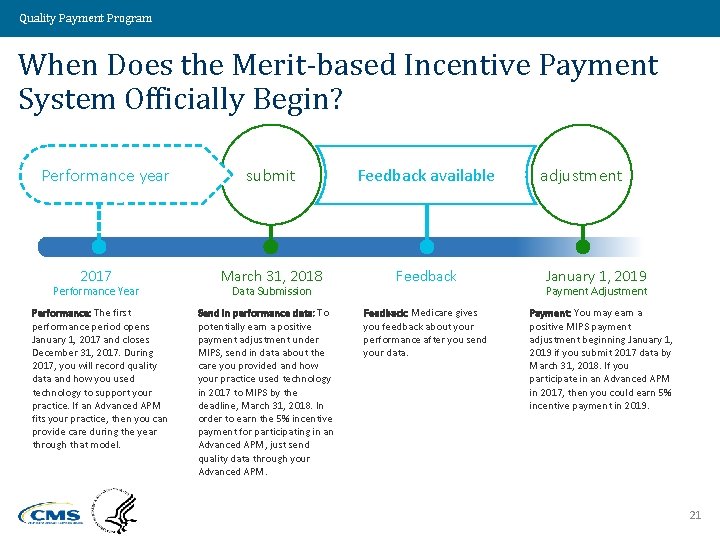
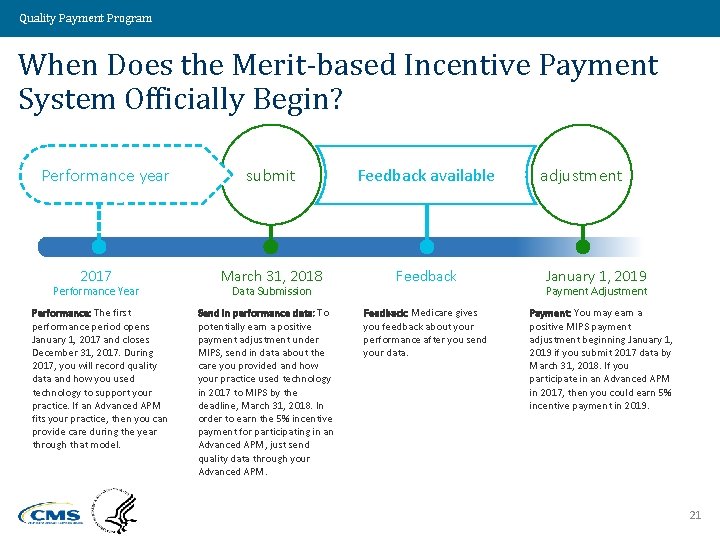
Quality Payment Program When Does the Merit-based Incentive Payment System Officially Begin? Performance year 2017 Performance Year Performance: The first performance period opens January 1, 2017 and closes December 31, 2017. During 2017, you will record quality data and how you used technology to support your practice. If an Advanced APM fits your practice, then you can provide care during the year through that model. submit Feedback available March 31, 2018 Feedback Data Submission Send in performance data: To potentially earn a positive payment adjustment under MIPS, send in data about the care you provided and how your practice used technology in 2017 to MIPS by the deadline, March 31, 2018. In order to earn the 5% incentive payment for participating in an Advanced APM, just send quality data through your Advanced APM. Feedback: Medicare gives you feedback about your performance after you send your data. adjustment January 1, 2019 Payment Adjustment Payment: You may earn a positive MIPS payment adjustment beginning January 1, 2019 if you submit 2017 data by March 31, 2018. If you participate in an Advanced APM in 2017, then you could earn 5% incentive payment in 2019. 21
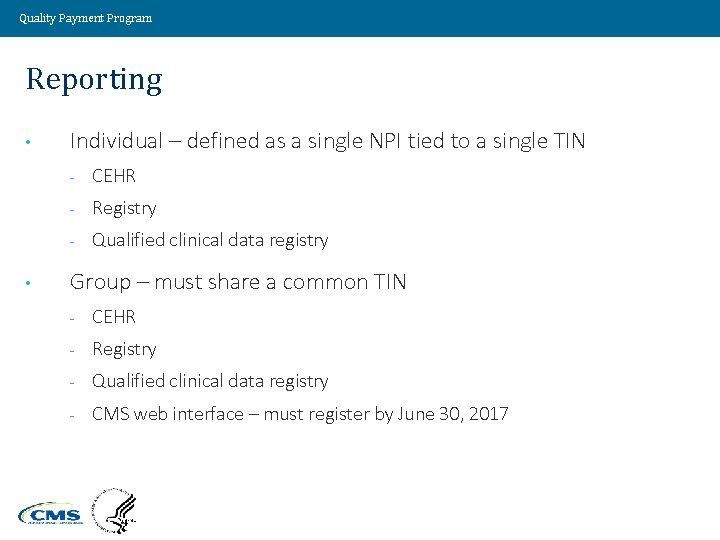
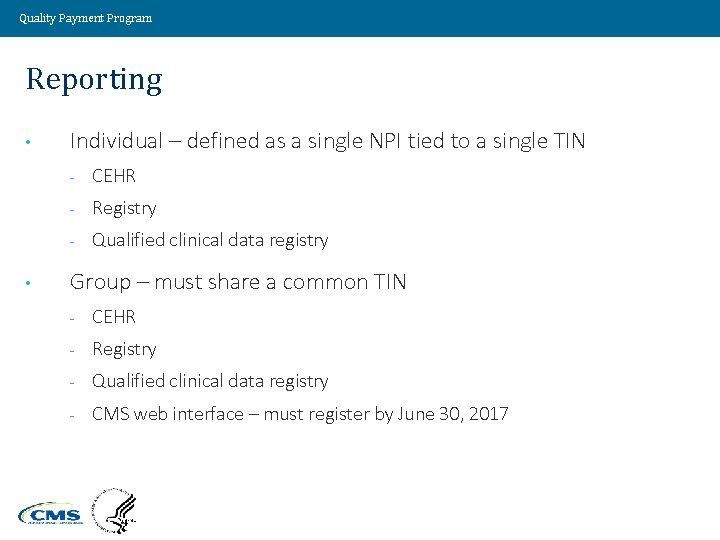
Quality Payment Program Reporting • • Individual – defined as a single NPI tied to a single TIN - CEHR - Registry - Qualified clinical data registry Group – must share a common TIN - CEHR - Registry - Qualified clinical data registry - CMS web interface – must register by June 30, 2017 Value Driven. Health Care. Solutions. 22
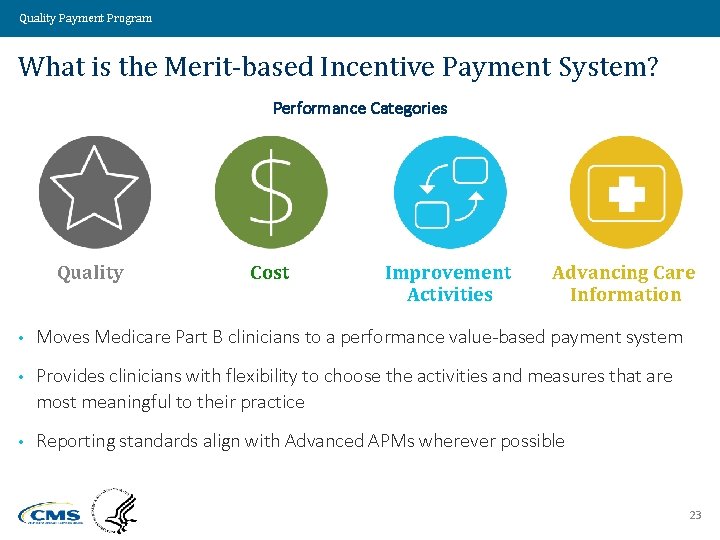
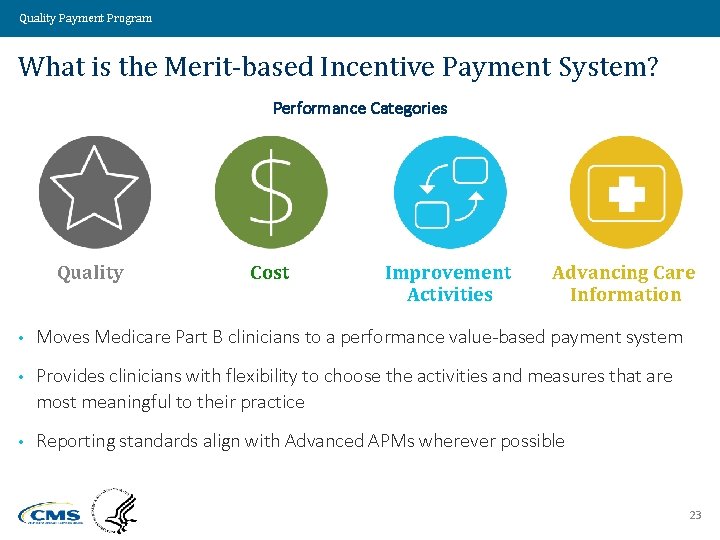
Quality Payment Program What is the Merit-based Incentive Payment System? Performance Categories Quality Cost Improvement Activities Advancing Care Information • Moves Medicare Part B clinicians to a performance value-based payment system • Provides clinicians with flexibility to choose the activities and measures that are most meaningful to their practice • Reporting standards align with Advanced APMs wherever possible 23
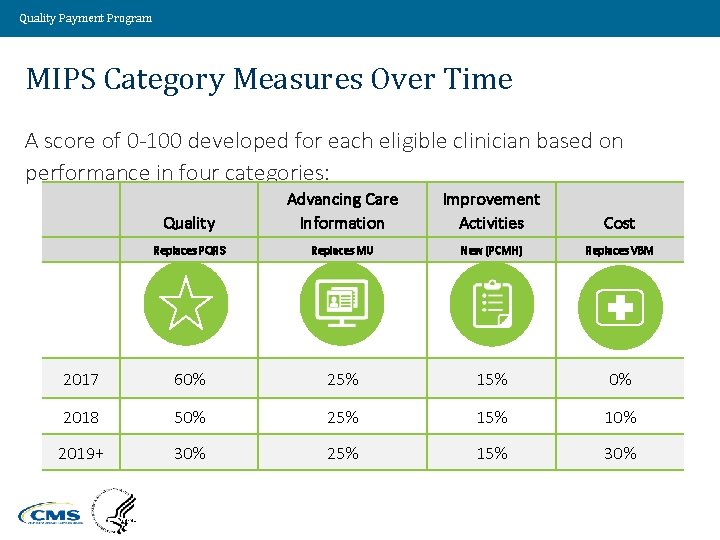
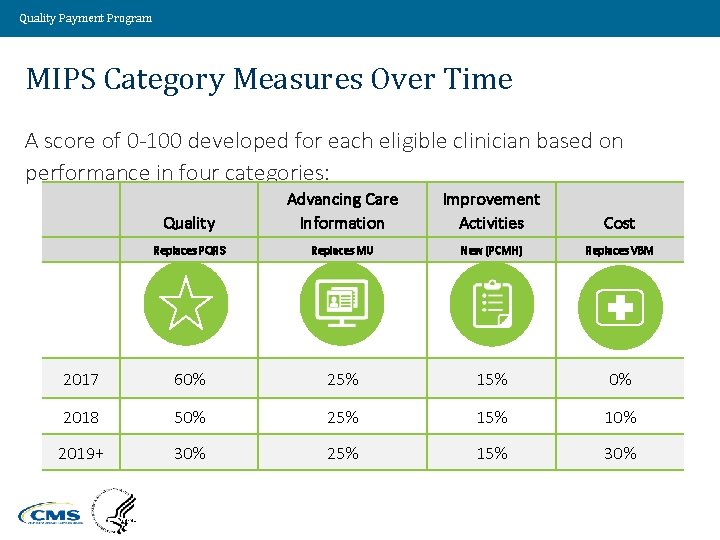
Quality Payment Program MIPS Category Measures Over Time A score of 0 -100 developed for each eligible clinician based on performance in four categories: Quality Advancing Care Information Improvement Activities Cost Replaces PQRS Replaces MU New (PCMH) Replaces VBM 2017 60% 25% 15% 0% 2018 50% 25% 10% 2019+ 30% 25% 15% 30% Value Driven. Health Care. Solutions. 24
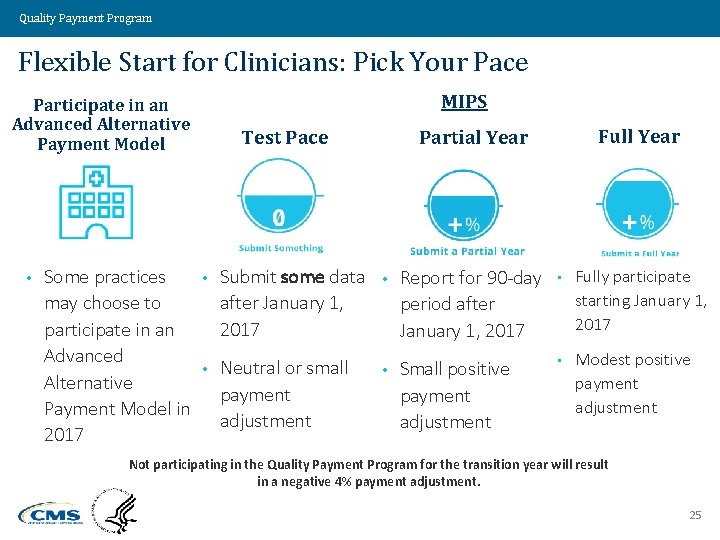
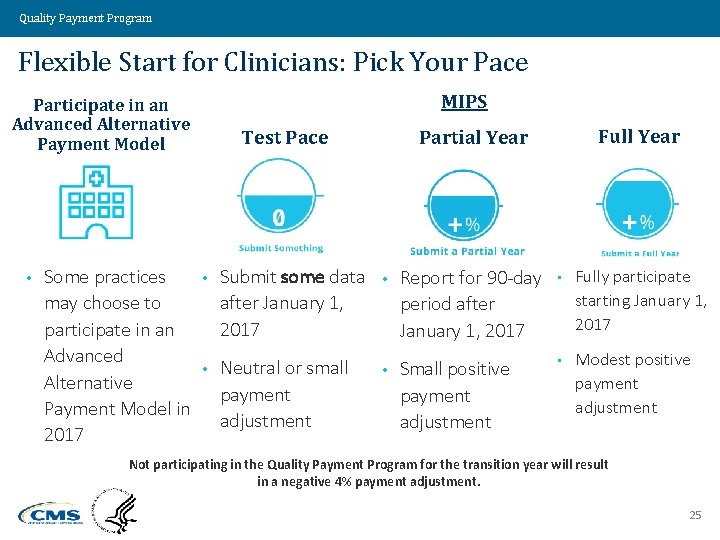
Quality Payment Program Flexible Start for Clinicians: Pick Your Pace MIPS Participate in an Advanced Alternative Payment Model • Some practices may choose to participate in an Advanced Alternative Payment Model in 2017 Test Pace Full Year Partial Year • Submit some data after January 1, 2017 • Report for 90 -day period after January 1, 2017 • Fully participate starting January 1, 2017 • Neutral or small payment adjustment • Small positive payment adjustment • Modest positive payment adjustment Not participating in the Quality Payment Program for the transition year will result in a negative 4% payment adjustment. 25
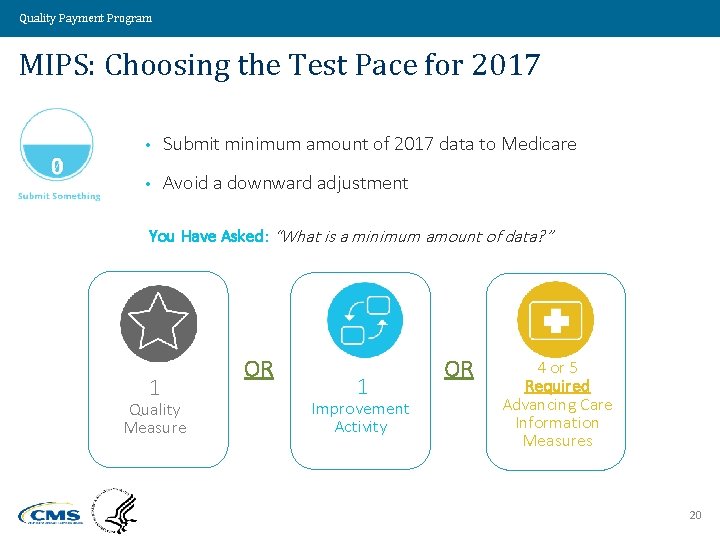
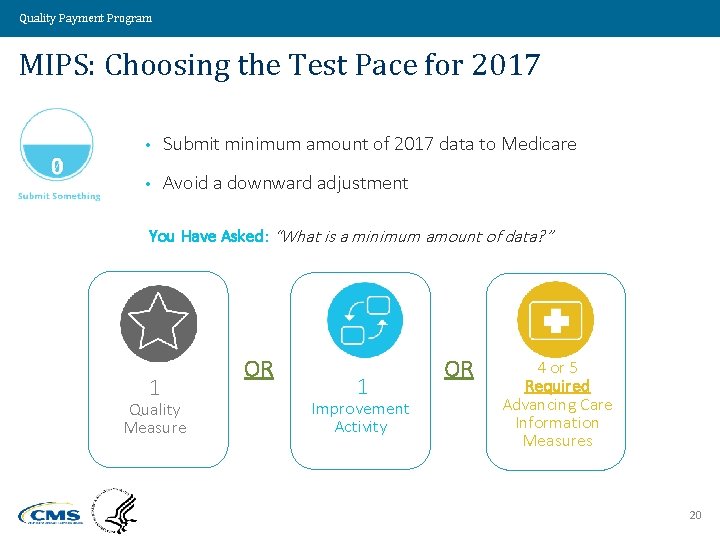
Quality Payment Program MIPS: Choosing the Test Pace for 2017 • Submit minimum amount of 2017 data to Medicare • Avoid a downward adjustment You Have Asked: “What is a minimum amount of data? ” 1 Quality Measure OR 1 Improvement Activity OR 4 or 5 Required Advancing Care Information Measures 20
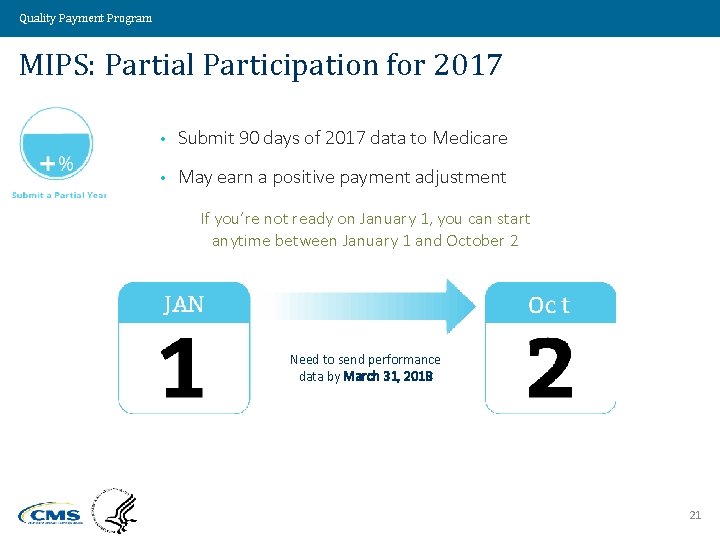
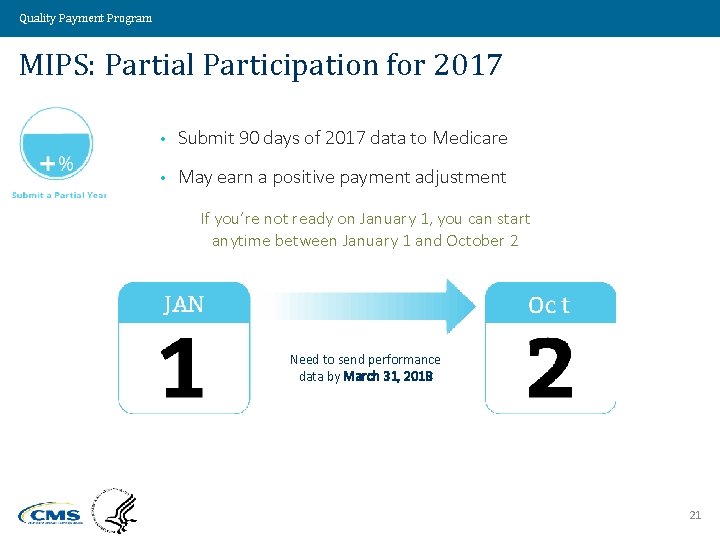
Quality Payment Program MIPS: Partial Participation for 2017 • Submit 90 days of 2017 data to Medicare • May earn a positive payment adjustment If you’re not ready on January 1, you can start anytime between January 1 and October 2 Need to send performance data by March 31, 2018 21
Quality Payment Program MIPS: Full Participation for 2017 • Submit a full year of 2017 data to Medicare • May earn a positive payment adjustment • Best way to earn largest payment adjustment is to submit data on all MIPS performance categories 22
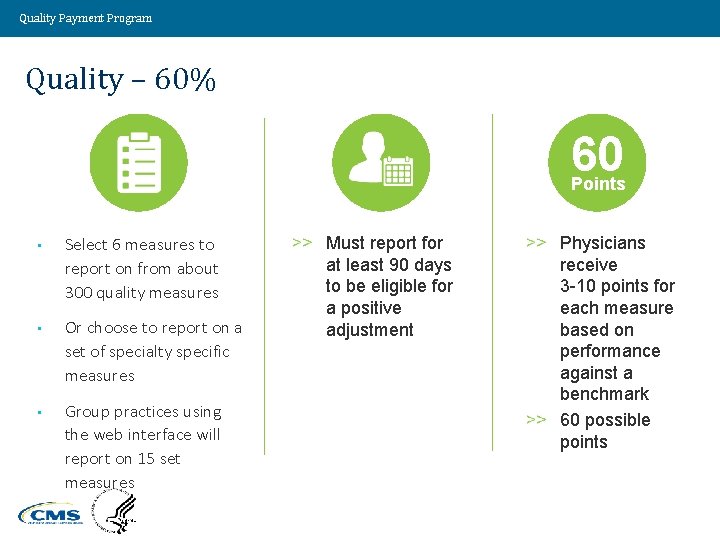
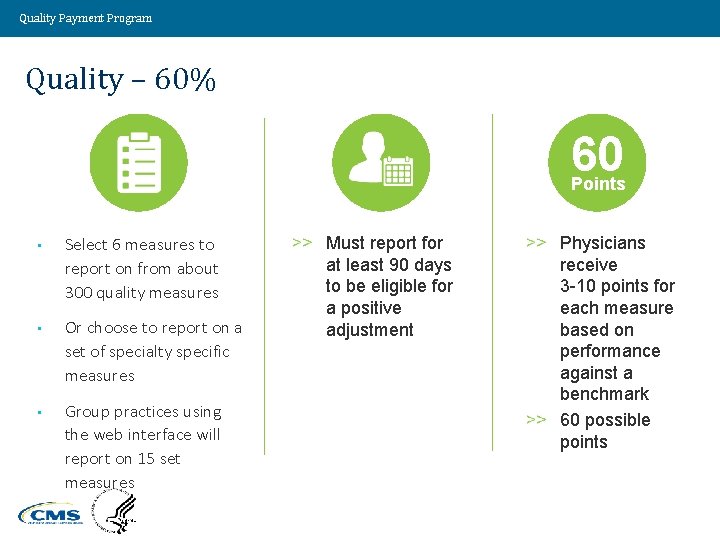
Quality Payment Program Quality – 60% 60 Points • Select 6 measures to report on from about 300 quality measures • Or choose to report on a set of specialty specific measures • Group practices using the web interface will report on 15 set measures Value Driven. Health Care. Solutions. Must report for at least 90 days to be eligible for a positive adjustment Physicians receive 3 -10 points for each measure based on performance against a benchmark 60 possible points 29
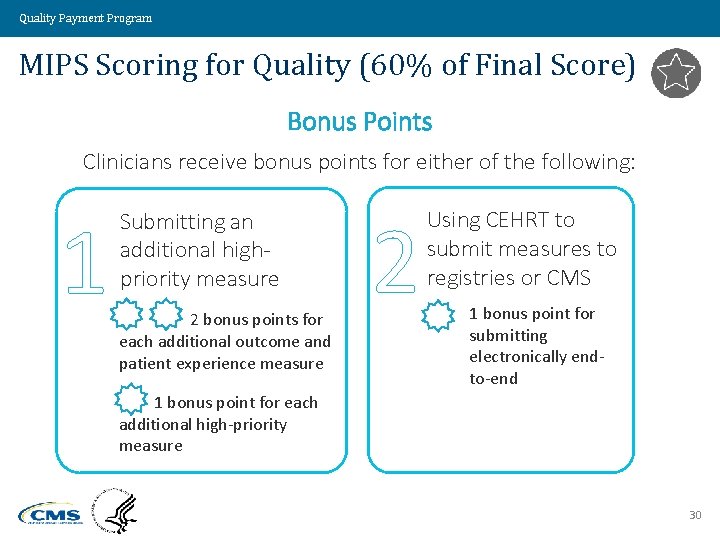
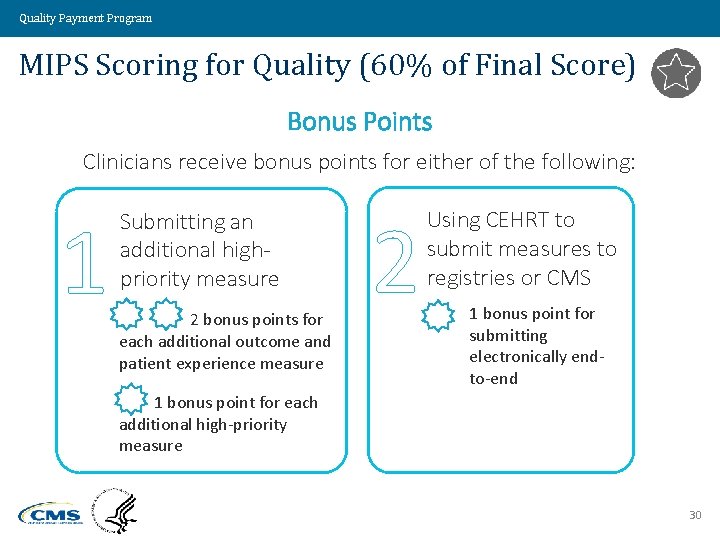
Quality Payment Program MIPS Scoring for Quality (60% of Final Score) Bonus Points Clinicians receive bonus points for either of the following: 1 Submitting an additional highpriority measure 2 bonus points for each additional outcome and patient experience measure 2 Using CEHRT to submit measures to registries or CMS 1 bonus point for submitting electronically endto-end 1 bonus point for each additional high-priority measure 30
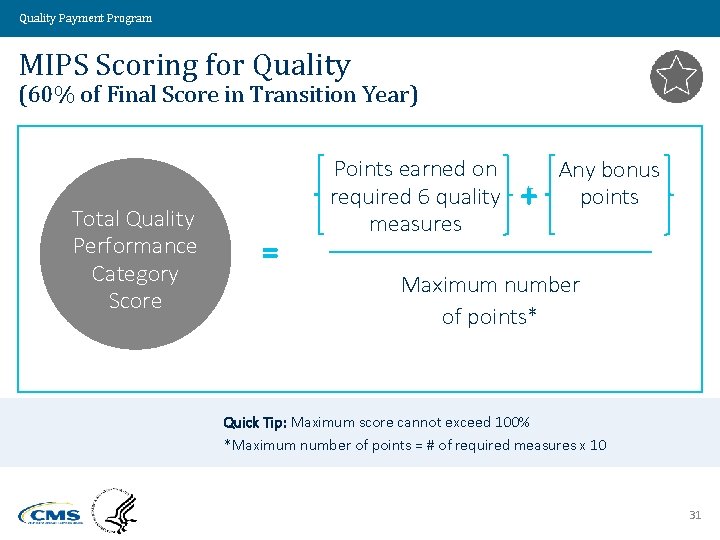
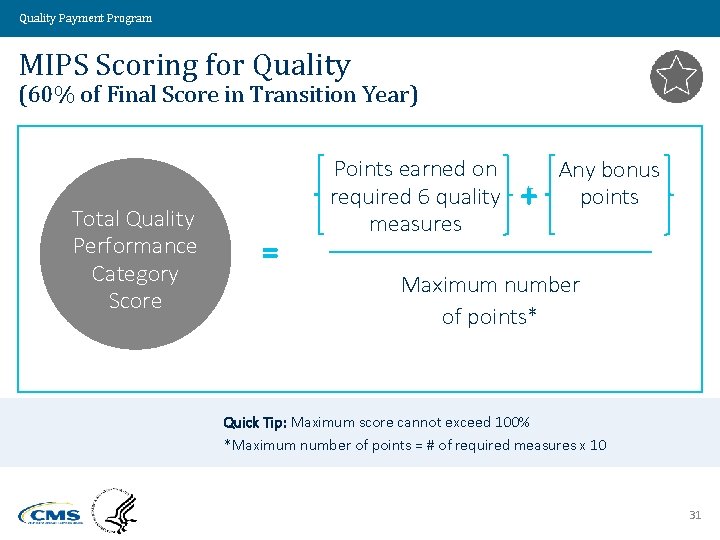
Quality Payment Program MIPS Scoring for Quality (60% of Final Score in Transition Year) Total Quality Performance Category Score = Points earned on required 6 quality measures + Any bonus points Maximum number of points* Quick Tip: Maximum score cannot exceed 100% *Maximum number of points = # of required measures x 10 31
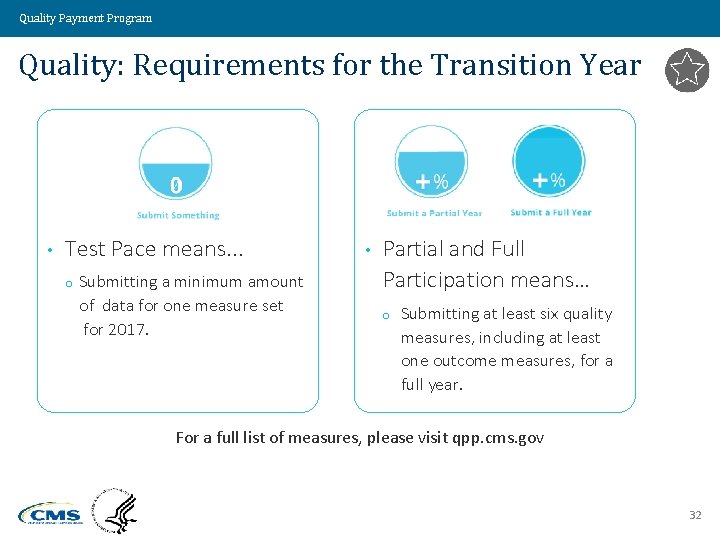
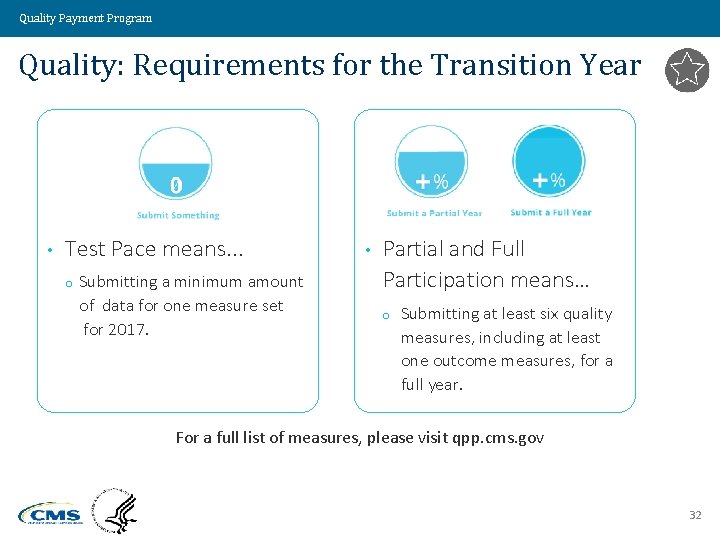
Quality Payment Program Quality: Requirements for the Transition Year • Test Pace means. . . o Submitting a minimum amount of data for one measure set for 2017. • Partial and Full Participation means… o Submitting at least six quality measures, including at least one outcome measures, for a full year. For a full list of measures, please visit qpp. cms. gov 32
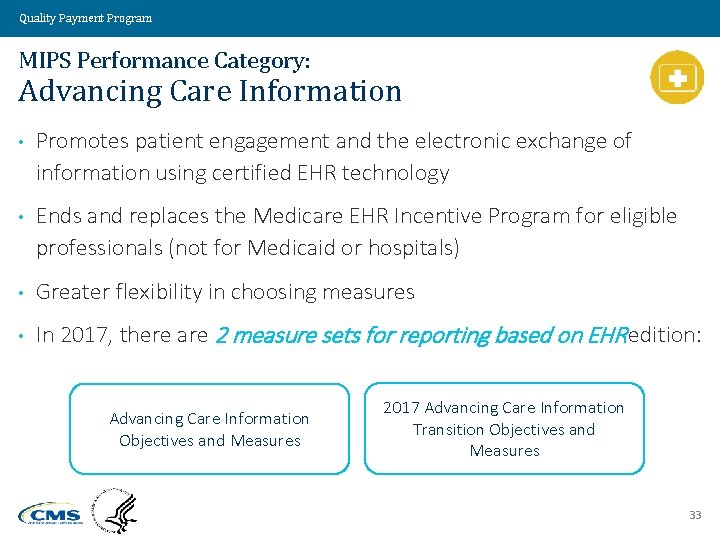
Quality Payment Program MIPS Performance Category: Advancing Care Information • Promotes patient engagement and the electronic exchange of information using certified EHR technology • Ends and replaces the Medicare EHR Incentive Program for eligible professionals (not for Medicaid or hospitals) • Greater flexibility in choosing measures • In 2017, there are 2 measure sets for reporting based on EHR edition: Advancing Care Information Objectives and Measures 2017 Advancing Care Information Transition Objectives and Measures 33
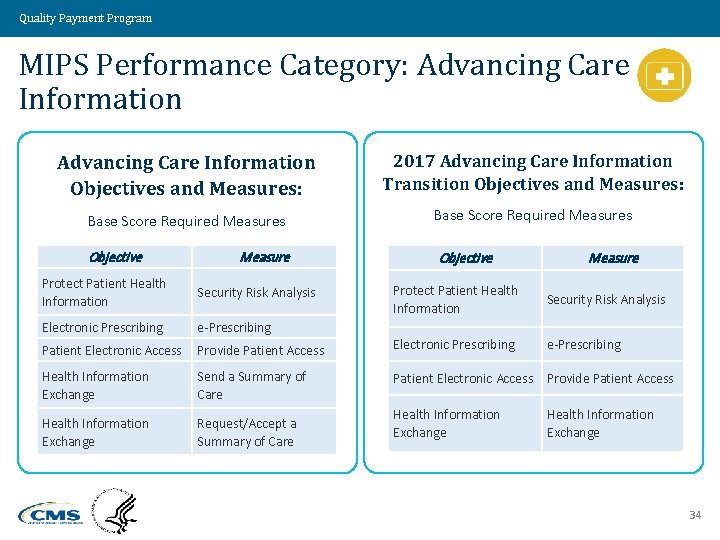
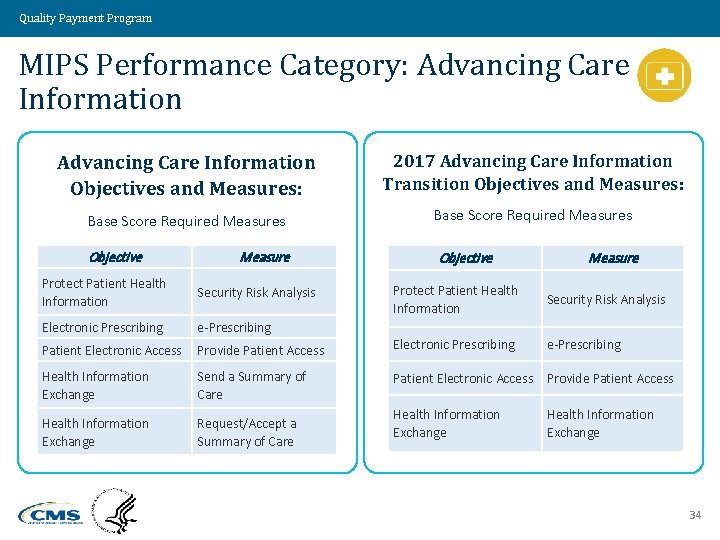
Quality Payment Program MIPS Performance Category: Advancing Care Information Objectives and Measures: 2017 Advancing Care Information Transition Objectives and Measures: Base Score Required Measures Objective Measure Protect Patient Health Information Security Risk Analysis Electronic Prescribing e-Prescribing Patient Electronic Access Objective Measure Protect Patient Health Information Security Risk Analysis Provide Patient Access Electronic Prescribing e-Prescribing Health Information Exchange Send a Summary of Care Patient Electronic Access Provide Patient Access Health Information Exchange Request/Accept a Summary of Care Health Information Exchange 34
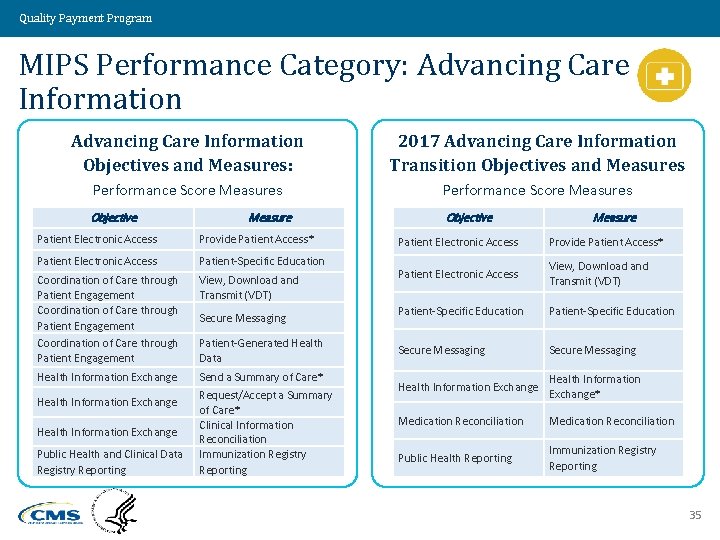
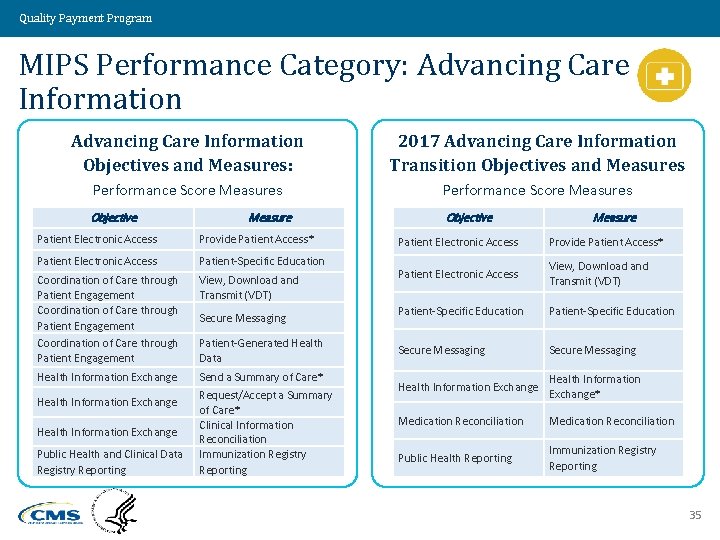
Quality Payment Program MIPS Performance Category: Advancing Care Information Objectives and Measures: 2017 Advancing Care Information Transition Objectives and Measures Performance Score Measures Objective Measure Patient Electronic Access Provide Patient Access* Patient Electronic Access Patient-Specific Education Coordination of Care through Patient Engagement View, Download and Transmit (VDT) Health Information Exchange Send a Summary of Care* Request/Accept a Summary of Care* Clinical Information Reconciliation Immunization Registry Reporting Health Information Exchange Public Health and Clinical Data Registry Reporting Secure Messaging Patient-Generated Health Data Measure Patient Electronic Access Provide Patient Access* Patient Electronic Access View, Download and Transmit (VDT) Patient-Specific Education Secure Messaging Health Information Exchange* Medication Reconciliation Public Health Reporting Immunization Registry Reporting 35
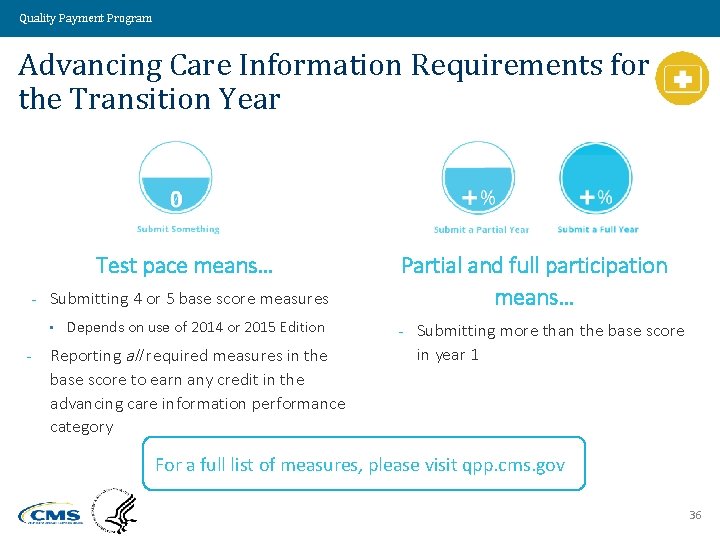
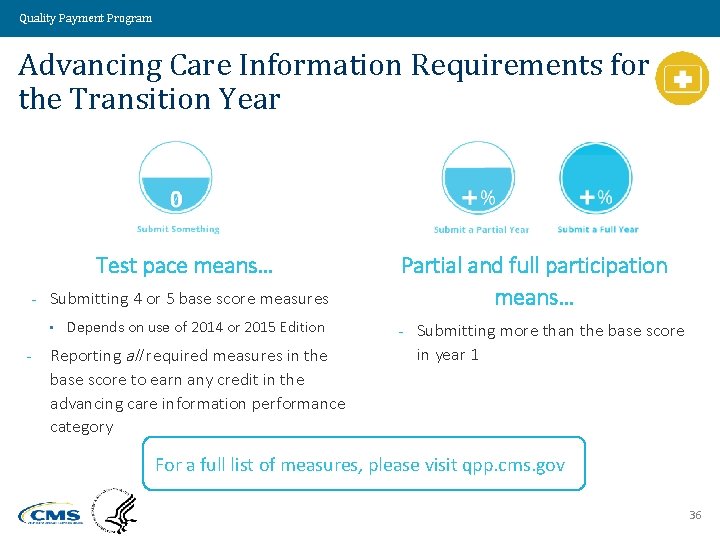
Quality Payment Program Advancing Care Information Requirements for the Transition Year Test pace means… - Submitting 4 or 5 base score measures • - Depends on use of 2014 or 2015 Edition Reporting all required measures in the base score to earn any credit in the advancing care information performance category Partial and full participation means… - Submitting more than the base score in year 1 For a full list of measures, please visit qpp. cms. gov 36
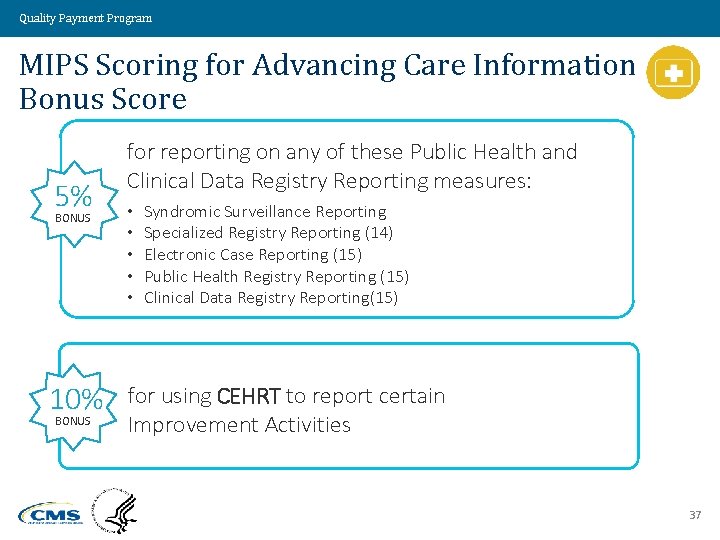
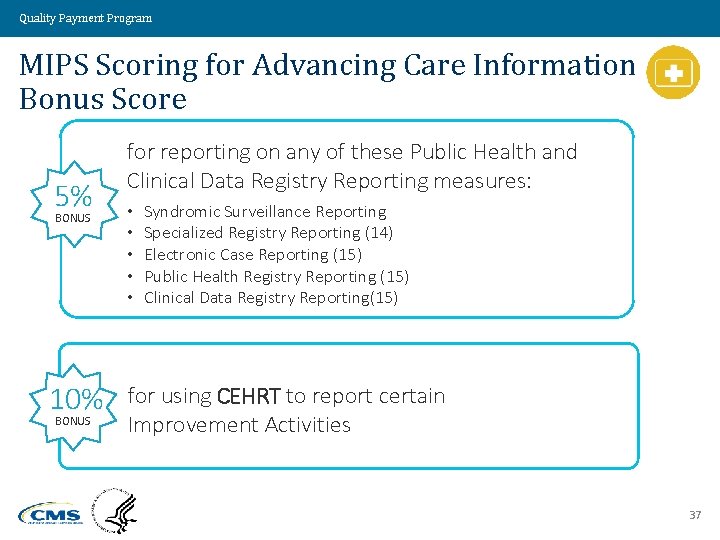
Quality Payment Program MIPS Scoring for Advancing Care Information Bonus Score 5% BONUS 10% BONUS for reporting on any of these Public Health and Clinical Data Registry Reporting measures: • • • Syndromic Surveillance Reporting Specialized Registry Reporting (14) Electronic Case Reporting (15) Public Health Registry Reporting (15) Clinical Data Registry Reporting(15) for using CEHRT to report certain Improvement Activities 37
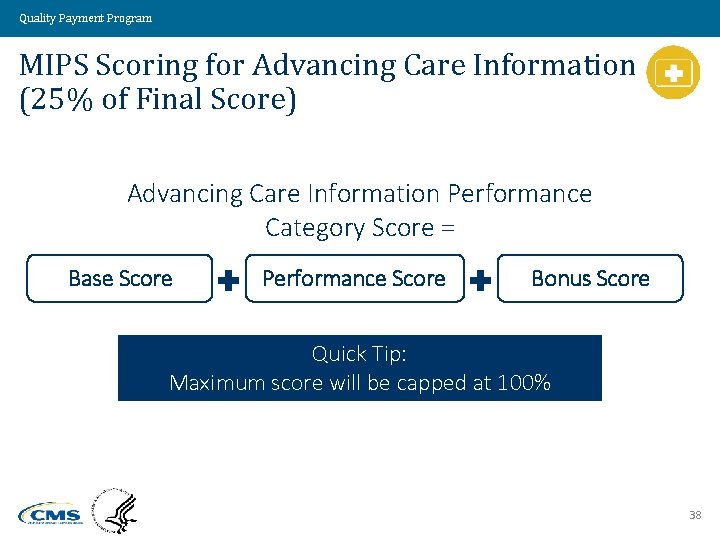
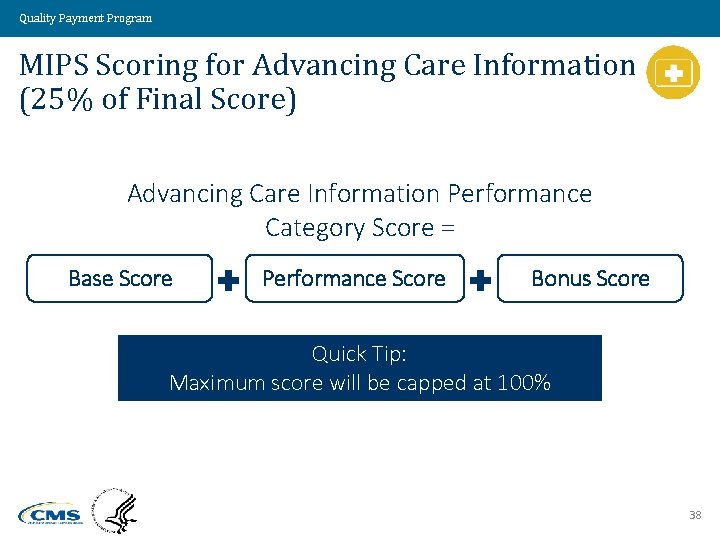
Quality Payment Program MIPS Scoring for Advancing Care Information (25% of Final Score) Advancing Care Information Performance Category Score = Base Score Performance Score Bonus Score Quick Tip: Maximum score will be capped at 100% 38
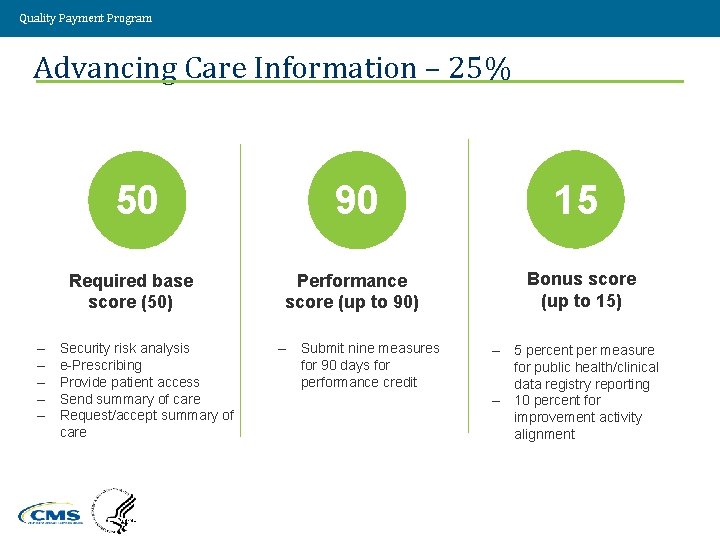
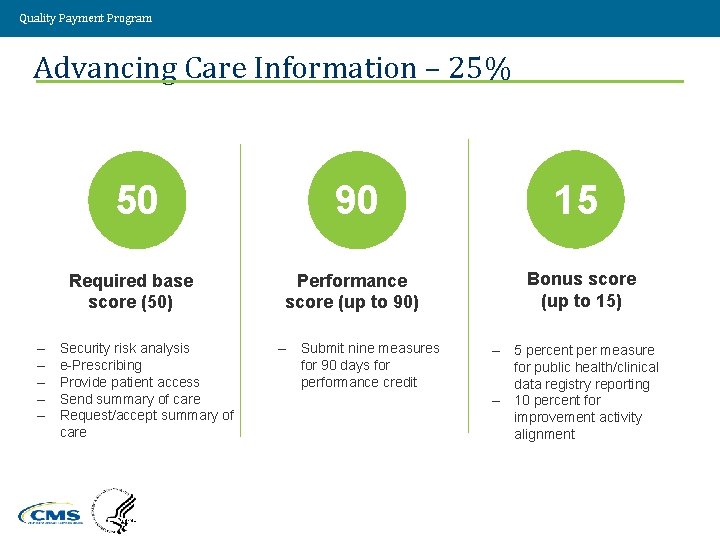
Quality Payment Program Advancing Care Information – 25% 50 Required base score (50) – – – Security risk analysis e-Prescribing Provide patient access Send summary of care Request/accept summary of care Value Driven. Health Care. Solutions. 90 Performance score (up to 90) – Submit nine measures for 90 days for performance credit 15 Bonus score (up to 15) – 5 percent per measure for public health/clinical data registry reporting – 10 percent for improvement activity alignment 39
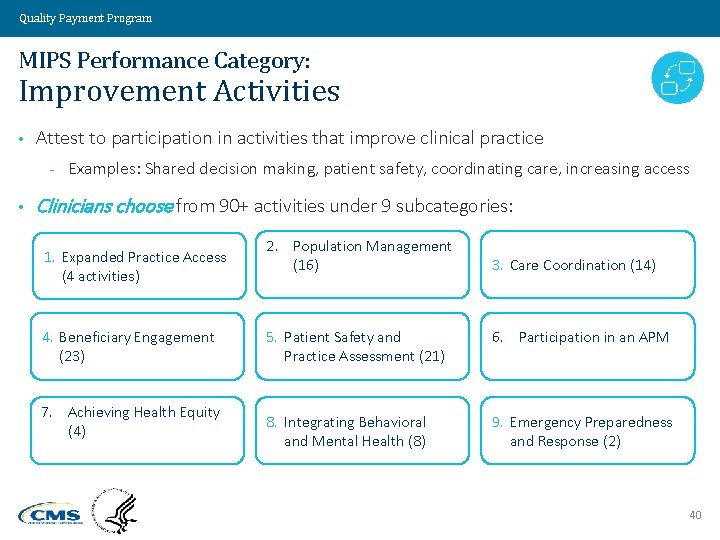
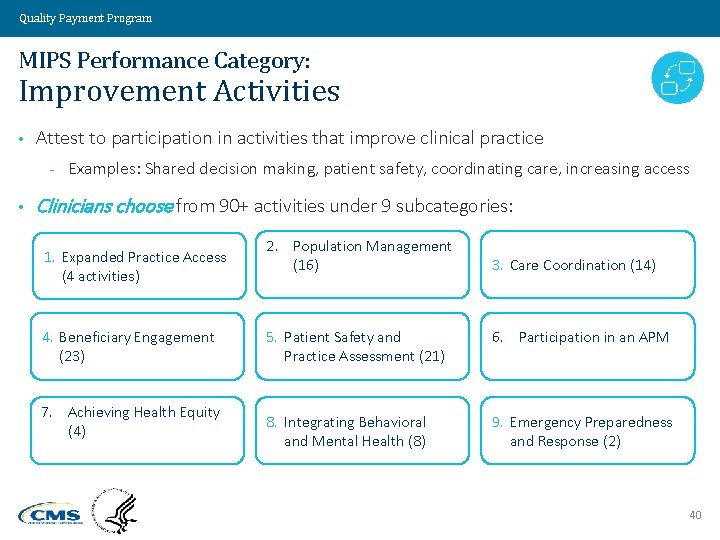
Quality Payment Program MIPS Performance Category: Improvement Activities • Attest to participation in activities that improve clinical practice - • Examples: Shared decision making, patient safety, coordinating care, increasing access Clinicians choose from 90+ activities under 9 subcategories: 1. Expanded Practice Access (4 activities) 4. Beneficiary Engagement (23) 7. Achieving Health Equity (4) 2. Population Management (16) 3. Care Coordination (14) 5. Patient Safety and Practice Assessment (21) 6. Participation in an APM 8. Integrating Behavioral and Mental Health (8) 9. Emergency Preparedness and Response (2) 40

Quality Payment Program Examples of Improvement Activities Same day appointments Extended office hours Value Driven. Health Care. Solutions. After hours access to care Test tracking system 41
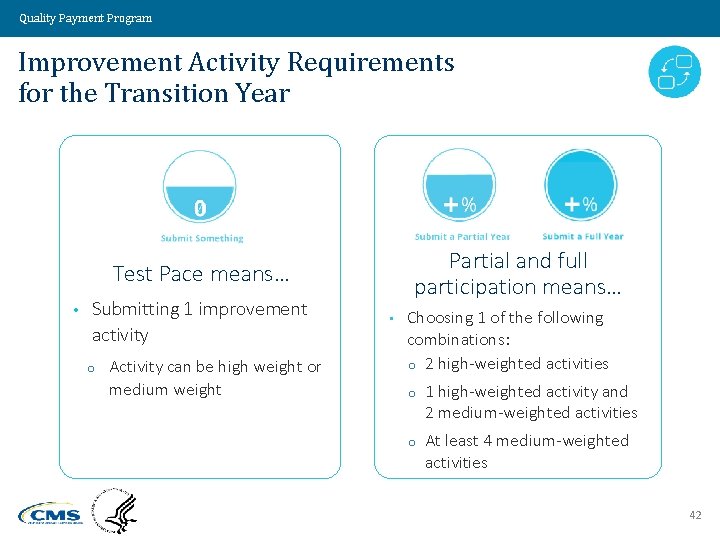
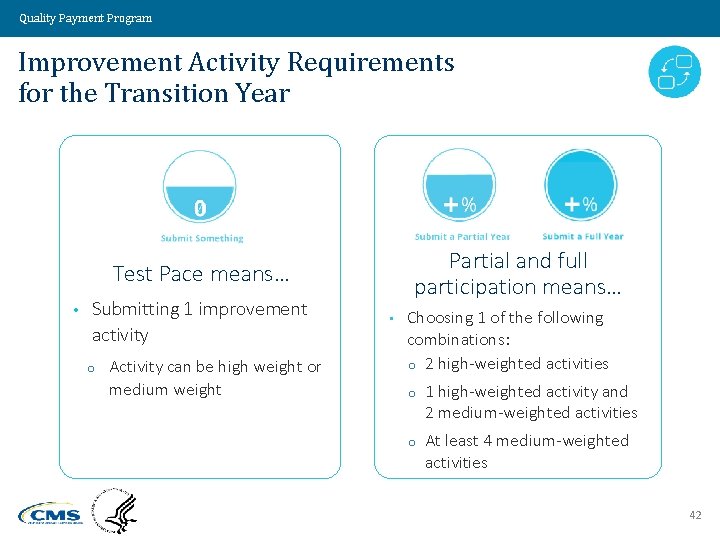
Quality Payment Program Improvement Activity Requirements for the Transition Year Partial and full participation means… Test Pace means… • Submitting 1 improvement activity o Activity can be high weight or medium weight • Choosing 1 of the following combinations: o 2 high-weighted activities o 1 high-weighted activity and 2 medium-weighted activities o At least 4 medium-weighted activities 42
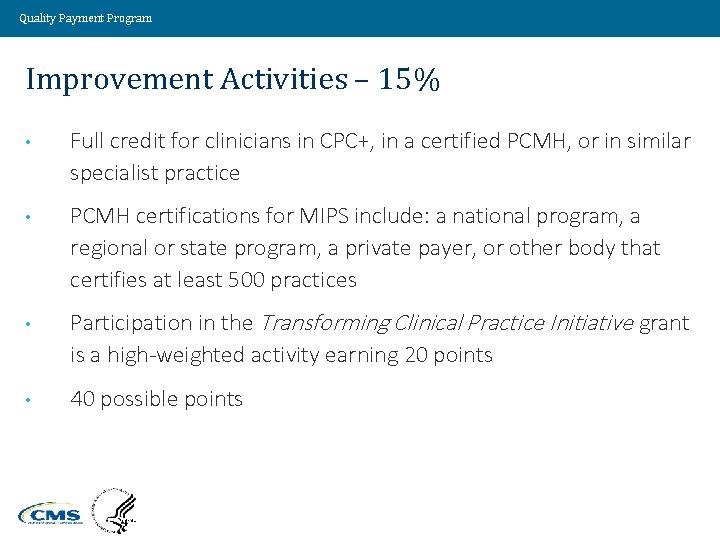
Quality Payment Program Improvement Activities – 15% • Full credit for clinicians in CPC+, in a certified PCMH, or in similar specialist practice • PCMH certifications for MIPS include: a national program, a regional or state program, a private payer, or other body that certifies at least 500 practices • Participation in the Transforming Clinical Practice Initiative grant is a high-weighted activity earning 20 points • 40 possible points Value Driven. Health Care. Solutions. 43
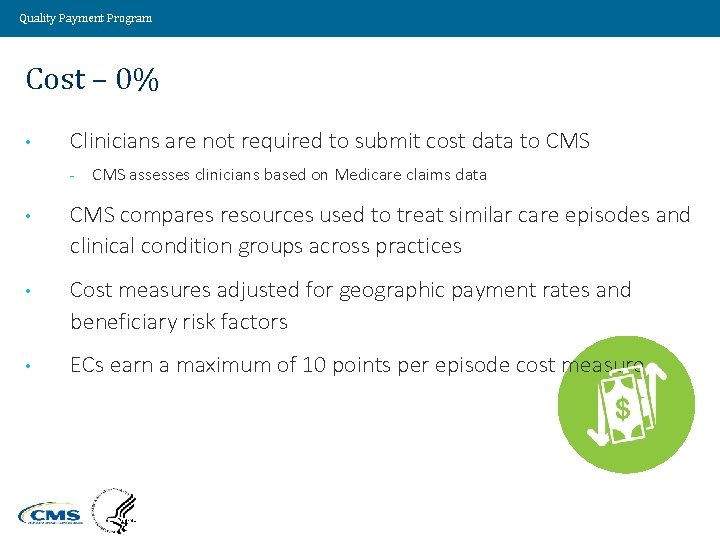
Quality Payment Program Cost – 0% • Clinicians are not required to submit cost data to CMS - CMS assesses clinicians based on Medicare claims data • CMS compares resources used to treat similar care episodes and clinical condition groups across practices • Cost measures adjusted for geographic payment rates and beneficiary risk factors • ECs earn a maximum of 10 points per episode cost measure Value Driven. Health Care. Solutions. 44
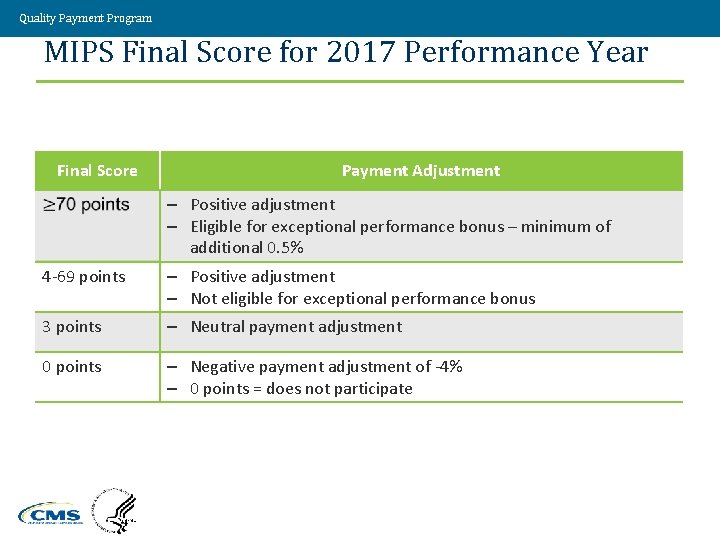
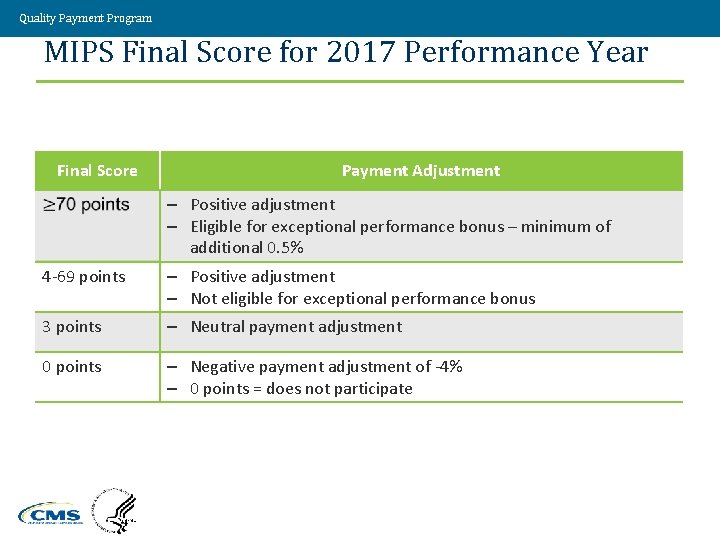
Quality Payment Program MIPS Final Score for 2017 Performance Year Final Score Payment Adjustment – Positive adjustment – Eligible for exceptional performance bonus – minimum of additional 0. 5% 4 -69 points – Positive adjustment – Not eligible for exceptional performance bonus 3 points – Neutral payment adjustment 0 points – Negative payment adjustment of -4% – 0 points = does not participate Value Driven. Health Care. Solutions. 45
Quality Payment Program Additional Incentive Payments and Support • • For 2019 -2024, maximum of $500 million per year in additional incentive payments may be available to distribute to ECs who have “exceptional performance” - Final score of 70 or higher qualifies for an additional payment in 2017 (2019 payment year) - Not budget neutral Technical support for small and rural practices Value Driven. Health Care. Solutions. 46
Quality Payment Program Performance Adjustments After 2017 • CMS will publish a “performance threshold” score at the start of each year • Each EC’s final score compared to the performance threshold score • No MIPS adjustment made to ECs with a score exactly at threshold • ECs with a score below threshold receive a negative payment adjustment • ECs with a score above threshold receive a positive payment adjustment factor Value Driven. Health Care. Solutions. 47
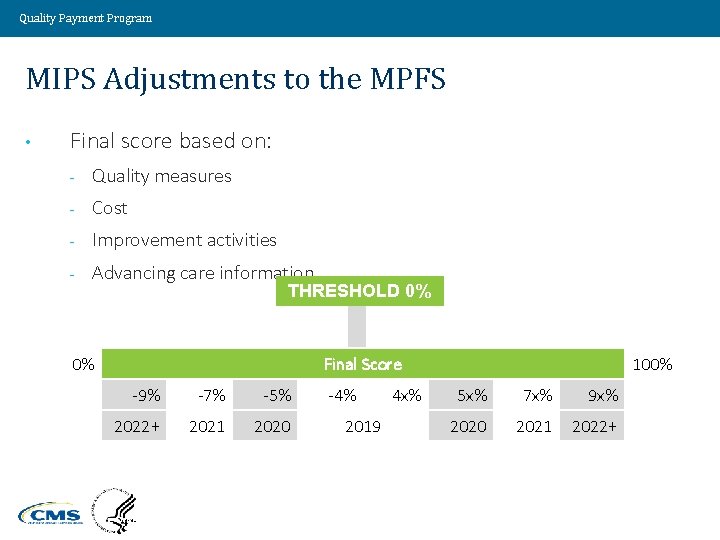
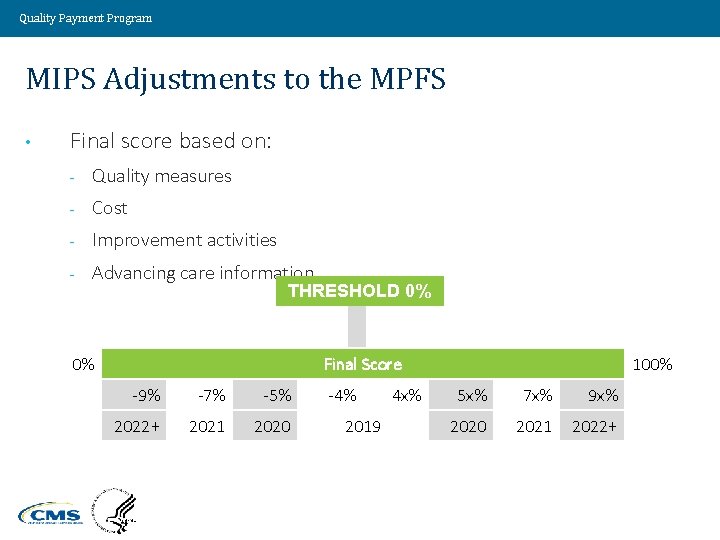
Quality Payment Program MIPS Adjustments to the MPFS • Final score based on: - Quality measures - Cost - Improvement activities - Advancing care information THRESHOLD 0% 0% Final Score -9% -7% -5% 2022+ 2021 2020 Value Driven. Health Care. Solutions. -4% 2019 4 x% 100% 5 x% 7 x% 9 x% 2020 2021 2022+ 48
Quality Payment Program Budget Neutrality >> Amounts accrued from penalties assessed against ECs with scores below the threshold will fund payments for ECs with scores above threshold Value Driven. Health Care. Solutions. 49
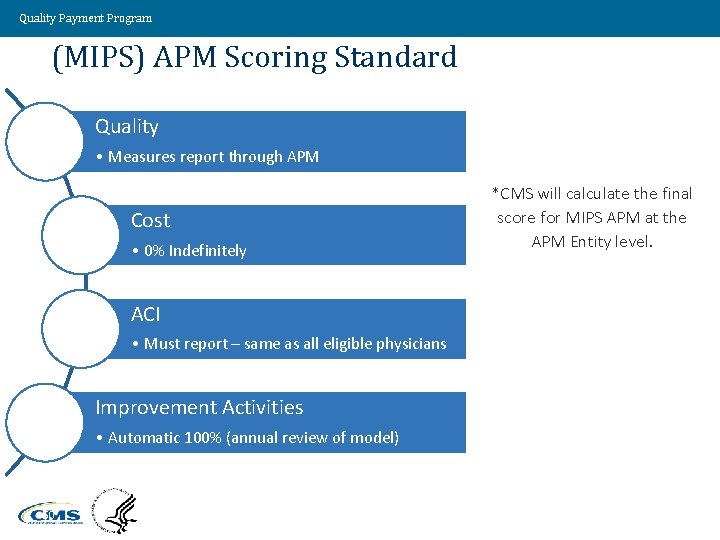
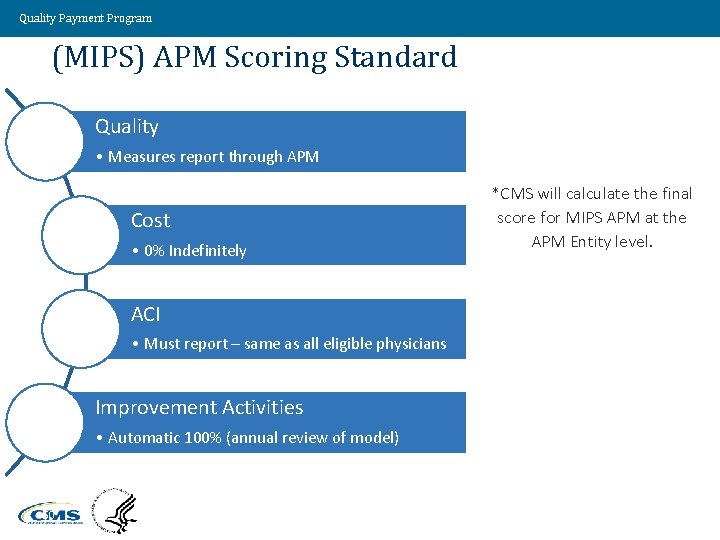
Quality Payment Program (MIPS) APM Scoring Standard Quality • Measures report through APM Cost • 0% Indefinitely ACI • Must report – same as all eligible physicians Improvement Activities • Automatic 100% (annual review of model) 50 *CMS will calculate the final score for MIPS APM at the APM Entity level.
Quality Payment Program Physician Compare Website • MIPS composite scores and individual performance category scores available on the CMS Physician Compare website • Patients can see health care providers rated on a scale of 0 to 100 and how physician compares to peers nationally Value Driven. Health Care. Solutions. 51
Quality Payment Program Thank You!!! Questions? ? ? paulfcc@aol. com pmartin@ketteringhealth. org
Quality Payment Program
Quality Payment Program