PAYMENT REFORM THE QUALITY INCENTIVE PAYMENT SYSTEM Kenneth
- Slides: 24
PAYMENT REFORM: THE QUALITY INCENTIVE PAYMENT SYSTEM Kenneth Goldblum, M. D.
Goals of P 4 P Improve quality (but is this quality? ) Reduce costs (does it? ) Enhance physician income without incenting utilization Serve as a check on utilization based reimbursement systems like ACO’s
Design Features Can incent processes or outcomes or behaviors (pay for participation) Can incent specific outcome measures but goals can be a moving target Can incent performance relative to group Can incent improvement Can use thresholds or graded approaches Can use single measures or composites Adjustments for small numbers/ practice aggregation
Issues What are the goals? Payer designed or doctor designed? How much of physician income is in play? What fraction of patients are involved? PCP versus specialist versus hospital Risk adjustment Patient demographics, allocation and other patient related issues Transparency/use of results?
Unintended Consequences Less emphasis on patient goals Avoidance of high risk or non adherent patients Excess focus on targeted measures to exclusion of other important care elements
RMMC 180 private practice Primary Care Doctor network in the four Philadelphia suburban counties in Pennsylvania. Designed and administered our own P 4 P program since 2001 Component of an arrangement with a large payer that supports infrastructure and has sharing of cost savings as another component
RMMC Enhancement Program Continues to evolve over time Physician designed and administered Goals are quality improvement, cost reduction, and physician income enhancement Incents both processes and outcomes Uses single and composite measures Rising bars with approaching ceilings?
Program Supports Organizational infrastructure Patient support via telephone calls from RMMC nurses Quality Improvement doctors in each practice Physician peer mentoring Learning Sessions for doctors and staff Reimbursed regional physician meetings with data sharing Web based tool for tracking and reporting
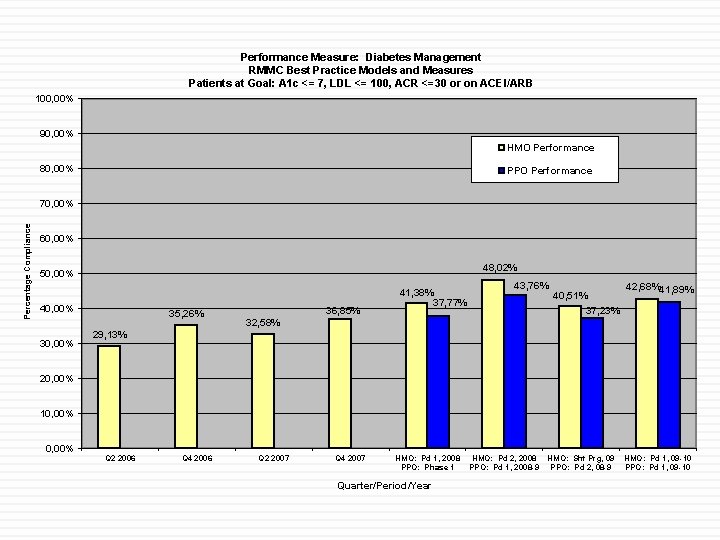
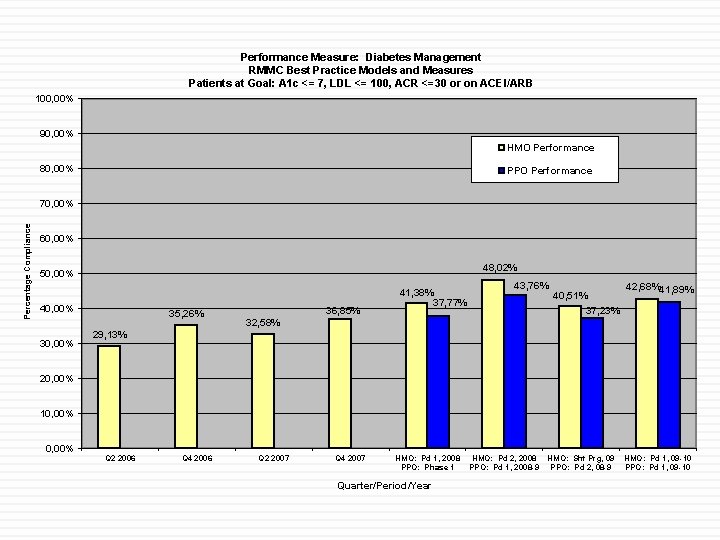
Performance Measure: Diabetes Management RMMC Best Practice Models and Measures Patients at Goal: A 1 c <= 7, LDL <= 100, ACR <=30 or on ACEI/ARB 100, 00% 90, 00% HMO Performance 80, 00% PPO Performance Percentage Compliance 70, 00% 60, 00% 48, 02% 50, 00% 40, 00% 35, 26% 36, 85% 41, 38% 37, 77% 43, 76% 40, 51% 37, 23% 42, 68%41, 89% 32, 58% 29, 13% 20, 00% 10, 00% Q 2 2006 Q 4 2006 Q 2 2007 Q 4 2007 HMO: Pd 1, 2008 PPO: Phase 1 Quarter/Period/Year HMO: Pd 2, 2008 PPO: Pd 1, 2008 -9 HMO: Sht Prg, 09 PPO: Pd 2, 08 -9 HMO: Pd 1, 09 -10 PPO: Pd 1, 09 -10
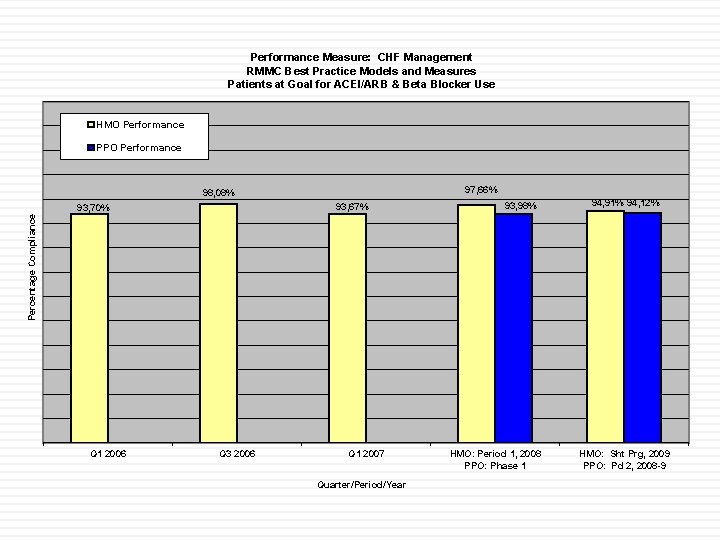
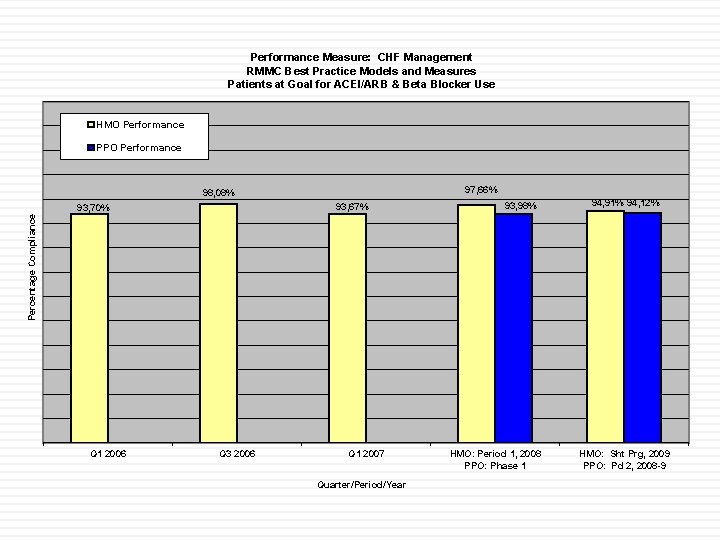
Performance Measure: CHF Management RMMC Best Practice Models and Measures Patients at Goal for ACEI/ARB & Beta Blocker Use HMO Performance PPO Performance 97, 66% 98, 08% 93, 67% 93, 98% 94, 91% 94, 12% Percentage Compliance 93, 70% Q 1 2006 Q 3 2006 Q 1 2007 Quarter/Period/Year HMO: Period 1, 2008 PPO: Phase 1 HMO: Sht Prg, 2009 PPO: Pd 2, 2008 -9
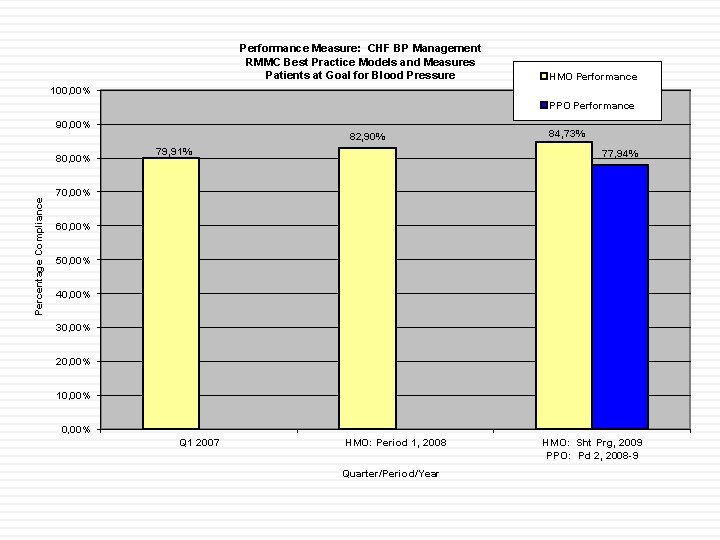
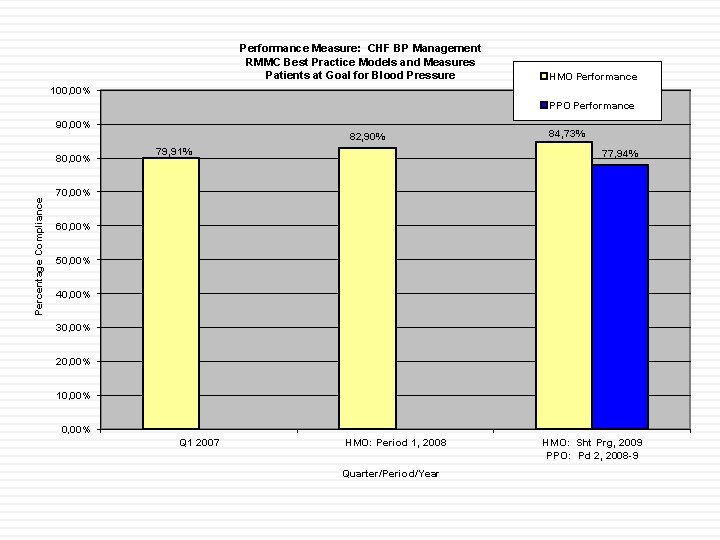
Performance Measure: CHF BP Management RMMC Best Practice Models and Measures Patients at Goal for Blood Pressure HMO Performance 100, 00% PPO Performance 90, 00% 82, 90% Percentage Compliance 80, 00% 79, 91% 84, 73% 77, 94% 70, 00% 60, 00% 50, 00% 40, 00% 30, 00% 20, 00% 10, 00% Q 1 2007 HMO: Period 1, 2008 Quarter/Period/Year HMO: Sht Prg, 2009 PPO: Pd 2, 2008 -9
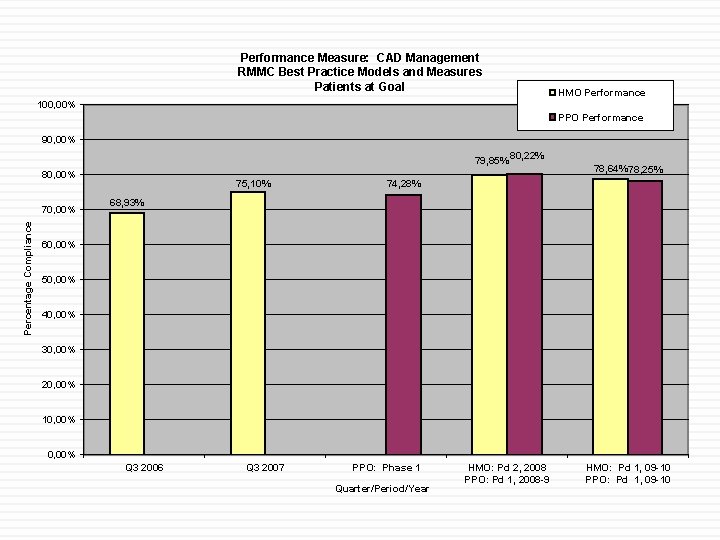
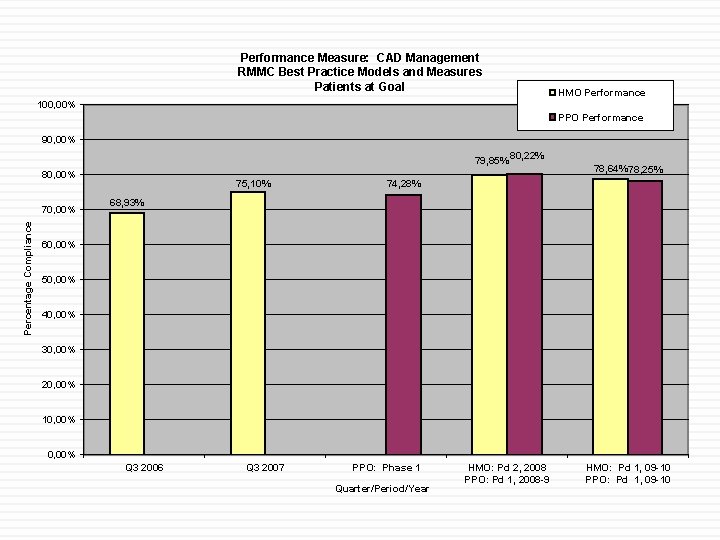
Performance Measure: CAD Management RMMC Best Practice Models and Measures Patients at Goal HMO Performance 100, 00% PPO Performance 90, 00% 79, 85% 80, 00% Percentage Compliance 70, 00% 75, 10% 80, 22% 78, 64% 78, 25% 74, 28% 68, 93% 60, 00% 50, 00% 40, 00% 30, 00% 20, 00% 10, 00% Q 3 2006 Q 3 2007 PPO: Phase 1 Quarter/Period/Year HMO: Pd 2, 2008 PPO: Pd 1, 2008 -9 HMO: Pd 1, 09 -10 PPO: Pd 1, 09 -10
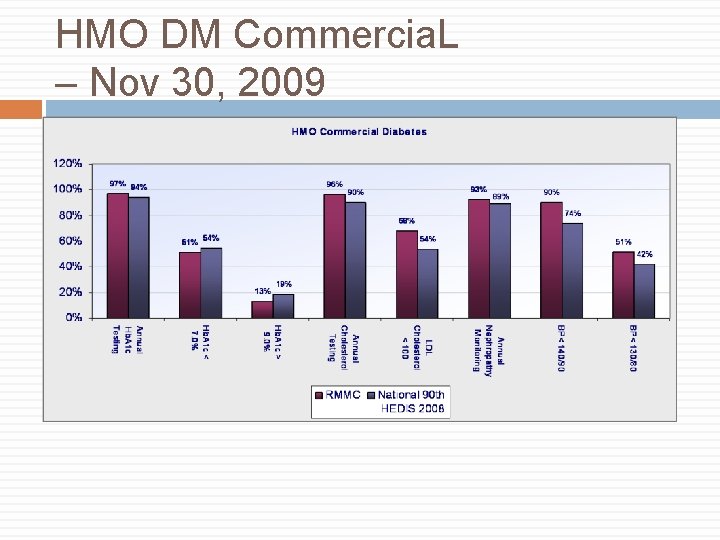
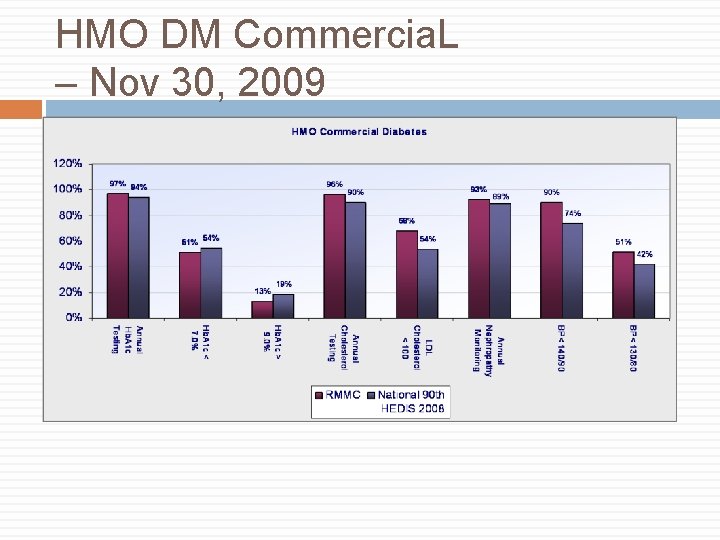
HMO DM Commercia. L – Nov 30, 2009
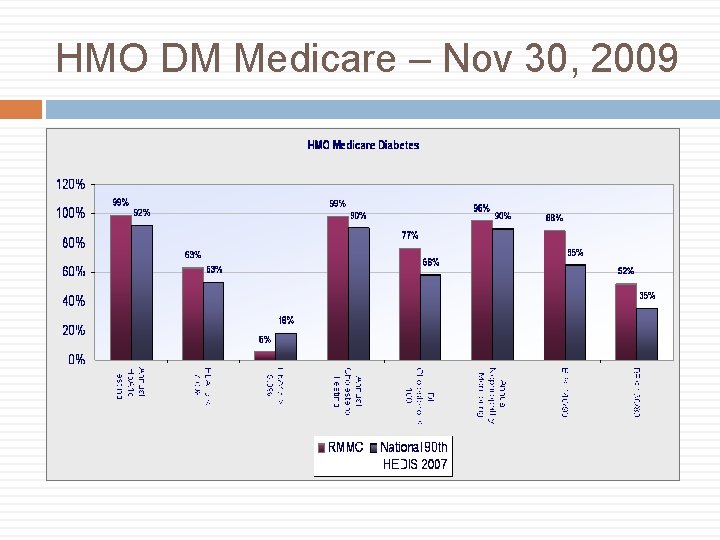
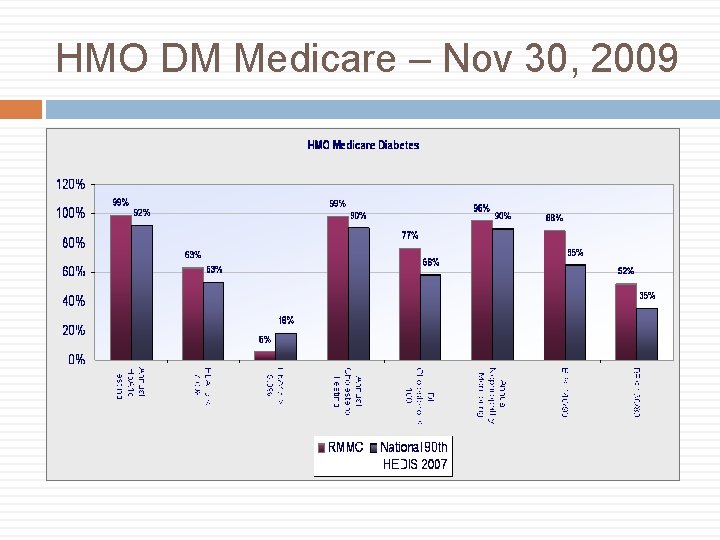
HMO DM Medicare – Nov 30, 2009
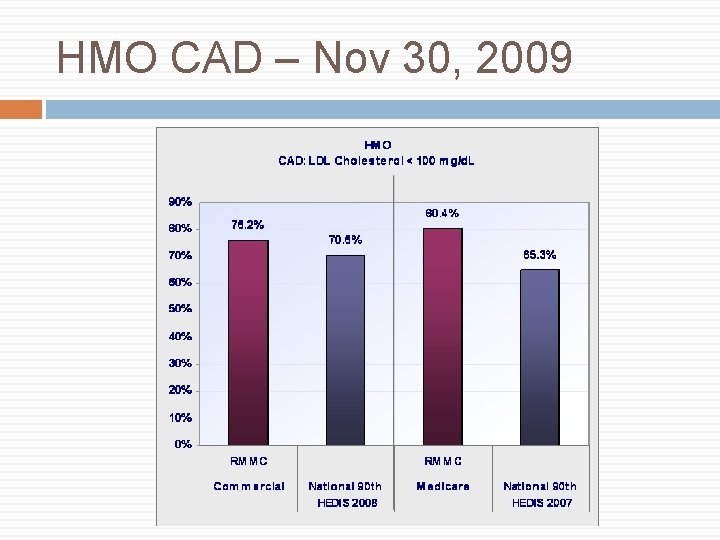
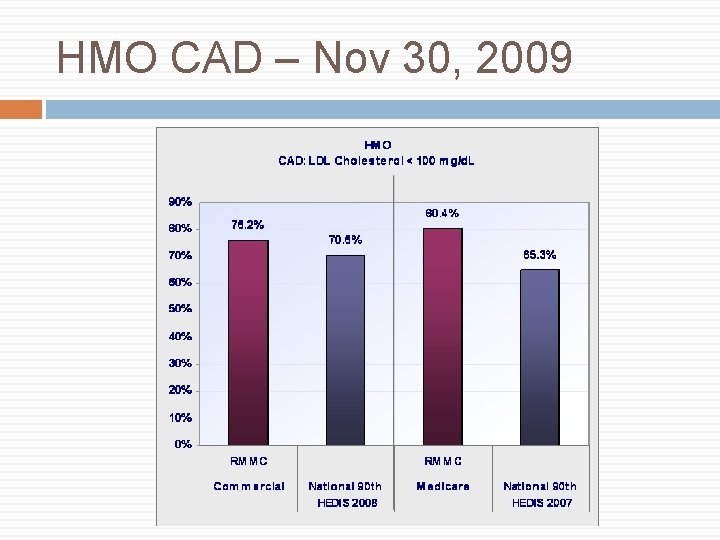
HMO CAD – Nov 30, 2009
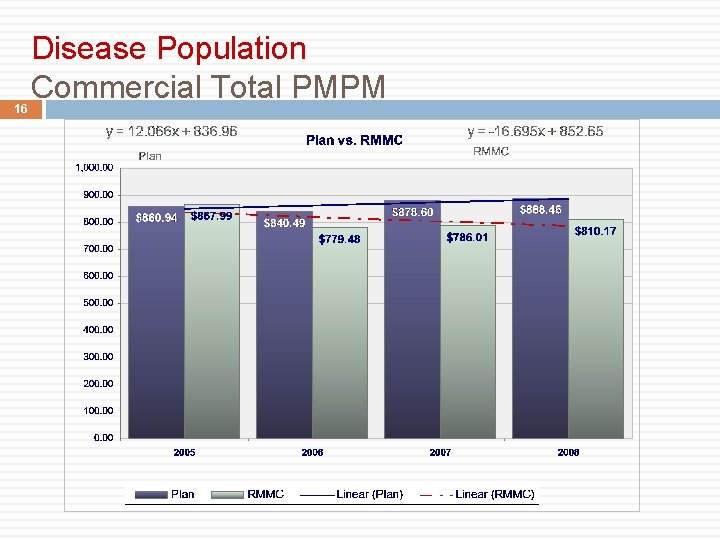
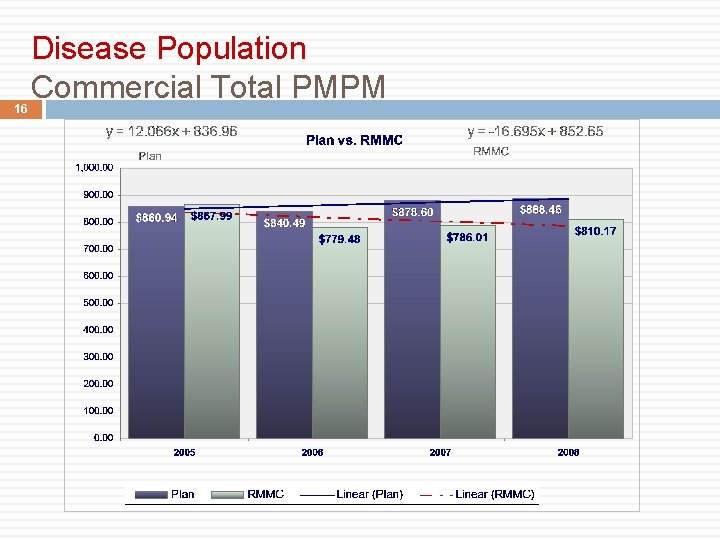
16 Disease Population Commercial Total PMPM
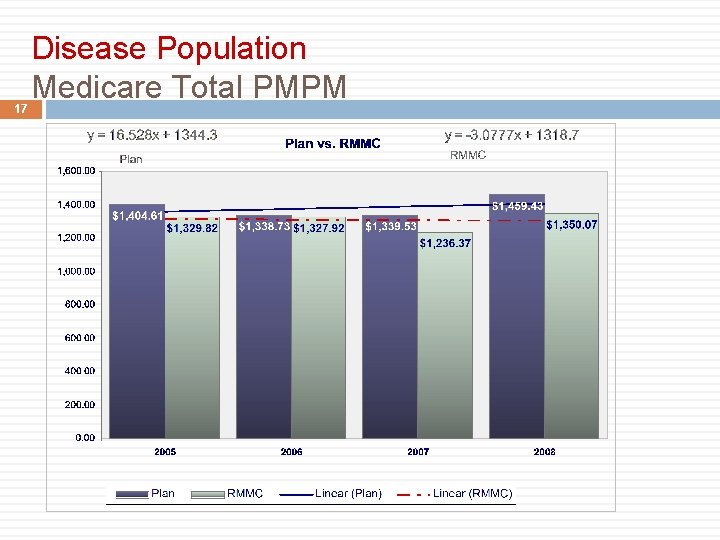
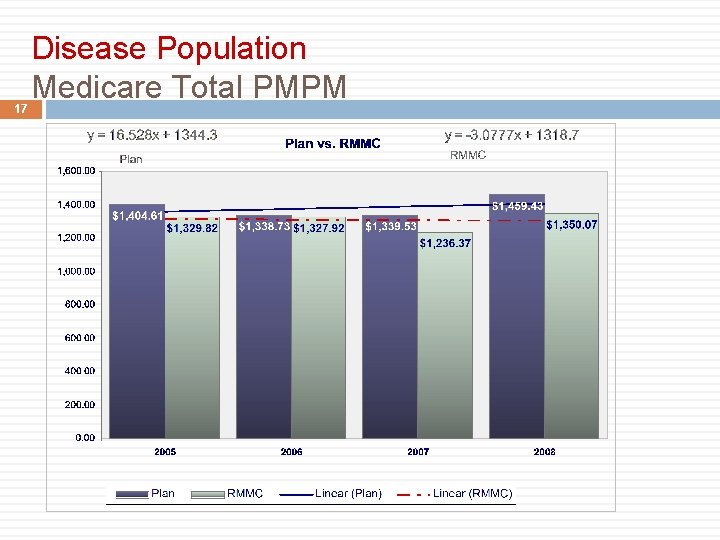
17 Disease Population Medicare Total PMPM
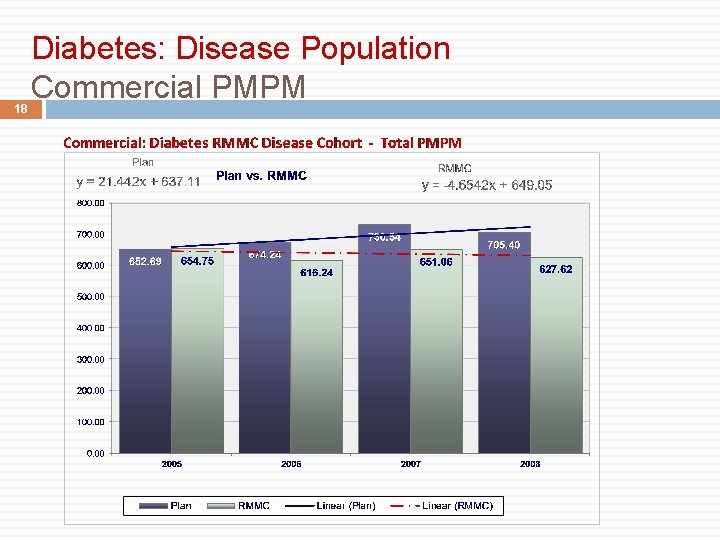
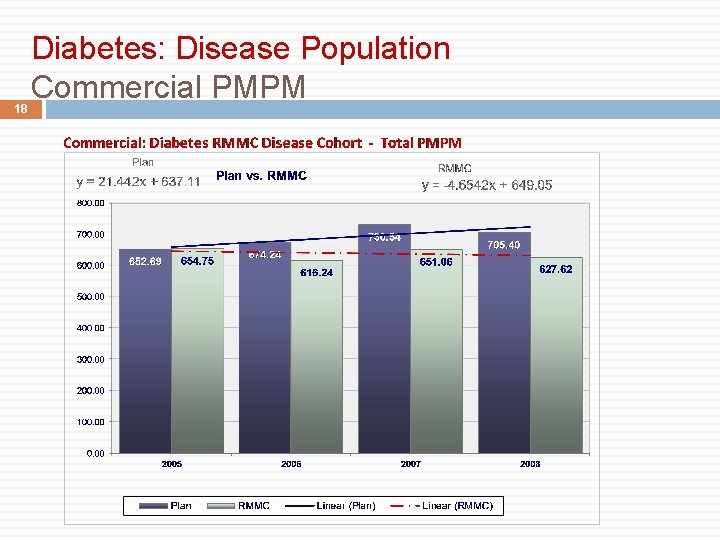
18 Diabetes: Disease Population Commercial PMPM
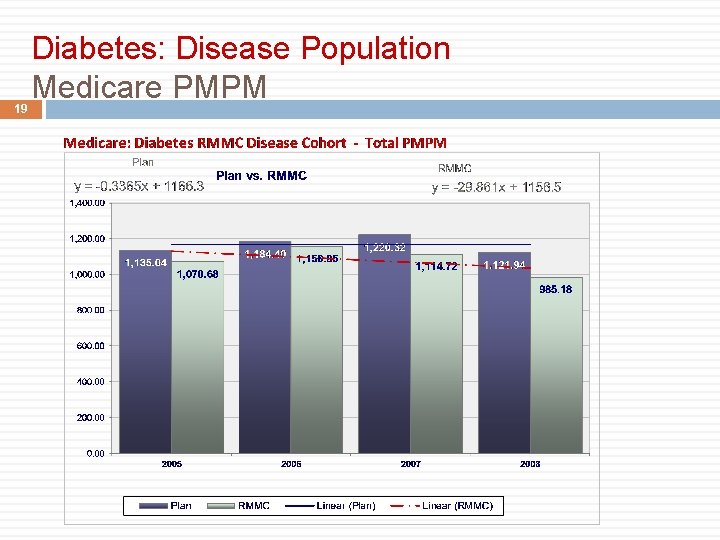
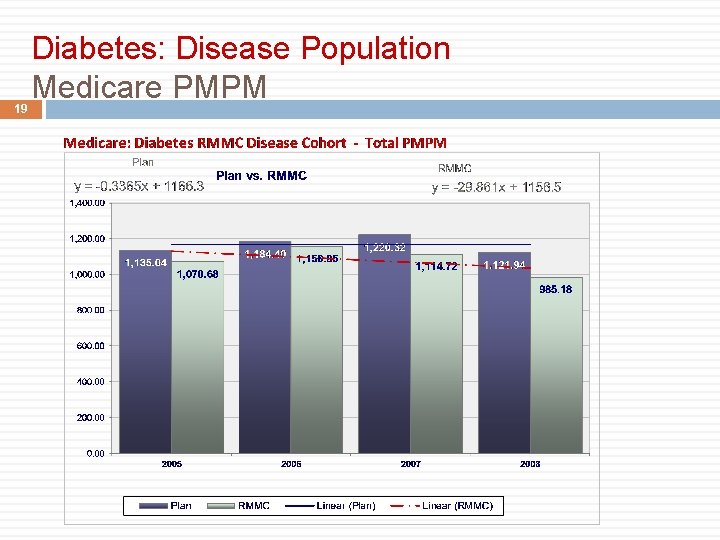
19 Diabetes: Disease Population Medicare PMPM
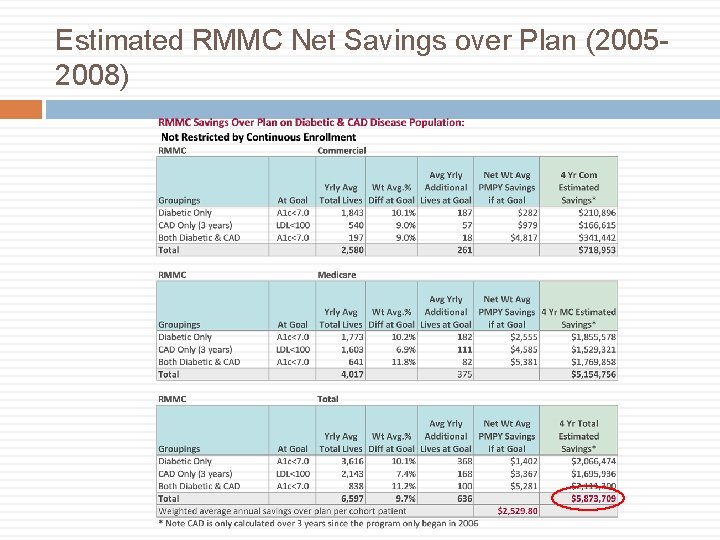
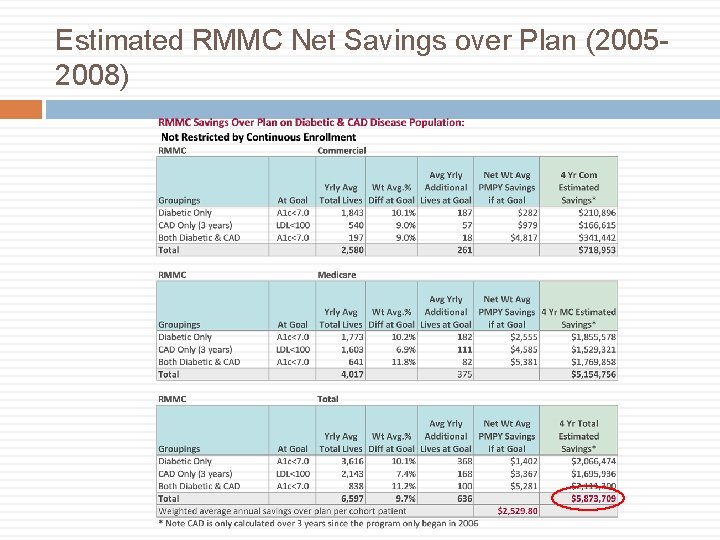
Estimated RMMC Net Savings over Plan (20052008)
What Doctors Learn Population Management QI processes Working in teams and using tools Result sharing Helping patients change their health behaviors
RMMC Conclusions It is possible to change PCP behavior but it takes about a 10% reimbursement bump Multiple avenues of support improve results Physician ownership is key The greater the degree of practice penetration the better Improved care of patients with chronic illness lowers costs No program is perfect but imperfect programs can still accomplish goals.
Whither P 4 P? Less free standing payer based programs? Certainly will be a component of PCMH More transparency for government/consumer purposes Specialist programs?
Reform and the ACO Reimbursement reform to drive cost lowering is a safe assumption My bet is that aligned incentives will prove the best route to cost control and ACO type integration will proliferate To the extent that certain outcomes drive costs, there will be P 4 P within the ACO. To the extent that the ACO will need to demonstrate quality, P 4 P will likely have a role