POSTPARTUM INTRAUTERINE CONTRACEPTIVE DEVICE Postpartum IUCD Training Course





- Slides: 39

POSTPARTUM INTRAUTERINE CONTRACEPTIVE DEVICE Postpartum IUCD Training Course JHPIEGO in partnership with Save the Children, Constella Futures, The Academy for Educational Development, The American College of Nurse-Midwives and IMA World Health
Objectives By the end of this presentation, participants will be able to l List the clinical criteria for provision of the IUCD in the postpartum setting l Describe the key method characteristics of the IUCD when provided postpartum l Discuss the advantages and limitations l Discuss the key elements of postpartum IUCD service provision 2
The Context for Postpartum IUCD l If we accept that pregnancy spacing of at least 24 months is recommended, and l If we recognize that there is large unmet need for postpartum FP, and l If we have learned that there have been advances in understanding the IUCD, and l If we see that the new focus on Skilled Attendance at Birth gives us a unique and new opportunity to provide women with postpartum FP, then…. 3
The Context for Postpartum IUCD l Then… l The postpartum IUCD is a potential answer to issues of: l Variety of different methods ―More choices increases satisfaction l Possibility of a long term reversible method ―IUCD may be an alternative to tubectomy for some couples l Access ―Immediate postpartum insertion is convenient for women 4
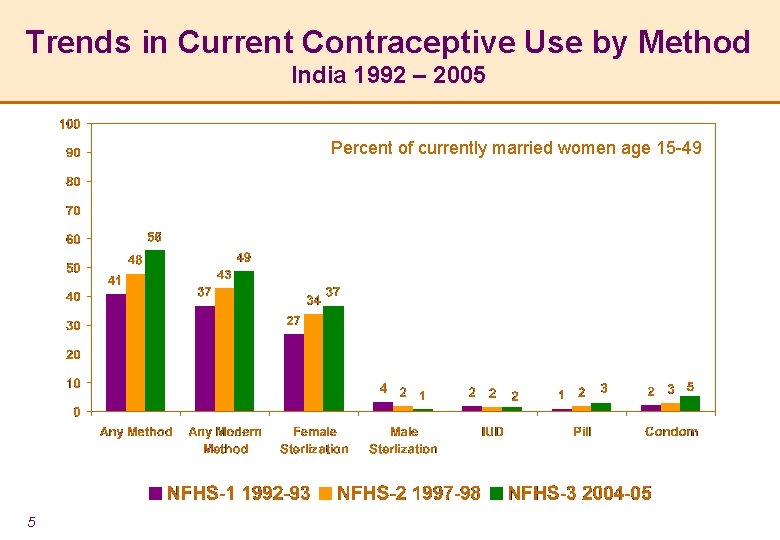
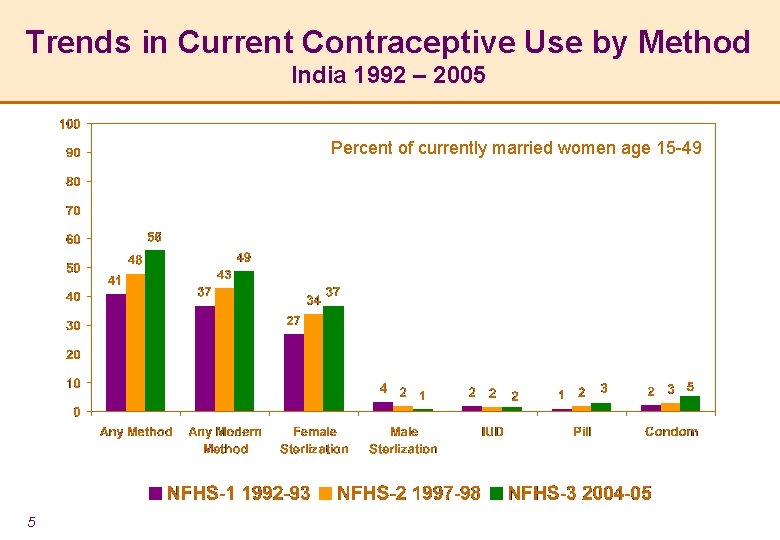
Trends in Current Contraceptive Use by Method India 1992 – 2005 Percent of currently married women age 15 -49 5
But…Resurgence of Interest in the IUCD l India-wide national strategy to increase IUCD services l Global changes in thinking about IUCD l New advances and new understanding about IUCD l Recent research has lead to important changes in WHO Medical Eligibility Criteria (MEC) l Rediscovering a “languishing innovation” l Despite persistent misconceptions, IUCD users have higher satisfaction rates (99% versus 91% for pill users) and continuation rates than users of many other methods l Risk of PID in IUCD users is negligible l Opportunities exist for program expansion 6
IUCDs – the Basics l Mechanism of action l Effectiveness and length of use l Advantages and limitations l Client assessment l Side effects and precautions 7
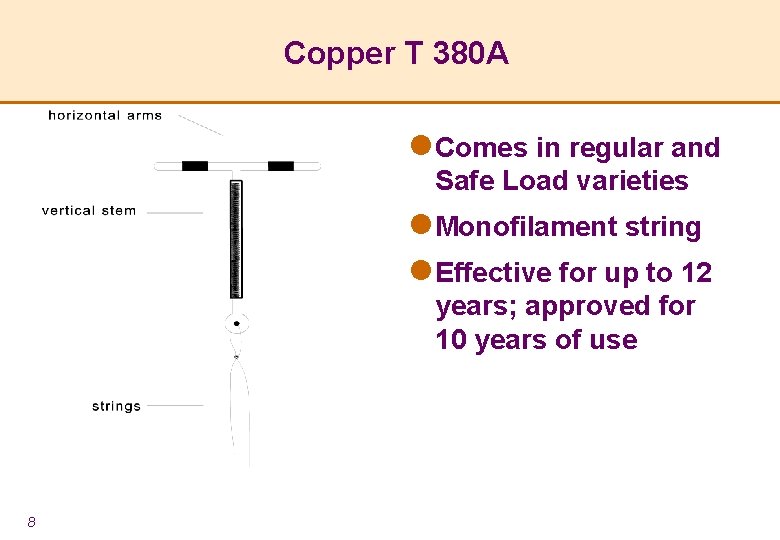
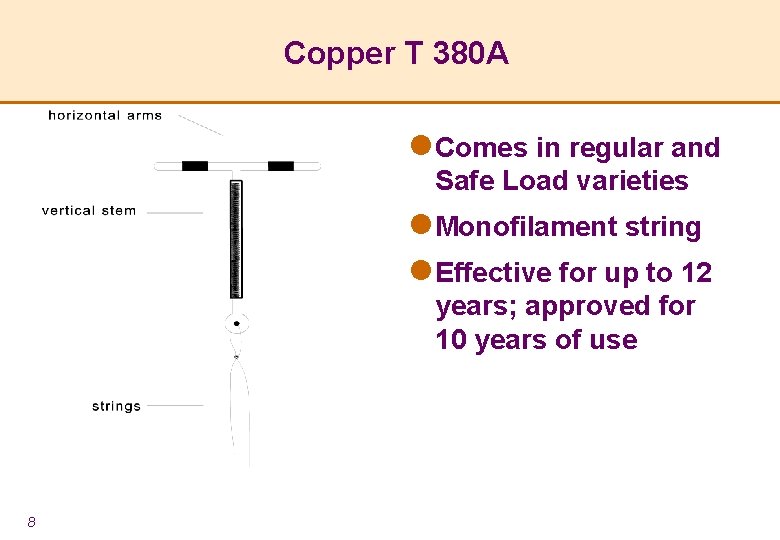
Copper T 380 A l Comes in regular and Safe Load varieties l Monofilament string l Effective for up to 12 years; approved for 10 years of use 8
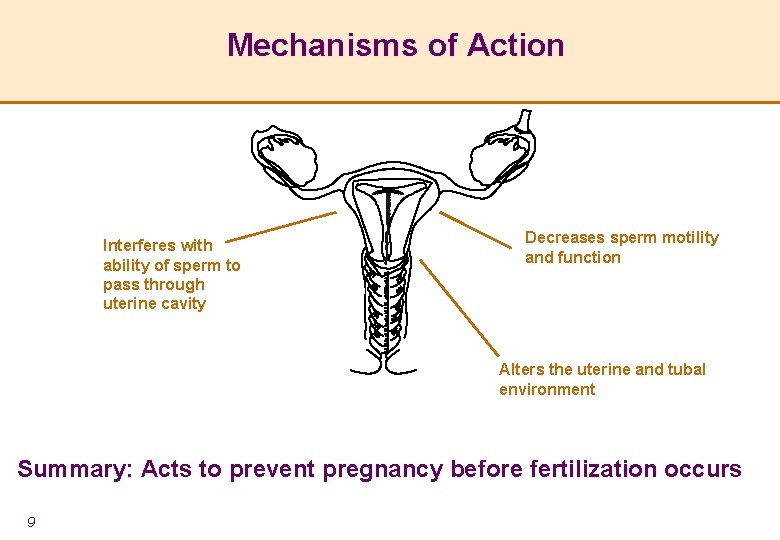
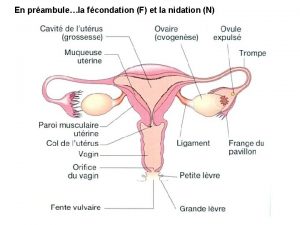
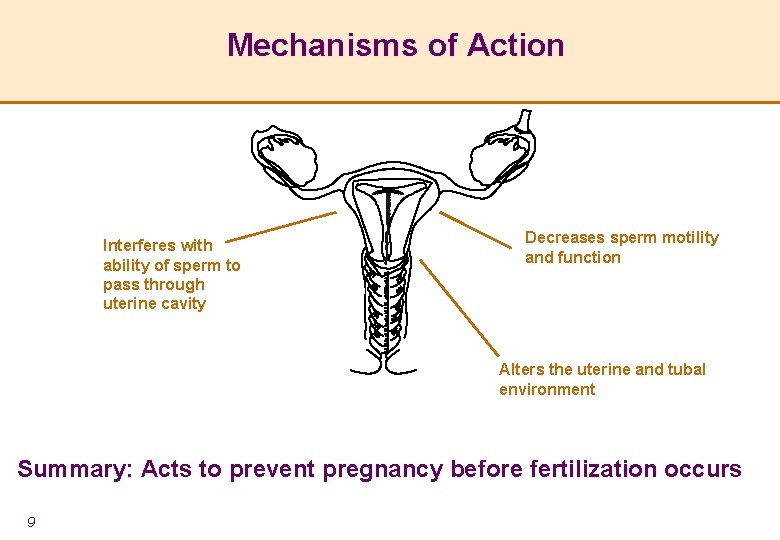
Mechanisms of Action Interferes with ability of sperm to pass through uterine cavity Decreases sperm motility and function Alters the uterine and tubal environment Summary: Acts to prevent pregnancy before fertilization occurs 9
Effectiveness l Effectiveness: > 99% effective l 6 – 8 pregnancies per 1 000 women in first year l Effective immediately upon insertion l Immediate return to fertility once removed l Effective for 10+ years l Can be used as short-term method 10
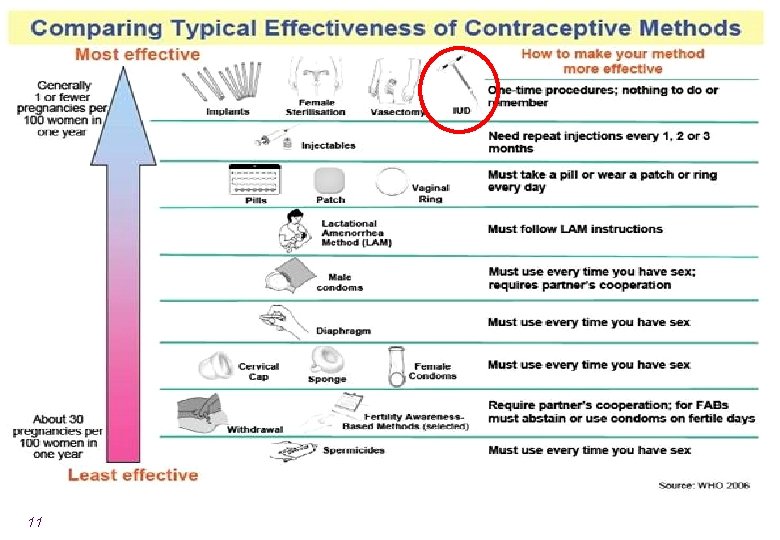
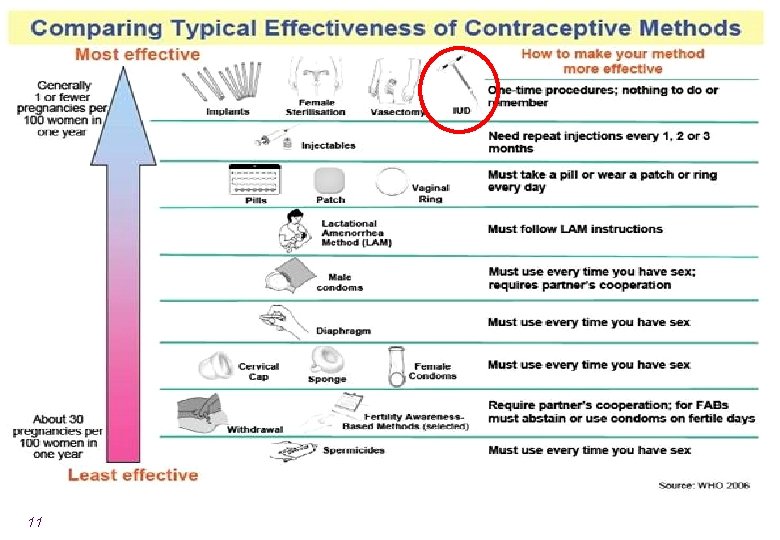
11
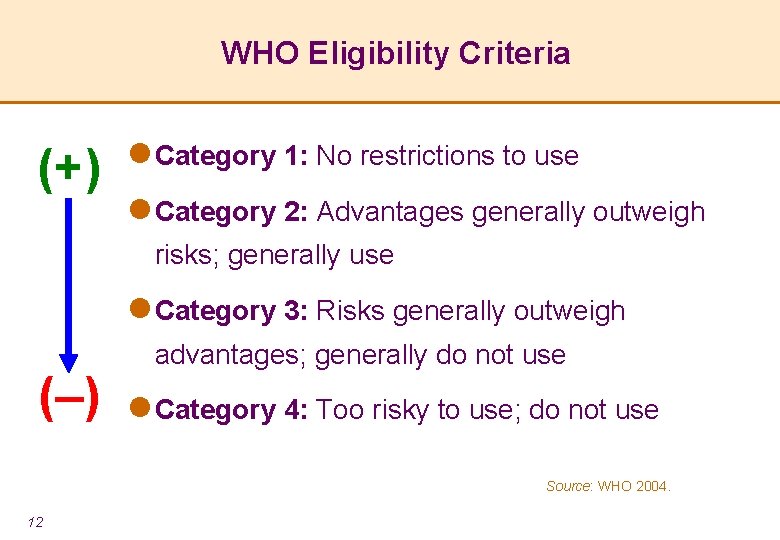
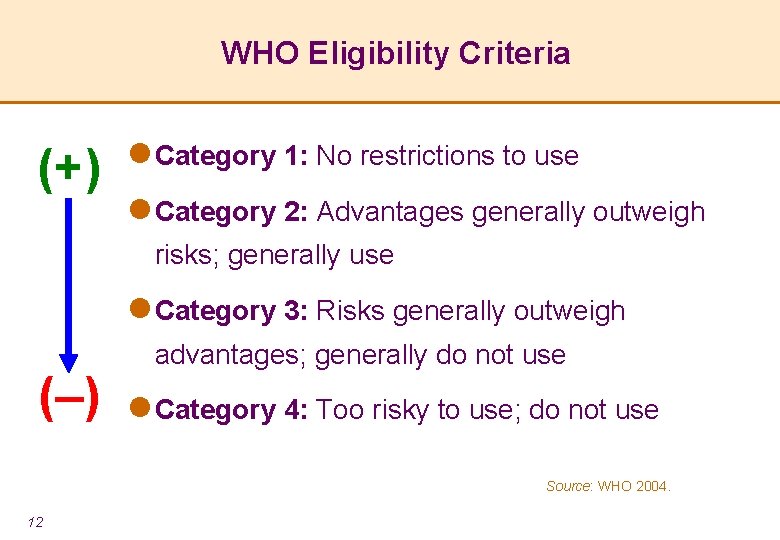
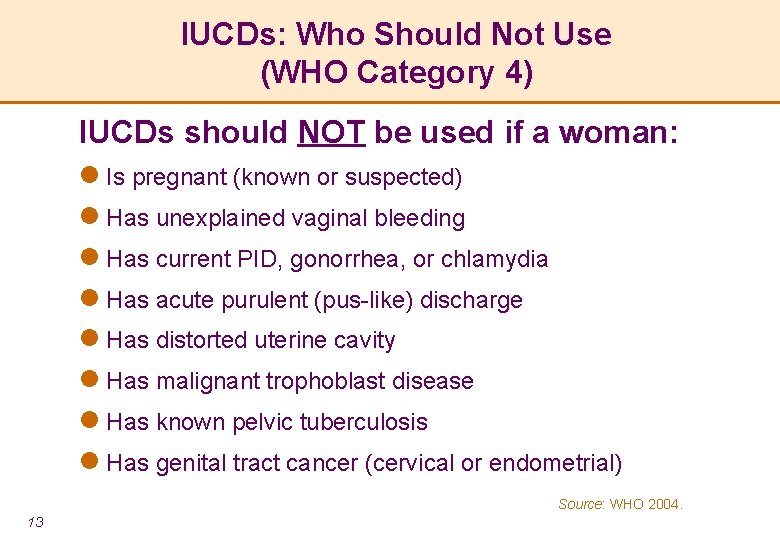
WHO Eligibility Criteria (+) l Category 1: No restrictions to use l Category 2: Advantages generally outweigh risks; generally use l Category 3: Risks generally outweigh ( ) advantages; generally do not use l Category 4: Too risky to use; do not use Source: WHO 2004. 12
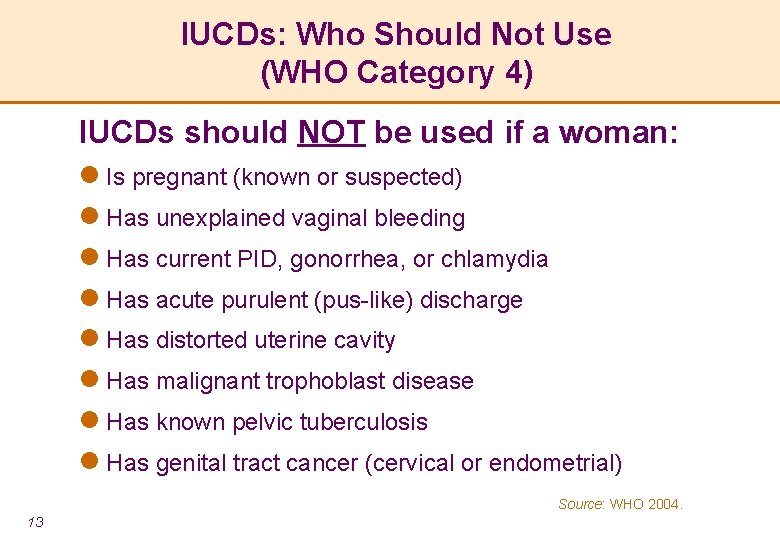
IUCDs: Who Should Not Use (WHO Category 4) IUCDs should NOT be used if a woman: l Is pregnant (known or suspected) l Has unexplained vaginal bleeding l Has current PID, gonorrhea, or chlamydia l Has acute purulent (pus-like) discharge l Has distorted uterine cavity l Has malignant trophoblast disease l Has known pelvic tuberculosis l Has genital tract cancer (cervical or endometrial) Source: WHO 2004. 13
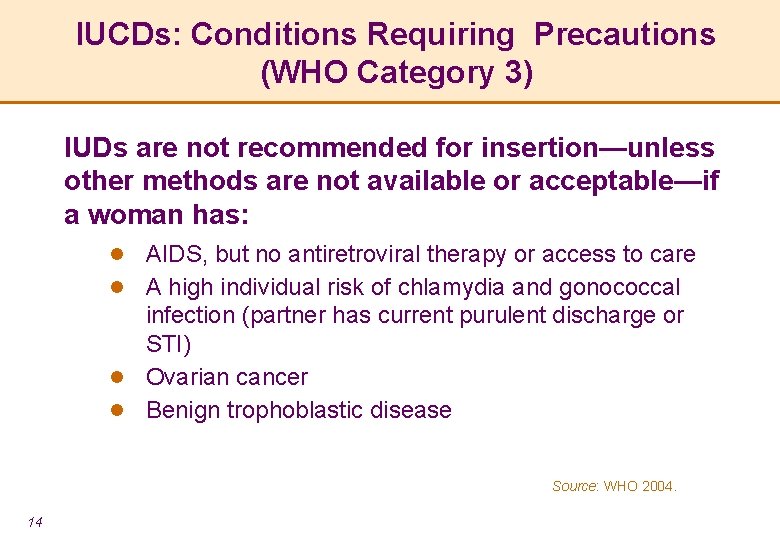
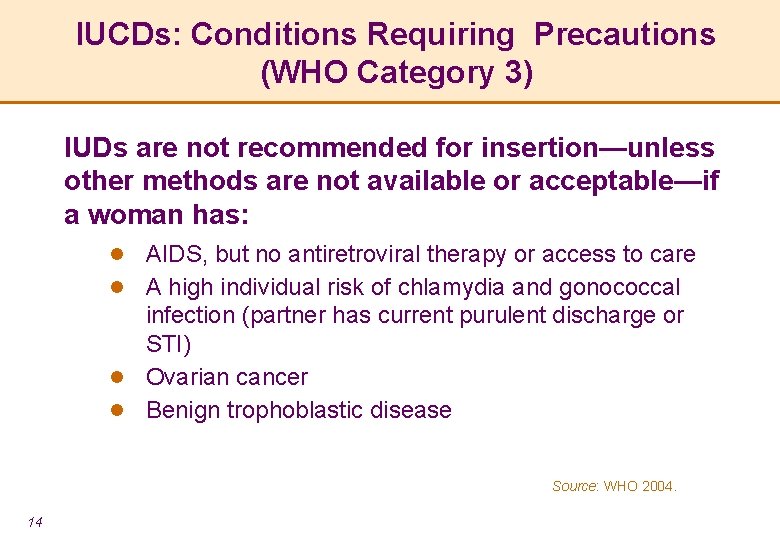
IUCDs: Conditions Requiring Precautions (WHO Category 3) IUDs are not recommended for insertion—unless other methods are not available or acceptable—if a woman has: AIDS, but no antiretroviral therapy or access to care l A high individual risk of chlamydia and gonococcal infection (partner has current purulent discharge or STI) l Ovarian cancer l Benign trophoblastic disease l Source: WHO 2004. 14
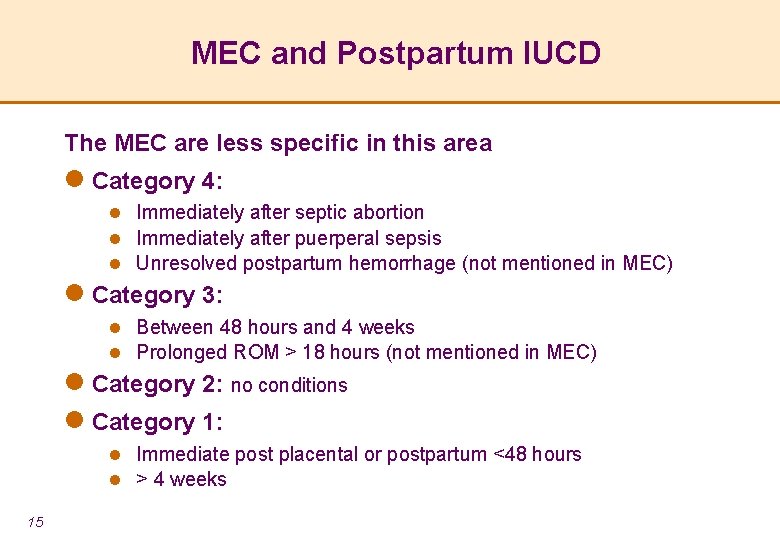
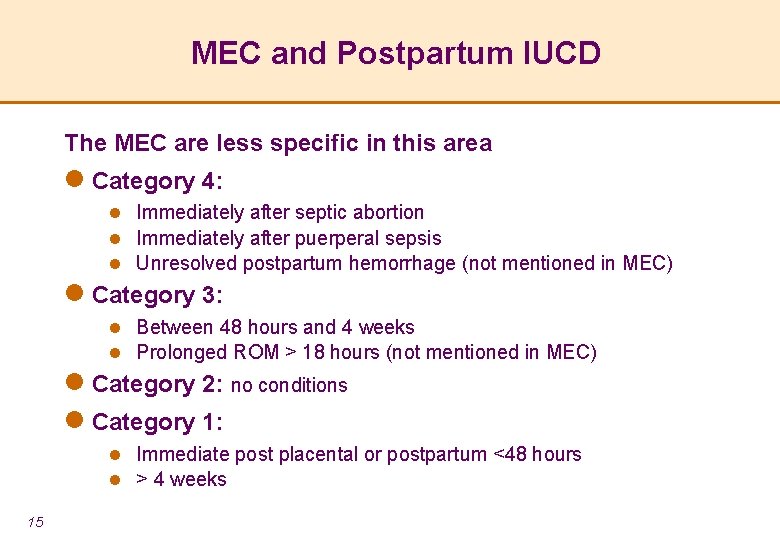
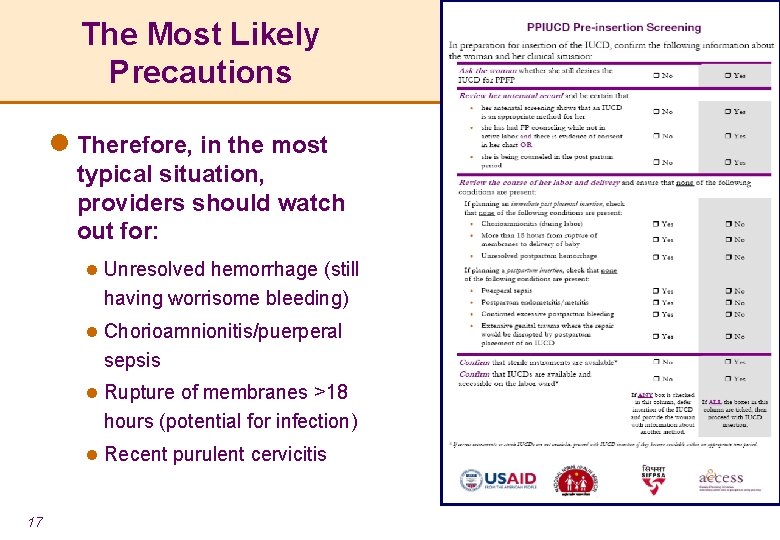
MEC and Postpartum IUCD The MEC are less specific in this area l Category 4: l Immediately after septic abortion l Immediately after puerperal sepsis l Unresolved postpartum hemorrhage (not mentioned in MEC) l Category 3: l Between 48 hours and 4 weeks l Prolonged ROM > 18 hours (not mentioned in MEC) l Category 2: no conditions l Category 1: l Immediate post placental or postpartum <48 hours l > 4 weeks 15
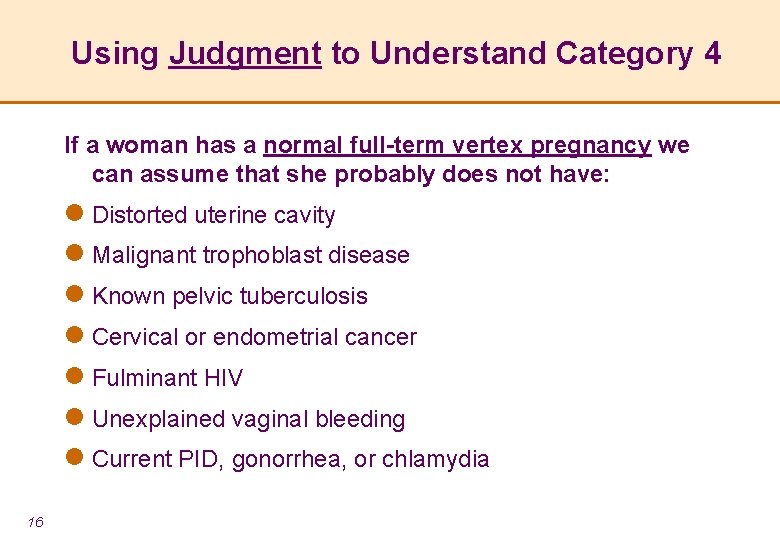
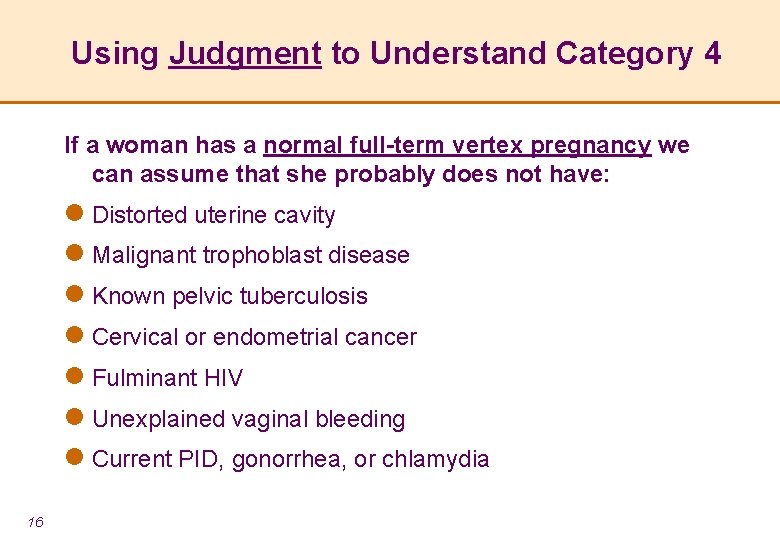
Using Judgment to Understand Category 4 If a woman has a normal full-term vertex pregnancy we can assume that she probably does not have: l Distorted uterine cavity l Malignant trophoblast disease l Known pelvic tuberculosis l Cervical or endometrial cancer l Fulminant HIV l Unexplained vaginal bleeding l Current PID, gonorrhea, or chlamydia 16
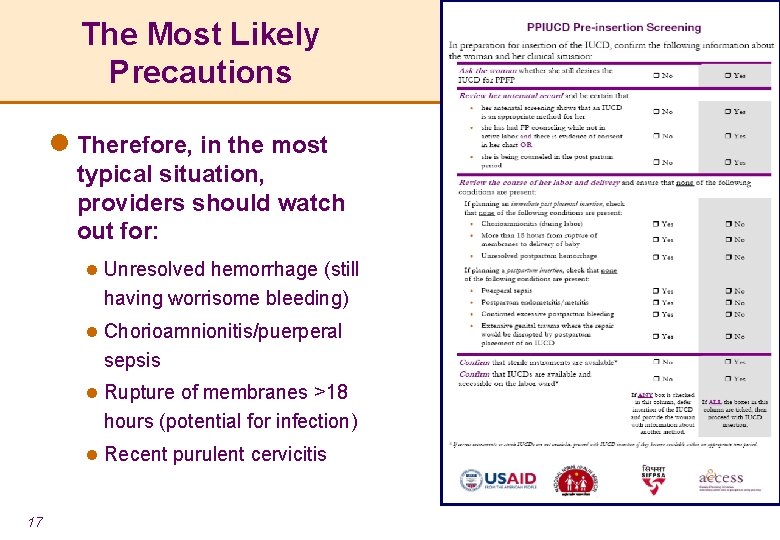
The Most Likely Precautions l Therefore, in the most typical situation, providers should watch out for: l Unresolved hemorrhage (still having worrisome bleeding) l Chorioamnionitis/puerperal sepsis l Rupture of membranes >18 hours (potential for infection) l Recent purulent cervicitis 17
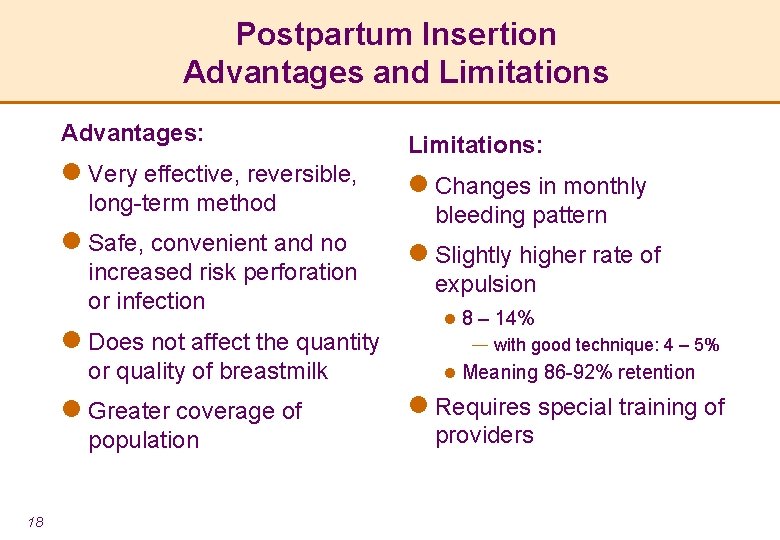
Postpartum Insertion Advantages and Limitations Advantages: l Very effective, reversible, long-term method l Safe, convenient and no increased risk perforation or infection l Does not affect the quantity or quality of breastmilk l Greater coverage of population 18 Limitations: l Changes in monthly bleeding pattern l Slightly higher rate of expulsion l 8 – 14% ― with good technique: 4 – 5% l Meaning 86 -92% retention l Requires special training of providers
IUCD and Anemia l Monthly menstrual bleeding increases slightly with the IUCD, especially in first 3 months l Blood loss which results in anemia is rare l Therefore, it is safe to provide an anemic woman with an IUCD (WHO MEC Category 2) l If a woman is anemic and has the IUCD in place, continue to treat anemia with iron/folate 19
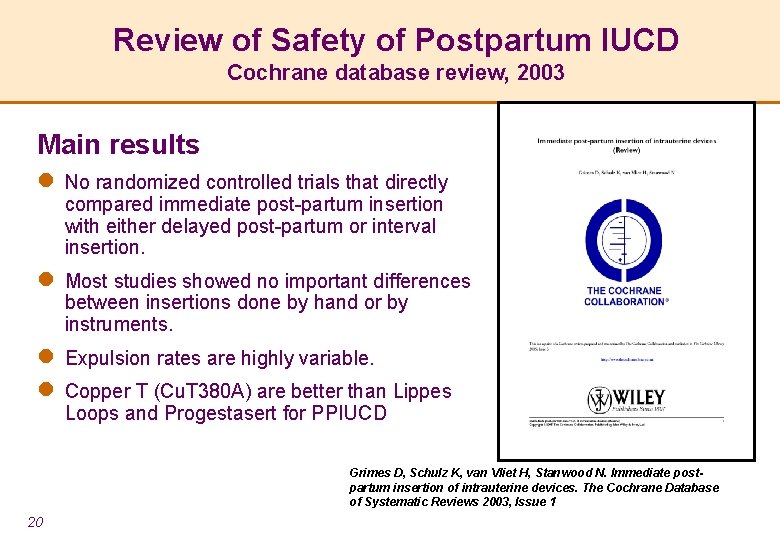
Review of Safety of Postpartum IUCD Cochrane database review, 2003 Main results l No randomized controlled trials that directly compared immediate post-partum insertion with either delayed post-partum or interval insertion. l Most studies showed no important differences between insertions done by hand or by instruments. l Expulsion rates are highly variable. l Copper T (Cu. T 380 A) are better than Lippes Loops and Progestasert for PPIUCD Grimes D, Schulz K, van Vliet H, Stanwood N. Immediate postpartum insertion of intrauterine devices. The Cochrane Database of Systematic Reviews 2003, Issue 1 20
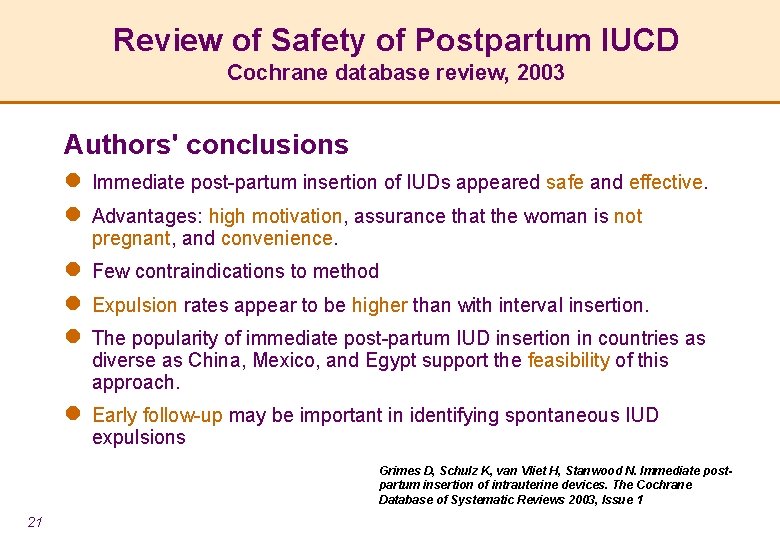
Review of Safety of Postpartum IUCD Cochrane database review, 2003 Authors' conclusions l Immediate post-partum insertion of IUDs appeared safe and effective. l Advantages: high motivation, assurance that the woman is not pregnant, and convenience. l Few contraindications to method l Expulsion rates appear to be higher than with interval insertion. l The popularity of immediate post-partum IUD insertion in countries as diverse as China, Mexico, and Egypt support the feasibility of this approach. l Early follow-up may be important in identifying spontaneous IUD expulsions Grimes D, Schulz K, van Vliet H, Stanwood N. Immediate postpartum insertion of intrauterine devices. The Cochrane Database of Systematic Reviews 2003, Issue 1 21
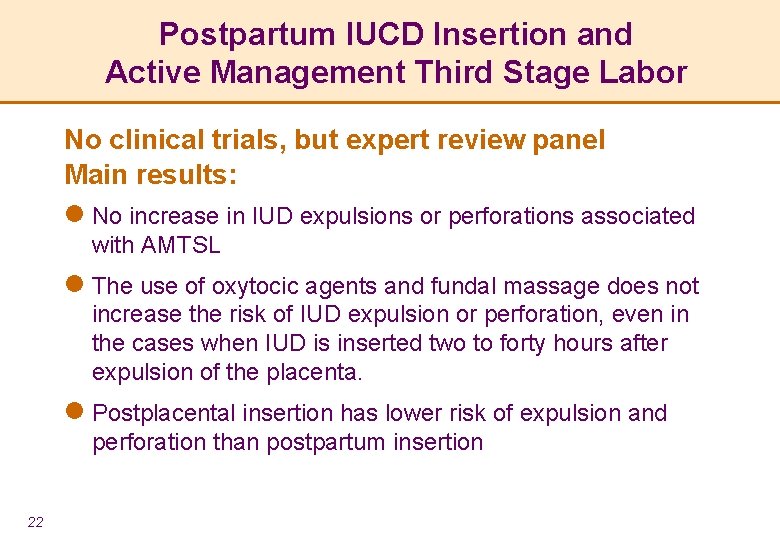
Postpartum IUCD Insertion and Active Management Third Stage Labor No clinical trials, but expert review panel Main results: l No increase in IUD expulsions or perforations associated with AMTSL l The use of oxytocic agents and fundal massage does not increase the risk of IUD expulsion or perforation, even in the cases when IUD is inserted two to forty hours after expulsion of the placenta. l Postplacental insertion has lower risk of expulsion and perforation than postpartum insertion 22
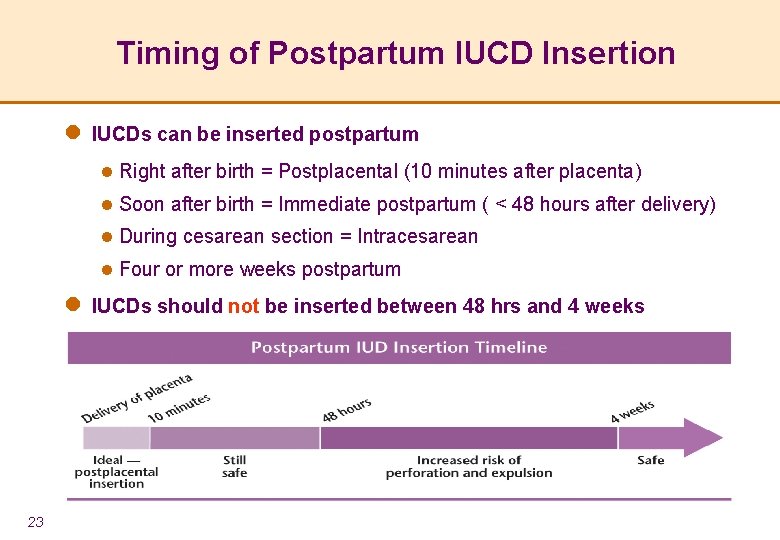
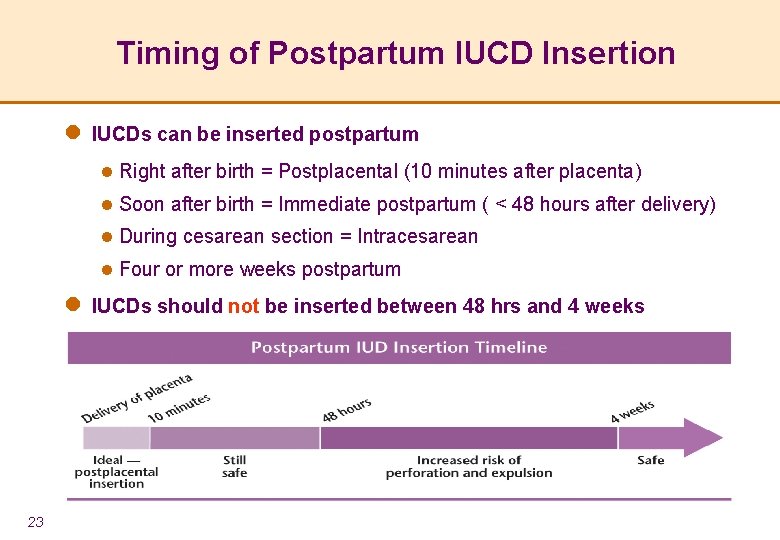
Timing of Postpartum IUCD Insertion l IUCDs can be inserted postpartum l Right after birth = Postplacental (10 minutes after placenta) l Soon after birth = Immediate postpartum ( < 48 hours after delivery) l During cesarean section = Intracesarean l Four or more weeks postpartum l IUCDs should not be inserted between 48 hrs and 4 weeks 23
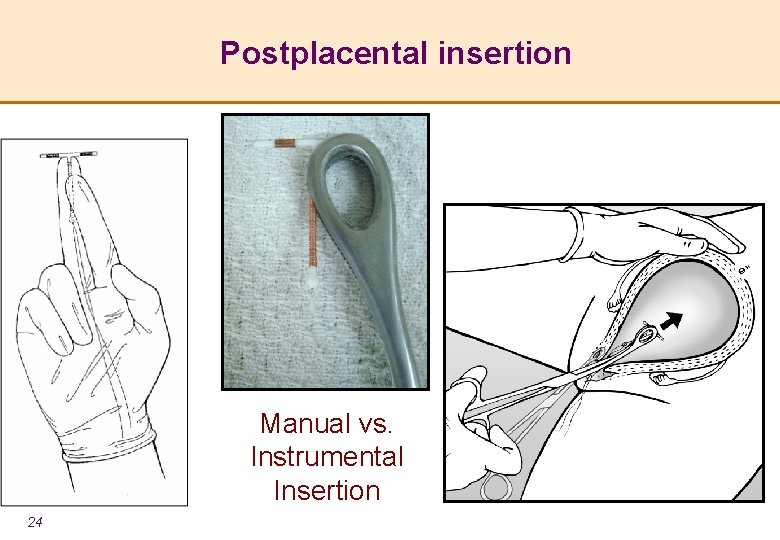
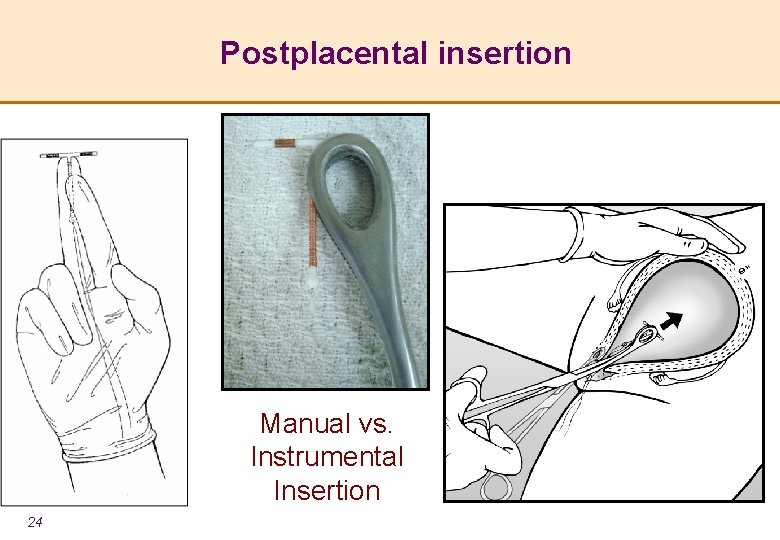
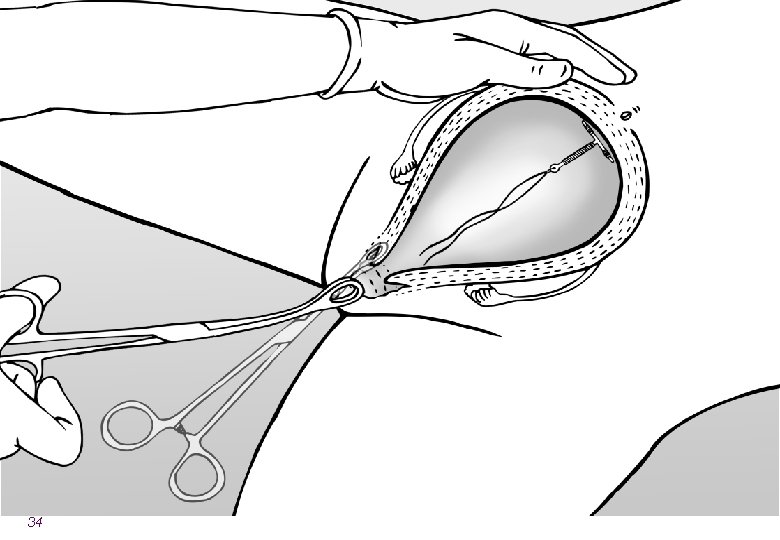
Postplacental insertion Manual vs. Instrumental Insertion 24
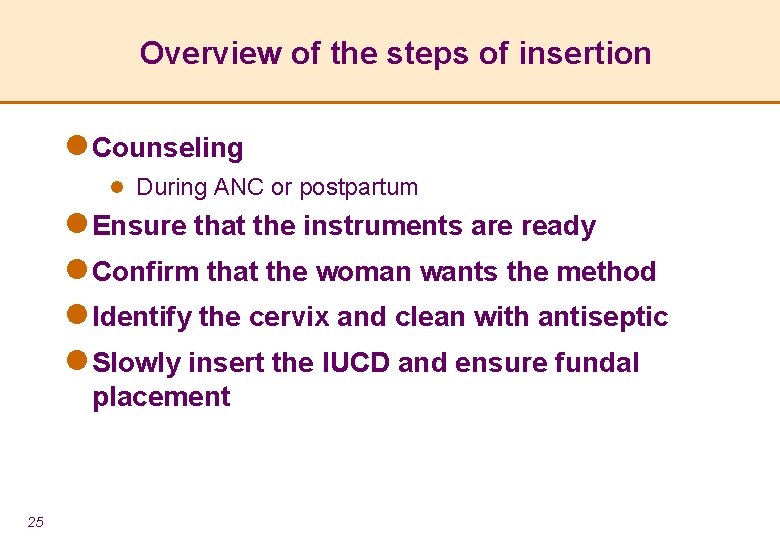
Overview of the steps of insertion l Counseling l During ANC or postpartum l Ensure that the instruments are ready l Confirm that the woman wants the method l Identify the cervix and clean with antiseptic l Slowly insert the IUCD and ensure fundal placement 25

26
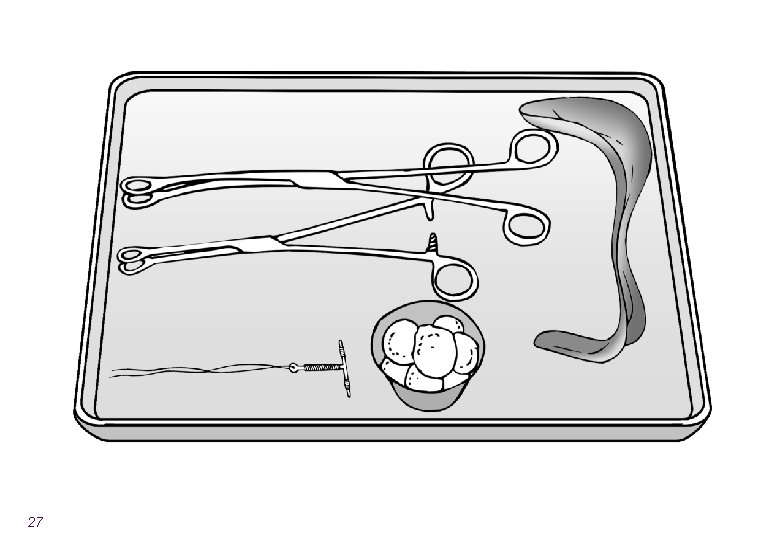
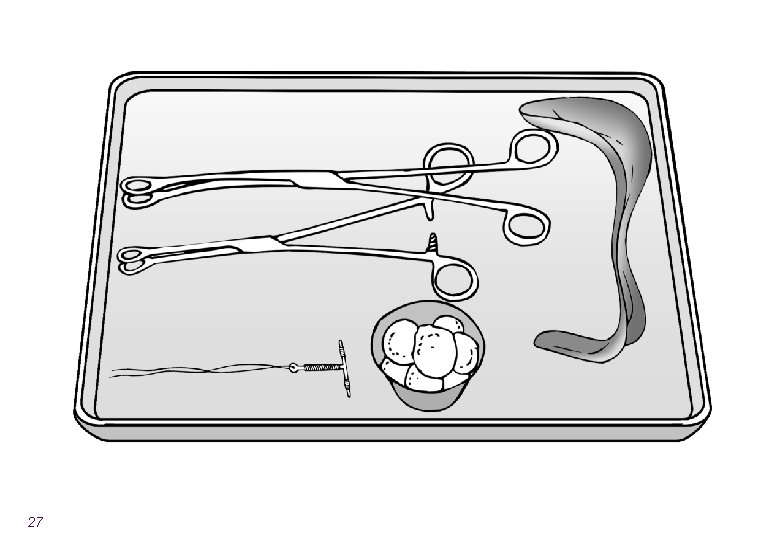
27

28

29
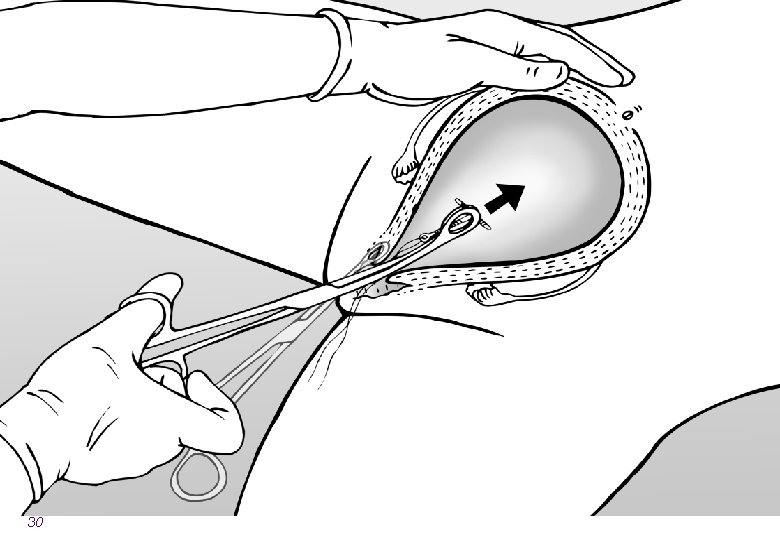
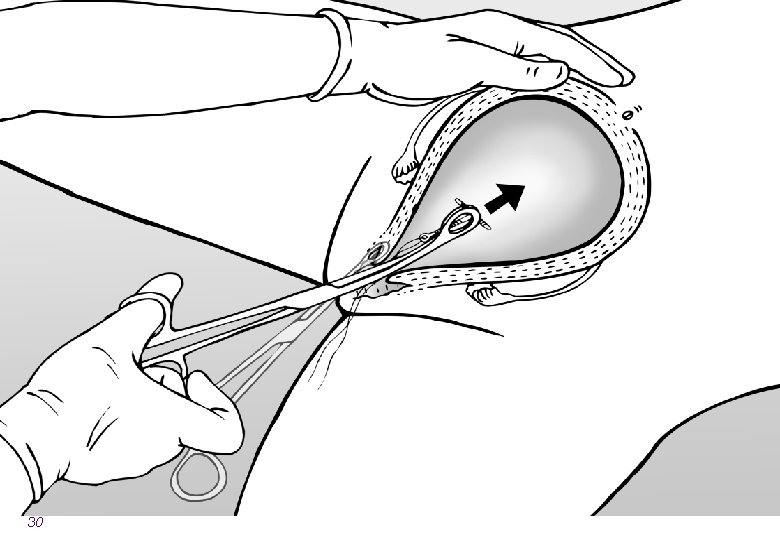
30
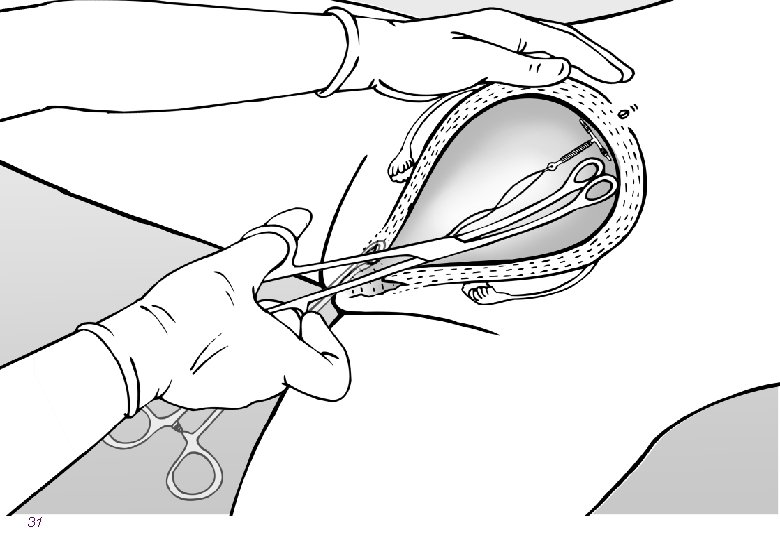
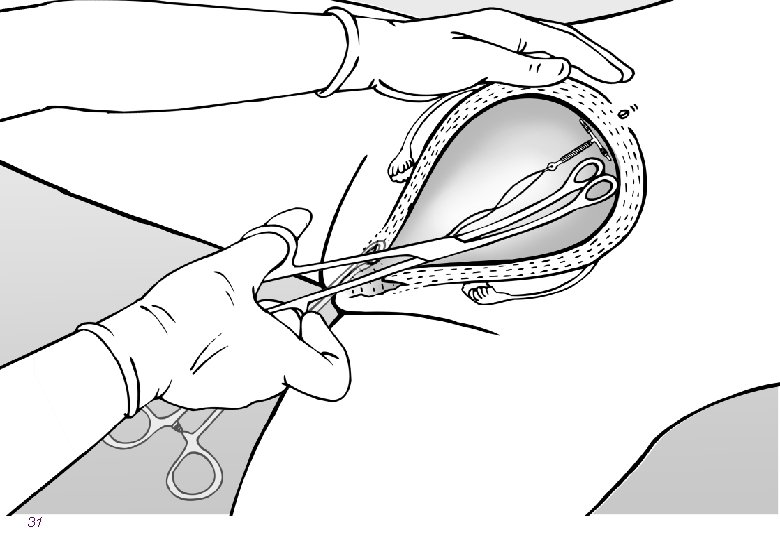
31
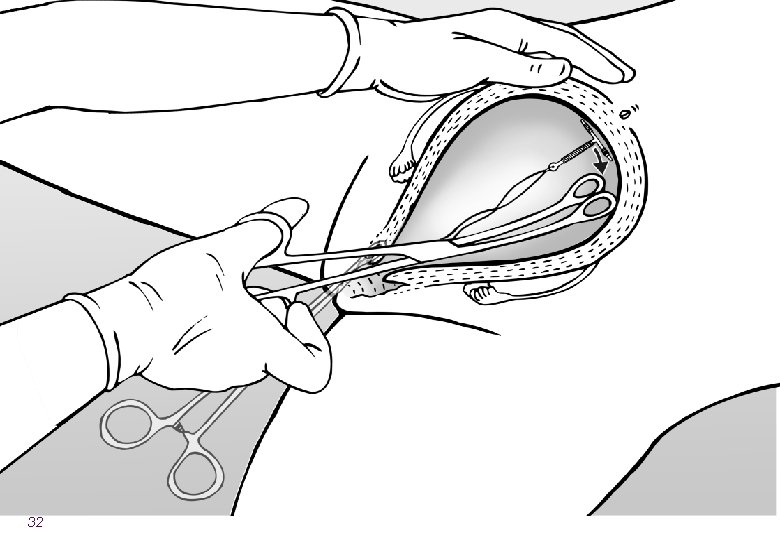
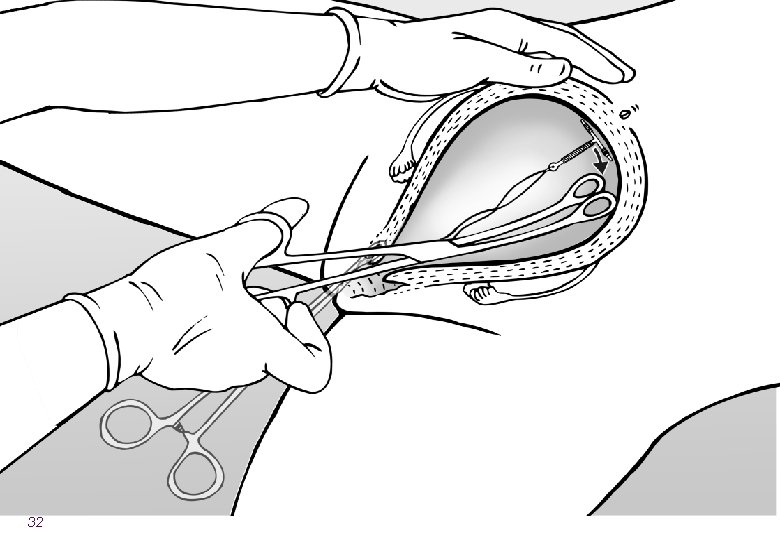
32

33
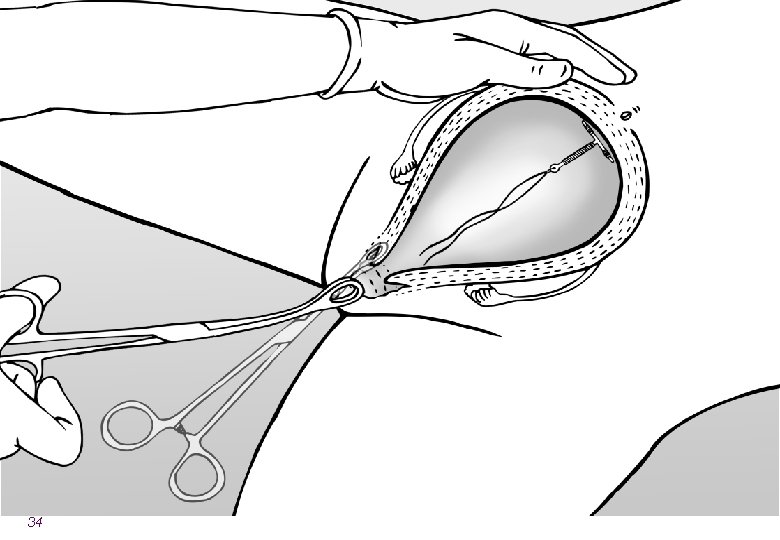
34
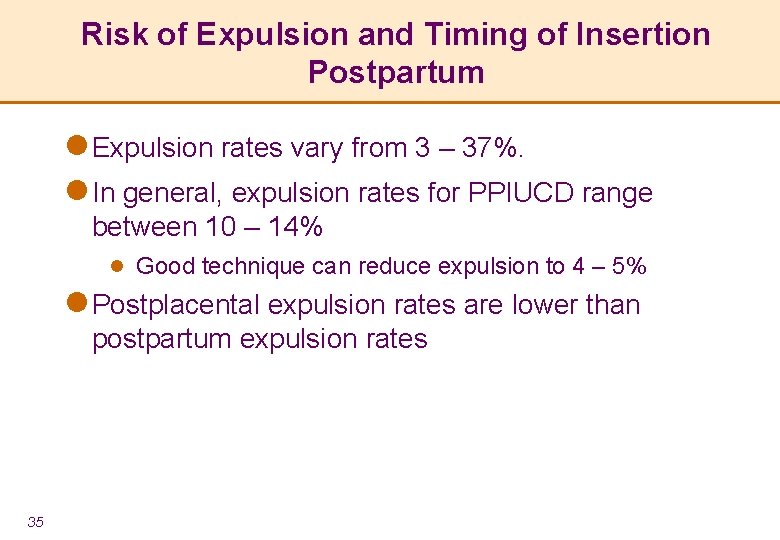
Risk of Expulsion and Timing of Insertion Postpartum l Expulsion rates vary from 3 – 37%. l In general, expulsion rates for PPIUCD range between 10 – 14% l Good technique can reduce expulsion to 4 – 5% l Postplacental expulsion rates are lower than postpartum expulsion rates 35
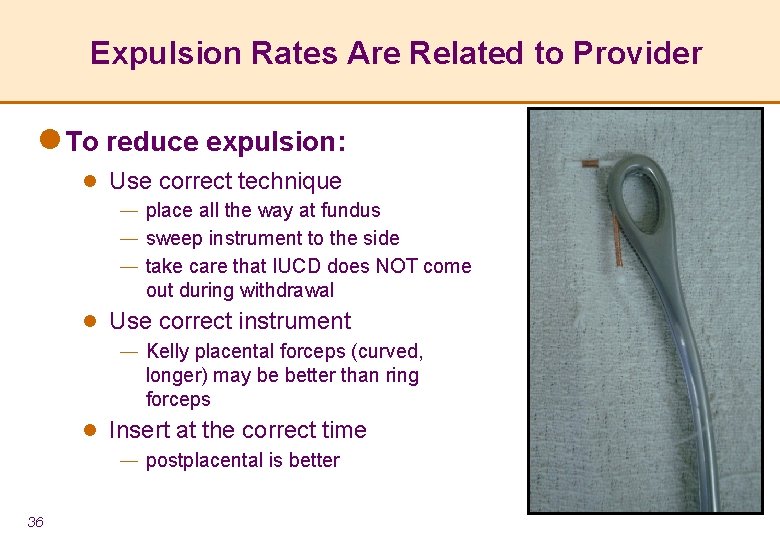
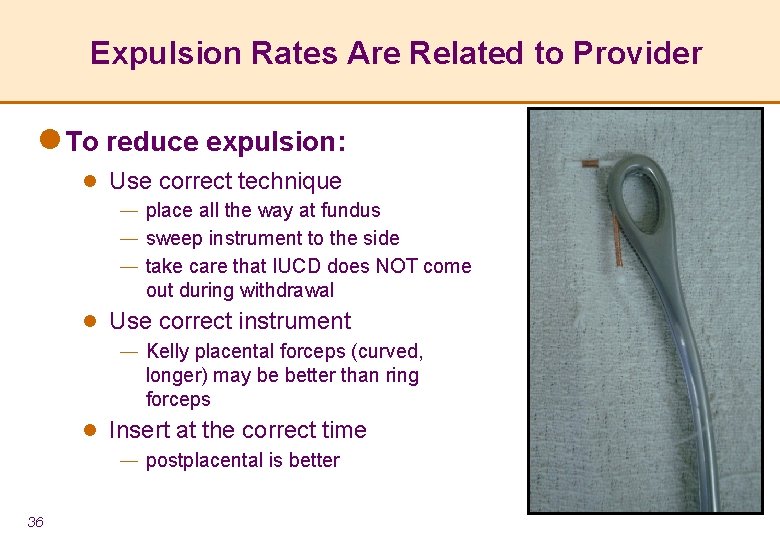
Expulsion Rates Are Related to Provider l To reduce expulsion: l Use correct technique ― place all the way at fundus ― sweep instrument to the side ― take care that IUCD does NOT come out during withdrawal l Use correct instrument ― Kelly placental forceps (curved, longer) may be better than ring forceps l Insert at the correct time ― postplacental is better 36
Management of Strings l Do not cut strings while placing IUCD postpartum, postplacental or intracesarean l During cesarean section, do NOT pass the strings through cervix; leave in lower uterine segment l Strings will typically descend during involution and curl in posterior vaginal fornix l Sometimes they may remain in the uterus, but this is not usually a problem l Strings CAN be cut at follow-up visit l If pelvic exam is not possible, then it is not necessary to cut strings l Strings SHOULD be cut if the woman complains or they protrude from introitus 37
Myths and Misconceptions We must work to correct misunderstandings: l IUCDs do not cause PID; insertion if there is undiagnosed cervicitis l l l l 38 may result in PID Do not increase the risk of contracting STIs, including HIV Do not make a woman infertile Do not increase the risk of miscarriage when a woman becomes pregnant after the IUCD is removed Do not cause birth defects Do not cause cancer Do not move to the heart or brain Do not cause pain or discomfort for the woman during sex Substantially reduce the risk of ectopic pregnancy
Postpartum IUCDs Summary l Safe and convenient way to provide an effective long term method l Part of a re-focus on health benefits of FP l Limitations of the method are few, especially postpartum precautions l Insertion times include postplacental, postpartum and intracesarean l Expulsion rates are related to provider skill 39
 Intrauterine device
Intrauterine device Intrauterine device
Intrauterine device Tableau comparatif contraception
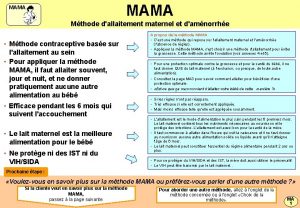
Tableau comparatif contraception Mama methode contraceptive
Mama methode contraceptive Contraceptive
Contraceptive Evonid
Evonid Neten contraceptive
Neten contraceptive Celine contraceptive pill
Celine contraceptive pill Intrauterine
Intrauterine Iucs
Iucs Metricure intrauterine
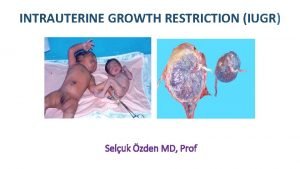
Metricure intrauterine Asymmetrical and symmetrical iugr
Asymmetrical and symmetrical iugr Symmetric growth restriction
Symmetric growth restriction Spalding sign
Spalding sign Input device output device storage device
Input device output device storage device Disadvantages of cavity wall
Disadvantages of cavity wall Course number and title
Course number and title Course interne moyenne externe
Course interne moyenne externe Uterine compression sutures
Uterine compression sutures Lochia rubra
Lochia rubra Haemabate
Haemabate Pph treatment algorithm
Pph treatment algorithm Lochia slideshare
Lochia slideshare Rubin's postpartum phases
Rubin's postpartum phases Vastus lateralis site for babies
Vastus lateralis site for babies Postpartum thyroiditis
Postpartum thyroiditis Lochia after delivery
Lochia after delivery Postpartum bleeding stages
Postpartum bleeding stages Lll mastitis
Lll mastitis Postpartum infection
Postpartum infection Postpartum stomach pain
Postpartum stomach pain Mk clinical management ug
Mk clinical management ug Postpartum prefix and suffix
Postpartum prefix and suffix Chapter 20 postpartum adaptations
Chapter 20 postpartum adaptations Postpartum hemorrhage
Postpartum hemorrhage Thyroid
Thyroid Steps of thyroid hormone synthesis
Steps of thyroid hormone synthesis Postnatal nursing diagnosis slideshare
Postnatal nursing diagnosis slideshare Postpartum infections
Postpartum infections Homan signs
Homan signs