CONGENITAL INFECTIONS Intrauterine and Perinatal Infetions The major






















- Slides: 65
CONGENITAL INFECTIONS Intrauterine and Perinatal Infetions

The major characteristics n Transplacental transmission n Various agents: viruses, bacteria, parasites n A similar clinical features: n multi-organ infection
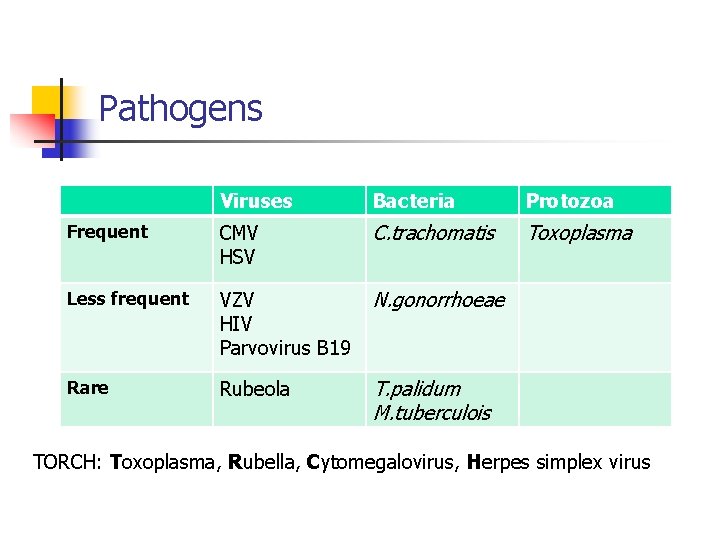
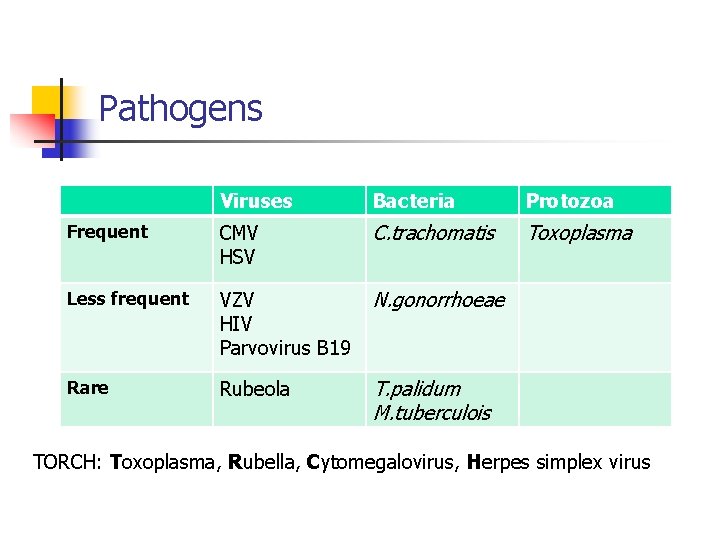
Pathogens Viruses Bacteria Protozoa Frequent CMV HSV C. trachomatis Toxoplasma Less frequent VZV HIV Parvovirus B 19 N. gonorrhoeae Rare Rubeola T. palidum M. tuberculois TORCH: Toxoplasma, Rubella, Cytomegalovirus, Herpes simplex virus

Clinical features n Generalized disease of the fetus / newborn n n n Intrauterine growth restriction Nonimmune hydrops (generalized edema) Anemia, leucopenia, thrombocytopenia Jaundice, hepto-splenomegaly Chorioretinitis, encephalitis Pneumonitis, myocarditis Congenital malforamtions n Depending on the time of infection and the pathogen

CYTOMEGALOVIRUS
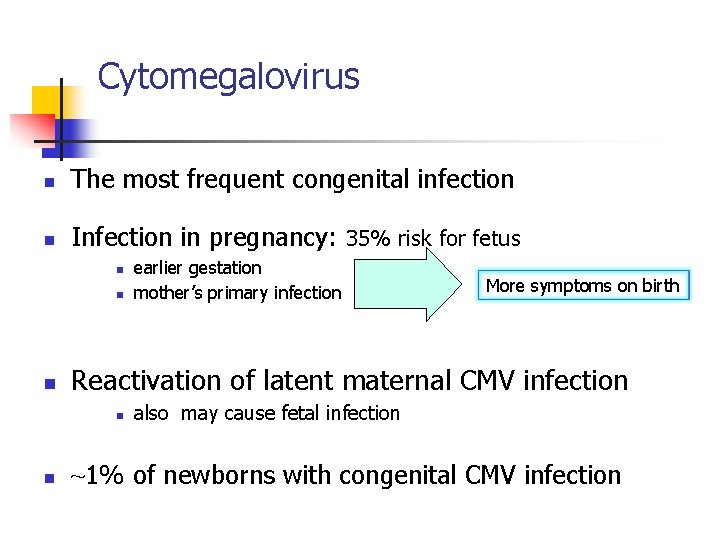
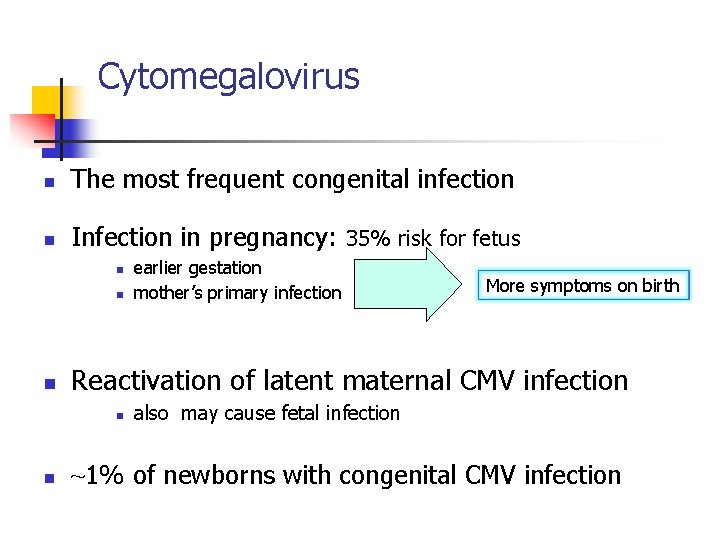
Cytomegalovirus n The most frequent congenital infection n Infection in pregnancy: 35% risk for fetus n n n More symptoms on birth Reactivation of latent maternal CMV infection n n earlier gestation mother’s primary infection also may cause fetal infection ~1% of newborns with congenital CMV infection

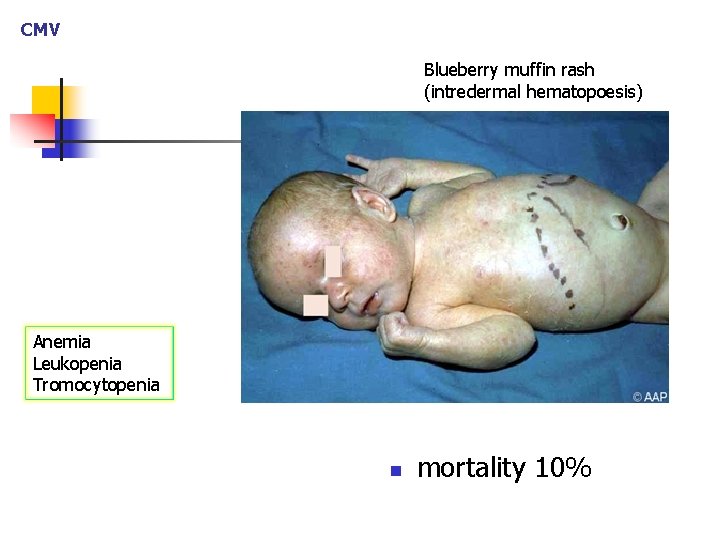
CMV Symptomatic disease on birth (10%) n Low birth weight for gestational age n Jaundice and hepato-splenomegaly n Hepatitis (does not become chronic) n Blueberry muffin rash n Leucocoria (chorioretinitis) n Microcephaly n n intracerebral periventricular calcifications generally with no symptoms of encephalitis
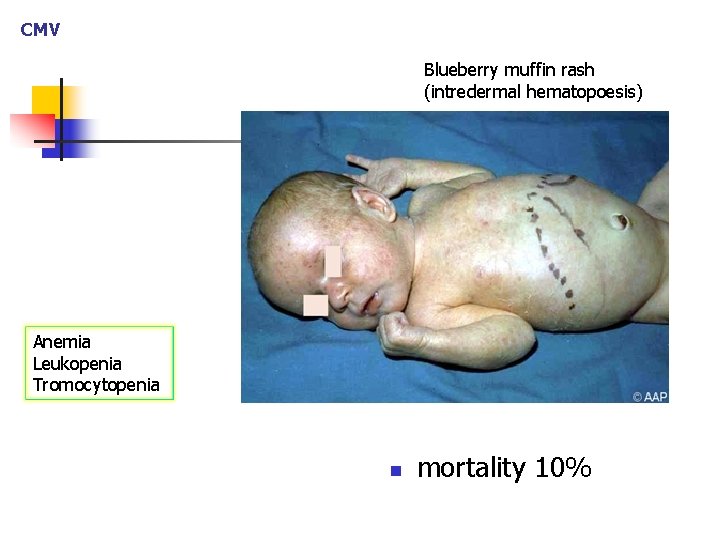
CMV Blueberry muffin rash (intredermal hematopoesis) Anemia Leukopenia Tromocytopenia n mortality 10%
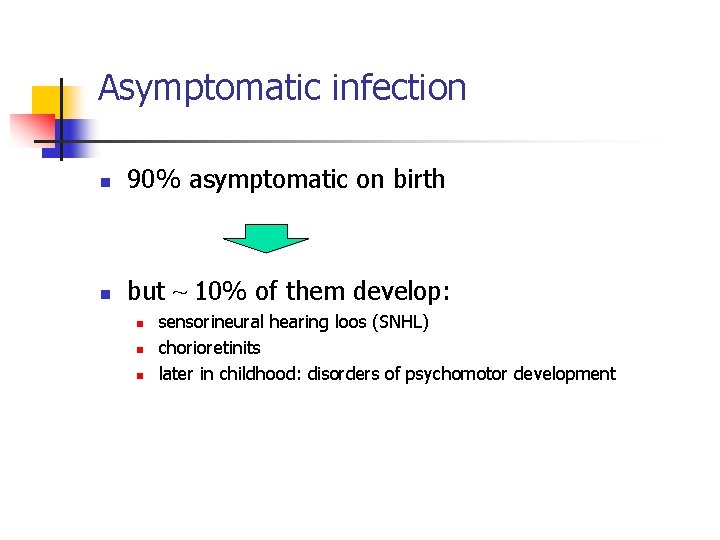
Asymptomatic infection n 90% asymptomatic on birth n but ~ 10% of them develop: n n n sensorineural hearing loos (SNHL) chorioretinits later in childhood: disorders of psychomotor development

CMV The so-called “asymptomatic" infections: n n Chorioretinitis Hearing loss May be the only consequences! Screening is required! n They may affect the child’s development
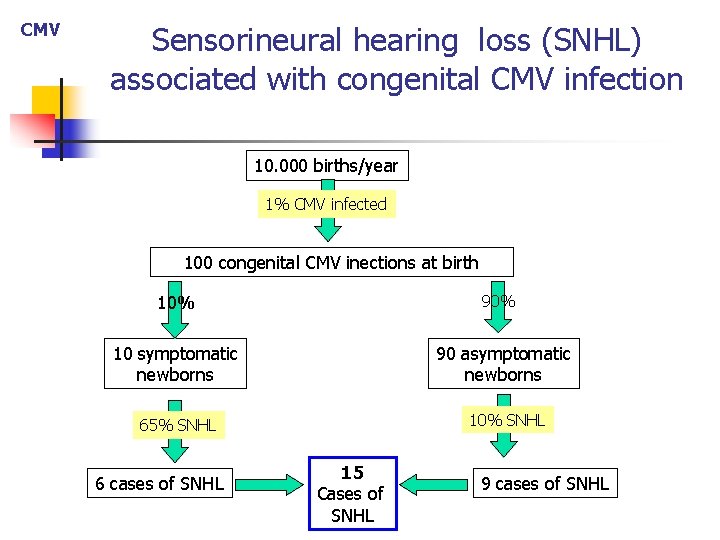
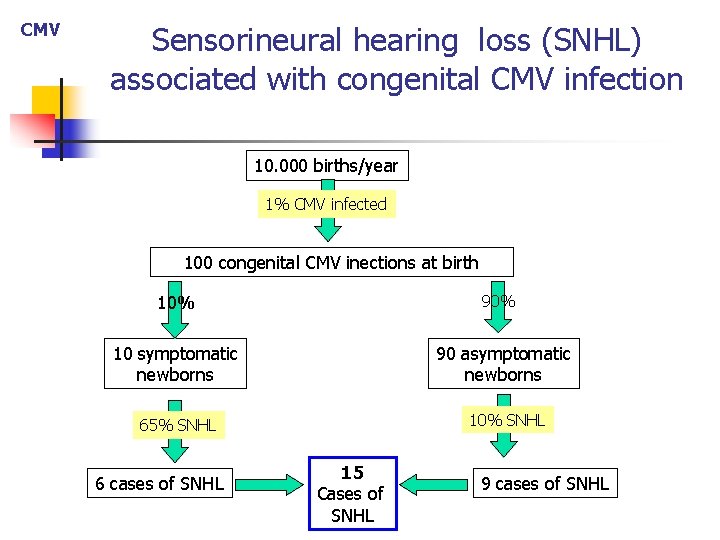
CMV Sensorineural hearing loss (SNHL) associated with congenital CMV infection 10. 000 births/year 1% CMV infected 100 congenital CMV inections at birth 10% 90% 10 symptomatic newborns 90 asymptomatic newborns 65% SNHL 10% SNHL 6 cases of SNHL 15 Cases of SNHL 9 cases of SNHL
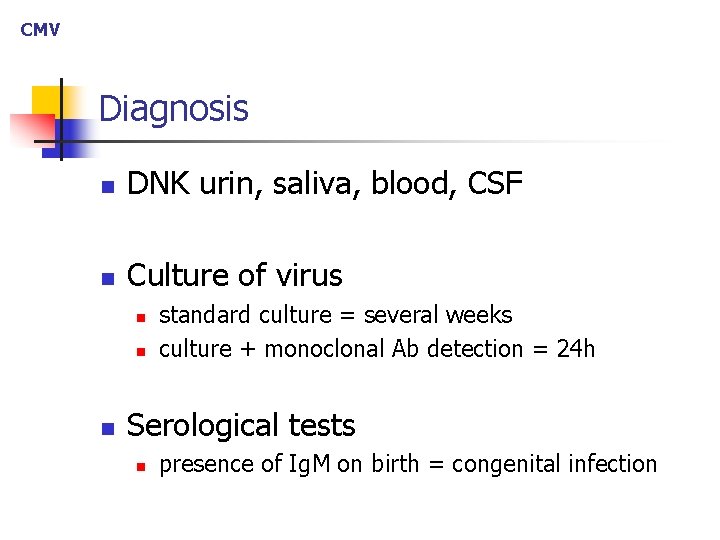
CMV Diagnosis n DNK urin, saliva, blood, CSF n Culture of virus n n n standard culture = several weeks culture + monoclonal Ab detection = 24 h Serological tests n presence of Ig. M on birth = congenital infection
CMV Therapy n Ganciclovir n may halt the progression of hearing loss
TOXOPLASMOSIS
Toxoplasmosis Patogenesis n Usually during mother’s primary infection n n reactivation of latent infection - extremely rare Transmission rate = overall 30 -40% n earlier maternal infection = the lower risk for fetal infection n later maternal infection = hihgher risk for fetal infection n n because of better placental blood flow transmission rate near to birth term ≈90%

Toxoplasmosis Symptoms n Severity of fetal disease n n the earlier infection = the more severe simptoms High risk period = 10 -24 gestational week n n Developed placental blood flow Vulnerable fetal period
Toxoplasmosis “Asymptomatic” disease at birth In most newborns- with no obvious simptoms n But by detailed examinations can reveal: n Chorioretinitis n Intracerebral cortical calcifications n n with inflammatory CSF finding Signs of hydocephalus classic triad
Toxoplasmosis Symptomatic disease on birth: n n n Low birth weight Jaundice (early, within 24 h postnatally) Hepato-splenomegaly Maculopapular rash Triad: choriretinitis, cerebral calcifications, hydocephalus n seizures are frequent High risk for permanent neurological sequellae
Diagnosis n Serologically n Ig. G seroconversion, or 4 -fold rise n n 1 -2 months to achive peak Presence of Ig. M, Ig. A or Ig. E confirms diagnosis n PCR n histological examination of the placenta

Other diagnostic procedures n ophthalmologic examination n hearing testing (Auditory Evoked Potentials) n CT of brain n LP: CSF examination
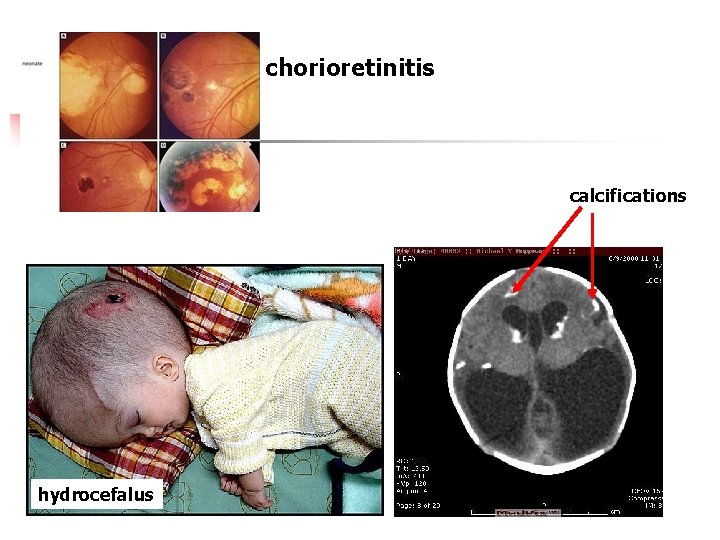
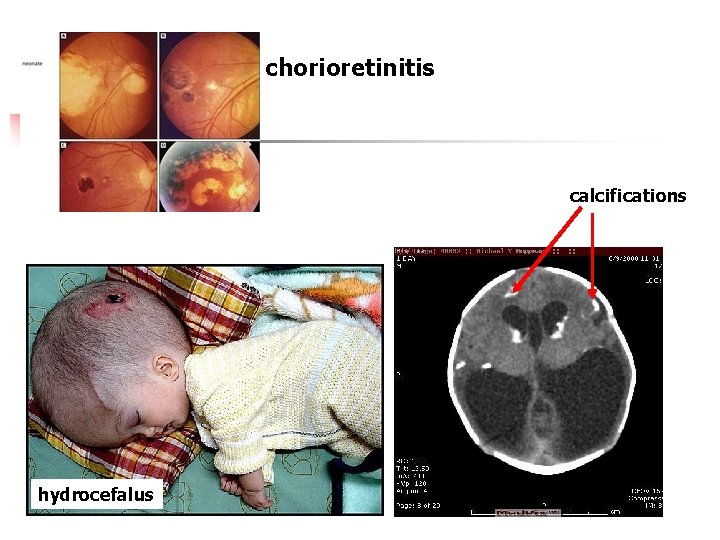
chorioretinitis calcifications hydrocefalus

Toksoplazma Therapy n Pyrimethamin + Sulfadiazin n n 12 months Therapy of infected pregnat women n if an infection is detected before birth
Toksoplazma Prevention n To prevent infection of pregnant women: n n Cooking of food or freezing or below -200 C Thorough hand hygiene: n n after preparing raw meat and vegetables after contact with cats
RUBELLA
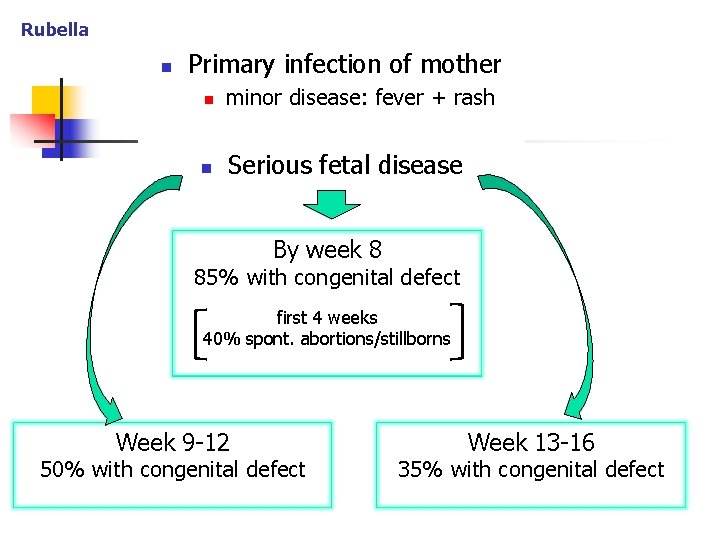
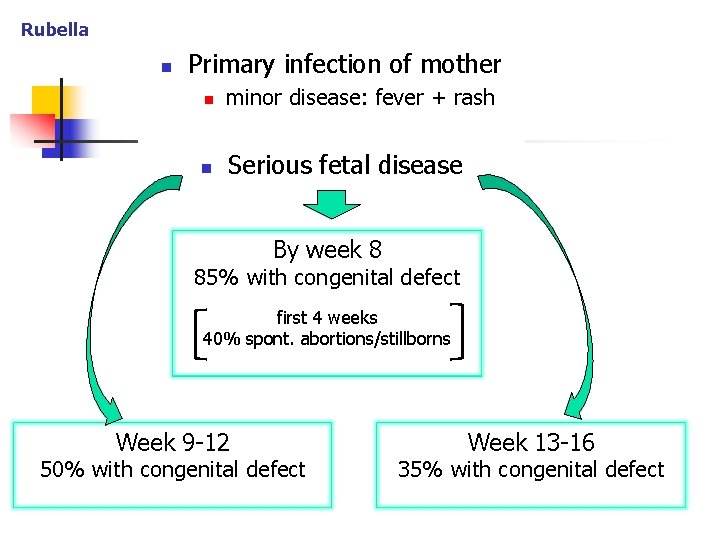
Rubella n Primary infection of mother n minor disease: fever + rash n Serious fetal disease By week 8 85% with congenital defect first 4 weeks 40% spont. abortions/stillborns Week 9 -12 50% with congenital defect Week 13 -16 35% with congenital defect
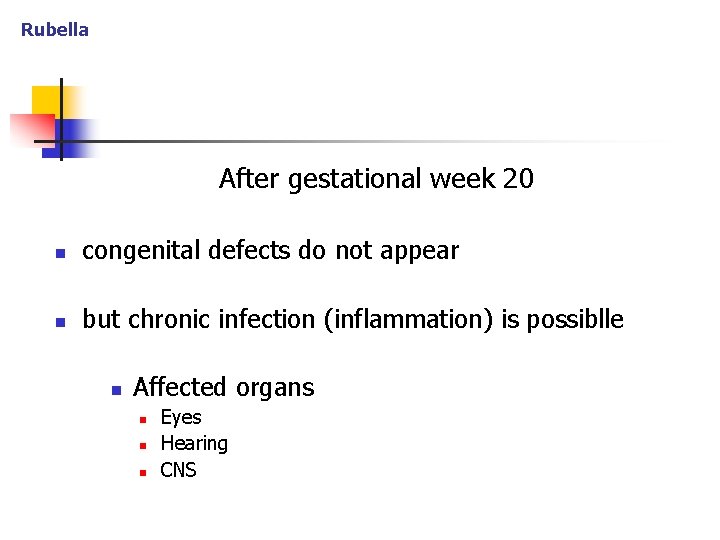
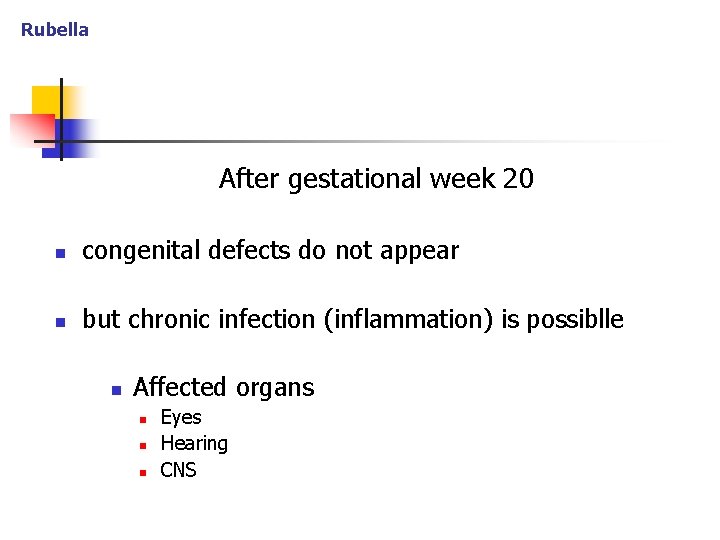
Rubella After gestational week 20 n congenital defects do not appear n but chronic infection (inflammation) is possiblle n Affected organs n n n Eyes Hearing CNS

Rubella Clinical features n Congenital malforamtions n Genealised disease on birth n “Asymptomatic” infectionon birth

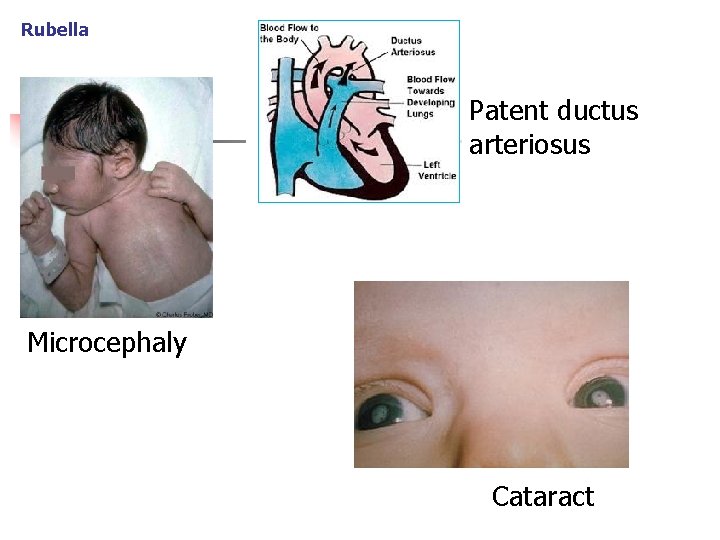
Rubella Congenital malformations n Cardiovascular n n patent ductus ateriosus Botagli pulmonary artery stenosis ventricular and atrial septal defects Eyes n Cataract, chorioretinitis, galucom n Hearing loos (SNHL) n Damage of CNS n n microcephaly, mental retardation spastic paralysis, ect. . .
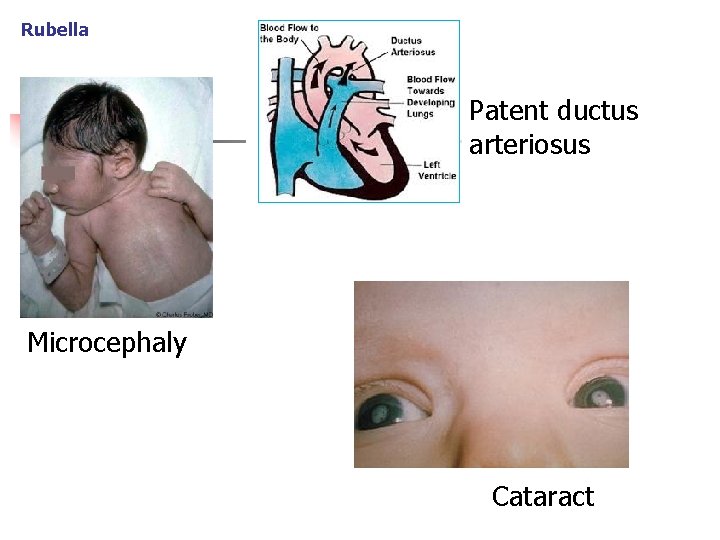
Rubella Patent ductus arteriosus Microcephaly Cataract

Rubella Symptomatic infectionon birth: generalised newborn disease n n n Low bith weight Jaundice, hepatosplenomegaly Thrombocytopenia Purpuric (blueberry muffin) rash Penumonitis Menignoencephalitis
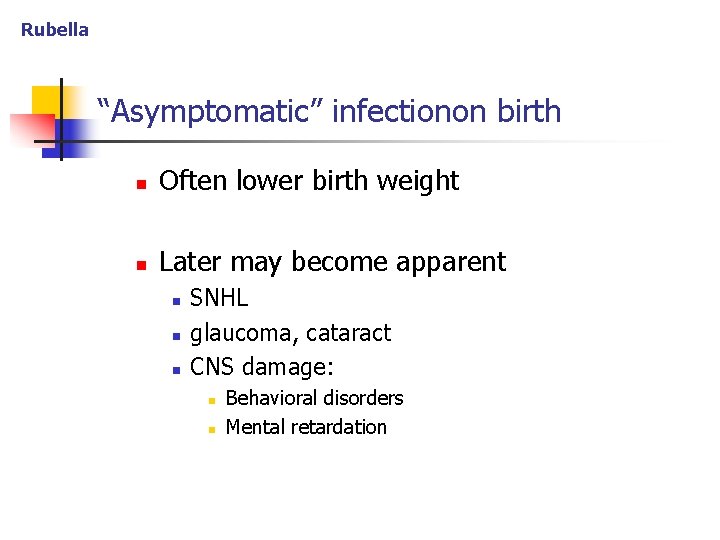
Rubella “Asymptomatic” infectionon birth n Often lower birth weight n Later may become apparent n n n SNHL glaucoma, cataract CNS damage: n n Behavioral disorders Mental retardation
Rubella Diagnosis Postnatally: 1. Serology - detection of antibodies n n Ig. M- evidence of fetal infection n produced only by child Ig. G- Initially can be maternal n later only child’s Ig. G remain 2. Viral culture (throat, urine, blood, CSF …)
Rubella Dijagnosis Prenatally 1. Viral culture of amniotic fluid 2. RNA hybridization from biopsied chorionic vill

Rubeola Prevention n MPR vaccine (live attenuated) 2. during 2 nd year of life at the beginning elementary school n Pregnant women - not to vaccinate: 1. n n viraemia and fetal infection is possible 3 mo. after vaccination pregnancy should be avoided CAUTION: virus is exreted by various body fluids for ≈ 1 year - Keep child away from unvaccinated pregnant woman -
HERPES SIMPLEX VIRUS TYPE 1 AND 2
HSV Epidemiology n 90% of HSV infections occurs during delivery n HSV-2 in 80% of cases n Most often symptoms of genital herpes are absent n n mother’s primary infection = high risk of trassmision recurrent genital heres = low risk of trasmission
Pathogensis n Intrauterine infection (rare) n n Transplacental trasmission from viremic mother dissemination to multiple organs n CNS- most freqently affected
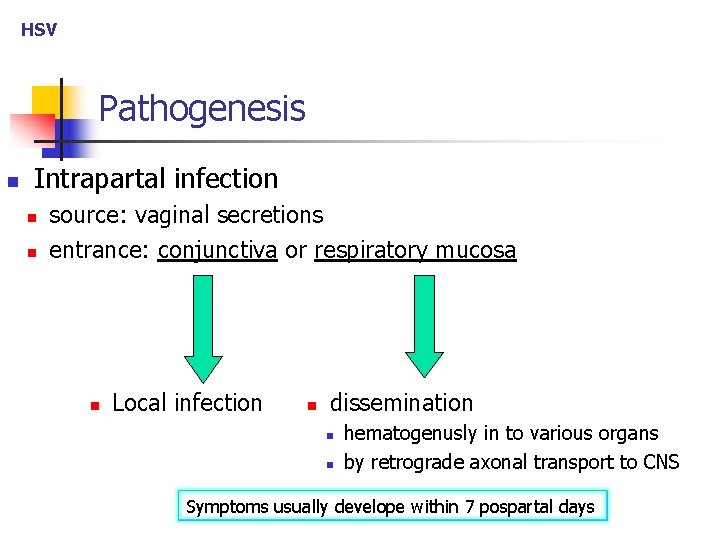
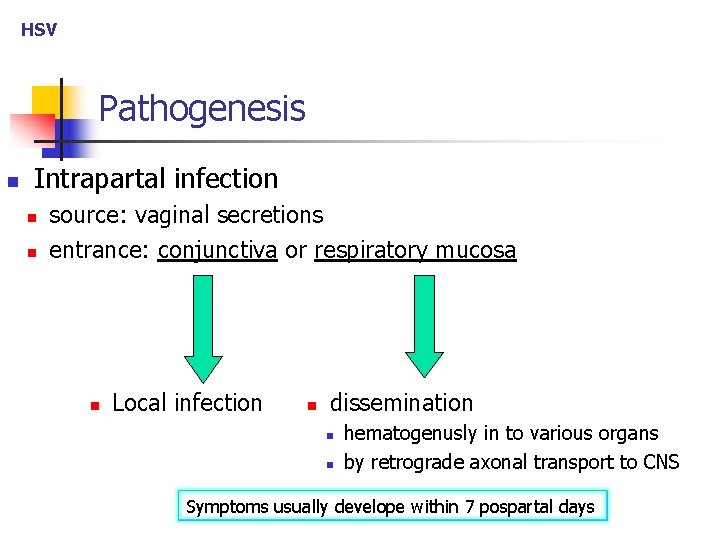
HSV Pathogenesis n Intrapartal infection n n source: vaginal secretions entrance: conjunctiva or respiratory mucosa n Local infection n dissemination n n hematogenusly in to various organs by retrograde axonal transport to CNS Symptoms usually develope within 7 pospartal days
HSV Clical features from Mild disease n vesicles or scarring of skin / mucous membranes …. to severe disease n generalized (disseminated) disease n encephalitis as the only manifestation n pneumonia as the only manifestation
HSV Disseminated disease n hepatitis, myocarditis, pneumonia, encefalitis n chorioretinitis, keratoconjunctivitis n rash (vesicles, bullae) in 70% n facilitate diagnosis

Diagnosis n Specimens: n n n swabs and aspirates of vesicles, conjunctiva, nasopharynx, rectum blood, CSF, urine, stool, Methods n n Viral culture PCR – evidence of viral DNA

Therapy n Aciclovir IV

Prevention: depending on circumstances of infection n n Primary infection of mother n risk for child = 50% n immediately introduce acyclovir therapy for mother!! mother Recurrent genital herpes n obtain swabs for viral dignosis n if symptoms are present - introduce acyclovir to child n otherwise - just follow up

SYPHILIS

Transmission n Hematogenous (transplacental) n n the most common Contact with mother’s chancre during birth n rare
Timing of sympomatic disease n Symptomatic at birth n Late neonatal onest n n Within 5 weeks postpartum Late onset n After 2 years of age
Symptomatic infection at birth n Stillbitrh n Generalised neonatal disease n Low birth weight, hepato-splenomegaly n Nonimmune hydrops + hemolytic anemia n Neutropenia and thromocytopenia
Late neonatal onset n Osteohondritis (metaphysitis), periostitis (new bone) n Rash: maculopapular desquamtive n Syphilitic rhinitis (hemorrhagic) n Hepatitis, lymphocytosis n Keratitis n CSF: pleocytosis + proteinorachia

Late onset: ≥ 2 years after birth Hutchinson triad: n Interstitial keratitis n 8 th n. damage (deafness) n Hutchinson teeth Spaced apart and noched incisors
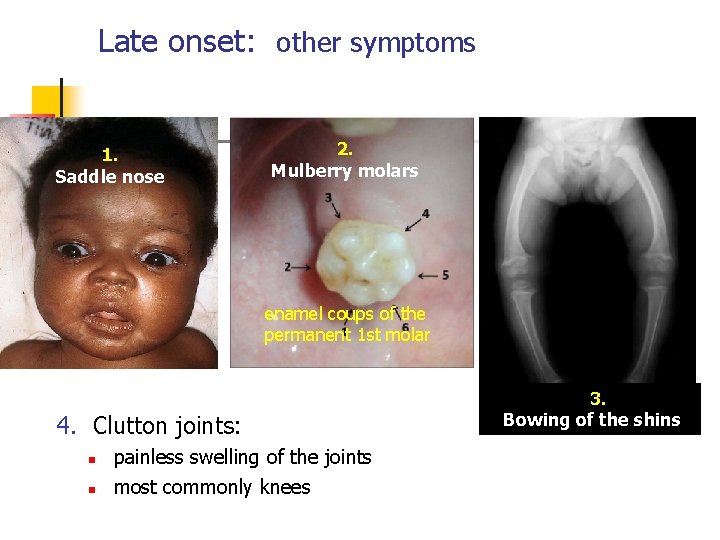
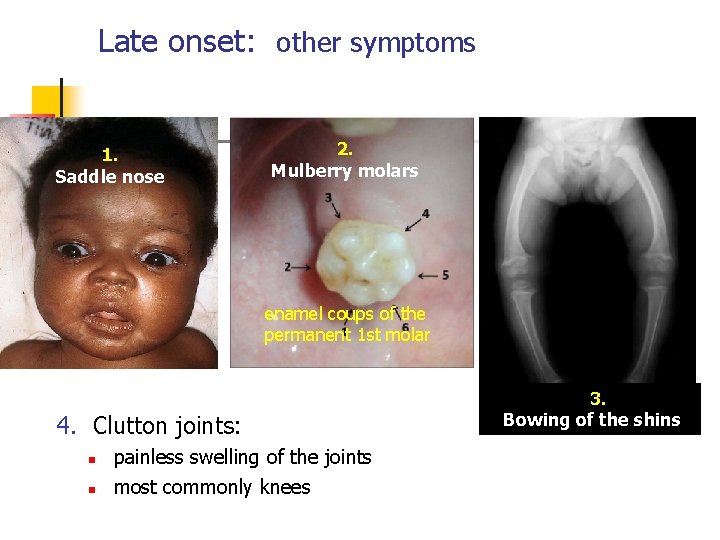
Late onset: other symptoms 1. Saddle nose 2. Mulberry molars enamel coups of the permanent 1 st molar 4. Clutton joints: n n painless swelling of the joints most commonly knees 3. Bowing of the shins
Diagnosis n Serology: n n n Non-treponemal Ab: VDRL, RPR Treponemal Ab: TPHA Who? n n All preganant women All newborns of positive mothers

Further evaluation of the child, if: n mother’s titers incease ≥ 4 -fold n child’s titers ≥ 4 -fold grater than mother’s titers n child of positive mother is asymptomatic n Infecion in late pregnacy- infant may incubate disease If diagnosis of congenital syphilis is estabilshed n LP and CSF serology should bi performed
Therapy n Penicillin G IV / 2 weeks Documeting cure n Falling Ab titers at month 3, 6 and 12 n In case of neurosyphilis: CSF Ab titers n every 6 months /3 years

CHLAMIDIA TRACHOMATIS
Epidemiology n Source: mother with genital infection n Infection occurs during childbirth n n risk for penumonia: up to 20% risk for conjunctivitis: up to 50%
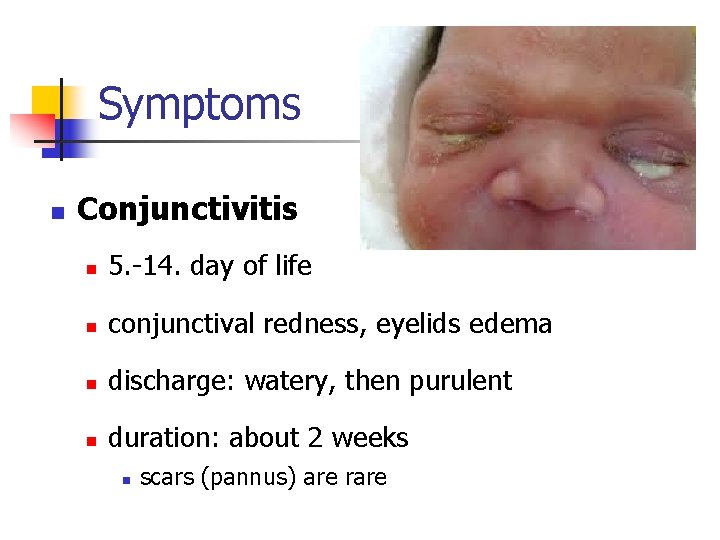
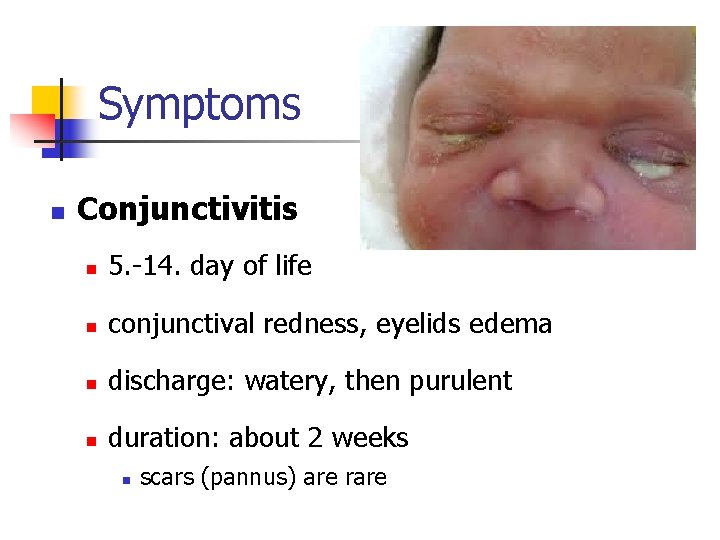
Symptoms n Conjunctivitis n 5. -14. day of life n conjunctival redness, eyelids edema n discharge: watery, then purulent n duration: about 2 weeks n scars (pannus) are rare
n Pneumonia n occurrence: 2 -19 weeks of age No fever dyspnea, attacks of "staccato" cough n chest X-ray: n n diffuse interstitial infiltrations, and hypeinfaltions

Diagnosis n Laboratory findings are nonspecific n slightly higher % eosinophils Pneumonia n serologic evidence Conjunctivitis: conjunctival scraping n n n detection of antigens (DF, ELISA)- usualy Direct microskopy or culture PCR
Differential diagnosis Neisseria gonorrhoeae conjunctivitis n Earlier onset: within first 5 days postpatrum n more serious disease: corneal ulceration
Therapy of Chl. trachomatis n Erythromycin PO /14 dana n Conjunctivitis and penumonia Topical prophylaxis: useless

NEISSERIA GONORHHOEAE
n Conjunctivitis (ophtalmia neonatorum) n n most common Other manifestations: n n n Scalp abscesss Vaginitis Disseminated disease (sepsis, meningitis)
Ophtalmia neonatorum n Onset: within first 5 days of life n Symptoms: n n Early disease: similar to chlamydial conjunctivitis Later: corneal ulceration/perforation Caution! n n the child should be hospitalized disseminated disease should be excluded/treated
Therapy n n Ceftriaxon IM / one dose + Frequent saline eye irrigation n Topical antibiotic? : Needless! Recomanded simultaneous testings for STDs: n n n C. trachomatis Syphilis HIV and HBV
Prophylaxis n Topical administration of : n n n silver nitrate, erytromicyn, or tetracycline
 Erytromicyn
Erytromicyn Iucs
Iucs Metricure intrauterine
Metricure intrauterine Intrauterine device
Intrauterine device Intrauterine device
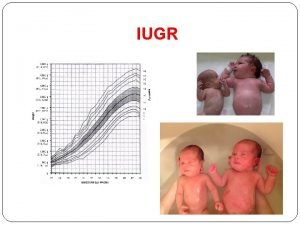
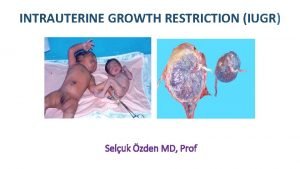
Intrauterine device Symmetrical and asymmetrical iugr
Symmetrical and asymmetrical iugr Asymmetrical intrauterine growth restriction
Asymmetrical intrauterine growth restriction Spalding sign
Spalding sign A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Understanding the mirai botnet
Understanding the mirai botnet Bone and joint infections
Bone and joint infections Methotrexate yeast infection
Methotrexate yeast infection Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Opportunistic infections
Opportunistic infections Opportunistic infections
Opportunistic infections Storch infections
Storch infections Storch infections
Storch infections Infections opportunistes digestives
Infections opportunistes digestives Eye infections
Eye infections Postpartum infections
Postpartum infections Genital infections
Genital infections Amber blumling
Amber blumling Ciliary escalator
Ciliary escalator Acute gingival infections
Acute gingival infections Clear perinatal quality
Clear perinatal quality Grof perinatal matrices
Grof perinatal matrices Fatin organ
Fatin organ Perinatal asphyxia
Perinatal asphyxia Perinatal asphyxia
Perinatal asphyxia Perinatal audit
Perinatal audit Uyarıcı zenginliği ve yoksunluğu nedir
Uyarıcı zenginliği ve yoksunluğu nedir Indiana perinatal quality improvement collaborative
Indiana perinatal quality improvement collaborative Certain conditions originating in the perinatal period
Certain conditions originating in the perinatal period Ccqi perinatal standards
Ccqi perinatal standards South dakota perinatal association
South dakota perinatal association Standing around crying
Standing around crying Perinatal
Perinatal Ruta materno perinatal
Ruta materno perinatal Waiter's tip deformity
Waiter's tip deformity Levene staging
Levene staging Rds pathophysiology
Rds pathophysiology Congenital pneumonia
Congenital pneumonia Piciorul stramb congenital
Piciorul stramb congenital Stumped cornea
Stumped cornea Differential cyanosis
Differential cyanosis Congenital rubella syndrome
Congenital rubella syndrome Congenital malformations
Congenital malformations Congenital voice disorders
Congenital voice disorders Hypothyroidism classification
Hypothyroidism classification Tetralogy of fallot xray
Tetralogy of fallot xray Squatting position in tetralogy of fallot
Squatting position in tetralogy of fallot Congenital fibrosis of the extraocular muscles
Congenital fibrosis of the extraocular muscles Proboscis lateralis
Proboscis lateralis Arytenoid anomaly
Arytenoid anomaly Non classical adrenal hyperplasia
Non classical adrenal hyperplasia Congenital rubella syndrome triad
Congenital rubella syndrome triad Endocardial cushion defect
Endocardial cushion defect Congenital rubella syndrome triad
Congenital rubella syndrome triad Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Congenital hydronephrosis
Congenital hydronephrosis Congenital hydronephrosis
Congenital hydronephrosis Congenital
Congenital Virilisation in females
Virilisation in females Congenital toxoplasmosis
Congenital toxoplasmosis Kode icd 10 palatoschisis
Kode icd 10 palatoschisis Congenital toxoplasmosis
Congenital toxoplasmosis