POSTPARTUM HAEMORRHAGE u With Mother Mortality Ratio of



- Slides: 16
POSTPARTUM HAEMORRHAGE
u With Mother Mortality Ratio of 276 per 100, 000 live births, the country has slipped from 147 to 149 th position, says report u Published in Dawn, May 6 th, 2015
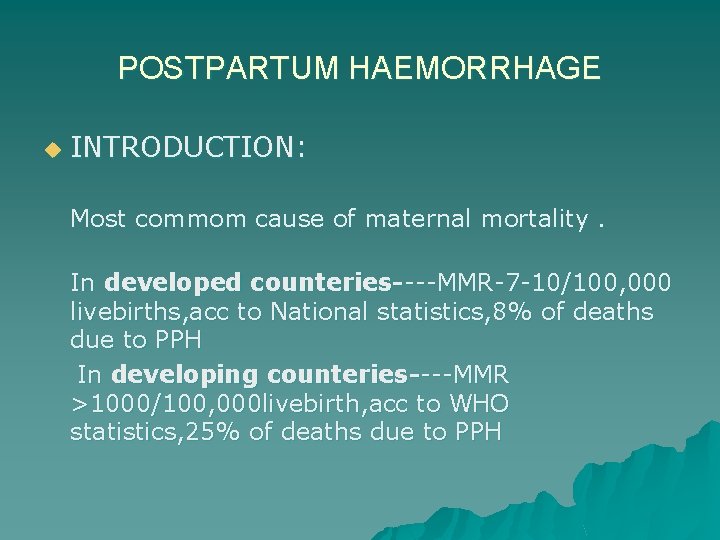
POSTPARTUM HAEMORRHAGE u INTRODUCTION: Most commom cause of maternal mortality. In developed counteries----MMR-7 -10/100, 000 livebirths, acc to National statistics, 8% of deaths due to PPH In developing counteries----MMR >1000/100, 000 livebirth, acc to WHO statistics, 25% of deaths due to PPH
PPH u DEFINATION: Blood loss in excess of 500 ml following a vaginal birth or a loss of greater than 1000 ml following c/section. OR Any blood loss that causes a major physiological change (e. g a fall in b. p)

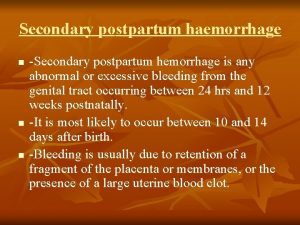
PPH u TYPES: Primary (in 1 st 24 hrs after delivery) Secondary (b/w 24 hrs & 6 -12 weeks postpartum)
PPH u AETIOLOGY: ( 4 Ts) Tone— Tissue— Trauma--Trombin--- .
PPH u RISK FACTORS: Overdistended uterus(multiple pregnancy , polyhydramnios, fetal macrosomia, ) Chorio amnionitis, Prolonged ROM, Prev c/section, APH, Induction of labour , Prolonged labour, Instrumental delivery , Prev H/O PPH , Coagulation disorders.
PPH u PATHOPHYSIOLOGY: al sutures or living ligatures Physiologic
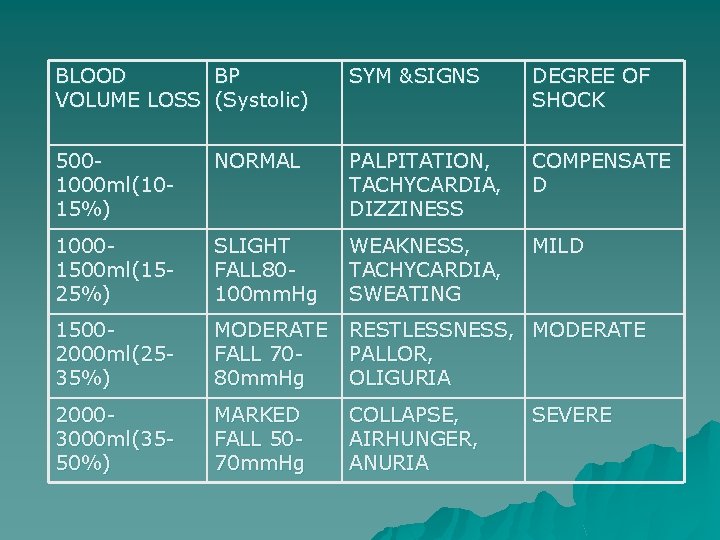
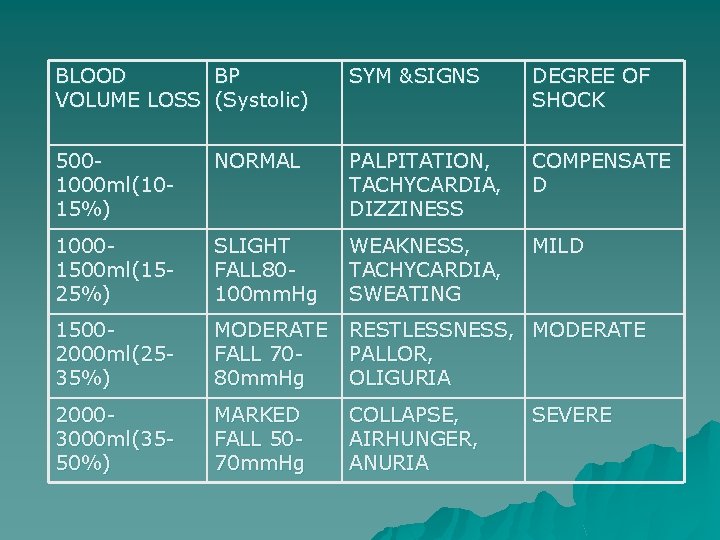
BLOOD BP VOLUME LOSS (Systolic) SYM &SIGNS DEGREE OF SHOCK 5001000 ml(1015%) NORMAL PALPITATION, TACHYCARDIA, DIZZINESS COMPENSATE D 10001500 ml(1525%) SLIGHT FALL 80100 mm. Hg WEAKNESS, TACHYCARDIA, SWEATING MILD 15002000 ml(2535%) MODERATE FALL 7080 mm. Hg RESTLESSNESS, MODERATE PALLOR, OLIGURIA 20003000 ml(3550%) MARKED FALL 5070 mm. Hg COLLAPSE, AIRHUNGER, ANURIA SEVERE
PPH u PREDICTION: Patients with identified risk factors(40%) should be transferred to centres where transfusion facilities & ICU available. Early & prophylactic interventional radiology for high risk. Introduction of strategies for PPH management.
PPH u PREVENTION: Antenatal assesment(anaemia, medical problems, ) Active management of 3 rd stage. (administration of uterotonic drugs, controlled cord traction, uterine massage after delivery of placenta) ACC TO 5 RCT + COCHRANE META ANALYSIS (>6000 WOMEN)----- 60% OF PPH ↓↓ BY ACTIVE MANAGEMENT
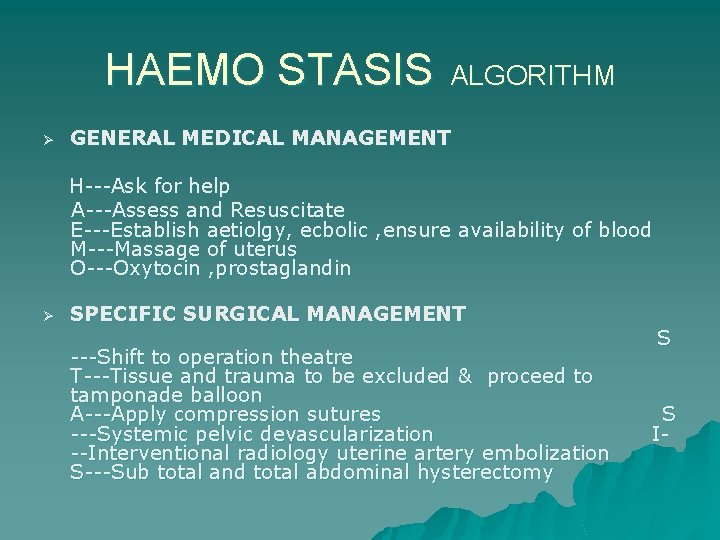
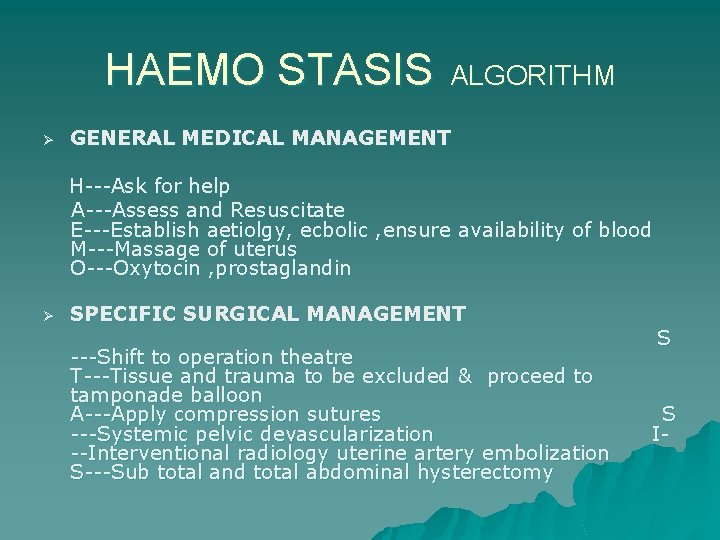
HAEMO STASIS Ø ALGORITHM GENERAL MEDICAL MANAGEMENT H---Ask for help A---Assess and Resuscitate E---Establish aetiolgy, ecbolic , ensure availability of blood M---Massage of uterus O---Oxytocin , prostaglandin Ø SPECIFIC SURGICAL MANAGEMENT ---Shift to operation theatre T---Tissue and trauma to be excluded & proceed to tamponade balloon A---Apply compression sutures ---Systemic pelvic devascularization --Interventional radiology uterine artery embolization S---Sub total and total abdominal hysterectomy S S I-
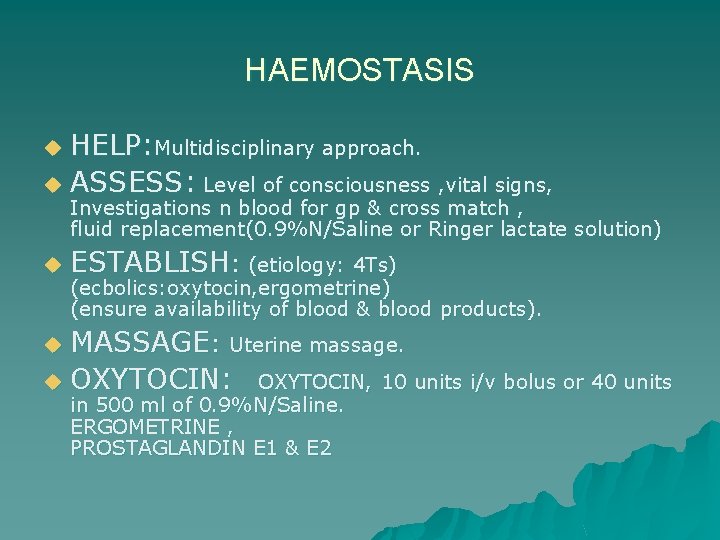
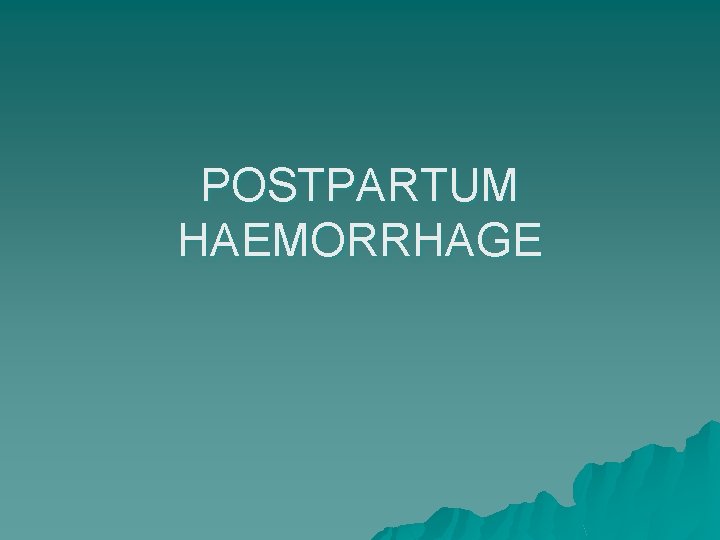
HAEMOSTASIS HELP: Multidisciplinary approach. u ASSESS: Level of consciousness , vital signs, u Investigations n blood for gp & cross match , fluid replacement(0. 9%N/Saline or Ringer lactate solution) u ESTABLISH: (etiology: 4 Ts) (ecbolics: oxytocin, ergometrine) (ensure availability of blood & blood products). MASSAGE: Uterine massage. u OXYTOCIN: OXYTOCIN, 10 units i/v bolus or 40 units u in 500 ml of 0. 9%N/Saline. ERGOMETRINE , PROSTAGLANDIN E 1 & E 2

HAEMOSTASIS u SHIFT: Theatre , anti shock garment, bimanual compression. TISSUE&TRAUMA : to be excluded n proceed to uterine u APPLY COMPRESSION SUTURES: u SYSTEMIC PELVIC DEVASCULARIZATION: u INTERVENTIONAL RADIOLOGY(Uterine artery embolization) Arterial embolisation under fluoroscopic u packing or tamponade with balloon(foley s catheter, other catheters) technique. B –Lynch suture Uterine , ovarian, internal iliac artery ligation. (40 -100% success rate) but expertise , hemodynamically stable pt required. guidance , prophylactic role in adherent placenta is there. u SUBTOTAL /TOTAL HYSTERECTOMY:

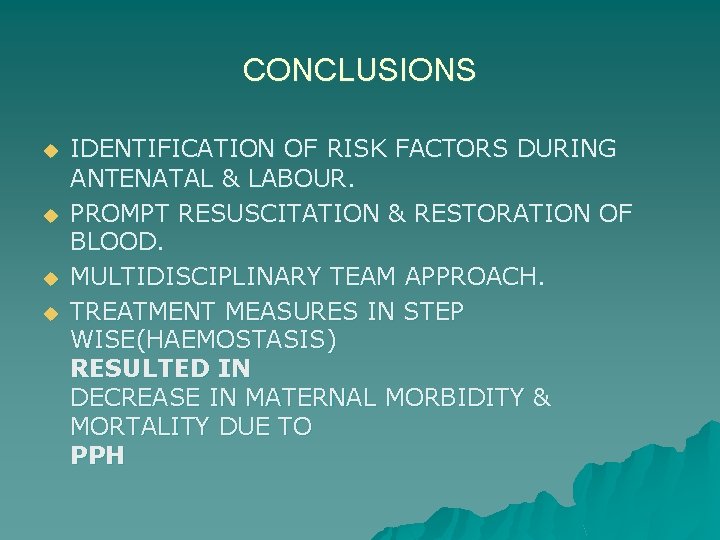
CONCLUSIONS u u IDENTIFICATION OF RISK FACTORS DURING ANTENATAL & LABOUR. PROMPT RESUSCITATION & RESTORATION OF BLOOD. MULTIDISCIPLINARY TEAM APPROACH. TREATMENT MEASURES IN STEP WISE(HAEMOSTASIS) RESULTED IN DECREASE IN MATERNAL MORBIDITY & MORTALITY DUE TO PPH
 Secondary postpartum haemorrhage
Secondary postpartum haemorrhage Secondary postpartum haemorrhage
Secondary postpartum haemorrhage Types of haemorrhage
Types of haemorrhage Cyphalic
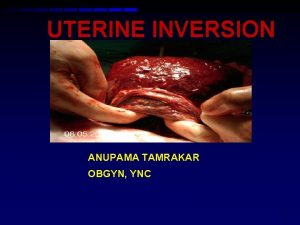
Cyphalic O sullivan hydrostatic method
O sullivan hydrostatic method Cns ischemic response
Cns ischemic response Mk clinical management ug
Mk clinical management ug Yellow smelly discharge postpartum
Yellow smelly discharge postpartum Causes of primary hypothyroidism
Causes of primary hypothyroidism Fundus fiddling
Fundus fiddling Pph treatment algorithm
Pph treatment algorithm Homan signs
Homan signs Postpartum prefix and suffix
Postpartum prefix and suffix Vastus lateralis site for babies
Vastus lateralis site for babies Carbimazole dose
Carbimazole dose Postpartum infection
Postpartum infection Lochia smell
Lochia smell