Hyperthyroid in Pregnancy Dr n mohammadi Fellowship of














- Slides: 60
Hyperthyroid in Pregnancy Dr. n mohammadi Fellowship of fetal medicine
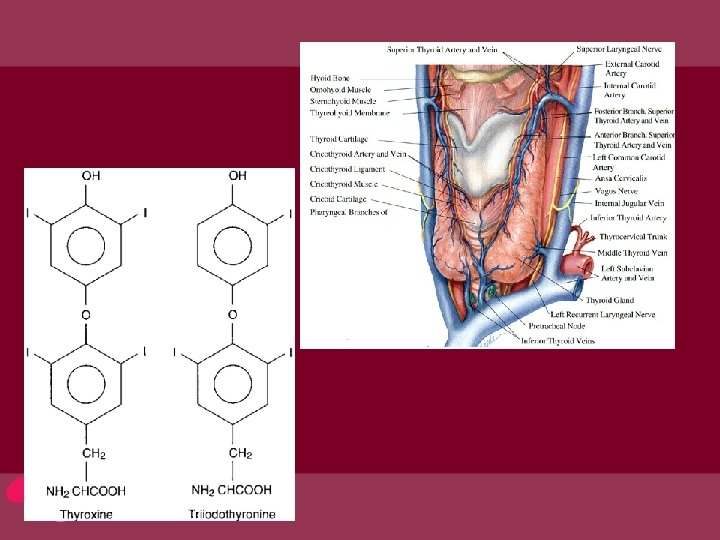
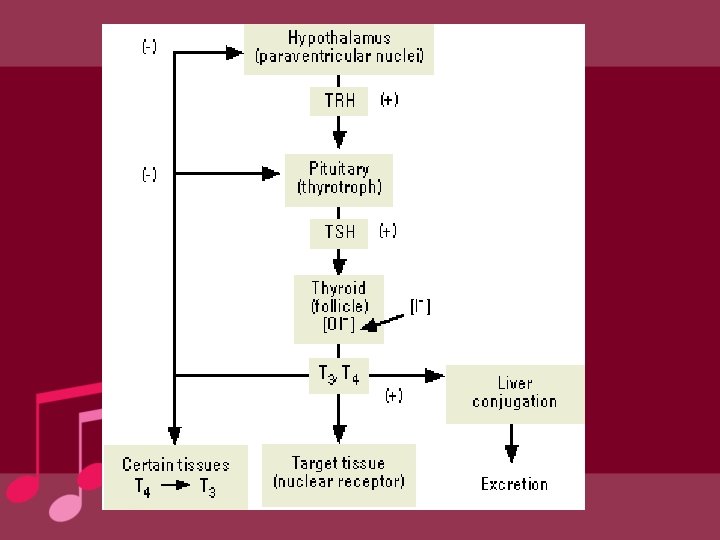
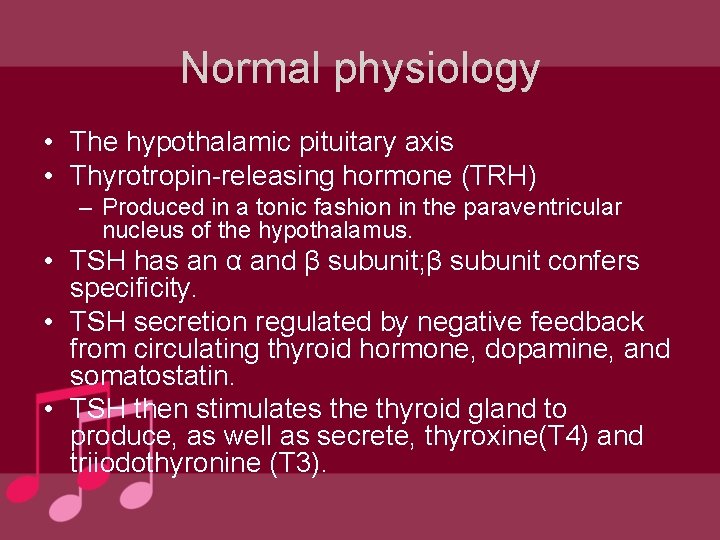
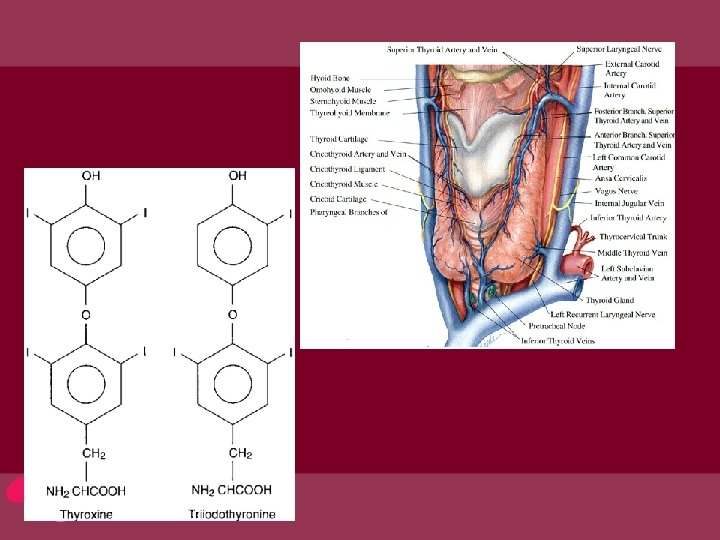
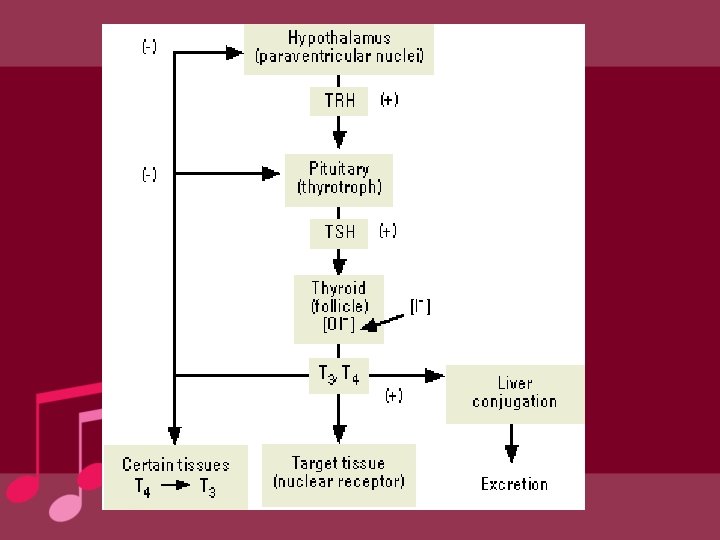
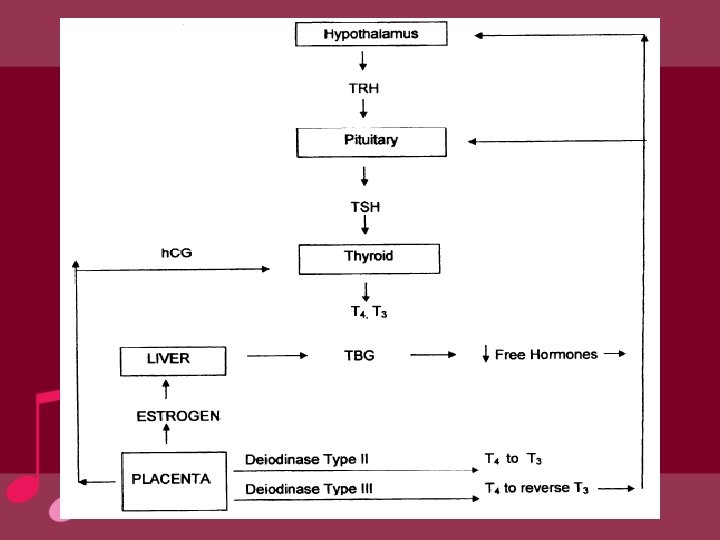
Normal physiology • The hypothalamic pituitary axis • Thyrotropin-releasing hormone (TRH) – Produced in a tonic fashion in the paraventricular nucleus of the hypothalamus. • TSH has an α and β subunit; β subunit confers specificity. • TSH secretion regulated by negative feedback from circulating thyroid hormone, dopamine, and somatostatin. • TSH then stimulates the thyroid gland to produce, as well as secrete, thyroxine(T 4) and triiodothyronine (T 3).
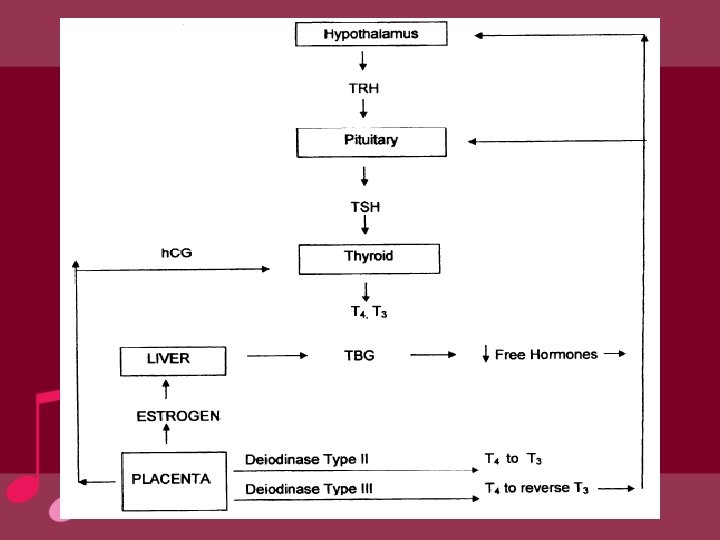
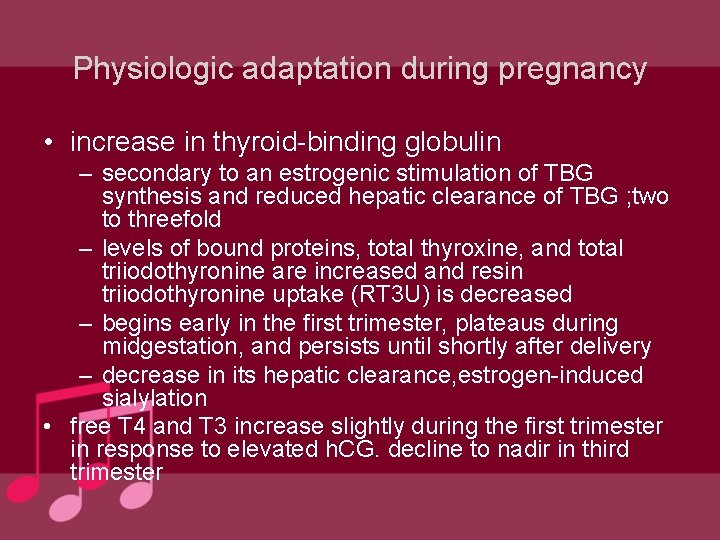
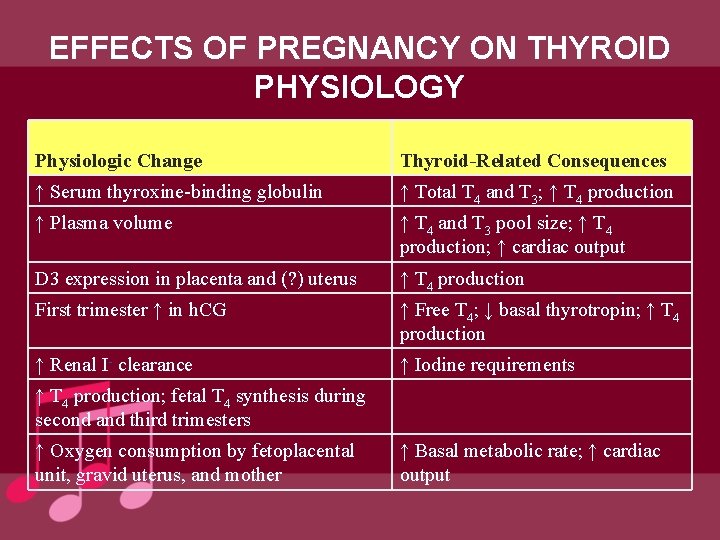
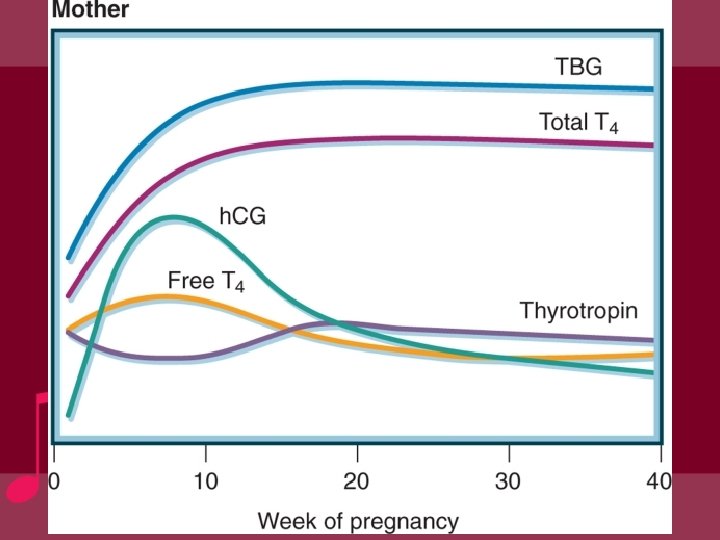
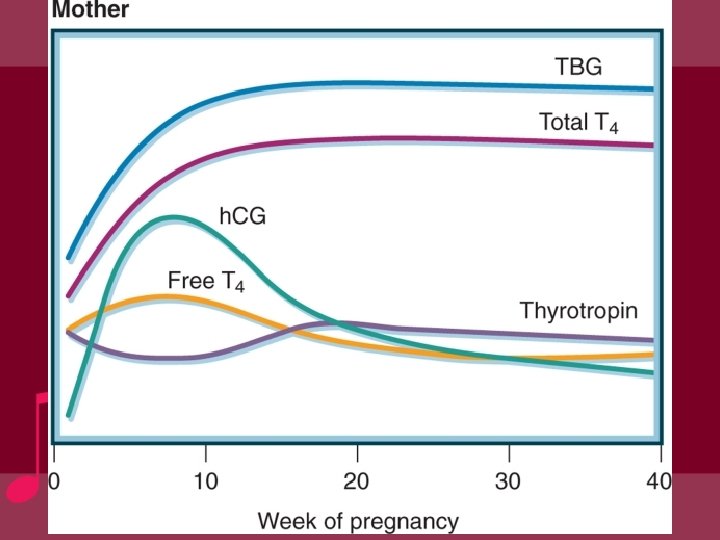
Physiologic adaptation during pregnancy • increase in thyroid-binding globulin – secondary to an estrogenic stimulation of TBG synthesis and reduced hepatic clearance of TBG ; two to threefold – levels of bound proteins, total thyroxine, and total triiodothyronine are increased and resin triiodothyronine uptake (RT 3 U) is decreased – begins early in the first trimester, plateaus during midgestation, and persists until shortly after delivery – decrease in its hepatic clearance, estrogen-induced sialylation • free T 4 and T 3 increase slightly during the first trimester in response to elevated h. CG. decline to nadir in third trimester
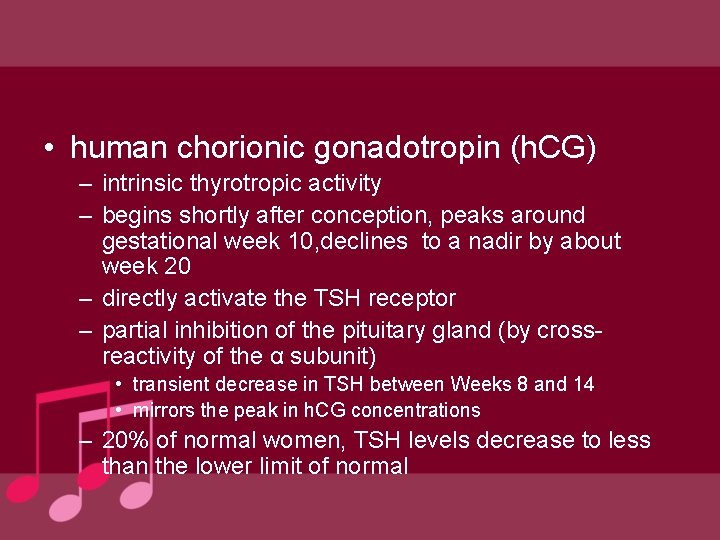
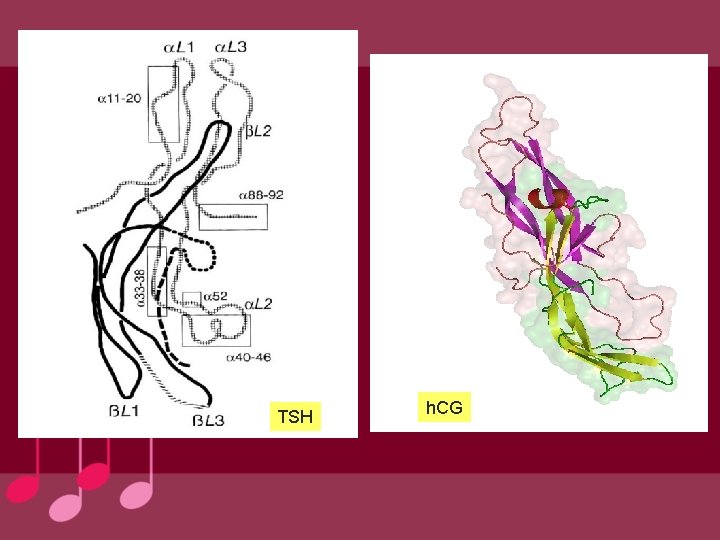
• human chorionic gonadotropin (h. CG) – intrinsic thyrotropic activity – begins shortly after conception, peaks around gestational week 10, declines to a nadir by about week 20 – directly activate the TSH receptor – partial inhibition of the pituitary gland (by crossreactivity of the α subunit) • transient decrease in TSH between Weeks 8 and 14 • mirrors the peak in h. CG concentrations – 20% of normal women, TSH levels decrease to less than the lower limit of normal
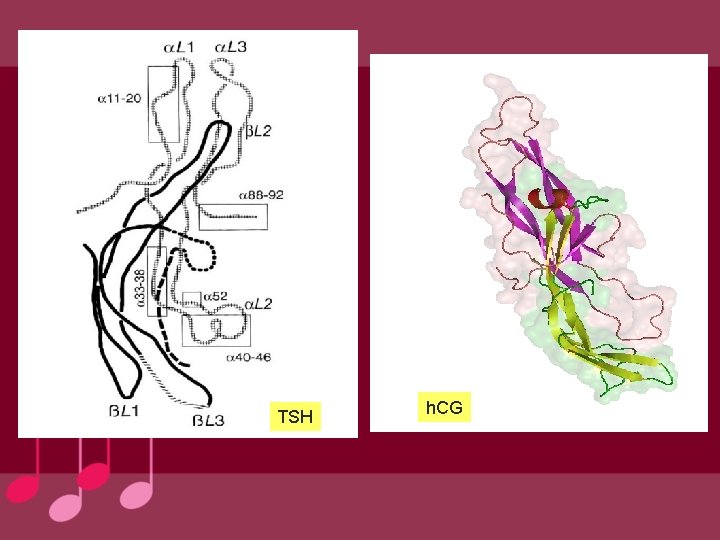
TSH h. CG

• A decrease in basal TSH of 0. 1 m. U/L was observed for every 10, 000 IU/L increment in h. CG • reduction in plasma iodide – fetal : monodeiodinase types II and III in the placenta – increased maternal glomerular filtration rate-increased renal clearance of iodide throughout pregnancy • transplacental passage of T 4 and iodide and placental metabolism of iodothyronines – stimulate the maternal thyroid ; depleting the maternal circulation of thyroid hormone and its precursors
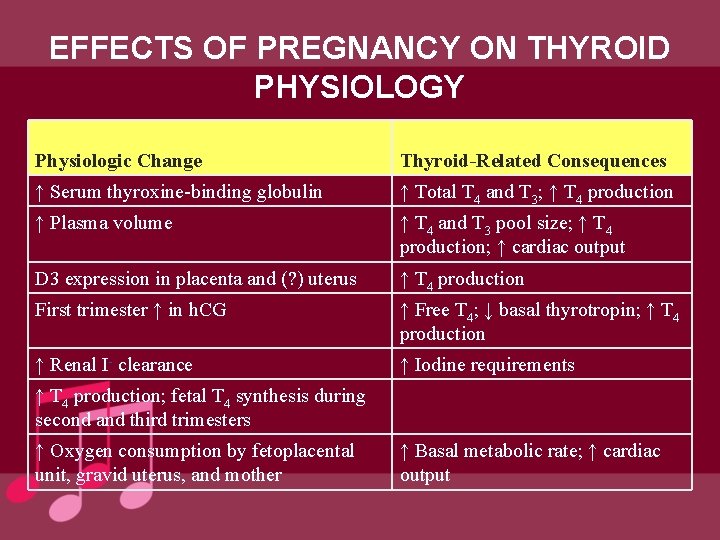
EFFECTS OF PREGNANCY ON THYROID PHYSIOLOGY Physiologic Change Thyroid-Related Consequences ↑ Serum thyroxine-binding globulin ↑ Total T 4 and T 3; ↑ T 4 production ↑ Plasma volume ↑ T 4 and T 3 pool size; ↑ T 4 production; ↑ cardiac output D 3 expression in placenta and (? ) uterus ↑ T 4 production First trimester ↑ in h. CG ↑ Free T 4; ↓ basal thyrotropin; ↑ T 4 production ↑ Renal I- clearance ↑ Iodine requirements ↑ T 4 production; fetal T 4 synthesis during second and third trimesters ↑ Oxygen consumption by fetoplacental unit, gravid uterus, and mother ↑ Basal metabolic rate; ↑ cardiac output
Screening for Thyroid Disease in Pregnancy A 24 -year-old woman was just diagnosed with her first pregnancy. She enjoys good general health. There is no h/o thyroid disease or Rx. Q: Should she have screening TFT? Thyroid 21: 1081 -1125, 2011
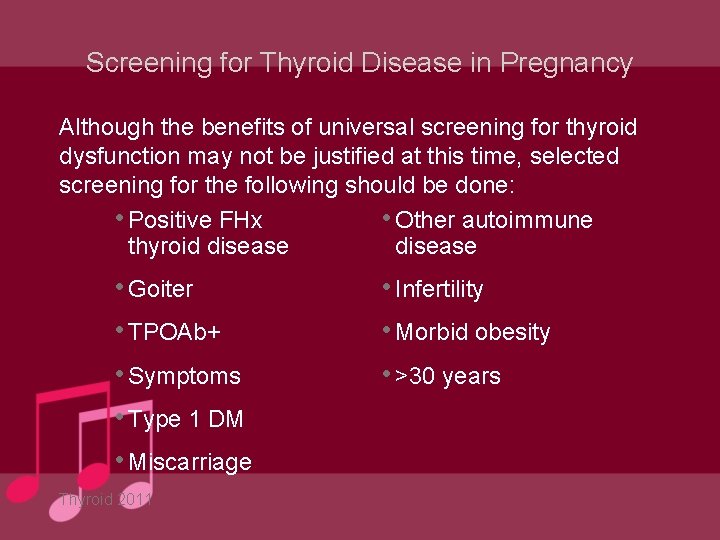
Screening for Thyroid Disease in Pregnancy Although the benefits of universal screening for thyroid dysfunction may not be justified at this time, selected screening for the following should be done: • Positive FHx • Other autoimmune thyroid disease • Goiter • TPOAb+ • Symptoms • Type 1 DM • Miscarriage Thyroid 2011 • Infertility • Morbid obesity • >30 years
TSH in Pregnancy A 28 -year-old woman who is 6 weeks pregnant has a routine serum TSH level of 4. 1 m. IU/L & FT 4 1. 3 ng/d. L Q: Is this TSH normal?
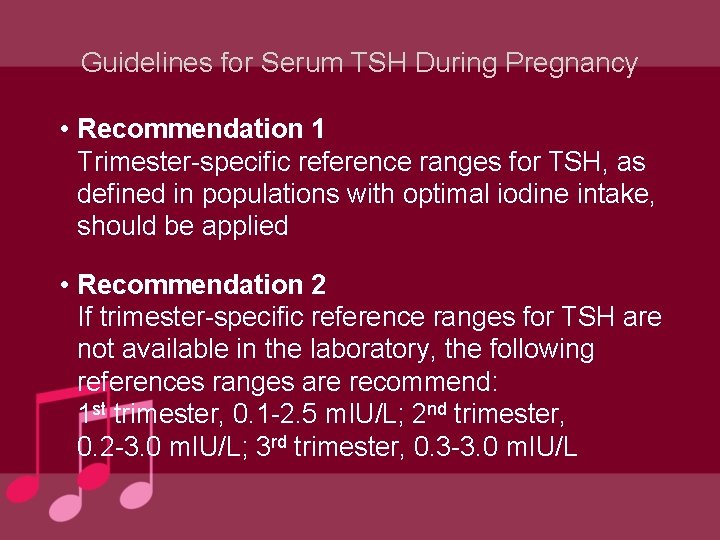
Guidelines for Serum TSH During Pregnancy • Recommendation 1 Trimester-specific reference ranges for TSH, as defined in populations with optimal iodine intake, should be applied • Recommendation 2 If trimester-specific reference ranges for TSH are not available in the laboratory, the following references ranges are recommend: 1 st trimester, 0. 1 -2. 5 m. IU/L; 2 nd trimester, 0. 2 -3. 0 m. IU/L; 3 rd trimester, 0. 3 -3. 0 m. IU/L
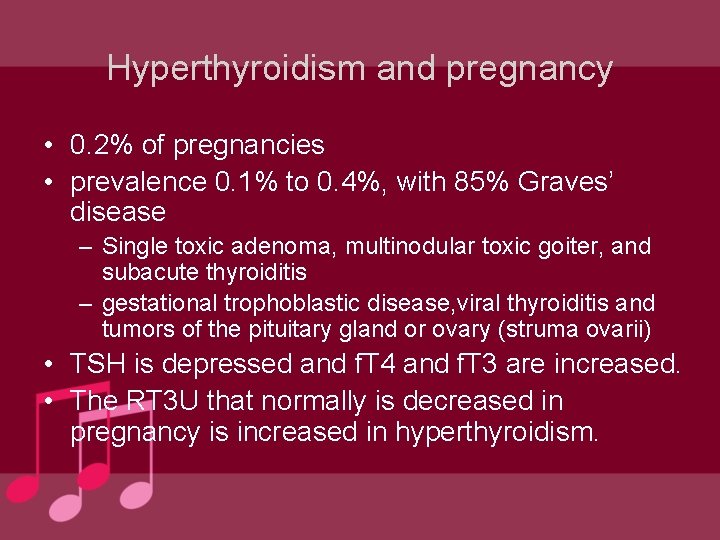
Hyperthyroidism and pregnancy • 0. 2% of pregnancies • prevalence 0. 1% to 0. 4%, with 85% Graves’ disease – Single toxic adenoma, multinodular toxic goiter, and subacute thyroiditis – gestational trophoblastic disease, viral thyroiditis and tumors of the pituitary gland or ovary (struma ovarii) • TSH is depressed and f. T 4 and f. T 3 are increased. • The RT 3 U that normally is decreased in pregnancy is increased in hyperthyroidism.

Hyperthyroidism and pregnancy • serum TSH value <0. 01 m. U/L and also a high serum free T 4 value • may be difficult to determine the cause – thyroid radionuclide imaging is contraindicated in pregnant women. • Measurement of thyrotropin receptor antibody (thyroid stimulating immunoglobulins) Graves' disease during pregnancy • transient hyperthyroidism in hyperemesis gravidarum and gestational transient thyrotoxicity (GTT)


Hyperthyroid manifestations • • Nonspecific symptoms; _Tachycardia _Heat intolerance _Increased perspiration • • Additional symptoms: _Anxiety _Hand tremor _Weigh loss despite a normal or increased appetite

Specific findings: • Goiter • ophthalmopathy
Hyperthyroidism and pregnancy • Severe maternal hyperthyroidism – – – increased risk of stillbirth preterm delivery intrauterine growth restriction Preeclampsia heart failure spontaneous abortion Fetal thyroid hyperfunction or hypofunction caused by TSHRAbs Fetal goiter from excessive antithyroid drug treatment Neonatal thyrotoxicosis Increased perinatal and maternal mortality Decreased IQ of offspring because of excessive use of antithyroid drugs

Transient hyperthyroidism during pregnancy & gestational transient thyrotoxicity (GTT) • hyperemesis gravidarum – severe nausea and vomiting leading to a 5% loss of body weight, dehydration, and ketosis. – absence of goiter and ophthalmopathy, and absence of the common symptoms and signs of hyperthyroidism – higher serum h. CG and estradiol concentrations – 60% have a subnormal serum TSH level (< 0. 4 m. U/L), 50% have an elevated serum free T 4 concentration – Severity positively correlated with maternal free T 4 levels but not to thyroid function. • 12% elevated free T 3 index – believed to be related to h. CG stimulation of the thyroid gland – Normalization of T 4 levels by midgestation. – Treatment is supportive care
• GTT – first trimester – related to h. CG stimulation of the thyroid gland – symptoms of hyperthyroidism and elevated free T 4 levels. – The thyroid gland usually is not enlarged – resolution of symptoms parallels the decline in h. CG levels – usually resolves spontaneously by 20 weeks’ gestation – beyond 20 weeks, repeat evaluation for other causes

Trophoblastic hyperthyroidism • hydatidiform mole (molar pregnancy) & choriocarcinoma. – high serum h. CG concentrations and abnormal h. CG isoforms • 55 to 60 percent had clinically evident hyperthyroidism • normal thyroid gland few symptoms of thyroid hormone excess. • some : findings of hyperthyroidism and a diffuse goiter – ophthalmopathy is not present • Nausea and vomiting may predominate
Trophoblastic hyperthyroidisem • Women with symtomatic moderate to severe hyperthyroidisem due to trophoblastic diseases require treatment. • This include women with total T 4 and total T 3> 1. 5 times the upper limit of nonpregnant women, require antithyroid therapy.
subclinical hyperthyroidism • Low TSH and normal free T 4. • associated with osteoporosis cardiovascular morbidity, and progression to overt thyrotoxicosis and thyroid failure. • not associated with adverse pregnancy outcomes • does not warrant treatment.

Graves’ disease • 95% of thyrotoxicosis during pregnancy. • activity level fluctuate during gestation, with – exacerbation during the first trimester – gradual improvement during the latter half. – exacerbation shortly after delivery • clinical scenarios. – stable Graves’ disease receiving thionamide therapy with exacerbation during early pregnancy. – in remission with a relapse of disease. – without prior history diagnosed with Graves’ disease de novo during pregnancy.

Graves’ disease • Diagnosis – difficult : hypermetabolic symptoms in normal pregnancy – thyroid examination: goiter (with or without bruit) – suppressed serum TSH level and usually elevated free and total T 4 serum concentrations. – TSH receptor antibodi • autoantibodies mimic TSH can cross the placenta and cause neonatal Graves’ disease

Graves’ disease • Pregnancy outcome • preterm labor – untreated (88%)/partially treated(25%) /adequately treated (8%) [ • preeclampsia – untreated twice • stillbirth – untreated (50%) /partially treated (16%) /adequately treated (0%) • small for gestational age • congenital malformations unrelated to thionamide therapy • Mother may have thyroid-stimulating hormone-binding inhibitory immunoglobulin (TBII), – cause transient neonatal hypothyroidism – fetal bradycardia, goiter, and growth restriction
Graves’ disease • Neonatal thyrotoxicosis : – 1% of infants – occur in euthyroid mother or has had surgical or radioactive 131 I treatments before pregnancy – fetal ultrasound to exclude evidence of fetal thyrotoxicosis (eg, an anterior fetal neck mass) or fetal tachycardia. – fetal goiter, advanced bone age, poor growth, and craniosynostosis, Cardiac failure and hydrops – Fetal blood sampling — Fetal blood for thyroid function tests by percutaneous umbilical vein sampling after 20 weeks of gestation • High maternal TSH receptor-stimulating antibody levels Fetal signs suggestive of thyroid disease History of a prior baby with hyperthyroidism
Thyroid storm • • • obstetric emergency extreme metabolic state 10% of pregnant women with hyperthyroidism high risk of maternal cardiac failure. fever, change in mental status, seizures, nausea, diarrhea, and cardiac arrhythmias. • inciting event (eg, infection, surgery, labor/delivery) and a source of infection • treatment immediately, even if serum free T 4, free T 3, and TSH levels are not known. • untreated thyroid storm can be shock, stupor, and coma.
Guidelines for clinical management of maternal hyperthyroidism during pregnancy • 1. Use the lowest dosage of thionamide (preferably PTU) to maintain maternal total T 4 concentrations in the upper one third of normal to slightly elevated range for pregnancy. – Normal range of total T 4 during pregnancy is estimated to be 1. 5 times the nonpregnant state • 2. Monitor maternal total T 4 serum concentration every 2– 4 weeks, and titrate thionamide as necessary. – Monitoring serum TSH may become useful later.
Guidelines for clinical management of maternal hyperthyroidism during pregnancy • 3. Measure TSH receptor antibodies (thyroidstimulating immunoglobulins or TSH receptor binding inhibitory immunoglobulins) at 26– 28 weeks to assess risk of fetal/neonatal hyperthyroidism. – TSH receptor antibody measurement is crucial in hypothyroid levothyroxine-treated women with a prior history of Graves’ disease, who do not appear thyrotoxic. • 4. Perform fetal ultrasound at weeks 26– 28 to assess potential fetal response to thionamide treatment and effect of TSH receptor antibodies on fetal thyroid function
Treatment • Thionamides • propylthiouracil (PTU) and methimazole(MMI) • Both cross the placenta with equal transfer kinetics. • Both can cause fetal goiter and hypothyroidism, usually mild and transient & dose-dependent • median time to normalization of maternal thyroid function – 7 weeks with PTU and 8 weeks with MMI • PTU more highly bound to albumin – theorize that MMI crosses the placenta in higher concentrations
Treatment • Thionamides • maternal : rash • rare birth defects in MMI: aplasia cutis, choanal atresia, esophageal atresia, and minor dysmorphic features • Low thyroid function at birth ½ neonates whose mothers received PTU or MMI and had serum T 4 concentrations within the normal (non-pregnant) range – normal IQ scores • Graves’ disease may ameliorate – thionamide discontinued in 30% during the final weeks – fall in serum TSH receptor-stimulating antibody concentrations and a rise in TSH receptor-blocking antibodies. • Graves' hyperthyroidism can worsen postpartum • do not recommend the use of T 4 with thionamide therapy during pregnancy.
Treatment • β-Adrenergic blockers • weaned as soon as the hyperthyroidism is controlled • occasional cases of neonatal growth restriction, hypoglycemia, respiratory depression, and bradycardia • increased frequency of first-trimester miscarriages • avoiding in the first trimester • Iodides • past reports of neonatal hypothyroidism after exposure to iodine • low-dose potassium iodide may be considered – Preparation for thyroidectomy – thionamide-intolerant patients refusing surgery.
Treatment • Surgery • Subtotal thyroidectomy : – persistently high dosages of thionamides (PTU > 600 mg/d, MMI > 40 mg/d) are required to control maternal disease – allergic or intolerant of both thionamides – noncompliant with medical therapy – compressive symptoms • second trimester, before gestational week 24 • prepared with a β-adrenergic blocking agent and a 10 - to 14 -day course of potassium iodide
Treatment • Radioactive iodine therapy • contraindicated • fetal thyroid gland begins to concentrate iodine after gestational week 10, Fetal thyroid tissue is present by 10 to 12 weeks – predisposing to congenital hypothyroidism • Nursing • Breast feeding in mothers taking PTU or MMI is safe • Thyroid function in newborn infants is unaffected • PTU is preferred because it is less concentrated in breast milk
Up to date_ATA • Suggest that PTU use be limited to first trimester only. • In the second trimester, switching from PTU to MMI • Initial lowest dose: PTU 50 mg two or three times daily and MMI 5 to 10 mg daily.
PTU associated liver failure: • Sudden onset- rapidly progressive • Routine monitoring of LFT is not recommended. • Malaise weakness nausea vomiting jundice dark urine light-colored stools.
A 32 -year-old woman pregnant 10 weeks presents with nausea, vomiting, and a 2 kg weight loss; her first pregnancy 2 years earlier was uncomplicated On exam she is dehydrated, euthyroid, without a goiter and has normal eyes TSH 0. 01 (<2. 5) FT 4 2. 1 (0. 8 -1. 8) FT 4 I 20 (5 -12)
Hyperthyroidism & Pregnancy Conclusions • Hyperemesis gravidarum is HCG-induced, reversible, and dosent requires ATD. • Measure TSH receptor Ab (TRAb), TBII assay • and TOTAL T 3 to distinguish from Graves’ disease.
Hyperthyroidism & Pregnancy • Recommendation 22 When serum TSH is suppressed (<0. 1) in the 1 st trimester, FT 4 should be obtained; TT 3 & TRAb may also be helpful • Recommendation 26 ATDs are not recommended for Rx of gestational hyperthyroidism

Hyperthyroidism & Pregnancy A 32 -year-old woman is 8 weeks pregnant; she reports palpitations, anxiety, heat intolerance and an 8 lb weight loss for 6 months On exam she is nervous, slightly hyperthyroid, has lid lag, and thyroid is x 2 enlarged TSH 0. 01 FT 4 2. 8 FT 4 I 16 (5 -12)
Postpartum thyroid disease • Postpartum thyroiditis – Dx: documenting abnormal TSH (elevated or suppressed) levels during the first year postpartum in the absence of positive TSI or a toxic nodule – hypo- or hyperthyroidism – classic presentation : – transient hyperthyroid phase that occurs 6 weeks to 6 months postpartum – followed by a hypothyroid phase that lasts for up to 1 year postpartum
Postpartum thyroiditis • autoimmune disorder with a self-limited hyperthyroid phase • within one year after parturition. • Presentations – Transient hyperthyroidism alone – Transient hypothyroidism alone – Transient hyperthyroidism followed by hypothyroidism and then recovery. • can also occur after spontaneous or induced abortion • 3 to 16 percent – higher, up to 25 percent, in women with type 1 diabetes mellitus , and in women with positive antithyroid antibodies (normal thyroid function)
Postpartum thyroiditis • like painless thyroiditis – variant form of chronic autoimmune thyroiditis (Hashimoto's thyroiditis). • high serum concentrations of anti-peroxidase antibodies • many eventually become hypothyroid or have a goiter • high serum antithyroid antibody concentrations early in pregnancy – decline later (as immunologic tolerance increases during pregnancy) – rise again after delivery • subclinical thyroid autoimmune disease early in pregnancy and soon after • Progression to permanent hypothyroidism – related to higher TSH concentrations and the antiperoxidase antibody titer – maternal age and female sex of the infant • Postpartum thyroiditis is likely to recur after subsequent pregnancies
• distinguished from Graves' hyperthyroidism, – hyperthyroidism in postpartum thyroiditis is usually mild (both clinically and biochemically), – thyroid enlargement is minimal – Graves' ophthalmopathy is absent. – by reevaluation in three to four weeks: postpartum thyroiditis improved • lymphocytic hypophysitis, – TSH normal or low, low free T 4 – postpartum thyroiditis, TSH elevated with decreased FT 4.

Postpartum thyroiditis • antithyroids : no role. • Hypothyroid : may require treatment and some • significant rate of residual hypothyroidism – Recommend: maintain thyroxine until childbearing is complete, with an attempt to wean off medication 1 year after the last delivery • Postpartum--signs/symptoms of thyroid dysfunction – symptoms mimic normal postpartum changes • TSH, free T 4, and antithyroid antibodies levels • postpartum depression and postpartum thyroiditis
Postpartum Graves’ disease • 60% Graves’ disease in the reproductive years; postpartum onset • euthyroid patients with Graves’ disease with TSI – increased risk of developing recurrent Graves’ disease if antithyroid medication was withheld • TSIs differentiate postpartum Graves’ disease from postpartum thyroiditis with a hyperthyroid component.
Thyroid cancer • Thyroid tumors ; most common endocrine neoplasms. • thyroid cancer accounts for 1% of all cancers. ¾ women; 1/2 reproductive years. • biopsy , Serum TSH and free T 4 levels, ultrasonography & Fine needle aspiration • Radionucleotide scanning is contraindicated during pregnancy • malignant or suspicious for papillary cancer, surgery at the earliest safe period • no evidence that pregnancy causes a reactivation of thyroid cancer or that exposure to radioactive iodine poses a risk to future pregnancies • maintained on thyroid replacement therapy with monitoring of TSH and free T 4 levels every 8 weeks.

Euthyroidism with autoimmune thyroid disease • increased risk for spontaneous miscarriage, subclinical hypothyroidism, and postpartum thyroiditis • Increase in serum TSH levels – most normal • presence of antithyroid antibodies – lack of thyroidal reserve in response to the stimulatory effects of pregnancy.
Euthyroidism with autoimmune thyroid disease • recommend initiating levothyroxine therapy in women with antithyroid antibodies – before pregnancy – TSH level greater than 2. 5 m. U/L. • Serum TSH should be monitored throughout pregnancy in all antithyroid antibody–positive women • maintain the TSH concentration at 2. 5 m. U/L or less.
CLINICAL PRACTICE GUIDELINE Management of Thyroid Dysfunction during Pregnancy and Postpartum: An Endocrine Society Clinical Practice Guideline • 1. HYPOTHYROIDISM AND PREGNANCY: MATERNAL • AND FETAL ASPECTS • 1. 1. 1. maternal hypothyroidism should be avoided. Targeted case finding is recommended at the first prenatalvisit or at diagnosis of pregnancy • 1. 1. 2. If hypothyroidism diagnosed before pregnancy, adjust preconception T 4 dose to reach a TSH ≤ 2. 5 U/ml before pregnancy. • 1. 1. 3. T 4 dose incremented by 4– 6 wk gestation and 30– 50% increase in dosage. • 1. 1. 4. If overt hypothyroidism is diagnosed during pregnancy, thyroid function tests should be normalized as rapidly as possible. – The T 4 dosage should be titrated to rapidly , maintain serum TSH ≤ 2. 5 U/ml in the first trimester (or 3 U/ml in the second and third trimesters) or to trimester-specific normal TSH ranges. – Thyroid function tests remeasured within 30– 40 d.
• 1. 1. 5. Women with thyroid autoimmunity who are euthyroid in the early stages of pregnancy are at risk of developing hypothyroidism and should be monitored for elevation of TSH above the normal range • 1. 1. 6. Subclinical hypothyroidism ; associated with an • adverse outcome for both the mother and offspring. – T 4 treatment - improve obstetrical outcome but has not been proved to modify long-term neurological development in the offspring. – Recommends T 4 replacement in women with subclinical hypothyroidism. • 1. 1. 7. After delivery, most hypothyroid women need a • decrease in the T 4 dosage they received during pregnancy
• 3. GESTATIONAL HYPEREMESIS AND HYPERTHYROIDISM • 3. 1. Thyroid function tests should be measured in all patients with hyperemesis gravidarum (5% weight loss, dehydration, and ketonuria) • 3. 2. Few women with hyperemesis gravidarum will require ATD treatment. • Overt hyperthyroidism believed due to coincident Graves’ disease should be treated with ATD. • Gestational hyperthyroidism with clearly elevated thyroid hormone levels (free T 4 above the reference range or total T 4 150% of top normal pregnancy value and TSH 0. 1 U/ml) and evidence of hyperthyroidism may require treatment as long as clinically necessary • 4. AUTOIMMUNE THYROID DISEASE AND MISCARRIAGE • 4. 1. universal screening for antithyroid antibodies and possible treatment cannot be recommended at this time.
• 6. IODINE NUTRITION DURING PREGNANCY • 6. 1. Women of childbearing age ; average iodine intake 150 g/d. • pregnancy and breastfeeding women should increase intake to 250 g • 6. 2. Iodine intake during pregnancy and breastfeeding should not exceed twice the daily recommended nutritional intake for iodine, i. e. 500 g iodine per day • 6. 3. To assess the adequacy of the iodine intake during pregnancy in a population, urinary iodine concentration should be measured in a cohort of the population. – Urinary iodine concentration should ideally range between 150 and 250 g/liter. • 6. 4. To reach the daily recommended nutrient intake for iodine, multiple means must be considered, tailored to the iodine intake level in a given population. – 1) countries with iodine sufficiency and/or with a well established universal salt iodization (USI) program, – 2) countries without a USI program or an established USI program where the coverage is known to be only partial, and finally – 3) remote areas with no accessible USI program and difficult socioeconomic conditions.

• 8. SCREENING FOR THYROID DYSFUNCTION DURING PREGNANCY • 1. Women with a history of hyperthyroid or hypothyroid disease, PPT, or thyroid lobectomy. • 2. Women with a family history of thyroid disease. • 3. Women with a goiter. • 4. Women with thyroid antibodies (when known). • 5. Women with symptoms or clinical signs suggestive of thyroid underfunction or overfunction, including anemia, elevated cholesterol, and hyponatremia.
• 6. Women with type I diabetes. • 7. Women with other autoimmune disorders. • 8. Women with infertility who should have screening with TSH as part of their infertility work -up. • 9. Women with previous therapeutic head or neck irradiation. • 10. Women with a history of miscarriage or preterm delivery.
 Pictures of spotting during pregnancy
Pictures of spotting during pregnancy Rameen mohammadi
Rameen mohammadi Ali akbar mohammadi
Ali akbar mohammadi Graph adt
Graph adt Dr masoud mohammadi
Dr masoud mohammadi Nihr advanced fellowship
Nihr advanced fellowship Church planting leadership fellowship
Church planting leadership fellowship Master fellowship
Master fellowship Umkc som
Umkc som New testament reformation fellowship
New testament reformation fellowship Daggy definition
Daggy definition Brazen grace fellowship
Brazen grace fellowship Full gospel businessmen fellowship
Full gospel businessmen fellowship Hea associate fellowship
Hea associate fellowship Howard shore lighthouse
Howard shore lighthouse Durer melancholia magic square
Durer melancholia magic square Ken emond british academy
Ken emond british academy Cgyg fellowship
Cgyg fellowship Sir henry wellcome postdoctoral fellowship
Sir henry wellcome postdoctoral fellowship Lsu hematology oncology fellowship
Lsu hematology oncology fellowship Epsrc fellowships
Epsrc fellowships Dr lee jong wook fellowship program
Dr lee jong wook fellowship program Six paths to god
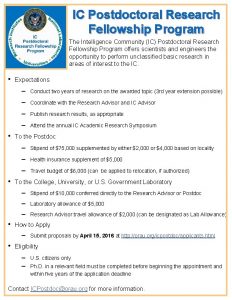
Six paths to god Ic postdoctoral fellowship
Ic postdoctoral fellowship Kingsley bedwell
Kingsley bedwell Family medicine fellowship
Family medicine fellowship Sir henry wellcome postdoctoral fellowships
Sir henry wellcome postdoctoral fellowships Metoda fernaldové
Metoda fernaldové Mrc senior clinical fellowship
Mrc senior clinical fellowship Eafps fellowship
Eafps fellowship Colin powell scholarship
Colin powell scholarship Eth career seed grant
Eth career seed grant Unc
Unc Newton international fellowship success rate
Newton international fellowship success rate Auterbangs
Auterbangs Christian friendship fellowship
Christian friendship fellowship Scnc3111
Scnc3111 Evangel christian fellowship
Evangel christian fellowship Secdef executive fellowship
Secdef executive fellowship Ebenezer bible fellowship church
Ebenezer bible fellowship church Xenos christian fellowship
Xenos christian fellowship Human frontiers postdoctoral fellowship
Human frontiers postdoctoral fellowship Selhurst evangelical church
Selhurst evangelical church Tetfund postdoctoral fellowship
Tetfund postdoctoral fellowship Graduate studies fellowship programs (korea foundation)
Graduate studies fellowship programs (korea foundation) Stanford children's administrative fellowship
Stanford children's administrative fellowship Michael flavin
Michael flavin Brain pool fellowship
Brain pool fellowship Ba postdoctoral fellowship
Ba postdoctoral fellowship Full gospel businessmen fellowship international ghana
Full gospel businessmen fellowship international ghana Ranzcp osce
Ranzcp osce Wharton fellowship program
Wharton fellowship program Esrc new investigator grant success rate
Esrc new investigator grant success rate Future leader fellowship round 7
Future leader fellowship round 7 All the believers were together
All the believers were together Jesus humunculi
Jesus humunculi Secdef executive fellowship
Secdef executive fellowship Sfi industry fellowship
Sfi industry fellowship Ent fellowship europe
Ent fellowship europe Fiu intelligence fellowship
Fiu intelligence fellowship Full gospel businessmen fellowship international - ghana
Full gospel businessmen fellowship international - ghana