Pharmacologic Treatment of Anxiety Disorders in Primary Care




- Slides: 52
Pharmacologic Treatment of Anxiety Disorders in Primary Care ©Yvonne Murphy, MD Associate Program Director Mac. Neal Family Medicine Residency 2013 May be used for educational purposes with credit to author.
Educational Objectives n n n ©Yvonne Murphy, MD Describe the types of presenting symptoms of anxiety disorders Name a validated screening test for GAD, PTSD, and SAD List the best non pharmacologic and the best class of pharmacologic treatments for anxiety Explain principles of initiating SSRI/SNRI use for anxiety treatment Explain general principles of prescribing benzodiazapines for anxiety
Anxiety Disorders – Prevalence n Social Phobia q n n 7% lifetime prevalence (10% women; 5% men) Panic Disorder q n 3% of primary care patients (1 in 30 people) PTSD q n 7% of primary care patients (1 of 13 people) Generalized Anxiety Disorder q n ©Yvonne Murphy, MD 2% lifetime prevalence 2: 1 ratio women to men; usual onset teens/20 s Family history in a first degree relative significantly increases risk
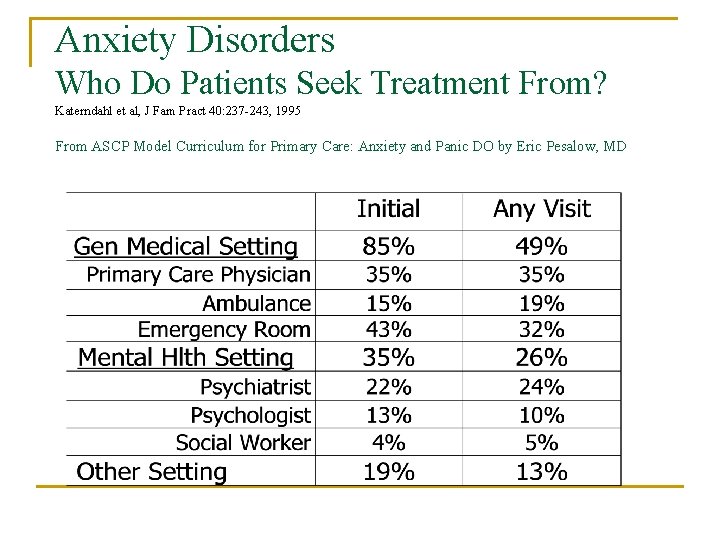
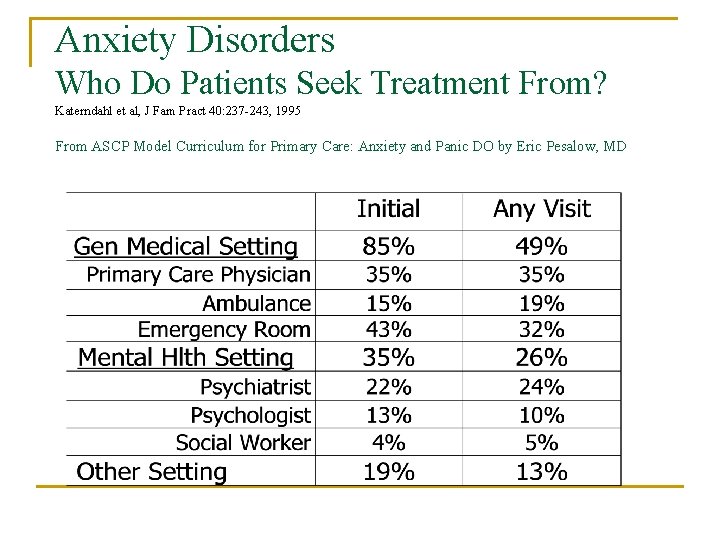
Anxiety Disorders Who Do Patients Seek Treatment From? Katerndahl et al, J Fam Pract 40: 237 -243, 1995 From ASCP Model Curriculum for Primary Care: Anxiety and Panic DO by Eric Pesalow, MD

Anxiety Disorders: KEY POINT- How do patients present? Katon et al, Am J Med 77: 101 -106, 1984 From ASCP Model Curriculum for Primary Care on Anxiety and Panic DO by Eric Pesalow, MD
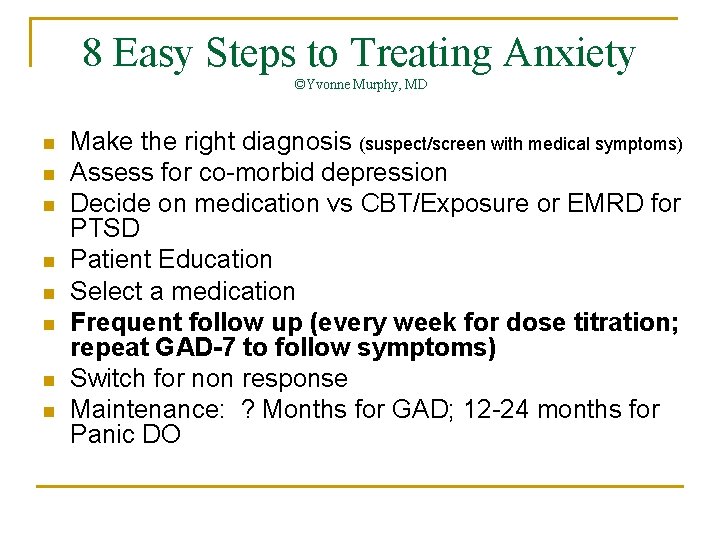
8 Easy Steps to Treating Anxiety with Medication ©Yvonne Murphy, MD n Make the right diagnosis q n n n n suspect/screen with medical symptoms Assess for co-morbid depression Decide on medication vs CBT/Exposure or EMRD for PTSD Patient Education Base selection of medication on individual patient factors (gender, co morbid medical conditions and medications, worst symptoms) Frequent follow up (1 week after initiation) Switch for non response Maintenance
Anxiety Disorders Making the Correct Diagnosis From ASCP Model Curriculum for Primary Care on Anxiety and Panic DO by Eric Pesalow, MD n Prevalence of Irritable Bowel Syndrome in the US is 10 -17% n 29% of patients with IBS have anxiety n 44% of patients with anxiety have IBS n Both syndromes improve with treatment of anxiety --Drossman et al, Ann Int Med 23: 688 -697, 1995 --Lydiard et al, Psychosom 24: 229 -234, 1993
Anxiety Disorders Making the Correct Diagnosis From ASCP Model Curriculum for Primary Care on Anxiety and Panic DO by Eric Pesalow, MD Chest Pain: n Anxiety with true ischemia (50%) n Anxiety with normal coronary arteries (60%) Beitman et al, Arch Int Med 147 -1548 -1552, 1987
Anxiety Disorders Making the Correct Diagnosis From ASCP Model Curriculum for Primary Care on Anxiety and Panic DO by Eric Pesalow, MD Paroxysmal Atrial Tachycardia n 59/107 misdiagnosed (32 panic, anxiety, stress) n Delay in diagnosis of 3 years, 4 months n Resolution of anxiety symptoms is 90% with Rx of PAT Lessmeier et al Arch Int Med 157: 537 -543, 1997
Anxiety Disorders Making the Correct Diagnosis From ASCP Model Curriculum for Primary Care on Anxiety and Panic DO by Eric Pesalow, MD n Normal Part of the Human Experience • n Primary Anxiety Disorder • • • n Life circumstances, Stress (make sure they have a true dx) Generalized Anxiety Disorder Panic Disorder Obsessive Compulsive Disorder Phobias Post Traumatic Stress Disorder Secondary Anxiety Disorder • • Substance induced Due to medical conditions
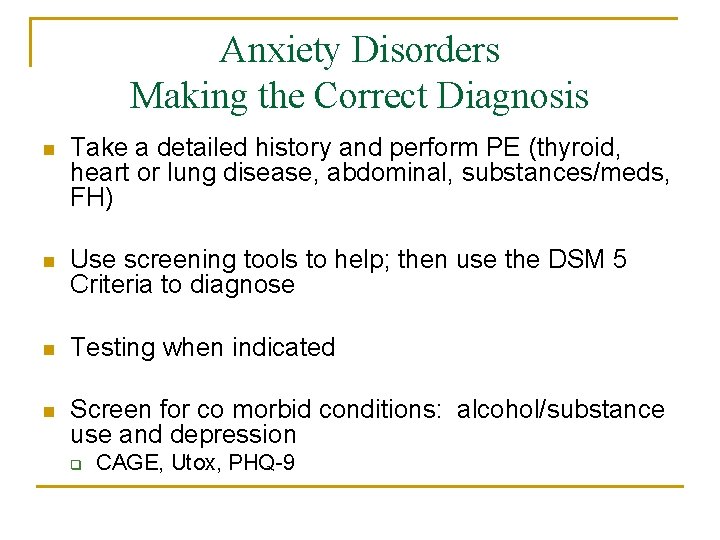
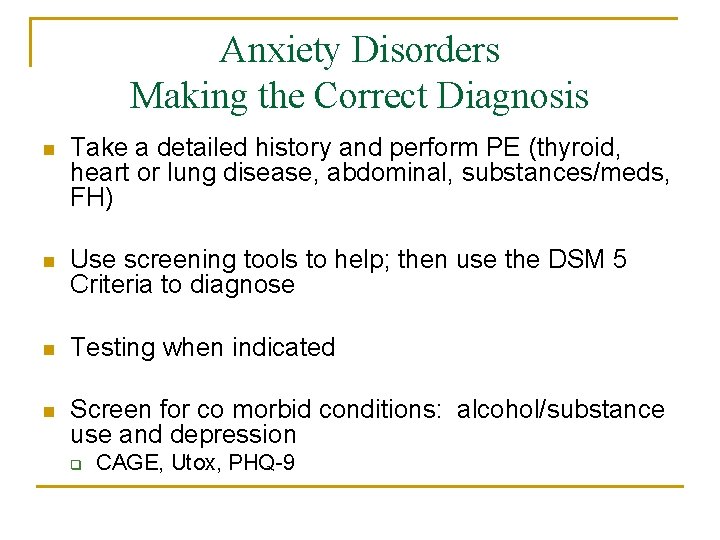
Anxiety Disorders Making the Correct Diagnosis n Take a detailed history and perform PE (thyroid, heart or lung disease, abdominal, substances/meds, FH) n Use screening tools to help; then use the DSM 5 Criteria to diagnose n Testing when indicated n Screen for co morbid conditions: alcohol/substance use and depression q CAGE, Utox, PHQ-9
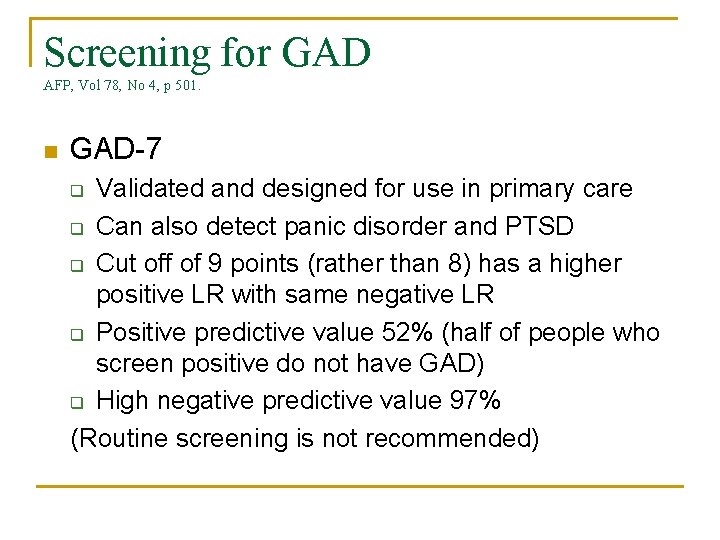
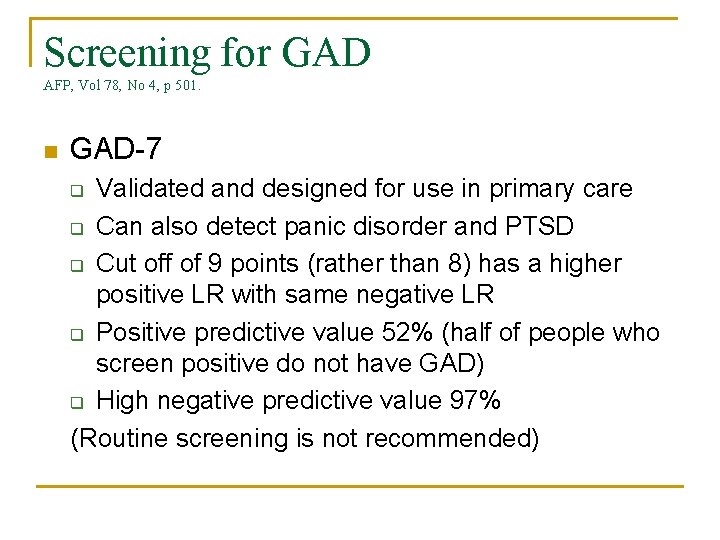
Screening for GAD AFP, Vol 78, No 4, p 501. n GAD-7 Validated and designed for use in primary care q Can also detect panic disorder and PTSD q Cut off of 9 points (rather than 8) has a higher positive LR with same negative LR q Positive predictive value 52% (half of people who screen positive do not have GAD) q High negative predictive value 97% (Routine screening is not recommended) q
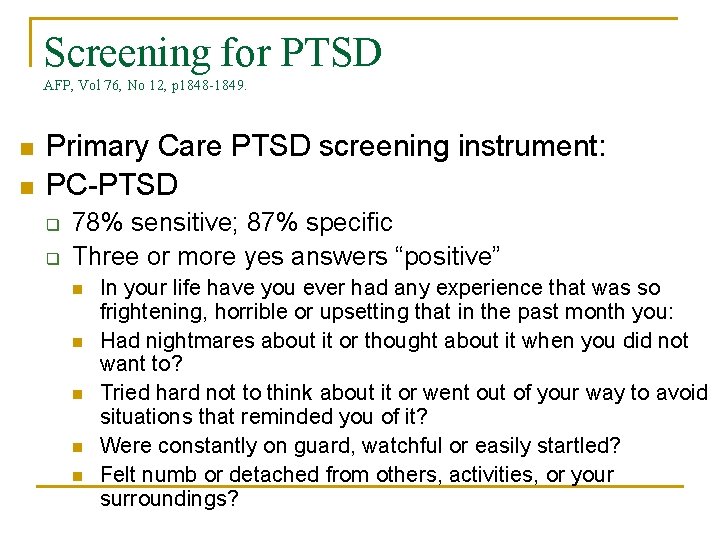
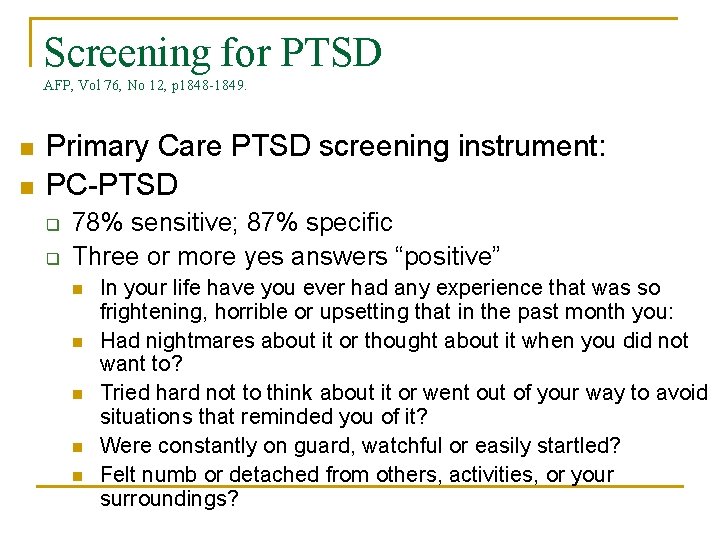
Screening for PTSD AFP, Vol 76, No 12, p 1848 -1849. n n Primary Care PTSD screening instrument: PC-PTSD q q 78% sensitive; 87% specific Three or more yes answers “positive” n n n In your life have you ever had any experience that was so frightening, horrible or upsetting that in the past month you: Had nightmares about it or thought about it when you did not want to? Tried hard not to think about it or went out of your way to avoid situations that reminded you of it? Were constantly on guard, watchful or easily startled? Felt numb or detached from others, activities, or your surroundings?
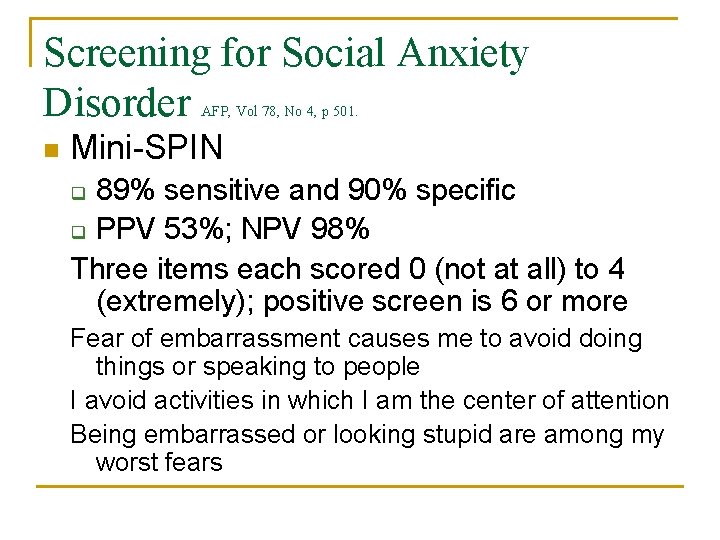
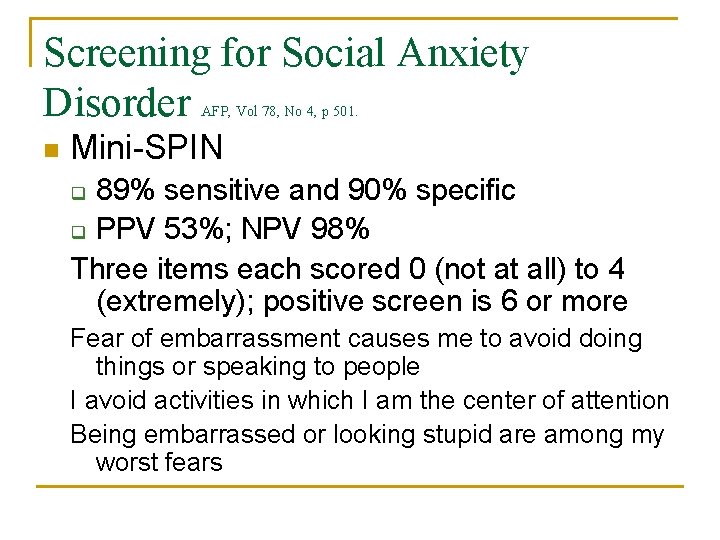
Screening for Social Anxiety Disorder AFP, Vol 78, No 4, p 501. n Mini-SPIN 89% sensitive and 90% specific q PPV 53%; NPV 98% Three items each scored 0 (not at all) to 4 (extremely); positive screen is 6 or more q Fear of embarrassment causes me to avoid doing things or speaking to people I avoid activities in which I am the center of attention Being embarrassed or looking stupid are among my worst fears
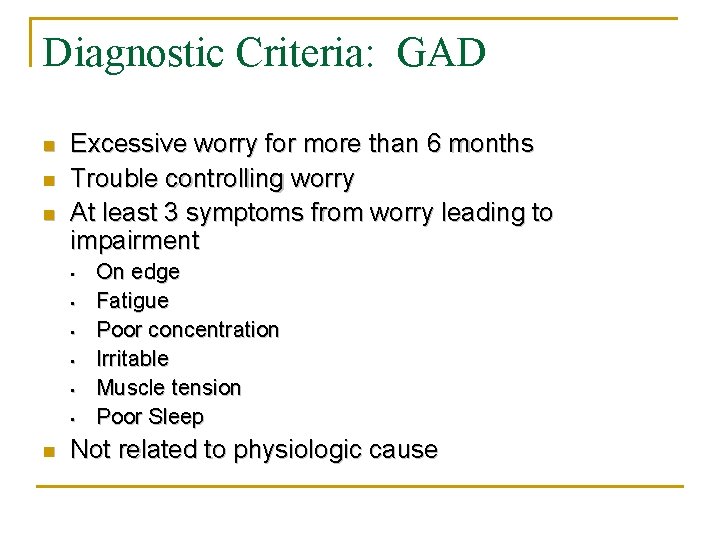
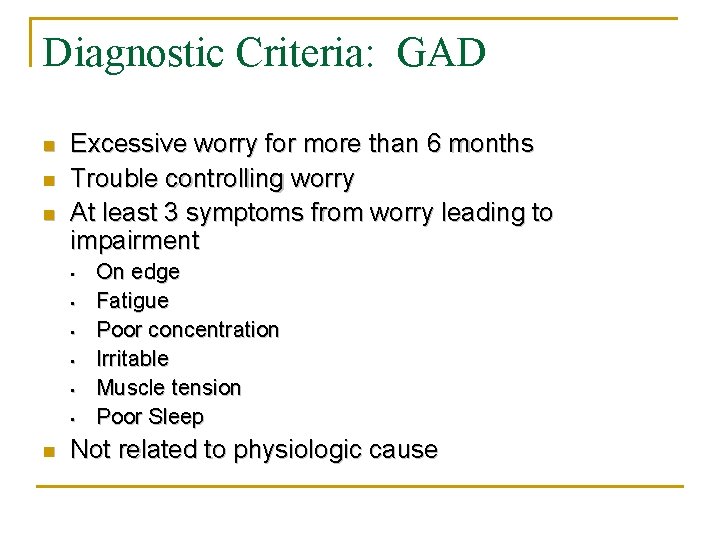
Diagnostic Criteria: GAD n n n Excessive worry for more than 6 months Trouble controlling worry At least 3 symptoms from worry leading to impairment • • • n On edge Fatigue Poor concentration Irritable Muscle tension Poor Sleep Not related to physiologic cause
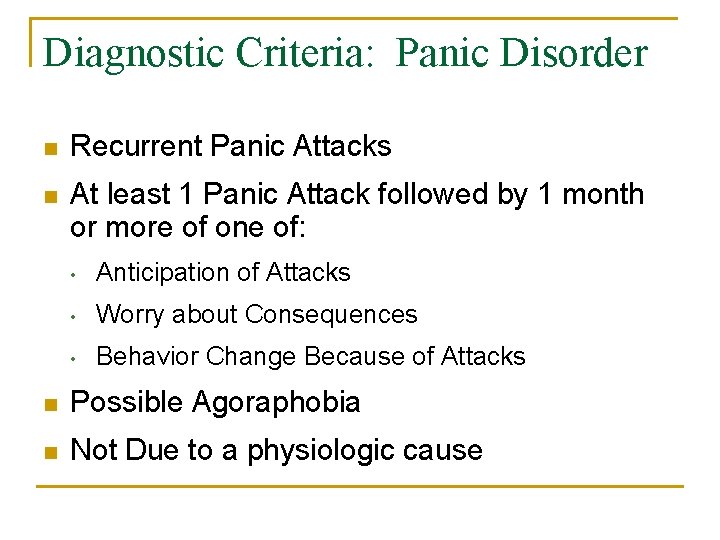
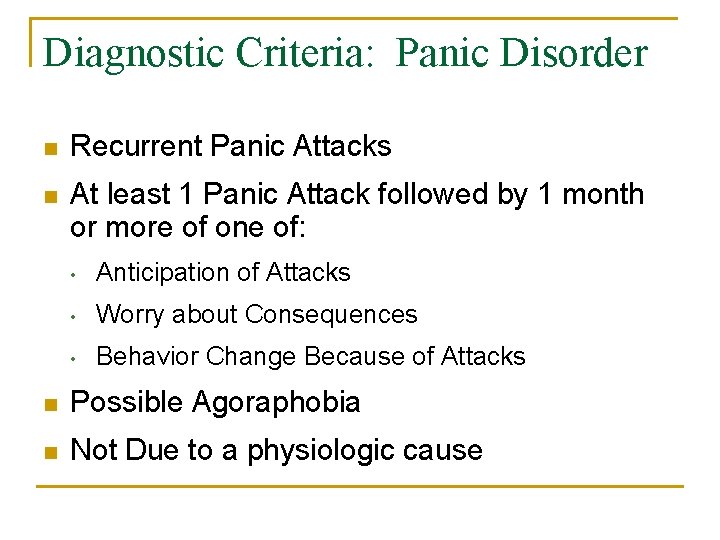
Diagnostic Criteria: Panic Disorder n Recurrent Panic Attacks n At least 1 Panic Attack followed by 1 month or more of one of: • Anticipation of Attacks • Worry about Consequences • Behavior Change Because of Attacks n Possible Agoraphobia n Not Due to a physiologic cause
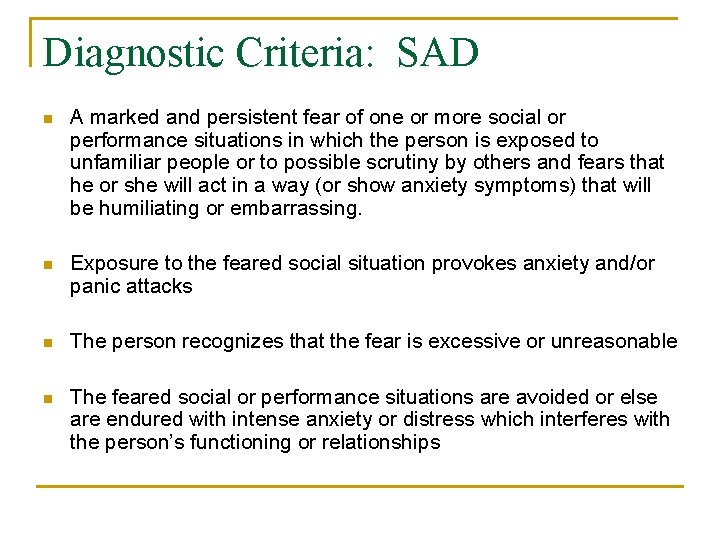
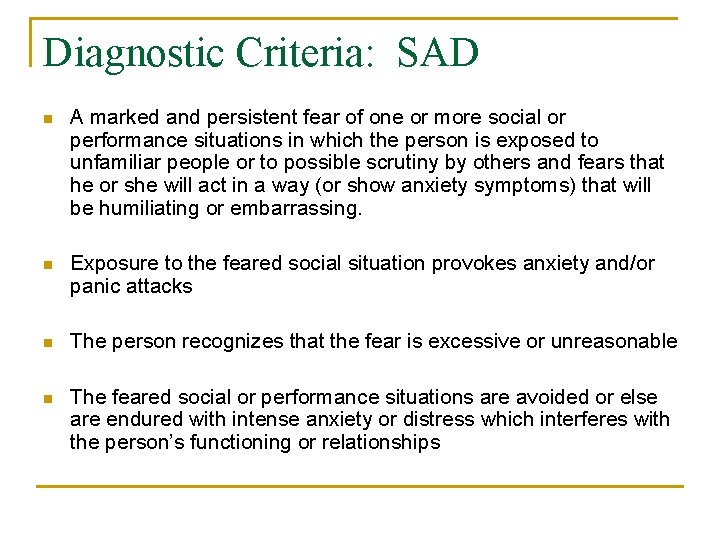
Diagnostic Criteria: SAD n A marked and persistent fear of one or more social or performance situations in which the person is exposed to unfamiliar people or to possible scrutiny by others and fears that he or she will act in a way (or show anxiety symptoms) that will be humiliating or embarrassing. n Exposure to the feared social situation provokes anxiety and/or panic attacks n The person recognizes that the fear is excessive or unreasonable n The feared social or performance situations are avoided or else are endured with intense anxiety or distress which interferes with the person’s functioning or relationships
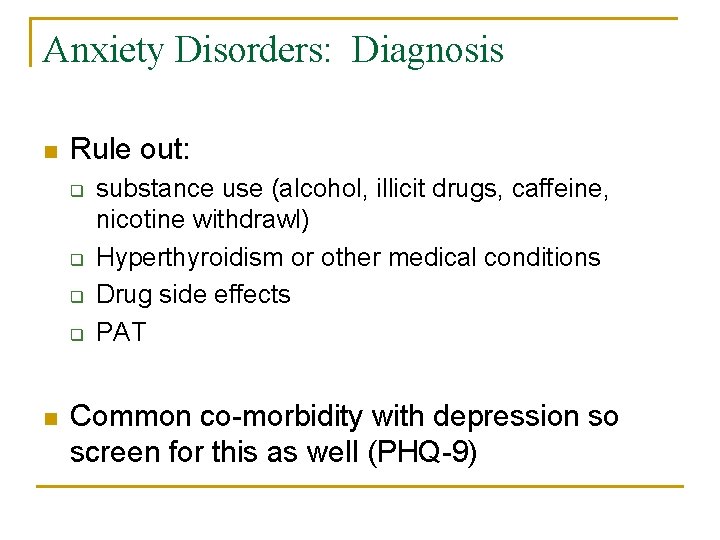
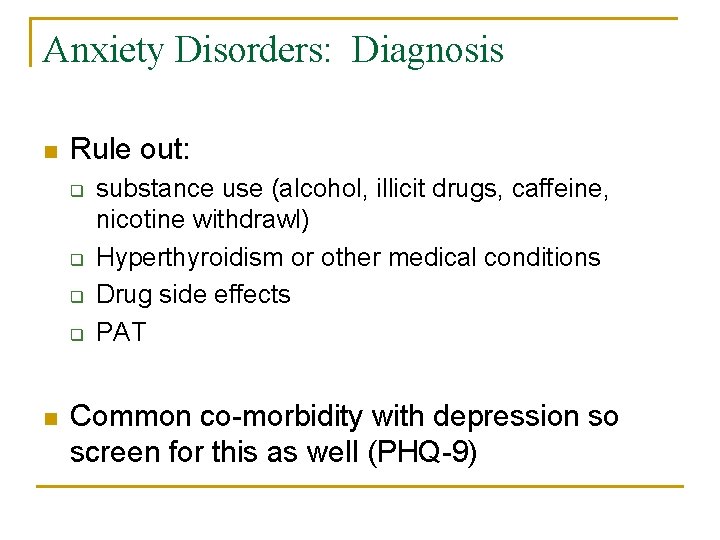
Anxiety Disorders: Diagnosis n Rule out: q q n substance use (alcohol, illicit drugs, caffeine, nicotine withdrawl) Hyperthyroidism or other medical conditions Drug side effects PAT Common co-morbidity with depression so screen for this as well (PHQ-9)
Anxiety Disorders: Natural History n Chronic, waxing/waning, with few complete remissions n Associated with higher utilization of primary care and healthcare services overall n Associated with significant disability
8 Easy Steps to Treating Anxiety ©Yvonne Murphy, MD n n n n Make the right diagnosis Assess for co-morbid depression Decide on medication vs CBT/Exposure or EMRD for PTSD Patient Education Base selection of medication on individual patient factors (gender, co morbid medical conditions and medications, worst symptoms) Frequent follow up (1 week after initiation) Switch for non response After 5 -8 months, assess need maintenance
CBT for Treatment of GAD n n 2005 meta-analysis of 65 randomized and nonrandomized controlled trials with 7739 participants - Level A Evidence CBT was effective for GAD, superior to no treatment (effect size = 0. 82) Treatment effects from CBT persist for 6 -12 months Response rates: q q 56 percent (range = 44 to 71 percent) end of treatment 57 percent (range =39 to 76 percent) at 6 to 12 mo follow-up
Treatment of Generalized Anxiety Disorder: Choices - KEY POINT n Cognitive Behavioral Therapy n n SSRI/SNRI Other: Buspirone, Pregabalin Benzodiazepines n Combination n
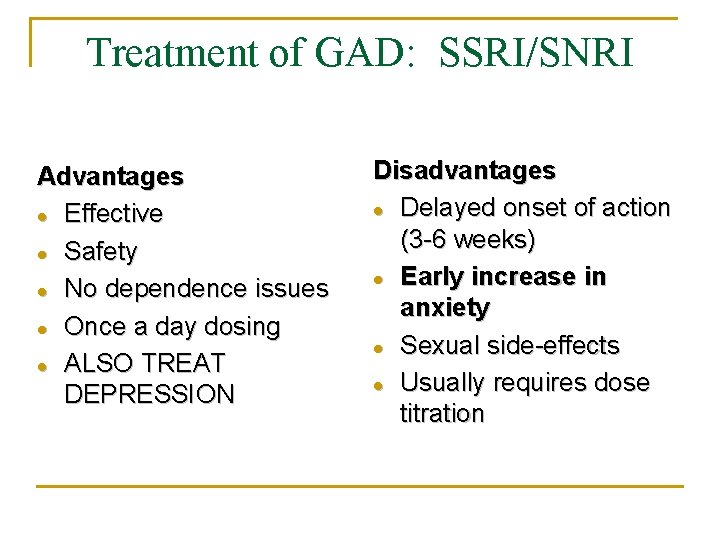
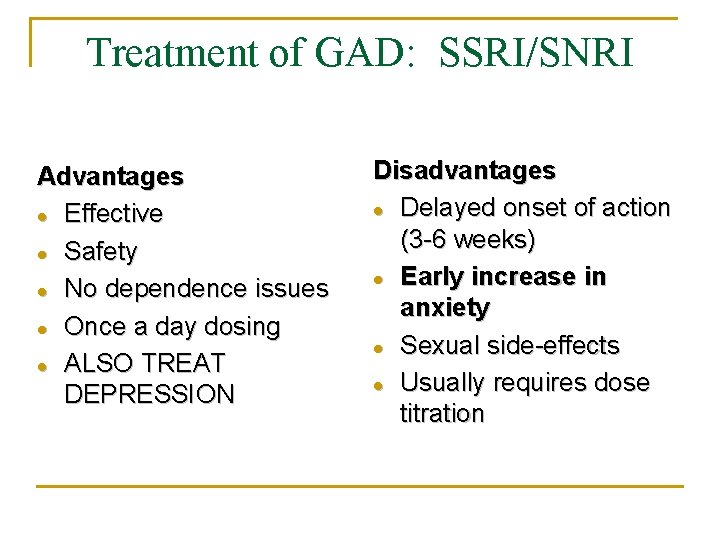
Treatment of GAD: SSRI/SNRI Advantages Effective Safety No dependence issues Once a day dosing ALSO TREAT DEPRESSION Disadvantages Delayed onset of action (3 -6 weeks) Early increase in anxiety Sexual side-effects Usually requires dose titration
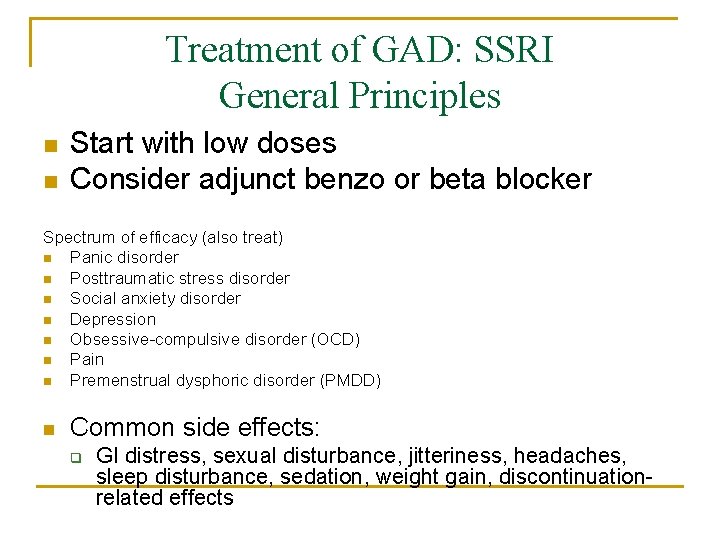
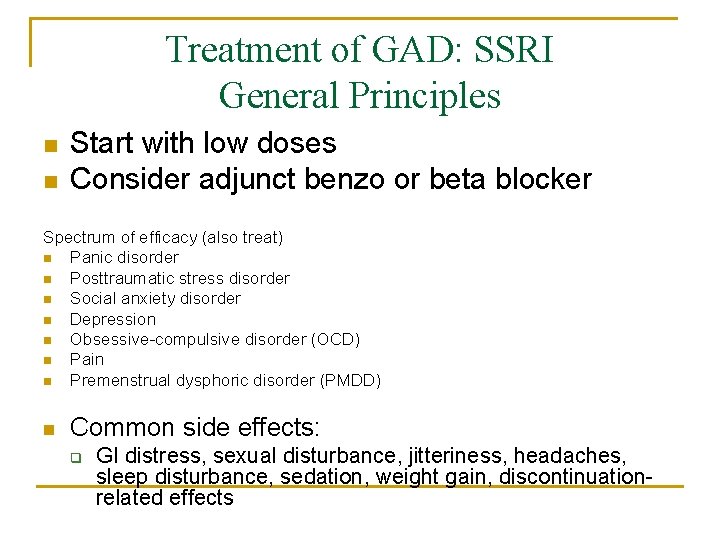
Treatment of GAD: SSRI General Principles n n Start with low doses Consider adjunct benzo or beta blocker Spectrum of efficacy (also treat) n Panic disorder n Posttraumatic stress disorder n Social anxiety disorder n Depression n Obsessive-compulsive disorder (OCD) n Pain n Premenstrual dysphoric disorder (PMDD) n Common side effects: q GI distress, sexual disturbance, jitteriness, headaches, sleep disturbance, sedation, weight gain, discontinuationrelated effects
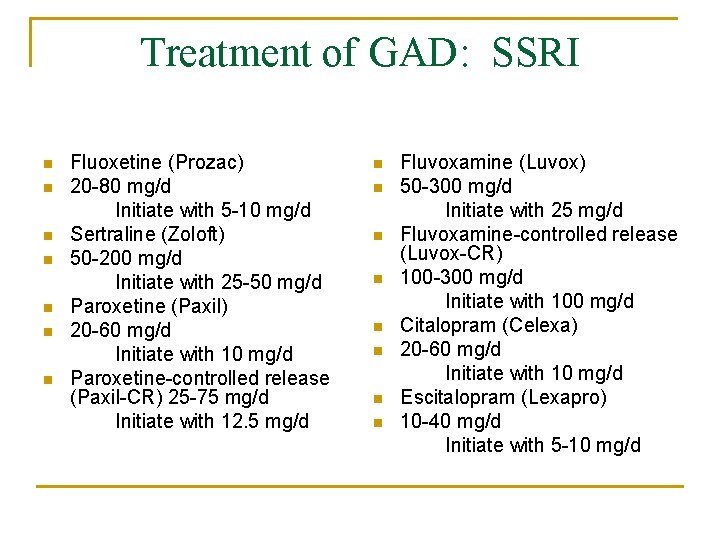
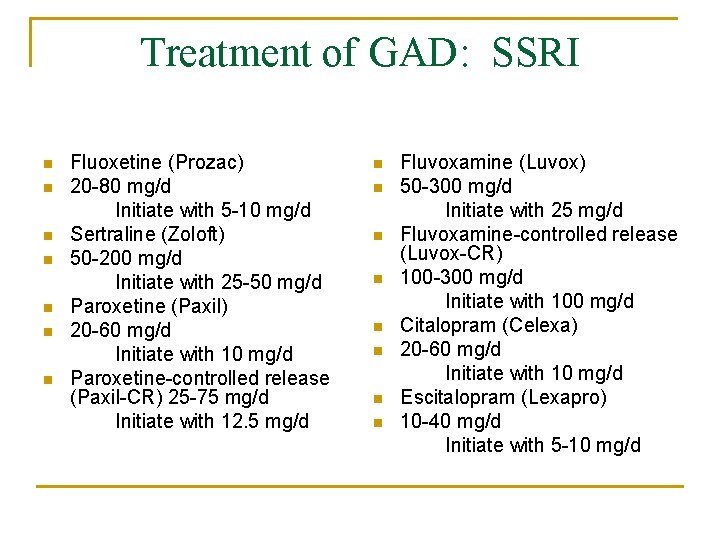
Treatment of GAD: SSRI n n n n Fluoxetine (Prozac) 20 -80 mg/d Initiate with 5 -10 mg/d Sertraline (Zoloft) 50 -200 mg/d Initiate with 25 -50 mg/d Paroxetine (Paxil) 20 -60 mg/d Initiate with 10 mg/d Paroxetine-controlled release (Paxil-CR) 25 -75 mg/d Initiate with 12. 5 mg/d n n n n Fluvoxamine (Luvox) 50 -300 mg/d Initiate with 25 mg/d Fluvoxamine-controlled release (Luvox-CR) 100 -300 mg/d Initiate with 100 mg/d Citalopram (Celexa) 20 -60 mg/d Initiate with 10 mg/d Escitalopram (Lexapro) 10 -40 mg/d Initiate with 5 -10 mg/d
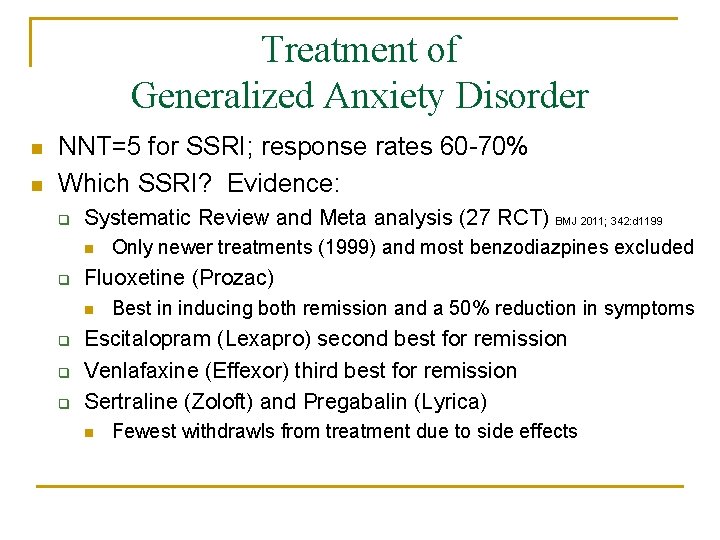
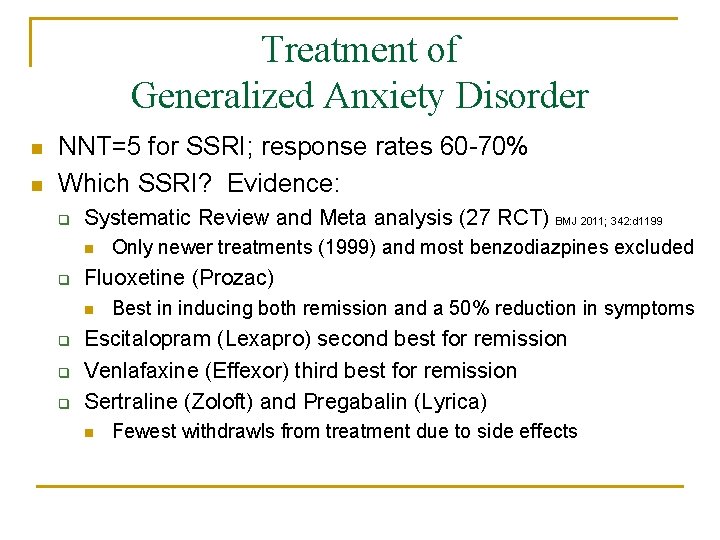
Treatment of Generalized Anxiety Disorder n n NNT=5 for SSRI; response rates 60 -70% Which SSRI? Evidence: q Systematic Review and Meta analysis (27 RCT) BMJ 2011; 342: d 1199 n q Fluoxetine (Prozac) n q q q Only newer treatments (1999) and most benzodiazpines excluded Best in inducing both remission and a 50% reduction in symptoms Escitalopram (Lexapro) second best for remission Venlafaxine (Effexor) third best for remission Sertraline (Zoloft) and Pregabalin (Lyrica) n Fewest withdrawls from treatment due to side effects
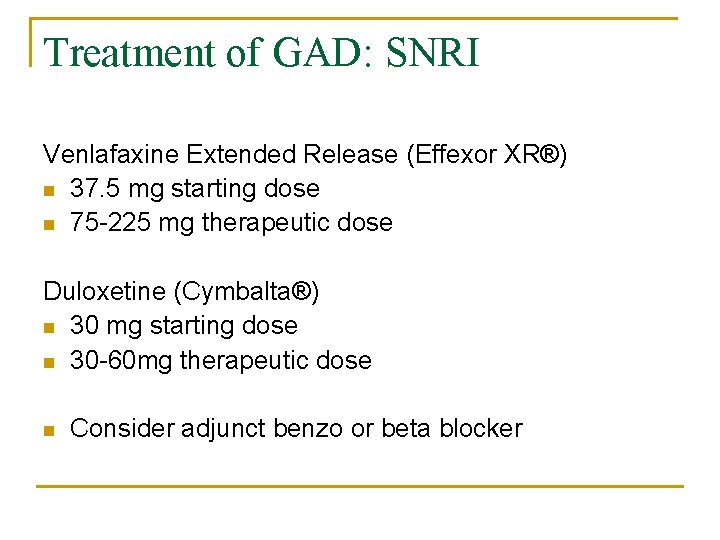
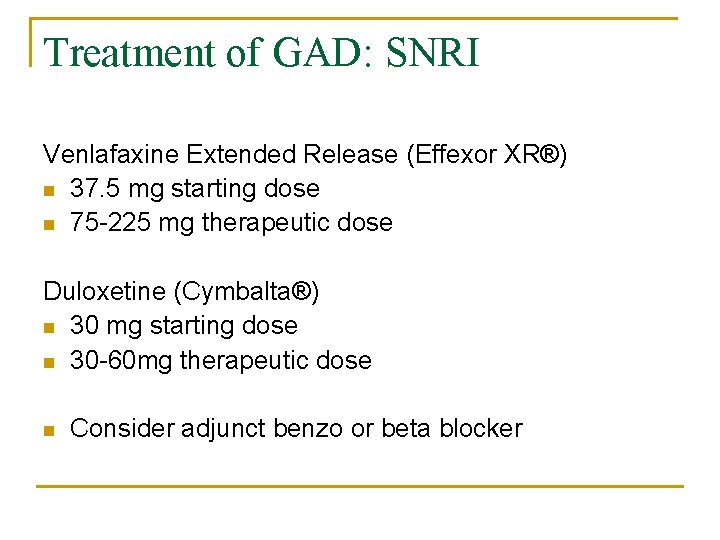
Treatment of GAD: SNRI Venlafaxine Extended Release (Effexor XR®) n 37. 5 mg starting dose n 75 -225 mg therapeutic dose Duloxetine (Cymbalta®) n 30 mg starting dose n 30 -60 mg therapeutic dose n Consider adjunct benzo or beta blocker
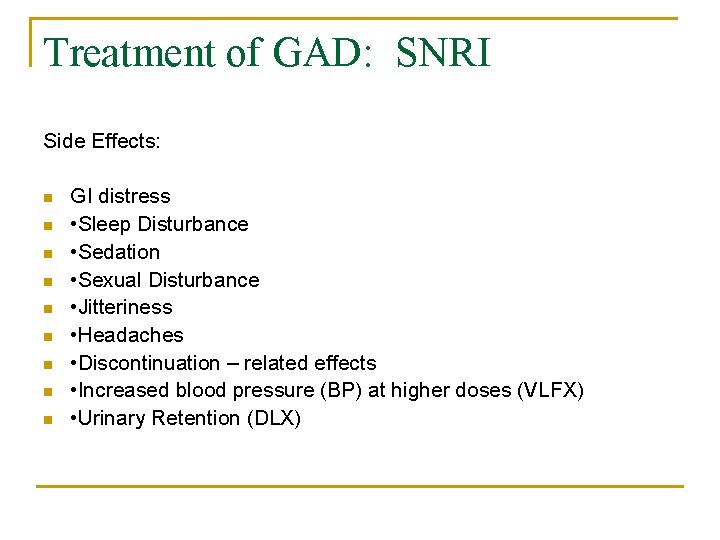
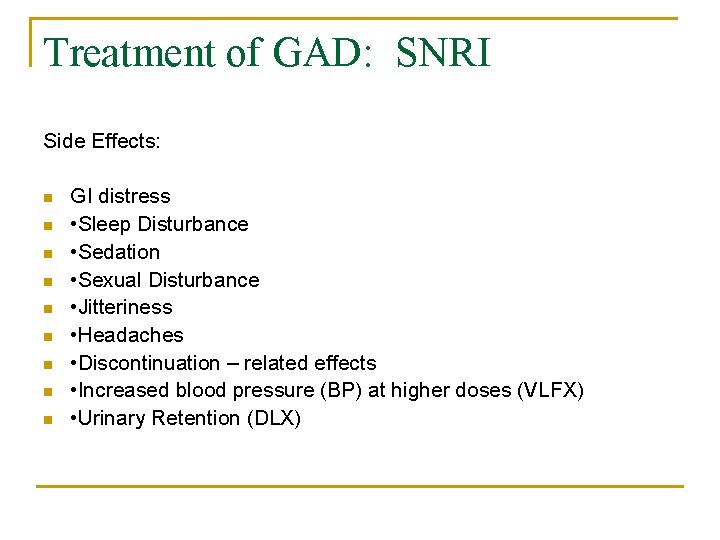
Treatment of GAD: SNRI Side Effects: n n n n n GI distress • Sleep Disturbance • Sedation • Sexual Disturbance • Jitteriness • Headaches • Discontinuation – related effects • Increased blood pressure (BP) at higher doses (VLFX) • Urinary Retention (DLX)

Treatment of GAD: Buspirone Adapted from Mayo Clinic Acute Psychiatry Review Course by Mark Pollack, MD n n n Initiate 50 -100 mg QD Noradrenergic and dopaminergic effects Limited data in anxiety q q n n Negative single-blind study (n = 12) in PD One positive open trial: possible efficacy for PD Side effects: activation, decreased seizure threshold at supramaximal doses Decreased propensity to cause sexual dysfunction
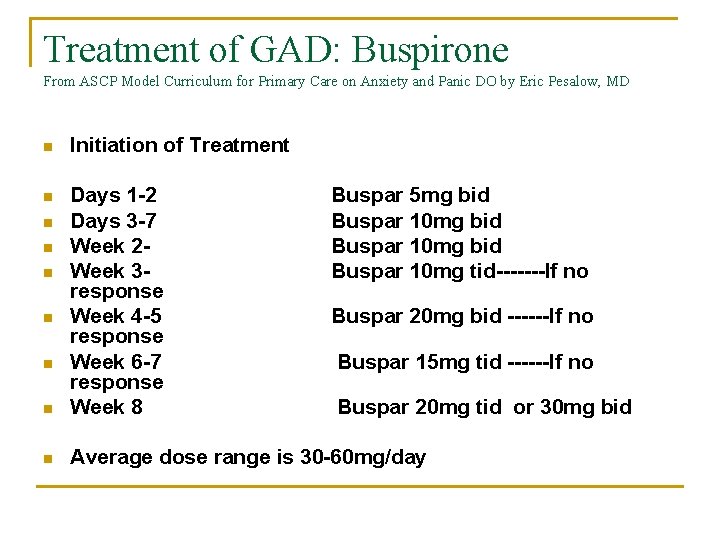
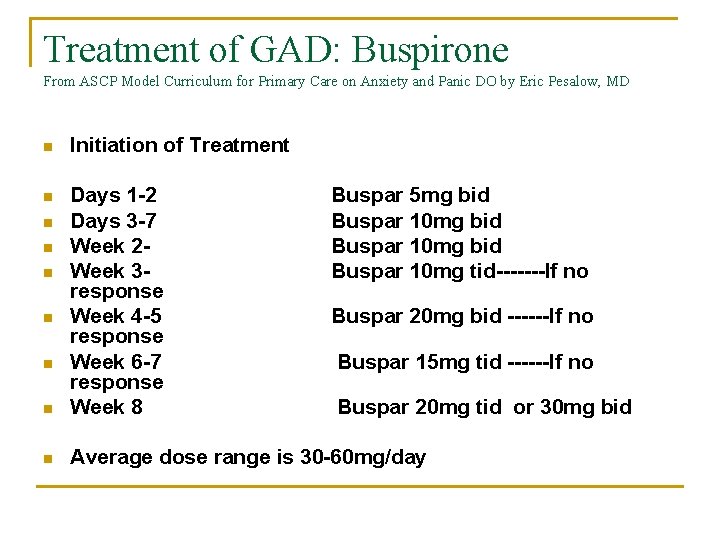
Treatment of GAD: Buspirone From ASCP Model Curriculum for Primary Care on Anxiety and Panic DO by Eric Pesalow, MD n Initiation of Treatment n n Days 1 -2 Days 3 -7 Week 2 Week 3 response Week 4 -5 response Week 6 -7 response Week 8 n Average dose range is 30 -60 mg/day n n n Buspar 5 mg bid Buspar 10 mg tid-------If no Buspar 20 mg bid ------If no Buspar 15 mg tid ------If no Buspar 20 mg tid or 30 mg bid
Treatment of GAD: Pregabalin n Approved in Europe for this indication but not in US Dose range 50 -300 mg Side effects sedation, dizziness
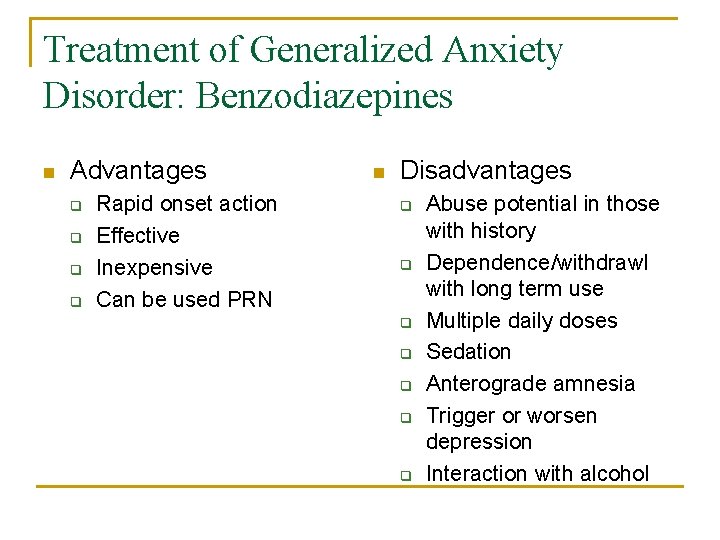
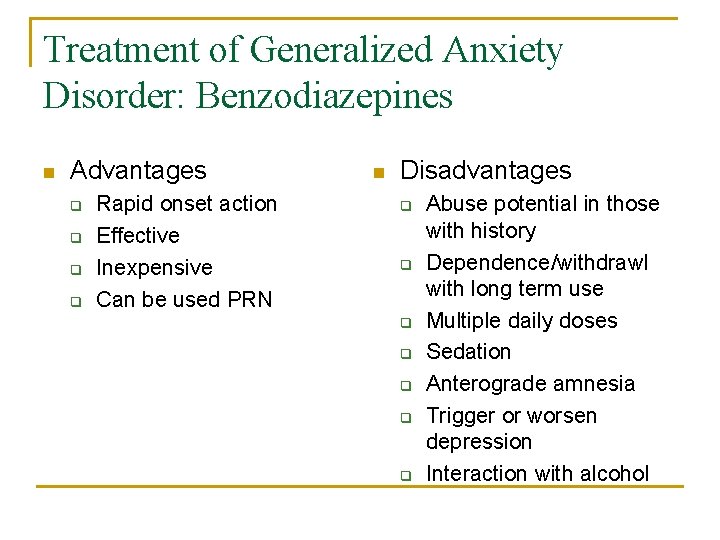
Treatment of Generalized Anxiety Disorder: Benzodiazepines n Advantages q q Rapid onset action Effective Inexpensive Can be used PRN n Disadvantages q q q q Abuse potential in those with history Dependence/withdrawl with long term use Multiple daily doses Sedation Anterograde amnesia Trigger or worsen depression Interaction with alcohol
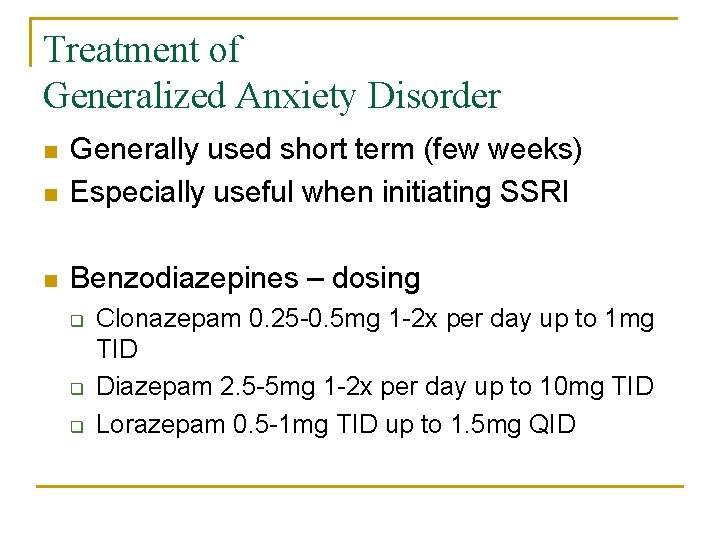
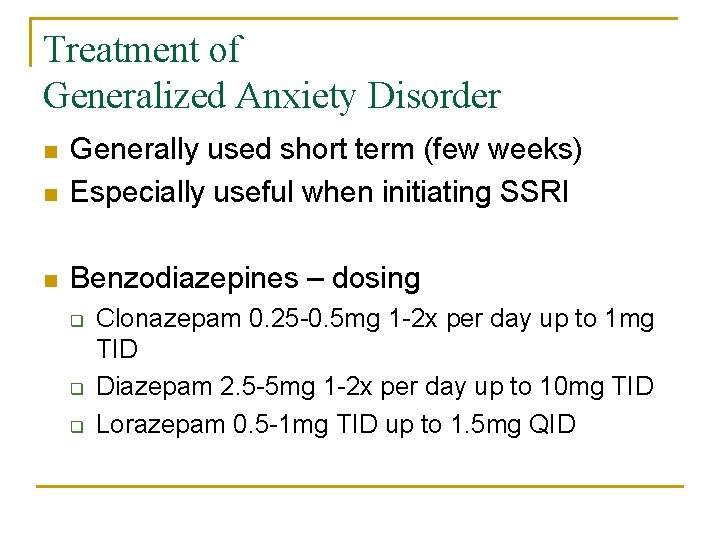
Treatment of Generalized Anxiety Disorder n Generally used short term (few weeks) Especially useful when initiating SSRI n Benzodiazepines – dosing n q q q Clonazepam 0. 25 -0. 5 mg 1 -2 x per day up to 1 mg TID Diazepam 2. 5 -5 mg 1 -2 x per day up to 10 mg TID Lorazepam 0. 5 -1 mg TID up to 1. 5 mg QID
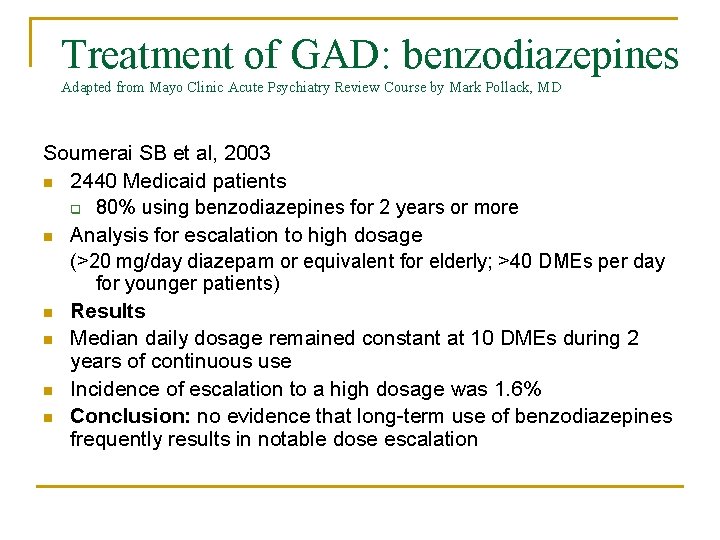
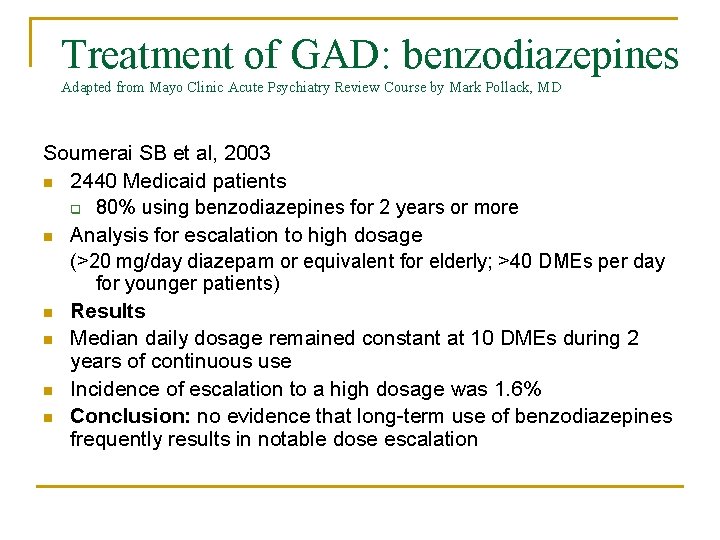
Treatment of GAD: benzodiazepines Adapted from Mayo Clinic Acute Psychiatry Review Course by Mark Pollack, MD Soumerai SB et al, 2003 n 2440 Medicaid patients q 80% using benzodiazepines for 2 years or more n Analysis for escalation to high dosage (>20 mg/day diazepam or equivalent for elderly; >40 DMEs per day for younger patients) n Results n Median daily dosage remained constant at 10 DMEs during 2 years of continuous use n Incidence of escalation to a high dosage was 1. 6% n Conclusion: no evidence that long-term use of benzodiazepines frequently results in notable dose escalation
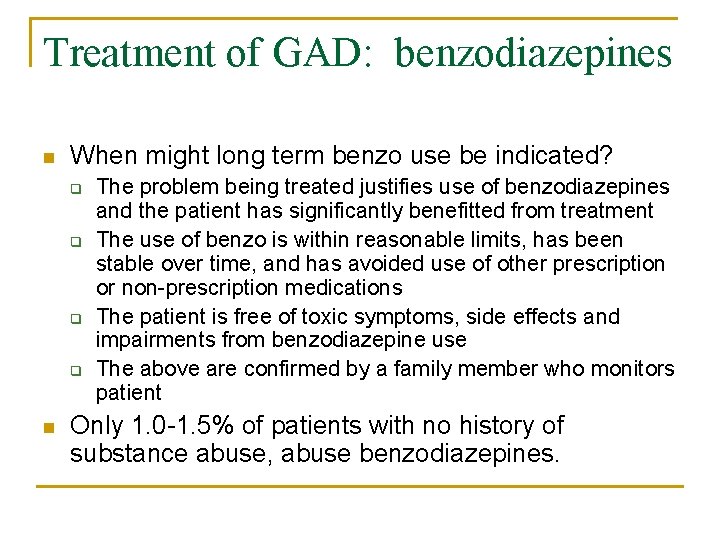
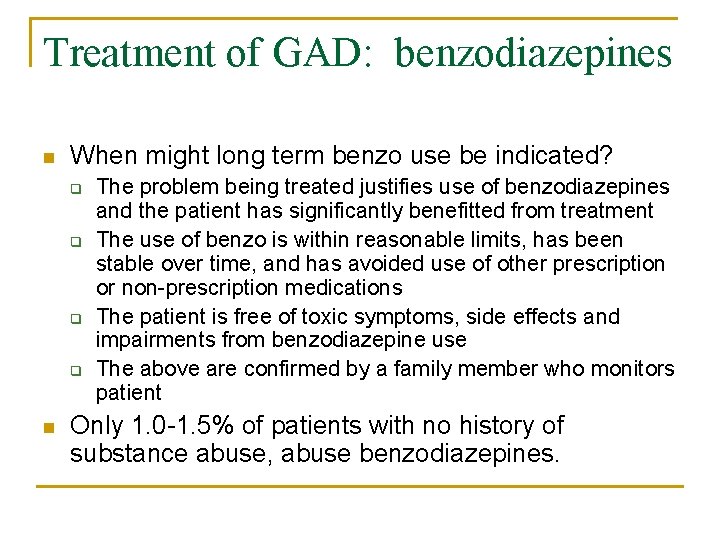
Treatment of GAD: benzodiazepines n When might long term benzo use be indicated? q q n The problem being treated justifies use of benzodiazepines and the patient has significantly benefitted from treatment The use of benzo is within reasonable limits, has been stable over time, and has avoided use of other prescription or non-prescription medications The patient is free of toxic symptoms, side effects and impairments from benzodiazepine use The above are confirmed by a family member who monitors patient Only 1. 0 -1. 5% of patients with no history of substance abuse, abuse benzodiazepines.
Panic Do n SSRIs/SNRIs n High Potency Benzodiazepines q n may interfere with CBT if used PRN Cognitive-Behavioral Therapy
Treatment of Panic DO: General Principles Aim is to be: n Free of panic attacks n Free of anticipatory anxiety n Return to avoided situations n Free of situational anxiety n Return to normal functioning and quality of life n General recommendation initial maintenance 12 -24 months well, longer if prior discontinuation failures
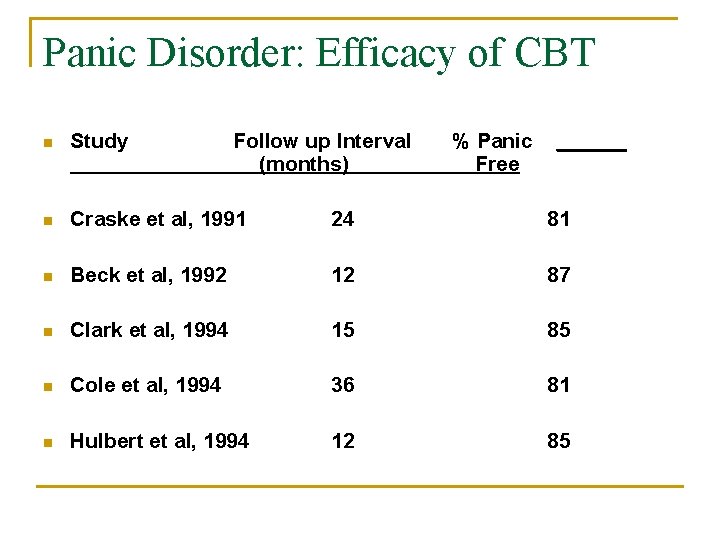
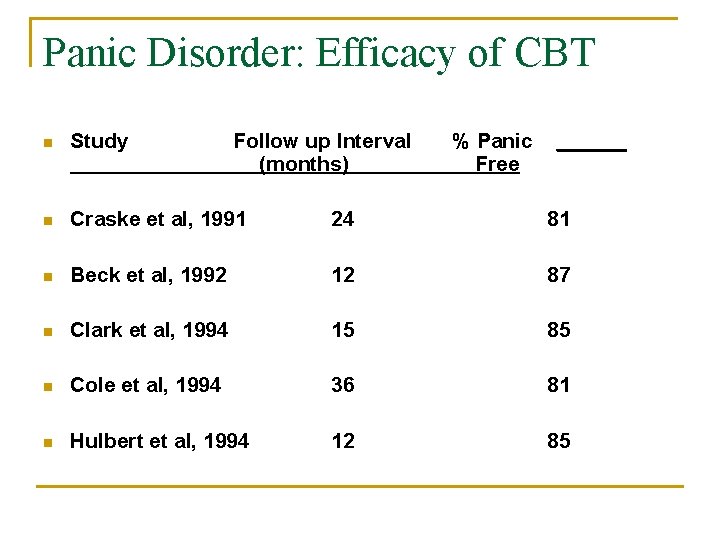
Panic Disorder: Efficacy of CBT n Study Follow up Interval (months) % Panic Free ______ n Craske et al, 1991 24 81 n Beck et al, 1992 12 87 n Clark et al, 1994 15 85 n Cole et al, 1994 36 81 n Hulbert et al, 1994 12 85
Social Phobia Disorder n n n SSRIs SNRI High Potency Benzodiazepines Beta Blockers q Give 1 -2 hours before discrete performance q Reduces physiologic symptoms but not emotional experience q Propranolol: 10 -40 mg po QD q Atenolol: 50 -150 mg po QD Other Agents Cognitive-Behavioral Therapy

OCD n SSRI (generally highest doses) n Exposure Therapy
Patient Education n Medications generally begin in work in 4 -6 weeks Anxiety may get worse in first several weeks before getting better Discuss side effects profile of medication and remind that most will diminish over time
8 Easy Steps to Treating Anxiety ©Yvonne Murphy, MD n Make the right diagnosis (suspect/screen with medical symptoms) n n n n Assess for co-morbid depression Decide on medication vs CBT/Exposure or EMRD for PTSD Patient Education Select a medication Frequent follow up (every week for dose titration) Switch or augment for non response Maintenance
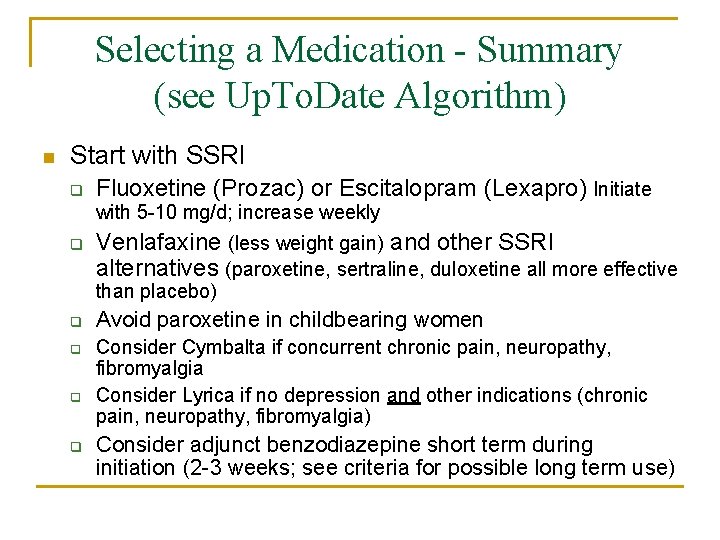
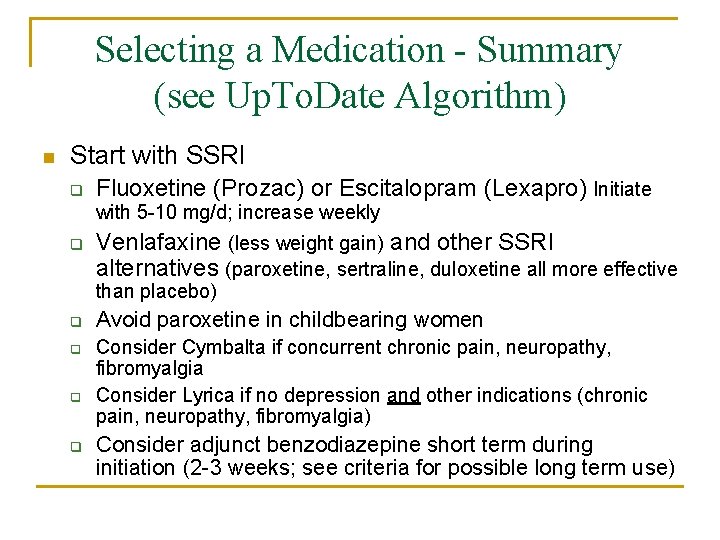
Selecting a Medication - Summary (see Up. To. Date Algorithm) n Start with SSRI q Fluoxetine (Prozac) or Escitalopram (Lexapro) Initiate with 5 -10 mg/d; increase weekly q Venlafaxine (less weight gain) and other SSRI alternatives (paroxetine, sertraline, duloxetine all more effective than placebo) q q Avoid paroxetine in childbearing women Consider Cymbalta if concurrent chronic pain, neuropathy, fibromyalgia Consider Lyrica if no depression and other indications (chronic pain, neuropathy, fibromyalgia) Consider adjunct benzodiazepine short term during initiation (2 -3 weeks; see criteria for possible long term use)

Selecting a Medication with concurrent medical conditions n Cardiac Disease: avoid citalopram >40 mg n Diabetes: duloxetine impairs glycemic control n Liver Disease: duloxetine contraindicated n Check for drug interactions
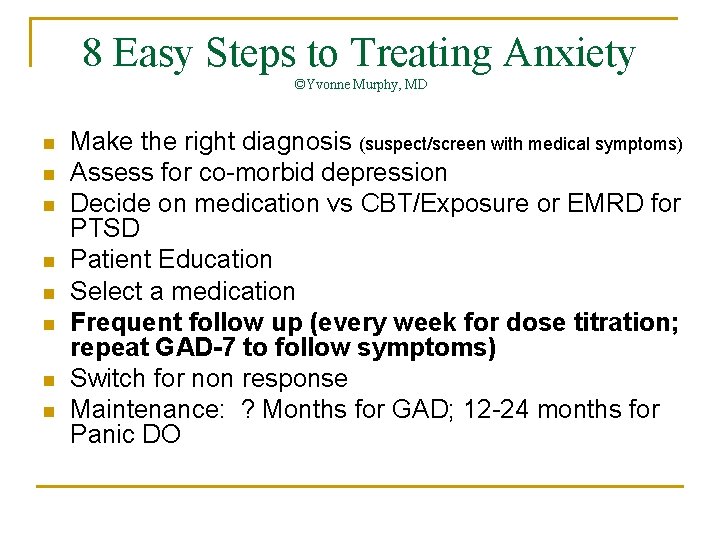
8 Easy Steps to Treating Anxiety ©Yvonne Murphy, MD n n n n Make the right diagnosis (suspect/screen with medical symptoms) Assess for co-morbid depression Decide on medication vs CBT/Exposure or EMRD for PTSD Patient Education Select a medication Frequent follow up (every week for dose titration; repeat GAD-7 to follow symptoms) Switch for non response Maintenance: ? Months for GAD; 12 -24 months for Panic DO
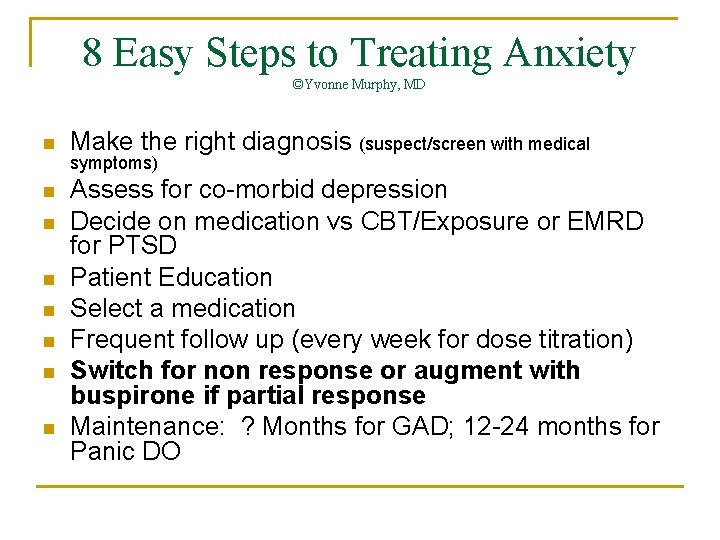
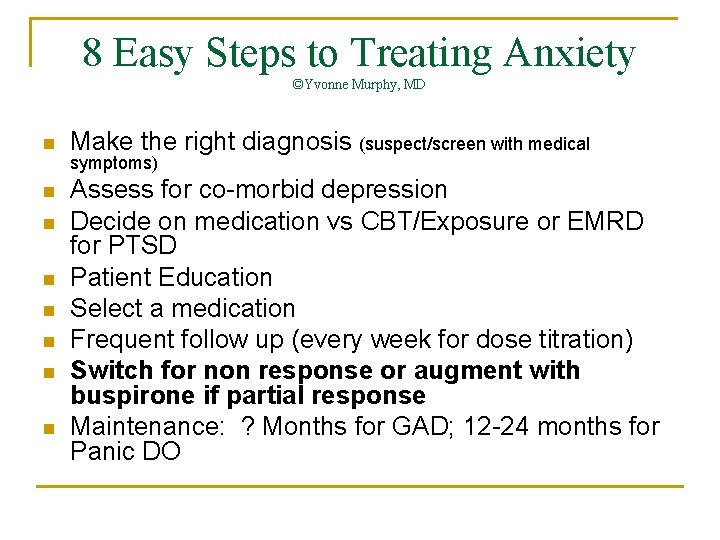
8 Easy Steps to Treating Anxiety ©Yvonne Murphy, MD n Make the right diagnosis (suspect/screen with medical n Assess for co-morbid depression Decide on medication vs CBT/Exposure or EMRD for PTSD Patient Education Select a medication Frequent follow up (every week for dose titration) Switch for non response or augment with buspirone if partial response Maintenance: ? Months for GAD; 12 -24 months for Panic DO n n n symptoms)
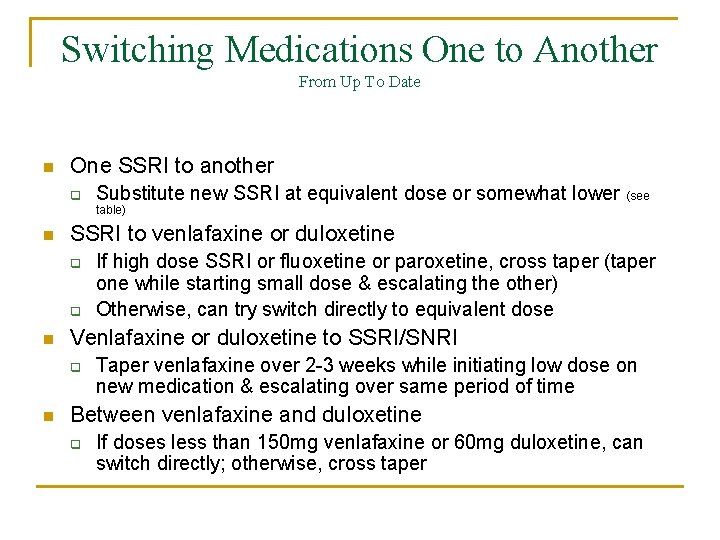
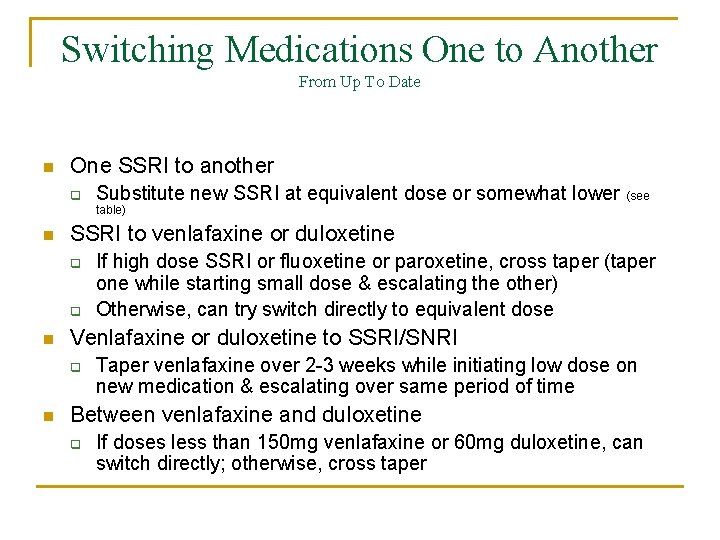
Switching Medications One to Another From Up To Date n One SSRI to another q Substitute new SSRI at equivalent dose or somewhat lower (see table) n SSRI to venlafaxine or duloxetine q q n Venlafaxine or duloxetine to SSRI/SNRI q n If high dose SSRI or fluoxetine or paroxetine, cross taper (taper one while starting small dose & escalating the other) Otherwise, can try switch directly to equivalent dose Taper venlafaxine over 2 -3 weeks while initiating low dose on new medication & escalating over same period of time Between venlafaxine and duloxetine q If doses less than 150 mg venlafaxine or 60 mg duloxetine, can switch directly; otherwise, cross taper
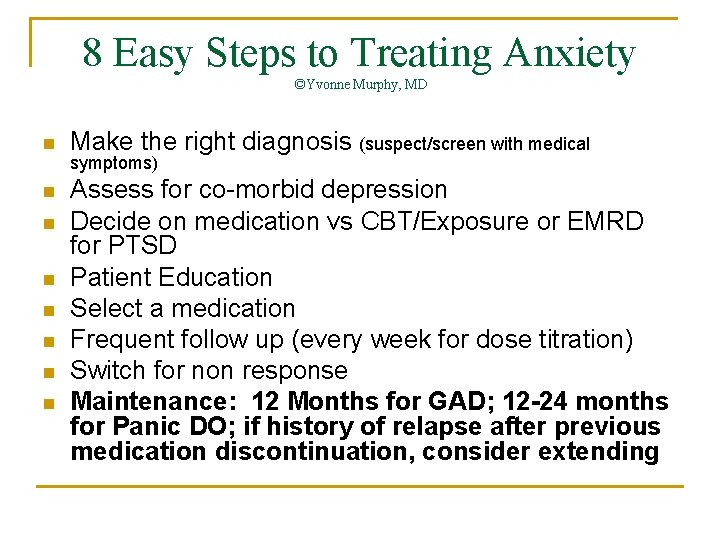
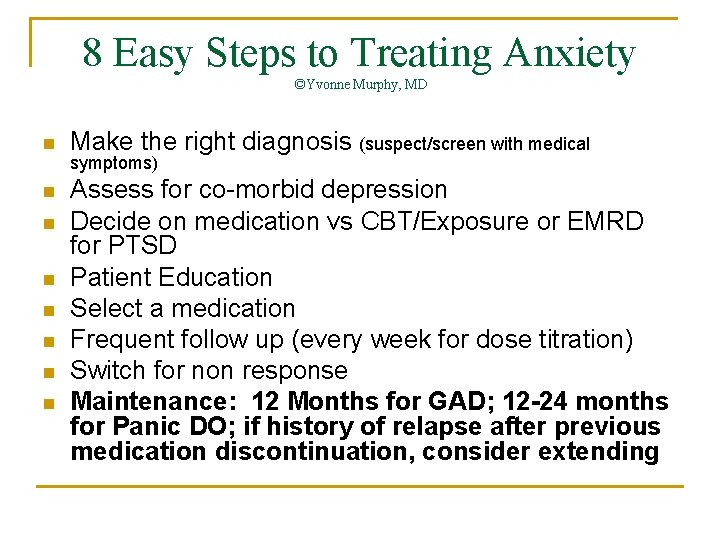
8 Easy Steps to Treating Anxiety ©Yvonne Murphy, MD n Make the right diagnosis (suspect/screen with medical n Assess for co-morbid depression Decide on medication vs CBT/Exposure or EMRD for PTSD Patient Education Select a medication Frequent follow up (every week for dose titration) Switch for non response Maintenance: 12 Months for GAD; 12 -24 months for Panic DO; if history of relapse after previous medication discontinuation, consider extending n n n symptoms)
Adjunct Treatment of Anxiety n Relaxation Therapies q q q n Deep breathing Progressive muscle relaxation Autogenic training Exercise
Resources for Patients n n www. freedomfromfear. org National Anxiety Foundation q n http: //www. lexington-on-line. com/naf. html Anxiety Disorders Association of America q www. adaa. org
Patient Case Insert case from your practice here
 7 rights of medication administration in order
7 rights of medication administration in order Primary secondary tertiary care
Primary secondary tertiary care Chapter 15 anxiety and obsessive-compulsive disorders
Chapter 15 anxiety and obsessive-compulsive disorders Anxiety disorders def
Anxiety disorders def Icd 10 anxietas
Icd 10 anxietas Multipath model of anxiety disorders
Multipath model of anxiety disorders Powerlessness nursing care plan
Powerlessness nursing care plan Unit 14 health and social care diabetes
Unit 14 health and social care diabetes Physiological disorders and their care
Physiological disorders and their care Nursing care of male patients with genitourinary disorders
Nursing care of male patients with genitourinary disorders Pneumatic reduction of intussusception
Pneumatic reduction of intussusception Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Wastewater treatment process primary secondary tertiary
Wastewater treatment process primary secondary tertiary Sewage treatment primary secondary and tertiary
Sewage treatment primary secondary and tertiary Anaerobic methane digester frq
Anaerobic methane digester frq Care and treatment reviews
Care and treatment reviews Dr martha williams
Dr martha williams Providing improper or unprofessional treatment or care
Providing improper or unprofessional treatment or care Igor areh
Igor areh Relaxation techniques test anxiety
Relaxation techniques test anxiety Exam anxiety symptoms
Exam anxiety symptoms I'm a perfect example of someone who has math anxiety
I'm a perfect example of someone who has math anxiety Neurotic anxiety example
Neurotic anxiety example Define neurotic
Define neurotic Examples of generalized anxiety disorder
Examples of generalized anxiety disorder Chapter 8 managing stress and anxiety
Chapter 8 managing stress and anxiety Neurotic anxiety example
Neurotic anxiety example Syntonic vs dystonic
Syntonic vs dystonic University of wisconsin integrative medicine anxiety
University of wisconsin integrative medicine anxiety Astrid zamora
Astrid zamora Frustration anxiety and tension
Frustration anxiety and tension Sharat chandran
Sharat chandran Generalized anxiety disorder dsm 5
Generalized anxiety disorder dsm 5 Freudian slip meaning
Freudian slip meaning Neurotic anxiety example
Neurotic anxiety example Example of pie charting in nursing
Example of pie charting in nursing Test anxiety essay
Test anxiety essay Chapter 18 managing anxiety
Chapter 18 managing anxiety Caregiver anxiety
Caregiver anxiety Dr fayad
Dr fayad School anxiety symptoms
School anxiety symptoms Ocd prevalence
Ocd prevalence Hildegard peplau levels of anxiety
Hildegard peplau levels of anxiety Apprehensive vs anxious
Apprehensive vs anxious Agoraphobia vs social anxiety
Agoraphobia vs social anxiety Agoraphobia vs social phobia
Agoraphobia vs social phobia Snri social anxiety
Snri social anxiety Explanation of anxiety disorder
Explanation of anxiety disorder Biopsychosocial ocd
Biopsychosocial ocd Stai items
Stai items B lynch suture
B lynch suture Chapter 5 lesson 1 dealing with anxiety and depression
Chapter 5 lesson 1 dealing with anxiety and depression Chapter 5 lesson 1 dealing with anxiety and depression
Chapter 5 lesson 1 dealing with anxiety and depression