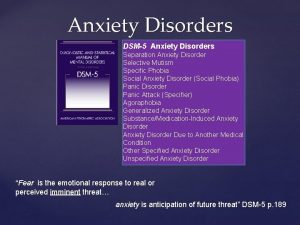
Introduction OCD is an anxiety disorder For diagnosis
- Slides: 22
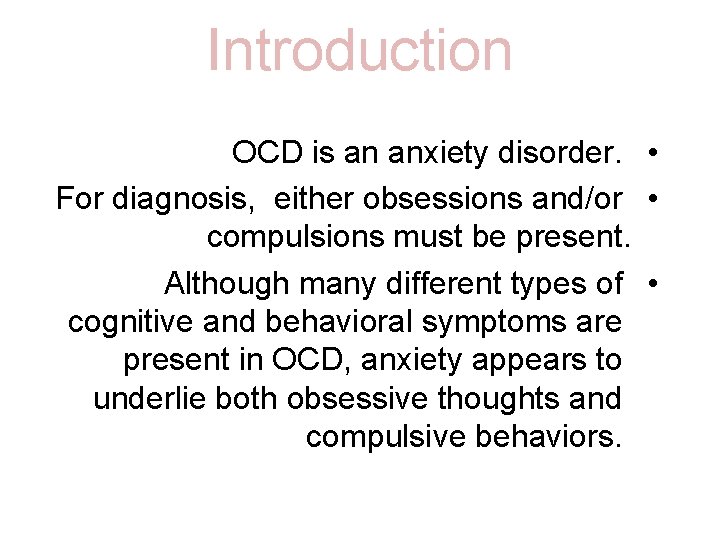
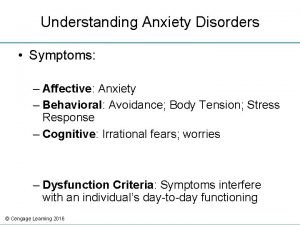
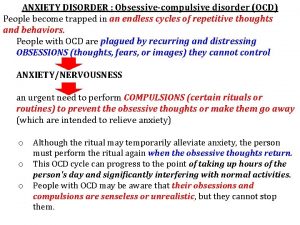
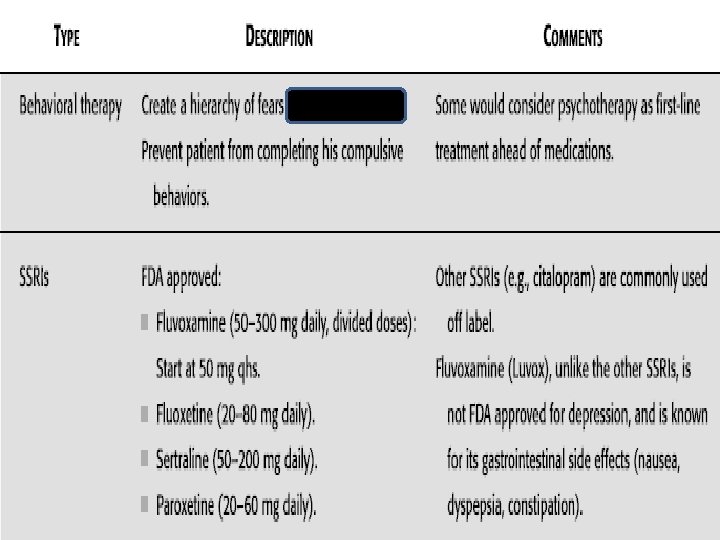
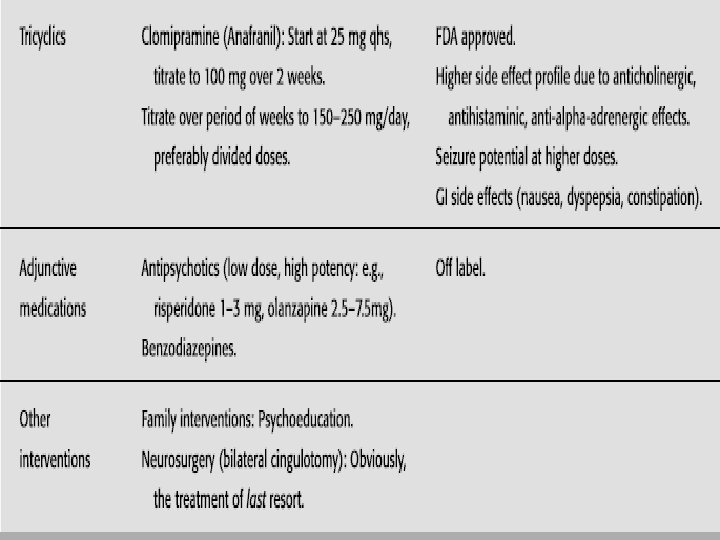
Introduction OCD is an anxiety disorder. • For diagnosis, either obsessions and/or • compulsions must be present. Although many different types of • cognitive and behavioral symptoms are present in OCD, anxiety appears to underlie both obsessive thoughts and compulsive behaviors.
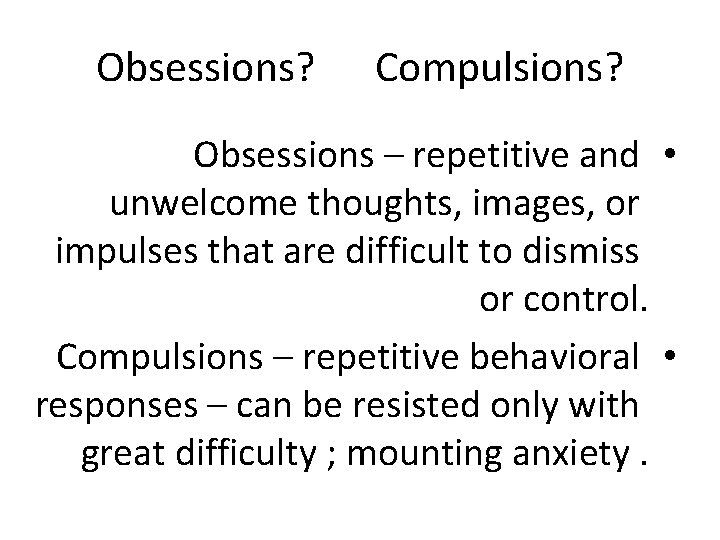
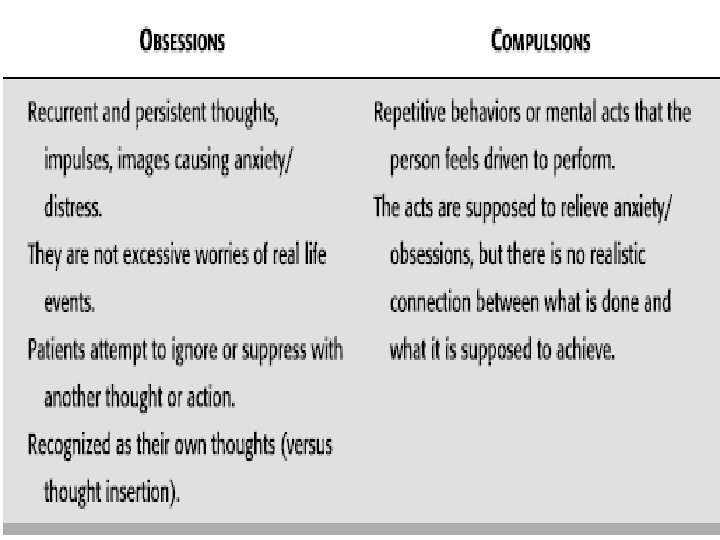
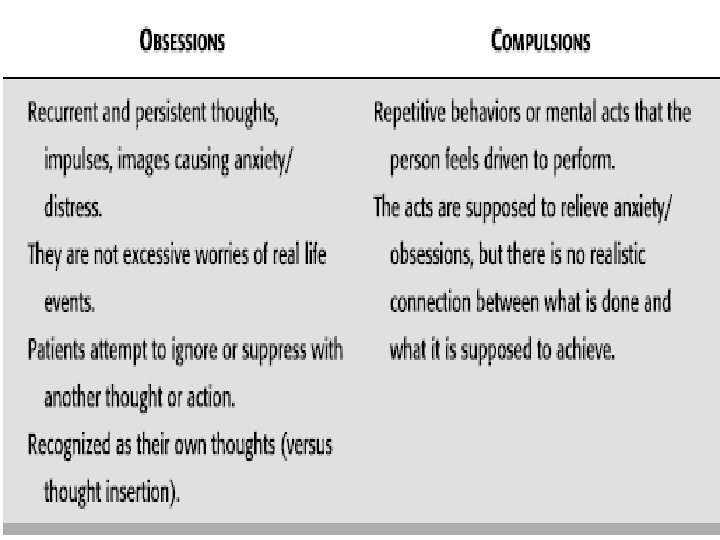
Obsessions? Compulsions? Obsessions – repetitive and • unwelcome thoughts, images, or impulses that are difficult to dismiss or control. Compulsions – repetitive behavioral • responses – can be resisted only with great difficulty ; mounting anxiety.
Obsessions Thoughts, images, or • impulses that repetitively occur to become out of one’s own control. Person suffering from • these obsessions finds them intrusive and disturbing – recognizes they don’t make sense.
Obsessions - continued Obsessions often accompanied by • uncomfortable feelings such as fear, disgust, or doubt. For example, people with OCD may worry • excessively about dirt and germs, and obsessed with the idea that they are contaminated or may contaminate others
Compulsions These are acts that are continually performed • to provide relief from discomfort caused by obsessions. OCD compulsions do not give the person • pleasure. For example, a person may repeatedly check • to see if their stove was left on in fear of burning the house down.
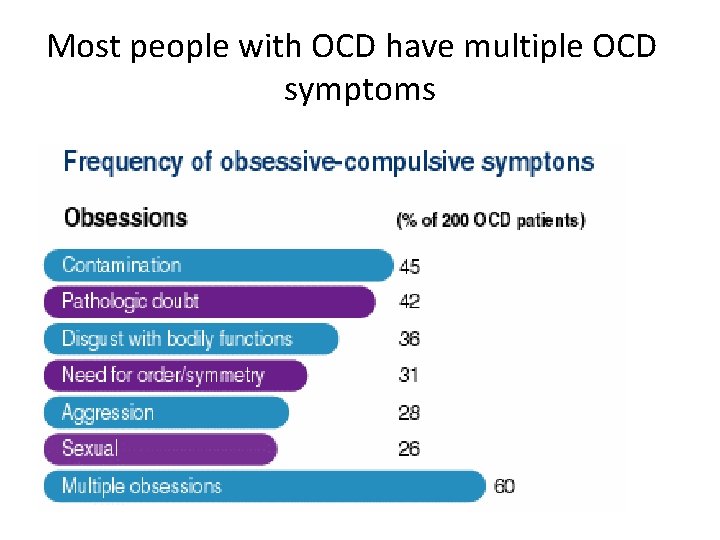
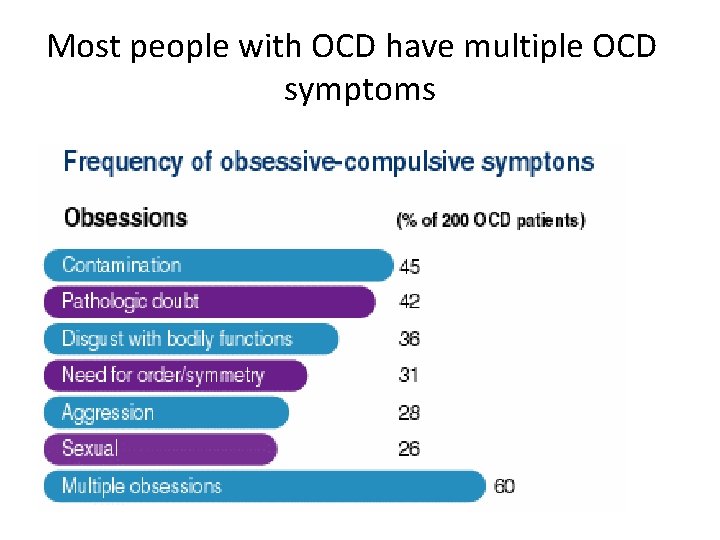
Most people with OCD have multiple OCD symptoms
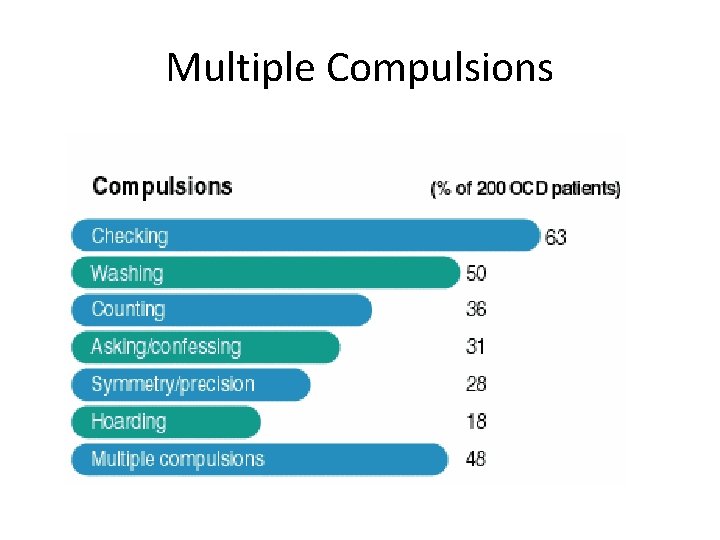
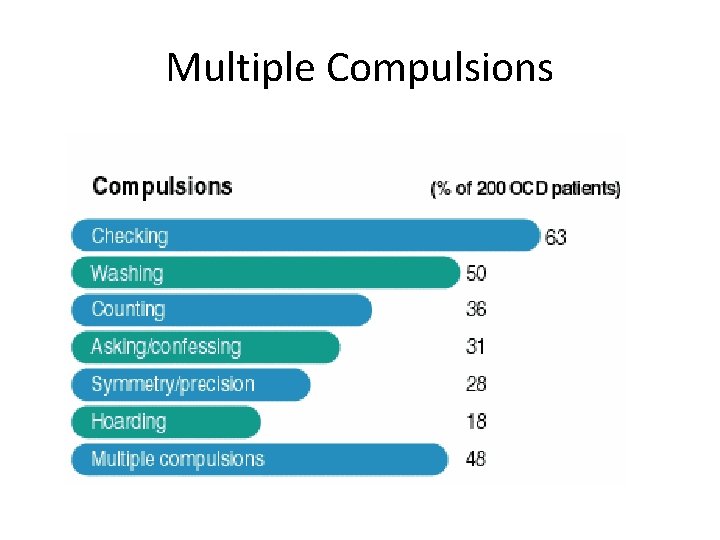
Multiple Compulsions
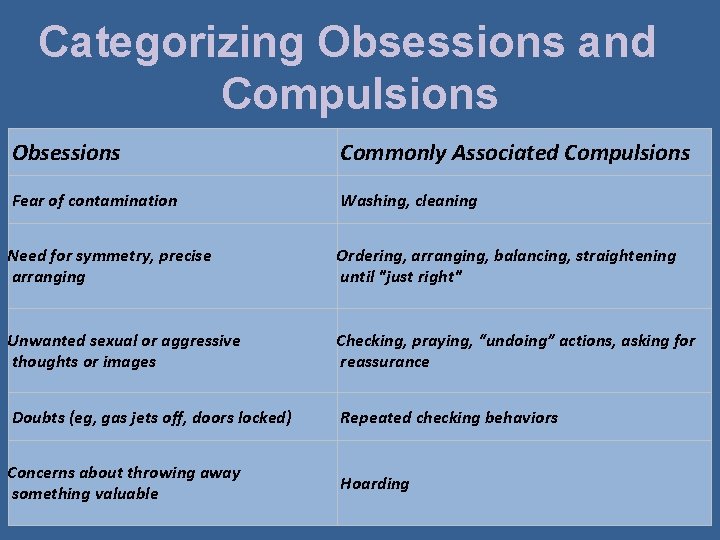
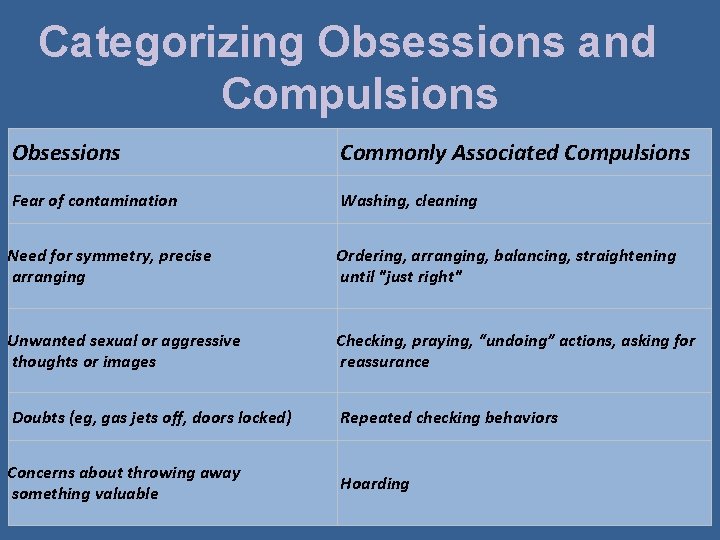
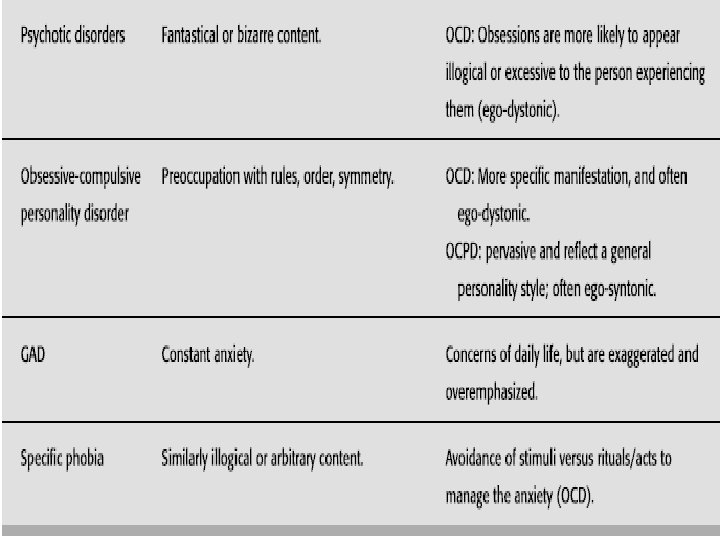
Categorizing Obsessions and Compulsions Obsessions Commonly Associated Compulsions Fear of contamination Washing, cleaning Need for symmetry, precise arranging Ordering, arranging, balancing, straightening until "just right" Unwanted sexual or aggressive thoughts or images Checking, praying, “undoing” actions, asking for reassurance Doubts (eg, gas jets off, doors locked) Repeated checking behaviors Concerns about throwing away something valuable Hoarding
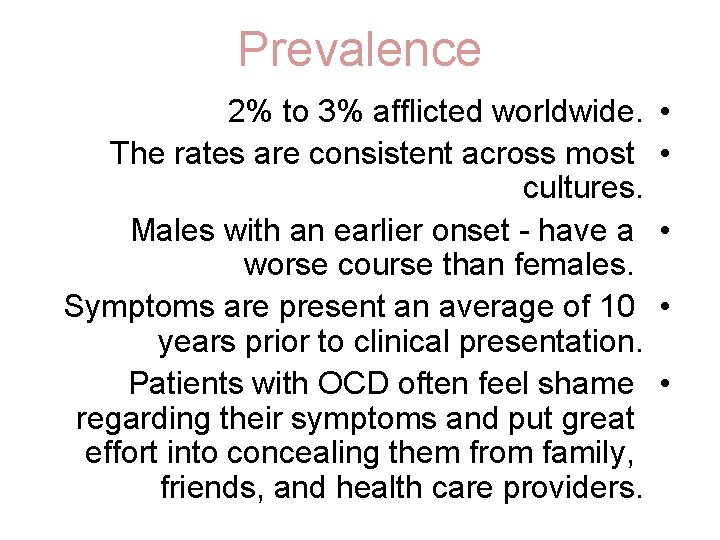
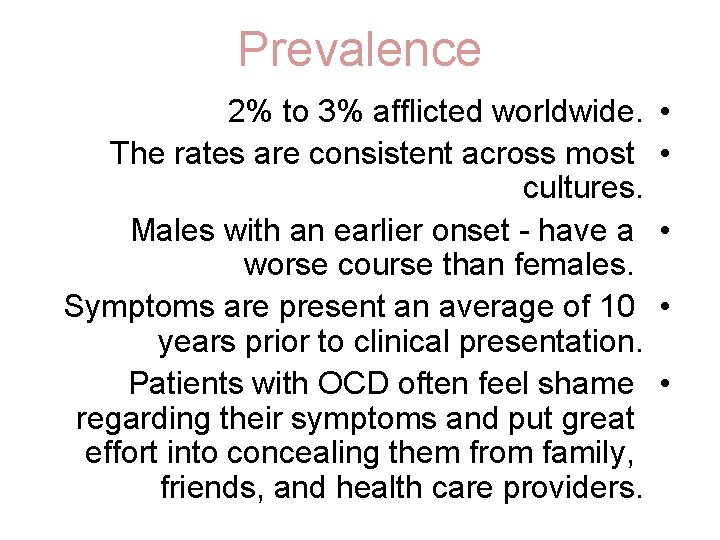
Prevalence 2% to 3% afflicted worldwide. The rates are consistent across most cultures. Males with an earlier onset - have a worse course than females. Symptoms are present an average of 10 years prior to clinical presentation. Patients with OCD often feel shame regarding their symptoms and put great effort into concealing them from family, friends, and health care providers. • • •
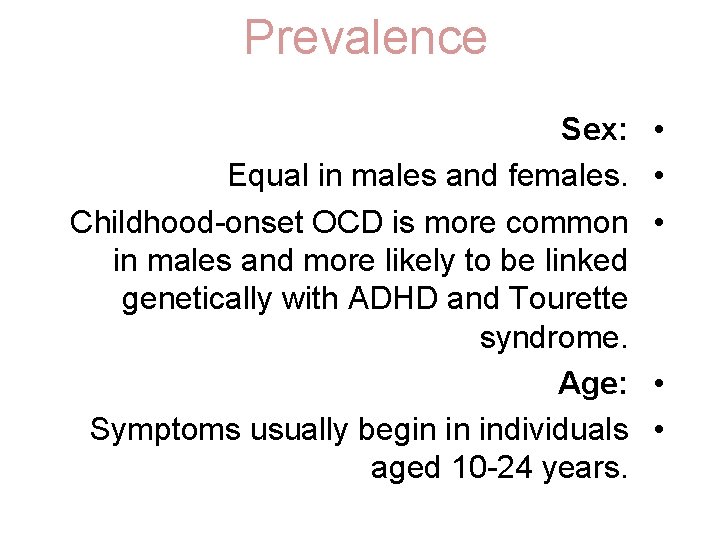
Prevalence Sex: Equal in males and females. Childhood-onset OCD is more common in males and more likely to be linked genetically with ADHD and Tourette syndrome. Age: Symptoms usually begin in individuals aged 10 -24 years. • • •
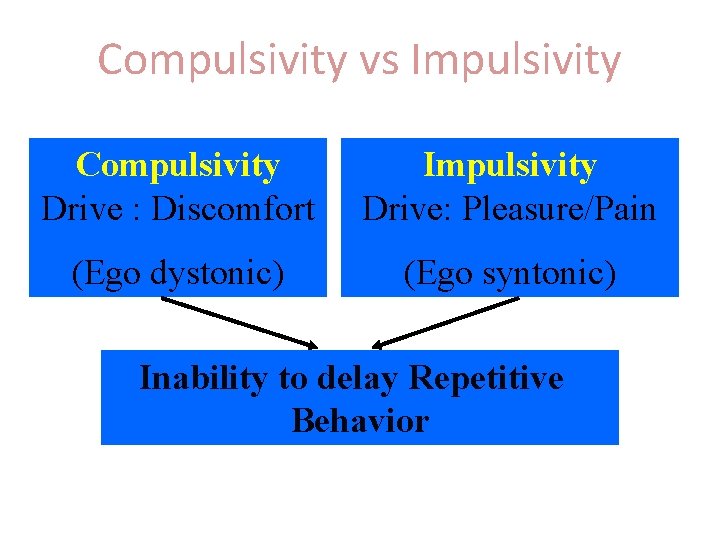
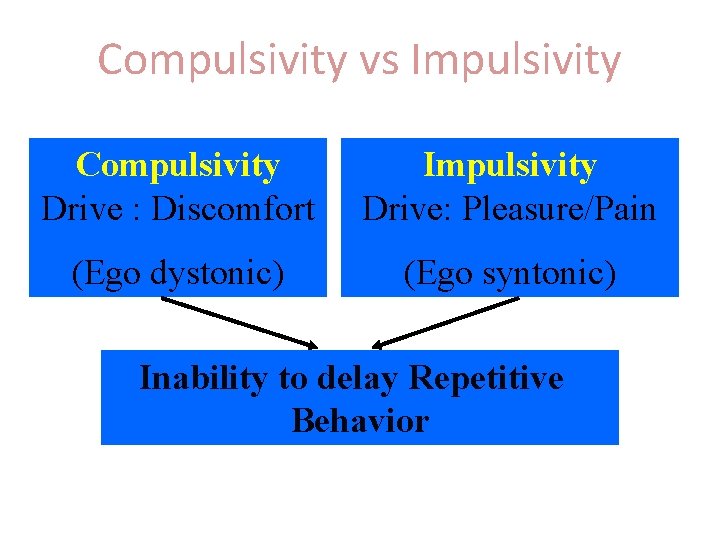
Compulsivity vs Impulsivity Compulsivity Drive : Discomfort Impulsivity Drive: Pleasure/Pain (Ego dystonic) (Ego syntonic) Inability to delay Repetitive Behavior
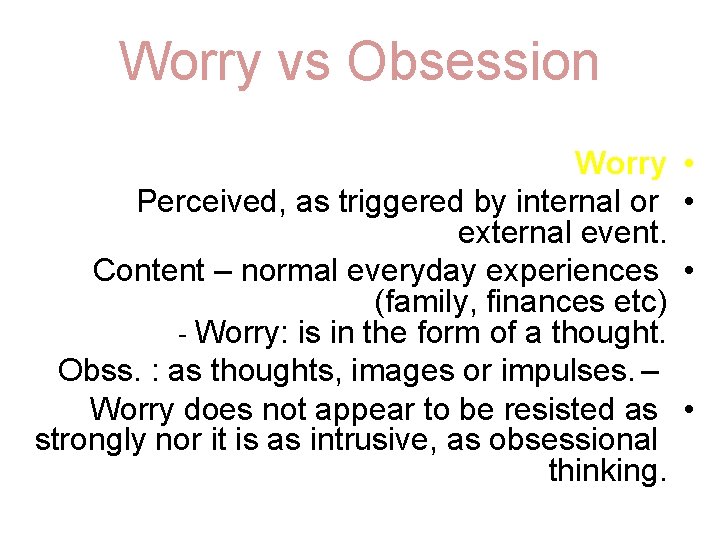
Worry vs Obsession Worry Perceived, as triggered by internal or external event. Content – normal everyday experiences (family, finances etc) - Worry: is in the form of a thought. Obss. : as thoughts, images or impulses. – Worry does not appear to be resisted as strongly nor it is as intrusive, as obsessional thinking. • •
Theories Scientist split into 2 groups • Psychological disorder – where people are responsible for feelings they have Abnormalities in the brain–
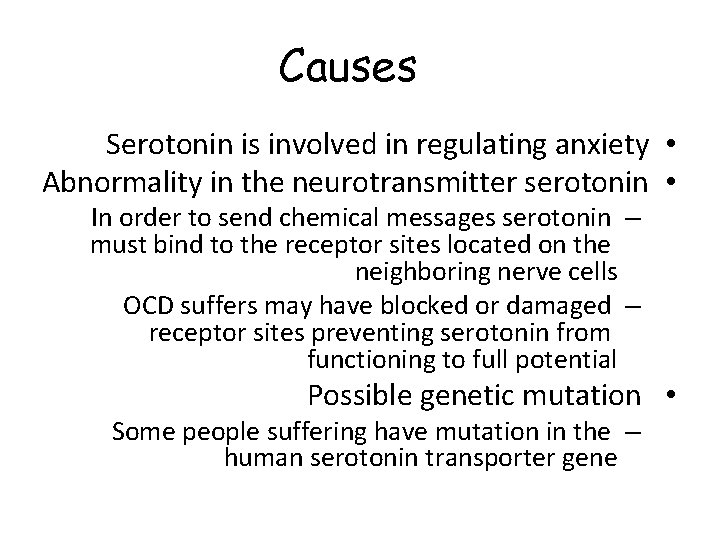
Causes Serotonin is involved in regulating anxiety • Abnormality in the neurotransmitter serotonin • In order to send chemical messages serotonin – must bind to the receptor sites located on the neighboring nerve cells OCD suffers may have blocked or damaged – receptor sites preventing serotonin from functioning to full potential Possible genetic mutation • Some people suffering have mutation in the – human serotonin transporter gene
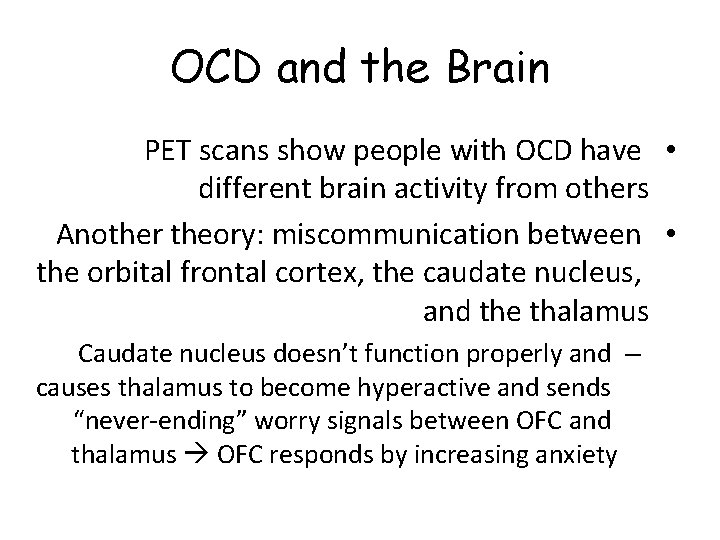
OCD and the Brain PET scans show people with OCD have • different brain activity from others Another theory: miscommunication between • the orbital frontal cortex, the caudate nucleus, and the thalamus Caudate nucleus doesn’t function properly and – causes thalamus to become hyperactive and sends “never-ending” worry signals between OFC and thalamus OFC responds by increasing anxiety
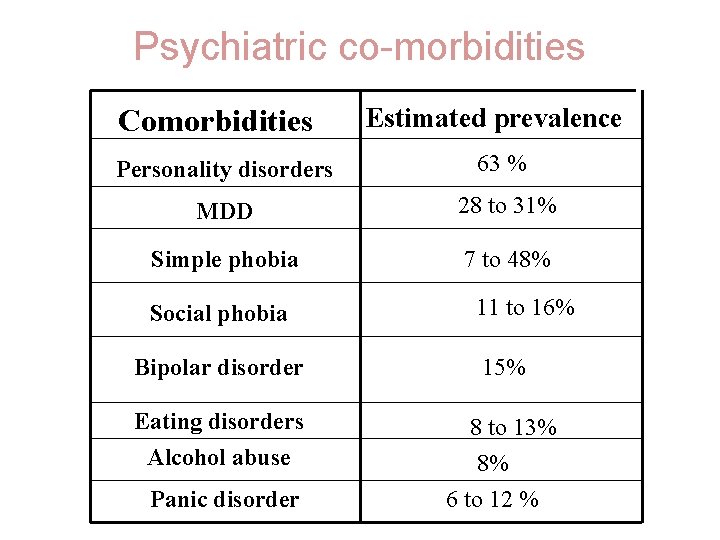
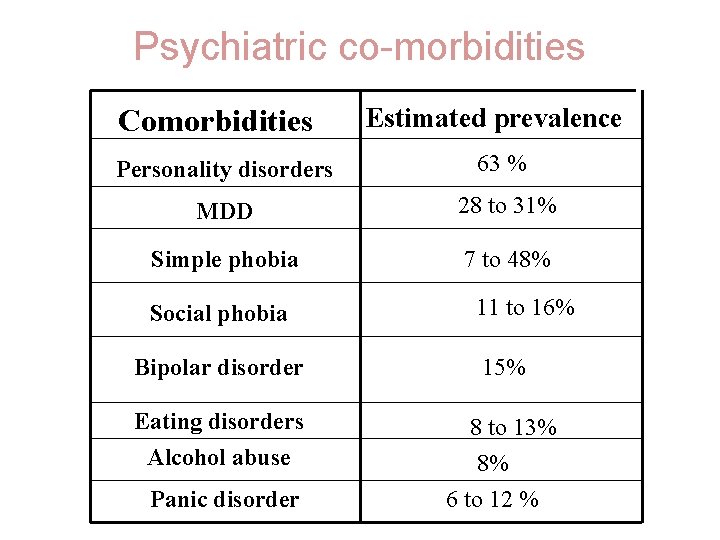
Psychiatric co-morbidities Comorbidities Estimated prevalence Personality disorders 63 % MDD 28 to 31% Simple phobia 7 to 48% Social phobia 11 to 16% Bipolar disorder 15% Eating disorders Alcohol abuse 8 to 13% 8% 6 to 12 % Panic disorder
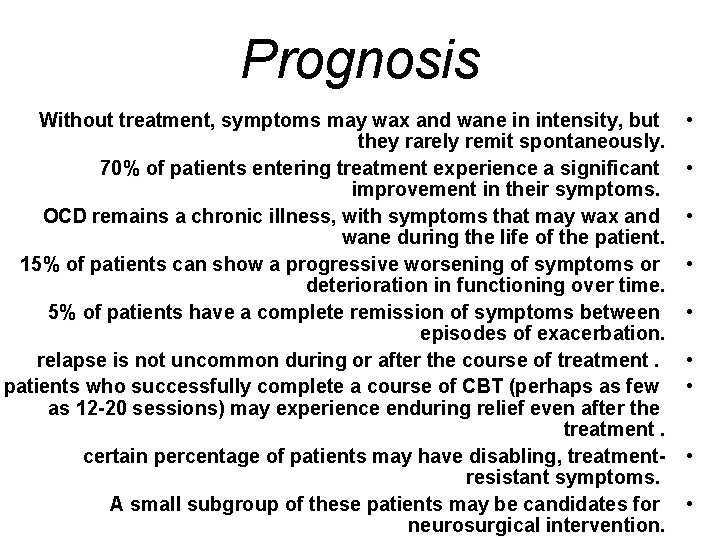
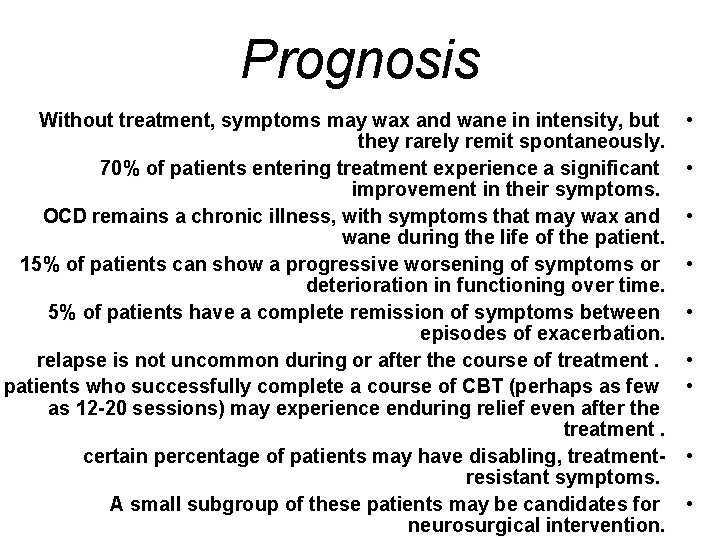
Prognosis Without treatment, symptoms may wax and wane in intensity, but they rarely remit spontaneously. 70% of patients entering treatment experience a significant improvement in their symptoms. OCD remains a chronic illness, with symptoms that may wax and wane during the life of the patient. 15% of patients can show a progressive worsening of symptoms or deterioration in functioning over time. 5% of patients have a complete remission of symptoms between episodes of exacerbation. relapse is not uncommon during or after the course of treatment. patients who successfully complete a course of CBT (perhaps as few as 12 -20 sessions) may experience enduring relief even after the treatment. certain percentage of patients may have disabling, treatmentresistant symptoms. A small subgroup of these patients may be candidates for neurosurgical intervention. • • •
 Anxiety disorder nursing diagnosis
Anxiety disorder nursing diagnosis Ego-dystonic
Ego-dystonic Ocd symptoms in adults
Ocd symptoms in adults Examples of generalized anxiety disorder
Examples of generalized anxiety disorder Astrid zamora
Astrid zamora Generalized anxiety disorder dsm 5
Generalized anxiety disorder dsm 5 Examples of generalized anxiety disorder
Examples of generalized anxiety disorder Explanation of anxiety disorder
Explanation of anxiety disorder Biopsychosocial ocd
Biopsychosocial ocd Explanation of anxiety disorder
Explanation of anxiety disorder Obsessive compulsive disorder ncp
Obsessive compulsive disorder ncp Ocd diagnosis criteria
Ocd diagnosis criteria Ocd diagnosis criteria
Ocd diagnosis criteria Nursing diagnosis ocd
Nursing diagnosis ocd Somatic vs factitious
Somatic vs factitious Nursing diagnosis for somatoform disorder
Nursing diagnosis for somatoform disorder Acute stress disorder diagnosis
Acute stress disorder diagnosis Hypothalamus eating disorders
Hypothalamus eating disorders Adjustment disorder nursing diagnosis
Adjustment disorder nursing diagnosis Dissociative fugue
Dissociative fugue What is the nursing process steps
What is the nursing process steps Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Second phase of nursing process
Second phase of nursing process